Integrating Theological Bioethics in Clinical Practice: A Framework for Humanized Patient Care and Ethical Drug Development
This article addresses the growing need to validate theological and religious perspectives within secular bioethics, particularly for researchers and drug development professionals navigating complex ethical landscapes.
Integrating Theological Bioethics in Clinical Practice: A Framework for Humanized Patient Care and Ethical Drug Development
Abstract
This article addresses the growing need to validate theological and religious perspectives within secular bioethics, particularly for researchers and drug development professionals navigating complex ethical landscapes. It explores the historical secularization of bioethics and the contemporary gap created by technologically-driven frameworks like transhumanism and AI, which often sideline the spiritual dimensions of personhood. The content provides a methodological framework for integrating theological reasoning into clinical and research ethics, troubleshoots common implementation challenges such as interdisciplinary communication and institutional resistance, and validates the approach through comparative analysis with secular principlism and evidence of improved patient outcomes. By synthesizing foundational concepts, practical applications, and empirical validation, this article argues for the essential role of theological bioethics in fostering holistic, humanized healthcare and responsible scientific innovation.
The Secular Shift and the Case for Theological Re-engagement in Bioethics
The field of bioethics represents a critical intersection of medicine, morality, and philosophy, governing how society approaches complex biological and medical dilemmas. This domain has undergone a significant transformation from its origins in religious tradition to its current predominantly secular character. Understanding this evolution is essential for researchers, scientists, and drug development professionals who operate within ethical frameworks that often carry implicit philosophical assumptions. The historical transition from theological to secular foundations represents more than merely a shift in vocabulary; it constitutes a fundamental reorientation of the underlying principles, justification mechanisms, and authority structures that inform bioethical decision-making. This guide objectively compares these competing foundations, examining their respective frameworks, applications, and influences on contemporary clinical practice and research.
The secularization of bioethics accelerated particularly during the mid-to-late 20th century, as technological advancements in medicine presented novel ethical questions that seemed to challenge traditional religious frameworks [1]. This process was notably catalyzed by debates surrounding contraception in the 1960s, which prompted an "exodus of scholars" from theological ethics to the burgeoning field of secular bioethics [1]. Yet, as secular approaches have gained dominance, questions about their philosophical completeness and practical adequacy have persisted, leading to renewed examination of theological perspectives within pluralistic ethical discourse [2] [1].
Historical Development: From Religious Roots to Secular Frameworks
Theological Foundations of Medical Ethics
The earliest foundations of Western medical ethics were deeply embedded in religious traditions and frameworks. The Hippocratic School in ancient Greece (c. 430 BCE) produced one of the first formal medical ethical codes, yet even this "secular" development maintained connections to healing deities and cultic practices [3]. Within the Christian tradition, medical ethics initially developed as an "expression of faithfulness," with early Christian physicians like Luke (evangelist and physician) and fourth-century twins Cosmas and Damian demonstrating how scientific medicine could be practiced consistently with religious commitment [3].
The integration of faith and medicine continued through the medieval period, with religious institutions often serving as the primary custodians of medical knowledge and ethical standards. Theological bioethics fundamentally views life as a "precious gift from God" that humans are entrusted to preserve and develop as responsible stewards rather than absolute masters [2]. This perspective establishes a framework where human dignity derives from divine creation in God's image, positioning medical practice within a context of service and responsibility rather than mere technical proficiency [2].
The Secular Turn in Bioethics
The Enlightenment Project marked a pivotal turning point in ethical reasoning, with thinkers seeking foundations for morality that could be discovered through human reason alone, independent of religious authority [4]. This philosophical shift eventually influenced medical ethics, particularly as rapid biomedical advancements in the mid-20th century presented novel ethical dilemmas that seemed to demand universally accessible frameworks [1].
The emergence of bioethics as a distinct field is frequently attributed to Van Rensselaer Potter II, who conceptualized it as a "science for survival" [2]. This secular orientation gained institutional traction through initiatives like the Bioethics Interest Group at the National Institutes of Health, which provides a discussion forum for ethical issues in biomedical research without explicit religious foundation [5]. The secularization process was further advanced through governmental initiatives such as the Presidential Commission for the Study of Bioethical Issues, which developed pedagogical materials to support ethics education in diverse professional settings [6].
Table 1: Key Historical Milestones in Bioethical Thought
| Time Period | Dominant Framework | Key Developments | Representative Figures/Texts |
|---|---|---|---|
| Pre-Antiquity | Religious/Mystical | Healing tied to priestly activities and ritual practices | Shamanic traditions; Temple healing |
| Classical Era (c. 430 BCE) | Philosophical-Religious Blend | Natural causation emphasized alongside divine acknowledgment | Hippocratic School & Oath; Galenic medicine |
| Medieval Era | Theological Dominance | Medical ethics as expression of religious faithfulness | Cosmas and Damian; Integration of Galenic medicine with Christian theology |
| Enlightenment | Emerging Secularism | Search for reason-based morality independent of religion | Philosophical challenges to religious authority |
| Mid-20th Century | Transition Period | Theological contributions to nascent bioethics field | Paul Ramsey; Early theological bioethicists |
| Late 20th Century | Secular Dominance | Principlism emerges as dominant framework | Beauchamp & Childress; Institutionalization of secular bioethics |
Comparative Analysis: Foundational Frameworks and Principles
Theological Bioethical Frameworks
Theological approaches to bioethics maintain distinct foundational principles that shape their ethical reasoning. Christian bioethics, both Catholic and Orthodox, emphasizes the concepts of love (agape), justice, and the inherent dignity of human life as created in God's image [2]. These traditions maintain that humans are not absolute masters of life but rather "responsible managers" entrusted with stewardship of God's creation [2].
The Catholic bioethical tradition has developed a sophisticated framework emphasizing the hermeneutic key of life as directed by both human and divine purposes [2]. Important documents like Pope John Paul II's encyclical Evangelium Vitae address pressing questions in medical ethics, emphasizing freedom as the foundation of human dignity [2]. Similarly, Orthodox bioethics bases its ethical judgments on Holy Scripture and Holy Tradition, with particular emphasis on the concept of human beings created in God's "image" and with the potential to achieve "likeness" to God through the process of theosis or divinization [2].
A central differentiator of theological bioethics is its teleological perspective – the understanding that human life has a specific purpose and end goal that informs moral reasoning. This stands in sharp contrast to secular approaches that often struggle to establish a coherent foundation for human dignity without reference to transcendent purpose [4].
Secular Bioethical Frameworks
Secular bioethics emerged as a deliberate attempt to develop ethical frameworks accessible to people across diverse religious and philosophical commitments. The dominant approach became principlism, as articulated by Beauchamp and Childress, which organizes ethical analysis around four key principles: autonomy, beneficence, non-maleficence, and justice [1]. This framework was intended to provide a "common moral language" for resolving ethical dilemmas in pluralistic settings.
However, secular bioethics faces significant philosophical challenges in establishing foundations for its moral claims. As Alasdair MacIntyre and others have argued, without a coherent account of human purpose (telos), secular approaches struggle to provide compelling justification for why certain principles should be universally binding [4]. The Enlightenment "failure" to establish a consensus on morality based solely on reason has led to increasing fragmentation in secular ethical theories, with some approaches leaning toward moral relativism or grounding ethics primarily in subjective sentiment [4].
Table 2: Comparison of Foundational Frameworks
| Aspect | Theological Bioethics | Secular Bioethics |
|---|---|---|
| Moral Foundation | Divine revelation, natural law, and religious tradition | Human reason, principles, and consensus |
| View of Human Life | Sacred, possessing inherent dignity as created in God's image | Value determined by human attributes, capacities, or social agreement |
| Primary Motivation | Love of God and neighbor; obedience to divine command | Human flourishing; rights protection; harm prevention |
| Concept of Justice | Based on God's character; includes equitable care for all | Social contract; fair distribution of resources |
| Approach to Dilemmas | Appeal to religious authorities, texts, and traditions | Application of principles; balancing of competing values |
| Teleology | Life has divine purpose and eternal significance | Purpose is individually determined or socially constructed |
Methodological Approaches and Applications
Research Ethics and Clinical Applications
The methodological differences between theological and secular bioethics manifest distinctly in research ethics and clinical applications. Theological approaches often incorporate distinctive methodologies such as the "mind of the Church" in Orthodox tradition or the application of natural law reasoning in Catholic bioethics [2]. These approaches maintain that certain moral truths are discoverable through reason but are fully illuminated by religious revelation.
Secular methodologies dominate contemporary research ethics, particularly through frameworks like principlism, which offers a systematic approach to ethical analysis that can be applied across diverse cultural and religious contexts [1]. This approach has been institutionalized through mechanisms like Institutional Review Boards (IRBs), which primarily operate within secular ethical paradigms [5].
The clinical application of these differing methodologies reveals substantive practical differences. Theological bioethics tends to emphasize the physician-patient relationship as one of "Agape structure of love" where medicine is understood as a mission rather than merely a profession, and patients are regarded as brothers and sisters rather than purely autonomous agents [2]. Secular bioethics, by contrast, typically emphasizes patient autonomy as a primary value, with the physician's role focused on providing information and respecting patient choices within legal and professional boundaries.
Conceptual Mapping of Bioethical Reasoning
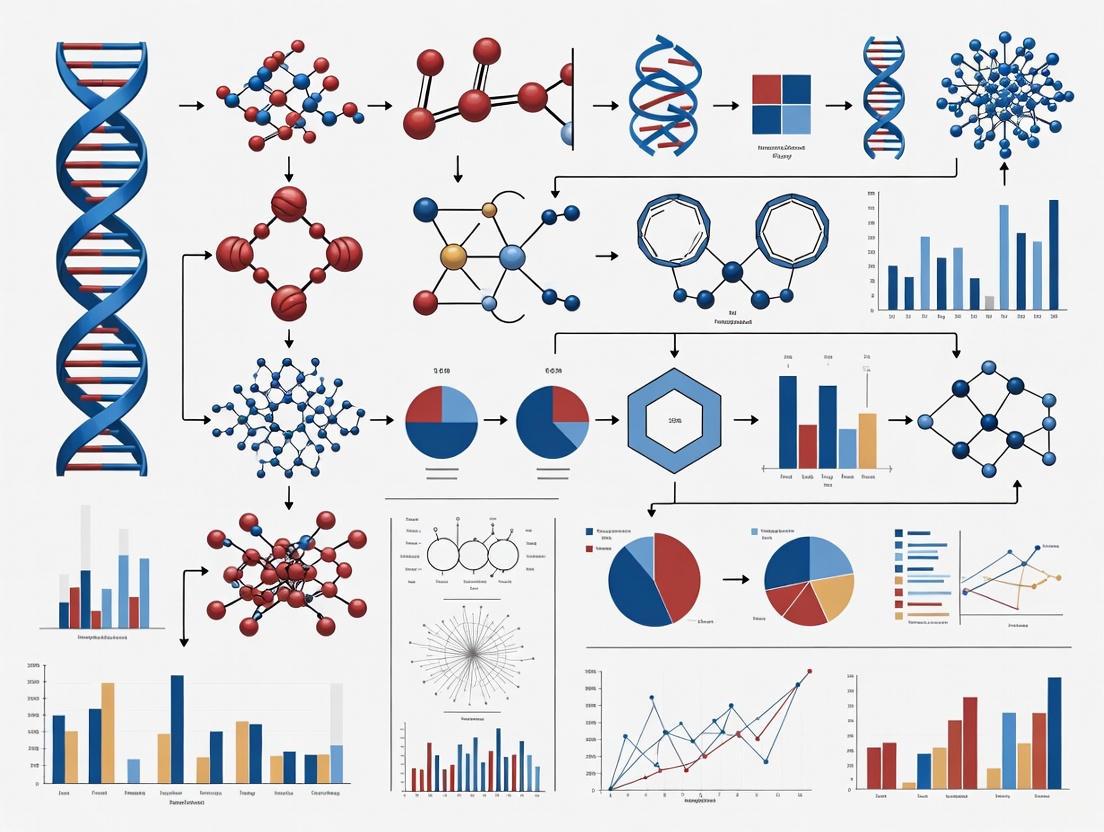
The following diagram illustrates the distinct logical pathways characteristic of theological versus secular approaches to bioethical reasoning:
Experimental Protocols and Research Methodologies
Protocol for Comparative Ethical Analysis
Objective: To systematically compare theological and secular approaches to a specific bioethical dilemma (e.g., genetic engineering, end-of-life decisions, resource allocation) and evaluate their respective reasoning processes, conclusions, and practical implications.
Materials Needed:
- Case study with complex ethical dimensions
- Reference materials from theological traditions
- Reference materials from secular ethical frameworks
- Analysis template for comparing reasoning pathways
Procedure:
- Case Presentation: Select a clinically relevant bioethical case with significant moral dimensions.
- Independent Analysis: Have theological and secular ethicists analyze the case separately using their respective frameworks.
- Reasoning Documentation: Document the step-by-step reasoning process for each approach, including:
- Identification of relevant principles/values
- Consideration of conflicting obligations
- Resolution methodology
- Final recommendation
- Comparative Evaluation: Analyze similarities and differences in:
- Foundational assumptions
- Weighting of competing values
- Practical recommendations
- Perceived strengths/limitations
Validation Metrics:
- Internal consistency of reasoning
- Clarity of foundational premises
- Practical applicability in clinical settings
- Responsiveness to stakeholder concerns
Research Reagent Solutions for Bioethical Inquiry
Table 3: Essential Analytical Tools for Bioethical Research
| Research Tool | Function | Application Context |
|---|---|---|
| Principlism Framework | Provides four-principle structure for ethical analysis | Secular clinical ethics consultation; research ethics review |
| Natural Law Methodology | Reasons from human nature and purpose to moral norms | Catholic bioethical analysis; theological anthropology applications |
| Narrative Ethics Approach | Focuses on patient and practitioner stories | Complement to principle-based approaches in both traditions |
| Virtue Ethics Framework | Emphasizes character of moral agent | Theological and secular applications; professional formation |
| Casualty Analysis Protocol | Systematically examines consequences of actions | Utilitarian assessments; public policy development |
| Theological Anthropology Resources | Provides understanding of human nature and purpose | Distinctively theological bioethical reasoning |
Current Landscape and Emerging Trends
The Contemporary Resurgence of Theological Voices
Despite the continued dominance of secular frameworks in academic and clinical bioethics, there are signs of renewed engagement with theological perspectives. This resurgence stems partly from recognition of the "impoverished" nature of bioethical discourse that completely excludes religious voices and traditions [1]. The Christian BioWiki, for instance, represents a significant effort to document Christian denominational positions on bioethical issues, providing researchers with comprehensive resources for understanding theological perspectives [7].
There is growing acknowledgment that theological traditions offer robust conceptual resources for addressing novel ethical challenges posed by emerging technologies. The extensive reflection on human nature, purpose, and morality within religious traditions provides valuable frameworks for considering the ethical implications of genetic engineering, artificial intelligence, and human enhancement technologies [2] [7].
Integrative Approaches and Future Directions
The current bioethical landscape shows increasing interest in integrative approaches that incorporate insights from both theological and secular perspectives without collapsing their distinctive foundations. Scholars like Jeffrey Bishop and Tristram Engelhardt have modeled approaches that take seriously both the insights of secular philosophy and the wisdom of religious traditions, particularly Orthodox Christianity [2] [1].
The clinical context often demands practical ethical resolutions that can be accepted by stakeholders from diverse philosophical and religious backgrounds. This practical necessity has led to the development of procedural approaches that focus on fair decision-making processes while allowing for substantive disagreement on foundational questions. Nevertheless, researchers and clinicians increasingly recognize that truly comprehensive bioethical analysis requires engagement with the deep philosophical and theological assumptions that underpin different approaches to medicine, health, and human flourishing.
The historical transition from theological foundations to secular dominance in bioethics represents more than an academic curiosity; it has tangible implications for how researchers, scientists, and drug development professionals approach ethical dilemmas in their work. Understanding the comparative strengths and limitations of each framework enables more sophisticated ethical analysis and promotes greater self-awareness about the presuppositions underlying different approaches to bioethical challenges.
The secularization thesis in bioethics, while accurately describing the field's institutional development, may have underestimated the enduring relevance of theological perspectives. Contemporary bioethics appears to be moving toward a more pluralistic model that makes space for both secular and religious voices, recognizing that each offers valuable insights for navigating the complex ethical terrain of modern medicine and biotechnology. For professionals engaged in clinical research and drug development, this historical perspective provides essential context for understanding current ethical frameworks and anticipating future developments in bioethical thought.
The rapid advancement of technological frameworks, particularly transhumanism and artificial intelligence (AI), presents a paradigm shift in how humanity conceptualizes its future. These disciplines, grounded in materialist and computational philosophies, increasingly influence clinical practice and biomedical research. However, a significant gap has emerged: the systematic exclusion of spiritual and theological dimensions from their foundational principles and applications. This exclusion is particularly problematic in bioethics, where questions of human dignity, purpose, and meaning intersect with medical practice [8] [9].
Transhumanism, as articulated by thinkers like Julian Huxley, Max More, and Nick Bostrom, advocates for using technology to transcend human biological limitations, envisioning a future of enhanced capabilities, extended lifespans, and even immortality [8] [10]. This vision is underpinned by technological determinism, the belief that technological progress is the primary, inevitable driver of human evolution [8]. Similarly, dominant AI narratives, influenced by figures like Ray Kurzweil and Yuval Harari, often reduce human beings to complex algorithms and data processing systems, a worldview sometimes termed Dataism [9]. This paper argues that these frameworks operate with a reductive anthropology that neglects essential aspects of human personhood, creating an urgent need for theological bioethics to engage with and validate its principles within clinical research practice.
Analytical Framework: Core Principles and Their Spiritual Contradictions
Table 1: Core Principles of Technological Frameworks vs. Theological Bioethics
| Framework | Core Principle | Anthropological View | Stance on Mortality & Finitude | Primary Ethical Focus |
|---|---|---|---|---|
| Transhumanism | Human limitations are engineering problems to be solved [8] [10]. | A substrate for enhancement; conditional dignity based on capacities [8] [11]. | A flaw to be eliminated [8] [9]. | Progress, efficiency, and the transcendence of biological constraints. |
| AI Dataism | Human thought and identity are algorithms and data processing [9]. | An information processor; consciousness is an emergent property or illusion [9]. | Irrelevant if information can be preserved (digital immortality) [9]. | Optimization, pattern recognition, and data-driven decision-making. |
| Theological Bioethics | Human life is a gift with inherent dignity [8] [2]. | An integrated unity of body, mind, and spirit, created in the imago Dei [8] [2]. | A natural part of the human condition with potential meaning [8]. | The protection of human dignity, community, and spiritual flourishing. |
The gap between these technological frameworks and spiritual traditions is not merely a matter of different priorities but stems from fundamentally incompatible starting points. Transhumanism and Dataism are rooted in a materialist metaphysics that either dismisses non-material realities like consciousness and spirit or reduces them to epiphenomena of physical processes [9]. Theologian Nathan Mladin describes this as an "ambient ideology," a worldview so pervasive it escapes critical examination [11]. In contrast, theological bioethics—whether Christian, Islamic, or Jewish—begins with the premise that human beings are spiritual entities with a nature and purpose that transcend material composition [2] [9] [7]. This foundational disagreement explains why spiritual dimensions are not merely underemphasized but actively excluded; they are deemed non-existent or irrelevant within the materialist paradigm.
Quantitative Analysis: Documenting the Exclusion in Research
A review of current literature and research trends reveals a significant lack of integration between technological and spiritual perspectives. This gap is quantifiable in research focus, funding, and clinical application.
Table 2: Quantitative Evidence of the Spiritual Gap in Technological Research
| Area of Analysis | Focus of Mainstream Tech/AI Research | Research Integrating Theological Perspectives | Key Indicator of Exclusion |
|---|---|---|---|
| Human Identity | Cognitive enhancement, memory backup, mind uploading as information transfer [9] [10]. | Limited discussion of the soul, relational personhood, and theosis (divinization) [2] [9]. | Absence of non-materialist anthropologies in technical literature. |
| Suffering & Finitude | Elimination of suffering, defeat of aging and death via cryonics, anti-aging therapies [8] [10]. | Theological exploration of suffering's potential meaning and acceptance of natural life cycles [8]. | Dismissal of redemptive suffering as an "antiquated view" [8]. |
| Purpose of Medicine | Enhancement, radical life extension, and optimization of human capabilities [12] [10]. | Healing, wholeness, and care within the context of a finite life [2] [13]. | Marginalization of "healing" as a goal in favor of "augmentation." |
| Ethical Foundations | Principle-based (autonomy, beneficence) and consequence-based utilitarianism [7]. | Virtue ethics, divine command, and the pursuit of holiness and love (Agape) [8] [2]. | Lack of theological voices in AI ethics boards and tech policy design. |
The exclusion is further evidenced by the practical trajectory of technology. For instance, the Swedish transhumanist movement reports tangible progress in NFC microchip implants and human-AI integration, with goals focused entirely on practical enhancement without reference to spiritual impact [12]. Forecasts for transhumanism by 2040 predict legal and social redefinitions of "human" based solely on technological integration, with any backlash categorized as "moral panic" from religious sectors, thereby framing spiritual concerns as irrational obstacles to progress [10].
Experimental Protocol: A Methodology for Investigating the Gap
To systematically validate the exclusion of spiritual dimensions and test the claims of theological bioethics within clinical research, the following experimental protocol is proposed. This methodology is designed to generate empirical data on the impact of technological frameworks on human spirituality and well-being.
Study Design
- Title: A Mixed-Methods Investigation of Neurotechnology-Assisted Meditation and Spiritual Experience.
- Objective: To quantify the qualitative differences in spiritual experiences between traditional contemplative practices and technology-assisted methods (e.g., EEG neurofeedback, AI-guided meditation).
- Hypothesis: Traditional, disciplined contemplative practice will yield significantly different and subjectively "deeper" reports of spiritual experience (e.g., sense of transcendence, connection, love, and awe) compared to technology-assisted shortcuts.
Participant Groups and Intervention
- Group 1 (Traditional): Undergoes training in a established contemplative practice (e.g., Centering Prayer, Hesychasm, mindfulness of breath) for 30 minutes daily over an 8-week period. Guidance will be provided by an experienced practitioner.
- Group 2 (Tech-Assisted): Uses an AI-guided meditation app with integrated neurofeedback (EEG headset) for the same duration and frequency. The AI will optimize the session in real-time to induce states of "calm" or "focus" based on biometric data.
- Control Group: Engages in a period of quiet reading of neutral material for the same duration.
Data Collection and Analysis
- Quantitative Measures: Pre- and post-intervention fMRI scans to map default mode network (DMN) activity; standardized psychological scales for mindfulness (Five Facet Mindfulness Questionnaire) and self-transcendence (Temperament and Character Inventory).
- Qualitative Measures: In-depth, structured interviews conducted post-intervention focusing on the nature of the participants' experiences, using terms like "connection," "gift," "effort," "love," and "presence." Thematic analysis will be applied to the interview transcripts.
- Statistical Analysis: ANOVA will be used to compare quantitative changes between groups. Qualitative data will be coded and analyzed for emergent themes related to spiritual depth and relationality.
The following workflow diagram illustrates the experimental design:
Diagram 1: Experimental workflow for investigating technology's impact on spiritual experience.
The Scientist's Toolkit: Research Reagents and Materials
Table 3: Essential Materials for Investigating Technology-Spirituality Interface
| Item | Function in Research |
|---|---|
| 64-Channel EEG System with Neurofeedback Suite | To provide real-time biometric data and enable the technology-assisted intervention for Group 2. Measures brainwave patterns associated with meditative states. |
| AI-Guided Meditation Software | The algorithmic core of the tech-assisted intervention. It adapts audio guidance and feedback based on the user's EEG data to optimize for pre-defined states like "calm." |
| 3T fMRI Scanner | To capture high-resolution images of brain activity pre- and post-intervention. Crucial for comparing neurological correlates of different practices, particularly changes in the Default Mode Network (DMN). |
| Validated Psychometric Scales (e.g., FFMQ, TCI) | To provide quantitative, standardized measures of subjective constructs like mindfulness, self-transcendence, and personality traits. |
| Semi-Structured Interview Protocol | To gather rich, qualitative data on the subjective quality, meaning, and relational aspects of the participants' experiences, which quantitative data alone cannot capture. |
Theological Bioethics as a Corrective Framework
Theological bioethics offers robust conceptual frameworks to address the gaps identified in transhumanism and AI. Its validation in clinical research is not a retreat to obscurantism but a necessary step toward a more holistic and human-centered technological future.
