Ethical Research with Vulnerable Populations: Balancing Protection, Participation, and Progress
This article provides a comprehensive guide for researchers and drug development professionals on the ethical engagement of vulnerable populations in clinical research.
Ethical Research with Vulnerable Populations: Balancing Protection, Participation, and Progress
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on the ethical engagement of vulnerable populations in clinical research. It explores the foundational ethical principles and historical context that shape current guidelines, offers methodological frameworks for obtaining genuine informed consent and building trust, addresses common challenges like dual-role conflicts and study termination ethics, and validates approaches against contemporary issues such as globalization and digital health. The content synthesizes the latest systematic reviews and case studies to deliver actionable strategies for conducting rigorous, ethical, and inclusive research.
From Belmont to Today: Defining Vulnerability and Learning from History
The ethical conduct of research is foundational to the integrity of the scientific enterprise and the protection of society. Historical abuses of human subjects, such as those uncovered in the Tuskegee Syphilis Study and Nazi medical experimentation, highlighted the critical need for a formalized ethical framework [1]. In response, the 1978 Belmont Report established three core principles—Respect for Persons, Beneficence, and Justice—which form the cornerstone of modern research ethics regulations and practice [1]. These principles provide a systematic framework for analyzing ethical issues and guiding researcher conduct.
Within the context of a broader thesis on vulnerable populations in research ethics, these principles take on heightened significance. Vulnerability in research is defined as "an identifiably increased likelihood of incurring additional or greater wrongs" due to participation [2]. The Belmont Report itself notes that "persons with diminished autonomy are entitled to protection," directly linking the ethical principles to the protection of vulnerable subjects [3]. This guide explores the application of these principles specifically within the context of research involving vulnerable populations, providing researchers, scientists, and drug development professionals with both the theoretical understanding and practical tools necessary for ethical research conduct.
The Principle of Respect for Persons
The principle of Respect for Persons incorporates two fundamental ethical convictions: first, that individuals should be treated as autonomous agents, and second, that persons with diminished autonomy are entitled to protection [1]. An autonomous person is "an individual capable of deliberation about personal goals and acting under the direction of such deliberation" [1]. This principle manifests primarily through the requirements for informed consent and additional protections for vulnerable populations.
Informed Consent in Practice
Informed consent is not merely a form to be signed, but rather an ongoing process of communication that ensures a potential subject understands the research and voluntarily agrees to participate [4]. The Belmont Report outlines the key elements necessary for valid informed consent:
- Information: Prospective subjects must be provided with all material information about the research, including its purpose, procedures, risks, benefits, and alternatives [1].
- Comprehension: The information must be presented in a manner and language that the subject can understand, acknowledging varying capacities for comprehension [1].
- Voluntariness: Agreement to participate must be given without coercion or undue influence, ensuring the decision is free and autonomous [1].
Application to Vulnerable Populations
Vulnerable populations often face challenges that compromise their ability to provide fully autonomous informed consent. Two dominant approaches to understanding vulnerability have emerged in research ethics: the categorical approach and the contextual approach [3].
Table 1: Approaches to Vulnerability in Research Ethics
| Approach | Description | Examples of Vulnerable Groups | Limitations |
|---|---|---|---|
| Categorical Approach | Considers certain groups or populations as inherently vulnerable [3]. | Children, prisoners, pregnant women, economically disadvantaged persons, persons with cognitive impairments [3] [1]. | Does not address persons with multiple vulnerabilities or variation within groups; may over-generalize [3]. |
| Contextual Approach | Identifies situations and contexts that render individuals vulnerable [3]. | A capable CEO experiencing chest pain in an ER; a non-native language speaker; a patient in a deferential doctor-patient relationship [3]. | Requires more nuanced assessment by researchers and IRBs; less prescriptive [3] [5]. |
For individuals with compromised capacity, such as those with dementia or cognitive impairments, the consent process requires special adaptations. Process consent is a method in which consent is viewed as ongoing rather than a one-time event, with continuous checks for understanding and willingness to continue [6]. When prospective participants lack capacity, researchers must identify a legally authorized representative (surrogate) to give permission for enrollment, while still finding ways to involve the person with diminished capacity in decision-making to the greatest extent possible [2] [6].
The Principle of Beneficence
The principle of Beneficence entails an obligation to act for the benefit of others by minimizing possible harms and maximizing potential benefits [1]. This principle goes beyond simply "do no harm" (nonmaleficence) to include actively promoting the welfare of research participants [7]. For vulnerable populations, this principle requires a careful and systematic assessment of risks and benefits.
Risk-Benefit Assessment
A favorable risk-benefit ratio is a cornerstone of ethical research [4]. Researchers must meticulously analyze potential risks, which can be physical, psychological, social, or economic, and work to minimize them [4] [1]. Simultaneously, potential benefits to the participant and to society must be identified. The doctrine of double effect is relevant here, where an action with a foreseen but unintended harmful effect (e.g., opioid sedation for pain relief) may be ethically permissible if the intended action is beneficial [7].
Table 2: Risk-Benefit Assessment Framework for Vulnerable Populations
| Assessment Component | Key Considerations for Vulnerable Populations | Protective Safeguards |
|---|---|---|
| Nature & Scope of Risks | Vulnerable groups may be at higher risk for certain physical, psychological, or social harms [5]. Risks must be contextual, not just categorical [3]. | Implement additional monitoring; consult with community representatives; use staged consent processes [3]. |
| Potential Benefits | Ensure benefits are not overstated ("therapeutic misconception"); consider whether the vulnerable group will have access to proven benefits [4]. | Clear communication of uncertainties; post-trial access plans; alignment of research with health needs of the community [4] [8]. |
| Risk Minimization | Requires special consideration of the vulnerable group's specific circumstances and capacities [2]. | Use of plain language; independent participant advocates; data safety monitoring boards [3] [4]. |
Methodological Considerations
The principle of beneficence also demands scientific validity [4]. A study must be designed in a way that will yield reliable and actionable results. It is unethical to expose participants, especially vulnerable ones, to any risk in a study that is so poorly designed that it cannot answer the research question [4]. This requires careful attention to study design, sample size, and statistical analysis to ensure the research is valid and feasible.
