From Principles to Practice: A Practical Guide to Implementing the Belmont Report in IRB Protocols
This article provides researchers, scientists, and drug development professionals with a comprehensive framework for applying the Belmont Report's ethical principles—Respect for Persons, Beneficence, and Justice—to Institutional Review Board (IRB) protocols.
From Principles to Practice: A Practical Guide to Implementing the Belmont Report in IRB Protocols
Abstract
This article provides researchers, scientists, and drug development professionals with a comprehensive framework for applying the Belmont Report's ethical principles—Respect for Persons, Beneficence, and Justice—to Institutional Review Board (IRB) protocols. It covers the historical foundation of these principles, details their methodological application in study design and consent processes, offers solutions for common challenges in risk assessment and vulnerable populations, and validates the approach by comparing it with other ethical codes like the Nuremberg Code and Declaration of Helsinki. The guide aims to equip professionals with the knowledge to develop ethically sound, compliant, and robust research protocols that prioritize human subject protection.
The Bedrock of Research Ethics: Understanding the Belmont Report's Core Principles
The implementation of the Belmont Report's ethical principles in modern Institutional Review Board (IRB) protocols cannot be fully understood without examining the critical historical milestones that necessitated their development. The period from the post-World War II era to the 1970s witnessed a profound transformation in the ethics of human subjects research, driven primarily by the exposure of egregious ethical violations in both international and domestic research settings. This document traces the trajectory from the Nuremberg Code, developed in response to Nazi war crimes, through the Tuskegee Syphilis Study, a domestic violation that shocked the American public, to the legislative response of the National Research Act of 1974. This historical context provides the essential foundation for appreciating the moral imperative behind the Belmont Report's principles and their practical application in contemporary research oversight [1] [2].
Historical Ethical Violations and Their Principles
The Nuremberg Code (1947)
Origin and Context
The Nuremberg Code emerged from the 1947 "Doctors' Trial" of Nazi physicians who conducted brutal and deadly experiments on concentration camp prisoners without their consent [3] [4]. During the trial, the defendants argued that no clear international laws differentiated between legal and illegal human experimentation, highlighting a critical regulatory gap [3]. The American judges presiding over the case subsequently articulated a 10-point statement to define the limits of permissible medical experimentation, which became known as the Nuremberg Code [4]. While initially created in response to these specific war crimes, the Code's significance later expanded to provide ethical guidance for human experimentation in broader contexts [3].
Key Principles and Directives
The Nuremberg Code established voluntary consent as its foundational and absolute requirement. This consent must be informed, comprehending, and freely given without any element of coercion [3]. The Code further outlined that experiments should be designed to yield fruitful results for the good of society, based on prior animal testing and knowledge of the disease, and conducted so as to avoid all unnecessary suffering [3] [2]. It introduced the critical concept of a favorable risk-benefit assessment, stating that the degree of risk should never exceed the humanitarian importance of the problem to be solved [3]. Finally, it affirmed the subject's right to terminate participation and the scientist's duty to end the experiment if continuation is likely to result in injury, disability, or death [4].
Table 1: Core Principles of the Nuremberg Code
| Principle Number | Ethical Focus | Key Requirement |
|---|---|---|
| 1 | Respect for Persons | Voluntary, informed, and comprehending consent is absolutely essential. |
| 2-3 | Beneficence | The experiment must yield socially valuable results, justified by prior knowledge. |
| 4-6 | Risk-Benefit Assessment | Risks must be minimized and proportionate to the humanitarian importance. |
| 9-10 | Subject and Researcher Autonomy | The subject may end participation; the scientist must terminate if risks escalate. |
The U.S. Public Health Service Untreated Syphilis Study at Tuskegee (1932-1972)
Study Design and Ethical Failures
The U.S. Public Health Service (USPHS) Untreated Syphilis Study at Tuskegee was a 40-year longitudinal study that began in 1932 with the stated aim of observing the natural history of untreated syphilis in 399 African American men with the disease and 201 without it [5] [6]. The study was fundamentally unethical from its inception. Researchers did not collect informed consent from participants, who were misled into believing they were receiving treatment for "bad blood," a local term encompassing various ailments [5] [6]. Most egregiously, researchers actively withheld effective treatment even after penicillin became the standard cure for syphilis in 1947 [5] [6]. The study continued until 1972 when it was terminated after public exposure by a news report [5].
Impact and Legacy
The Tuskegee study resulted in severe harm to its participants; by the end, 28 men had died directly from syphilis, 100 from related complications, at least 40 spouses had been infected, and the disease had been passed to 19 children at birth [6]. The subsequent public outrage led to Congressional hearings and, in 1974, a $10 million out-of-court settlement for the participants and their heirs [5] [6]. The study’s legacy is a profound and persistent mistrust of public health officials and medical research within African American communities and other marginalized groups [6]. It stands as a stark American example of the failure to adhere to the Nuremberg Code's principles, particularly regarding justice in the selection of subjects, as a vulnerable population was exploited for research [2].
Table 2: Tuskegee Syphilis Study Timeline and Consequences
| Year | Event | Consequence |
|---|---|---|
| 1932 | Study begins | 600 African American men enrolled without informed consent. |
| 1947 | Penicillin becomes standard treatment | Researchers deliberately withhold treatment to continue observation. |
| 1972 | Associated Press exposes study | Public outrage forces the study to end. |
| 1973 | Congressional Hearings | Scrutiny of unethical research practices. |
| 1974 | Out-of-court settlement | $10 million distributed to participants and heirs. |
| 1997 | Presidential Apology | President Bill Clinton formally apologizes on behalf of the U.S. government. |
The Regulatory Response: National Research Act and the Birth of the Belmont Report
The National Research Act of 1974
The National Research Act (NRA) was signed into law by President Richard Nixon on July 12, 1974, as a direct legislative response to the public outcry over the Tuskegee Syphilis Study [7] [2]. The Act was designed to address glaring deficiencies in the oversight of research involving human subjects. Its primary provision was the creation of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research [7]. This Commission was tasked with the critical mission of identifying comprehensive ethical principles and developing guidelines for the conduct of human subjects research [1].
The Belmont Report: From History to Application
The work of the National Commission culminated in 1979 with the publication of the Belmont Report [8]. This report synthesized the lessons from past ethical failures into a framework of three core principles to guide the ethical conduct of research:
- Respect for Persons: This principle acknowledges the autonomy of individuals and requires that they be provided the opportunity to make informed choices. It also mandates protection for persons with diminished autonomy [8]. This addresses the failures of both the Nazi experiments and Tuskegee by making informed consent a central requirement.
- Beneficence: This principle extends beyond "do no harm" to an obligation to maximize possible benefits and minimize possible harms [8] [2]. It requires a systematic assessment of risks and benefits, directly responding to the unnecessary suffering and death permitted in prior unethical studies.
- Justice: This principle requires the fair distribution of the burdens and benefits of research [8] [2]. It specifically guards against the exploitation of vulnerable populations, a direct ethical lesson from Tuskegee where a disadvantaged group bore all the risks.
The Belmont Report also operationalized these principles by outlining their applications: Informed Consent (from Respect for Persons), Assessment of Risks and Benefits (from Beneficence), and Selection of Subjects (from Justice) [1].
Implementation Framework: Translating History into IRB Protocol
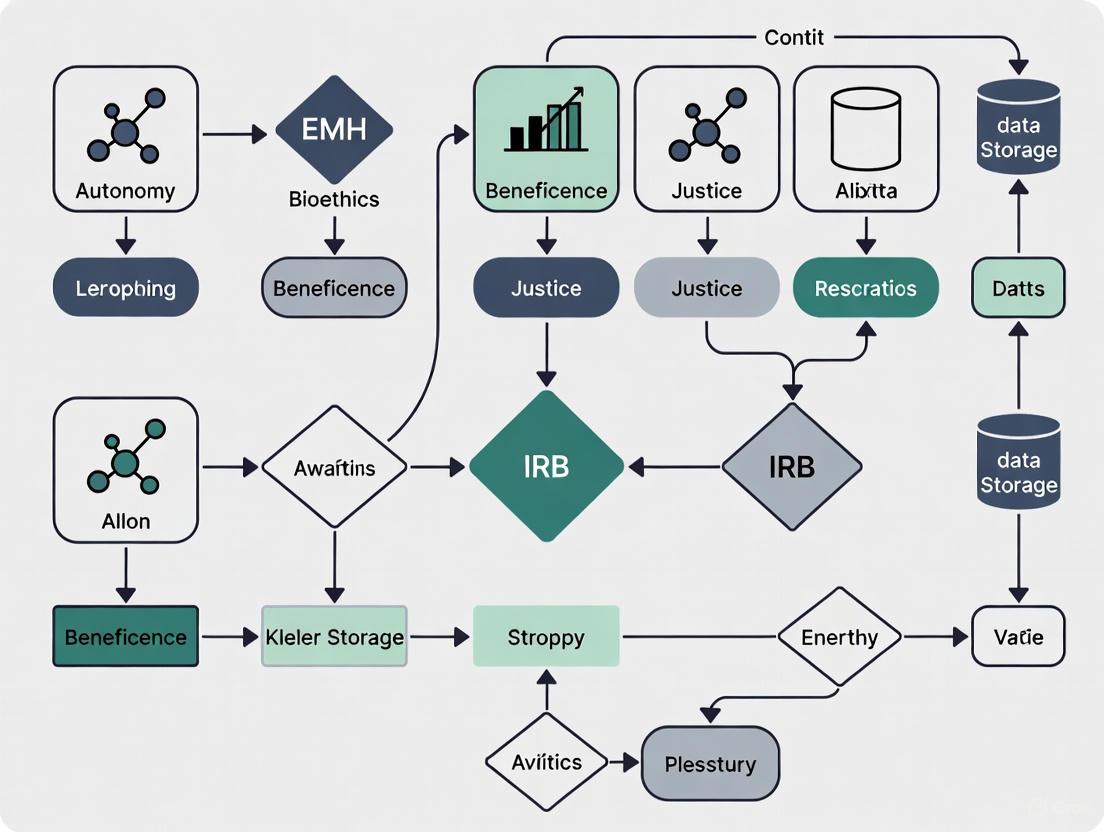
The following diagrams and tools illustrate how the historical lessons and ethical principles are systematically integrated into modern research oversight.
Logical Workflow: From Ethical Violations to Modern IRB Application
IRB Review Protocol: Operationalizing the Belmont Report
The Institutional Review Board (IRB) is the practical embodiment of the regulations stemming from the National Research Act and the ethical framework of the Belmont Report [9] [2]. An IRB is an appropriately constituted group formally designated to review and monitor biomedical research to protect the rights and welfare of human subjects [9]. The following protocol details the application of the Belmont principles during IRB review.
Table 3: IRB Review Checklist Based on Belmont Report Principles
| Belmont Principle | Application | IRB Review Questions | Historical Context Link |
|---|---|---|---|
| Respect for Persons | Informed Consent | - Is the consent process voluntary and free from coercion?- Is the information complete and comprehensible?- Are provisions made for vulnerable populations? | Addresses lack of consent in Nuremberg and Tuskegee. |
| Beneficence | Risk-Benefit Assessment | - Are risks minimized?- Are risks reasonable in relation to anticipated benefits?- Is data safety monitoring planned? | Responds to unnecessary harm in Nazi experiments and Tuskegee. |
| Justice | Subject Selection | - Are selection criteria equitable?- Are vulnerable populations targeted only for compelling scientific reasons?- Are the populations bearing the risks also likely to benefit from the research? | Counters exploitation of prisoners and African American men. |
The Scientist's Toolkit: Essential Reagents for Ethical Research
This toolkit outlines the essential components, derived from historical lessons, that every researcher must utilize to conduct ethical human subjects research.
Table 4: Research Reagent Solutions for Ethical Conduct
| Tool/Reagent | Function in Ethical Research | Historical Justification |
|---|---|---|
| IRB-Approved Protocol | Serves as the formal authorization to proceed with research, confirming ethical and regulatory compliance. | Mandated by the National Research Act of 1974 in response to Tuskegee. |
| Informed Consent Document | Provides the mechanism for ensuring participants understand the research and voluntarily agree to participate. | A direct response to the fundamental violation of the Nuremberg Code and Tuskegee Study. |
| Data Safety Monitoring Plan (DSMP) | Outlines procedures for ongoing review of data to ensure participant safety and study integrity. | Embodies the beneficence principle, preventing unnecessary harm as seen in past unethical studies. |
| Vulnerable Population Safeguards | Additional protective procedures for participants with diminished autonomy (e.g., children, prisoners). | Addresses historical exploitation of vulnerable groups in Willowbrook and Tuskegee. |
| Certificate of Confidentiality | Protects identifiable research information from forced disclosure to entities like courts or employers. | Upholds the principle of Respect for Persons by protecting participant privacy. |
The path from the Nuremberg Code and the Tuskegee Syphilis Study to the National Research Act of 1974 and the Belmont Report represents a necessary evolution in the ethical consciousness of the scientific community. These historical events are not mere anecdotes but the foundational pillars upon which modern human research protections are built. The Belmont Report's principles of Respect for Persons, Beneficence, and Justice provide the indispensable ethical compass, while the IRB system, created by the National Research Act, serves as the enforcing mechanism. For today's researchers and drug development professionals, a deep understanding of this history is not optional—it is a professional obligation. It ensures that the grave errors of the past inform a more ethical and responsible future for human subjects research.
The Belmont Report, formally published in 1979, established a foundational framework for ethical research involving human subjects in the United States [10]. It was created by the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research in direct response to egregious ethical violations in historical studies, such as the Tuskegee Syphilis Study [2]. The report articulates three fundamental ethical principles—Respect for Persons, Beneficence, and Justice—which serve as the ethical compass for designing, reviewing, and conducting research [8] [11]. These principles are not merely theoretical concepts; they provide the underlying moral foundation for federal regulations, including the Common Rule (45 CFR 46), and form the core of the Institutional Review Board (IRB) evaluation process [11] [2]. This document provides detailed application notes and protocols for researchers, scientists, and drug development professionals to effectively implement these pillars within their IRB protocols and research practices.
The Historical Context and Creation of the Belmont Report
The path to the Belmont Report was paved by a history of ethical transgressions in research. Key documents like the Nuremberg Code (1947) and the Declaration of Helsinki (1964) were early attempts to establish international ethical standards [2]. However, events like the Willowbrook State School study, where children with mental disabilities were deliberately infected with hepatitis, and the Brooklyn Jewish Chronic Disease Hospital study, which involved injecting cancer cells into elderly patients without consent, highlighted the persistent vulnerability of certain populations [2]. The public revelation of the Tuskegee Syphilis Study, in which hundreds of African-American men were left untreated for syphilis for decades without their knowledge, became the catalyst for congressional action [2].
In 1974, the U.S. Congress passed the National Research Act, which led to the creation of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research [10]. This commission was tasked with identifying the comprehensive ethical principles that should govern human subjects research. The result of their work was the Belmont Report, a concise document that has endured as the cornerstone of research ethics for over four decades [1] [11].
Deconstructing the Ethical Pillars
The three principles outlined in the Belmont Report are designed to be broad and adaptable, providing a framework for analyzing the ethical considerations of research. The following table summarizes their core components and regulatory translations.
Table 1: The Three Ethical Principles of the Belmont Report
| Ethical Principle | Core Ethical Conviction | Primary Regulatory Applications |
|---|---|---|
| Respect for Persons | Individuals should be treated as autonomous agents; persons with diminished autonomy are entitled to protection [8]. | Informed Consent; Respect for Privacy [8] [11]. |
| Beneficence | Do not harm; maximize possible benefits and minimize possible harms [8]. | Assessment of Risks and Benefits; Favorable Risk-Benefit Ratio [12] [8]. |
| Justice | The benefits and burdens of research must be distributed fairly [8]. | Fair Subject Selection; Equitable Recruitment [12] [10]. |
Pillar 1: Respect for Persons
The principle of Respect for Persons incorporates two distinct ethical convictions: first, that individuals should be treated as autonomous agents, and second, that persons with diminished autonomy are entitled to additional protections [8].
Application to Informed Consent: The primary practical application of this principle is the process of informed consent [8] [11]. This is not merely the act of signing a form, but a dynamic process of information exchange. To be valid, consent must be voluntary, competent, and informed [8]. Researchers must ensure that prospective participants make their own decision about whether to join a study based on a clear understanding of what it involves [12]. The Belmont Report specifies that subjects must be provided with all the information they need to make that decision, including the research procedures, their purposes, any potential risks and anticipated benefits, and alternative procedures [8]. They must also be given the opportunity to ask questions and must understand that they can withdraw from the research at any time without penalty [12] [8].
Protocol for Research with Vulnerable Populations: The second moral requirement of this principle obliges researchers to protect individuals with diminished autonomy. These can include children, prisoners, individuals with intellectual or cognitive disabilities, or educationally or economically disadvantaged persons [11] [2]. The protocol for such groups involves:
- Justification for Inclusion: The research protocol must provide a strong scientific justification for including these populations. It is unethical to select them merely for convenience [12] [2].
- Proxy Consent: For those who cannot provide consent for themselves (e.g., young children or adults with severe dementia), permission must be obtained from a legally authorized representative [11] [2].
- Assent: Even when proxy consent is obtained, the prospective subject's affirmative agreement (assent) should be sought to the extent they are capable. A child's dissent, for example, should generally be respected, though regulations may allow a parent's permission to override it in certain therapeutic contexts [11].
Pillar 2: Beneficence
The principle of Beneficence extends beyond simply "do no harm" to an affirmative obligation to secure the well-being of research participants [8]. This is expressed through two complementary rules: "(1) do not harm and (2) maximize possible benefits and minimize possible harms" [8].
Application to Systematic Risk-Benefit Assessment: This principle requires a thorough and systematic analysis of the risks and benefits associated with the research [12] [10]. Researchers must scrutinize the study design to identify all foreseeable risks, which can be physical, psychological, social, or economic [12]. Similarly, potential benefits must be identified, which may accrue to the individual subject or to society in the form of generalized knowledge [8]. The IRB's role is to determine that the risks have been minimized to the greatest extent possible and that the remaining risks are justified by the anticipated benefits [12] [2].
Protocol for Ongoing Risk Monitoring: The ethical obligation of beneficence does not end after the initial IRB approval. It requires continuous vigilance throughout the study. The research protocol must include:
- Data and Safety Monitoring Plan (DSMP): A clear plan for monitoring collected data to ensure participant safety, especially in clinical trials. This may involve an independent Data and Safety Monitoring Board (DSMB) for higher-risk studies.
- Procedures for Adverse Events: Defined procedures for identifying, documenting, reporting, and managing any adverse events or unexpected effects that participants experience [12].
- Dissemination of New Information: A commitment to inform participants of any new information that emerges during the course of the research that might change their assessment of the risks and benefits of participating [12]. If their welfare is compromised, the protocol must ensure appropriate treatment and, when necessary, removal from the study [12].
Pillar 3: Justice
The principle of Justice demands fairness in the distribution of the burdens and benefits of research [8] [10]. It addresses the ethical concern that no single group or class of individuals should be systematically selected to bear the risks of research simply because of their easy availability, compromised position, or social standing, while other, more privileged groups reap the benefits [8].
Application to Fair Subject Selection: The primary application of justice is in the recruitment and selection of research subjects [12] [11]. The scientific goals of the study must be the primary basis for recruiting participants, not vulnerability, privilege, or other unrelated factors [12]. Historically, injustices have occurred when dependent populations (e.g., prisoners, racial minorities, institutionalized patients) were selected for risky research because they were convenient or easy to manipulate [2]. Conversely, justice also requires that specific groups (e.g., women or children) should not be excluded from the opportunity to participate in and benefit from research without a sound scientific reason [12].
Protocol for Equitable Recruitment and Inclusion: To uphold justice, a research protocol must demonstrate:
- Inclusion and Exclusion Justification: All criteria for including or excluding potential subjects must be directly related to the research question and not based on race, gender, economic status, or culture alone [12] [10].
- Vulnerable Population Safeguards: If the research includes vulnerable groups, the protocol must detail the additional safeguards in place to protect their rights and welfare [2].
- Benefit Sharing: The protocol should consider whether the populations that are assuming the risks of the research are in a position to enjoy its benefits. Research on a disease that predominantly affects a specific group should, if successful, be made available to that group [12] [10].
The Researcher's Toolkit: Operationalizing the Belmont Principles
Conceptual Framework and Workflow Diagram
The following diagram illustrates the logical relationship between the Belmont Report's ethical principles and their practical applications in the IRB review process, providing a workflow for researchers.
Belmont Principles to IRB Workflow
Essential Materials and Reagent Solutions for Ethical Research
While ethical research does not rely on physical reagents, it requires a set of conceptual tools and documented plans. The following table details these essential "research reagents" for implementing the Belmont principles.
Table 2: Essential Protocol Components for Ethical Research
| Item | Function & Purpose | Belmont Principle Addressed |
|---|---|---|
| Informed Consent Document (ICD) | A comprehensive, understandable document that provides all key information about the study, allowing a potential subject to make a voluntary, informed decision [13]. | Respect for Persons |
| Institutional Review Board (IRB) Protocol | The formal application submitted for ethical review. It details the study's rationale, methodology, and, crucially, plans for subject protection [2]. | All Three Principles |
| Data and Safety Monitoring Plan (DSMP) | A proactive plan for monitoring participant safety and data integrity throughout the trial. It may specify stopping rules if risks outweigh benefits [12]. | Beneficence |
| Recruitment Materials & Scripts | All advertisements, flyers, and verbal scripts used to enroll participants. These must be fair, not coercive, and approved by the IRB [12] [13]. | Justice, Respect for Persons |
| Data Anonymization/Pseudonymization Protocol | A method for protecting participant privacy by removing or replacing identifying information with codes, safeguarding confidentiality [13]. | Respect for Persons |
| Adverse Event Reporting Plan | A formal procedure for identifying, documenting, reporting to the IRB, and managing any unplanned or harmful events experienced by a participant [12]. | Beneficence |
Advanced Applications and Protocol Scenarios
Ethical Challenges in Dissemination & Implementation Research
Emerging research fields like Dissemination and Implementation (D&I) research present unique ethical challenges that require careful application of the Belmont principles [14]. These studies, which aim to integrate evidence-based interventions into routine care, often blur the lines between research and clinical practice. Key ethical questions include:
- Is it Human Subjects Research? Determining whether a D&I study qualifies as human subjects research can be complex, as some projects may be classified as quality improvement and exempt from IRB oversight, even when collecting patient-level data [14].
- Who is the Research Participant? In multilevel interventions targeting patients, clinicians, and health systems, it can be challenging to identify all research participants and determine from whom informed consent is required [14].
- Clinical Equipoise: It can be difficult to justify equipoise (genuine uncertainty about the superior intervention) in D&I studies because the intervention itself is already evidence-based. The ethical uncertainty often lies in the implementation strategy, not the intervention's efficacy [14].
