Evaluating Quality Criteria for Empirical Ethics Research: Standards, Methods, and Best Practices
This article provides a comprehensive framework for evaluating quality criteria in empirical ethics research, addressing a critical gap in methodological standards.
Evaluating Quality Criteria for Empirical Ethics Research: Standards, Methods, and Best Practices
Abstract
This article provides a comprehensive framework for evaluating quality criteria in empirical ethics research, addressing a critical gap in methodological standards. Targeting researchers, scientists, and drug development professionals, it explores foundational concepts of research ethics board composition and expertise, examines emerging methodological standards including rapid evaluation approaches, addresses common implementation challenges and optimization strategies, and discusses validation frameworks for assessing research quality. By synthesizing recent empirical evidence and international guidelines, this resource offers practical guidance for enhancing rigor, transparency, and ethical integrity in empirical ethics studies across biomedical and clinical research contexts.
Understanding Empirical Ethics Research: Core Principles and Current Landscape
Defining Empirical Ethics Research and Its Role in Evidence-Based Ethics
Empirical ethics research represents a significant methodological shift in bioethics, integrating socio-empirical research methods with normative ethical analysis to address concrete moral questions in medicine and science [1]. This approach has evolved from purely theoretical philosophical discourse to a multidisciplinary field that systematically investigates ethical issues using data collected from real-world contexts [2]. The emergence of what has been termed the "empirical turn" in bioethics over the past two decades reflects growing recognition that ethical decision-making must be informed by actual practices, experiences, and values of stakeholders rather than relying exclusively on abstract principles [3]. This comparative guide examines the fundamental characteristics of empirical ethics research, its relationship with evidence-based ethics, and the quality criteria essential for conducting rigorous studies in this evolving field.
Conceptual Definitions and Key Distinctions
What is Empirical Ethics Research?
Empirical ethics research utilizes methods from social sciences—such as anthropology, psychology, and sociology—to directly examine issues in bioethics [4]. This methodology investigates how moral values and ethical norms operate in real-world contexts, contrasting with purely theoretical ethics by grounding moral inquiry in observable human behavior and societal practices [5]. By employing techniques including surveys, interviews, ethnographic observations, and case studies, empirical ethics research provides data on actual moral decision-making processes, offering evidence about what people actually think, want, feel, and believe about ethical dilemmas [3].
What is Evidence-Based Ethics?
Modeled after evidence-based medicine, evidence-based ethics has been defined as "the conscientious, explicit, and judicious use of current best evidence in making decisions about the conduct of research" [4]. A non-trivial interpretation of this concept distinguishes between "evidence" as high-quality empirical information that has survived critical appraisal versus lower-quality empirical information [6]. This approach demands that ethical decisions integrate individual expertise with the best available external evidence from systematic research, with particular attention to the quality and validity of the empirical information being utilized [6].
Comparative Relationship
The relationship between empirical ethics and evidence-based ethics represents a continuum of methodological rigor. While all evidence-based ethics incorporates empirical elements, not all empirical ethics research meets the stringent criteria to be considered "evidence-based." The key distinction lies in the systematic critical appraisal of evidence quality and the explicit process for integrating this evidence with ethical reasoning [6]. Empirical ethics provides the methodological toolkit for gathering data about ethical phenomena, while evidence-based ethics provides a framework for evaluating and applying that data in ethical decision-making [2] [6].
Quantitative Growth and Methodological Distribution
The evolution of empirical ethics research can be tracked quantitatively through its representation in leading bioethics journals. A comprehensive analysis of nine peer-reviewed journals in bioethics and medical ethics between 1990 and 2003 revealed significant trends in methodological approaches and publication patterns.
Table 1: Prevalence of Empirical Research in Bioethics Journals (1990-2003)
| Journal | Total Publications | Empirical Studies | Percentage Empirical |
|---|---|---|---|
| Nursing Ethics | 367 | 145 | 39.5% |
| Journal of Medical Ethics | 761 | 128 | 16.8% |
| Journal of Clinical Ethics | 604 | 93 | 15.4% |
| Bioethics | 332 | 22 | 6.6% |
| Cambridge Quarterly of Healthcare Ethics | 332 | 18 | 5.4% |
| Hastings Center Report | 565 | 13 | 2.3% |
| Theoretical Medicine and Bioethics | 315 | 9 | 2.9% |
| Kennedy Institute of Ethics Journal | 264 | 5 | 1.9% |
| Christian Bioethics | 194 | 2 | 1.0% |
| Overall | 4029 | 435 | 10.8% |
Table 2: Methodological Approaches in Empirical Bioethics Research (1990-2003)
| Research Paradigm | Number of Studies | Percentage |
|---|---|---|
| Quantitative Methods | 281 | 64.6% |
| Qualitative Methods | 154 | 35.4% |
| Total | 435 | 100% |
The data reveal several important trends. First, the proportion of empirical research in bioethics journals increased steadily from 5.4% in 1990 to 15.4% in 2003 [7]. Second, the distribution of empirical research varies significantly across journals, with clinically-oriented publications (Nursing Ethics, Journal of Medical Ethics, and Journal of Clinical Ethics) containing the highest percentage of empirical studies [7]. Third, quantitative methodologies dominated the empirical landscape during this period, representing nearly two-thirds of all empirical studies [7].
Methodological Frameworks and Experimental Protocols
Research Designs in Empirical Ethics
Empirical ethics research employs diverse methodological approaches, each with distinct protocols for data collection and analysis:
Survey Research: Utilizes structured questionnaires to quantify attitudes, beliefs, and experiences of relevant stakeholders. For example, research on stored biological samples has employed survey methods to determine that most research participants prefer simple binary choices regarding future research use of their samples rather than detailed checklists of specific diseases [8]. Standard protocols include validated instruments, probability sampling where possible, and statistical analysis of responses.
Semi-structured Interviews: Collects rich qualitative data through guided conversations that allow participants to express nuanced perspectives in their own words. This approach is particularly valuable for exploring complex moral reasoning and contextual factors influencing ethical decisions [3]. Protocols typically include interview guides, audio recording, transcription, and thematic analysis using coding frameworks.
Ethnographic Observation: Involves extended engagement in natural settings to understand ethical practices as they occur in context. This method is especially useful for identifying discrepancies between formally stated ethical policies and actual behaviors [3]. Standard protocols include field notes, participant observation, and iterative analysis moving between data and theoretical frameworks.
Experimental Designs: Employ controlled conditions to test ethical interventions or measure their effectiveness. For instance, randomized controlled trials have been used to evaluate different approaches to improving research participants' understanding of informed consent documents [8]. Protocols follow standard experimental procedures with manipulation of independent variables and measurement of dependent variables.
Table 3: Methodological Framework for Empirical Ethics Research
| Research Category | Definition | Primary Methods | Application Examples |
|---|---|---|---|
| Descriptive | Assessing what "is" - current practices, beliefs, or attitudes | Surveys, interviews, observational studies | Documenting how ethics committees make decisions [4] |
| Comparative | Comparing the "is" to the "ought" | Normative analysis of empirical data | Identifying gaps between ethical guidelines and actual practices [4] |
| Intervention | Testing approaches to reconcile "is" and "ought" | Experimental trials, policy pilots | Evaluating ethics education programs [4] |
| Consensus | Analysis of multiple lines of evidence to establish norms | Delphi methods, systematic reviews | Developing guidelines for research ethics board composition [4] |
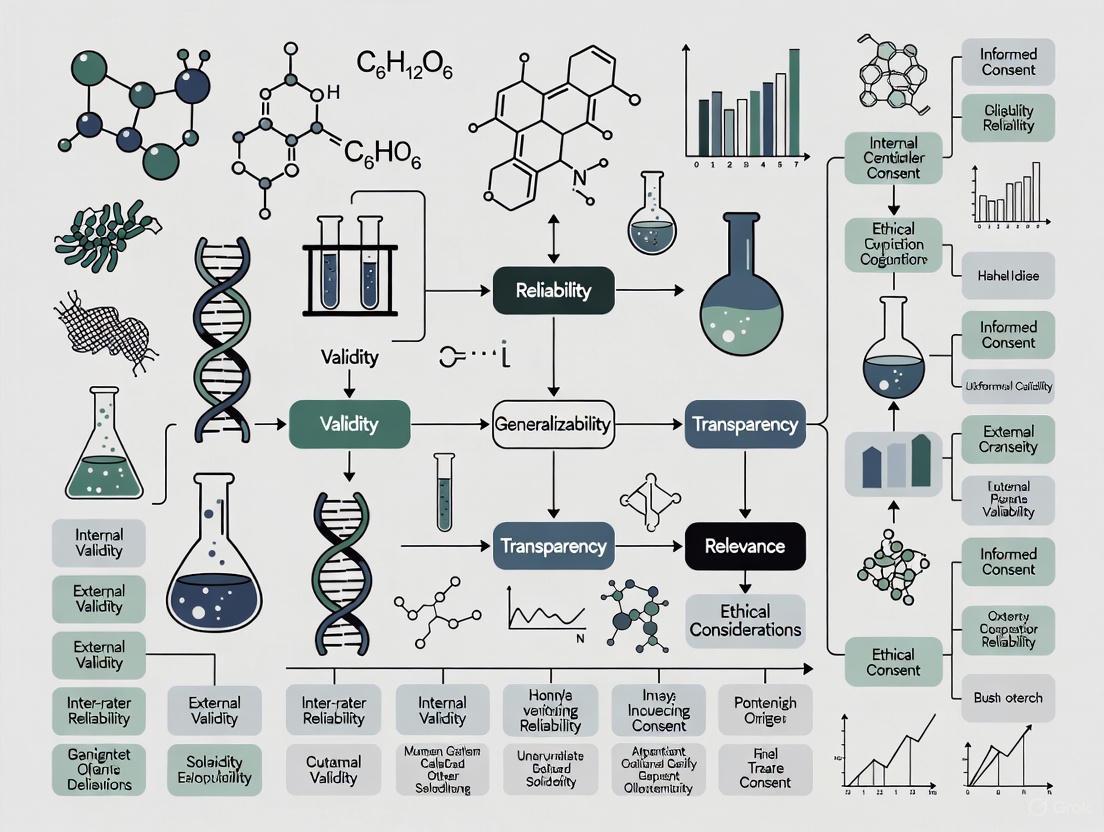
Conceptual Workflow for Empirical Ethics Research
The following diagram illustrates the integrated methodology that characterizes empirical ethics research, showing how normative and empirical approaches combine to produce ethically justified outcomes:
Quality Assessment Framework for Empirical Ethics Research
Evaluating the quality of empirical ethics research requires assessing both normative and empirical dimensions. The following criteria provide a framework for critical appraisal:
Normative Quality Criteria
Theoretical Adequacy: The ethical theory or framework selected must be adequate for addressing the specific issue at stake [1]. Different theoretical approaches (consequentialist, deontological, virtue ethics, etc.) may yield divergent normative evaluations, making the justification for theory selection essential [1].
Transparency: Researchers should explicitly state and justify their normative presuppositions and the ethical framework guiding the analysis [1]. This includes acknowledging values and biases that might influence research design or interpretation [6].
Reasoned Application: The process of applying normative frameworks to empirical findings should follow a systematic, well-reasoned approach rather than ad hoc justification [1]. This includes careful consideration of how empirical data informs, modifies, or challenges ethical principles.
Empirical Quality Criteria
Methodological Rigor: Research design, data collection, and analysis should meet established standards for empirical research in the relevant social scientific discipline [6]. This includes appropriate sampling strategies, valid measurement instruments, and proper analytical techniques.
Contextual Sensitivity: The research design should account for how contextual factors—organizational structures, cultural norms, power dynamics—influence ethical practices and perceptions [3]. This enhances the validity of findings by acknowledging the situated nature of ethical decision-making.
Reflexivity: Researchers should critically examine how their own positions, assumptions, and interactions might influence the research process and findings [3]. This includes considering how research questions are framed and whose perspectives are included or excluded.
Integrative Quality Criteria
Procedural Justification: The process of integrating empirical findings with normative analysis should be explicitly described and justified [1] [6]. Researchers should explain how facts inform values without committing naturalistic fallacies (deriving "ought" directly from "is").
Practical Applicability: The research should produce findings that can inform real-world ethical decisions, policies, or practices [3]. This includes consideration of implementability and potential consequences of applying the research findings.
Conducting rigorous empirical ethics research requires familiarity with diverse methodological approaches and tools. The following table outlines key resources and their applications:
Table 4: Essential Methodological Resources for Empirical Ethics Research
| Method Category | Specific Methods | Primary Application | Key Considerations |
|---|---|---|---|
| Quantitative Approaches | Surveys, questionnaires, structured observations | Measuring prevalence of attitudes, testing hypotheses about ethical behaviors | Requires validated instruments, appropriate sampling strategies, statistical expertise |
| Qualitative Approaches | In-depth interviews, focus groups, ethnographic observation | Exploring moral reasoning, understanding ethical dilemmas in context | Demands researcher reflexivity, careful attention to power dynamics in data collection |
| Mixed Methods | Sequential or concurrent quantitative and qualitative data collection | Providing comprehensive understanding of complex ethical issues | Requires careful integration of different data types, may involve larger research teams |
| Systematic Review Methods | Meta-analysis, meta-synthesis, scoping reviews | Synthesizing existing empirical research on specific ethical questions | Essential for evidence-based ethics; must address quality appraisal of included studies [9] |
Comparative Analysis: Evidence-Based Ethics in Practice
The application of evidence-based approaches to ethics presents both opportunities and challenges. The following diagram illustrates the conceptual structure and procedural flow of evidence-based ethics:
Practical Applications and Limitations
Evidence-based ethics finds application across multiple domains:
Research Ethics Committees: Empirical research on REB composition and functioning informs evidence-based approaches to improving ethical review processes [9]. Studies have examined how different forms of expertise (scientific, ethical, legal, community perspectives) influence review quality and outcomes [9].
Clinical Ethics Consultation: Evidence-based approaches can improve the quality and consistency of ethics consultation services by systematically evaluating consultation outcomes and methods [8].
Policy Development: Evidence-based ethics supports the development of ethically sound policies by integrating empirical data about stakeholder values, preferences, and experiences with normative analysis [3].
However, evidence-based ethics faces significant limitations. The approach risks privileging quantifiable data over important qualitative ethical considerations and may implicitly favor certain values through its methodological choices [2] [6]. There remains ongoing debate about appropriate quality criteria for empirical research in ethics and how to differentiate between high and low-quality information [6].
Empirical ethics research represents an essential methodology for addressing complex ethical challenges in healthcare, research, and emerging technologies. By systematically integrating robust empirical data with thoughtful normative analysis, this approach grounds ethical reflection in the actual experiences, values, and practices of relevant stakeholders. The evidence-based ethics movement further strengthens this approach by emphasizing critical appraisal of empirical evidence and transparent procedures for integrating evidence with ethical decision-making.
As the field continues to develop, researchers should prioritize methodological rigor, theoretical transparency, and practical applicability. Quality empirical ethics research must meet standards for both empirical social science and normative ethics while developing integrative frameworks that respect the distinctive contributions of each approach. For drug development professionals and researchers, understanding these methodologies enables critical appraisal of empirical ethics literature and contributes to more ethically informed practices and policies.
Essential Components of Effective Research Ethics Boards (REBs)
Research Ethics Boards (REBs), also known as Institutional Review Boards (IRBs) or Research Ethics Committees (RECs), serve as independent committees tasked with reviewing, approving, and monitoring biomedical and behavioral research involving human participants [10] [11]. Their fundamental mission is to protect the rights, safety, and welfare of individuals who volunteer to take part in research studies [11] [12]. This protective role emerged from a history of research misconduct and abuse, leading to the development of national and international regulations [13] [12]. Effective REBs operate as more than just bureaucratic hurdles; they are vital partners in the research enterprise, ensuring that the search for scientific knowledge does not come at the cost of human dignity or well-being. By upholding rigorous ethical standards, they foster public trust in scientific research and ensure that the benefits of research are realized responsibly [11].
This guide evaluates the essential components that contribute to an REB's effectiveness, framed within a broader thesis on quality criteria for empirical ethics research. For researchers, scientists, and drug development professionals, understanding these components is crucial for navigating the ethics review process successfully and for appreciating the structural and operational elements that underpin robust ethical oversight.
Foundational Ethical Principles and History
The operation of all REBs is guided by a set of core ethical principles, primarily derived from key historical documents that emerged in response to ethical breaches in research.
Historical Context and Governing Principles
The need for ethical oversight became glaringly apparent after the atrocities of World War II, leading to the Nuremberg Code in 1947, which established the absolute necessity of voluntary consent [12]. This was followed by the Declaration of Helsinki in 1964, which further solidified guidelines for clinical research [12] [14]. In the United States, the public exposure of the Tuskegee Syphilis Study prompted the National Research Act of 1974, which formally created IRBs [10] [12]. The subsequent Belmont Report articulated three fundamental principles that continue to provide the ethical framework for human subjects research [12] [14]:
- Respect for Persons: Recognizing the autonomy of individuals and protecting those with diminished autonomy, often operationalized through the informed consent process [11] [12].
- Beneficence: The obligation to maximize benefits and minimize possible harms to research participants [11] [12].
- Justice: Ensuring the fair distribution of the benefits and burdens of research, so that no particular group is unfairly burdened or excluded [11] [12].
In Canada, the Tri-Council Policy Statement (TCPS2) is the prevailing national standard, providing a comprehensive framework for the ethical conduct of research involving humans [13] [15] [14].
Table 1: Historical Foundations of Research Ethics
| Document/Event | Year | Key Contribution | Impact on REB Function |
|---|---|---|---|
| Nuremberg Code | 1947 | Established the requirement for voluntary informed consent | Foundation for modern consent standards and the right to withdraw without penalty [12]. |
| Declaration of Helsinki | 1964 | Stressed physician-investigators' responsibilities to their patients | Emphasized the well-being of the subject over the interests of science and society [12]. |
| Tuskegee Syphilis Study | Revealed 1972 | Long-term study withholding treatment from Black men with syphilis | Catalyzed the National Research Act and formal creation of IRBs in the U.S. [12]. |
| The Belmont Report | 1979 | Articulated three core principles: Respect for Persons, Beneficence, Justice | Provides the primary ethical framework for REB review and federal regulations [12] [14]. |
| Tri-Council Policy Statement (TCPS2) | Current | Canadian policy for ethical conduct of research involving humans | Mandatory standard for all research funded by Canada's three federal research agencies [13] [14]. |
Core Structural Components of an Effective REB
The effectiveness of an REB is contingent upon its foundational structure, which ensures its independence, competence, and capacity to conduct thorough reviews.
Diverse and Qualified Membership
A multidisciplinary composition is critical for a competent and comprehensive review of research proposals. Regulations typically mandate a minimum of five members [12], but effective boards often include a diverse group with varied expertise and perspectives [15] [11]. The membership should include:
- Scientific Members: Individuals with expertise in the specific research disciplines and methodologies commonly reviewed (e.g., medicine, psychology, social sciences) [15] [12].
- Non-Scientific Members: Members from diverse backgrounds, including law, ethics, and community representatives, to provide non-specialist perspectives [15] [10] [12].
- Legal and Ethical Expertise: At least one member knowledgeable in law and one in ethics to guide complex legal and ethical considerations [15].
- Community Representation: Members recruited from the general population and specific communities (e.g., Indigenous communities) to safeguard community values and participant interests [15]. This diversity helps ensure that the REB can adequately assess the scientific validity, potential risks and benefits, and community acceptability of the research [11].
Operational Independence and Institutional Support
For an REB to function effectively, it must be independent from undue influence. The REB must have the authority to approve, require modifications in, or disapprove research, and its decisions should be free from coercion or interference from institutional or sponsor interests [10] [16]. As noted by Health Canada, institutions are required to provide "necessary and sufficient ongoing financial and administrative resources" to support the REB's functioning [13]. This includes:
- Adequate Administrative Support: Sufficient staff to manage the workflow, from application intake to communication with researchers [13].
- Protected Time for Members: REB membership requires a significant time commitment for reviewing materials and attending meetings, which must be recognized and supported by the institution [15].
- Clear Reporting Lines: While administratively supported by the institution, the REB should report to a high level (e.g., to a deputy minister or president) to preserve its independent voice [15].
Operational and Procedural Components
Beyond its structure, the REB's day-to-day processes are fundamental to its efficiency and effectiveness.
Systematic Review Workflow
The ethics review process is often perceived as a "black box," but effective REBs operate through a well-defined, multi-stakeholder workflow [13]. Inefficiencies often arise from applications stalling or moving backward in the process due to incomplete submissions or poor communication.
Diagram 1: REB Review Workflow and Stakeholders
This workflow illustrates the critical roles and potential backflows that cause delays. The model shows that researchers, administrators, and REB members all share accountability for the timely movement of an application [13].
Comprehensive Documentation and Review Criteria
The review process is anchored in a set of essential documents that form the backbone of any clinical trial or research study [17]. These documents ensure compliance, protect participants, and provide an audit trail [17]. The core documents required for review typically include:
- Research Protocol: The comprehensive blueprint for the study, detailing objectives, design, methodology, and statistical considerations [17].
- Informed Consent Form (ICF): The document ensuring participants are provided all necessary information in plain language to make a voluntary decision [17].
- Investigator's Brochure (IB): A compilation of all clinical and non-clinical data on the investigational product [17].
- Case Report Form (CRF): The tool for standardized data collection from each participant [17].
- Clinical Study Report (CSR): The comprehensive summary of the entire clinical trial upon completion [17].
The REB then evaluates these documents against a set of rigorous criteria [14]:
- Scientific Soundness & Methodology: The research must be scientifically valid and justified [14].
- Risk-Benefit Analysis: Potential benefits must significantly outweigh potential harms [14].
- Informed Consent Process: The process for obtaining voluntary, informed consent must be adequate [14].
- Privacy & Confidentiality: Robust measures must be in place to protect participant data [14].
- Selection & Recruitment: The selection of participants must be fair and just [14].
Performance Metrics and Global Comparison
A key challenge for REBs is balancing thoroughness with efficiency. Lengthy review times are a consistent complaint within the research community and can have serious consequences, including the loss of research resources and delays in patient access to new therapies [13].
Quantitative Review Timelines Across Countries
A global comparison of ethical review protocols reveals significant heterogeneity in review timelines, which can impact international research collaboration [18]. The table below summarizes the typical approval timelines for different study types across a selection of countries.
Table 2: International Comparison of Ethical Approval Timelines
| Country / Region | Audit / Routine Review | Observational Study | Randomized Controlled Trial (RCT) | Key Regulatory Features |
|---|---|---|---|---|
| United Kingdom | Local audit registration | 1-3 months [18] | >6 months [18] | Decision-making tool to classify studies; arduous process for interventional studies [18]. |
| Belgium | >3-6 months [18] | >3-6 months [18] | 1-3 months [18] | Lengthy process for audits/observational studies; written consent mandatory for all research [18]. |
| India & Ethiopia | >3-6 months [18] | >3-6 months [18] | 1-3 months [18] | Protracted review for lower-risk studies; local or national-level review [18]. |
| Hong Kong & Vietnam | Audit registration / Waiver review [18] | Information Missing | Information Missing | Shorter lead times for audits; initial review to assess need for formal process [18]. |
| General Timeline | Varies widely | 1-3 months [18] | 1-6+ months [18] | Centralized review for multisite trials enhances efficiency [13] [18]. |
Strategies for Improving Efficiency
To address delays, stakeholders can adopt targeted best practices [13]:
- Researchers: Develop scientifically sound proposals and ensure applications are thorough and complete from the outset. Understand and apply research ethics standards before submission [13].
- REB Members: Understand and consistently apply ethics standards, respect review timelines, and participate in ongoing education [13].
- Institutions: Provide necessary administrative support responsive to workload variations and promote a culture of respect for the ethics review process [13].
- Systemic Improvements: Moving toward regionalized or centralized ethics review for multi-site research can dramatically improve efficiency by eliminating redundant reviews at each center [13] [18].
For researchers preparing an ethics application, understanding the required materials and their function is crucial. The following table details the "research reagent solutions" – the essential documents and resources needed for a successful REB submission.
Table 3: Essential Research Reagents for REB Submission
| Item / Document | Category | Primary Function | Key Considerations |
|---|---|---|---|
| Research Protocol | Pre-trial Document | Serves as the study's blueprint, detailing objectives, design, methodology, and statistical plan [17]. | Must be scientifically rigorous and feasible; basis for regulatory oversight [17]. |
| Informed Consent Form (ICF) | Pre-/During-trial Document | Ensures participant autonomy by providing all necessary information in plain language for a voluntary decision [17]. | Requires REB approval; must outline risks, benefits, confidentiality, and right to withdraw [17]. |
| Investigator's Brochure (IB) | Pre-trial Document | Compiles all relevant clinical/non-clinical data on the investigational product for investigator safety assessment [17]. | Must be regularly updated as new safety information emerges [17]. |
| Case Report Form (CRF) | During-trial Document | Standardized tool (paper/electronic) for collecting data from each participant to ensure consistency [17]. | Design should align with the protocol and minimize data entry errors [17]. |
| Tri-Council Policy Statement (TCPS 2) | Guidance Document | The prevailing Canadian standard for ethical research; guides REB evaluation criteria [15] [14]. | Researchers should be familiar with its principles before designing studies and submitting applications [13]. |
| REB Application Checklist | Administrative Document | Institutional-specific list to ensure all components of the application are complete upon submission [13]. | Consulting this and the REB in advance of submission prevents delays [13]. |
Effective Research Ethics Boards are not defined by a single component but by a synergistic integration of multiple elements. They are built upon a foundation of core ethical principles, operationalized through a diverse and independent structure, and maintained via systematic and transparent procedures. The efficiency of their operation, measured through metrics like review timelines, is as critical as their adherence to ethical rigor. As the landscape of research becomes increasingly global and complex, the continued evolution and standardization of REB processes—while preserving their fundamental protective role—will be essential. For the research community, engaging with the REB as a partner from the earliest stages of study design, armed with a clear understanding of these essential components, is the most effective strategy for ensuring that valuable research can proceed ethically and without unnecessary delay.
