Navigating the Methodological Landscape: A Comparative Study of Empirical Bioethics Approaches for Biomedical Research
This article provides a systematic comparison of empirical bioethics methodologies, tailored for researchers, scientists, and drug development professionals.
Navigating the Methodological Landscape: A Comparative Study of Empirical Bioethics Approaches for Biomedical Research
Abstract
This article provides a systematic comparison of empirical bioethics methodologies, tailored for researchers, scientists, and drug development professionals. It explores the foundational theories and historical context of the field, details specific methodological approaches for integrating empirical data with normative analysis, addresses common challenges and proposes solutions for rigorous research, and validates findings through established standards and emerging trends. The content synthesizes current scholarly consensus and empirical research to offer a practical guide for designing, implementing, and evaluating robust empirical bioethics studies in biomedical contexts.
Understanding the Empirical Bioethics Terrain: History, Definitions, and Core Debates
The field of bioethics has undergone a significant transformation over recent decades, marked by a pronounced "empirical turn" that integrates social science research methods into traditionally normative inquiry [1]. This shift represents a movement from abstract philosophical reasoning toward engaged research that addresses practical ethical questions in healthcare and medicine [1]. The empirical turn gained momentum due to several factors: dissatisfaction with the abstract nature of theoretical bioethics, increasing engagement with clinical ethics practice, and the growing prominence of evidence-based medicine in the 1990s [1].
Empirical bioethics can be understood as research that "collects and analyses empirical data" to inform bioethical questions [1]. This approach recognizes that ethical analysis must be grounded in the actual experiences, values, and contexts of those affected by biomedical advancements [2]. The fundamental role of empirical research in bioethics resides in its potential to "inform abstract principles into workable practices and its capacity to ensure that bioethicists are in touch with the actual experiences of those affected" [1]. This methodological evolution has created a vibrant interdisciplinary field that combines normative ethical analysis with empirical investigation of real-world ethical practices and challenges.
Quantitative Landscape: Measuring the Empirical Turn
Growth of Empirical Research in Bioethics Journals
The increasing dominance of empirical approaches in bioethics is clearly demonstrated through quantitative analysis of publications in leading journals. A comprehensive review of nine major bioethics journals from 2004 to 2015 provides compelling evidence of this trend [1].
Table 1: Empirical Publications in Bioethics Journals (2004-2015)
| Journal | Total Original Papers | Empirical Papers | Percentage Empirical | Dominant Methodology |
|---|---|---|---|---|
| Journal of Medical Ethics | 2,150 | 540 | 25.1% | Quantitative |
| Nursing Ethics | 1,023 | 360 | 35.2% | Qualitative |
| Bioethics | 587 | 45 | 7.7% | Mixed Methods |
| Cambridge Quarterly of Healthcare Ethics | 412 | 22 | 5.3% | Mixed Methods |
| Hastings Center Report | 478 | 18 | 3.8% | Qualitative |
| Theoretical Medicine and Bioethics | 392 | 12 | 3.1% | Mixed Methods |
| Journal of Clinical Ethics | 285 | 8 | 2.8% | Qualitative |
| Kennedy Institute of Ethics Journal | 140 | 1 | 0.7% | Qualitative |
| Christian Bioethics | 100 | 1 | 1.0% | Qualitative |
| Total/Average | 5,567 | 1,007 | 18.1% | Varies by Journal |
The data reveals that empirical work constituted 18.1% of all original publications across these nine bioethics journals during this period [1]. This represents a significant increase from the 1990-2003 period, when only 10.8% of articles used empirical designs [1]. The growing volume is mainly attributable to two journals: Journal of Medical Ethics and Nursing Ethics, which together accounted for 89.4% of all empirical papers published in these venues [1]. The analysis also reveals distinct methodological preferences, with Journal of Medical Ethics publishing significantly more quantitative papers, while Nursing Ethics favored qualitative approaches [1].
Expanding Scope of Empirical Bioethics
The empirical turn encompasses more than just a quantitative increase in publications; it represents a fundamental expansion of how bioethical inquiry is conducted. Empirical bioethics research now addresses a wide spectrum of objectives, from understanding the context of bioethical issues to developing and justifying moral principles [2]. A qualitative exploration of researchers' views identified a continuum of acceptable objectives for empirical research in bioethics (ERiB), ranging from modest to highly ambitious aims [2].
Table 2: Researcher Perspectives on Acceptable Objectives for Empirical Bioethics
| Objective | Acceptance Level | Key Rationales |
|---|---|---|
| Understanding the context of a bioethical issue | Unanimous agreement | Provides essential grounding for normative analysis |
| Identifying ethical issues in practice | Unanimous agreement | Reveals real-world ethical challenges |
| Describing stakeholder attitudes and behaviors | High agreement | Documents actual moral views and practices |
| Evaluating how ethical recommendations work in practice | High agreement | Tests implementation and practical impact |
| Informing policy development | Moderate agreement | Connects research to practical application |
| Recommending changes to specific ethical norms | Moderate agreement | Uses data to refine specific guidelines |
| Developing and justifying moral principles | Contested | Faces philosophical challenges (e.g., is-ought gap) |
| Using empirical research as a source of morality | Contested | Raises fundamental methodological concerns |
Researchers largely agreed that understanding context and identifying ethical issues in practice were fundamental objectives for empirical bioethics [2]. However, more ambitious goals—particularly using empirical research to develop and justify moral principles—generated significant debate [2]. The is-ought gap was not considered an absolute obstacle to ERiB, but rather "a warning sign to critically reflect on the normative implications of empirical results" [2].
Methodological Approaches: Comparative Analysis
Typology of Empirical Bioethics Methodologies
The field of empirical bioethics has developed diverse methodological approaches to integrate empirical research with normative analysis. These approaches vary in their epistemological foundations, methods of integration, and intended outcomes.
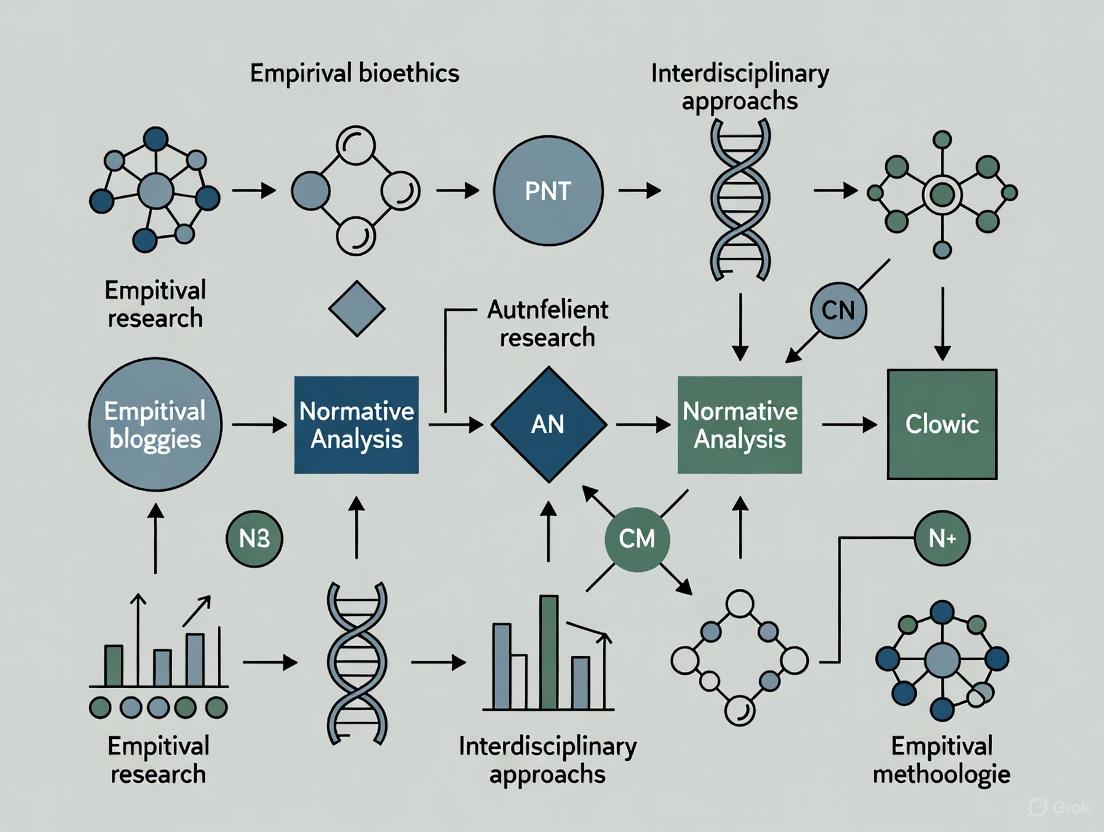
Diagram 1: Empirical Bioethics Methodological Approaches
The Principle-Based Empirically Grounded Roadmap Approach (PERA)
A recent methodological innovation in empirical bioethics is the Principle-Based Empirically Grounded Roadmap Approach (PERA), developed specifically for addressing ethical challenges in digital mental healthcare technologies [3]. PERA represents an advanced integrated methodology that responds to the unique characteristics of technology development contexts where the technological design is largely predetermined and features embedded co-development practices [3].
The PERA methodology involves three core components: (1) mapping principles from ethics literature, (2) conducting a scoping review of moral intuitions among technology developers, and (3) collecting original empirical data on specific use cases [3]. These elements are synthesized using abductive reasoning to produce a tangible output—an ethics roadmap designed to guide future iterations of the technology [3]. This approach advances empirical bioethics methodology by providing both practical tools for ethics researchers in technology projects and a means to generate empirically grounded conceptual contributions [3].
"Big Bioethics" and Large-Scale Approaches
A more recent development in the field is the emergence of "Big Bioethics," which leverages large-scale datasets to examine ethical questions [4]. This approach involves empirical bioethics research—often surveys or retrospective reviews of patient outcomes—that collect and analyze data from very large numbers of people, typically involving several thousand individuals [4]. Such studies have the statistical power to examine subtle differences in psychosocial and behavioral outcomes between subgroups, including historically underrepresented populations [4].
"Big Bioethics" represents a response to the increasing scale of translational research in healthcare and the growing availability of large datasets [4]. This approach enables researchers to identify atypical patient experiences and less common ethical perspectives that might go undetected in smaller qualitative studies [4]. However, the adoption of "Big Bioethics" also raises challenges, including the need for specialized methodological expertise and concerns about maintaining the field's commitment to understanding marginalized perspectives, which has traditionally been associated with qualitative approaches [4].
"Hidden" Empirical Bioethics
An important methodological consideration in empirical bioethics is the recognition that much ethically relevant empirical research remains "hidden" from the view of bioethicists [5]. Studies that provide data directly relevant to bioethical issues often appear in non-ethics journals, are published by professionals who do not identify as ethicists, and lack ethics-related keywords [5]. One analysis found that less than 50% of such articles discussed the ethical implications of their findings, and only a small minority contained keywords clearly related to research ethics [5].
This "hidden" empirical bioethics poses challenges for the field, as valuable data remains inaccessible to ethicists who may not encounter it through conventional literature searches in bioethics venues [5]. Addressing this problem requires encouraging researchers in other fields, editors, and database indexers to add ethics-related keywords when data are highly relevant to ethical debates, and training ethicists to search for relevant data using non-ethics terms [5].
Experimental Protocols and Research Reagents
Essential Methodological Tools for Empirical Bioethics
Conducting rigorous empirical bioethics research requires specific methodological approaches and tools. The field draws on diverse disciplinary traditions, each contributing essential research reagents to the interdisciplinary enterprise.
Table 3: Research Reagent Solutions for Empirical Bioethics
| Research Reagent | Function | Application Context |
|---|---|---|
| Qualitative Interview Protocols | Elicit detailed stakeholder perspectives | Understanding lived experience of ethical issues |
| Systematic Scoping Reviews | Map existing literature and identify gaps | Preliminary stage of PERA methodology |
| Validated Survey Instruments | Quantify attitudes, beliefs, behaviors | Large-scale "Big Bioethics" studies |
| Mixed-Methods Designs | Integrate qualitative and quantitative approaches | Comprehensive analysis of complex ethical issues |
| Abductive Reasoning Frameworks | Generate best explanations from incomplete data | PERA methodology for developing ethics roadmaps |
| Interdisciplinary Team Structures | Combine normative and empirical expertise | All integrated empirical bioethics research |
| Ethical Framework Analysis | Connect empirical findings to normative principles | Normative analysis of empirical data |
| Large-Scale Dataset Analytics | Identify patterns across diverse populations | "Big Bioethics" approaches with statistical power |
Integrated Research Workflow
The implementation of empirical bioethics research typically follows a structured workflow that integrates normative and empirical components throughout the research process. The following diagram illustrates this integrative approach:
Diagram 2: Empirical Bioethics Research Workflow
Current Debates and Future Directions
Methodological Tensions and Integration Challenges
The empirical turn in bioethics continues to generate important methodological debates regarding how empirical and normative dimensions should relate to one another. A central tension concerns the "is-ought" problem—the philosophical challenge of deriving normative conclusions from empirical facts [2]. While bioethicists generally agree that empirical research can inform ethical analysis, there is less consensus about how directly empirical findings should shape normative conclusions [2].
Researchers have proposed various approaches to integration, but "there is no consensus as to how this integration ought to manifest" [1]. Some scholars advocate for more ambitious integration, where empirical research directly contributes to developing and justifying moral principles [2]. Others maintain a more modest view, seeing empirical research as primarily providing context and identifying practical ethical issues without directly determining normative conclusions [2]. This tension reflects broader debates about the proper goals and methods of bioethics as an interdisciplinary field.
Emerging Trends and Training Initiatives
The field of empirical bioethics continues to evolve, with several emerging trends shaping its future direction. There is growing recognition of the need for "big bioethics" approaches that can keep pace with the scale of contemporary biomedical research [4]. Simultaneously, methodological innovation continues, as exemplified by the development of the PERA framework for digital mental health technologies [3].
Training initiatives have emerged to support the development of empirical bioethics expertise. The Empirical Bioethics Summer School, for instance, provides beginner/intermediate level training for researchers with some familiarity with empirical bioethics [6]. This four-day program covers key topics including: understanding what empirical bioethics is and exploring typologies; designing empirical bioethics research projects; methodological approaches to integration; and addressing challenges in the field [6]. Such training opportunities reflect the ongoing professionalization of empirical bioethics as a distinct subfield with its own methodologies, vocabulary, and standards of excellence.
The field also continues to grapple with practical challenges, including the inconsistent adoption of policies regarding artificial intelligence in bioethics publishing [7] and the need to ensure that empirical bioethics research maintains its commitment to giving voice to marginalized perspectives while embracing new methodological opportunities [4]. As empirical bioethics matures, these debates and innovations will likely continue to shape its development as an interdisciplinary field that bridges the normative and the empirical.
The Social Science Critique: Challenging the Foundations of Traditional Bioethics
The emergence of empirical bioethics in the early 21st century represented a direct response to mounting criticism from social scientists who questioned the foundations and methodology of traditional philosophical bioethics. This critique fundamentally challenged bioethics' self-understanding and its approach to real-world ethical problems.
Social scientists argued that traditional bioethics suffered from several critical limitations. It often privileged idealized, rational thought while tending to exclude or marginalize social and cultural factors, treating them as irrelevant to ethical analysis [8]. This approach resulted in ethical frameworks that were abstract and disconnected from the lived moral experiences of patients, families, and healthcare professionals [8] [9]. Furthermore, traditional bioethics implicitly assumed that social reality divided neatly along the same categories as philosophical theories, failing to recognize the complex, contextual nature of moral problems in healthcare settings [8].
This critique demanded a fundamental reorientation of bioethical inquiry—one that would root ethical analyses in the empirical reality of healthcare practices and moral experiences [8]. The call was for bioethics to become more self-critical, skeptical of claims made by scientists and clinicians, and rigorously engaged with the actual contexts in which ethical dilemmas arise [8]. This foundational critique set the stage for the development of more empirically-grounded approaches to bioethics.
The Empirical Turn: Quantitative Evidence of a Shifting Field
The theoretical critique of traditional bioethics coincided with a measurable shift in publication patterns within leading bioethics journals. Empirical research began to claim an increasingly significant place in bioethical scholarship, marking what came to be known as "the empirical turn" in bioethics [10] [9].
Table 1: Growth of Empirical Research in Bioethics Journals (1990-2003)
| Time Period | Total Publications | Empirical Studies | Percentage |
|---|---|---|---|
| 1990-1996 | 1,857 | 126 | 6.8% |
| 1997-2003 | 2,172 | 309 | 14.2% |
| Overall (1990-2003) | 4,029 | 435 | 10.8% |
Source: Borry et al. (2006) analysis of nine peer-reviewed bioethics journals [10]
This quantitative analysis of nine major bioethics journals revealed a statistically significant increase (χ² = 49.0264, p<.0001) in empirical research publications between 1990 and 2003 [10]. The proportion of empirical studies grew from just 5.4% in 1990 to 15.4% in 2003, demonstrating a clear trend toward empirical approaches [10]. The distribution of this research was uneven across journals, with Nursing Ethics (39.5%), Journal of Medical Ethics (16.8%), and Journal of Clinical Ethics (15.4%) publishing the highest percentages of empirical studies [10].
Methodologically, early empirical bioethics was dominated by quantitative approaches (64.6%), though qualitative methods were also recognized as particularly valuable for understanding values, personal perspectives, and contextual circumstances [10]. The main topics of empirical research reflected pressing clinical concerns, with prolongation of life and euthanasia being the most frequently studied subject [10].
Classifying Empirical Bioethics Research: A Hierarchical Framework
As empirical bioethics developed, scholars proposed various frameworks to categorize and understand the diverse ways in which empirical research could contribute to bioethical inquiry. One influential framework proposed four hierarchical categories that represent increasing levels of normative ambition [11].
Table 2: Hierarchy of Empirical Bioethics Research
| Category | Primary Question | Examples | Methodologies |
|---|---|---|---|
| Lay of the Land | "What are current practices, opinions, or beliefs?" | Attitudes toward end-of-life care; Ethics committee composition surveys [11] | Quantitative surveys; Qualitative interviews |
| Ideal vs. Reality | "How well does practice match our ethical ideals?" | Racial disparities in healthcare; Informed consent comprehension studies [11] | Comparative analysis; Outcome studies |
| Improving Care | "How can we bring practice closer to ethical ideals?" | Interventions to reduce disparities; Consent process improvements [11] | Intervention studies; Quality improvement research |
| Changing Ethical Norms | "Should our ethical ideals change based on evidence?" | Using multiple empirical studies to question existing norms [11] | Synthesis of multiple empirical studies |
This framework demonstrates how empirical research in bioethics ranges from primarily descriptive studies that map the current ethical landscape to more ambitious normative projects that seek to refine or revise ethical norms based on empirical findings [11]. The hierarchy reflects increasing complexity in the relationship between empirical data and normative conclusions, with the highest level involving the use of cumulative empirical evidence to potentially transform ethical frameworks themselves.
Researcher Perspectives on Appropriate Objectives
A recent qualitative study exploring the views of bioethics researchers themselves reveals how those actively working in the field perceive the appropriate objectives for empirical bioethics research [2]. This research provides crucial insight into how the theoretical debate about empirical bioethics has been internalized and interpreted by practicing scholars.
Researchers expressed strongest agreement with objectives focused on "understanding the context of a bioethical issue" and "identifying ethical issues in practice" [2]. These objectives were seen as relatively uncontroversial and clearly valuable. More ambitious objectives—particularly "striving to draw normative recommendations" and "developing and justifying moral principles"—generated significantly more disagreement and debate among researchers [2].
The classical philosophical problem of the is-ought gap (the challenge of deriving normative conclusions from purely descriptive premises) was not generally seen as an insurmountable barrier to empirical bioethics [2]. Rather, researchers treated it as an important caution—a reason to engage in critical reflection about the normative implications of empirical results [2]. There was recognition that while empirical data alone cannot determine ethical conclusions, it can provide an essential "testing ground" for elements of normative theory [2].
Methodological Approaches: From Multi-Disciplinarity to Interdisciplinarity
The development of empirical bioethics has involved ongoing methodological innovation and reflection. Early approaches often simply combined empirical methods with ethical analysis, but more sophisticated methodologies have emerged that seek to truly integrate empirical and normative approaches [9].
Key Methodological Frameworks
Reflexive Balancing: This approach, proposed by Ives (2014), emphasizes the need for continuous reflection and adjustment between empirical findings and normative frameworks [9]. It acknowledges that both empirical research and ethical analysis require iterative refinement when brought into conversation with each other.
Critical Bioethics: Building on the social science critique, this approach maintains skepticism toward claims made by scientists and clinicians while insisting that ethical analyses must be rooted in empirical research [8]. It aims to produce "rigorous normative analysis of lived moral experience" rather than abstract ethical theorizing [8].
Feminist Epistemologies: These approaches actively resist strict divisions between empirical and normative inquiry, treating them as co-constitutive and intertwined [9]. This perspective has made significant contributions to empirical bioethics theory and methodology by challenging binary thinking about facts and values [9].
Experimental Protocol Template for Empirical Bioethics
Recent methodological development has focused on creating standardized approaches to empirical bioethics research. One team has formalized a protocol template suitable for all types of humanities and social sciences investigations in health, including empirical bioethics [12]. This template adapts and modifies the "Standards for Reporting Qualitative Research (SRQR)" to render it suitable for quantitative, qualitative, and mixed-method approaches in bioethics [12]. The template helps researchers structure their inquiries to ensure both empirical rigor and normative relevance.
Research Reagent Solutions: Essential Methodological Tools
Conducting rigorous empirical bioethics research requires specific methodological "reagents" – essential approaches and tools that facilitate the integration of empirical and normative analysis.
Table 3: Essential Methodological Tools for Empirical Bioethics Research
| Tool | Function | Application Example |
|---|---|---|
| Qualitative Interview Protocols | Explore lived experiences and moral reasoning of stakeholders | Understanding patient experiences in clinical trials as treatment [13] |
| Standardized Protocol Templates | Ensure methodological rigor and comprehensive reporting | Health research protocols template for empirical bioethics [12] |
| Mixed-Method Research Designs | Combine quantitative and qualitative approaches for comprehensive understanding | Studying both prevalence and experiences of ethical issues [10] [2] |
| Reflexive Balancing Framework | Systematically navigate between empirical findings and normative theory | Methodological approach for interdisciplinary bioethics [9] |
| Empirical Bioethics Taxonomy | Classify different types and purposes of empirical bioethics research | Categorizing studies from descriptive to normative [11] |
Signaling Pathways: The Logical Structure of Empirical Bioethics
The following diagram illustrates the conceptual pathway through which the social science critique transformed traditional bioethics and stimulated the development of empirical approaches.
Conceptual Pathway from Critique to Empirical Bioethics
Current Applications and Future Directions
Empirical bioethics continues to evolve and address emerging ethical challenges in healthcare and biotechnology. Its approaches are particularly valuable for navigating novel ethical terrain where traditional ethical frameworks provide limited guidance.
Application to Emerging Technologies
The ongoing development of organ-on-a-chip technology demonstrates how empirical bioethics approaches are applied to emerging biotechnologies [14]. These microdevices that emulate human organs using human cells present novel ethical questions that benefit from empirically-informed analysis. Research in this area examines ethical considerations related to informed consent, community engagement, and personalized medicine models using patient-derived cells [14]. These analyses draw on empirical data about public attitudes, stakeholder perspectives, and actual laboratory practices to develop ethically robust guidance.
Interdisciplinary Integration
The future of empirical bioethics appears to be moving toward deeper interdisciplinary integration rather than simple multidisciplinary cooperation [9]. This involves dissolving the traditional empirical/normative divide and developing approaches that treat facts and values as co-constitutive rather than separate domains [9]. This deeper integration requires researchers to develop collaborative relationships that enable interdisciplinary critique and methodological innovation [9].
The field continues to grapple with challenges of methodological rigor and epistemic authority when working across traditional disciplinary boundaries [9]. However, the continued development of specialized training opportunities, such as the Empirical Bioethics Summer School [6], indicates the ongoing institutionalization and professionalization of this interdisciplinary field.
The emergence and development of empirical bioethics represents a fundamental transformation in how bioethics conceptualizes its subject matter and methodologies. Arising in response to powerful social science critiques of traditional approaches, empirical bioethics has established itself as a rigorous interdisciplinary field that systematically integrates empirical research with normative analysis. While tensions remain between different epistemological approaches and disciplinary orientations, the field has developed sophisticated methodologies and conceptual frameworks for addressing complex ethical problems in healthcare and biotechnology. As novel ethical challenges continue to emerge in biomedical research and clinical practice, empirical bioethics provides essential tools for developing ethically robust, empirically-informed responses.
Empirical bioethics has emerged as a critical interdisciplinary field that bridges philosophical inquiry with social science research methods to address complex ethical questions in healthcare and medicine. This field underwent a significant 'empirical turn' several decades ago in response to critiques that traditional bioethics had failed to adequately account for social context and lived experience [15]. Within this evolved landscape, two distinct methodological approaches have gained prominence: the consultative approach and the dialogical approach. These methodologies represent different poles on a spectrum of how empirical data and ethical analysis are integrated, each with distinct philosophical foundations, research processes, and applications. Understanding this spectrum is essential for researchers, scientists, and drug development professionals who must navigate methodological choices in addressing ethical challenges in healthcare innovation and clinical practice.