Protocol Guidance: Researchers should engage with their IRB early in the design phase of D&I studies. The protocol should explicitly define all groups interacting with the research, justify the level of risk for each group, and detail a tailored consent process (which may include cluster consent or waivers of consent) that is appropriate for the study design and context [14].
Protocol: Resolving Conflicts Between Ethical Principles
The Belmont Principles can sometimes conflict with one another, requiring careful balancing by both the researcher and the IRB [11].
Scenario: Pediatric Research In research involving children, the principle of Respect for Persons (honoring the child's dissent) may conflict with Beneficence (allowing a parent to consent to a potentially beneficial therapy) or Justice (conducting research to gain knowledge for other children with the same condition) [11].
Resolution Protocol:
- Prioritize Consensus: The researcher's first duty is to facilitate a consensus between the child and parent/guardian, respecting the child's developing autonomy [11].
- Risk-Benefit Analysis:
- If the research is greater than minimal risk but offers direct benefit to the child, the IRB may allow the parent's permission to override the child's dissent to obtain that benefit (favoring Beneficence) [11].
- If the research is greater than minimal risk with no direct benefit (only generalizable knowledge for others), the IRB will generally require a higher level of protection, such as permission from both parents, to ensure the risks are reasonable in relation to the knowledge gained (favoring Justice and Beneficence over individual Respect for Persons in this specific context) [11].
The three pillars of the Belmont Report—Respect for Persons, Beneficence, and Justice—provide a durable and essential framework for ensuring that the pursuit of scientific knowledge does not come at the cost of human rights or dignity. For researchers, scientists, and drug development professionals, these principles are not abstract ideals but practical guides that must be meticulously operationalized in every aspect of a study, from its initial design and IRB protocol to its final execution and dissemination of results. By systematically applying these principles through robust informed consent procedures, rigorous risk-benefit analyses, and equitable subject selection, the research community upholds its ethical integrity, maintains public trust, and ensures that scientific progress is made in a morally defensible manner.
The transition from the Belmont Report's ethical principles to the codified requirements of the Common Rule and FDA regulations represents a critical evolution in human research protections. Published in 1979 by the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research, the Belmont Report established three fundamental ethical principles: respect for persons, beneficence, and justice [8]. This document emerged in direct response to ethical violations in historical studies, most notably the Tuskegee Syphilis Study, where hundreds of African-American men were left untreated for syphilis without their informed consent [2] [15]. The Belmont Report provided the ethical foundation, but required regulatory force to ensure consistent application across the research landscape.
The regulatory frameworks that followed—the Federal Policy for the Protection of Human Subjects (Common Rule) and the FDA's human subject regulations—operationalized these ethical principles into specific requirements for researchers, sponsors, and institutions [16] [17]. The Common Rule was first published in 1991 and has been adopted by 15 federal departments and agencies, creating a unified standard for publicly funded research [16]. Simultaneously, the FDA developed its regulations under 21 CFR Parts 50 and 56, governing clinical investigations for products under its jurisdiction [16] [17]. This application note examines how each Belmont principle was translated into specific regulatory requirements and provides practical guidance for implementation within modern Institutional Review Board (IRB) protocols.
Operationalizing the Belmont Principles
Principle 1: Respect for Persons
The principle of respect for persons incorporates two ethical convictions: individuals should be treated as autonomous agents, and persons with diminished autonomy are entitled to protection [8]. This principle recognizes the personal dignity and autonomy of individuals and requires special protection for those with diminished autonomy [18].
The regulatory frameworks translate this principle primarily through informed consent requirements and special protections for vulnerable populations. The Common Rule and FDA regulations mandate that investigators obtain legally effective informed consent from subjects or their legally authorized representatives before including them in research, with few exceptions [16] [17]. This process must include eight specific elements of information, ensuring subjects enter research voluntarily and with adequate information [8]. For vulnerable populations like children, prisoners, and individuals with diminished decision-making capacity, additional safeguards are required to protect their rights and welfare [8] [2].
Table: Translation of Respect for Persons into Regulatory Requirements
| Ethical Component | Regulatory Manifestation | Key Regulatory Citations |
|---|---|---|
| Voluntary Participation | Informed consent as a process without coercion | 45 CFR 46.116; 21 CFR 50.20 |
| Adequate Information | Required elements of informed consent | 45 CFR 46.116(a); 21 CFR 50.25(a) |
| Comprehension | Consent information in understandable language | 45 CFR 46.116(a)(4); 21 CFR 50.20 |
| Special Populations | Additional protections for vulnerable groups | 45 CFR 46 Subparts B, C, D; 21 CFR 50.55-56 |
Principle 2: Beneficence
The principle of beneficence obligates researchers to secure the well-being of participants by maximizing possible benefits and minimizing possible harms [8] [2]. This principle extends beyond the medical maxim of "do no harm" to include an obligation to promote the welfare of research participants through a careful risk-benefit analysis [8].
Regulations operationalize beneficence through systematic risk assessment and requiring favorable risk-benefit ratios. IRBs must determine that risks to subjects are minimized by using procedures that are consistent with sound research design and that do not unnecessarily expose subjects to risk [19] [20]. Additionally, IRBs must assess whether risks are reasonable in relation to anticipated benefits, if any, to subjects and the importance of the knowledge that may reasonably be expected to result [2]. This systematic assessment ensures that the research design adequately protects participants' welfare.
Table: Beneficence Implementation in Research Oversight
| Ethical Obligation | Regulatory Implementation | IRB Review Considerations |
|---|---|---|
| Assess Risks | Systematic review of all potential harms | Physical, psychological, social, economic risks |
| Maximize Benefits | Design optimization to enhance benefits | Direct benefits to subjects, societal benefits |
| Risk-Benefit Analysis | Justifiable relationship between risks and benefits | Favorable risk-benefit ratio for acceptable research |
| Ongoing Monitoring | Continuing review of approved research | Annual review, adverse event reporting |
Principle 3: Justice
The principle of justice requires that the benefits and burdens of research be distributed fairly [18] [2]. This principle addresses concerns about exploiting vulnerable populations or selectively enrolling subjects based on convenience rather than scientific reasons [8].
The Common Rule and FDA regulations implement justice primarily through equitable subject selection [19]. IRBs must ensure that subject selection is equitable by considering the purposes of the research and the setting in which it will be conducted [19]. The regulations specifically prohibit systematically selecting subjects simply because of their easy availability, compromised position, or susceptibility to manipulation [8]. Special populations such as prisoners, children, and other vulnerable groups receive additional protections to prevent exploitation [17].
Regulatory Framework and Implementation
The Common Rule: Structure and Revisions
The Common Rule, formally known as the Federal Policy for the Protection of Human Subjects, established uniform standards for human subjects research across federal departments and agencies [16]. Originally promulgated in 1991, the Common Rule underwent significant revisions that took effect in 2018 to address changes in the research landscape, including the growth in clinical trials, use of electronic health data, and sophisticated analysis techniques [16]. These revisions modernized the regulations to reduce burden, delay, and ambiguity while maintaining core ethical protections [16].
Key provisions of the revised Common Rule include:
- Streamlined continuing review: Elimination of annual continuing review requirements for certain minimal risk research [16]
- Expanded exemptions: New categories of exempt research based on minimal risk provisions [16]
- Single IRB review: Requirement for use of a single IRB for multi-institutional research in the United States [16] [19]
- Enhanced informed consent: New "key elements" section and rearranged content to facilitate understanding [16]
The revised Common Rule also introduced three "burden-reducing provisions" that institutions could implement early, including the revised definition of "research," allowance for no annual continuing review of certain categories, and elimination of the requirement for IRBs to review grant applications [16].
FDA Human Subject Regulations
The Food and Drug Administration regulations provide parallel but distinct oversight for clinical investigations involving products regulated by the FDA, including drugs, biological products, medical devices, and electronic products [16] [17]. While the FDA regulations share common ethical foundations with the Common Rule, there are important differences that researchers must recognize.
The FDA framework includes:
- Informed consent requirements (21 CFR Part 50): Standards for obtaining and documenting informed consent [17]
- IRB regulations (21 CFR Part 56): Standards for IRB composition, operation, and responsibility for reviewing FDA-regulated research [17]
- Investigational requirements (21 CFR Parts 312 and 812): Procedures governing use of investigational new drugs and devices [17]
Notable differences between FDA and Common Rule regulations include qualifications for exemptions and requirements for waivers of consent [16]. The 21st Century Cures Act mandates harmonization between Common Rule and FDA human subjects regulations, signaling ongoing alignment between these frameworks [16].
Practical Application: IRB Protocols and Procedures
IRB Composition and Function
The Institutional Review Board serves as the primary mechanism for implementing Belmont principles and regulatory requirements at the institutional level [21] [19]. Federal regulations mandate specific composition requirements to ensure comprehensive review capability:
- Minimum of five members with diverse backgrounds [19]
- Scientific and non-scientific representation, including at least one member with scientific and one with non-scientific background [19] [2]
- Community representation through at least one member not affiliated with the institution [19]
- Diversity in gender, race, cultural background, and sensitivity to community attitudes [19]
IRBs maintain written procedures for initial and continuing review, reporting of unanticipated problems, and ensuring prompt reporting of serious or continuing noncompliance [19] [20]. The IRB holds authority to approve, require modifications to, or disapprove research activities based on regulatory and ethical criteria [19].
Levels of IRB Review
Based on risk assessment and regulatory categories, IRBs conduct three levels of review:
- Exempt Review: For specific categories of minimal risk research involving no more than the level of risk encountered in everyday life [19] [15]. Exempt research requires initial IRB determination but not ongoing oversight.
- Expedited Review: For minimal risk research falling within nine specific categories defined by federal regulations [19]. A designated IRB reviewer rather than the full board conducts the review.
- Full Board Review: Required for research greater than minimal risk and studies involving vulnerable populations [19]. These studies require review by a fully convened IRB quorum and annual continuing review.
Table: IRB Review Categories and Criteria
| Review Level | Risk Level | Examples | Consent Requirements |
|---|---|---|---|
| Exempt | No more than minimal risk | Retrospective data analysis, educational tests | Often waived for secondary data |
| Expedited | Minimal risk | Prospective data collection, blood sampling | Required unless waiver granted |
| Full Board | Greater than minimal risk | Drug trials, invasive procedures, vulnerable populations | Comprehensive informed consent |
Documentation and Reporting Requirements
Effective implementation of Belmont principles requires robust documentation and reporting systems. Key requirements include:
- Unanticipated Problem Reporting: Investigators must promptly report all unanticipated problems involving risks to subjects or others [20]. These include any incident, experience, or outcome that is unexpected, related or possibly related to research participation, and suggests greater risk of harm than previously known [20].
- Protocol Deviations: Departures from the IRB-approved protocol must be reported, with major deviations (those impacting subject safety or risk-benefit ratio) reported promptly, and minor deviations summarized at continuing review [20].
- Informed Consent Documentation: IRBs must review and approve all informed consent documents to ensure they contain required elements in understandable language [19] [15].
- Continuing Review: Most research requires at least annual review by the IRB, though the revised Common Rule eliminated this requirement for certain minimal risk categories [16] [19].
Research Reagent Solutions: Essential Materials for Ethical Research Implementation
Table: Essential Materials for IRB Protocol Development and Ethical Review
| Research Reagent | Function/Application | Implementation Guidance |
|---|---|---|
| Belmont Report Framework | Ethical foundation for protocol design | Apply three principles systematically to all study aspects |
| Informed Consent Templates | Standardized consent documentation | Customize for specific population and risk profile |
| Vulnerability Assessment Tool | Identification of special population needs | Implement additional safeguards for vulnerable groups |
| Risk-Benefit Worksheet | Systematic evaluation of study risks/benefits | Document minimization strategies and benefit maximization |
| Federal Regulations (45 CFR 46) | Common Rule compliance reference | Apply to all federally funded human subjects research |
| FDA Regulations (21 CFR 50, 56) | Regulatory standards for clinical investigations | Required for drug, device, and product research |
Experimental Protocol: Implementing Belmont Principles in IRB Submissions
Protocol Title: Systematic Integration of Ethical Principles in Human Subjects Research
Purpose: This protocol provides a standardized methodology for integrating Belmont Report principles into human research protocols, ensuring consistent application of ethical standards and regulatory compliance.
Background: The Belmont Report establishes three fundamental principles—respect for persons, beneficence, and justice—that form the ethical foundation for human subjects protections in the United States [8] [2]. Federal regulations (Common Rule and FDA) operationalize these principles, but researchers must actively implement them in study design and conduct.
Materials Required:
- Research protocol document
- Informed consent templates
- Vulnerability assessment checklist
- Risk-benefit analysis worksheet
- Regulatory reference materials (45 CFR 46, 21 CFR 50/56)
Procedure:
Step 1: Respect for Persons Implementation
- Develop comprehensive informed consent process with all required elements [8] [17]
- Ensure consent information is presented in language understandable to prospective subjects
- Implement additional protections for persons with diminished autonomy (children, cognitive impairment, prisoners)
- Establish procedures for ongoing consent throughout research participation
Step 2: Beneficence Implementation
- Conduct systematic risk assessment identifying all potential harms (physical, psychological, social, economic)
- Design study to minimize risks through sound methodology and safety monitoring
- Maximize potential benefits through appropriate subject selection and research design
- Document favorable risk-benefit ratio with specific justification
Step 3: Justice Implementation
- Justify subject selection criteria based on scientific objectives, not convenience or vulnerability
- Ensure equitable distribution of research burdens and benefits across participant groups
- Implement additional safeguards for vulnerable populations routinely involved in research
- Assess and address potential for exploitation or undue influence
Step 4: IRB Integration and Documentation
- Submit complete research protocol including ethical integration documentation
- Respond to IRB requests for modification or clarification
- Implement approved protocol with fidelity to ethical commitments
- Report unanticipated problems or protocol deviations promptly
Timeline: The ethical integration process should begin during initial study design and continue through protocol development, IRB review, study implementation, and final reporting.
Quality Control: Implement ongoing monitoring of ethical compliance through regular protocol audits, consent process verification, and adverse event surveillance.
The bridge from the Belmont Report to contemporary regulations represents a dynamic system that continues to evolve with changing research paradigms. Recent developments, including the Revised Common Rule (2018) and emerging guidelines for pervasive data research (2024), demonstrate the ongoing adaptation of ethical principles to new research contexts [16] [22]. The single IRB mandate for multi-site studies and provisions for limited IRB review of certain exempt research reflect continuing efforts to streamline oversight while maintaining ethical rigor [19].
For researchers and IRB professionals, understanding this foundational relationship between ethical principles and regulatory requirements enables more effective protocol design and ethical review. By systematically applying the Belmont principles throughout the research lifecycle—from initial design through implementation and dissemination—the research community can maintain public trust and ensure the ethical conduct of human subjects research in increasingly complex scientific landscapes.
The Belmont Report, formally published in 1979, emerged from the work of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research, which was created by the National Research Act of 1974 [8] [23]. This foundational document was a direct response to grave ethical failures in research, most notably the Public Health Service (PHS) Tuskegee Study, where participants were deceived and denied effective treatment, and the Nuremberg Trials, which uncovered horrific human experimentation during World War II [23] [24]. The Report established three fundamental ethical principles—Respect for Persons, Beneficence, and Justice—to govern all research involving human subjects [8]. Rather than being a static historical document, the Belmont Report provides a durable analytical framework that continues to guide the ethical design, review, and conduct of modern scientific inquiry, ensuring that the well-being and rights of participants are paramount [10].
Core Ethical Principles and Their Regulatory Applications
The Belmont Report's three principles translate into specific regulatory requirements and practices within Institutional Review Board (IRB) protocols. The table below summarizes these principles and their practical applications.
Table 1: The Three Ethical Principles of the Belmont Report and Their Applications
| Ethical Principle | Core Meaning | Application in Research & IRB Protocols |
|---|---|---|
| Respect for Persons | Recognition of the autonomy of individuals and the requirement to protect those with diminished autonomy [8] [10]. | - Informed Consent Process: Providing ample information in an understandable manner, ensuring voluntary participation free from coercion, and offering the right to withdraw [8] [11]. |
| Beneficence | The obligation to maximize possible benefits and minimize potential harms [8] [24]. | - Systematic Assessment of Risks and Benefits: A rigorous analysis to ensure that the risks to subjects are justified by the anticipated benefits [8] [1]. |
| Justice | The requirement to distribute the burdens and benefits of research fairly [10] [24]. | - Equitable Selection of Subjects: Ensuring that no racial, sexual, or economic group is systematically selected simply because of its easy availability, compromised position, or societal biases [8] [10]. |
The following diagram illustrates the logical relationship between these principles and their primary applications in research oversight.
Advanced Protocol Implementation: From Principle to Practice
Application Note: Implementing a Valid Informed Consent Process
Objective: To establish a consent process that truly embodies the principle of Respect for Persons, moving beyond a mere signed form to a dynamic, ongoing educational interaction.
Background: Informed consent is the practical application of Respect for Persons, ensuring individuals enter research voluntarily and with adequate information [8]. This is challenged in modern research involving complex biological therapies, big data, and genomic research, where risks may be uncertain or difficult to quantify.
Protocol Methodology:
Comprehension Assessment:
- Procedure: Develop a short, non-leading questionnaire or a "teach-back" method where the prospective subject explains the study's key elements in their own words.
- Documentation: Record the assessment method and outcome in the research record. The IRB should review and approve the tool.
- Rationale: Ensures the information was not only provided but also understood, which is crucial for populations with diminished autonomy or when dealing with highly technical concepts [8].
Documentation of Process:
- Procedure: Beyond the consent form signature, document the process itself. This includes the identity of the person obtaining consent, the date and location, the version of the consent form used, and a note on the overall interaction.
- Rationale: Creates an audit trail that demonstrates a meaningful process was followed, not just a form was signed.
Ongoing Consent for Longitudinal Studies:
- Procedure: For long-term studies, implement a process for re-consent. Triggers for re-consent may include the emergence of new significant risks or benefits, substantial protocol changes, or at pre-specified intervals (e.g., annually).
- Rationale: Respects the autonomous choice of the participant throughout the research relationship, acknowledging that their continued participation should be informed [11].
Application Note: Conducting a Systematic Risk-Benefit Analysis
Objective: To provide IRBs with a rigorous, evidence-based framework for justifying the risks of research by the potential benefits, fulfilling the principle of Beneficence.
Background: The principle of Beneficence requires that researchers and IRBs not only "do no harm" but also "maximize possible benefits and minimize possible harms" [8]. This analysis is foundational to IRB approval.
Protocol Methodology:
Risk Identification and Categorization:
- Procedure: Create a comprehensive list of all foreseeable risks, categorizing them by:
- Type: Physical, psychological, social, economic, legal.
- Likelihood: Remote, unlikely, possible, probable, certain.
- Magnitude: Trivial, minor, serious, catastrophic.
- Duration: Transient, prolonged, permanent.
- Procedure: Create a comprehensive list of all foreseeable risks, categorizing them by:
Benefit Identification and Categorization:
- Procedure: List all anticipated benefits, clearly distinguishing:
- Direct benefit to the subject: Therapeutic studies only.
- Indirect benefit to the subject: e.g., access to healthcare, monetary compensation.
- Benefit to society: e.g., generation of new knowledge.
- Procedure: List all anticipated benefits, clearly distinguishing:
Systematic Assessment and Justification:
- Procedure: Weigh the categorized risks against the categorized benefits. The assessment must demonstrate that the risks are minimized and are reasonable in relation to the knowledge gained and/or the potential direct benefit to the subject.
- IRB Deliberation: The IRB must systematically consider alternatives to the proposed procedures and ensure the assessment is non-arbitrary and fact-based [8].
Table 2: Framework for Risk-Benefit Assessment in IRB Protocols
| Component | Assessment Criteria | Evidence for IRB Review |
|---|---|---|
| Risk Minimization | - Are all proposed procedures essential?- Are there safer alternative methods?- Are safety monitoring plans adequate? | - Protocol scientific rationale.- Literature on alternative methods.- Data safety monitoring plan (DSMP). |
| Benefit Maximization | - Is the research design sound and valid?- Will the study generate meaningful knowledge?- Are direct benefits to subjects realistic? | - Biostatistician review.- Preclinical and preliminary data.- Clinical equipoise statement. |
| Risk Justification | - Do the benefits to society/participants outweigh the risks?- Are the risks justified for the participant population? | - Summary of risks vs. benefits.- Justification for participant selection (link to Justice). |
Navigating Ethical Tensions: The Interplay of Principles
The principles of the Belmont Report are not always easily aligned and can come into conflict, requiring careful balancing by researchers and IRBs [11]. For example, in research involving children, the principle of Respect for Persons mandates honoring a child's dissent. However, if the research offers a direct therapeutic benefit (Beneficence) or is vital for generating knowledge for a condition that affects children as a class (Justice), the IRB may permit a parent's permission to override the child's dissent [11]. Another modern tension involves Justice in genomic research; to avoid creating "genetic orphans," efforts must be made to include diverse populations to ensure all groups can benefit from the advances, which itself requires a Respect for Persons through culturally competent consent processes.
The Scientist's Toolkit: Essential Safeguards in Human Subjects Research
The following institutional and regulatory mechanisms serve as critical tools for implementing the ethical principles of the Belmont Report.
Table 3: Key Institutional Safeguards for Human Subjects Research
| Safeguard / Reagent | Primary Function | Role in Upholding Ethical Principles |
|---|---|---|
| Institutional Review Board (IRB) | An independent committee that reviews, approves, and monitors research involving human subjects [24]. | Serves as the primary operational mechanism for ensuring all three principles are applied to every research protocol before initiation and during conduct [8] [23]. |
| Informed Consent Form | The document used to provide key information to potential subjects and to document their voluntary agreement to participate. | The primary tool for fulfilling Respect for Persons, ensuring autonomous, informed, and voluntary participation [8] [11]. |
| Data Safety Monitoring Board (DSMB) | An independent group of experts that monitors patient safety and treatment efficacy data while a clinical trial is ongoing [24]. | A critical component of Beneficence, actively working to protect subjects from harm by recommending trial modification or termination if risks outweigh benefits [24]. |
| Federalwide Assurance (FWA) | A formal commitment by an institution to the U.S. government that it will comply with federal regulations for the protection of human subjects [8]. | The binding agreement that holds an institution accountable for implementing a program guided by the Belmont Report's principles, thereby enforcing Justice and Beneficence at an organizational level [8]. |
| Protocol & Investigator's Brochure | The detailed plan for conducting the research and the compilation of clinical and non-clinical data on the investigational product. | Provides the essential information required for the IRB to perform a systematic Risk-Benefit Assessment (Beneficence) and ensure the scientific validity of the study. |
The workflow for ethical review and oversight, integrating these safeguards, is depicted below.