The Principle of Justice
The principle of Justice addresses the fair distribution of the burdens and benefits of research [1]. Historically, the burdens of research often fell disproportionately on vulnerable populations, while the benefits flowed primarily to more privileged groups [1]. This principle demands a careful examination of the selection of research subjects.
Fair Subject Selection
The primary basis for recruiting participants should be the scientific goals of the study—not vulnerability, privilege, or ease of availability [4]. Fair subject selection requires that:
- Populations that are likely to benefit from the research should not be excluded without a compelling scientific reason [4].
- Groups should not be targeted for research simply because of their easy availability, compromised position, or manipulability [1].
- There should be a fair distribution of the burdens of research across different societal groups, avoiding the systematic selection of any group due to their vulnerability [1].
Vulnerability and Justice
The link between justice and vulnerability is profound. A justice-based account of vulnerability points to unequal conditions and/or opportunities for research subjects as a source of vulnerability [5]. The systematic exclusion of vulnerable groups from research can also be a violation of justice, as it may prevent these populations from benefiting from the knowledge gained through research [5] [2]. The goal is to avoid both the underprotection of vulnerable groups (by exploiting them in research) and their overprotection (by systematically excluding them, thus limiting the generalizability of research findings and their access to potential benefits) [5].
Experimental Protocols and Ethical Safeguards
Institutional Review and Oversight
The Institutional Review Board (IRB) is a primary mechanism for ensuring ethical research conduct. IRBs provide independent review of research proposals to protect the rights and welfare of human subjects [4] [1]. When research involves vulnerable populations, the IRB's role is particularly critical. Researchers must provide the IRB with a detailed plan outlining how they will address the specific vulnerabilities of the participant population, including adequate safeguards and a robust informed consent process [3] [1].
Recent updates to federal regulations, such as the 2024 Public Health Service (PHS) Policies on Research Misconduct, emphasize the importance of institutional responsibilities in maintaining research integrity, including clearer requirements for investigations and extended timelines for inquiries [9]. These regulatory frameworks provide the structure for holding researchers accountable.
Protocol for Research with Cognitively Vulnerable Populations
Research Question: What is the experience of care among individuals living with early-stage dementia?
Ethical Justification: Including persons with dementia in research that affects their treatment and care is essential for developing person-centered interventions. Exclusion challenges ethical practice by silencing their voices [6].
Methodology & Ethical Safeguards:
- Capacity Assessment: Implement a structured, objective capacity assessment prior to enrollment, using tools validated for research consent in dementia [2].
- Process Consent: Adopt a "process consent" model, where consent is reaffirmed throughout the research journey. Before each data collection session, briefly re-explain the study and confirm continued assent [6].
- Surrogate Consent: For participants who lack capacity to provide independent informed consent, obtain permission from a legally authorized representative [2] [6].
- Assent and Dissent: Even when surrogate consent is obtained, respect the participant's ongoing expression of assent (willingness) or dissent (withdrawal). Any sign of distress or opposition should be honored immediately [6].
- Caregiver Involvement: Enroll primary caregivers with their own informed consent, as they may be more involved as the participant's cognitive impairment worsens [2].
The Scientist's Toolkit: Essential Materials for Ethical Research
Table 3: Research Reagent Solutions for Ethical Practice
| Tool/Reagent | Function in Ethical Research |
|---|---|
| Validated Capacity Assessment Tools | Provides an objective measure of a potential participant's understanding and decision-making capacity, crucial for research with cognitively impaired populations [2]. |
| Plain-Language Consent Templates | Facilitates true comprehension by presenting information in clear, accessible language, avoiding technical jargon. May require cultural adaptation and translation [3] [4]. |
| Independent Participant Advocate | A third party, unaffiliated with the research team, who can help the participant understand their rights and ensure participation is voluntary, particularly important for institutional or deferential vulnerability [3]. |
| Data Anonymization & Encryption Software | Protects participant confidentiality and privacy, a key aspect of Respect for Persons and Beneficence, by securing data and removing identifiable information [1]. |
| Cultural & Linguistic Consultation Services | Ensures research materials and the consent process are respectful and comprehensible across language and cultural barriers, addressing communicative vulnerability [3] [10]. |
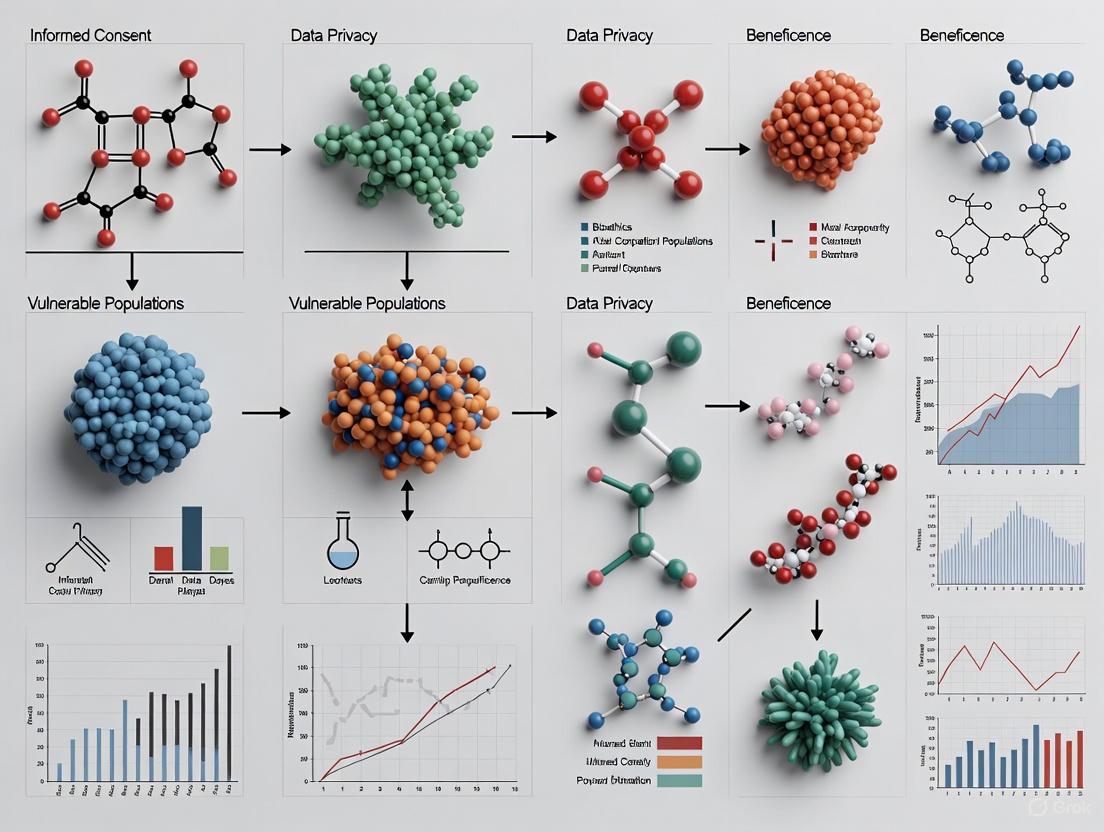
Visualizing the Ethical Framework
The following diagram illustrates the logical relationship between the core ethical principles, their practical applications, and the overarching goal of protecting vulnerable populations in research.