Empirical ethics research (EER) represents an important and innovative development in bioethics, directly integrating socio-empirical research with normative-ethical analysis to produce knowledge that would not be possible using either approach alone [19]. This interdisciplinary field uses methodologies from descriptive disciplines like sociology, anthropology, and psychology—including surveys, interviews, and observation—but maintains a strong normative objective aimed at developing ethical analyses, evaluations, or recommendations [19]. The fundamental challenge, and the core thesis of this evaluation, is that poor methodology in EER does not merely render a study scientifically unsatisfactory; it risks generating misleading ethical analyses that deprive the work of scientific and social value and can lead to substantive ethical misjudgments [19]. Therefore, establishing robust quality criteria is not merely an academic exercise but an ethical necessity in itself. This guide evaluates these criteria across three critical domains: scientific rigor, ethical integrity, and participant perspective, providing a framework for researchers to assess and improve their empirical ethics work.
Domain Comparison: Scientific, Ethical, and Participant Perspectives
The quality of EER depends on meeting interdependent criteria across three foundational domains. The table below synthesizes these core components, their quality benchmarks, and the consequences of their neglect.
| Domain | Core Components | Key Quality Criteria | Consequences of Poor Implementation |
|---|---|---|---|
| Scientific Perspective [19] [20] [21] | - Primary Research Question- Theoretical Framework- Methodology & Data Analysis | - Clarity and focus of the primary research question.- Appropriate and justified methodological choice (qualitative/quantitative).- Rigorous experimental design (e.g., randomization, control groups, blinding) to establish causation.- Accurate and transparent data presentation. | - Inability to establish cause-and-effect (causation).- Results confounded by lurking variables.- Misleading findings and wasted resources.- Undermines scientific validity and ethical analysis. |
| Ethical Perspective [19] [20] [21] | - Research Ethics & Scientific Ethos- Interdisciplinary Integration- Normative Reflection | - Approval by an Institutional Review Board (IRB).- Informed consent from participants.- Data privacy and confidentiality.- Minimization of risks.- Explicit integration of empirical findings with normative argumentation. | - Direct harm or exploitation of research subjects.- Violation of legal and professional standards.- "Crypto-normative" conclusions where evaluations are implicit and unexamined.- Study fails to achieve its normative purpose. |
| Participant Perspective [19] [20] [21] | - Participant Safety & Autonomy- Mitigation of Bias- Transparency | - Participant well-being is prioritized over research goals.- Use of placebos and blinding to counter power of suggestion (e.g., placebo effect).- Procedures are clearly explained, and participation is voluntary. | - Physical or psychological harm to participants.- Coercion and erosion of trust in research.- Biased results due to participant or researcher expectations (e.g., in non-blinded studies). |
Experimental Protocols for Establishing Causation
A core requirement from the scientific perspective is the ability to design experiments that can reliably test hypotheses and support causal inferences. The following protocols are fundamental.
Randomized Controlled Trial (RCT)
The RCT is the gold standard experimental design for isolating the effect of a treatment and establishing cause-and-effect relationships [20] [21].
Detailed Methodology:
- Definition of Variables: Identify the explanatory variable (the treatment or intervention being tested) and the response variable (the outcome being measured) [21].
- Recruitment and Random Assignment: Recruit a sample of participants from the target population. Randomly assign these participants to either a treatment group (which receives the active intervention) or a control group (which receives a placebo or standard treatment) [20]. Randomization ensures that all potential lurking variables are spread equally among the groups, making the treatment the only systematic difference [21].
- Blinding: Implement a double-blind procedure where neither the participants nor the researchers interacting with them know which group is receiving the active treatment. This prevents biases in reporting and interpretation due to the power of suggestion or expectation [21].
- Execution and Data Collection: Administer the treatments for a predefined period under controlled conditions. Measure the resulting changes in the response variable for all participants [20].
- Analysis: Compare the outcomes of the treatment and control groups using appropriate statistical tests. A statistically significant difference in the response variable can be attributed to the explanatory variable due to the random assignment [21].
Example: Investigating Aspirin and Heart Attacks
- Population: Men aged 50 to 84 [21].
- Sample & Experimental Units: 400 men recruited for the study [21].
- Explanatory Variable: Oral medication (aspirin vs. placebo) [21].
- Treatments: Aspirin and a placebo [21].
- Response Variable: Whether a subject had a heart attack [21].
Observational Study and Its Limitations
In contrast to experiments, observational studies are based on observations or measurements without manipulating the explanatory variable [21].
Detailed Methodology:
- Identification of Cohort: Identify a group of subjects to be studied.
- Measurement: Record data on variables of interest for these subjects. This can be done prospectively (following subjects forward in time) or retrospectively (using historical data).
- Analysis: Look for apparent associations or correlations between the explanatory and response variables.
Key Limitation: An observational study can only identify an association between two variables; it cannot prove causation [20] [21]. This is because of potential confounding (lurking) variables—other unmeasured factors that could be the true cause of the observed effect [21].
Example: Vitamin E and Health An observational study might find that people who take vitamin E are healthier. However, this does not prove vitamin E is the cause. The improved health could be due to lurking variables, such as the fact that vitamin E users may also exercise more, eat a better diet, or avoid smoking [21].
Visualizing Workflows in Empirical Ethics Research
Effective data visualization is crucial for communicating complex research designs and findings. The following diagrams, created with DOT language and adhering to specified color and contrast rules, illustrate key workflows.
Empirical Ethics Research Workflow
Experimental vs. Observational Study Design
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of EER requires both conceptual and practical tools. The following table details key "reagents" and their functions in the research process.
| Item / Solution | Function in Empirical Ethics Research |
|---|---|
| Theoretical Framework [19] | Provides the underlying philosophical and social science concepts that guide the research question, methodology, and interpretation of findings. |
| Validated Data Collection Instruments [19] | Ensures the reliability and validity of collected data. Includes pre-tested survey questionnaires, structured interview guides, and standardized observation protocols. |
| Interdisciplinary Research Team [19] | A collaborative group with expertise in both normative ethics and empirical social science methods. Crucial for overcoming methodological biases and achieving genuine integration. |
| Institutional Review Board (IRB) Protocol [20] [21] | A formal research plan submitted for approval to an ethics board. It details how the study will minimize risks, obtain informed consent, and protect participant privacy. |
| Blinding Materials (Placebos) [20] [21] | Inactive substances or fake treatments that are indistinguishable from the real intervention. They are essential for controlling for the placebo effect in experimental designs. |
| Data Visualization Software [22] [23] | Tools (e.g., Tableau, R/ggplot2, Datawrapper) used to create effective charts and graphs that accurately and clearly communicate data patterns and relationships. |
| Qualitative Data Analysis Software | Software (e.g., NVivo, MAXQDA) that aids in the systematic coding, analysis, and interpretation of non-numerical data from interviews, focus groups, or documents. |
| Informed Consent Documents [20] [21] | Legally and ethically required forms that clearly explain the study's purpose, procedures, risks, and benefits to participants, ensuring their voluntary agreement is based on understanding. |
Data Visualization Principles for Accessible Communication
Presenting data effectively is a key component of scientific rigor. Adhering to established principles ensures that visuals are accurate, informative, and accessible to all readers, including those with color vision deficiencies [24].
- Diagram First: Prioritize the information and message before engaging with software. Focus on the core story (e.g., a comparison, trend, or distribution) rather than defaulting to a specific chart type [22].
- Use an Effective Geometry: Select the chart type that best represents your data. Avoid misuse of geometries; for example, bar plots are for amounts and counts, but should not be used to show group means with distributional information [22]. Use scatterplots for relationships, box plots or violin plots for distributions, and line charts for trends over time [22] [25].
- Use Color Strategically: Color should enhance readability, not overwhelm. Use it to highlight key data points or to distinguish categories [25] [23]. Ensure sufficient color contrast; for normal text, the Web Content Accessibility Guidelines (WCAG) AA standard requires a contrast ratio of at least 4.5:1 [26] [27].
- Keep it Simple (Avoid Chartjunk): Eliminate unnecessary elements like excessive gridlines, decorations, or 3D effects that distract from the data. Maximize the data-ink ratio, which is the amount of ink used for data versus the total ink in the figure [22] [25].
- Provide Context with Labels: Always include clear titles, axis labels, and legends where necessary. This ensures viewers can understand what the data represents without confusion [23].
Current Gaps in Empirical Research on Ethics Review Quality
The quality of ethics review is a cornerstone of ethical research involving human subjects. Research Ethics Boards (REBs), also known as Institutional Review Boards (IRBs) or Ethics Review Committees (ERCs), carry the critical responsibility of protecting participant rights and welfare. While international guidelines outline membership composition and procedural standards, a significant disconnect exists between these normative frameworks and the empirical evidence supporting specific configurations for optimal performance. This analysis identifies and systematizes the current empirical research gaps concerning ethics review quality, providing researchers with a roadmap for future investigative priorities.
Major Identified Research Gaps
A 2025 scoping review of empirical research on REB membership and expertise highlights a "small and disparate body of literature" and explicitly concludes that "little evidence exists as to what composition of membership expertise and training creates the conditions for a board to be most effective" [9]. The table below summarizes the core empirical gaps clustered into four central themes.
Table 1: Core Empirical Gaps in Ethics Review Research
| Thematic Area | Specific Empirical Gap | Key Question Lacking Evidence |
|---|---|---|
| REB Membership & Expertise | Optimal composition of scientific expertise [9] | What specific mix of scientific expertise enables most effective review of diverse protocols? |
| Effectiveness of ethical, legal, and regulatory training [9] | Which training modalities most improve review quality and decision-making? | |
| Impact of identity and perspective diversity [9] | How does demographic/professional diversity concretely affect review outcomes and participant protection? | |
| Informing Policy & Guidelines | Evidence-based updates to ethics guidelines [28] | How can empirical data on gaps directly inform and improve official ethics guidelines? |
| Guidance for novel trial designs (e.g., Stepped-Wedge CRTs) [28] | What specific ethical frameworks are needed for complex modern trial designs? | |
| Oversight of Evolving Methodologies | Purview over big data and AI research [29] | How can REBs effectively oversee research with novel risks (privacy, algorithmic discrimination)? |
| Functional capacity for data-intensive review [29] | Do REBs possess necessary technical expertise and procedures for big data/AI protocol review? | |
| System Efficiency & International Collaboration | Quality and efficiency metrics for review models [30] | What metrics best measure the quality and efficiency of ethics review systems? |
| Practical implementation of mutual recognition models [30] | How can reciprocity, delegation, and federation models be operationalized effectively across borders? |
Unexplored Dimensions of REB Membership and Training
The composition and training of REBs represent a foundational gap. Despite clear guidelines recommending multidisciplinary membership, the empirical evidence demonstrating which specific combinations of expertise lead to more effective human subject protection is notably absent [9]. Furthermore, while some training is standard, research has not established which formats—online modules, workshops, or other methods—most significantly improve committee members' review capabilities [9]. The inclusion of community members is intended to represent participant perspectives, but empirical studies have not robustly measured the causal impact of this diversity on the ethical quality of review decisions [9].
The Challenge of Novel Research Methodologies
The rapid evolution of research methodologies has created a significant lag in ethical oversight. The emergence of big data research exposes "purview weaknesses," where studies can evade review entirely, and "functional weaknesses," where REBs lack the specialized expertise to evaluate risks like privacy breaches and algorithmic discrimination [29]. Similarly, in clinical trial design, the adoption of cluster randomized trials (CRTs) and stepped-wedge designs has outpaced the development of specific ethics guidance. A 2025 citation analysis identified 24 distinct gaps in the seminal Ottawa Statement guidelines for CRTs, highlighting a pressing need for evidence-based guidance updates [28].
System-Level Inefficiencies and the Need for New Metrics
At a systemic level, the prevailing model of replicated, local ethics review for multi-site and international research is often inefficient without clear evidence of improved participant protection [30]. While alternative models like reciprocity, delegation, and federation have been proposed, empirical research is needed to define the metrics for evaluating their quality and efficiency [30]. Without this evidence, the implementation of these streamlined models remains challenging.
Experimental Protocols for Gap Investigation
To address these gaps, researchers can employ several empirical methodologies. The following diagram outlines a sequential mixed-methods approach to investigate a specific research gap, combining qualitative and quantitative data for a comprehensive analysis.
Figure 1: A sequential mixed-methods protocol for investigating ethics review gaps.
Detailed Methodology:
- Scoping and Systematic Reviews: As demonstrated in the 2025 review on REB membership, this method is essential for mapping the existing literature and precisely identifying where evidence is lacking. The process involves identifying research questions, selecting relevant studies, and systematically charting the data to summarize findings [9].
- Qualitative Inquiry: Semi-structured interviews and focus groups with key stakeholders—including REB chairs, members, researchers, and research participants—are critical. This approach explores complex phenomena, such as how REBs deliberate on big data risks or how community members perceive their role, providing rich, contextual insights that surveys alone cannot capture [9].
- Quantitative Surveys: Following qualitative analysis, surveys can test hypotheses and measure the prevalence of certain views or practices across a larger population. For example, a survey could quantify the percentage of REBs that have specific training modules on AI ethics or measure the correlation between certain membership characteristics and perceived review quality [31].
- Citation and Document Analysis: This method involves systematically analyzing publications, guidelines, and policy documents. The 2025 gap analysis of the Ottawa Statement used this to great effect, reviewing 53 articles that cited the guideline to identify 24 specific areas where guidance was missing or inadequate [28].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Methodological Tools for Empirical Ethics Research
| Research Tool / Reagent | Primary Function in Investigation |
|---|---|
| Systematic Review Protocol | Provides a structured, replicable plan for comprehensively identifying, selecting, and synthesizing all relevant literature on a specific ethics topic [9]. |
| Semi-Structured Interview Guide | Ensures consistent coverage of key topics (e.g., training experiences, challenges with big data) while allowing flexibility to explore novel participant responses [9]. |
| Stakeholder-Specific Survey Instrument | Quantifies attitudes, experiences, and practices across a large sample of a target group (e.g., REB members, researchers) to generate generalizable data [31]. |
| Qualitative Data Analysis Software (e.g., NVivo) | Aids in the efficient organization, coding, and thematic analysis of large volumes of textual data from interviews or documents [28]. |
| Citation Tracking & Analysis Matrix | Enables systematic identification and review of publications that have engaged with a key guideline or paper to catalog critiques and identified gaps [28]. |
| Data Anonymization Framework | Protects participant confidentiality by providing a secure protocol for removing or encrypting identifiable information from collected data, which is crucial when studying ethics professionals [32]. |
The empirical foundation for ensuring high-quality ethics review is characterized by significant, evidence-based gaps. Critical questions about the optimal composition and training of REBs, effective oversight of big data and AI research, and the implementation of efficient international review models remain largely unanswered. Addressing these gaps requires a concerted effort from the research community, employing rigorous mixed-methods approaches, including scoping reviews, qualitative studies, and quantitative surveys. Filling these empirical voids is not merely an academic exercise; it is essential for building a more robust, effective, and trustworthy system for protecting human research participants in an evolving scientific landscape.
International Guidelines and Regulatory Frameworks (CIOMS, Common Rule)
The global landscape of health-related research is governed by a complex framework of ethical guidelines and regulatory requirements designed to protect human participants. Two of the most influential frameworks are the International Ethical Guidelines for Health-related Research Involving Humans developed by the Council for International Organizations of Medical Sciences (CIOMS) and the Common Rule (45 CFR Part 46) codified in United States regulations. While both share the fundamental goal of ethical research conduct, they differ significantly in their origin, scope, structure, and application. This guide provides a systematic comparison of these frameworks, focusing on their practical implications for research ethics boards (REBs), also known as institutional review boards (IRBs), and researchers operating in an international context. Understanding these distinctions is crucial for designing and implementing quality empirical ethics research that meets international standards [9] [33].
Framework Origins and Philosophical Underpinnings
The CIOMS guidelines and the U.S. Common Rule emerged from distinct historical contexts and philosophical traditions, shaping their fundamental approaches to research ethics.
CIOMS Guidelines: Developed collaboratively through the World Health Organization and UNESCO, CIOMS provides internationally applicable guidelines that are aspirational and principle-based. They are designed to be adapted across diverse cultural, economic, and legal environments, particularly in low- and middle-income countries. The guidelines build upon the Declaration of Helsinki and emphasize global health justice and contextual application. A key philosophical commitment is their focus on vulnerability and the need for community engagement, reflecting a global perspective on research ethics that seeks to be relevant beyond well-resourced settings [9] [33].
The Common Rule: As a U.S. federal regulation, the Common Rule is a legally binding, prescriptive framework primarily governing federally funded or supported research within the United States. It operationalizes the ethical principles outlined in the Belmont Report—respect for persons, beneficence, and justice—into specific regulatory requirements. Its philosophical basis is rooted in a rights-based approach within a specific regulatory culture, emphasizing procedural compliance and standardized protections across all institutions subject to its authority. The Common Rule's revisions aim to reduce administrative burden while maintaining rigorous participant protections, reflecting a focus on regulatory efficiency within a specific national context [33] [34].
Table 1: Foundational Characteristics of CIOMS and the Common Rule
| Characteristic | CIOMS Guidelines | U.S. Common Rule |
|---|---|---|
| Nature of Document | International ethical guidelines | U.S. federal regulation |
| Legal Status | Non-binding, aspirational | Legally binding for covered research |
| Primary Scope | Global; health-related research | U.S.; federally conducted/supported research |
| Philosophical Basis | Declaration of Helsinki; global health justice | Belmont Report; regulatory compliance |
| Regulatory Authority | None (advisory) | OHRP, FDA (for FDA-regulated research) |
| Key Revision Drivers | International expert consensus | Federal rulemaking process |
Structural Comparison and Key Provisions
A detailed analysis of structural elements reveals how each framework organizes its ethical requirements, with significant implications for research implementation and oversight.
Research Ethics Board (REB) Composition and Function
The requirements for ethics committee composition and operation highlight fundamental differences in approach between the two frameworks.
CIOMS REB Composition: CIOMS Guideline 23 mandates multidisciplinary membership with clearly specified categories of expertise. Required members include physicians, scientists, other professionals (nurses, lawyers, ethicists, coordinators), and community members or patient representatives who can represent participants' cultural and moral values. A distinctive feature is the recommendation to include members with personal experience as study participants. The guidelines explicitly state that committees must include both men and women and should invite representatives of relevant advocacy groups when reviewing research involving vulnerable populations. This framework emphasizes the collective competency and diverse perspective of the REB as essential for ethical review [9].
Common Rule IRB Composition: The Common Rule (45 CFR §46.107) specifies that an IRB must have at least five members with varying backgrounds. The composition must include at least one scientist, one non-scientist, and one member who is not otherwise affiliated with the institution. The regulation emphasizes that no IRB may consist entirely of men or women, and it must include representatives from diverse racial and cultural backgrounds. It also requires the IRB to be sufficiently qualified through the experience and expertise of its members to promote respect for its advice and counsel. The requirements are more focused on structural composition and conflict of interest avoidance rather than specific experiential backgrounds [9] [34].
Scope and Applicability
The domains of research covered by each framework differ substantially, reflecting their distinct purposes.
CIOMS Scope: The guidelines apply broadly to "health-related research involving humans," a comprehensive category that encompasses clinical, biomedical, and health-related socio-behavioral research. Their applicability is universal in intent, designed to provide guidance for any country seeking to establish or strengthen ethical review standards, with particular relevance for resource-limited settings [9] [33].
Common Rule Scope: The Common Rule applies specifically to "human subjects research" that is conducted or supported by any U.S. federal department or agency that has adopted the policy. It also applies to research that is submitted to the FDA as part of a marketing application for drugs or biological products, regardless of funding source. The definition of "human subject" focuses on a living individual about whom an investigator obtains data through intervention or interaction, or identifiable private information. This creates a more legally circumscribed domain of application [34].
Analytical Framework for Empirical Ethics Research
Evaluating the practical implementation of these frameworks requires robust empirical ethics research methodologies. The "road map" of quality criteria for empirical ethics provides a structured approach for such comparative analysis [19].
Quality Criteria for Empirical Ethics Research
Empirical ethics research integrates descriptive empirical methodologies with normative ethical analysis, requiring specific quality standards to ensure methodological rigor and ethical relevance.
- Primary Research Question: The research question must clearly bridge empirical inquiry and normative analysis, specifying how data collection will inform ethical evaluation of the frameworks.
- Theoretical Framework and Methods: The study must employ a sound empirical methodology (quantitative, qualitative, or mixed methods) appropriate for the research question, while also making explicit the normative ethical framework (e.g., principism, capabilities approach) used for analysis.
- Relevance: The research must demonstrate practical significance for REB/IRB operations, regulatory policy, or the protection of research participants, moving beyond purely theoretical discussion.
- Interdisciplinary Research Practice: The research process should facilitate genuine integration between empirical and normative dimensions, avoiding the mere juxtaposition of descriptive findings with ethical conclusions.
- Research Ethics and Scientific Ethos: The empirical investigation itself must adhere to rigorous ethical standards, including appropriate review, informed consent, confidentiality, and reflexivity about researcher positionality [19].
Experimental Protocol for Framework Comparison
The following protocol provides a methodological template for conducting empirical comparisons of ethical frameworks in practice.
Objective: To systematically compare the implementation of CIOMS guidelines and Common Rule requirements in REB/IRB review processes and outcomes.
Methodology:
- Site Selection: Identify multiple REBs/IRBs operating under each framework in comparable research institutions.
- Data Collection:
- Document Analysis: Systematically review REB/IRB standard operating procedures, membership rosters, and training materials.
- Structured Observation: Observe REB/IRB meetings reviewing identical simulated research protocols.
- Surveys and Interviews: Administer validated questionnaires and conduct semi-structured interviews with REB/IRB members and researchers.
- Variables Measured:
- REB/IRB Composition: Demographic diversity, expertise domains, member experience.
- Review Process Characteristics: Time to approval, number of revisions requested, specific concerns raised.
- Decision-Making Patterns: Emphasis on scientific, ethical, or regulatory considerations in deliberations.
- Participant Perspective Integration: Frequency and nature of community member contributions.
Analysis:
- Quantitative: Compare composition metrics and review outcomes using statistical methods (e.g., t-tests, chi-square).
- Qualitative: Employ thematic analysis to identify patterns in deliberation content and decision-making rationales.
- Integration: Synthesize quantitative and qualitative findings to evaluate how framework differences manifest in practical outcomes.
Conceptual Workflow for Empirical Ethics Research
The diagram below illustrates the integrated process for conducting empirical ethics research comparing ethical frameworks.
Comparative Analysis of Key Provisions
Direct comparison of specific provisions reveals how each framework addresses core ethical requirements, with implications for research implementation and participant protection.
Table 2: Detailed Comparison of Key Ethical Provisions
| Ethical Requirement | CIOMS Guidelines | U.S. Common Rule | Practical Implications for Research |
|---|---|---|---|
| Informed Consent | Emphasizes contextual adaptation and cultural appropriateness; requires understanding assessment. | Standardized required elements; specific regulatory language; waiver provisions under certain conditions. | CIOMS offers flexibility for diverse settings; Common Rule ensures consistency but may lack cultural nuance. |
| Vulnerable Populations | Explicit recognition of context-dependent vulnerability; requires special protections and representation. | Specifically enumerates vulnerable categories (pregnant women, prisoners, children); subparts B-D provide additional regulations. | CIOMS approach is more fluid and inclusive; Common Rule provides specific but potentially limited categorization. |
| Community Engagement | Strong emphasis on community consultation and participation in research design and review. | Limited requirements for community representation in IRB composition; no mandatory community consultation. | CIOMS promotes deeper stakeholder involvement; Common Rule focuses primarily on procedural representation. |
| Post-Trial Obligations | Explicitly addresses post-trial access to beneficial interventions; global fairness focus. | No specific requirement for post-trial access provision; focuses primarily on trial period protections. | CIOMS promotes greater responsibility for research sustainability; Common Rule limits obligations to study duration. |
| Training Requirements | Emphasizes continuous education and knowledge updating for all REB members. | Requires education on regulatory requirements but less emphasis on ongoing ethical training. | CIOMS supports deeper ethical deliberation capacity; Common Rule ensures regulatory compliance knowledge. |
Researchers conducting empirical studies on ethical frameworks require specific conceptual and methodological tools. The following table outlines key resources for rigorous investigation.