The consultative approach typically treats empirical data as input for ethical analysis conducted primarily by researchers, while the dialogical approach emphasizes mutual understanding and co-construction of knowledge through dialogue between researchers and participants [16]. As the field continues to evolve, some scholars are now advocating for a 'theoretical turn' that encourages more deliberate integration of empirical research with philosophical theory [15]. This comparative guide examines these methodological poles through their theoretical foundations, practical applications, and relative strengths, providing researchers with evidence-based guidance for methodological selection in empirical bioethics research.
Theoretical Foundations and Definitions
Consultative Approach
The consultative approach represents a more traditional model of empirical bioethics where researchers primarily maintain control over the ethical analysis while consulting stakeholders for their perspectives and experiences. This method is characterized by a sequential process where data collection precedes ethical analysis, with researchers acting as the primary interpreters of empirical findings. The approach is grounded in the assumption that while stakeholder experiences provide crucial contextual information, the specialized training of ethicists is necessary for rigorous normative analysis.
In consultative methodology, empirical data serves as a testing ground for elements of normative theory [2]. Researchers identify ethical issues in practice and understand the context of bioethical issues through engagement with stakeholders, but retain authority over the final ethical analysis and recommendations. This approach aligns with what some have termed "the handmaiden model," where social science methods serve to document facts that ethicists then use in their normative arguments [2]. The consultative approach is particularly prevalent in research aiming to develop evidence-based policy recommendations or clinical guidelines where researcher expertise drives the normative conclusions.
Dialogical Approach
The dialogical approach represents a more integrated methodology that emphasizes mutual understanding achieved through collaboration rather than shared understanding imposed by researchers [16]. Rooted in dialogical self-theory and narrative approaches, this methodology conceptualizes knowledge as co-created through dialogue between different perspectives [16] [17]. Unlike the consultative approach, dialogical methods treat participants as active collaborators in the ethical analysis rather than merely as sources of data.
The philosophical foundations of the dialogical approach draw from Bakhtinian dialogism, which views knowledge as emerging through genuine dialogue between different voices and perspectives [16] [17]. This approach produces knowledge that is pluralistic and multivocal, intentionally including underrepresented voices that might be silenced in traditional methodologies [16]. In practice, dialogical bioethics involves creating spaces where diverse stakeholders (patients, clinicians, researchers) engage in structured dialogue about ethical questions, with the research outcomes emerging from these interactions rather than being determined solely by researcher analysis.
Table: Theoretical Foundations of Consultative and Dialogical Approaches
| Dimension | Consultative Approach | Dialogical Approach |
|---|---|---|
| Epistemology | Knowledge derived from expert analysis of stakeholder data | Knowledge co-constructed through dialogue between multiple perspectives |
| Researcher Role | Expert analyst who maintains control over ethical reasoning | Facilitator and participant in collaborative meaning-making |
| Participant Role | Sources of empirical data about experiences and values | Active collaborators in ethical reflection and analysis |
| Primary Strength | Clear normative conclusions based on ethical expertise | Inclusion of diverse voices and contextual understanding |
| Integration Method | Sequential: empirical data collection followed by ethical analysis | Concurrent: ethical analysis emerges through dialogical process |
Comparative Analysis of Methodological Characteristics
Research Processes and Integration Methods
The consultative and dialogical approaches differ significantly in their research processes, particularly in how they integrate empirical and normative elements. Consultative methodologies typically employ a linear sequence where empirical data collection precedes ethical analysis. For example, researchers might conduct interviews or surveys to gather stakeholder perspectives on an ethical issue, then analyze this data using philosophical frameworks independently of the participants [2]. This separation of data collection from ethical analysis allows for methodological clarity but risks imposing external theoretical frameworks on participant experiences.
Dialogical approaches employ an integrative process where empirical and normative elements interweave throughout the research. These methodologies create spaces for what is termed "therapeutic conversations" that transcend linear intervention models [17]. In practice, this might involve facilitated dialogues where patients, clinicians, and ethicists collaboratively explore ethical questions, with insights emerging through the dialogical process itself. The integration occurs in real-time through what is described as "self-reflexive dialogue" and "dialogue between the researcher and others" including interviewees, supervisors, and collaborators [16]. This process values the unique perspectives each participant brings to understanding complex phenomena.
Applications in Healthcare and Research Contexts
Both methodological approaches have distinct applications across healthcare and research contexts, with each offering particular advantages for different research questions and settings. Consultative approaches have proven valuable in contexts requiring clear normative guidance or policy development, such as establishing guidelines for ethical research protocols [12]. The structured nature of consultative methodology lends itself well to producing actionable recommendations for institutional ethics committees or clinical practice guidelines.
Dialogical approaches excel in contexts requiring deep understanding of diverse perspectives and ethical complexities, such as person-centered care in acute settings [18] or cross-cultural healthcare relationships [19]. These methods have been successfully applied in mental health contexts, where the exploration of patient experiences and values benefits from collaborative meaning-making [17] [19]. The emphasis on mutual understanding makes dialogical approaches particularly suitable for exploring contested ethical terrain where multiple legitimate perspectives exist, such as in cross-cultural research or community engagement initiatives.
Table: Methodological Applications and Outputs
| Research Context | Consultative Approach Applications | Dialogical Approach Applications |
|---|---|---|
| Clinical Ethics | Development of clinical guidelines and protocols | Understanding patient experiences of moral dilemmas |
| Research Ethics | Protocol review and compliance assessment | Stakeholder engagement in ethical governance |
| Mental Health | Analysis of ethical issues in treatment practices | Collaborative exploration of therapeutic relationships |
| Cross-Cultural Settings | Identifying cultural variations in ethical attitudes | Facilitating mutual understanding across differences |
| Policy Development | Evidence-based policy recommendations | Inclusive deliberation processes |
Experimental Protocols and Research Designs
Protocol Template for Empirical Bioethics Research
Recent methodological advances have produced formalized protocol templates suitable for various humanities and social sciences investigations in health, including empirical bioethics. These templates build upon the Standards for Reporting Qualitative Research (SRQR) but have been adapted to overcome limitations of being restricted to qualitative approaches [12]. The refined template is equally suitable for quantitative, mixed-method, and integrated approaches, serving as a highly adaptable base for empirical bioethics research regardless of methodological orientation.
The standardized protocol includes several key components: (1) clear articulation of the ethical question and its practical significance; (2) methodological approach and justification; (3) data collection procedures; (4) integration strategy for empirical and normative elements; (5) analysis framework; and (6) dissemination plan. For consultative approaches, the protocol typically specifies separate sections for empirical data collection and ethical analysis, while dialogical approaches describe facilitated dialogue processes and collaborative analysis methods [12]. This protocol standardization enhances methodological rigor while allowing flexibility for different epistemological orientations.
Data Collection and Analysis Procedures
The consultative and dialogical approaches employ distinct data collection and analysis procedures reflecting their different epistemological commitments. Consultative methodologies often utilize structured interviews, surveys, or document analysis to gather data about stakeholder experiences and values [2]. Analysis typically involves thematic analysis of empirical data followed by application of ethical frameworks by researcher experts. This separation allows for clear methodological demarcation but risks disconnecting ethical analysis from lived experiences.
Dialogical approaches employ facilitated dialogues, group discussions, or narrative exchanges that simultaneously generate data and facilitate ethical reflection [16] [17]. Analysis focuses on understanding the evolution of perspectives through dialogue and identifying insights that emerge through collaborative exchange. Rather than applying predetermined ethical frameworks, dialogical analysis seeks to identify how ethical understanding develops through multivocal engagement. These procedures have been refined through empirical bioethics training programs that specifically teach dialogical integration methodologies [6] [18].
Research Reagents and Methodological Tools
Essential Research Solutions for Empirical Bioethics
Conducting rigorous empirical bioethics research requires specific methodological "reagents" and tools that facilitate data collection, analysis, and integration of empirical and normative elements. These tools differ significantly between consultative and dialogical approaches, reflecting their distinct epistemological commitments and research processes.
Table: Essential Methodological Tools for Empirical Bioethics Research
| Tool Category | Consultative Approach Tools | Dialogical Approach Tools | Function and Application |
|---|---|---|---|
| Data Collection Instruments | Structured interview protocols; Survey questionnaires; Data extraction forms | Dialogue facilitation guides; Narrative elicitation techniques; Group process protocols | Gather empirical data about ethical issues (consultative) or create conditions for collaborative dialogue (dialogical) |
| Analysis Frameworks | Thematic analysis coding schemes; Ethical framework application tools; Normative analysis templates | Dialogical content analysis; Polyvocal interpretation methods; Position exchange mapping | Analyze empirical data (consultative) or interpret dialogical exchanges (dialogical) |
| Integration Methodologies | Sequential integration protocols; Empirical data mapping to ethical concepts; Normative recommendation development | Reciprocal elucidation processes; Mutual understanding facilitation; Collaborative meaning-making techniques | Connect empirical findings with ethical analysis through researcher mediation (consultative) or stakeholder collaboration (dialogical) |
| Validation Methods | Member checking; Peer debriefing; Theoretical triangulation | Dialogical validation; Stakeholder resonance assessment; Process authenticity verification | Ensure trustworthiness of findings through methodological rigor (consultative) or dialogical authenticity (dialogical) |
Comparative Performance and Outcomes
Empirical Evidence and Research Findings
The comparative performance of consultative and dialogical approaches can be evaluated through their application in various research contexts and the distinct outcomes they generate. Research indicates that consultative approaches are particularly effective for producing clear normative guidance and actionable recommendations for specific ethical dilemmas [2]. Studies using consultative methodologies have successfully identified ethical issues in clinical practice and developed context-sensitive guidelines for complex healthcare scenarios. The strength of these approaches lies in their ability to leverage ethical expertise while being informed by stakeholder experiences.
Dialogical approaches demonstrate particular strength in generating rich contextual understanding and inclusive ethical insights that incorporate diverse perspectives. Studies employing dialogical methods have revealed nuanced understandings of ethical issues in clinical relationships [19] and mental health care [17]. For example, research on online health communities revealed significant cross-cultural differences in how patients express concerns and how professionals respond, with Italian patients using more indirect and polite forms while Polish patients employed a more direct style [19]. These culturally nuanced understandings emerged through dialogical engagement with diverse participant voices.
Methodological Strengths and Limitations
Each methodological approach presents distinct strengths and limitations that make them suitable for different research questions and contexts. Consultative approaches offer methodological clarity, efficiency in analysis, and clear attribution of normative authority. These strengths make them valuable for policy development and time-sensitive ethical analysis. However, they risk imposing external frameworks on participant experiences and may miss important nuances embedded in diverse perspectives [2].
Dialogical approaches excel in including marginalized voices, generating mutual understanding, and revealing unexpected insights through collaborative exchange. These methods are particularly valuable for exploring complex ethical terrain where multiple legitimate perspectives exist. However, they can be methodologically demanding, time-intensive, and may produce less definitive normative guidance [16]. The choice between approaches ultimately depends on research questions, resources, and whether the primary goal is definitive normative guidance or deep understanding of multiple perspectives.
Table: Performance Comparison Across Methodological Criteria
| Evaluation Criteria | Consultative Approach | Dialogical Approach |
|---|---|---|
| Normative Clarity | High - produces clear ethical recommendations | Variable - may generate multiple legitimate perspectives |
| Stakeholder Inclusion | Moderate - includes voices as data sources | High - active collaboration in ethical analysis |
| Methodological Transparency | High - clear separation of empirical and normative elements | Moderate - integrated process can be complex to document |
| Cross-Cultural Sensitivity | Variable - risks imposing dominant ethical frameworks | High - designed to accommodate diverse perspectives |
| Practical Applicability | High - produces actionable recommendations | Variable - insights may require further translation |
The consultative and dialogical approaches represent distinct but complementary poles on the methodological spectrum of empirical bioethics. Rather than positioning these approaches as mutually exclusive, researchers are increasingly recognizing the value of methodological pluralism that selects approaches based on specific research questions, contexts, and goals. The ongoing evolution of empirical bioethics suggests a growing emphasis on deliberate integration of empirical and theoretical elements, with some scholars advocating for a 'theoretical turn' that strengthens engagement with philosophical theory while maintaining robust empirical foundations [15].
For researchers, scientists, and drug development professionals, understanding this methodological spectrum enables more informed choices about research design. Consultative approaches offer efficiency and normative clarity for contexts requiring definitive guidance, while dialogical approaches provide depth and inclusion for exploring complex ethical terrain. Future methodological development will likely focus on refined integration techniques and hybrid approaches that leverage the strengths of both poles while mitigating their limitations. As empirical bioethics continues to mature, this methodological sophistication will enhance its contribution to addressing pressing ethical challenges in healthcare innovation and practice.
Empirical bioethics emerged as a response to the perception that purely philosophical approaches were insufficient to address the complexity of real-world bioethical issues [20]. This interdisciplinary field seeks to integrate empirical data about stakeholder values, attitudes, and experiences with normative ethical theorizing [21]. Despite decades of methodological development, fundamental philosophical tensions persist regarding how to bridge the descriptive "is" of empirical research with the normative "ought" of ethical prescriptions [2]. This comparison guide examines the current landscape of empirical bioethics methodologies, their philosophical underpinnings, and their capacity to generate justified normative conclusions.
Comparative Analysis of Empirical Bioethics Approaches
A systematic review of the field identified 32 distinct methodological approaches for integrating empirical research with normative analysis [21]. These can be broadly categorized into three main types based on their structure and philosophical commitments.
Table 1: Typology of Empirical Bioethics Methodologies
| Methodological Category | Philosophical Orientation | Locus of Moral Authority | Key Characteristics | Primary Limitations |
|---|---|---|---|---|
| Consultative Approaches (e.g., Reflective Equilibrium) | Coherentist epistemology | Researcher as independent thinker | Researcher conducts back-and-forth reflection between empirical data and ethical principles until moral coherence is achieved [20] | Process often described as vague; weight given to empirical data versus theory remains unclear [20] |
| Dialogical Approaches (e.g., Inter-ethics) | Deliberative democratic | Stakeholders in dialogue | Relies on dialogue between researchers and participants to reach shared understanding and normative conclusions [21] [20] | Application of ethical theories may depend on facilitator's subjective judgment [20] |
| Inherent Integration Approaches | Pragmatist | Practice and experience | Normative and empirical dimensions are intertwined from the project's inception rather than combined sequentially [20] | Lack of clear methodological steps may raise questions about justification of conclusions |
Hierarchical Framework for Empirical Research in Bioethics
Beyond methodological typologies, empirical research contributes to bioethics at different levels of normative significance. One framework classifies these contributions into four hierarchical categories, from descriptive to normative.
Table 2: Four-Level Hierarchy of Empirical Research in Bioethics
| Level | Primary Research Question | Example Studies | Normative Significance |
|---|---|---|---|
| 1. Lay of the Land | "What are current practices, opinions, or beliefs?" | Studies of ethics committee composition; surveys of end-of-life care attitudes [11] | Descriptive foundation; informs decision-making without direct normative claims |
| 2. Ideal Versus Reality | "To what extent does practice align with ethical ideals?" | Research on disparities in healthcare delivery; studies of informed consent comprehension [11] | Identifies ethical shortcomings in current practice; demonstrates need for improvement |
| 3. Improving Care | "How can we bring practice closer to ethical ideals?" | Interventions to reduce healthcare disparities; programs to improve informed consent processes [11] | Develops and tests practical strategies to implement ethical norms |
| 4. Changing Ethical Norms | "Should our ethical frameworks evolve based on empirical findings?" | Syntheses of multiple empirical studies to challenge or refine ethical principles [11] | Uses cumulative empirical evidence to propose modifications to ethical theory |
Researcher Perspectives on Methodological Implementation
Recent qualitative research exploring bioethics scholars' experiences reveals both consensus and contention regarding appropriate objectives for empirical bioethics research.
Researcher Consensus and Debate on Objectives
Qualitative exploration with researchers conducting empirical bioethics reveals varying levels of acceptance for different research objectives [2]:
Universally Accepted Objectives:
- Understanding the context of a bioethical issue
- Identifying ethical issues in practice
Contentious Objectives:
- Striving to draw normative recommendations
- Developing and justifying moral principles
The is-ought gap was not considered an insurmountable obstacle by most researchers but rather a warning sign prompting critical reflection on the normative implications of empirical results [2]. The potential of empirical research to be useful for bioethics was mostly based on the reasoning pattern that empirical data can provide a testing ground for elements of normative theory [2].
Methodological Protocols in Empirical Bioethics
Reflective Equilibrium Protocol
The most familiar consultative method, reflective equilibrium, follows this systematic protocol [20]:
- Initial Position Mapping: Identify preliminary moral intuitions about the case
- Theory Examination: Consider relevant ethical principles and theories
- Empirical Data Integration: Incorporate empirical findings about stakeholder experiences, attitudes, or practices
- Coherence Seeking: Engage in iterative reflection to align moral intuitions, principles, and empirical observations
- Equilibrium Achievement: Reach a state of reflective coherence where all elements support a normative position
Dialogical Integration Protocol
Dialogical approaches employ a different methodological structure [21] [20]:
- Stakeholder Identification: Recruit diverse participants with relevant perspectives and experiences
- Structured Deliberation: Facilitate dialogue using established deliberative techniques
- Ethical Framework Introduction: Introduce ethical concepts to enrich discussion without predetermined conclusions
- Shared Understanding Development: Collaboratively develop moral perspectives through exchange
- Normative Conclusion Formulation: Arrive at justified normative positions through collective reasoning
Essential Research Reagents for Empirical Bioethics
Unlike laboratory sciences, empirical bioethics relies on methodological and analytical tools rather than physical reagents.
Table 3: Essential Methodological Reagents for Empirical Bioethics Research
| Research Reagent | Function | Examples of Application |
|---|---|---|
| Qualitative Interview Protocols | Elicit rich, nuanced data about moral experiences and reasoning | Exploring how patients conceptualize autonomy in clinical decision-making [2] |
| Deliberative Dialogue Frameworks | Structure stakeholder discussions to generate morally justified outcomes | Facilitating conversations between clinicians, patients, and policymakers on resource allocation [20] |
| Normative-Analytical Templates | Systematically trace relationships between empirical findings and ethical principles | Mapping how facts about cultural variations in truth-telling inform norms of disclosure [11] |
| Reflective Equilibrium Worksheets | Document the iterative process of achieving coherence between data and theory | Tracking how initial intuitions about disability evolve after engagement with empirical evidence [20] |
| Integration Methodologies | Explicit frameworks for combining empirical and normative analysis (e.g., symbiotic ethics, grounded moral analysis) [20] | Providing structured approaches to ensure empirical data properly informs normative conclusions |
Current Challenges and Future Directions
Despite methodological proliferation, researchers report ongoing challenges with integration, describing their processes with "an air of uncertainty and overall vagueness" [20]. This indeterminacy represents a double-edged sword—allowing flexibility while potentially obscuring insufficient methodological understanding.
The most significant tension remains between researchers who view empirical data as primarily illuminating context and those who advocate for its capacity to directly inform normative recommendations [2]. This divide reflects deeper philosophical disagreements about moral justification that play out within bioethical methodology [21].
Future methodological development must address the need for both conceptual clarity and practical applicability, enabling researchers to navigate the fundamental tension between descriptive and normative claims while producing work that meaningfully contributes to resolving pressing bioethical dilemmas in healthcare and research.
Empirical bioethics is an interdisciplinary field that integrates empirical findings from the social sciences with normative, philosophical analysis to address practical issues in healthcare, medicine, and research [20] [22]. This integration aims to address the complexity of human practices more effectively than purely philosophical approaches alone [20]. Despite general agreement that empirical research is relevant to bioethical argument, significant methodological diversity exists regarding how to classify research aims and integrate empirical data with normative analysis [23] [20] [2]. This guide provides a comparative analysis of the predominant typologies used to classify research aims in empirical bioethics, from merely describing attitudes toward the more ambitious goal of changing ethical norms, offering researchers a structured overview of the methodological landscape.
A central challenge in this field is the is-ought gap, a philosophical problem highlighting the difficulty of deriving ethical prescriptions (what "ought" to be) solely from empirical facts (what "is") [24] [2] [25]. Despite this challenge, empirical research is widely recognized as crucial for illuminating the context of ethical issues, testing the practical application of norms, and informing the development of ethical recommendations [2] [11] [25]. The typologies discussed below represent different ways scholars have organized these varied aims into a coherent framework.
Comparative Framework of Research Aims
Kon's Hierarchical Framework of Empirical Research
One influential classification, proposed by Kon, organizes empirical research in bioethics into a four-level hierarchy that increases in normative ambition [11]. This framework is instrumental for understanding how different research questions contribute to the field, with each level building upon the knowledge generated by the previous one.
The table below summarizes this hierarchical model:
Table 1: Kon's Hierarchical Framework of Empirical Research in Bioethics
| Category | Primary Research Question | Example | Normative Ambition |
|---|---|---|---|
| Lay of the Land | "What are current practices, opinions, or beliefs?" | Studies surveying the attitudes of physicians, patients, or ethics committee members on a specific issue [11]. | Low |
| Ideal Versus Reality | "To what extent does clinical practice match ethical ideals?" | Research documenting disparities in healthcare provision across different racial or ethnic groups [11]. | Low to Medium |
| Improving Care | "How can we bring practice closer to ethical ideals?" | Interventions or programs designed to improve the process of informed consent for clinical research [11]. | Medium |
| Changing Ethical Norms | "Should our ethical ideals be revised based on empirical data?" | Using aggregated empirical findings to argue for a change in specific ethical norms or guidelines [11]. | High |
Categorical Objectives of Empirical Research
Complementing Kon's hierarchical model, other scholars have proposed a list of distinct objectives for Empirical Research in Bioethics (ERiB). A qualitative study exploring the acceptability of these objectives among bioethics researchers found varying levels of support, revealing a clear preference for more modest aims [2] [25].
The continuum of objectives, from least to most ambitious, along with researcher agreement, is detailed below:
Table 2: Researcher Agreement on Objectives of Empirical Bioethics Research
| Research Objective | Description | Level of Ambition | Researcher Agreement |
|---|---|---|---|
| Understanding Context | Exploring the context and reality of a bioethical issue [2]. | Low | Unanimous agreement [2] [25]. |
| Identifying Ethical Issues | Pinpointing ethical problems as they manifest in practice [2]. | Low | Unanimous agreement [2] [25]. |
| Informing Applied Ethics | Providing data to enrich the application of ethical principles in specific settings [2]. | Medium | Supported, with varying degrees of agreement [2] [25]. |
| Testing Ethical Theory | Examining the validity of concepts, principles, or theories in real-world settings [2]. | Medium | Supported, with varying degrees of agreement [2] [25]. |
| Evaluating Interventions | Assessing how an ethical recommendation or intervention plays out in practice [2] [25]. | Medium | Supported, with varying degrees of agreement [2] [25]. |
| Drawing Normative Recommendations | Using empirical data to suggest changes to specific ethical norms or practices [2]. | High | The most contested objective [2] [25]. |
| Developing/Justifying Moral Principles | Using empirical research to contribute to the development or justification of general moral principles [2]. | High | The most contested objective [2] [25]. |
Methodological Approaches for Integration
A systematic review identified 32 distinct methodologies for integrating empirical research with normative analysis in bioethics, which can be broadly categorized by their underlying philosophical commitments and analytical processes [23]. Understanding these methodologies is crucial for selecting the right approach to match a study's aims.
Dialogical and Consultative Methodologies
The majority of integrative methodologies can be classified as either dialogical or consultative, which represent two different orientations toward how normative conclusions are reached [23].
Table 3: Core Methodological Approaches in Empirical Bioethics
| Methodology | Description | Key Feature | Example Methods |
|---|---|---|---|
| Consultative | The researcher analyzes empirical data independently as an external thinker to develop a normative conclusion [23] [20]. | Researcher-driven analysis | Reflective Equilibrium, Reflexive Balancing [23] [20]. |
| Dialogical | Relies on structured dialogue among stakeholders (e.g., researchers, participants) to reach a shared understanding and normative conclusion [23] [20]. | Collaborative, process-driven analysis | Inter-ethics, Dialogical Empirical Ethics [23] [20]. |
The Reflective Equilibrium Method
One prominent consultative method is Reflective Equilibrium, a process tailored for empirical bioethics projects [20]. It is a two-way dialogue between ethical principles, values, and empirical data (often from the researcher's own study) [20]. The researcher, or "the thinker," moves back and forth between the normative underpinnings and the empirical facts until a state of moral coherence, or "equilibrium," is produced [20]. The workflow of this iterative process is visualized below.
Key Research Reagents for Empirical Bioethics
Executing a rigorous empirical bioethics study requires specific methodological "reagents" or tools. The table below details essential components for designing and implementing such research, explaining the function of each.