The Belmont Report has proven to be a remarkably resilient document. Its power lies not in providing specific answers to every ethical dilemma, but in offering a robust analytical framework—a "compass" rather than a checklist—for navigating the complex moral landscape of human subjects research [10]. As new frontiers in science emerge, from advanced gene therapies and artificial intelligence to novel public health crises, the core principles of Respect for Persons, Beneficence, and Justice provide a stable foundation for ethical deliberation. The ongoing relevance of the Belmont Report is a testament to its profound insight. By rigorously applying its principles through detailed protocols and institutional safeguards, the research community can maintain public trust, protect the rights and welfare of research participants, and responsibly pursue the scientific innovations that will benefit all of humanity.
Operationalizing Ethics: A Step-by-Step Guide to Applying Belmont Principles in Your Protocol
The Belmont Report, published in 1979, established Respect for Persons as one of three fundamental ethical principles for protecting human research subjects [25] [8]. This principle acknowledges the autonomy of individuals and requires that subjects with diminished autonomy are entitled to additional protections [8]. The practical application of Respect for Persons is realized through a robust informed consent process—a cornerstone of ethical research conduct that goes far beyond simply obtaining a signature on a document [26]. This protocol provides detailed guidance for researchers, IRB members, and drug development professionals on implementing a truly comprehensive informed consent process that embodies this foundational ethical principle. A well-constructed consent process ensures that participation is voluntary, informed, and ongoing, thereby safeguarding participant dignity and autonomy throughout the research lifecycle.
Core Principles and Regulatory Framework
The Belmont Report's Ethical Foundation
The Belmont Report emerged partly in response to ethical abuses in research, most notably the Tuskegee Syphilis Study, and continues to shape modern research ethics [25] [27]. Its principle of Respect for Persons incorporates two key ethical convictions: first, that individuals should be treated as autonomous agents capable of making their own decisions, and second, that persons with diminished autonomy are entitled to additional protection [8]. This dual obligation directly informs the requirements for informed consent, requiring researchers to ensure subjects enter research voluntarily with adequate information presented in comprehensible terms [8]. The Report makes specific recommendations about the information that should be conveyed to research subjects, including the research procedures, their purposes, risks and anticipated benefits, alternative procedures, and a statement offering subjects the opportunity to ask questions and withdraw at any time [8].
Regulatory Requirements and Guidelines
The ethical principles outlined in the Belmont Report are codified in various federal regulations, primarily the Federal Policy for the Protection of Human Subjects (the "Common Rule") found in 45 CFR part 46 [25] [17]. These regulations provide the legal framework for informed consent requirements, emphasizing that consent must be legally effective and procured only under circumstances that provide the prospective subject sufficient opportunity to consider whether to participate [26]. The Food and Drug Administration (FDA) has additional informed consent regulations under 21 CFR Part 50 that apply to clinical investigations of drugs, medical devices, and biological products [17]. Recently, regulatory guidance has emphasized the need for a "concise and focused" presentation of key information at the beginning of the consent document to help potential participants understand why they might or might not want to participate in a research study [28] [29]. This reflects an evolving understanding of how to make consent processes more meaningful and effective.
Table 1: Key Regulatory Documents Governing Informed Consent
| Document/Guideline | Year Issued/Revised | Primary Focus | Jurisdiction/Application |
|---|---|---|---|
| The Belmont Report | 1979 | Ethical Principles (Respect for Persons, Beneficence, Justice) | All NIH-funded human subjects research [8] |
| Nuremberg Code | 1947 | Voluntary consent essential for human experimentation | Foundation for modern consent standards [26] [17] |
| Declaration of Helsinki | 1964 (multiple revisions) | Ethical principles for medical research involving human subjects | International biomedical research [17] |
| Common Rule (45 CFR 46) | 2018 (revised) | Basic HHS policy for protection of human research subjects | Federally funded research in the U.S. [25] [28] |
| FDA Regulations (21 CFR 50) | Ongoing | Informed consent requirements for clinical investigations | FDA-regulated clinical trials [29] [17] |
Essential Components of a Valid Informed Consent Process
A comprehensive informed consent process consists of several interdependent components, each requiring careful attention to ensure ethical and regulatory compliance.
Information Disclosure: Key Elements
Federal regulations mandate specific elements of information that must be provided to all prospective research subjects [28]. The 2018 Common Rule revision introduced the requirement that the consent document begin with a "concise and focused" presentation of key information that helps potential participants understand why they might or might not want to participate in the research [28] [29]. Recent guidance suggests this key information summary should include specific elements presented in a structured format.
Table 2: Essential Elements of Informed Consent
| Element Category | Specific Requirements | Practical Application |
|---|---|---|
| Key Information Summary | Statement that project is research; purpose, duration, procedures; risks; benefits; alternatives [28] | Use headings, plain language (6th-8th grade level); present before detailed information [29] |
| Voluntary Participation | Statement that participation is voluntary; no penalty for refusal or withdrawal [26] | Explain process for withdrawal; emphasize no penalty at multiple points in process |
| Risk Disclosure | Reasonably foreseeable risks/discomforts [28] | Categorize by severity and frequency; include physical, psychological, social, economic risks |
| Benefit Description | Reasonably expected benefits to subjects or others [28] | Distinguish between direct and societal benefits; avoid overstating potential benefits |
| Confidentiality | How data will be stored, secured, accessed; who will have access [26] | Describe data protection measures; include certificate of confidentiality if applicable |
| Compensation | Details of any compensation; contact information for questions [26] | Clearly state compensation schedule; proration policy if participant withdraws early |
Comprehension and Voluntariness
Assessment of comprehension is a critical yet often overlooked component of the consent process [26]. Researchers must ensure prospective subjects truly understand the information being presented, which requires more than just providing a document to sign. Effective strategies include teach-back methods (asking participants to explain key concepts in their own words), using plain language at an appropriate reading level (generally 8th grade level or lower), and employing visual aids to explain complex procedures [28] [26]. The consent process must be free of any coercion or undue influence, with special protections for vulnerable populations who may be more susceptible to such pressures [8] [26]. This is particularly important for populations with diminished autonomy, such as children, prisoners, individuals with impaired decision-making capacity, or economically or educationally disadvantaged persons [8].
Documentation and Ongoing Consent
For most non-exempt research, informed consent must be documented with a written consent form signed by the participant or their legally authorized representative [28]. However, the consent process should be viewed as ongoing throughout the research study, not a single event that occurs at enrollment [26]. Researchers should conduct continued check-ins with participants to confirm consistent willingness to participate, provide opportunities for questions and concerns, and update consent when significant new information becomes available or when the study procedures change [26]. For research involving biological specimens, genetic analysis, or higher-risk interventions, additional consent elements and documentation are typically required [28].
Experimental Protocol: Implementing a Comprehensive Informed Consent Process
Pre-Consent Preparation Phase
Objective: To ensure all materials and processes are properly developed and reviewed before engaging with potential participants.
Materials and Reagents:
- IRB-approved protocol and consent documents
- Visual aids and supplementary materials for explaining complex concepts
- Accessibility resources (e.g., large print, translation services, screen-reader compatible digital formats)
Procedure:
- Protocol Finalization: Ensure the research protocol has received full IRB approval, including all consent-related materials [28].
- Consent Document Development:
- Use institutional templates that incorporate required regulatory elements and recommended language [28] [29].
- Write at an 8th-grade reading level or lower, using the Flesch-Kincaid Grade Level formula to verify readability [28] [26].
- Begin with a key information section using the new structured format with specific headings [29]:
- "It is up to you whether you take part in the research"
- "Why are we doing the research, how long will it take, and what will be done?"
- "What are the most common or serious risks?"
- "What are the benefits?"
- "What can you do instead of being in the research?"
- "What if you are injured during the research?"
- "What are the costs or payments?"
- (Optional) "How participating in the research may affect your daily life" [29]
- Researcher Training: Train all study staff on the consent process, including how to explain study procedures, answer common questions, and assess understanding without coercion [26].
- Accessibility Compliance: Ensure all digital consent materials (including online platforms, surveys, and participant portals) conform to WCAG 2.1 AA standards for accessibility by April 2026, as required by the Americans with Disabilities Act [29].
Consent Execution Phase
Objective: To conduct the consent discussion and documentation in a manner that ensures genuine understanding and voluntary participation.
Materials and Reagents:
- IRB-approved consent documents
- Quiet, private space for discussion
- Materials for assessing understanding (e.g., open-ended questions)
Procedure:
- Initial Discussion:
- Comprehension Assessment:
- Verify the participant understands the purpose, procedures, risks, benefits, and alternatives to participation.
- Confirm they understand their right to withdraw at any time without penalty.
- For complex studies, consider using a comprehension quiz to identify areas needing further explanation.
- Voluntariness Reinforcement:
- Explicitly state that participation is voluntary and refusal will not affect their relationship with the institution or access to standard care.
- Allow sufficient time for decision-making (at least 24 hours for higher-risk studies when feasible).
- Documentation:
- Obtain the participant's signature on the IRB-approved consent form after ensuring comprehension.
- Provide the participant with a copy of the signed document.
- For remote consent, use IRB-approved electronic consent processes with proper identity verification.
Post-Consent Maintenance Phase
Objective: To maintain ongoing communication with participants and ensure consent remains informed and voluntary throughout the study.
Materials and Reagents:
- Updated consent documents (if applicable)
- Communication tools for keeping in touch with participants
Procedure:
- Ongoing Check-ins: At each study visit or contact, briefly confirm the participant's continued willingness to participate and address any new questions or concerns [26].
- Consent Updates: If new information emerges that might affect a participant's willingness to continue (e.g., new risks identified in other study participants), obtain reaffirmed consent using an IRB-approved updated consent document.
- Process Evaluation: Periodically assess the consent process through participant feedback to identify areas for improvement.
- Documentation of Updates: Maintain careful documentation of any consent updates or reaffirmations in the research record.
The above diagram illustrates the comprehensive, multi-phase workflow for implementing a valid informed consent process that truly embodies the principle of Respect for Persons, from initial preparation through ongoing maintenance.
Research Reagent Solutions: Essential Materials for Consent Implementation
Table 3: Essential Resources for Effective Consent Processes
| Tool/Resource | Primary Function | Application Context |
|---|---|---|
| IRB-Approved Consent Templates | Provides regulatory-compliant structure with required language and elements [28] | Drafting study-specific consent documents; ensuring all required elements are included |
| Readability Assessment Tools (Flesch-Kincaid) | Measures reading level of consent documents; ensures appropriate comprehension level [26] | Verifying consent materials are at 8th grade level or lower; identifying complex passages |
| Accessibility Validation Tools (WAVE, aXe) | Checks digital compliance with WCAG 2.1 AA standards [29] | Ensuring online consent materials, surveys, and platforms are accessible to people with disabilities |
| Alternative Consent Formats (Video, PowerPoint) | Presents key information in multimedia formats to enhance understanding [29] | Supporting comprehension for low-literacy populations; explaining complex procedures visually |
| Comprehension Assessment Questions | Verifies participant understanding of key study elements [26] | Ensuring genuine informed consent; identifying areas needing further explanation |
| Digital Signature Platforms | Enables remote documentation of consent with identity verification | Obtaining valid consent for decentralized or remote clinical trials |
Discussion: Contemporary Challenges and Innovative Approaches
Implementing truly ethical informed consent processes faces several contemporary challenges. Approximately 20% of participants misunderstand risks, and 15% of studies lack resources for adequate diversity in recruitment [27]. The move toward digital and decentralized trials creates new challenges for ensuring authentic consent in virtual environments. Additionally, the increasing complexity of research, particularly in genetic studies and advanced therapeutics, makes comprehensible explanation of risks and benefits more difficult.
Innovative approaches are emerging to address these challenges. Some researchers are developing multimedia consent tools (videos, interactive modules) that can present key information more effectively than text-alone documents [29]. The FDA and OHRP have encouraged researchers to "develop innovative ways and utilize available technologies to provide key information" and to "consider developing alternate ways to present key information" [29]. Structured comprehension assessment tools are being integrated directly into consent processes to verify understanding before proceeding with enrollment. Furthermore, community engagement approaches are being used in the development of consent materials to ensure they are culturally appropriate and comprehensible to the target population.
A comprehensive informed consent process is the primary practical application of the Belmont Report's principle of Respect for Persons in human subjects research. By moving beyond a signature-focused approach to embrace a truly process-oriented model, researchers honor participant autonomy and build the foundation for ethical research conduct. This requires careful attention to information disclosure, comprehension assessment, and ongoing voluntariness throughout the research relationship. As research methodologies evolve, particularly with increasing digitalization and complexity, the informed consent process must similarly adapt while maintaining its fundamental ethical commitments. The protocols and guidelines presented here provide a framework for implementing consent processes that truly respect persons as autonomous agents, thereby fulfilling both the ethical mandate of the Belmont Report and regulatory requirements governing human subjects research.
The principle of beneficence, as articulated in the Belmont Report, forms a cornerstone of ethical research involving human subjects. It encompasses a dual obligation: to maximize anticipated benefits while systematically minimizing potential risks [8]. For Institutional Review Board (IRB) protocols, translating this ethical principle into practice requires a structured, transparent, and evidence-based risk-benefit analysis. This process ensures that the welfare of research participants is safeguarded and that the research design is sound and ethically justifiable. A well-executed analysis demonstrates respect for persons and justice by ensuring that the risks to which participants are exposed are warranted by the potential value of the knowledge gained. This document provides detailed application notes and protocols for implementing a rigorous risk-benefit assessment framework within IRB submissions, aligning with contemporary regulatory guidance and methodological standards.
Foundational Frameworks and Regulatory Context
The ethical mandate for risk-benefit analysis is embedded within international regulatory standards for human research protection and drug development.
The Belmont Report's Principles
The Belmont Report establishes three core principles. Respect for Persons requires acknowledging autonomy and protecting those with diminished autonomy, typically achieved through informed consent. Beneficence obligates researchers to not only protect participants from harm but also to secure their well-being by maximizing benefits and minimizing harms. Justice requires the fair distribution of both the burdens and benefits of research [8]. The IRB's application of these principles involves a deliberate and systematic review of the research plan to ensure these ethical convictions are upheld.
Contemporary Regulatory Guidance
Recent regulatory documents refine the application of beneficence in drug development. The U.S. Food and Drug Administration (FDA) emphasizes that a benefit-risk assessment is a "case-specific, multi-disciplinary assessment of science and medicine" [30]. This assessment integrates diverse data sources, including clinical and non-clinical data, patient experience data, and real-world evidence, to form a comprehensive judgment [30]. Similarly, China's Center for Drug Evaluation (CDE) has released draft guidelines encouraging a structured approach, including the integration of multi-regional clinical trial (MRCT) data and real-world evidence (RWE) to strengthen assessments [31]. These guidelines highlight the importance of considering regional differences in disease characteristics and patient demographics, ensuring the analysis is contextually relevant.
Quantitative Data Analysis for Risk-Benefit Assessment
A rigorous analysis moves beyond qualitative description to a quantitative evaluation of potential outcomes. The following data types and analytical methods are critical for an evidence-based assessment.
Table 1: Core Quantitative Data Types for Risk-Benefit Analysis
| Data Category | Specific Data Points | Source in Research Protocol |
|---|---|---|
| Benefit Data | Primary efficacy endpoint(s); Secondary efficacy endpoints; Patient-Reported Outcomes (PROs); Quality of Life measures | Primary and secondary objectives; Statistical Analysis Plan (SAP); Outcome measures section |
| Risk Data | Incidence of Adverse Events (AEs); Incidence of Serious Adverse Events (SAEs); Laboratory abnormalities; Discontinuation rates due to AEs | Safety monitoring plan; Harms section; Stopping rules |
| Contextual Data | Natural history of disease/condition; Risks and benefits of standard of care or alternative interventions; Unmet medical need | Background and rationale; Choice of comparator |
Advanced Analytical Methods
To synthesize these data, researchers should employ robust quantitative data analysis methods [32]. The choice of method depends on the research question and data type.
- Descriptive Analysis: Serves as the starting point, summarizing what the data shows about benefits and risks (e.g., mean improvement in a symptom score, incidence rate of a specific adverse event).
- Diagnostic Analysis: Helps understand why certain outcomes occurred by examining relationships between variables (e.g., using regression analysis to identify patient subgroups that experience greater benefit or higher risk) [32].
- Predictive Analysis: Uses historical data and statistical modeling to forecast future trends and potential long-term outcomes, which is particularly valuable for chronic conditions [32].
The FDA guidance notes that data may be collected specifically to address benefit-risk questions or come from "routinely collected... real-world-data sources" [30]. Furthermore, sponsors should not wait for periodic reports to communicate "a potentially serious safety concern that could have an impact on a drug’s benefit-risk profile," underscoring the need for proactive, ongoing analysis [30].
Application Notes: A Protocol for IRB Submission
Integrating a rigorous risk-benefit analysis into an IRB protocol requires attention to both content and presentation. The following section provides a detailed, actionable protocol.
Protocol Development and Reporting Standards
Adherence to established reporting guidelines ensures protocol completeness and transparency. The updated SPIRIT 2025 Statement provides a checklist of 34 minimum items for trial protocols, reflecting methodological advances and emphasizing open science [33]. Key new items relevant to risk-benefit analysis include:
- Open Science Section: Plans for trial registration, protocol and statistical analysis plan access, and data sharing [33].
- Patient and Public Involvement: Details on how patients or the public will be involved in the design, conduct, and reporting of the trial, which can directly inform the understanding of benefits and risks [33].
- Enhanced Harms Reporting: A stronger focus on the assessment and description of harms, ensuring risks are adequately characterized [33].
Similarly, the CONSORT 2025 Statement should be referenced for planning the eventual reporting of trial results to ensure transparency and completeness [34].
The Risk-Benefit Assessment Workflow
The following diagram illustrates the logical workflow for conducting and documenting a rigorous risk-benefit analysis, from initial design to final IRB review.
The Scientist's Toolkit: Essential Reagents for Risk-Benefit Analysis
Table 2: Key Research Reagent Solutions for Risk-Benefit Analysis
| Item/Tool | Function in Risk-Benefit Analysis |
|---|---|
| Structured Benefit-Risk Framework (e.g., FDA Guidance) | Provides a systematic template for listing, summarizing, and weighing evidence on benefits and risks, ensuring all key factors are considered [30]. |
| Patient Experience Data | Provides information on patients' experiences with a disease or condition and their preferences regarding treatment, informing the patient-centricity of the analysis [30]. |
| Real-World Evidence (RWE) | Complements clinical trial data by providing information on intervention effects in routine clinical practice, offering a broader view of benefits and risks [31]. |
| Model-Informed Drug Development (MIDD) | Uses quantitative models to support benefit-risk assessments, particularly for innovative therapies, by extrapolating or predicting outcomes [31]. |
| Statistical Analysis Software (e.g., R, SAS) | Enables the performance of quantitative analyses essential for the assessment, including descriptive statistics, regression modeling, and significance testing [32]. |
Experimental Protocol: A Detailed Methodology
This section provides a step-by-step experimental protocol for executing a risk-benefit analysis suitable for inclusion in an IRB application.
Protocol Title: Quantitative and Qualitative Assessment of Benefit-Risk Profile for [Intervention Name] in [Population/Condition].
1. Objective: To systematically evaluate and document the potential benefits and risks associated with participation in the research study "[Study Title]" to ensure the ethical principle of beneficence is upheld.
2. Materials:
- Preclinical and clinical data (from pilot studies, literature, or similar interventions).
- Summary of known risks and benefits for standard of care or alternative interventions.
- Data collection tools for new benefits and risks (e.g., Case Report Forms, PRO instruments).
- Statistical analysis plan (SAP) specifying methods for analyzing efficacy and safety endpoints.
3. Methodology: 1. Benefit Identification and Quantification: - List all potential benefits to participants (e.g., direct medical benefit, improved quality of life, contribution to knowledge). - For each benefit, specify the primary metric for measurement (e.g., change in disease score, response rate) and the source of data (e.g., primary endpoint, secondary endpoint). - Where possible, estimate the magnitude and probability of benefits based on available evidence.
4. Deliverables:
- A comprehensive Benefit-Risk section within the IRB protocol.
- A structured summary table for IRB review.
- Documentation of the risk management plan.
Upholding the principle of beneficence is an active and continuous process that extends from protocol design through to the dissemination of results. By implementing a structured, transparent, and evidence-based risk-benefit analysis—informed by ethical principles like those in the Belmont Report, contemporary regulatory guidance, and robust quantitative methods—researchers can fulfill their ethical duty to protect participants. This approach not only strengthens the scientific and ethical validity of IRB protocols but also fosters trust between the research community and the public it serves.
The Belmont Report's principle of Justice requires the fair distribution of both the benefits and burdens of research, mandating that participant selection must be equitable and not systematically directed toward any particular group without ethically sound justification [25]. This principle arises from a history of research abuses where disadvantaged populations bore research risks while privileged groups reaped the benefits. In contemporary implementation, Institutional Review Boards (IRBs) operationalize this principle through 45 CFR 46.111(a)(3), which explicitly requires that "selection of subjects is equitable" [35]. For researchers, this translates to a positive obligation to identify and overcome systemic barriers that exclude underserved populations while avoiding the exclusion of groups based on gender, race, national origin, religion, creed, education, or socioeconomic status without scientific justification [36]. The enduring relevance of the Belmont framework lies in its capacity to address contemporary challenges in research ethics, including ensuring that recruitment strategies do not perpetuate health disparities by excluding populations most affected by the conditions under study [25].
Practical Application: The REP-EQUITY Toolkit for Protocol Development
The REP-EQUITY toolkit provides a structured, seven-step methodology for implementing equitable recruitment practices in clinical research protocols [37]. Developed through systematic review and expert consensus, this toolkit guides investigators in facilitating representative and equitable sample selection, addressing the critical gap between ethical principles and practical implementation. The toolkit's algorithmic approach ensures that considerations of justice are integrated throughout study design rather than being addressed as an afterthought.
Table: The REP-EQUITY Toolkit for Representative and Equitable Recruitment
| Step | Key Question | Protocol Implementation |
|---|---|---|
| 1. Definition | What are the relevant underserved groups? | Identify groups using available demographic and health burden data; justify data collection choices [37]. |
| 2. Objectives | What is the aim regarding representativeness and equity? | Define whether the goal is hypothesis testing about group differences, hypothesis generation, or ensuring just distribution of research risks/benefits [37]. |
| 3. Sample Requirements | How will the sample proportion of underserved individuals be defined? | Justify proportions based on generalizability to populations of interest, equity impact, and feasibility [37]. |
| 4. Recruitment Goals | What are the recruitment goals? | Align goals with statistical power requirements, exploratory analyses, and generalizability needs [37]. |
| 5. Strategy | How will external factors be managed? | Formulate plans to address logistical, communication, and trust barriers [37]. |
| 6. Evaluation | How will representation be evaluated? | Plan analysis of enrollment against recruitment goals with transparent reporting [37]. |
| 7. Legacy | What is the legacy of using the toolkit? | Consider impact on community trust and research generalizability [37]. |
Application of this toolkit begins with explicitly defining underserved groups relevant to the research context, which may include populations marginalized by demographic characteristics, socioeconomic status, geographic location, or health status [37]. For protocol development, investigators must then establish specific aims relating to equity and representativeness, whether for hypothesis testing about differences between groups, generating hypotheses about such differences, or ensuring a just distribution of research risks and benefits. The sample proportion of individuals with characteristics associated with being underserved must be explicitly defined and justified in terms of generalizability to the population of interest and the equitable distribution of research participation burdens and benefits.