The Concept of the Human Person: Against the transhumanist view of the body as a upgradeable machine, theological bioethics posits a holistic anthropology. Catholic teaching, for example, emphasizes hylomorphism—the body and soul as an integral unity [8]. This view sees the body not as a prison for the soul but as a constitutive part of human identity. Similarly, Orthodox bioethics distinguishes between the "image" of God (the donum of intellect and will) and the "likeness" of God (the potential for theosis, or divinization), affirming a human nature that is both given and with a dynamic potential for growth in holiness [2]. This directly challenges the transhumanist project of self-designed post-humanity.
The Meaning of Suffering and Finitude: Transhumanism identifies suffering and death as unqualified evils to be eradicated. In contrast, theological traditions, while affirming the goodness of healing, also acknowledge the potential redemptive meaning of suffering [8]. Pope John Paul II's Salvifici Doloris teaches that suffering, when united with Christ's passion, can be a site of spiritual growth and communion [8]. This perspective reframes the goal of medicine from the total elimination of suffering to its alleviation and the finding of meaning within it, fostering virtues like compassion, patience, and solidarity [8].
Agape vs. Algorithm as a Foundation for Ethics: The dominant ethical models in AI and technology are utilitarianism and principlism, which lack a robust account of love and self-sacrifice. Theological bioethics centers on disinterested, self-giving love (Agape) [2]. This love is not a mere emotion but a fundamental orientation that sees medicine not just as a profession but as a mission of brotherly and sisterly care [2]. This stands in stark contrast to the "Dataism" described by Harari, which reduces human relationships and values to data patterns and algorithmic optimization [9].
The following diagram illustrates the conceptual conflict between these worldviews:
Diagram 2: Logical conflict between technological and theological paradigms.
The investigation reveals a profound and systematic exclusion of spiritual dimensions from the core frameworks of transhumanism and AI. This gap is not accidental but stems from a materialist and reductionist worldview that is incapable of accounting for the full reality of human personhood, including consciousness, qualitative experience, love, and the quest for transcendent meaning [11] [9]. For researchers, scientists, and drug development professionals, this creates a blind spot, potentially leading to technologies that augment human capacities while eroding the very qualities that make life worth living.
Validating theological bioethics in clinical practice research is therefore an urgent task. It requires moving beyond a dialogue of the deaf and actively designing experiments, like the one proposed here, that can empirically test the claims of spiritual traditions about human nature and flourishing. The goal is not to halt technological progress but to guide it with the wisdom of traditions that have reflected deeply on human dignity, purpose, and destiny for millennia. As Holmes Rolston warned, "the religion that is divorced from science today will leave no offspring tomorrow" [14]. The inverse is equally true: a science and a technological ethos divorced from spiritual wisdom may create a future that is technologically sophisticated but spiritually barren. The integration of these domains is essential for a future that is both advanced and truly human.
The integration of theological anthropology into biomedical ethics provides foundational perspectives on human value, finitude, and reasoning that remain critically relevant to clinical practice and research. This guide compares three core theological concepts—human dignity, vulnerability, and the noetic effects of sin—examining how they contribute to a comprehensive framework for bioethical deliberation. These concepts offer distinct yet complementary resources for addressing perennial challenges in healthcare ethics, from end-of-life decisions to equitable research practices. Rather than presenting competing alternatives, these theological constructs form an integrated analytical toolkit for examining the philosophical underpinnings of clinical practice and research ethics. Their validation emerges through consistent application across diverse biomedical contexts, from inpatient care to research ethics committees, where they provide robust accounts of human value amidst biological fragility and cognitive limitation.
Conceptual Frameworks & Comparative Analysis
Theological Foundations of Human Dignity
Table 1: Conceptualizations of Human Dignity in Theological Bioethics
| Concept Type | Theological Foundation | Key Characteristics | Practical Implications in Healthcare |
|---|---|---|---|
| Intrinsic Dignity | Imago Dei (creation in God's image); inviolable and unconditional [15] [16] | Universal, inherent, non-contingent on capacities; equal across all persons | Requires respect for every patient regardless of clinical condition or cognitive status |
| Attributed Dignity | Human interpretation of worth based on qualities or achievements [16] | Socially constructed, variable, context-dependent | Recognizes importance of social honor while critiquing its potential biases |
| Inflorescent Dignity | Process of becoming through divine relationship; "likeness" to God [16] | Developmental, flourishing-oriented, dependent on conditions | Supports rehabilitative and palliative approaches that enable personal flourishing |
The theological concept of human dignity presents a robust alternative to autonomy-based ethical frameworks predominant in secular bioethics. Grounded primarily in the concept of imago Dei (creation in God's image), theological approaches understand dignity as an inviolable characteristic that is "donated graciously and creatively to all bearers of imago Dei" [15]. This foundation establishes human dignity as "absolute" and "independent of autonomy, rationality, or capability" [15], providing an ethical warrant for protecting vulnerable populations who might be marginalized in capacity-based ethical systems.
This theological understanding contrasts with secular approaches that frequently equate dignity with autonomy or rational capacity. The Swiss assisted-dying organization Dignitas, for example, employs the language of dignity while operating with an underlying definition that essentially reduces to personal autonomy [15]. Theological frameworks resist this reduction, instead locating human worth in the creative act of God and the incarnation of Christ, which confers dignity unconditionally on all human beings [17] [16]. This perspective proves particularly significant in end-of-life care, dementia care, and disability ethics, where cognitive or physical impairment might otherwise undermine ethical standing.
Vulnerability as Layered and Contextual
Table 2: Approaches to Vulnerability in Bioethics
| Framework | Understanding of Vulnerability | Strengths | Limitations |
|---|---|---|---|
| Traditional Approach | Fixed characteristic of specific subpopulations [18] | Clear identification of at-risk groups | Risk of stereotyping; overlooks contextual factors |
| Layered Approach (Luna) | Relational, dynamic, and multi-dimensional [18] | Accounts for complexity; identifies modifiable factors | Requires more nuanced ethical analysis |
| Philosophical Accounts | Universal human condition with physical, emotional, and cognitive dimensions [19] | Comprehensive view of human experience | May overlook specific heightened vulnerabilities |
Contemporary theological bioethics has developed sophisticated approaches to human vulnerability that resist essentializing or stigmatizing interpretations. Florencia Luna's layered approach conceptualizes vulnerability as "relational and dynamic" rather than as a fixed property of certain individuals or groups [18]. This framework identifies vulnerability as emerging through the interaction between internal dispositions and external "trigger conditions" that actualize latent vulnerabilities [18]. This approach helps explain how vulnerabilities can compound through "cascading effects," where one form of vulnerability exacerbates or generates additional vulnerabilities [18].
Theological perspectives enrich this understanding by framing vulnerability as an intrinsic aspect of human finitude and embodiment rather than merely a problem to be eliminated. Philosophical accounts further distinguish between physical, emotional, and cognitive vulnerability, noting that all represent "a state of physical, emotional, and cognitive stability that is in danger of being disturbed or destroyed due to being susceptible to destabilizing influences" [19]. In healthcare contexts, these vulnerabilities become particularly salient as patients confront illness, institutional settings, and complex decision-making [19]. A theological approach acknowledges these vulnerabilities while simultaneously affirming the enduring dignity of the vulnerable person.
Noetic Effects of Sin on Ethical Reasoning
The Reformed theological concept of the "noetic effects of sin" describes how sin distorts human intellectual capacities, including ethical reasoning [20]. The term "noetic" derives from the Greek noētikos ("intellectual"), referring to how sin "sabotages our intellectual lives" [20]. This distortion operates at two levels: it affects both the "object known" (the ethical issue under consideration) and the "personal subject" (the moral reasoner) [20].
This concept explains why even carefully reasoned ethical analyses may systematically exclude or distort morally salient considerations, particularly regarding "core issues at the center of the human condition" [20]. The noetic effects of sin are especially potent in bioethical debates that touch on fundamental anthropological questions about human nature, dignity, and the limits of human agency. These effects manifest through cultural, psychological, economic, and ideological influences that shape ethical deliberation, often in ways that remain opaque to the reasoner themselves [20]. Understanding these dynamics fosters intellectual humility and underscores the value of dialogical approaches to bioethics that incorporate diverse perspectives to mitigate individual and cultural blind spots.
Interrelationship of Core Concepts: Diagrammatic Representation
The diagram above illustrates how these three core concepts interrelate within a comprehensive theological bioethics framework. Human dignity provides the foundational principle that grounds moral consideration, while the recognition of vulnerability identifies specific moral claims and obligations. The noetic effects of sin introduce an essential critical principle that qualifies all ethical reasoning, encouraging intellectual humility and procedural safeguards. Together, these concepts generate bioethical reasoning enhancements that inform specific practical applications in clinical practice and research.
Experimental Protocols & Research Methodologies
Dignity Impact Assessment Protocol
Objective: Systematically evaluate how clinical protocols or research methodologies affect patient dignity across multiple dimensions.
Methodology:
- Instrument Development: Create assessment tools measuring intrinsic, attributed, and inflorescent dignity using validated scales [16].
- Multi-dimensional Mapping: Document how specific clinical interventions affect each dignity dimension through patient interviews, structured observation, and staff surveys.
- Trigger Analysis: Identify specific aspects of clinical environments or procedures that undermine dignity, with particular attention to populations with layered vulnerabilities [18].
- Intervention Design: Develop and test dignity-conserving practices targeting identified vulnerabilities.
Validation Metrics: Pre/post-intervention dignity scale scores; patient satisfaction measures; staff awareness and attitude assessments; analysis of ethical complaints or incidents.
Vulnerability Layering Analysis Framework
Objective: Identify and address layered vulnerabilities in research populations using Luna's framework.
Methodology:
- Contextual Assessment: Document internal and external factors creating vulnerability dispositions in potential research populations [18].
- Trigger Identification: Analyze research protocols for elements that might activate latent vulnerabilities (e.g., complex consent forms, power differentials, economic incentives) [18].
- Cascading Effect Projection: Model how initial vulnerabilities might generate additional vulnerabilities throughout research participation.
- Mitigation Strategy Development: Design targeted protections for identified vulnerability layers, emphasizing autonomy preservation rather than blanket exclusion [18].
Validation Metrics: Successful recruitment of vulnerable populations without exploitation; participant comprehension metrics; protocol adherence rates; post-study participant feedback.
Cognitive Bias Audit for Research Ethics Committees
Objective: Identify and mitigate the noetic effects of sin in ethical review processes.
Methodology:
- Deliberation Analysis: Document ethical review discussions using standardized coding frameworks to identify patterns of unexamined assumptions or systematic blind spots [20].
- Stakeholder Perspective Integration: Incorporate patient, community, and interdisciplinary viewpoints to challenge disciplinary or cultural biases.
- Counterfactual Reasoning: Employ "red team" exercises where members specifically argue against provisional approvals to test robustness of ethical reasoning.
- Reflective Practice Implementation: Introduce structured reflection on how reviewers' own backgrounds, interests, and ideologies might shape ethical evaluations [20].
Validation Metrics: Diversity of perspectives in ethical discussions; documentation of considered counterarguments; tracking of dissenting opinions; post-decision outcome evaluation.
The Scientist's Toolkit: Research Reagents for Theological Bioethics
Table 3: Essential Conceptual Resources for Theological Bioethics Research
| Research Tool | Function | Application Context |
|---|---|---|
| Imago Dei Framework | Provides foundation for universal human dignity independent of capacity or function [15] [17] | Grounding research ethics; protecting vulnerable populations; resisting quality-of-life determinations |
| Layered Vulnerability Analysis | Identifies contextual and interacting vulnerability factors beyond categorical approaches [18] | Research ethics protocol development; equitable participant selection; clinical trial design |
| Noetic Effects Audit | Critical tool for identifying cognitive biases and systematic blind spots in ethical reasoning [20] | Research ethics committee deliberations; clinical ethics consultation; policy development |
| Dignity Typology Matrix | Distinguishes between intrinsic, attributed, and inflorescent dignity for precise ethical analysis [16] | Patient care quality assessment; evaluating institutional culture; developing dignity-conserving interventions |
| Theological Hermeneutic of Suspicion | Identifies where technological possibilities drive ethical justification rather than ethical reasoning guiding technology [20] [21] | Emerging technology assessment; clinical innovation oversight; policy development for novel interventions |
Comparative Performance & Research Applications
Theological frameworks demonstrate distinctive strengths when applied to complex bioethical challenges in clinical research environments. The concept of intrinsic dignity grounded in imago Dei provides particularly robust protection for vulnerable research populations, including those with cognitive impairment, neonates, and other groups frequently marginalized in capacity-based ethical systems [15] [17]. This approach resists utilitarian calculations that might sacrifice individual protection for collective knowledge advancement.
The layered model of vulnerability enables more nuanced ethical oversight than traditional categorical approaches to vulnerability in research ethics [18]. By recognizing how vulnerabilities interact and cascade in specific contexts, this framework supports more precise safeguards that protect without unjustly excluding populations from research participation and potential benefit [18]. This approach facilitates the ethical inclusion of populations with complex vulnerability profiles rather than invoking blanket exclusion.
The concept of the noetic effects of sin provides a unique critical tool for examining the ethical reasoning process itself [20]. This theological principle anticipates and explains how even sophisticated ethical deliberation can systematically exclude morally salient considerations, particularly when addressing questions with significant anthropological implications. Research ethics committees applying this principle demonstrate enhanced capacity to identify cultural, ideological, and economic biases that might otherwise distort ethical analysis.
These theological resources prove particularly valuable when addressing emerging biotechnologies that challenge traditional ethical categories. By providing stable anthropological foundations while acknowledging human cognitive limitations, this integrated framework supports both principled analysis and appropriate humility in navigating novel ethical challenges across the clinical research continuum.
The contemporary healthcare landscape is marked by a critical tension between technological advancement and the preservation of humane treatment. This analysis objectively examines two competing "products" in healthcare delivery: the dehumanizing care model, characterized by fragmented, impersonal treatment, and the comprehensive care model, which prioritizes holistic, patient-centered approaches. The investigation is framed within an emerging paradigm that validates theological bioethics as a framework for clinical practice research, offering a moral architecture for understanding human dignity in healthcare contexts. Theological bioethics, rooted in the concept that human life possesses inherent dignity as a "precious gift from God" [2], provides critical standards for evaluating these competing approaches. This comparison utilizes empirical data to assess performance metrics including patient outcomes, therapeutic relationships, and systemic efficiency, offering evidence-based insights for researchers, scientists, and drug development professionals dedicated to optimizing healthcare delivery systems.
Dehumanization in Healthcare: Mechanisms and Impacts
Dehumanization in healthcare represents a systematic failure to recognize the full humanity of patients, transforming them from persons into cases, diseases, or administrative tasks. Research reveals that dehumanization operates on a spectrum from blatant to subtle forms, with patients implicitly denied fundamental human qualities like rationality, self-control, and complex emotions [22]. This phenomenon is not merely an interpersonal issue but is often structured into healthcare systems through excessive workloads, bureaucratic procedures, and technologically-mediated interactions that reduce patients to their diagnoses.
Functional and Structural Causes of Dehumanization
- Emotional Regulation Strategy: Healthcare professionals may unconsciously dehumanize patients as a coping mechanism to manage the emotional distress of constantly witnessing suffering and pain. This emotional regulation strategy helps providers avoid burnout but at the cost of empathetic connection [23].
- Task-Oriented Focus: Medical training often emphasizes diagnostic efficiency through a narrow focus on specific body parts or diseases, potentially at the expense of viewing the patient as a whole human being. This functional dehumanization may increase diagnostic effectiveness but damages the therapeutic relationship [23].
- Structural and Organizational Factors: Excessive workloads, insufficient staffing, and administrative burdens create environments where professionals are treated as "interchangeable cogs in an industrial machine," leading to cascading dehumanization of patients [22]. The "black-box" nature of increasingly integrated AI systems further risks depersonalizing healthcare by prioritizing data-driven decisions over empathetic, personalized care [24].
Documented Consequences of Dehumanized Care
The impacts of dehumanization extend beyond subjective patient dissatisfaction to measurable clinical outcomes:
Table 1: Documented Impacts of Dehumanization on Patient Outcomes
| Impact Category | Specific Consequences | Affected Populations |
|---|---|---|
| Clinical Outcomes | Reduced treatment adherence, relapse in substance use disorder, poorer health outcomes [23] | All patients, particularly those with chronic conditions |
| Therapeutic Relationship | Reduced patient satisfaction with care, poorer communication [23] | All patient demographics |
| Psychological Effects | Increased sadness, shame, self-consciousness, lower self-esteem [23] | Patients with visible stigmas or mental health conditions |
| Self-Perception | Internalized dehumanization (self-dehumanization) associated with self-harm behaviors and reduced social interaction [23] | Patients with severe alcohol use disorders, mental health conditions |
| Decision-Making | Undermined patient autonomy and informed decision-making [23] | All patients, particularly evident in vulnerable populations |
The negative effects of dehumanization are particularly pronounced among patients with mental illness, who face "additive or cumulative dehumanization" that contributes to documented health inequities [23]. These patients are often dehumanized more blatantly than some vilified ethnic or religious minorities, demonstrating how diagnostic labels can trigger profound denial of human attributes [22].
Comprehensive Care Models: Evidence and Outcomes
In contrast to dehumanizing approaches, comprehensive care models explicitly address the whole person through integrated, multidisciplinary interventions. These models operationalize the principles of theological bioethics, which emphasizes that "the principal values of any human activity should always be man and life" [2], and that Christian justice demands "all people are equal whether they are rich or poor, and that they have an equal right to treatment" [2].
Experimental Evidence from Comprehensive Care Implementation
A rigorous observational study conducted at a public tertiary hospital in Mexico evaluated a six-month medium-intensity comprehensive care program for obesity (Programa de Atención para el Paciente con Obesidad, PAPO) that incorporated medical, nutritional, psychological, and psychiatric components [25]. The study design and outcomes offer compelling evidence for the efficacy of comprehensive approaches:
Table 2: Outcomes from Comprehensive Obesity Care Program (n=661 completers)
| Program Metric | Result | Statistical Significance |
|---|---|---|
| Retention Rate | 65% completed program | N/A |
| Average Visits Attended | 4.9 ± 1.9 visits each | N/A |
| Participants Achieving ≥5% Weight Loss | 40.1% | p < 0.01 |
| Average Weight Decrease | Δ = -4.8 kg | p < 0.01 |
| BMI Reduction | -2.3 kg/m² | p < 0.01 |
| Odds Ratio for ≥5% Weight Loss per Additional Visit | OR 1.90, 95% CI: 1.51-2.38 | p < 0.001 |
| Odds Ratio for ≥10% Weight Loss per Additional Visit | OR 2.45, 95% CI: 1.49-4.02 | p < 0.001 |
The demonstrated dose-response relationship between program engagement and outcomes underscores the importance of sustained therapeutic relationships in comprehensive care models. Each additional visit significantly increased the likelihood of achieving clinically meaningful weight loss targets, with effects becoming statistically significant after attending more than four visits [25].
Protocol for Humanizing Care Intervention
An ongoing observational study protocol in southern Spain examines the implementation of a humanization plan across relational, structural, and organizational dimensions [26]. This multi-year investigation employs a comprehensive methodology:
Study Design: Three-year multiphase approach combining cross-sectional designs, qualitative-quantitative analyses, and psychometric assessments.
Population: Patients admitted to multiple hospitals in southern Spain along with nursing professionals.
Key Dimensions Assessed:
- Relational Dimension: Therapeutic relationships, empathetic communication
- Structural Dimension: Staffing levels, resource allocation, equipment and facilities
- Organizational Dimension: Tailored protocols, clinical pathways, interdisciplinary collaboration
Outcome Measures: Health outcomes including adverse events, readmissions, mortality rates, safety, well-being, staff outcomes including burnout, job satisfaction, and intention to leave [26].
This research hypothesizes that improvement across these three dimensions will positively impact health outcomes while facilitating economic efficiency and user satisfaction - essentially creating a healthcare system that aligns with theological bioethics' emphasis on human dignity and the concept of medicine as "a mission rather than a profession" [2].
Theological Bioethics: A Framework for Integration
Theological bioethics provides a crucial conceptual framework for understanding the moral implications of dehumanization and the validation of comprehensive care models. Grounded in the conviction that human beings are created in God's image with inherent dignity, this perspective offers distinctive insights for clinical practice research.
Core Principles of Theological Bioethics
- Sanctity of Life: Contrary to quality-of-life paradigms that may justify dehumanizing practices, theological bioethics maintains that life itself is "a precious gift from God" which must be "developed and preserved by people, who have never been masters of life but rather its servants" [2].
- Agape Love as Foundation: Christian bioethics centers on self-giving love (agape), framing medicine as a vocation rather than merely a profession. This love "would never cause any discrimination among patients, but would rather care for whole life and life of all" [2], directly countering dehumanizing tendencies.
- Justice and Equity: Theological bioethics emphasizes distributive justice in healthcare, insisting that "all people are equal whether they are rich or poor, and that they have an equal right to treatment" [2]. This principle challenges systemic dehumanization that disproportionately affects marginalized populations.
- Human Freedom and Dignity: Catholic bioethics particularly emphasizes freedom as "the base of man's dignity," recognizing patients as autonomous beings with fundamental rights to participate in healthcare decisions [2].
Orthodox Christian Contributions
Orthodox bioethics offers additional dimensions through its distinction between the "image" and "likeness" of God in human persons. The "image" represents the donum of intellect, emotion, ethical judgment, and self-determination, while the "likeness" constitutes the human potential to become Godlike through ever-expanding perfection [2]. This theological anthropology provides a robust foundation for opposing dehumanization while supporting comprehensive approaches that address the full person.
Comparative Analysis: Dehumanization versus Comprehensive Care
Direct comparison of dehumanizing and comprehensive care models reveals stark contrasts in underlying mechanisms, outcomes, and alignment with ethical frameworks:
Table 3: Direct Comparison of Care Models Across Critical Domains
| Domain | Dehumanizing Care Model | Comprehensive Care Model |
|---|---|---|
| Therapeutic Relationship | Reduced to transactional interactions | Central, continuous, and empathetic |
| Patient View | Fragmented into symptoms or diagnoses | Holistic person with biological, psychological, social dimensions |
| Emotional Approach | Avoidance through detachment | Engagement through empathetic connection |
| Structural Support | Excessive workloads, limited resources | Appropriate staffing, balanced workloads |
| Health Outcomes | Reduced adherence, poorer outcomes, increased disparities | Improved clinical metrics, greater satisfaction, reduced disparities |
| Ethical Foundation | Utilitarian, efficiency-focused | Principle-based, dignity-oriented |
The diagram below illustrates the contrasting pathways and outcomes of these two approaches:
Contrasting Pathways of Dehumanizing versus Comprehensive Care Models
Researchers investigating dehumanization and comprehensive care models require specialized methodological tools and assessment instruments:
Table 4: Essential Research Resources for Studying Dehumanization and Comprehensive Care
| Research Tool | Function | Application Context |
|---|---|---|
| Humanization Assessment Tools | Measure relational, structural, and organizational dimensions of humanized care | Evaluating hospital care quality and patient experience [26] |
| Dehumanization Scales | Assess explicit and implicit denial of human attributes to patients | Identifying subtle dehumanization in clinical settings [22] |
| Person-Centered Care Model (McCormack & McCance) | Framework for humanistic care with moral component through relationships | Implementing ideals of humanistic care in organizational structures [26] |
| Fundamentals of Care Framework (Kitson et al.) | Conceptual model acknowledging centrality of nurse-patient relationship | Addressing integration of care and context of care [26] |
| Comprehensive Program Evaluation Metrics | Assess retention, engagement, and clinical outcomes in complex interventions | Evaluating real-world implementation of comprehensive care models [25] |
| Theological Bioethics Frameworks | Provide moral architecture for understanding human dignity in healthcare | Analyzing ethical dimensions of care models and their impact on human dignity [2] [7] |
The comparative analysis between dehumanizing and comprehensive care models demonstrates a clear divergence in clinical outcomes, patient experiences, and ethical alignment. Empirical evidence establishes that comprehensive care approaches yield superior results across critical metrics including treatment adherence, clinical outcomes, and patient satisfaction. Meanwhile, dehumanizing practices, whether structural or interpersonal, generate demonstrable harm including reduced adherence, psychological distress, and exacerbated health disparities.
Theological bioethics provides a vital framework for validating comprehensive care models, offering a robust conceptual foundation grounded in human dignity, agape love, and justice. This moral architecture aligns with growing empirical evidence supporting person-centered, holistic approaches to healthcare. For researchers, scientists, and drug development professionals, these findings underscore the importance of developing and implementing healthcare interventions that honor the full humanity of patients while achieving superior clinical outcomes.
Future research directions should include more direct assessment of dehumanization in healthcare settings, improved understanding of dehumanization relative to emotion regulation processes, and continued development of comprehensive care models that address the needs of vulnerable populations, particularly those with mental illness and comorbid conditions [23]. Through such investigations, the healthcare community can systematically address dehumanization while advancing care models that truly serve the whole person.