Table 4: Essential Research Reagents for Empirical Bioethics Studies
| Research Reagent | Function & Purpose | Example Application |
|---|---|---|
| Semi-Structured Interviews | To gather rich, qualitative data on participants' experiences, moral reasoning, and views on a bioethical issue. | Exploring how clinicians experience and navigate ethical dilemmas in end-of-life care [20]. |
| Systematic Literature Reviews | To synthesize existing empirical data from a wide range of sources, forming a comprehensive evidence base for normative analysis. | Reviewing clinical evidence on tube feeding outcomes in patients with advanced dementia to inform ethical debates [5]. |
| Dialogical Workshops | To facilitate structured, collaborative discourse among stakeholders, enabling the co-creation of normative insights. | Bringing together patients, researchers, and ethicists to develop guidelines for a contentious clinical practice [23] [20]. |
| Qualitative Coding & Thematic Analysis | To systematically identify, analyze, and report patterns (themes) within qualitative data, linking empirical findings to ethical concepts. | Analyzing interview transcripts to understand key factors that influence volunteers' decision to participate in research [20] [2]. |
| The Wide Reflective Equilibrium Framework | To provide a structured methodological process for integrating empirical findings with ethical principles and considered judgments. | Justifying a normative recommendation by showing its coherence with empirical data on patient preferences and principles of autonomy [20]. |
Discussion: Navigating Methodological Challenges
Researcher Perspectives on Ambitious Aims
Despite the availability of numerous methodologies, the process of integration in practice is often described as vague and indeterminate [20]. Interviews with bioethics scholars reveal an "air of uncertainty" surrounding how to combine the normative and the empirical effectively [20]. This indeterminacy is a double-edged sword: it allows for methodological flexibility but also risks obscuring a lack of understanding of the theoretical underpinnings of empirical bioethics research [20].
This practical uncertainty is reflected in the divergent views researchers hold regarding the objectives of their work. As shown in Table 2, while understanding context and identifying ethical issues receive unanimous support, the more ambitious aims—particularly drawing normative recommendations and developing moral principles—are the most contested [2] [25]. This suggests that the acceptability of an objective is inversely related to its normative ambition. Researchers are generally comfortable using empirical data to inform the normative realm, primarily as a "testing ground for elements of normative theory," but are more cautious about using it to determine normative conclusions [2] [25].
The "Hidden" Nature of Ethically Relevant Data
A significant practical challenge in empirical bioethics is that much ethically relevant empirical research is "hidden" from view [5]. Key studies are often published in non-ethics journals by professionals who do not identify as ethicists, and without ethics-related keywords [5]. For example, a foundational study on tube feeding in patients with advanced dementia was published in JAMA by geriatric physicians, and a study on suicide risk in antidepressant trials was published in a psychiatry journal; both have been extensively cited in ethical debates [5]. This highlights that the value of empirical research for bioethics lies in its scientific rigor and relevance, not in the affiliation of the investigators or the journal it is published in [5] [11]. Researchers must therefore be skilled at searching beyond traditional bioethics sources and collaborating with professionals from other fields to access this critical data [5].
The typologies of research in empirical bioethics, from describing attitudes to changing norms, provide a valuable map for navigating this complex field. Kon's hierarchical framework and the continuum of research objectives offer complementary lenses for classifying research aims and understanding their varying levels of normative ambition. While a diverse toolkit of methodologies exists—from reflective equilibrium to dialogical approaches—successful research requires careful selection of a method that aligns with the study's goals and a clear-eyed view of the challenges, including the is-ought gap and the practical difficulties of integration. For drug development professionals and other researchers, this comparative guide underscores that the most effective empirical bioethics research is often that which thoughtfully matches its methodological approach to the specific research question, whether its aim is to describe a landscape or to help reshape its normative boundaries.
A Practical Guide to Prominent Empirical Bioethics Methods and Their Application
Comparative Analysis of Empirical Bioethics Methodologies
Within the expanding field of empirical bioethics, a critical challenge persists: how to effectively integrate diverse stakeholder perspectives to navigate complex moral questions in healthcare and biomedical research. This guide provides a comparative analysis of prominent empirical bioethics methodologies, with a specific focus on evaluating dialogical approaches that facilitate moral learning through structured stakeholder collaboration. For researchers, scientists, and drug development professionals, selecting an appropriate methodology is paramount for generating ethically robust and practically applicable results. This article objectively compares the performance, data requirements, and outputs of key methodological approaches, supporting the broader thesis that the conscious comparative study of these methods enriches the entire discipline. We present experimental data and detailed protocols to illustrate how these approaches are operationalized in contemporary bioethical research.
Methodological Comparison
Empirical bioethics methodologies vary significantly in their procedures, analytical frameworks, and ultimate objectives. The table below provides a structured comparison of four prominent approaches, highlighting their distinct applications in facilitating stakeholder dialogue.
Table 1: Comparative Analysis of Empirical Bioethics Methodologies
| Methodology | Primary Procedure | Key Analytical Approach | Typical Output | Illustrative Case Study |
|---|---|---|---|---|
| Comparative Cross-Cultural Analysis [26] | Qualitative data collection (e.g., surveys, interviews) across different cultural or national settings. | Thematic analysis to identify similarities and differences in ethical attitudes and practices. | Evidence base for understanding cultural nuances; informs training and policy. | Comparison of Chinese and Japanese doctors' attitudes toward patient death and error disclosure [26]. |
| Stakeholder Roundtables [27] | Structured, facilitated discussions among diverse stakeholders (e.g., industry, regulators, patients). | Consensus-building and normative argumentation to define metrics and ethical frameworks. | Ethical frameworks, reporting standards, and consensus statements. | Yale/EY roundtable developing metrics for patient centricity and clinical trial transparency in pharma [27]. |
| Media Debate Analysis [28] | Systematic collection and examination of media content (news, social media). | Qualitative content analysis to identify prevailing moral arguments and societal values. | Map of public moral landscape; identification of overlooked or emergent ethical problems. | Analysis of public discourse on AI in healthcare to identify biases and societal concerns [29] [28]. |
| Empirical Qualitative Engagement [26] | In-depth interviews and focus groups with key stakeholders within a specific context. | Grounded theory or descriptive qualitative analysis to unpack granular factors and lived experiences. | Deep, context-specific understanding of a phenomenon and its underlying ethical dimensions. | Study of factors leading to the proliferation and fragmentation of medical clinics in Pakistan [26]. |
Experimental Protocols and Workflows
To ensure methodological rigor and reproducibility, this section details the experimental protocols for two key dialogical approaches: the Stakeholder Roundtable and Media Debate Analysis.
Protocol 1: Stakeholder Roundtable for Metric Development
This protocol is modeled on the "Ethics, Trust + Patient Centricity in Pharma" roundtable [27], designed to define success metrics through collaborative dialogue.
- Participant Recruitment and Preparation: Convene a multidisciplinary group of 40-60 stakeholders. This includes pharmaceutical executives, regulatory officials (e.g., from FDA, EMA), patient advocacy leaders (e.g., from Global Genes, NORD), academic bioethicists, and investors [30] [27].
- Structured Agenda Facilitation: Execute a full-day agenda with timed sessions:
- Opening Keynotes (1.5 hours): Set the stage with talks from former FDA commissioners and lead bioethicists on ethical commitments and current performance trends [27].
- Focused Panel Discussions (3 hours): Conduct panels on specific themes, such as clinical trial transparency and demographic representation. Each panel includes brief opening remarks followed by moderated discussion [27].
- Small Group Brainstorming (1 hour): Divide participants into small, facilitated groups of approximately 10 people to brainstorm specific projects, themes, and metrics [27].
- Plenary Synthesis (1.5 hours): Reconvene for a full roundtable discussion to share small-group outputs and define collective next steps [27].
- Data Collection and Analysis: Data consists of audio recordings, transcribed proceedings, and written outputs from brainstorming sessions. Analysis involves thematic synthesis to identify consensus points, contested areas, and concrete, measurable metrics for ethical performance.
- Output Implementation: The synthesized findings are used to shape accountability tools, such as refining the "Good Pharma Scorecard" to advance patient-centric and trustworthy practices in medicines development [27].
The following diagram illustrates the iterative, collaborative workflow of this roundtable protocol.
Protocol 2: Systematic Media Debate Analysis
This protocol, derived from established research in the field, outlines the process for analyzing media debates to understand the public dimension of bioethical issues [28].
- Research Question and Source Definition: Formulate a precise question (e.g., "How are ethical concerns about AI-driven insurance denials framed in public media?"). Define the media corpus, including specific news outlets (legacy media) and public social media platforms, setting a date range and search terms [29] [28].
- Data Collection and Corpus Compilation: Systematically gather all relevant media items using database searches (e.g., LexisNexis) and platform APIs. Apply inclusion/exclusion criteria to create a final corpus for analysis.
- Qualitative Content Analysis: Code the media content in multiple passes. The first pass identifies broad themes (e.g., "bias," "accountability," "efficiency"). Subsequent passes perform a deeper analysis of ethical arguments, rhetorical frames, and the presence or absence of specific stakeholder voices [29] [28].
- Interpretation and Ethical Evaluation: Synthesize the coded data to map the dominant "moral landscape" of the issue. The analysis can identify morally problematic media framings (e.g., age-based stereotypes) and evaluate the quality of public ethical deliberation [28].
The workflow for this analytical method is a sequential, research-driven process, as shown below.
The Scientist's Toolkit: Research Reagents and Materials
Successful implementation of dialogical bioethics research requires both conceptual and practical tools. The table below details key "research reagents" essential for conducting the experiments and analyses described in this guide.
Table 2: Essential Materials for Empirical Bioethics Research
| Item | Function in Research | Application Example |
|---|---|---|
| Stakeholder Map | A visual tool identifying all relevant individuals, groups, and organizations with a stake in the bioethical issue. | Ensuring representative participation in a roundtable on clinical trial demographics, including patients, regulators, and industry scientists [27]. |
| Structured Interview/Focus Group Guides | A pre-defined set of open-ended questions used to ensure consistency and comprehensiveness in qualitative data collection. | Exploring the attitudes of Chinese and Japanese physicians using a uniform hypothetical scenario about patient death [26]. |
| Qualitative Data Analysis Software (e.g., NVivo, Atlas.ti) | Software designed to facilitate the coding, categorization, and thematic analysis of unstructured text data. | Managing and analyzing large corpora of media reports or interview transcripts to identify emergent ethical themes [28]. |
| Consensus-Building Frameworks (e.g., Delphi method) | Structured communication techniques used to distill the opinions of experts into a cohesive group judgment. | Facilitating small-group brainstorming sessions in a roundtable to define core metrics for patient centricity [27]. |
| Ethical Framework Template | A skeletal structure outlining key ethical principles (e.g., autonomy, justice, beneficence) to guide normative analysis. | Developing a religiously sensitive ethical framework for conducting clinical post-mortem examinations in Saudi Arabia [26]. |
Discussion of Performance and Outcomes
Each methodological approach offers distinct advantages and generates different forms of evidence, making them suited to specific research questions within the drug development and biomedical research landscape.
Stakeholder Roundtables excel in generating normative frameworks and actionable metrics. Their performance is measured by their ability to forge consensus among powerful, often competing, stakeholders. For example, the roundtable involving the FDA, EMA, and pharmaceutical companies directly addresses revising global industry standards for clinical trial transparency [27]. The primary data supporting their efficacy is the adoption of their outputs into policy tools like the Good Pharma Scorecard.
Media Debate Analyses provide critical insights into the societal context in which bioethical decisions are made. Their value lies in identifying public concerns, such as algorithmic bias in AI-driven insurance denials or the erosion of trust in health technologies, which may be overlooked in expert-driven dialogues [29] [28]. The quantitative data from one analysis revealed that only 16% of bioethics journals had a clear AI policy, highlighting a significant gap between a pressing public issue and institutional guidance [7]. This method's outcome is a map of the public moral landscape, which is essential for anticipating implementation challenges and ensuring the social robustness of ethical guidelines.
Comparative Cross-Cultural and Qualitative Studies deliver granular, context-specific understanding that prevents the uncritical transplantation of ethical norms. The experimental data from the China-Japan study revealed that fear of physical reprisals significantly influenced Chinese doctors' communication practices following a medical error—a finding with immediate implications for designing culturally competent ethics training [26]. The performance of this method is validated by its ability to uncover such critical, ground-level nuances that inform effective and localized ethical practice.
In conclusion, the dialogical approaches compared herein are not mutually exclusive but are complementary. A comprehensive empirical bioethics strategy may leverage media analysis to identify a public problem, use qualitative studies to understand its on-the-ground impact, and convene a stakeholder roundtable to develop a consensus-based solution. For professionals in drug development, this multifaceted understanding is crucial for navigating the complex interplay of science, ethics, and society, ultimately fostering moral learning that is both deeply informed and broadly legitimate.
Within the interdisciplinary field of empirical bioethics, consultative methodologies position the researcher as the primary agent who synthesizes empirical data and normative analysis. Unlike dialogical approaches that rely on stakeholder deliberation, consultative methods emphasize the scholar's systematic reflection to achieve justified ethical conclusions [31]. This guide provides a comparative analysis of two prominent consultative methods: Reflexive Balancing and the Wide Reflective Equilibrium (WRE). Despite the growing popularity of empirical bioethics, a systematic review identified 32 distinct methodologies, revealing considerable heterogeneity and uncertainty regarding their application and integration processes [31] [23]. This comparison examines their operational protocols, application data, and practical implementation to inform researchers and professionals in drug development and biomedical science.
Methodological Foundations
Wide Reflective Equilibrium (WRE)
The Wide Reflective Equilibrium, with origins in John Rawls' moral philosophy, is a coherentist method of ethical justification that seeks to achieve mutual coherence among three tiers of beliefs: (a) considered moral judgments, (b) moral principles, and (c) relevant background theories [32] [33]. Norman Daniels later refined this approach, arguing that incorporating background theories provides independent justificatory support for moral principles beyond mere alignment with pre-existing judgments [32]. The method is resolutely anti-foundationalist, granting no element permanent immunity from revision during the reflective process [33].
In bioethics applications, WRE functions as a "back-and-forth" process where researchers systematically adjust between empirical findings (often about stakeholder values and experiences) and normative frameworks until achieving a coherent equilibrium [20]. This equilibrium is considered "reflective" because the thinker understands how their principles and judgments interrelate, and "wide" because it incorporates diverse philosophical arguments and theoretical considerations beyond immediate moral intuitions [32] [33].
Reflexive Balancing
Reflexive Balancing, developed specifically for empirical bioethics contexts, shares WRE's coherentist approach but operates with a more focused pragmatic orientation. Jonathan Ives describes this method as a structured process of "reflexive balancing" that explicitly navigates between empirical data and ethical theory while maintaining critical awareness of the researcher's position and influence throughout the analytical process [23] [20].
This approach emphasizes practical applicability to concrete bioethical problems, particularly in healthcare and research settings. While retaining the mutual adjustment feature of WRE, Reflexive Balancing typically foregrounds the researcher's reflexive engagement with the subject matter, acknowledging the inevitable influence of their theoretical commitments and methodological choices on the resulting ethical analysis [20].
Comparative Analysis: Operational Characteristics
Table 1: Methodological Comparison of Reflexive Balancing and Wide Reflective Equilibrium
| Characteristic | Reflexive Balancing | Wide Reflective Equilibrium |
|---|---|---|
| Primary Source | Developed by Ives specifically for bioethics | Adapted from Rawls/Daniels' moral philosophy |
| Theoretical Scope | Focused on bioethical problems | Broad moral and political philosophy |
| Core Process | Reflexive mutual adjustment with researcher positionality | Systematic coherence-seeking among three belief sets |
| Key Elements | Empirical data, ethical principles, researcher reflexivity | Considered judgments, moral principles, background theories |
| Researcher Role | Explicitly reflexive and self-critical | Impartial systematizer |
| Primary Output | Contextually justified normative position | Coherent belief system in equilibrium |
Application Data and Performance Metrics
Empirical studies on the application of these methods reveal distinctive patterns. A systematic review of explicit WRE applications identified only 23 instances across 19 studies, discussing 50 equilibria, with researchers reporting a successfully reached equilibrium in 19 cases [32]. This scarcity suggests significant implementation challenges despite the method's theoretical prominence.
Both methods face criticisms regarding procedural vagueness. Researchers report uncertainty about how much weight to assign empirical data versus ethical theory during the adjustment process, with some describing an "air of uncertainty" surrounding practical implementation [20]. This indeterminacy represents a double-edged sword—allowing flexibility while potentially obscuring insufficient methodological rigor.
Table 2: Application Metrics for Wide Reflective Equilibrium Based on Empirical Review
| Metric | Findings |
|---|---|
| Total Applications Identified | 23 applications in 19 studies |
| Equilibria Discussed | 50 equilibria across all applications |
| Reported Successful Equilibria | 19 reached equilibrium states |
| Methodological Clarity | Significant variation in adjustment processes and criteria |
| Field Implementation | Applied across various disciplines and topics |
Experimental Protocols and Workflows
Wide Reflective Equilibrium Implementation Protocol
The WRE method follows a structured iterative process aimed at achieving coherence across multiple belief systems. The protocol involves specific operational stages with distinct cognitive tasks and methodological requirements at each phase.
Stage 1: Element Identification
- Considered Moral Judgments: Collect moral intuitions about particular cases or general rules that meet Rawlsian conditions of being made with adequate information, under favorable circumstances for judgment, and without distorting influences [33]. These judgments are not raw intuitions but those where "our moral capacities are most likely to be displayed without distortion" [33].
- Moral Principles: Formulate candidate principles that potentially systemize the identified judgments. These principles should have explanatory power beyond merely matching existing judgments.
- Background Theories: Identify relevant philosophical, social, and scientific theories that could independently support or challenge moral principles.
Stage 2: Systematic Comparison
- Conduct coherence checking between all three element sets, identifying conflicts and supportive relations.
- Document incoherencies where principles contradict judgments, judgments conflict with background theories, or principles lack theoretical support.
Stage 3: Mutual Adjustment
- Engage in systematic revision of conflicting elements—this may involve rejecting, modifying, or reinterpreting judgments, principles, or theoretical commitments.
- No element enjoys permanent privileging; even initially confident judgments may be revised if they persistently conflict with otherwise coherent principles supported by background theories.
Stage 4: Equilibrium Achievement
- Reach a state where all three element sets form a coherent network of mutual support.
- The equilibrium remains provisional and subject to revision with new arguments, evidence, or cases.
Reflexive Balancing Experimental Protocol
Reflexive Balancing follows a similarly iterative structure but incorporates explicit reflexive components throughout the process, emphasizing the researcher's positionality and practical orientation toward bioethical problem-solving.
Stage 1: Empirical Engagement
- Collect rich qualitative data about stakeholder experiences, values, and contextual factors through interviews, observations, or document analysis.
- Approach data with phenomenological sensitivity to capture lived moral experiences rather than pre-theorized ethical positions.
Stage 2: Normative Framework Selection
- Identify relevant ethical theories, principles, and concepts that illuminate the empirical domain.
- Consider multiple theoretical frameworks to avoid premature theoretical closure.
Stage 3: Reflexive Positioning
- Conduct explicit researcher reflexivity exercises to identify personal, theoretical, and methodological commitments that might shape analysis.
- Document positionality statements regarding the researcher's relationship to the subject matter.
Stage 4: Iterative Balancing
- Engage in deliberate shuttling between empirical findings and normative frameworks, adjusting interpretations of both as needed.
- Make transparent trade-offs when perfect coherence proves unattainable in complex practical contexts.
Stage 5: Contextual Justification
- Develop pragmatically oriented normative conclusions that address the specific problem context while maintaining philosophical rigor.
- Explicitly acknowledge remaining tensions or limitations in the achieved balance.
Table 3: Essential Research Resources for Consultative Empirical Bioethics
| Resource Category | Specific Examples | Function in Research Process |
|---|---|---|
| Qualitative Data Collection | Semi-structured interviews, focus groups, ethnographic observation | Gathers stakeholder experiences and contextual moral understandings |
| Normative Analysis Frameworks | Principlism (autonomy, beneficence, non-maleficence, justice), consequentialism, deontology | Provides systematic structure for ethical analysis |
| Reflexivity Tools | Positionality statements, research journals, peer debriefing | Enhances critical awareness of researcher influence on analysis |
| Coherence Assessment Methods | Consistency checking, explanatory power evaluation, theoretical support mapping | Systematically evaluates fit between empirical and normative elements |
| Theoretical Resources | Philosophical texts, sociological theories, scientific background literature | Supplies background theories for wide reflective equilibrium |
Comparative Strengths and Implementation Challenges
Wide Reflective Equilibrium
Advantages:
- Offers systematic comprehensiveness through its triple-element structure (judgments, principles, theories) [32] [33]
- Provides robust justificatory framework through independent support from background theories
- Represents the "dominant method" in moral and political philosophy with extensive theoretical development [33]
Implementation Challenges:
- Requires significant philosophical expertise to identify and evaluate relevant background theories
- Faces practical difficulties in achieving stable equilibrium given the complexity of balancing three element sets
- Shows relatively scarce application in empirical bioethics despite theoretical prominence [32]
Reflexive Balancing
Advantages:
- Emphasizes practical applicability to concrete bioethical problems
- Incorporates essential researcher reflexivity as methodological component
- Acknowledges contextual constraints of real-world bioethics consultation
Implementation Challenges:
- Risks under-specification of how exactly reflexivity informs the balancing process
- May lack theoretical comprehensiveness compared to WRE's triple-element structure
- Faces potential subjectivity concerns without robust mechanisms for independent justification
Both Reflexive Balancing and Wide Reflective Equilibrium offer structured approaches for integrating empirical research with normative analysis in bioethics. The WRE provides a more comprehensive justificatory framework through its incorporation of background theories, while Reflexive Balancing emphasizes pragmatic applicability and researcher positionality. The choice between methods depends on research context, with WRE suited for foundational normative inquiry and Reflexive Balancing offering advantages for context-specific bioethics consultation. Despite procedural differences, both methods reject algorithmic approaches to ethical justification in favor of systematic reflective processes that acknowledge the complex relationship between moral theory and practical reasoning. Their successful application requires transparency about methodological choices and theoretical commitments during the integration process.
Within the field of empirical bioethics, researchers are increasingly tasked with developing methodological approaches that are both normatively robust and empirically sound. Among the various justificatory strategies, the method of wide reflective equilibrium (WRE) has emerged as a prominent candidate for addressing complex clinical ethics dilemmas. Originally developed by John Rawls in political philosophy and refined by Norman Daniels for ethical justification, WRE seeks coherence among multiple levels of moral reasoning [32] [34]. This case study examines the application of reflective equilibrium to clinical ethics through a comparative lens, evaluating its implementation against other methodological approaches in empirical bioethics. We present experimental data from existing studies and provide a detailed protocol for applying WRE to clinical ethics dilemmas, with particular attention to its capacity to integrate diverse moral perspectives and generate justified ethical conclusions.
The fundamental premise of reflective equilibrium is that ethical justification does not prioritize either abstract theories or particular case judgments, but instead seeks coherence across three distinct levels: considered moral judgments about specific cases, moral principles or rules, and relevant background theories [34] [35]. This multi-layered approach offers a structured methodology for addressing the complex value conflicts that frequently arise in clinical settings, from end-of-life decisions to resource allocation dilemmas.
Theoretical Framework: Understanding Reflective Equilibrium
Core Components of Wide Reflective Equilibrium
The wide reflective equilibrium method operates through a systematic process of reflection and adjustment among three primary components:
- Considered Moral Judgments: These are our confident ethical intuitions about specific cases or scenarios, made under conditions that minimize bias and external pressure [34]. In clinical ethics, these might include judgments about whether a particular end-of-life decision is morally acceptable.
- Moral Principles: These are general ethical rules or guidelines that inform our decision-making, such as principles of autonomy, beneficence, non-maleficence, and justice [32] [35].
- Background Theories: These include relevant factual beliefs, sociological data, and theoretical frameworks that bear on the ethical issue at hand [32]. In healthcare contexts, this might encompass empirical research on patient outcomes, cultural beliefs about illness, or economic analyses of resource allocation.
The Process of Achieving Equilibrium
The method involves working back and forth among these three components, revising elements at any level as needed to achieve an "acceptable coherence" among them [34]. This process is "reflective" because it involves critical examination of all components, and "wide" because it incorporates background theories in addition to judgments and principles. The equilibrium reached is temporary and remains open to revision in light of new evidence or perspectives [32] [34].
Table 1: Core Components of Wide Reflective Equilibrium in Clinical Ethics
| Component Level | Description | Clinical Ethics Example |
|---|---|---|
| Considered Moral Judgments | Confident ethical intuitions about specific cases made under conditions minimizing bias | A clinician's judgment that a particular patient's request for life-sustaining treatment should be respected |
| Moral Principles | General ethical rules or guidelines that inform decision-making | Principles of autonomy, beneficence, non-maleficence, and justice |
| Background Theories | Relevant factual beliefs, sociological data, and theoretical frameworks | Empirical research on patient outcomes, cultural beliefs about illness, economic analyses |
Comparative Experimental Data: WRE in Clinical Ethics Research
Empirical Study on Moral Reasoning Patterns
A 2025 comparative study examining ethical dilemmas among healthcare professionals provides compelling data on divergent moral reasoning patterns [36]. The study involved 244 participants (51 senior medical students and 193 practicing physicians) who completed an adapted version of the Defining Issues Test, version 2 (DIT-2), assessing three classical dilemmas: end-of-life decision-making, access to life-saving medication, and reintegration of a fugitive [36].
The findings revealed significant differences in how these groups approach ethical conflicts:
- Physicians consistently endorsed conventional, law-based reasoning, emphasizing legality and professional codes
- Medical students demonstrated greater variability, indecision, and openness to compassion-driven justifications
In the "Jan and the Drug" and "Fugitive" dilemmas, significant between-group differences highlighted tensions between legality, empathy, and justice (p < 0.01) [36]. These differences in reasoning patterns indicate differing vulnerabilities to moral distress, particularly when legal and compassionate perspectives conflict.