The core ethical principles of Respect for Persons, Beneficence, and Justice provide an indispensable framework for conducting research with vulnerable populations. Moving beyond a rigid, categorical view of vulnerability to a more nuanced, contextual understanding allows researchers to identify specific sources of vulnerability and implement proportionate safeguards. This involves robust informed consent processes, meticulous risk-benefit analyses, and a steadfast commitment to fair subject selection. As the research landscape evolves, with new challenges such as those highlighted during the COVID-19 pandemic and addressed by frameworks like the PREPARED Code [8], the continued application of these principles ensures that the pursuit of scientific knowledge remains firmly grounded in the protection of human dignity, rights, and welfare. For researchers, this is not merely a regulatory obligation but a fundamental professional responsibility.
The history of clinical research is marked by profound ethical failures that have irrevocably shaped modern regulatory frameworks. The examination of three pivotal cases—the Nazi medical experiments, the Tuskegee Syphilis Study, and the Willowbrook hepatitis studies—reveals a consistent pattern of exploitation where autonomous decision-making was systematically denied to vulnerable populations. These historical violations directly catalyzed the development of foundational ethical documents, beginning with the Nuremberg Code in 1947, which established the non-negotiable requirement for voluntary informed consent [11] [12]. The legacy of these abuses extends beyond the creation of rules; it instilled a fundamental principle that continues to guide research ethics: the protection of vulnerable populations is paramount to conducting morally justifiable research.
This whitepaper analyzes these historical cases through the lens of vulnerability, examining how systemic power imbalances and compromised consent capacities led to egregious harms. Furthermore, it traces the evolution of ethical thought from the Nuremberg Code through the Belmont Report to contemporary guidelines, which have progressively refined the concept of vulnerability from a simple categorical approach to a more nuanced analytical framework [5] [13]. For researchers, scientists, and drug development professionals, understanding this history and its enduring legacy is not an academic exercise but a professional imperative. It provides the essential context for the rigorous ethical standards and oversight mechanisms that underpin legitimate clinical research today [12].
Historical Case Studies: Analysis of Ethical Violations
The following cases represent critical benchmarks in the history of research ethics. Each exemplifies unique ethical failures and collectively highlighted the urgent need for formal protections for human participants.
The Nuremberg Code (1947)
Background and Context: The Nuremberg Code was formulated in 1948 in direct response to the atrocities committed by Nazi physicians during World War II [14] [11]. An American military war crimes tribunal prosecuted 23 Nazi physicians and administrators for conducting lethal and traumatic medical experiments on concentration camp prisoners without their consent [11]. These experiments included exposure to extreme temperatures, low air pressures, ionizing radiation, and infectious diseases, as well as wound-healing and surgical studies, including vivisections [14]. The judicial condemnation of these acts resulted in the codification of ten standards for physicians to follow when carrying out experiments on human participants.
Ethical Violations and Core Principles: The Nazi experiments constituted the most fundamental violations of ethical principles. They were characterized by a complete absence of voluntary consent, the infliction of extreme harm and suffering, and the use of a coerced and captive population [14] [12]. The experiments were designed not for the benefit of the participants, but for state interests, such as advancing military medicine. In the subsequent "Doctors' Trial," the defendants argued that no international law differentiated between legal and illegal human experimentation, highlighting a critical regulatory gap [15].
The resulting Nuremberg Code established ten standards, with the first and foremost principle being voluntary consent, which it describes as "absolutely essential" [11]. Other key standards include the right of a participant to withdraw, the requirement that experiments should yield fruitful results for the good of society, and the principle that a study should never be conducted if there is reason to believe death or disabling injury may occur [11]. It placed the responsibility for ensuring ethical conduct squarely on the researcher.
The Tuskegee Syphilis Study (1932-1972)
Background and Context: The U.S. Public Health Service conducted a 40-year observational study titled the "Untreated Syphilis Study in the Negro Male" in Tuskegee, Alabama [16]. The study aimed to document the natural progression of syphilis in 400 African American men who had the disease, alongside a control group of 201 men without it [16] [11]. The participants were primarily poor, rural sharecroppers who were offered incentives such as free medical examinations, free meals, and burial insurance [11]. Crucially, they were not informed of their diagnosis; researchers told them they were being treated for "bad blood" [16] [11].
Ethical Violations and Core Principles: The Tuskegee study is a landmark case of pervasive ethical failure rooted in injustice and deception.
- Lack of Informed Consent: Researchers never collected informed consent from participants and deliberately withheld information about their disease [16].
- Withholding of Treatment: The most egregious violation was the deliberate denial of treatment. Even after penicillin became the standard, effective treatment for syphilis in the 1940s, researchers actively prevented participants from accessing it [16] [11] [12].
- Injustice and Vulnerability: The study targeted a socially and economically vulnerable population—disadvantaged African American men [11]. The risks and burdens of the research were placed entirely on this group, while the potential benefits of understanding the disease were for society at large, a clear violation of the principle of justice [11].
- The study ended in 1972 only after a news story alerted the public and Congress to its ethical problems [14] [16]. A subsequent advisory panel concluded the study was ethically unjustified. In 1997, President Bill Clinton issued a formal presidential apology on behalf of the U.S. government [16] [11].
