Ethical Safeguards: A Comprehensive Guide to the Informed Consent Process for Vulnerable Populations in Clinical Research
This article provides researchers, scientists, and drug development professionals with a strategic framework for navigating the ethical and practical complexities of obtaining informed consent from vulnerable populations.
Ethical Safeguards: A Comprehensive Guide to the Informed Consent Process for Vulnerable Populations in Clinical Research
Abstract
This article provides researchers, scientists, and drug development professionals with a strategic framework for navigating the ethical and practical complexities of obtaining informed consent from vulnerable populations. Covering foundational principles from regulatory policy to contemporary analytical models of vulnerability, the guide details adaptable methodologies for diverse groups, proactive solutions for common challenges like comprehension barriers and power dynamics, and validation techniques to ensure process integrity. By synthesizing current guidelines and evidence-based strategies, this resource aims to equip clinical teams to uphold the highest standards of ethical research while promoting equitable participation.
Understanding Vulnerability and Ethical Frameworks in Human Subjects Research
In the context of research ethics, vulnerability represents a multifaceted concept critical to the protection of human subjects. The Oxford English Dictionary defines it as "the quality of being susceptible to harm, influence, or attack" [1]. Within healthcare research, vulnerability is often associated with a perceived loss of power relative to others, coupled with heightened exposure to various risks, including physical, psychological, emotional, cultural, and economic threats [1]. This sense of vulnerability intensifies with diminished self-confidence and challenges in navigating unfamiliar health-related situations [1]. For researchers, understanding and properly assessing vulnerability is essential for implementing ethical safeguards, particularly during the informed consent process, ensuring that care and research protocols are tailored to the unique needs of each individual.
The Common Rule, a federal standard of ethics, oversight, and transparency in government-funded research involving human subjects, specifically contains provisions to protect particular vulnerable populations such as pregnant women, human fetuses, prisoners, and children [2]. Historically, vulnerability was often approached through a categorical lens, identifying specific groups considered at risk. However, modern frameworks recognize vulnerability as a dynamic state that requires analytical assessment rather than simple group classification. This shift enables researchers to better protect participants through tailored consent processes and study designs that address their specific circumstances and capacities.
Vulnerability Categories and Assessment Frameworks
Categorical Groups of Vulnerable Populations
Vulnerable populations in clinical research settings refer to groups of people who can be harmed, manipulated, coerced, or deceived by unscrupulous researchers because of their limited decision-making ability, lack of power, or disadvantaged status [3]. These populations include children, prisoners, individuals with impaired decision-making capacity, or those who are economically or educationally disadvantaged [3]. Aday's seminal work highlighted several populations considered particularly vulnerable, including high-risk mothers and infants, the chronically ill and disabled, individuals with AIDS, those with mental illnesses, alcohol or substance abusers, individuals prone to suicide or homicide, abusive families, the homeless, and immigrants and refugees [1].
Table 1: Traditional Categorical Vulnerable Populations in Research
| Population Category | Key Vulnerability Factors | Common Ethical Concerns |
|---|---|---|
| Children | Limited capacity for understanding; legal inability to provide consent | Coercion by authority figures; inability to comprehend risks |
| Prisoners | Restricted autonomy; potential for undue influence | Perceived coercion to participate; limited alternatives |
| Economically Disadvantaged | Financial pressures; limited access to healthcare | Undue inducement; unequal benefits distribution |
| Cognitively Impaired | Diminished decision-making capacity | Challenges assessing understanding; potential for exploitation |
| Seriously Ill Patients | Desperation for treatment; therapeutic misconception | Overestimation of benefits; underestimation of risks |
Analytical Frameworks for Vulnerability Assessment
Moving beyond categorical approaches, modern vulnerability assessment employs multidimensional frameworks that evaluate various contributing factors. Havrilla defines vulnerability as "a state of dynamic openness and opportunity for individuals, groups, communities, or populations to respond to community and individual factors through the use of internal and external resources in a positive (resilient) or negative (risk) manner along a continuum of illness (oppression) to health (growth)" [1]. This conceptualization acknowledges vulnerability as a dynamic state rather than a fixed characteristic, emphasizing the continuum along which individuals may move based on available resources and support systems.
The shift from categorical to analytical frameworks represents a significant evolution in research ethics. Rather than applying predetermined protections based solely on group membership, researchers now assess individual circumstances, contextual factors, and specific research demands. This approach allows for more tailored safeguards that address actual rather than presumed vulnerabilities. Analytical frameworks consider intersecting factors such as decision-making capacity, situational pressures, understanding of research concepts, and power differentials that may affect a participant's ability to provide truly informed consent.
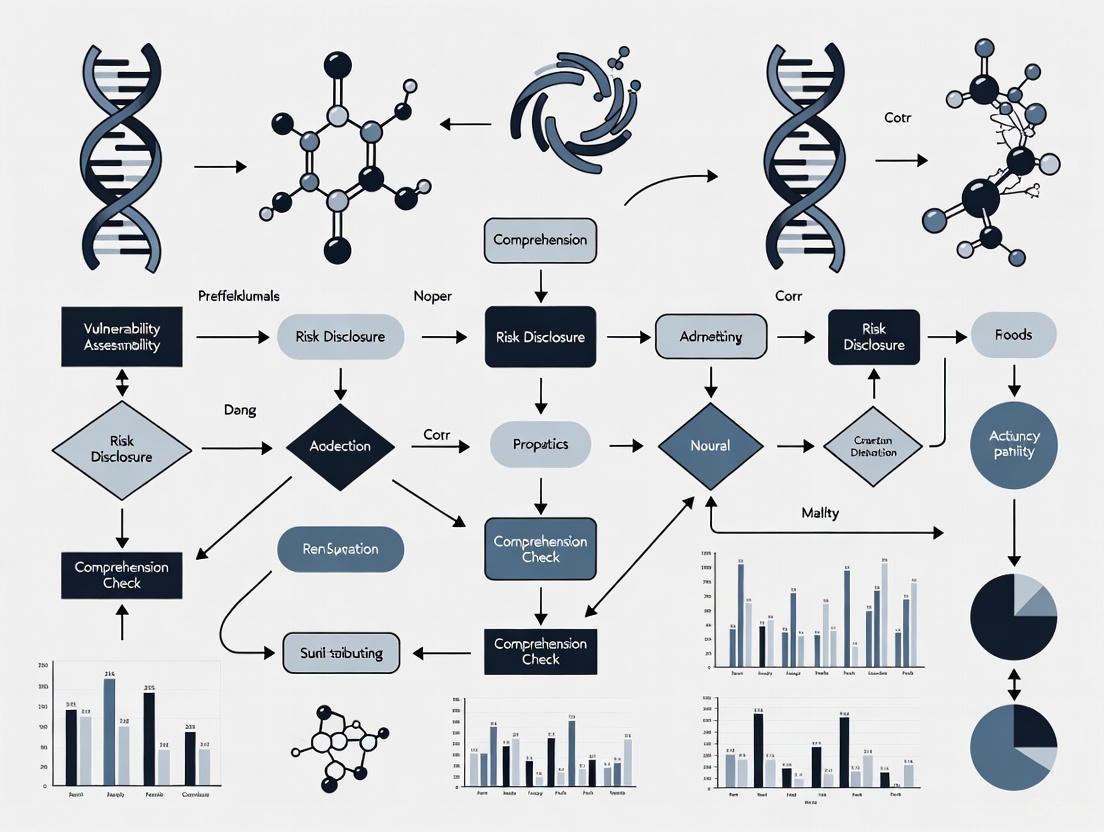
Diagram 1: Analytical Framework for Vulnerability Assessment in Research. This diagram illustrates the multidimensional factors contributing to vulnerability assessment and their relationship to tailored consent processes and ethical research participation.
Application Notes: Vulnerability Assessment Instruments and Protocols
Available Vulnerability Assessment Instruments
A recent scoping review identified 13 distinct instruments used to assess vulnerability at the individual and/or family level in healthcare contexts [1]. These instruments vary widely in terms of dimensions, number of items, target populations, and modes of completion. Some instruments focus on specific aspects such as socioeconomic status, health behaviors, or access to services [1]. The review demonstrates the complexity of the vulnerability concept and the need for instruments adapted to specific determinants/factors, such as environmental, biological, and social factors, as well as the specificities of target populations and contexts of assessment and intervention.
Table 2: Characteristics of Vulnerability Assessment Instruments in Healthcare Research
| Instrument Name | Target Population | Key Assessment Domains | Completion Method |
|---|---|---|---|
| Vulnerable Elders Survey | Older adults | Functional status, self-rated health, age | Self-report or interviewer-administered |
| Social Vulnerability Index (SVI) | General population | Socioeconomic status, household composition, disability, minority status, housing/transportation | Composite index from existing data |
| Perceived Vulnerability Scale (PVS) | Adults | Subjective perception of vulnerability to health threats | Self-report |
| Vulnerability Scale for the Elderly (VSE) | Older adults | Social support, economic resources, health status, environmental factors | Interviewer-administered |
| HRCA Vulnerability Index | Older adults | Physical health, functional capacity, social resources | Professional assessment |
Experimental Protocol: Comprehensive Vulnerability Assessment for Informed Consent
Protocol Objectives and Scope
This protocol provides a standardized methodology for assessing vulnerability factors that may impact the informed consent process in research involving human subjects. The primary objective is to identify individual-specific vulnerability factors that might compromise a potential participant's ability to provide voluntary, informed consent. The assessment follows a multidimensional approach that considers decision-making capacity, situational factors, understanding, and power differentials rather than relying solely on categorical group membership.
The protocol applies to all potential research participants, with particular attention to populations historically classified as vulnerable. The assessment should be conducted by trained research staff familiar with research ethics and vulnerability concepts, ideally during the initial screening process before the formal consent discussion begins. The outcome informs modifications to the consent process to ensure comprehension and voluntariness.
Materials and Equipment
Table 3: Research Reagent Solutions for Vulnerability Assessment
| Item | Function | Application Notes |
|---|---|---|
| Vulnerability Assessment Tool | Standardized instrument to evaluate vulnerability dimensions | Select instrument based on population and research context; ensure cultural appropriateness |
| Decision-Making Capacity Assessment | Structured evaluation of understanding, appreciation, reasoning, and choice | Use validated tools such as MacCAT-CR or UBACC for clinical trials |
| Understanding Assessment Tool | Measure comprehension of research concepts | Develop study-specific quiz with key elements; aim for 100% comprehension |
| Environmental Assessment Checklist | Evaluate context where consent is obtained | Assess privacy, comfort, time pressure, and potential coercive influences |
| Cultural/Linguistic Support Materials | Facilitate communication across language and cultural barriers | Professional interpreters, translated materials at appropriate literacy levels |
Step-by-Step Procedures
Step 1: Pre-Assessment Preparation (Time: 15-20 minutes)
- Review the proposed research protocol to identify potential vulnerability factors specific to the study (e.g., complex procedures, high risk, novel interventions)
- Select appropriate assessment instruments based on the target population and research context
- Prepare the physical environment to ensure privacy and comfort for the assessment
- Arrange for interpretation services or specialized communication assistance if needed
Step 2: Initial Screening (Time: 10-15 minutes)
- Conduct a preliminary assessment of demographic and situational factors
- Identify obvious categorical vulnerabilities (e.g., cognitive impairment, limited English proficiency)
- Determine if additional resources are needed for the full assessment
- Document initial observations in the research record
Step 3: Multidimensional Assessment (Time: 20-30 minutes)
- Administer selected vulnerability assessment instruments using standardized procedures
- Evaluate decision-making capacity using structured tools if indicated
- Assess understanding of basic research concepts through simple explanation and questioning
- Identify situational pressures that might affect participation decisions
- Document all assessment results using standardized forms
Step 4: Analysis and Interpretation (Time: 15-20 minutes)
- Review assessment results to identify specific vulnerability factors
- Determine the magnitude and nature of potential vulnerabilities
- Assess how identified vulnerabilities might impact the consent process
- Develop recommendations for consent process modifications
- Document the analysis and recommendations
Step 5: Consent Process Tailoring (Time: Variable)
- Implement recommended modifications to the consent process
- This may include: simplified consent forms, extended discussion time, use of multimedia materials, involvement of surrogate decision-makers, additional educational sessions
- Ensure all modifications are documented and approved by the IRB if required
Step 6: Ongoing Monitoring (Time: Throughout study participation)
- Continuously assess for emerging vulnerabilities during study participation
- Monitor understanding retention at regular intervals
- Be alert to changes in circumstances that might create new vulnerabilities
- Document and address any new vulnerability concerns promptly
Diagram 2: Vulnerability Assessment Workflow for Informed Consent. This diagram outlines the sequential steps for conducting a comprehensive vulnerability assessment to support ethical informed consent processes in research with human subjects.
Data Analysis and Interpretation
Analysis of vulnerability assessment data should focus on identifying specific barriers to informed consent rather than simply categorizing individuals as vulnerable or not. Quantitative data from standardized instruments should be interpreted according to established cutoff scores where available. Qualitative observations should be systematically reviewed for patterns indicating potential vulnerabilities. The overall assessment should result in a vulnerability profile that identifies specific factors requiring accommodation in the consent process.
Key interpretation principles include:
- Consider vulnerabilities as context-specific rather than absolute
- Recognize that multiple minor vulnerabilities may have cumulative effects
- Assess the interaction between different vulnerability factors
- Prioritize vulnerabilities that directly impact decision-making capacity or voluntariness
- Consider compensatory strengths and resources the individual may possess
Troubleshooting and Optimization
Common challenges in vulnerability assessment include:
- Resistance from participants who may feel stigmatized by the assessment: Address by normalizing the process and emphasizing its protective purpose
- Discrepancies between different assessment tools: Resolve through clinical judgment and consideration of the specific research context
- Time constraints in busy clinical settings: Optimize by using brief screening tools followed by targeted in-depth assessment when needed
- Cultural or linguistic barriers: Address through use of validated translated instruments and professional interpreters
- Uncertainty in interpretation: Consult with ethics committee or colleagues experienced in vulnerability assessment
Discussion: Implications for Research Ethics and Practice
The evolution from categorical to analytical frameworks for understanding vulnerability has significant implications for research ethics and practice. Modern approaches recognize that vulnerability exists on a continuum and is influenced by multiple interacting factors [1]. This perspective allows for more nuanced and individualized protection of research participants while facilitating appropriate inclusion of potentially vulnerable populations.
Current regulations acknowledge the need for special protections for vulnerable populations. The Common Rule specifically contains provisions to protect particular vulnerable populations such as pregnant women, human fetuses, prisoners, and children [2]. However, an analytical approach complements these categorical protections by requiring researchers to assess individual vulnerability factors regardless of group membership. This is particularly important for individuals who may experience vulnerability due to intersecting factors that don't fit neatly into predefined categories.
The development of validated assessment instruments provides researchers with practical tools to implement analytical vulnerability assessment [1]. These instruments enable systematic evaluation of vulnerability factors rather than reliance on intuition or assumptions. However, instrument selection must be guided by consideration of the specific research context and population, as no single tool is appropriate for all situations.
Engaging vulnerable populations in research requires careful attention to ethical safeguards while avoiding inappropriate exclusion. As noted by Dr. Muhammad Waseem, "While vulnerable populations are considered at higher risk of harm or injustice in research, since they often cannot protect themselves through valid informed consent, they are also underrepresented and underserved in clinical research" [3]. Excluding vulnerable populations from research can perpetuate health disparities by limiting the generalizability of findings and access to potentially beneficial experimental treatments.
The analytical framework presented in this document provides a structured approach to vulnerability assessment that supports ethical inclusion of vulnerable populations through tailored consent processes and ongoing monitoring. This approach respects the principles of justice, beneficence, and respect for persons that form the foundation of research ethics, while advancing scientific validity through appropriate inclusion of diverse populations.
The Belmont Report, published in 1979, established the foundational ethical principles for conducting research involving human subjects in the United States. Its creation was prompted by historical ethical abuses, most notably the Tuskegee Syphilis Study, and it continues to shape modern research ethics [4]. The Report's principles were later operationalized into federal regulations through the Federal Policy for the Protection of Human Subjects, commonly known as the Common Rule (45 CFR part 46) [4]. The relationship between these guidelines and evolving international standards is critical for today's researchers, particularly when developing protocols for vulnerable populations who require additional protections. Recent regulatory trends in 2025 show agencies like the FDA and EMA increasing their focus on ensuring these populations are protected with stricter ethical and procedural safeguards [5] [6]. This document outlines application notes and detailed protocols for navigating this complex regulatory environment, with a specific focus on obtaining ethically valid informed consent from vulnerable participants.
Core Ethical Principles and Regulatory Frameworks
The Belmont Report's Three Ethical Pillars
The Belmont Report elucidates three core ethical principles that must govern all human subjects research [4]:
- Respect for Persons: This principle acknowledges the autonomy of individuals and requires protecting those with diminished autonomy. It mandates that subjects enter research voluntarily and with adequate information, forming the bedrock of the informed consent process.
- Beneficence: This principle extends beyond "do no harm" to maximizing possible benefits and minimizing potential risks. It requires a systematic assessment of all research risks and benefits.
- Justice: This principle addresses the fair distribution of the burdens and benefits of research. It requires that the selection of subjects be scrutinized to avoid systematically recruiting vulnerable populations simply for administrative convenience or due to their compromised position.
The Common Rule: Operationalizing Ethics
The Common Rule translates the ethical principles of Belmont into enforceable regulations for IRBs, sponsors, and investigators [4]. Key revisions that impact research involving vulnerable populations include:
- Informed Consent Revisions: The revised Common Rule requires that consent forms begin with a "concise and focused presentation of key information" to help prospective subjects understand reasons for or against participation. The form must be organized to facilitate comprehension [7].
- Exempt Research Categories: The Rule outlines categories of research that may be exempt from full IRB review. Several categories were modified or added, some of which have specific provisions for collecting identifiable, sensitive information, requiring IRBs to ensure adequate privacy and confidentiality safeguards are in place [7].
- Elimination of Continuing Review: For many minimal-risk studies that have progressed to data analysis or are eligible for expedited review, continuing review is no longer mandated. However, IRBs retain the discretion to require it for studies with specific risk profiles, such as those conducted internationally or where non-compliance is a concern [7].
International Harmonization and 2025 Trends
Globally, regulatory agencies are working to harmonize standards. The International Council for Harmonisation's (ICH) Guideline for Good Clinical Practice E6(R3) maintains ties to the ethical framework of the Belmont Report [4]. Key 2025 trends include:
- Increased Focus on Vulnerable Populations: Regulatory bodies like the U.S. HHS and FDA are refining guidelines and regulations for protecting children, pregnant women, prisoners, and other vulnerable groups. This drive for harmonization aims to simplify ethical reviews and provide consistent oversight while ensuring the highest protection standards [6].
- Patient-Centricity: The European Medicines Agency (EMA) is prioritizing patient engagement, including integrating patient-reported outcomes in trials and involving patient advocacy groups early in development [8].
- Decentralized Trials and Technology: Following the pandemic, models like decentralized and hybrid clinical trials are being promoted to improve access and convenience. This involves using digital platforms and wearable devices, which must be implemented with careful attention to the digital literacy and access of vulnerable participants [8].
Table 1: Core Ethical Principles and Their Application to Vulnerable Populations
| Ethical Principle (Belmont) | Regulatory Manifestation (Common Rule/ICH) | Application to Vulnerable Populations |
|---|---|---|
| Respect for Persons | Informed consent process; documentation of voluntary participation [4] [7]. | Requires assessments of decisional capacity; use of legally authorized representatives; and assent procedures for children or adults with impaired capacity. |
| Beneficence | Thorough risk-benefit analysis by IRB; ongoing monitoring of safety data [4]. | Demands stringent justification for including vulnerable individuals in research, ensuring risks are justified by potential benefits to them or their population. |
| Justice | Equitable selection of subjects; scrutiny of recruitment methods [4]. | Protects against the systematic over-use of vulnerable groups for convenience and promotes fair access to the benefits of research. |
Application Notes: Implementing Ethical Protocols for Vulnerable Populations
Implementing the Belmont principles and Common Rule requirements demands careful, practical planning. The following notes address key application areas.
Defining and Identifying Vulnerability
Vulnerability in research arises from a potential for exploitation due to an impaired ability to protect one's own interests. Key populations include [5]:
- Children and minors
- Pregnant women, fetuses, and neonates
- Prisoners and incarcerated persons
- Individuals with cognitive or intellectual disabilities
- Economically or educationally disadvantaged persons
- Patients in emergency settings
Application Note 1.1: Vulnerability is context-specific. A university professor may be vulnerable in a study related to a life-threatening personal illness, while a prisoner may not be vulnerable in a study on social structures if their participation is truly voluntary and anonymous. The protocol must justify the specific population and describe the additional safeguards implemented.
The Enhanced Informed Consent Process
For vulnerable populations, the consent process is an ongoing dialogue, not a single event. Key elements include [5]:
- Capacity Assessment: Implement a brief, validated tool to assess a potential subject's understanding of the study's key elements, especially for populations with fluctuating or questionable capacity.
- Process Consent: For individuals with progressive cognitive disorders, re-evaluate understanding at regular intervals throughout the study.
- Assent and Respect: Even when formal consent is provided by a representative, seek the affirmative agreement (assent) of the individual if they have some level of understanding. Respect any signs of dissent.
- Witnesses and Advocates: Utilize independent, unaffiliated witnesses or patient advocates during the consent discussion to ensure the process is free from coercion and that information is adequately conveyed.
Experimental Protocols: Consent and Oversight Workflows
Protocol: Developing an Informed Consent Plan for a Vulnerable Population
Objective: To create a comprehensive, ethically sound informed consent plan for research involving adults with mild cognitive impairment (MCI).
Materials: See "Research Reagent Solutions" in Section 5.
Methodology:
Pre-Study Phase
- IRB Consultation: Engage with the IRB early to discuss the population, justification for inclusion, and the proposed consent process. Determine if a waiver of some consent elements is possible or required.
- Consent Form Development: Draft the consent form using plain language at a 6th-grade reading level. Adhere to the revised Common Rule requirement by starting with a concise summary of key information (purpose, procedures, risks, benefits, alternatives). Use large, legible fonts (e.g., 14-point).
- Capacity Assessment Tool Selection: Select and validate a brief capacity assessment tool (e.g., the University of California, San Diego Brief Assessment of Capacity to Consent [UBACC]) to be administered prior to the full consent discussion.
Consent Execution Phase
- Environment Setting: Conduct the consent discussion in a quiet, private, and comfortable environment free from distractions.
- Participant and Representative Presence: The potential participant must be present with their legally authorized representative (LAR).
- Information Disclosure: The investigator explains the study, using the simplified consent form and any auxiliary aids (e.g., pictograms, videos).
- Teach-Back Method: After explaining a key concept (e.g., "randomization"), ask the participant to explain it back in their own words to confirm understanding.
- Capacity Assessment: The study coordinator administers the brief capacity tool.
- Decision and Documentation: Based on the capacity assessment, the primary consent is provided by either the participant (if deemed capable) or the LAR. The participant's assent is sought regardless. All parties present, including the witness, sign and date the consent form.