Table 2: Moral Reasoning Patterns Among Healthcare Professionals [36]
| Participant Group | Reasoning Approach | Primary Influences | Vulnerability to Moral Distress |
|---|---|---|---|
| Practicing Physicians (n=193) | Conventional, law-based | Professional codes, legality | When professional obligations conflict with patient needs |
| Medical Students (n=51) | Varied, compassion-driven | Empathy, justice principles | When systemic constraints prevent compassionate action |
Application in Research Ethics Committees
Further evidence for the utility of reflective equilibrium comes from empirical research on Research Ethics Committees (RECs). A 2021 study revealed that reviewers on ethics committees implicitly use reflective equilibrium when evaluating research proposals, working back and forth between universal principles and the specific contexts of each application [37]. The study identified three key processes at work in ethical review:
- Emotion and intuition - Initial gut responses to applications
- Imagination and creative thinking - Considering scenarios and perspectives
- Intuition and trust - Balancing personal judgment with established norms
This research demonstrates how reflective equilibrium functions in practice within institutional ethics review processes, offering a coherent and grounded account of review work [37].
Experimental Protocol: Applying WRE to Clinical Ethics Dilemmas
Study Design and Participant Selection
Objective: To systematically apply the wide reflective equilibrium method to a specific clinical ethics dilemma, documenting the process and outcomes.
Case Selection: Identify a clinically relevant ethics dilemma with significant moral dimensions. Suitable cases might include:
- End-of-life decision-making for terminally ill patients
- Allocation of scarce medical resources
- Disclosure of medical errors
- Parental refusal of recommended treatment for a child
Participant Recruitment: Engage a diverse group of 15-20 stakeholders, including:
- 5-6 clinical professionals (physicians, nurses, social workers)
- 3-4 hospital administrators or policy experts
- 4-5 patient representatives or community advocates
- 2-3 bioethicists or moral philosophers
Data Collection and Analysis Procedure
The research platform employs a structured multi-stage process:
Initial Elicitation Phase (Weeks 1-2):
- Conduct individual interviews to elicit participants' initial considered judgments about the case
- Identify relevant moral principles each participant views as applicable
- Document background theories and empirical beliefs informing participants' positions
Structured Deliberation Phase (Weeks 3-6):
- Facilitate 3-4 group sessions where participants present and discuss their positions
- Identify points of conflict and coherence between judgments, principles, and theories
- Encourage reflection on inconsistencies and consideration of alternative viewpoints
Equilibrium Seeking Phase (Weeks 7-8):
- Guide participants through a process of revising elements at any of the three levels to achieve greater coherence
- Document which elements participants are willing to revise and which they hold fixed
- Continue iterations until no further revisions are proposed or time constraints are reached
Outcome Assessment Phase (Weeks 9-10):
- Document the final reflective equilibrium (or equilibria) reached
- Assess the degree of consensus or divergence among participants
- Evaluate the justificatory strength of the resulting position(s)
Methodological Implementation Tools
Implementing the WRE method effectively requires specific methodological tools and approaches:
Digital Bioethics Platforms: Recent advances in digital methods for empirical bioethics research have led to the development of specialized platforms that can support the WRE process [38]. These platforms can help manage the complex data generated during WRE applications and facilitate collaboration among researchers with different methodological backgrounds.
Visualization Techniques: Knowledge visualization approaches can make ethical frameworks more accessible to diverse stakeholders [39]. For WRE applications, visual representations of the relationships between judgments, principles, and background theories can help participants understand connections and conflicts within the moral framework.
Iterative Dialogue Protocols: Structured approaches to facilitated dialogue are essential for productive reflection. These should encourage participants to:
- Articulate reasons for their moral positions
- Consider alternative perspectives
- Identify implicit assumptions in their reasoning
- Be willing to revise elements at any level to achieve greater coherence
Table 3: Essential Methodological Tools for Reflective Equilibrium Research
| Tool Category | Specific Resource | Application in WRE Research |
|---|---|---|
| Theoretical Framework | Daniels' Wide Reflective Equilibrium Specification [32] | Provides the foundational three-level structure for ethical justification |
| Data Collection Instruments | Adapted Defining Issues Test (DIT-2) [36] | Measures moral reasoning patterns and identifies conflicts between principles and judgments |
| Digital Research Platforms | Modular Bioethics Research Platform [38] | Supports implementation of digital methods and management of complex qualitative data |
| Analysis Tools | Qualitative Coding Software (NVivo, MAXQDA) | Facilitates thematic analysis of deliberative sessions and interview transcripts |
| Visualization Methods | Knowledge Visualization Systems [39] | Creates accessible representations of complex ethical frameworks and relationships |
Comparative Analysis: WRE Versus Alternative Methodological Approaches
When evaluated against other methodological approaches in empirical bioethics, WRE demonstrates distinctive strengths and limitations:
Advantages of the WRE Approach
- Comprehensive Justification: Unlike purely principle-based or case-based approaches, WRE integrates multiple sources of moral reasoning, potentially leading to more robust justifications [32] [34].
- Flexibility and Responsiveness: The method accommodates new evidence and perspectives, allowing ethical positions to evolve in light of additional information [34].
- Empirical-Normative Integration: WRE provides a structured approach to integrating empirical data (as background theories) with normative reasoning, addressing a key challenge in empirical bioethics [35].
- Conflict Resolution Potential: By making explicit the connections and tensions between different levels of moral reasoning, WRE can help identify pathways to resolve ethical disagreements [37].
Challenges and Limitations
- Operationalization Complexity: Translating abstract background theories into concrete moral principles presents significant practical challenges [35].
- Resource Intensity: The iterative process of achieving reflective equilibrium requires substantial time and facilitation resources [32].
- Assessment Difficulties: Determining when a stable equilibrium has been reached remains methodologically challenging [32] [35].
- Power Dynamics: The quality of the equilibrium process can be affected by unequal power relations among participants, potentially privileging some perspectives over others [35].
This case study demonstrates that wide reflective equilibrium offers a systematic and justificatorily robust methodology for addressing clinical ethics dilemmas. The comparative experimental data reveals how this approach can illuminate divergent moral reasoning patterns among different stakeholder groups, particularly between experienced clinicians and trainees [36]. The detailed experimental protocol provides a roadmap for implementing WRE in clinical ethics contexts, with specific tools and processes to support its application.
For the field of empirical bioethics, WRE represents a promising approach to bridging the gap between normative theory and empirical research. By systematically integrating considered judgments, moral principles, and relevant background theories, this method offers a responsive framework for addressing complex clinical ethics dilemmas in evolving healthcare contexts. Future methodological development should focus on addressing the identified challenges, particularly regarding operationalization, assessment criteria, and power dynamics within deliberative processes.
The successful application of WRE to clinical ethics requires continued refinement of digital tools [38], visualization techniques [39], and facilitation approaches to make this powerful justificatory method more accessible to researchers and clinicians working at the intersection of empirical research and normative analysis.
Policy development in research ethics increasingly requires navigating complex, "wicked problems" characterized by multiple stakeholders, conflicting values, and no clear right answers [40]. Within the broader comparative study of empirical bioethics methodologies, dialogical approaches represent a distinct pathway for integrating empirical findings with normative analysis. Unlike purely philosophical or consultative methods, dialogical methods rely on structured stakeholder deliberation to develop ethical guidance and policies that are both contextually grounded and morally defensible. This case study examines the application of dialogical methods in research ethics policy development, comparing its theoretical foundations, practical implementation, and outcomes with other prominent empirical bioethics methodologies.
The fundamental challenge in empirical bioethics lies in the integration of empirical data with normative reasoning [20]. Dialogical methods address this challenge by making the integration process itself collaborative and deliberative, positioning stakeholders as active participants in ethical deliberation rather than merely as sources of empirical data. As this case study will demonstrate, this approach offers unique advantages for developing research ethics policies that are practically workable while maintaining ethical rigor.
Theoretical and Methodological Foundations
Dialogical methods in empirical bioethics are characterized by their deliberative and participatory nature, where ethical norms are developed through structured dialogue among stakeholders rather than through top-down application of ethical theories [20]. This approach contrasts with more traditional bioethics methodologies that maintain a clearer separation between empirical description and normative prescription.
The theoretical underpinnings of dialogical approaches position ethics as a communal practice rather than an individual cognitive exercise. This perspective is exemplified in the Path2Integrity project, which "starts from the premise that researchers are members of an active scientific community which continuously discusses, reflects and (re-)develops practices that together constitute responsible conduct of research" [41]. This view recognizes that ethical norms are continually negotiated within communities of practice, making dialogue essential for their development and legitimacy.
Dialogical methods can be distinguished from other empirical bioethics approaches through their core characteristics:
- Stakeholder Integration: Unlike consultative methods where researchers maintain control over normative analysis, dialogical methods engage stakeholders directly in ethical deliberation [20]
- Process-Oriented: The focus is on the deliberative process itself as the site of ethical development rather than on predetermined outcomes
- Contextual Sensitivity: Ethical solutions emerge from specific contexts and are attuned to practical constraints and possibilities
Table 1: Comparison of Empirical Bioethics Methodologies
| Methodology | Approach to Integration | Primary Focus | Researcher Role |
|---|---|---|---|
| Dialogical | Collaborative deliberation among stakeholders | Developing shared understanding through dialogue | Facilitator, participant |
| Consultative | Researcher analyzes empirical data to develop normative conclusions | Applying ethical theory to empirical findings | External analyst |
| Reflective Equilibrium | Back-and-forth adjustment between principles and cases | Achieving coherence in moral beliefs | "Thinker" refining personal coherence |
| Inherent Integration | Empirical and normative dimensions intertwined from start | Holistic understanding of ethical phenomena | Integrated researcher |
Dialogical Approaches in Practice: Key Examples
Policy Dialogues in Public Health
Policy dialogues represent a structured application of dialogical methods to public health policy development. As defined in the literature, a policy dialogue is "a tool which promotes evidence-informed policy-making" that "involves deliberation about a high-priority issue, informed by a synthesis of the best-available evidence, where potential policy interventions are discussed by stakeholders" [40]. These dialogues are characterized by five core features: they are (i) focused on a high-priority issue, (ii) evidence-informed, (iii) deliberative, (iv) participatory, and (v) action-oriented [40].
Practical examples demonstrate the application of policy dialogues to complex research ethics challenges. For instance, policy dialogues have been conducted in Moldova to address policies to reduce alcohol-related harm, and in Hungary to develop strategies for combating antimicrobial resistance [40]. These examples illustrate how dialogical methods can address research ethics issues that involve "conflicting stakeholder interests – including those of government, individuals and commercial actors – and the need for widespread behaviour change" [40].
The Path2Integrity Learning Programme
The Path2Integrity project exemplifies the application of dialogical methods to research integrity training. The project employs a "twofold dialogical approach: First, the main goal of the learning programme is to conduct a dialogue and second the programme offers dialogue-based learning methods such as storytelling and role-playing to achieve this goal" [41]. This approach aims to build participants' capacity to "engage in rational argumentation, set shared objectives and norms, establish preconditions for dialogue, weigh the pros and cons of different possible courses of action and, in general, become active participants in discourses on responsible conduct of research" [41].
The pedagogical foundation of Path2Integrity emphasizes the development of discursive competence through structured dialogue, positioning this as essential for navigating the normative challenges of research practice. This approach aligns with the broader recognition in research integrity training that engaging, interactive methods such as role-playing and collaborative discussion are more effective than passive knowledge transmission [41].
Comparative Methodological Analysis
Integration Mechanisms Across Methods
A key differentiator among empirical bioethics methodologies is their approach to integrating empirical and normative dimensions. Dialogical methods achieve integration through structured deliberation that engages stakeholders directly in normative deliberation. This contrasts with:
- Consultative approaches where researchers maintain primary responsibility for normative analysis based on empirical data gathered from stakeholders [20]
- Reflective equilibrium which involves a "back-and-forth" adjustment between ethical principles and empirical cases conducted primarily by the researcher [20]
- Inherent integration methods where the empirical and normative are fundamentally intertwined from the research outset [20]
Each approach embodies a different understanding of where ethical expertise resides and how empirical facts should inform normative conclusions. Dialogical methods are distinctive in their distributed approach to ethical expertise, recognizing stakeholders as possessing crucial ethical insight based on their experiences and positions.
Methodological Strengths and Limitations
Table 2: Strengths and Limitations of Empirical Bioethics Methodologies
| Methodology | Strengths | Limitations |
|---|---|---|
| Dialogical | - Generates contextually nuanced solutions- Enhances legitimacy and buy-in- Identifies shared values across stakeholders | - Time and resource intensive- Requires skilled facilitation- May struggle with power imbalances |
| Consultative | - Clear analytical framework- Efficient use of researcher expertise- Methodologically familiar to ethicists | - Limited stakeholder ownership- May miss important contextual factors- Privileges academic ethical expertise |
| Reflective Equilibrium | - Systematic approach to coherence- Responsive to counterexamples- Philosophically rigorous | - Individualistic orientation- Dependent on researcher's moral intuitions- Complex to implement fully |
| Inherent Integration | - Holistic understanding- Avoids artificial separation of facts and values- Methodologically innovative | - Methodologically vague- Difficult to articulate process- Challenging to evaluate rigor |
Dialogical methods particularly excel in contexts where policy implementation requires broad stakeholder buy-in or where ethical challenges involve competing values that lack clear prioritization. However, they face challenges related to practical feasibility and the potential for power dynamics to distort deliberative processes [40] [20].
Research with empirical bioethics scholars reveals that despite the availability of multiple integration methodologies, there often remains an "air of uncertainty and overall vagueness" about how integration actually occurs in practice [20]. This methodological vagueness represents a significant challenge for the field, though some scholars argue it allows beneficial flexibility.
Experimental Protocol: Implementing a Policy Dialogue
Protocol Design and Structure
Implementing a policy dialogue for research ethics policy development requires careful structuring to balance deliberative openness with methodological rigor. The following protocol provides a template for researchers seeking to apply dialogical methods:
Phase 1: Preparation (4-6 weeks)
- Issue Identification and Scoping: Define the specific research ethics challenge, identify key questions, and determine dialogue scope through preliminary stakeholder interviews
- Evidence Synthesis: Compile and synthesize best available evidence regarding the ethical issue, including scientific literature, case examples, and relevant ethical frameworks
- Stakeholder Mapping and Recruitment: Identify and recruit diverse stakeholders representing relevant perspectives (researchers, ethics committee members, research participants, policymakers, etc.)
- Pre-Dialogue Materials: Develop concise background materials summarizing key evidence and ethical considerations for distribution to participants
Phase 2: Dialogue Convening (1-2 days)
- Structured Deliberation: Facilitate dialogue using methods that ensure balanced participation, such as roundtable discussions, small group work, and scenario analysis
- Evidence Integration: Systematically examine how different forms of evidence (scientific, experiential, ethical) bear on the policy challenge
- Option Development: Identify and refine potential policy approaches that respond to ethical considerations and practical constraints
- Conclusion Formulation: Develop specific policy recommendations, implementation considerations, and identification of points of agreement and disagreement
Phase 3: Follow-up and Implementation (2-4 weeks)
- Documentation and Reporting: Produce a comprehensive report detailing dialogue process, evidence considered, and outcomes
- Results Dissemination: Share findings with relevant decision-making bodies and broader stakeholder communities
- Implementation Support: Engage with relevant institutions to support policy implementation and monitoring
This protocol emphasizes the importance of being "evidence-informed, deliberative, participatory and action-oriented" – key characteristics of effective policy dialogues [40].
Ethical Considerations and Safeguards
Dialogical methods require attention to specific ethical considerations:
- Power Imbalances: Implement structured facilitation techniques to ensure equitable participation across stakeholder groups with differing status and authority
- Confidentiality vs. Transparency: Establish clear agreements regarding what aspects of deliberation will remain confidential and what will be publicly reported
- Managing Expectations: Be transparent about the advisory nature of policy dialogue outcomes and their relationship to formal decision-making processes
The experimental protocol should include specific mechanisms to address these considerations, such as ground rules for discussion, anonymous voting on sensitive issues, and independent facilitation.
Visualization of Methodological Processes
Dialogical Method Workflow
The following diagram illustrates the structured workflow of a dialogical method for research ethics policy development:
Dialogical Method Workflow for Policy Development
This workflow highlights the iterative nature of dialogical methods, where option generation and normative refinement may require returning to structured dialogue to address new questions or concerns that emerge during deliberation.
Comparative Integration Pathways
The following diagram contrasts the integration pathways of different empirical bioethics methodologies:
Comparative Integration Pathways in Bioethics
This comparative visualization highlights how dialogical methods centralize stakeholder deliberation as the mechanism for integrating empirical and normative dimensions, whereas other approaches position integration primarily as a researcher-driven process.
Research Reagents and Tools
Table 3: Essential Methodological Resources for Dialogical Approaches
| Resource Category | Specific Tool/Resource | Function in Dialogical Research |
|---|---|---|
| Facilitation Frameworks | Structured Dialogical Design | Provides methodological framework for organizing effective stakeholder dialogues and managing group dynamics |
| Ethical Guidance | IFAPP International Ethics Framework [42] | Offers ethical guidance for professionals navigating industry-academia interfaces in pharmaceutical medicine |
| Protocol Development | Empirical Bioethics Protocol Template [43] | Supports rigorous study design and documentation for empirical bioethics research |
| Training Materials | Path2Integrity Learning Cards [41] | Provides structured materials for research integrity training using dialogical methods |
| Analysis Tools | Qualitative Data Analysis Software (e.g., MAXQDA) [20] | Supports systematic analysis of dialogue transcripts and qualitative data |
| Reporting Standards | SRQR (Standards for Reporting Qualitative Research) [43] | Ensures comprehensive reporting of qualitative components in dialogical research |
These methodological "reagents" provide essential support for implementing dialogical approaches with sufficient rigor and transparency to produce credible outcomes. The empirical bioethics protocol template [43] is particularly valuable for addressing the unique epistemological and methodological requirements of research that integrates empirical and normative dimensions.
Dialogical methods offer a distinctive approach within the broader landscape of empirical bioethics methodologies, characterized by their collaborative approach to integration and their potential to develop contextually attuned ethical guidance. For research ethics policy development, these methods are particularly valuable for addressing complex challenges that involve multiple stakeholders with legitimate but potentially conflicting perspectives.
The comparative analysis presented in this case study suggests that the choice of empirical bioethics methodology should be guided by the specific policy context and goals. Dialogical methods are especially appropriate when policy success depends on broad stakeholder ownership or when ethical challenges involve fundamental value conflicts that cannot be resolved through technical expertise alone. However, these advantages must be balanced against the significant practical resources required for effective implementation.
As research ethics continues to grapple with emerging challenges posed by technological innovation, globalization, and evolving research practices, dialogical methods provide an important approach for developing policies that are both ethically sound and practically implementable. Their emphasis on inclusive deliberation and collaborative norm-making offers a promising path forward for research ethics in an increasingly complex scientific landscape.
The field of bioethics is witnessing a significant empirical shift, with a growing reliance on research methods from the social sciences to inform ethical analysis and guideline development [44]. This evolution necessitates robust methodologies for creating and implementing consensus guidelines in interdisciplinary contexts, such as healthcare. Such guidelines are often the product of collaboration among diverse experts, including physicians, nurses, ethicists, and methodologies [45] [46]. The core challenge lies in effectively integrating empirical data with normative reasoning to establish standards of practice that are both evidence-based and ethically sound [44]. This guide compares prominent methodological approaches for developing and evaluating these interdisciplinary guidelines, providing a framework for researchers and drug development professionals engaged in this complex field.
Comparative Analysis of Methodological Approaches
The implementation of interdisciplinary guidelines can be studied through various methodological lenses. The table below compares three distinct approaches identified in the literature: a comparative observational study, a guideline development process, and a survey of researcher practices.
Table 1: Comparison of Empirical Methodologies in Bioethics and Interdisciplinary Guidelines
| Methodology | Core Objective | Data Collection Instrument | Sample Size & Population | Key Quantitative Findings |
|---|---|---|---|---|
| Comparative Observational Study [36] | Compare moral reasoning patterns and vulnerability to moral distress. | Adapted Defining Issues Test, Version 2 (DIT-2) with 3 ethical dilemmas [36]. | 244 participants (51 senior medical students; 193 physicians) [36]. | Physicians consistently endorsed conventional, law-based reasoning. Significant differences in responses to dilemmas between groups (p < 0.01) [36]. |
| Systematic Guideline Development (GRADE) [46] | Formulate evidence-based clinical practice guidelines for left atrial appendage occlusion (LAAO). | Systematic literature review and evidence synthesis using GRADE framework [46]. | Multidisciplinary guideline panel with <50% industry conflicts [46]. | Produced 8 evidence-based recommendations; 75% (6/8) were conditional, supported by low or very low certainty evidence [46]. |
| Cross-Sectional Survey Research [44] | Describe attitudes and conduct of bioethics researchers regarding empirical methods. | Anonymous online survey with sections on attitudes, training, and research conduct [44]. | 200 bioethics researchers from 12 European countries [44]. | 87.5% (175/200) have used empirical methods; only 35% of those integrated empirical data with normative analysis [44]. |
Detailed Experimental Protocols
Understanding the mechanics of these methodologies is crucial for evaluating their rigor and applicability. This section details the experimental protocols for the key approaches compared above.
Protocol for Comparative Moral Reasoning Study
The study on moral reasoning in medical students and physicians provides a model for quantitative, cross-sectional comparison in bioethics [36].
- Study Design: A cross-sectional, observational study.
- Population & Sampling: 244 participants (51 senior medical students and 193 physicians) were recruited. The physician cohort had a median of 12 years of professional experience [36].
- Instrumentation: An adapted version of the Defining Issues Test, version 2 (DIT-2) was used. The instrument presented three classical dilemmas ("Doctor’s Dilemma," "Jan and the Drug," "The Fugitive"). For each, participants completed a decision task, a rating task (importance scoring of arguments), and a ranking task [36].
- Data Analysis: Responses were analyzed using descriptive statistics and chi-square tests to identify differences in decision choices and underlying reasoning patterns between the groups [36].
- Reliability & Validity: The DIT-2 is a widely validated tool. The adapted version was translated into Romanian, back-translated, and reviewed by a panel of bioethics and medical education experts to ensure cultural and contextual accuracy [36].
Protocol for Clinical Practice Guideline Development
The SCAI/HRS guidelines for LAAO exemplify a rigorous, internationally recognized standard for creating interdisciplinary consensus guidelines [46].
- Panel Assembly: A balanced, multidisciplinary guideline panel was convened, with strict management of conflicts of interest (less than 50% of members had significant industry ties) [46].
- Question Formulation: The panel formulated and prioritized clinical questions in a PICO (Population, Intervention, Comparison, Outcome) format [46].
- Evidence Review & Synthesis: A technical review team of clinical and methodological experts conducted systematic reviews, synthesized data, and graded the certainty of evidence for each outcome using the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) methodology [46].
- Recommendation Formulation: The panel developed recommendations informed by the evidence synthesis and using the GRADE evidence-to-decision framework. Recommendations were categorized as either "strong" or "conditional" with explicit interpretations for each [46].
Workflow for Interdisciplinary Guideline Implementation
The following diagram visualizes the multi-stage, iterative workflow for implementing interdisciplinary guidelines, synthesizing elements from the analyzed methodologies [36] [45] [46].
The Researcher's Toolkit: Essential Reagents for Empirical Bioethics
Successful empirical research in bioethics and guideline implementation relies on a suite of methodological "reagents." The table below details key tools and their functions.
Table 2: Essential Research Reagents for Empirical Bioethics and Guideline Work
| Tool / Reagent | Category | Primary Function | Application Example |
|---|---|---|---|
| Defining Issues Test (DIT-2) [36] | Psychometric Instrument | Measures the development of moral judgment by presenting ethical dilemmas and analyzing reasoning patterns. | Comparing moral reasoning between professional groups (e.g., physicians vs. students) to identify training needs [36]. |
| GRADE Framework [46] | Methodological Framework | Provides a transparent and systematic approach for grading the quality of evidence and strength of recommendations in guidelines. | Formulating conditional vs. strong recommendations in clinical practice guidelines, such as for LAAO therapy [46]. |
| ABCDEF Bundle [45] | Implementation Tool | An integrated, interoperational framework for operationalizing clinical guidelines (e.g., for Pain, Agitation, Delirium, Immobility, and Sleep) into daily practice. | Helping ICU teams systematically apply the 2025 PADIS guidelines to improve patient mobility and manage delirium [45]. |
| Structured Survey Instrument [44] | Data Collection Tool | Gathers standardized data on attitudes, self-reported practices, and demographic information from a target population. | Assessing the prevalence of empirical method use and training gaps among bioethics researchers in Europe [44]. |
| Warehouse-Native Analytics [47] | Data Analysis Platform | Allows experimentation and analysis against core business and clinical metrics stored in a data warehouse, ensuring a single source of truth. | Tracking the impact of a new guideline on complex, cross-functional journey metrics (e.g., patient recovery time, resource use) rather than isolated clicks [47]. |
Discussion and Comparative Synthesis
The comparative analysis reveals critical insights for conducting research on interdisciplinary guidelines. The observational study protocol [36] is powerful for identifying variation in practices and underlying cognitive processes, but it is limited to describing what is rather than prescribing what ought to be. In contrast, the formal guideline development protocol [46] is explicitly normative, aiming to establish standards of care, yet it is often constrained by a foundation of low or very low certainty evidence. The survey research [44] highlights a significant gap in the field: while most bioethics researchers use empirical methods, a majority lack the training or clear methodologies to successfully integrate their findings with normative analysis.