The Willowbrook Hepatitis Study (1956-1970)
Background and Context: From 1956 to 1970, researchers conducted studies at the Willowbrook State School, a New York institution for "mentally handicapped" children [11] [12]. The research aimed to study the course of viral hepatitis and the effectiveness of an immunoglobulin for inoculating against it [11]. Willowbrook was severely overcrowded, housing over 6,000 residents in a facility designed for 4,000, and conditions were deplorable, with insufficient food, attendants, or sanitation [17].
Ethical Violations and Core Principles: The ethical breaches at Willowbrook involved the exploitation of a highly vulnerable population and a coercive consent process.
- Intentional Infection of Children: Researchers deliberately infected children with the hepatitis virus [11]. They administered the virus to newly admitted children, often disguised within a "vaccination" protocol [11].
- Coerced Parental Consent: While some form of consent was obtained from parents, the context was highly coercive. The school was overcrowded, and there is evidence that the institution only admitted children whose parents gave permission for them to be in the study, holding admission hostage to recruitment [17] [11] [12]. This represents a profound undue influence.
- Exploitation of the Vulnerable: The participants were children with intellectual disabilities, a group with diminished autonomy and a high degree of vulnerability. They were institutionalized and could not advocate for themselves, making them easy subjects for exploitation [12].
- Public Exposure and Legacy: The horrific conditions at Willowbrook were exposed to the public in 1972 by journalist Geraldo Rivera, whose footage showed children "rotting" in their own waste [17]. This exposé fueled public outrage and a class-action lawsuit, which culminated in a 1975 consent decree mandating improved conditions and the deinstitutionalization of residents [17].
Table 1: Comparative Analysis of Major Ethical Violations in Human Subjects Research
| Case Study | Dates | Vulnerable Population | Key Ethical Violations | Primary Ethical Principle Violated |
|---|---|---|---|---|
| Nazi Experiments | 1939-1945 | Concentration camp prisoners [14] | - Non-consensual, fatal experiments- Intentional infliction of harm [12] | Respect for Persons, Beneficence |
| Tuskegee Syphilis Study | 1932-1972 | African American men [16] | - Lack of informed consent- Withholding of known treatment (penicillin) [16] [11] | Justice, Respect for Persons |
| Willowbrook Hepatitis Study | 1956-1970 | Children with intellectual disabilities [11] [12] | - Intentional infection with pathogen- Coerced parental consent [11] | Respect for Persons, Beneficence |
The Evolution of Ethical Protections and Conceptualizing Vulnerability
The historical violations detailed above served as catalysts for the development of increasingly sophisticated ethical frameworks and regulations designed to protect human research participants.
From Nuremberg to Belmont: A Timeline of Ethical Guidance
The progression of ethical thought can be traced through several key documents that built upon the lessons of past abuses:
- The Nuremberg Code (1947): Established the absolute necessity of voluntary consent and laid down nine other standards for ethical research, shifting responsibility to the investigator [11].
- The Declaration of Helsinki (1964): Adopted by the World Medical Association, this declaration addressed research on patient populations and explicitly stated that the interests of the individual patient must take precedence over the interests of society [11]. It has been revised multiple times to address emerging ethical challenges.
- The Belmont Report (1979): This seminal report, created in direct response to the Tuskegee scandal, identified three core ethical principles that should guide research involving human subjects [5] [11]:
- Respect for Persons: Recognizing the autonomy of individuals and protecting those with diminished autonomy. This principle is operationalized through the process of informed consent.
- Beneficence: The obligation to maximize possible benefits and minimize possible harms. This is applied through a systematic assessment of risks and benefits.
- Justice: The requirement to ensure the fair distribution of the burdens and benefits of research. This addresses the selection of subjects to avoid exploiting vulnerable populations [11].
The following diagram illustrates the causal relationship between historical abuses and the development of these major ethical codes:
Conceptualizing Vulnerability in Research Ethics
The notion of vulnerability was formally introduced into research ethics through The Belmont Report, which defined vulnerable people as those in a "dependent state and with a frequently compromised capacity for free consent," citing examples such as racial minorities, the very sick, and the institutionalized [5] [13]. Since then, policy documents and guidelines have struggled to operationalize this concept. A systematic review of research ethics policy documents reveals two primary approaches to conceptualizing vulnerability [5] [13]:
The Group-Based (or Categorical) Approach: This traditional approach identifies specific groups as inherently vulnerable. Common categories include children, prisoners, pregnant women, individuals with intellectual or mental disabilities, and economically or educationally disadvantaged persons [5]. This approach is pragmatically simple for ethics committees but can be over-inclusive and stigmatizing.
The Analytical Approach: This more recent and nuanced approach focuses on the potential sources or contexts that create vulnerability, rather than predefined groups. It includes three main accounts:
- Consent-based accounts: Vulnerability stems from a compromised capacity to provide voluntary, informed consent due to undue influence, coercion, or reduced autonomy.
- Harm-based accounts: Vulnerability is defined as a higher probability of incurring harm or exploitation during research.
- Justice-based accounts: Vulnerability arises from systemic, social, or economic inequalities that lead to unfair distribution of research burdens and benefits [5] [13].
Table 2: Analytical Framework for Sources of Vulnerability in Research
| Source of Vulnerability | Definition | Historical Example |
|---|---|---|
| Consent-Based | Compromised capacity for autonomous, informed decision-making due to coercion, undue influence, or diminished mental capacity. | Willowbrook parents coerced into consenting for their child's admission [17] [11]. |
| Harm-Based | Increased susceptibility to physical, psychological, social, or economic harm as a result of research participation. | Nazi experiment subjects and Tuskegee participants who suffered death and disability [14] [12]. |
| Justice-Based | Systemic inequities leading to the unfair selection of and burden placed on particular populations. | Selection of exclusively African American men for the Tuskegee study [16] [11]. |
The following diagram maps the relationship between historical cases, the vulnerable groups involved, and the primary sources of their vulnerability:
The Modern Legacy: Applications and Contemporary Challenges
The legacy of historical violations is deeply embedded in the everyday practice of clinical research, from protocol design to regulatory oversight. The ethical frameworks born from past failures provide guidance for navigating modern complexities.
The Scientist's Toolkit: Essential Components for Ethical Research
The following table details key components derived from ethical guidelines that are now non-negotiable for conducting research with human participants.