Ongoing Consent Process
- Re-assessment Triggers: Define criteria for re-assessing consent capacity (e.g., significant decline in clinical status, before a new invasive procedure).
- Continuing Communication: Provide a "Consent Passport" — a wallet-sized card with the study contact information and key facts — to the participant and their caregiver.
The following workflow diagrams the key decision points and procedures in this enhanced consent process.
Protocol: Implementing a Single IRB (sIRB) Model for Multi-Site Research
Objective: To streamline the ethical review process for a multi-site clinical trial involving pregnant women, ensuring consistent application of protections for this vulnerable population.
Materials: sIRB Reliance Agreement templates; Central IRB contact information; Study protocol and consent documents.
Methodology:
- Determination of sIRB of Record: The lead study sponsor, in consultation with site investigators, identifies and selects the sIRB of record. This is often a central, commercial IRB with specific expertise in the relevant therapeutic area and vulnerable population.
- Reliance Agreements: Each participating research site executes a formal reliance agreement with the sIRB of record. This agreement cedes the local IRB's review authority for this study to the sIRB, while the local institution retains responsibility for local context issues (e.g., site investigator qualifications, local resources).
- Single Submission and Review: The study sponsor submits the complete protocol, informed consent documents, and recruitment materials to the sIRB of record for initial review.
- Local Context Review: While the sIRB reviews the overall ethical soundness of the study, the local IRB at each site conducts a "local context review." This includes assessing cultural and linguistic appropriateness of consent forms, feasibility, and local legal or regulatory requirements.
- Communication and Coordination: The sIRB communicates its approval, required modifications, or disapproval to the study sponsor and all relying sites. All subsequent amendments, continuing reviews, and reportable events are submitted to the sIRB, ensuring harmonized oversight.
The Scientist's Toolkit: Research Reagent Solutions
For researchers designing studies involving vulnerable populations, the following "reagents" — essential procedural tools and documents — are critical for ensuring ethical integrity and regulatory compliance.
Table 2: Essential Research Reagents for Ethical Research with Vulnerable Populations
| Research 'Reagent' (Tool/Document) | Function & Purpose | Application Example |
|---|---|---|
| Legally Authorized Representative (LAR) | An individual or judicial body authorized under applicable law to provide consent on behalf of a prospective subject. | Provides informed consent for an adult with advanced dementia to participate in a study on nutrition. |
| Simplified Consent Form with Pictograms | A consent document written at a low reading level, using images to explain complex concepts like randomization or risks. | Enhancing comprehension for participants with intellectual disabilities or low literacy. |
| Capacity to Consent Assessment Tool | A validated, brief questionnaire to objectively assess a potential subject's understanding of key study elements. | The UBACC tool is used to determine if an individual with schizophrenia can consent for themselves. |
| Assent Document | A simplified document, written for the comprehension level of the individual, used to seek affirmative agreement from those who cannot give legal consent. | Obtaining agreement from a 10-year-old child to participate in a pediatric trial. |
| Witness to Consent Process | An impartial third party who observes the entire consent discussion and attests that the information was clearly presented and given voluntarily. | Ensuring the integrity of the consent process for non-literate participants or in settings with a perceived power imbalance (e.g., prison). |
| sIRB Reliance Agreement | A formal document that establishes the ceding of IRB review authority from a local IRB to a central sIRB for a specific study. | Standardizing the ethical oversight of a multi-site clinical trial for a rare disease in children. |
| Vulnerability-Specific SOP | A Standard Operating Procedure that details the extra steps and safeguards required for a specific vulnerable group. | An SOP for recruiting economically disadvantaged participants, detailing compensation fairness and transportation assistance. |
Application Notes: Integrating Core Ethical Principles into Research with Vulnerable Populations
The application of the four core ethical principles—autonomy, beneficence, non-maleficence, and justice—requires careful consideration and additional safeguards when research involves vulnerable populations. These principles provide a framework for ensuring that the informed consent process is both ethically sound and effective.
Table 1: Core Ethical Principles and Their Application to Informed Consent
| Ethical Principle | Definition | Application to Informed Consent for Vulnerable Populations |
|---|---|---|
| Autonomy | Respect for an individual's right to self-determination and decision-making [9] [10]. | The foundation for informed consent; requires ensuring genuine understanding and voluntary agreement, free from coercion [9] [11]. |
| Beneficence | The obligation to act for the benefit of others, promoting their welfare [9] [12]. | Requires that the research has a favorable risk-benefit ratio and offers a potential benefit to the participant or their community [9]. |
| Non-Maleficence | The duty to avoid or minimize harm [9] [10]. | Mandates the identification and mitigation of all foreseeable physical, psychological, social, and economic risks [9] [12]. |
| Justice | The duty to treat individuals equitably and fairly [9] [12]. | Requires the fair selection of research participants and ensuring that vulnerable groups are not unduly burdened nor unjustly excluded from the benefits of research [9] [13]. |
Engaging vulnerable populations in research necessitates moving beyond a one-size-fits-all consent form. A contextual and analytical approach is now recommended over a purely categorical one, which simply labels certain groups as vulnerable [13]. This involves a tailored assessment of the specific sources of vulnerability in a given research context. Key considerations include:
- Building Trust: In long-term studies, sustained relationships and recognizing participants’ intrinsic value are critical for genuine consent [14].
- Cultural Relevance: In some cultures, collective decision-making is the norm, and written consent may be perceived as a sign of mistrust. Guidelines must be adapted to local contexts [14].
- Comprehension: Language and literacy barriers, along with power imbalances, present significant challenges that can be mitigated by involving community members and trained interpreters, and by using tools like the "Teach Back Method" [11] [14].
Experimental Protocols for Ethical Consent
Protocol for Developing and Testing Culturally Relevant Consent Materials
Objective: To develop and validate informed consent materials that are accessible, understandable, and culturally appropriate for a specific vulnerable population.
Background: Standard consent forms often fail to account for cultural norms, varying health literacy levels, and diverse communication preferences, which can systematically exclude vulnerable groups from research [14]. This protocol uses a Design Thinking and Participatory Action Research (PAR) framework to create participant-centric solutions [14].
Methodology:
- Co-Development Workshop: Convene a panel including community representatives, cultural brokers, ethicists, and researchers to draft initial consent materials in plain language [14].
- Material Preparation: Create two versions of key consent "snippets" (paragraph-length sections):
- Original: An Institutional Review Board (IRB)-approved version.
- Modified: A version rewritten to improve readability by reducing character length and using less complex language [15].
- Participant Testing: Recruit eligible participants from the target population (N=79, for example) [15]. Present them with paired snippets and survey them on:
- Preference for original or modified text.
- Perceived clarity and comprehensiveness.
- Any new questions elicited by the content.
- Data Analysis:
- Quantitative: Use statistical tests (e.g., regression analysis) to determine if preferences are significantly influenced by text length, content topic (e.g., risks), or participant demographics (e.g., age, ethnicity) [15].
- Qualitative: Thematically analyze open-ended feedback to identify recurring concerns and information gaps [15] [14].
Expected Outcomes: Data-driven guidelines for consent form structure and wording tailored to the population. For instance, results may show that participants consistently prefer shorter text for explaining study risks and that consent materials effectively elicit informed questions from prospective participants [15].
Protocol for an Analytical Vulnerability Assessment
Objective: To systematically identify and mitigate context-specific vulnerabilities during the study design and consent process.
Background: Vulnerability is not inherent but can arise from individual circumstances or the research context itself [13] [16]. An analytical framework ensures appropriate, preventive, and respectful measures for all participants.
Methodology:
- Structured Assessment: Evaluate the research protocol against eight categories of vulnerability [16]:
- Cognitive/Communicative: Inability to process or understand consent information due to language, literacy, or mental capacity.
- Institutional: Subordination to a formal authority (e.g., prisoners, students).
- Deferential: Informal subordination (e.g., patient to doctor, spouse to spouse).
- Medical: Illness may cloud judgment or create undue influence.
- Economic: Payment may induce undue risk-taking.
- Social: Risk of discrimination based on race, gender, etc.
- Legal: Fear of legal repercussions from participation.
- Study-Induced: Vulnerability created by the study design (e.g., deception).
- Safeguard Implementation: For each identified vulnerability, document specific mitigation strategies in the research protocol. Examples include:
Diagram: Analytical Framework for Vulnerability and Safeguards in Research.
The Scientist's Toolkit: Essential Reagents for Ethical Research
Table 2: Research Reagent Solutions for Ethical Consent
| Item | Function in Ethical Research Protocol |
|---|---|
| Plain Language Guidelines | Provides rules for writing consent forms at an accessible reading level (e.g., 6th-8th grade), improving comprehension for all participants [15] [11]. |
| Readability Analysis Software | A tool (e.g., online readability calculator) to quantitatively assess and improve the readability of consent materials by analyzing character length, syllable count, and sentence structure [15]. |
| Multimedia Consent Resources | The use of videos, animations, or interactive websites to convey complex study information (e.g., data flows in digital health research), accommodating different learning preferences and literacy levels [14]. |
| Teach-Back Method Protocol | A structured communication technique where researchers ask participants to explain the study in their own words. This assesses and ensures true understanding, rather than mere signature acquisition [11] [14]. |
| Certificate of Confidentiality | A legal document issued by a public health agency (e.g., NIH in the U.S.) to protect participant privacy by shielding research data from forced disclosure in legal proceedings [16]. |
| Trained Interpreter Services | Professional interpreters (including for American Sign Language) are essential to overcome language barriers and ensure non-English speaking or hearing-impaired participants receive complete information [11]. |
The ethical enrollment of vulnerable populations in research necessitates a robust understanding of the foundational normative justifications for their protection and inclusion. The concept of vulnerability in research ethics, first formally introduced by the 1979 Belmont Report, serves as a critical mechanism to identify individuals or groups who require special protections to prevent harm and exploitation [13] [17]. Over time, scholarly and policy discourse has crystallized around three primary accounts that justify why a person is deemed vulnerable: consent-based, harm-based, and justice-based approaches [13].
These accounts are not merely theoretical; they directly inform regulatory guidelines and practical protocols for research involving human subjects. A systematic review of policy documents reveals a tendency to define vulnerability in close relation to the capacity for informed consent [13] [18]. This document synthesizes these normative justifications into structured application notes and experimental protocols, providing researchers, scientists, and drug development professionals with a framework for ethically sound and methodologically rigorous research involving vulnerable populations.
Theoretical Foundations and Policy Context
The evolution of vulnerability as an independent ethical principle is reflected in major international guidelines. The Declaration of Helsinki, for instance, has significantly refined its stance on vulnerability across its revisions. The 7th revision (2013) characterizes vulnerability as an "increased likelihood of being wronged or of incurring additional harm," a definition that aligns closely with harm-based accounts [19]. The latest 8th revision further emphasizes the context-dependent and dynamic nature of vulnerability, moving beyond static group labels to focus on situational factors [19].
Contemporary thought supports a shift from a "group-based notion" of vulnerability (the "labelling approach") to an "analytical approach" [13]. The former categorizes individuals as vulnerable based on group membership (e.g., children, prisoners), while the latter focuses on identifying the potential sources and conditions that create vulnerability within a specific research context [13]. The three normative accounts provide the analytical framework for this nuanced identification process.
Table 1: Core Accounts of Vulnerability in Research Ethics
| Normative Account | Core Justification for Vulnerability | Primary Ethical Principle | Common Policy Manifestations |
|---|---|---|---|
| Consent-Based | Compromised capacity to provide free, voluntary, and informed consent due to individual or situational factors [13]. | Respect for Autonomy | Requirements for surrogate decision-makers, enhanced consent processes, and assessment of decisional capacity [20] [21]. |
| Harm-Based | Increased probability of incurring physical, psychological, social, or economic harm during research [13] [19]. | Beneficence / Non-maleficence | Mandated additional safety monitoring, rigorous risk-benefit assessment, and implementation of specific protective measures [17]. |
| Justice-Based | Systemic inequalities and structural injustices that lead to unfair distribution of research burdens or exclusion from research benefits [13]. | Justice | Guidelines promoting equitable selection of participants, inclusion of underrepresented groups, and community engagement [20] [22]. |
Application Notes and Experimental Protocols
Protocol 1: Implementing a Multi-Layered Digital Informed Consent Process
Background: The i-CONSENT guidelines recommend tailoring the informed consent process to improve comprehension and accessibility for diverse populations, including vulnerable groups [23]. This protocol outlines a method for developing and testing electronic informed consent (eIC) materials, a key tool for addressing consent-based vulnerability.
Objective: To create and validate eIC materials that achieve high comprehension and satisfaction rates among vulnerable populations, thereby mitigating consent-based vulnerabilities.
Experimental Workflow:
Methodology:
- Define Target Population: Identify the specific vulnerable population (e.g., minors, pregnant women, adults with cognitive impairments) and the study context (e.g., a vaccine clinical trial) [23].
- Co-creation and Design:
- Convene a multidisciplinary team including clinicians, ethicists, and communication experts.
- Conduct participatory design sessions (e.g., design thinking workshops) with representatives from the target population to gather input on content, format, and usability [23].
- Multi-format Development: Develop eIC materials in multiple, accessible formats to cater to different preferences and cognitive styles. Offer a combination of:
- Layered Web Content: A modular website allowing users to click for more detailed information [23].
- Narrative Videos: Use storytelling or question-and-answer formats to explain key concepts [23].
- Printable Documents: Text-based materials with integrated images and clear formatting [23].
- Customized Infographics: Visual representations of procedures, risks, and rights [23].
- Professional Translation and Cultural Adaptation: For multinational trials, translate materials professionally and adapt content to ensure cultural and contextual appropriateness [23].
- Cross-Cultural Implementation: Deploy the validated materials across different countries and settings, using a secure digital platform.
- Comprehension Assessment:
- Satisfaction Evaluation: Assess participant satisfaction using Likert scales and usability questions, with scores ≥80% considered acceptable [23].
- Data Analysis and Refinement: Use multivariable regression models to identify predictors of comprehension (e.g., gender, education, prior trial experience). Refine materials based on quantitative and qualitative feedback [23].
Key Outcomes: A study implementing this protocol with 1,757 participants across three countries demonstrated high objective comprehension (mean scores >82%) and satisfaction rates (exceeding 97%) among minors, pregnant women, and adults [23].
Protocol 2: Ethical Inclusion of Adults Lacking Decisional Capacity
Background: Adults with cognitive impairments are often excluded from clinical research due to challenges in obtaining informed consent, creating a justice-based vulnerability through underrepresentation and a lack of treatment options for their population [21]. This protocol provides a framework for their ethical inclusion.
Objective: To enroll adults who lack the capacity to provide independent informed consent into clinical trials while upholding ethical principles through robust surrogate decision-making and additional safeguards.
Ethical Enrollment Workflow:
Methodology:
- Protocol Review by IRB/REC: The research protocol must receive approval from an Institutional Review Board or Research Ethics Committee, which must verify that the inclusion of adults lacking capacity is scientifically justified and that all additional safeguards are in place [20] [17].
- Capacity Assessment: Implement a standardized and validated tool to assess the potential participant’s capacity to understand the research information and make an independent decision [21].
- Appoint a Legally Authorized Representative (LAR): If capacity is lacking, identify a surrogate decision-maker (LAR) as defined by local law and regulation to make decisions on the participant's behalf [20] [21].
- Surrogate Informed Consent Process: The investigator must provide the LAR with all relevant study information. The LAR must then provide informed consent based on their knowledge of the participant's preferences and best interests [20].
- Participant Assent: Even if formal consent is provided by the LAR, the potential participant must be included in the process to the greatest extent possible. Their willingness to participate (assent) should be sought, and any objection or sign of distress must be respected [20].
- Ongoing Monitoring and Communication: The consent process is continuous. The research team must maintain communication with both the participant and the LAR throughout the study, providing updates and reaffirming agreement, especially if the participant's condition or the study risks change [24].
- Re-consent if Capacity Returns: If the participant's decisional capacity improves, the researcher must seek direct informed consent from the participant for continued participation [24].
The Scientist's Toolkit: Essential Reagents for Ethical Research
Table 2: Key Research Reagent Solutions for Vulnerability and Consent Studies
| Item/Tool | Function/Brief Explanation | Exemplary Use Case |
|---|---|---|
| Adapted QuIC Questionnaire | A validated tool to quantitatively measure objective and subjective comprehension of informed consent information [23]. | Core outcome measure in Protocol 1 to validate the efficacy of eIC materials [23]. |
| Digital Consent Platform | A secure software platform to host and deliver layered eIC materials (videos, text, infographics) and record participant engagement [23]. | Deployment vehicle for multi-format consent materials in multinational trials [23]. |
| Decisional Capacity Assessment Tool | A standardized instrument (e.g., MacArthur Competence Assessment Tool for Clinical Research) to evaluate a person's ability to understand, appreciate, and reason about research participation [21]. | Critical for Protocol 2 to determine the need for surrogate decision-making [21]. |
| Community Advisory Board (CAB) | A group of community stakeholders and patient advocates that provides input on trial design, recruitment strategies, and consent materials to ensure cultural and ethical acceptability [20]. | Addresses justice-based vulnerability by ensuring research aligns with community needs and builds trust [20] [22]. |
| IRB/REC Vulnerability Checklist | A checklist derived from policy guidelines to systematically identify potential sources of consent-, harm-, and justice-based vulnerability in a study protocol [13] [17]. | Used by ethics committees and researchers during study design and review to ensure adequate safeguards [13]. |
The consent-based, harm-based, and justice-based accounts of vulnerability provide a complementary, rather than mutually exclusive, framework for protecting and including vulnerable populations in research. The consent-based account directly tackles the challenge of ensuring autonomy when capacity or freedom is compromised, leading to practical solutions like the eIC protocols and surrogate decision-making outlined above [13] [23] [21]. The harm-based account compels researchers and ethics committees to conduct a more nuanced risk-benefit analysis, recognizing that the same research procedure may pose a higher risk to some individuals or groups, thus necessitating additional monitoring and safeguards [13] [19]. Finally, the justice-based account critiques the historical exclusion of vulnerable groups, arguing that it perpetuates health disparities by generating evidence that does not apply to all patients [13] [20]. This justification drives policies that mandate the equitable inclusion of these populations.
A sophisticated understanding of these justifications is crucial for modern drug development professionals. Regulatory bodies like the FDA and EMA encourage the involvement of multiple stakeholders—including patients, industry, and academia—early in clinical trial design to address these very issues [20]. The WHO's guidance on best practices for clinical trials further underscores the global imperative to "ensure ethical standards, particularly regarding informed consent, protection of vulnerable populations, and risk-benefit analysis" [22]. By systematically applying the principles and protocols described in this document, researchers can navigate the complex ethical landscape of vulnerability, advancing scientific knowledge while steadfastly upholding the rights and welfare of all research participants.
Application Note: Policy Landscape and Quantitative Synthesis
Background and Context
The ethical conduct of research with human subjects necessitates special protections for vulnerable populations to ensure equitable participation and prevent exploitation. This application note synthesizes findings from a systematic review of policy documents to elucidate how vulnerability is conceptualized, classified, and operationalized within research ethics frameworks, with particular relevance to the informed consent process [13]. The historical foundation for this discourse was established by The Belmont Report (1979), which first formally identified "vulnerable people" as those in a "dependent state and with a frequently compromised capacity to free consent" [13]. A significant challenge in this domain is balancing the imperative to protect potentially vulnerable individuals from research-related harms with the parallel need to ensure their equitable access to research benefits and participation, thereby preventing their underrepresentation in scientific advancement [13] [25].
Quantitative Synthesis of Policy Document Classifications
Analysis of 79 policy documents included in the 2025 systematic review reveals distinct patterns in the classification of vulnerable groups and the normative justifications provided for these classifications [13] [26]. The following tables synthesize the quantitative findings from this analysis, providing a structured overview for researchers and ethics committees.
Table 1: Prevalence of Vulnerable Group Classifications in Policy Documents (n=79)
| Vulnerable Population Category | Frequency of Identification | Primary Ethical Concern |
|---|---|---|
| Minors/Children | High | Inability to provide legally binding informed consent; reliance on parental permission and assent processes [27] [25]. |
| Individuals with Cognitive/Intellectual Disabilities | High | Diminished capacity to understand research participation and provide informed consent; reliance on legally authorized representatives [13] [25]. |
| Prisoners | High | Compromised free consent due to institutional dependency and potential for undue influence [13]. |
| The Very Sick or Terminally Ill | High | Potential vulnerability due to therapeutic misconception and heightened hope for benefit when no other treatment options exist [13]. |
| Economically or Educationally Disadvantaged | Medium | Potential for undue influence due to perceived financial or other benefits [13]. |
| Pregnant Women | Medium | Complexities involving the welfare of both the woman and the fetus [13]. |
| Elderly with Frailty or Dementia | Medium | Fluctuating or impaired decision-making capacity, requiring tailored consent processes like process consent [25]. |
| Refugees and Internally Displaced Persons | Emerging | Vulnerability due to legal status, language barriers, and potential trauma [25]. |
Table 2: Normative Justifications for Vulnerability in Research Ethics
| Justification Framework | Core Principle | Operational Focus in Policy Documents |
|---|---|---|
| Consent-Based Accounts | Respect for Autonomy | Focuses on a participant's compromised capacity to provide voluntary, informed, and comprehending consent due to internal (e.g., cognitive state) or external (e.g., undue influence) factors [13] [27]. |
| Harm-Based Accounts | Beneficence and Non-Maleficence | Defines vulnerability as a heightened probability of incurring harm or injury during research, necessitating enhanced risk-benefit assessments [13]. |
| Justice-Based Accounts | Justice | Identifies vulnerability as arising from systemic inequalities and social marginalization that create unfair burdens or limit access to research benefits [13]. |
Protocol for Systematic Analysis of Policy Classifications
Experimental Workflow and Methodology
The following protocol outlines a detailed methodology for systematically identifying, analyzing, and synthesizing policy document classifications of vulnerable populations, replicating and extending the approach of the foundational 2025 systematic review [13].
Figure 1: Systematic review workflow for policy analysis.
Reagent and Resource Solutions for Policy Analysis
Table 3: Research Reagent Solutions for Systematic Policy Review
| Item/Tool | Function/Application | Specification/Example |
|---|---|---|
| PRISMA-Ethics Guideline | Provides a structured framework for conducting and reporting systematic reviews in research ethics, ensuring methodological rigor [13]. | Used to define the protocol, search strategy, and reporting standards. |
| QUAGOL Methodology | Guides the qualitative data analysis and synthesis process for policy document content, moving from summarization to conceptual scheme creation [13] [26]. | Applied during data extraction to develop summaries and identify key themes. |
| International Compilation of Human Research Standards | Serves as a primary source list for identifying relevant national and international policy documents for inclusion [13]. | 2024 Edition; ensures comprehensive coverage of global standards. |
| Structured Data Extraction Form | A standardized tool (digital or manual) for capturing consistent data points from each policy document. | Fields for: document name, year, vulnerable groups listed, definition of vulnerability, provisions, and normative justification. |
| Reference Management Software | Essential for organizing identified documents, managing citations, and facilitating the screening process. | Tools like Zotero, EndNote, or Mendeley. |
Conceptual Framework for Analytical Approaches
The systematic review identifies two predominant conceptual approaches to vulnerability that underpin policy document classifications, each with distinct implications for the informed consent process [13] [25].