Quantitative Benchmarks and Recruitment Metrics
Effective equitable recruitment strategies require understanding current recruitment landscapes and establishing measurable goals. Contemporary data reveals significant challenges in recruitment efficiency and diversity that must be addressed through targeted strategies.
Table: Recruitment Benchmarks and Efficiency Metrics
| Metric | Current Benchmark | Equity Implications |
|---|---|---|
| Time to Hire/Enroll | 41 days (24% increase since 2021) [38] | Prolonged processes disproportionately exclude those unable to sustain lengthy participation consideration. |
| Interview Process | 20 interviews per hire (42% increase since 2021) [38] | Extensive time commitments create barriers for economically disadvantaged populations. |
| Sourced vs. Inbound Applicants | Sourced applicants are 5× more likely to be hired than inbound applicants [38] | Passive recruitment perpetuates existing homogeneity; proactive sourcing is essential for diversity. |
| Candidate Passthrough Rates | 3× less likely to get hired today than three years ago [38] | Increased competition requires enhanced support for underrepresented candidates throughout funnel. |
| Diversity Funnel Metrics | Women face lower passthrough rates at top of funnel but higher success in later stages [38] | Bias operates differently across stages, requiring targeted intervention points. |
Recent data indicates that candidate passthrough rates have declined significantly, with prospective applicants now three times less likely to be hired compared to three years ago [38]. This intensified competition heightens the risk that underrepresented populations may be disproportionately filtered out without intentional intervention. Furthermore, disparities in conversion rates across demographic groups persist, with considerable variability by industry and department, underscoring the importance of addressing biases at different stages of the recruitment process to ensure fair opportunities for all candidates [38].
Experimental Protocols for Equitable Recruitment
Protocol 1: Multi-Site EHR-Derived Cohort Recruitment
Purpose: To systematically identify and recruit underrepresented populations across multiple healthcare settings while respecting privacy considerations and local administrative variations.
Methodology:
- Stakeholder Engagement: Convene representatives from all participating sites, including patient advocates from target underserved populations, during protocol development phase [37].
- Data Governance: Establish centralized data processing with distributed analysis where possible to minimize transfer of protected health information [35].
- Identification Algorithm: Develop standardized criteria for identifying potentially eligible participants across systems while accounting for variations in data collection practices.
- Contact Protocol: Implement tiered contact approach beginning with clinician introduction followed by research team contact where permitted [35].
- Barrier Assessment: Collect systematic data on reasons for non-participation to iteratively refine recruitment approach.
Ethical Considerations: This protocol requires careful attention to privacy expectations and compliance with HIPAA regulations regarding use of medical records for recruitment purposes [35]. The IRB must approve waivers of authorization when researchers are accessing protected health information for recruitment. Multi-site recruitment using EHR-derived cohorts requires special planning for patient privacy, data limitations, security, and variance in local administrative practices [35].
Protocol 2: Community-Embedded Recruitment for Hard-to-Reach Populations
Purpose: To increase participation of groups historically underrepresented in research through trusted community channels.
Methodology:
- Community Partnership: Identify and formalize partnerships with community-based organizations serving target populations at least 6 months before recruitment begins.
- Cultural Adaptation: Translate and culturally adapt all recruitment materials with community input, ensuring appropriate literacy levels and cultural resonance.
- Navigator Program: Train individuals from community organizations to serve as research navigators who provide information and support throughout recruitment process.
- Compensation Structure: Provide fair compensation for participation time that does not become unduly influential [35].
- Transportation/Logistical Support: Implement practical support systems to remove common participation barriers.
Ethical Considerations: This approach requires careful attention to therapeutic misconception, particularly when clinical care providers are involved in recruitment [35]. Patients may believe that research participation will directly benefit them, even when told there is no assured benefit. Additionally, researchers must ensure that community partnerships are equitable and avoid tokenism.
Visualization of Equitable Recruitment Workflow
The following workflow diagram illustrates the systematic approach for implementing equitable recruitment strategies throughout the study lifecycle:
Equitable Recruitment Implementation Workflow: This diagram outlines the sequential process for integrating equity considerations throughout research recruitment.
Table: Research Reagent Solutions for Equitable Recruitment
| Tool/Resource | Function | Implementation Guidance |
|---|---|---|
| IRB-Approved Recruitment Materials | Ensure all participant-facing materials meet ethical standards | Submit final versions of advertisements, scripts, and letters for IRB approval before use; use institutional templates when available [35]. |
| Multi-Language Consent Documents | Overcome language barriers for non-English speakers | Translate consent materials and use certified interpreters; research with prospect of direct benefit should generally allow enrollment of non-English speakers [35]. |
| Cultural Adaptation Framework | Ensure materials are culturally appropriate | Engage community representatives in material development and review; assess literacy levels and cultural metaphors [37]. |
| Database Recruitment Protocol | Enable ethical contact of patients for research | Maintain separate IRB-approved protocol for developing databases of potential participants who provide prior consent for future contact [35]. |
| Structured Interview Guides | Reduce bias in screening processes | Implement standardized questions and evaluation rubrics to minimize interviewer bias; 72% of organizations now use structured interviews to reduce bias [39]. |
| Participant Navigation System | Support participants through study process | Train staff specifically to help participants understand and complete study requirements, particularly for complex protocols [37]. |
| Centralized Recruitment Monitoring Dashboard | Track diversity metrics in real-time | Implement system to monitor enrollment demographics against targets with regular reporting to study leadership [37]. |
Implementation of these tools requires proactive planning and resource allocation in the study design phase. The regulatory foundation for these approaches stems from requirements that recruitment and selection of participants must be equitable within the confines of the study, with fair distribution of both research benefits and burdens [35]. Furthermore, payment structures must be carefully designed so they compensate for time and inconvenience without becoming coercive, especially for economically disadvantaged populations [36].
Integrating the Belmont Report's principle of Justice into modern IRB protocols requires moving beyond mechanistic inclusion criteria to actively addressing structural barriers to participation. The strategies outlined in this application note provide a framework for operationalizing ethical principles into practical recruitment methodologies. As the research landscape evolves with increasing use of digital recruitment methods, artificial intelligence, and multi-site collaborations, the enduring framework of the Belmont Report continues to provide essential guidance for ensuring equity in human subjects research [25]. By implementing systematic approaches like the REP-EQUITY toolkit, establishing quantitative benchmarks, and utilizing specialized research reagents, investigators can fulfill the ethical mandate of just participant selection while enhancing the scientific validity and generalizability of their research findings.
The Belmont Report's ethical principles—Respect for Persons, Beneficence, and Justice—provide the foundational moral framework for research involving human subjects [2]. Translating these abstract principles into a formally approved research protocol requires researchers to demonstrate concrete compliance to an Institutional Review Board (IRB). This committee is formally designated to review and monitor biomedical research to protect the rights and welfare of human subjects [9]. This article provides researchers and drug development professionals with detailed application notes and protocols, framed within the broader thesis of implementing the Belmont Report, to navigate the IRB submission process successfully. A meticulously prepared submission not only ensures regulatory compliance but also embodies the ethical commitments that are central to responsible research.
The Belmont Report: From Principle to Practice
The Belmont Report, published in 1979, was a direct response to historical ethical abuses in research, such as the Tuskegee Syphilis Study [2]. It established three core principles that now form the backbone of federal regulations governing human subjects research in the United States, particularly the Common Rule [1] [2]. The challenge for contemporary researchers is to operationalize these principles into every aspect of their study design and protocol documentation.
The following table outlines the core applications of each Belmont principle as defined by the report and their concrete manifestations in IRB protocols.
Table 1: Implementing the Belmont Report's Principles in IRB Protocols
| Belmont Principle | Ethical Meaning | Practical Application in IRB Protocols |
|---|---|---|
| Respect for Persons | Recognizing the autonomy of individuals and protecting those with diminished autonomy [2]. | - Informed Consent Process & Documentation: Providing all required elements of information in an understandable format and obtaining voluntary agreement [40].- Protecting Vulnerable Populations: Implementing additional safeguards for participants such as children, prisoners, and individuals with impaired decision-making capacity [41] [42]. |
| Beneficence | The obligation to maximize possible benefits and minimize possible harms [2]. | - Risk-Benefit Assessment: Providing a detailed analysis that justifies the risks to subjects in relation to the anticipated benefits and the importance of the knowledge gained [42].- Data Safety Monitoring: Describing plans for ongoing safety monitoring, potentially including a Data Safety Monitoring Board (DSMB) for higher-risk studies [41]. |
| Justice | Ensuring the fair distribution of the burdens and benefits of research [2]. | - Equitable Subject Selection: Providing clear inclusion and exclusion criteria that are scientifically justified and do not unfairly target or exclude specific groups without a valid reason [41] [42].- Avoiding Exploitation: Ensuring that vulnerable populations are not selected for research due to their easy availability or manipulability rather than the scientific requirements of the study. |
The following workflow diagram illustrates how these ethical principles are systematically translated into a research plan and evaluated during the IRB review process.
Essential Elements of an IRB Submission Protocol
A well-structured research protocol is the primary document the IRB uses to evaluate the ethical and scientific validity of a study. The protocol must provide a complete and clear description of the research to allow the IRB to assess it against the federal criteria for approval [41]. The following section outlines the essential elements, with particular attention to how they reflect Belmont principles.
Protocol Narrative and Scientific Rationale
The introduction of the protocol must establish the scientific foundation and necessity of the research.
- Introduction/Rationale: This section should indicate the specific reasons for the study, the research question, and a review of relevant literature that justifies why the study is needed. It should clearly state the hypothesis and the scientific knowledge expected to result [42].
- Objectives: The study objectives should be specific, quantifiable, and congruent with the study design [42]. They must be based on the research question and limited in scope and number to ensure the study is feasible and focused.
This section fulfills the Beneficence principle by establishing the potential value of the knowledge to be gained, which is weighed against the risks to participants.
Detailed Methods and Procedures
The methods section must provide a granular description of all research activities. Clarity here is crucial for the IRB to evaluate risks accurately.
- Study Design: Specify the design (e.g., randomized controlled trial, observational cohort, survey). For clinical research, a schematic of study events by visit is highly recommended to clarify the timing of tests and procedures [42].
- Study Procedures: Provide a clear and detailed list of all procedures (e.g., interviews, blood draws, drug administration, diagnostic tests). The protocol must distinguish which procedures are part of standard clinical care and which are performed solely for research purposes [41] [42].
- Data Analysis Plan: Describe the statistical methods and plans for data analysis prospectively to avoid the introduction of bias by changing the analysis during the study [41].
Subject Population and Selection Criteria
This section directly addresses the Justice principle by ensuring the equitable selection of subjects [42].
- Inclusion/Exclusion Criteria: Provide complete and detailed lists of eligibility criteria. These should be designed to make the study as inclusive as possible while excluding individuals whose participation would unacceptably increase their risks or confound the data. The rationale for each criterion should be explained [41] [42].
- Recruitment: Describe how participants will be identified, approached, and recruited. The methods must be free of coercion and undue influence [43].
- Vulnerable Populations: If the research includes groups vulnerable to coercion (e.g., children, prisoners, individuals with cognitive impairments), the protocol must describe the additional safeguards implemented to protect their rights and welfare [41]. Justification for their inclusion must be provided.
Risks and Benefits Analysis
A rigorous and honest assessment of risks and benefits is the core of the Beneficence principle [42].
- Potential Risks: Identify all foreseeable physical, psychological, social, and economic risks. For each risk, describe its probability and magnitude. The protocol must also state how risks will be minimized through sound research design and procedures [41].
- Potential Benefits: Distinguish between direct benefits to the participant and the broader benefits to society from the generation of new knowledge. Avoid overstating or exaggerating direct benefits to participants [42].
- Risk-Benefit Ratio: Justify that the risks are reasonable in relation to the anticipated benefits. The IRB will consider only those risks and benefits that may result from the research, as distinguished from those of routine care [42].
Informed Consent Process and Documentation
The informed consent process is the primary practical application of Respect for Persons. It is not merely a form to be signed, but a dynamic process of information exchange [40].
- Consent Process: Describe the setting, the person who will obtain consent, and how it will be conducted to ensure the participant has adequate time to ask questions and consider participation [41].
- Consent Document: The written consent form must include all basic elements required by federal regulations (45 CFR 46.116(a)), such as a statement that the study involves research, a description of risks and benefits, and an explanation of confidentiality [40]. The language must be understandable to the participant and may not include any exculpatory language through which the participant waives their legal rights [40].
- Documentation of Consent: Specify how consent will be documented, typically with a signed form. The protocol must justify any request for a waiver of consent or its documentation [41].
Confidentiality and Data Safety Management
Protecting participant privacy and ensuring data confidentiality are ongoing obligations throughout the research.
- Privacy and Confidentiality: Describe procedures to protect participant privacy during recruitment and data collection. Explain how data will be anonymized or de-identified, stored, transferred, and analyzed to maintain confidentiality [41].
- Data Safety Monitoring: For research involving more than minimal risk, the protocol must include a plan for monitoring data to ensure participant safety. This could range from periodic review by the Principal Investigator to the use of an independent Data Safety Monitoring Board (DSMB) [41].
The Researcher's Toolkit: Essential Materials for Ethical and Regulatory Compliance
Preparing a successful IRB submission requires careful preparation of documents and, for experimental research, precise planning of materials. The following table details key components and reagents essential for this process.
Table 2: Essential Research Reagents and Documentation for IRB Submissions
| Item / Reagent Solution | Function / Purpose in Protocol | Key Considerations |
|---|---|---|
| Informed Consent Form Template | Provides the structural framework for creating a consent document that includes all regulatory-required elements [40]. | Must be institution-specific. Avoids exculpatory language. Serves as evidence that consent was obtained [40]. |
| FDA Form 1572 (for IND Studies) | Documents the investigator's commitment to key obligations when conducting a study under an Investigational New Drug Application [41]. | Required for FDA-regulated drug trials. Lists key study personnel and committed clinical sites. |
| Investigational Product (Drug/Biologic) | The therapeutic agent whose safety and/or efficacy is being evaluated [41]. | Regulatory status (IND number or exemption rationale) must be provided to the IRB. Requires detailed description of storage, preparation, and dosing [41]. |
| Validated Assessment Kits | Standardized and calibrated tools (e.g., ELISA kits, validated survey instruments) to ensure reliable and consistent data collection. | Use of validated tools strengthens research integrity. Protocols should specify the make and model of key diagnostic equipment. |
| Data Safety Monitoring Plan (DSMP) | A formal document outlining procedures for ongoing review of study data to identify any unexpected safety issues [41]. | Crucial for studies with more than minimal risk. May mandate a DSMB for complex, high-risk trials [41]. |
Experimental Protocol: A Framework for Ethical Clinical Trial Design
This protocol framework is designed for an interventional clinical trial, incorporating the essential ethical elements required for IRB review.
Protocol Title
A Phase [X] Study to Investigate [Intervention] in [Population] for [Condition].
Hypothesis
[State the testable hypothesis, e.g., "The intervention Drug X is superior to placebo in improving the primary outcome measure Y in adults with condition Z after 12 weeks of treatment."]
Objectives
- Primary Objective: [Single, quantifiable objective, e.g., "To evaluate the efficacy of Drug X compared to placebo as measured by the change in baseline in outcome Y at Week 12."]
- Secondary Objectives: [Limited number of additional objectives, e.g., "To assess the safety and tolerability of Drug X," and "To evaluate the effect of Drug X on quality of life using the ABC questionnaire."]
Methodology
- Study Design: [e.g., "A randomized, double-blind, placebo-controlled, parallel-group, multi-center study."]
- Intervention Description: Provide a detailed description of the intervention and control, including dosage, route of administration, and frequency. For drugs/devices, include the storage and preparation instructions [41].
- Subject Selection:
- Inclusion Criteria: [List, e.g., "Men and women aged 18-75," "Confirmed diagnosis of Z," "Willing and able to provide informed consent."]
- Exclusion Criteria: [List, e.g., "History of hypersensitivity to the study drug," "Participation in another clinical trial within 30 days," "Pregnant or nursing women." Justify exclusions related to gender or minority status [42].]
- Study Procedures and Visit Schedule: A tabular schedule of activities is essential.
Table 3: Example Study Visit Schedule and Procedures
| Procedure | Screening (Week -2) | Baseline (Day 1) | Treatment Visit (Week 4) | End of Study (Week 12) |
|---|---|---|---|---|
| Informed Consent | X | |||
| Medical History | X | |||
| Eligibility Lab Tests | X | (X) | ||
| Physical Examination | X | X | ||
| Administer Study Drug | X | X | X | |
| Efficacy Outcome Y | X | X | X | |
| Adverse Event Assessment | X | X | X |
- Statistical Analysis: Pre-specify the statistical methods, including the sample size calculation with power, the primary analysis population (e.g., Intent-to-Treat), and the statistical test for the primary endpoint [41].
Ethical Considerations
- Informed Consent: All potential subjects will be provided with the IRB-approved informed consent form. A qualified member of the research team will explain the study in detail and answer all questions. Subjects will be given sufficient time to decide before signing [40].
- Risk Minimization: Risks are minimized by [e.g., "frequent safety monitoring," "dose adjustments based on predefined criteria," "using procedures consistent with sound research design"].
- Confidentiality: All participant data will be stored in a secure, password-protected database identified by a unique study code. Documents with personal identifiers will be stored separately in a locked cabinet [41].
- Compensation for Injury: The consent form will include a statement regarding the availability of compensation and medical treatment in the event of a research-related injury, in accordance with institutional policy [9].
Successfully documenting ethical compliance for an IRB submission is a rigorous process that demands a deliberate and thorough approach. By systematically translating the ethical principles of the Belmont Report—Respect for Persons, Beneficence, and Justice—into every component of the research protocol, investigators do more than just satisfy a regulatory requirement. They build a foundation of trust with participants, the institution, and the public, and they affirm their commitment to the highest standards of scientific and ethical research conduct. A well-prepared protocol that clearly demonstrates this integration is the most critical tool for securing timely IRB approval and ensuring the protection of the individuals who make research possible.
Navigating Complexities: Troubleshooting Common Ethical Challenges in IRB Submissions
The effective management of unanticipated problems and protocol deviations represents a critical operational function within human subjects research, serving as a practical application of the ethical principles first articulated in the Belmont Report. This foundational document, which outlines the ethical principles of respect for persons, beneficence, and justice, provides the moral framework upon which modern regulatory standards are built [44] [45]. Institutional Review Boards (IRBs) are charged with ensuring that research is conducted in accordance with these principles, which require not only prospective review of research protocols but also ongoing surveillance of research activity [20]. Protocol deviations—departures from the IRB-approved research plan—occur frequently in clinical research and warrant systematic management to protect subject welfare and data integrity while upholding these core ethical commitments [46] [47].
The Belmont Report's principle of beneficence obligates researchers to maximize possible benefits and minimize potential harms, creating a direct imperative for robust deviation management systems that identify and address departures from protocols designed specifically to protect subjects [44]. Similarly, respect for persons requires that subjects voluntarily consent to participate in research according to specific parameters; deviations from these parameters without proper oversight undermine this fundamental ethical requirement [45]. This application note establishes detailed protocols for classifying, reporting, and managing protocol deviations through the ethical lens established by the Belmont framework, providing researchers, scientists, and drug development professionals with practical tools to implement these principles in daily research operations.
Defining Protocol Deviations and Unanticipated Problems
Regulatory Definitions and Classifications
A protocol deviation is formally defined as "any change, divergence, or departure from the study design or procedures defined in the protocol" [48] [46] [49]. These departures range from minor administrative variances to significant deviations that may affect subject rights, safety, or data integrity. The International Council for Harmonisation (ICH) E3 guideline further distinguishes a critical subcategory of important protocol deviations as those "that may significantly impact the completeness, accuracy, and/or reliability of key study data or that may significantly affect a subject's rights, safety, or well-being" [48] [46] [49].
TransCelerate BioPharma Inc. has enhanced these foundational definitions with clarifying principles that specify a protocol deviation must involve (1) an event that actually occurred (not theoretical), (2) relationship to the protocol or documents referenced in the protocol, and (3) independence from fault or blame, ensuring objective identification [49]. These clarifications help prevent over-reporting of trivial issues that can obscure meaningful safety signals.
Unanticipated problems represent a related but distinct category, defined by three mandatory criteria: (1) unexpected nature (in terms of nature, severity, or frequency), (2) related or possibly related to research participation, and (3) suggestion that the research places subjects or others at greater risk of harm than was previously known or recognized [20]. While all unanticipated problems involving risks to subjects must be reported, not all protocol deviations rise to the level of unanticipated problems [20] [50].
Table 1: Classification of Protocol Deviations
| Deviation Category | Definition | Impact Level | Examples |
|---|---|---|---|
| Important/Major | May significantly impact subject rights, safety, welfare, or key study data integrity | High | Enrolling subjects in violation of key eligibility criteria; failing to collect primary endpoint data; administering expired investigational product [46] [20] [50] |
| Non-Important/Minor | Does not affect rights, safety, welfare, or reliability of study data | Low | Follow-up visits outside required timeframe due to participant schedule; blood samples drawn at close but not exact protocol-specified times [48] [50] |
| Emergency | Implemented immediately to eliminate apparent immediate hazard to subject | Critical | Protocol change required immediately to protect life or physical well-being of participant [50] |
Intentionality and Timing Considerations
The FDA's 2024 draft guidance further classifies deviations by intentionality, distinguishing between unintentional deviations (unplanned departures typically identified after occurrence) and planned deviations (intentional departures from the protocol for a single participant arranged in advance) [48]. This distinction carries significant regulatory implications for reporting and documentation requirements.
For drug studies, planned deviations generally require sponsor and IRB approval prior to implementation, except when necessary to eliminate an apparent immediate hazard [48]. In device studies, deviations typically require FDA and IRB approval prior to implementation, with similar emergency exceptions [48]. This classification system enables appropriate regulatory oversight while permitting necessary flexibility when subject welfare is at immediate risk.
The Ethical Framework: Connecting Belmont Principles to Deviation Management
Operationalizing the Belmont Report
The ethical principles articulated in the Belmont Report provide the foundational rationale for rigorous deviation management rather than serving as operational directives themselves. The Belmont Report's three core principles translate to specific operational requirements in deviation management:
Respect for Persons manifests in deviation management through protection of informed consent parameters. When subjects consent to participate in research, they agree to specific procedures, risks, and benefits outlined in the IRB-approved protocol. Deviations from these parameters without appropriate oversight fundamentally violate the autonomy and self-determination that this principle protects [44] [45]. For example, enrolling subjects who do not meet eligibility criteria or implementing unapproved procedures subverts the informed consent process by exposing subjects to research conditions they did not explicitly authorize.