Table 3: Essential Components for Ethical Clinical Research
| Component | Function in Upholding Ethics | Originating Principle/Document |
|---|---|---|
| Informed Consent Form | Documents the process of providing full information and obtaining voluntary, comprehending agreement from a participant. | Nuremberg Code [11], Respect for Persons (Belmont) [11] |
| Institutional Review Board (IRB)/Ethics Committee | An independent committee that reviews research protocols to ensure ethical soundness and the protection of participants' rights and welfare. | Declaration of Helsinki [12], The Belmont Report [12] |
| Protocol-Benefit/Risk Analysis | A systematic assessment within the research protocol to justify the risks posed to participants by the potential benefits of the knowledge gained. | Beneficence (Belmont) [11], Declaration of Helsinki [11] |
| Vulnerability Assessment | A proactive evaluation to identify potential sources of vulnerability among the proposed participant population and to outline additional safeguards. | The Belmont Report [11], CIOMS/ICH-GCP Guidelines [5] |
| Data Safety Monitoring Board (DSMB) | An independent group of experts that monitors participant safety and treatment efficacy data while a clinical trial is ongoing. | Beneficence (Belmont), post-Tuskegee regulatory refinement [12] |
Contemporary Ethical Challenges
While modern regulations are robust, new ethical challenges continuously emerge, requiring researchers to apply foundational principles in novel contexts [12]:
- Globalization of Clinical Trials: Conducting research in low- and middle-income countries raises concerns about informed consent in different cultural contexts, the standard of care provided to control groups, and the potential for exploitation of economically disadvantaged populations [12]. The principle of justice demands that host communities have access to the fruits of the research.
- Inclusion vs. Protection of Vulnerable Populations: There is a necessary tension between protecting vulnerable groups from potential harm and ensuring their equitable representation in research. Over-protection can lead to a lack of data on how treatments work in these populations, perpetuating health inequities [5] [12]. The modern trend is toward carefully managed inclusion with additional safeguards, rather than blanket exclusion.
- Emerging Technologies: The use of artificial intelligence, genomic data, and digital health tools poses new challenges regarding informed consent for data re-use, data privacy, and algorithmic fairness [12]. These technologies can also create new vulnerable groups, such as those marginalized by algorithmic bias.
The historical violations of Tuskegee, Willowbrook, and the Nazi era are not merely dark chapters in a closed book. They are living history whose lessons are codified in the very fabric of modern clinical research ethics. These cases unequivocally demonstrate that without rigorous ethical frameworks and constant vigilance, scientific curiosity can override human dignity, particularly for the most vulnerable among us.
The evolution from the Nuremberg Code to the analytical approach to vulnerability represents a maturation of ethical thought—from a reactive set of rules to a proactive, principle-based system. For today's researchers, scientists, and drug development professionals, this legacy imposes a solemn responsibility. It is not enough to simply comply with regulations. True ethical conduct requires a deep-seated commitment to the principles of respect, beneficence, and justice, and a critical self-awareness that acknowledges the potential for vulnerability in all research contexts. By embedding these principles into every stage of research—from design and recruitment to publication and post-trial access—the scientific community can honor the victims of past abuses by ensuring that their legacy is the unwavering protection of every human participant.
What Makes a Population Vulnerable? Moving Beyond Labels to an Analytical Approach
The protection of vulnerable populations is a cornerstone of modern research ethics, yet the operationalization of this concept often relies on outdated categorical models. Historically, guidelines have used a "labeling approach," identifying vulnerability based solely on an individual's membership in a predefined group, such as children, prisoners, or the economically disadvantaged [13]. This method, while pragmatically simple for research ethics committees, risks being both over-inclusive and under-inclusive. It may fail to identify vulnerable individuals outside standard categories while also applying unnecessary protections to group members not actually experiencing vulnerability in a specific research context [13] [5].
Contemporary ethical discourse now champions a shift toward an "analytical approach" that focuses on the specific sources and contexts that create vulnerability [13] [5]. This framework moves beyond mere categorization to diagnose the underlying conditions that compromise free and informed consent, increase risk of harm, or perpetuate injustice. This technical guide provides researchers, scientists, and drug development professionals with the conceptual tools and practical methodologies to implement this analytical approach, ensuring both ethical rigor and equitable participation in research.
Core Analytical Frameworks: Deconstructing Vulnerability
The analytical approach to vulnerability dissects the concept into three primary normative accounts, each focusing on a distinct source of compromised ethical standing in research settings. The following diagram illustrates the structure of this analytical framework.
Consent-Based Accounts
This framework locates vulnerability primarily in impairments to the capacity for providing free and informed consent [13] [5]. Vulnerability arises when potential participants have a compromised ability to understand the research, appreciate its consequences, or voluntarily decide without undue influence. This can stem from intrinsic factors (e.g., cognitive impairments, developmental stage) or extrinsic factors (e.g., coercive pressures in hierarchical relationships) [18]. For instance, a prisoner's consent may be considered vulnerable not merely due to their status as an inmate, but because the institutional context creates a potential for coercion or undue inducement that must be specifically assessed and mitigated [13].
Harm-Based Accounts
This perspective defines vulnerability in relation to a heightened probability of incurring physical, psychological, social, or economic harm during research [13] [5]. The focus is on the participant's relative inability to absorb or recover from research-related risks. For example, a patient with a terminal illness may be vulnerable not simply because of their diagnosis, but because their compromised physical state makes them more susceptible to the side effects of an experimental therapy or less able to cope with additional burdens. This account requires a contextual analysis of the specific research interventions in relation to the participant's resilience and resources [18].
Justice-Based Accounts
Justice-based accounts point to unequal conditions and opportunities as the source of vulnerability [13] [5]. This framework emphasizes distributive justice, focusing on populations that have been historically underrepresented in research or unfairly burdened by it. Vulnerability arises from systemic factors that limit access to the benefits of research participation or disproportionately expose groups to risks. This includes populations experiencing health disparities due to social determinants of health, such as poverty, discrimination, or lack of access to care [19]. The core ethical imperative here is to ensure fair inclusion and address health inequities through research.
Operationalizing the Analytical Framework: Assessment and Application
The table below translates traditional vulnerable population categories into their potential vulnerability sources according to the analytical framework, demonstrating that single groups often face multiple, overlapping sources of vulnerability that require distinct safeguards.