Table 3: Essential Research Reagents for Empirical Ethics Studies
| Research Reagent | Function in Empirical Ethics Research | Example Application |
|---|---|---|
| Validated Survey Instruments | Quantitatively measure REB/IRB member attitudes, perceptions, and experiences with ethical frameworks. | Assessing member confidence in reviewing specific protocol types across different regulatory environments. |
| Structured Observation Protocols | Systematically document REB/IRB deliberation dynamics, communication patterns, and decision-making processes. | Comparing how scientific vs. ethical considerations are weighted in deliberations under different frameworks. |
| Semi-Structured Interview Guides | Explore in-depth perspectives on implementation challenges, interpretive differences, and practical impacts. | Understanding how REB/IRB chairs navigate ambiguities in ethical guidelines when reviewing complex protocols. |
| Simulated Research Protocols | Standardized research scenarios used to evaluate consistency of review outcomes across different REBs/IRBs. | Testing how identical research proposals are evaluated under CIOMS-guided vs. Common Rule-guided review. |
| Document Analysis Frameworks | Systematically code and analyze REB/IRB policies, minutes, and correspondence for comparative assessment. | Identifying differences in required consent form elements and review procedures across regulatory frameworks. |
| Normative Analysis Frameworks | Provide structured approaches for evaluating the ethical implications of empirical findings. | Applying ethical principles to assess the practical implementation differences identified through empirical research. |
The comparative analysis reveals that CIOMS guidelines and the Common Rule represent complementary but distinct approaches to research ethics governance. CIOMS offers a flexible, principle-based framework with strong emphasis on contextual adaptation, community engagement, and global applicability, making it particularly valuable for international research and resource-limited settings. In contrast, the Common Rule provides a detailed, legally binding regulatory framework that ensures standardized protections and procedural compliance within the U.S. research context.
For researchers and ethics committee members operating in a globalized research environment, understanding these distinctions is essential for designing ethically sound studies that satisfy multiple regulatory standards. The optimal approach often involves applying the universal principles of CIOMS within the specific regulatory requirements of the Common Rule where applicable. Future empirical research should continue to examine how these frameworks interact in practice, particularly as international collaborative research increases and regulatory systems continue to evolve. The quality criteria for empirical ethics research provide a robust methodology for conducting these important comparative investigations [19].
Implementing Rigorous Methods: Standards and Reporting Frameworks
Empirical ethics research provides critical insights into complex healthcare dilemmas, bridging descriptive evidence and normative reflection [19]. This interdisciplinary field, which integrates methodologies from social sciences with philosophical analysis, has seen substantial growth; one quantitative analysis of nine bioethics journals revealed a statistically significant increase in empirical research publications from 1990 to 2003 [7]. However, this expansion has surfaced persistent methodological concerns, particularly regarding how to maintain scientific rigor while responding to urgent ethical questions in real-time.
The emergence of rapid evaluation approaches addresses the critical factor of timeliness in influencing the utility of research findings, especially in contexts like humanitarian crises, evolving health services, or global health emergencies [35]. These approaches are characterized by their short duration, use of multiple data collection methods, team-based research structures, and formative designs that provide actionable findings to policymakers and practitioners [35]. Despite their potential, rapid methods face significant challenges including questions about validity, reliability, and representativeness due to compressed timeframes, potentially leading to unfounded interpretations and conclusions [35].
To address these challenges, the STREAM (Standards for Rapid Evaluation and Appraisal Methods) framework was developed through a rigorous consensus process [35]. This framework establishes methodological standards specifically designed for rapid research contexts, providing guidance for improving transparency, completeness of reporting, and overall quality of rapid studies [36]. For empirical ethics researchers, STREAM offers a structured approach to navigating the tension between methodological rigor and practical urgency, ensuring that rapid findings maintain scientific integrity while remaining responsive to pressing ethical dilemmas.
Understanding the STREAM Framework
Development and Structure
The STREAM framework was developed through a meticulous four-stage consensus process designed to incorporate diverse expert perspectives [35]. The development methodology began with a steering group consultation, followed by a three-stage e-Delphi study involving stakeholders with experience in conducting, commissioning, or participating in rapid evaluations [35]. This process culminated in a stakeholder consensus workshop and a piloting exercise to refine the standards for practical application [35]. The e-Delphi study employed strict consensus thresholds, requiring 70% or more of participants to rate an item as relevant with 15% or less rating it as irrelevant for inclusion [35].
Through this rigorous process, 38 distinct standards were established, organized to guide the entire research lifecycle from initial design through implementation and reporting [35]. These standards address fundamental concerns in rapid research methodology, including transparency in reporting, maintaining methodological rigor, ensuring ethical practice, and enhancing the validity and utility of findings produced within compressed timeframes [35]. The framework is designed to be flexible enough to accommodate various rapid evaluation approaches while establishing clear benchmarks for quality.
Scope and Application
STREAM is intentionally designed for broad application across multiple research contexts and methodologies [36]. The framework applies to observational studies, qualitative research, mixed-methods approaches, and service quality improvement studies—essentially any research形式 utilizing rapid evaluation approaches [36]. This breadth of application makes it particularly valuable for empirical ethics research, which often employs diverse methodological approaches to address complex normative questions.
The framework serves three primary functions for researchers: (1) as guidelines for designing and implementing rapid evaluations and appraisals; (2) as reporting templates to ensure complete and transparent documentation of methods; and (3) as a quality assessment tool for evaluating existing rapid studies [36]. This multi-function approach addresses the critical need for standardized reporting in rapid research, where adaptations and methodological shortcuts can sometimes obscure important limitations or methodological decisions [35].
For empirical ethics researchers operating in time-sensitive contexts, STREAM provides a structured approach to maintaining scientific integrity while delivering timely findings. The framework helps researchers navigate common challenges in rapid research, such as balancing breadth and depth of data collection, managing team-based variability in data interpretation, and ensuring representative sampling despite shorter fieldwork periods [35].
Comparative Analysis: STREAM Versus Alternative Approaches
Methodological Comparison
When evaluated against other methodological standards, STREAM demonstrates distinct characteristics tailored specifically to the challenges of rapid research. Unlike broader empirical ethics quality criteria, which provide a "road map" of reflective questions across categories like primary research question, theoretical framework, relevance, and interdisciplinary practice [19], STREAM offers concrete, actionable standards for maintaining rigor within time-constrained environments.
The following table compares STREAM's key characteristics with general quality criteria for empirical ethics research and traditional non-rapid methodological standards:
Table 1: Comparison of STREAM with Alternative Methodological Approaches
| Aspect | STREAM Framework | General Empirical Ethics Quality Criteria [19] | Traditional Non-Rapid Standards |
|---|---|---|---|
| Time Consideration | Explicitly designed for compressed timelines | Time-neutral | Assumes extended timeframes |
| Methodological Flexibility | High flexibility with transparency requirements | Methodology-dependent | Often methodology-specific |
| Integration of Empirical & Normative | Implicit in design for ethics contexts | Explicit focus on integration | Often separate processes |
| Transparency Emphasis | High focus on reporting adaptations | Moderate focus on transparency | Standardized reporting |
| Primary Application | Rapid evaluations, appraisals, assessments | Broad empirical ethics research | Discipline-specific research |
| Development Process | Formal Delphi study & consensus workshop [35] | Theoretical analysis & working group [19] | Various development methods |
STREAM's development process represents a significant strength, employing rigorous consensus-building methods that incorporated diverse stakeholder perspectives [35]. The framework addresses a critical gap in methodological standards, as no previously published guidelines specifically focused on rapid evaluations and appraisals existed before STREAM's development [35].
Application in Empirical Ethics
For empirical ethics research, STREAM addresses specific methodological challenges that distinguish it from other approaches. While general quality criteria for empirical ethics emphasize the integration of descriptive and normative statements and the importance of interdisciplinary team work [19], STREAM provides practical guidance on maintaining this integration under time constraints.
A key advantage of STREAM for empirical ethics is its explicit attention to validity threats unique to rapid methodologies. These include short-term data collection periods that may miss evolving ethical perspectives, reliance on easily accessible participants potentially lacking diversity of viewpoints, compressed analysis periods allowing limited critical reflection, and variability in team-based data interpretation [35]. By addressing these threats through standardized practices, STREAM helps empirical ethics researchers produce findings with greater methodological integrity.
Unlike discipline-specific guidelines, STREAM's broad applicability makes it particularly valuable for the inherently interdisciplinary nature of empirical ethics, which combines methodologies from social sciences with normative analysis [19]. The framework facilitates the "analytical distinction between descriptive and normative statements" that is essential for evaluating their validity in empirical ethics research [19], while providing guidance on maintaining this distinction when working within compressed timeframes.
Experimental Protocols and Validation
STREAM Development Methodology
The experimental protocol for developing the STREAM framework was characterized by rigorous, systematic consensus-building. The process began with a comprehensive systematic review to identify methods used to ensure rigor, transparency, and validity in rapid evaluation approaches [35] [37]. This review informed the initial list of items for the e-Delphi study, which was further refined through steering group consultation [35].
The e-Delphi study implemented a structured three-round survey process using the Welphi platform, with invitations extended to 283 potential participants identified through purposive sampling [35]. The participant selection criteria specifically included stakeholders with experience in "conducting, participating, reviewing or using findings from rapid studies" [35], ensuring that the resulting standards were grounded in practical expertise. The target sample size of 50-80 participants accounted for anticipated attrition across rounds [35].
Following the Delphi process, a stakeholder consensus workshop was conducted in June 2023 to refine the clarity and practical application of the standards [35]. The final validation stage involved a piloting exercise to understand STREAM's validity in practice [35]. This multi-stage development methodology aligns with established protocols for reporting guideline development, including registration on the EQUATOR network and publication of a protocol on the Open Science Framework [35].
Implementation Workflow
The following diagram illustrates the sequential development and implementation process for the STREAM framework:
Validation Outcomes
The validation process for STREAM demonstrated its practical utility across multiple dimensions. The e-Delphi study achieved consensus on 38 standards through its structured ranking process, where participants rated each statement's relevance on a 4-point Likert scale [35]. The piloted implementation of STREAM allowed researchers to assess the framework's viability in actual research settings, leading to refinements that enhanced its practical application [35].
Unlike earlier approaches to empirical ethics quality that provided primarily theoretical guidance [19], STREAM's development incorporated empirical testing and iterative refinement. The framework addresses specific methodological shortcomings identified in prior research, including the lack of transparency in rapid study methods and adaptations made throughout the research process [35]. This empirical grounding in both development and validation distinguishes STREAM from more theoretically-derived quality criteria.
Essential Research Toolkit for Implementation
Implementing the STREAM framework effectively requires utilizing specific methodological tools and approaches. The following research reagent solutions provide the essential components for applying STREAM standards to rapid evaluation projects in empirical ethics research:
Table 2: Research Reagent Solutions for STREAM Implementation
| Tool Category | Specific Solution | Function in STREAM Implementation |
|---|---|---|
| Consensus Building Tools | e-Delphi Platform (e.g., Welphi) | Facilitates structured expert consensus on methodological standards [35] |
| Reporting Guidelines | EQUATOR Network Standards | Enhances transparency and completeness of reporting [35] |
| Protocol Registries | Open Science Framework (OSF) | Provides public study registration and protocol documentation [35] |
| Stakeholder Engagement | Consensus Workshops | Enables collaborative refinement of standards [35] |
| Piloting Frameworks | Field Testing Protocols | Validates practical application of standards in diverse contexts [35] |
| Systematic Review Methods | PRISMA-guided Reviews | Identifies methodological gaps and best practices [37] |
These research reagents collectively address the core challenges in rapid evaluation methodologies. The consensus-building tools enable the development of standardized approaches that maintain flexibility for different research contexts. Reporting guidelines and protocol registries directly address the transparency issues that have plagued rapid research, where methodological adaptations often go unreported [35]. Stakeholder engagement mechanisms ensure that the resulting standards remain grounded in practical research realities rather than theoretical ideals.
For empirical ethics researchers, these tools facilitate the crucial integration of empirical and normative elements—a core challenge in the field [19]. By providing structured approaches to methodological transparency, STREAM's research reagents help researchers maintain clear distinctions between descriptive findings and normative conclusions, thereby enhancing the overall validity of empirical ethics research conducted under time constraints.
Implications for Empirical Ethics Research
Advancing Methodological Rigor
The STREAM framework introduces significant advancements for maintaining methodological rigor in empirical ethics research. By providing 38 specific standards tailored to rapid contexts, STREAM addresses the fundamental tension between timeliness and validity that has long challenged researchers in this field [35]. For empirical ethics, this is particularly crucial given the potential consequences of methodological shortcomings—as noted in prior research, "poor methodology in an EE study results in misleading ethical analyses, evaluations or recommendations" which "not only deprives the study of scientific and social value, but also risks ethical misjudgement" [19].
STREAM's structured approach to transparency in reporting helps mitigate common validity threats in rapid empirical ethics research, including short-term data collection that may not capture evolving ethical perspectives, reliance on easily accessible participants potentially lacking diversity of viewpoints, and compressed analysis periods allowing limited critical reflection [35]. By establishing clear standards for documenting methodological adaptations and limitations, STREAM enables more accurate assessment of findings' reliability and transferability.
Future Directions and Applications
The development of STREAM represents an important milestone in a broader evolution toward standardized methodologies in empirical research. As the field continues to recognize the importance of both empirical and normative elements in bioethical inquiry—evidenced by the significant increase in empirical publications in bioethics journals between 1990 and 2003 [7]—frameworks like STREAM provide essential guidance for maintaining quality amidst growing methodological diversity.
Future applications of STREAM in empirical ethics research could include adapting the standards for specific ethical domains such as clinical ethics consultation, research ethics committee deliberations, or emerging technology assessment. The framework's flexibility makes it suitable for addressing timely ethical questions in rapidly evolving fields like genetics, artificial intelligence, and pandemic response, where traditional lengthy research timelines may fail to provide timely guidance.
As empirical ethics continues to develop as an interdisciplinary field, STREAM offers a promising approach for bridging methodological divides between social scientific and philosophical inquiry. By establishing common standards for rigorous rapid research, the framework facilitates more meaningful collaboration across disciplines while maintaining the distinctive strengths of each approach to ethical investigation.
Research reporting guidelines are systematically developed tools designed to improve the transparency and quality of scientific publications. They provide specific recommendations, often in the form of checklists or flow diagrams, to ensure authors comprehensively report all essential elements of their research methodology and findings [38]. The EQUATOR Network (Enhancing the QUAlity and Transparency Of health Research) serves as a central hub for these resources, operating as an international initiative that "develops and maintains a comprehensive collection of online resources providing up-to-date information, tools, and other materials related to health research reporting" [38]. Founded in 2006, the EQUATOR Network maintains a searchable library of over 250 reporting guidelines and supports their implementation through educational resources and toolkits [39] [40] [38].
For empirical ethics research, which often employs diverse methodological approaches, rigorous reporting is particularly crucial. Transparent methodology allows readers to critically assess the interpretive process and the validity of ethical analyses derived from empirical data. Adherence to reporting guidelines ensures that the complex methodological decisions inherent in ethics research—from data collection to normative analysis—are fully visible and evaluable.
Key Reporting Guidelines for Health Research
The EQUATOR Network library catalogs guidelines for various study designs, each addressing the unique reporting requirements of different research methodologies [40]. The table below summarizes the core, high-use guidelines essential for health researchers.
Table 1: Foundational Reporting Guidelines for Key Study Designs
| Study Type | Guideline Name | Primary Function | Key Components | Relevance to Ethics Research |
|---|---|---|---|---|
| Randomized Trials | CONSORT (Consolidated Standards of Reporting Trials) [41] | Standardizes reporting of randomized controlled trials (RCTs). | Checklist and participant flow diagram [38]. | Reports ethics of trial conduct; RCTs evaluating ethics interventions. |
| Observational Studies | STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) [38] | Improves reporting of cohort, case-control, and cross-sectional studies. | Checklist for contextualizing causal claims [38]. | Common design for studying real-world ethical practices. |
| Systematic Reviews | PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) [38] | Ensures complete reporting of systematic reviews and meta-analyses. | Checklist and flow diagram for study selection [38]. | Essential for systematic reviews of ethics literature. |
| Case Reports | CARE (Case Reports) [42] | Provides structure for reporting clinical case information. | Detailed narrative checklist [42]. | Publishing and analyzing individual clinical ethics cases. |
| Non-Randomized Intervention Evaluations | TREND (Transparent Reporting of Evaluations with Nonrandomized Designs) [43] | Aims to improve the reporting quality of nonrandomized behavioral and public health intervention studies. | Checklist for study design, methods, and findings [43]. | Evaluating ethics education interventions or policy changes. |
Specialized and Emerging Guidelines
Beyond these foundational guidelines, numerous specialized extensions and emerging standards address niche methodological needs. For instance, the TARGET Statement provides a framework for the "Transparent Reporting of Observational Studies Emulating a Target Trial," guiding analyses of observational data that aim to estimate causal effects [44]. This is crucial for generating robust evidence from real-world data when RCTs are not feasible.
Several important guidelines are also under development, reflecting the evolving nature of research methodologies. These include:
- PRISMA-Ethics: An official extension currently being developed to address the particularities of systematic reviews on ethically sensitive topics, which often involve conceptual and qualitative syntheses [45].
- PRISMA-AI: An extension to standardize the reporting of systematic reviews investigating Artificial Intelligence (AI) in medicine, ensuring technical details required for reproducibility are clearly documented [45].
- MISTIC: A guideline under development for reporting methodological studies, which "appraise the design, conduct, analysis and reporting of other studies" [46]. This is highly relevant for meta-research in empirical ethics.
Comparative Analysis of Guideline Implementation
Methodology for Comparing Reporting Quality
To objectively assess the impact of reporting guidelines, a common experimental protocol involves comparing the completeness of publications before and after the introduction of a specific guideline or between adherent and non-adherent reports.
- Study Selection: Researchers identify a sample of published articles from a defined time period, often stratified into pre-guideline and post-guideline publication cohorts.
- Quality Assessment: Each article is evaluated against the relevant reporting guideline checklist (e.g., CONSORT, STROBE). Items are scored based on whether the required information is clearly reported, partially reported, or not reported.
- Data Analysis: The overall completeness of reporting is calculated, typically as a percentage of adequately reported items from the total checklist. Statistical analyses (e.g., t-tests, regression models) are then used to compare the mean scores between the pre- and post-guideline groups, controlling for potential confounders like journal impact factor.
Table 2: Experimental Data on the Impact of Reporting Guidelines
| Guideline (Study Focus) | Comparison Groups | Key Metric: Mean Completeness of Reporting | Observed Outcome / Effect Size |
|---|---|---|---|
| CONSORT for RCTs | Pre-CONSORT (1994) vs. Post-CONSORT (1998) publications in key medical journals. | Percentage of CONSORT checklist items fully reported. | Significant improvement in the reporting of key methodological aspects like randomization methods and allocation concealment. |
| STROBE for Observational Studies | Articles citing STROBE vs. matched controls not citing STROBE. | Adherence score based on the STROBE checklist. | Studies citing STROBE demonstrated significantly better reporting of titles, abstracts, objectives, methods, and results. |
| PRISMA for Systematic Reviews | Pre-PRISMA (2004-2008) vs. Post-PRISMA (2009-2013) systematic reviews. | Percentage of PRISMA checklist items satisfactorily reported. | Statistically significant increase in the reporting of structured summaries, protocols, search strategies, and risk of bias assessments. |
| CARE for Case Reports | Case reports published using the CARE checklist vs. those published before its release. | Fulfillment of core case report elements (e.g., patient history, diagnostic findings). | CARE-based reports showed more consistent and complete inclusion of clinical data, intervention details, and patient outcomes. |
Workflow for Applying Reporting Guidelines
The following diagram illustrates the standard workflow a researcher should follow to select and apply the appropriate reporting guideline, from the initial study design phase to manuscript submission.
Successful implementation of reporting guidelines relies on a suite of key resources. The table below details these essential tools and their primary functions in the research and publication process.
Table 3: Essential Research Reagent Solutions for Transparent Reporting
| Resource Name | Category | Primary Function | Source / Access |
|---|---|---|---|
| EQUATOR Network Library | Database | A comprehensive, searchable database of reporting guidelines for all health research designs [39] [40]. | EQUATOR Network Website |
| Explanation & Elaboration (E&E) Documents | Guidance Document | Provides the rationale for each checklist item with examples of good reporting, which is crucial for correct interpretation [41] [42]. | Published alongside main guidelines; linked in the EQUATOR Library. |
| GoodReports Tool | Online Platform | An interactive website that hosts online, fillable versions of key reporting guideline checklists, such as those for CARE case reports [42]. | GoodReports Website |
| Author Toolkit | Educational Resource | A collection of practical help and resources on the EQUATOR site to support authors in writing and publishing high-impact research [39] [38]. | EQUATOR Network website "Toolkits" section. |
| CARE Flow Diagram | Methodology Aid | A visual guide to help clinicians systematically collect and report data from patient encounters or chart reviews for case reports [42]. | Available for download from the CARE website. |
Reporting guidelines curated by the EQUATOR Network are indispensable tools for enhancing the transparency, reproducibility, and overall quality of health research. For the field of empirical ethics, their rigorous application is not merely a technical exercise but a fundamental component of methodological rigor. By ensuring the complete and transparent reporting of how empirical data on ethical issues is collected, analyzed, and interpreted, researchers strengthen the validity of their findings and their contribution to the broader discourse. As the research landscape evolves with new methodologies in AI, modeling, and qualitative synthesis, the ongoing development of guidelines like PRISMA-AI and PRISMA-Ethics will continue to provide the critical scaffolding necessary for trustworthy science.
Incorporating Ethical Elements into Research Reporting
Empirical ethics research occupies a unique interdisciplinary space, integrating socio-empirical investigations with normative ethical analysis to address complex moral questions in fields like medicine and clinical research [19] [1]. Unlike purely descriptive research, empirical ethics aims to generate normative conclusions and recommendations, making transparent and ethical reporting practices particularly crucial [19]. The methodology of empirical ethics research involves what can be understood as "mixed judgments," containing both normative propositions and descriptive or empirical premises [1]. This hybrid nature creates distinctive ethical challenges throughout the research process—from design to dissemination.
Poor methodological execution or reporting in empirical ethics does not merely compromise scientific quality; it risks generating misleading ethical analyses that can have tangible negative consequences when translated into practice [19]. Research has demonstrated that the composition, expertise, and training of Research Ethics Boards (REBs) significantly influence their decision-making processes, yet evidence regarding optimal composition remains limited [47] [9]. This underscores the importance of transparent reporting that allows for critical evaluation of research ethics processes and outcomes.
This article examines key ethical considerations in reporting empirical ethics research, with particular attention to interdisciplinary methodology, transparency in normative frameworks, and ethical data presentation. We compare different approaches to addressing these challenges and provide evidence-based recommendations for enhancing ethical reporting practices.
Quality Criteria for Empirical Ethics Research: A Comparative Analysis
Methodological Rigor in Interdisciplinary Research
Empirical ethics research employs diverse methodological approaches, each with distinctive strengths and ethical considerations. The table below compares four prominent methodological frameworks used in empirical ethics research:
| Methodological Approach | Key Characteristics | Primary Ethical Considerations | Suitable Research Questions |
|---|---|---|---|
| Graphical Model Selection [48] | Uses probabilistic graphical models to display relationships among ethically-salient variables; reveals patterns of stakeholder perspectives | Visual representation of complex ethical perspectives; preserves nuance in ethical viewpoints | How do different stakeholder groups conceptualize ethical acceptability in research? |
| Quality Criteria Road Map [19] | Provides reflective questions across multiple domains: primary research question, theoretical framework, methods, relevance, interdisciplinary practice | Ensures integration of empirical and normative elements; maintains philosophical rigor | What constitutes valid interdisciplinary methodology in empirical ethics? |
| Transparent Theory Selection [1] | Systematic approach to selecting and justifying ethical theories as normative background; addresses pluralism | Explicit justification of normative framework; acknowledges theoretical limitations | How does selection of ethical theory influence empirical ethics research outcomes? |
| Critical Data Ethics Framework [49] | Emphasizes ethics throughout research cycle; focuses on power dynamics and vulnerable populations | Addresses data justice issues; protects vulnerable groups; considers political dimensions of data | How do data practices affect marginalized communities in ethics research? |
Each approach offers distinct advantages for different research contexts. Graphical model selection excels in visualizing complex relationships between ethical perspectives [48], while the quality criteria road map provides comprehensive guidance for interdisciplinary research design [19]. The choice of methodology should align with the research question while explicitly addressing associated ethical considerations.
Theoretical Framework Transparency
The selection and justification of normative ethical theories constitutes a critical methodological decision in empirical ethics research that requires transparent reporting [1]. Unlike purely empirical research, empirical ethics must explicitly address its normative foundations, as these frameworks fundamentally shape research questions, data interpretation, and conclusions.
A systematic approach to theory selection should consider three key criteria [1]:
- Adequacy for the issue: The ethical theory must provide appropriate conceptual resources for the specific ethical problem under investigation
- Suitability for research design: The theory must align with the study's purposes and methodological approach
- Interrelation with empirical frameworks: Compatibility between the ethical theory and theoretical backgrounds of the socio-empirical research components
Research indicates that inadequate attention to theory selection can result in "crypto-normative" conclusions where implicit evaluations are made without explicit justification [19]. Transparent reporting requires researchers to document their theory selection process, including consideration of alternative frameworks and rationales for their ultimate choice.