Figure 2: Conceptual models for vulnerability classification.
Operational Protocol for Consent Process with Vulnerable Populations
Building on the synthesized classifications, this protocol provides actionable steps for integrating vulnerability assessments and appropriate safeguards into the informed consent process for clinical trials and research studies.
Table 4: Operational Protocol for Informed Consent with Vulnerable Populations
| Protocol Step | Detailed Procedure | Rationale & Regulatory Reference |
|---|---|---|
| 1. Pre-Study Vulnerability Assessment | - Identify which, if any, pre-defined vulnerable groups are likely to be enrolled.- Conduct a context-specific analysis of potential sources of vulnerability (e.g., power imbalances, economic dependency, cognitive state) [25]. | Shifts from a purely labels-based to a layers-based approach, ensuring tailored protections. Required by most international guidelines and Ethics Committee (EC) submissions [13] [25]. |
| 2. Protocol & Consent Form Development | - Justify the scientific necessity of including vulnerable participants.- Describe all specific safeguards in the research protocol.- Adapt the Informed Consent Form (ICF) language to be understandable (non-technical) and the process to be accessible [27]. | Adheres to ICH GCP E6 principles and the Declaration of Helsinki. Ensures information is comprehensible to the participant or their legal representative [27]. |
| 3. Ethics Committee Review & Approval | - Submit the full protocol, adapted ICF, and participant information materials.- Obtain explicit EC approval for the inclusion of participants who cannot give personal consent (e.g., for non-therapeutic research) [27]. | Mandatory under ICH GCP. EC must expressly approve this aspect, especially for research with no direct benefit [27]. |
| 4. Participant-Level Consent Process | For capable adults: Conduct the standard informed consent process, ensuring voluntariness and absence of undue influence.For those with limited capacity (e.g., dementia): Implement a "process consent" approach, involving ongoing consent discussions and capacity reassessment throughout the study [25].For minors: Obtain parental/legal representative permission and seek the child's assent (affirmative agreement) appropriate to their developmental stage [27] [25].For illiterate participants: Use an impartial witness during the entire informed consent discussion. The witness attests to the integrity of the process [27]. | Respects the principle of autonomy in a manner proportionate to the individual's capacity. Process consent acknowledges the fluctuating nature of capacity in some conditions. Assent respects the developing autonomy of the child [25]. |
| 5. Documentation & Monitoring | - Ensure the ICF is signed and dated by the participant or their legal representative before any trial procedures.- Provide a copy of the signed ICF to the participant/representative.- Monitor the consent process and participant well-being throughout the trial, re-consenting if new relevant information emerges [27]. | Documentary requirement per ICH GCP E6. Ongoing monitoring ensures continued willingness and upholds the ethical principle of respect for persons. |
This structured application note and protocol set provides researchers, scientists, and drug development professionals with a synthesized evidence base and actionable framework for ethically engaging vulnerable populations in research, with a specific focus on implementing a robust and tailored informed consent process.
Adapting Consent Processes: Practical Strategies for Diverse Vulnerable Groups
The process of obtaining genuine informed consent is a cornerstone of ethical research, particularly when working with vulnerable populations. Traditional consent models, often developed within Western paradigms, can be extractive and fail to account for cultural nuances, language barriers, and power dynamics. This creates a significant risk of participation without full comprehension. A shift towards culturally relevant consent is therefore not merely an ethical nicety, but a fundamental requirement for equitable and valid research. This document provides application notes and protocols for integrating these principles into research involving vulnerable populations, drawing on recent empirical studies.
Quantitative Insights: The Impact of Barriers and Interventions
Data underscores systemic deficiencies in standard consent processes for linguistically diverse and vulnerable groups, while also quantifying the benefits of targeted interventions.
Table 1: Language Barriers and Documentation of Informed Consent
| Population Group | Rate of Fully Documented Consent | Statistical Significance (p-value) | Key Finding |
|---|---|---|---|
| English-Speaking Patients | 53% | 0.003 | Baseline for comparison [28] |
| Patients with Limited English Proficiency (LEP) | 28% | LEP patients were 3.1 times less likely to have fully documented consent, even with on-site interpreters available [28] |
Table 2: Efficacy of an Interpreter Access Intervention
| Metric | Pre-Intervention (LEP Patients) | Post-Intervention (LEP Patients) | English-Speaking Patients (Post) |
|---|---|---|---|
| Adequate Informed Consent Rate | 29% | 54% | 74% |
| 30-Day Hospital Readmission Rate | 17.8% | 13.4% | Increased slightly [29] |
| Intervention | Standard interpreter access | Dual-handset interpreter phones at every bedside with 24/7 access to professional interpreters [29] | Not applicable |
Experimental Protocols for Culturally Relevant Consent
The following protocols provide actionable methodologies for designing and implementing a culturally competent consent process.
Protocol: Co-Developing Consent Materials with Communities
This protocol, based on Participatory Action Research (PAR) and Design Thinking frameworks, ensures consent processes are shaped by the communities they are intended to serve [14].
- Objective: To collaboratively create informed consent guidelines and materials that are culturally relevant, accessible, and trustworthy from the perspective of the target population.
- Materials:
- Recruitment materials co-designed with community gatekeepers.
- Venues that are neutral, accessible, and comfortable for participants.
- Audio recording equipment and secure data storage.
- Materials for participatory activities (e.g., large paper, markers).
- Procedure:
- Establish Partnerships: Identify and engage with Community Advisory Boards (CABs), local leaders, and relevant community-based organizations from the inception of the research [30].
- Participant Recruitment: Purposively sample a diverse group of stakeholders, including former research participants, CAB members, and community members representing different demographics (e.g., age, gender, nationality) and, if applicable, different language groups and literacy levels [14] [30].
- Facilitate Focus Group Discussions (FGDs): Conduct FGDs segregated by factors like age and sex to encourage open dialogue. Use open-ended questions to explore:
- Perceived motivations for and barriers to research participation.
- Experiences with and preferences for communication (oral vs. written).
- Trusted sources of information and entities.
- Understanding of core consent concepts (e.g., voluntary participation, right to withdraw).
- Specific feedback on the language and clarity of draft consent materials [14] [30].
- Iterative Material Design: Use insights from FGDs to create simplified consent forms and alternative aids (e.g., pictorial guides, audio recordings). Present these drafts back to focus groups for further feedback in a continuous cycle of refinement [14].
- Community Validation Workshops: Present the finalized guidelines and materials to a broader group of community stakeholders to confirm their acceptability and relevance [30].
- Data Analysis: Transcribe and analyze data using an inductive thematic approach to identify key barriers and facilitators [14].
The workflow for establishing an effective consent process is outlined below.
Protocol: Implementing the Consent Process with Linguistic Justice
This protocol operationalizes the co-developed materials, focusing on overcoming language and literacy barriers during the actual consent interaction.
- Objective: To ensure that every potential participant genuinely understands the research information, regardless of their language proficiency or literacy level.
- Materials:
- Finalized consent materials in all relevant languages and formats.
- Access to trained professional interpreters (in-person or via dual-handset phones). Do not use ad-hoc interpreters like family members [29].
- Audio-visual aids (e.g., short explanatory videos, diagrams).
- Procedure:
- Pre-Consent Preparation: Identify the participant's primary language and preferred mode of communication ahead of the meeting. Secure a trained interpreter who is also skilled in cultural mediation [14] [30].
- Environment Setting: Conduct the consent conversation in a private, comfortable setting. Allocate sufficient time without rushing. Introduce the interpreter and explain their role to all parties.
- Interactive Information Sharing:
- Assessing Understanding with the Teach-Back Method: After explaining a key concept (e.g., voluntary participation, risks), ask the participant to explain it back in their own words. This is not a test of the participant, but of the researcher's ability to communicate clearly. Correct any misunderstandings and re-explain as needed [14].
- Documenting the Process: For participants with LEP, document in the consent form that the discussion was conducted in their primary language with the assistance of a qualified interpreter. Include the interpreter's name and signature on the form [28].
- Reaffirming Consent: Treat consent as an ongoing process, not a one-time event. Recheck understanding and willingness to continue at key points throughout the research study [14].
The Scientist's Toolkit: Essential Reagents for Ethical Consent
This table details key resources required to implement a culturally relevant consent process effectively.
Table 3: Research Reagent Solutions for Ethical Consent
| Item | Function & Rationale |
|---|---|
| Community Advisory Board (CAB) | A group of community stakeholders that provides ongoing input on study design, consent materials, and recruitment strategies to ensure cultural and ethical appropriateness [30]. |
| Professional Interpreters | Trained linguists who provide accurate translation and cultural mediation. Essential for ensuring LEP participants receive identical information to English-speaking participants. Dual-handset phones provide immediate access [28] [29]. |
| Multi-Format Consent Tools | Consent information presented in various formats (e.g., short videos, pictorial flowcharts, audio recordings) to accommodate different literacy levels and learning preferences [14]. |
| Plain Language Guides | Documents that replace complex scientific and legal jargon with simple, clear terminology that is easily understood and can be accurately translated into local languages [30]. |
| Teach-Back Method Protocol | A structured method for assessing participant comprehension by asking them to explain the study back to the researcher, ensuring understanding is genuine and not assumed [14]. |
The relationships and workflow between these key tools and the desired outcomes are visualized below.
Electronic informed consent (eConsent) utilizes digital media—such as text, graphics, audio, video, and interactive websites—to convey study information and obtain consent via electronic devices [31]. A systematic review of 35 studies demonstrates that eConsent can significantly improve participant comprehension of clinical trial information, enhance engagement with content, and is rated as more acceptable and usable compared to traditional paper-based consenting [32]. For research involving vulnerable populations, eConsent offers unique opportunities to overcome barriers such as distrust, health literacy challenges, and logistical difficulties in accessing research opportunities [33] [34]. This application note provides detailed protocols and evidence-based recommendations for the effective implementation of eConsent, with a specific focus on enhancing understanding and equity in research participation.
Informed consent is a cornerstone of ethical clinical research. However, traditional paper-based consent processes present significant challenges, particularly for vulnerable and underrepresented populations. These challenges include lengthy and complex forms, difficulties in maintaining understanding, and logistical barriers to participation [33] [32].
eConsent represents a paradigm shift, moving beyond mere digitization of paper forms to a dynamic, participant-centered process. It incorporates multimedia, interactive elements, and accessibility features to make consent information more understandable and engaging [34] [35]. For vulnerable populations—including low-income individuals, racial and ethnic minorities, and those with cognitive or health challenges—eConsent can mitigate known recruitment barriers such as distrust of the research community, lack of awareness about medical research, and concerns over privacy and confidentiality [33].
The COVID-19 pandemic accelerated the adoption of remote and decentralized clinical trial methods, with eConsent playing a pivotal role [31] [36]. Research indicates that compared to paper-based consent, eConsent leads to a better understanding of clinical trial information, greater engagement with content, and higher ratings of acceptability and usability among participants [32]. Furthermore, fully electronic consent collection has been shown to significantly increase the initial validity of consent forms from 67.38% to 99.46%, thereby improving patient inclusion rates and data quality [37].
Quantitative Evidence: Comparative Effectiveness of eConsent
The following tables summarize key quantitative findings from comparative studies and systematic reviews on the effectiveness of eConsent versus traditional paper-based methods.
Table 1: Impact of eConsent on Key Participant Outcomes [32]
| Outcome Measure | Number of Assessing Studies | Findings from "High Validity" Studies | Significance |
|---|---|---|---|
| Comprehension | 20 out of 35 (57%) | 6 studies reported significantly better understanding of at least some concepts with eConsent | ( P < .05 ) |
| Acceptability | 8 out of 35 (23%) | 1 study reported statistically significant higher satisfaction scores with eConsent | ( P < .05 ) |
| Usability | 5 out of 35 (14%) | 1 study reported statistically significant higher usability scores with eConsent | ( P < .05 ) |
| Cycle Time | Reported in multiple studies | Increased time spent with eConsent content, reflecting greater participant engagement | Not Significant |
Table 2: Operational and Quality Impacts of eConsent Implementation [37] [38]
| Metric | Paper-Based Consent | Tablet-Based eConsent | Context & Implications |
|---|---|---|---|
| Initial CF Validity | 67.38% | 99.46% | Based on a COVID-19 cohort study (n=2,753); higher validity reduces need for re-consenting and data loss [37]. |
| Patient Satisfaction | Baseline | 96% rated video satisfactory; 94% rated quiz satisfactory | Janssen pilot study (n=76); features enhanced understanding and engagement [38]. |
| Site Staff Feedback | Baseline | 77% reported eConsent improved the entire consent process; 69% noted improved patient engagement | Janssen pilot study; staff observed process enhancements despite variable impact on time [38]. |
| Older Adult Adaptation | N/A | High satisfaction and "easy" to "very easy" use, despite low prior tablet experience (27%) | Demonstrates acceptability across age groups and digital literacy levels [38]. |
Experimental Protocols and Workflows
Core Protocol for Remote eConsent Implementation
This protocol is adapted from successful implementations at UK Clinical Trials Units using the REDCap platform, which can be applied to studies involving vulnerable populations [31] [36].
Objective: To obtain informed consent from participants remotely using an electronic system, ensuring regulatory compliance, maintaining data integrity, and enhancing participant understanding.
Materials:
- REDCap Software Platform: A secure, web-based application for building and managing online surveys and databases. No-cost options are available for academic research [36].
- Communication Tools: Telephone or video conferencing software for initial discussion and identity verification.
- Device with Internet Access: For the participant to access the eConsent system.
Procedure:
- Pre-Consent Discussion and Information Provision:
- A researcher introduces the study to the potential participant via phone or video call.
- The researcher explains the option of eConsent and confirms the participant's interest and access to a suitable device.
- The Participant Information Sheet (PIS) is sent to the participant electronically (e.g., via email) or by post, allowing time for review.
Verbal Consent for Data Processing:
- Before any confidential information is entered into the eConsent system, the researcher obtains verbal consent from the participant for the processing of their personal data as required by data protection regulations (e.g., GDPR) [36].
Identity Verification:
- The researcher verifies the participant's identity. This can be done visually on a video call, by checking basic identifiers (name, date of birth), or in-person at a subsequent visit before any study intervention is administered [36].
System Access and Electronic Consent:
- The researcher sends a unique link to the REDCap eConsent form via email.
- The participant opens the link and reviews the electronic Consent Form (eICF), which may include embedded multimedia (videos, audio clips) and interactive knowledge checks.
- The participant provides their electronic signature. Per regulatory guidance, this can be a simple electronic signature (e.g., a typed name) for many research contexts, provided it is unique to the signer and linked to the record [39].
Documentation and Copy Provision:
- The completed eICF is locked in the system, generating an audit trail.
- A copy of the signed eICF is automatically emailed to the participant for their records.
Workflow Diagram: Remote eConsent Process
The diagram below illustrates the sequential and parallel steps in a standardized remote eConsent process, highlighting the roles of both research staff and participants.
The Scientist's Toolkit: Essential Reagents and Materials for eConsent
Table 3: Research Reagent Solutions for eConsent Implementation
| Item / Solution | Function / Purpose in eConsent | Example & Notes |
|---|---|---|
| eConsent Platform | Core software for creating, delivering, and managing electronic consent forms. | REDCap: A widely used, secure, no-cost platform for academic research with a built-in eConsent module [31] [36]. Commercial platforms also exist. |
| Multimedia Components | To enhance comprehension and engagement by presenting information in multiple formats. | Instructional Videos: Explain key study concepts [38]. Interactive Diagrams: Illustrate study design. Audio Narration: Supports low literacy. |
| Interactive Comprehension Checks | To assess and reinforce participant understanding of key study elements during the consent process. | Embedded Quizzes: Multiple-choice questions on risks, procedures, and rights [38]. Feedback is provided for incorrect answers. |
| Electronic Signature Solution | To capture a legally valid signature electronically. | Platforms like DocuSign or built-in tools in REDCap. Must meet regulatory requirements for intent and attribution [39]. |
| Accessibility Features | To ensure the eConsent process is inclusive for participants with diverse abilities and language preferences. | Screen Reader Compatibility, Variable Font Sizes, Multiple Language Options [34] [36]. |
| Identity Verification Protocol | To confirm the identity of the participant providing remote consent, as per regulator guidance [36]. | Process may involve video call confirmation, checking government-issued ID, or asking security questions (e.g., mother's maiden name) [39] [36]. |
Adaptation for Vulnerable Populations: Tailoring the Protocol
A one-size-fits-all approach is insufficient for vulnerable groups. Tailoring the eConsent process is critical for ethical and effective implementation.
Addressing Distrust and Building Rapport: Leverage trusted community settings and staff. Research in Community Health Centers (CHCs) shows that alignment between study aims and CHC goals, combined with trusted relationships between CHC staff and patients, is a key facilitator of successful recruitment and consent [33]. eConsent platforms can be deployed within these trusted environments.
Tailoring for Health Literacy and Cognition: Utilize multimedia and interactive features to simplify complex information. Data shows that participants with conditions like schizophrenia may show high engagement but require more time, while those with ADHD may score lower on knowledge checks, necessitating tailored support and content presentation [40]. Features like a built-in dictionary or the ability to flag unfamiliar words can significantly aid understanding [38].
Ensuring Technological Accessibility: Provide technical support and alternative options. For populations with limited technology access or proficiency, offer in-center support at CHCs or the continued option of paper-based consent. A hybrid model ensures inclusivity and does not exclude those who are less digitally literate [34] [36].
The implementation of eConsent represents a significant advancement in the ethical conduct of research, particularly for vulnerable populations. By enhancing comprehension, engagement, and accessibility, eConsent can help overcome longstanding barriers to the equitable inclusion of these groups in research. The protocols and evidence presented herein provide a framework for researchers to design and implement eConsent processes that are not only compliant with regulatory standards but are also truly participant-centered.
Future developments should focus on creating more adaptive and intelligent eConsent systems that can dynamically tailor content based on a participant's real-time comprehension and preferences. Continued collaboration with patients, community stakeholders, ethics committees, and regulators is essential to ensure that the promise of eConsent is fully realized, making research participation a more informed, understandable, and accessible endeavor for all.
Within the broader context of safeguarding autonomy in vulnerable populations research, the informed consent process presents unique challenges. Traditional written consent forms can create barriers related to literacy, language, culture, and disability [41]. Oral consent—also referred to as verbal consent—emerges as a critical ethical alternative, shifting the focus from a signature on a document to a meaningful, participatory dialogue [42] [43].
This protocol details the design and documentation of rigorous oral consent processes tailored for research involving vulnerable populations. It provides application notes to ensure these processes meet ethical and regulatory standards while respecting the circumstances of the participants.
Regulatory and Ethical Framework
Oral consent is recognized as an ethically valid alternative to written consent in multiple regulatory contexts. The Canadian Institutes of Health Research, for instance, acknowledges it as an ethically equivalent option, particularly when documented adequately [42]. In the United States, the Federal Regulations (45 CFR 46) allow an Institutional Review Board (IRB) to waive the requirement for signed consent in two primary scenarios [44]:
- When the research presents no more than minimal risk and involves procedures that would not normally require written consent outside of a research context.
- When the only record linking the subject to the research would be the consent form, and a breach of confidentiality would be the principal risk to the subject.
For research that is determined to be exempt from the full federal regulations, a consent discussion may be sufficient without a formal signature [44]. It is critical to note that for studies reviewed at a full board level because they involve more than minimal risk, a signed consent form is typically required [44]. The foundational ethical principle, as stated in the Nuremberg Code, is that "the voluntary consent of the human subject is essential," emphasizing comprehension and free power of choice over the medium of documentation [43].
Table 1: Regulatory Thresholds for Oral Consent
| Review Level / Risk Category | Signed Consent Typically Required? | Basis for Waiver or Alternative |
|---|---|---|
| Exempt Research | No | A formal signature is not required by regulation [44]. |
| Expedited Review (Minimal Risk) | Can be waived | If the research is minimal risk and a signature is the main confidentiality risk, or if procedures normally don't require written consent [44]. |
| Full Board Review (>Minimal Risk) | Yes | Generally required; waiver is not typical [44]. |
Designing the Oral Consent Process
A valid oral consent process is not merely the reading of a script, but a comprehensive, interactive dialogue designed to ensure true understanding.
Core Information Elements
The information disclosed must be comprehensive and delivered in a manner that is easily understandable. The goal is to facilitate an "understanding and enlightened decision" [43]. Essential elements include [45] [43]:
- Purpose of the research: A clear statement of the study's aims.
- Procedures and duration: A description of all research activities, their frequency, and the total expected time commitment.
- Risks and discomforts: A frank discussion of any potential physical, psychological, social, or economic harms.
- Potential benefits: A realistic explanation of any direct benefits to the participant or to society.
- Alternatives to participation: For interventional research, the alternatives available outside the study.
- Confidentiality: Precise details on how data will be handled, stored, protected, and eventually destroyed, and who will have access.
- Voluntary participation and right to withdraw: An explicit statement that participation is voluntary and that the participant may withdraw at any time without penalty or loss of benefits to which they are otherwise entitled [45].
- Compensation: If applicable, details of any compensation for participation.
- Contact information: Who to contact for study-related questions and for questions about participants' rights.
Readability and Comprehension
All information must be presented at an appropriate comprehension level. For the general public, it is considered best practice to aim for an 8th-grade reading level [43]. Tools like the Flesch-Kincaid Grade Level formula can help assess readability, focusing on sentence length and word complexity [43]. The language should be conversational and free of exculpatory language that waives or appears to waive any of the participant's legal rights [43].
Documenting the Oral Consent Process
Adequate documentation is mandatory to provide an audit trail and verify that the ethical process occurred. This documentation substitutes for the participant's signature and must be approved by an IRB or Research Ethics Board (REB) [42] [44].
Table 2: Methods for Documenting Oral Consent
| Documentation Method | Description | Best Use Cases |
|---|---|---|
| Written Summary by Researcher | The researcher creates detailed notes in the participant's file or a study log, confirming that the consent discussion took place and that the participant agreed. | All research contexts, providing a standard and verifiable record. |
| Audio Recording | The entire consent conversation is recorded with the participant's explicit permission. | Complex studies where a verbatim record is valuable; requires robust data privacy plans [44]. |
| IRB-Approved Consent Script | A precise script, pre-approved by the REB/IRB, is used to guide the discussion. The researcher notes the participant's agreement. | Telephone interviews or standardized minimal-risk studies [42] [44]. |
| Study Information Sheet | A written document containing all consent elements is provided to the participant. The subsequent oral discussion is documented, but the participant does not sign the sheet [44]. | When providing written information is beneficial, but collecting a signature is inadvisable due to confidentiality concerns. |
The following diagram illustrates the relationship between the core consent elements, the interactive process, and the resulting documentation.