Table 1: Analytical Mapping of Traditionally Vulnerable Populations
| Population Category | Primary Vulnerability Sources | Contextual Factors Modifying Risk |
|---|---|---|
| Children & Minors [18] | Consent-Based (developing decision-making capacity) [13] | Age, maturity, psychological state, family dynamics [18] |
| Pregnant Women [18] | Harm-Based (risk to fetus and mother) [18] | Stage of pregnancy, availability of pre-clinical toxicity data [18] |
| Prisoners [13] | Consent-Based (institutional coercion) [13] | Prison conditions, nature of the research, potential for parole |
| Economically/Educationally Disadvantaged [13] | Justice-Based (unfair access) & Consent-Based (undue inducement) [13] [5] | Level of disadvantage, social context, research topic |
| Cognitively Impaired [18] | Consent-Based (impaired comprehension/capacity) [13] [18] | Fluctuation in capacity, availability of LARs, study complexity [18] |
| Terminally Ill [18] | Harm-Based (increased susceptibility) & Consent-Based (therapeutic misconception) [13] | Prognosis, availability of standard treatment, level of pain/distress |
Methodologies for Contextual Vulnerability Assessment
Implementing the analytical approach requires structured methodologies to replace categorical checklists.
Systematic Review Protocol for Policy Analysis: A rigorous methodology for analyzing how vulnerability is conceptualized involves systematic reviews of policy documents following PRISMA-Ethics guidance [13] [5]. The process includes:
- Search Strategy: Comprehensive searching of policy sources (e.g., International Compilation of Human Research Standards), databases (PubMed, Web of Science), and grey literature (Google Scholar) using structured search strings [5].
- Screening & Data Extraction: Independent screening of documents against eligibility criteria, followed by extraction of data pertaining to definitions, listed populations, justifications, and provisions [13] [5].
- Qualitative Analysis: Using frameworks like the QUAGOL methodology to analyze and synthesize findings, identifying recurring patterns and conceptual gaps in policy guidance [5].
Staged Review Process for Research Ethics Committees (RECs): A practical protocol for RECs and researchers to apply the analytical approach involves:
- Protocol-Driven Identification: Requiring researchers to justify not only if vulnerable populations are included, but to analyze why they might be vulnerable in the specific study context.
- Source-Specific Safeguard Matching: Mandating that proposed safeguards (e.g., independent consent monitors, data safety monitoring boards) are directly linked to the identified sources of vulnerability (consent, harm, justice) rather than applying generic protections [18] [19].
- Ongoing Monitoring: Implementing continued ethics review to assess if vulnerability profiles change during the research, requiring re-consent or additional safeguards [18].
Effectively engaging with vulnerable populations requires specialized tools and resources to translate ethical principles into practice.
Table 2: Essential Research Reagent Solutions for Vulnerable Populations Research
| Tool/Resource | Function/Purpose | Application Example |
|---|---|---|
| Bilingual Research Assistants [19] | Overcome language barriers; ensure accurate translation of consent materials and data collection; build trust with non-English speaking participants. | Recruiting and conducting informed consent and interviews with Spanish-speaking participants in their native language [19]. |
| Legally Authorized Representative (LAR) Protocols [18] | Provide a structured mechanism for obtaining informed consent on behalf of potential participants who lack decision-making capacity. | Outlining in the study protocol the conditions for seeking surrogate consent for individuals with fluctuating cognitive impairment [18]. |
| Data Safety Monitoring Board (DSMB) [18] | Provide independent oversight of study data and participant safety, particularly crucial when risks are uncertain or participants have diminished resilience. | A DSMB conducts interim analyses to recommend trial continuation, modification, or termination based on emerging benefit-risk data for a vulnerable group [18]. |
| Trauma-Informed Interview Guides [19] | Semi-structured guides developed with clinical expertise (e.g., from Licensed Clinical Social Workers) to minimize re-traumatization during data collection. | An LCSW reviews and refines an interview guide for survivors of violence to ensure questions are phrased sensitively and avoid psychological harm [19]. |
| Community Advisory Board (CAB) [19] | Integrate community perspectives into research design and conduct; ensure cultural appropriateness; build mutual trust and respect. | A CAB comprising community members provides feedback on recruitment strategies and consent form readability for a study involving homeless individuals [19]. |
The movement from a label-based to an analytical approach in identifying vulnerable populations represents a critical evolution in research ethics. This framework provides researchers and ethics committees with a more precise, contextual, and ethically robust methodology for safeguarding participant rights and well-being. By systematically analyzing the sources of vulnerability—whether rooted in consent, harm, or justice—and deploying tailored safeguards, the research community can better fulfill its dual imperative: to protect participants from harm while ensuring their equitable inclusion in the benefits of scientific research. This nuanced practice is fundamental to conducting ethically sound and socially responsible science.
Within research ethics, vulnerability serves as a crucial regulatory category, signaling to researchers and ethics committees that some participants may be at an increased risk of harm or wrong [20]. Since its formal introduction in the 1979 Belmont Report, the concept has been central to safeguarding participants, yet its conceptualization and application have been subjects of ongoing debate [5] [21] [20]. A significant advancement in this discourse is the emergence of an analytical approach to vulnerability, which moves beyond merely listing vulnerable groups to examining the underlying sources and contexts that create vulnerability [5] [21]. This approach is structured around three primary normative justifications: consent-based, harm-based, and justice-based accounts [5]. Understanding these distinct yet sometimes overlapping justifications is essential for researchers, scientists, and drug development professionals to design and conduct ethically sound research that adequately protects all participants.
Theoretical Foundations of the Three Accounts
The analytical approach to vulnerability seeks to identify the specific conditions and sources that render a potential research participant vulnerable. The following table summarizes the core principles, sources, and implications of the three primary accounts.