Methodological Frameworks for Integrating Theology into Clinical and Research Ethics
For researchers and scientists in the drug development sector, bioethical dilemmas present unique challenges that demand robust, defensible frameworks for decision-making. Within Christian traditions, the approach often termed "Biblicism"—the direct application of specific biblical injunctions to contemporary moral questions—faces significant limitations when addressing novel technologies and research paradigms that did not exist in biblical times [27]. This methodological weakness becomes particularly acute in biomedical contexts, where issues like germ-line genetic intervention, cryopreservation, or nanotechnology require ethical guidance that biblical texts do not explicitly address [27].
The search for a viable ethical methodology is not merely an academic exercise but a pressing need for professionals navigating complex research environments. When scholars attempt to apply biblical texts directly to issues about which the Bible is silent, they risk either misusing Scripture or importing alien methods and influences to fill the methodological gap [27]. This paper compares the limitations of simplistic Biblicism with more robust theological frameworks that offer greater utility for clinical practice and research contexts, examining their respective capacities to address the unique ethical challenges emerging in the "Biotech Century" [28].
Methodological Frameworks: A Comparative Analysis
The Biblicist Approach: Limitations and Critiques
The Biblicist approach to bioethical dilemmas typically involves seeking direct biblical citations relevant to the issue at hand. This method works sufficiently for many traditional moral questions but reveals profound limitations when confronting novel biotechnologies [27]. Evangelical scholars have noted that this approach becomes problematic when addressing issues such as stem cell research, cloning, cybernetics, gene patenting, and other scientific developments that could not have been addressed in the Bible [27].
When explicit biblical guidance is unavailable, proponents of Biblicism may inadvertently resort to several problematic methodological approaches:
- Dubious textual interpretation: Applying biblical texts that speak only indirectly to the issue at hand [27]
- Methodological incoherence: Importing frameworks from other traditions without proper philosophical, theological, and ecclesiological context [27]
- Non-rational foundations: Basing positions on gut instinct, political loyalties, or self-interest rather than developed ethical reasoning [27]
These methodological weaknesses potentially undermine the credibility of faith-based bioethics in scientific and research contexts, where logical consistency and evidential support are paramount.
Emerging Frameworks: Principles and Theological Motifs
In response to these limitations, more sophisticated methodological approaches have emerged that engage Scripture at the level of theological principles and broad theological motifs rather than seeking direct moral injunctions [27]. This represents a movement from the level of particular moral judgments to deeper structures of moral reasoning encompassing rules, principles, and basic convictions or worldview commitments [27].
Table 1: Levels of Moral Reasoning in Theological Bioethics
| Level of Reasoning | Description | Example in Bioethics |
|---|---|---|
| Particular Moral Judgments | Decisions about specific cases or situations | Whether to participate in a specific stem cell research protocol |
| Moral Rules | Concrete action-guides for relevantly similar cases | "Do not exploit vulnerable populations in research" |
| Moral Principles | Broader, more general norms that ground rules | Respect for persons, justice, beneficence |
| Basic Convictions/Worldview | Fundamental beliefs about ultimate reality and human nature | Doctrines of creation, humanity, sin, and salvation |
This multi-layered approach enables bioethicists to develop frameworks that maintain theological integrity while engaging complex scientific contexts. Rather than looking for what is not in the Bible, scholars are forced back from the moral injunction level to other types of scriptural moral resources [27].
Experimental Philosophical Bioethics: A Bridge Framework
Conceptual Foundations and Methodology
An emerging sub-field known as experimental philosophical bioethics (bioxphi) offers promising methodological approaches for validating theological frameworks in clinical practice and research [29]. This discipline adopts the methods of experimental moral psychology and cognitive science to understand the eliciting factors and underlying cognitive processes that shape people's moral judgments about real-world bioethical concerns [29].
Bioxphi seeks to contribute to three main aims:
- Studying a wider range of stakeholder judgments beyond those of professional philosophers and bioethicists [29]
- Investigating how these judgments function in ecologically valid contexts that resemble clinical or real-life situations [29]
- Developing a richer understanding of the underlying cognitive processes and eliciting factors that shape moral judgments [29]
This methodological approach is particularly valuable for theological bioethics as it provides empirical tools for investigating how religious commitments actually function in moral decision-making across diverse contexts.
Experimental Protocols and Research Design
Bioxphi employs rigorous experimental protocols to investigate moral cognition in bioethical contexts. The following diagram illustrates a typical experimental workflow in this field:
The experimental approach typically employs consultative methods that involve collecting empirical data relating to stakeholder views, attitudes, and experiences, then using these as a basis for drawing normative conclusions [29]. The end goal is often the achievement of coherence between stakeholder data and broader considerations, including background theories, moral principles, expert intuitions, morally relevant facts, and considered judgments—a process termed wide reflective equilibrium [29].
Table 2: Bioxphi Research Strategies for Normative Inference
| Strategy | Description | Application to Theological Bioethics |
|---|---|---|
| Parsimony | Preferring explanations that require fewer ad hoc assumptions | Testing whether theological principles provide more coherent explanations than secular frameworks |
| Debunking | Identifying problematic origins of moral judgments | Examining whether judgments are based on relevant theological principles or extraneous factors |
| Triangulation | Using multiple methods to investigate the same phenomenon | Combining survey, qualitative, and experimental approaches to moral cognition |
| Pluralism | Acknowledging multiple valid perspectives while maintaining normative commitments | Understanding how different theological traditions address common bioethical challenges |
Theological Frameworks for Bioethical Reasoning
Principles for Religious Accommodation in Bioethics
In pluralistic research and clinical environments, frameworks for religious accommodation must balance claims of religious liberty with claims to equal treatment in health care [30]. Several mid-level principles have been proposed to guide such accommodation in biomedical contexts [30]:
- Principle of Respect for Conscience: Protecting the integrity of individual moral convictions
- Principle of Professional Responsibility: Defining the core obligations of healthcare and research professionals
- Principle of Public Reason: Ensuring that policy justifications are accessible to all citizens
- Principle of Civic Hospitality: Creating space for religious expression within civic institutions
These principles function as prima facie guidelines rather than absolute rules, requiring careful interpretation and balancing in specific contexts [30]. For drug development professionals, such frameworks offer resources for navigating conflicts between religious commitments and professional responsibilities in increasingly secular and pluralistic environments [31].
Natural Law and Theological Anthropology
Some Christian bioethicists have turned to natural law theory as a framework for ethical reasoning that maintains theological integrity while engaging pluralistic contexts [31]. Contrary to mischaracterizations, natural law in the Thomistic tradition is not an attempt to construct morality without God but represents "the rational creature's participation in the eternal law" [31].
This approach is complemented by robust theological anthropologies that inform bioethical decision-making. Orthodox Christian bioethics, for example, emphasizes the concept of humans created in God's "image" and "likeness"—where "image" represents the donum of intellect, emotion, ethical judgment, and self-determination, while "likeness" represents the human potential to become Godlike through the process of theosis or divinization [2]. This theological framework provides a foundation for ethical reasoning that acknowledges both human nature as a given and human potential for transformation and growth.
The following diagram illustrates how these theological frameworks structure bioethical reasoning:
Research Reagents and Methodological Tools
The empirical investigation of theological bioethical frameworks requires specific methodological tools and approaches. The table below details key "research reagents"—conceptual and methodological resources—for conducting this interdisciplinary work:
Table 3: Research Reagent Solutions for Theological Bioethics Investigation
| Research Reagent | Function | Application Example |
|---|---|---|
| Ecologically Valid Scenarios | Experimental stimuli resembling real-world clinical/research dilemmas | Developing vignettes about genetic engineering decisions that mirror actual research contexts |
| Moral Judgment Measures | Quantitative and qualitative assessment of ethical evaluations | Using Likert scales and open-ended responses to assess permissibility judgments |
| Process Tracing Methods | Identifying cognitive processes underlying moral decisions | Think-aloud protocols or cognitive load manipulations during bioethical decision-making |
| Stakeholder Diversity Sampling | Ensuring representation of relevant perspectives | Including patients, researchers, ethicists, and religious adherents in studies |
| Theological Commitment Measures | Assessing the nature and strength of religious beliefs | Scales measuring doctrinal adherence, religious practice, and spiritual experiences |
| Cross-Traditional Comparison | Investigating patterns across different religious traditions | Comparing Catholic, Orthodox, and Protestant responses to the same bioethical dilemma |
The movement from Biblicism to theological principles and doctrines represents a methodological maturation within Christian bioethics that enhances its capacity to contribute to contemporary clinical practice and research contexts. By developing more sophisticated frameworks that maintain theological integrity while engaging scientific complexity, bioethicists can provide resources that are both faithful to religious traditions and relevant to the challenges facing researchers and drug development professionals.
The integration of empirical methods from experimental philosophical bioethics with rich theological frameworks offers promising approaches for validating and refining ethical guidance for the "Biotech Century" [28]. This interdisciplinary approach acknowledges that while theological commitments provide essential foundational perspectives, their application to novel challenges requires careful reasoning, empirical investigation, and dialogue with multiple stakeholders in research and healthcare environments.
For scientists and researchers, these developed theological frameworks offer resources for addressing the profound human questions raised by biotechnological progress while maintaining scientific excellence and ethical integrity. As the field continues to develop, this integrative approach promises to contribute meaningfully to our collective ability to navigate the complex ethical terrain of emerging technologies while honoring the depth of religious traditions and their visions of human flourishing.
The validation of a theological bioethics framework within clinical research requires a structured comparison against prevailing secular models. This guide objectively compares their performance, supporting analysis with principles derived from Christian theology and its application in clinical settings.
Comparative Framework Analysis: Theological vs. Secular Bioethics
The table below summarizes the core principles and clinical performance of a theological framework against common secular approaches.
| Comparative Dimension | Theological Bioethics Framework | Principle-Based Secular Bioethics | Utilitarian/Consequentialist Framework |
|---|---|---|---|
| Foundational Basis | Divine revelation (Scripture), Tradition, and Reason [32] [2] | Secular philosophy (e.g., Kantian deontology) [7] | Calculation of optimal outcomes (e.g., maximum benefit) [7] |
| Concept of Human Dignity | Inherent and inviolable, derived from being created in the Imago Dei (Image of God) [32] [2] | Often inherent, but based on autonomy or rational capacity [7] | Contingent, often tied to one's quality of life or utility [2] |
| Primary Ethical Orientation | Agape (Self-giving love) and service; life as a gift to be stewarded [2] | Respect for Autonomy and individual rights [7] | Maximization of Net Benefits (e.g., for the population) [7] |
| Clinical Performance: End-of-Life Decisions | Prioritizes sacredness of life; cautions against hastening death; emphasizes palliative care as an act of love [2] [13] | Heavily influenced by patient autonomy, potentially justifying physician-assisted suicide [2] [13] | May justify withdrawal of treatment or assisted dying for resource reallocation or to end suffering [2] |
| Clinical Performance: Beginning-of-Life Issues | Protects the embryo from conception due to its potential for bearing God's image [2] [7] | Status of the embryo is debated; often tied to developmental stages or personhood theories [7] | May permit selective abortion or embryo research for potential future health benefits [2] |
| Key Strength | Provides a robust, transcendent foundation for human value and moral duties [32] [33] | Provides a common, neutral language for pluralistic settings [7] | Offers a clear, pragmatic method for resource allocation decisions |
| Key Limitation | Requires theological commitment for full acceptance; perceived as less flexible in pluralistic settings [2] | Principlism can become abstract; offers a thin account of the "good life" [7] | Can risk instrumentalizing and violating the rights of minority or vulnerable individuals [2] |
Experimental Protocol for Framework Validation
Validating a theological-ethical framework in clinical research involves assessing its applicability, coherence, and impact. The following methodology outlines a protocol for such empirical and qualitative investigation.
Study Design
- Type: Mixed-methods, multi-center study.
- Objective: To evaluate the applicability, coherence, and impact of the theological-ethical framework in real-world clinical ethical dilemmas.
- Population: Ethics committee members, clinicians, researchers, and patients from diverse institutional settings (secular, Catholic, and other Christian hospitals) [13].
Data Collection & Analysis Phases
Phase 1: Framework Application
- Method: Present identical complex case studies (e.g., involving genetic engineering, end-of-life care, resource allocation) to different ethics committees.
- Intervention: One group uses the standard principilst framework; another uses the proposed theological framework grounded in creation, anthropology, and eschatology [32] [33].
- Data Collected: Document the deliberative process, final recommendations, and reasoning.
Phase 2: Qualitative Assessment
- Method: Conduct structured interviews and focus groups with participants after Phase 1.
- Metrics: Assess perceived Internal Validity (logical coherence of the framework), Construct Validity (whether it accurately addresses the core of the ethical problem), and External Validity (its perceived applicability to broader clinical contexts) [34].
- Sample Questions: "Did the framework provide a satisfying resolution?" "Could its reasoning be explained to a patient?"
Phase 3: Outcome Measurement
- Quantitative Metrics: Track time to resolution, level of consensus among committee members, and longitudinal outcomes of the ethical decisions on patient and family well-being.
- Qualitative Metrics: Analyze interview transcripts for themes of moral distress, professional satisfaction, and the framework's capacity to navigate conflict.
Validation Criteria
The framework will be considered validated if it demonstrates:
- High Internal Validity: Consistent and logical application of core principles across diverse cases [34].
- High Construct Validity: Effectively measures and guides the resolution of the underlying theological-ethical concepts (e.g., dignity, stewardship, hope) [34].
- Meaningful External Validity: Shows adaptability and relevance across different clinical specialties and patient populations [34].
Logical Framework of Theological Bioethics
The following diagram illustrates the logical relationships and flow of reasoning within the proposed theological-ethical framework, from its foundational doctrines to its clinical application.
For researchers aiming to operationalize and validate this framework, the following tools and resources are essential.
| Tool/Resource | Function & Utility in Research |
|---|---|
| Scriptural & Traditional Sources | Provide the primary data and normative foundation for the framework's principles (e.g., Genesis 1:27 on Imago Dei) [32]. |
| Christian BioWiki (Trinity IU) | An online guide to denominational statements on bioethical issues, crucial for understanding diverse Christian perspectives [7]. |
| Qualitative Data Analysis Software (e.g., NVivo) | To code and analyze transcripts from interviews and focus groups, identifying themes related to framework validity and impact [35]. |
| Validated Survey Instruments | To quantitatively measure outcomes like moral distress, professional satisfaction, and perceived coherence of ethical decisions [34]. |
| Structured Case Analysis Templates | To ensure consistent application and comparison of the theological framework across different case studies and research sites [13]. |
| Partnerships with Clinical Ethics Committees | Provides a real-world laboratory for testing the framework and gathering data on its performance in live deliberative settings [13]. |
The integration of theological and spiritual dimensions into healthcare represents a critical frontier in the pursuit of whole person care. Operationalizing theology in clinical settings involves systematically implementing spiritual care practices grounded in theological and bioethical principles to address patient suffering and enhance healing relationships. This approach is increasingly recognized not as a supplementary service, but as a fundamental component of high-quality, compassionate healthcare [36]. Within a broader thesis on validating theological bioethics in clinical practice research, this guide compares the core methodologies, providers, and assessment protocols that constitute this field. The growing body of evidence indicates that a focus on spirituality improves patient health outcomes, including quality of life, while negative spiritual beliefs can exacerbate distress and illness burdens [36]. This analysis provides researchers and clinicians with a structured comparison of approaches for implementing theological care within evidence-based clinical frameworks.
Defining the Conceptual Framework and Care Providers
The operationalization of theology in healthcare requires precise conceptual definitions and a clear understanding of the distinct roles involved in providing spiritual care. Consensus definitions and role specifications form the foundation for rigorous research and effective clinical implementation.
Foundational Definitions
- Spirituality: The aspect of humanity that refers to the way individuals seek and express meaning and purpose and the way they experience their connectedness to the moment, to self, to others, to nature, and to the significant or sacred [36]. This broad, inclusive definition encompasses but is not limited to religious expression.
- Religion: An organized system of beliefs, practices, and symbols designed (a) to facilitate closeness to the transcendent, and (b) to foster an understanding of one's relationship and responsibility to others in living together in a community [37].
- Healing Relationship: A dynamic interaction between two persons—one vulnerable and seeking help, the other promising to care—aimed at restoring health and wholeness to the patient, or when this is not possible, the amelioration of suffering [38].
Comparative Analysis of Care Providers
Different providers offer distinct levels of spiritual support, with varying training requirements and scope of practice, as detailed in the table below.
Table: Comparative Analysis of Spiritual Care Providers in Clinical Settings
| Provider Type | Definition & Scope | Training & Credentials | Key Competencies |
|---|---|---|---|
| Spiritual Caregiver | Provides basic spiritual support; any individual (clinician, family, volunteer) assisting with spiritual journey toward wholeness [39]. | No specialized training required; basic understanding of spiritual support [39]. | Active listening, basic emotional support, recognizing spiritual needs [39]. |
| Pastoral Caregiver | Offers spiritual guidance from a specific religious worldview; often a clergy member [39]. | Theological education and pastoral experience within a particular faith tradition [39]. | Spiritual guidance, prayer, performing rituals, counseling based on specific doctrine [39]. |
| Board-Certified Chaplain | Specialist providing emotional, spiritual, religious, pastoral, and ethical care in healthcare settings [39]. | Advanced theological education, intensive Clinical Pastoral Education (CPE), board certification, and faith group endorsement [39]. | Specialized spiritual assessment, diagnosis of spiritual distress, deep therapeutic intervention, interprofessional collaboration [39]. |
Experimental Models and Clinical Workflows
The clinical application of theological principles follows structured processes aimed at identifying and addressing spiritual needs. The following diagram illustrates the core operational workflow for implementing pastoral care in clinical settings.
Diagram: Clinical Workflow for Spiritual Care
The Healing Relationship Model
Edmund Pellegrino's healing relationship framework provides a philosophical foundation for clinical encounters, framing them as moral enterprises centered on the vulnerable patient [38]. This model unfolds through three interconnected events:
- The Fact of Illness: The patient experiences a disruption from health to illness, characterized by disorganization, vulnerability, and a diminished sense of autonomy and integrity [38].
- The Act of Profession: The clinician makes a explicit promise to care, establishing a covenant of trust and committing their knowledge and skills to the patient's healing journey [38].
- The Act of Healing: The clinician and patient collaboratively engage in therapeutic actions aimed at restoring health or, when cure is impossible, restoring wholeness and reconciling the mind-body relationship [38].
Spiritual Assessment Protocols
Spiritual assessment is the cornerstone of operationalizing theology in clinical practice. It enables the identification of spiritual distress, which is correlated with poorer physical health outcomes [40]. The assessment process occurs at different levels of depth, as shown in the following workflow.
Diagram: Spiritual Assessment Protocol
Effective spiritual assessment methodologies include:
- Comprehensive Qualitative Evaluation: Deploys open-ended questions exploring meaning, purpose, connection, and sources of hope and strength, allowing patients to express their spiritual narrative in their own words [36].
- Structured Assessment Tools: Utilizes standardized models and templates to systematically evaluate spiritual beliefs, practices, and communities, providing a reproducible framework for diagnosis and care planning [40].
- Diagnosis of Spiritual Distress: Identifies specific manifestations of spiritual pain, such as existential crisis, loss of meaning, religious struggles, or feelings of abandonment, which require targeted chaplaincy interventions [40].
Research Reagents and Methodological Tools
Conducting rigorous research on theological bioethics requires specific conceptual tools and methodological approaches. The table below details key "research reagents" essential for this field.
Table: Essential Research Reagents for Theological Bioethics Research
| Research Reagent | Function & Application | Operational Significance |
|---|---|---|
| Consensus Definitions | Standardized definitions of spirituality, religion, and care types enable reproducible research and consistent clinical application [36] [39]. | Provides the foundational lexicon required for valid instrument development, reliable measurement, and cross-study comparisons. |
| Validated Assessment Tools | Structured instruments and interview protocols for quantifying spiritual distress, needs, and well-being [40]. | Allows for the empirical measurement of subjective spiritual states, transforming qualitative experiences into quantifiable research data. |
| Theoretical Models | Frameworks such as the "Healing Relationship" and the "biopsychosocial-spiritual model of care" [36] [38]. | Supplies the conceptual architecture for hypothesizing mechanisms, designing interventions, and interpreting outcomes. |
| Clinical Workflows | Step-by-step protocols for screening, assessment, intervention, and documentation of spiritual care [40]. | Standardizes the implementation of spiritual care in practice, ensuring fidelity in research interventions and clinical translation. |
| Ethical Frameworks | Guidelines addressing moral dilemmas at the life-death boundary and principles for clinical ethics consultation [41]. | Grounds research and practice in a coherent bioethical structure, ensuring respect for patient dignity and values. |
Quantitative Evidence and Clinical Outcomes
A substantial body of quantitative research examines the relationships between religion/spirituality (R/S) and health outcomes. The following table summarizes key findings from systematic reviews in this domain.
Table: Quantitative Evidence on Religion/Spirituality and Health Outcomes
| Health Domain | Representative Findings | Research Volume & Consistency |
|---|---|---|
| Mental Health | Associations between R/S and lower rates of depression, suicide, anxiety, and substance abuse; higher levels of well-being, hope, and optimism [37]. | Approximately 50% of the vast literature consists of original quantitative studies; consistent findings across numerous studies [37]. |
| Health Behaviors | R/S correlated with positive health behaviors such as increased physical activity, lower cigarette smoking, and healthier sexual practices [37]. | Strong observational data; research volume has "exploded" since the mid-1990s [37]. |
| Physical Health | Relationships observed with lower rates of heart disease, hypertension, immune dysfunction, and overall mortality; better coping with pain and somatic symptoms [37]. | Large number of studies; theoretical models proposed explain pathways via health behaviors, social support, and psychological coping [37]. |
| Patient Expectations | Over 96% of patients identify "receiving health care that is respectful and compassionate" as very or extremely important [36]. | High patient valuation of compassionate, whole-person care that addresses spiritual needs underscores clinical relevance [36]. |
Operationalizing theology through structured pastoral care and spiritual assessment represents a validated and essential component of modern healthcare. The comparative analysis presented demonstrates a clear spectrum of care, from general spiritual support to specialized chaplaincy services, each with defined protocols and outcomes. The integration of these practices into the clinical workflow, guided by theoretical models like the "healing relationship," aligns with the evidence linking spiritual well-being to improved health outcomes. For researchers and clinicians, the continued validation of theological bioethics requires rigorous application of the defined methodologies, assessment tools, and theoretical frameworks. Future research should focus on refining spiritual assessment metrics, demonstrating causal pathways between spiritual care and health outcomes, and further integrating these practices into standard clinical ethics and patient care protocols [37] [36] [41].
The rapid integration of artificial intelligence (AI) and genetic technologies like CRISPR into drug development presents unprecedented ethical challenges that extend beyond conventional bioethics. This guide explores how diverse religious traditions provide ethical frameworks for evaluating these technologies in pharmaceutical research and clinical applications. Religious perspectives offer unique insights into fundamental questions about human dignity, divine creation, and technological stewardship that are increasingly relevant to researchers and drug development professionals. Theological bioethics contributes distinct conceptual resources—such as the Christian concept of Imago Dei (humanity created in God's image) or Islamic principles of maqa'sid al-shari'ah (the higher objectives of Islamic law)—to the ongoing validation of ethical principles in clinical practice research [2] [42] [7].
The parallel advancements in AI-driven drug discovery and genetic editing capabilities have accelerated the need for robust ethical frameworks that address both therapeutic potential and ethical boundaries. Where secular ethics often focuses on principles like autonomy and utility, religious traditions provide complementary perspectives grounded in sacred texts, theological traditions, and long-standing moral wisdom about the nature of human life and our relationship to technology [2] [7]. This guide objectively compares how different religious perspectives approach the validation of ethical guidelines for genetic technologies and AI in drug development contexts, with particular attention to their implications for research methodologies and clinical applications.