Beneficence requires researchers to maximize benefits and minimize harms, creating positive obligations for protocol compliance [44]. Research protocols are specifically designed with scientific validity and subject protection in mind; deviations from these protocols may compromise both objectives. The systematic identification and management of deviations represents a practical implementation of the obligation to protect subjects from harm [20] [47]. The Belmont Report's principle of beneficence underpins the regulatory requirement that deviations affecting subject safety be reported promptly and addressed systematically.
Justice concerns the fair distribution of research benefits and burdens across participant populations. Consistent protocol application ensures equitable treatment of all research subjects, while deviations may introduce inequities in how different subjects experience research procedures and risks [44] [45]. Proper deviation management ensures that no subset of participants bears disproportionate risk due to protocol non-adherence.
Ethical Analysis Framework for Protocol Deviations
The following decision tree provides a systematic method for evaluating protocol deviations through an ethical lens, ensuring consistent application of Belmont principles across various deviation scenarios:
Comprehensive Protocol: Deviation Management Workflow
Deviation Identification and Assessment Protocol
A systematic approach to deviation management begins with prospective planning and continues through study closure. The following workflow outlines a comprehensive deviation management system aligned with both regulatory requirements and ethical principles:
Protocol Deviation Assessment Plan (PDAP) Development: Prior to study initiation, create a protocol-specific PDAP that documents the management approach for potential deviations [46] [49]. This living document should be maintained until the last study data has been reviewed and should include:
- Prospective identification of potential important deviations
- Classification criteria and categorization methodology
- Thresholds at which non-important deviations may become important through recurrence
- Frequency of data reviews and trend analyses
- Feedback and escalation pathways
- Documentation, approval, and archiving requirements [46]
Training Requirements: Investigators must train study site personnel on the protocol and all amendments, while study team members (including CRAs and CROs) should receive additional training on the PDAP and updates [46]. Training should emphasize the ethical implications of protocol adherence rather than merely regulatory compliance.
Identification Methods: Implement both programmatic (electronic data capture systems) and manual processes for deviation identification [46] [49]. Programmatic identification should focus on automated checks for protocol parameters, while manual processes should address information not captured in electronic systems.
Reporting Framework and Timelines
Reporting requirements for protocol deviations vary based on their classification, intentionality, and regulatory context. The following tables summarize specific reporting obligations for sponsors and investigators:
Table 2: Sponsor Reporting Requirements for Protocol Deviations
| Deviation Type | Drug Studies | Device Studies |
|---|---|---|
| Intentional Important | Obtain IRB approval prior to implementation; notify FDA per reporting timelines; for urgent situations, allow immediate implementation with subsequent reporting [48] | Obtain FDA and IRB approval prior to implementation; for urgent situations, allow immediate implementation with records inspection and reporting within 5 business days [48] |
| Unintentional Important | Report to FDA and share information with investigators and IRB within specified reporting timelines [48] | Report to FDA and share information with investigators and IRB within specified reporting timelines [48] |
| Not Important | May report on semi-annual or annual basis via cumulative events report [48] | Allow investigators to implement deviations after review; report per requirements [48] |
Table 3: Investigator Reporting Responsibilities for Protocol Deviations
| Deviation Type | Drug Studies | Device Studies |
|---|---|---|
| Intentional Important | Obtain sponsor and IRB approval prior to implementation; for urgent situations, implement immediately and promptly report to sponsor and IRB [48] | Obtain sponsor, FDA, and IRB approval prior to implementation; for urgent situations, implement immediately, maintain records, and report within 5 business days [48] |
| Unintentional Important | Report to sponsor and IRB within specified reporting timelines [48] | Report to sponsor and IRB within specified reporting timelines [48] |
| Not Important | Report to sponsor during monitoring activities; follow IRB reporting requirements [48] | Implement and report to sponsor within 5 days' notice [48] |
Emergency Deviation Protocol: When a deviation is necessary to eliminate an apparent immediate hazard to a subject, investigators may implement the change immediately without prior approval [48] [50]. The sponsor and IRB must be notified as soon as possible—for device studies, this notification must occur within 5 days [50]. These deviations are always considered unanticipated problems involving risks to subjects or others [50].
Research Reagent Solutions and Documentation Tools
Table 4: Essential Materials for Protocol Deviation Management
| Tool/Resource | Function | Implementation Example |
|---|---|---|
| Protocol Deviation Assessment Plan (PDAP) | Protocol-specific document defining important deviation criteria and management processes | Excel-based template documenting protocol-level important deviations with classification thresholds [49] |
| Electronic Data Capture (EDC) Systems | Automated identification of potential deviations through programmed checks | System alerts for eligibility criterion violations or missed safety assessments [46] [47] |
| Clinical Trial Management System (CTMS) | Centralized tracking and reporting of deviation metrics | Cumulative reporting of deviation trends across sites for continuing review submissions [46] |
| Decision Tree Tool | Visual guide for consistent classification of important vs. non-important deviations | Application of standardized criteria to determine reporting pathway for specific deviation events [46] [49] |
| Quality Management System | Framework for implementing corrective and preventive actions (CAPA) | Investigation of root causes for recurring deviations and implementation of systematic improvements [46] [47] |
Analytical Framework for Deviation Impact Assessment
The statistical analysis of protocol deviations requires both quantitative and qualitative assessment methods. The following protocol outlines a comprehensive approach to deviation impact analysis:
Data Collection Methodology: Establish systematic documentation of all deviations, including frequency, type, root cause, and subject impact. Categorize deviations according to a standardized classification system (e.g., eligibility criteria violations, visit window deviations, procedural errors) [46] [47].
Trend Analysis Protocol: Implement regular reviews (quarterly recommended) of deviation patterns across study sites, investigators, and procedures. Utilize statistical process control methods to identify special cause variation that may indicate systematic problems requiring intervention [46].
Per-Protocol Analysis Determination: For important deviations affecting eligibility criteria or primary endpoint data, establish a blinded endpoint adjudication committee to determine whether specific cases should be excluded from per-protocol analysis populations [46]. Document all exclusions and justifications in the statistical analysis plan.
Root Cause Analysis Technique: Apply the "5 Whys" methodology to important deviations to identify underlying system issues rather than individual errors. Categorize root causes as protocol-related (overly complex procedures), site-related (training deficiencies), participant-related (non-adherence), or system-related (resource constraints) [47].
Effective management of unanticipated problems and protocol deviations requires more than regulatory compliance—it demands a fundamental commitment to the ethical principles that safeguard research participants. By implementing the systematic approaches outlined in this application note, researchers can operationalize the Belmont Report's principles of respect for persons, beneficence, and justice within their deviation management programs. The integration of prospective planning through PDAPs, structured assessment using ethical frameworks, and comprehensive reporting mechanisms creates a robust system that protects both research participants and data integrity.
As clinical research grows increasingly complex, the incidence of protocol deviations continues to challenge research teams [47]. However, by embracing these challenges as opportunities to strengthen ethical oversight rather than merely administrative burdens, the research community can fulfill its moral obligations while advancing scientific knowledge. The frameworks and protocols presented here provide practical implementation roadmaps that align regulatory requirements with foundational ethical principles, enabling researchers to conduct scientifically valid research that respects the dignity and rights of every participant.
The Belmont Report, published in 1979, established three fundamental ethical principles for protecting human research subjects: Respect for Persons, Beneficence, and Justice [8]. These principles form the ethical foundation for the federal regulations governing human subjects research, including the Common Rule (45 CFR 46) [11]. For researchers, Institutional Review Boards (IRBs), and drug development professionals, translating these broad ethical principles into concrete, actionable protocols is paramount, especially when research involves populations vulnerable to coercion or undue influence.
Vulnerable populations are defined as subjects likely to be vulnerable to coercion or undue influence, including children, prisoners, individuals with impaired decision-making capacity, or economically or educationally disadvantaged persons [51]. The Belmont Report stipulates that respect for persons entails acknowledging autonomy and protecting those with diminished autonomy, while justice requires the fair distribution of research burdens and benefits [8] [11]. This application note provides detailed strategies and protocols for implementing these principles specifically for children, prisoners, and cognitively impaired adults within IRB applications and study designs.
Ethical Foundations and Regulatory Frameworks
The Belmont Report's three principles directly inform the specific regulatory protections for vulnerable groups outlined in the Code of Federal Regulations.
Respect for Persons: This principle manifests through the requirement for informed consent. It demands that individuals are treated as autonomous agents and that those with diminished autonomy, such as children or cognitively impaired adults, are entitled to additional protections [8] [11]. This involves obtaining permission from legally authorized representatives and, where possible, seeking the assent of the vulnerable individual themselves [51].
Beneficence: This principle goes beyond simply "do no harm" and requires an obligation to maximize possible benefits and minimize possible harms [8]. For IRBs and researchers, this entails a systematic assessment of risks and benefits. The Belmont Report advises that the "risks and benefits must be fairly presented" in the informed consent process and that "investigators should examine whether the risks are justified by the benefits" [8].
Justice: The principle of justice addresses the equitable selection of research subjects [8]. It requires that the types of subjects enrolled in research are appropriate given the research's purpose and that the risks and benefits of research are distributed fairly across society. This principle guards against systematically selecting vulnerable populations simply because of their availability or manipulability [8] [11].
Table 1: Mapping Belmont Principles to Regulatory Protections for Vulnerable Populations
| Belmont Principle | Core Ethical Duty | Regulatory Manifestation (45 CFR 46) |
|---|---|---|
| Respect for Persons | Recognize autonomy; protect those with diminished autonomy. | Subpart B: Pregnant Women, Human FetusesSubpart C: PrisonersSubpart D: ChildrenRequirements for Legally Authorized Representatives (LARs) and Assent |
| Beneficence | Maximize benefits; minimize harms. | Requirement for risk-benefit analysis [51] [8]Justification for greater-than-minimal-risk research involving children [51] |
| Justice | Ensure fair distribution of risks and benefits. | Equitable subject selection [8]Additional safeguards for economically/educationally disadvantaged persons [51] |
Application Notes & Experimental Protocols
Population-Specific Safeguards and IRB Workflows
Implementing the Belmont Report requires distinct workflows for each vulnerable population. The following protocol outlines the ethical considerations and IRB application requirements.
Diagram 1: IRB Protocol Workflow for Vulnerable Populations
Detailed Protocol: Children
Objective: To enroll children in research while complying with Subpart D of 45 CFR 46 and upholding the Belmont principles through parental permission and child assent.
Background: Children are defined as persons who have not attained the legal age for consent to treatments or procedures under the applicable law [51]. The IRB must classify the research into one of three approval categories [51].
Materials:
- IRB Initial Review Application
- Parental Permission Document(s)
- Child Assent Document/ Script
- Study Instruments (e.g., surveys, clinical measures)
Procedure:
- IRB Application: On the Vulnerable Participants page of the Initial Review Application, select "children" and provide [51]:
- Justification for the inclusion of children.
- The proposed approval category (see Table 2).
- Detailed description of the assent process and documentation.
- Parental Permission: Obtain and document permission from parents(s). The requirement for one or both parents' signature is determined by the IRB based on the risk level of the research [51].
- Child Assent: Obtain assent from all children capable of providing it. The IRB does not generally require a separate assent document; assent can be documented in a signature block on the parental permission form [51].
- Ongoing Review: The research team and IRB must continuously evaluate that the risks to children are justified and that adequate provisions for assent and parental permission remain in place [51].
Table 2: IRB Approval Categories for Research Involving Children
| Approval Category | Risk Level | Key Justifying Criteria | Parental Permission Requirement |
|---|---|---|---|
| Category 1 | Minimal Risk | Risks do not exceed those of daily life. | Permission from one parent is generally sufficient. |
| Category 2 | Greater than Minimal Risk with Prospect of Direct Benefit | Risk is justified by anticipated benefit; relation of risk to benefit is at least as favorable as alternatives. | Permission from one parent is generally sufficient. |
| Category 3 | Greater than Minimal Risk with No Prospect of Direct Benefit | Risk is minor increase over minimal; procedures are commensurate with actual/expected experiences; research likely yields generalizable knowledge about subject's condition. | Permission from both parents is required (unless one is deceased, unknown, or incompetent). |
Detailed Protocol: Prisoners
Objective: To conduct research involving prisoners in accordance with Subpart C of 45 CFR 46, ensuring justice by protecting against coercion due to their incarcerated status.
Background: A prisoner is any individual involuntarily confined in a penal institution [51]. Note that the state of California does not allow state prisoners to be enrolled in clinical trials or other biomedical studies [51].
Materials:
- IRB Initial Review Application
- Informed Consent Document
- Documentation of approved research category under 45 CFR 46.306(a)(2)
Procedure:
- IRB Application: Select the "prisoners" box on the Vulnerable Participants page. The research must be specifically approved for this population [51].
- Category Justification: Justify that the proposed research fits into one of the permitted categories (e.g., study of criminal behavior, prisons as institutions, conditions affecting prisoners as a group) [51].
- IRB Ethical Findings: The IRB must make seven additional findings to approve the research, including [51]:
- Any advantages of participation do not impair the prisoner's ability to weigh risks.
- Risks are commensurate with those accepted by non-prisoner volunteers.
- Subject selection is fair and not influenced by prison authorities.
- Parole boards are not informed of participation.
- Adequate provisions for follow-up care are in place, if needed.
Detailed Protocol: Cognitively Impaired Adults
Objective: To enroll adults with impaired decision-making capacity in research using a Legally Authorized Representative (LAR) and respecting the autonomy of the subject through assent where possible.
Background: A cognitively impaired adult has reached the legal age of consent but may lack the capacity to comprehend the consent process [51]. Federal regulations and institutional policy often restrict such enrollment to research relating to the cognitive impairment, lack of capacity, or serious/life-threatening conditions specific to the subjects [51].
Materials:
- IRB Initial Review Application
- Capacity Assessment Tool/Script
- LAR Consent Document
- Subject Assent Document/Script
Procedure:
- IRB Application: Select the "Cognitively Impaired Adults" box and describe [51]:
- The process for determining decision-making capacity.
- The plan for obtaining assent from subjects capable of providing it.
- The plan for obtaining consent if a subject regains capacity.
- Capacity Assessment: Prior to consent, implement a documented process to determine whether a prospective subject has the capacity to provide informed consent.
- LAR Consent: Obtain informed consent from a Legally Authorized Representative as defined by state law or institutional policy [51].
- Subject Assent: Obtain assent from all adults who lack capacity but are capable of some level of comprehension and agreement [51].
The Scientist's Toolkit: Essential Research Reagents and Materials
For researchers designing studies involving vulnerable populations, the following "reagents" are essential for ensuring ethical conduct and regulatory compliance.
Table 3: Essential Reagents for Ethical Research with Vulnerable Populations
| Tool/Reagent | Function & Application | Key Considerations |
|---|---|---|
| IRB Application Template | Formal document for requesting IRB review of research protocol. | Must accurately describe vulnerable population safeguards, consent/assent processes, and data security [52]. |
| Informed Consent/Permission Documents | Provides prospective subjects/LARs with information required for voluntary decision-making. | Must be in language understandable to the subject/LAR [51] [8]. For non-English speakers, translated versions are required. |
| Child Assent Script/Document | Communicates research information to a child in an age-appropriate manner to seek their agreement. | Content and language should be tailored to the child's developmental level; documented per IRB policy [51]. |
| Capacity Assessment Tool | Structured interview or script to evaluate an adult's ability to understand research procedures and provide informed consent. | Should be validated and appropriate to the population and complexity of the research [51]. |
| De-identification Protocol | A detailed plan for removing direct and indirect identifiers from research data to protect participant confidentiality. | Must address both the 18 HIPAA identifiers and indirect identifiers that could lead to re-identification when combined [53]. |
| Data Security Plan | A formal plan outlining how collected data will be stored, secured, and eventually shared or destroyed. | Often forgotten by early-career researchers; required by many IRB submission portals [52]. |
Data Management and Confidentiality
Upholding the Belmont principle of Respect for Persons extends to protecting participant confidentiality through careful data management. IRB protocols should balance the need for scientific data sharing with the imperative to protect subjects.
- Incorporate Data Sharing in the IRB Protocol: Explicitly address in the IRB application what data will be archived versus shared, what information will be destroyed, and how future data use will be managed [53].
- Informed Consent Language: The consent form should explicitly state how data will be processed and shared, including de-identification methods, what data will be shared, and where it will be shared (e.g., a named repository) [53].
- De-identification vs. Anonymization: A de-identified dataset is not the same as an anonymized one. Researchers should use language such as "de-identified" or "confidential" in their IRB applications and consent forms [53]. The process must remove all 18 HIPAA direct identifiers and carefully examine indirect identifiers (e.g., specific dates, geographical information) that could lead to re-identification when combined with other data [53].
Integrating the ethical principles of the Belmont Report into the practical design and review of research is a dynamic process requiring vigilance and expertise. For vulnerable populations like children, prisoners, and cognitively impaired adults, this integration is non-negotiable. By implementing the specific application notes, protocols, and data management strategies outlined in this document, researchers and IRBs can fulfill their shared ethical duty to ensure that the autonomy, welfare, and equitable treatment of every research subject is robustly protected. This not only ensures regulatory compliance but also strengthens the integrity and social value of the research enterprise.
Balancing Risks and Benefits in Early-Phase Clinical Trials and Novel Therapies
Early-phase clinical trials (Phase 0, I, and II) represent the critical translational bridge from preclinical research to established therapeutic interventions in human populations. These trials carry inherent uncertainty and significant ethical challenges due to their limited safety and efficacy data, necessitating a rigorous framework for risk-benefit analysis. The Belmont Report's ethical principles—respect for persons, beneficence, and justice—provide the foundational framework for Institutional Review Board (IRB) evaluation of these studies [8]. Within this framework, IRBs must balance scientific innovation with participant protection, particularly as novel therapeutic modalities increase in complexity.
Recent evidence indicates that early-phase trials present substantial challenges for IRBs. A 2025 national survey of IRB chairs revealed that two-thirds found risk-benefit analysis for early-phase trials more challenging than for later-phase trials, while more than one-third did not feel "very prepared" to assess scientific value or risks and benefits to participants [54]. This guidance document addresses these challenges by providing structured application notes and experimental protocols aligned with Belmont principles for researchers and IRBs navigating this complex landscape.
Current Landscape: Quantitative Analysis of Early-Phase Trial Challenges
IRB Preparedness and Perceived Challenges
A national survey of IRB chairs provides crucial insights into the current state of risk-benefit assessment for early-phase trials, highlighting significant operational and preparedness challenges that inform protocol development [54].
Table 1: IRB Chair Perspectives on Early-Phase Trial Review (n=148)
| Survey Dimension | Response Category | Percentage of Respondents |
|---|---|---|
| Perceived difficulty | Found early-phase more challenging than later phases | 66% |
| Self-rated performance | Felt IRB does "excellent" or "very good" job | 91% |
| Preparedness | Did not feel "very prepared" for key analysis aspects | 36% |
| Desire for resources | Valued additional standardized resources | 68% |
Phase-Specific Risk Characteristics
Understanding the distinct risk-benefit profiles across trial phases enables more precise ethical analysis and protocol design [55].
Table 2: Risk-Benefit Profiles Across Clinical Trial Phases
| Trial Phase | Primary Objectives | Typical Sample Size | Key Risk Considerations | Potential Benefits |
|---|---|---|---|---|
| Phase 0 | Microdosing to determine if agent reaches target | 10-15 | Minimal therapeutic benefit; burden of extra tests | Contributes to scientific knowledge |
| Phase I | Determine safety, dosage, and identify side effects | 10-30 | Highest uncertainty; dose-limiting toxicities | Possible therapeutic benefit in serious illnesses |
| Phase II | Assess efficacy and further evaluate safety | 25-100 | Efficacy uncertainty; less common side effects emerge | Higher likelihood of direct therapeutic benefit |
| Phase III | Compare to standard treatment; confirm efficacy | Hundreds to thousands | Risk of inferior outcomes compared to standard care | Potential access to superior new treatment |
Ethical Framework: Operationalizing Belmont Report Principles
Application of Foundational Ethical Principles
The Belmont Report establishes three fundamental principles that must be systematically applied to early-phase trial review [8]:
Respect for Persons: This principle requires acknowledging participant autonomy through comprehensive informed consent and protecting those with diminished autonomy. In early-phase trials, this necessitates explicit disclosure of the highly uncertain benefit-risk profile, including the primarily scientific rather than therapeutic purpose of the research. For early-phase oncology trials, this is particularly crucial as participants often have limited therapeutic options and may therapeutic misconception.
Beneficence: This principle extends beyond "do no harm" to maximizing possible benefits and minimizing possible harms. For IRBs reviewing early-phase trials, this requires rigorous assessment of preclinical evidence quality, particularly for neurology trials where "preclinical studies are frequently subject to numerous problems with both design and reporting" and "preclinical neuroscience studies are also plagued by publication bias in favor of positive studies" [54].
Justice: This principle requires fair participant selection and equitable distribution of risks and benefits. In early-phase trials, this demands scrutiny of participant vulnerability and avoidance of exploitation of populations with limited treatment options. IRB review must ensure that "subjects are selected fairly and that the risks and benefits of research are distributed equitably" [8].
Risk-Benefit Assessment Methodology
The Belmont Report outlines a systematic assessment method where IRBs "gather and assess information about all aspects of the research, and consider alternatives systematically and in a non-arbitrary way" [8]. The following diagram illustrates this systematic approach to risk-benefit assessment:
Systematic Risk-Benefit Assessment
Application Notes: Implementing Ethical Principles in Trial Design
Contemporary Regulatory and Methodological Framework
The SPIRIT 2025 guidelines provide an updated framework for protocol development that aligns with ethical requirements, emphasizing that "readers should not have to infer what was probably done; they should be told explicitly" [56]. Key enhancements relevant to early-phase trials include:
- Explicit Risk-Benefit Justification: Protocols must document how risks are justified by potential benefits to participants or society, with particular attention to uncertainty in early-phase studies.
- Comprehensive Preclinical Evidence Assessment: Given that "in numerous cases, early phase trials have been launched on the backs of equivocal, or even unfavorable, supporting preclinical evidence" [54], protocols must critically evaluate translational foundations.
- Structured Benefit Characterization: Clear differentiation between direct therapeutic benefit and scientific knowledge gains, with transparent communication to participants.
Advanced Analytics for Risk Mitigation
Modern clinical trial data analytics revolutionizes risk assessment in early-phase trials through several technological advancements [57] [58]:
- Predictive Analytics: Machine learning models trained on historical trial data can forecast patient responses and identify subtle safety signals, enabling proactive risk management.
- Real-World Data Integration: Analysis of electronic health records and other real-world data sources provides context for evaluating potential risks and designing more targeted trials.
- Centralized Monitoring Solutions: Risk-based monitoring approaches allow sponsors to focus resources on the highest risk aspects of trial conduct, improving both efficiency and participant protection.