Experimental Protocols and Data Presentation in Ethics Research
Data Collection Methodologies
Empirical ethics research employs diverse data collection methods, each with distinctive ethical implications. The following experimental protocol exemplifies a comprehensive approach to assessing perspectives on research ethics:
Protocol: Assessing Stakeholder Perspectives on Ethical Acceptability of Research [48]
- Study Population: Recruitment of 179 participants across four groups: (1) volunteers with mental illness (schizophrenia, depression, anxiety); (2) volunteers with physical illness (cancer, HIV/AIDS, diabetes); (3) healthy research participants; and (4) research-naive healthy individuals
- Survey Instrument: 301-item questionnaire with 23 open-ended questions, assessing domains including importance of medical research, subjective views on participation, and perceptions of risk
- Data Collection Procedure: Interviews conducted within 7 days of consenting to clinical protocols; sessions lasting 1.5-2 hours; compensation provided
- Ethical Safeguards: Written informed consent; no sharing of research data with clinical teams; IRB approval
- Analytical Method: Graphical model selection to display interrelationships among ethically-salient perspectives
This protocol demonstrates key ethical considerations in empirical ethics research, including protection of vulnerable populations, appropriate compensation, and separation of research data from clinical care.
Ethical Data Visualization Practices
Effective and ethical data presentation is particularly crucial in empirical ethics research, where visual representations of findings can influence interpretation of normative conclusions. The following diagram illustrates key relationships in empirical ethics research using Graphviz:
Empirical Ethics Research Flow
Adherence to ethical visualization principles requires attention to multiple dimensions of data presentation [50]:
- Accuracy and Transparency: Use complete datasets, avoid manipulative axes scaling, and clearly document data sources and limitations
- Accessibility: Implement colorblind-friendly palettes, provide alternative text, ensure sufficient contrast, and accommodate varying data literacy levels
- Bias Mitigation: Actively identify and address confirmation bias, cultural bias, and color bias in visual representations
- Privacy Protection: Anonymize sensitive information, group data to prevent identification, and verify consent for data sharing
These practices are particularly important in empirical ethics research, where visual representations of complex ethical perspectives must preserve nuance while remaining accessible to diverse audiences.
Analytical Frameworks and Quality Assessment Tools
Implementing robust ethical reporting practices requires specific conceptual tools and frameworks. The following table outlines essential resources for enhancing ethical reporting in empirical ethics research:
| Tool Category | Specific Resource | Function in Ethical Reporting |
|---|---|---|
| Quality Assessment | "Road Map" of Quality Criteria [19] | Provides reflective questions for evaluating research quality across multiple domains |
| Theoretical Justification | Transparent Theory Selection Framework [1] | Guides explicit justification of normative frameworks and acknowledgment of theoretical limitations |
| Data Analysis | Graphical Model Selection [48] | Enables visualization of complex relationships between ethical perspectives while preserving nuance |
| Critical Evaluation | Critical Data Ethics Framework [49] | Facilitates examination of power dynamics and protection of vulnerable populations in data practices |
| Reporting Standards | REB Composition Guidelines [9] | Provides benchmarks for reporting ethics review processes and board expertise |
These tools collectively address the distinctive challenges of reporting empirical ethics research, particularly the integration of empirical and normative elements and the transparent documentation of methodological choices.
Implementing Ethical Visualization Tools
Selecting appropriate technological tools is essential for implementing ethical data presentation practices. Research comparing data ethics incorporation in academic curricula identifies several platforms with features supporting ethical visualization [49]:
- Tableau: Creates public dashboards with data source transparency and accessibility compliance features
- Power BI: Includes data masking, secure sharing capabilities, and bias detection algorithms
- D3.js: Enables fully customizable visualizations with accessibility guideline implementation
When selecting visualization tools, researchers should prioritize features that support data transparency, privacy protection, accessibility, and bias prevention [50]. These technical capabilities align with the broader ethical obligations of empirical ethics researchers to communicate findings accurately and responsibly.
Incorporating robust ethical elements into research reporting requires systematic attention to methodological transparency, interdisciplinary integration, and responsible communication practices. The comparative analysis presented in this article demonstrates that no single approach satisfies all ethical reporting requirements; rather, researchers must select and combine methodologies appropriate to their specific research questions and contexts.
The future of ethical reporting in empirical ethics research will likely involve continued refinement of quality criteria, development of more sophisticated analytical frameworks, and enhanced training in ethical visualization techniques. By adopting the tools and approaches outlined in this analysis, researchers can enhance the transparency, rigor, and societal value of empirical ethics research, ultimately contributing to more trustworthy ethical guidance for complex practical problems across healthcare and scientific domains.
In the fast-paced environments of health services research and empirical ethics, the demand for timely evidence often conflicts with the necessity for methodologically robust findings. This guide compares the performance of various rapid evaluation approaches against traditional, longer-term designs, examining the trade-offs and solutions that define modern methodological choices. The drive to better align evaluative processes with the decision-making timelines of service planners and policymakers has made rapid evaluation an essential, yet carefully considered, tool in the researcher's toolkit [51]. This analysis synthesizes experimental data and methodological frameworks to provide a clear comparison of how different approaches balance the critical demands of speed and scientific rigor.
Defining the Methodological Spectrum
What Constitutes Rapid Evaluation?
Rapidity in evaluation is not defined by a single timeframe but rather exists on a spectrum. Studies labeled as "rapid" can range from durations of six days to three years, reflecting the context-dependent nature of timeliness in research [51]. Beyond overall duration, rapidity might also refer to contracted time periods for commissioning, mobilizing new studies, or reporting findings [51].
Methodologically, rapid evaluation encompasses several distinct approaches, which can be categorized into four main types according to Norman et al. [51]:
- Methodologies specifically designed for rapid evaluation
- Reduced scope or less time-intensive methodologies
- Alternative technologies for rapid data acquisition/analysis or use of existing datasets
- Discrete elements of non-rapid studies undertaken rapidly
In qualitative research, rapid approaches may include analyses based on recordings or notes (eliminating transcription time) and methods for rapidly summarizing data such as mind maps or structured rapid assessment procedure sheets. In quantitative research, techniques may involve scenario-based counterfactuals, measurement of interim endpoints, and modeling longer-term outcomes from early data [51].
Comparative Analysis of Methodological Trade-offs
Key Trade-offs Between Rapid and Traditional Evaluations
Table 1: Methodological Trade-offs in Rapid Versus Traditional Evaluation Approaches
| Aspect | Rapid Evaluation | Traditional Evaluation | Key Trade-offs |
|---|---|---|---|
| Timeframe | Days to months (typically aligned with decision windows) [51] | Months to years | Timeliness vs. Depth: Rapid approaches provide actionable evidence when needed but may lack longitudinal perspective |
| Evidence Quality | "Good enough" for specific, time-bound decisions [51] | Comprehensive, seeking high certainty | Practicality vs. Generalizability: Rapid evidence addresses immediate needs but may have limited transferability |
| Methodological Compromises | Often requires simplified approaches, smaller samples, accelerated analysis [51] | More comprehensive methods, larger samples, thorough analysis | Efficiency vs. Robustness: Speed often requires accepting greater uncertainty in findings [52] |
| Suitability | Ideal for formative learning, innovation refinement, time-critical decisions [51] | Better for "high stakes" topics where evidence robustness is paramount [51] | Contextual Fit vs. Universal Application: Each approach serves different decision-making needs |
| Recruitment Approach | Often limited to easily accessible sites and participants [51] | Can employ more systematic, representative sampling | Accessibility vs. Representation: Rapid methods may sacrifice diversity for speed |
Experimental Data on Methodological Comparisons
Few studies have directly compared rapid and non-rapid approaches using the same dataset. However, one notable experiment analyzed the same qualitative dataset using both rapid and non-rapid analysis approaches [51]. The findings revealed:
- Considerable overlap in the results and recommendations between approaches
- Reduced depth and detail when using more deductive approaches to achieve rapidity
- Similar core insights despite methodological differences
This experimental comparison suggests that while rapid approaches can identify central themes and recommendations, they may miss nuanced understandings that emerge from more prolonged, inductive analytical processes [51].
Frameworks for Methodological Choice
The Certainty-Rigor Framework
A developing framework for right-fit methodological selection proposes that the level of rigor should correlate with the team's level of certainty about the program design being investigated [53]. This approach suggests:
- With less certainty, less rigor is needed - When confidence in a program design is low, less rigorous methods are appropriate for initial testing and adaptation
- With more certainty, more rigor is needed - As confidence grows, more rigorous methods should be employed to validate effects
This framework utilizes four criteria to assess certainty and determine appropriate methodological rigor [53]:
Table 2: Four Dimensions of Certainty in the Rigor Framework
| Dimension | Low Certainty End of Spectrum | High Certainty End of Spectrum |
|---|---|---|
| Context | New or highly dynamic environment | Stable, well-understood environment |
| Maturity | Early-stage innovation or program | Established, well-tested program |
| Precision | Broad learning questions focused on general direction | Specific questions requiring precise measurement |
| Urgency | Immediate decision deadline allowing only rapid methods | Longer timeframe permitting comprehensive assessment |
Rapid Evidence Synthesis (RES) Framework
The Greater Manchester Applied Research Collaboration has developed a structured approach to Rapid Evidence Synthesis that delivers assessments within two weeks while maintaining methodological integrity [54]. This framework incorporates several key elements to balance speed and rigor:
- Systematic but streamlined processes enabling replicable, transparent delivery
- GRADE Evidence to Decision framework for assessing evidence certainty and relevance
- Flexible question sets with provisions for category-level appraisal or component analysis
- Explicit consideration of relevance to local context alongside evidence reliability
Experimental implementation of this RES approach demonstrates that it requires approximately two days of researcher time spread over a two-week period, though more complex innovations may require additional resources [54]. Stakeholders in the decision-making process have found this approach "both timely and flexible" while valuing its "combination of rigour and speed" [54].
Solutions for Maintaining Rigor in Rapid Contexts
Methodological Adaptations Across Research Approaches
Table 3: Methodological Adaptations for Maintaining Rigor in Rapid Evaluation
| Research Approach | Rapid Adaptations | Rigor Maintenance Strategies |
|---|---|---|
| Qualitative Methods | Rapid analysis techniques (e.g., mind maps, RAP sheets); analysis from recordings/notes (avoiding transcription) [51] | Researcher reflexivity; triangulation; structured rapid assessment procedures; member checking when possible [55] |
| Quantitative Methods | Analysis of short-term outcomes; extrapolation from prior evidence; real-time monitoring; use of interim endpoints [52] | Clear documentation of uncertainty; sensitivity analysis; validation with existing datasets; transparency about limitations [52] |
| Mixed Methods | Simultaneous rather than sequential data collection; accelerated synthesis approaches [52] | Intentional integration of different data sources; team-based analysis to incorporate multiple perspectives; explicit mapping of convergent/discordant findings [51] |
| Evidence Synthesis | Rapid review methodologies; streamlined search and extraction; focused question formulation [54] | Systematic search strategies (even if limited); quality appraisal using standardized tools; transparent reporting of limitations [54] |
Infrastructure and Process Solutions
Research teams conducting rapid evaluation have developed specific infrastructures and processes that reduce the need for methodological compromises [51]. These include:
- Advanced data sharing agreements that permit use of routine data (e.g., Hospital Episode Statistics) across multiple projects without renegotiation [52]
- Trusted Research Environments or data safe havens that provide secure access to sensitive data while streamlining governance processes
- Flexible rapid response teams with expertise in both rapid methods and substantive domains
- Structured rapid assessment protocols that maintain consistency despite compressed timeframes
Table 4: Key Research Reagent Solutions for Rapid Evaluation
| Tool/Resource | Function | Application Context |
|---|---|---|
| Rapid Assessment Procedure (RAP) Sheets | Structured templates for rapid qualitative data summarization | Qualitative data analysis in compressed timeframes [51] |
| GRADE Evidence to Decision Framework | Systematically assesses evidence certainty and relevance to specific contexts | Rapid evidence synthesis and policy decision support [54] |
| Routine Health System Data | Pre-collected administrative data for near real-time analysis | Quantitative evaluation when primary data collection is infeasible [52] |
| Trusted Research Environments | Secure data access platforms with pre-approved governance | Accelerated access to sensitive or restricted datasets [52] |
| Structured Rapid Evaluation Protocols | Standardized methodologies for specific rapid evaluation scenarios | Ensuring consistency and comparability across rapid studies [51] |
| Flexible Rapid Response Teams | Multidisciplinary teams with both methodological and subject expertise | Comprehensive rapid assessment of complex health innovations [51] |
The methodological landscape for balancing rapidity and rigor continues to evolve, with researchers developing increasingly sophisticated approaches to deliver timely yet trustworthy evidence. The experimental data and frameworks presented demonstrate that rapid evaluation serves specific, practical purposes rather than replacing more comprehensive long-term designs. By carefully matching methodological choices to decision contexts, employing structured approaches to maintain quality, and transparently acknowledging limitations, researchers can provide "good enough" evidence for time-critical decisions without sacrificing scientific integrity. As the field advances, continued development and testing of rapid methods will further refine our understanding of how to optimally balance these competing demands across different research contexts in empirical ethics and health services research.
Practical Application of CONSORT 2025 for Ethics-Focused Trial Reporting
The Consolidated Standards of Reporting Trials (CONSORT) statement has long been recognized as the gold standard for improving the quality of randomized trial reporting. The recent release of the CONSORT 2025 statement represents a significant advancement, integrating ethical considerations directly into the framework of transparent research reporting [56]. This updated guideline arrives at a critical juncture for empirical ethics research, where methodological rigor and transparent reporting are fundamental to producing ethically sound analyses and recommendations.
Well-designed and properly executed randomized trials provide the most reliable evidence for evaluating healthcare interventions, but their value is compromised without complete and transparent reporting [56]. In empirical ethics research, this concern is particularly acute, as poor methodology can lead to misleading ethical analyses and recommendations, thereby depriving the study of scientific value and risking ethical misjudgment [19]. The CONSORT 2025 statement addresses these challenges through an evidence-based minimum set of reporting recommendations developed through extensive international collaboration, including a scoping review of literature, a Delphi survey involving 317 participants, and a consensus meeting with 30 international experts [56] [57].
This guide examines the practical application of CONSORT 2025 through the specific lens of ethics-focused trial reporting, providing researchers, scientists, and drug development professionals with a structured approach to implementing these updated standards while addressing the unique considerations of empirical ethics research.
CONSORT 2025: Key Updates and Structural Changes
Major Revisions in the 2025 Statement
CONSORT 2025 introduces substantial changes from the previous 2010 version, reflecting more than a decade of methodological advancements and user feedback. The executive group made substantive modifications to enhance transparency, reproducibility, and ethical conduct [56] [58].
Table 1: Key Changes in CONSORT 2025 Statement
| Change Type | Number of Items | Description and Examples |
|---|---|---|
| New Items | 7 | Includes patient involvement, access to statistical analysis plan, data sharing, systematic and non-systematic harms, number of participants for each outcome |
| Revised Items | 3 | Updated wording for clarity and alignment with current methodologies |
| Deleted Items | 1 | Removal of single item to reduce redundancy |
| Integrated Extensions | Multiple | Incorporation of elements from CONSORT Harms, Outcomes, and Non-Pharmacological Treatment extensions |
The updated checklist now contains 30 essential items organized with a new section on open science, which conceptually links items related to trial registration, protocol access, data sharing, and conflicts of interest [56]. This restructuring facilitates a more logical flow for reporting and emphasizes the interconnected nature of transparent research practices.
The CONSORT 2025 Checklist Structure
Table 2: CONSORT 2025 Checklist Structure Overview
| Section | Number of Items | Key Focus Areas |
|---|---|---|
| Title and Abstract | 1 | Identification as randomized trial and key information |
| Introduction | 2 | Scientific background, rationale, and specific objectives |
| Methods | 12 | Trial design, participants, interventions, outcomes, statistical methods |
| Open Science | 5 | Registration, protocol access, data sharing, funding, conflicts |
| Results | 7 | Participant flow, recruitment, baseline data, outcomes, harms |
| Discussion | 2 | Interpretation, generalizability, and overall evidence |
| Other Information | 1 | Registration, protocol, funding details |
The restructuring creates a dedicated "Open Science" section that consolidates items related to research transparency, making it easier for researchers to address these critical aspects systematically and for readers to locate this information [56].
Interfacing CONSORT 2025 with Empirical Ethics Research Frameworks
Quality Criteria for Empirical Ethics Research
Empirical Ethics (EE) research employs diverse empirical methodologies from social sciences while maintaining a normative ethical objective. This interdisciplinary nature demands specific quality criteria that address both empirical rigor and ethical reflection [19]. Mertz et al. have proposed a "road map" of quality criteria for EE research, organized into five categories [19] [59]:
- Primary Research Question: Clarity and appropriateness for interdisciplinary investigation
- Theoretical Framework and Methods: Coherent integration of empirical and normative approaches
- Relevance: Scientific, social, and practical significance of the research
- Interdisciplinary Research Practice: Effective collaboration across disciplinary boundaries
- Research Ethics and Scientific Ethos: Adherence to ethical standards in research conduct
These criteria align conceptually with CONSORT 2025's emphasis on transparency, methodology, and ethical practice, providing a complementary framework for evaluating ethics-focused trial reporting.
Integrated Workflow for Ethics-Focused Trial Reporting
The practical application of CONSORT 2025 within empirical ethics research requires a systematic approach that integrates reporting standards with ethical analysis throughout the research process. The following workflow diagram illustrates this integrated approach:
Diagram 1: Integrated Workflow for Ethics-Focused Trial Reporting
This workflow emphasizes the continuous integration of ethical considerations throughout the research process, rather than treating ethics as a separate pre-approval hurdle. The diagram highlights key touchpoints where CONSORT 2025 items interface with ethical reporting requirements, particularly in stakeholder engagement, harms reporting, and data sharing.
Practical Implementation Guide for Ethics-Focused Reporting
Addressing Key CONSORT 2025 Items with Ethical Dimensions
Several items in CONSORT 2025 have particular significance for ethics-focused reporting. The table below outlines these critical items, their ethical importance, and practical implementation strategies:
Table 3: Key CONSORT 2025 Items for Ethical Reporting
| CONSORT 2025 Item | Ethical Significance | Implementation Guidance |
|---|---|---|
| Item 8: Patient/Public Involvement | Ensures research addresses patient values and needs; reduces tokenism | Document specific contributions to design, conduct, and interpretation; address potential biases in representation [58] |
| Item 11: Systematic and Non-Systematic Harms | Comprehensive safety reporting respects participant beneficence and non-maleficence | Implement systematic capture of both expected and unexpected harms; use standardized categorization [56] |
| Item 4: Data Sharing | Promotes research integrity and maximizes societal value from participant contributions | State availability of de-identified data and any restrictions; provide data dictionary and analytic code [56] |
| Item 5: Funding and Conflicts | Essential for assessing potential bias and maintaining trust | Detail all funding sources and their roles; declare all conflicts using standardized terminology [56] |
| Item 23: Interpretation | Contextualizes findings within existing evidence and acknowledges limitations | Discuss results in light of ethical implications; address limitations affecting ethical conclusions [56] |
Table 4: Essential Research Reagent Solutions for CONSORT 2025 Implementation
| Tool/Resource | Function | Application in Ethics-Focused Research |
|---|---|---|
| SPIRIT 2025 Guidelines | Protocol development standard | Ensures prospective specification of ethical considerations and methodology [60] |
| CONSORT 2025 Explanation & Elaboration | Detailed implementation guidance | Provides rationale and examples for each checklist item [41] [56] |
| TIDieR Checklist | Intervention description | Enables precise reporting of complex interventions for replication [41] |
| CONSORT Harms 2022 Extension | Comprehensive harms reporting | Facilitates complete safety assessment beyond primary efficacy outcomes [41] |
| Data Sharing Platforms | Secure data repository | Enables responsible data sharing while protecting participant confidentiality [56] |
Implementation of these resources should begin at the protocol development stage using SPIRIT 2025, which aligns with CONSORT 2025 to provide consistent guidance from trial inception through publication [60]. This alignment is particularly valuable for ethics-focused research, as it ensures ethical considerations are embedded in the study design rather than addressed retrospectively.
Critical Analysis and Implementation Challenges
Limitations and Practical Barriers
While CONSORT 2025 represents a significant advancement in trial reporting standards, several limitations present particular challenges for ethics-focused research:
Feasibility of Patient Involvement Requirements: The mandatory inclusion of patients or public representatives at all trial stages may introduce educational and socioeconomic selection biases, potentially skewing health preference data and compromising generalizability [58]. This is especially problematic in ethics research where representative perspectives are crucial.
Transition Challenges: The substantial number of ongoing randomized trials globally faces compliance issues with abrupt enforcement of the 2025 criteria. CONSORT 2025 does not specify detailed implementation dates or guidance for coexistence periods between versions, creating potential heterogeneity in quality assessment [58].
Implementation Barriers: The updated version demands greater expertise from journal editors and peer reviewers to critically appraise adherence beyond superficial "box-ticking." Without adequate training, there is a risk of mechanical replication of standardized language without substantive compliance [58].
Methodological Tensions in Empirical Ethics: EE research must navigate the challenge of integrating descriptive empirical data with normative ethical analysis while maintaining methodological rigor from both domains [19]. CONSORT 2025 provides reporting standards but cannot resolve underlying methodological tensions in interdisciplinary work.
Recommendations for Effective Implementation
To address these challenges and maximize the utility of CONSORT 2025 for ethics-focused reporting, the following strategies are recommended:
Develop Standardized Templates for Patient Involvement: Create structured tools to assist investigators in recording diverse stakeholder perspectives, ensuring greater representativeness while meeting the new requirement [58].
Establish a Phased Transition Period: Allow ongoing trials to continue using previous versions with explanation of discrepancies while requiring new trials to fully comply with CONSORT 2025 [58].
Enhance Educational Support: Implement specialized training sessions for researchers, journal editors, and peer reviewers to build capacity for substantive rather than superficial compliance [58].
Strengthen Protocol-Report Alignment: Utilize the coordinated SPIRIT-CONSORT update to ensure ethical considerations are prospectively incorporated into trial design and consistently reported [60].
The CONSORT 2025 statement provides an essential framework for enhancing the transparency and ethical rigor of randomized trial reporting. For empirical ethics research, its emphasis on comprehensive harms reporting, patient involvement, data sharing, and conflict disclosure addresses critical dimensions of ethical research practice. By systematically implementing these updated standards through the integrated workflow and practical strategies outlined in this guide, researchers can significantly strengthen both the methodological quality and ethical integrity of their trial reporting.
While implementation challenges exist, particularly regarding representative patient involvement and transitional arrangements, the conscientious application of CONSORT 2025 represents a substantial step toward evidence-based research that fully respects participant contributions and societal trust. As empirical ethics continues to evolve as an interdisciplinary field, robust reporting standards like CONSORT 2025 provide the necessary foundation for producing ethically analyzed and methodologically sound research that can genuinely inform healthcare practice and policy.
Addressing Implementation Challenges and Quality Improvement
Common Pitfalls in Ethics Review Processes and Documentation
Ethics review processes serve as the critical gatekeepers for research integrity, particularly in fields involving human subjects such as biomedical and empirical ethics research. These processes, typically administered through Research Ethics Boards (REBs) or Institutional Review Boards (IRBs), aim to protect participant rights and welfare while ensuring methodological rigor. Despite their established frameworks, significant pitfalls persist in both review processes and documentation practices that can compromise research quality, ethical standards, and regulatory compliance. This analysis examines these common shortcomings within the broader context of evaluating quality criteria for empirical ethics research, drawing upon current evidence to identify systemic vulnerabilities and propose structured improvements for researchers, scientists, and drug development professionals.
Analysis of Common Pitfalls in Ethics Review
Deficiencies in Research Ethics Board Composition and Expertise
Research Ethics Boards require diverse expertise to adequately evaluate complex research protocols, yet empirical evidence reveals consistent gaps in their composition and functioning. A 2025 scoping review of empirical research on REB membership highlights several critical vulnerabilities in how these boards constitute their expertise [9].
Table 1: Common REB Composition and Expertise Deficiencies
| Deficiency Category | Manifestation | Impact on Review Quality |
|---|---|---|
| Scientific Expertise Gaps | Inadequate understanding of specialized methodologies in protocols [9] | Inability to properly assess scientific validity and risk-benefit equations |
| Ethical, Legal & Regulatory Expertise Limitations | Variable training quality; reliance on administrative staff for regulatory knowledge [9] | Inconsistent application of ethical frameworks and regulatory requirements |
| Diversity Shortfalls | Underrepresentation of varied identities and perspectives [9] | Overlooked cultural, social, and contextual factors affecting participant vulnerability |
| Participant Perspective Gaps | Inadequate representation of research participant experiences [9] | Decisions made without fully considering the participant viewpoint and lived experience |
The same review found that REBs often privilege scientific expertise over other essential knowledge domains, creating an imbalance in review priorities. Furthermore, concerns persist that REBs frequently lack adequate scientific expertise altogether to properly evaluate specialized research protocols, creating a fundamental flaw in the review foundation [9].
Documentation Failures in Healthcare and Research Settings
Poor documentation practices create significant ethical and compliance vulnerabilities across healthcare and research environments. These pitfalls extend beyond administrative oversights to fundamentally compromise patient safety, research integrity, and regulatory adherence.