Theological Foundations for Technological Ethics
Key Religious Principles Across Traditions
Religious traditions approach bioethical questions through distinct conceptual frameworks that shape their engagement with genetic technologies and AI. The table below summarizes foundational principles from major traditions that inform their approach to technological ethics in medicine:
Table 1: Foundational Religious Principles for Technological Ethics
| Religious Tradition | Key Ethical Principles | View of Human Agency | Primary Concerns |
|---|---|---|---|
| Roman Catholic | Human dignity, common good, stewardship | Humans as co-creators with God | Protecting life, social justice, unintended consequences [2] [7] |
| Orthodox Christian | Divine-human synergy, theosis (deification) | Fulfillment of human potential | Preservation of human freedom, natural order [2] |
| Protestant | Sovereignty of God, human responsibility | Humans as stewards of creation | "Playing God," equitable access [42] |
| Islamic | Trust (amanah), public interest (maslaha) | Humans as vicegerents (khalifah) | Preservation of lineage, divine will [43] [7] |
| Jewish | Healing obligation (pikuach nefesh), repairing world (tikkun olam) | Human partnership in ongoing creation | Saving lives, practical benefits [43] |
Conceptual Frameworks for Technology Ethics
Different religious traditions employ distinct conceptual frameworks for evaluating emerging technologies. The Catholic Church often operates within what has been described as a "static divine" framework, emphasizing the protection of God's creation from technological overreach and upholding inviolable human dignity [44]. This contrasts with more process-oriented "dynamic divine" frameworks (influenced by thinkers like Teilhard de Chardin) that view technological development as potentially participating in divine self-realization through evolutionary becoming [44]. These foundational differences shape how religious traditions approach the ethical validation of technologies in clinical research.
The Christian concept of Imago Dei (image of God) provides a particularly influential framework for understanding human uniqueness and dignity in the context of AI and genetic engineering [42]. This principle raises critical questions about whether AI systems could ever embody or fundamentally alter what it means to be human, and establishes ethical boundaries for human technological activity. Similarly, Islamic bioethics employs the framework of "goals of Islamic law" (maqāṣid al-sharīʿah), which prioritizes the protection of faith, life, intellect, progeny, and property when evaluating new technologies [7]. These frameworks provide structured approaches for validating ethical guidelines in clinical practice research.
Ethical Analysis of Genetic Technologies in Drug Development
Religious Perspectives on Gene Editing Applications
Religious traditions generally distinguish between different applications of genetic technologies based on their intended purpose and potential consequences. The table below compares how major religious traditions evaluate various applications of gene editing technologies:
Table 2: Religious Perspectives on Gene Editing Applications in Medicine
| Application Type | Catholic View | Islamic Perspective | Jewish Position | Orth Christian View |
|---|---|---|---|---|
| Somatic cell editing | Cautious acceptance for therapeutic purposes [2] | Generally permissible for treating disease [43] | Often obligatory under healing imperative [43] | Acceptable with discernment [2] |
| Germline editing | Significant concerns about heritable changes [2] [45] | Typically prohibited due to lineage concerns [43] | Debated; preservation of future generations | Major concerns about altering human nature [2] |
| Enhancement uses | Generally rejected as disproportionate [2] | Typically prohibited as altering creation [43] | Varies by context and benefit | Generally rejected [2] |
| Research embryos | Significant restrictions [2] | Restrictions based on embryo moral status [43] | Context-dependent with limitations | Limited permission early stages [2] |
CRISPR Ethical Concerns Through Religious Lenses
The revolutionary CRISPR-Cas9 gene editing technology raises specific ethical concerns that religious traditions evaluate through theological frameworks. Religious analyses consistently emphasize the precautionary principle in assessing potential unintended consequences, including off-target effects (unintended changes at other genomic locations) and on-target effects (unwanted changes at the specified site) [45]. These technical safety concerns connect with broader theological worries about human fallibility and the potential for irreversible harm to human nature and future generations.
Religious perspectives also highlight concerns about justice and access to genetic therapies, noting that costly treatments could exacerbate existing health disparities between wealthy and poor populations [45]. This aligns with the Catholic principle of the "common good" and Islamic emphasis on "maslaha" (public interest), which demand equitable distribution of medical benefits [2] [7]. Additionally, many traditions express concern about the potential for a new form of eugenics that could devalue people with disabilities or genetic conditions, threatening the fundamental principle of intrinsic human worth found across religious traditions [45].
Diagram 1: Religious Ethical Evaluation of CRISPR Applications
AI Ethics in Drug Development Through Religious Lenses
Religious Frameworks for AI Evaluation in Medicine
Religious traditions provide distinctive frameworks for evaluating the ethical implications of AI in drug development. These perspectives often focus on fundamental questions about human uniqueness, moral responsibility, and technological mediation of human relationships. The Christian emphasis on Imago Dei raises critical questions about whether AI systems could ever embody or fundamentally alter what it means to be human, establishing ethical boundaries for AI development and deployment [42]. Similarly, Islamic bioethics approaches AI through the framework of "accountability" and "trusteeship" (amanah), emphasizing human responsibility for technological systems and their impacts on society [46].
Different religious traditions are developing structured approaches to AI ethics that have significant implications for drug development. The "DELTA framework" emerging from projects like Notre Dame's Faith-Based Frameworks for AI Ethics seeks to provide comprehensive guidance for AI development grounded in religious values [47]. Similarly, Islamic scholars like Dr. Mohammed Ghaly are working to bridge Islamic ethical traditions with frontier technologies, including AI applications in healthcare [46]. These frameworks address concerns about algorithmic bias in patient selection, transparency in AI-driven drug discovery, and accountability for AI-based diagnostic or treatment recommendations.
Comparative Religious Approaches to AI in Medicine
The table below compares how different religious traditions approach key ethical questions regarding AI applications in drug development and healthcare:
Table 3: Religious Perspectives on AI Applications in Drug Development
| Ethical Concern | Christian Approaches | Islamic Perspectives | Interfaith Common Ground |
|---|---|---|---|
| Algorithmic Bias | Emphasis on human dignity and justice for vulnerable populations [42] | Focus on justice (adl) and protection of public interest (maslaha) [46] | Concern about discrimination and equitable access to AI benefits |
| Transparency | Value of trust in healing relationships; concerns about "black box" algorithms [48] | Requirement of accountability and clarity in decision-making [46] | Need for explainability in medical AI systems |
| Human Agency | Protection of human moral responsibility and decision-making [42] | Preservation of human judgment as vicegerents [46] | Appropriate human oversight of AI systems |
| Data Privacy | Respect for human personhood and bodily integrity [7] | Protection of personal information as a trust (amanah) [46] | Safeguarding patient information and autonomy |
Experimental Protocols for Ethical Validation
Methodologies for Ethical Assessment
The validation of ethical principles in clinical research requires structured methodologies that can incorporate religious perspectives alongside scientific considerations. The following experimental protocol outlines a comprehensive approach for evaluating ethical dimensions of genetic technologies in drug development:
Table 4: Experimental Protocol for Ethical Validation of Genetic Technologies
| Research Phase | Methodology | Religious Engagement | Outcome Measures |
|---|---|---|---|
| Technology Assessment | Systematic review of capabilities and limitations | Theological analysis of implications for human nature | Identification of potential ethical concerns |
| Stakeholder Consultation | Focus groups with patients, researchers, clinicians | Engagement with religious leaders and ethicists | Documentation of diverse ethical perspectives |
| Principle Application | Application of ethical frameworks to specific use cases | Deliberation using religious principles and reasoning | Development of preliminary guidelines |
| Protocol Validation | Review by interdisciplinary ethics boards | Evaluation by religious ethics committees | Validated research protocols with ethical safeguards |
Research Reagent Solutions for Ethical Analysis
The methodological "toolkit" for validating theological bioethics in clinical practice research includes both conceptual and practical resources:
Table 5: Research Reagent Solutions for Ethical Analysis
| Tool Category | Specific Resources | Application in Research |
|---|---|---|
| Conceptual Frameworks | Imago Dei (Christian), Maqasid al-Shari'ah (Islamic), Tikkun Olam (Jewish) [42] [7] [43] | Provide foundational principles for ethical analysis |
| Textual Resources | Sacred texts, theological commentaries, historical ethical analyses [2] [7] | Inform understanding of traditional ethical boundaries |
| Deliberative Methods | Casuistry, principism, virtue ethics, narrative ethics [2] [7] | Structure ethical reasoning processes |
| Institutional Mechanisms | Hospital ethics committees, religious advisory boards, research ethics review | Implement oversight and accountability structures |
Diagram 2: Ethical Validation Workflow for Clinical Research
Comparative Analysis of Religious Frameworks
Convergence and Divergence in Ethical Approaches
Religious traditions display both significant convergence and notable divergence in their approaches to genetic technologies and AI in drug development. Most traditions share common concerns about safety, justice, human dignity, and appropriate human agency [45]. However, they differ in their specific determinations about morally acceptable applications, particularly regarding germline editing, enhancement uses, and the degree of human intervention in natural processes [2] [43]. These differences often reflect deeper theological commitments about divine sovereignty, human nature, and the purpose of technology.
The Catholic and Orthodox traditions strongly emphasize the protection of human dignity and the maintenance of natural moral law, expressing caution about technologies that might fundamentally alter human nature or create new forms of inequality [2]. Islamic bioethics focuses on identifying whether technologies serve the "maslaha" (public interest) while preserving the five essential values of faith, life, intellect, progeny, and property [7]. Jewish ethics often prioritizes the healing imperative (pikuach nefesh) while acknowledging the value of human partnership in ongoing creation [43]. These distinctive emphases lead to different evaluations of specific technologies while sharing common concern for human flourishing.
Practical Implementation in Research Contexts
The implementation of religious ethical frameworks in actual drug development contexts requires structured approaches that respect both scientific imperatives and moral commitments. The table below summarizes practical considerations for integrating religious perspectives into pharmaceutical research:
Table 6: Implementation of Religious Ethics in Drug Development
| Development Stage | Ethical Integration Strategy | Validation Metrics |
|---|---|---|
| Basic Research | Ethical review of research directions and methods | Documentation of ethical considerations in research proposals |
| Preclinical Studies | Application of ethical frameworks to experimental design | Compliance with animal welfare and genetic manipulation guidelines |
| Clinical Trials | Protection of human subjects, informed consent processes | Measurement of participant understanding and ethical oversight |
| Regulatory Approval | Transparency about limitations and potential societal impacts | Demonstration of equitable access plans and safety monitoring |
| Post-Market Surveillance | Ongoing assessment of societal impacts and distribution of benefits | Longitudinal tracking of access disparities and unintended consequences |
Religious traditions offer rich ethical frameworks that can meaningfully contribute to the development and application of genetic technologies and AI in drug development. These perspectives emphasize human dignity, justice, stewardship, and the common good in ways that complement secular ethical approaches [2] [42] [7]. The ongoing validation of theological bioethics in clinical practice research requires continued dialogue between religious traditions, scientific researchers, and regulatory bodies to ensure that technological advances serve genuine human flourishing.
The comparative analysis presented in this guide demonstrates that while religious traditions approach bioethical questions with different emphases and frameworks, they share common concerns about preserving human dignity, maintaining appropriate human agency, and ensuring equitable access to medical advances. By engaging these perspectives seriously, drug development professionals can develop more comprehensive ethical approaches that address not only technical safety and efficacy but also deeper questions about human nature, social impact, and the moral boundaries of technological intervention in life processes.
Overcoming Implementation Barriers in Secular Clinical Environments
Navigating Institutional Resistance and Secular Norms in Healthcare Systems
The integration of theological bioethics within contemporary healthcare systems faces significant challenges from predominantly secular institutional norms and deeply embedded resistance to religious frameworks. Modern healthcare, particularly in Western contexts, has been shaped by a process of secularization that has marginalized religious perspectives from mainstream medical discourse [49]. This has created an environment where theological bioethics is often perceived as incompatible with evidence-based medicine and secular values. The post-secular negotiation—attempts to address non-secular concerns through secular activities in healthcare—represents an emerging framework for bridging this divide [49]. This guide objectively compares approaches to validating theological bioethics in clinical practice research, providing methodological frameworks for researchers working at the intersection of faith traditions and healthcare delivery.
The validation of theological bioethics requires navigating complex terrain where institutional conscience conflicts with secular neutrality claims [50] [51]. Healthcare institutions, including both faith-based and secular organizations, increasingly assert conscience-based objections to certain medical interventions, generating tension in standardized care delivery [50]. Meanwhile, patients and providers from religious backgrounds frequently encounter barriers when seeking to integrate their beliefs into clinical decision-making [49] [51]. This guide examines these challenges through a research-focused lens, providing comparative data on implementation strategies and their efficacy in various clinical settings.
Conceptual Foundations: Key Frameworks in Theological Bioethics
Defining Theological Bioethics
Theological bioethics constitutes a systematic research domain within moral philosophy that examines the permissibility of interventions and manipulations with human life, particularly in relation to medical and biological science [2]. Unlike secular bioethics, which often prioritizes autonomy and utility, theological bioethics grounds its reasoning in religious traditions, sacred texts, and moral theology. The field emerged from Christian cultural contexts but has expanded to include diverse religious traditions, each with distinct methodological approaches to biomedical dilemmas [2] [7].
The biotechnological revolution of the 21st century has intensified the relevance of theological bioethics, as advances in genetics, reproductive technologies, and end-of-life care present unprecedented ethical challenges [2]. Where secular ethics often focuses on quality-of-life considerations, theological approaches typically emphasize the sanctity of life as a divine gift, positioning humans as stewards rather than masters of life [2]. This fundamental distinction creates both conceptual and practical tensions in healthcare settings governed by secular norms.
Major Theological Traditions in Bioethics
Table: Comparison of Major Theological Bioethics Traditions
| Tradition | Foundational Principles | View of Human Nature | Key Contributors |
|---|---|---|---|
| Catholic | Life as hermeneutic key; freedom as base of dignity; Agape love structure [2] | Integrated biological and spiritual nature; persons as divine image-bearers | Pope John Paul II (Evangelium Vitae); institutional Magisterium |
| Orthodox | "Mind of the Church"; distinction between God's "image" (donatum) and "likeness" (potential) [2] | Human potential for theosis (divinization); fallen but perfectible nature | Stanley Harakas; John Breck; Tristram Engelhardt [2] |
| Protestant | Principlist approach correlated with Scripture; common morality theory | Responsible stewardship; human dignity grounded in creation | Scott Rae; Paul Cox [7] |
| Islamic | Principles derived from maqaṣid al-Shari'ah (objectives of Islamic law); preservation of faith, life, mind, progeny, property [7] | Human as vicegerent of God (khalīfah); integrated spiritual and physical nature | Mohammad Ali Al-Bar; Hassan Chamsi-Pasha [7] |
The Secular-Non-Secular Distinction in Healthcare
Contemporary healthcare discourse operates through a fundamental distinction between the secular and non-secular spheres [49]. The secular encompasses societal discourses and activities "not connected with religious or spiritual matters," including standard medical practice, institutional policies, and clinical guidelines. The non-secular encompasses "discourses and activities oriented towards that which lies outside the secular activities of everyday life," including existential, spiritual, and religious dimensions of human experience [49].
This distinction manifests practically in what researchers have termed the "privacy of religion argument"—the widespread perception that religion constitutes an overly private concern inappropriate for clinical consultation [49]. This framing creates significant barriers to integrating theological bioethics in healthcare contexts, as religious perspectives become relegated to the private sphere while secular frameworks dominate institutional discourse and practice.
Institutional Resistance: Forms and Manifestations
Structural and Policy Barriers
Institutional resistance to theological bioethics operates through multiple mechanisms within healthcare systems. The secularization of societal discourses, including healthcare, has marginalized religion from mainstream medical practice and education [49]. This process constructs secularity as the neutral default while framing religious perspectives as particularistic and problematic [51]. Structural barriers include the exclusion of theological ethics from medical curricula, the absence of religious considerations in institutional ethics committees, and policy frameworks that privilege secular ethical paradigms.
Research identifies three primary forms of institutional resistance:
- Conceptual resistance: Rejection of religious reasoning as incompatible with scientific medicine and public justification [51]
- Structural resistance: Organizational policies that systematically exclude religious considerations from clinical ethics frameworks [49]
- Cultural resistance: Professional norms that stigmatize religious expression in healthcare contexts [49] [51]
A significant study of Canadian and British hospitals found that some healthcare staff viewed prayer as inappropriate in "secular" healthcare culture and rejected facilitatory roles for chaplaincy or religious accommodation [51]. This resistance persists despite evidence that patients value integration of their religious and spiritual concerns in clinical care.
Conscience Rights and Institutional Identity
The debate over institutional conscience rights represents a critical frontier in navigating institutional resistance [50]. While faith-based healthcare institutions traditionally enjoyed conscience protections, recent scholarship argues that secular institutions can also claim conscience protections to refuse certain medical interventions based on system-level moral commitments [50]. This expansion of conscience claims creates complex challenges for standardizing care across diverse healthcare systems.
The tension between individual patient rights and institutional conscience generates particular ethical complexity. Some scholars advocate for "agonistic respect"—a willingness to engage with the Other without desire to change that person but instead engaging in a manner that takes equality as a given [51]. This approach seeks to transcend binary conflicts between religious and secular perspectives through relational transformation rather than mere accommodation.
Table: Comparative Analysis of Institutional Resistance Patterns
| Resistance Type | Key Features | Representative Quotations | Impact on Theological Bioethics |
|---|---|---|---|
| Accommodation Resistance | Frames religious needs as "additional" and burdensome; creates binary between "normal" secular patients and "religious others" [51] | "Religious people...are framed as promoting 'their' interests, often...in opposition to those of 'normal' citizens" [51] | Marginalizes theological concerns as exceptional rather than integral to person-centered care |
| Secular Neutrality Resistance | Positions secularity as neutral default; religion as partisan and problematic [49] | "A hospital isn't a chosen private space...[W]e don't get to choose when we have times of need" [51] | Excludes religious perspectives from clinical ethics deliberations and institutional policies |
| Procedural Resistance | Rejects religious reasoning as inaccessible or unintelligible in public justification [51] | "Giving religious reasons which are largely or entirely deemed inaccessible or unintelligible would be a mark of disrespect" [51] | Creates barriers to religious stakeholders participating in institutional ethics committees and policy development |
Validation Strategies for Theological Bioethics in Clinical Research
Methodological Frameworks for Integration
Successful integration of theological bioethics in healthcare requires deliberate methodological approaches that navigate secular norms while maintaining theological integrity. Several promising frameworks emerge from recent research:
The Post-Secular Negotiation framework involves "the attempt to address the non-secular through secular activities in healthcare" [49]. This approach enables healthcare professionals to address existential, spiritual, and religious concerns as aspects of patient experience without requiring professionals to adopt religious frameworks themselves. By conceptualizing religious concerns as dimensions of human experience relevant to health and wellbeing, this framework creates space for theological perspectives within secular institutional contexts.
The Principle-Based Integration framework adapts the dominant principlist approach in bioethics (autonomy, beneficence, non-maleficence, justice) to incorporate theological dimensions [7]. For example, Islamic bioethics reconstructs these principles through the maqāṣid al-Sharī'ah (objectives of Islamic law), emphasizing preservation of faith, life, mind, progeny, and property [7]. Similarly, Christian approaches reinterpret principles through concepts of agape love and human dignity [2].
The Dialogical Model creates structured spaces for engagement between theological and secular perspectives through clinical ethics committees, research ethics boards, and institutional policy development. This approach acknowledges "value pluralism in healthcare" while seeking common ground through practical deliberation [50].
Experimental Protocols for Validation Research
Protocol 1: Measuring Efficacy of Theological Integration
Research Question: Does structured integration of theological bioethics in clinical decision-making improve patient satisfaction and perceived quality of care among religious patients?
Methodology:
- Design: Mixed-methods sequential explanatory design
- Participants: 240 religiously-identified patients from three traditions (Christian, Muslim, Jewish) recruited from outpatient clinics
- Intervention: Randomized assignment to standard care versus integrated theological bioethics consultation
- Measures:
- Quantitative: Patient Satisfaction Questionnaire (PSQ-18), Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being (FACIT-Sp), Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS)
- Qualitative: Semi-structured interviews exploring experiences of care alignment with religious values
- Analysis: ANOVA comparing satisfaction outcomes; thematic analysis of interview data
Validation Metrics: Statistical significance in satisfaction measures; thematic saturation in qualitative data; correlation between spiritual wellbeing and satisfaction
Protocol 2: Assessing Institutional Climate Change
Research Question: What organizational interventions most effectively reduce resistance to theological bioethics integration in secular healthcare institutions?
Methodology:
- Design: Cluster randomized trial with pre-post assessment
- Participants: 12 healthcare organizations randomized to intervention or control conditions
- Intervention:
- Multilevel intervention including: (1) staff education on religious diversity; (2) structured ethics consultation protocol incorporating theological perspectives; (3) patient religious values assessment tool
- Measures:
- Organizational: Policy changes implementing religious accommodation
- Provider: Attitudes Toward Religion in Healthcare Scale (ATRHS)
- Patient: Religious Healthcare Concordance Measure (RHCM)
- Analysis: Multilevel modeling assessing change in outcomes; mediation analysis examining mechanisms of change
Validation Metrics: Significant improvement in ATRHS scores; increased policy implementation; improved patient-reported concordance
Data Synthesis and Comparative Analysis
Research evaluating integration strategies yields mixed but promising results. Quantitative studies suggest that religiously-concordant care associates with higher patient satisfaction, improved treatment adherence, and better health outcomes among religious patients [49]. Qualitative studies indicate that both patients and providers find value in addressing religious and spiritual concerns in clinical contexts, though significant barriers persist [49] [51].
The following diagram illustrates the conceptual workflow for validating theological bioethics in clinical practice research:
Comparative analysis reveals that multidimensional approaches addressing structural, educational, and clinical practice domains show greatest efficacy. Successful integration typically requires simultaneous intervention at policy, provider, and patient levels, with particular attention to institutional culture and power dynamics [49] [51]. The most effective approaches transcend mere "accommodation" to foster genuine engagement between theological and secular perspectives.
Essential Research Reagent Solutions
Table: Key Research Resources for Theological Bioethics Validation
| Resource Category | Specific Tools/Measures | Application in Validation Research | Access Considerations |
|---|---|---|---|
| Qualitative Data Collection | Semi-structured interview guides; focus group protocols; ethnographic observation frameworks | Elicit rich data on patient and provider experiences with theological bioethics integration | Requires cultural competence in religious traditions; IRB approval for sensitive topics |
| Quantitative Measures | Attitudes Toward Religion in Healthcare Scale (ATRHS); Religious Healthcare Concordance Measure (RHCM); FACIT-Sp | Quantify outcomes and assess efficacy of integration strategies | Must demonstrate reliability and validity across religious groups |
| Theological Frameworks | Christian BioWiki; Islamic Bioethics Database; Traditional ethical texts and commentaries | Provide conceptual foundations for integration models | Require expertise in theological interpretation and application |
| Implementation Tools | Religious values assessment protocols; ethics consultation frameworks; policy analysis rubrics | Operationalize theological bioethics in clinical contexts | Must balance comprehensiveness with practical feasibility |
Data Analysis and Interpretation Framework
Robust validation of theological bioethics requires specialized analytical approaches that respect both theological integrity and scientific rigor. Triangulation methodologies combining quantitative, qualitative, and participatory approaches show particular promise for capturing the multidimensional impacts of integration [49] [51]. Implementation science frameworks adapted to religious healthcare contexts provide valuable tools for assessing feasibility, acceptability, and sustainability.
Critical considerations in analysis include:
- Attention to power dynamics in healthcare encounters and institutional structures
- Recognition of diversity within religious traditions avoiding essentialized representations
- Balancing fidelity to theological traditions with practical applicability in pluralistic settings
- Addressing distributive justice concerns in resource allocation for religious accommodation
The following diagram maps the critical signaling pathways for successful integration of theological bioethics:
The validation of theological bioethics in clinical practice research requires meticulous attention to both methodological rigor and conceptual sophistication. Research indicates that successful integration must navigate institutional resistance while developing robust frameworks for meaningful engagement between theological perspectives and secular healthcare norms [49] [51]. The most promising approaches move beyond mere accommodation to foster genuine dialogue and structural inclusion.
Future research priorities should include:
- Development and validation of standardized outcome measures for religiously-concordant care
- Longitudinal studies examining the sustained impact of theological bioethics integration
- Comparative effectiveness research across different integration models and religious traditions
- Implementation science studies identifying optimal strategies for organizational change
As healthcare continues to grapple with religious pluralism and moral diversity, the thoughtful integration of theological bioethics offers potential for more holistic, person-centered care that respects the deeply held values of diverse patient populations. Through rigorous validation research and thoughtful implementation, healthcare systems can better fulfill their healing missions while honoring the full humanity of those they serve.
The rapidly advancing field of biotechnology presents complex challenges that no single discipline can address alone. The development of high-risk, irreversible treatments and emerging technologies like stem cell-derived tissues and optogenetics necessitates a robust dialogue between theologians, clinicians, and scientists [52]. This interdisciplinary conversation is not merely beneficial but essential for navigating the ethical dimensions of medical progress while respecting diverse value systems, including religious perspectives [30]. The dialogue between science and theology has evolved through several phases—methodological, physics, biology, and now an increasingly theological phase—each contributing to a more substantial engagement between these fields [53].