This synthesis underscores that no single methodology is sufficient. A robust approach involves:
- Utilizing validated instruments like the DIT-2 to ensure reliability and allow for cross-study comparisons [36].
- Adhering to structured frameworks like GRADE to enhance the transparency, legitimacy, and credibility of the resulting guidelines [46].
- Employing implementation bundles and integrated analytics to translate abstract guidelines into measurable actions and outcomes in complex interdisciplinary settings [45] [47].
Implementing consensus guidelines for interdisciplinary work is a complex, multi-method endeavor that sits at the intersection of empirical research and normative analysis. This guide has compared key methodological approaches, detailing their protocols and tools. The findings indicate that the field is moving toward greater empiricism but requires more rigorous training for researchers in methodological integration [44]. Future research should prioritize closing the identified evidence gaps that lead to conditional recommendations [46] and developing more sophisticated tools for evaluating the real-world impact of guidelines on both process metrics and patient-centered outcomes. For researchers and drug development professionals, mastering this blend of empirical rigor and ethical reasoning is no longer optional but a fundamental standard of practice.
Overcoming Common Challenges: Ensuring Rigor in Empirical Bioethics Research
The field of empirical bioethics faces a persistent challenge: the "vagueness critique," which questions the rigor, reproducibility, and transparency of its methodologies. This critique stems from a lack of clear documentation and standardized processes for integrating empirical data with normative analysis. This guide provides a comparative analysis of contemporary methodologies, highlighting how structured protocols, digital tools, and integrated reporting frameworks can achieve the transparency necessary to bolster the scientific credibility of empirical bioethics research.
Comparative Analysis of Empirical Bioethics Methodologies
The table below objectively compares three methodological approaches, evaluating their capacity to address transparency and the vagueness critique through specific features and experimental support.
Table 1: Comparative Analysis of Empirical Bioethics Methodologies
| Methodology | Core Transparency Features | Key Experimental Support & Data | Addressing Vagueness |
|---|---|---|---|
| Design Bioethics & Digital Tools [48] [38] | - Purpose-built digital games & VR scenarios- Embeds context, narrative, and embodiment- Enables data collection at scale | - A digital platform prototype was developed, providing three digital methods composed of functional components [38].- In a real-life test, the platform was used to investigate visual risk communication about COVID-19 on Twitter, with researchers requesting and using new features in-situ [38]. | Converts abstract ethical reasoning into observable, in-context decision-making within a structured digital environment. |
| Structured Protocol Templates [43] | - Standardized sections for epistemological positioning- Explicit instructions for theoretical frameworks and bias management- Flexible but documented consent and data protection plans | - A novel protocol template was formalized, reorganizing and rewriting the SRQR standards to be suitable for quantitative, qualitative, and mixed-methods approaches [43].- The template includes 22 sections, with a specific epistemological section to clarify the research foundation [43]. | Imposes methodological discipline and requires researchers to explicitly justify and document their integrative process. |
| Integrated Drug Development Frameworks [49] [50] [51] | - Cross-functional team establishment- Mandatory stage-gate reviews with all stakeholders- Digital data management (e.g., Electronic Lab Notebooks) | - The FDA's Clinical Data Summary Pilot concluded with lessons for a harmonized disclosure system, proposing an international library for clinical data to improve public access [50].- Stage-gate reviews are implemented throughout development, ensuring a process cannot advance until all stakeholders have understood and endorsed the current state [51]. | Provides a model for transparent, documented, and collaborative processes that can be adapted from technical development to ethical analysis. |
Detailed Experimental Protocols
Protocol for Digital Bioethics Experiments
This protocol is based on the development and testing of a research platform for digital bioethics [38].
- Objective: To leverage digital tools (e.g., games, VR, text-based scenarios) for empirical ethics research, enabling situated engagement with moral dilemmas and data collection at scale [48].
- Theoretical Scaffolding: Researchers must first select a theoretical framework (e.g., pragmatism, feminist bioethics) that justifies the importance of context, narrative, and embodiment in moral decision-making. This framework guides the entire design process [48].
- Platform and Tool Development:
- Persona Creation: Define abstract users (personas) representing researchers to derive functional requirements [38].
- Modular Architecture: Implement a client-server platform using a micro-service and micro-frontend approach. The frontend uses a framework like Angular, and the backend uses a Python framework like Flask with pandas for data management [38].
- Component Implementation: Digital methods are not built as monoliths but are split into functional components (e.g., data filtering, analysis) that can be recombined [38].
- In-Situ Testing and Iteration: Collaborate with researchers to use the platform prototype in a real study. Gather feedback continuously and implement improvements through multiple prototyping cycles until the features meet research needs precisely [38].
Protocol for Structured Ethics Proposal Design
This protocol utilizes the novel template designed for humanities and social sciences in health [43].
- Objective: To provide a clear, comprehensive, and evaluable research plan for empirical bioethics studies, ensuring methodological soundness and ethical compliance.
- Template Application:
- Epistemological Justification: In the dedicated epistemological section, investigators must specify the humanities and social sciences disciplines involved and the underlying theoretical foundations [43].
- Methodological Rigor: Detail the research approach (qualitative, quantitative, mixed). The protocol requires explicit description of data collection, analysis techniques, and, crucially, the procedure for integrating empirical findings with normative ethical analysis [43].
- Contextualized Ethical Safeguards: Justify the chosen form of informed consent (written, oral, waived) and data protection measures (anonymization vs. pseudonymization) based on the specific study context to minimize bias and maintain practical feasibility [43].
- Oversight and Evaluation: Submit the completed protocol to an Institutional Review Board (IRB) or Research Ethics Board (REB) with appropriate expertise for approval, which is mandatory for publication in many international journals [43].
Visualization of Workflows
Digital Bioethics Platform Architecture
The diagram below illustrates the client-server architecture of a research platform designed to empower researchers in conducting digital bioethics experiments [38].
End-to-End Transparent Development
This workflow synthesizes principles from integrated drug development and empirical research to show a path for transparent research lifecycle management [52] [43] [51].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and tools for conducting transparent empirical bioethics research.
Table 2: Essential Research Reagents and Tools for Transparent Empirical Bioethics
| Item/Tool | Function in Research |
|---|---|
| Structured Protocol Template [43] | Provides a standardized framework for detailing a study's epistemology, methodology, ethical safeguards, and data integration plan, ensuring all critical elements are documented. |
| Digital Research Platform [38] | A modular software system that provides pre-implemented digital methods (e.g., for data collection and analysis), lowering the technical barrier for conducting digital bioethics studies. |
| Electronic Lab Notebook (ELN) [51] | A digital system for centrally recording experimental data, decisions, and rationales during the research process, creating a transparent and accessible development history. |
| Authentication & Authorization Infrastructure (AAI) [38] | Provides secure, centralized user authentication for research platforms, protecting data integrity and enabling controlled collaboration between researchers. |
| Clinical Study Reports (CSRs) & Summaries [50] | Detailed documents from clinical trials; making summaries publicly available (as tested in FDA pilots) increases transparency in the scientific basis for drug approvals and related ethical reviews. |
Interdisciplinary collaboration, particularly in fields like empirical bioethics, is essential for addressing complex problems in healthcare and drug development. However, these collaborations often face significant challenges arising from the differing epistemological frameworks that disciplines bring to a research project. Epistemological frameworks encompass the fundamental beliefs about what constitutes relevant phenomena to study, which methods to employ, what counts as sufficient evidence, and the ultimate value of the research findings [53]. In interdisciplinary teams, such as those involving philosophers, social scientists, natural scientists, and healthcare professionals, these differences can lead to what has been termed "disciplinary capture"—where the project's key decisions about methods, evidence, and research goals default to the framework of a single, often dominant, discipline [53]. This phenomenon can leave collaborators feeling that their expertise has been ignored or undervalued, ultimately undermining the collaborative potential.
The field of empirical bioethics exemplifies these challenges. As a discipline that seeks to integrate social scientific empirical data with normative ethical theorizing, it embodies the very epistemological tensions this guide explores [21]. A systematic review of empirical bioethics methodologies identified 32 distinct methodological approaches, which can be broadly categorized as either dialogical or consultative, representing two extreme poles of methodological orientation [21]. This heterogeneity reflects deeper meta-ethical and epistemological disagreements within moral philosophy and bioethical analysis. For researchers, scientists, and drug development professionals, successfully navigating this complex landscape requires a clear understanding of both the philosophical underpinnings and the practical methodological options available for conducting rigorous, integrated research.
Comparative Analysis of Empirical Bioethics Methodologies
The field of empirical bioethics has responded to the challenge of integration by developing a spectrum of methodological approaches. These approaches differ in how they manage epistemological differences, particularly regarding the locus of moral authority and the process of integrating empirical data with normative analysis.
Table 1: Comparative Methodological Approaches in Empirical Bioethics
| Methodology Type | Description | Epistemological Orientation | Key Features | Reported Strengths |
|---|---|---|---|---|
| Critical Applied Ethics [21] | Gives precedence to moral theory but allows empirical research to refine it. | Theory-led, with one-way accommodation to data. | Uses empirical data to inform premises or support factual claims within a theoretical framework. | Maintains strong theoretical grounding while being somewhat responsive to contextual realities. |
| Integrated Empirical Ethics [21] | Gives equal authority to both theory and data, allowing mutual adjustment. | Dialogical and reciprocal. | Iterative process where both theory and data interpretation are adjusted in light of each other. | Achieves genuine integration; produces conclusions that are both theoretically sound and contextually grounded. |
| Design Bioethics [54] | Uses purpose-built, engineered tools (e.g., digital games) for bioethics research. | Pragmatic and innovative; prioritizes ecological validity and engagement. | Creates immersive, interactive research environments to study moral decision-making in realistic contexts. | Enhances participant engagement and data authenticity; particularly effective for hard-to-reach groups like adolescents. |
A systematic review of the field highlights that the fundamental question concerning justificatory authority—how researchers can articulate why their conclusions should be considered better or worse than alternatives—remains unresolved [21]. This underscores that the choice of methodology is not merely technical but involves deep philosophical commitments about the nature of moral knowledge and how it is produced. When planning a study, researchers must therefore think carefully about the nature of the normative claims they wish to generate and how these align with their epistemological starting points [21].
Experimental Protocols in Empirical Bioethics
To illustrate how these methodological principles are applied in practice, this section details two contrasting experimental protocols from recent research. The first exemplifies the innovative "Design Bioethics" approach, while the second represents a more traditional, vignette-based method.
Protocol 1: Design Bioethics Approach using a Digital Game
A 2022 study pioneered the "Design Bioethics" methodology by creating and testing a digital game, "Tracing Tomorrow," against a standard vignette survey [54].
- Research Aim: To compare a purpose-built bioethics game with a standard vignette survey across several dimensions of participant engagement and ethical insight.
- Sample and Recruitment: The study recruited 301 UK adolescents aged 16-18 years via social media and research networks. Participants were randomized to either the game or survey condition [54].
- Intervention - Bioethics Game: "Tracing Tomorrow" is a digital game exploring digital phenotyping for mental health. It presents participants with a narrative containing ethically charged dilemmas and decisions, requiring them to make choices about what they would do in realistic scenarios (e.g., whether to disclose a mental health risk assessment to parents or friends). The game is interactive, personalized, and features a continuous narrative [54].
- Comparison - Vignette Survey: The control group completed a traditional online survey containing descriptively rich questions posing equivalent dilemmas about mental health tracking technologies. The questions and multiple-choice response options were identical to those in the game and presented in the same order, but lacked the interactivity, personalization, and narrative continuity [54].
- Outcome Measures: Quantitative measures were used to assess:
- Presence: The participant's sense of being in the environment created by the tool.
- Cognitive Absorption: A state of deep involvement, encompassing temporal dissociation, immersion, enjoyment, and control.
- Emotional Engagement.
- Mental Health Ethics Insight: Subjective judgment of gained understanding.
- Perceived Authenticity: The extent to which participants felt their answers reflected their own attitudes.
- Curiosity/Motivation: To learn more about the issues presented [54].
- Results: Participants in the game condition reported significantly greater presence, emotional engagement, cognitive absorption, and mental health ethics insight. Perceived authenticity and curiosity were equivalent between the two methods, demonstrating that the game achieved superior engagement without compromising authenticity [54].
Protocol 2: Traditional Vignette-Based Survey
This protocol outlines the standard methodology against which the Design Bioethics approach was compared.
- Research Aim: To gather data on ethical attitudes and decision-making using a traditional, static survey format.
- Methodology: A cross-sectional survey employing written vignettes (short, descriptive scenarios) of ethical dilemmas.
- Data Collection Instrument: A questionnaire containing one or more hypothetical, text-based scenarios. Each scenario is followed by a series of structured questions, often using Likert scales or multiple-choice formats to capture respondents' judgments, behavioral intentions, or ethical evaluations [54] [55].
- Procedure: Participants receive the survey electronically or on paper. They read the vignettes and independently select their responses without interaction or feedback from the research instrument.
- Analysis: Primarily quantitative, using statistical analyses (e.g., descriptive statistics, correlation analyses, regression models) to identify patterns, relationships, and group differences in the responses [55].
Diagram 1: Empirical Bioethics Workflow
The Scientist's Toolkit: Essential Reagents for Empirical Bioethics Research
Successful interdisciplinary research in empirical bioethics requires both conceptual and practical tools. The following table details key "research reagents" – the essential methodological components and frameworks needed to design and execute a rigorous study.
Table 2: Essential Research Reagents for Empirical Bioethics
| Research Reagent | Function | Application Context |
|---|---|---|
| Methodological Framework [21] | Provides the overarching structure and philosophical justification for integrating empirical and normative work. | Guides the entire research process, from design to justification of conclusions; e.g., choosing between Critical Applied Ethics or Integrated Empirical Ethics. |
| Typology of Research Strategies [21] [56] | Helps clarify the aims of the research and the relationship between data and theory (e.g., complete authority to theory vs. equal authority). | Used in the planning phase to align the team on the project's epistemological commitments and intended outcomes. |
| Integrated Evaluation Framework (e.g., CRAFT-MD) [56] | Offers a structured approach for testing and validating complex interventions in realistic, controlled environments. | Evaluating tools in clinical settings; uses simulated AI agents to interact with the tool being tested, focusing on natural dialogues. |
| Purpose-Built Research Tools (e.g., Tracing Tomorrow game) [54] | Creates immersive, engaging environments to study moral deliberation and decision-making with high ecological validity. | Investigating ethically complex topics where context and realism are crucial for generating authentic participant responses. |
| Protocol Template for Health Research [12] | Standardizes the reporting and planning of investigations in humanities and social sciences in health. | Ensuring methodological rigor and completeness in study design; suitable for quantitative, qualitative, and mixed-methods approaches. |
| Interdisciplinary Communication Norms [53] | Establishes shared expectations and practices for discussing epistemological differences and resolving disagreements. | Used throughout a project to prevent "disciplinary capture" and ensure all collaborators meaningfully shape the research. |
Navigating Epistemological Differences and Quality Control
The tension between interdisciplinary collaboration and maintaining rigorous quality control is a central challenge. This tension often arises because quality control mechanisms are typically discipline-specific, relying on established standards of evidence, peer review processes, and agreed-upon criteria for what constitutes valid knowledge [57]. In collaborative, interdisciplinary science, the distribution of cognitive resources among team members creates relations of epistemic dependence, where each researcher must trust the contributory expertise of others [57]. This interdependence challenges traditional, discipline-bound models of accountability and quality assurance.
To manage these tensions and avoid the pitfall of disciplinary capture, research teams should adopt proactive strategies [53]:
- Early Integration of Diverse Expertise: Involve all disciplines, particularly social scientists and ethicists, from the very inception of the project, not as add-ons but as core contributors to the research questions and design.
- Explicit Attention to Epistemological Frameworks: Create a space for open discussion about each collaborator's disciplinary assumptions, including their views on causation, evidence, and research goals.
- Institutional Support: Secure funding and institutional recognition that acknowledges the extra time and resources required for genuine epistemological integration.
- Adaptive Mindset: Cultivate an openness to importing and adapting concepts, methods, and standards of evidence from other disciplines to create a novel, fit-for-purpose methodological approach [53].
Engaging with these strategies meaningfully requires researchers to grapple with fundamental questions about what kinds of moral claims they want to make, how these claims can be justified, and what constitutes a coherent methodological process for achieving them [21]. While this heterogeneity in empirical bioethics can present a challenge to the field's legitimacy, it is also a source of richness and should be welcomed as a sign of methodological vitality.
Empirical bioethics is an interdisciplinary field that seeks to address bioethical questions by integrating empirical data about stakeholder values, attitudes, and experiences with normative ethical theorizing [21]. This integration promises to ground bioethical analysis in the realities of lived experience while maintaining systematic, critical reflection on how we ought to act [21] [58]. Despite several decades of development since the "empirical turn" in bioethics, the field continues to grapple with fundamental methodological challenges and competency gaps. A systematic review identified 32 distinct methodologies for integrating empirical and normative approaches, with most falling into either dialogical or consultative categories, representing two extreme poles of methodological orientation [21] [23]. This comparison guide examines current methodological approaches, their experimental validation, and the training resources needed to bridge persistent competency gaps in empirical bioethics research.
Comparative Analysis of Empirical Bioethics Methodologies
Traditional Versus Innovative Methodological Approaches
Table 1: Comparison of Traditional and Innovative Empirical Bioethics Methods
| Method Characteristic | Traditional Vignette Surveys | Interactive Digital Games | Text-Based Ethical Frameworks | Interactive Visualizations |
|---|---|---|---|---|
| Engagement Dimensions | Limited emotional engagement | High presence and cognitive absorption [54] | Standard knowledge transfer | Enhanced user experience [59] |
| Participant Insight | Moderate ethics insight | Greater mental health ethics insight [54] | Foundational understanding | Improved knowledge application [59] |
| Contextual Sensitivity | Limited context simulation | Rich, immersive environments [54] | Abstract principle presentation | Contextualized guidance |
| Methodological Flexibility | Fixed question-response format | Adaptive narrative structures [54] | Linear documentation | Interactive exploration [59] |
| Empirical-Normative Integration | Consultative (researcher-driven) | Potentially more integrated approaches | Theoretical foundation | Balanced theory-application [59] |
Experimental Validation of Methodological Innovations
Table 2: Experimental Outcomes of Innovative Bioethics Methods
| Experimental Measure | Traditional Method Performance | Innovative Method Performance | Statistical Significance | Sample Characteristics |
|---|---|---|---|---|
| Sense of Presence | Lower in vignette surveys [54] | Higher in digital games [54] | Statistically significant [54] | 301 UK adolescents [54] |
| Cognitive Absorption | Moderate engagement [54] | Deep involvement in games [54] | Statistically significant [54] | Randomized controlled trial [54] |
| Knowledge Acquisition | Text-only: baseline learning [59] | Interactive-visual: improved understanding [59] | Statistically significant [59] | 80 health researchers [59] |
| User Experience | Standard educational materials [59] | More pleasing episodic experience [59] | Statistically significant [59] | University-based participants [59] |
| Ethical Deliberation Support | Adequate for basic deliberation [59] | Effective for applied deliberation [59] | Equivalent performance [59] | Early-stage researchers [59] |
Detailed Experimental Protocols in Empirical Bioethics
Digital Game Versus Vignette Survey Protocol
A 2022 study directly compared a purpose-built "bioethics game" called "Tracing Tomorrow" with a standard vignette survey to investigate digital phenotyping for mental health in adolescent populations [54]. The experimental protocol was preregistered on the Open Science Framework and received ethics approval from the University of Oxford Medical Sciences Interdivisional Medical Ethics Committee [54].
The study employed a between-subjects design with 301 UK adolescents aged 16-18 years, randomly assigned to either the game condition (n=103) or the vignette survey condition (n=198) [54]. The digital game presented ethically charged dilemmas and decisions within an interactive narrative structure where participants made decisions about mental health risk assessment disclosure while having opportunities to access additional information on key themes [54]. The vignette survey presented descriptively equivalent questions and multiple-choice responses in a traditional online survey format, maintaining identical question order but lacking interactivity, personalization, and narrative continuity [54].
Primary outcome measures included sense of presence, emotional engagement, cognitive absorption, mental health ethics insight, perceived authenticity, and curiosity/motivation to learn more [54]. Quantitative measures were administered immediately after task completion, followed by qualitative questions about participants' experiences compared to previous surveys [54]. The study was powered at 0.80 with probability of type I error (α) set at 0.01, requiring a total sample of 296 to detect a small to medium effect size (d = 0.4) for two-tailed comparisons [54].
Interactive Visualization Versus Text-Only Framework Protocol
A 2023 randomized controlled trial compared interactive visualizations to text-only ethical frameworks as ethics learning tools for health researchers and professionals [59]. The study employed a pre-, mid-, and post-test design using the Qualtrics survey platform with 80 university-based early-stage health researchers randomly assigned to control (text-only document) or experimental (interactive-visual) conditions [59].
The experimental intervention transformed ethical framework content into an interactive-visual format, while the control condition presented equivalent content in a conventional text-only document format [59]. Primary outcome variables included learning (measured using a knowledge questionnaire), deliberation (assessed through case studies), and user experience (measured using the SED/UD Scale) [59]. Statistical analysis utilized descriptive statistics and mixed-effects linear regression to determine between-group differences [59].
Visualization of Empirical Bioethics Methodological Processes
Empirical Bioethics Research Workflow
Methodological Integration Approaches
Table 3: Essential Research Reagents for Empirical Bioethics
| Tool Category | Specific Methods | Function in Research | Application Context |
|---|---|---|---|
| Data Collection Reagents | Semi-structured interviews [60] | Elicit rich qualitative data on moral experiences | Exploring stakeholder perspectives |
| Digital games (e.g., Tracing Tomorrow) [54] | Create immersive environments for ethical decision-making | Studying moral deliberation in context | |
| Vignette surveys [54] | Present standardized ethical scenarios | Comparing responses across populations | |
| Integration Frameworks | Reflective equilibrium [60] | Systematic back-and-forth between theory and data | Researcher-driven normative analysis |
| Dialogical methods [60] | Facilitate collaborative deliberation | Participatory ethics with stakeholders | |
| Reflexive balancing [9] | Critical reflection on methodological assumptions | Ensuring methodological coherence | |
| Analysis Tools | Thematic analysis [60] | Identify patterns in qualitative data | Interpreting empirical findings |
| Ethical framework analysis [59] | Apply theoretical frameworks to empirical data | Normative analysis of empirical findings | |
| Interactive visualizations [59] | Translate ethical concepts into accessible formats | Ethics education and deliberation |
Discussion: Addressing Competency Gaps Through Training
The comparative analysis reveals significant differences in how methodological approaches facilitate the integration of empirical and normative components, which represents a central competency challenge in empirical bioethics [60]. Despite the proliferation of methodologies, researchers report uncertainty and vagueness about how to practically implement integration, describing the process as challenging and often obscure [60]. This methodological indeterminacy represents a double-edged sword—allowing flexibility but potentially obscuring insufficient understanding of theoretical-methodological foundations [60].
The experimental evidence demonstrates that innovative methods like digital games and interactive visualizations can enhance engagement, understanding, and application of ethical knowledge compared to traditional approaches [54] [59]. However, these tools require specialized competencies in both empirical methods and normative analysis that extend beyond conventional disciplinary training. A proposed "theoretical turn" in empirical bioethics emphasizes more deliberate integration of empirical methods with philosophical theory to better fulfill the distinctive aims of bioethics as a practically oriented, normative inquiry [15].
Specialized training opportunities like the Empirical Bioethics Summer School (Amsterdam, June 2025) address these competency gaps by providing beginner/intermediate level courses focusing on understanding empirical bioethics typologies, research design, empirical methods, and methodological approaches to integration [6]. Such training emphasizes developing researchers' ability to clearly articulate how theoretical positions are selected for integration, explain and justify integration methods, and transparently report how integration is executed [6] [60].
The comparison of empirical bioethics methodologies reveals a rapidly evolving field with increasing methodological sophistication and experimental validation of innovative approaches. While traditional methods like vignette surveys and interviews remain valuable, evidence suggests that purpose-built digital tools like interactive games and visualizations can enhance engagement, understanding, and contextual sensitivity when addressing ethical questions. The persistent competency gaps in integrating empirical and normative components highlight the need for specialized training that moves beyond binary thinking about the empirical and normative toward genuinely interdisciplinary approaches. As the field continues to develop, researchers must carefully consider the nature of the claims they wish to generate and select methodologies that align with their research aims while maintaining transparency about the integration process. Future methodological development should focus on refining integration techniques, validating innovative tools across diverse populations, and enhancing training opportunities that bridge the empirical-normative divide.
Empirical bioethics is a rapidly evolving field that integrates empirical research methods with ethical analysis to address complex problems in health and medicine. This guide provides a structured comparison of the practical hurdles researchers face, focusing on three core areas: securing funding in a volatile landscape, navigating the institutional review board (IRB) process, and meeting modern publication expectations for transparency. Aimed at researchers, scientists, and drug development professionals, this analysis uses current data and protocols to offer a realistic overview of the research environment. The guide is framed within a broader thesis on comparative empirical bioethics methodologies, providing a foundational understanding of the operational challenges and their potential solutions.