The Researcher's Toolkit: Essential Materials for Implementation
Successfully implementing an oral consent process requires specific materials and tools, which should be prepared and approved prior to participant recruitment.
Table 3: Essential Research Reagents and Tools for Oral Consent
| Tool / Reagent | Function | Application Notes |
|---|---|---|
| IRB-Approved Consent Script | Ensures consistent and complete disclosure of all required information to every participant. | Scripts should be tested for readability and comprehension with a sample audience representative of the study population. |
| Oral Consent Card | A brief, portable aid listing key discussion points to ensure all consent elements are covered verbally [44]. | Particularly useful in anthropological or field-based research to maintain procedural rigor without formal written documents. |
| Documentation Form (for researcher) | A standardized template for the researcher to record the date, time, and method of consent, and the participant's agreement. | This form is part of the study's essential documents and is stored separately from the raw data to maintain confidentiality. |
| Audio Recorder | To create a verbatim record of the consent dialogue. | Must be used only with explicit participant consent for this specific procedure. Requires a secure data storage and encryption plan. |
| Visual Aids & Supplementary Materials | To explain complex study procedures, timelines, or concepts in simple, visual terms [43]. | Enhances understanding, especially for participants with lower literacy or in cross-cultural contexts. |
| Readability Assessment Tool | Software or formula (e.g., Flesch-Kincaid) to verify that all language is at an appropriate comprehension level [43]. | A critical step in the development phase of all consent materials, including scripts and information sheets. |
Special Considerations for Vulnerable Populations
The oral consent process must be adapted with additional safeguards when working with vulnerable groups. Vulnerable populations are defined as disadvantaged community subgroups unable to make informed choices, protect themselves from risks, or safeguard their own interests [45]. This includes individuals with physical, psychological, or social vulnerabilities [45].
- Non-Literate or Non-Native Language Speakers: For participants who cannot read the local language, the entire process must be oral. A third-party witness should be present during the consent discussion to verify that the information was fully explained and that the participant's consent was voluntary and informed [41]. The witness should not be a member of the research team.
- Children and Minors: For pediatric research, the process involves both parental permission and the child's assent. The assent should be obtained orally from the child using age-appropriate language. For research categorized as greater than minimal risk with no direct benefit (Category 3), regulations may require permission from both parents [41].
- Individuals in Hierarchical Relationships: When recruiting students, employees, or prisoners, special care must be taken to avoid coercion. The individual inviting participation should not be in a position of authority (e.g., a professor should not directly recruit their own students) [41] [45]. Consent must be obtained by an independent team member, and it must be explicitly stated that participation or non-participation will not affect grades, employment status, or privileges [41].
The following workflow provides a visual guide to implementing a rigorous oral consent process, incorporating key decision points and safeguards.
A well-designed and meticulously documented oral consent process is a powerful tool for conducting ethical research with vulnerable populations. By prioritizing a meaningful dialogue over a procedural signature, researchers can foster trust, enhance understanding, and truly respect the autonomy of participants. This protocol provides a framework for integrating oral consent into research practice, ensuring it meets the highest standards of ethical rigor and regulatory compliance.
Obtaining truly informed consent from participants is a cornerstone of ethical clinical research. This process requires more than just delivering information; it demands confirming that the participant has understood the key details of the study, including its purpose, procedures, risks, and benefits. This is particularly critical when working with vulnerable populations, who may face additional barriers to comprehension due to factors such as health literacy, cognitive impairment, or situational stress. This document outlines a structured approach to assessing comprehension, combining the evidence-based Teach-Back method with modern interactive tools to ensure participants are not just informed, but also comprehending.
Core Methodology: The Teach-Back Method
The Teach-Back method is a simple, quick, and effective technique used to confirm a person's understanding of information that has been explained to them. It is not a test of the participant, but rather a check on how well the researcher has explained the concepts [46].
Definition and Purpose
- What it is: A closed-loop communication method where a researcher asks a participant to explain in their own words what they have just been told.
- What it is not: A test of the participant's intelligence or memory. It is a quality check on the researcher's ability to provide clear information.
- Primary Objective: To identify and immediately clarify any misconceptions or gaps in understanding regarding the informed consent process.
Detailed Experimental Protocol
Implementing the Teach-Back method effectively requires a structured yet empathetic approach. The following workflow outlines the key steps from initiation to confirmation of understanding.
Step-by-Step Protocol:
Introduction and Setting:
- Conduct the conversation in a private, quiet setting to minimize distractions.
- Begin by building rapport and explaining the purpose of the conversation: "I want to make sure I've done a good job of explaining this study. So I'm going to ask you to explain it back to me in your own words. This helps me make sure everything is clear."
Information Delivery:
- Explain a single, key concept from the informed consent form (e.g., the main purpose of the study, a specific procedure, or a potential side effect).
- Use plain language, avoid jargon, and break down complex information into smaller chunks.
Eliciting Understanding:
- Ask a non-threatening, open-ended question to initiate the Teach-Back [46]. For example:
- "Can you tell me how you would describe this study to a friend or family member?"
- "Just to be sure I was clear, could you explain back to me what you believe will happen in the first visit?"
- "What might you tell your doctor is a potential risk of being in this study?"
- Ask a non-threatening, open-ended question to initiate the Teach-Back [46]. For example:
Assessment and Clarification:
- Listen carefully to the participant's response.
- If understanding is correct: Acknowledge and reinforce the correct understanding. "Thank you, that's exactly right. You've got it." Then, proceed to the next concept.
- If there is a misunderstanding or gap: This indicates a need for re-explanation. Do not blame the participant. Take responsibility and re-explain the information using different words or methods. "I apologize, I don't think I explained that clearly enough. Let me try again..." After re-explaining, return to Step 3 and ask a new Teach-Back question to confirm the new explanation was effective.
Documentation:
- Document in the research record that the Teach-Back method was used and that understanding was confirmed. Note any concepts that required re-explanation.
Enhancing Assessment with Interactive Tools
While Teach-Back assesses verbal comprehension, interactive digital tools can provide additional, objective data on how participants engage with consent materials and can help identify points of confusion non-intrusively.
The following table summarizes key features of UX research tools that can be adapted for comprehension assessment in a research setting [47] [48].
Table 1: Comparison of Interactive User Research Tools for Comprehension Assessment
| Tool Name | Primary Method | Key Features for Consent Research | Pricing Model |
|---|---|---|---|
| UserTesting [48] | Recorded user sessions | Captures real-time video, audio, and facial expressions of participants interacting with digital consent forms. Provides deep qualitative insight. | Custom/Enterprise |
| Maze [48] | Rapid prototype testing | Integrates with design tools (Figma, Adobe XD) to test mock-ups of consent forms. Can run quick comprehension "tests" with multiple-choice questions. | Starts at $99/month |
| FullSession [48] | User behavior analytics | Session Replays: Watch recordings of how users scroll and interact with a web-based consent form.Heatmaps: Aggregate data showing where users click, scroll, and spend time. Identifies confusing sections. | Starts at $39/month |
| Lyssna [48] | Quick impression tests | Five-Second Tests: Show a section of a consent form for five seconds to test immediate comprehension and recall of key points. | Starts at $89/month |
| UXtweak [48] | Usability testing | Task-Based Testing: Ask participants to find specific information within a consent form (e.g., "Find the contact number for the research ethics board"). | Starts at $99/month |
Protocol for Unmoderated Consent Form Testing
This protocol uses tools like FullSession or UXtweak to gather behavioral data on how a digital consent form is understood.
Step-by-Step Protocol:
Tool Setup and Recruitment:
- Choose a tool based on required features and budget (see Table 1).
- Upload or link to a digital version of the informed consent form within the tool.
- Recruit a representative sample of participants, which may include individuals from the target vulnerable population or a proxy group, ensuring appropriate incentives are provided.
Task Design:
- Create realistic, task-based instructions for participants. Examples include:
- "Please read through this consent form. Your task is to explain the main purpose of the study in your own words when you are finished."
- "Find the section that lists the potential risks of participation. What is one risk mentioned?"
- "Using the information in this form, how many study visits are required?"
- Enable screen recording, audio recording (for think-aloud protocols), and mouse-tracking.
- Create realistic, task-based instructions for participants. Examples include:
Data Collection:
- Participants complete the tasks asynchronously and without a researcher present to avoid bias [47].
- The tool automatically records all interactions, including clicks, scrolls, time-on-page, and verbal commentary.
Data Analysis:
- Behavioral Metrics: Analyze quantitative data such as success/failure rates on tasks, time to complete tasks, and dropout points.
- Session Replays: Watch recordings to observe hesitations, rereading of specific paragraphs, or signs of frustration.
- Heatmap Analysis: Use click and scroll heatmaps to identify which sections attract the most attention and which are ignored [48]. High engagement on a complex section may indicate confusion.
Integration with Qualitative Findings:
- Correlate findings from the interactive tools with results from the verbal Teach-Back method. For instance, if a heatmap shows participants spending disproportionate time on a risks section, and Teach-Back reveals common misunderstandings of those risks, this provides strong, multi-modal evidence for revising that section.
The Scientist's Toolkit: Research Reagent Solutions
This section details the essential "materials" and tools required to implement a robust capacity and comprehension assessment protocol.
Table 2: Essential Research Reagents and Tools for Comprehension Assessment
| Item / Tool | Category | Function in Comprehension Assessment |
|---|---|---|
| Structured Teach-Back Script | Protocol | Provides a standardized set of open-ended questions to ensure consistent application of the method across all participants and researchers. |
| Digital Consent Form Platform | Software | Serves as the testable artifact for interactive tools. Allows for easy iteration and updating based on assessment findings. |
| Unmoderated Usability Testing Tool (e.g., FullSession) [48] | Tool | Enables large-scale, asynchronous collection of behavioral data (clicks, scrolls, time) on how the consent form is navigated and understood. |
| Session Recording & Replay Module [48] | Tool Feature | Allows researchers to qualitatively observe the participant's journey through the consent form, identifying points of confusion non-intrusively. |
| Heatmap Generator (Click/Scroll) [48] | Tool Feature | Visually aggregates data from multiple users to identify areas of high and low engagement on a consent form, highlighting sections that may be unclear or confusing. |
| Plain Language Glossary | Document | A reference document for researchers to replace technical jargon with simple, accessible language during explanations and in consent form revisions. |
Data Presentation and Visualization Specifications
All quantitative data gathered from interactive tools and qualitative observations from Teach-Back should be synthesized to guide decision-making.
Table 3: Summary of Comprehension Metrics and Interpretation
| Assessment Method | Metric | How to Measure | Interpretation & Action |
|---|---|---|---|
| Teach-Back | Comprehension Accuracy Rate | Percentage of key concepts explained correctly by the participant on the first try. | Low Rate: Indicates poor explanation clarity. Revise language, use more visuals, and retrain staff. |
| Teach-Back | Concepts Requiring Re-explanation | The specific study elements (e.g., risks, compensation) most frequently misunderstood. | Pattern Identification: Highlights sections of the consent form that need immediate revision and simplification. |
| Interactive Tools | Task Success Rate | Percentage of participants who correctly complete a defined task (e.g., finding key information). | High Failure Rate: Suggests poor information architecture or hidden information. Restructure the layout. |
| Interactive Tools (Heatmaps) | Average Dwell Time | Mean time spent on a specific section or page of the digital consent form. | Abnormally High/Low: Can indicate confusion/clarity. Correlate with task success and verbal feedback. |
| Interactive Tools (Click Maps) | Click Density | Aggregation of all clicks on interactive elements (or non-interactive elements mistaken for links). | Misclicks: Reveal user expectations and potential misunderstandings about the interface or content. |
Diagram Specifications for Reporting
All diagrams and visualizations generated for reports or publications must adhere to the following specifications to ensure accessibility and professional presentation:
- Max Width: 760px
- Color Palette: Restrict to
#4285F4,#EA4335,#FBBC05,#34A853,#FFFFFF,#F1F3F4,#202124,#5F6368. - Color Contrast Rule: Ensure sufficient contrast between arrow/symbol colors and their background. Avoid using the same color for foreground elements (text, arrows, symbols) as for the background.
- Node Text Contrast Rule (Critical): For any node (e.g., rectangle, circle) that contains text, the text color (
fontcolor) must be explicitly set to have high contrast against the node's background color (fillcolor). For example, use light-colored text on dark fills (#FFFFFFon#34A853) and dark-colored text on light fills (#202124on#FFFFFF).
Within the ethical framework of research involving vulnerable populations, obtaining initial informed consent is a necessary but insufficient safeguard. Ongoing consent is a dynamic, continuous process that maintains a dialogue with participants throughout the research lifecycle, ensuring their participation remains voluntary and informed as study circumstances or the participant's own capacity evolves [43] [49]. This process is paramount when working with vulnerable groups—such as individuals with cognitive impairments, fluctuating health conditions, or those in dependent situations—who may be particularly susceptible to coercion or may experience changes in their ability to understand the research [50] [51]. This application note provides researchers, scientists, and drug development professionals with structured protocols and tools to implement robust ongoing consent procedures, framed within the broader thesis that ethical research with vulnerable populations requires moving beyond a single consent event to a sustained partnership.
Conceptual and Regulatory Framework
Defining Ongoing Consent and Re-consent
The informed consent process is fundamentally a process of trust and respect, spread throughout a study, rather than a single signature or verbal affirmation [43]. Ongoing consent operationalizes this principle through continuous engagement, while re-consent is a specific, documented event within that process, required when specific material changes occur in the study or participant status [49].
- Ongoing Consent: A continuous, interactive dialogue that allows for the reaffirmation of participation willingness, provides opportunities for questions, and confirms consistent willingness to be part of the study [43].
- Re-consent: A formal process of obtaining informed consent again using a revised, IRB-approved consent form when significant new information or changes to the protocol arise [49].
Ethical and Regulatory Foundations
The ethical imperative for ongoing consent is rooted in the Belmont Report's principle of Respect for Persons, which requires protecting individuals with diminished autonomy [51]. Legally, the Nuremberg Code establishes that voluntary consent is essential, and the participant "should be able to exercise free power of choice" without constraint [43]. Federal regulations (45 CFR 46.116) further mandate that informed consent must be sought under circumstances that minimize the possibility of coercion or undue influence [43].
Recent regulatory developments emphasize inclusion. The 2024 updates to Section 504 of the Rehabilitation Act prohibit unnecessary exclusion of people with cognitive disabilities from clinical research, implying that systems to support their ongoing consent are a matter of civil rights, not just ethical practice [50]. This shifts the focus from blanket exclusion to implementing robust, continuous consent processes that empower participation.
Table 1: Triggers Mandating the Re-consent Process
| Trigger Category | Specific Examples | Rationale & Reference |
|---|---|---|
| Protocol Amendments | Significant changes to study procedures, objectives, risks, or benefits [49]. | Ensures participant awareness and agreement to the new research structure. |
| Emerging Information | New information about risks associated with the study intervention [49]. | Upholds the ethical duty to inform and allows for re-evaluation of risk-benefit. |
| Temporal Changes | Extension of the study timeline beyond the originally agreed duration [49]. | Participation is based on an original time commitment; a significant extension requires renewed agreement. |
| Participant Status | A child participant reaches the age of majority during the study [49]. | The now-adult participant must provide their own legally valid consent. |
| Participant Capacity | A change in a participant's cognitive abilities or circumstances [49]. | May necessitate the involvement of a Legally Authorized Representative (LAR) to provide consent on their behalf. |
Quantitative Assessment of Consent Processes
Empirical evidence highlights the critical challenges in the consent process that ongoing dialogues aim to address. Surveys of research staff reveal significant concerns about participant comprehension and procedural barriers.
Table 2: Research Staff Perspectives on Consent Process Challenges (n=115)
| Reported Challenge | Percentage of Staff | Implication for Ongoing Consent |
|---|---|---|
| Concerned about participant understanding of complex information | 56% | Validates the need for continuous comprehension checks, such as the Teach-Back method [52]. |
| Felt information leaflets were too long and/or complicated | 63% | Supports the use of simplified, ongoing summaries and visual aids instead of relying solely on dense documents [52]. |
| Felt time constraints were a barrier | 40% | Highlights that the initial consent may be rushed, making follow-up discussions crucial for clarifying misunderstandings [52]. |
| Felt "very confident" or "confident" facilitating consent | 74.4% | Indicates a majority of staff have the baseline confidence to engage in more complex, ongoing consent dialogues [52]. |
Proposed Experimental Protocols and Methodologies
Protocol 1: Implementing a Tiered Capacity Assessment and Assent Process
This protocol is designed for research involving adults with uncertain or impaired decision-making capacity (DMC), a population often unfairly excluded from research [50]. The goal is to systematically respect autonomy through a tiered process of capacity assessment and assent.
1. Background and Rationale: DMC is a functional ability that can vary depending on time, place, and context [50]. A one-time capacity assessment at enrollment is inadequate. This protocol provides a framework for continuous evaluation.
2. Materials and Reagents:
- Evaluation of Capacity to Consent (ECCE) tool or similar validated instrument.
- IRB-approved assent script with visual aids.
- Documentation form for recording capacity assessment and assent process.
3. Procedure: 1. Initial Assessment: Prior to the initial consent discussion, a qualified member of the research team assesses the potential participant's DMC using a structured tool. Document the outcome. 2. Consent/Assent: If capacity is sufficient, proceed with the standard informed consent process. If capacity is impaired or uncertain, obtain consent from the Legally Authorized Representative (LAR). 3. Assent Process: For the participant with impaired DMC, conduct an assent discussion using the simplified script and visual aids. Document the participant's affirmative agreement (verbal, head nod, thumbs up) or dissent [51]. 4. Ongoing Re-assessment: Re-assess DMC at pre-specified intervals (e.g., before each new study phase, after hospitalizations, or when staff observe potential confusion) [51]. 5. Documentation: Record all assessments and communications in the participant's research record.
4. Data Analysis: The primary outcome is the proportion of participants with impaired DMC for whom a valid assent process was documented at all required timepoints. Qualitative analysis of staff and LAR feedback on the feasibility of the process should also be conducted.
Protocol 2: A Scheduled Dialogue Framework for Longitudinal Studies
This protocol ensures ongoing consent is operationalized as a scheduled, structured activity in long-term studies, rather than an ad-hoc response to problems.
1. Background and Rationale: The consent process is a process, not an event, built on trust and respect spread throughout a study [43]. This protocol institutionalizes that principle.
2. Materials and Reagents:
- "Consent Check-in" guide, a short document summarizing the study's key elements (purpose, procedures, risks) in simple language.
- Teach-Back technique script (e.g., "Please tell me in your own words what we will be doing in this next phase of the study.").
- Participant feedback mechanism (e.g., a short, anonymous survey).
3. Procedure: 1. Schedule: Integrate brief (10-15 minute) "Consent Check-ins" into the study visit schedule (e.g., every 3-6 months, or before major protocol transitions). 2. Execution: At the check-in, a researcher uses the guide to briefly review the study. The researcher then uses the Teach-Back technique to assess understanding [52]. 3. Re-affirmation: Explicitly ask the participant, "Knowing this, do you still wish to continue in the study?" This reaffirms the voluntary nature of participation. 4. Feedback: Offer the participant a mechanism to provide anonymous feedback on their experience in the study. 5. Documentation: Note the completion of the check-in and any participant questions or concerns in the study record. A signature is not typically required unless the check-in coincides with a formal re-consent event.
4. Data Analysis: Monitor the rate of participant retention and withdrawal following check-ins. Thematic analysis of participant feedback can be used to improve the research experience and consent materials.
The Scientist's Toolkit: Reagents and Materials
Table 3: Essential Materials for Implementing Ongoing Consent Protocols
| Tool Name | Function/Application | Protocol Usage |
|---|---|---|
| Teach-Back Script | A standardized set of questions to ask participants to explain study concepts in their own words. | Used in Consent Check-ins (Protocol 2) to verify comprehension and identify areas needing clarification [52]. |
| Validated Capacity Assessment Tool (e.g., ECCE) | A structured instrument to objectively evaluate a person's understanding, appreciation, and reasoning about the research study. | Applied in Tiered Capacity Assessment (Protocol 1) to determine the appropriate consent/assent pathway at multiple timepoints [50] [51]. |
| IRB-Approved Visual Aids | Simplified diagrams, illustrations, or pictograms explaining study procedures, risks, and timelines. | Leveraged in both protocols to enhance understanding, particularly during the assent process for individuals with impaired DMC [43] [20]. |
| Assent Documentation Form | A form designed to record the participant's affirmative agreement (verbal or non-verbal) to participate, separate from the LAR's consent form. | Critical for Protocol 1 to formally document the outcome of the assent discussion and respect the autonomy of the participant [51]. |
Visualization of Workflows and Pathways
The following diagrams illustrate the logical workflows for the proposed ongoing consent protocols, providing a clear visual guide for implementation.
Diagram 1: Tiered Capacity and Assent Workflow for Participants with Impaired DMC. This flowchart outlines the process for continuously evaluating a participant's decision-making capacity and engaging them and their representative in the consent process.
Diagram 2: Scheduled Dialogue Framework for Longitudinal Studies. This workflow demonstrates the integration of regular, structured dialogues to maintain ongoing consent and voluntariness throughout a research study.
Adopting a rigorous framework for ongoing consent is a critical evolution in the ethical conduct of research with vulnerable populations. The protocols and tools detailed herein provide a practical roadmap for translating the principle of continuous dialogue into actionable practice. By moving beyond a single consent event to a sustained partnership, researchers can better uphold the core ethical tenets of respect for persons, beneficence, and justice, ensuring that the voluntariness of every participant is not only established at the outset but meticulously maintained throughout the entire research journey.
Overcoming Common Challenges and Enhancing Consent Comprehension
Application Note: Core Principles and Regulatory Framework
Informed consent is a foundational requirement in ethical research involving human subjects. A valid consent process requires that study information is presented "in language understandable to the subject" [53]. Achieving this with vulnerable populations, particularly those facing literacy or language barriers, requires dedicated strategies that go beyond simple translation. Transparent and complete reporting of these processes is crucial for evaluating the reliability of research findings [54]. The core objective is to ensure that potential participants can make a truly informed decision about their involvement in research, thereby upholding the ethical principle of respect for persons.
Regulatory bodies like the Office of Human Research Protections (OHRP) strongly encourage providing written consent materials in a participant's primary language [55]. The FDA and OHRP encourage the inclusion of diverse subject populations to ensure equitable subject selection [56]. While regulations focus significantly on the consent document, researchers must also prepare for the entire ongoing consent conversation, which includes providing new information, updates, and ongoing education in a language understandable to the participant [56].
Experimental Protocol 1: Consent Form Simplification and Readability Assessment
This protocol provides a detailed methodology for developing and validating simplified English consent forms to address literacy barriers.