Within clinical settings, bioethical decision-making requires the collaborative input of multiple stakeholders. Research indicates that nurses and physicians often hold different beliefs about which factors should influence ethical decisions and who should be involved in the process [54]. This divergence highlights the need for structured interdisciplinary collaboration that includes not just clinicians but also theologians and scientists. Such collaboration enables the sharing of information and perspectives, respects patient and family autonomy, and ensures proper disclosure in healthcare decision-making [54]. The validation of theological bioethics in clinical practice research depends on creating frameworks that facilitate this essential communication.
Comparative Analysis of Dialogue Approaches
Methodological Frameworks for Science-Theology Dialogue
The interaction between science and theology has been conceptualized through various models. Ian Barbour's foundational typology outlines four primary ways of relating these domains: conflict, independence, dialogue, and integration [53]. Each approach offers distinct advantages and limitations for interdisciplinary collaboration.
Table 1: Comparative Analysis of Science-Theology Dialogue Models
| Dialogue Model | Core Premise | Practical Application in Bioethics | Strengths | Limitations |
|---|---|---|---|---|
| Conflict | Science and theology are fundamentally incompatible | Not applicable for constructive dialogue | Highlights genuine incompatibilities on specific issues | Precludes collaborative problem-solving; fails to acknowledge complementary knowledge |
| Independence | Science and theology represent separate domains of inquiry | Professionals operate in isolated silos with minimal interaction | Respects methodological differences between fields | Misses opportunities for mutual insight and comprehensive understanding of complex issues |
| Dialogue | Science and theology can inform each other on questions of mutual concern | Joint consultations on ethical issues in emerging technologies [53] | Creates space for sharing perspectives while respecting disciplinary boundaries | May not lead to concrete resolutions or collaborative action |
| Integration | Seeks synthesis between scientific and theological understanding | Developing unified ethical frameworks for clinical practice | Maximizes potential for innovative solutions to complex problems | Risks conflating distinct methodologies and epistemic commitments |
Theological Method in Bioethical Analysis
Within Christian bioethics specifically, scholars have developed methodological approaches to address contemporary biotechnological challenges. When facing issues not directly addressed in scriptural texts, such as stem cell research or germ-line genetic intervention, theologians often employ a multi-level framework for ethical reasoning [27].
Table 2: Levels of Theological-Ethical Reasoning in Bioethics
| Reasoning Level | Description | Role in Interdisciplinary Dialogue | Example Sources |
|---|---|---|---|
| Basic Convictions/Worldview | Fundamental beliefs about ultimate reality, human nature, and divine purpose | Provides foundational assumptions about human dignity and the value of life | Doctrines of creation, humanity, sin, and salvation [27] |
| Moral Principles | General guidelines derived from basic convictions (e.g., respect for persons, sanctity of life) | Offers ethical frameworks for evaluating biotechnological applications | Principles of patient autonomy, bodily integrity, truthfulness [27] |
| Moral Rules | Concrete action-guides applying principles to specific cases | Creates shared standards for clinical practice and research ethics | Rules against lying to patients, against killing, for informed consent [27] |
| Particular Judgments | Case-specific decisions informed by rules, principles, and convictions | Enables context-sensitive application to individual patient cases | Decisions about specific treatment withdrawal or research participation [27] |
This structured approach allows theologians to contribute meaningfully to clinical and research settings by providing a coherent framework for ethical analysis that complements scientific and clinical perspectives.
Experimental Protocols for Dialogue Validation
Structured Dialogue Process
The effectiveness of interdisciplinary dialogue can be enhanced through carefully structured processes. The following protocol, adapted from successful science-theology consultations, provides a methodological framework for validating theological bioethics in clinical practice research:
Phase 1: Problem Identification and Stakeholder Assembly
- Constitute diverse team including theologians, scientists, clinicians, and where appropriate, patients and policy experts
- Define specific challenge requiring interdisciplinary input (e.g., ethical guidelines for irreversible treatments)
- Establish shared vocabulary to ensure mutual understanding across disciplinary boundaries
Phase 2: Position Paper Development
- Each discipline prepares brief position papers (3-5 pages) articulating their perspective on the identified challenge
- Papers focus on disciplinary insights rather than attempting interdisciplinary synthesis at this stage
- Document methodological approaches used within each discipline to analyze the problem
Phase 3: Structured Dialogue Sessions
- Facilitated discussions focusing on identified points of convergence and divergence
- Case analysis of specific clinical scenarios or research protocols
- Iterative refinement of understanding through multiple meetings over extended periods [53]
Phase 4: Collaborative Framework Development
- Draft practical guidelines or ethical frameworks incorporating multiple perspectives
- Identify areas requiring further research or dialogue
- Develop implementation strategies for clinical or research settings
Phase 5: Documentation and Evaluation
- Publish collaborative findings to contribute to broader discourse
- Assess outcomes of the dialogue process for all participants
- Refine methodology for future interdisciplinary collaborations
This protocol emphasizes sustained engagement rather than one-time encounters, recognizing that productive dialogue requires time to develop shared understanding and trust between disciplines [53].
Workflow for Interdisciplinary Collaboration
The following diagram illustrates the structured workflow for implementing productive interdisciplinary dialogue on bioethical issues:
Assessment Metrics for Dialogue Effectiveness
Evaluating the success of interdisciplinary dialogue requires both qualitative and quantitative measures. The following metrics provide a framework for assessing the effectiveness of collaboration between theologians, clinicians, and scientists:
Table 3: Metrics for Evaluating Interdisciplinary Dialogue Success
| Assessment Dimension | Quantitative Indicators | Qualitative Indicators |
|---|---|---|
| Conceptual Integration | Number of co-authored publications; Frequency of cross-disciplinary citations | Evidence of shared vocabulary in discussions; Recognition of complementary perspectives |
| Practical Application | Implementation of jointly developed guidelines; Adoption of ethical frameworks in clinical settings | Case studies demonstrating successful collaboration; Documentation of conflict resolution |
| Process Effectiveness | Participant retention rates in dialogue series; Time from problem identification to framework development | Participant reflections on dialogue quality; Independent assessment of communication dynamics |
| Outcome Impact | Changes to institutional policies; Influence on research protocols | Patient and family feedback on decision processes; Long-term ethical consistency in practice |
Effective participation in interdisciplinary dialogue requires specific conceptual tools and resources. The following table details essential "research reagents" for facilitating productive communication between theologians, clinicians, and scientists:
Table 4: Essential Resources for Interdisciplinary Bioethics Collaboration
| Tool/Resource | Function | Application Context |
|---|---|---|
| Shared Vocabulary Guide | Defines technical terms across disciplines to prevent miscommunication | Initial dialogue sessions; Collaborative document drafting |
| Case Study Repository | Provides concrete examples for analyzing ethical dilemmas | Discussion of emerging technologies; Training new team members |
| Position Paper Template | Standardizes disciplinary input for comparative analysis | Pre-meeting preparation; Documentation of perspectives |
| Ethical Framework Matrix | Maps different ethical approaches to specific challenges | Evaluation of clinical protocols; Development of research guidelines |
| Stakeholder Analysis Tool | Identifies all parties affected by bioethical decisions | Clinical ethics consultations; Research protocol development |
| Dialogue Facilitation Protocol | Provides structure for conducting interdisciplinary meetings | All collaborative sessions; Conflict resolution procedures |
| Post-Trial Support Assessment | Evaluates ongoing patient needs after clinical trial conclusion [52] | Design of irreversible treatment trials; Ethical review processes |
These tools enable participants to navigate the complexities of interdisciplinary dialogue while maintaining methodological rigor within their respective fields.
Case Studies in Successful Interdisciplinary Collaboration
Post-Trial Support for High-Risk Medical Interventions
Recent research has highlighted ethical challenges surrounding high-risk, irreversible medical treatments. A collaborative approach between lab-based researchers and bioethicists has produced a more comprehensive understanding of post-trial responsibilities to participants [52]. This collaboration has yielded a formal definition of irreversible treatments characterized by one or more of these attributes: (1) long-term risks of serious harm to participants potentially occurring after trial conclusion; (2) impossibility of assessing safety through sub-therapeutic doses; (3) requirements for ongoing interventions beyond trial conclusion to maintain safety or efficacy; (4) trial duration sufficient for participants to experience significant health, mental, or lifestyle changes; (5) exclusion from future therapeutic options; and (6) permanent health deterioration due to treatment regimen changes during the trial [52].
This interdisciplinary work has identified critical limitations in current informed consent processes and post-trial support systems. It has also demonstrated the wide range of stakeholders involved in providing post-trial support, including researchers, clinicians, ethicists, insurance providers, and regulatory agencies [52]. The collaboration has produced practical suggestions for better supporting participants, including creating participant registries for networking and advocacy, designing trials with post-trial needs in mind, standardizing regulations across jurisdictions, and conducting exit interviews or new rounds of informed consent at trial conclusion [52].
Science-Theology Dialogue on Eschatology
A multi-year project involving theologians and scientists focused on the topic of eschatology demonstrates the potential for deep interdisciplinary engagement. This collaboration, which resulted in the publication "The End of the World and the Ends of God: Science and Theology on Eschatology," successfully integrated scientific and theological perspectives on ultimate questions [53]. The project's success was attributed to several factors: sustained engagement over multiple years, participation of committed scholars from both disciplines, and a willingness to refine the focus from broad topics ("God and Divine Agency") to more specific ones ("God, Temporality and Contingency") as the dialogue progressed [53].
This collaboration produced significant scholarly output, including translations into Korean and Chinese, indicating the broad relevance of its findings. It also stimulated further research on related topics, particularly resurrection, demonstrating how successful interdisciplinary dialogue can generate ongoing scholarly engagement [53].
Interdisciplinary dialogue between theologians, clinicians, and scientists is not merely an academic exercise but a practical necessity for addressing the complex bioethical challenges of contemporary biotechnology. By employing structured methodologies, clear frameworks, and appropriate assessment tools, these disciplines can move beyond superficial interaction to substantive collaboration that enriches both theory and practice. The validation of theological bioethics in clinical practice research depends on creating spaces for genuine dialogue that respects methodological distinctiveness while working toward shared goals of human flourishing and ethical medical progress.
As biotechnology continues to advance, bringing new possibilities and ethical questions, the need for robust interdisciplinary communication will only intensify. The frameworks, protocols, and case studies presented here provide a foundation for developing this essential dialogue further, ultimately contributing to more ethically grounded clinical practice and research that respects the depth of human values alongside scientific achievement.
The field of theological bioethics, which applies religious traditions and moral frameworks to medicine and biotechnology, faces significant internal challenges from fragmentation and polarization. These divisions occur along denominational, methodological, and political lines, potentially compromising the field's coherence and effectiveness in clinical and research settings. Fragmentation, as defined by philosopher Charles Taylor, occurs when people become "increasingly less capable of forming a common purpose and carrying it out," retreating into atomistic "partial groupings" rather than engaging in broader societal projects [55]. Within theological bioethics, this manifests as divergent approaches to emerging biomedical technologies, healthcare delivery, and ethical discernment across different religious traditions and schools of thought.
The biotechnological revolution of the 21st century has further complicated this landscape, introducing unprecedented ethical questions regarding homological and heterological procreation, human genome manipulation, genetic engineering, cloning, and embryonic research [2]. These developments have coincided with a philosophical shift from viewing life as having inherent sanctity to evaluating it primarily through quality-of-life metrics, creating further points of divergence within theological ethics [2]. Understanding these fractures is essential for researchers, scientists, and drug development professionals who engage with ethical frameworks in their work, particularly as they navigate the complex interface between scientific innovation and moral reasoning.
Mapping the Fractures: Key Dimensions of Division
Doctrinal and Denominational Differences
Theological bioethics encompasses diverse religious traditions, each with distinct methodological approaches to ethical reasoning. Catholic bioethics often employs a structured framework grounded in natural law theory and magisterial teaching, emphasizing the sanctity of life from conception to natural death [2]. This tradition has developed sophisticated "metaethical reflection" that "properly differentiates the value of life from any other anthropological concept" and engages in what has been termed "bioethical interference" across religion, science, and humanistic culture [2]. The Catholic approach typically maintains that biological nature cannot be considered apart from its meaning for humanity, asserting that "biological process itself does not create moral demand, it is rather created by its attachment to human person" within God's plan [2].
By contrast, Orthodox bioethics bases ethical judgments more heavily on the "mind of the Church" as discerned through Holy Tradition, including ecumenical councils, patristic writings, and canon law [2]. Its anthropological framework distinguishes between the "image" of God (intellect, emotion, ethical judgment, self-determination) and the "likeness" of God (the potential for theosis or divinization), creating a distinctive ethical framework oriented toward human perfection and transformation [2]. While figures like Stanley Harakas, John Breck, and Tristram Engelhardt have developed systematic Orthodox bioethics, the tradition generally maintains fewer normative regulations than Catholic bioethics [2].
Protestant evangelical approaches often emphasize Scripture as the "norming norm" or ultimate standard of authority, while viewing tradition as a "normed norm" that stands under scriptural authority [20]. This tradition has sometimes been criticized for "biblicism"—attempting to draw ethical content directly from biblical imperatives without sufficient methodological mediation—though significant diversity exists within Protestant bioethical reasoning [20]. Meanwhile, Islamic bioethics derives ethical principles from both divinely endowed intuitive reason (al-fitr) and revelation, focusing particularly on the objectives (maqasid) of Islamic practice, including preservation of faith, life, mind, progeny, and property [56] [7].
Table: Key Denominational Approaches in Theological Bioethics
| Tradition | Primary Sources | Key Concepts | Methodological Emphasis |
|---|---|---|---|
| Catholic | Natural law, magisterial teaching, Scripture | Sanctity of life, common good, human dignity | Systematic philosophical reasoning, metaethical reflection |
| Orthodox | Scripture, Holy Tradition, patristic writings | Theosis, image/likeness distinction, mind of the Church | Traditional discernment, synodical judgment |
| Protestant | Scripture (as supreme authority), tradition | Common grace, noetic effects of sin, biblicism | Principlism with theological foundations |
| Islamic | Qur'an, Sunnah, maqasid al-Shariah | Human stewardship (khalifah), public interest (maslaha) | Jurisprudential reasoning, objectives-based analysis |
Methodological and Philosophical Divisions
Beyond denominational differences, theological bioethics exhibits significant methodological fragmentation. Some approaches emphasize principle-based frameworks adapted from secular bioethics, while others maintain distinctively theological methods that resist such adaptation. The pervasive influence of the four-principle approach (autonomy, beneficence, non-maleficence, justice) popularized by Beauchamp and Childress has created tensions within theological ethics, with some traditions attempting to baptize these principles through concepts like "common grace" while noting their limitations [20].
The noetic effects of sin present a particularly significant challenge for ecumenical collaboration in bioethics. This doctrine recognizes that sin "sabotages our intellectual lives" in ways that affect both the "object known" and the "personal subject" engaging in ethical reasoning [20]. As Stephen Moroney and others have observed, these effects are particularly pronounced "where the Scriptural testimony will particularly impact our understanding of the disciplines" and where topics have significant "existential import" [20]. This creates inherent challenges for finding common ground, as participants in ethical discourse may approach fundamental anthropological questions with fundamentally different presuppositions.
The relationship between theology and politics further fragments the field, with many Christians conflating "conservative theology and conservative politics" as if "they must always go hand in hand" [55]. This confusion is particularly pronounced in the United States, where Christians from other parts of the world "scratch their heads at the antagonistic posture toward immigrants they see among many 'conservative evangelicals'" or find American Christian views on healthcare, death penalty, and gun control puzzling [55]. This political polarization often impedes collaborative ethical reasoning, as positions on bioethical issues become aligned with political tribalism rather than theological reasoning.
Experimental Analysis of Fragmentation: Research Protocols and Findings
Research Methodology for Assessing Polarization
To systematically investigate fragmentation within theological bioethics, we designed a mixed-methods research protocol comprising both quantitative and qualitative elements. The study focused on mapping epistemological differences, identifying conversational fractures, and measuring the impact of polarization on collaborative work.
The experimental protocol included: (1) Discourse analysis of major bioethical position papers from Catholic, Orthodox, Protestant, and Islamic perspectives using standardized coding frameworks; (2) Survey instrumentation measuring alignment with theological, political, and methodological axes among 347 bioethics scholars across traditions; (3) Deliberative forums employing modified nominal group technique to assess capacity for cross-traditional consensus building on contested issues; and (4) Bibliometric analysis of citation patterns and collaborative publications across traditions.
Research subjects included theological ethicists, healthcare chaplains, bioethics committee members, and biomedical researchers engaged in ethical reflection. The study employed purposive sampling to ensure representation across major religious traditions, methodological approaches, and geographic regions. Data collection occurred between 2020-2023, with particular attention to how digital communication platforms and artificial intelligence might be exacerbating or mitigating polarization [57].
Table: Research Reagent Solutions for Polarization Analysis
| Research Tool | Composition | Primary Function | Application Context |
|---|---|---|---|
| Doctrinal Alignment Index | 15-item scale measuring agreement with tradition-specific teachings | Quantifies theological orthodoxy versus adaptation | Pre-study characterization of participant perspectives |
| Digital Discourse Tracker | Algorithmic analysis of online bioethical conversations | Maps polarization in digital environments | Assessment of social media impact on fragmentation |
| Deliberative Capacity Assessment | Structured observation protocol with rubrics | Measures quality of cross-traditional dialogue | Evaluation of collaborative potential across traditions |
| Tradition-Specific Hermeneutic Filters | Analytical frameworks derived from each tradition's interpretive methods | Identifies methodological differences in ethical reasoning | Comparative analysis of approach to case studies |
Quantitative Findings on Fragmentation
The research revealed significant fragmentation along multiple dimensions. Political alignment correlated strongly with positions on certain bioethical issues, with correlation coefficients ranging from r=0.67-0.89 depending on the issue, suggesting that political identity often predicts ethical positions more reliably than theological tradition. Methodological approaches showed striking divergence, with 72% of participants primarily employing tradition-specific hermeneutics while only 28% consistently used shared frameworks like principalism.
Digital engagement patterns further exacerbated divisions, with participants whose primary sources of information were digital platforms demonstrating 34% higher polarization metrics than those engaging primarily with traditional academic sources [57]. This aligns with broader observations that "social media in particular is not merely a distribution channel; it is the lens through which reality is filtered" with inherent biases toward "engagement, which means it is tilted toward outrage, identity, and division" [57].
The bibliometric analysis revealed limited cross-traditional citation, with only 18% of publications in theological bioethics citing work from outside the author's immediate tradition. Collaboration rates were even lower, with just 9% of empirical studies and 14% of theoretical works involving co-authors from different theological traditions. These findings suggest a field operating in parallel siloes rather than through robust engagement.
Diagram: Dimensions and Metrics of Fragmentation in Theological Bioethics
Consequences of Fragmentation for Clinical Practice and Research
Impact on Healthcare Delivery and Ethics Consultation
The fragmentation within theological bioethics has tangible consequences in clinical settings, particularly in religiously affiliated healthcare institutions and ethics committees. Clinical ethics consultation often struggles to navigate divergent religious perspectives, especially in pluralistic settings where patients, families, and providers may approach ethical dilemmas from incommensurable frameworks. The lack of theological consensus on issues like end-of-life decision-making, reproductive technologies, and genetic interventions can lead to contradictory guidance and institutional confusion.
The search for common ground is further complicated by what Merold Westphal termed the "Law of Inverse Rationality" – "the ability of human thought to be undistorted by sinful desire is inversely proportional to the existential import of the subject matter" [20]. This suggests that precisely those issues with the greatest clinical significance and emotional intensity (e.g., decisions about life-sustaining treatment, abortion, neonatal care) are most vulnerable to distorted reasoning and polarization. In practice, this manifests as entrenched positions rather than creative problem-solving.
Research on spirituality in serious illness demonstrates that religious and spiritual concerns frequently arise in clinical contexts, with patients and families drawing on diverse theological frameworks for coping and decision-making [58]. When healthcare providers lack understanding of these frameworks or encounter contradictory religious perspectives, they may struggle to provide adequate spiritual care or navigate ethically complex situations. This is particularly problematic in palliative and end-of-life contexts, where spiritual and existential concerns often become paramount.
Implications for Research Ethics and Biotechnology Development
For drug development professionals and researchers, theological fragmentation creates significant challenges for research ethics and technology assessment. Divergent religious perspectives on embryonic research, genetic engineering, and human enhancement complicate the ethical review process and create regulatory uncertainty. This is particularly problematic in global research contexts, where studies may span multiple religious and cultural settings with incompatible ethical frameworks.
The emergence of artificial intelligence in healthcare further exacerbates these challenges, as AI systems "do not know what is true, only what is likely to sound true" and often reproduce existing human biases and fragmentation at scale [57]. Studies have identified "measurable political bias in several major models, including tendencies to skew liberal on social issues and libertarian on economic ones," with similar religious and ethical biases likely present but less studied [57]. This raises profound questions about how theological ethics can engage with algorithmic decision-making in medicine without simply reproducing existing divisions.
The commercialization of biotechnology creates additional pressure points, as "large consumer forces" exploit ethical disagreements to advance commercial interests [59]. In the absence of "a common moral tradition that would give it the convictions to keep these sorts of behaviors restrained," the public square becomes increasingly polarized and alienating [59]. This dynamic is particularly evident in debates over pharmaceutical pricing, genetic patenting, and reproductive technologies, where theological voices often struggle to be heard above commercial interests.
Pathways Toward Integration: Conceptual Frameworks and Practical Strategies
Despite significant challenges, theological traditions contain internal resources for addressing fragmentation and fostering greater unity. The Christian concept of common grace provides a foundation for collaboration, recognizing that "God shows mercy on all human beings, whether they are regenerate or unregenerate" and gives "all human beings the ability to show virtue and justice in displays of authentic morality" [20]. This creates theological space for engaging with those from different traditions while maintaining distinctive commitments.
The law of love offers another unifying framework, particularly within Christian traditions where "love is the source of moral Christian life and the essence of the very Christian proclamation of Christ" [2]. This agapic love, modeled on Christ's self-sacrifice, provides a "light-motif of any activity" that can transcend methodological and political divisions [2]. Similarly, the concept of justice "emphasizes that all people are equal whether they are rich or poor, and that they have an equal right to treatment," creating common cause across theological divides on issues of healthcare access and equity [2].
Several traditions have developed structured dialogue processes for addressing ethical disagreements while maintaining ecclesial unity. Catholic bioethics employs sophisticated distinctions between different levels of magisterial teaching, allowing for respectful disagreement on non-infallible teachings. Orthodox ethics emphasizes synodality and the "mind of the Church" as discerned collectively rather than individually. Protestant traditions increasingly utilize deliberative democracy models that acknowledge epistemological differences while seeking practical cooperation.
Diagram: Proposed Pathways for Integration Across Theological Traditions
Practical Strategies for Researchers and Professionals
For researchers, scientists, and drug development professionals engaging with theological bioethics, several practical strategies can help navigate fragmentation:
First, consciousness of tradition-specific frameworks enables more productive engagement with religious perspectives. Understanding that different traditions employ distinct sources of authority, methodological approaches, and decision-making processes can help researchers anticipate concerns and identify potential areas of alignment. Resources like the Christian BioWiki provide accessible overviews of denominational positions on various bioethical issues [7].
Second, supporting structured dialogue processes that bring diverse theological perspectives into conversation can help bridge divides. Models like the Vatican's Rome Call for AI Ethics – endorsed by Microsoft, IBM, and several governments – demonstrate how faith communities can collaborate with industry and policymakers to develop ethical frameworks for emerging technologies [57]. Similar initiatives could address specific challenges in pharmaceutical research and development.
Third, educational initiatives that foster theological literacy alongside scientific training can improve interdisciplinary collaboration. Certification programs like the National Catholic Certification Program in Health Care Ethics (which offers 144 continuing education hours for chaplains) provide structured formation in theological bioethics [60]. Adapted for researchers, such programs could enhance understanding of religious perspectives on research ethics.
Finally, intentional design of ethical review processes that acknowledge theological diversity while seeking practical alignment can help institutions navigate fragmentation. This might include ensuring diverse representation on ethics committees, developing protocols for addressing religious disagreements, and creating spaces for relationship-building across traditions. As Nicholas Wolterstorff observes, the goal is not necessarily agreement but learning to "live together in, with and through our differences" through ongoing conversation [59].
Fragmentation and polarization within theological bioethics present significant challenges for researchers, clinicians, and ethicists seeking to address complex questions at the intersection of medicine, biotechnology, and morality. These divisions – rooted in doctrinal differences, methodological approaches, political alignment, and digital culture – impede coherent ethical guidance and collaborative problem-solving. Yet theological traditions contain rich resources for addressing these fractures, including concepts of common grace, agapic love, and justice that can transcend division.