Funding Landscape Comparison
The funding environment for scientific research, particularly in the United States, has undergone significant disruption in 2025. Researchers must now navigate a landscape characterized by uncertainty and new types of risks. The following table summarizes the key dimensions of this challenge.
Table 1: Comparative Analysis of the 2025 Research Funding Landscape
| Aspect | Traditional Federal Funding (Pre-2025) | Current Funding Environment (2025) |
|---|---|---|
| Primary Source | Stable federal grants from agencies like NSF and NIH [61]. | Unreliable federal sources; emergence of venture capital, private foundations, and foreign institutions [61] [62]. |
| Predictability | Reliable, multi-year grant cycles and review panels [63]. | High uncertainty; federal grants terminated, reviews suspended, and institutional budget cuts [61] [64]. |
| Impact on Personnel | Supported graduate students and postdocs with stipends [61]. | Graduate admissions revoked; researchers fired; labs downsized or closed [61] [64]. |
| Research Focus | Broad support for basic research and specific public health priorities [64]. | Topic-specific terminations (e.g., DEI, climate change, LGBTQ+ health); shift towards applied, industry-aligned research [61] [64]. |
| Geopolitical Impact | The U.S. as a primary destination for global scientific talent [61]. | "Brain drain" as U.S. students and researchers seek opportunities abroad [61] [64]. |
The human and institutional impacts of these funding shifts are profound. A survey of hundreds of biomedical researchers revealed a widespread "sense of doom," with reports of severe anxiety, low morale, and career changes driven by financial insecurity [64]. The instability forces difficult decisions, from reducing graduate student admissions to considering relocation to countries with more robust scientific investment, such as those in Europe [61] [64]. For institutions, the National Association of College and University Business Officers (NACUBO) identifies "Managing Unreliable Funding Sources" as the top concern for 2025, forcing real-time financial decisions and improvisation [62].
Institutional Review Board (IRB) Workflow
The IRB is formally designated to review and monitor biomedical research involving human subjects to protect their rights and welfare [65]. Navigating this process is a critical step for any empirical bioethics study. The following workflow diagram and accompanying explanation outline the key stages from preparation to approval.
Diagram 1: IRB Review and Approval Workflow.
Workflow Stages Explained
- Preparation (Develop Protocol): Before submission, researchers must prepare a detailed research protocol and informed consent documents. A newly formalized template is available for empirical bioethics and other health-related investigations, adapting standards for reporting qualitative research to be suitable for quantitative and mixed-methods approaches [12].
- Submission and Review (Submit to IRB): The IRB review is a group process. A convened meeting must have a quorum of members present, including at least one scientist and one non-scientist [65]. Members with conflicting interests must abstain from review and voting [65].
- IRB Decision (Decision): The IRB can approve, require modifications, or disapprove the research [65]. For multi-site studies, the NIH Single IRB policy often mandates using a central IRB to streamline ethical review [66].
Publication & Transparency Standards
Journal publication expectations have increasingly emphasized transparency and open science. The Transparency and Openness Promotion (TOP) Guidelines, updated in 2025, provide a key framework that journals are adopting. The guidelines offer a structured approach to making research more verifiable.
Table 2: TOP 2025 Guidelines: Key Research Practices and Implementation Levels
| Research Practice | Level 1: Disclosed | Level 2: Shared & Cited | Level 3: Certified |
|---|---|---|---|
| Study Registration | Author states if/where registered [67]. | Study is registered, and citation is provided [67]. | Independent party certifies timely/complete registration [67]. |
| Data Transparency | Author states if/where data are available [67]. | Data are cited from a trusted repository [67]. | Independent party certifies data and metadata deposition [67]. |
| Analysis Code Transparency | Author states if/where code is available [67]. | Analytic code is cited from a trusted repository [67]. | Independent party certifies code deposition and documentation [67]. |
| Study Protocol | Author states if/where protocol is available [67]. | Study protocol is publicly shared and cited [67]. | Independent party certifies protocol was shared timely and is complete [67]. |
Beyond these research practices, the TOP framework introduces Verification Practices like Results Transparency and Computational Reproducibility, where an independent party verifies that results are reported completely and can be reproduced with the shared data and code [67]. It also promotes specific Verification Study types, such as Replication and Registered Reports, which are designed to strengthen the evidence base of published findings [67].
Experimental Protocols & Reagent Solutions
Detailed Methodology for an Empirical Bioethics Study
The following protocol is adapted from the health research protocol template suitable for empirical bioethics [12].
- 1. Research Question & Background: Define the specific ethical dilemma and the empirical question to be investigated. Justify the need for an integrated empirical-ethical approach and summarize the relevant scholarly literature.
- 2. Study Design: Select and describe the methodology (e.g., qualitative interviews, quantitative surveys, mixed-methods). Explain why this design is appropriate for addressing both the empirical and normative components of the research question.
- 3. Participant Recruitment: Detail the sampling strategy (e.g., purposive, random), inclusion/exclusion criteria, and recruitment procedures. Justify the sample size.
- 4. Data Collection: For qualitative components, describe the interview guide or observation framework. For quantitative components, specify the survey instruments or data extraction tools. All data collection procedures must be approved by the IRB.
- 5. Data Analysis: Outline the plan for analyzing empirical data (e.g., thematic analysis, statistical tests) and the method for integrating findings with ethical analysis (e.g., reflective equilibrium, principlism).
- 6. Ethical Considerations: Submit the full protocol, consent forms, and data management plan for approval by the relevant IRB. The protocol should explicitly address confidentiality, data security, and conflict of interest [65] [12].
Research Reagent Solutions
In empirical bioethics, "reagents" are often methodological tools rather than laboratory chemicals. The following table details essential resources for navigating the core practical hurdles.
Table 3: Key Research Reagent Solutions for Empirical Bioethics
| Item | Function | Example/Source |
|---|---|---|
| Health Research Protocol Template | Provides a structured, adaptable outline for writing research protocols suitable for humanities and social sciences in health, including empirical bioethics [12]. | Template from Stoeklé et al. (2025), adapted from the Standards for Reporting Qualitative Research (SRQR) [12]. |
| IRB Written Procedures | Documents the institution's specific policies for initial and continuing review, meeting conduct, and informed consent, which investigators must follow [65]. | Local Institutional Review Board. |
| TOP Guidelines Framework | A policy framework used by journals and funders to implement open science standards, increasing the verifiability of research claims [67]. | Center for Open Science (COS) [67]. |
| myIDP Tool | A self-directed online tool for career exploration and planning, crucial for researchers navigating an uncertain funding and job market [61]. | myIDP.sciencecareers.org |
| Single IRB (sIRB) | For multi-site studies, a centralized IRB review mechanism that avoids duplicate reviews, improving efficiency as required by policies like the NIH sIRB mandate [66]. | NIH Policy on sIRB Use [66]. |
In the evolving field of empirical bioethics, the explicit justification and strategic integration of methodological choices is paramount for advancing robust research. As biomedical research increasingly involves complex scenarios—from real-world experimentation with emerging technologies to the application of blockchain for ethical goals—researchers face mounting pressure to employ methodologies that are both transparent and effective [68] [69]. This guide provides a comparative analysis of prominent methodological approaches, supported by experimental data and detailed protocols, to equip researchers and drug development professionals with the tools needed for rigorous comparative study in empirical bioethics.
Comparative Analysis of Methodological Performance
The table below summarizes the core characteristics and performance metrics of key methodologies relevant to empirical bioethics research, based on current literature and experimental findings.
Table 1: Comparative Performance of Methodological Approaches in Bioethics Research
| Methodology | Primary Application Context | Reported Efficacy/Performance | Key Strengths | Notable Limitations |
|---|---|---|---|---|
| BrainSwarming | Innovative idea generation for conceptual goals and intangible resources [68] | 115 ideas in 15 minutes vs. 100 ideas in 60 minutes for traditional brainstorming [68] | Overcomes psychological obstacles to innovation; effective for abstract problems [68] | Requires facilitation; may need adaptation for highly technical domains |
| Generic Parts Technique (GPT) | Engineering and design problems; enhancing creative problem-solving [68] | 67.4% more likely to solve insight problems than controls (Cohen’s d = 1.59) [68] | Systematically helps notice obscure features; reduces functional fixedness [68] | May be less intuitive for novices; requires training |
| Scoping Review | Mapping empirical research landscapes and identifying research gaps [70] | Effective for disparate, cross-disciplinary literature (e.g., REB membership research) [70] | Provides comprehensive overview of research fields; identifies evidence gaps [70] | Time-intensive; may not assess quality of included studies |
| Real-World Experimentation Ethics | Emerging technology testing (e.g., autonomous vehicles, smart cities) [69] | Identifies problematic inconsistencies in research ethics demands [69] | Addresses gaps in current research ethics guidelines for novel technologies [69] | Lack of standardized regulatory frameworks; ethical risks |
Detailed Experimental Protocols
BrainSwarming Protocol for Bioethical Problem-Solving
BrainSwarming represents an Innovation Enhancing Technique (IET) that visually maps problem-solving through a two-dimensional graph, particularly effective for addressing conceptual goals in bioethics [68].
Experimental Workflow:
- Problem Definition: Place a short description of the ultimate goal (e.g., "furthering ethical goals in biomedicine") at the top of the graph.
- Resource Identification: List all available resources (e.g., "blockchain technology") at the bottom of the graph.
- Goal Refinement: Iteratively break down the primary goal into more specific, refined sub-goals, creating a downward network. For bioethics, this may involve specifying the four principles of biomedical ethics: beneficence, justice, autonomy, and non-maleficence [68].
- Resource Decomposition: Use techniques like the Generic Parts Technique (GPT) to break resources into their fundamental components and features. For blockchain, this includes elements like Immutable Audit Trail, Consensus Mechanism, and Smart Contracts [68].
- Solution Path Identification: Draw connecting lines between refined goals and resource components where they intersect to form potential solutions. This process successfully identified 100 potential solutions for applying blockchain to bioethical goals in a documented case study [68].
Diagram 1: BrainSwarming Methodology Workflow
Generic Parts Technique (GPT) Protocol
The Generic Parts Technique is a systematic approach to overcoming functional fixedness by reinterpreting resources through decomposition and neutral redescription [68].
Experimental Workflow:
- Decomposition: For each resource object, ask: "Can this object be broken down further?" If yes, decompose it into its constituent parts.
- Neutral Redescription: For each part, ask: "Does this description imply a use?" If yes, reframe the description in neutral, non-functional terms to avoid preconceived notions of utility.
- Iteration: Repeat this two-step process until no further meaningful decomposition or neutral redescription is possible. This process can utilize dictionary definitions or etymology when direct decomposition is challenging [68].
Scoping Review Methodology for REB Membership Analysis
Scoping reviews are particularly valuable for mapping disparate empirical research on topics such as Research Ethics Board (REB) membership and expertise [70].
Experimental Workflow:
- Identify Research Questions: Define clear questions focused on describing the current state of literature and identifying research gaps.
- Identify Relevant Studies: Conduct systematic searches across multiple databases (e.g., PubMed, PsychINFO, Scopus) using comprehensive search terms, supplemented by hand-searching key journals.
- Study Selection: Apply predetermined eligibility criteria to titles, abstracts, and full texts, with multiple reviewers to minimize bias.
- Chart Data: Extract relevant variables using a standardized data charting form developed by the research team.
- Collate and Summarize: Synthesize results through descriptive analysis and thematic summary, focusing on patterns in the evidence related to the research questions [70].
The Scientist's Toolkit: Essential Research Reagents
The table below details key methodological tools and their functions for empirical bioethics research.
Table 2: Essential Reagents for Empirical Bioethics Methodological Research
| Research Reagent/Tool | Primary Function | Application Context |
|---|---|---|
| BrainSwarming Graph | Visualizes problem-solving pathways and facilitates simultaneous idea generation [68] | Generating innovative solutions to conceptual bioethics problems [68] |
| Generic Parts Technique (GPT) | Helps overcome functional fixedness by decomposing resources into neutral components [68] | Enhancing creative problem-solving in research design and ethics protocol development [68] |
| Scoping Review Framework | Maps existing literature and identifies research gaps in emerging or complex topics [70] | Systematic analysis of empirical research on REB composition, training, and expertise [70] |
| Citation Analysis Taxonomy | Categorizes how empirical findings are applied in tool design research [71] | Understanding knowledge translation between empirical research and practical applications [71] |
| WCAG Contrast Guidelines | Ensures visual materials meet accessibility standards for diverse audiences [72] [73] | Creating inclusive research dissemination materials and accessible data visualizations [74] |
The strategic selection and explicit justification of methodological approaches is fundamental to advancing empirical bioethics research. Techniques like BrainSwarming and GPT offer structured pathways for innovative problem-solving, while systematic approaches like scoping reviews provide comprehensive landscape analyses of existing evidence. By employing these methodologies with transparency and rigor, researchers can enhance the quality, reproducibility, and impact of their work in the complex intersection of ethics, science, and technology development.
Assessing Methodological Rigor and Exploring Future Directions
Empirical bioethics has emerged as a critical interdisciplinary field that integrates social scientific research with normative ethical analysis to address complex problems in healthcare and medicine. However, this interdisciplinarity has presented significant challenges, with the field characterized by considerable methodological diversity and heterogeneity. A systematic review identified 32 distinct methodologies within empirical bioethics, creating challenges for researchers, funders, and journals in evaluating quality and coherence [21]. As Davies et al. warned, "The shortcuts that can be taken when explaining and justifying work undertaken within clear disciplinary silos are not available to empirical bioethics. There is no standard approach to cite, there is no accepted methodology or set of methods to fall back on" [75].
In response to these challenges, a consensus project was undertaken with 16 academics from 5 European countries, representing diverse disciplinary backgrounds, who sought to generate and reach agreement on standards of practice for empirical bioethics research [75]. Using a modified Delphi approach, this project succeeded in establishing 15 consensus standards organized into 6 domains of research practice [75]. These standards provide a crucial framework for validating research quality in an increasingly important field that spans the interests of researchers, scientists, and drug development professionals engaged in evidence-based ethical analysis.
The Consensus Development Process: A Modified Delphi Approach
The consensus process that generated the 15 standards employed a rigorous modified Delphi technique, which is a well-established structured method for achieving consensus among experts [75]. Unlike traditional Delphi methods that maintain participant anonymity through multiple questionnaire rounds, this adaptation utilized facilitated group discussions at the Brocher Foundation in May 2015. This modification allowed for immediate clarification of ambiguous or controversial issues—particularly valuable given the conceptual and linguistic diversity of the international participants, many of whom were working in a second language [75].
The process involved multiple rounds of discussion and refinement, with participants able to immediately respond and seek clarification on contentious points. This approach facilitated a nuanced understanding of disagreements and ultimately enabled the diverse group of scholars to reach consensus on all 15 standards outlined in the final report [75]. The success of this process is particularly notable given the radical differences in methodological commitments and views about the nature of ethics among participants [76].
The 15 Consensus Standards: Domains and Applications
The 15 consensus standards are organized into six domains that represent key aspects of empirical bioethics research practice. These domains provide a comprehensive framework for designing, conducting, and evaluating empirical bioethics research.
Domain 1: Aims
The standards in this domain establish the fundamental orientation of empirical bioethics research.
Standard 1: The research should "address a normative issue that is oriented towards practice" [76]. This positions empirical bioethics as fundamentally concerned with practical ethical challenges rather than abstract theoretical questions.
Standard 2: The research must "integrate empirical methods with ethical argument in order to address this normative issue" [76]. This establishes the interdisciplinary nature of genuine empirical bioethics work.
Standard 3: Researchers should "clearly state the normative issue and explain why it is important" [75]. This ensures transparency about the research's ethical significance.
Domain 2: Questions
This domain focuses on the formulation of research questions that properly bridge the empirical-normative divide.
Standard 4: Research questions should be "answerable through integration" of empirical and normative approaches [75].
Standard 5: The questions must be "appropriate for the stated aims" of the research [75].
Domain 3: Integration
Integration represents the core methodological challenge in empirical bioethics, and this domain contains several critical standards.
Standard 6: Researchers must "clearly state and justify the theoretical position that informs their approach to integration" [75].
Standard 7: The "method of integration should be explained and justified" [75].
Standard 8: Researchers should "be transparent in informing how the method of integration was executed" [75].
Domain 4: Conduct of Empirical Work
These standards address the empirical component of the research.
Standard 9: The "empirical methods should be appropriate for the empirical questions" [75].
Standard 10: The "empirical methods should be employed rigorously" according to disciplinary standards [75].
Domain 5: Conduct of Normative Work
These standards address the philosophical or ethical component of the research.
Standard 11: The "normative approach should be appropriate for the normative questions" [75].
Standard 12: The "normative approach should be employed rigorously" according to disciplinary standards [75].
Domain 6: Training and Expertise
These final standards address the competencies required for conducting interdisciplinary empirical bioethics research.
Standard 13: The "research team should have appropriate expertise in, or understanding of, the relevant empirical methods" [75].
Standard 14: The "research team should have appropriate expertise in, or understanding of, the relevant normative methods" [75].
Standard 15: The "research team should have appropriate expertise in, or understanding of, the method of integration" [75].
Table 1: The 15 Consensus Standards for Empirical Bioethics Research
| Domain | Standard Number | Key Requirement |
|---|---|---|
| Aims | 1 | Address a practice-oriented normative issue |
| 2 | Integrate empirical methods with ethical argument | |
| 3 | Clearly state and explain the normative issue's importance | |
| Questions | 4 | Formulate questions answerable through integration |
| 5 | Ensure questions align with stated aims | |
| Integration | 6 | State and justify theoretical position on integration |
| 7 | Explain and justify method of integration | |
| 8 | Be transparent about execution of integration | |
| Conduct of Empirical Work | 9 | Use empirical methods appropriate to questions |
| 10 | Employ empirical methods rigorously | |
| Conduct of Normative Work | 11 | Use normative approaches appropriate to questions |
| 12 | Employ normative approaches rigorously | |
| Training & Expertise | 13 | Have appropriate empirical expertise |
| 14 | Have appropriate normative expertise | |
| 15 | Have appropriate integration expertise |
Methodological Approaches to Integration: A Comparative Analysis
The consensus standards provide a framework for evaluating research quality, but they operate alongside diverse methodological approaches to the central challenge of integration—the process of combining empirical findings with normative analysis. Research with bioethics scholars reveals that integration often remains challenging in practice, with many researchers describing an "air of uncertainty and overall vagueness" in their approaches [20].
Three Primary Methodological Orientations
Systematic analysis of empirical bioethics methodologies has identified three primary orientations toward integration, each with distinct approaches to justifying normative conclusions [21]:
Table 2: Methodological Approaches to Empirical-Normative Integration
| Methodological Approach | Definition | Key Characteristics | Examples |
|---|---|---|---|
| Consultative | Researcher analyzes data independently to develop normative conclusions | Researcher as external thinker; Relies on philosophical methods | Reflective Equilibrium [20] |
| Dialogical | Relies on stakeholder dialogue to reach shared understanding | Collaborative process; Emphasis on mutual learning | Inter-ethics [21] |
| Inherent Integration | Normative and empirical are intertwined from project inception | Rejects empirical/normative binary; Co-constitutive approach | Feminist epistemology [9] |
The Reflexive Balancing Methodology
One particularly developed methodology that exemplifies the consultative approach is Reflexive Balancing, which provides a detailed experimental protocol for integration:
Phase 1: Initial Position Mapping
- Identify and articulate preliminary moral judgments about the research topic
- Formulate initial ethical principles and theories relevant to the issue
- Acknowledge and document pre-existing biases and assumptions
Phase 2: Empirical Data Collection
- Employ rigorous qualitative or quantitative methods to gather relevant facts
- Focus on understanding lived experiences, practices, and contexts
- Maintain openness to challenging initial assumptions
Phase 3: Iterative Reconciliation
- Systematically compare empirical findings with initial moral judgments
- Identify points of coherence and tension between facts and values
- Adjust both moral judgments and principle interpretations in response
- Continue process until equilibrium is achieved
Phase 4: Normative Conclusion Justification
- Articulate the refined normative position reached through balancing
- Provide transparent account of how empirical data influenced conclusions
- Demonstrate coherence of final position [20]
Visualization of Research Workflows and Methodological Relationships
The following diagrams illustrate key workflows and relationships in empirical bioethics research, helping to visualize how the consensus standards apply throughout the research process.
Empirical Bioethics Research Workflow
Methodological Approaches to Integration
Essential Research Reagents: Tools for Empirical Bioethics
Conducting rigorous empirical bioethics research requires specific methodological "reagents" or tools. The following table details essential components for designing studies that meet the consensus standards.
Table 3: Essential Research Reagents for Empirical Bioethics
| Research Reagent | Function | Application Context |
|---|---|---|
| Qualitative Interview Protocols | Elicit rich data on moral experiences and reasoning | Understanding contextual factors in ethical decision-making |
| Structured Ethical Dilemma Scenarios | Present standardized ethical challenges for response | Comparative analysis of moral reasoning across groups |
| Reflective Equilibrium Framework | Systematically reconcile facts with moral judgments | Consultative integration approaches |
| Stakeholder Deliberation Guides | Facilitate structured dialogue among diverse participants | Dialogical integration methods |
| Normative Analysis Templates | Guide systematic ethical analysis using philosophical frameworks | Applying theoretical ethics to empirical findings |
| Integration Transparency Checklists | Document how empirical and normative elements are connected | Ensuring methodological rigor and accountability |
The 15 consensus standards for empirical bioethics represent a significant achievement in the maturation of a heterogeneous field. By providing a structured framework for evaluating research quality across six domains of research practice, these standards address fundamental challenges of interdisciplinary work that integrates empirical and normative approaches. The continuing development of specific methodological approaches—including consultative, dialogical, and inherent integration methods—provides researchers with multiple pathways to meet these standards while maintaining flexibility for innovation.
For researchers, scientists, and drug development professionals, these standards offer a validation toolkit for designing, conducting, and evaluating empirical bioethics research. The ongoing refinement of these standards through critical engagement and practical application will continue to enhance the rigor, transparency, and practical relevance of empirical bioethics in addressing complex ethical challenges in healthcare and medicine [75] [76]. As the field continues to evolve, the consensus standards provide a stable foundation for validating research quality while accommodating methodological diversity and innovation.
Empirical bioethics is an interdisciplinary field that addresses ethical issues in healthcare and the life sciences by integrating empirical data from the social sciences with normative, philosophical analysis [21] [77]. This integration promises to ground ethical reflection in the realities of lived experience, making it more relevant and applicable to complex practical dilemmas [78] [20]. Despite its growth, the field is characterized by a striking heterogeneity of methodologies, with one systematic review identifying 32 distinct approaches [21] [79]. This comparative guide objectively examines the primary methodological families, their operational protocols, and their relative strengths and limitations to inform researchers, scientists, and drug development professionals in their study design.
A Landscape of Methodological Approaches
The multitude of methodologies in empirical bioethics can be broadly categorized based on how and where the integration between empirical data and normative analysis occurs. The following diagram maps the primary methodological families and their relationships.
Diagram 1: A typology of empirical bioethics methodologies.
These approaches differ fundamentally in their locus of moral authority—that is, whether the normative conclusion is developed primarily by the researcher or emerges from a collaborative process with stakeholders [21] [20].
Comparative Analysis of Methodological Families
The table below provides a detailed comparison of the three main methodological families, weighing their key characteristics, strengths, and limitations.
| Methodological Family | Key Characteristics & Experimental Protocol | Strengths | Limitations |
|---|---|---|---|
| Consultative (Researcher-Driven) | Protocol: The researcher independently collects empirical data (e.g., via interviews or surveys) and then performs a normative analysis. The "integration" is a back-and-forth process of adjustment within the researcher's own thinking, often using a framework like Reflective Equilibrium [20]. | • Produces clearly argued normative conclusions [21].• Leverages expert knowledge in ethical theory [21].• Method is managed by a single researcher or team. | • Risk of researcher bias dominating the analysis [20].• Can be perceived as "top-down" or less democratic [21].• The process of integration can feel vague and difficult to articulate [20]. |
| Dialogical (Stakeholder-Driven) | Protocol: Stakeholders (e.g., patients, clinicians) are engaged in structured, facilitated dialogues (e.g., Moral Case Deliberation). The normative conclusion is forged through collective discussion, with the researcher acting as a facilitator rather than sole authority [21] [20]. | • Conclusions are directly grounded in stakeholder experiences and values [21].• Enhances the democratic legitimacy and practical relevance of outcomes [21].• Makes the normative reasoning process transparent and collaborative. | • Can be logistically challenging and time-consuming to organize [21].• May not produce a single, generalizable normative theory [21].• Requires specific skills in facilitation and group dynamics. |
| Inherent Integration | Protocol: The empirical and normative dimensions are intertwined from the start of the research project. For example, in Symbiotic Ethics, empirical work is designed to explicitly explore the normative dimensions of a practice, and ethical analysis is refined in continuous dialogue with the data [20]. Digital Bioethics uses computational methods to analyze online ethical debates [80]. | • Avoids the "add-on" feel of other methods, creating a more cohesive research design [20].• Can access novel data sources (e.g., public online discourse) [80].• Potentially offers a more naturalistic understanding of ethics-in-practice. | • The methodology can be complex and difficult to describe with clarity [20].• May be challenging for reviewers and funders from traditional disciplines to evaluate [21].• Digital methods raise new ethical concerns about privacy and data use [80]. |
Standards for High-Quality Empirical Bioethics Research
In response to the methodological diversity and challenges of integration, a European consensus project established 15 standards of practice to guide researchers in producing high-quality work [81]. These standards are organized into six domains, providing a practical checklist for research design, execution, and reporting.