Table 3: Research Reagent Solutions for Enhanced Risk-Benefit Assessment
| Tool Category | Specific Solutions | Function in Risk-Benefit Assessment |
|---|---|---|
| Data Collection Platforms | Electronic Data Capture (EDC) Systems, Clinical Data Management Systems (CDMS) | Standardize data collection, eliminate transcription errors, provide real-time safety monitoring |
| Risk Assessment Tools | Risk-Based Monitoring (RBM) solutions, Predictive Analytics models | Identify sites with potential quality issues, predict adverse events, enable targeted monitoring |
| Analytical Platforms | AI/ML algorithms, Biomarker Discovery tools | Analyze complex datasets to identify safety signals, predict treatment response, stratify patients |
| Participant-Centric Technologies | Wearable sensors, Digital biomarkers, Patient-reported outcome platforms | Provide continuous, objective safety data, capture patient experience, enhance benefit assessment |
Experimental Protocols: Structured Approaches to Risk-Benefit Analysis
Protocol 1: Preclinical Evidence Assessment
Purpose: Systematically evaluate the quality and translational potential of preclinical evidence supporting an early-phase trial.
Methodology:
- Evidence Quality Scoring: Adapt the SPIRIT 2025 framework to rate preclinical study quality across multiple dimensions [56]:
- Experimental design rigor (blinding, randomization, power analysis)
- Model system relevance to human pathophysiology
- Reproducibility across independent laboratories
- Publication bias assessment
Translational Concordance Analysis: Evaluate consistency of therapeutic effects across multiple model systems and dose ranges, with particular attention to "neuroscience preclinical studies, as the unique nature of human cognition, behavior, emotion, and volition means that there are no reliable animal models in which to study these phenomena" [54].
Safety Signal Integration: Systematically catalog and weight all observed adverse effects in preclinical studies, regardless of statistical significance or publication status.
Deliverable: Preclinical Evidence Assessment Report quantifying translational uncertainty and identifying potential risk areas requiring enhanced monitoring.
Protocol 2: Dose Optimization Strategy
Purpose: Implement FDA Project Optimus guidance to optimize dosing strategies rather than simply identifying maximum tolerated dose [59].
Methodology:
- Multi-Cohort Design: Implement parallel cohort expansions at multiple dose levels to characterize dose-response relationships for both efficacy and toxicity.
- Biomarker-Guided Escalation: Incorporate pharmacodynamic biomarkers to assess biological effects below maximum tolerated dose.
- Adaptive Design Elements: Utilize Bayesian adaptive methods to efficiently allocate participants to informative dose levels based on accumulating data.
Deliverable: Comprehensive dose optimization justification including safety, efficacy, and pharmacodynamic profiles across the tested dose range.
Protocol 3: Novel Endpoint Validation
Purpose: Develop and validate novel endpoints appropriate for early-phase trials of novel therapeutic modalities.
Methodology:
- Endpoint Hierarchy Establishment: Define primary, secondary, and exploratory endpoints with clear conceptual alignment with clinical benefit.
- Biomarker Qualification: For surrogate endpoints, establish mechanistic link to clinical outcomes and analytical validation using FDA Biomarker Qualification framework.
- Patient-Centered Outcome Integration: Incorporate patient-perspective endpoints through structured engagement and validated patient-reported outcome measures.
Deliverable: Validated endpoint package with documented measurement properties and clinical relevance.
Case Study: Novel Therapy Implementation with Ethical Framework
Application to Giredestrant in Breast Cancer
The phase 3 evERA Breast Cancer study evaluating giredestrant, a next-generation selective oestrogen receptor degrader, demonstrates practical application of risk-benefit principles in novel therapy development [60]:
Risk-Benefit Considerations:
- Novel Mechanism Advantage: Giredestrant's unique action as both a degrader and full antagonist potentially addresses resistance to existing endocrine therapies, justifying first-in-human trial risks.
- Patient Population Selection: Focus on ER-positive, HER2-negative advanced breast cancer patients with limited options and high unmet need aligns with justice principles.
- Administration Benefits: Oral administration convenience versus first-generation injectables represents meaningful non-efficacy benefit for participants.
Trial Outcomes: The giredestrant-everolimus combination demonstrated statistically significant improvement in progression-free survival (8.77 months versus 5.49 months) with manageable safety profile, validating the risk-benefit assessment in earlier trial phases [60].
Technology-Enhanced Risk Assessment Workflow
Modern clinical trial data analytics enables more dynamic risk-benefit assessment throughout trial conduct. The following diagram illustrates this continuous assessment process:
Continuous Risk-Benefit Assessment
Balancing risks and benefits in early-phase clinical trials requires systematic integration of ethical principles with modern methodological approaches. The Belmont Report provides the indispensable ethical foundation, while contemporary analytical technologies and regulatory frameworks offer practical implementation tools. As therapeutic modalities increase in complexity, maintaining this integration will be essential for advancing innovative treatments while upholding the highest standards of participant protection. IRBs and researchers should collaborate to implement these structured approaches, addressing the identified preparedness gaps through standardized processes and enhanced resources.
Maintaining Privacy and Confidentiality in the Era of Data Sharing and Genomics
The foundational ethical principles outlined in the Belmont Report—Respect for Persons, Beneficence, and Justice—provide a crucial framework for Institutional Review Board (IRB) protocols in genomic research [1]. As genomic technologies evolve, enabling unprecedented data sharing and analysis, implementing these principles requires careful consideration of privacy, confidentiality, and ethical data management practices. The integration of artificial intelligence, cloud computing, and multi-omics approaches has amplified both the potential benefits and ethical complexities of genomic research [61]. This document provides application notes and detailed protocols to help researchers, scientists, and drug development professionals maintain these ethical commitments while advancing genomic science.
Ethical Framework and Regulatory Landscape
Core Ethical Principles from the Belmont Report
The Belmont Report establishes three primary ethical principles for research involving human subjects, each with specific implications for genomic research [1]:
- Respect for Persons: Recognizes the autonomy of individuals and requires protecting those with diminished autonomy. In genomics, this translates to meaningful informed consent processes that clearly explain how genetic data will be used, stored, and shared, including any potential future research uses.
- Beneficence: Obligates researchers to maximize benefits and minimize potential harms. For genomic data, this requires implementing robust security measures to prevent unauthorized access or breaches that could lead to genetic discrimination or privacy violations.
- Justice: Demands fair distribution of research benefits and burdens. This principle necessitates addressing equitable access to genomic research participation and ensuring that data sharing practices do not exacerbate existing health disparities.
Current Regulatory Requirements and Guidance
Genomic research operates within a complex regulatory environment that continues to evolve. Key current requirements include:
- NIH Genomic Data Sharing (GDS) Policy: Applies to NIH-funded research generating large-scale genomic data, including genome-wide association studies (GWAS), single nucleotide polymorphism (SNP) arrays, and genome sequences [62]. The policy expects researchers to obtain Institutional Certification for genomic data sharing as part of the initial IRB application process.
- HIPAA Protections for Deceased Individuals: While the Common Rule only applies to living individuals, HIPAA privacy protections extend to an individual's protected health information for 50 years after death [63]. Research involving deceased individuals' genomic data requires proper authorization from family or a legally authorized executor.
- Enhanced Security for Sensitive Data: Recent analyses have identified significant national security risks associated with foreign access to American genomic data, leading to increased scrutiny of data management practices and recommendations for stronger oversight mechanisms [64].
Table: Key Regulatory Frameworks for Genomic Data Privacy
| Regulatory Framework | Scope/Application | Key Requirements |
|---|---|---|
| Belmont Report Ethical Principles | All human subjects research | Respect for Persons, Beneficence, Justice in research design and conduct |
| NIH Genomic Data Sharing Policy | NIH-funded large-scale genomic research | Data sharing, institutional certification, privacy protections |
| HIPAA Privacy Rule | Protected health information | Protections for 50 years after death, authorization requirements |
| SPIRIT 2025 Statement | Clinical trial protocols | 34-item checklist including data sharing plans and privacy protections |
Application Notes: Implementing Ethical Principles in Genomic Research
Informed Consent Protocols for Genomic Data Sharing
Obtaining meaningful informed consent represents a primary implementation of the Respect for Persons principle. Current best practices include:
- Tiered Consent Options: Provide participants with clear choices regarding future research use of their genomic data. Researchers should "limit the number of choices to avoid participant confusion and later administrative complexity" while still offering meaningful options [62].
- Comprehensive Data Sharing Disclosures: Clearly explain how data will be shared, including whether it will be deposited in controlled-access repositories, made available to commercial entities, or shared with international collaborators.
- Withdrawal Conditions: Specify whether participants can withdraw their data from repositories and any limitations on this right, particularly for data that has already been included in analyses or shared with other researchers.
Data Security and Access Control Measures
Implementing the Beneficence principle requires robust technical and administrative safeguards for genomic data:
- De-identification Standards: Remove direct identifiers from genomic data and specimens, storing the "key to the code" separately in a secure manner [62]. Note that complete anonymization of genomic data is increasingly challenging due to the inherent identifiability of genetic information.
- Access Tiering and Authentication: Implement tiered access controls based on data sensitivity, requiring stronger authentication for more sensitive datasets. The SPIRIT 2025 guidelines emphasize specifying data access procedures in research protocols [33].
- Security Compliance Monitoring: Develop procedures to "proactively and comprehensively monitor researcher compliance with data management and security measures" rather than relying solely on self-reporting [64].
Table: Documenting Data Security Implementation for IRB Protocols
| Security Domain | Implementation Evidence | Belmont Principle |
|---|---|---|
| Data Encryption | Specification of encryption standards for data at rest and in transit | Beneficence |
| Access Controls | Description of role-based access and authentication mechanisms | Respect for Persons |
| Data Monitoring | Procedures for auditing data access and detecting violations | Justice |
| International Transfers | Documentation of compliance with international data transfer restrictions | Justice |
Addressing Justice Considerations in Genomic Research
The Justice principle requires special attention to equitable implementation of genomic research:
- Vulnerable Population Protections: Implement additional safeguards when researching communities with historical experiences of research exploitation or limited access to healthcare resources.
- Global Equity Considerations: Be mindful of power asymmetries in international research collaborations, particularly when collecting data in settings "characterised by high deprivation, risk and power asymmetries" [65].
- Benefit Sharing: Develop plans to ensure that research benefits, such as access to resulting therapies or diagnostics, are distributed fairly among contributing populations.
Experimental Protocols for Genomic Privacy Protection
Protocol: Implementing Federated Learning for Privacy-Preserving Genomic Analysis
Background: Federated learning enables training machine learning models on decentralized genomic data without transferring sensitive information to central servers, aligning with the Beneficence principle by minimizing privacy risks.
Materials:
- Research Reagent Solutions:
- Federated Learning Framework: Software platform (e.g., NVIDIA FLARE, Flower) for coordinating distributed model training
- Differential Privacy Library: Tools (e.g., TensorFlow Privacy, OpenDP) for adding calibrated noise to protect individual data points
- Secure Multi-Party Computation Protocols: Cryptographic tools for privacy-preserving collaborative analysis
- Homomorphic Encryption Libraries: Software (e.g., Microsoft SEAL, PALISADE) enabling computation on encrypted genomic data
Procedure:
- Initialization Phase:
- Deploy standardized containerized analysis environments to each participating institution
- Implement identity verification and authentication mechanisms for all nodes
- Establish secure communication channels between coordinating server and participating sites
Model Training Cycle:
- Distribute initial global model to all participating sites
- Each site trains model locally on their genomic data without transferring raw data
- Sites submit only model parameter updates to coordinating server
- Aggregate updates using secure aggregation protocols
- Update global model and repeat until convergence criteria met
Privacy Protection Measures:
- Apply differential privacy mechanisms to model updates before transmission
- Implement secure multi-party computation for aggregation steps
- Log all data access attempts and model interactions for audit purposes
Validation and Testing:
- Evaluate final model performance on held-out test datasets
- Assess privacy protection levels through formal privacy analysis
- Document model performance characteristics and potential limitations
Protocol: Ethical Framework Implementation for IRB Review of Genomic Studies
Background: This protocol provides a structured approach for IRBs to evaluate genomic research protocols through the lens of Belmont Report principles, ensuring comprehensive ethical review.
Materials:
- Research Reagent Solutions:
- Belmont Principle Assessment Checklist: Structured tool for evaluating Respect for Persons, Beneficence, and Justice implementations
- Genomic Data Sharing Impact Questionnaire: Instrument for assessing privacy risks of proposed data sharing practices
- Vulnerable Population Protection Guidelines: Special considerations for research involving potentially vulnerable groups
- Data Security Verification Tools: Checklists for reviewing technical and administrative safeguards
Procedure:
- Respect for Persons Evaluation:
- Review informed consent documents for clarity about genomic data uses
- Verify participants receive clear information about future research uses and sharing practices
- Assess whether consent process allows meaningful choices about data participation levels
- Confirm provisions for participant withdrawal of data where feasible
Beneficence Assessment:
- Evaluate data security plans for protecting genomic information
- Review procedures for handling incidental findings and returning results to participants
- Assess balance of potential benefits against privacy risks and psychological harms
- Verify plans for genetic counseling resources when appropriate
Justice Analysis:
- Examine participant selection criteria for fair inclusion and exclusion
- Review plans for equitable distribution of research benefits
- Assess potential for the research to exacerbate health disparities
- Evaluate fair access to research participation across diverse populations
Documentation and Approval:
- Document specific measures addressing each ethical principle
- Identify any required protocol modifications to meet ethical standards
- Provide clear rationale for approval decisions with reference to Belmont principles
- Specify ongoing monitoring requirements for approved genomic studies
Protocol: Secure Genomic Data Repository Management
Background: Secure repositories for genomic data must implement comprehensive privacy protections while enabling appropriate research access, balancing the Belmont principles of Beneficence (through security) and Justice (through appropriate access).
Materials:
- Research Reagent Solutions:
- Data Use Agreement Templates: Standardized agreements specifying permitted data uses and security requirements
- Data Access Committee Governance Framework: Structured processes for reviewing and approving data access requests
- Security Audit Tools: Software for monitoring compliance with data security policies
- Violation Reporting System: Mechanisms for reporting and investigating potential data security breaches
Procedure:
- Repository Establishment:
- Implement tiered access levels based on data sensitivity and researcher credentials
- Deploy encryption for data at rest and in transit using current standards
- Establish data use agreements specifying permitted research uses and security requirements
- Create data access committees with appropriate expertise to review requests
Access Management:
- Require researcher certification in ethical data handling practices
- Implement multi-factor authentication for repository access
- Log all data access and queries for audit purposes
- Conduct regular reviews of authorized users and their access levels
Security Monitoring:
- Perform proactive audits of researcher compliance with data security measures
- Monitor for unusual access patterns or data download activities
- Implement automated alerts for potential security violations
- Conduct periodic penetration testing and vulnerability assessments
Violation Response:
- Establish clear procedures for investigating potential security violations
- Define consequences for policy violations, including access revocation
- Develop communication protocols for reporting breaches to affected individuals
- Maintain records of violations and corrective actions taken
Table: Common Genomic Data Security Violations and Prevention Strategies
| Violation Type | Examples | Prevention Strategies |
|---|---|---|
| Research Conduct Outside Approved Scope | Using data for unapproved research purposes | Clear data use agreements, regular audits of research outputs |
| Security Breaches | Compromised servers, unauthorized access | Strong authentication, encryption, network monitoring |
| Improper Data Sharing | Sharing with unauthorized collaborators | Access controls, training, data use agreements |
| Inadequate De-identification | Failure to remove direct identifiers | Automated de-identification tools, verification processes |
Emerging Challenges and Future Directions
Genomic research continues to evolve rapidly, presenting new ethical challenges for implementing Belmont Report principles:
- Artificial Intelligence Integration: As AI and machine learning become increasingly embedded in genomic analysis, new privacy challenges emerge related to model inversion attacks and membership inference attacks that could potentially re-identify individuals [61].
- Cross-Border Data Sharing: Increasing international collaboration creates complex jurisdictional issues for data protection, particularly with identified risks of foreign access to genomic data [64].
- Multi-Omics Integration: Combining genomic data with other data types (transcriptomics, proteomics, metabolomics) increases re-identification risks and complicates privacy protection efforts [61].
- Direct-to-Consumer Genomics: The growing direct-to-consumer genetic testing market creates new data ecosystems with varying privacy standards and consent mechanisms [61].
Future protocol development must address these evolving challenges while maintaining fidelity to the foundational ethical principles established in the Belmont Report. Ongoing monitoring of technological developments and regular updates to security protocols will be essential for maintaining privacy and confidentiality in genomic research.
Benchmarking Belmont: Validating Your Approach Through Comparative Ethical Frameworks
The evolution of ethical frameworks from the Nuremberg Code to the Belmont Report represents a critical transformation in the protection of human research subjects. This transition marks a shift from a singular focus on voluntary consent to a comprehensive system of three ethical principles and their practical applications [1]. The development of these guidelines emerged from necessary responses to historical ethical failures, beginning with the atrocities of Nazi medical experiments and continuing through domestic scandals like the Tuskegee Syphilis Study [23] [66]. For contemporary researchers and institutional review boards (IRBs), understanding this evolution is not merely an academic exercise but a fundamental requirement for implementing ethically sound research protocols that protect participant autonomy, welfare, and rights while facilitating scientifically valid inquiry.
The Nuremberg Code, established in 1947 as a direct response to the horrors revealed during the Doctors' Trial, laid the essential foundation by emphasizing voluntary consent as its first and absolute principle [1] [23]. However, this initial framework proved insufficient to address complex ethical challenges in research, particularly involving vulnerable populations or balancing risks and benefits [1]. Decades later, the Belmont Report, published in 1979, expanded this foundation into a comprehensive three-principle system that now underpins modern ethical oversight and IRB protocols [8] [2]. This document explores both the historical context and practical applications of this ethical evolution, providing researchers with actionable guidance for implementing these principles within contemporary research settings.
Historical Context: From Nuremberg to Belmont
The Nuremberg Code (1947)
The Nuremberg Code emerged from the 1947 military tribunal prosecuting Nazi physicians for unethical human experimentation conducted in concentration camps [23] [2]. American judges presiding over the case developed a 10-point code establishing standards for ethical human research, with the absolute requirement of voluntary consent as its cornerstone [23]. The Code's first principle explicitly states that the human subject "should have sufficient knowledge and comprehension of the elements of the subject matter involved as to enable him to make an understanding and enlightened decision" [23]. This represented a radical departure from previous practices where researcher discretion primarily governed participant treatment.
The Code additionally established other foundational concepts, including the requirement that experiments should yield fruitful results for the good of society, be based on prior animal testing and natural history knowledge, avoid unnecessary physical and mental suffering, not conduct experiments where death or disabling injury is expected, and have risks that never exceed humanitarian importance [23] [67]. Despite its comprehensive nature, the Nuremberg Code had significant limitations in its applicability to medical research contexts and provided insufficient guidance for protecting vulnerable populations who might not possess decision-making capacity [1] [2].
The Declaration of Helsinki (1964)
Adopted by the World Medical Association in 1964, the Declaration of Helsinki built upon the Nuremberg Code by distinguishing between clinical research combined with professional care and non-therapeutic clinical research [1]. This distinction acknowledged that research ethics required more nuanced approaches than the Nuremberg Code provided. The Declaration introduced the concept of independent committee review (the precursor to modern IRBs) and emphasized that participant welfare should always take precedence over scientific and societal interests [1] [67].
A critical advancement in the Declaration was its attention to vulnerable populations and the need for special protections when research participants could not provide fully autonomous consent [1]. Whereas the Nuremberg Code focused primarily on the competent adult individual, the Declaration of Helsinki acknowledged that certain populations required additional safeguards, though specific guidance for implementing these protections remained limited in early versions [1].
The Tuskegee Syphilis Study and Public Outcry
The Tuskegee Syphilis Study (1932-1972) conducted by the U.S. Public Health Service represented a profound ethical failure in domestic research [66]. In this study, 600 African American men—399 with latent syphilis and 201 as controls—were deceived about their condition and denied effective treatment even after penicillin became the standard cure in 1947 [66]. Participants were misled into believing they were receiving treatment when in fact researchers were observing the natural progression of untreated syphilis [66].
The study's exposure in 1972 sparked public outrage and directly led to the National Research Act of 1974, which created the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research [23] [66]. This Commission was charged with identifying comprehensive ethical principles for human subjects research, culminating in the Belmont Report [66] [2].
Comparative Analysis: Nuremberg Code vs. Belmont Report
Table 1: Fundamental Differences Between the Nuremberg Code and Belmont Report
| Aspect | Nuremberg Code (1947) | Belmont Report (1979) |
|---|---|---|
| Primary Focus | Individual voluntary consent | Comprehensive three-principle system |
| Core Principles | Voluntary consent; assessment of risks and benefits | Respect for persons, beneficence, justice |
| View of Subjects | Autonomous decision-makers | Persons with varying degrees of autonomy |
| Application Scope | All human research | All human research with specific guidance |
| Vulnerable Populations | Limited consideration | Explicit protections and considerations |
| Regulatory Impact | Limited direct adoption in U.S. law | Directly influenced U.S. federal regulations (Common Rule) |
| Implementation Mechanism | Researcher responsibility | Institutional Review Board (IRB) oversight |
From Single Principle to Comprehensive Framework
The Nuremberg Code established voluntary consent as the absolute essential requirement for ethical research, stating that "the voluntary consent of the human subject is absolutely essential" [23]. This principle reflected the specific context of its creation—a response to the coerced participation of concentration camp prisoners in brutal experiments [1]. While the Code mentioned other considerations like risk-benefit assessment and scientific validity, it positioned voluntary consent as the non-negotiable foundation [23].
The Belmont Report significantly expanded this framework by identifying three fundamental ethical principles: respect for persons, beneficence, and justice [8]. This tripartite system acknowledged that ethical research requires more than just autonomous consent—it demands active protection of participants' welfare and equitable distribution of research benefits and burdens [8] [2]. The Report explicitly recognized that while autonomy is crucial, many potential research participants have diminished autonomy requiring additional protections [8].
Practical Applications and Regulatory Implementation
The Belmont Report translated its three ethical principles into specific applications for research practice: informed consent (derived from respect for persons), assessment of risks and benefits (derived from beneficence), and selection of subjects (derived from justice) [1] [8]. This practical framework provided IRBs with systematic approaches for reviewing research protocols, moving beyond the Nuremberg Code's primary focus on consent alone [1].
Whereas the Nuremberg Code had limited direct influence on U.S. regulations, the Belmont Report directly shaped the Common Rule (45 CFR 46)—the federal policy for human subjects protection adopted by multiple federal agencies [1] [2]. The Report's principles are clearly reflected in regulations governing gene therapy clinical trials and policies requiring public review of approved protocols [1]. This regulatory impact has made the Belmont Report the foundational document for IRB operations at institutions conducting federally-funded research [8].