Materials and Reagents
Table 1: Research Reagent Solutions for Consent Simplification
| Item Name | Function/Explanation |
|---|---|
| Word Processing Software | Used for drafting and revising consent documents; the "Compare" feature is essential for tracking changes between versions [55]. |
| Readability Assessment Tool | Software or online calculators that apply formulas (e.g., Flesch Reading Ease, Flesch-Kincaid Grade Level) to quantitatively determine the reading grade level of a text. |
| Lay Terminology Glossary | A reference of common, non-technical words to replace complex medical or scientific jargon (e.g., "high blood pressure" instead of "hypertension") [53]. |
Step-by-Step Procedure
- Initial Drafting: Draft the consent form using the second-person perspective ("you") and avoid statements starting with "You understand..." [53].
- Jargon Replacement: Systematically replace technical terms with lay language from a validated glossary [53].
- Formatting for Clarity: Employ a 12-point font or larger for vulnerable groups. Integrate visual aids like flowcharts and tables to enhance comprehension [53].
- Readability Testing: Input the finalized text into a readability assessment tool. The target is a 6th to 8th-grade reading level for adult participants [53].
- Iterative Refinement: Revise the text based on readability scores and feedback from a simplified consent expert or a patient advisory group.
- Validation (Optional): Where resources allow, employ empirical methods like the Public Deliberation approach to engage patients and the community in collective decision-making to improve consent processes, comparing results to traditional surveys or interviews [57].
Experimental Protocol 2: Multi-Step Translation and Quality Control
This protocol outlines a rigorous methodology for translating consent materials from English into another language, using Spanish as an example, to ensure accuracy and cultural appropriateness.
Materials and Reagents
Table 2: Research Reagent Solutions for Translation
| Item Name | Function/Explanation |
|---|---|
| Native Speaker Translators | Individuals with native proficiency in the target language and different dialects, who also possess an appreciation of sociocultural factors affecting interpretation [55]. |
| Back Translator | An independent translator, naive to the original English documents, who translates the forward-translated version back into English [55]. |
| Comparison Software | A word processor with a document "Compare" feature to identify discrepancies between the original and back-translated versions [55]. |
| Coding Software (e.g., NVivo) | Qualitative data analysis software to systematically code and categorize types of translation errors across multiple professional translations [55]. |
Step-by-Step Procedure
- Initial Forward Translation: Two native speakers of the target language (preferably of different dialects) produce independent forward translations. One translation is generated, and the second reviewer compares it to the original to identify potential problems (e.g., regionally specific language, change of meaning) [55].
- Consensus and Reconciliation: The two translators discuss identified issues to reach a resolution, producing a single reconciled forward translation [55].
- Back Translation: A separate native speaker, who has not seen the original English documents, translates the reconciled version back into English [55].
- Discrepancy Analysis: Use software to compare the back-translated version with the original English. Discrepancies are categorized as:
- Forward Translation Revision: The team reviews problematic discrepancies and consults with additional native speakers to revise the forward translation accordingly [55].
- Quality Benchmarking (Optional): Commission translations from professional firms. Compare these against the research team's translation using a standardized coding rubric to identify common error types (e.g., mistranslation, failure to specify) and further refine the materials [55].
Experimental Protocol 3: Integrating Professional Interpreters in the Consent Process
This protocol details the integration of qualified interpreters to facilitate oral communication with non-English-speaking participants during the consent process and throughout the study.
Materials and Reagents
Table 3: Research Reagent Solutions for Interpretation
| Item Name | Function/Explanation |
|---|---|
| Certified Medical Interpreter (CMI) | A professionally credentialed interpreter with training in medical terminology and ethics. Use of an impartial interpreter is encouraged over friends and family [56]. |
| Translated Long Form Consent Document | The full consent document, translated via a rigorous process (see Protocol 2), which is provided to the participant [56]. |
| Short Form Consent Document | A short form written consent document, used only in unexpected situations when a translated long form is not available [56]. |
Step-by-Step Procedure
- Interpreter Selection and Briefing: Secure a Certified Medical Interpreter (CMI) or a professional with experience in clinical research. Brief the interpreter on the study's purpose, procedures, and key terminology to ensure conceptual accuracy [56].
- Pre-Session Meeting: The principal investigator and interpreter meet before the consent conversation to review the process and clarify any complex concepts.
- Facilitated Consent Discussion: The interpreter facilitates the entire conversation between the researcher and the participant, ensuring all information is conveyed accurately and in a culturally appropriate manner. The interpreter's role is to translate, not to explain or obtain consent.
- Documenting Consent: The participant signs the translated long form consent document. The principal investigator and a witness also sign both the English and translated versions. The interpreter may also sign a dedicated signature line if required by the IRB [56].
- Ongoing Interpretation: Plan for the same interpreter to be available for all subsequent study visits to ensure consistency and build trust, providing ongoing education and conveying new information [56].
Within the overarching ethical framework of informed consent for vulnerable populations research, ensuring voluntary participation is a paramount challenge. Truly voluntary consent is free from coercion—the overt threat of harm to obtain compliance—and undue influence, which involves the use of excessive, inappropriate, or unwarranted rewards or persuasion that can override an individual's ability to make a voluntary decision [58] [59]. These influences are often rooted in inherent power dynamics, where the researcher holds a position of authority, knowledge, or status that can implicitly pressure a potential participant to comply, even against their own judgment or will [58] [60]. For researchers and drug development professionals, navigating these challenges is not merely an ethical obligation but a critical component of research integrity, essential for the validity of the data and the protection of both participants and the institution.
Vulnerable populations in clinical research, such as detained persons, those with cognitive or psychiatric conditions, economically disadvantaged groups, and those in dependent relationships (e.g., students, patients), are at a heightened risk of these influences [61] [5] [60]. It is crucial to recognize that vulnerability does not automatically equate to an impaired capacity for consent. A 2025 study on detained individuals with ADHD, for instance, found no significant difference in the understanding of consent or willingness to participate compared to those without ADHD, though the overall level of understanding was low across the entire cohort [61]. This underscores that the onus is on the research design and the researcher to create an environment and a process that mitigates these pressures and empowers all individuals to make a free and informed choice.
The following tables consolidate empirical findings and regulatory observations related to coercion, understanding, and participant compensation, providing a evidence-based foundation for protocol development.
Table 1: Understanding and Acceptance of Informed Consent in a Vulnerable Population
| Population | Study Focus | Understanding of IC (Mean Score) | Acceptance Rate (Signed IC) | Key Finding | Citation |
|---|---|---|---|---|---|
| Detained Individuals (Total n=183) | Association of ADHD with IC understanding and willingness to participate. | ADHD+: 5.2 | ADHD+: 83.3% | No significant association found between ADHD and understanding or willingness to participate. Overall understanding was low. | [61] |
| ADHD-: 4.9 (p=.468) | ADHD-: 84.9% (p=.814) |
Table 2: IRB Considerations and Participant Compensation Models
| Concept / Model | Key Definition / Principle | Implications for Research Practice |
|---|---|---|
| Undue Inducement | An offer of an "excessive, unwarranted, inappropriate, or improper reward" that overcomes a person's free will [59]. | IRBs often wrestle with this concept, sometimes relying on "gut feelings." Requires vigilance to ensure compensation does not obscure risks. |
| Wage Payment Model | A model advocating for a standard, low wage for participant time, which can be raised for more onerous or uncomfortable procedures [59]. | Helps standardize compensation and avoid offers that are disproportionately attractive, thereby reducing the risk of undue inducement. |
| Market Model | A model based on supply and demand, potentially offering higher payment for higher risk or rare populations [59]. | Can be ethically challenging as it may incentivize participants to underestimate risks for financial gain. |
| Reimbursement Model | A model focused solely on covering participants' expenses, including costs from missed work [59]. | Minimizes financial incentive but may not adequately compensate for time and effort, potentially disadvantaging certain groups. |
Application Notes & Experimental Protocols
Protocol for Pre-consent Environment and Recruitment
Aim: To establish a neutral and low-pressure environment from the initial point of contact to minimize perceived power imbalances and set the stage for a voluntary decision.
Methodology:
- Recruitment Material Review:
- All recruitment materials (flyers, online ads, scripts) must be pre-approved by the IRB/EC.
- Action: Present compensation information proportionally. It should not be the most prominent feature of the advertisement. Clearly state that compensation is for time and travel [58] [59].
- Action: Use language that emphasizes voluntariness, e.g., "You are invited to consider participating," rather than "You are eligible to participate."
- Setting and Introductions:
- Conduct the consent discussion in a private, neutral setting, not in a clinical room during a routine care appointment unless unavoidable (with additional safeguards).
- Action: The person obtaining consent should introduce themselves and clearly state their role (e.g., "a member of the research team") and explicitly distinguish this from the clinical care team, if applicable.
- Action: Begin the interaction with a clear, scripted statement affirming voluntariness: "Before we begin, I want to be clear that your decision to participate or not participate in this research will not affect your medical care, your legal status, or your relationship with this institution in any way" [58].
Protocol for the Dynamic Consent Process
Aim: To implement consent as an ongoing, interactive process that assesses and ensures understanding and continued willingness, rather than a single event centered on a signature.
Methodology:
- Structured Information Disclosure:
- Action: Utilize a layered consent form with a concise summary at the beginning. Employ plain language, avoiding technical jargon.
- Action: For populations with potential cognitive vulnerabilities (e.g., ADHD, mental illness), adapt the process. This may include using visual aids, breaking information into shorter sessions, or involving a trusted, independent advisor to support understanding [61] [60].
Assessment of Understanding (Teach-Back Method):
- Action: After explaining a key concept (e.g., risks, randomization, right to withdraw), ask the participant to explain it back in their own words. Do not proceed until the concept is correctly understood.
- Action: Incorporate open-ended questions into the process, such as:
- "Can you tell me what you would do if you wanted to stop being in the study?"
- "What are the main downsides or risks for you if you participate?"
- "What will happen on a typical visit?" [58]
Documenting Voluntariness:
- Action: Beyond the signature, document in a note to file the key elements of the consent process, including the setting, who was present, that voluntariness was explicitly discussed, and that understanding was assessed.
Protocol for Managing Incentives and Compensation
Aim: To structure financial incentives and other compensation in a way that facilitates participation without becoming the primary reason for participation, thus avoiding undue influence.
Methodology:
- Compensation Structure and Review:
- Action: Adopt a wage-payment model as a benchmark, setting compensation at a level that is commensurate with the time and burden imposed on the participant, rather than the level of risk [59].
- Action: Propose the compensation structure to the IRB/EC with a justification based on local standards and the principle of fairness. Actively seek their guidance to avoid undue inducement [59].
- Disbursement Schedule:
- Action: Avoid large, lump-sum payments, especially at the end of the study, which could deter a participant from withdrawing even if they wish to.
- Action: Structure compensation as partial payments distributed throughout the study or a small bonus for completion, making it clear that the participant will be compensated for all time spent in the study even if they withdraw early.
Protocol for Ongoing Monitoring and Withdrawal
Aim: To reinforce voluntariness throughout the entire research lifecycle by ensuring participants feel able to withdraw without penalty or judgment.
Methodology:
- Re-affirmation of Consent:
- Action: At the beginning of each study visit or procedure, briefly re-state the key elements of the study and reaffirm the participant's continued willingness to be involved.
- Action: Train all research staff to recognize nonverbal cues of discomfort or hesitation and to respond by gently checking in with the participant (e.g., "You look a little unsure, would you like me to go over that part again?").
- Facilitating Easy Withdrawal:
- Action: Provide participants with a direct, low-effort method of withdrawal, such as a dedicated phone number or email address managed by someone independent of the immediate research team.
- Action: If a participant withdraws, ensure the process is respectful and without argument. Follow the protocol for final compensation and, if applicable, arrange for responsible follow-up care.
Visual Workflows and Diagrams
Consent Voluntariness Workflow
Compensation Model Decision Tree
The Scientist's Toolkit: Essential Reagents & Materials
Table 3: Key Research Reagent Solutions for Ethical Consent Research
| Item / Tool | Function in Experimental Protocols |
|---|---|
| Plain Language Consent Templates | Standardized, jargon-free templates form the baseline for clear communication, ensuring all participants receive core information in an accessible format. |
| Teach-Back Assessment Script | A structured set of open-ended questions used to objectively evaluate a participant's comprehension of key study concepts after the initial disclosure. |
| Vulnerability-Specific Communication Aids | Tailored materials (e.g., pictorial aids for low literacy, simplified schedules for ADHD) used to adapt the core consent protocol to specific population needs [61] [60]. |
| IRB/EC Compensation Justification Template | A pre-formatted document to guide researchers in presenting a structured rationale for proposed participant payment, facilitating ethical review and compliance [59]. |
| Consent Process Documentation Form | A standardized checklist and note-to-file template for consistently recording key elements of the consent interaction, providing an audit trail for voluntariness. |
| Digital Recruitment Content Library | A centralized, version-controlled repository of all IRB-approved recruitment materials (ads, flyers, scripts) to ensure consistent and compliant messaging across all channels. |
Application Notes: The Challenge of Time and Information in Informed Consent
Informed consent is a cornerstone of ethical research, yet its integrity is often compromised by information overload and time constraints, particularly when working with vulnerable populations. The core challenge lies in balancing the ethical imperative to provide comprehensive information with the practical need to ensure that information is actually understood by a potential participant.
The digitalization of work and life has exacerbated the problem of information overload, a state where the amount of information exceeds an individual's processing capacity, leading to stress and impaired decision-making [62]. In clinical research, this is reflected in consent documents that are often excessively long and complex. A 2025 analysis of Patient Information Sheets (PISs) and Informed Consent Forms (ICFs) from UK COVID-19 trials revealed a median length of 5,139 words, requiring approximately 21.4 minutes to read [63]. Despite guidelines recommending that such documents be written for a reading age of 9-11 years, all analysed forms were classified as 'difficult' for comprehension, with a median reading age of 14 years or higher [63]. This complexity systematically disadvantages individuals with lower health literacy and can be a significant barrier to genuine informed consent.
Simultaneously, time pressure in clinical settings can lead to rushed consent processes. Decisions are often solicited shortly before a procedure, denying participants a sufficient period for reflection, questioning, and consultation [11]. This is antithetical to a patient-centered approach, which requires a structured, two-way dialogue in a calm setting [11]. For vulnerable populations, who may face additional barriers such as language, cultural differences, or health-related stress, these challenges are magnified, threatening the ethical principles of respect for persons and autonomy [11].
Table 1: Quantitative Analysis of Consent Form Complexity (Gourlay et al., 2025)
| Metric | Median Value (Range) | Interpretation & Benchmark |
|---|---|---|
| Document Length | 5139 words (1559-7026) | Requires substantial time investment to read |
| Estimated Reading Time | 21.4 min (6.5-29.3 min) | Often occurs under time pressure in clinical settings |
| Flesch-Kincaid Grade Level (FKGL) | 9.8 (9.1-10.8) | Reading age of 14-15 years; above recommended 6th-8th grade level |
| Flesch Reading Ease (FRES) | 54.6 (47.0-58.3) | Classified as "difficult" for comprehension (scores below 60) |
Experimental Protocols for Structured Decision-Making
Protocol 1: A Participatory, Tiered-Length Consent Process
This protocol, adapted from Faisal et al. (2025), uses a community-engaged approach and a multi-format information structure to improve understanding and trust among ethnic minority groups [63].
Methodology:
- Community Partnership: Collaborate with community leaders and cultural brokers from the target population to facilitate access and foster dialogue. These partners assist with live translation, script development, and co-creating resources.
- Structured Information Delivery:
- Visual Storyboards: Develop graphical representations of the trial process to provide an intuitive overview.
- Multilingual Videos: Create short videos in relevant native languages (e.g., Urdu, Mandarin, Cantonese, Bangla) explaining the trial's purpose, procedures, and the importance of diverse participation. These serve as a primary, accessible information layer.
- Abridged Consent Form: A concise, 2-3 page document written in plain language (targeting 6th-8th grade level) covering the essential elements: nature of the procedure, risks, benefits, and alternatives [11] [53].
- Supplementary Information Sheet: A separate, detailed document providing comprehensive information for participants who desire more in-depth knowledge, without overloading the primary consent form.
- Dedicated Decision-Making Time: After the initial information session, a mandatory reflection period of at least 24 hours is instituted before consent is finalized. This allows participants to discuss the trial with family, friends, or their community.
Key Experiment Cited: This protocol was implemented and tested in a PPIE (Patient and Public Involvement and Engagement) project in Bristol, UK, involving Somali, South Asian, and Chinese communities. Workshops used simulated recruitment scenarios to refine the approach [63].
Protocol 2: Telemedicine-Enhanced Informed Consent
This protocol leverages telemedicine to decentralize the consent process, reducing geographic and time barriers while maintaining interactivity.
Methodology:
- Pre-Consent Information Pack: A package containing the abridged consent form, supplementary information sheet, and links to informational videos is sent to the participant electronically at least 72 hours before the scheduled consent discussion.
- Synchronous Video Discussion: A dedicated telemedicine appointment is conducted between the researcher and the potential participant (and their family/support person if desired). This session focuses on:
- Using the teach-back method to assess understanding, where the participant explains the information in their own words [11].
- Encouraging and answering questions in an interactive dialogue.
- Ensuring the participant is in a comfortable, self-selected environment, which can reduce the perceived power dynamics of a clinical setting.
- Asynchronous Follow-up: After the video discussion, a summary of the conversation and a copy of the consent form are sent to the participant. They are given another 24-48 hours to make a final decision before providing formal consent.
Key Experiment Cited: A 2025 survey study of cancer patients at Memorial Sloan Kettering Cancer Center found that 57% of patients who had clinical trial discussions via telemedicine preferred it for the informed consent process, citing reduced travel and time burdens [63].
Protocol 3: Readability-Optimized and Preference-Tested Consent
This protocol employs a human-centered design and iterative testing to create consent materials that align with the readability preferences and information needs of the target population.
Methodology:
- Readability Analysis and Modification: Use free, web-based readability software to analyze original consent text. Independently, multiple research team members rewrite text snippets to improve metrics like character length, Flesch Kincaid Reading Ease, and lexical density, then agree on a final, optimized version [15].
- Preference Testing Survey: Recruit participants who are eligible for the parent study. Present them with pairs of text snippets—the original and the modified version—and survey their preferences. Quantitative analysis identifies which snippets are preferred and how factors like age, sex, and topic (e.g., risks) influence choice [15].
- Iterative Refinement: Use the survey feedback to refine the consent materials. Qualitative analysis of participant comments is crucial, as it often reveals new questions not addressed in the original material, indicating gaps in understanding [15].
Key Experiment Cited: A 2025 survey study (N=79) for a digital health study found that participants were 1.20 times more likely to prefer modified text over the original when the original character length was longer, especially for text explaining study risks. Older participants, however, were 1.95 times more likely to prefer the original, highlighting the need for demographic-specific tailoring [15].
Diagram 1: Protocol Selection for Informed Consent
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for Implementing Consent Protocols
| Tool / Solution | Function / Description | Application Context |
|---|---|---|
| Plain Language Glossary | Provides lay terminology substitutes for complex medical/scientific terms (e.g., "high blood pressure" for "hypertension"). | Essential for all protocols to achieve a 6th-8th grade reading level [53]. |
| Readability Calculator Software | Web-based tool to quantitatively assess and improve text metrics (Flesch-Kincaid, character length, lexical density). | Core to Protocol 3 for systematic optimization of consent materials [15]. |
| Multilingual Video Platform | Hosting and distribution platform for co-created, accessible video resources in multiple languages. | Critical for Protocol 1 to engage diverse populations and explain complex trial concepts [63]. |
| Secure Telemedicine Platform | HIPAA-compliant video conferencing software that supports screen-sharing for visual aids and recording (with consent). | The technological backbone of Protocol 2, enabling remote, interactive consent discussions [63]. |
| Structured Consent Template | An IRB-approved template written in the 2nd person ("you"), using a 12-point font and clear sections for risks, benefits, and alternatives. | Foundational for all protocols to ensure regulatory compliance and consistent, clear formatting [53]. |
| Community Advisory Board (CAB) | A group of community members and patient advocates who provide ongoing feedback on study design, materials, and consent processes. | Vital for Protocol 1 to ensure cultural and linguistic appropriateness and build trust [63]. |
| Teach-Back Assessment Guide | A structured script or set of questions for researchers to verify participant comprehension after information is provided. | A key component of Protocol 2, used during the synchronous video discussion to ensure understanding [11]. |
Within the critical context of obtaining genuine informed consent from vulnerable populations, the implementation of plain language and an 8th-grade reading level standard is an ethical and methodological necessity. Vulnerable populations often face compounded barriers to understanding complex research protocols, including cognitive stressors, educational disparities, and linguistic challenges. Utilizing convoluted, high-level language can invalidate the consent process by undermining true comprehension. Adhering to a plain language framework ensures that consent documents and study communications are designed so that participants can find, understand, and use the information to make an autonomous decision [64]. This approach aligns with the highest standards of ethical research by prioritizing participant welfare and the validity of the informed consent process.
Core Standards and Rationale
The 8th-Grade Reading Level Standard
A foundational standard for plain language in public-facing documents, including research consent forms, is achieving an 8th-grade reading level [65]. This benchmark is not arbitrary but is grounded in the goal of universal accessibility. Adhering to this standard allows individuals to read with less effort, facilitates accurate translation for non-English speakers—including children who may translate for their parents—and ensures more precise translation into other languages [65]. This is particularly crucial for vulnerable populations, who may experience additional cognitive load or have limited English proficiency.
Quantitative Justification
The demographic necessity of this standard is underscored by data from California, which indicates that 19% of Californians speak English "less than very well," and 44% of residents over age 5 speak a language other than English at home [65]. While regional, these figures highlight a national reality of linguistic diversity that researchers must accommodate to ensure equitable access to research participation.
Table 1: Plain Language Writing Standards
| Principle | Application Example | Rationale |
|---|---|---|
| Use Simple Words | Use "use" instead of "utilize" [64]. | Familiar words reduce cognitive load and are understood more quickly. |
| Explain Jargon | Define "Area Median Income (AMI)" in plain language the first time it is used [65] [64]. | Ensals participants understand critical technical terms relevant to the study. |
| Acronyms | Spell out the full term first, followed by the acronym in parentheses (e.g., Research Ethics Committee (REC)) [65]. | Prevents confusion and ensures clarity for all readers. |
| Active Voice | "You must complete the survey" instead of "The survey must be completed by you." [65] [64]. | Creates direct, clear sentences and tells people what they need to do. |
| Short Sentences | Aim for sentences under 25 words and communicate one piece of new information at a time [64]. | Prevents complex syntax from obscuring the main message. |
| Positive Instructions | "You must apply by February 10" instead of "If you do not apply by February 10, your application will not be accepted." [65]. | It is easier for people to understand what they should do than to decipher double negatives. |
Experimental Protocol: Plain Language Review for Informed Consent Documents
This protocol provides a detailed methodology for systematically reviewing and revising informed consent forms (ICFs) to ensure they meet plain language and 8th-grade readability standards, specifically tailored for research involving vulnerable populations.
Pre-Review Preparation
- Objective: To identify and rectify elements within the draft ICF that impede comprehension for the prospective participant.
- Materials: Draft informed consent form, Microsoft Word processor (or equivalent with readability statistics), plain language review worksheet, and the organization's style guide if available [64].