Diagram 2: Domains and standards for empirical bioethics research [81].
The Researcher's Toolkit: Essential Methodological Components
Successful empirical bioethics research requires the strategic use of specific "reagents" or methodological components. The table below details key tools and their functions in the research process.
| Research Component | Function in Empirical Bioethics |
|---|---|
| Reflective Equilibrium | A core philosophical method where the researcher iteratively moves back and forth between ethical principles, case judgements, and empirical data to achieve a coherent moral position [20]. |
| Structured Dialogues | Facilitated discussions (e.g., Moral Case Deliberation) used in dialogical approaches to generate shared understanding and normative conclusions among stakeholders [21] [20]. |
| Qualitative Interviews | A primary empirical method for collecting in-depth, nuanced data on stakeholder experiences, values, and reasoning, providing the rich context for normative analysis [77]. |
| Systematic Reviews | Used to map and synthesize existing methodological or ethical literature, providing a justified foundation for a study's normative and empirical components [21]. |
| Computational Social Science Methods | A set of emerging techniques in Digital Bioethics for collecting and analyzing large-scale digital data (e.g., from social media) to understand how public bioethical debates unfold online [80]. |
The empirical bioethics landscape offers a spectrum of methodologies, each with a distinct profile of strengths and weaknesses. The choice of approach is not neutral; it hinges on the nature of the research question and the kind of normative claim the researcher seeks to make [21]. Consultative methods offer analytical rigor, dialogical approaches enhance democratic legitimacy, and inherent integration strives for a more naturalistic fusion of facts and values.
The future of the field lies in researchers making transparent and justified methodological choices, clearly articulating how they navigate the challenges of integration [20] [81]. While methodological plurality is a strength, adherence to emerging standards of practice is crucial for ensuring the rigor, credibility, and impact of empirical bioethics research [81]. For researchers in drug development and healthcare, selecting a methodology aligned with their specific aims is the critical first step in producing ethical analyses that are both philosophically sound and genuinely applicable to real-world challenges.
The field of bioethics has witnessed a significant transformation over recent decades, characterized by an increasing incorporation of empirical research methods into traditionally normative inquiries. This "empirical turn" represents a fundamental shift in how bioethicists approach their research, moving beyond purely philosophical analysis to embrace data-driven insights from the social sciences. Empirical bioethics has emerged as an interdisciplinary endeavor that seeks to integrate empirical findings regarding stakeholder values, attitudes, beliefs, and experiences with normative ethical theorizing [21]. The growing prevalence of this approach reflects a recognition that ethical analysis must be grounded in the realities of lived experience and contextual understanding to effectively address complex bioethical issues in healthcare and biomedicine.
The rise of empirical bioethics can be seen as a response to the social science critique of philosophical bioethics, which challenged what was perceived as insufficient attention to contextual factors in traditional bioethical analysis [21]. This has resulted in what many scholars now describe as a distinct "empirical turn" in bioethics, marked by not only an increase in empirical studies but also the emergence of dedicated journals and methodological frameworks supporting this integrative approach [82]. As the field continues to evolve, understanding how bioethicists actually use and integrate empirical methods becomes crucial for assessing the current state and future trajectory of bioethics research.
Quantitative Landscape of Empirical Methods in Bioethics
Prevalence and Growth of Empirical Research
The integration of empirical methods into bioethics has demonstrated substantial growth over time. A comprehensive quantitative analysis of nine peer-reviewed bioethics journals between 1990 and 2003 revealed a significant increase in empirical research publications, rising from 5.4% in 1990 to 15.3% by 2003 [10]. Statistical analysis confirmed this growth was significant (χ2 = 49.0264, p<.0001), with the period 1997-2003 showing a higher number of empirical studies (n = 309) compared to 1990-1996 (n = 126) [10]. This trend has likely continued, with more recent surveys indicating that the majority of bioethics researchers (87.5%) now report using or having used empirical methods in their work [82].
Table 1: Prevalence of Empirical Research in Bioethics Journals (1990-2003)
| Time Period | Number of Empirical Studies | Percentage of Total Publications |
|---|---|---|
| 1990 | Not specified | 5.4% |
| 1990-1996 | 126 | Not specified |
| 1997-2003 | 309 | Not specified |
| 2003 | Not specified | 15.3% |
The distribution of empirical research across bioethics journals appears uneven. The same study found that three journals accounted for the majority (84.1%) of empirical research in bioethics: Nursing Ethics (39.5%, n = 145), Journal of Medical Ethics (16.8%, n = 128), and Journal of Clinical Ethics (15.4%, n = 93) [10]. This concentration suggests that certain subfields or disciplinary orientations within bioethics may be more receptive to empirical approaches than others.
Current Usage Patterns and Methodological Training
Contemporary survey data from a study of 200 bioethics researchers across 12 European countries provides detailed insights into current usage patterns and methodological competencies:
Table 2: Empirical Methods Usage and Training Among Bioethics Researchers
| Aspect Surveyed | Findings | Percentage |
|---|---|---|
| Use of empirical methods | Use or have used empirical methods | 87.5% (n=175) |
| Training in qualitative methods | Received at least some training | 61.0% |
| Training in quantitative methods | Received at least some training | 59.0% |
| Methodological expertise | Self-identify as experts in methods they use | 6% or less |
| Lack of training among users | Used empirical methods without methodological training | 22.9% |
| Integration experience | Have integrated empirical data with normative analysis | 35.0% |
| Future integration plans | Plan to integrate in current projects | 59.8% |
The data reveals several important patterns. First, while the vast majority of bioethicists engage with empirical methods, a significant portion (22.9%) do so without having received formal methodological training [82]. Second, the proportion of researchers who consider themselves experts in the methods they use is remarkably low (6% or less), suggesting a potential confidence gap or recognition of methodological complexity [82]. Third, there appears to be a substantial intention-action gap regarding integration, with nearly 60% of researchers planning to integrate empirical data with normative analysis in current projects, compared to only 35% who reported having done so in the past [82].
Methodological Approaches and Integration Frameworks
Spectrum of Empirical Bioethics Methodologies
A systematic review of empirical bioethics methodologies identified 32 distinct methodologies for integrating empirical research with normative analysis [23] [21]. These methodologies can be broadly categorized based on their epistemological orientations and approaches to moral authority. The majority of these methodologies (n = 22) can be classified as either dialogical or consultative, representing two extreme poles of methodological orientation [21].
Dialogical approaches emphasize stakeholder participation and collaborative meaning-making, often drawing on deliberative democratic principles or hermeneutic traditions. These methodologies include approaches such as "dialogical empirical ethics" [20] and "inter-ethics" [21], where normative conclusions emerge through structured dialogue between researchers and participants. Consultative approaches, in contrast, position the researcher as the primary agent of integration, who collects and analyzes empirical data before applying normative frameworks. These include methodologies such as "reflexive balancing" [20] and "wide reflective equilibrium" [20], where the researcher engages in an iterative process of adjusting ethical principles and judgments in light of empirical findings.
Table 3: Typology of Empirical Bioethics Methodologies
| Methodology Type | Key Characteristics | Examples |
|---|---|---|
| Dialogical | Relies on dialogue between stakeholders to reach shared understanding; emphasizes collaborative meaning-making | Dialogical empirical ethics, Inter-ethics |
| Consultative | Researcher analyzes data independently to develop normative conclusions; positions researcher as external thinker | Reflexive balancing, Wide reflective equilibrium |
| Hybrid | Combines elements of both dialogical and consultative approaches; integrates multiple perspectives | Hermeneutic approach, Symbiotic ethics, Grounded moral analysis |
The wide reflective equilibrium methodology deserves particular attention as one of the most frequently discussed integration approaches [20]. This method involves a two-way dialogue between ethical principles, values, and judgments on one hand, and practice (empirical data) on the other. The researcher engages in a back-and-forth process between normative underpinnings and empirical facts until reaching a point of moral coherence or "equilibrium" [20]. However, researchers have noted practical challenges in implementation, including questions about how much weight to give empirical data versus ethical theory and how to determine when equilibrium has been achieved [20].
Visualizing the Empirical-Normative Integration Process
The following diagram illustrates the core process of integrating empirical and normative approaches in bioethics research, highlighting the iterative nature of this methodological framework:
Integration Process of Empirical and Normative Approaches in Bioethics
This visualization captures the dynamic interplay between empirical data collection methods and normative frameworks, mediated through specific integration processes that yield distinct research outputs. The diagram highlights how diverse methodological approaches contribute to the integrative work that characterizes contemporary empirical bioethics.
Research Reagent Solutions: Methodological Tools for Empirical Bioethics
The conduct of rigorous empirical bioethics research requires specific methodological tools and approaches that facilitate the integration of empirical data with normative analysis. The following table details essential "research reagents" in this context – not laboratory chemicals, but rather methodological tools and frameworks that enable robust empirical bioethics research.
Table 4: Essential Methodological Tools for Empirical Bioethics Research
| Tool Category | Specific Methods/Approaches | Primary Function in Empirical Bioethics |
|---|---|---|
| Qualitative Research Methods | In-depth interviews, Focus groups, Ethnography, Phenomenology | Capture rich, contextual data on stakeholder experiences, values, and moral reasoning processes [83] |
| Quantitative Research Methods | Surveys, Statistical analysis, Cross-sectional studies | Identify patterns, distributions, and correlations in ethical attitudes and behaviors across populations [10] |
| Experimental Approaches | Randomized Controlled Trials (RCTs), Behavioral experiments, Experimental philosophical bioethics ("bioxphi") | Test causal hypotheses about moral decision-making and evaluate interventions designed to address ethical issues [84] [83] |
| Integration Methodologies | Wide reflective equilibrium, Dialogical empirical ethics, Reflexive balancing, Grounded moral analysis | Provide structured processes for combining empirical findings with normative analysis to generate ethically justified conclusions [23] [21] [20] |
| Mixed-Methods Designs | Sequential explanatory/exploratory designs, Concurrent triangulation | Combine strengths of qualitative and quantitative approaches to provide comprehensive understanding of bioethical issues [82] |
These methodological "reagents" enable researchers to address different aspects of bioethical inquiry. Qualitative approaches are particularly valuable for understanding the lived experience of moral dilemmas and the contextual factors that shape ethical decision-making [83]. Quantitative methods allow researchers to document prevalence of attitudes and practices and test associations between variables relevant to bioethical questions [10]. Experimental approaches, particularly those emerging from the subfield of experimental philosophical bioethics ("bioxphi"), use controlled experiments to understand the psychological and cognitive processes underlying moral judgments [84].
The integration methodologies represent perhaps the most distinctive "reagents" in empirical bioethics, as they provide the crucial bridge between descriptive findings and normative conclusions. These include well-established approaches like wide reflective equilibrium, which involves iterative adjustment between ethical principles, moral intuitions, and empirical data [20], as well as more collaborative approaches like dialogical ethics that engage stakeholders directly in the process of normative reflection [21].
Comparative Analysis of Researcher Attitudes and Practices
Acceptable Objectives of Empirical Bioethics Research
Researchers in the field display varying levels of acceptance regarding different potential objectives for empirical bioethics research. A qualitative exploration of researchers' views revealed a continuum of acceptability, with more modest objectives receiving broader endorsement than more ambitious ones [2].
The objectives of "understanding the context of a bioethical issue" and "identifying ethical issues in practice" received unanimous agreement among researchers [2]. These objectives represent what might be considered the foundational contributions of empirical research to bioethics – providing essential contextual understanding and surfacing ethical issues as they manifest in real-world settings.
In contrast, more ambitious objectives were considerably more contested. The goals of "striving to draw normative recommendations" and "developing and justifying moral principles" generated much greater debate among researchers [2]. This pattern suggests that while the descriptive contributions of empirical research to bioethics are widely accepted, the legitimacy of using empirical data to directly inform normative conclusions remains contested within the field.
Interestingly, the traditional philosophical concern about the "is-ought gap" (the problem of deriving prescriptive statements from descriptive facts) was not generally viewed as an insurmountable barrier to empirical bioethics. Instead, researchers treated it as a warning sign prompting critical reflection on the normative implications of empirical results [2].
Challenges in Methodological Implementation
Despite the proliferation of methodological frameworks for empirical bioethics, researchers report significant challenges in implementation. Interviews with researchers revealed an "air of uncertainty and overall vagueness" surrounding integration methods [20]. This vagueness manifests in several ways:
First, researchers described practical difficulties in applying methodological frameworks like reflective equilibrium, particularly regarding how much weight to give empirical data versus ethical theory and how to determine when equilibrium has been achieved [20]. Second, researchers reported challenges in navigating the different epistemological assumptions and quality standards that characterize the disciplinary traditions being brought together in empirical bioethics [82] [9].
The collaborative nature of many empirical bioethics approaches also presents implementation challenges. Dialogical methods that involve stakeholders in normative reflection require skills in facilitation and conflict mediation that may fall outside traditional bioethics training [20]. Similarly, interdisciplinary collaboration between bioethicists and social scientists necessitates navigating different publication cultures, reward structures, and criteria for evaluating research quality [9].
These implementation challenges may help explain why, despite 87.5% of bioethicists reporting use of empirical methods, only 35% have attempted to integrate empirical data with normative analysis [82]. They also highlight the need for more specific guidance and training in empirical bioethics methodologies.
The survey data presented in this analysis reveals a field in transition. The widespread adoption of empirical methods by bioethics researchers signals a significant methodological shift, while the ongoing challenges in integration and implementation suggest this transition remains incomplete. Several key implications emerge for the future development of empirical bioethics.
First, there is a clear need for enhanced methodological training specifically tailored to the challenges of empirical bioethics. The finding that 22.9% of researchers using empirical methods lack methodological training, combined with the low percentage who self-identify as experts in their methods, indicates a substantial training gap that could undermine the rigor and credibility of empirical bioethics research [82].
Second, the field would benefit from continued development and refinement of integration methodologies. The "vagueness" and uncertainty researchers report in applying existing frameworks [20], combined with the identification of 32 distinct methodologies [23] [21], suggests a need for more precise guidance on how to implement these approaches in practice.
Third, the contested nature of more ambitious objectives for empirical bioethics [2] indicates a need for ongoing philosophical and methodological reflection on the legitimate aims and boundaries of the field. As empirical bioethics continues to mature, developing shared standards for evaluating the success of integrative approaches will be crucial for maintaining the field's credibility and impact.
For drug development professionals and other stakeholders, these findings highlight both the promise and the challenges of empirical bioethics approaches. The ability to ground ethical analysis in robust empirical data offers the potential for more contextually sensitive and practically relevant ethical guidance. At the same time, the methodological complexities of integration require transparent reporting and careful justification of how empirical findings inform normative conclusions.
As the field moves forward, the continued development of rigorous, transparent, and methodologically self-conscious approaches to empirical bioethics will be essential for realizing its potential to address the complex ethical challenges in contemporary healthcare and biomedical research.
The field of bioethics has experienced a significant "empirical turn" in recent decades, marked by a growing recognition that ethical analysis must be grounded in the realities of human practices and experiences [54]. However, despite this shift, methodological innovation in empirical bioethics has notably trailed behind adjacent fields. While psychology, neuroscience, and social sciences have embraced advanced digital methods and computational approaches, bioethics research has largely remained confined to traditional methodologies such as surveys, interviews, and vignette studies [54]. This methodological conservatism presents a significant limitation, particularly as bioethics seeks to address increasingly complex ethical questions arising from technological and medical advancements.
The emerging field of Design Bioethics represents a purposeful response to this methodological gap. This approach advocates for the "design and use of purpose-built, engineered tools for bioethics research, education and engagement" [54]. Rather than simply importing methods from other disciplines, Design Bioethics encourages the creation of tailored methodological innovations specifically designed to investigate bioethical concerns. This conceptual framework aligns with broader methodological discussions in empirical bioethics, which seek to integrate empirical findings with normative analysis through various approaches including dialogical, consultative, and integrated methodologies [21] [20]. Against this backdrop, Computational Social Science (CSS) emerges as a promising partner discipline, offering novel approaches to studying complex social phenomena through computational tools, large-scale data analysis, and sophisticated modeling techniques [85] [86] [87].
Computational Social Science: A Primer for Bioethics Researchers
Computational Social Science (CSS) represents an interdisciplinary field that leverages computational tools and digital data to study human behavior and social dynamics. Sitting at the intersection of computer science, statistics, and social sciences, CSS enables researchers to analyze massive datasets from social media platforms, digital communications, and other online sources to uncover patterns in social behavior and relationships [85] [87]. This methodological approach moves beyond traditional analytical techniques, offering the capacity to study social phenomena at unprecedented scale and granularity.
The methodological toolkit of CSS includes several powerful approaches particularly relevant to bioethics research. Data mining and natural language processing enable the extraction of insights from large textual corpora, which could be applied to ethical discourse analysis. Social network analysis examines relationship structures and information flow, potentially mapping how ethical perspectives spread through professional communities. Machine learning algorithms can identify complex patterns in data that might elude traditional statistical methods, offering potential for predicting ethical tensions or modeling decision processes [85] [87] [88]. These approaches are complemented by agent-based modeling, which simulates interactions between individuals to observe emergent collective behaviors, and culturomics, which studies cultural trends through analysis of massive text collections [87].
CSS has demonstrated significant potential across multiple domains with clear bioethical implications. In public health, CSS approaches have been used to analyze mobility data during the COVID-19 pandemic to inform policy decisions on vaccination and reopening efforts [87]. In studying political polarization, CSS methods have revealed how exposure to opposing views can intensify partisan divides and how specific communication strategies might mitigate this effect [87]. Climate change perceptions have been analyzed through Twitter data, showing how social media discourse can strengthen support for environmental action [87]. These applications demonstrate the capacity of CSS methods to address complex, value-laden social issues with direct relevance to bioethical inquiry.
Comparative Methodology: Traditional Approaches versus Digital Innovations
Established Empirical Bioethics Methodologies
Traditional empirical bioethics research has primarily operated within a limited methodological spectrum, with two dominant approaches emerging according to systematic reviews of the field. The landmark systematic review by Davies et al. (2015) identified 32 distinct empirical bioethics methodologies, which can be broadly categorized into consultative and dialogical approaches [21]. Consultative methodologies position the researcher as an external analyst who independently collects and analyzes empirical data to develop normative conclusions. This category includes approaches like reflective equilibrium, where researchers engage in iterative refinement between ethical principles and empirical observations [20]. In contrast, dialogical methodologies emphasize collaborative sense-making between researchers and stakeholders, using facilitated discussions to reach shared understanding of ethical issues [21]. A third category, inherent integration approaches, attempts to intertwine empirical and normative elements from the outset of research projects [20].
Table 1: Traditional Empirical Bioethics Methodologies
| Methodology Type | Key Characteristics | Example Approaches | Primary Strengths |
|---|---|---|---|
| Consultative | Researcher as external analyst; independent data collection and analysis | Reflective equilibrium; reflexive balancing | Systematic analysis; theoretical rigor |
| Dialogical | Collaborative sense-making; stakeholder engagement | Moral case deliberation; inter-ethics | Contextual understanding; practical relevance |
| Inherent Integration | Empirical and normative elements intertwined from project inception | Grounded moral analysis; symbiotic ethics | Holistic understanding; avoids artificial separation |
Despite their established utility, these traditional approaches face significant methodological challenges. Research reveals an "air of uncertainty and overall vagueness" surrounding integration methods, with researchers often struggling to clearly articulate how empirical findings inform normative conclusions [20]. The practical steps for integration frequently remain underspecified, creating challenges for consistency and rigor in empirical bioethics research [20]. Additionally, traditional methods often rely on small, homogenous samples, potentially limiting the generalizability of findings, particularly for informing health policy that affects diverse populations [54].
Digital Methodologies in Bioethics
Digital innovations in bioethics methodology offer promising alternatives to address these limitations. The "Tracing Tomorrow" study provides a compelling example of Design Bioethics in practice, comparing a purpose-built digital game against a traditional vignette survey for exploring adolescent perspectives on digital phenotyping in mental health [54]. This randomized study with 301 UK adolescents demonstrated several advantages of the digital game approach. Participants in the game condition reported significantly higher levels of presence (immersion in the scenario), emotional engagement, cognitive absorption, and insight into mental health ethics compared to the vignette survey group [54]. These differences occurred while maintaining equivalent levels of perceived authenticity and curiosity to learn more about the topic.
Table 2: Digital Game vs. Traditional Vignette Survey Outcomes
| Engagement Dimension | Digital Game | Traditional Vignette Survey | Statistical Significance |
|---|---|---|---|
| Sense of Presence | Significantly Higher | Lower | p < 0.01 |
| Emotional Engagement | Significantly Higher | Lower | p < 0.01 |
| Cognitive Absorption | Significantly Higher | Lower | p < 0.01 |
| Mental Health Ethics Insight | Significantly Higher | Lower | p < 0.01 |
| Perceived Authenticity | Equivalent | Equivalent | Not Significant |
| Curiosity/Motivation to Learn | Equivalent | Equivalent | Not Significant |
The theoretical rationale for these digital innovations centers on their capacity to better capture the contextual, social, and relational nature of moral deliberation. While vignette surveys attempt to simulate ethical decision-making, they have limited ability to imitate real-life reactions and create vivid representations of moral issues [54]. Digital games and narrative environments create more immersive, engaging contexts where participants make decisions in real time, potentially yielding more authentic and valid data that better reflects their true values and preferences [54]. This enhanced ecological validity addresses core theoretical commitments in bioethics regarding the situated nature of moral reasoning.
Experimental Protocols and Research Workflows
Digital Bioethics Research Protocol
The "Tracing Tomorrow" study exemplifies a rigorous experimental protocol for comparing digital and traditional bioethics methodologies. The research employed a randomized design where participants were automatically assigned to either the digital game condition or an equivalent vignette-based survey after providing consent [54]. The study specifically targeted UK adolescents aged 16-18 years, with recruitment conducted through social media campaigns and existing research networks. To ensure data quality, the protocol incorporated timing checks to automatically exclude participants who repeatedly answered questions implausibly quickly [54]. This methodological rigor is particularly crucial in digital research environments where attention cannot be directly observed.
The digital game itself was carefully designed as a narrative experience presenting ethically charged dilemmas and decisions about mental health tracking technologies. Participants progressed through a storylined structure where they faced decisions about disclosing mental health risk assessments to parents and friends [54]. The comparative vignette survey presented descriptively rich questions posing equivalent dilemmas in a traditional online survey format, maintaining the same sequence of questions and response options but without the interactive, personalized narrative context of the game [54]. Following the intervention, all participants completed standardized quantitative measures assessing presence, cognitive absorption, perceived authenticity, ethical insight, and motivation for further engagement, allowing for direct comparison between methodological approaches.
Computational Social Science Workflow
CSS research follows a distinct workflow that leverages large-scale digital data and computational analysis. The process typically begins with data acquisition from digital sources such as social media platforms, online forums, or administrative databases [85] [87]. For example, migration researchers have collaborated with technology companies to analyze the activities of billions of social media users to track population movements [86]. This data collection phase is followed by preprocessing and cleaning, where raw digital data is transformed into structured formats suitable for computational analysis, addressing challenges such as different platform penetration rates across populations [86].
The analytical phase employs specialized computational techniques tailored to the research question. Network analysis examines relationship structures and information flow between actors [87]. Natural language processing extracts meaning from textual data at scale, enabling researchers to track evolving discourse on ethical issues [87]. Machine learning algorithms identify complex patterns and can be used for tasks such as predicting poverty levels from mobile phone metadata or estimating migration flows using demographic accounting techniques [86] [87]. The final stage involves interpreting computational findings through social science theories and ethical frameworks, ensuring that pattern recognition translates to meaningful understanding of bioethical phenomena.
Conducting rigorous research in digital bioethics and computational social science requires familiarity with a suite of methodological tools and approaches. The following table summarizes key "research reagents" – essential methodological components and their functions – for scholars entering this emerging field.
Table 3: Digital Bioethics Research Toolkit
| Tool Category | Specific Methods/Techniques | Primary Function | Example Applications in Bioethics |
|---|---|---|---|
| Digital Engagement Platforms | Serious games; Interactive narratives; Virtual scenarios | Create immersive ethical decision-making environments; Enhance ecological validity | "Tracing Tomorrow" game for mental health ethics research [54] |
| Computational Analysis Tools | Natural language processing; Machine learning; Network analysis | Analyze large-scale textual data; Identify patterns in ethical discourse; Map stakeholder networks | Tracking evolution of public discourse on Twitter during health crises [87] |
| Data Collection Innovations | Social media data scraping; Mobile phone metadata analysis; Digital trace data | Access large, diverse samples; Study behavior in naturalistic settings; Enable real-time data collection | Using mobile phone location data to study poverty distributions [87] |
| Integration Frameworks | Design Bioethics; Reflective equilibrium; Dialogical empirical ethics | Bridge empirical findings and normative analysis; Maintain methodological rigor while innovating | Combining stakeholder dialogues with ethical analysis in clinical ethics [20] |
| Validation Approaches | Timing checks; Attention measures; Multimethod comparison | Ensure data quality in digital environments; Validate new methods against established approaches | Comparing digital game responses with traditional survey results [54] |
This toolkit continues to evolve rapidly, with emerging technologies creating new possibilities for bioethics research. Large language models (LLMs) and other generative AI tools show potential for automating data annotation and synthesis, scaling research projects beyond previous limitations [86]. Meanwhile, advances in causal inference methodologies are strengthening CSS's ability to address crucial questions about causality in social science research [86]. For bioethics scholars, these developments offer exciting opportunities to study the ethical implications of AI systems while simultaneously leveraging those same systems as research tools.