Implementing Belmont Report Principles in IRB Protocols
Application of Respect for Persons
The principle of respect for persons incorporates two ethical convictions: individuals should be treated as autonomous agents, and persons with diminished autonomy are entitled to protection [8]. In practical IRB protocol implementation, this principle requires researchers to:
- Ensure subjects enter research voluntarily with adequate information presented in comprehensible terms [8]
- Provide comprehensive information including research procedures, purposes, risks and anticipated benefits, alternative procedures, and the right to ask questions and withdraw at any time [8]
- Implement additional safeguards for populations with diminished autonomy (children, prisoners, individuals with impaired decision-making capacity) [8]
- Honor participant privacy and maintain confidentiality of data [8]
For IRB applications, researchers must detail specific procedures for assessing and ensuring comprehension, especially when working with vulnerable populations. The protocol should explicitly address how informed consent will be obtained, documented, and periodically reaffirmed for longitudinal studies [8] [52].
Application of Beneficence
The principle of beneficence obligates researchers to secure participants' well-being through two complementary rules: "do not harm" and "maximize possible benefits and minimize possible harms" [8]. Practical implementation requires:
- Systematic assessment of risks and benefits [8]
- Ensuring that risks are reasonable in relation to anticipated benefits [2]
- Implementing procedures to minimize risks through careful study design [8]
- Establishing data monitoring plans to identify unforeseen risks during the study [2]
In IRB protocols, researchers must provide detailed risk-benefit analyses that justify the research design and demonstrate appropriate risk minimization strategies [8] [52]. The protocol should explicitly address how the research design maximizes potential benefits while reducing risks to the fullest extent possible [8].
Application of Justice
The principle of justice requires the fair selection of research subjects and equitable distribution of research benefits and burdens [8]. Implementation requires researchers to:
- Avoid systematically selecting subjects based on easy availability, compromised position, or societal biases [8]
- Ensure inclusion and exclusion criteria relate directly to the research problem rather than convenience [8]
- Distribute research benefits and burdens fairly across potential participant populations [2]
- Consider whether vulnerable populations are being targeted for potentially high-risk research that primarily benefits other groups [8]
In IRB applications, researchers must justify subject selection criteria and demonstrate that participant pools appropriately represent populations that might benefit from the research findings [8] [52]. The protocol should address whether any groups are unjustly excluded from potential benefits of participation [2].
Experimental Protocols and Methodologies
Protocol for Ethical Risk-Benefit Assessment
Table 2: Systematic Risk-Benefit Assessment Protocol
| Assessment Phase | Methodology | Documentation Requirement |
|---|---|---|
| Pre-Study Risk Identification | Comprehensive literature review; consultation with content experts; review of similar studies | Table of identified risks with likelihood and severity estimates |
| Benefit Analysis | Identification of direct and societal benefits; consideration of knowledge advancement | Description of potential benefits to participants and society |
| Risk Minimization Planning | Protocol modifications; safety monitoring plans; inclusion/exclusion criteria refinement | Detailed procedures for risk reduction with rationale |
| Risk-Benefit Justification | Comparison of minimized risks to anticipated benefits; consideration of alternatives | Narrative justification explaining net benefit |
| Ongoing Monitoring | Data safety monitoring plan; stopping rules for unacceptable risks | Schedule for periodic review; adverse event reporting procedures |
The IRB protocol must detail a systematic approach to risk-benefit assessment, following the Belmont Report's guidance that researchers and review bodies should gather and assess information about all aspects of the research and consider alternatives systematically [8]. This methodology aims to make the assessment process more rigorous and communication between the IRB and investigator less ambiguous [8].
Protocol for Informed Consent Implementation
The informed consent process must extend beyond simple documentation to ensure genuine comprehension and voluntary participation. Implementation protocols should include:
- Comprehension assessment through teach-back methods or simple questionnaires [68]
- Process consenting for longitudinal studies with ongoing consent discussions [8]
- Cultural and linguistic appropriateness of consent materials [52]
- Vulnerable population adaptations including assent procedures for children and consent capacity assessment for cognitively impaired adults [8] [2]
The IRB application should include all consent documents, recruitment materials, and detailed procedures for ensuring participant comprehension [52]. For research involving non-English speakers, translated materials and interpreter services must be documented [52].
Visualization of Ethical Framework Evolution
Diagram 1: Evolution of Research Ethics Framework
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Protocol Components for Ethical Research Implementation
| Component | Function | Implementation Example |
|---|---|---|
| Comprehensive Consent Template | Ensures all required elements of informed consent are included | Template including research purpose, procedures, risks, benefits, alternatives, confidentiality, contacts, voluntary participation |
| Vulnerable Population Protocol | Additional safeguards for participants with diminished autonomy | Child assent forms; consent capacity assessment tools; prisoner advocate consultation |
| Risk-Benefit Worksheet | Systematic approach to risk-benefit analysis | Structured template identifying physical, psychological, social, economic risks; direct/indirect benefits; risk minimization strategies |
| Data Safety Monitoring Plan | Ongoing protection of participant welfare during study | Independent data monitoring committee; predefined stopping rules; adverse event reporting procedures |
| Cultural Competence Guide | Ensures appropriateness for diverse populations | Translation resources; cultural consultation; community advisory board formation |
| Ethical Framework Checklist | Aligns protocol with Belmont principles | Checklist verifying respect for persons, beneficence, and justice applications throughout research design |
The evolution from the Nuremberg Code's foundational emphasis on voluntary consent to the Belmont Report's comprehensive three-principle framework represents significant maturation in research ethics oversight. For today's researchers and IRB professionals, this evolution necessitates protocol designs that simultaneously address autonomous decision-making, risk-benefit optimization, and equitable subject selection. The integration of these frameworks enables more nuanced ethical analysis than either document alone provides.
Contemporary research challenges—including global clinical trials, genetic research, and studies involving vulnerable populations—require the sophisticated ethical analysis made possible by combining Nuremberg's emphasis on voluntary participation with Belmont's systematic principles [1] [2]. Successful IRB protocols explicitly demonstrate how all three Belmont principles inform study design, implementation, and monitoring. By understanding this ethical evolution and implementing these comprehensive frameworks, researchers contribute to maintaining public trust while advancing scientific knowledge ethically and responsibly.
The Belmont Report and the Declaration of Helsinki constitute foundational pillars for ethical human subjects research. While often mentioned together, they serve distinct purposes and audiences. The Declaration of Helsinki establishes a global framework of ethical principles primarily for physicians engaged in medical research, emphasizing patient welfare and care within the research context [69]. In contrast, the Belmont Report provides an ethical foundation for researchers and Institutional Review Boards (IRBs) in the United States, outlining principles that directly informed U.S. federal regulations [8] [1]. This application note delineates the specific responsibilities mandated by each document, providing protocols for their effective implementation within IRB frameworks and modern drug development.
Core Principles and Comparative Analysis
The Declaration of Helsinki: A Physician's Ethical Compass
The World Medical Association's Declaration of Helsinki, first adopted in 1964 and revised numerous times, is a statement of ethical principles for physicians conducting medical research involving human participants [69] [70]. It distinguishes between medical research and medical care, asserting that the patient's health and well-being must be the physician's first consideration [69]. Its core principles include:
- Patient-Physician Relationship: It binds the physician with the words of the Declaration of Geneva: "The health and well-being of my patient will be my first consideration" [69].
- Risk-Benefit Assessment: Requires that medical research involving human participants may only be conducted if the importance of the objective outweighs the risks and burdens to the research participants [69].
- Vulnerable Populations and Justice: Mandates that groups underrepresented in medical research should be provided appropriate access to participation, while those in situations of vulnerability should receive specific protections [69].
- Informed Consent: Emphasizes free and informed consent as an essential component of respect for individual autonomy, requiring detailed information disclosure in plain language [69].
The Belmont Report: A Framework for Researcher and IRB Oversight
The Belmont Report, issued in 1979, identifies three fundamental ethical principles for all human subject research in the U.S. [8] [1]. It was created by the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research and directly influenced U.S. federal regulations. Its three principles are:
- Respect for Persons: This principle acknowledges the autonomy of individuals and requires protecting those with diminished autonomy. It translates into the requirement for informed consent, ensuring subjects enter research voluntarily with adequate information [8].
- Beneficence: This principle requires not only avoiding harm but also maximizing possible benefits and minimizing possible harms. This leads to a systematic assessment of risks and benefits [8].
- Justice: This principle addresses the fair distribution of the burdens and benefits of research, requiring that subjects are selected fairly and not simply because of their easy availability or compromised position [8].
Comparative Analysis of Key Elements
Table 1: Comparative Analysis of the Declaration of Helsinki and Belmont Report
| Aspect | Declaration of Helsinki | Belmont Report |
|---|---|---|
| Primary Audience | Physicians globally [69] [71] | U.S. Researchers, IRBs, & regulators [8] [71] |
| Core Ethical Foundation | Physician's duty to prioritize patient health; distinctions between research and care [69] | Three principles: Respect for Persons, Beneficence, Justice [8] |
| Scope & Focus | Medical research involving human participants [69] [70] | All biomedical and behavioral research involving human subjects [8] [1] |
| Informed Consent Emphasis | Full disclosure of aims, methods, funding, conflicts of interest; right to withdraw; specific information for vulnerable groups [69] | Voluntariness, comprehension, disclosure of key information (procedures, risks, benefits, alternatives) [67] [8] |
| Regulatory Impact | International gold standard; influences international guidelines and journal requirements [67] [71] | Directly foundational to U.S. Common Rule (45 CFR 46) and FDA regulations [8] [1] |
| Role in IRB Review | Provides high-level ethical principles for committee consideration [67] | Serves as the primary ethical framework for IRB review in the U.S.; provides a method for risk/benefit justification [8] |
Table 2: Quantitative Data on Document Evolution and Influence
| Document | Year of Origin | Number of Revisions (as of 2025) | Core Principles/Elements | Primary Geographic Influence |
|---|---|---|---|---|
| Declaration of Helsinki | 1964 [69] | 10+ (latest 2024) [70] | 32 paragraphs in 3 sections [67] | Global [71] |
| Belmont Report | 1979 [8] [1] | 1 (unchanged) | 3 Principles, 3 Applications [8] | United States [71] [1] |
Implementation Protocols for IRBs and Researchers
Protocol 1: Integrating Ethical Frameworks into IRB Review Workflows
This protocol ensures IRB protocols systematically address the requirements of both ethical frameworks.
Workflow Diagram 1: Ethical Review Process for IRB Protocols
Procedure:
- Protocol Submission: Researchers submit complete study documentation.
- Administrative Review: IRB staff verify completeness and correct formatting.
- Ethical Principle Assessment: The IRB committee conducts a systematic review against both frameworks.
- Belmont Report Application:
- Respect for Persons: Scrutinize informed consent documents for clarity, comprehensiveness, and absence of coercive language. Assess process for subjects with diminished autonomy [8].
- Beneficence: Systematically evaluate the risk-benefit ratio. Ensure risks are minimized and justified by potential benefits to subjects or society [8].
- Justice: Evaluate subject selection criteria to ensure fair distribution of burdens and benefits, avoiding vulnerable populations solely for administrative convenience [8].
- Declaration of Helsinki Application:
- Physician & Patient Welfare: Verify that the protocol design prioritizes participant health and well-being, especially when research is combined with care [69].
- Vulnerable Population Check: Confirm that appropriate safeguards and justifications are in place if the research includes vulnerable groups [69].
- Belmont Report Application:
- Committee Deliberation: The IRB discusses findings and identifies required modifications.
- Decision & Communication: The IRB communicates its approval, modifications required, or disapproval to the researcher.
Protocol 2: Informed Consent Document Development
This protocol provides a detailed methodology for creating informed consent documents that satisfy both Belmont and Helsinki standards.
Table 3: Essential Elements for Informed Consent Documents
| Element | Belmont Report Requirement [67] [8] | Declaration of Helsinki Requirement [67] [69] | Implementation Protocol |
|---|---|---|---|
| Research Nature | Identification of study as research; description of procedures [67] | Aims, methods, sources of funding, researcher affiliations [67] [69] | Use a clear title and header stating "Research Study." Describe procedures timeline and all involved institutions. |
| Risks & Benefits | Description of foreseeable risks and potential benefits [67] [8] | Anticipated benefits, potential risks, and burdens [67] [69] | List risks and benefits separately. Differentiate direct benefits to subjects from societal benefits. |
| Voluntariness | Statement that participation is voluntary [67] | Right to refuse and withdraw without reprisal [67] [69] | Include explicit statements: "Your participation is voluntary," and "You may quit at any time without penalty." |
| Alternative Procedures | Disclosure of alternative procedures if study involves therapy [67] [8] | (Implied in the context of research combined with care) [69] | For therapeutic research, list standard treatment options available outside the study. |
| Contact Information | Opportunity to ask questions; contact name [67] | Contact name for further information [67] [69] | Provide names and 24/7 contact information for the Principal Investigator and the IRB. |
| Conflicts of Interest | (Not explicitly listed) | Potential conflicts of interest [67] [69] | Disclose sponsor, significant payments to investigators, and any institutional financial interests. |
Experimental Protocol for Consent Validation:
- Objective: To assess the readability, comprehension, and voluntariness of the informed consent document.
- Materials: Draft consent document, validated readability assessment tool, comprehension questionnaire.
- Procedure:
- Readability Assessment: Apply assessment tools to ensure the document is at an 8th-grade reading level or lower.
- Pilot Testing: Recruit 5-10 individuals from the study's target population. Ask them to read the document.
- Comprehension Testing: Administer a questionnaire assessing understanding of key study aspects: purpose, procedures, risks, benefits, alternatives, voluntariness, and right to withdraw.
- Debriefing: Interview participants about their perception of the document's clarity and any perceived pressure to participate.
- Data Analysis: Calculate comprehension scores for each key area. A predetermined threshold must be met before the consent form is deemed acceptable for use.
- Document Revision: Revise the consent form based on feedback to address areas of poor comprehension or ambiguity.
The Scientist's Toolkit: Essential Reagents for Ethical Research
Table 4: Key Research Reagent Solutions for Ethical Protocol Implementation
| Tool/Reagent | Function in Ethical Research | Application Example |
|---|---|---|
| Informed Consent Templates | Standardizes disclosure of all required ethical elements, ensuring consistency and compliance. | IRB-provided templates pre-populated with required language for withdrawal rights and contact information. |
| Readability Assessment Software | Quantifies the reading level of consent documents, ensuring comprehension for the target population. | Using tools to revise a complex consent form from a 12th-grade to an 8th-grade reading level. |
| Vulnerability Assessment Checklist | Systematically identifies participants requiring additional protections, addressing Justice and vulnerability. | A checklist for studies involving children, prisoners, or cognitively impaired individuals to trigger specific safeguards. |
| Data Safety Monitoring Plan | Operationalizes the principle of Beneficence by providing a formal mechanism to monitor risks throughout the study. | A predefined plan for an independent data committee to review unblinded safety data in a high-risk clinical trial. |
| Conflict of Interest Disclosure Form | Manages potential compromises of researcher objectivity, a key requirement of the Declaration of Helsinki. | Mandatory annual disclosure of financial interests for all researchers involved in human subjects research. |
Successfully navigating the landscape of research ethics requires a nuanced understanding of how the Belmont Report and Declaration of Helsinki complement each other. The Belmont Report provides the foundational ethical principles for U.S. researchers and IRBs, while the Declaration of Helsinki outlines the specific duties of physicians engaged in global medical research. By implementing the structured protocols and tools provided in this application note, research professionals can ensure their work not only complies with regulatory requirements but also upholds the highest standards of ethical integrity, thereby protecting research participants and advancing science responsibly.
The Belmont Report's Direct Influence on 45 CFR 46 and the Common Rule
The Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research, published in 1979, established the foundational ethical framework for research involving human subjects in the United States [25]. Created by the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research, the report was drafted in direct response to ethical abuses in research, most notably the Tuskegee Syphilis Study [23]. Its primary legacy lies in its direct influence on the codification of federal regulations, particularly the Federal Policy for the Protection of Human Subjects, commonly known as the Common Rule (45 CFR Part 46) [25] [16]. This document provides detailed application notes and protocols for researchers, scientists, and drug development professionals to implement the Belmont Report's ethical principles within Institutional Review Board (IRB) protocols and research practices.
The Three Ethical Principles and Their Regulatory Corollaries
The Belmont Report elucidates three fundamental ethical principles: Respect for Persons, Beneficence, and Justice [8]. The following table summarizes these principles and their practical applications in regulatory oversight.
Table 1: Core Ethical Principles of the Belmont Report and Their Regulatory Applications
| Ethical Principle | Definition | Regulatory Application in 45 CFR 46 |
|---|---|---|
| Respect for Persons | Recognizes the autonomy of individuals and requires protection for those with diminished autonomy [8] [11]. | Informed Consent (§46.116): Requirements for information disclosure, comprehension, and voluntariness [8] [72]. |
| Beneficence | Obligates researchers to maximize benefits and minimize possible harms to subjects [8] [11]. | Assessment of Risks and Benefits (§46.111): Systematic IRB review to ensure risks are justified and minimized [8]. |
| Justice | Requires the fair distribution of both the burdens and benefits of research [8] [11]. | Selection of Subjects (§46.111): Equitable selection of subjects to avoid vulnerable populations bearing disproportionate risks [8]. |
Direct Regulatory Influence and the Evolution of the Common Rule
Codification into Federal Regulation
The Belmont Report's principles are explicitly embedded within the Code of Federal Regulations. 45 CFR 46.101(c) states that department or agency heads retain final judgment on covered activities and "this judgment shall be exercised consistent with the ethical principles of the Belmont Report" [73]. Furthermore, §46.101(i) allows for waivers of certain policy provisions provided that alternative procedures are "consistent with the principles of the Belmont Report" [73]. This direct referencing establishes the Belmont Report as the ethical standard for interpreting and applying the federal regulations [1].
The Common Rule and Its Revisions
The Common Rule, first published in 1991 and codified by 15 federal departments and agencies, is the primary embodiment of the Belmont Report's principles in U.S. research regulation [16]. The "Revised Common Rule," which took effect in 2019, modernized the regulations but retained the Belmont Report as its ethical foundation [16] [72] [74]. Key updates, such as new requirements for informed consent to facilitate a prospective subject's understanding, further operationalize the principle of Respect for Persons [72].
Protocol Implementation: Translating Principles into Practice
Experimental Workflow for Ethical Protocol Design
The following diagram illustrates a systematic workflow for designing research protocols that integrate Belmont principles into IRB review and research execution.
The Researcher's Toolkit: Essential Reagents for Ethical Research
This toolkit outlines critical components for implementing the Belmont principles in human subjects research.
Table 2: Essential Research Reagents for Ethical Protocol Implementation
| Tool/Reagent | Function in Ethical Implementation | Relevant Ethical Principle |
|---|---|---|
| Comprehensive Consent Form | Provides clear, organized information to facilitate subject understanding and voluntary choice [72]. | Respect for Persons |
| Risk-Benefit Assessment Matrix | A structured tool to document and systematically compare potential harms and anticipated benefits [8]. | Beneficence |
| Subject Recruitment Plan | Details inclusion/exclusion criteria and recruitment methods to ensure equitable selection and avoid targeting vulnerable groups [8]. | Justice |
| IRB Protocol Application | Formal document for ethical review, ensuring regulatory compliance with 45 CFR 46 [73] [74]. | All Three Principles |
| Data Safety Monitoring Plan (DSMP) | Protocol for ongoing review of data to ensure subject safety and research integrity during execution. | Beneficence |
| Assent Documents (for children) | Age-appropriate materials to obtain agreement from subjects incapable of giving full consent [11]. | Respect for Persons |
Detailed Methodology: Implementing the Informed Consent Process
The following protocol provides a step-by-step methodology for implementing the principle of Respect for Persons through a meaningful informed consent process, as required by §46.116 [72].
Protocol Title: Informed Consent Process for Non-Exempt Human Subjects Research
Objective: To ensure prospective subjects or their legally authorized representatives are provided with information necessary for a voluntary, informed, and comprehended decision about research participation.
Materials:
- IRB-approved informed consent document(s)
- Layperson-friendly summaries or visual aids (if applicable)
- Quiet, private space for discussion
- Documentation method (signed form, electronic record, or IRB-approved waiver of documentation)
Procedure:
- Pre-Interaction Preparation: Verify the use of the most recent IRB-approved consent form and version. All study team members interacting with potential subjects must be trained on the protocol and consent process.
- Initial Engagement and Setting: Engage the potential subject in a private setting with minimal distractions. Clearly introduce yourself as a researcher and state that you are inviting them to participate in a research study.
- Presentation of Key Information: Begin the conversation with a concise and focused presentation of the key information most likely to assist in understanding the reasons for or against participation, as required by §46.116(a)(5) [72]. This includes:
- The fact that this is a research study.
- The purpose of the research, its expected duration, and the procedures involved.
- The reasonably foreseeable risks or discomforts.
- The reasonably expected benefits, if any, to the subject or others.
- Appropriate alternative procedures or courses of treatment, if any.
- Detailed Explanation: Proceed through the entire consent document, section by section. Use language that is understandable to the subject, avoiding technical jargon. Key topics to emphasize include:
- The voluntary nature of participation and the right to withdraw at any time without penalty.
- Procedures for maintaining privacy and confidentiality of records.
- Whom to contact for answers to questions about the research, research subjects' rights, and in the event of a research-related injury.
- If applicable, disclose any prospective clinical trial consent form posting plans [74] and the possibility of commercial profit from the research [72].
- Assessment of Understanding: Use the "teach-back" method by asking open-ended questions (e.g., "Can you tell me in your own words what this study involves?") to assess the subject's comprehension of the key elements.
- Authorization / Documentation: After all questions are answered and understanding is confirmed, provide the subject sufficient time to make their decision. Obtain legally effective informed consent by having the subject or their legally authorized representative sign the IRB-approved consent form, unless this requirement has been waived by the IRB.
- Post-Consent Provision: Provide the subject with a copy of the signed consent document.
Advanced Applications and Contemporary Challenges
Ethical Review and Decision Matrix for IRBs
IRB members can utilize the following structured matrix to guide ethical review and ensure the principles of the Belmont Report are satisfied during protocol evaluation.
Table 3: IRB Ethical Review Decision Matrix
| Review Dimension | Guiding Questions for IRB Review | Belmont Principle |
|---|---|---|
| Informed Consent | Does the process ensure comprehension? Is it free of coercion? Are protections for vulnerable populations adequate? [8] [72] | Respect for Persons |
| Risk-Benefit Analysis | Are risks minimized? Are the risks reasonable in relation to the knowledge gained? Is data monitoring sufficient? [8] | Beneficence |
| Subject Equity | Are the subjects selected fairly? Is the recruitment pool appropriate for the research goals? Are vulnerable populations protected from overuse? [8] | Justice |
| Privacy & Confidentiality | Are there adequate provisions to protect subject privacy and the confidentiality of data? [8] | Respect for Persons, Beneficence |
| Protocol Integrity | Is the research design sound enough to yield valuable data, thereby justifying the use of human subjects? [23] | Beneficence, Justice |
Navigating Principle Conflicts in Complex Research
The Belmont Principles can conflict, requiring careful balancing. Research involving children exemplifies this challenge: a child's dissent (Respect for Persons) may conflict with a guardian's permission to enroll the child in research that offers direct benefit (Beneficence) or benefits other children with the same condition (Justice) [11]. In such cases, the IRB and researchers must carefully weigh the particulars of the study, the risks, and the subject population to find an ethically sound balance, sometimes favoring Beneficence and Justice over a child's dissent under specific, regulated circumstances [11].