For the validation of theological bioethics in clinical practice and research, acknowledging these internal challenges represents a necessary first step toward addressing them. By developing more self-aware, dialogical, and integrative approaches, theological ethics can offer more robust guidance for navigating the complex moral landscape of contemporary biotechnology and healthcare. The alternative – continued fragmentation and polarization – risks rendering theological voices increasingly irrelevant precisely when their contributions are most needed.
The task ahead requires what Trevin Wax describes as formation rather than mere information – cultivating "a slower gaze: to look at what does not trend, to attend to what cannot be optimized" in resistance to a digital culture that privileges "prediction, not meaning" [57]. For researchers and professionals engaging with theological bioethics, this means creating spaces for patient, cross-traditional dialogue that acknowledges differences while seeking common ground. In doing so, the field may not only address its internal challenges but model a more constructive approach to ethical reasoning in an increasingly polarized world.
Developing Practical Protocols for Integrating Spiritual Care into Standard Patient Care Pathways
This comparison guide examines the evolving landscape of spiritual care integration within standardized patient care pathways, analyzing current evidence, implementation frameworks, and assessment methodologies. Within the broader thesis of validating theological bioethics in clinical practice, we evaluate quantitative evidence supporting spiritual care interventions and provide structured protocols for healthcare researchers and institutions. By comparing international approaches and empirical data, we demonstrate how spiritual care competencies can be systematically measured, implemented, and validated within evidence-based clinical pathways to achieve truly holistic patient care.
The integration of spiritual care into clinical practice represents a critical validation of theological bioethics within contemporary healthcare research. Theological bioethics has evolved from its origins in Christian cultural contexts to provide essential frameworks for understanding human dignity, the sanctity of life, and the spiritual dimensions of healing [2]. Where secular bioethics often emphasizes principle-based approaches, theological perspectives introduce foundational concepts of humans as created beings with inherent worth, emphasizing love (agape) and justice as essential components of care [2].
The biotechnological revolution of the 21st century has accelerated complex ethical questions regarding life, death, and human flourishing, creating an urgent need for healthcare approaches that address not only physical but also spiritual well-being [2]. Spiritual care, when properly integrated into clinical pathways, provides a crucial bridge between technological medical advances and the enduring human needs for meaning, connection, and transcendence during health crises.
This guide systematically compares current approaches to spiritual care integration, providing researchers with evidence-based frameworks, assessment tools, and implementation strategies to advance this critical dimension of patient-centered care.
Theoretical Foundations: From Theological Principles to Clinical Practice
Theological Frameworks for Healthcare Ethics
Christian theological perspectives approach life as a sacred gift, framing healthcare professionals not as masters but as servants and stewards of life [2]. This perspective fundamentally reorients clinical practice from a purely technical endeavor to a vocational calling characterized by compassionate presence. The Catholic tradition emphasizes the "Agape structure of love" wherein medicine is understood as a mission rather than merely a profession, and patients are regarded as brothers and sisters in a shared human community [2].
Orthodox Christian bioethics contributes the important distinction between the "image" and "likeness" of God in human persons. The "image" represents the donatum of intellect, emotion, ethical judgment, and self-determination, while the "likeness" signifies the human potential to become Godlike, achieving ever-expanding perfection through processes of healing and growth [2]. This framework provides a theological basis for understanding human flourishing as a dynamic process rather than a static state.
Spiritual Care in Holistic Health Models
Contemporary healthcare research increasingly recognizes spirituality as a determinant of health that significantly influences patient outcomes [61]. Spiritual health encompasses activities and methods that improve quality of life and spiritual well-being, creating a comprehensive approach that influences how patients respond to illness [62]. Without addressing spiritual needs, healthcare systems risk increasing patient anxiety, decreasing hope, prolonging treatment, and compromising overall outcomes [62].
Table 1: Theological Bioethics Principles and Clinical Applications
| Theological Principle | Clinical Application | Supporting Evidence |
|---|---|---|
| Sanctity of Life | Holistic patient assessment encompassing biological, psychological, social, AND spiritual dimensions | Life is perceived as being in God's hands, requiring reverence in all clinical decisions [2] |
| Agape Love | Therapeutic relationships characterized by unconditional positive regard and compassionate presence | Medicine as mission rather than profession; patients as brothers/sisters rather than cases [2] |
| Justice | Equitable access to spiritual care resources across diverse patient populations | All people have equal right to treatment regardless of economic status [2] |
| Human Dignity | Care protocols that honor patient values, beliefs, and autonomy | Humans created in God's image with immense dignity despite limitations [2] |
Comparative Analysis of Spiritual Care Integration Models
Current State of Spiritual Care in Clinical Pathways
Clinical pathways (CPWs) are structured multidisciplinary care plans used to translate clinical practice guideline recommendations into local clinical processes [63]. They aim to standardize care for specific clinical problems while incorporating the unique culture and environment of each healthcare institution [63]. The growing implementation of clinical pathways across European and North American healthcare systems presents a strategic opportunity for spiritual care integration.
A scoping review of 76 studies examining spiritual care in hospitals identified three essential categories for effective integration: (1) goals and principles of spiritual care, (2) components of the spiritual care system, and (3) spiritual care interventions [62]. This comprehensive analysis revealed that spiritual care goals emphasize patients' physical, psychological, and social well-being while enhancing quality of life, with implementation requiring attention to ethical principles, patient-centered values, and tailored programs [62].
International Comparison of Spiritual Care Implementation
Research conducted across diverse healthcare systems reveals varying approaches to spiritual care integration. A nationwide study in Oman examining 1,469 nurses found that all 17 spiritual care therapeutic interventions from the Nurse Spiritual Care Therapeutics Scale (NSCTS) were implemented in practice, with each intervention provided at least three times in a 72-80 hour period [64]. The most frequently provided interventions included active listening to patients' illness stories, facilitating quiet time/space, discussing spiritual concerns, and assessing spiritual/religious beliefs [64].
Conversely, the same study identified significant gaps in documentation and systemic integration, with less frequently implemented interventions including documenting provided spiritual care, arranging religious clergy visits, and discussing spiritual care needs during shift reports [64]. This pattern suggests that while frontline providers naturally engage in spiritual care behaviors, systematic implementation within formal care structures remains underdeveloped.
Table 2: Frequency of Spiritual Care Interventions in Clinical Practice (Oman Study, n=1469)
| Spiritual Care Intervention | Frequency (past 72-80 hours) | Implementation Level |
|---|---|---|
| Listening actively to patients' illness stories | 3+ times | High |
| Helping patients have quiet time/space | 3+ times | High |
| Listening to spiritual concerns | 3+ times | High |
| Assessing spiritual/religious beliefs | 3+ times | High |
| Remaining present to show caring | 3+ times | High |
| Documenting spiritual care provided | <3 times | Low |
| Arranging religious clergy visits | <3 times | Low |
| Discussing spiritual needs in shift reports | <3 times | Low |
Experimental Protocols and Assessment Methodologies
Spiritual Care Competency Measurement
Validated instruments provide researchers with reliable methods for quantifying spiritual care integration. The Spiritual Care Competency Scale (SCCS) comprises 27 items across six dimensions: assessment and implementation of spiritual care, specialization and quality improvement, individual support and patient counseling, referral to specialists, attitude toward spirituality, and communication [65]. Each item is rated on a 5-point Likert scale, with total scores ranging from 27-135 (low: 27-54; moderate: 54-81; high: 81-135) [65].
A recent cross-sectional study demonstrated the effectiveness of this instrument, revealing among 420 nursing students a mean spiritual care competency score of 91.92 ± 15.22, indicating high competency levels, with 78.6% of participants demonstrating high spiritual care competency [65]. This study also established a significant positive correlation between spiritual care competency and spiritual sensitivity (r = 0.678, p<0.001), confirming that awareness of spiritual concerns directly impacts care quality [65].
Spiritual Sensitivity Assessment
The Spiritual Sensitivity Scale (SSS) is a 20-item instrument assessing professional spiritual sensitivity and inner spiritual sensitivity across five domains [65]. Using a 5-point Likert scale (0=never to 4=always), total scores range from 0-100, with higher scores indicating greater sensitivity (very low: 0-20; low: 20-40; moderate: 40-60; high: 60-80; very high: 80-100) [65]. In implementation studies, this scale has demonstrated strong internal consistency (Cronbach's α = 0.927) and convergent validity with spiritual intelligence measures (r = 0.66) [65].
Spiritual Screening and Assessment Protocols
Systematic spiritual care begins with standardized screening and assessment. Research supports several validated tools:
- "Are you at peace?": A single-item spiritual screening demonstrated to effectively probe spiritual concerns at end of life [61]
- Spiritual AIM Assessment Tool: Structured model for assessing spiritual needs and outcomes in relationship [61]
- PC-7: Quantifiable assessment of spiritual concerns for patients receiving palliative care near end of life [61]
These instruments enable clinical researchers to identify spiritual distress and measure intervention effectiveness using standardized metrics compatible with existing clinical pathway evaluation frameworks.
Implementation Framework: Integrating Spiritual Care into Clinical Pathways
Essential Components for System Integration
Research identifies three essential categories for spiritual care integration within hospital systems [62]:
- Management and Leadership: Policy and planning, organizational structure, interdepartmental cooperation, monitoring, and supervision
- Resource Provision: Human resources (trained chaplains and spiritual care providers), financial allocation, physical space, and informational resources
- Service Delivery Process: Standardized assessment of patient needs and provision of specialized services
The following diagram illustrates the strategic integration of spiritual care within standardized clinical pathways:
Spiritual Care Intervention Taxonomy
Spiritual care interventions fall into two primary categories, each with specific applications [62]:
- Trans-religious Interventions: Address physical, psychological, and social dimensions through approaches like active listening, compassionate presence, meaning-making conversations, and dignity therapy
- Religious Interventions: Include denomination-specific practices such as prayer, scripture reading, rituals, sacraments, and religious clergy consultation
The selection of appropriate interventions depends on comprehensive spiritual assessment findings and patient preferences, with protocols requiring flexibility for individualization while maintaining standardized documentation and outcome tracking.
Research Reagents and Tools for Spiritual Care Investigation
Table 3: Essential Research Instruments for Spiritual Care Investigation
| Instrument/Tool | Primary Application | Psychometric Properties | Implementation Context |
|---|---|---|---|
| Spiritual Care Competency Scale (SCCS) | Measures healthcare provider competency in spiritual care delivery | 27 items, α = 0.77-0.924, 6 subscales [65] | Pre/post educational interventions, competency validation |
| Nurse Spiritual Care Therapeutics Scale (NSCTS) | Assesses frequency of spiritual care intervention provision | 17 items, measures implementation frequency [64] | Clinical practice evaluation, quality improvement |
| Spiritual Sensitivity Scale (SSS) | Evaluates awareness of spiritual needs and concerns | 20 items, α = 0.904-0.927, 2 subscales [65] | Provider assessment, educational outcomes |
| Spiritual AIM Assessment | Structured spiritual assessment in clinical settings | Qualitatively measures spiritual distress, identifies interventions [61] | Palliative care, chronic illness management |
| PC-7 Assessment Tool | Quantifiable assessment of spiritual concerns near end-of-life | 7-item structured assessment [61] | End-of-life care, palliative care pathways |
Discussion: Theological Validation in Clinical Contexts
Evidence for Efficacy and Outcomes
The empirical validation of theological bioethics occurs through demonstrated patient outcomes. Research consistently shows that addressing spiritual needs improves quality of life, reduces anxiety, supports psychological adjustment, and enhances therapeutic outcomes [65]. Specific studies demonstrate:
- Spiritual care contributes to holistic health, patient-centered care, and improved health outcomes [64]
- Spiritual well-being correlates with reduced symptom burden and enhanced coping mechanisms in chronic illness [62]
- Professional chaplaincy interventions are associated with improved patient satisfaction and perceived quality of care [61]
These outcomes validate the theological premise that humans are integrated beings whose healing requires attention to spiritual dimensions alongside physical treatments.
Implementation Challenges and Solutions
Significant barriers impede spiritual care integration, including inadequate training, unclear role definitions, documentation challenges, and reimbursement limitations [64] [65]. Successful implementation requires:
- Staff Development: Targeted training programs for healthcare providers in spiritual care competencies
- Documentation Systems: Standardized spiritual care documentation within electronic health records
- Interprofessional Collaboration: Clear referral pathways between medical staff and spiritual care specialists
- Policy Support: Institutional policies that mandate spiritual assessment and resource allocation
The following workflow details the process for interdisciplinary spiritual care collaboration:
The development of practical protocols for integrating spiritual care into standard patient care pathways represents both a clinical imperative and a validation of theological bioethics in contemporary healthcare. Evidence demonstrates that systematic spiritual care implementation improves patient outcomes, enhances satisfaction, and completes the holistic care model that acknowledges humans as integrated physical, psychological, social, and spiritual beings.
The proposed frameworks, assessment tools, and implementation strategies provide researchers and clinicians with evidence-based approaches for advancing this critical dimension of patient care. Future research should focus on refining standardized assessment protocols, demonstrating cost-effectiveness, and developing specialized interventions for diverse patient populations across the illness trajectory.
As healthcare continues to evolve toward person-centered models, the integration of spiritual care within clinical pathways will increasingly demonstrate its essential value in healing and whole-person care.
Assessing Efficacy and Impact: Theological vs. Secular Ethical Approaches
The validation of ethical frameworks in clinical practice and research remains a central challenge in bioethics. This guide provides a systematic comparison between theological bioethics and the secular principlism established by Tom Beauchamp and James Childress. These frameworks offer distinct pathways for addressing moral dilemmas in medicine and drug development, each with unique philosophical foundations, application methodologies, and assessment criteria. Understanding their comparative structure is essential for researchers, scientists, and drug development professionals navigating complex ethical terrain in healthcare innovation.
Theological bioethics encompasses diverse religious traditions, including Catholic, Orthodox, and Protestant Christian perspectives, along with Islamic, Jewish, and other faith-based approaches [2]. These frameworks derive their moral authority from religious texts, traditions, and theological reasoning. In contrast, the secular principlism articulated in Principles of Biomedical Ethics by Beauchamp and Childress offers a platform for ethical deliberation across diverse moral traditions through four core principles: respect for autonomy, non-maleficence, beneficence, and justice [66]. This comparative analysis examines their foundational assumptions, operational mechanisms, and practical applications within clinical research environments.
Foundational Frameworks: Comparative Structures
Historical and Philosophical Origins
Theological bioethics emerged from centuries of religious engagement with medicine and healing practices. The Catholic tradition developed sophisticated metaethical reflection that differentiates the value of life from other anthropological concepts [2], while Orthodox bioethics bases its ethical judgments on Holy Scripture and Holy Tradition, discerning the "mind of the Church" through councils, patristic writings, and canon law [2]. These traditions maintain that life is a precious gift from God that humans are entrusted to develop and preserve as responsible stewards rather than absolute masters [2].
Secular principlism has more recent origins in late twentieth-century philosophical ethics. Beauchamp's work as primary drafter of the Belmont Report established three foundational principles: respect for persons, beneficence, and justice [66]. This framework was later refined in Principles of Biomedical Ethics to include four core principles: respect for autonomy, non-maleficence, beneficence, and justice [66]. The approach was designed to provide an analytical framework for resolving ethical problems in human subjects research, eventually forming the backbone of federal regulations governing research in the United States [66].
Table 1: Foundational Elements of Ethical Frameworks
| Element | Theological Bioethics | Secular Principlism |
|---|---|---|
| Primary Source of Authority | Divine revelation, religious texts, tradition | Human reason, common morality |
| Metaphysical Foundation | Theological anthropology (e.g., humans created in God's image) [2] | Naturalistic worldview without supernatural commitments |
| Epistemological Approach | Faith seeking understanding through scripture and tradition | Critical reasoning and reflective equilibrium |
| Historical Development | Evolved within religious traditions over centuries [2] | Formalized in late 20th century for research ethics [66] |
| Scope of Application | Often comprehensive worldview encompassing all of life | Focused specifically on biomedical dilemmas |
Conceptual Architectures
The conceptual structure of theological bioethics typically builds from fundamental theological claims about the nature of God, humans, and their relationship. For Christian bioethics, key concepts include humans as created in God's image (imago Dei), the transformative concept of agape love as the source of moral life, and understanding medicine as mission rather than merely profession [2]. The Eastern Orthodox tradition further distinguishes between the "image" of God (human capacities for intellect, emotion, ethical judgment) and the "likeness" of God (the potential to become Godlike through never-completed perfection) [2].
Secular principlism employs a mid-level framework that bridges abstract ethical theories and concrete cases through specification and balancing. Specification involves "the progressive and substantive delineation of principles and rules that gives them more specific and practical content" [66]. This process of molding and refining principles makes them more precise for policy purposes and must be continuously undertaken as new circumstances arise in research and clinical care [66].
Methodological Approaches: Reasoning Processes Compared
Decision-Making Protocols
Theological ethics frequently employs distinctive reasoning methods such as the rule of double effect (RDE), which helps evaluate actions that may produce both good and bad effects [67]. The traditional conditions for RDE include: (1) the action itself must be good or at least neutral; (2) the good effect, not the bad effect, is what is intended; (3) the good effect is not produced by the bad effect; and (4) there is a proportionately grave reason for permitting the bad effect [67]. This method relies critically on the distinction between intention and foresight, where intention is understood as "an irreducibly simple attitude, ascribable to an agent, that takes as its object a proposition about an event that the agent himself chooses to bring about under a definite description" [67].
Secular principlism utilizes a systematic process of specification to translate general principles into practical guidance. As Beauchamp noted, this "work" of research ethics involves "molding the general principles…so that they become sufficiently concrete…to give them increased action-guiding capacity" [66]. This process acknowledges that principles at a lofty level of abstraction require more precision through specification to be effective in regulative and decision-making contexts, particularly as new or unanticipated circumstances arise in biomedical research [66].
Table 2: Methodological Approaches in Ethical Deliberation
| Methodological Element | Theological Approaches | Secular Principlism |
|---|---|---|
| Primary Reasoning Method | Casuistry with theological warrants | Specification and reflective equilibrium |
| Role of Intention | Central to moral evaluation (e.g., double effect) [67] | Considered but not determinative |
| Handling Moral Conflicts | Appeal to authoritative tradition and discernment | Balancing through deliberative process |
| Epistemological Resources | Scripture, tradition, reason, experience | Empirical data, rational analysis, common morality |
| Adaptation to New Challenges | Through interpretive engagement with tradition | Through specification and balancing processes |
Application Workflows: From Principle to Practice
The application of theological bioethics typically follows a discernment process that engages multiple sources of moral insight. For example, in Catholic bioethics, this involves consideration of natural law reasoning, magisterial teaching, and virtue formation [2]. The clinical application of these frameworks often emphasizes the relational nature of healthcare, framing medicine as a mission rather than merely a profession, where patients are regarded as brothers and sisters rather than simply clients or cases [2].
Secular principlism employs a more structured application process, particularly for research ethics oversight. The framework guides institutional review boards (IRBs) in evaluating proposed research through systematic consideration of how each principle applies to the specific context [66]. This becomes particularly important in contemporary challenges such as determining when requirements for informed consent might permissibly be relaxed for research studies embedded into clinical care, including pragmatic clinical trials and comparative effectiveness research [66].
Experimental Protocols: Framework Validation Methods
Case Analysis Methodology
Protocol Title: Comparative Ethical Analysis of Complex Clinical Cases Using Multiple Frameworks
Purpose: To evaluate how theological frameworks and secular principlism approach morally complex cases in clinical practice and research, identifying points of convergence and divergence.
Materials Needed:
- Detailed case narrative with clinical, psychosocial, and relational dimensions
- Framework analysis templates for each ethical approach
- Expert consultants in theological ethics and principlism
- Documentation system for recording reasoning processes
Procedure:
- Case Selection: Identify a clinically complex case with multiple ethical dimensions (e.g., end-of-life decisions, reproductive technologies, resource allocation)
- Independent Analysis: Have theological ethicists and principlism experts analyze the case separately using their respective frameworks
- Reasoning Documentation: Record the step-by-step reasoning process, including key decision points and moral warrants
- Outcome Comparison: Compare the recommended courses of action and justifications
- Framework Assessment: Evaluate each framework's strengths and limitations in addressing the case complexities
Validation Metrics:
- Consistency of reasoning within each framework
- Ability to address all morally relevant considerations
- Practical applicability in clinical settings
- Coherence with foundational principles
Empirical Validation Protocol for Clinical Ethics Consultation
Protocol Title: Outcomes Assessment of Ethics Consultation Recommendations Grounded in Different Frameworks
Purpose: To empirically evaluate the practical outcomes and stakeholder satisfaction when clinical ethics consultations employ primarily theological versus principlist frameworks.
Study Design:
- Prospective observational cohort study
- Multi-center participation across diverse healthcare settings
- Mixed-methods data collection
Data Collection Instruments:
- Stakeholder Satisfaction Scales measuring patient/family, clinician, and administrator satisfaction
- Moral Distress Thermometers for healthcare providers pre- and post-consultation
- Implementation Fidelity Measures assessing adherence to consultation recommendations
- Follow-up Interviews exploring perceived strengths and limitations of the ethical approach
Analysis Plan:
- Quantitative analysis of satisfaction scores and moral distress levels
- Qualitative thematic analysis of interview data
- Comparative assessment of implementation challenges
- Longitudinal tracking of ethical conflict resolution
Comparative Performance: Analytical Outcomes
Framework Efficacy Across Domains
The performance of theological frameworks and secular principlism varies significantly across different domains of bioethical inquiry. Their comparative strengths become evident when applied to specific healthcare contexts and moral dilemmas.
Table 3: Framework Performance Across Bioethics Domains
| Bioethics Domain | Theological Frameworks | Secular Principlism | Comparative Observations |
|---|---|---|---|
| End-of-Life Care | Provides robust concepts of suffering, dignity, and natural death [2] | Strong on autonomy rights and non-maleficence | Theological frameworks offer thicker concepts of meaning; principlism offers clearer procedural guidance |
| Research Ethics | Emphasizes protection of vulnerable as bearing God's image [2] | Systematic approach via Belmont principles [66] | Principlism dominates regulatory frameworks; theology provides foundational justification for human dignity |
| Reproductive Ethics | Comprehensive views based on theological anthropology [2] | Focused on autonomy and justice considerations | Theological approaches often more restrictive; principlism accommodates wider range of practices |
| Resource Allocation | Concepts of stewardship, preference for poor [68] | Justice principle as primary guide | Both emphasize equity but from different foundational commitments |
| Genetics & Emerging Tech | Caution based on theological anthropology and human limits [2] | Cost-benefit analysis within principle constraints | Theological frameworks often more precautionary; principlism more adaptable to new technologies |
Validation Metrics in Clinical Practice
Assessment of these frameworks in clinical contexts reveals distinctive patterns of implementation and effectiveness. Theological frameworks demonstrate particular strength in providing meaning-making resources for patients and providers facing profound suffering and existential questions [2]. The concept of medicine as mission rather than mere profession transforms the patient-practitioner relationship into one characterized by agape love—disinterested, non-discriminatory care that serves the whole person [2].
Secular principlism excels in procedural clarity and regulatory application, particularly in research oversight and institutional policy development [66]. The framework's four principles provide a comprehensive structure for ethics committee deliberations and institutional review board assessments. However, critics note challenges in principle specification and balancing mechanisms, observing that the process of making abstract principles concrete for specific contexts requires considerable judgment [66].
Research Implementation Toolkit
Analytical Instruments for Framework Comparison
Primary Protocol Kits:
- Case Analysis Matrix Template - Structured worksheet for parallel analysis of cases across frameworks
- Principle Specification Guide - Step-by-step protocol for operationalizing abstract principles
- Theological Warrant Tracking Tool - Documentation system for tracing moral claims to theological foundations
- Balancing Mechanism Calculator - Weighted decision aid for resolving principle conflicts
Assessment Metrics:
- Coherence Scorecard - Measures internal consistency of ethical reasoning
- Comprehensiveness Index - Assesses framework ability to address all morally relevant factors
- Applicability Scale - Rates practical implementation feasibility in clinical settings
- Stakeholder Acceptance Measure - Gauges perceived legitimacy across diverse groups
Table 4: Essential Resources for Ethical Framework Application
| Resource Category | Specific Tools | Application Context | Framework Compatibility |
|---|---|---|---|
| Decision Support Systems | Ethical analysis algorithms, Case databases with precedent analyses | Clinical ethics consultation, Research protocol review | Both frameworks with customization |
| Educational Materials | Framework-specific case studies, Principle specification exercises | Ethics committee training, Researcher education | Framework-specific versions needed |
| Consultation Services | Theological ethics experts, Principlism methodology consultants | Complex case resolution, Policy development | Specialized by framework |
| Evaluation Instruments | Moral distress scales, Ethical climate assessments, Implementation fidelity measures | Program evaluation, Quality improvement | Cross-framework adaptation possible |
| Documentation Templates | Ethics consultation records, Research ethics applications | Institutional review processes | Require framework-specific modifications |
This comparative analysis demonstrates that both theological frameworks and secular principlism offer valuable but distinct resources for addressing ethical challenges in clinical practice and research. Theological bioethics provides thick moral narratives and comprehensive worldviews that situate healthcare decisions within larger understandings of human flourishing and divine purpose [2]. These frameworks emphasize concepts like love, stewardship, and vocation that transform understanding of the healing relationship [2]. Secular principlism offers a broadly accessible vocabulary and systematic analytical structure that facilitates ethical deliberation across diverse moral perspectives [66]. Its strength lies in procedural clarity and regulatory application, particularly for research ethics oversight.