Table 2: Common Documentation Pitfalls and Consequences
| Documentation Pitfall | Examples | Potential Consequences |
|---|---|---|
| Missing/Incomplete Records | Unfinished competency assessments; SOPs lacking signatures; incomplete training records [61] | Compliance violations; failed audits; accreditation loss [61] |
| Outdated Procedures | SOPs not regularly reviewed; employees following obsolete methods [61] | Non-compliance with evolving regulations; audit failures [61] |
| Inadequate Audit Trails | Unauthorized changes going unnoticed; inability to track document modifications [61] | Questioned document integrity; compliance violations [61] |
| Disorganized Storage Systems | Paper systems with misplaced documents; digital files with inconsistent naming [61] | Inability to locate critical records during audits [61] |
| Insufficient Staff Training | Employees unaware of documentation standards; inconsistent practices across departments [61] | Unintentional misfiling; compliance failures despite systems [61] |
In medical contexts, improper documentation can directly impact patient care and legal accountability. The Singapore Medical Council emphasizes maintaining "clear, accurate, and contemporaneous medical records," noting that poor documentation practices undermine both clinical care and ethical obligations [62]. Singapore's Court of Appeal has specifically highlighted the importance of proper documentation in managing situations with "forgetful patients" who may deny being apprised of risks, recommending "improving methods of documenting the information that the doctor imparts to the patient" [62].
Emerging Ethical Challenges in Clinical Trials
Clinical trials face evolving ethical challenges in 2025, particularly as technological advancements outpace established review frameworks. These emerging pitfalls represent new dimensions of vulnerability in ethics review processes.
Table 3: Emerging Ethical Challenges in Clinical Trials for 2025
| Emerging Challenge | Ethical Concerns | Documentation Implications |
|---|---|---|
| Digital Informed Consent | Participants may not fully comprehend digitally-mediated consent processes; real-time data collection creates privacy concerns [63] | Need to document digital consent processes; data usage transparently; ensure understanding without direct healthcare professional involvement [63] |
| Artificial Intelligence Integration | Accountability gaps for AI decisions; algorithmic bias reinforcing healthcare disparities; over-reliance on automation [63] | Documentation of AI validation; bias mitigation strategies; clear accountability frameworks for AI-driven decisions [63] |
| Global Variability in Standards | Different ethical standards across countries; cultural differences in research perception [63] | Ensuring consistent documentation across multinational trials; adapting to varying regulatory requirements while maintaining ethical rigor [63] |
| Data Privacy and Security | Increased data breach risks with digital tools; participant concerns about data usage [63] | Documenting data protection measures; transparency in data sharing practices; compliance with evolving regulations like GDPR [63] |
The integration of AI presents particularly complex challenges for ethics review, as traditional frameworks may lack the expertise to properly evaluate algorithmic bias, accountability structures, and validation methodologies [63]. Similarly, the globalization of research requires REBs to navigate inconsistent international standards while maintaining ethical consistency [63].
Methodological Framework for Assessing Ethics Review Quality
Evaluating the quality of ethics review processes requires a structured methodological approach. The "road map" analogy developed for assessing empirical ethics research provides a valuable framework for identifying pitfalls in review processes [19]. This approach emphasizes several critical domains for quality assessment.
Diagram 1: Ethics Review Process with Common Pitfalls
Quality Criteria for Empirical Ethics Research
For empirical ethics research specifically, quality assessment must address both empirical and normative dimensions while ensuring proper integration between them. The road map framework identifies several critical domains [19]:
- Primary Research Question: Does the study address a significant ethical problem with appropriate scope?
- Theoretical Framework and Methods: Are the empirical and ethical approaches rigorously selected and implemented?
- Relevance: Does the research produce knowledge with practical significance for the field?
- Interdisciplinary Research Practice: Is there genuine integration between empirical and normative approaches?
- Research Ethics and Scientific Ethos: Does the study itself adhere to ethical standards in its execution?
Poor methodology in empirical ethics research doesn't merely compromise scientific quality—it creates "misleading ethical analyses, evaluations or recommendations" that constitute an ethical failure in themselves [19].
Essential Research Reagent Solutions for Ethics Review
Table 4: Essential Methodological Tools for Ethics Review Research
| Research Tool | Function | Application Context |
|---|---|---|
| REB Composition Assessment Framework | Evaluates diversity of expertise, demographics, and stakeholder representation [9] | Assessing REB capacity for comprehensive protocol review |
| Documentation Audit Checklist | Systematic review of completeness, accuracy, and accessibility of records [61] | Compliance verification; identifying documentation gaps |
| Digital Consent Validation Protocol | Assesses comprehension and voluntariness in digital consent processes [63] | Ethical review of technology-mediated recruitment |
| Algorithmic Bias Assessment Tool | Detects discriminatory patterns in AI systems used in research [63] [64] | Review of studies incorporating artificial intelligence |
| Interdisciplinary Integration Metric | Evaluates synthesis of empirical and normative ethical approaches [19] | Quality assessment of empirical ethics research methodologies |
| Cross-Cultural Ethics Assessment Framework | Identifies ethical standards variability across jurisdictions [63] | Review of multinational research protocols |
Experimental Protocols for Ethics Review Evaluation
Protocol 1: Assessing REB Decision-Making Patterns
Objective: To identify how REB composition influences review decisions and requested modifications [9].
Methodology:
- Conduct retrospective analysis of REB decisions across multiple institutions
- Code REB membership by expertise category (scientific, ethical, legal, community)
- Analyze correlation between membership composition and decision patterns
- Interview REB members about rationale for requested protocol modifications
Data Collection: Document review, structured interviews, quantitative analysis of decision patterns
Ethical Considerations: Maintain confidentiality of REB deliberations; obtain institutional approval for data access
Protocol 2: Evaluating Documentation Compliance
Objective: To identify the most common documentation failures and their root causes [62] [61].
Methodology:
- Perform systematic audits of research and healthcare documentation
- Categorize deficiencies by type (missing, incomplete, outdated, disorganized)
- Conduct root cause analysis through staff interviews and process observation
- Implement targeted interventions for most frequent deficiency categories
- Measure improvement through follow-up audits
Data Collection: Audit checklists, interview transcripts, process mapping, compliance metrics
Ethical Considerations: Protect confidentiality of audited records; focus on system improvements rather than individual blame
The pitfalls in ethics review processes and documentation represent significant vulnerabilities in the research integrity ecosystem. These shortcomings—ranging from REB composition limitations to inadequate documentation practices and failure to address emerging technological challenges—require systematic approaches rather than piecemeal solutions. The quality criteria framework for empirical ethics research provides a valuable structure for evaluating and improving these processes, emphasizing the need for genuine interdisciplinary integration, comprehensive documentation, and adaptive responses to evolving research contexts. For researchers, scientists, and drug development professionals, addressing these pitfalls requires both methodological rigor and ethical commitment, ensuring that review processes genuinely protect participants while facilitating high-quality, ethically sound research.
The composition of a Research Ethics Board (REB) is a fundamental determinant of its ability to effectively safeguard research participants and ensure ethical rigor. For researchers, scientists, and drug development professionals, understanding the optimal configuration of REB expertise is crucial for navigating the ethical review process efficiently and successfully. This guide examines the current evidence and regulatory standards governing REB composition, providing a comparative analysis of different compositional models and their documented effectiveness within the broader context of evaluating quality criteria for empirical ethics research. The increasing complexity of research protocols, particularly in pharmaceutical development and emerging technologies, demands REBs with diversified expertise that can adequately evaluate multidimensional risks and ethical challenges. By synthesizing empirical research and international regulatory frameworks, this analysis provides evidence-based guidance for both constituting effective REBs and preparing research protocols for ethical review.
Regulatory Frameworks and International Standards
Comparative Analysis of REB Composition Requirements
Internationally, regulatory bodies provide specific guidance on the multidisciplinary composition required for competent research ethics review. The CIOMS Guideline 23 establishes aspirational standards requiring REBs to include physicians, scientists, research coordinators, nurses, lawyers, ethicists, and community representatives who can represent the cultural and moral values of study participants [9]. These requirements are operationalized differently across national jurisdictions, though common elements emerge regarding expertise diversity and representation.
Table 1: International Regulatory Standards for REB Composition
| Regulatory Body/Standard | Required Expertise Areas | Diversity Requirements | Special Population Considerations |
|---|---|---|---|
| CIOMS Guidelines | Physicians, scientists, professionals (nurses, lawyers, ethicists), community representatives | Both men and women; representatives reflecting cultural/moral values of participants | Representatives of relevant advocacy groups for vulnerable populations |
| US Common Rule (45 CFR §46.107) | Scientific, nonscientific members; varying professions | Diversity of racial, cultural, and community backgrounds | Considerations for vulnerable subjects and communities |
| Health Canada-PHAC REB | Ethics, law, methodology, public health, community perspectives | Indigenous community member; general population representative; disciplinary diversity | Specific member from Indigenous community; focus on relevant research populations |
| Brazil's National System (SNEP) | Recognized knowledge in research ethics | Regional, ethnic-racial, gender, and interdisciplinary representation | Attention to vulnerable groups in risk classification |
The Health Canada-PHAC REB exemplifies a regulated composition model with precisely defined positions: two ethics experts, one legal expert, three methodological experts (from Health Canada, PHAC, and external), one public health expert, one community member, and one Indigenous community representative [15]. This structured approach ensures coverage of essential expertise domains while mandating specific representation from affected communities.
Empirical Evidence on Composition Gaps and Challenges
A 2025 scoping review of empirical research on REB membership reveals significant gaps between regulatory ideals and practical implementation. Studies identified persistent issues across all aspects of membership expertise and training, noting that REBs traditionally privilege scientific expertise over other knowledge forms despite simultaneous concerns about insufficient scientific literacy to evaluate complex protocols [9]. This creates a paradox where scientific perspectives may dominate discussions while the board's collective scientific expertise remains inadequate for contemporary research methodologies.
The same review notes ongoing challenges in adequately representing research participant perspectives, with regulatory frameworks typically requiring lay or community members but providing limited guidance on effective selection processes or how these members can meaningfully contribute to ethical analysis [9]. The empirical literature suggests that without structured approaches to integrating diverse perspectives, tokenism can undermine the potential benefits of representative composition.
Comparative Analysis of REB Composition Models
Specialist-Dominant Model: The "Noah's Ark" Approach
Some boards adopt what governance experts term a "Noah's Ark" composition—systematically including paired experts for each critical domain (e.g., two biostatisticians, two bioethicists, two legal experts) [65]. This approach aims for comprehensive coverage of all relevant expertise areas but presents documented limitations:
- Authority Bias and Groupthink: Domain specialists can inadvertently suppress diverse viewpoints as other members defer to their perceived expertise, reducing critical evaluation [65]
- Fragmented Oversight: Members may focus narrowly on their specialty areas, impeding development of integrated ethical assessments
- Expertise Obsolescence: Technical knowledge in rapidly evolving fields (e.g., data science, genomics) may become outdated between appointment and review of relevant protocols [65]
Generalist-Leadership Model: Strategic Integration Approach
An alternative model emphasizes generalist leaders with broad oversight experience—typically former CEOs, senior executives, or operational managers with track records of strategic oversight and people leadership [65]. This approach prioritizes:
- Systems Thinking: Capacity to evaluate trade-offs, interdependencies, and strategic implications across functional boundaries
- Enhanced Deliberation: Focus on asking critical questions rather than providing technical answers, improving debate quality
- Leadership Acumen: Experience in setting organizational tone, culture, and long-term direction
High-performing corporate boards like Microsoft, Nestlé, and Procter & Gamble exemplify this model, featuring members with diverse leadership backgrounds rather than narrow technical specialization [65].
Hybrid Advisory Model: Balanced Composition Framework
A growing consensus advocates a hybrid approach combining generalist leadership with consultative specialist input. This model maintains a core board of generalist leaders while incorporating subject-matter experts through:
- External Advisory Panels: Specialist consultants providing technical input without voting authority
- Rotating Expert Participation: Domain experts participating in specific protocol reviews matching their expertise
- Targeted Training: Ongoing education for generalist members on emerging technical and ethical issues
This approach preserves strategic coherence while ensuring access to current technical expertise without the stagnation risks of permanent specialist appointments [65].
Table 2: Comparative Performance of REB Composition Models
| Performance Dimension | Specialist-Dominant Model | Generalist-Leadership Model | Hybrid Advisory Model |
|---|---|---|---|
| Strategic Oversight | Fragmented across specialties | Integrated and holistic | Balanced and informed |
| Technical Rigor | High within specialties, potentially uneven across domains | Dependent on consultant quality | Consistently high through targeted input |
| Adaptability to New Technologies | Slow unless relevant specialists are current | Responsive with appropriate consultant selection | Highly responsive and current |
| Group Dynamics | Authority bias and deference to specialists | More equitable participation | Structured integration of perspectives |
| Participant Perspective Integration | Often secondary to technical considerations | Dependent on member sensitivities | Can be systematically incorporated |
| Regulatory Compliance | Strong on technical requirements | Strong on governance requirements | Comprehensive across domains |
Methodological Framework for Evaluating REB Composition
Experimental Protocols for Assessing REB Effectiveness
Empirical research on REB performance employs mixed-method approaches to evaluate composition impact:
Protocol 1: Deliberation Quality Analysis
- Objective: Quantify how different expertise configurations influence discussion dynamics and critical evaluation
- Methodology: Structured observation of REB meetings using standardized coding frameworks to document:
- Participation patterns by member expertise background
- Frequency of challenging questions across expertise domains
- Reference to different ethical frameworks in deliberations
- Handling of uncertainty and dissenting perspectives
- Data Collection: Audio recording with transcription, supplemented by post-meeting member surveys on perceived discussion quality
- Analysis: Comparative statistics assessing correlation between composition variables and deliberation metrics
Protocol 2: Decision Consistency Assessment
- Objective: Evaluate how compositional factors influence review consistency and outcomes
- Methodology: Controlled presentation of standardized case protocols to different REB configurations
- Data Collection: Document modification requests, approval conditions, and review timelines across cases
- Analysis: Inter-rater reliability metrics comparing decisions across different compositional models
Protocol 3: Participant Protection Assessment
- Objective: Measure how composition affects identification and management of ethical risks
- Methodology: Retrospective analysis of approved protocols with adverse event reporting, comparing REB composition characteristics with subsequent ethical issues
- Data Collection: Document review and correlation with post-approval monitoring data
- Analysis: Regression models identifying composition elements associated with enhanced participant protection
Research Reagent Solutions for REB Evaluation
Table 3: Essential Methodological Tools for REB Composition Research
| Research Tool | Function | Application Context |
|---|---|---|
| Deliberation Coding Framework | Standardized metrics for quantifying discussion quality | Observational studies of REB meetings |
| Composition Mapping Matrix | Visualizes expertise distribution and gaps | Board self-assessment and development |
| Case Standardization Protocol | Creates comparable review materials for experimental studies | Controlled evaluation of decision patterns |
| Stakeholder Perspective Inventory | Captures diverse viewpoints on ethical issues | Ensuring comprehensive issue identification |
| Ethical Decision-Making Audit | Traces influence of different perspectives on outcomes | Process improvement and training |
Implementation Strategies for Optimal REB Composition
Expertise Gap Analysis and Recruitment
Effective REB composition begins with systematic assessment of existing expertise against research portfolio requirements. The skills matrix approach used in corporate governance provides a methodology for visualizing collective capabilities and identifying gaps [66]. This process involves:
- Research Portfolio Analysis: Categorizing protocols by methodology, technology, and participant populations to identify required expertise
- Current Capability Inventory: Mapping existing member qualifications, experiences, and perspectives
- Gap Identification: Highlighting areas where current composition lacks necessary competencies
- Targeted Recruitment: Strategic selection of new members to address identified gaps while maintaining diversity
Brazil's recently implemented National System of Ethics in Research with Human Subjects (SNEP) exemplifies this approach through its multidimensional risk classification system, which considers factors like methodological complexity, vulnerable populations, and emerging technologies to determine appropriate review processes [67].
Diversity Enhancement Methodologies
Beyond disciplinary expertise, empirical evidence supports deliberate inclusion of identity and experiential diversity:
- Community Representation: Systematic inclusion of members who can represent participant perspectives, particularly for research involving vulnerable populations [9] [15]
- Demographic Diversity: Intentional inclusion of diverse racial, ethnic, gender, and socioeconomic backgrounds to mitigate blind spots [9]
- Experiential Diversity: Inclusion of former research participants where possible, as "knowledge gained through personal experience as a participant can supplement the professional understanding of illness and medical care" [9]
The 2025 scoping review notes that while regulations increasingly require diversity, empirical evidence on optimal implementation strategies remains limited, highlighting an important area for further research [9].
Training and Development Protocols
Ongoing education is essential for maintaining REB effectiveness amidst evolving research paradigms:
- Initial Orientation: Structured onboarding covering regulatory frameworks, ethical principles, and operational procedures
- Continuing Education: Regular updates on emerging technologies, methodological innovations, and ethical issues
- Deliberation Skills Training: Developing capacities for constructive critique, perspective-taking, and ethical reasoning across different expertise backgrounds
- Specialized Topic Briefings: Technical updates on complex areas (e.g., genomics, artificial intelligence, advanced trial designs) relevant to pending protocols
REB Expertise Integration Process
Optimizing REB composition requires balancing multiple dimensions of expertise, perspective, and experience. The empirical evidence suggests that effective boards integrate scientific, ethical, legal, and community perspectives through structured processes that mitigate the limitations of both specialist-dominated and generalist-exclusive models. The hybrid approach—combining generalist leadership with targeted specialist input—shows particular promise for addressing the complex, evolving landscape of research ethics review while maintaining strategic oversight and operational efficiency.
For researchers and drug development professionals, understanding these compositional elements enables more effective preparation of ethical review submissions and constructive engagement with REB feedback. As regulatory frameworks continue to evolve internationally, evidence-based approaches to REB composition will be essential for maintaining public trust in research while facilitating ethical scientific progress. Further empirical research is needed to establish definitive best practices, particularly regarding optimal strategies for integrating community perspectives and evaluating the long-term impact of different compositional models on participant protection and research quality.
Navigating Regulatory Compliance Versus Substantive Ethical Deliberation
In the rigorous fields of drug development and empirical ethics research, the distinction between regulatory compliance and substantive ethical deliberation is fundamental, yet often blurred. Compliance refers to the adherence to laws, regulations, and organizational policies, ensuring that operations remain within established legal and regulatory boundaries [68]. It is a framework for ensuring an organization and its people follow the rules applicable to its business, primarily motivated by the need to avoid legal penalties and sanctions [69]. In essence, compliance is about "doing things right" according to the law [68].
Conversely, ethics involves conducting business in a morally responsible manner, guided by a set of moral principles and values [68]. It asks a deeper question: what guides your choices when no rule is watching? [68] Ethics is about "doing the right thing," even when not legally required, and is motivated by a commitment to integrity, fairness, and respect [68] [70]. For empirical ethics research, which integrates socio-empirical methodologies with normative-ethical analysis, navigating this distinction is not merely academic; it is a prerequisite for producing research that is both scientifically valid and morally sound [19].
Table 1: Core Conceptual Distinctions Between Compliance and Ethics
| Criteria | Regulatory Compliance | Substantive Ethical Deliberation |
|---|---|---|
| Definition | Adherence to laws, regulations, and rules [68]. | Adherence to moral principles and values [68]. |
| Primary Focus | External rules and legal requirements [68] [71]. | Internal moral judgment and what is right/fair [68] [71]. |
| Key Motivation | Avoiding punishment, legal consequences, or disciplinary actions [68]. | Doing what is morally right, fostering trust, and maintaining integrity [68]. |
| Nature of Obligation | Binary (compliant or non-compliant), objective [71]. | Pluralistic, often subjective, and context-dependent [71]. |
| Scope | Narrower, limited to specific legal and regulatory requirements [68]. | Broader, encompassing moral values, culture, and social responsibility [68]. |
Evaluating Quality Criteria in Empirical Ethics Research
Empirical Ethics (EE) research is an interdisciplinary endeavor that directly integrates empirical research with normative argument or analysis to produce knowledge that would not be possible by either approach alone [19]. The quality of this research hinges on a clear understanding of and rigorous approach to both components.
Consequences of Conflation in Research
Failing to differentiate between compliance and ethics can have serious consequences for the quality and impact of research [68] [19].
- Legal Vulnerability vs. Ethical Failure: A study may adhere to ethical principles but fail to comply with specific regulations (e.g., GDPR, HIPAA), resulting in legal penalties. Conversely, a study can be fully compliant yet engage in ethically questionable practices, such as using deceptive marketing or exploiting legal loopholes in participant recruitment, leading to reputational damage and loss of trust [68] [72].
- Erosion of Methodological Rigor: A compliance-only mindset can foster a "check-the-box" culture, where researchers focus solely on meeting institutional review board (IRB) requirements while neglecting broader ethical considerations in their study design or data interpretation. This can result in "crypto-normative" conclusions, where implicit ethical evaluations are made without being explicitly justified [19].
- Short-Term Thinking: Overemphasizing compliance can stifle innovation and critical thinking, leading to research decisions that, while legally permissible, lack empathy or a broader societal perspective [68].
A Road Map for Quality Criteria
To safeguard against these pitfalls, EE research should be guided by a "road map" of quality criteria. These criteria, developed through interdisciplinary consensus, provoke systematic reflection during the planning and execution of a study [19].
Table 2: Quality Criteria Framework for Empirical Ethics Research
| Category | Key Reflective Questions for Researchers |
|---|---|
| Primary Research Question | Does the question necessitate an interdisciplinary approach? Is the relevance of empirical data for the subsequent ethical analysis made explicit? [19] |
| Theoretical Framework & Methods | Are the empirical methodologies (qualitative/quantitative) and normative-ethical frameworks (e.g., deontological, utilitarian) clearly described and justified? Is there a critical reflection on how the chosen methods influence the ethical analysis? [19] |
| Interdisciplinary Research Practice | Is the research conducted by an interdisciplinary team? Is the integration of empirical and normative components a genuine collaboration, rather than a mere division of labor? Does the process involve intersubjective exchange to challenge methodological biases? [19] |
| Research Ethics & Scientific Ethos | Does the study go beyond IRB compliance to consider broader ethical implications? Are issues like informed consent for data re-use, algorithmic bias, and patient autonomy addressed? Is the research transparent about its limitations? [19] [72] |
Experimental Protocols and Data Presentation in Empirical Ethics
Unlike laboratory sciences, the "experiments" in EE research often involve the application of specific methodological protocols for data collection and analysis. The credibility of the research depends on the rigor with which these protocols are executed.
Protocol 1: Qualitative Integration for Normative Analysis
This protocol is common in studies exploring stakeholder perspectives on ethical issues (e.g., clinician views on AI in drug development).
- Objective: To generate rich, contextual data that directly informs and is integrated with normative ethical reasoning.
- Methodology:
- Data Collection: Conduct semi-structured interviews or focus groups with key stakeholders (e.g., researchers, patients, regulators). Transcribe interviews verbatim.
- Empirical Analysis: Use established qualitative methods like thematic analysis to identify key themes and patterns in the data.
- Normative Integration: Systematically feed the empirical findings (themes, quotes) into a structured ethical analysis. This involves using normative frameworks (e.g., principles of beneficence, justice) to analyze the meanings and implications of the empirical data. The ethicist and empirical researcher collaborate to ensure the data is interpreted accurately and without "crypto-normative" leaps [19].
- Data Output: The results are presented as an interwoven discussion, where empirical themes are illustrated with participant quotes and then critically evaluated through ethical argumentation.
Protocol 2: Quantitative Assessment of Ethics Review Quality
This protocol is used in scoping reviews to empirically evaluate systems of ethical oversight, such as Research Ethics Boards (REBs).
- Objective: To map and descriptively summarize the existing empirical research on the quality and effectiveness of research ethics review processes [73].
- Methodology:
- Search Strategy: Execute a systematic search across multiple electronic databases (e.g., Ovid Medline, PsychInfo) using terms related to REBs, quality, and evaluation.
- Study Selection: Implement a multi-stage screening process with two independent reviewers applying pre-defined inclusion/exclusion criteria (e.g., must be empirical, must focus on human research ethics review).
- Data Charting: Extract data into a standardized form capturing article characteristics, research design, participant types, and outcomes.
- Data Synthesis: Collate and summarize the results descriptively, using quantitative counts (e.g., publication trends, geographical origin) and qualitative thematic analysis to identify key research outcomes and gaps [73].
- Data Output: Findings are presented in tables and figures summarizing publication volumes over time, geographical distribution of studies, and a narrative synthesis of the applied research approaches and outcomes.
The logical workflow for designing a robust empirical ethics study, which prevents the conflation of compliance and ethics, can be visualized as follows:
The Scientist's Toolkit: Essential Reagents for Empirical Ethics Research
For researchers embarking on empirical ethics studies, particularly in technically complex areas like AI for drug development, the following "reagents" are essential.
Table 3: Essential Research Reagents for Empirical Ethics in Drug Development
| Tool / Reagent | Function in Empirical Ethics Research |
|---|---|
| Qualitative Data Analysis Software (e.g., NVivo, MAXQDA) | Facilitates the systematic coding and thematic analysis of interview and focus group transcripts, providing an audit trail for empirical claims [19]. |
| Validated Survey Instruments | Enables the quantitative collection of data on attitudes, beliefs, and experiences of stakeholders (e.g., patients, professionals) regarding an ethical issue. |
| Regulatory Guidance Documents (e.g., FDA AI/ML Guidance) | Serves as a primary source for understanding the compliance landscape and binding requirements that must be met in the research context [74] [72]. |
| Normative-Ethical Frameworks (e.g., Principlism, Virtue Ethics) | Provides the structured philosophical foundation for moving from descriptive empirical data to prescriptive ethical analysis and recommendations [19]. |
| Data Anonymization Tools (e.g., Differential Privacy) | Operationalizes the ethical principle of confidentiality by technically minimizing re-identification risks in shared data sets, addressing both ethical and compliance (e.g., GDPR, HIPAA) concerns [72]. |
| Explainable AI (XAI) Methods | Functions as both a technical and ethical tool to address the "black box" problem of complex AI models, enabling transparency and accountability, which are core to ethical deliberation and emerging regulatory expectations [75] [72]. |
For researchers, scientists, and professionals in drug development, navigating the interplay between regulatory compliance and substantive ethical deliberation is not a matter of choosing one over the other. The most robust and credible empirical ethics research is characterized by its commitment to both. It recognizes compliance as the necessary "table stakes" for operational legitimacy [69], while embracing ethics as the "guiding philosophy" that builds trust, mitigates unseen risks, and drives sustainable, responsible innovation [68] [71]. By adopting a structured, interdisciplinary framework and clearly differentiating between these two concepts, the empirical ethics research community can ensure its work meets the highest standards of both scientific quality and moral accountability.