The Belmont Report, formally published in 1979, established three fundamental ethical principles—Respect for Persons, Beneficence, and Justice—for the protection of human subjects in research [8]. These principles provide the foundational moral framework that guides the oversight of modern clinical research, including the complex and rapidly advancing field of gene therapy. The report was created by the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research in response to a growing recognition of the need for comprehensive ethical guidelines, particularly for vulnerable populations [1]. While the Belmont Report's principles are broadly applied, their effect is notably clear in the development of oversight for gene therapy clinical trials, where the line between research and therapy can be blurred and the potential for long-term consequences is significant [1]. This application note analyzes the specific impact of the Belmont principles on gene therapy trial oversight, providing researchers and IRB members with structured data and protocols for implementation.
Analytical Framework: Mapping Belmont Principles to Gene Therapy Oversight
Table 1: Core Ethical Principles of the Belmont Report and Their Applications
| Ethical Principle | Core Meaning & Requirements | Application to Gene Therapy Clinical Trials |
|---|---|---|
| Respect for Persons | Acknowledging autonomy and protecting persons with diminished autonomy [8]. Requires voluntary participation and adequate information. | - Enhanced informed consent processes that address the irreversible nature of gene therapy.- Special safeguards for populations with uncertain or impaired decision-making capacity (e.g., some pediatric or neurological patients) [75]. |
| Beneficence | The obligation to secure the well-being of subjects. Expressed as: (1) do not harm, and (2) maximize possible benefits and minimize possible harms [8]. | - Rigorous pre-clinical assessment and justification of the risk-benefit ratio for a novel, permanent intervention.- Mandatory long-term follow-up (LTFU) studies to monitor for delayed adverse events [76]. |
| Justice | The fair distribution of the burdens and benefits of research. Requires fair selection of subjects to avoid exploiting vulnerable populations [8]. | - Equitable inclusion and exclusion criteria that do not unnecessarily screen out people with cognitive or other disabilities [75].- Ensuring access to trials for populations that stand to benefit from the therapy. |
The visual workflow below outlines how these ethical principles are operationalized within the institutional review board (IRB) protocol review process for a gene therapy trial.
Quantitative Analysis of Current IRB Policy Landscape
The practical implementation of Belmont's principles, particularly Respect for Persons, is reflected in IRB policies governing the enrollment of individuals with uncertain or impaired decision-making capacity (DMC). A 2025 cross-sectional study of IRB policies at 94 top-funded U.S. research institutions provides critical benchmarking data.
Table 2: Analysis of IRB Policies for Adults with Uncertain or Impaired Decision-Making Capacity
| Policy Characteristic | Percentage of Institutions (%) | Implications for Gene Therapy Trials |
|---|---|---|
| Policies requiring EXCLUSION of people with uncertain/impaired DMC unless inclusion is scientifically justified [75] | 41.5% | Creates a significant barrier to enrollment for gene therapies targeting conditions that may affect cognitive capacity (e.g., neurodegenerative diseases). |
| Policies requiring INCLUSION of people with uncertain/impaired DMC unless exclusion is scientifically justified [75] | 5.3% | Reflects a modern, justice-oriented approach aligned with HHS Section 504 non-discrimination rules, but is not yet the norm. |
| Policies providing guidance on assessing decision-making capacity [75] | 44.7% | Highlights a need for more standardized tools and training for investigators to evaluate capacity in the context of complex gene therapy protocols. |
| Policies requiring IRB member knowledgeable about needs of people with uncertain/impaired DMC for relevant reviews [75] | 30.9% | Suggests that most IRBs may lack specialized expertise to adequately review protocols involving vulnerable populations common in gene therapy. |
This data underscores a ongoing tension in the field: the ethical imperative to protect vulnerable populations from harm versus the imperative to include them fairly in research that could offer benefit [75]. The 2024 updates to Section 504 of the Rehabilitation Act, which prohibits discrimination against people with disabilities in clinical research, are now pushing institutions toward more inclusive policies that align with the Belmont principle of Justice [75].
Experimental Protocols for Operationalizing Ethical Principles
Protocol 1: Enhanced Informed Consent Process for Gene Therapy
This protocol provides a detailed methodology for obtaining valid informed consent, directly applying the principle of Respect for Persons.
- Objective: To ensure prospective subjects, or their legally authorized representatives (LARs), possess a genuine understanding of the unique aspects of a gene therapy trial necessary to make a voluntary, informed decision.
- Background: Standard consent processes are often inadequate for gene therapy due to the therapy's potential irreversibility, novel mechanisms of action, and requirement for long-term follow-up [76].
- Materials:
- Layperson-Readable Consent Document: Written at a 6th-8th grade reading level, developed with input from health literacy experts and patient advocacy groups [77].
- Multi-Media Aids: Video animations explaining the genetic mechanism of action and the long-term follow-up process.
- Teach-Back Assessment Script: A structured questionnaire for the investigator to assess subject comprehension.
- Decision-Making Capacity (DMC) Assessment Tool: A short, validated tool (e.g., the University of California, San Diego Brief Assessment of Capacity to Consent - UBACC, adapted for the specific protocol) [75].
- Procedural Steps:
- Pre-Consent Discussion: Provide a summary video and a one-page infographic to the subject/LAR at least 24 hours before the formal consent discussion.
- Structured Consent Discussion: The investigator conducts the discussion in a quiet, private setting. Key topics must be explicitly addressed:
- The concept of permanence and irreversibility of the genetic intervention.
- The distinction between research and established therapy.
- The potential for unknown long-term risks (e.g., off-target effects, delayed immune responses, tumorigenesis).
- The mandatory nature of long-term follow-up, including its duration (e.g., 10-15 years), procedures, and the conditions under which a subject can withdraw from interventional procedures but remain in follow-up for safety monitoring [76].
- Teach-Back Assessment: Immediately after the discussion, the investigator asks the subject/LAR to explain in their own words: (a) the main purpose of the study, (b) the primary potential benefits, (c) the most serious risks, and (d) what the long-term follow-up entails. Inadequate understanding triggers a re-explanation and re-assessment.
- DMC Evaluation (if applicable): For populations where DMC may be fluctuating or impaired, a qualified professional administers the DMC tool. Results are documented.
- Waiting Period: Enforce a mandatory 24-48 hour waiting period between the initial consent discussion and signature to allow for reflection and questions.
- Documentation: The signed consent form is witnessed, and the teach-back/DMC assessment is documented in the study file.
Protocol 2: Implementing an Ethics-Based Long-Term Follow-Up (LTFU) Framework
This protocol operationalizes the principle of Beneficence by systematically monitoring for delayed risks and benefits.
- Objective: To proactively collect long-term safety and efficacy data on a gene therapy product while minimizing burden on participants, thereby fulfilling the ethical duty to maximize knowledge of benefits and harms.
- Background: LTFU studies are crucial for understanding the overall benefit-risk profile of gene therapies, but they pose significant burdens on patients, caregivers, and sponsors [76].
- Materials:
- LTFU Protocol Toolkit: A comprehensive document outlining study objectives, visit schedules, data collection methods (e.g., telehealth, mobile phlebotomy, electronic patient-reported outcomes [ePROs]), and contingency plans [76].
- Data Management System: A secure, 21 CFR Part 11-compliant electronic data capture (EDC) system capable of long-term data storage and integration with electronic health records.
- Biorepository: Facilities for the long-term storage of biological samples (e.g., blood, DNA) collected at specified intervals.
- Procedural Steps:
- LTFU Protocol Design: The LTFU study should be designed concurrently with the main clinical trial protocol. Key design elements include:
- Duration: Align with regulatory guidance (e.g., FDA recommends at least 5 years, often up to 15 years).
- Visit Schedule: A risk-based approach, with more frequent monitoring in early years tapering off later.
- Data Points: Clinical outcomes, immunogenicity, vector persistence, bioanalytics (e.g., integration sites), and quality of life metrics [76].
- Informed Consent Integration: The commitment and details of LTFU must be explicitly described in the main trial's informed consent document.
- Participant Engagement Plan: Develop a plan to maintain participant contact over time, which may include newsletters, annual check-in calls, a dedicated participant portal, and modest compensation for time and burden.
- Withdrawal Conditions Clarification: Clearly define in the consent form that while participants can withdraw from interventional parts of the study, continued safety follow-up via public health data (e.g., cancer registries, death registries) may be necessary unless the participant explicitly objects (partial withdrawal) [76].
- Data Monitoring: An independent Data and Safety Monitoring Board (DSMB) should be commissioned to review accumulated LTFU data periodically to identify any delayed safety signals.
- LTFU Protocol Design: The LTFU study should be designed concurrently with the main clinical trial protocol. Key design elements include:
The Scientist's Toolkit: Essential Reagents and Research Solutions
Table 3: Key Research Reagent Solutions for Gene Therapy Development and Oversight
| Item Name | Function / Application | Ethical Oversight Consideration |
|---|---|---|
| Viral Vector (e.g., AAV, Lentivirus) | Delivery vehicle for transferring therapeutic genetic material into human cells. | The specific tropism (cell-targeting) and potential for germline integration must be thoroughly evaluated and disclosed in the IRB application and informed consent as a key risk [1]. |
| PCR Assay Kits (qPCR, ddPCR) | Quantitative detection of vector copy number, biodistribution, and persistence in patient samples over the long term. | Essential for generating the long-term safety data required by the principle of Beneficence. Validation data for these assays are critical for regulatory and IRB approval. |
| Next-Generation Sequencing (NGS) Reagents | Comprehensive analysis of vector integration sites and screening for off-target effects in the genome. | Directly addresses the risk of insertional mutagenesis. Protocols must specify how and when NGS will be performed, and how potentially incidental findings will be handled ethically. |
| Immunoassay Kits (e.g., ELISA) | Detection of host immune responses (e.g., neutralizing antibodies) against the viral vector or transgene product. | Data on immunogenicity is crucial for the risk-benefit assessment. Strong immune responses can limit efficacy and pose safety risks, which must be explained to potential subjects. |
| Validated DMC Assessment Tool | A structured instrument to evaluate a potential subject's understanding, appreciation, and reasoning about the trial. | Operationalizes Respect for Persons. Its use should be pre-specified in the protocol for studies likely to enroll subjects with conditions that may impair cognitive function [75]. |
| Model Diversity Action Plan (DAP) | A framework for setting goals and strategies for enrolling a racially and ethnically diverse patient population. | A practical tool for implementing the principle of Justice, ensuring the trial population reflects the population affected by the disease [76]. |
The Belmont Report is not a historical artifact but a living document whose principles have directly shaped the rigorous oversight framework for modern gene therapy trials. From mandating enhanced informed consent (Respect for Persons) and long-term safety monitoring (Beneficence) to driving more equitable inclusion policies (Justice), the Report's influence is profound and measurable. The quantitative data on IRB policies reveals both progress and persistent challenges, particularly in the fair inclusion of populations with diminished decision-making capacity. As gene therapies continue to evolve, with new technologies like CRISPR-based editing and in vivo delivery, the continued application of the Belmont principles by researchers, sponsors, and IRBs will be paramount. This will ensure that scientific innovation proceeds with the necessary ethical safeguards, maintaining public trust and, ultimately, fulfilling the core mission of medical research: to improve human health in a manner that is both effective and morally sound.
Conclusion
Successfully implementing the Belmont Report in IRB protocols requires more than a checkbox mentality; it demands a deep, principled commitment to protecting human subjects throughout the research lifecycle. By grounding protocols in Respect for Persons, Beneficence, and Justice, researchers not only ensure regulatory compliance but also build the foundational trust that ethical science requires. The key takeaways are the necessity of a meaningful informed consent process, a systematic and documented risk-benefit analysis, and a proactive approach to fair subject selection. As biomedical research advances into new frontiers like gene editing, artificial intelligence, and globalized trials, the enduring principles of the Belmont Report will continue to provide the essential ethical compass, guiding the development of future regulations and ensuring that scientific progress never outstrips our commitment to human dignity and rights.
References
- 1. The creation of the Belmont Report and its effect on ethical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9700634/]
- 2. Ethical Guidelines and the Institutional Review Board [https://pmc.ncbi.nlm.nih.gov/articles/PMC10885741/]
- 3. Nuremberg Code - Wikipedia [https://en.wikipedia.org/wiki/Nuremberg_Code]
- 4. Nuremberg Code | History, Date, & 10 Points | Britannica [https://www.britannica.com/topic/Nuremberg-Code]
- 5. About The Untreated Syphilis Study at Tuskegee [https://www.cdc.gov/tuskegee/about/index.html]
- 6. Tuskegee Experiment: The Infamous Syphilis Study [https://www.history.com/articles/the-infamous-40-year-tuskegee-study]
- 7. National Research Act [https://en.wikipedia.org/wiki/National_Research_Act]
- 8. Belmont Report - Human Research Protection Program [https://irb.wisc.edu/regulatory-information/belmont-report/]
- 9. Institutional Review Boards Frequently Asked Questions [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/institutional-review-boards-frequently-asked-questions]
- 10. The Belmont Report - Human Subjects Office [https://hso.research.uiowa.edu/about-human-subjects-office/regulations-and-policies/belmont-report]
- 11. The Belmont Report - Ethical Principles [https://www.washington.edu/research/hsd/guidance/ethical-principles/belmont/]
- 12. Guiding Principles for Ethical Research [https://www.nih.gov/health-information/nih-clinical-research-trials-you/guiding-principles-ethical-research]
- 13. Ethical Considerations in Research | Types & Examples [https://www.scribbr.com/methodology/research-ethics/]
- 14. Developing ethical standards for dissemination and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10629054/]
- 15. Do You Need IRB Review... and Why? - Harvard CUHS [https://cuhs.harvard.edu/do-you-need-irb-review-and-why]
- 16. The Common Rule Changes and Update - Key Solutions Blog [https://www.keyusa.com/blog/common-rule]
- 17. Ethical Guidelines, Federal Regulations and State Statutes [https://rci.ucmerced.edu/irb/resources/ethical-guidelines-regulations-and-statutes]
- 18. IRB Background and Purpose [https://www.belmont.edu/irb/about/background.html]
- 19. What Every Clinical Researcher Should Know About ... [https://acrpnet.org/2025/10/21/what-every-clinical-researcher-should-know-about-institutional-review-boards]
- 20. BSD/UCMC IRB Policies - Biological Sciences Division [https://biologicalsciences.uchicago.edu/irb/irb-policies]
- 21. Institutional Review Board [https://www.belmont.edu/irb/]
- 22. Ethical Guidelines for Research Using Pervasive Data [https://www.federalregister.gov/documents/2024/12/11/2024-29064/ethical-guidelines-for-research-using-pervasive-data]
- 23. The History of the Belmont Report | 2020 | IRB Blog [https://www.tc.columbia.edu/institutional-review-board/irb-blog/2020/the-history-of-the-belmont-report/]
- 24. The Belmont Report: Protecting People in Clinical Trials [https://thepatientstory.com/treatments/clinical-trials/the-belmont-report/]
- 25. Still Timely After All These Years: How the Belmont Report ... [https://acrpnet.org/2025/08/06/still-timely-after-all-these-years-how-the-belmont-report-continues-to-shape-research-ethics]
- 26. The Requirements for Informed Consent (Series #1) [https://www.tc.columbia.edu/institutional-review-board/irb-blog/2025/informed-consent-the-requirements-for-informed-consent-series-1/]
- 27. The Three Principles Of The Belmont Report: Respect For ... [https://coursepivot.com/blog/which-of-the-following-are-the-three-principles-discussed-in-the-belmont-report/]
- 28. Informed Consent Guidelines & Templates [https://hrpp.umich.edu/irb-health-sciences-and-behavioral-sciences-hsbs/informed-consent-guidelines-templates/]
- 29. September 2025 IRB Connection Newsletter [https://hso.research.uiowa.edu/0925]
- 30. FDA issues final Guidance on Benefit-Risk Assessment [https://www.gmp-compliance.org/gmp-news/fda-issues-final-guidance-on-benefit-risk-assessment]
- 31. Guidelines on Benefit-Risk Assessment for New Drug ... [https://cisema.com/en/guidelines-on-benefit-risk-assessment/]
- 32. A Practical Guide to Quantitative Data Analysis Methods ... [https://www.looppanel.com/blog/quantitative-data-analysis-methods]
- 33. SPIRIT 2025 statement: Updated guideline for protocols of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037212/]
- 34. CONSORT 2025 Statement - Reporting guideline [https://www.equator-network.org/reporting-guidelines/consort/]
- 35. Subject Selection and Recruitment - IRB - UC Davis [https://irb.ucdavis.edu/project-guidance/subject-selection/]
- 36. Subject Enrollment - UCI Office of Research - UC Irvine [https://research.uci.edu/human-research-protections/subject-enrollment/]
- 37. A toolkit for capturing a representative and equitable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10719102/]
- 38. 10 takeaways from the 2025 recruiting benchmarks report - Gem [https://www.gem.com/blog/10-takeaways-from-the-2025-recruiting-benchmarks-report]
- 39. 100+ Recruitment Statistics Every HR Should Know in 2025 [https://www.selectsoftwarereviews.com/blog/recruiting-statistics]
- 40. Informed Consent: The Elements of ... [https://www.tc.columbia.edu/institutional-review-board/irb-blog/2025/informed-consent-the-elements-of-informed-consent-documents-series-2/]
- 41. Drafting a Research Plan for IRB Review and ... [https://www.wcgclinical.com/insights/drafting-a-research-plan-for-irb-review-and-research-conduct/]
- 42. Protocol Elements | Human Research Protection Program ... [https://hrpp.research.virginia.edu/teams/irb-hsr/researcher-guide-irb-hsr/protocol-elements]
- 43. Create an IRB Protocol | Guide to Using RASS & PI Dashboard [https://guide.rass.cornell.edu/institutional-review-board-for-human-participant-research/create-an-irb-protocol/]
- 44. Protocol Deviations - Prospective Clinical Trials Involving the ... [https://libraryinfo.bhs.org/c.php?g=785118&p=5623227]
- 45. Global Standards for Interventional Clinical Studies [https://www.pfizer.com/science/clinical-trials/integrity-and-transparency/global-clinical-trial-standards]
- 46. Protocol Deviations: A Holistic Approach from Defining to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8238759/]
- 47. Managing Protocol Deviations: A Guide for Clinical Trials [https://intuitionlabs.ai/articles/managing-protocol-deviations]
- 48. Protocol Deviations Explained: Understanding the FDA's ... [https://www.wcgclinical.com/insights/protocol-deviations-explained-understanding-the-fdas-draft-guidance/]
- 49. Assets Protocol Deviations - Clinical Trials [https://www.transceleratebiopharmainc.com/assets/protocol-deviations/]
- 50. Reporting Protocol Deviations [https://www.hopkinsmedicine.org/institutional-review-board/guidelines-policies/guidelines/protocol-deviations]
- 51. Vulnerable Populations - IRB - UC Davis [https://irb.ucdavis.edu/project-guidance/vulnerable-pops/]
- 52. Writing Your First IRB Proposal: Insights For Pre-doctoral ... [https://www.tc.columbia.edu/institutional-review-board/irb-blog/2025/writing-your-first-irb-proposal-insights-for-pre-doctoral-students/]
- 53. IRB considerations - Data management good practices [https://libguides.umn.edu/c.php?g=1164012&p=8497456]
- 54. Results of a National Survey of IRB Chairs - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609048/]
- 55. Phases of Clinical Trials [https://www.cancer.org/cancer/managing-cancer/making-treatment-decisions/clinical-trials/phases-of-clinical-trials.html]
- 56. SPIRIT 2025 explanation and elaboration: updated guideline ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12128891/]
- 57. Clinical trial data analytics: Revolution in 2025 [https://lifebit.ai/blog/clinical-trial-data-analytics/]
- 58. 2025 Clinical Data Trend Report [https://www.veeva.com/2025-clinical-data-trend-report/]
- 59. The early phase advantage: the key to de-risking your ... [https://www.clinicaltrialsarena.com/comment/the-early-phase-advantage-the-key-to-de-risking-your-clinical-trials/]
- 60. ESMO 2025: Novel treatment combination improves ... [https://ecancer.org/en/news/27151-esmo-2025-novel-treatment-combination-improves-progression-free-survival-in-metastatic-oestrogen-receptor-positive-her-2-negative-breast-cancer]
- 61. 2025 and Beyond: The Future of Genomic Data Analysis ... [https://blog.crownbio.com/2025-and-beyond-the-future-of-genomic-data-analysis-and-innovations-in-genomics-services]
- 62. Research Involving Genetic, Genomic, and/or DNA Collection ... [https://az.research.umich.edu/medschool/guidance/research-involving-genetic-genomic-andor-dna-collection-or-analysis/]
- 63. Guidance on genomic research with deceased patients [https://www.wcgclinical.com/insights/guidance-on-genomic-research-with-deceased-patients/]
- 64. Human Genomic Data: HHS Could Better Track Use of ... [https://www.gao.gov/products/gao-25-107377]
- 65. Ethics and Equity: Addressing Violations of the Belmont ... [https://www.sciencedirect.com/science/article/pii/S2452292925000074]
- 66. A Brief History of the Development of Clinical Research [https://medinstitute.com/blog/a-brief-history-of-the-development-of-clinical-research-principals-guidelines-and-regulations/]
- 67. A Summary of Important Documents in the Field of Research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2632196/]
- 68. A Modern History of Informed Consent and the Role of Key ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7993430/]
- 69. WMA Declaration of Helsinki – Ethical Principles for ... [https://www.wma.net/policies-post/wma-declaration-of-helsinki/]
- 70. Declaration of Helsinki – WMA [https://www.wma.net/what-we-do/medical-ethics/declaration-of-helsinki/]
- 71. Comparing the Belmont Report, Helsinki Declaration, and ... [https://www.linkedin.com/pulse/comparing-belmont-report-helsinki-declaration-ich-gcp-kiprono-mutai-xfgwf]
- 72. Informed Consent and the Revised Common Rule [https://bioethics.hms.harvard.edu/journal/consent-common-rule]
- 73. 45 CFR Part 46 -- Protection of Human Subjects [https://www.ecfr.gov/current/title-45/subtitle-A/subchapter-A/part-46]
- 74. The Common Rule - IRB - UC Davis [https://irb.ucdavis.edu/project-guidance/federal-funding/]
- 75. An Analysis of Institutional Review Board Policies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12227281/]
- 76. Tools Archives - MRCT Center [https://mrctcenter.org/resource_type/tools/]
- 77. Clinical trials ethics [https://www.novonordisk.com/science-and-technology/bioethics/clinical-trials-ethics.html]