- Defined Audience and Purpose: Before review, explicitly define the participant population (e.g., "adults with low literacy levels," "non-native English speakers," "adolescents"). Confirm the document's primary purpose is to facilitate an informed decision about research participation [64].
Step-by-Step Procedure
Readability Score Assessment:
- Activate the readability statistics feature in your word processor.
- Run a spelling and grammar check on the entire ICF document.
- Record the Flesch-Kincaid Grade Level score. The target is 8th grade or lower [65] [64].
- A high score (e.g., grade 13) signals a need for significant structural simplification.
Systematic Content Review:
- Check that the title and section headings are descriptive and make sense when read alone [64].
- Verify that the most critical information (e.g., study purpose, key procedures, main risks) is positioned at the beginning of the document and of each section [64].
- Identify long paragraphs (>5-6 lines) and sentences (>25 words). Mark these for potential splitting.
- Convert long lists of items embedded in sentences into bulleted or numbered lists for scannability [64].
- Scrutinize all instructions for participants. Ensure they are logically ordered and include all critical information (e.g., what to gather, timelines, who to contact) without gaps [64].
Language and Tone Analysis:
- Jargon and Acronyms: Identify all technical terms (e.g., "randomization," "biobank," "adverse event"). For each, either replace with a common word or provide a plain language definition upon first use [65] [64].
- Word Choice: Replace formal or unfamiliar words (e.g., "obtain," "commence," "upon completion of") with simpler alternatives (e.g., "get," "start," "after") [64].
- Voice and Structure: Convert passive voice constructions to active voice. Ensure the document directly addresses the reader using "you" [65] [64].
- Phrasal Verbs: Replace phrasal verbs (e.g., "look up," "put off") with simpler verbs to aid machine translation and non-native speakers [64].
Accessibility and Data Presentation Check:
- Ensure link text (if any) is descriptive (e.g., "Download the participant information sheet," not "click here") [64].
- If the ICF contains charts or tables, verify they have clear titles, labels, and necessary context for interpretation [64].
- Check that any data presented follows best practices for clarity, as outlined in Section 4 of this document.
Feedback and Revision
- Provide two types of feedback to the document author: High-level (structural and organizational issues) and Specific (line-by-line suggestions for rewriting) [64].
- For patterns of issues (e.g., consistent use of passive voice), provide a representative before-and-after example to illustrate the revision principle [64].
- The final ICF must be approved by the relevant Research Ethics Committee (REC) and provided in both English and the participant's primary language [66].
Data Presentation and Visualization Protocols
Effective data presentation is crucial, both within the consent form to explain study details and in the subsequent research publication.
Choosing Between Tables and Charts
The choice between a table and a chart depends on the message and the audience's needs. For consent forms aimed at participants, simplified charts are often better for conveying high-level concepts, while detailed tables may be appended for completeness.
Table 2: Charts vs. Tables: Application Guide
| Aspect | Best Use Cases for Charts | Best Use Cases for Tables |
|---|---|---|
| Primary Function | Showing trends, patterns, and relationships quickly [67]. | Presenting detailed, precise values for in-depth analysis [67]. |
| Data Type | Summarized or processed data for a general audience [67]. | Raw data for analytical audiences who need exact numbers [67]. |
| Ideal Context | Presentations, reports, and consent forms where visual impact and quick understanding are key [67]. | Scientific publications, technical appendices, and financial reports where precision is critical [67]. |
| Strengths | Engaging; simplifies complex data; reveals patterns [67]. | High precision; handles multidimensional data; less prone to misinterpretation of values [67]. |
| Weaknesses | Can lack specific details; may be misleading if scaled improperly [67]. | Requires more cognitive effort to see trends; can become crowded with large data volumes [67]. |
Data Visualization Best Practices for Readability
When creating charts or diagrams for participant-facing materials or publications, adhere to these principles to maximize clarity and accessibility.
- Choose the Right Chart: Use bar charts for comparisons, line charts for trends over time, and pie/doughnut charts sparingly for part-to-whole relationships with few categories [68] [69] [70].
- Maintain a High Data-Ink Ratio: Remove unnecessary chart elements like heavy gridlines, 3D effects, and distracting backgrounds. Every mark on the graphic should convey information [69] [70].
- Use Color Strategically and Accessibly:
- Use a limited palette of 5-7 colors to avoid overwhelming the viewer [70].
- Ensure sufficient contrast between text and its background. For standard text, the Web Content Accessibility Guidelines (WCAG) require a contrast ratio of at least 4.5:1, and 7:1 for enhanced contrast [71].
- Use tools like ColorBrewer to select colorblind-safe palettes. Do not rely solely on color to convey meaning [69].
- Establish Clear Context: Use descriptive titles and clear axis labels. Annotate key events or data points to guide interpretation [69].
- Start Axes at Zero for Bar Charts: Starting the y-axis above zero for bar charts can visually exaggerate differences and mislead the viewer [70].
The following workflow diagram synthesizes the key steps of the plain language review protocol into a visual guide.
The Scientist's Toolkit: Research Reagent Solutions for Plain Language Implementation
Table 3: Essential Tools for Plain Language Implementation
| Tool Name | Function | Application in Consent Form Development |
|---|---|---|
| Hemingway Editor | Checks readability grade level and highlights hard-to-read sentences [65]. | Used to quantitatively assess and iteratively improve the reading level of the draft ICF. |
| Microsoft Word Readability Statistics | Provides Flesch-Kincaid Grade Level score within the word processor [64]. | Integrated into the document creation process for ongoing readability checks during writing. |
| Plain Language Review Worksheet | A structured checklist to guide the evaluation of a document against plain language principles [64]. | Ensures a systematic and comprehensive review, preventing oversight of key elements. |
| Color Contrast Analyzer | Tools (e.g., WebAIM Contrast Checker) verify that text/background color pairs meet WCAG guidelines [71]. | Critical for designing accessible participant-facing materials, including charts and slides. |
| Organization Style Guide | Provides plain language definitions for key technical terms and standardizes usage [64]. | Promotes consistency and clarity in how recurring complex concepts are explained across all study documents. |
Therapeutic misconception (TM) occurs when research participants fail to recognize the fundamental differences between clinical research and ordinary therapeutic care [72]. This misconception constitutes a critical ethical challenge, as it can seriously undermine the validity of informed consent. Participants under therapeutic misconception inaccurately attribute a primacy of therapeutic intent and individualized care, typical of clinical settings, to research procedures [72]. The core of TM involves participants' failure to grasp that the risks they face from research protocols are inherently different from those involved in receiving ordinary treatment. This is particularly problematic in research involving vulnerable populations, where understanding and appreciation of research constraints are essential for ethical participation.
Theoretical Framework and Quantitative Evidence
Empirical Evidence of Risk Appreciation Failure
Intensive interviews with 155 subjects from 40 clinical trials revealed significant deficits in participants' appreciation of research-related risks. The data demonstrate that a majority of subjects sign consent documents with only minimal understanding of the specific disadvantages inherent to research design [72].
Table 1: Appreciation of Risks Among Clinical Trial Participants
| Category of Reported Risk/Disadvantage | Percentage of Subjects |
|---|---|
| None reported (despite explicit questioning) | 23.9% |
| Only incidental disadvantages (e.g., travel distance) | 2.6% |
| Only disadvantages associated with standard treatment | 14.2% |
| Only disadvantages of experimental intervention | 45.8% |
| Any risks from research design itself (e.g., randomization, blinding) | 13.5% |
Conceptualizing Vulnerability in Research
A systematic review of research ethics policy documents identifies that vulnerability is often conceptualized through three primary analytical accounts [13]:
- Consent-based accounts: Vulnerability stems from impaired capacity to provide free and informed consent due to conditions such as undue influence or reduced autonomy.
- Harm-based accounts: Vulnerability arises from a higher probability of incurring harm or injury during research participation.
- Justice-based accounts: Vulnerability originates from unequal conditions and opportunities among research subjects.
This framework is essential for developing targeted strategies to address therapeutic misconception in vulnerable populations, where barriers to understanding research nature are compounded by additional vulnerabilities.
Protocols for Managing Therapeutic Misconception
Comprehensive Consent Process Protocol
Objective: To ensure participants, particularly those from vulnerable populations, distinguish research participation from clinical care through a structured, culturally relevant consent process.
Materials:
- Simplified consent documents
- Visual aids and multimedia resources
- "Teach Back Method" toolkit
- Culturally adapted information sheets
- Trained interpreter services
Procedure:
Pre-Consent Preparation (1-2 weeks before consent)
- Identify potential participants using inclusion/exclusion criteria.
- Assess individual vulnerability factors using the analytical framework (consent-based, harm-based, justice-based).
- Prepare materials adapted to cultural, literacy, and linguistic needs.
- Engage community representatives for input on approach strategies.
Initial Disclosure Session (60-90 minutes)
- Begin with relationship building rather than immediate information delivery.
- Clearly state the fundamental difference between research and treatment using explicit statements: "This is research, not standard medical care."
- Explain key research design elements using straightforward language:
- Randomization: "You will be assigned to a group by chance, like flipping a coin."
- Blinding: "Neither you nor the researcher will know which treatment you receive."
- Protocol Restrictions: "Your treatment will follow a set plan rather than being adjusted specifically for you."
- Primary Purpose: "The main goal is to gain knowledge, not to provide you with the best possible treatment."
- Use visual aids to illustrate research design concepts.
- Allow time for questions and emotional processing.
Understanding Assessment (20-30 minutes)
- Apply the "Teach Back Method":
- Ask participants to explain in their own words the purpose of the study.
- Have them describe key procedures like randomization and blinding.
- Request they articulate at least three potential disadvantages of participation.
- Assess specifically for therapeutic misconception by asking:
- "How is being in this study different from regular doctor visits?"
- "Do you think the treatments you will receive in this study are chosen specifically for your personal benefit?"
- Document level of understanding and specific areas of confusion.
- Apply the "Teach Back Method":
Decision Counseling Session (48 hours later)
- Revisit areas of identified misunderstanding.
- Address new questions that may have emerged.
- Discuss potential impacts of participation on daily life.
- Provide additional resources for consultation (family members, community advisors).
Consent Documentation
- Use simplified consent forms with clear section headings.
- Include visual elements where appropriate.
- Ensure appropriate witness presence for vulnerable participants.
- Document the entire process, not just the signature.
Validation: Repeat understanding assessment at first study visit to reinforce concepts and identify persistent misconceptions.
Community Engagement Protocol
Objective: To enhance the social value of research and address therapeutic misconception through meaningful community partnership.
Procedure:
Community Identification
- Define community by geographic proximity, shared disease state, or shared identity.
- Map community power structures and influential stakeholders.
Partnership Development
- Establish community advisory boards with representation from vulnerable subgroups.
- Develop formal memoranda of understanding regarding roles and responsibilities.
- Implement training for both researchers and community members.
- Create mechanisms for ongoing communication and feedback.
Collaborative Research Design
- Involve community members in developing research questions and methodology.
- Jointly review informed consent processes and materials.
- Collaborate on recruitment strategies that minimize undue influence.
- Establish community standards for acceptable risk-benefit ratios.
Implementation and Monitoring
- Include community members in data collection where appropriate.
- Establish joint monitoring of participant understanding and experience.
- Create community feedback loops for study progress and findings.
Dissemination
- Develop community-friendly result summaries.
- Co-present findings at community forums.
- Ensure research benefits are shared with the community.
Table 2: Essential Research Reagent Solutions for Managing Therapeutic Misconception
| Item | Function | Application Notes |
|---|---|---|
| Simplified Consent Framework | Reduces complexity of standard consent forms; enhances comprehension | Use 6th-8th grade reading level; incorporate visual elements; limit to essential information |
| Cultural Adaptation Toolkit | Adapts materials to specific cultural contexts and literacy needs | Include visual aids, multimedia resources, and culturally appropriate examples; involve community representatives in development |
| Therapeutic Misconception Assessment Scale | Identifies and quantifies presence of therapeutic misconception | Administer pre- and post-consent; use open-ended questions about research purpose and design |
| Community Engagement Studio Model | Facilitates community input into research design and consent processes | Structured approach based on established models; requires trained facilitators; essential for vulnerable population research |
| "Teach Back" Method Protocol | Verifies participant understanding through explanation in own words | Standardized approach for assessing comprehension; requires documentation of participant explanations |
| Multimedia Consent Resources | Presents consent information through alternative modalities | Videos, interactive websites; particularly useful for low-literacy populations; requires technical infrastructure |
Workflow Diagram
Implementation and Ethical Considerations
Addressing Systemic Barriers
Implementation of these protocols requires addressing systemic barriers within research institutions and ethics review processes. Institutional Review Boards (IRBs) should strengthen requirements for research to yield "fruitful results for the good of society" by interpreting this to require that clinical research answers to the priorities of participating communities [73]. Current IRB procedures often mismatch with community-engaged research practices, creating obstacles such as:
- Advance copy requirements for community-facing materials that impede iterative development
- Time-consuming amendment processes for minor protocol changes based on community input
- CITI certification requirements that create barriers for community members
- Burdensome compensation documentation procedures
Cultural Adaptation Strategies
Research in vulnerable and multicultural contexts demonstrates that culturally relevant informed consent requires addressing several key factors [14]:
- Trust-building: Establishing sustained relationships rather than transactional interactions
- Power imbalances: Actively mitigating hierarchy between researchers and participants
- Timing and clarity: Providing information in manageable segments with clear language
- Gender and cultural dynamics: Adapting approaches to specific population characteristics
Effective strategies include using trained interpreters rather than family members, employing audio-visual methods to enhance understanding, and recognizing participants' intrinsic value beyond their research participation.
Managing therapeutic misconception requires a multifaceted approach that addresses both individual understanding and systemic research practices. The protocols outlined provide a framework for differentiating research from clinical care, particularly when working with vulnerable populations. By implementing structured consent processes, meaningful community engagement, and ongoing monitoring, researchers can enhance ethical practice while maintaining scientific rigor. Future work should focus on adapting these approaches to specific vulnerable populations and evaluating their effectiveness in reducing therapeutic misconception while promoting equitable participation in research.
Evaluating Consent Effectiveness and Comparing International Approaches
Application Note: Foundational Concepts and Current Landscape
AN-001: Within the ethical framework of research involving human participants, particularly vulnerable populations, the principles of comprehension and voluntariness are pillars of valid informed consent [74] [75]. A voluntary decision is characterized by an individual's intentional action, free from substantial controlling influences or coercion [76]. Despite their importance, studies indicate that participant understanding of key trial elements is often inadequate, and systematic assessment of this understanding is not a universal practice [77] [75]. A recent systematic review highlighted significant variability in the approaches used to measure participant understanding and identified only three tools with robust psychometric properties: the Deaconess Informed Consent Comprehension Questionnaire (DICCQ), the Participatory and Informed Consent (PIC) tool, and the Process and Quality of Informed Consent (P-QIC) [78]. This application note provides a structured overview of validated assessment tools and detailed protocols for their implementation to strengthen the process validity of informed consent in research involving vulnerable groups.
Table 1: Validated Tools for Assessing Informed Consent Comprehension
| Tool Name | Key Measured Constructs | Method of Administration | Psychometric Properties |
|---|---|---|---|
| Deaconess Informed Consent Comprehension Questionnaire (DICCQ) | Understanding of study procedures, risks, benefits, alternatives, randomization, and rights [78]. | Structured questionnaire or interview. | High validity and reliability [78]. |
| Participatory and Informed Consent (PIC) Tool | Participant understanding and the quality of the consent process [78]. | Not specified in detail; designed for participant reporting. | High validity and reliability [78]. |
| Process and Quality of Informed Consent (P-QIC) | Participant understanding and the quality of the consent process [78]. | Not specified in detail; designed for participant reporting. | High validity and reliability [78]. |
| Decision Making Control Instrument (DMCI) | Perceived voluntariness, with subscales for Self-Control, Absence of Control, and Others' Control [76]. | 9-item self-report questionnaire. | High internal consistency (α=0.83); construct validity established [76]. |
| Comprehension Assessment Tool (Sample) | Trial background, design, procedures, and participants' rights [79]. | Scored questionnaire (e.g., 28.9 ± 3.1 out of a maximum score) [79]. | Used in Phase I trials; scores can be analyzed by education level [79]. |
Table 2: Investigator Practices in Assessing Comprehension and Capacity (Survey Data)
| Research Context | Percentage Assessing Comprehension/Decisional Capacity | Percentage Using a Formal Questionnaire | Percentage Using a Validated Tool |
|---|---|---|---|
| All Research Studies (n=102) | Approximately 66% [77] | 9 of 102 respondents [77] | 3 of 102 respondents [77] |
| Pediatric Research | No statistically significant difference from adult research [77] | Not separately reported | Not separately reported |
| Interview/Questionnaire Studies | 64% (27 of 42) [77] | Not separately reported | Not separately reported |
| Procedure/Treatment Studies | 70% (42 of 60) [77] | Not separately reported | Not separately reported |
Experimental Protocols for Assessment
Protocol P-01: Comprehensive Comprehension Assessment Using a Validated Tool
Aim: To quantitatively evaluate a participant's understanding of a clinical trial's key elements prior to enrollment. Materials: Approved informed consent document, validated comprehension tool (e.g., DICCQ, PIC, P-QIC), quiet/private space for interaction. Procedure:
- Consent Discussion: The investigator or a trained consent educator conducts the standard informed consent discussion using the approved document [74].
- Low-Literacy Enhancements: For vulnerable populations or those with limited health literacy, integrate enhanced communication techniques:
- Use visual aids and graphics to represent key study concepts (e.g., randomization, timeline, procedures) [80].
- Apply the teach-back method, asking the participant to explain key concepts in their own words to ensure understanding [80].
- Simplify language, avoid jargon, and use ample white space in supporting materials [80].
- Assessment Administration: After the discussion, administer the selected validated comprehension tool. This can be a structured interview or a self-reported questionnaire.
- Scoring and Action:
- Score the assessment according to the tool's manual.
- If comprehension is inadequate, revisit misunderstood concepts using alternative explanations and re-assess. Do not proceed with enrollment until adequate understanding is confirmed.
- Documentation: Document the assessment process, scores, and any corrective steps taken in the research record.
Protocol P-02: Quantifying Perceived Voluntariness with the DMCI
Aim: To measure a participant's or parent's perception of the voluntariness of their decision to enroll in a research study. Materials: Decision Making Control Instrument (DMCI), which is a 9-item questionnaire measuring three oblique dimensions: Self-Control, Absence of Control, and Others' Control [76]. Procedure:
- Timing: Administer the DMCI after the participant or parent (for pediatric research) has made the decision to enroll or decline participation, ideally within 10 days of the decision [76].
- Administration: Provide the participant with the DMCI in a private setting, ensuring they understand that their responses are confidential and will not affect their care or participation.
- Data Collection: Collect the completed questionnaire.
- Scoring and Analysis:
- Score the instrument as a whole and for its three subscales [76].
- Higher scores on the Self-Control subscale indicate a greater perception of personal agency in the decision.
- The tool has demonstrated high internal consistency (0.83) and construct validity, correlating with measures of affect, trust, and decision self-efficacy [76].
- Use of Data: The results can be used for research purposes to understand factors influencing voluntariness and to refine the consent process to minimize undue influence.
Protocol P-03: Integrated Workflow for Consent Process Validity
The following diagram illustrates a comprehensive workflow for integrating assessments of comprehension and voluntariness into the informed consent process for research involving vulnerable populations.
Diagram 1: Integrated consent validity workflow.
The Scientist's Toolkit: Essential Reagents & Materials
Table 3: Research Reagent Solutions for Consent Process Validity
| Item Name | Function/Application in Consent Research |
|---|---|
| Validated Comprehension Tools (DICCQ, PIC, P-QIC) | Standardized instruments to quantitatively assess a participant's understanding of the research study's critical elements, ensuring the "informed" component of consent is met [78]. |
| Voluntariness Assessment Instrument (DMCI) | A psychometrically validated questionnaire to measure a participant's perception of control and freedom from coercion in the decision-making process [76]. |
| Low-Literacy Visual Aids & Graphics | Illustrative materials (e.g., study timelines, procedure diagrams) that augment text-heavy consent forms to improve comprehension among participants with limited health literacy or from diverse educational backgrounds [80]. |
| Teach-Back Technique Protocol | A structured communication method where participants are asked to explain study concepts in their own words, allowing the research team to identify and correct misunderstandings in real-time [80]. |
| Capacity Assessment Checklist | A guide for researchers to systematically evaluate a potential participant's capacity to understand, appreciate, reason, and express a choice regarding research participation, which is crucial for vulnerable groups [81]. |
The enrollment of vulnerable populations in research presents a fundamental ethical tension for Institutional Review Boards (IRBs) and researchers: balancing the imperative to protect potentially vulnerable individuals from harm and exploitation with the equally important principle of justice, which requires fair access to research benefits [50]. Federal regulations mandate that IRBs provide special consideration to vulnerable subjects, explicitly identifying populations including children, prisoners, pregnant women, mentally disabled persons, and economically or educationally disadvantaged persons [82] [83]. The ethical and legal validity of research participation hinges on a valid consent process, which requires that consent be voluntary, informed, and given by an individual with sufficient capacity [43].
Historically, protectionist policies have led to the systematic exclusion of vulnerable groups, particularly those with uncertain or impaired decision-making capacity [50]. Recent analysis indicates that 41.5% of institutions maintain policies that require exclusion of people with uncertain or impaired decision-making capacity unless inclusion is scientifically justified, while only 5.3% have policies that require inclusion unless exclusion is justified [50]. This protectionist stance faces increasing ethical and legal challenges, including updated regulations for Section 504 of the Rehabilitation Act that prohibit unnecessary exclusion of people with disabilities from research [50]. This evolving landscape requires researchers to develop sophisticated, ethically sound protocols that both protect and appropriately include vulnerable populations.
Understanding Vulnerability: A Multi-Dimensional Framework
Vulnerability in research ethics is not merely a label applied to specific groups, but rather a condition that can arise from various sources that may compromise an individual's ability to provide fully voluntary, informed consent. The IRB-SBS identifies eight distinct categories of vulnerability, providing researchers and IRBs with an analytical framework for identifying and addressing potential ethical concerns [16].