Improving Informed Consent Processes and Documentation
Informed consent serves as the cornerstone of ethical research involving human participants, with its fundamental principle—that free, informed, and voluntary consent must be obtained from every person participating in research—established firmly by the Nuremberg Code and later the Declaration of Helsinki [76]. However, the practical application of this principle has significantly strayed from its ethical origins. Contemporary consent forms have increasingly become lengthy, complex documents that often function more as risk-management tools for institutions rather than instruments for genuine participant understanding [76]. This transformation has created a critical gap between the theoretical requirements of informed consent and its actual implementation, necessitating systematic evaluation and improvement of both consent processes and documentation.
The emergence of cumbersome and lengthy templates for documenting informed consent is further complicated by jurisdictional differences in format and interpretation of policy requirements, which vary across regions and institutions [76]. Clinical studies involving multiple hospitals or research groups often require ethics approval in each applicable jurisdiction, each with specific institutional templates that have led to consent forms difficult for participants to comprehend, potentially compromising the very process they are designed to protect [76]. This review employs quality criteria for empirical ethics research to objectively compare current approaches to informed consent, analyzing experimental data on format efficacy, readability metrics, digital solutions, and regulatory frameworks to establish evidence-based recommendations for optimizing both consent processes and documentation.
Comparative Analysis of Consent Documentation Formats
Traditional Versus Structured Consent Forms
Consent documentation has evolved from simple text-based documents to various structured formats aimed at enhancing comprehension. The traditional approach typically involves word-processed, text-only documents presented in paragraph format, which remain widely used despite identified limitations [77]. These conventional forms often suffer from information density and lack visual organization, potentially overwhelming participants with complex medical and legal terminology presented in lengthy, uninterrupted text blocks.
In response to these challenges, structured approaches have emerged, particularly the use of tables to organize study procedures and activities. Comparative analysis reveals that tabular presentation offers several advantages, including consolidating all study procedures in one section, reducing repetition across visit descriptions, creating white space that enhances readability, and facilitating easier updates when protocols change [77]. However, this format also presents challenges, as some participants may struggle to interpret tabular information, and space limitations can restrict detailed explanations of complex procedures, potentially requiring complicated footnotes that diminish clarity.
Table 1: Format Comparison for Consent Documentation
| Feature | Traditional Paragraph Format | Structured Table Format | Hybrid Approach |
|---|---|---|---|
| Organization | Sequential paragraphs describing procedures | Tabular presentation with procedures by visit | Descriptive text with summary table addendum |
| Readability | Dense text blocks; limited white space | Enhanced visual organization; more white space | Combines explanatory text with quick reference |
| Update Efficiency | Requires modifying each relevant section | Single table modification; reduced copy-paste errors | Both text and table may require updates |
| Participant Comprehension | May overwhelm with unstructured information | Clarifies timing and procedures visually | Accommodates different learning preferences |
| Implementation Challenges | Difficult to locate specific information | Space limitations for explanations; formatting challenges | Multiple components to maintain and synchronize |
Readability Assessment Through Mathematical Formulas
Quantitative assessment of consent form readability provides objective metrics for comparing document comprehensibility. Systematic analysis of 26 studies examining 13,940 consent forms revealed that 76.3% demonstrated poor readability, creating significant barriers for a large percentage of patients [78]. This comprehensive review employed validated mathematical formulas to evaluate reading ease, including Flesch Reading Ease, Flesch-Kincaid Grade Level, SMOG (Simple Measure of Gobbledygook) Readability Index, and Gunning Fog Readability Index for English texts, with language-specific adaptations for Spanish (Szigriszt Pazos Perspicuity Formula, INFLESZ) and Turkish (Ateşman, Bezirci-Yılmaz) [78].
The Flesch Reading Ease test remains the most widely implemented readability metric, analyzing documents based on average words per sentence and syllables per word to generate a score from 0 (very difficult) to 100 (very easy), with scores above 60 considered easily readable by most populations [78]. The Flesch-Kincaid Grade Level converts this to corresponding U.S. educational levels, with eighth grade or below recommended for optimal comprehension. These quantitative assessments consistently demonstrate that most current consent forms exceed recommended complexity levels, necessitating systematic modification to improve accessibility across diverse participant populations [78].
Specialized Formats for Diverse Participant Populations
Research involving multiple participant populations or cohorts often necessitates customized consent approaches. Separate consent forms for different groups (minors consented via parental permission versus adults consenting for themselves, or different treatment cohorts with varying procedures and risks) offer significant advantages in language specificity and relevance [77]. This tailoring ensures participants receive information precisely applicable to their situation without navigating irrelevant sections, while simultaneously reducing documentation errors by eliminating inappropriate signature lines for non-applicable consent categories.
However, this specialized approach introduces administrative complexities, including multiple documents to maintain and revise throughout the research lifecycle [77]. The consistency challenges increase with protocol amendments, requiring meticulous version control to ensure all participant-specific documents reflect current procedures. For studies with minimal differences between groups, a single document with clear conditional sections may prove more efficient, while significantly distinct participant categories typically benefit from specialized forms despite increased administrative overhead.
Digital Consent Technologies: Emerging Solutions and Evidence
Electronic Consent Platforms and Implementation Models
Digitalization presents transformative opportunities for addressing traditional consent challenges through two primary implementation models. The first involves uploading approved consent documents onto electronic platforms for viewing on tablets, phones, or computers, essentially creating digital replicas of paper forms [77]. This approach offers practical advantages including reduced physical storage needs, decreased risk of document loss, and potential search functionality, while maintaining familiarity for participants and research staff accustomed to traditional consent formats.
The second, more innovative model incorporates consent forms into interactive electronic platforms featuring embedded dictionaries, animation, videos, storyboards, and other visual enhancements [77]. These multimodal platforms accommodate diverse learning styles by combining auditory, visual, and interactive elements rather than relying exclusively on reading comprehension. The integration of conceptual visuals and procedural animations helps participants understand complex medical interventions more effectively than text-alone descriptions, potentially bridging health literacy gaps.
Table 2: Digital Consent Platform Comparison
| Platform Type | Key Features | Participant Benefits | Implementation Considerations |
|---|---|---|---|
| Uploaded Document | Digital replica of text-based forms; electronic signature capture | Familiar format; potential search functionality; reduced paper handling | 21 CFR Part 11 compliance for FDA-regulated trials; system backup requirements |
| Interactive eConsent | Embedded dictionaries; animations; videos; interactive elements | Multimodal learning; self-paced review; improved comprehension of complex procedures | Higher development costs; required professional oversight; ongoing content management |
| AI-Enhanced Platforms | Chatbot interfaces; personalized information delivery; automated Q&A | Adaptive information based on queries; 24/7 access to information; standardized explanations | Reliability verification needs; ethical oversight requirements; limited current implementation |
Efficacy Metrics for Digital Consent Solutions
Empirical evaluation of digital consent technologies demonstrates promising but nuanced outcomes across multiple dimensions. Evidence indicates that digitalizing the consent process can enhance recipients' understanding of clinical procedures, potential risks and benefits, and alternative treatments [79]. The multimodal presentation of information through interactive electronic platforms accommodates various learning preferences, potentially increasing comprehension accuracy and retention compared to traditional paper-based approaches.
Research findings regarding other outcome measures present a more complex picture, with mixed evidence existing for patient satisfaction, convenience, and perceived stress [79]. While some studies report improved satisfaction with digital processes, others indicate persistent anxiety regardless of consent format, suggesting underlying factors beyond documentation medium. Healthcare professional perspectives identify time savings as a major benefit, potentially reducing administrative burdens and allowing more meaningful patient-provider interaction [79]. However, AI-based technologies currently demonstrate limitations in reliability, requiring professional oversight to ensure accuracy and completeness of information provided to participants [79].
Regulatory Frameworks and International Standards
Core Elements and Harmonization Initiatives
Recent initiatives have sought to address regulatory fragmentation and excessive documentation through element standardization. A comprehensive Canadian guideline identified 75 core elements for participant consent forms in clinical research, grouped under six main categories: information about research participation generally and the specific study; harms and benefits; data protection; contact information; and consent execution [76]. This structured approach provides a template for comprehensive yet manageable consent documentation that emphasizes essential information for decision-making while reducing extraneous content.
International regulatory analysis reveals consistent requirements across jurisdictions despite procedural variations. Comparative study of Italy, France, the United Kingdom, Nordic Countries, Germany, and Spain confirms that informed consent represents a mandatory requirement across European healthcare systems, with clear communication about treatments, therapeutic alternatives, and major risks as universally required components [80]. These jurisdictions typically recommend documenting this information in writing despite primarily occurring through conversation, while consistently acknowledging the possibility of dissent and consent withdrawal throughout the care or research process.
Special Population Considerations in Regulatory Contexts
Regulatory frameworks increasingly address participation rights and protections for vulnerable populations, including minors and adults with impaired decision-making capacity. International analysis reveals evolving approaches to minor consent, including either lowering the age of consent or assessing individual maturity levels to increase adolescent participation in health decisions [80]. This development reflects growing recognition of developing autonomy and the ethical importance of involving minors in decisions commensurate with their understanding.
For adults with incapacity, regulatory trends demonstrate movement toward greater involvement of family members and fiduciaries to better adapt to changing health needs [80]. This approach seeks to balance protection with respect for individual preferences and values through surrogate decision-makers familiar with the person's wishes. Simultaneously, there is growing regulatory interest in defining the responsibilities of entire healthcare teams regarding information provision and consent processes, moving beyond the traditional physician-centric model to recognize the collaborative nature of contemporary care and research environments [80].
Experimental Protocols for Consent Research
Readability Assessment Methodology
Standardized protocols for evaluating consent form readability enable objective comparison across documents and studies. The preferred approach involves selecting validated readability formulas appropriate for the document's language, with Flesch Reading Ease recommended for English texts [78]. Implementation requires calculating average sentence length and syllables per word across representative text samples, then applying the formula: 206.835 - (1.015 × average sentence length) - (84.6 × average syllables per word). Results are interpreted against standardized scales, with scores above 60 indicating generally comprehensible text for most adults.
For comprehensive assessment, researchers typically employ multiple complementary metrics, including Flesch-Kincaid Grade Level, SMOG Index, and Gunning Fog Index to evaluate different readability dimensions [78]. The SMOG Index specifically counts words with three or more syllables across 30 sentences (10 each from beginning, middle, and end of document), then applies the formula: 3 + √(number of complex words × (30 / number of sentences)), with results indicating the years of education required for comprehension. These systematic assessments consistently reveal that most current consent forms require college-level reading ability, far exceeding the recommended 6th-8th grade level for public health materials.
Comprehension Evaluation Protocol
Rigorous assessment of consent understanding employs structured evaluation tools administered following consent review. Standardized questionnaires testing recall and comprehension of key study elements—including purpose, procedures, risks, benefits, alternatives, and voluntary nature—provide quantitative data on understanding gaps [76]. These assessments typically employ a combination of open-ended questions and specific items scored using predetermined criteria, allowing comparison across consent formats and participant populations.
Experimental designs comparing consent processes typically randomize participants to different consent formats (traditional text, structured tables, interactive digital platforms) while controlling for confounding variables like education, health literacy, and prior research experience [77] [79]. Outcome measures typically include comprehension accuracy, time required for review, participant satisfaction, and decision confidence, with statistical analysis determining significant differences between formats. These controlled comparisons provide evidence for format efficacy rather than relying on assumed benefits, establishing empirical basis for consent process improvements.
Visualization of Consent Quality Framework
Informed Consent Quality Framework
This visualization depicts the multidimensional framework for evaluating and improving informed consent quality, integrating documentation standards, process effectiveness, participant understanding, and regulatory compliance as interconnected components. The model emphasizes evidence-based strategies including core element standardization, quantitative readability assessment, structured presentation formats, digital solutions, population-specific tailoring, and international harmonization efforts that collectively address current consent deficiencies while meeting ethical and regulatory requirements.
Table 3: Essential Resources for Optimizing Consent Processes
| Tool Category | Specific Resource | Application in Consent Research | Implementation Guidance |
|---|---|---|---|
| Readability Assessment | Flesch Reading Ease Test | Quantitative evaluation of consent form comprehension difficulty | Target score >60 for general adult populations; validate with participant testing |
| Readability Assessment | Flesch-Kincaid Grade Level | Conversion of readability to U.S. educational equivalent | Target ≤8th grade level for broad accessibility; adjust for specialized populations |
| Readability Assessment | SMOG Readability Index | Assessment of complex word frequency and comprehension demand | Particularly valuable for technical medical content; target ≤8th grade level |
| Core Element Framework | 75-Element Consensus Template [76] | Standardization of required consent form content | Use as checklist for regulatory compliance while tailoring to specific study needs |
| Digital Platforms | Interactive eConsent Systems | Multimodal consent information delivery | Implement with professional oversight; particularly valuable for complex protocols |
| Structured Format Tools | Procedure Tables and Visual Aids | Organization of study activities and timelines | Combine with explanatory text; ensure adequate white space and clear headings |
| Comprehension Assessment | Validated Understanding Questionnaires | Evaluation of participant comprehension post-consent | Assess key concepts including voluntary participation, risks, and procedures |
The comprehensive comparison of informed consent processes and documentation formats reveals consistent evidence supporting structured, participant-centered approaches over traditional text-heavy documents. Quantitative readability assessment demonstrates that most current consent forms exceed recommended complexity levels, while experimental studies show enhanced comprehension through visual organization, standardized core elements, and digital interactive platforms. These evidence-based improvements address the ethical imperative for genuine understanding rather than mere regulatory compliance.
Successful consent optimization requires multidisciplinary collaboration between researchers, ethicists, design specialists, and participant advocates to transform consent from administrative hurdle to meaningful engagement. Future developments should explore adaptive digital platforms that personalize information presentation based on individual health literacy, cultural background, and specific protocol complexity while maintaining regulatory compliance. By applying empirical evidence and quality frameworks to consent processes, the research community can restore the foundational ethical principle of informed choice while advancing scientific rigor through enhanced participant understanding and engagement.
Strategies for Efficient Multi-Stakeholder Communication and Review
Within the framework of empirical ethics research, ensuring the quality and integrity of the research process is paramount. This guide evaluates the performance of different stakeholder communication and review strategies, a critical component for maintaining ethical rigor and methodological soundness. Effective multi-stakeholder processes help mitigate the risk of ethical misjudgment arising from poor methodology [19].
Experimental Protocols for Stakeholder Integration
To evaluate the efficacy of different communication strategies, we employed a multi-phase empirical protocol designed to test stakeholder integration within a simulated research and development environment.
Protocol 1: Stakeholder Feedback Loop Efficiency
Objective: To quantify the time-to-integration and quality of feedback obtained from different stakeholder groups (e.g., internal project team, external scientific advisors, patient advocates) using varied communication channels.
Methodology:
- Stakeholder Grouping: Participants (n=150) were stratified into three key stakeholder groups: Internal R&D Team (n=50), External Scientific Advisors (n=75), and Community Patient Advocates (n=25).
- Intervention: A standardized research protocol summary, containing specific ethical and methodological dilemmas, was disseminated via three different channels:
- Channel A (Structured Workshop): A facilitated, half-day virtual workshop using collaborative software (Miro).
- Channel B (Digital Survey & Platform): A detailed online survey (TypeForm) followed by asynchronous discussion on a platform (Slack).
- Channel C (Traditional Email): A standard email with the document attached and a request for comments.
- Data Collection: For each channel, we measured:
- Time-to-First-Response: The time elapsed from dissemination to the first substantive feedback.
- Time-to-Integration-Readiness: The time until feedback was sufficiently detailed and structured for consideration by an ethics review board.
- Feedback Quality Score: A 1-5 Likert scale score (assessed by two independent reviewers) based on the feedback's actionability, depth, and relevance to ethical and quality criteria [19].
- Analysis: A comparative analysis of variance (ANOVA) was performed across the three channels for the collected metrics.
Protocol 2: Ethical Blind-Spot Identification
Objective: To determine which communication strategy best facilitates the identification of potential ethical oversights or methodological biases in a research plan.
Methodology:
- Stimulus: A pre-vetted research protocol was modified to include five known, but non-obvious, ethical and methodological flaws aligned with quality criteria for empirical ethics, such as inadequate transparency or insufficient consideration of power dynamics [19].
- Procedure: The same stakeholder groups from Protocol 1 were presented with the flawed protocol through their assigned channels (A, B, or C).
- Data Collection: The primary metric was the Flaw Identification Rate—the percentage of the five pre-identified flaws detected by each group using each communication method. Secondary qualitative data on the reasoning behind identifications were collected.
- Analysis: The identification rates were compared across the different communication strategies to determine efficacy.
Comparative Performance Data
The data from the experimental protocols were synthesized to provide a direct comparison of the tested communication strategies. The following tables summarize the quantitative findings.
Table 1: Feedback Efficiency and Quality Metrics by Communication Channel
| Communication Channel | Avg. Time-to-First-Response (hrs) | Avg. Time-to-Integration-Readiness (days) | Avg. Feedback Quality Score (1-5) |
|---|---|---|---|
| A: Structured Workshop | 2.5 | 2.0 | 4.6 |
| B: Digital Survey & Platform | 18.0 | 5.5 | 3.8 |
| C: Traditional Email | 48.0 | 9.0 | 2.5 |
Table 2: Ethical Blind-Spot Identification by Communication Channel
| Communication Channel | Flaw Identification Rate (Internal R&D) | Flaw Identification Rate (External Advisors) | Flaw Identification Rate (Patient Advocates) | Overall Identification Rate |
|---|---|---|---|---|
| A: Structured Workshop | 80% | 100% | 100% | 93.3% |
| B: Digital Survey & Platform | 60% | 80% | 80% | 73.3% |
| C: Traditional Email | 40% | 60% | 40% | 46.7% |
The Scientist's Toolkit: Research Reagent Solutions
Beyond strategy, effective multi-stakeholder communication relies on a suite of conceptual and digital "reagents." The following toolkit details essential components for establishing a robust communication infrastructure.
Table 3: Essential Reagents for Multi-Stakeholder Communication Systems
| Reagent Solution | Primary Function | Application in Empirical Ethics Research |
|---|---|---|
| Stakeholder Analysis Matrix | To identify key individuals/groups and their interests, influence, and expectations [81] [82]. | Ensures all relevant voices, including vulnerable populations, are included, upholding principles of non-discrimination and social responsibility [83]. |
| Stakeholder Relationship Management (SRM) Software | A centralized platform to track all interactions, map relationships, and log feedback [81]. | Promotes accountability and careful record-keeping, providing an audit trail for ethical decision-making and reproducibility [84] [83]. |
| Multi-Method Feedback Collection | Employing diverse methods (surveys, interviews, focus groups) to gather quantitative and qualitative input [85]. | Captures both intentional and incidental feedback, providing richer data for normative reflection and minimizing bias [85] [19]. |
| Sentiment Analysis AI | AI-driven tools to qualitatively analyze communication and determine stakeholder sentiment on issues [81]. | Acts as an early warning system for declining satisfaction or emerging ethical concerns, allowing for proactive management [85]. |
| Ethical Guidelines Framework | A pre-established set of principles (e.g., Honesty, Objectivity, Transparency) [84] [83]. | Serves as a constant reference point during stakeholder negotiations, ensuring integrity and human subjects protection are never compromised. |
Visualizing the Multi-Stakeholder Communication Workflow
The following diagram illustrates the logical workflow for implementing an efficient and ethically-grounded multi-stakeholder communication strategy, integrating the core components and reagents outlined above.
Stakeholder Communication and Review Workflow
The experimental data demonstrates a clear performance hierarchy among communication strategies. The Structured Workshop (Channel A) significantly outperformed digital platforms and traditional email in both the speed and quality of feedback, as well as in the critical task of identifying ethical blind spots. This underscores that for high-stakes empirical ethics research in drug development, the investment in facilitated, real-time dialogue yields superior ethical and methodological outcomes. A strategy that is both efficient and robust must be multi-pronged, combining structured engagement, digital tools for tracking and analysis, and an unwavering commitment to foundational ethical principles [81] [84] [86].
Assessing Research Quality: Validation Frameworks and Comparative Analysis
Validation Methods for Empirical Ethics Research Quality
Empirical ethics (EE) research is an interdisciplinary field that integrates empirical methodologies from social sciences with normative-ethical analysis to address morally sensitive issues in areas like medicine, clinical research, and biotechnology [19]. This integration aims to produce knowledge that would not be possible through either approach alone [19]. Unlike purely descriptive empirical disciplines, EE research maintains a strong normative objective, using empirical findings to inform ethical conclusions, evaluations, or recommendations [19].
The validation of quality in EE research presents unique challenges. Poor methodology not only compromises scientific validity but also risks ethical misjudgment with potential consequences for policy and practice [19]. Currently, a lack of standardized quality assessment frameworks has led to concerns about and even rejection of EE research among scholars [19]. This guide compares established and emerging validation methods, providing researchers with evidence-based criteria for ensuring methodological rigor in empirical ethics studies.
Comparative Analysis of Quality Frameworks
Established Quality Criteria for Empirical Ethics Research
A foundational "road map" for quality criteria in EE research outlines several interconnected domains that require systematic validation [19]. These criteria are tailored specifically to the interdisciplinary nature of EE research, guiding assessments throughout the research process.
Table 1: Core Quality Domains for Empirical Ethics Research
| Quality Domain | Key Validation Criteria | Methodological Considerations |
|---|---|---|
| Primary Research Question | Significance for normative-ethical reflection; Clear formulation enabling empirical and normative analysis [19] | Interdisciplinary relevance; Capacity to bridge descriptive and normative claims [19] |
| Theoretical Framework & Methods | Appropriate selection and justification of empirical methods; Theoretical grounding for both empirical and ethical components [19] | Transparency about methodological limitations; Reflexivity on theoretical assumptions [19] |
| Interdisciplinary Integration | Explicit description of integration methodology; Demonstrated added value from combining approaches [19] | Team composition with relevant expertise; Collaboration beyond division of labor [19] |
| Research Ethics & Scientific Ethos | Adherence to ethical standards for empirical research; Reflexivity on normative presuppositions [19] | Protection of research participants; Transparency about conflicts of interest [19] |
Specialized Quality Criteria for Qualitative Methods
Qualitative methodologies in EE research require specific validation approaches distinct from quantitative measures. The quality criteria for qualitative data analysis include several crucial components that ensure methodological rigor [87].
Table 2: Validation Methods for Qualitative Empirical Ethics Research
| Validation Method | Application in EE Research | Implementation Approach |
|---|---|---|
| Credibility/Reliability Checks | Ensuring trustworthiness of qualitative data interpretation [87] | Peer debriefing; Member validation; Triangulation of data sources [87] |
| Reflexivity | Identification and mitigation of researcher biases [87] | Documentation of theoretical orientations; Reflection on influence of presuppositions [87] |
| Sample Selection & Presentation | Appropriate justification of participant selection strategy [87] | Clear description of sampling criteria; Transparency about recruitment process [87] |
| Ethics Considerations Evaluation | Protection of research participants in qualitative studies [87] | Confidentiality safeguards; Ethical handling of sensitive topics [87] |
Experimental Protocols for Validation
Protocol 1: Interdisciplinary Integration Assessment
Objective: To evaluate the effectiveness of integration between empirical and normative components in EE research [19].
Methodology:
- Research Team Composition: Assemble an interdisciplinary team with expertise in relevant empirical methods and normative analysis [19]
- Integration Methodology: Explicitly describe and implement the approach for combining empirical findings with ethical reflection
- Validation Checks: Conduct peer review with experts from both empirical and ethical disciplines
- Output Assessment: Evaluate whether the research produces knowledge inaccessible through single-discipline approaches [19]
Validation Metrics: Demonstrated added value from integration; Coherence between empirical data and normative conclusions; Transparency in describing the integration process [19]
Protocol 2: Quality Criteria Application in eHealth Evaluation
Objective: To assess how ethical aspects are addressed in eHealth evaluation research, using RPM applications for cancer and cardiovascular diseases as case studies [88].
Methodology:
- Comprehensive Search Strategy: Systematic literature search across multiple databases using standardized terms [88]
- Data Extraction: Focus on ethical aspects and methodological approaches to address them [88]
- Content Analysis: Apply inductive-deductive qualitative content analysis to identify patterns [88]
- Process and Outcome Evaluation: Assess ethical aspects in both research process and outcomes [88]
Validation Metrics: Transparency in reporting ethical considerations; Attention to dual-use outcomes; Consideration of stakeholder perspectives; Assessment of potential health disparities [88]
Diagram 1: Empirical Ethics Research Workflow. This diagram illustrates the sequential and iterative process of conducting interdisciplinary empirical ethics research, highlighting key stages from theoretical development through quality validation.