Table 1: Comparative Analysis of Normative Justifications for Vulnerability
| Account of Vulnerability | Core Ethical Principle | Source of Vulnerability | Key Question for Researchers | Protective Measures |
|---|---|---|---|---|
| Consent-Based | Respect for Persons / Autonomy [5] [20] | Compromised capacity for autonomous decision-making and informed consent due to cognitive impairment, undue influence, or coercion [5] [21]. | Is the participant's consent truly informed, comprehended, and free from coercion? [10] | Use of surrogate decision-makers, enhanced consent processes, independent consent monitors, continuous assessment of willingness to participate [5] [22]. |
| Harm-Based | Beneficence / Non-maleficence [20] | Increased likelihood of incurring additional or greater physical, psychological, social, or economic harm [13] [21] [20]. | What are the specific risks to this participant, and are they greater than those faced by a "standard" participant? | Robust risk-benefit analysis, protocol modifications to minimize risks, close monitoring, provision of counseling and medical support, clear plans for managing adverse events. |
| Justice-Based | Justice / Equity [5] [20] | Systemic, social, or economic inequalities that lead to unfair distribution of research burdens or exclusion from research benefits [5] [21]. | Is the recruitment fair, and will the research perpetuate or alleviate existing health disparities? [21] | Fair selection of participants, inclusive recruitment strategies, community engagement, ensuring research addresses the needs of the group, post-trial access to benefits. |
The Evolution from Group-Based to Analytical Approaches
Historically, research ethics guidelines employed a "group-based" or "labelling" approach, identifying vulnerability through membership in predefined categories such as children, prisoners, or the economically disadvantaged [5] [21]. While pragmatically simple, this approach has been criticized for being both over-inclusive and under-inclusive, potentially stereotyping individuals and overlooking context-specific vulnerabilities [21] [20].
The analytical framework addresses these shortcomings by reframing vulnerability as a dynamic and relational state, rather than a fixed property of an individual or group [21] [20]. As articulated in the 8th revision of the Declaration of Helsinki (2024), individuals or groups may find themselves in "a situation of more vulnerability" due to a combination of fixed, contextual, or dynamic factors [21]. This nuanced view recognizes that a participant's vulnerability can change over the course of a study and can arise from the research design itself, not just from pre-existing participant characteristics [5].
Operationalizing the Frameworks: A Research Lifecycle Workflow
Effectively addressing vulnerability requires a proactive and integrated strategy throughout the entire research process. The following diagram maps the application of the three normative accounts onto key stages of study design, review, and conduct.
Diagram 1: Integrating Vulnerability Assessments into the Research Workflow. LARs = Legally Authorized Representatives.
Experimental and Methodological Implications
Translating the theoretical accounts into actionable research practices requires specific methodological considerations. For instance, a community-based participatory research (CBPR) approach is a powerful method for addressing justice-based vulnerabilities. It engages community members as equal partners in designing, implementing, and disseminating research, thereby ensuring the study addresses community priorities and avoids harm [22]. To manage consent-based vulnerabilities, researchers might employ validated competency assessment tools or design multi-stage, simplified consent processes with ongoing comprehension checks [10] [22]. For harm-based vulnerabilities, Data and Safety Monitoring Boards (DSMBs) provide independent oversight, particularly for high-risk studies, to review accumulating data for unexpected adverse events [20].
Essential Toolkit for Ethical Research with Vulnerable Participants
Navigating the ethical landscape of vulnerability requires a set of conceptual and practical tools. The following table functions as a "scientist's toolkit," detailing key resources and their applications grounded in the three normative accounts.
Table 2: Research Reagent Solutions for Ethical Engagement with Vulnerability
| Tool / Framework | Primary Ethical Account | Function in Research Practice |
|---|---|---|
| Belmont Report Principles [5] [20] | Foundational | Provides the three foundational ethical principles (Respect for Persons, Beneficence, Justice) that underpin all modern research ethics and the specific accounts of vulnerability. |
| Analytical Vulnerability Framework [5] [21] | All (Consent, Harm, Justice) | Shifts the focus from labelling groups to analyzing situational and contextual sources of vulnerability, enabling more precise and respectful protections. |
| Community-Based Participatory Research (CBPR) [22] | Justice-Based | A collaborative approach to research that equitably involves community partners in the process to build trust, ensure relevance, and share power. |
| Enhanced Consent Protocols [5] [10] | Consent-Based | Procedures beyond standard consent, such as using independent consent monitors, surrogate decision-makers, and culturally/linguistically adapted materials. |
| Stakeholder Engagement Process [20] | Justice-Based | A structured process for involving patients, advocates, and community representatives in protocol development and review to identify and mitigate potential injustices and harms. |
| Dynamic Risk Assessment [21] | Harm-Based | A continuous process of evaluating potential harms that considers how a participant's vulnerability may change during the study, requiring adaptable safeguards. |
The consent-based, harm-based, and justice-based accounts of vulnerability provide a sophisticated and necessary framework for contemporary research ethics. Moving beyond static checklists of vulnerable groups, this analytical approach demands that researchers, scientists, and regulators critically assess the specific reasons why an individual or population might be at elevated risk within a given research context [5] [21] [20]. The ultimate goal is not to exclude vulnerable populations from research—which can perpetuate injustice and health disparities—but to include them with appropriate, carefully considered protections in place [21]. By systematically applying these normative justifications throughout the research lifecycle, from initial design to final dissemination, the scientific community can uphold its ethical obligations while advancing knowledge that is both robust and equitable.
This technical guide examines the profound and enduring influence of the Belmont Report on modern research ethics guidelines, with particular focus on the protection of vulnerable populations. Through systematic analysis of current literature and regulatory frameworks, we trace the evolution of ethical principles from their foundational expression in 1979 to their contemporary operationalization in global research standards. The analysis demonstrates how the Report's three ethical principles—Respect for Persons, Beneficence, and Justice—have fundamentally reshaped regulatory approaches to vulnerability, transitioning from rigid categorical protections toward more nuanced, context-sensitive frameworks. Current systematic reviews of policy documents reveal ongoing challenges in consistently defining and protecting vulnerable populations, while emerging regulatory trends for 2025 indicate continued refinement of these Belmont-inspired protections. This whitepaper provides researchers, scientists, and drug development professionals with both theoretical understanding and practical methodologies for implementing these ethical frameworks in contemporary clinical research environments.
The Belmont Report, formally titled "Ethical Principles and Guidelines for the Protection of Human Subjects of Research," was published in 1979 by the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research [23]. This landmark document emerged against a backdrop of historical ethical abuses in research and was designed to identify comprehensive ethical principles for human subjects research [24]. The Department of Health, Education, and Welfare (now Health and Human Services) subsequently incorporated the Report's principles into federal regulations, forming the core of what became known as the Common Rule (45 CFR 46) [23].