The integration of digital methods and computational social science approaches represents a promising frontier for empirical bioethics research. Evidence from comparative studies indicates that purpose-built digital tools can enhance key dimensions of research engagement, including presence, emotional involvement, and cognitive absorption, while maintaining methodological rigor [54]. These advantages address longstanding theoretical commitments in bioethics regarding the contextual nature of moral deliberation while simultaneously offering practical solutions to methodological challenges such as sample diversity and scale.
The future of empirical bioethics methodology likely lies in thoughtful integration rather than wholesale replacement of traditional approaches. Digital innovations offer exciting possibilities for enhancing research engagement, accessing larger and more diverse samples, and studying ethical decision-making in more ecologically valid contexts [54]. At the same time, established methodologies like reflective equilibrium and dialogical approaches provide crucial frameworks for navigating the complex process of integrating empirical findings with normative analysis [21] [20]. The most productive path forward may involve leveraging digital tools to enrich these established integration approaches rather than treating innovation and tradition as opposing poles.
For bioethics researchers pursuing methodological innovation, several principles emerge from this analysis. First, methodological choice should be guided by theoretical commitments regarding the nature of moral reasoning and how it is best studied [54]. Second, digital tools should be purpose-built or carefully adapted to address specific bioethical research questions rather than imported uncritically from other fields [54]. Third, methodological innovation must be accompanied by rigorous validation and transparent reporting of how empirical findings inform normative conclusions [20]. Finally, researchers should remain mindful of ethical considerations in digital methodologies, including privacy concerns in data collection and the potential for algorithmic bias in computational approaches [88]. By embracing these principles while exploring the rich methodological landscape emerging at the intersection of bioethics and computational social science, researchers can develop increasingly sophisticated approaches to understanding the complex ethical challenges in healthcare and technology.
The field of bioethics has undergone a significant transformation in recent decades, marked by a pronounced 'empirical turn' that integrates social science methodologies into traditionally philosophical inquiries. This shift emerged in response to critiques that bioethics had failed to adequately account for social context and lived experience, creating a need for approaches that ground ethical analysis in real-world data [15]. Empirical bioethics has since evolved into a established discipline that systematically investigates ethical issues in healthcare and research using qualitative, quantitative, and mixed methods approaches.
This comparative guide examines the methodologies through which empirical findings successfully inform and shift ethical norms, with particular focus on applications relevant to researchers, scientists, and drug development professionals. The growing institutionalization of this field is evidenced by dedicated training programs such as the Empirical Bioethics Summer School, which provides structured education on integrating empirical methods with ethical analysis [6]. As the field matures, there is increasing recognition of the need for a 'theoretical turn' that encourages more deliberate integration of empirical research with philosophical theory, creating a bidirectional exchange that enriches both domains [15].
Methodological Approaches in Empirical Bioethics
Comparative Framework of Research Methodologies
Empirical bioethics employs diverse methodological approaches to investigate and influence ethical norms. The table below compares the primary methodologies, their applications, and their normative impacts.
Table 1: Comparative Analysis of Empirical Bioethics Methodologies
| Methodology | Primary Applications | Data Sources | Normative Impact Mechanisms | Key Strengths | Key Limitations |
|---|---|---|---|---|---|
| Qualitative Approaches | Exploring stakeholder perspectives, understanding contextual factors | Interviews, focus groups, ethnographic observation [6] | Identifying value conflicts, revealing practical ethical challenges | Rich contextual data, identifies unanticipated issues | Limited generalizability, potential for researcher bias |
| Quantitative Surveys | Measuring prevalence of attitudes, identifying demographic correlations | Structured questionnaires, statistical analysis [43] | Establishing consensus positions, tracking normative shifts over time | Generalizable results, measurable trends | May oversimplify complex ethical issues |
| Mixed Methods | Comprehensive assessment of complex ethical issues | Combined qualitative and quantitative data [43] | Triangulation of findings, connecting attitudes with reasoning | Complementary strengths, more robust conclusions | Methodological complexity, integration challenges |
| Systematic Reviews | Synthesizing existing empirical research | Literature analysis, evidence mapping [70] | Identifying evidence gaps, informing guideline development | Comprehensive overview, establishes knowledge base | Dependent on primary study quality |
| Protocol Analysis | Evaluating decision-making processes | Ethical deliberation records, think-aloud protocols [89] | Improving review processes, identifying heuristic biases | Insights into actual decision-making | Artificial settings may limit ecological validity |
Specialized Empirical Approaches
Beyond these broad categories, specialized methodological approaches have been developed to address specific challenges in empirical bioethics. Visualization for visualization (Vis4Vis) represents an emerging approach that uses sophisticated data visualization techniques to analyze complex empirical data from studies incorporating eye tracking, electrodermal activity sensors, electroencephalography, and interaction logs [89]. This approach is particularly valuable for studying complex decision-making processes in environments like Research Ethics Board (REB) deliberations, where traditional observation methods may capture only superficial aspects of the evaluation process.
Another significant development is the creation of standardized protocol templates specifically designed for empirical bioethics research. These templates adapt reporting standards from qualitative research to accommodate the distinctive epistemological and methodological requirements of normative-empirical collaboration [43]. The practical implementation of such templates addresses significant challenges in ensuring methodological rigor while maintaining flexibility appropriate for studying complex ethical phenomena.
Key Research Areas and Empirical Findings
Research Ethics Board Composition and Function
Empirical research has fundamentally influenced norms regarding REB composition and expertise. A comprehensive scoping review of empirical research on REB membership reveals how evidence has shaped understanding of optimal board composition [70]. The research has examined four critical dimensions of REB expertise:
Table 2: Empirical Findings on REB Composition and Expertise
| Expertise Domain | Current Evidence Base | Empirical Findings | Normative Impact |
|---|---|---|---|
| Scientific Expertise | Small but diverse body of international literature [70] | Concerns about adequate scientific expertise despite privileging of scientific perspectives | Recognition of need for broader methodological competence beyond narrow scientific domains |
| Ethical, Legal & Regulatory Expertise | Varied training approaches documented | Limited formal training, reliance on administrative staff for regulatory knowledge [70] | Increased standardization of ethics training requirements for REB members |
| Diversity of People & Perspectives | Studies on member composition and identity | Regulatory requirements for diversity often minimally implemented | Strengthened emphasis on demographic and perspective diversity in guidelines |
| Research Participant Perspectives | Growing recognition of importance | Formal requirements for participant representation generally absent | Increasing inclusion of community representatives and patient advocates |
This empirical research has demonstrated that REB membership and its local "idioculture" play a key role in decisions made, not only regarding whether to approve projects but also in requesting modifications to consent documents, safety monitoring, and addressing concerns such as undue inducement [70]. The empirical finding that REBs may privilege scientific expertise over other forms of knowledge has prompted normative shifts toward more balanced recognition of multiple expertise domains.
Internet Research Ethics
The emergence of internet-based research has created novel ethical challenges that have been extensively studied using empirical methods. Research on emotional contagion through social media platforms, such as Facebook's controversial study, highlights the complex ethical terrain of digital research environments [90]. Empirical investigations have revealed significant gaps in how traditional research ethical norms guide researchers studying online spaces.
Three primary criticisms of existing research ethical norms in internet research contexts have been identified through empirical study:
Inconsistency: Guidelines across different organizations and disciplines contain significant contradictions, particularly regarding concepts of public versus private space in digital environments [90].
Opacity: Norms are often formulated with insufficient clarity to provide practical guidance for the novel ethical dilemmas encountered in internet research [90].
Complexity Management: Existing norms struggle to handle the moral complexity of issues faced by researchers studying vulnerable groups and sensitive topics online [90].
These empirical findings have driven normative evolution toward more contextual approaches that emphasize researcher reflection and case-based reasoning rather than uniform application of predetermined rules. This represents a significant shift from traditional research ethics frameworks toward more flexible, principle-based approaches that acknowledge the distinctive features of digital research spaces.
Drug Development Ethics
In drug development, empirical bioethics has influenced norms through systematic study of ethical decision-making across the development pipeline. The Model-Informed Drug Development (MIDD) framework exemplifies how empirical data and modeling approaches inform ethical decisions regarding trial design, risk-benefit assessment, and regulatory approval [91].
Empirical research has been particularly influential in shaping ethical approaches to first-in-human studies, where model-based dose prediction strategies have created more ethical approaches to initial human testing [91]. The "fit-for-purpose" modeling approach represents a normative shift toward context-sensitive ethical analysis that aligns methodological choices with specific ethical questions and concerns throughout the five stages of drug development: discovery, preclinical testing, clinical trials, regulatory approval, and post-market surveillance [91].
Signaling Pathways: From Empirical Data to Normative Shift
The process through which empirical findings influence ethical norms follows identifiable pathways that can be visualized as a conceptual framework. The diagram below illustrates the primary signaling pathway from data collection to normative integration.
This pathway illustrates the essential process through which empirical observations become integrated into ethical norms. The critical transition from theoretical engagement to normative proposal development represents what has been termed the "theoretical turn" in empirical bioethics, where deliberate integration of empirical findings with philosophical theory creates robust normative frameworks [15]. The feedback loops demonstrate the iterative nature of this process, where implemented norms generate new empirical questions that initiate further cycles of inquiry.
Experimental Protocols in Empirical Bioethics Research
Standardized Protocol Template
The methodological rigor of empirical bioethics has been strengthened through the development of specialized protocol templates. Recent work has formalized a protocol template suitable for all types of humanities and social sciences investigations in health, including empirical bioethics specifically [43]. This template adapts the Standards for Reporting Qualitative Research (SRQR) to overcome limitations restricted to qualitative approaches, creating a framework equally suitable for quantitative and mixed methods approaches.
The protocol includes several distinctive sections that facilitate the transition from empirical data to normative analysis:
Epistemological Positioning: Explicit articulation of the theoretical framework connecting empirical observations to normative conclusions [43]
Ethical Theory Application: Detailed description of how chosen ethical theories will inform the interpretation of empirical data [43]
Contextualized Consent Procedures: Flexible approaches to informed consent that acknowledge how exhaustive information may influence participant behavior and study validity [43]
Data Protection Balance: Responsible pseudonymization approaches that enable deeper analysis while protecting participant confidentiality [43]
This protocol structure represents a significant methodological advancement that explicitly addresses the distinctive challenges of research that bridges empirical investigation and normative analysis.
Research Reagent Solutions: Essential Methodological Tools
The following table details key "research reagents" - essential methodological tools and approaches - used in empirical bioethics research, with explanations of their functions in investigating and influencing ethical norms.
Table 3: Essential Methodological Tools in Empirical Bioethics Research
| Methodological Tool | Function in Empirical Bioethics | Application Examples | Impact on Norm Development |
|---|---|---|---|
| Semi-structured Interview Guides | Elicit rich qualitative data on ethical experiences and perspectives | Understanding stakeholder views on ethical issues in clinical trials [6] | Identifies disconnects between formal norms and lived experience |
| Standardized Protocol Templates | Ensure methodological rigor and comprehensive reporting | Health research protocols for empirical bioethics [43] | Standardizes approaches across studies, enabling comparison and synthesis |
| Visualization Analytics (Vis4Vis) | Analyze complex behavioral data from ethical decision-making | Eye tracking during REB protocol review [89] | Reveals unconscious patterns in ethical evaluation processes |
| Scoping Review Methodologies | Systematically map existing empirical research on ethical topics | Review of REB membership expertise literature [70] | Identifies evidence gaps and establishes knowledge base for guideline development |
| Deliberative Engagement Frameworks | Structure stakeholder dialogue on normative implications | Integrating patient perspectives in research ethics [70] | Creates legitimate processes for normative development from empirical findings |
| Mixed Methods Integration Strategies | Combine qualitative and quantitative approaches | Connecting survey data with in-depth interview analysis [43] | Provides both breadth and depth in understanding ethical phenomena |
The comparative analysis presented in this guide demonstrates that empirical findings successfully inform and shift ethical norms through multiple methodological pathways. The most significant normative impacts occur when rigorous empirical research engages deliberately with theoretical frameworks through structured processes that include diverse stakeholder perspectives.
The evidence indicates that the evolving methodology of empirical bioethics has created increasingly sophisticated approaches to investigating and influencing ethical norms. The development of specialized protocol templates, visualization methodologies, and integrative frameworks represents significant methodological advancement that strengthens the field's capacity to generate meaningful normative insights from empirical data.
For researchers, scientists, and drug development professionals, understanding these methodological approaches provides valuable tools for addressing ethical challenges in their work. The continuing evolution of empirical bioethics methodology promises enhanced capacity to respond to emerging ethical challenges in increasingly complex research and healthcare environments, particularly at the intersection of technological innovation and human values.
Conclusion
The comparative analysis of empirical bioethics methodologies reveals a heterogeneous yet maturing field, characterized by a productive tension between dialogical and consultative approaches. Successful navigation of this landscape requires researchers to make deliberate, transparent, and justified choices about how to integrate empirical data with normative analysis, adhering to emerging consensus standards. For biomedical and clinical research, this methodological rigor promises more contextually grounded, legitimate, and actionable ethical guidance. Future directions should focus on enhancing interdisciplinary training, further developing digital methods, and conducting meta-research to evaluate the real-world impact of different methodological choices on policy and practice, ultimately strengthening the contribution of bioethics to complex challenges in drug development and healthcare.
References
- 1. An update on the “empirical turn” in bioethics: analysis of ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-018-0246-9]
- 2. Acceptable objectives of empirical research in bioethics [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-022-00845-1]
- 3. Integrating ethics in digital mental healthcare technologies... [https://pubmed.ncbi.nlm.nih.gov/40736629/]
- 4. Blog - The Need for “Big Bioethics” Research [https://bioethicstoday.org/blog/the-need-for-big-bioethics-research/]
- 5. What Counts as Empirical Research in Bioethics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2838431/]
- 6. : 2025 Summer School | Bristol Medical School... Empirical Bioethics [https://www.bristol.ac.uk/population-health-sciences/centres/ethics/seminars/2025/empirical-bioethics-summer-school.html]
- 7. Artificial intelligence policies in bioethics and health humanities [https://pmc.ncbi.nlm.nih.gov/articles/PMC12226874/]
- 8. Critical bioethics: beyond the social science critique of ... [https://pubmed.ncbi.nlm.nih.gov/15146853/]
- 9. Beyond Binaries: Dissolving the Empirical/Normative Divide [https://pmc.ncbi.nlm.nih.gov/articles/PMC7048068/]
- 10. Empirical research in bioethical journals. A quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2565792/]
- 11. The Role of Empirical Research in Bioethics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2826359/]
- 12. a template for empirical bioethics and other investigations [https://pubmed.ncbi.nlm.nih.gov/40551148/]
- 13. Clinical trials as treatment option: Bioethics and health care ... [https://www.sciencedirect.com/science/article/abs/pii/S0277953609006108]
- 14. Bioethical implications of organ-on-a-chip on modernizing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10615722/]
- 15. Is it time for a 'theoretical turn' in empirical bioethics? [https://asbh25.eventscribe.net/ajaxcalls/PresentationInfo.asp?PresentationID=1658770]
- 16. a dialogical approach to qualitative research [https://link.springer.com/article/10.1057/s41267-025-00776-0]
- 17. Psychotherapy focusing on dialogical and narrative perspectives [https://pmc.ncbi.nlm.nih.gov/articles/PMC11333309/]
- 18. Empirical Bioethics Summer School 2025 - VU Amsterdam [https://xendens.com/n/64/nieuws/empirical-bioethics-summer-school-2025---vu-amsterdam]
- 19. A comparative study of Italian and Polish | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0333011]
- 20. Researchers' Views on Doing Empirical Bioethics [https://link.springer.com/article/10.1007/s11673-023-10286-z]
- 21. A systematic review of empirical bioethics methodologies [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-015-0010-3]
- 22. guides.library.georgetown.edu/bioethicsresources [https://guides.library.georgetown.edu/bioethicsresources]
- 23. A systematic review of empirical bioethics methodologies [https://pubmed.ncbi.nlm.nih.gov/25885575/]
- 24. Empirical and Normative Bioethics Methods [https://philosophicalbioethics.com/?page_id=1034]
- 25. Acceptable objectives of empirical research in bioethics [https://pmc.ncbi.nlm.nih.gov/articles/PMC9794471/]
- 26. Insights from the Coalface of Bioethics [https://link.springer.com/article/10.1007/s41649-025-00394-w]
- 27. 2025 Roundtable: Ethics, Trust + Patient Centricity in Pharma [https://bioethicsinternational.org/event/join-us-bei-ey-yales-roundtable-on-ethics-trust-patient-centricity-in-pharma-defining-metrics-for-success/]
- 28. Bioethics at the intersection of politics, society, and healthcare [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-025-01233-1]
- 29. 2025 CCTS Bioethics Forum Explores the Ethics ... [https://www.uab.edu/ccts/news-events/center-news/2025-bioethics-forum-recap]
- 30. 2025 RARE Drug Development Symposium [https://globalgenes.org/rare-drug-development-symposium-2025/]
- 31. A systematic review of empirical bioethics methodologies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4357052/]
- 32. Applications of the Wide Reflective Equilibrium [https://link.springer.com/article/10.1007/s10892-023-09458-1]
- 33. Reflective Equilibrium - Stanford Encyclopedia of Philosophy [https://plato.stanford.edu/entries/reflective-equilibrium/]
- 34. Reflective Equilibrium - Stanford Encyclopedia of Philosophy [https://plato.stanford.edu/archives/fall2018/entries/reflective-equilibrium/]
- 35. Rawls's Wide Reflective Equilibrium as a Method for Engaged ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5888768/]
- 36. Moral Distress in Ethical Dilemmas: A Comparative Study of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12524078/]
- 37. Ethics review, reflective equilibrium and reflexivity - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8866750/]
- 38. A Platform to Develop and Apply Digital Methods for Empirical ... [https://formative.jmir.org/2022/5/e28558/]
- 39. Visualizing an Ethics Framework: A Method to Create ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6996733/]
- 40. An ethical analysis of policy dialogues [https://health-policy-systems.biomedcentral.com/articles/10.1186/s12961-023-00962-2]
- 41. Fostering Research Integrity through Training - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12640486/]
- 42. IFAPP International Ethics Framework - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12245974/]
- 43. Health research protocols: a template for empirical bioethics ... [https://health-policy-systems.biomedcentral.com/articles/10.1186/s12961-025-01362-4]
- 44. The use of empirical research in bioethics - BMC Medical Ethics [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-017-0239-0]
- 45. Why the 2025 Update to the PADIS Guidelines ... [https://www.aacn.org/blog/key-takeaways-2025-update-padis-guidelines]
- 46. 2025 SCAI/HRS Clinical Practice Guidelines ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12485513/]
- 47. Scaling experimentation program's metrics in 2025 [https://www.optimizely.com/insights/blog/metrics-for-your-experimentation-program/]
- 48. Design Bioethics: A Theoretical Framework and Argument for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8676709/]
- 49. Drug Development Tool Qualification Process [https://www.fda.gov/drugs/drug-development-tool-ddt-qualification-programs/drug-development-tool-qualification-process-transparency-provisions]
- 50. FDA Continues to Support Transparency and Collaboration ... [https://www.socra.org/blog/fda-continues-to-support-transparency-and-collaboration-in-drug-approval-process-as-the-clinical-data-summary-pilot-concludes/]
- 51. A Quick Guide to End-to-End Transparency in Drug ... [https://dsinpharmatics.com/a-quick-guide-to-end-to-end-transparency-in-drug-substance-development/]
- 52. Integrating drug substance and drug product development [https://www.patheon.com/us/en/insights-resources/blog/integrating-drug-substance-and-drug-product-development.html]
- 53. Epistemological obstacles to interdisciplinary research [https://i2insights.org/2017/10/31/epistemology-and-interdisciplinarity/]
- 54. Testing Design Bioethics Methods: Comparing a Digital ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9612923/]
- 55. A new prescription for empirical ethics research in pharmacy [https://pmc.ncbi.nlm.nih.gov/articles/PMC2598230/]
- 56. An evaluation framework for clinical use of large language ... [https://www.nature.com/articles/s41591-024-03328-5]
- 57. Collaboration, interdisciplinarity, and the epistemology of ... [https://www.sciencedirect.com/science/article/abs/pii/S0039368115001442]
- 58. Introduction to Empirical and Normative Bioethics [https://philosophicalbioethics.com/?page_id=761]
- 59. How Interactive Visualizations Compare to Ethical ... [https://pubmed.ncbi.nlm.nih.gov/37074681/]
- 60. The Vagueness of Integrating the Empirical and the Normative [https://pmc.ncbi.nlm.nih.gov/articles/PMC11288993/]
- 61. US science research was gutted in 2025. How will it rebuild? [https://cen.acs.org/careers/US-science-research-gutted-2025/103/web/2025/08]
- 62. Funding Uncertainty Leads NACUBO's Top 5 Higher ... [https://www.nacubo.org/Press-Releases/2025/Funding-Uncertainty-Leads-NACUBOs-Top-5-Higher-Education-Business-Issues-of-2025]
- 63. All government shutdowns disrupt science − in 2025, the ... [https://gettysburgconnection.org/all-government-shutdowns-disrupt-science-%E2%88%92-in-2025-the-consequences-extend-far-beyond-a-lapse-in-funding/]
- 64. A sense of doom is overwhelming U.S. biomedical researchers [https://www.statnews.com/2025/08/26/federal-research-funding-instability-survey-hundreds-sense-of-doom/]
- 65. Institutional Review Boards Frequently Asked Questions [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/institutional-review-boards-frequently-asked-questions]
- 66. Institutional Review Board [http://orwh.od.nih.gov/toolkit/human-subjects-protections/institutional-review-board]
- 67. TOP Guidelines [https://www.cos.io/initiatives/top-guidelines]
- 68. BrainSwarming, blockchain, and bioethics: applying ... [https://www.nature.com/articles/s41598-023-50232-y]
- 69. Towards a research ethics of real-world experimentation ... [https://www.sciencedirect.com/science/article/pii/S2666659624000246]
- 70. A Scoping Review of Empirical Research on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12490803/]
- 71. How Does Empirical Research Facilitate Creation Tool ... [https://arxiv.org/html/2507.15244v1]
- 72. Yellow, Purple, and the Myth of “Accessibility Limits Color ... [https://stephaniewalter.design/blog/yellow-purple-and-the-myth-of-accessibility-limits-color-palettes/]
- 73. Contrast requirements for WCAG 2.2 Level AA [https://www.makethingsaccessible.com/guides/contrast-requirements-for-wcag-2-2-level-aa/]
- 74. UI Color Palette 2025: Best Practices, Tips, and Tricks for ... [https://www.interaction-design.org/literature/article/ui-color-palette?srsltid=AfmBOoqVySDB1on1CISg0HgrvPERnWOo9RSjTAUpCQcZtz6de65lEz24]
- 75. Standards of practice in empirical bioethics research [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-018-0304-3]
- 76. Setting standards for empirical bioethics research: a response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6044088/]
- 77. Empirical Methods in Bioethics [https://www.encyclopedia.com/science/encyclopedias-almanacs-transcripts-and-maps/empirical-methods-bioethics]
- 78. The strengths and limitations of empirical bioethics [https://pubmed.ncbi.nlm.nih.gov/21355433/]
- 79. A systematic review of empirical bioethics methodologies - ORA [https://ora.ox.ac.uk/objects/uuid:83f6823d-3632-4b72-8aab-c8a12147f21a]
- 80. introducing new methods for the study of bioethical issues [https://philpapers.org/rec/SCHDBI-11]
- 81. Standards of practice in empirical bioethics research [https://pmc.ncbi.nlm.nih.gov/articles/PMC6038185/]
- 82. The use of empirical research in bioethics: a survey of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5741864/]
- 83. Bioethics and Medical Humanities: Find Biomedical Research ... [https://hslguides.osu.edu/bioethics-medical-humanities/research-ethics]
- 84. Bioethics, Experimental Approaches. [https://philarchive.org/rec/LEWBEA]
- 85. Social Science: Understanding and Shaping Our Digital ... [https://www.graydi.us/blog/gray-insights/computational-social-science-understanding-and-shaping-our-digital-world]
- 86. Unveiling New Dimensions with Computational Social ... [https://web.socsc.hku.hk/school_news/unveiling-new-dimensions-with-computational-social-science/]
- 87. Data analytics: solving real-world problems one formula at a ... [https://lpsonline.sas.upenn.edu/features/data-analytics-solving-real-world-problems-one-formula-time-computational-social-science]
- 88. Computational Social Science in a Social World [https://dlab.berkeley.edu/news/computational-social-science-social-world-challenges-and-opportunities]
- 89. Vis4Vis: Visualization for ( Empirical ) Visualization Research [https://link.springer.com/chapter/10.1007/978-3-030-34444-3_10]
- 90. Research Ethical Norms, Guidance and the Internet [https://link.springer.com/article/10.1007/s11948-021-00342-5]
- 91. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]