Table: Categories of Vulnerability in Human Subjects Research
| Vulnerability Category | Description | Common Populations Affected | Key Safeguards |
|---|---|---|---|
| Cognitive or Communicative | Inability to process, understand, or reason through consent information [16] | Individuals with mental disabilities, dementia, low literacy, language barriers [16] | Capacity assessment, surrogate consent, simplified documents, assent process [16] [84] |
| Institutional | Subject to formal authority structures where consent may be coerced [16] | Prisoners, students, employees [16] [82] | Third-party recruitment and consent, anonymity protections [16] |
| Deferential | Informal subordination to an authority figure [16] | Patients, abuse victims, spouse/partner relationships [16] | Sensitive recruitment plan, private consent environment [16] |
| Medical | Medical state may cloud judgment about research participation [16] | Terminally or acutely ill patients [16] [82] | Clear distinction between research and treatment, waiting periods [16] |
| Economic | Economic situation may unduly influence participation due to payments [16] | Economically disadvantaged persons [16] [82] | Reasonable payment that does not constitute undue inducement [16] |
| Social | Risk of discrimination based on race, gender, ethnicity, age, etc. [16] | Racial/ethnic minorities, underserved communities [16] [84] | Culturally competent consent process, diverse research team [16] |
| Legal | Lack of legal consent capacity or fear of legal repercussions [16] | Undocumented individuals, children, those engaged in illegal activities [16] [84] | Certificates of Confidentiality, alternative consent methods [16] |
| Study Vulnerability | Vulnerability created by the research design itself [16] | Participants in deception research [16] | Thorough debriefing, post-trial consent [16] |
This framework moves beyond broad categorizations toward a tailored approach where IRBs assess each participant's specific situation and the research context [16]. The fundamental question is whether prospective subjects are "likely to be vulnerable to coercion or undue influence" within the specific circumstances of the proposed research [84]. This requires researchers to carefully analyze their study design, recruitment methods, and participant population to identify which dimensions of vulnerability are relevant and what specific safeguards must be implemented.
Regulatory Framework and Quantitative Analysis of IRB Policies
The regulatory foundation for protecting human subjects derives from the Belmont Report's ethical principles and the Nuremberg Code, which established that "the voluntary consent of the human subject is essential" [43] [50]. These principles are codified in the Federal Regulations (45 CFR 46 and 21 CFR 50/56) which require IRBs to provide special protections for vulnerable populations [85] [83]. Specifically, 45 CFR 46.111(b) states that when some or all subjects are likely to be vulnerable to coercion or undue influence, "additional safeguards should be included in the study to protect the rights and welfare of these subjects" [84].
A recent cross-sectional study of IRB policies at 94 top-funded U.S. research institutions reveals significant variations in how institutions approach adults with uncertain or impaired decision-making capacity, a common vulnerability factor [50].
Table: Analysis of IRB Policies for Adults with Uncertain or Impaired Decision-Making Capacity
| Policy Element | Percentage of Institutions | Key Findings |
|---|---|---|
| Default Stance on Inclusion | 41.5% require exclusion unless inclusion is scientifically justified [50] | Protectionist approach remains dominant in institutional policies |
| Risk-Based Eligibility | 54.3% make eligibility dependent on research risks [50] | Majority recognize the need for risk-calibrated approaches |
| Consent/Assent Guidance | 77.7% provide guidance on obtaining consent or assent [50] | Most institutions offer some procedural direction |
| Capacity Assessment Guidance | 44.7% provide guidance on assessing decision-making capacity [50] | Less than half offer specific assessment methodologies |
| IRB Membership Requirements | 30.9% require IRB member knowledgeable about this population [50] | Minority ensure specialized expertise at the review level |
This data demonstrates that while most institutions provide some guidance on consent procedures, there are significant gaps in capacity assessment guidance and IRB expertise requirements. Furthermore, the predominant exclusionary default stance may violate principles of justice and, following recent updates to Section 504 of the Rehabilitation Act, potentially constitute disability discrimination by unnecessarily screening out people with cognitive disabilities [50].
Protocol Application: Special Requirements for Specific Vulnerable Populations
Federal regulations establish specific additional protections for certain vulnerable populations, particularly children, prisoners, and pregnant women/fetuses [84]. Researchers must be aware of these specific requirements when designing studies involving these populations.
Research Involving Children
Definition: Children are persons who have not attained the legal age for consent to treatments or procedures under applicable law [84].
Requirements: Research must be specifically approved by the IRB under one of three categories, each with distinct requirements for parental permission and child assent [84]:
- Minimal Risk Research: Requires permission of one parent and child assent when capable.
- Greater than Minimal Risk with Prospect of Direct Benefit: Requires permission of one parent and child assent when capable.
- Greater than Minimal Risk with No Prospect of Direct Benefit: Requires permission of both parents and child assent when capable; this category also has additional restrictions [84].
Protocol Application:
- Parental Permission: Develop a comprehensive parental permission document that contains all standard consent elements but is written from the perspective of a parent giving permission for their child's participation.
- Child Assent: Create an age-appropriate assent process that may include a simplified written document, verbal explanation, or other interactive methods to ensure the child understands what participation involves. The UC Davis IRB generally documents assent in the children's signature block on the consent template rather than requiring a separate document [84].
- Capacity Considerations: Implement a developmentally appropriate process to assess the child's understanding and willingness to participate, recognizing that capacity for assent varies with age, maturity, and psychological state.
Research Involving Prisoners
Definition: Any individual involuntarily confined or detained in a penal institution [84].
Requirements: Research must be specifically approved by the IRB and satisfy seven additional regulatory criteria beyond the standard requirements [84]. Note that some jurisdictions, including California, prohibit state prisoners from enrolling in clinical trials or other biomedical studies [84].
Protocol Application:
- IRB Review Considerations: The IRB must ensure that any advantages associated with participation do not impair a prisoner's ability to weigh the risks of the research against the value of such advantages in the limited-choice prison environment [84].
- Fair Subject Selection: Implement recruitment procedures that ensure selection of subjects is fair to all prisoners and not vulnerable to arbitrary or discriminatory practices.
- Parole Considerations: Include provisions to ensure that a prisoner's participation in research is not taken into account by parole boards, and clearly communicate this protection during consent.
- Follow-up Procedures: If follow-up examinations or procedures are necessary after the prisoner's release, these must be explained during consent, with clear plans for implementation.
Research Involving Adults with Impaired Decision-Making Capacity
Definition: Persons who have reached the legal age of consent but may lack the decision-making capacity to comprehend the consent process and voluntarily choose to participate [84].
Requirements: Adults who lack capacity to consent may only be enrolled in research under specific conditions, generally limited to research relating to their cognitive impairment, lack of capacity, or serious or life-threatening conditions, when the necessary study cannot be conducted using subjects who are not cognitively impaired [84].
Protocol Application:
- Capacity Assessment: Implement a validated capacity assessment tool appropriate for the study population and risk level. Document the assessment process and findings.
- Surrogate Decision-Makers: Identify and utilize Legally Authorized Representatives (LARs) according to state law and institutional policy to provide consent on behalf of potential subjects.
- Assent Process: Even when using surrogate consent, obtain assent from all adults who lack capacity but are capable of providing some agreement to participation.
- Dynamic Consent: For conditions where capacity may fluctuate, implement procedures to re-evaluate capacity throughout the study and obtain direct consent if capacity improves [83].
Diagram: Vulnerability Assessment and Safeguard Implementation Pathway
Experimental Protocols: Assessing Capacity and Implementing Consent Safeguards
Protocol 1: Decision-Making Capacity Assessment
Purpose: To systematically evaluate a potential research subject's capacity to provide informed consent, particularly when cognitive or communicative vulnerabilities are suspected.
Methodology:
- Initial Screening: Utilize a standardized screening tool appropriate to the population (e.g., MacArthur Competence Assessment Tool for Clinical Research [MacCAT-CR], University of California Brief Assessment of Capacity to Consent [UBACC]).
- Four Capacity Standards Assessment:
- Understanding: Assess ability to comprehend information about the research purpose, procedures, risks, benefits, and alternatives. Use teach-back method where subjects explain key concepts in their own words.
- Appreciation: Evaluate ability to apply the information to one's own situation and recognize potential consequences of participation.
- Reasoning: Assess comparative thought processes when considering different choices and their consequences.
- Expression of Choice: Document clear communication of a decision.
- Severity Threshold: Establish predetermined thresholds for acceptable performance on standardized measures, calibrated to study risk level.
- Documentation: Record assessment results, including specific areas of impairment if capacity is deemed limited.
Implementation Notes:
- For higher risk studies, implement more rigorous assessment with specialized psychological or neurological consultation when indicated.
- For fluctuating conditions, schedule capacity assessments at optimal times and consider repeated assessments at predetermined intervals.
- Ensure assessment tools are validated for the specific study population and available in appropriate languages and formats.
Protocol 2: Enhanced Consent Process for Vulnerable Populations
Purpose: To obtain valid informed consent while addressing specific vulnerabilities through process adaptations.
Methodology:
- Pre-Consent Preparation:
- Adapt consent materials to appropriate literacy level (aim for 8th-grade reading level for general adult populations) [43].
- Translate materials for non-English speakers and create accessible formats for visually or hearing impaired individuals.
- Prepare visual aids, simplified summaries, or interactive multimedia tools to enhance comprehension.
- Consent Environment:
- Conduct consent discussions in private settings free from potential coercive influences.
- For institutional or deferential vulnerability, utilize neutral third parties for consent discussions.
- Allow adequate time for information processing and questions, potentially across multiple sessions.
- Interactive Consent Discussion:
- Employ open-ended questions to assess understanding: "Can you tell me in your own words what this study involves?"
- Specifically address potential misconceptions, particularly for medically vulnerable populations who may confuse research with treatment.
- Clearly explain voluntary nature of participation and right to withdraw without penalty.
- Authorization and Documentation:
- Obtain signatures from subjects with adequate capacity or from legally authorized representatives when appropriate.
- For subjects with diminished but present capacity, obtain assent in addition to surrogate consent.
- Document the entire consent process, including specific measures taken to address vulnerabilities.
Table: Research Reagents and Tools for Ethical Vulnerability Assessment
| Tool/Reagent | Function | Application Context | Key Features |
|---|---|---|---|
| MacCAT-CR | Structured interview to assess decision-making capacity [50] | Higher-risk studies involving cognitively vulnerable populations | Evaluates understanding, appreciation, reasoning, and choice |
| UBACC | Brief screening tool for assessment of consent capacity [50] | Minimal risk studies or initial screening | 10-item scale, requires ~10 minutes to administer |
| Flesch-Kincaid Formula | Readability assessment for consent documents [43] | All consent form development | Provides grade-level score; available in Microsoft Word |
| Certificate of Confidentiality | Federal certificate protecting sensitive data [16] | Research with legally vulnerable populations | Protects against compulsory legal disclosure |
| LAR Designation Protocol | Process for identifying legally authorized representatives [84] | Research with adults lacking consent capacity | Follows state-specific hierarchy for surrogate decision-makers |
Ethical research with vulnerable populations requires moving beyond simplistic protectionism toward a nuanced approach that balances safeguard implementation with fair access. Researchers must recognize that "inability to consent does not limit participation in a study but instead requires that additional safeguards and consent procedures are followed" [16]. The evolving regulatory landscape, including updated Section 504 regulations, increasingly mandates that exclusionary practices must be scientifically justified rather than based on convenience or overbroad protectionist concerns [50].
Successful protocols will incorporate proactive vulnerability assessments, customized consent processes, and ongoing monitoring to ensure that ethical standards are maintained throughout the research lifecycle. Furthermore, researchers should advocate for and help develop IRB policies that promote appropriate inclusion while maintaining rigorous protections, ensuring that research evidence ultimately benefits all populations, including those most vulnerable.
Obtaining genuine informed consent is a cornerstone of ethical research, yet this process presents profound challenges in Low- and Middle-Income Countries (LMICs) and humanitarian settings. The fundamental principles of respect for persons, beneficence, and justice, as outlined in the Belmont Report, mandate a consent process that ensures information, comprehension, and voluntariness [86]. In stable, high-resource environments, standard written consent protocols may suffice. However, in contexts characterized by displacement, conflict, cultural diversity, and urgency, a rigid adherence to these standards can undermine ethical goals by excluding the most vulnerable populations from research participation or rendering consent a mere formality rather than a meaningful process.
This analysis synthesizes evidence-based consent models and practical protocols derived from global research. It is framed within a broader thesis on protecting autonomy in vulnerable populations research, arguing that ethical rigor is demonstrated not by uniform procedure, but by the adaptability and responsiveness of the consent process to specific contextual barriers and facilitators. The following sections provide a comparative analysis of documented challenges, evaluate adaptable consent frameworks, and present detailed protocols for implementation, equipping researchers and drug development professionals with the tools to uphold the highest ethical standards in complex global contexts.
Comparative Analysis of Challenges and Adaptive Strategies
Research in humanitarian emergencies and LMICs must navigate a unique constellation of barriers that can compromise the integrity of the informed consent process. A scoping review of informed consent in humanitarian emergencies identified 11 recurring challenges, which are summarized in the table below alongside evidenced strategies for mitigation [86].
Table 1: Key Challenges and Corresponding Mitigation Strategies in Humanitarian Settings
| Challenge | Description | Recommended Adaptive Strategy |
|---|---|---|
| Language & Cultural Context [86] [14] | Tailoring information to local language, cultural norms, and concepts of health and research; overcoming reliance on written text in oral cultures. | Engage local research communities and interpreters; use audio-visual aids; employ "Teach Back" method [86] [14]. |
| Lack of Trust & Power Imbalance [86] [14] | Historical exploitation, marginalization, or perceived authority of researchers leading to therapeutic misconception or coerced agreement. | Build sustained relationships with communities; ensure transparency on commercial interests; use reciprocal dialogue [86] [14]. |
| Vulnerability & Reduced Capacity [86] | Increased susceptibility to coercion due to trauma, displacement, or status (e.g., unaccompanied minors, undocumented persons). | Implement dynamic consent; provide adequate time for decision-making; use independent participant advocates [86]. |
| Security & Privacy Concerns [86] | Fear that data could endanger participants or their families (e.g., revealing undocumented status or political views). | Utilize robust data anonymization; secure data storage; clearly communicate safety protocols to participants [86]. |
| Literacy Barriers [86] | Standard written consent forms are inaccessible to individuals with low literacy or sensory impairments. | Use alternatives to written consent (oral consent witnessed by a third party); provide information in braille, audio, or sign language [86] [87]. |
A critical insight from recent literature is the role of emerging technologies, particularly Large Language Models (LLMs), in enhancing consent processes. LLMs can be powerful tools for translating and simplifying complex medical information into locally appropriate language. However, an ethical perspective cautions against using LLMs for "active empathy," which could create a misleading emotional connection. Instead, their use should be limited to "passive empathy"—recognizing and signaling patient distress cues like fear or uncertainty—and then alerting a human healthcare provider. This approach leverages the analytical strengths of AI while preserving the irreplaceable authenticity of human empathy in the clinical relationship [88].
A Framework for Consent: Selecting an Ethical Model
Given the diverse challenges, no single consent model is universally applicable. A practical framework for humanitarian settings proposes six types of consent, each suited to different levels of urgency, risk, and complexity [89]. The following diagram maps these models to guide researchers in selecting the most appropriate approach.
Consent Model Selection Workflow
Detailed Experimental Protocols for Ethical Implementation
Protocol 1: Culturally Grounded Consent Co-Development
This protocol is adapted from a study in Lebanon that used Design Thinking and Participatory Action Research (PAR) to create culturally relevant guidelines [14].
- Objective: To collaboratively develop and validate a context-specific informed consent process with affected communities.
- Materials:
- Recruitment materials co-designed with community representatives.
- Audio-recording equipment and secure storage.
- Facilitator guides for participatory workshops.
- Prototypes of consent materials (e.g., draft leaflets, visual aids, scripts for oral explanations).
- Methodology:
- Stakeholder Mapping and Engagement: Identify and engage key stakeholders, including local community leaders, potential research participants, healthcare workers, and cultural brokers.
- Participatory Workshops: Conduct a series of facilitated workshops with mixed groups of stakeholders.
- Activity 1: Problem Identification: Use open-ended questions to explore perceptions of research, trust, and decision-making.
- Activity 2: Solution Prototyping: Co-design consent materials and procedures. This may involve creating visual storyboards, simplifying language in information sheets, or role-playing consent discussions.
- Iterative Testing and Refinement: Test the prototype consent process with a small group from the target population. Use the "Teach Back" method—where participants explain the information back in their own words—to assess comprehension. Refine materials based on feedback.
- Guideline Finalization: Synthesize insights into a formal consent guideline for the specific research context and population.
- Outcome Measures: Level of participant comprehension assessed via Teach Back; qualitative feedback on the acceptability and perceived respectfulness of the process.
Protocol 2: Dynamic Consent for Longitudinal Studies in Displaced Populations
This protocol addresses the challenge of maintaining consent and engagement with refugee or internally displaced populations over time [86].
- Objective: To implement a consent process that allows participants ongoing control over their involvement and data use in a multi-year study.
- Materials:
- Mobile phone-based application (e.g., SMS-based system, lightweight app) or a paper-based booklet for participants with low connectivity.
- Multi-lingual information resources (short videos, icon-based instructions).
- Secure database to track and manage individual consent preferences.
- Methodology:
- Initial Consent with Tiered Options: At enrollment, present participants with clear, tiered options for participation (e.g., level of data collection, types of follow-up, future use of samples/data).
- Ongoing Communication: Establish a low-burden communication channel (e.g., quarterly SMS check-ins, annual phone calls) to update participants on study progress and remind them of their right to withdraw or change preferences.
- Preference Updates: Enable participants to easily update their consent preferences through the established channel. The system should log all changes to create a consent audit trail.
- Re-consent for Major Changes: If the study protocol undergoes significant changes, trigger a formal re-consent process using the initial tiered model.
- Outcome Measures: Participant retention rates; frequency and nature of consent preference changes; participant satisfaction with level of control.
Protocol 3: Ethical Integration of Large Language Models (LLMs) in Information Delivery
This protocol outlines a safe, assistive role for LLMs in the consent process, aligning with the principle of "passive empathy" [88].
- Objective: To use an LLM to improve the accessibility and comprehension of informed consent information without simulating human empathy.
- Materials:
- A secure, possibly offline, instance of a vetted LLM.
- Pre-approved, source consent documents.
- A device with a user interface for the researcher.
- Methodology:
- Information Simplification and Translation: The researcher inputs complex study information into the LLM with prompts to simplify the text to a target literacy level and translate it into the local language.
- Question Anticipation: The LLM can be used to generate a list of potential questions and clear answers that a participant might have, which the researcher can use to prepare for the consent discussion.
- Distress Keyword Monitoring: During the consent conversation, the researcher can use the LLM in real-time (via text input) to transcribe and flag participant statements that contain keywords indicating confusion, fear, or uncertainty (e.g., "I don't understand," "worried," "scared").
- Human-in-the-Loop Validation: The LLM's outputs are never shown directly to the participant. The flagged cues serve as an alert for the human researcher to pause, clarify, empathetically address the participant's concern, and confirm understanding.
- Outcome Measures: Time required to achieve participant comprehension; number of participant-initiated questions; researcher assessment of the tool's utility in identifying unspoken concerns.
The Scientist's Toolkit: Essential Reagents for Ethical Consent
Beyond conceptual frameworks, ethical consent requires practical tools. The following table details key "research reagents" – materials and methods – essential for conducting ethical consent processes in vulnerable populations.
Table 2: Essential Reagents for Ethical Consent in Global Contexts
| Research Reagent | Function & Application | Key Considerations |
|---|---|---|
| Multi-Format Information Sheets | Presents study information in accessible formats (e.g., large print, braille, audio, video, pictorial storyboards). | Essential for participants with sensory impairments or low literacy. Videos should include subtitles and sign language [87]. |
| Trained Cultural Interpreters | Facilitates accurate linguistic translation and cultural mediation between the research team and participants. | Crucial for navigating nuanced concepts. Avoid using family members or untrained staff to ensure accuracy and confidentiality [86] [14]. |
| Digital Consent Platforms | Manages dynamic consent preferences, sends reminders, and facilitates re-consent via mobile devices. | Must have low data usage, be usable on basic phones (SMS), and offer an offline analog option to prevent digital exclusion [86]. |
| Teach-Back & Feedback Scripts | Structured scripts for researchers to assess understanding by asking participants to explain the study back in their own words. | A validated method to confirm true comprehension beyond mere assent. Correct misunderstandings immediately [11] [14]. |
| Community Advisory Board (CAB) | A group of trusted community representatives who provide ongoing oversight and guidance on the research and consent process. | Builds trust, ensures cultural relevance, and serves as a conduit for community concerns throughout the study lifecycle [14]. |
This analysis demonstrates that ethical consent in LMICs and humanitarian settings is not a one-time signature but a dynamic, culturally resonant, and relationship-dependent process. The lessons from global contexts consistently point away from standardization and toward adaptation, co-creation, and continuous engagement. The proposed frameworks and detailed protocols provide a pathway for researchers to move beyond a compliance-based checklist approach to a truly ethical, participant-centered practice.
Future directions will be shaped by the responsible integration of technology, such as LLMs used as assistive tools for comprehension, and the continued development of context-specific guidelines. The ultimate goal is to democratize research participation, ensuring that vulnerability and context are not barriers to inclusion but imperatives for developing more robust, respectful, and ethical consent models. This evolution is critical for upholding the principles of equity and justice that underpin all research involving human subjects.
In research involving vulnerable populations, robust documentation and secure audit trails are fundamental to upholding the ethical principles of informed consent and process transparency. An audit trail is a secure, computer-generated, time-stamped log that records all actions related to electronic records, capturing who did what, when, and, where appropriate, why [90] [91]. For researchers working with vulnerable participants—such as detained individuals, those with limited health literacy, or patients in emergency settings—these systems provide an indelible record that helps ensure consent is obtained appropriately, voluntary participation is safeguarded, and the integrity of all research data is maintained [61] [80] [75]. This document outlines the application of compliant audit trail systems and detailed protocols to meet regulatory requirements and protect both participants and research integrity.
Regulatory Framework and Core Requirements
Audit trail requirements are mandated by multiple regulatory frameworks to ensure data integrity and trustworthiness. The following table summarizes the core requirements from key regulators.
Table 1: Core Audit Trail Requirements Across Regulatory Frameworks
| Regulatory Body / Guideline | Core Audit Trail Requirement | Key Citation |
|---|---|---|
| FDA 21 CFR Part 11 | Use of secure, computer-generated, time-stamped audit trails to independently record the date and time of operator entries and actions that create, modify, or delete electronic records. Record changes must not obscure previously recorded information. [92] [91] | |
| EU Annex 11 (GMP) | Based on a risk assessment, a system-generated audit trail should record all GMP-relevant changes and deletions. The reason for change must be documented. Audit trails must be available, intelligible, and regularly reviewed. [92] | |
| ICH E6(R3) Good Clinical Practice (GCP) | Ensures that audit trails, reports, and logs are not disabled. Stipulates that audit trails should not be modified except in rare, justified circumstances with maintained logs of such actions. [92] | |
| OECD GLP Principles | Promotes a risk-based approach to data lifecycle management, requiring data to be attributable, legible, contemporaneous, original, and accurate (ALCOA+), evidenced by immutable audit trails. [90] |
The foundational principle across all regulations is that audit trails must be automated, secure, and tamper-evident [90]. They must capture:
- Attributability: The identity of the user or instrument responsible for the action [90] [91].
- Action and Context: The specific event (create, edit, delete, etc.), the affected record, and the previous and new values [90] [91].
- Timestamp: The exact date and time of the action from a controlled system clock [90] [91].
- Reason for Change: Where required, the rationale for the modification [92] [90].
Experimental Protocol: Audit Trail Review and Management
This protocol provides a detailed methodology for the regular review of audit trails associated with electronic informed consent systems and related research data.