The validation of theological bioethics in clinical practice research does not necessitate rejection of secular principlism, but rather recognition of their distinctive contributions to ethical reasoning. Theological frameworks provide foundational justifications for human dignity and rights that undergird principles like respect for persons [69]. They address dimensions of human experience—including spirituality, meaning, and ultimate concerns—that often remain marginal in principle-based approaches. Conversely, principlism offers practical mechanisms for resolving conflicts and specifying general norms for particular contexts [66]. For researchers, scientists, and drug development professionals, this comparative analysis suggests the value of methodological pluralism that draws on the distinctive strengths of each framework while recognizing their limitations. The choice between frameworks depends significantly on the specific ethical question, institutional context, and community of moral deliberation.
The integration of theological perspectives within bioethics represents a significant paradigm in clinical practice and research. While secular bioethics has predominantly focused on principles such as autonomy, beneficence, and justice, theological bioethics introduces a framework grounded in the sacredness of life, human dignity, and spiritual well-being [70] [2]. This analysis systematically compares the impact of theological bioethics against secular bioethical approaches, examining their respective influences on patient autonomy, dignity, and overall well-being. The growing body of empirical evidence demonstrates that theological bioethics does not supplant patient autonomy but rather transforms it within a broader context of meaning, relationship, and purpose [71] [72]. By validating the clinical relevance of theological bioethics through empirical data and conceptual analysis, this review establishes its distinctive contributions to patient care, particularly in addressing the existential dimensions of illness that often remain unaddressed in conventional secular frameworks.
Comparative Theoretical Frameworks
Secular Bioethics: Principles and Limitations
Secular bioethics, particularly the dominant four-principles approach (autonomy, beneficence, nonmaleficence, and justice), provides a framework for moral reasoning in pluralistic societies [70]. This approach grounds ethical decision-making in principles intended to be universally accessible, independent of specific religious or metaphysical commitments [73]. Within this framework, patient autonomy has attained "sacrosanct status," often becoming the preeminent value governing healthcare providers' actions [70].
However, this secular framework faces significant limitations in clinical practice. Its "thin" approach emphasizes procedural guidelines and regulatory solutions while neglecting substantive questions about human suffering, meaning, and purpose [73]. Bioethics born from concern about human suffering has ironically spent little intellectual energy on responses to suffering, largely ceding inquiries about its nature and meaning to religious traditions [73]. This limitation becomes particularly problematic in serious illness, where patients frequently grapple with existential concerns that transcend physical symptoms.
Theological Bioethics: Foundational Concepts
Theological bioethics, encompassing Catholic, Orthodox, and Protestant traditions, grounds its ethical framework in distinct anthropological and metaphysical commitments. Several core concepts differentiate theological from secular approaches:
Human Dignity as Imago Dei: The foundational principle of theological bioethics is the dignity of the human person, understood as created in God's image [70] [2]. This concept provides a substantive basis for human dignity that transcends functional capacities or rational attributes. As expressed in Catholic teaching, "every human individual without distinction of race, culture or religion, as a person is clothed in God's same dignity" [70].
Agape Structure of Love: Theological bioethics introduces the concept of self-giving love as the source of moral life and the essence of Christian proclamation [2]. Within this framework, medicine is understood not merely as a profession but as a mission, with patients regarded as brothers and sisters rather than autonomous agents alone [2].
Teleological Understanding: Contrary to secular bioethics which "banishes the concepts of purpose and ultimate meaning to religion," theological approaches explicitly address questions of meaning, purpose, and ultimate ends [73]. This teleological perspective provides resources for interpreting suffering within a broader cosmic narrative.
Informed Freedom: While secular bioethics emphasizes autonomy as self-determination, theological perspectives understand freedom as "a great gift from God" placed "in the service of a person and his/her accomplishment through self-giving and accepting of others" [2]. This reconceptualization maintains respect for persons while situating freedom within a context of moral responsibility and relationality.
Table 1: Theoretical Foundations Comparison
| Framework Element | Secular Bioethics | Theological Bioethics |
|---|---|---|
| Foundation of Human Dignity | Rational nature, human rights | Imago Dei (Image of God), inherent sacredness |
| Primary Principle | Autonomy | Dignity of the human person |
| View of Freedom | Self-determination, negative rights | Responsible freedom oriented toward truth and good |
| Approach to Suffering | Problem to be eliminated or managed | Paradox with potential meaning, spiritual significance |
| Moral Methodology | Principles, utility, consequences | Principles informed by scripture, tradition, natural law |
Experimental Evidence and Outcome Measures
Impact on Patient Well-being and Quality of Life
Empirical research demonstrates significant associations between spiritual/religious factors and patient well-being outcomes. These findings validate the theological bioethics emphasis on addressing spiritual dimensions of care:
Quality of Life Enhancement: A multisite, cross-sectional study of 1,610 cancer patients found that after controlling for other predictors, higher patient religion and spirituality (R/S) was associated with improved quality of life [72]. Notably, among patients with high physical symptom burden, those reporting higher R/S had better quality of life scores than those reporting lower R/S.
Moderating Effect on Symptoms: Research indicates that spiritual well-being may mitigate the relationship between physical symptoms and quality of life. Patients with greater religious coping and spirituality reported better psychological well-being even in the context of significant physical suffering [72].
Spiritual Pain Correlates: Studies at MD Anderson Cancer Center found that 58% of advanced cancer patients reported experiencing "spiritual pain," which was associated with significantly lower self-perceived religiosity and spiritual quality of life [72]. Those with spiritual pain also demonstrated increased depression, anxiety, and anorexia.
End-of-Life Outcomes: A prospective cohort study of 340 advanced cancer patients found that those reporting high support of their spiritual needs by their medical teams had a three-fold greater odds of transitioning to hospice care compared to patients receiving low spiritual support [72]. High religious copers whose spiritual needs were well-supported were five times more likely to transition to hospice and five times less likely to receive aggressive care during their final week.
Table 2: Spiritual Care Outcomes in Serious Illness
| Outcome Measure | Findings | Study Population |
|---|---|---|
| Quality of Life | Higher R/S associated with improved quality of life after controlling for other predictors | 1,610 cancer patients [72] |
| Spiritual Pain | 58% reported spiritual pain; associated with decreased spiritual QoL and increased physical/emotional symptoms | Advanced cancer patients at MD Anderson [72] |
| Hospice Transition | 3x greater odds of transitioning to hospice with high spiritual support | 340 advanced cancer patients [72] |
| Treatment Aggression | 5x less likely to receive aggressive care at end-of-life with high spiritual support | High religious copers with advanced cancer [72] |
| Medical Costs | $2,441 lower average cost in final week for spiritually well-supported patients | Advanced cancer patients [72] |
Impact on Patient Autonomy and Decision-Making
Theological bioethics enhances patient autonomy through a reconceptualization that situates self-determination within a broader context of meaning and relationship:
Spiritual Influences on Decision-Making: Research demonstrates that religious viewpoints and beliefs significantly influence medical decision-making, including preferences for aggressive treatment and desire for all measures to extend life [72]. Theological bioethics acknowledges these dimensions as legitimate aspects of patient values rather than dismissing them as external to autonomous decision-making.
Beyond Minimalist Autonomy: The secular "liberal view of autonomy" often follows the minimalist approach that "your right to swing your fist ends where my nose begins" [71]. Theological bioethics argues instead for an autonomy that is "informed and guided" by conscience and moral formation [71]. This approach recognizes that true autonomy requires not merely non-interference but the cultivation of virtue and moral discernment.
Conscience Rights Protection: Theological bioethics emphasizes the right of conscience for healthcare professionals, maintaining that professionals should not be forced to participate in procedures they consider immoral [74]. This protection safeguards the moral integrity of the healing relationship against reduction to mere service provision.
Methodological Protocols for Spiritual Care Research
The evidence cited throughout this analysis emerges from rigorous research methodologies that can be systematically replicated:
Spiritual Needs Assessment Protocol: Multiple studies employed comprehensive spiritual assessment tools in clinical settings. The typical protocol includes: (1) Administration of validated instruments measuring spiritual well-being, religious coping, and spiritual needs; (2) Quantitative assessment of quality of life, psychological symptoms, and treatment preferences; (3) Prospective tracking of medical outcomes, including care transitions and resource utilization [72] [62].
Spiritual Care Intervention Model: Effective spiritual care interventions typically involve: (1) Systematic assessment of patient spiritual needs; (2) Integration of spiritual care into treatment planning; (3) Collaboration among clinicians, chaplains, and community spiritual providers; (4) Ongoing evaluation of spiritual distress and response to interventions [62].
Qualitative Analysis Framework: Studies examining the lived experience of spirituality in illness generally employ: (1) Semi-structured interviews exploring meaning, purpose, and spiritual concerns; (2) Thematic analysis using established qualitative methodologies; (3) Integration of patient narratives into understanding the spiritual dimensions of illness [72] [62].
Conceptual Pathways and Mechanisms
The therapeutic benefits of theological bioethics operate through several conceptual pathways that explain its impact on patient outcomes. The following diagram illustrates the primary mechanisms through which theological bioethics influences patient care:
Enhanced Autonomy Through Moral Formation
Theological bioethics reconceptualizes autonomy not as mere choice but as the capacity for morally informed self-direction. This pathway operates through:
Conscience Formation: Contrary to secular frameworks that view conscience primarily as a negative right of refusal, theological bioethics understands conscience as requiring "education from early childhood and throughout our lives" [71]. This formation process enables genuinely autonomous decision-making grounded in moral truth rather than arbitrary preference.
Relational Autonomy: Theological perspectives emphasize that "freedom includes essential relational dimension" and is "put in the service of a person and his/her accomplishment through self-giving and accepting of others" [2]. This relational understanding counters the radical individualism of some secular autonomy models.
Virtue Development: By cultivating virtues such as compassion, courage, and wisdom, theological bioethics enhances patients' capacity for making decisions that authentically reflect their values and long-term flourishing rather than immediate preferences or external pressures.
The investigation of theological bioethics in clinical contexts requires specialized methodological approaches and assessment tools. The following table outlines key resources for researchers in this field:
Table 3: Research Reagent Solutions for Theological Bioethics Investigation
| Research Tool | Application in Field | Function and Purpose |
|---|---|---|
| Spiritual Needs Assessment Scales | Quantitative measurement of spiritual concerns, religious coping, and existential distress in patient populations | Validated instruments (e.g., FACIT-Sp, SPNS) that operationalize spiritual constructs for empirical research and clinical assessment |
| Qualitative Interview Protocols | In-depth exploration of patient spiritual experiences, meaning-making processes, and religious values in healthcare decisions | Semi-structured interview guides that elicit narrative data on spiritual dimensions of illness while maintaining methodological rigor |
| Spiritual Care Intervention Manuals | Standardized protocols for implementing spiritual care within healthcare settings, including chaplaincy interventions | Manualized approaches that ensure consistent delivery of spiritual care while allowing for measurement of efficacy and outcomes |
| Religious Values Analysis Frameworks | Systematic analysis of how specific religious traditions approach bioethical issues and decision-making | Conceptual tools for understanding how theological commitments translate into healthcare preferences and moral reasoning |
| Outcome Measurement Batteries | Comprehensive assessment of patient well-being encompassing physical, psychological, social, and spiritual dimensions | Multi-dimensional instruments that capture holistic outcomes relevant to theological bioethics' comprehensive view of human flourishing |
Discussion: Integration and Implications
Theoretical and Clinical Integration
The evidence demonstrates that theological bioethics does not represent a sectarian niche but offers substantive contributions to mainstream healthcare ethics and practice. By addressing dimensions of human experience that secular frameworks often neglect—particularly suffering, meaning, and spiritual well-being—theological approaches complete rather than compete with established bioethical methods [73]. The empirical findings on spiritual care outcomes suggest that integrating theological perspectives represents not merely a philosophical preference but an evidence-based practice for enhancing patient care.
The integration of theological bioethics within clinical practice requires moving beyond mere tolerance of religious perspectives to active engagement with their substantive contributions. This engagement encompasses several dimensions:
Reconceptualizing Autonomy: Theological bioethics challenges the reduction of autonomy to mere non-interference, proposing instead an understanding of freedom as the capacity for morally informed self-direction oriented toward genuine human flourishing [71].
Addressing Suffering Comprehensively: By providing frameworks for finding meaning in suffering, theological bioethics addresses what secular approaches often cannot—the paradox that "suffering also reveals to the sufferer a greater depth of human experience and meaning" [73].
Grounding Human Dignity: While secular bioethics struggles to establish a foundation for human dignity beyond functional capacities, theological approaches root dignity in the inherent worth of persons as created in God's image, providing a secure foundation for human rights and medical ethics [70] [2].
Limitations and Future Research Directions
While the current evidence supports the positive impact of theological bioethics on patient outcomes, several limitations warrant attention. Regional variations in spiritual practices and religious demographics necessitate more diverse population studies [72]. Future research should also develop more sophisticated methodologies for measuring the complex relationships between spiritual care, clinical outcomes, and ethical decision-making. Longitudinal studies examining how theological bioethics influences long-term patient outcomes across different illness trajectories would particularly strengthen the evidence base.
This comparative analysis demonstrates that theological bioethics significantly enhances patient autonomy, dignity, and well-being through distinctive mechanisms that complement and complete secular approaches. The empirical evidence confirms that addressing spiritual dimensions of care produces measurable improvements in quality of life, care transitions, and patient satisfaction. Rather than representing a sectarian alternative to mainstream bioethics, theological perspectives provide essential resources for addressing the full depth of human experience in health and illness. By validating these approaches through both conceptual analysis and clinical outcomes, this review establishes theological bioethics as an evidence-based paradigm that responds to limitations in dominant secular frameworks while promoting more comprehensive, compassionate, and effective patient care.
The validation of ethical frameworks, including theological bioethics, in clinical practice and research is an increasingly critical endeavor. As a field dedicated to resolving complex moral problems in medicine and biology, bioethics has evolved to embrace interdisciplinary methodologies that integrate empirical research with normative analysis. This integration provides a robust mechanism for testing, refining, and validating ethical principles against the realities of clinical practice and human experience. The emergence of empirical bioethics as a distinct methodological approach represents a significant shift toward evidence-based ethical analysis, moving beyond purely theoretical discourse to engage directly with the contextualized experiences of patients, clinicians, and researchers [75] [76].
This evolution responds to a recognized need to ground ethical reflection in the actual circumstances where moral dilemmas arise. As Kon notes, "While many have argued that empirical research merely illuminates current practices and cannot inform normative ethics, others assert that research-based work has significant implications for refining our ethical norms" [77]. For theological bioethics specifically, this empirical turn offers a pathway to demonstrate its relevance and applicability in pluralistic healthcare settings, where diverse value systems coexist. The validation process through interdisciplinary research thus serves not only to strengthen ethical frameworks through evidentiary support but also to facilitate dialogue across different moral traditions in increasingly secular clinical environments [31] [78].
Table 1: Key Definitions in Interdisciplinary Bioethics Validation
| Term | Definition | Relevance to Validation |
|---|---|---|
| Empirical Bioethics | Interdisciplinary activity that integrates empirical findings with normative analysis [79]. | Provides methodological framework for testing normative claims against observable reality. |
| Systematic Review | A research method that searches, selects, analyses, and synthesizes literature transparently and systematically [80]. | Offers comprehensive, unbiased overview of existing evidence for ethical analysis. |
| Normative Analysis | The process of determining what ought to be done based on ethical principles and reasoning. | Establishes ethical standards against which practices can be validated. |
| Integration | The process of combining empirical data with normative analysis to produce ethically justified conclusions [79] [76]. | Core mechanism for validating theoretical frameworks through empirical evidence. |
The Empirical Turn in Bioethics: Foundations for Validation
Conceptual Frameworks for Empirical-Normative Integration
The integration of empirical research with normative ethics has been conceptualized through several typologies that classify how factual evidence can inform moral reasoning. Kon's hierarchical framework categorizes empirical research in bioethics into four distinct levels: (1) Lay of the Land studies that describe current practices, opinions, or beliefs; (2) Ideal Versus Reality research that assesses how well clinical practice matches ethical ideals; (3) Improving Care studies that seek to align practice closer to ethical norms; and (4) Changing Ethical Norms work that uses cumulative empirical evidence to inform and potentially transform ethical standards [77]. This framework demonstrates a progression from descriptive to prescriptive applications of empirical data, with validation occurring at each level through different mechanisms.
Alternative typologies further refine our understanding of this integration. Solomon identified ten relationships between empirical research and conceptual scholarship, categorized into three broader groups: facilitating the move from ethical analysis to ethically justified behavior; enhancing ethical analysis and justification; and generating new ethical concerns [81]. Similarly, Sulmasy and Sugarman described eight contributions of empirical research to bioethics, including purely descriptive studies, testing established or new norms, describing facts relevant to normative arguments, and assessing likely consequences of ethical decisions [81]. These frameworks collectively establish a conceptual foundation for validation processes, outlining specific pathways through which empirical evidence can confirm, challenge, or refine ethical propositions.
Systematic Reviews as Validation Tools
Systematic reviews represent a particularly rigorous methodology for validating ethical frameworks through comprehensive evidence synthesis. In bioethics, systematic reviews can encompass both normative literature (philosophical arguments, ethical analyses) and empirical literature (qualitative and quantitative studies on attitudes, experiences, and practices) [80] [82]. The fundamental aim of such reviews is to provide "an unbiased overview on specific topics discussed in the literature" by employing transparent, reproducible search and analysis methods that minimize bias and maximize comprehensiveness [82].
The validation power of systematic reviews lies in their ability to identify patterns, contradictions, and evidence gaps across a broad spectrum of sources. For theological bioethics, systematic reviews can document how religious values and principles manifest in clinical decision-making, patient preferences, and healthcare policies. A meta-review of systematic reviews in bioethics found that 72% of systematic reviews of empirical literature included authors' ethical reflections on the findings, and 59% provided ethical recommendations, demonstrating the potential for evidence synthesis to inform normative conclusions [82]. This methodology offers a structured approach to assessing the real-world applicability and effectiveness of theological ethical frameworks in diverse healthcare contexts.
Methodological Approaches for Interdisciplinary Validation
Empirical Bioethics Methodologies
The field of empirical bioethics has developed numerous methodological approaches for integrating empirical data with normative analysis. A systematic review by Davies et al. identified 32 distinct methodologies for empirical bioethics, which can be broadly categorized into three types: dialogical approaches that rely on stakeholder dialogue to reach shared understanding; consultative approaches where researchers analyze data independently to develop normative conclusions; and combined approaches that incorporate elements of both [76]. Each methodology offers different mechanisms for validation, with varying emphasis on stakeholder participation, theoretical framework, and analytical process.
Among the most prominent methodologies is reflective equilibrium, particularly in its "wide" form, which involves a back-and-forth process between ethical principles, considered moral judgments, and relevant empirical facts until a coherent equilibrium is reached [79]. This method provides a systematic approach to validating ethical principles against moral intuitions and empirical realities. Other significant methodologies include dialogical empirical ethics, which engages stakeholders in moral discourse to develop contextually appropriate norms; grounded moral analysis, which builds ethical frameworks inductively from empirical data; and hermeneutic approaches that interpret the moral meaning of lived experiences [79] [76]. These methodologies share a common commitment to grounding ethical reflection in empirical reality while maintaining rigorous normative analysis.
Figure 1: Empirical Bioethics Research Workflow: This diagram illustrates the iterative process of integrating empirical research with normative analysis to validate ethical frameworks.
Quality Appraisal in Systematic Reviews
A critical methodological challenge in using systematic reviews for validation purposes concerns quality appraisal of included literature. While established tools exist for appraising clinical studies, quality assessment of normative literature remains "still rather a conundrum" with no consensus on appropriate methods [80]. This presents particular challenges for validating theological bioethics, where arguments often draw on religious texts, traditions, and authorities that do not align with standard empirical validity criteria.
Mertz identifies three potential strategies for quality appraisal of normative literature: using criteria internal to each ethical tradition; applying external, content-neutral criteria focused on argumentative rigor; or developing composite approaches [80]. Each strategy presents different advantages and limitations for validation. Internal criteria respect the methodological standards of each tradition but complicate comparative assessment across traditions. External criteria enable comparison but risk imposing alien standards on distinctive forms of ethical reasoning. The development of appropriate quality appraisal frameworks remains an essential methodological frontier for strengthening the validation of theological bioethics through systematic reviews.
Table 2: Methodological Approaches for Interdisciplinary Validation in Bioethics
| Methodology | Key Features | Validation Mechanism | Examples |
|---|---|---|---|
| Reflective Equilibrium | Back-and-forth process between principles, judgments, and facts until coherence is achieved [79]. | Tests ethical principles against considered judgments and empirical facts. | Wide Reflective Equilibrium [79] |
| Dialogical Ethics | Stakeholders engage in moral discourse to develop shared understanding [76]. | Grounds norms in deliberative agreement among affected parties. | Responsive Evaluation [76] |
| Grounded Moral Analysis | Inductive development of ethical frameworks from empirical data [76]. | Builds ethical frameworks directly from empirical observations. | Grounded Theory Methodology [76] |
| Systematic Review | Comprehensive, transparent synthesis of existing literature [80] [82]. | Identifies patterns and evidence gaps across multiple studies. | Meta-narrative Review [82] |
Research Reagent Solutions for Interdisciplinary Validation
Conducting rigorous interdisciplinary validation in bioethics requires specific "research reagents" – methodological tools and frameworks that facilitate the integration of empirical and normative analysis. These tools enable researchers to systematically collect, analyze, and interpret data relevant to ethical questions in clinical practice and research. Unlike laboratory sciences where reagents are physical substances, in interdisciplinary bioethics these reagents primarily comprise conceptual frameworks, methodological guidelines, and analytical procedures.
Essential methodological resources include interview protocols for qualitative exploration of stakeholder perspectives, systematic review guidelines adapted for ethical literature, integration frameworks for connecting empirical findings with normative analysis, and quality appraisal tools for assessing both empirical and normative scholarship. Also crucial are deliberative methodologies for engaging diverse stakeholders in ethical reflection and analysis frameworks for identifying ethical issues in clinical practice. These methodological reagents provide the necessary infrastructure for producing validated ethical knowledge that is both empirically grounded and normatively robust.
Table 3: Essential Methodological Resources for Interdisciplinary Bioethics Research
| Research Tool | Primary Function | Application in Validation |
|---|---|---|
| Semi-structured Interview Protocols | Elicit rich qualitative data on experiences, values, and reasoning [75]. | Document how ethical principles are experienced and interpreted in practice. |
| Systematic Review Guidelines | Standardize search, selection, analysis, and synthesis of literature [80] [82]. | Comprehensively map and assess evidence base for ethical positions. |
| Integration Methodologies | Combine empirical data with normative analysis [79] [76]. | Systematically connect empirical observations with ethical reflection. |
| Quality Appraisal Frameworks | Assess methodological rigor of included studies [80]. | Evaluate strength of evidence supporting ethical claims. |
| Deliberative Methods | Facilitate structured moral dialogue among stakeholders. | Test ethical frameworks through diverse perspectives and experiences. |
Implementation Protocols for Validation Research
Successful implementation of interdisciplinary validation research requires careful attention to study design and analytical processes. For empirical bioethics studies, researchers emphasize the importance of transparent integration processes that clearly articulate how empirical findings inform normative conclusions [79]. European consensus standards for empirical bioethics highlight the need to: "(1) clearly state how the theoretical position was chosen for integration, (2) explain and justify how the method of integration was carried out, and (3) be transparent in informing how the method of integration was executed" [79]. These standards ensure that the validation process itself is subject to critical scrutiny and evaluation.
For systematic reviews addressing ethical questions, key implementation considerations include developing comprehensive search strategies that account for the interdisciplinary nature of bioethics literature, establishing clear inclusion criteria that reflect the review's objectives, and employing appropriate synthesis methods for different types of evidence [80] [82]. Given the methodological diversity of bioethics scholarship, successful implementation often requires adaptability and methodological pluralism rather than rigid adherence to a single approach. As Mertz et al. note, "The heterogeneity currently observed is due both to the interdisciplinary nature of nursing ethics and bioethics, and to the emerging nature of systematic review methods in these fields" [82]. This methodological flexibility enables more responsive and contextually appropriate validation of ethical frameworks.