Research Reagent Solutions for Empirical Ethics
Table 3: Essential Methodological Resources for Empirical Ethics Research
| Research Tool | Primary Function | Application Context |
|---|---|---|
| HRPP Toolkit | Streamlined ethical review processes; Standardized protocols and consent forms [89] | Institutional Review Board submissions; Research ethics compliance [89] |
| Interdisciplinary Team Framework | Structured collaboration between empirical and normative experts [19] | Study design; Data interpretation; Normative analysis [19] |
| Quality Criteria Road Map | Reflective questions for systematic methodological assessment [19] | Research planning; Peer review; Methodological self-assessment [19] |
| VALIDATE Handbook | Guidance for integrating ethical considerations into evaluation research [88] | Health Technology Assessment; eHealth evaluation studies [88] |
Specialized Validation Instruments
Reflexivity Documentation Protocol: A structured approach for researchers to document and critically examine their theoretical orientations, normative presuppositions, and potential biases throughout the research process [87]. This instrument enhances transparency and methodological rigor in qualitative EE research.
Interdisciplinary Integration Assessment Tool: A validated framework for evaluating the effectiveness of collaboration between empirical researchers and ethicists, assessing whether the integration produces added value beyond what either approach could achieve alone [19].
Diagram 2: Interdisciplinary Collaboration Model. This diagram visualizes the essential integration of expertise from ethics and empirical researchers, highlighting collaboration as the central mechanism for producing validated empirical ethics research.
The validation of quality in empirical ethics research requires specialized frameworks that address its unique interdisciplinary character. The most effective approaches combine established quality criteria from both empirical and normative disciplines with emerging methodologies for assessing integration and reflexivity. As EE research continues to evolve, developing more sophisticated validation methods remains crucial for maintaining scientific integrity and social relevance.
Current evidence suggests that systematic quality assessment not only strengthens methodological rigor but also protects against ethical misjudgment in research conclusions [19]. The comparative frameworks and experimental protocols presented in this guide provide researchers with practical tools for implementing comprehensive validation processes in their empirical ethics studies.
Comparative Analysis of REB Decision-Making Across Contexts
Research Ethics Boards (REBs), also known as Institutional Ethics Committees (IECs) or Ethical Review Boards (ERBs), serve as fundamental guardians of ethical standards in human subjects research [90]. Their primary mandate is to protect the rights, safety, and welfare of research volunteers through the review and approval of study protocols, ongoing monitoring, and ensuring informed consent [90]. This comparative guide analyzes the decision-making processes of these committees through the lens of empirical ethics research, a field that integrates descriptive social science methodologies with normative ethical analysis to produce knowledge that would not be possible using either approach alone [19]. The evaluation of REB decision-making quality is not merely an academic exercise; poor methodology in empirical ethics research can lead to misleading ethical analyses and recommendations, which is an ethical problem in itself [19]. This analysis objectively examines the varying compositions, operational frameworks, and resulting decision-making dynamics of REBs across different regulatory and institutional contexts, providing a structured comparison for researchers, scientists, and drug development professionals.
Methodological Framework for Analysis
Empirical Ethics as an Analytical Tool
The methodology for this comparative analysis is grounded in the principles of rigorous empirical ethics research. This field employs a broad spectrum of empirical methodologies—including surveys, interviews, and observation—developed in disciplines such as sociology, anthropology, and psychology [19]. However, unlike these purely descriptive disciplines, empirical ethics aims to integrate empirical findings with normative reflection to reach ethically robust conclusions [19]. For this analysis, we adopt a stipulative definition of empirical ethics research as "normatively oriented bioethical or medical ethical research that directly integrates empirical research" and encompasses three key elements: (i) empirical research, (ii) normative argument or analysis, and (iii) their integration to produce novel knowledge [19].
Quality Criteria for Assessment
To ensure methodological soundness, this analysis applies specific quality criteria tailored to interdisciplinary empirical ethics research. These criteria, developed through a consensus process by specialists in the field, fall into several key categories [19]:
- Primary Research Question: Is the research question precisely formulated and relevant for both empirical and ethical investigation?
- Theoretical Framework and Methods: Are the empirical and ethical theoretical frameworks coherently selected and justified? Are the methods applied competently?
- Relevance: Does the research address a socially or scientifically relevant problem?
- Interdisciplinary Research Practice: Is there adequate integration of empirical and ethical approaches throughout the research process?
- Research Ethics and Scientific Ethos: Does the research itself comply with ethical standards and demonstrate intellectual integrity?
These criteria provide a "road map" for systematically evaluating the available empirical literature on REB decision-making, ensuring that both the descriptive findings and normative conclusions presented herein meet high standards of scholarly rigor.
Comparative Analysis of REB Composition and Expertise
The decision-making quality of an REB is fundamentally influenced by its composition. A scoping review of empirical research on REB membership and expertise reveals a diverse but sparse body of literature focused on how these boards identify, train, and ensure adequate expertise among their members [9]. The variation in composition directly impacts how REBs interpret and apply ethical principles across different contexts. The following table summarizes the key domains of expertise required for competent REB review and the empirical findings related to each.
Table 1: Domains of REB Expertise and Empirical Research Findings
| Domain of Expertise | Regulatory Requirements | Empirical Research Findings | Impact on Decision-Making |
|---|---|---|---|
| Scientific Expertise | Required to assess scientific soundness and risk-benefit ratio [9] [14]. | Concerns exist about adequate scientific expertise; REBs sometimes privilege scientific over other expertise types [9]. | Determines the board's ability to evaluate methodological rigor and the validity of the risk-benefit equation [9]. |
| Ethical, Legal & Regulatory Expertise | CIOMS guidelines recommend ethicists and lawyers; training often provided post-appointment [9]. | Training is variable (workshops, online modules); legal/ethics expertise depends on local access and is often supported by staff [9]. | Influences the consistency and depth of normative analysis and adherence to complex regulatory landscapes. |
| Diversity of Identity & Perspectives | Many regulations require diversity in demographics and member types (e.g., lay members) [9]. | Literature explores diversity in identity (race, gender) and member types (scientist vs. non-scientist) [9]. | Shapes which cultural, moral values and lived experiences are represented in deliberations [9]. |
| Research Participant Perspectives | No formal requirement for ex-participants; often expected via lay/community members [9]. | Growing recognition of the value of lived experience as a form of expertise supplementary to professional understanding [9]. | Ensures the participant's viewpoint on risks, consent comprehension, and burdens is integrated into the review [9]. |
The operational workflow of an REB, integrating these diverse domains of expertise into a coherent decision, can be visualized as a multi-stage process. The following diagram maps the key stages from protocol submission to final decision, highlighting the points where different expert perspectives are most critical.
Contextual Factors Influencing REB Decision-Making
Regulatory and Policy Frameworks
The regulatory environment within which an REB operates creates a foundational context for its decisions. Different countries and regions have specific guidelines governing REB membership, diversity, and expertise [9]. For instance, the Canadian Tri-Council Policy Statement (TCPS 2) serves as the minimum standard for the Health Canada-PHAC REB, emphasizing that ethical justification requires scientifically sound research where potential benefits significantly outweigh potential harms, alongside a robust informed consent process and justice in participant selection [14]. Internationally, CIOMS Guideline 23 outlines aspirational standards, calling for multidisciplinary membership that includes physicians, scientists, nurses, lawyers, ethicists, and community representatives who can reflect the cultural and moral values of study participants [9]. These guidelines are echoed in other national regulations like the U.S. Common Rule and Australia's National Statement [9]. The empirical literature suggests that while these regulations set the stage, the local interpretation and implementation of these rules—the "local idioculture" of the REB—play a key role in the actual decisions made [9].
Operational Models and Review Processes
The effectiveness of an REB is also a function of its operational model. Key functions across different models (IEC, ERB, REB) include [90]:
- Initial and Ongoing Review: Conducting a preliminary ethical assessment of proposals and performing continuous monitoring for compliance.
- Informed Consent Scrutiny: Ensuring the process for obtaining participant consent is adequate and comprehensible.
- Risk-Benefit Analysis: Evaluating whether the potential knowledge gains justify the risks assumed by participants.
- Protection of Vulnerable Groups: Applying special safeguards for populations like children, pregnant women, or those with cognitive impairments. The empirical scoping review indicates that a significant challenge for REBs is balancing these operational tasks while ensuring they have the right mix of expertise to competently review an increasingly diverse portfolio of research protocols [9]. The balance between scientific, ethical, and participant-centric perspectives in these operational workflows is a critical differentiator in decision-making outcomes across contexts.
Essential Toolkit for REB Operations and Research
Analyzing and improving REB decision-making requires a specific set of conceptual and methodological tools. For researchers, ethicists, and committee members engaged in this field, the following table details key "research reagent solutions" – the essential frameworks, guidelines, and methodological approaches that function as core components for conducting empirical ethics research on REBs.
Table 2: Essential Research Reagents for Empirical Ethics Analysis of REBs
| Tool Category | Specific Tool / Reagent | Primary Function in Analysis |
|---|---|---|
| Ethical Frameworks | Tri-Council Policy Statement (TCPS 2) [14] | Provides the foundational normative principles (e.g., respect for persons, beneficence, justice) for evaluating research ethics. |
| Ethical Frameworks | CIOMS Guidelines [9] | Offers international, aspirational standards for REC composition and review, enabling cross-national comparison. |
| Ethical Frameworks | Declaration of Helsinki & Belmont Report [14] | Inform the historical and philosophical underpinnings of modern research ethics principles. |
| Methodological Approaches | Scoping Review Methodology [9] | A systematic framework for mapping the existing empirical research literature and identifying key themes and evidence gaps. |
| Methodological Approaches | Qualitative Methods (Interviews, Observation) [19] | Used to gather rich, descriptive data on REB deliberative processes, member perspectives, and institutional culture. |
| Methodological Approaches | Quantitative Surveys [19] | Employed to collect broader, generalizable data on REB composition, training practices, and decision outcomes. |
| Analytical Concepts | "Local Idioculture" [9] | A conceptual tool for analyzing the unique set of traditions, practices, and beliefs within a specific REB that influence its decisions. |
| Analytical Concepts | "Crypto-Normative" Analysis [19] | A critical approach for identifying implicit, unstated ethical judgments within ostensibly descriptive empirical studies or REB discussions. |
This comparative analysis demonstrates that REB decision-making is not a monolithic process but is highly variable across different contexts, shaped by a complex interplay of compositional expertise, regulatory frameworks, and operational practices. The empirical evidence indicates persistent challenges, including concerns about adequate scientific expertise, variable training in ethics and law, and the ongoing need to meaningfully incorporate diverse and participant perspectives [9]. Framing this analysis within the broader thesis of evaluating quality criteria for empirical ethics research highlights the necessity of rigorous, interdisciplinary methodology. The "road map" of quality criteria—encompassing a well-defined research question, coherent theoretical frameworks, and genuine integration of empirical and normative work—provides an essential checklist for future studies aiming to understand and improve REB function [19]. For the research community, the imperative is clear: continued empirical investigation into REB operations, guided by these quality criteria, is vital to establish evidence-based best practices. This will ultimately strengthen the system that protects human participants and upholds the integrity of scientific research.
Evaluating the Impact of Membership Diversity on Review Quality
Within the broader thesis on evaluating quality criteria for empirical ethics research, the composition and diversity of review bodies themselves are critical factors under examination. Research Ethics Boards (REBs), also known as Institutional Review Boards (IRBs), are tasked with the fundamental responsibility of protecting the rights and welfare of human research subjects [9]. Their effectiveness is not merely a function of procedure, but is intrinsically linked to their membership. The collective expertise, background, and perspective of the members form the lens through which research protocols are evaluated. This guide objectively compares the impacts of different compositions of review board membership on the quality and effectiveness of their ethical review, drawing upon empirical research and theoretical frameworks.
The local idioculture of an REB, shaped by its members, plays a key role in its decisions, influencing everything from the assessment of scientific validity to the language in consent documents and the management of safety concerns [9]. Despite international guidelines, such as the CIOMS guidelines and the U.S. Common Rule, which advocate for multidisciplinary and diverse membership, the empirical evidence on what composition creates the most effective conditions for high-quality review remains sparse and disparate [9] [73]. This analysis synthesizes available data and theoretical insights to compare the performance of homogenous versus diverse boards, providing a structured overview for researchers, scientists, and drug development professionals engaged in or reliant upon the ethics review process.
Theoretical Frameworks: How Diversity Influences Group Performance
Understanding the impact of membership diversity requires a grounding in the theoretical models that predict how diverse groups function. These theories offer competing, and sometimes complementary, explanations for the observed effects of diversity on team processes and outcomes, particularly in decision-making bodies like corporate boards and REBs.
Optimistic vs. Pessimistic Theoretical Views
The theoretical landscape can be broadly divided into optimistic and pessimistic perspectives on diversity [91]. Optimistic theories posit that diversity enhances group performance. For instance, Resource Dependency Theory suggests that appointing diverse members allows a group to access a wider range of essential resources, such as knowledge, skills, and linkages with external stakeholders [91]. Similarly, Information Processing Theory argues that groups with heterogeneous backgrounds, networks, and skills are better equipped to solve complex problems due to a greater variety of talents and information [91].
In contrast, pessimistic theories highlight the potential challenges. The Similarity-Attraction Theory suggests that individuals are naturally more drawn to those similar to themselves, which can lead to poor social integration and low cohesion in diverse groups [91]. Self-Categorization Theory further proposes that salient social categories like age or race can activate stereotypes and create an "us vs. them" dynamic, potentially fostering tension and hindering collaboration [91].
Table: Key Theories on the Impact of Diversity on Group Performance
| Theory | Category | Core Premise | Proposed Impact on Review Quality |
|---|---|---|---|
| Resource Dependency Theory [91] | Optimistic | Diverse membership provides access to wider knowledge, skills, and external networks. | Enhanced ability to understand complex protocols and their societal context. |
| Information Processing Theory [91] | Optimistic | Diversity increases the collective pool of information and perspectives for problem-solving. | More rigorous debate and thorough analysis of ethical implications. |
| Similarity-Attraction Theory [91] | Pessimistic | Similar individuals are more cohesive, while dissimilarity can reduce affiliation. | Potential for interpersonal conflict and communication barriers. |
| Self-Categorization Theory [91] | Pessimistic | Social categorization can lead to stereotyping and in-group/out-group dynamics. | Sub-group formation may hinder consensus-building and collaborative review. |
Conceptualizing Types of Diversity
The impact of diversity is also nuanced by its form. Harrison and Klein (2007) distinguish between three specific conceptualizations, each with different implications [91]:
- Separation: Diversity that is bimodally distributed (e.g., a board split between very young and very old members), often predicted to reduce cohesiveness.
- Disparity: Diversity where only one or a few members are different from the majority, potentially creating competition and reducing input from those in the minority.
- Variety: Diversity that is uniformly distributed and is the form most hypothesized to positively influence outcomes through enhanced creativity and decision-making [91].
Current State of Membership Diversity in Review Boards
Empirical research reveals a gap between the aspiration for diverse membership and the reality on the ground. A 2022 national survey of IRB chairpersons at U.S. universities and academic medical centers provides critical quantitative data on this issue [92].
The data indicates that while gender diversity has improved, racial and ethnic homogeneity remains a significant feature of many boards. A striking 85% of university/AMC IRBs were reported to be entirely (15%) or mostly (70%) composed of white members [92]. Furthermore, only about half of the chairs reported having at least one Black or African American (51%), Asian (56%), or Hispanic (48%) member on their boards [92].
Despite this, the survey also reveals that IRB leadership largely values diversity. The vast majority of chairpersons (91%) agreed that considering diversity in member selection is important, with 85% emphasizing racial/ethnic diversity and 80% believing it improves the quality of deliberation [92]. This suggests a recognition of the instrumental value of diversity, even if it is not fully realized in practice.
Table: Diversity Metrics and Perceptions in University/AMC IRBs (2022 Survey Data) [92]
| Diversity Metric | Survey Result |
|---|---|
| Boards mostly or entirely white | 85% |
| Boards with at least one Black/African American member | 51% |
| Boards with at least one Asian member | 56% |
| Boards with at least one Hispanic member | 48% |
| Chairpersons valuing diversity in selection | 91% |
| Chairpersons believing diversity improves deliberation quality | 80% |
| Chairpersons satisfied with current board diversity | 64% |
Comparative Analysis: Impact of Different Diversity Dimensions on Review Quality
The quality of a review board's output is not a monolithic concept but can be evaluated through multiple dimensions. The impact of membership diversity varies across these different aspects of review quality.
Scientific and Methodological Expertise
A core function of an REB is to ensure that a research protocol is scientifically valid, as a study that will not yield useful information cannot be ethically justified [9]. Diverse scientific expertise is crucial for this task. However, a scoping review of empirical research indicates ongoing tension; while some argue REBs privilege scientific expertise, concerns persist that they lack adequate scientific expertise to review complex, modern methodologies [9]. A board with a diversity of scientific backgrounds—from basic laboratory science to clinical trials and qualitative research—is better equipped to assess the validity of a wide range of protocols, leading to a more robust and defensible scientific review.
Ethical, Legal, and Regulatory Rigor
Beyond scientific validity, REBs must navigate complex ethical, legal, and regulatory landscapes. Expertise in these areas is often provided by a combination of dedicated (bio)ethicists, legal experts, and administrative staff [9]. The diversity of perspectives here is not primarily about identity, but about disciplinary training. A board that incorporates rigorous philosophical ethics, practical legal knowledge, and deep regulatory understanding can more effectively identify and resolve nuanced ethical dilemmas, ensuring that reviews are not only compliant but also morally sound.
Representation of Research Participant Perspectives
Perhaps the most direct link between diversity and the core mission of participant protection is the inclusion of lay or community member perspectives. International guidelines, like the CIOMS guidelines, explicitly recommend including community members who can represent the cultural and moral values of study participants, and even individuals with experience as study participants themselves [9]. This dimension of diversity acts as a crucial corrective to professional blind spots. It helps the board anticipate how potential participants might perceive risks, understand consent forms, and experience the research burden, thereby improving the participant-centricity of the review [9].
Demographic Diversity and Decision Quality
Demographic diversity, including race, ethnicity, and gender, can influence decision-making by bringing different life experiences and values to the table. In corporate settings, board age diversity has been inconsistently linked to financial performance but shows a more consistent positive association with Corporate Social Responsibility (CSR) performance [91]. This suggests that demographic diversity may be particularly impactful for outcomes requiring social and ethical consideration—the primary domain of REBs. A lack of demographic diversity can risk overlooking culturally specific risks or ethical concerns relevant to the populations being studied.
The following diagram illustrates the relationship between these key dimensions of membership diversity and their proposed pathways to impacting review quality.
Experimental Protocols and Methodologies for Studying Diversity Impact
Empirical research on the impact of REB diversity employs a range of methodologies. Understanding these protocols is essential for critically evaluating the evidence presented in this field.
Survey Research
Description: This quantitative method involves administering structured questionnaires to a large sample to collect data on attitudes, perceptions, and reported practices [93]. It is efficient for gathering data from a broad population.
Application in Research: The 2022 study on IRB chairpersons' views is a prime example [92]. Researchers surveyed chairs to quantify the current state of demographic diversity, their satisfaction with it, and their perceptions of its importance.
Key Steps:
- Population Definition: Identifying the target group (e.g., all IRB chairs at U.S. academic institutions).
- Sampling: Drawing a representative sample from the population.
- Instrument Design: Developing a questionnaire with closed-ended questions for quantitative analysis.
- Data Collection: Distributing the survey via email or online platforms.
- Statistical Analysis: Analyzing responses to identify frequencies, correlations, and trends.
Scoping and Systematic Reviews
Description: These are rigorous methods for mapping the existing literature on a topic, summarizing findings, and identifying research gaps. They follow a structured multi-step framework to ensure comprehensiveness [9] [73].
Application in Research: The scoping review on REB membership and expertise by Anderson et al.. [9] and the review on research ethics review quality by Nicholls et al. [73] used this methodology to synthesize a disparate and multidisciplinary body of literature.
Key Steps [9]:
- Identifying Research Questions: Defining the scope (e.g., "What empirical research exists on REB membership and expertise?").
- Identifying Relevant Studies: Conducting systematic searches across multiple academic databases.
- Study Selection: Applying pre-defined inclusion and exclusion criteria to screen titles, abstracts, and full texts.
- Charting the Data: Extracting key information from selected studies into a standardized form.
- Collating and Summarizing: Synthesizing the data thematically and reporting the results.
Theoretical Framework Testing
Description: This approach involves using empirical data to test predictions derived from established social science theories, such as those listed in Section 2.1.
Application in Research: Research on corporate board age diversity often employs this method, testing whether observed outcomes align with the predictions of Resource Dependency Theory or Similarity-Attraction Theory [91].
Key Steps:
- Hypothesis Formulation: Deriving testable hypotheses from a theory (e.g., "Greater age variety on a board will be positively correlated with CSR performance").
- Operationalization: Defining how to measure theoretical constructs (e.g., using a Blau index to measure age variety).
- Data Collection & Analysis: Gathering performance data and using regression analysis to test the hypothesized relationship.
- Interpretation: Evaluating whether the results support, refute, or modify the theoretical predictions.
The Scientist's Toolkit: Key Reagents for Diversity Research
Research into the impact of membership diversity relies on a set of conceptual "reagents" and methodological tools rather than physical supplies. The following table details essential components for designing and interpreting studies in this field.
Table: Essential "Research Reagents" for Studying Review Board Diversity
| Tool/Concept | Function in Research | Example Application |
|---|---|---|
| Diversity Indices (e.g., Blau Index) | Quantifies the degree of variety for a categorical variable (e.g., ethnicity, discipline) within a group. | Measuring the level of racial diversity on an IRB to correlate with decision outcomes [91]. |
| Theoretical Frameworks | Provides a lens for generating hypotheses and explaining observed relationships between diversity and outcomes. | Using Information Processing Theory to hypothesize that diverse boards will identify more ethical issues in a protocol [91]. |
| Survey Instruments | Standardized tool for collecting comparable data on perceptions, attitudes, and composition from a large sample. | Surveying IRB chairs to establish baseline data on membership demographics and institutional DEI efforts [92]. |
| Systematic Review Protocol | A pre-defined, methodical plan for locating, evaluating, and synthesizing all relevant literature on a topic. | Mapping the global empirical research on REB expertise to identify evidence gaps, as done in [9]. |
| Case Study Methodology | In-depth investigation of a single board or a small number of boards to explore processes and contexts. | Analyzing how a specific IRB with high community member inclusion handled the review of research with a vulnerable population. |
| Qualitative Coding | Process of categorizing and interpreting non-numerical data (e.g., interview transcripts, meeting minutes). | Identifying themes in how board members describe the role of lay perspectives in their deliberations. |
Empirical Assessment of Ethics Review Outcomes Under New Regulations
The EU Clinical Trials Regulation (CTR) represents one of the most significant recent regulatory shifts designed to harmonize and streamline the ethical evaluation of clinical research across member states [94]. A core objective of this regulation is to safeguard participants' rights, safety, and well-being while ensuring the reliability of trial data through a centralized review process [94]. For researchers, sponsors, and drug development professionals, understanding the real-world impact of such sweeping regulatory change is crucial for planning and conducting multinational trials. This guide provides an empirical comparison of ethics review outcomes before and under the initial implementation of the new framework, offering data-driven insights into its effects on review efficiency, focus, and consistency.
Analytical Methods: How the Empirical Assessment Was Conducted
The comparative analysis presented in this guide is primarily based on a robust empirical study that examined 6,740 Requests for Information (RFIs) issued by Belgian Medical Research Ethics Committees (MRECs) across 266 trial dossiers [94]. The methodology can be summarized as follows:
- Study Period & Regulatory Context: The analysis spanned from 2017 to 2024, capturing data from both the five-year CTR pilot phase and the first two years of the fully operational Clinical Trials Information System (CTIS) [94]. This allowed for a direct comparison of review characteristics across different regulatory regimes.
- Data Source & Processing: The primary data was sourced from an Excel file provided by the Belgian government, which listed all trials submitted for ethics assessment during the study period. Assessment reports and RFIs were categorized using a structured codebook [94].
- Analytical Framework: Researchers employed a framework content analysis to scrutinize the RFIs [94]. The analysis focused on:
- The number of RFIs issued per trial.
- The content and focus of RFIs (e.g., scientific, ethical, procedural).
- The relationship between RFIs and trial outcomes (approval, conditional approval, refusal).
- Differences in review patterns between Belgium acting as a Reporting Member State (RMS) versus a Concerned Member State (MSC), and between commercial and non-commercial trials [94].
This method provides a quantitative and qualitative basis for comparing the practical workings of ethics review under the new regulation.
Comparative Data: Review Outcomes and Efficiency
The empirical data reveals clear trends in the volume and nature of ethics review interactions before and under the CTR implementation. The table below summarizes key quantitative findings.