Purpose
To define a standardized procedure for the review of audit trails to ensure the integrity of electronic records related to the informed consent process and participant data in research involving vulnerable populations.
Scope
This protocol applies to all principal investigators, data managers, quality assurance personnel, and study coordinators responsible for the management, review, and oversight of electronic data in studies involving vulnerable populations.
Materials and Reagents
Table 2: Essential Research Reagents and Solutions for Audit Trail Management
| Item / Solution | Function / Application |
|---|---|
| Compliant Electronic Data Capture (EDC) System | A computerized system designed for clinical research that generates and maintains a secure, 21 CFR 11-compliant audit trail for all data entries and modifications. [90] [91] |
| Write-Once-Read-Many (WORM) Storage or Immutable Cloud Archive | A storage solution that prevents the alteration or deletion of audit trail files and original records, ensuring long-term data integrity and endurance. [90] |
| Controlled Time Server | A secure time source synchronized to a recognized standard to ensure all audit trail timestamps are accurate and contemporaneous. [90] |
| Unique User Credentials | Individualized login IDs and passwords to ensure all actions in the system are attributable to a specific individual. [90] [91] |
Procedure
Pre-Review Configuration
- Define Critical Data: In the study protocol or a separate data integrity plan, identify which data points are considered critical to the study's conclusions and the informed consent process. This includes, but is not limited to, participant eligibility criteria, consent form versioning and signatures, and primary outcome measures [92] [90].
- Establish Review Frequency: Determine the schedule for audit trail reviews:
- Regular Review: For critical data, the audit trail should be reviewed in conjunction with the data itself, and before final approval of the data set [91].
- Scheduled Periodic Review: For system-wide integrity, a periodic review (e.g., weekly, monthly) of all audit trail entries should be performed based on a risk assessment [91].
Execution of Review
- Access the Audit Trail: Log into the EDC or data management system and navigate to the audit trail viewer for the specific record or data set under review.
- Verify Completeness: Confirm that every creation, modification, or deletion of a data point is recorded in the audit trail. There should be no unexplained gaps in the data history [90].
- Scrutinize Individual Entries: For each entry, verify the following against the ALCOA++ principles:
- Attributable: Is the user identity clearly recorded and authorized for that action?
- Legible & Contemporaneous: Is the entry human-readable and does the timestamp match the expected workflow sequence?
- Original & Accurate: Are the old and new values recorded accurately?
- Reason for Change: For critical data modifications, is a valid reason provided (e.g., "correcting data entry error," "updating based on source documentation")? [92] [90]
- Identify Anomalies: Flag any instances of:
- Changes made by unauthorized users.
- Modifications to critical data without a documented reason.
- A high frequency of changes from a single user that could indicate a problem with training or data integrity.
- Changes made outside of expected working hours without a valid clinical reason.
Post-Review Actions
- Document the Review: The reviewer must document the completion of the audit trail review, including the date, scope of the review, any anomalies found, and the reviewer's signature.
- Investigate and Resolve Anomalies: All flagged anomalies must be investigated promptly. The investigation, root cause, and corrective/preventive actions (CAPA) must be fully documented.
- Archive Records: Ensure that the audit trails are retained for the required period (often as long as the subject electronic records, which can be 10-15 years or more) and are readily available for regulatory inspection [90] [91].
Workflow Visualization: Informed Consent and Audit Trail Lifecycle
The following diagram illustrates the integrated lifecycle of the informed consent process and its associated audit trail in research involving vulnerable populations.
Application Notes: Tailoring for Vulnerable Population Research
Enhancing Comprehension with Transparency: For vulnerable populations, such as participants with limited health literacy or detained individuals, the consent process itself must be tailored using low-literacy communication techniques, visual aids, and the teach-back method [80]. A robust audit trail provides a transparent record that these adaptive measures were followed correctly, demonstrating that genuine informed consent was sought. This is crucial when overall understanding of consent information may be low, as noted in some vulnerable groups [61].
Waivers of Consent in Emergency Research: In emergency care research where informed consent may be waived for vulnerable, incapacitated patients, the role of documentation and audit trails becomes even more critical [75]. The audit trail must immutably record the justification for the waiver, the approval from the ethics committee, and all subsequent data entries. This creates a defensible chain of custody for data obtained under these exceptional circumstances, ensuring that the rights and welfare of the participant are protected despite the lack of prospective consent.
System Selection for Compliance: When selecting electronic systems for managing informed consent and research data, it is imperative to verify that the system has built-in, non-disableable audit trail functionality that meets regulatory standards. Systems without adequate audit trail capabilities are not acceptable in a modern, regulated research environment [92] [90].
Application Notes and Protocols
Protocol for Implementing Interactive Digital Interventions
Objective: To enhance comprehension, engagement, and autonomy in the informed consent process for vulnerable populations through interactive digital methods.
Experimental Methodology:
- Platform: Web-based interactive program structured into multiple learning units (e.g., 6 units) [93].
- Interactive Features: Integrate videos, quizzes, and scenario-based discussions that simulate real-life decision-making contexts [93].
- Theoretical Framework: Ground the intervention in Life Skills Theory and Health Literacy (functional, communicative, and critical literacy) to build resilience and decision-making capacity [93].
- Procedure:
- Pre-Assessment: Administer baseline tests measuring knowledge, health literacy, and engagement.
- Intervention Delivery: Participants engage with the self-paced digital program.
- Post-Assessment: Re-administer tests after intervention completion.
- Evaluation Metrics: Use validated scales to measure knowledge gains, functional literacy, critical literacy, communicative literacy, cognitive engagement, and emotional engagement [93].
Quantitative Efficacy Data: Table 1: Efficacy of Interactive Digital Interventions on Consent-Related Competencies
| Outcome Measure | Pre-Test Mean (SD) | Post-Test Mean (SD) | Statistical Significance (p-value) |
|---|---|---|---|
| Knowledge | Baseline | Post-Intervention | < .01 [93] |
| Health Literacy | Baseline | Post-Intervention | < .01 [93] |
| Functional Literacy | Baseline | Post-Intervention | < .01 [93] |
| Critical Literacy | Baseline | Post-Intervention | .01 [93] |
| Communicative Literacy | Baseline | Post-Intervention | .02 [93] |
| Learner Engagement | Baseline | Post-Intervention | < .01 [93] |
Protocol for Developing and Using Culturally Relevant Simplified Forms
Objective: To create and deploy informed consent forms and processes that are accessible and meaningful across diverse cultural and literacy levels.
Experimental Methodology:
- Design Framework: Utilize a Design Thinking (DT) and Participatory Action Research (PAR) framework to collaboratively develop materials with the target community [14].
- Key Simplification Strategies:
- Language & Literacy: Translate forms and use plain language. Involve trained interpreters and community members in the process to ensure clarity and cultural relevance [14].
- Trust-Building: Acknowledge power imbalances and focus on building sustained relationships. Frame the researcher-participant relationship as a "reciprocal dialogue" [14].
- Timing and Clarity: Allow sufficient time for the consent process. Ensure forms are concise and straightforward [14].
- Verification Technique: Employ the "Teach Back Method", where participants explain the information back in their own words to confirm understanding [14].
- Alternative Formats: Supplement paper forms with audio-visual methods (e.g., explanatory videos, websites) to aid understanding, especially in oral cultures [14].
Quantitative Efficacy Data: Table 2: Impact of Process and Presentation on Informed Consent
| Intervention Strategy | Reported Effect | Key Metric |
|---|---|---|
| Personalized Digital Content | Significantly improved success rates in health interventions [94]. | Relative Risk (RR) 1.86 [94] |
| Interactive SMS Messages | More than doubled quit rates in smoking cessation studies [94]. | Relative Risk (RR) 2.14 [94] |
| Multimedia & Visual Aids | Improved understanding and engagement, particularly in low-literacy populations [14]. | Participant comprehension and recall |
| Teach Back Method | Enhanced verified understanding of consent information [14]. | Accuracy of participant recall |
Protocol for Multimedia and Technology-Driven Consent
Objective: To leverage specific technology types to improve the reach, engagement, and effectiveness of consent information delivery.
Experimental Methodology:
- Technology Comparison: Compare the efficacy of different digital delivery channels, such as SMS, mobile apps, telephone calls, and emails, in randomized controlled trials [94].
- Content Customization:
- Evaluation: Measure outcomes like point prevalence abstinence for health interventions or, by analogy, correct comprehension of consent key points [94].
Quantitative Efficacy Data: Table 3: Comparative Efficacy of Digital Intervention Types
| Technology Type | Relative Efficacy (vs. Standard Care) | Statistical Certainty |
|---|---|---|
| Interactive Apps | Highest relative efficacy (P-score 0.95) [94] | Very Low (Wide CI) [94] |
| Interactive SMS | RR 2.14 [94] | Moderate [94] |
| SMS (Standard) | RR 1.63 - 1.72 [94] | Low to Very Low [94] |
| Telephone | RR 1.59 [94] | Low [94] |
| Multicomponent | RR 1.56 [94] | Low [94] |
| Web-Based | RR 1.30 [94] | Low [94] |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Digital and Simplified Consent Research
| Item / Solution | Function / Application |
|---|---|
| Web-Based Interactive Platform | Hosts modular content (videos, quizzes, scenarios) for scalable, standardized intervention delivery [93]. |
| Plain Language Guidelines | Provide a framework for simplifying complex trial information to an accessible reading level without losing scientific accuracy [14]. |
| Multimedia Kits (Audio/Video) | Create supplementary consent materials to overcome literacy barriers and cater to oral culture traditions [14]. |
| Digital Data Analytics Suite | Tracks participant engagement metrics (time spent, quiz results, module completion) for objective process evaluation [93] [95]. |
| Validated Engagement & Literacy Scales | Quantitatively measure outcomes like cognitive/emotional engagement and functional/critical health literacy pre- and post-intervention [93]. |
| Structured Teach-Back Script | A standardized tool to verify participant understanding qualitatively and ensure informed consent is genuinely achieved [14]. |
Conclusion
Safeguarding the informed consent process for vulnerable populations is a dynamic ethical imperative that requires moving beyond a one-time signature to a culturally sensitive, continuous dialogue. Success hinges on integrating foundational ethical principles with adaptable methodologies—such as simplified documents, the teach-back method, and e-consent—tailored to specific vulnerabilities. Proactively addressing comprehension barriers, power dynamics, and situational coercion is essential for genuine voluntariness. Future efforts must focus on developing standardized, evidence-based validation tools for consent comprehension and promoting equitable inclusion to ensure that scientific progress does not come at the cost of exploiting those most in need of protection and benefit. The future of ethical research lies in a participant-centric model that balances rigorous science with profound respect for human autonomy.
References
- 1. An Overview of Instruments to Assess Vulnerability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427976/]
- 2. Common Rule Research Alert: New Proposed "Federal ... [https://www.hinshawlaw.com/en/insights/healthcare-alert/common-rule-research-alert-new-proposed-federal-policy-for-the-protection-of-human-subjects]
- 3. With the Right Approach, Vulnerable Populations Can and ... [https://acrpnet.org/2025/10/29/with-the-right-approach-vulnerable-populations-can-and-should-be-engaged-in-research]
- 4. Still Timely After All These Years: How the Belmont Report ... [https://acrpnet.org/2025/08/06/still-timely-after-all-these-years-how-the-belmont-report-continues-to-shape-research-ethics]
- 5. Regulatory Focus on Vulnerable Populations in Clinical ... [https://www.linkedin.com/pulse/regulatory-focus-vulnerable-populations-clinical-research-rudy-malle-qxy8e]
- 6. Trendspotting: Predictions for Clinical Research in 2025 [https://www.clinicalresearchnewsonline.com/news/2025/01/07/trendspotting-predictions-for-clinical-research-in-2025]
- 7. Revised Common Rule - Institutional Review Board [https://www.belmont.edu/irb/common-rule.html]
- 8. Global Regulatory Trends for 2025: What Life Sciences ... [https://www.mrlcg.com/resources/blog/global-regulatory-trends-for-2025--what-life-sciences-companies-need-to-know/]
- 9. Principles of Clinical Ethics and Their Application to Practice [https://pmc.ncbi.nlm.nih.gov/articles/PMC7923912/]
- 10. Guide to medical law and ethics in healthcare [https://www.medicalprotection.org/uk/guidance/medical-ethics]
- 11. Informed Consent - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK430827/]
- 12. Ethical Principles [https://www.cdc.gov/niosh/learning/safetyculturehc/module-5/11.html]
- 13. Vulnerability in research ethics: A systematic review of policy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12212517/]
- 14. Developing guidelines for culturally relevant informed consent [https://journals.plos.org/mentalhealth/article?id=10.1371/journal.pmen.0000174]
- 15. Factors Influencing Informed Consent Preferences in ... [https://www.jmir.org/2025/1/e63349/]
- 16. Vulnerable Participants [https://hrpp.research.virginia.edu/teams/irb-sbs/researcher-guide-irb-sbs/vulnerable-participants]
- 17. The concept of 'vulnerability' in research ethics: an in-depth ... [https://health-policy-systems.biomedcentral.com/articles/10.1186/s12961-016-0164-6]
- 18. Vulnerability in research ethics: A systematic review of policy ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0327086]
- 19. Chasing 'vulnerability' across six decades of the ... [https://link.springer.com/article/10.1007/s40592-025-00235-4]
- 20. Considerations for enrolling Vulnerable Populations in ... [https://tfscro.com/resources/regulatory-considerations-for-enrolling-vulnerable-populations-in-clinical-trials/]
- 21. Advances and challenges in conducting ethical trials ... [https://www.sciencedirect.com/science/article/abs/pii/S1551714420301324]
- 22. Guidance for best practices for clinical trials [https://www.who.int/our-work/science-division/research-for-health/implementation-of-the-resolution-on-clinical-trials/guidance-for-best-practices-for-clinical-trials]
- 23. Digital Informed Consent/Assent in Clinical Trials Among ... [https://humanfactors.jmir.org/2025/1/e65569]
- 24. a qualitative study of clinical research nurses' experiences [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-023-07844-6]
- 25. Ethics and Consent in Research with Vulnerable Participants [https://researchmethodscommunity.sagepub.com/blog/ethics-and-consent-in-research-with-vulnerable-participants]
- 26. Vulnerability in research ethics: A systematic review of ... [https://pubmed.ncbi.nlm.nih.gov/40591537/]
- 27. Aspects of vulnerable patients and informed consent in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3551442/]
- 28. The Impact of Language Barriers on Documentation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2078548/]
- 29. Language Barriers, Informed Consent, and Effective ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5515794/]
- 30. 'Some parts of the consent form are written using complex ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-024-01147-4]
- 31. Designing e-consent protocols for pragmatic clinical trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC11331622/]
- 32. Comparative Effectiveness of eConsent: Systematic Review [https://pmc.ncbi.nlm.nih.gov/articles/PMC10504628/]
- 33. Lessons learned obtaining informed consent in research with... [https://bmcresnotes.biomedcentral.com/articles/10.1186/1756-0500-5-624]
- 34. Opportunities for eConsent to enhance consumer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7540460/]
- 35. Journal of Medical Internet Research - Implementation of Electronic... [https://www.jmir.org/2020/10/e19129]
- 36. Approaches and experiences implementing remote, electronic ... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-024-08149-y]
- 37. The benefits of fully electronic consent management and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12516701/]
- 38. eConsent Study Provides Insights to Shape Industry Adoption [https://www.appliedclinicaltrialsonline.com/view/econsent-study-provides-insights-shape-industry-adoption]
- 39. Guidance: Electronic Informed Consent [https://research.lehigh.edu/policies-guidance-forms/guidance-electronic-informed-consent]
- 40. Differences in eConsent among diagnosis groups [https://www.sciencedirect.com/science/article/pii/S2451865423001461]
- 41. 知情同意過程常見問題案例探討 [https://www.ntuh.gov.tw/RECO/FormData!detail.action?af=152112]
- 42. Verbal consent in biomedical research: moving toward a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11906376/]
- 43. The Requirements for Informed Consent (Series #1) [https://www.tc.columbia.edu/institutional-review-board/irb-blog/2025/informed-consent-the-requirements-for-informed-consent-series-1/]
- 44. Oral/Verbal Consent [https://hrpp.research.virginia.edu/teams/irb-sbs/researcher-guide-irb-sbs/consent/oralverbal-consent]
- 45. How to obtain informed consent for research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5980471/]
- 46. Use the Teach-back Method - NIDDK [https://www.niddk.nih.gov/health-information/professionals/clinical-tools-patient-management/diabetes/game-plan-preventing-type-2-diabetes/how-talk-patients-about-prediabetes-diagnosis/use-teach-back-method]
- 47. Tools for Unmoderated Usability Testing [https://www.nngroup.com/articles/unmoderated-user-testing-tools/]
- 48. 11 Best UX Research Tools to Test in 2025 [https://www.fullsession.io/blog/best-ux-research-tools/]
- 49. Ongoing Consent & Re-Consent - One UNC Clinical Research [https://clinicalresearch.unc.edu/playbooks/my-study-lifecycle/study-conduct/ongoing-consent-and-re-consent/]
- 50. An Analysis of Institutional Review Board Policies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12227281/]
- 51. Research with Adults Lacking Capacity to Consent [https://www.wcgclinical.com/insights/navigating-ethical-challenges-research-with-adults-lacking-capacity-to-consent/]
- 52. An evaluation of the process of informed consent [https://pmc.ncbi.nlm.nih.gov/articles/PMC8371296/]
- 53. Drafting the Informed Consent Form - UCI Office of Research [https://research.uci.edu/human-research-protections/subject-enrollment/informed-consent/drafting-the-informed-consent-form/]
- 54. CONSORT 2025 explanation and elaboration - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11995452/]
- 55. Developing informed consent materials for non-English- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6218315/]
- 56. Non-English Speaking Research Subjects: What's in the ... [https://www.advarra.com/blog/non-english-speaking-research-subjects-whats-regs/]
- 57. Improving Consent Processes for Clinical Research Using ... [https://www.pcori.org/research-results/2019/improving-consent-processes-clinical-research-using-public-deliberation-methods]
- 58. Preventing Coercion and Influence in Research Consent [https://www.solutionsirb.com/preventing-coercion-and-influence-in-research-consent/]
- 59. How IRBs view and make decisions about coercion and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3604028/]
- 60. Safeguarding Vulnerable in Social Work Populations Research [https://www.numberanalytics.com/blog/safeguarding-vulnerable-populations-in-social-work-research]
- 61. in Informed : The Case of Detained... Consent Vulnerable Populations [https://pubmed.ncbi.nlm.nih.gov/40340590/]
- 62. Dealing with information overload: a comprehensive review [https://pmc.ncbi.nlm.nih.gov/articles/PMC10322198/]
- 63. March 2025 - Center for Informed Consent Integrity [https://ge2p2global-centerforinformedconsentintegrity.org/2025/03/]
- 64. How to conduct a plain language review [https://www.mass.gov/info-details/how-to-conduct-a-plain-language-review]
- 65. Write in plain language - Innovation Hub [https://hub.innovation.ca.gov/content-design/principles/write-in-plain-language/index.html]
- 66. Recommended format for a 'research protocol' [https://www.who.int/groups/research-ethics-review-committee/recommended-format-for-a-research-protocol]
- 67. Charts vs. Tables: When to Use One Over the Other? [https://wpdatatables.com/charts-vs-tables/]
- 68. 7 Types of Comparison Charts for Effective Data Visualization [https://ninjatables.com/types-of-comparison-charts/?srsltid=AfmBOoqQsjoTC4y2vnLwpGcSd9t6N8C4inTPEF_QGezlrkuYe-Gjg2j5]
- 69. 10 Essential Data Visualization Best Practices for 2025 [https://www.timetackle.com/data-visualization-best-practices/]
- 70. 9 Key Data Visualization Best Practices for 2025 [https://querio.ai/article/data-visualization-best-practices]
- 71. has enhanced Text | ACT contrast | WAI | W3C Rule [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 72. Therapeutic misconception and the appreciation of risks in ... [https://www.sciencedirect.com/science/article/abs/pii/S0277953603003381]
- 73. An Antidote to the Social Value Misconception - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12459346/]
- 74. Improving participant comprehension in the informed consent ... [https://www.ncbi.nlm.nih.gov/books/NBK74087/]
- 75. A review of informed consent and how it has evolved ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7047905/]
- 76. The Decision Making Control Instrument to Assess Voluntary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3175347/]
- 77. Methods and Practices of Investigators for Determining ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2826361/]
- 78. Measuring and evaluating participant understanding ... - Sciety [https://sciety.org/articles/activity/10.21203/rs.3.rs-7375295/v1?utm_source=sciety_labs_article_page]
- 79. Development of tool for the assessment of comprehension ... [https://www.sciencedirect.com/science/article/abs/pii/S1551714411001388]
- 80. Advancing Informed Consent for Vulnerable Populations [https://pmc.ncbi.nlm.nih.gov/articles/PMC4338326/]
- 81. Ethical Considerations When Vulnerable Populations are ... [https://rethinkingclinicaltrials.org/news/grand-rounds-ethics-and-regulatory-series-january-13-2023-ethical-considerations-when-vulnerable-populations-are-subjects-in-pragmatic-trials-emily-a-largent-jd-phd-rn/]
- 82. Vulnerable Populations :: Institutional Review Board [https://www.swarthmore.edu/institutional-review-board/vulnerable-populations]
- 83. 111.8 Organization Policy on Research Involving ... [https://www.hopkinsmedicine.org/institutional-review-board/guidelines-policies/organization-policies/111-8]
- 84. Vulnerable Populations - IRB - UC Davis [https://irb.ucdavis.edu/project-guidance/vulnerable-pops/]
- 85. Institutional Review Boards Frequently Asked Questions [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/institutional-review-boards-frequently-asked-questions]
- 86. Scoping review and thematic analysis of informed consent in ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-024-01125-w]
- 87. Strategies to Enhance Inclusion in Informed Consent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12477491/]
- 88. Large language models for surgical informed consent [https://pubmed.ncbi.nlm.nih.gov/40074323/]
- 89. Navigating Ethical Consent in Humanitarian Settings [https://hereiamstudio.com/insights/ethical-consent-humanitarian-research]
- 90. GLP Audit Trails: A Guide to Compliant File Systems [https://intuitionlabs.ai/articles/glp-compliant-file-system-audit-trails]
- 91. What are the FDA audit trail requirements for clinical trials? [http://www.agathalife.com/en/resources/what-are-the-fda-audit-trail-requirements-for-clinical-trials]
- 92. Audit Trail Requirements for a Digitalized Regulated Lab [https://www.technologynetworks.com/informatics/articles/audit-trail-requirements-for-a-digitalized-regulated-laboratory-401729]
- 93. Effectiveness of an Interactive Digital Intervention Program ... [https://www.jmir.org/2025/1/e76109]
- 94. Efficacy of digital interventions for smoking cessation by ... [https://www.nature.com/articles/s41562-025-02295-2]
- 95. Digital interventions in mental health: An overview and future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12051054/]