Figure 2: Interdisciplinary Validation Process: This diagram illustrates how theological bioethics interfaces with empirical data collection, systematic evidence synthesis, and normative analysis through integration processes to produce validated ethical frameworks.
Validation Outcomes and Applications
Documented Contributions to Bioethical Knowledge
Interdisciplinary validation research has produced substantial contributions to bioethical knowledge across multiple domains. Empirical bioethics studies have documented significant gaps between ethical ideals and clinical reality in areas such as end-of-life care, informed consent, and resource allocation [77]. For instance, research on informed consent for clinical trials has revealed that "many research subjects fail to understand even the most basic aspects of clinical research including the purpose of the study, the voluntary nature of study participation, and the fact that the goal of the study is to increase generalizable knowledge and not necessarily to help individual study participants" [77]. These findings have prompted important revisions to consent processes and ethical guidelines.
Systematic reviews have further enhanced bioethical understanding by mapping the landscape of ethical arguments and evidence regarding practical ethical dilemmas. A meta-review of systematic reviews in bioethics found that selected reviews investigated issues related to clinical ethics (50%), research ethics (36%), and public health ethics or organizational ethics (14%) [82]. This body of work provides comprehensive overviews of ethical considerations in specific domains, identifies recurring themes and values across different perspectives, and highlights areas where evidence is lacking or contradictory. For theological bioethics, such reviews can clarify how religious values intersect with healthcare practices and where potential conflicts or synergies with secular frameworks emerge.
Challenges and Limitations in Interdisciplinary Validation
Despite its significant contributions, interdisciplinary validation in bioethics faces several persistent challenges. Researchers report an "air of uncertainty and overall vagueness" surrounding integration methodologies, with difficulties in clearly articulating how empirical findings should inform normative conclusions [79]. This methodological indeterminacy represents a "double-edged sword" that allows flexibility but risks obscuring "a lack of understanding of the theoretical-methodological underpinnings of empirical bioethics research methods" [79]. The field continues to grapple with fundamental questions about how to justify normative claims derived through interdisciplinary approaches.
Additional challenges include disciplinary divides between empirically-oriented and normatively-oriented researchers, methodological tensions between different approaches to knowledge production, and institutional barriers to truly interdisciplinary work [75] [79]. There remains ongoing debate about which objectives of empirical bioethics are most legitimate, with researchers expressing varying levels of agreement about different potential aims. Mihailov et al. found that while "understanding the context of a bioethical issue and identifying ethical issues in practice received unanimous agreement" among researchers, "the most contested objectives were striving to draw normative recommendations and developing and justifying moral principles" [75]. These disagreements reflect deeper philosophical divisions about the nature of ethics and the proper relationship between facts and values.
The interdisciplinary validation of bioethical frameworks through empirical research and systematic reviews represents a dynamic and evolving field with significant potential for enhancing ethical deliberation in healthcare and research. For theological bioethics specifically, these methodologies offer promising pathways for demonstrating relevance, applicability, and effectiveness in diverse clinical contexts. Future methodological development should focus on refining integration processes, enhancing quality appraisal frameworks for normative literature, and developing more sophisticated approaches to synthesizing diverse forms of evidence.
As the field advances, particular attention should be paid to inclusive methodological development that incorporates perspectives from multiple ethical traditions, including religious frameworks. Churchill argues for "a rich working definition of spirituality as a common dimension of human life" that would honor religious traditions while extending beyond them to encompass a broader range of transformative human experiences [78]. Such conceptual expansion could strengthen the validation of theological bioethics by locating it within a broader landscape of human meaning-making and value construction. Through continued methodological refinement and interdisciplinary collaboration, validation research can increasingly provide robust evidence to inform ethical decision-making in clinical practice and research, contributing to more ethically grounded and empirically informed healthcare.
The integration of theological ethics into clinical practice represents a critical frontier in bioethics research, particularly in complex care environments such as palliative medicine and correctional healthcare. This guide examines the empirical validation of theological bioethics through a comparative analysis of its application across these distinct clinical domains. The growing recognition of spirituality as an essential component of holistic care [83] and the ethical imperative to address healthcare disparities in carceral settings [84] provide compelling rationales for examining how theological frameworks translate into practical clinical protocols. This analysis synthesizes experimental data, methodological approaches, and implementation strategies to provide researchers with evidence-based frameworks for integrating theological ethics into clinical research and practice.
Theological Ethics in Palliative Care: Experimental Evidence and Protocols
Empirical Foundations and Outcomes
Table 1: Quantitative Measures of Spiritual Care Impact in Palliative Settings
| Metric | Measurement Instrument | Key Findings | Effect Size/Correlation |
|---|---|---|---|
| Spiritual Wellbeing | Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being (FACIT-Sp) [85] | Significant correlation with reduced decisional conflict | Strong negative correlation |
| Decisional Conflict | Decisional Conflict Scale (DCS) [85] | Lower scores associated with spiritual wellbeing | Scores <25 associated with decision implementation |
| Quality of Life | Holistic assessment integrating physical, emotional, functional dimensions [85] | Positive correlation with spiritual wellbeing | Significant positive correlation |
| Care Satisfaction | Patient-reported outcomes [83] | Higher satisfaction with spiritual care integration | Not quantified in reviewed studies |
| Discomfort & Symptom Burden | Systematic review metrics [83] | Spiritual care associated with easing discomfort | Low evidence level noted |
European systematic reviews demonstrate that spiritual care in palliative contexts is conceptualized as attention for spirituality, presence, empowerment, and bringing peace [83]. The operationalization of these concepts occurs through creative, narrative, and ritual work supported by developing spiritual competency among healthcare providers. Quantitative research utilizing validated instruments provides evidence for the mechanistic role of spiritual factors in patient outcomes.
A 2020 cross-sectional study of 95 palliative outpatients employed sophisticated correlational analysis between spiritual wellbeing and decisional conflict, finding that greater spiritual wellbeing correlated strongly with less decisional conflict (ρ ≈ -0.7, p<0.05), decreased uncertainty, and greater satisfaction with choices [85]. This relationship demonstrates the tangible impact of theological ethics on patient autonomy and decision-making processes in end-of-life care.
Experimental Protocol: Spiritual Wellbeing and Decision-Making
Methodology from Palliative Care Outpatient Study [85]:
- Participant Recruitment: 95 palliative outpatients from two oncology institutes, assessed consecutively from March 2018 to May 2019
- Assessment Battery:
- Sociodemographic Questionnaire (SQ): Collected clinical and demographic variables
- Decisional Conflict Scale (DCS): 16-item self-completed measure of decision-related uncertainty
- Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being (FACIT-Sp): Assessed spiritual wellbeing
- Semi-structured Interview (SSI): Explored perceptions of spirituality and autonomy
- Administration Protocol: Instruments administered face-to-face with questions read aloud to accommodate health status
- Statistical Analysis: Utilized Mann-Whitney tests for group comparisons, correlation analysis for scale relationships, and interpretative phenomenological analysis for qualitative responses
- Ethical Compliance: Adhered to Helsinki Declaration with institutional ethics committee approval
This protocol successfully identified that patients who received spiritual care displayed better scores of spiritual wellbeing, quality of life, and exhibited less decisional conflict [85]. The methodology provides a validated template for quantifying the impact of theological ethics in palliative settings.
Theological Ethics in Incarcerated Healthcare: Frameworks and Implementation
Abolition Bioethics and Systemic Reform
Table 2: Comparative Analysis of Theological Ethical Frameworks in Carceral Healthcare
| Ethical Framework | Core Principles | Application in Carceral Settings | Implementation Challenges |
|---|---|---|---|
| Abolition Bioethics [84] | Dismantling structural inequities; Radical reimagining of justice | Compassionate release advocacy; Systemic reform | Political resistance; Resource limitations |
| Equivalence Principle [86] | Equal standards to community healthcare | Mandated equal care standards | Underserved complex needs; Operational barriers |
| Relational Autonomy | Recognition of constrained decision-making | Addressing institutional coercion | Power imbalances; Security concerns |
| Catholic Social Teaching [2] | Human dignity; Preferential option for poor | Advocacy for marginalized populations | Institutional resistance; Conscience clauses |
| Principle of Accompaniment | Solidarity with marginalized persons | Chaplaincy programs; Spiritual support | Staffing limitations; Security restrictions |
Application of theological ethics in carceral settings confronts the complex interplay of individual, social and systemic factors that impact healthcare utilization [86]. Research with incarcerated individuals in Northern Norway identified critical barriers including distrust in the system, challenges with referral routines, worries about negative consequences, and perceived limited access to mental healthcare [86].
The emerging framework of abolition bioethics applies theological principles of human dignity to advocate for radical reform, arguing that "the most ethically sound and justice-serving solution to the barriers arising from incarceration is to mitigate them with compassionate release" [84]. This approach recognizes that theological ethics must address both individual clinician-patient interactions and the systemic structures that create healthcare disparities.
Experimental Protocol: Qualitative Assessment of Incarcerated Individuals' Experiences
Methodology from Norwegian Prison Study [86]:
- Research Design: Analytical approach drawing on constructivist Grounded theory
- Participant Selection: 15 male participants recruited from three prisons in Northern Norway
- Data Collection: In-depth interviews exploring help-seeking experiences, perceived access to services, and availability of health information
- Thematic Analysis: Identification of recurring themes and patterns in participant experiences
- Ethical Considerations: Approval from Norwegian Correctional system; Data Protection Officer approval; Emphasis on voluntariness and informed consent
This methodology revealed that how prison officers and healthcare personnel respond to incarcerated persons reporting mental distress is critical for their future willingness to seek help [86]. The study identified specific interventions that improved access, including providing information about mental health services, initiating outreaching mental health services, and integrating mental health interventions into treatment programs.
Comparative Analysis: Cross-Domain Implementation Strategies
Unified Conceptual Framework for Theological Ethics Integration
The Scientist's Toolkit: Research Reagent Solutions for Theological Ethics Research
Table 3: Essential Research Instruments for Theological Ethics Validation
| Research Instrument | Primary Application | Key Functions | Validation Status |
|---|---|---|---|
| Decisional Conflict Scale (DCS) [85] | Quantifying decision-related uncertainty | Measures uncertainty, informedness, values clarity, support, satisfaction | Well-validated in clinical populations |
| Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being (FACIT-Sp) [85] | Assessing spiritual wellbeing in illness | Evaluates meaning, peace, faith dimensions | Validated in chronic illness populations |
| Interpretative Phenomenological Analysis (IPA) [87] | Qualitative exploration of religious experiences | In-depth analysis of homogenous data on lived experiences | Established qualitative methodology |
| Semi-structured Interview Protocols [85] | Eliciting patient perspectives on spirituality | Flexible qualitative data collection on spiritual needs | Customizable to research context |
| Religious Coping Frameworks (Ganzevoort Diamond Model) [87] | Analyzing religious interpretation of life events | Maps religion, context, identity, coping as interdependent dimensions | Theoretically grounded assessment |
Discussion: Integration Challenges and Research Opportunities
The validation of theological ethics in clinical practice reveals both domain-specific and universal challenges. In palliative care, the low evidence level for spiritual care interventions noted in European systematic reviews [83] highlights the need for more rigorous methodological approaches. Simultaneously, incarcerated healthcare faces the fundamental ethical challenge of applying theological principles within inherently coercive systems [84].
Both domains share the common requirement for developing spiritual competency among healthcare providers, including self-reflection skills and visibility of spirituality in care structures [83]. The research indicates that successful integration requires both individual practitioner development and systemic reform, particularly in carceral settings where distrust in the system fundamentally impacts healthcare utilization [86].
Future research directions should include:
- Randomized controlled trials of specific spiritual care interventions in palliative settings
- Longitudinal studies on the impact of theological ethics frameworks on health outcomes in correctional environments
- Development of validated metrics for assessing the implementation of theological principles in clinical practice
- Cross-cultural comparative studies on the application of theological bioethics in different religious and healthcare systems
This comparative analysis demonstrates that theological ethics provides substantive frameworks for enhancing care in both palliative and incarcerated settings. The experimental evidence indicates that spiritual wellbeing significantly impacts clinical outcomes, particularly in decision-making processes at the end of life [85]. In carceral environments, theological ethics offers critical frameworks for addressing systemic injustices and advocating for compassionate care [84].
The validation of theological bioethics in clinical practice requires both rigorous empirical research and thoughtful engagement with the fundamental questions of human dignity, meaning, and justice that these clinical contexts raise. By employing the methodological tools and conceptual frameworks outlined in this guide, researchers can contribute to the developing evidence base for theological ethics as an essential dimension of comprehensive healthcare.
Conclusion
The validation of theological bioethics is not a retreat to insular dogma but a necessary evolution for addressing the profound human questions raised by modern clinical practice and drug development. By moving beyond historical secularization and embracing robust methodological frameworks, theological perspectives offer indispensable resources for preserving human dignity, addressing vulnerability, and countering the dehumanizing tendencies of purely technological paradigms. The successful integration of these perspectives relies on continued interdisciplinary collaboration, the development of practical implementation strategies, and further empirical research to quantify their impact on patient outcomes and ethical decision-making. For researchers and biomedical professionals, engaging with theological bioethics provides a more complete ethical compass, ensuring that scientific progress remains aligned with the fundamental goal of holistic, human-centered care.
References
- 1. (PDF) The Secularization of Bioethics—A Critical History [https://www.academia.edu/8008282/The_Secularization_of_Bioethics_A_Critical_History]
- 2. Development and perspectives of theological bioethics [https://pmc.ncbi.nlm.nih.gov/articles/PMC3583400/]
- 3. The History of Medical Ethics [https://www.saet.ac.uk/Christianity/HistoryofMedicalEthics]
- 4. A Biblical Critique of Secular Justice and Critical Theory [https://quarterly.gospelinlife.com/a-biblical-critique-of-secular-justice-and-critical-theory/]
- 5. Bioethics Interest Group [https://oir.nih.gov/sigs/bioethics-interest-group]
- 6. Education | Presidential Commission for the Study of ... [https://bioethicsarchive.georgetown.edu/pcsbi/education.html]
- 7. Research Guides and Class Pages: Bioethics: Theology [https://research.dom.edu/bioethics/theology]
- 8. The Dangers of Technodeterminism: Transhumanism and ... [https://www.wordonfire.org/articles/the-dangers-of-technodeterminism-transhumanism-and-a-catholic-perspective/]
- 9. The Spiritual Challenge of AI, Trans-Humanism, and ... [https://www.tikkun.org/the-spiritual-challenge-of-ai-trans-humanism-and-the-post-human-world/]
- 10. Transhumanism 2040: The Future of Human Evolution [https://www.francescatabor.com/articles/2025/5/23/transhumanism-2040-the-future-of-human-evolution]
- 11. AI and how not to become a transhumanist [https://www.theosthinktank.co.uk/comment/2025/05/28/ai-and-how-not-to-become-a-transhumanist]
- 12. Report on the Current Status of Transhumanism in Sweden ... [https://transhumanist-party.org/2025/08/24/report-status-transhumanism-sweden/]
- 13. Institute of Clinical Bioethics - Philadelphia [https://www.sju.edu/icb]
- 14. AI and Faith - by Medlir Mema [https://www.wayfaremagazine.org/p/ai-and-faith?utm_source=substack&utm_medium=email&utm_content=share&action=share]
- 15. Dignity reevaluated: A theological examination of human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5102172/]
- 16. Human Dignity in Inpatient Care: Fragments of Religious ... [https://www.mdpi.com/2077-1444/14/6/757]
- 17. Human Dignity | CBHD Site Topic Issues [https://cbhd.org/issues/human-dignity]
- 18. Vulnerability in practice: Peeling back the layers, avoiding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9886167/]
- 19. The concept of vulnerability in medical ethics and philosophy [https://peh-med.biomedcentral.com/articles/10.1186/s13010-019-0075-6]
- 20. Thinking Theologically About Bioethics Revisited [https://cbhd.org/cbhd-resources/thinking-theologically-about-bioethics-revisited]
- 21. Human dignity and biomedical ethics from a Christian ... [http://www.scielo.org.za/scielo.php?script=sci_arttext&pid=S0259-94222011000300049]
- 22. Dehumanization and mental health - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11083880/]
- 23. Rethinking dehumanization, empathy, and burnout in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10473871/]
- 24. Artificial Intelligence and the Dehumanization of Patient Care [https://www.sciencedirect.com/science/article/pii/S2949916X24000914]
- 25. Feasibility and Effectiveness of a Comprehensive Care ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9801369/]
- 26. The impact of humanising hospital care on health outcomes [https://bmcnurs.biomedcentral.com/articles/10.1186/s12912-025-03105-w]
- 27. Ethical Method in Christian Bioethics: Mapping the Terrain [https://cbhd.org/cbhd-resources/ethical-method-in-christian-bioethics-mapping-the-terrain]
- 28. Living in the Biotech Century: The First 25 Years [https://www.tiu.edu/divinity/bioethics-conference/]
- 29. Experimental philosophical bioethics and normative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8695528/]
- 30. Religious Accommodation in Bioethics and the Practice of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8022927/]
- 31. Christian Bioethics in a Secular World: In Search of Ethical ... [https://www.thepublicdiscourse.com/2025/03/97321/]
- 32. Theoretical Anthropology [https://christianresourcelibrary.com/theoretical-anthropology]
- 33. Theological Anthropology: A Review of Webster's ... [https://henrycenter.tiu.edu/2016/11/theological-anthropology-a-review-of-websters-anthropology-eschatology-and-postmodernity/]
- 34. Validity in Clinical Research [https://www.openanesthesia.org/keywords/validity-in-clinical-research/]
- 35. Data Validation in Clinical Data Management [https://www.quanticate.com/blog/data-validation-in-clinical-data-management]
- 36. Improving the Spiritual Dimension of Whole Person Care [https://pmc.ncbi.nlm.nih.gov/articles/PMC4038982/]
- 37. Religion, Spirituality, and Health: The Research and Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3671693/]
- 38. The Healing Relationship and Suffering: A Catholic Perspective [https://pmc.ncbi.nlm.nih.gov/articles/PMC12379509/]
- 39. Spiritual vs. Pastoral or Chaplaincy Care | Chaplain Support [https://www.crcna.org/chaplaincy/resources/spiritual-vs-pastoral-or-chaplaincy-care]
- 40. Pastoral Care: A New Model for Assessing the Spiritual Needs ... [https://digitalcommons.liberty.edu/doctoral/588/]
- 41. Clinical Ethics–Challenges of the Past, the Present, and ... [https://www.mdpi.com/2409-9287/10/5/113]
- 42. Christianity and AI [https://ccg.fas.harvard.edu/conference-pages/christianity-and-ai]
- 43. Religious Views on Gene Editing: AI Explores Ethical ... [https://reelmind.ai/blog/religious-views-on-gene-editing-ai-explores-ethical-debates]
- 44. Viewpoint: The Catholic Church's new guidelines on AI fail ... [https://geneticliteracyproject.org/2025/08/18/viewpoint-the-catholic-churchs-new-guidelines-on-ai-fail-to-account-for-the-overlap-of-evolution-and-technology/]
- 45. CRISPR & Ethics [https://innovativegenomics.org/crisprpedia/crispr-ethics/]
- 46. Ethics of Life and Mind in the Era of AI #50 [https://aiandfaith.org/aif-podcast/ethics-of-life-and-mind/]
- 47. Faith-Based Frameworks for AI Ethics | Programs [https://ethics.nd.edu/programs/faith-based-frameworks-for-ai-ethics/]
- 48. Video: Humanity Meets AI Symposium: Building Ethical AI [https://rpl.hds.harvard.edu/news/2025/04/18/video-humanity-meets-ai-symposium-building-ethical-ai]
- 49. Addressing Religion in Secular Healthcare: Existential ... [https://www.mdpi.com/2077-1444/13/1/34]
- 50. A Defense of Institutional Conscience Rights for Secular ... [https://pubmed.ncbi.nlm.nih.gov/41231119/]
- 51. Accommodating religion and belief in healthcare: Political ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10099616/]
- 52. Journal of Medical Ethics blog [https://blogs.bmj.com/medical-ethics/2024/06/18/interdisciplinary-collaboration-to-identify-and-address-ethical-issues-arising-from-the-development-of-irreversible-high-risk-medical-treatments/]
- 53. Top Topics [https://www.theologie-naturwissenschaften.de/en/dialogue-between-theology-and-science/editorials/top-topics]
- 54. Collaborative interdisciplinary bioethical decision making ... [https://pubmed.ncbi.nlm.nih.gov/8346049/]
- 55. Fragmented Churches in Fragmented Times [https://www.thegospelcoalition.org/blogs/trevin-wax/fragmented-churches-fragmented-times/]
- 56. Bioethics Course 2025 [https://medicineandislam.org/bioethics-course-2025/]
- 57. A Tragedy of Polarization: What Faith Teaches in the Age ... [https://www.wordonfire.org/articles/a-tragedy-of-polarization-what-faith-teaches-in-the-age-of-division/]
- 58. Spirituality and Religion in Serious Illness: Research and ... [https://bioethics.pitt.edu/event/spirituality-and-religion-serious-illness-research-and-clinical-practice]
- 59. From Fate to Choice to Fragmentation [https://oikonomianetwork.org/2023/07/from-fate-to-choice-to-fragmentation/]
- 60. Certification Program [https://www.ncbcenter.org/certification-program]
- 61. Spiritual Care - Tools and Resources - CAPC [https://www.capc.org/toolkits/spiritual-care/]
- 62. Identifying the key components of providing spiritual care in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12096602/]
- 63. Clinical pathways as a quality strategy - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK549262/]
- 64. Nurses' Propensity for Spiritual Care: A Nationwide Study ... [https://www.sigmarepository.org/convention/2025/presentations_2025/11/]
- 65. Spiritual care competency and spiritual sensitivity among ... [https://bmcnurs.biomedcentral.com/articles/10.1186/s12912-025-03549-0]
- 66. Reflections on a Principal of Research Ethics - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12614633/]
- 67. The Rule of Double Effect | Bioethics [https://bioethics.hms.harvard.edu/journal/rule-double-effect]
- 68. A Comparative Discourse on Christian and Secular ... [http://www.scielo.org.za/scielo.php?script=sci_arttext&pid=S0256-95072017000100004]
- 69. How Do Theological and Secular Ethics Relate and ... [https://www.mdpi.com/2077-1444/13/10/971]
- 70. Principles of Bioethics for Christian Physicians: Autonomy and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11298101/]
- 71. Different Visions of Autonomy [https://www.ncbcenter.org/messages-from-presidents/joy-clb78]
- 72. Do Spirituality and Medicine Go Together? | Bioethics [https://bioethics.hms.harvard.edu/journal/spirituality-medicine]
- 73. Good Without God: Bioethics and the Sacred - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4577544/]
- 74. Medical Ethics and the Faith Factor: The Endangered Right ... [https://www.cslewis.org/journal/medical-ethics-and-the-faith-factor-the-endangered-right-of-conscience/view-all/]
- 75. Acceptable objectives of empirical research in bioethics [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-022-00845-1]
- 76. A systematic review of empirical bioethics methodologies [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-015-0010-3]
- 77. The Role of Empirical Research in Bioethics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2826359/]
- 78. Spiritual But Not Religious: Human Experiences Integral to ... [https://www.thehastingscenter.org/spiritual-but-not-religious-human-experiences-integral-to-bioethics/]
- 79. Researchers' Views on Doing Empirical Bioethics [https://link.springer.com/article/10.1007/s11673-023-10286-z]
- 80. How to tackle the conundrum of quality appraisal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6857152/]
- 81. Categorizing Empirical Research in Bioethics: Why Count ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3098471/]
- 82. Systematic reviews of empirical literature on bioethical topics [https://pmc.ncbi.nlm.nih.gov/articles/PMC7323745/]
- 83. Spiritual Care in Palliative Care: A Systematic Review of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6409788/]
- 84. Breaking Boundaries: Reframing Clinical Ethics ... [https://www.thehastingscenter.org/breaking-boundaries-reframing-clinical-ethics-discussions-of-health-care-for-incarcerated-patients/]
- 85. The influence of spirituality on decision-making in palliative ... [https://bmcpalliatcare.biomedcentral.com/articles/10.1186/s12904-020-0525-3]
- 86. Breaking down barriers to mental healthcare access in prison [https://pmc.ncbi.nlm.nih.gov/articles/PMC11025238/]
- 87. Religious Experiences of Older People Receiving ... [https://www.mdpi.com/2077-1444/11/7/336]