Table 1: Comparative Outcomes of Ethics Review Under the New Regulation
| Review Metric | Pilot & Initial Implementation Phases | Key Changes & Observations |
|---|---|---|
| Overall RFI Volume | 6,740 RFIs across 266 dossiers [94] | A discernible decline over time, largely driven by a reduction in typographical and linguistic remarks [94]. |
| Review Focus (Part I - Clinical) | RFIs centered on scientific and methodological robustness [94] | Increased attention to emerging trial modalities like decentralized trials, e-consent, and data collection on ethnicity [94]. |
| Review Focus (Part II - Participant-centric) | Heavy focus on the quality and clarity of Informed Consent Forms (ICFs) [94] | Continued strong emphasis on ICFs, highlighting their enduring critical role in participant protection [94]. |
| Review Role (RMS vs. MSC) | Analysis of RFIs based on Belgium's role in the centralized procedure [94] | Member States Concerned (MSCs) raised fewer RFIs in Part I than the Reporting Member State (RMS), prompting reflection on the efficiency of full multi-state review for this section [94]. |
| Inter-Committee Consistency | Observations across 15 accredited Belgian MRECs [94] | Significant variability persisted in the formulation and scope of ethical feedback, despite harmonization goals [94]. |
Shifting Trends: Key Themes in Post-Implementation Review
The Balance Between Ethics and Compliance
A notable finding from the empirical assessment is a growing emphasis on regulatory compliance, which sometimes occurred at the expense of deeper ethical deliberation [94]. The study notes that the strict timelines and procedural constraints of the CTR can limit the opportunity for timely discussion of complex ethical concerns during the initial admissibility assessment [94]. This suggests that while efficiency may improve, the depth of ethical analysis could be a point of attention for researchers and committees alike.
Evolution of Committee Expertise and Focus
Parallel research on Research Ethics Board (REB) composition underscores that effective review requires a multidisciplinary membership with expertise spanning science, ethics, law, and community representation [9]. International guidelines, such as the CIOMS guidelines, recommend that REBs include physicians, scientists, nurses, lawyers, ethicists, and community members who can represent the cultural and moral values of study participants [9]. The empirical assessment of the CTR aligns with this, showing that RFIs increasingly address complex, modern challenges like decentralized trials and e-consent, demanding diverse and up-to-date expertise from committee members [9] [94].
Evaluating ethics review systems is a distinct research endeavor. The table below outlines key methodological tools and approaches used in the field.
Table 2: Key Reagents and Methods for Empirical Ethics Research
| Tool / Method | Primary Function | Application in Context |
|---|---|---|
| Request for Information (RFI) Analysis | To quantitatively and qualitatively assess the focus and frequency of committee queries. | Served as the primary data source for tracking review focus and stringency under the new regulation [94]. |
| Scoping Review Methodology | To map the extent, range, and nature of research activity on a topic and identify research gaps. | A well-established method for summarizing disparate literature on ethics review quality and effectiveness [9] [73] [95]. |
| Framework Content Analysis | To systematically categorize and interpret qualitative data from documents like assessment reports. | Used to code and analyze the content of thousands of RFIs into structured themes (e.g., scientific, ethical, procedural) [94]. |
| Stakeholder Surveys (e.g., User Satisfaction) | To measure perceptions of ethics service quality among researchers, participants, and committee members. | An empirical measure used in other contexts to assess the value and impact of ethics services from multiple perspectives [96]. |
Visualizing the Regulatory Workflow and Its Assessment
The following diagram illustrates the key stages of the ethics review process under the EU CTR, based on the empirical study, and highlights the points where assessment data was captured.
Figure 1: This workflow of the ethics review process under the EU CTR highlights the Request for Information (RFI) phase as a critical node for empirical assessment. The study analyzed RFI data to evaluate review outcomes, focusing on aspects like volume, content related to Part I and Part II, and the final committee decisions [94].
Empirical evidence from the initial years of the EU CTR indicates a mixed outcome. On one hand, the regulation has been associated with a discernible increase in efficiency, evidenced by a decline in total RFIs, particularly of a typographical nature [94]. On the other hand, challenges remain regarding the variability in feedback between different MRECs and a perceptible shift towards a compliance-oriented checklist approach that may risk marginalizing deeper ethical deliberation [94]. For the research community, these findings underscore the importance of preparing exceptionally clear and methodologically sound dossiers that pre-empt common RFIs, while also being prepared for ongoing inconsistencies in feedback across different national committees. Future success will likely depend on a combination of regulatory adherence and proactive, ethical study design.
Developing Metrics for Evaluating Ethical Analysis Depth and Rigor
The increasing integration of empirical data with normative-ethical analysis has created a pressing need for robust metrics to evaluate the depth and rigor of such interdisciplinary work. Empirical ethics research combines methodologies from social sciences, such as surveys and interviews, with philosophical ethical analysis to produce knowledge that would not be possible using either approach alone [19]. This field faces a fundamental challenge: a lack of established consensus regarding assessment criteria for evaluating research ethics review processes and ethical analysis quality [95] [73]. Without standardized evaluation metrics, the scientific community struggles to assess the quality of empirical ethics research, potentially leading to methodological inconsistencies and ethical misjudgments [19].
This guide compares methodological approaches for developing and applying quality metrics in empirical ethics research, providing researchers with practical frameworks, experimental protocols, and visualization tools to enhance the assessment of ethical analysis in scientific studies.
Comparative Analysis of Methodological Approaches
Theoretical Foundations for Metric Development
The development of metrics for evaluating ethical analysis requires understanding both the metrics of ethics (how ethics can be measured) and the ethics of metrics (how measurement itself shapes ethical practice) [97]. This dual perspective acknowledges that metrics function both as representations of ethical quality and as performative forces that constitute ethical practices within research communities.
Table 1: Theoretical Frameworks for Ethics Evaluation Metrics
| Framework Component | Description | Application Context |
|---|---|---|
| Representation Approach | Metrics capture or demonstrate ethics through measurable indicators | Quantitative assessment of procedural compliance and documentation |
| Performativity Approach | Metrics shape or constitute ethics by influencing researcher behavior | Qualitative assessment of ethical reasoning and decision-making processes |
| Integrated Evaluation | Combines empirical assessment with ethical principle application | Comprehensive evaluation spanning both process and outcome domains [88] |
| Process Domain Ethics | Focuses on ethical aspects of research conduct and decision-making | Evaluation of stakeholder inclusion, value judgments, and power dynamics [88] |
| Outcome Domain Ethics | Addresses ethical consequences and unintended effects of research | Assessment of dual-use potential, societal impacts, and distributive justice [88] |
Current Research Gaps and Challenges
A comprehensive scoping review of empirical research relating to quality and effectiveness of research ethics review reveals significant gaps in current evaluation methodologies. No identified studies reported using an underlying theory or framework of ethics review quality/effectiveness to guide study design or analyses [95] [73]. The research landscape is fragmented, with studies varying substantially regarding outcomes assessed, though most focus primarily on structure and timeliness of ethics review rather than deeper analytical rigor [95].
Few studies on ethics review evaluation originated from outside North America and Europe, indicating geographical limitations in perspective [73]. Additionally, no controlled trials—randomized or otherwise—of ethics review procedures or processes were identified, pointing to a significant methodological gap in establishing evidence-based best practices [95].
Experimental Protocols for Metric Validation
Protocol 1: Quality Criteria Assessment for Empirical Ethics
This protocol enables systematic evaluation of ethical analysis quality in empirical ethics research, based on established quality criteria [19].
Objective: To validate a comprehensive set of quality metrics for assessing ethical analysis depth and rigor in interdisciplinary empirical ethics research.
Materials and Equipment:
- Research protocols for evaluation
- Quality assessment framework checklist
- Inter-rater reliability measurement tools
- Statistical analysis software (e.g., R, SPSS)
- Qualitative data analysis software (e.g., NVivo, MAXQDA)
Procedure:
- Define Primary Research Question: Formulate the core ethical question with both empirical and normative components [19].
- Establish Theoretical Framework: Select and justify the combination of empirical and ethical theories guiding the research [19].
- Methodological Selection: Choose empirical methods appropriate to the research question and theoretical framework.
- Interdisciplinary Integration: Develop explicit procedures for integrating empirical findings with ethical analysis.
- Stakeholder Inclusion: Identify relevant stakeholders and their roles in the research process.
- Ethical Reflection: Apply reflexive practices regarding researcher values and potential biases.
- Data Collection: Gather both empirical data and normative ethical analysis.
- Integration Analysis: Systematically combine empirical and ethical components to generate normative conclusions.
- Peer Validation: Submit research process and findings to interdisciplinary peer review.
- Impact Assessment: Evaluate potential societal and practical impacts of the research.
Validation Metrics:
- Inter-coder reliability coefficients (>0.8 target)
- Construct validity measures through expert consensus
- Criterion validity against established ethical framework applications
- Predictive validity for real-world ethical decision-making
Figure 1: Quality Metric Validation Workflow
Protocol 2: Ethical Framework Visualization and Assessment
This protocol adapts knowledge visualization techniques to make ethical frameworks more accessible and applicable, enabling better evaluation of how researchers understand and apply ethical guidance [98].
Objective: To develop and validate interactive visualization tools for ethical frameworks that improve researcher comprehension and application of ethical principles.
Materials and Equipment:
- Ethical framework documents
- Qualitative content analysis tools
- Visualization software (e.g., Tableau, D3.js)
- Usability testing platform
- Pre-post comprehension assessment instruments
Procedure:
- Content Analysis: Conduct qualitative content analysis of ethical framework documents using open and axial coding [98].
- Knowledge Structure Mapping: Identify key elements, stakeholders, knowledge types, and connections within the framework.
- Visualization Design: Create multiple visual representations (alluvial diagrams, concept maps, systems maps) of the ethical framework [98].
- Expert Review: Submit visualizations to content experts for review and refinement.
- Interactive Development: Develop interactive functionality to allow users to explore framework content through visualization.
- User Testing: Assess comprehension, application accuracy, and usability with target researcher populations.
- Iterative Refinement: Modify visualizations based on user feedback and performance metrics.
- Comparative Assessment: Compare outcomes between text-based and visualization-based framework understanding.
Evaluation Metrics:
- Framework comprehension scores
- Application accuracy in case scenarios
- Time to correct ethical decision
- User satisfaction measures
- Long-term retention of ethical principles
Visualization of Ethics Evaluation Framework
The complex relationship between ethical principles, research stakeholders, and evaluation metrics can be effectively represented through a systems mapping approach that shows interconnections and dependencies.
Figure 2: Ethics Evaluation Framework System
Research Reagent Solutions for Ethics Evaluation
Table 2: Essential Methodological Tools for Ethics Evaluation Research
| Research Reagent | Function | Application Example |
|---|---|---|
| Quality Criteria Road Map | Provides reflective questions for systematic research planning | Ensuring comprehensive coverage of ethical aspects in study design [19] |
| Interactive Framework Visualization | Makes complex ethical guidance accessible through visual representation | Improving researcher understanding of multi-layered ethical frameworks [98] |
| Dual-Coding Assessment Protocol | Evaluates both verbal and visual information processing | Testing effectiveness of different ethics communication methods [98] |
| Stakeholder Analysis Matrix | Identifies and maps relevant stakeholders and their interests | Ensuring appropriate inclusion of affected parties in ethical analysis [88] |
| Integration Methodology Framework | Provides structured approach to combining empirical and normative elements | Facilitating genuine interdisciplinary knowledge production [19] |
| Bias Identification Tool | Detects and mitigates cognitive and methodological biases | Maintaining objectivity in ethical evaluation metrics [99] |
| Ethical Impact Assessment | Evaluates potential consequences and unintended effects | Assessing downstream implications of research ethics decisions [88] |
Comparative Analysis of Evaluation Data
Table 3: Quantitative Assessment of Ethics Evaluation Approaches
| Evaluation Approach | Implementation Complexity | Stakeholder Inclusion | Interdisciplinary Integration | Evidence Strength |
|---|---|---|---|---|
| Procedural Compliance Metrics | Low | Limited | Minimal | Moderate |
| Stakeholder Satisfaction Assessment | Medium | Comprehensive | Partial | Medium |
| Ethical Framework Application | High | Moderate | Substantial | Strong |
| Integrated Process-Outcome Evaluation | High | Comprehensive | Extensive | Strong |
| Visualization-Enhanced Assessment | Medium | Moderate | Substantial | Medium-Strong |
The development of robust metrics for evaluating ethical analysis depth and rigor requires moving beyond procedural compliance to address both the process and outcome domains of ethics [88]. Effective evaluation frameworks must integrate empirical assessment with normative ethical principles while acknowledging the performative power of metrics themselves [97]. The experimental protocols and visualization tools presented in this guide provide researchers with practical methodologies for assessing and enhancing ethical analysis in empirical research. As the field of empirical ethics continues to evolve, further refinement of these metrics through controlled trials and interdisciplinary collaboration will be essential for establishing evidence-based best practices in ethics evaluation [95] [73].
Conclusion
The evaluation of quality criteria for empirical ethics research requires a multifaceted approach that integrates diverse expertise, rigorous methodology, and continuous improvement. Key takeaways include the necessity of multidisciplinary REB composition with appropriate scientific, ethical, and participant perspectives; the importance of implementing standardized reporting frameworks like CONSORT 2025 and STREAM while ensuring they adequately address ethical elements; the value of balancing regulatory compliance with substantive ethical deliberation; and the need for robust validation methods to assess research quality. Future directions should focus on developing evidence-based best practices for REB training and composition, enhancing the integration of ethical reporting elements into methodological guidelines, creating standardized metrics for evaluating ethics research quality, and fostering international harmonization of ethics review standards while accommodating contextual diversity. These advances will significantly strengthen the rigor and impact of empirical ethics research in protecting participants and enhancing research integrity across biomedical and clinical domains.
References
- 1. The normative background of empirical-ethical research [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-015-0016-x]
- 2. Evidence-based ethics? On evidence-based practice and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1298300/]
- 3. Fifteen years of doing 'empirical ethics': from academia to ... [https://www.linkedin.com/pulse/fifteen-years-doing-empirical-ethics-from-academia-industry-mckeown-mntee]
- 4. Evidence-Based Research Ethics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3586321/]
- 5. Empirical Ethics Research → Area [https://lifestyle.sustainability-directory.com/area/empirical-ethics-research/]
- 6. Evidence-based ethics – What it should be and what it shouldn't [https://bmcmedethics.biomedcentral.com/articles/10.1186/1472-6939-9-16]
- 7. Empirical research in bioethical journals. A quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2565792/]
- 8. The Relevance of Empirical Research in Bioethics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2632190/]
- 9. A Scoping Review of Empirical Research on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12490803/]
- 10. Beginner's Guide to institutional review boards (IRBs) [https://www.advarra.com/blog/beginners-guide-to-institutional-review-boards/]
- 11. Research Ethics Board - Clinical Research Explained [https://viares.com/blog/clinical-research-explained/research-ethics-board/]
- 12. Ethical Guidelines and the Institutional Review Board [https://pmc.ncbi.nlm.nih.gov/articles/PMC10885741/]
- 13. Improving the process of research ethics review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5803582/]
- 14. Research Ethics Board: Policies, guidelines and resources [https://www.canada.ca/en/health-canada/services/science-research/science-advice-decision-making/research-ethics-board/policy-guidelines-resources.html]
- 15. Research Ethics Board: About the REB - Health Canada [https://www.canada.ca/en/health-canada/services/science-research/science-advice-decision-making/research-ethics-board/about-us.html]
- 16. Research Ethics Board (REB) [https://participantsmtl.altasciences.com/en/research-ethics-board-reb]
- 17. List of Essentials Documents in Research Ethics [https://www.infonetica.net/articles/research-ethics-essential-documents]
- 18. Global comparison of research ethical review protocols [https://pmc.ncbi.nlm.nih.gov/articles/PMC11975204/]
- 19. Research across the disciplines: a road map for quality criteria ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/1472-6939-15-17]
- 20. 1.4 Experimental Design and Ethics – Statistics Study Guide [https://pressbooks.montgomerycollege.edu/statnotes/chapter/unit1-section1-4/]
- 21. Experimental Design and Ethics | Introduction to Statistics [https://courses.lumenlearning.com/introstats1/chapter/experimental-design-and-ethics/]
- 22. Principles of Effective Data Visualization - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7733875/]
- 23. What Is Data Visualization? Benefits, Types & Best Practices [https://ischool.syracuse.edu/what-is-data-visualization/]
- 24. Using color | U.S. Web Design System (USWDS) [https://designsystem.digital.gov/design-tokens/color/overview/]
- 25. Designing Effective Data Visualizations [https://guides.library.jhu.edu/datavisualization/design]
- 26. Contrast Checker [https://webaim.org/resources/contrastchecker/]
- 27. Color Accessibility on the Web | UTHSC Branding Guidelines [https://uthsc.edu/brand/accessibility-colors.php]
- 28. Gaps in the Ottawa Statement on the Ethical Design and ... [https://researchintegrityjournal.biomedcentral.com/articles/10.1186/s41073-025-00166-y]
- 29. Ethics review of big data research: What should stay and what ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-021-00616-4]
- 30. Ethics review for international data-intensive research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4838154/]
- 31. 2025 Investigative Case Management Benchmark Report [https://www.caseiq.com/resources/investigative-case-management-benchmark-2025]
- 32. The importance of ethical considerations in research and ... [https://lpsonline.sas.upenn.edu/features/importance-ethical-considerations-research-and-clinical-trials]
- 33. CIOMS cited [https://cioms.ch/cioms-cited/]
- 34. Clinical Research Regulation For United States | ClinRegs [https://clinregs.niaid.nih.gov/country/united-states]
- 35. Developing Standards for Rapid Evaluation and Appraisal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12256111/]
- 36. Projects: STREAM [https://www.rapidresearchandevaluation.com/stream-project]
- 37. STREAM | Faculty of Population Health Sciences [https://www.ucl.ac.uk/population-health-sciences/stream]
- 38. The EQUATOR Network and research reporting guidelines [https://www.wolterskluwer.com/en/expert-insights/authors-equator-network]
- 39. EQUATOR Network | Enhancing the QUAlity and ... [https://www.equator-network.org/]
- 40. Search for reporting guidelines [https://www.equator-network.org/reporting-guidelines-study-design/experimental-studies/]
- 41. CONSORT 2025 Statement - Reporting guideline [https://www.equator-network.org/reporting-guidelines/consort/]
- 42. Consensus-based Clinical Case Reporting Guideline ... [https://www.equator-network.org/reporting-guidelines/care/]
- 43. the TREND statement - Reporting guideline [https://www.equator-network.org/reporting-guidelines/improving-the-reporting-quality-of-nonrandomized-evaluations-of-behavioral-and-public-health-interventions-the-trend-statement/]
- 44. the TARGET Statement - Reporting guideline [https://www.equator-network.org/reporting-guidelines/22462/]
- 45. Reporting guidelines under development for systematic ... [https://www.equator-network.org/library/reporting-guidelines-under-development/reporting-guidelines-under-development-for-systematic-reviews/]
- 46. Reporting guidelines under development for other study ... [https://www.equator-network.org/library/reporting-guidelines-under-development/reporting-guidelines-under-development-for-other-study-designs/]
- 47. A Scoping Review of Empirical Research on ... [https://pubmed.ncbi.nlm.nih.gov/41032647/]
- 48. A Novel Use of Graphical Models in Empirical Ethics Inquiry [https://pmc.ncbi.nlm.nih.gov/articles/PMC4423405/]
- 49. Reframing data ethics in research methods education [https://educationaltechnologyjournal.springeropen.com/articles/10.1186/s41239-023-00380-y]
- 50. Ethical Data Visualization Guide: 5 Best Practices [https://text2infographic.com/blog/ethical-data-visualization-guide-5-best-practices]
- 51. We can evaluate rapidly, but should we? Researchers' and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12411679/]
- 52. Methods for rapid evaluation - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/n/ukhsdr1111/s3/]
- 53. Getting Rigor Right: A Framework for Methodological ... [https://www.ghspjournal.org/content/11/Supplement_2/e2200243]
- 54. Rapid evidence synthesis to enable innovation and adoption ... [https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-022-02106-z]
- 55. A Review of the Quality Indicators of Rigor in Qualitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7055404/]
- 56. CONSORT 2025 statement: updated guideline for reporting ... [https://www.nature.com/articles/s41591-025-03635-5]
- 57. CONSORT 2025 statement: Updated guideline for ... [https://pubmed.ncbi.nlm.nih.gov/40228477/]
- 58. Viewpoints of investigator on CONSORT 2025 statement ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12170029/]
- 59. a road map for quality criteria in empirical ethics research [https://pubmed.ncbi.nlm.nih.gov/24580847/]
- 60. consort-spirit.org: Home [https://www.consort-spirit.org/]
- 61. Avoiding Documentation Pitfalls That Lead to Compliance ... [https://staffready.com/2025/02/05/avoiding-documentation-pitfalls-that-lead-to-compliance-violations/]
- 62. Keeping good documentation: the ethical and legal issues ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12503401/]
- 63. Top challenges with clinical trial ethics in 2025 [https://clinicaltrialrisk.org/clinical-trial-design/top-challenges-with-clinical-trial-ethics/]
- 64. Publication Ethics [https://icml.cc/Conferences/2025/PublicationEthics]
- 65. Reevaluating Board Composition [https://internationalbanker.com/finance/reevaluating-board-composition/]
- 66. The 2025 Guide to Board Composition [Types, Roles, Strategies] [https://governanceatwork.io/blog/board-composition/]
- 67. Regulation of the Clinical Research Law and next steps [https://www.soutocorrea.com.br/en/client-alerts/regulation-of-the-clinical-research-law-and-next-steps/]
- 68. Compliance vs. ethics: what is the difference and why it matters [https://community.trustcloud.ai/docs/grc-launchpad/grc-101/compliance/compliance-vs-ethics-what-is-the-difference-and-why-it-matters/]
- 69. What's The Difference Between Compliance And Ethics? [https://www.forbes.com/sites/bruceweinstein/2019/05/09/whats-the-difference-between-compliance-and-ethics/]
- 70. Ethics and Compliance: One in the Same? [https://www.wichita.edu/administration/internalaudit/blog/2019-07-10-compliance.php]
- 71. Ep.12: Ethics vs. Compliance — Culture. Data. Ethics. [https://www.cdeadvisors.com/betterwaypodcast/ethicsvscompliance]
- 72. Artificial Intelligence and Regulatory Realities in Drug ... [https://globalforum.diaglobal.org/issue/april-2025/artificial-intelligence-and-regulatory-realities-in-drug-development-a-pragmatic-view/]
- 73. A Scoping Review of Empirical Research Relating to Quality ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0133639]
- 74. Considerations for the Use of Artificial Intelligence [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/considerations-use-artificial-intelligence-support-regulatory-decision-making-drug-and-biological]
- 75. 2025 Life Sciences Regulatory Outlook [https://www.deloitte.com/us/en/services/consulting/articles/life-sciences-regulatory-outlook.html]
- 76. Core elements of consent documentation for clinical research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12448764/]
- 77. Assessing Different Consent Form Formats [https://www.wcgclinical.com/insights/function-over-form-assessing-different-consent-form-formats/]
- 78. Readability of Informed Consent Forms for Medical and ... [https://www.mdpi.com/2039-7283/15/2/26]
- 79. Digitalizing informed consent in healthcare: a scoping review [https://pmc.ncbi.nlm.nih.gov/articles/PMC12225439/]
- 80. Comparative study on informed consent regulation in ... [https://www.sciencedirect.com/science/article/pii/S1752928X24000362]
- 81. Stakeholder Communication: Benefits, Best Practices, and ... [https://simplystakeholders.com/stakeholder-communication/]
- 82. 8 Tips for Managing Multiple Stakeholders [https://fiscalnote.com/blog/8-tips-for-managing-multiple-stakeholders]
- 83. What Is Ethics in Research & Why Is It Important? [https://www.niehs.nih.gov/research/resources/bioethics/whatis]
- 84. Ethical Guidelines for Statistical Practice [https://www.amstat.org/your-career/ethical-guidelines-for-statistical-practice]
- 85. Stakeholder Feedback: Methods & Best Practices [https://simplystakeholders.com/stakeholder-feedback/]
- 86. The Ultimate Stakeholder Communication Plan for 2024 [https://www.ocmsolution.com/stakeholder-communication-plan/]
- 87. Criteria for qualitative methods in human reliability analysis [https://www.sciencedirect.com/science/article/pii/S0951832017310268]
- 88. JMIR Research Protocols - Examining Practices Related to Ethical ... [https://www.researchprotocols.org/2025/1/e60849]
- 89. Navigating Ethical Approval Processes in 2024- 2025 : IRB and Beyond [https://editverse.com/navigating-ethical-approval-processes-in-2024-2025-irb-and-beyond/]
- 90. Understanding Roles and Importance of IEC, ERB, and ... [https://clival.com/blog/understanding-roles-and-importance-of-iec-erb-and-reb-in-clinical-trials]
- 91. What’s age got to do with it? The effect of board member age... [https://link.springer.com/article/10.1007/s11301-022-00294-5]
- 92. Views of IRB Chairpersons at U.S. Universities and ... [https://philpapers.org/rec/CHUDII]
- 93. questionpro.com/blog/ empirical - research [https://www.questionpro.com/blog/empirical-research/]
- 94. Ethics review or compliance check? an empirical analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506313/]
- 95. A Scoping Review of Empirical Research Relating to Quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4520456/]
- 96. Empirical assessments of clinical ethics services [https://pmc.ncbi.nlm.nih.gov/articles/PMC2493408/]
- 97. The Metrics of Ethics and the Ethics of Metrics [https://ideas.repec.org/a/kap/jbuset/v175y2022i1d10.1007_s10551-021-05004-x.html]
- 98. Visualizing an Ethics Framework: A Method to Create ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6996733/]
- 99. Data Visualization Ethics → Term [https://fashion.sustainability-directory.com/term/data-visualization-ethics/]