The Report's enduring significance lies in its articulation of three fundamental ethical principles that continue to govern human subjects research: Respect for Persons, Beneficence, and Justice [23]. These principles established a coherent framework that has demonstrated remarkable resilience and adaptability to evolving research paradigms over more than four decades. The Report's conceptualization of vulnerable populations as those in a "dependent state and with a frequently compromised capacity to free consent" established the foundation for all subsequent ethical guidelines addressing research with vulnerable groups [5].
Table: Historical Context of the Belmont Report
| Timeline | Document/Event | Significance for Vulnerable Populations |
|---|---|---|
| 1947 | Nuremberg Code | Emphasized voluntary consent but lacked provisions for vulnerable groups unable to provide consent |
| 1964 | Declaration of Helsinki (1st version) | Distinguished therapeutic/non-therapeutic research but provided limited protection frameworks |
| 1974 | National Research Act | Established National Commission that would draft the Belmont Report |
| 1979 | Belmont Report | First comprehensive ethical framework explicitly addressing vulnerable populations |
| 1980s-1990s | Common Rule Implementation | Codified Belmont principles with specific subparts for vulnerable populations |
The Belmont Report's Ethical Framework and Vulnerable Populations
The Belmont Report's treatment of vulnerable populations represents a sophisticated balance between protection and inclusion, establishing guiding principles that remain relevant to contemporary research ethics.
The Three Ethical Principles
The Report established three fundamental principles that collectively address the ethical dimensions of research with vulnerable populations:
Respect for Persons: This principle incorporates two ethical convictions: first, that individuals should be treated as autonomous agents, and second, that persons with diminished autonomy are entitled to protection [23]. The Report acknowledges that autonomy is not absolute and that some individuals require extensive protection, potentially even to the point of excluding them from harmful research [23]. This principle recognizes that vulnerability often stems from compromised autonomy and establishes corresponding protections.
Beneficence: Going beyond simply avoiding harm, this principle requires researchers to make positive efforts to secure participants' well-being [23]. The complementary expressions of this principle—"(1) do not harm and (2) maximize possible benefits and minimize possible harms"—create affirmative obligations toward all research subjects, with special significance for vulnerable populations who may bear disproportionate risks [23].
Justice: This principle addresses the fair distribution of research burdens and benefits, requiring that subject selection be equitable and not systematically directed toward vulnerable groups simply because of their availability or compromised position [23]. The Report explicitly connects justice to vulnerability by prohibiting the selection of subjects due to "easy availability, compromised position, or racial, sexual, economic, or cultural biases" [23].
Conceptualizing Vulnerability
The Belmont Report introduced a nuanced understanding of vulnerability that acknowledged both inherent and situational factors. The Report defined "vulnerable people" as those in a "dependent state and with a frequently compromised capacity to free consent," specifically mentioning racial minorities, economically disadvantaged people, the very sick, and the institutionalized as examples [5]. This conceptualization acknowledged that vulnerability could arise from various sources while recognizing that the "extent of protection afforded should depend upon the risk of harm and the likelihood of benefit" [23].
Evolution from Belmont to Contemporary Regulatory Frameworks
The transition from the Belmont Report's principlism to contemporary regulatory frameworks reveals both continuity and evolution in the protection of vulnerable populations, with significant developments in how vulnerability is conceptualized and operationalized.
Regulatory Codification: The Common Rule
The Belmont principles were codified into federal regulations through the Common Rule (45 CFR 46), which implemented specific subparts providing additional protections for vulnerable populations:
- Subpart B: Additional protections for pregnant women, human fetuses, and neonates
- Subpart C: Additional protections for prisoners
- Subpart D: Additional protections for children
This regulatory structure reflected what contemporary scholars term the "category" or "group-based notion" of vulnerability, also known as the "labelling approach" [5]. This approach identifies vulnerability based on membership in predetermined groups (e.g., children, prisoners, pregnant women) and establishes specific protections for each category [5]. While pragmatically simpler for research ethics committees, this approach has been criticized for its potential to be both over-inclusive and under-inclusive in identifying vulnerability [5].
The Analytical Approach to Vulnerability
Contemporary research ethics has witnessed the emergence of an analytical approach that shifts focus from categorical labels to the underlying sources and conditions of vulnerability [5]. This approach provides three main accounts of vulnerability:
- Consent-based accounts: Vulnerability stems primarily from compromised capacity to provide free and informed consent due to conditions such as undue influence, limited decision-making capacity, or situational pressures [5].
- Harm-based accounts: Vulnerability is conceptualized as an increased probability of incurring harm during research, requiring enhanced safeguards regardless of categorical group membership [5].
- Justice-based accounts: Vulnerability arises from unequal conditions and opportunities that create disparities in research participation or benefit distribution [5].
Table: Comparative Approaches to Vulnerability in Research Ethics
| Aspect | Categorical (Group-Based) Approach | Analytical Approach |
|---|---|---|
| Definition | Identifies vulnerability based on group membership | Identifies vulnerability based on individual and contextual factors |
| Examples | Children, prisoners, pregnant women, cognitively impaired | Those with compromised consent capacity, elevated risk of harm, or subject to unjust distribution of risks/benefits |
| Regulatory Preference | Historically dominant, simpler to implement | Increasingly favored in theoretical literature |
| Practical Implementation | Clearer boundaries but potentially rigid | More nuanced but operationally challenging |
| Coverage | May miss vulnerable individuals outside predefined categories | Potentially more comprehensive but less predictable |
Current Landscape: Systematic Analysis of Policy Guidelines
Recent comprehensive analysis of policy documents reveals how vulnerability is conceptualized and operationalized in contemporary research ethics frameworks. A 2025 systematic review of policy documents published in PLOS ONE analyzed 79 policy guidelines to provide a comprehensive overview of vulnerability in research ethics [5] [13].
Key Findings from the Systematic Review
The systematic review identified several recurring patterns in how policy documents address vulnerability:
Definitional Tendencies: Most policy documents demonstrate a preference for identifying and defining specific vulnerable groups rather than providing a general definition of vulnerability itself [5] [13]. This reflects the persistent influence of the categorical approach despite theoretical preference for analytical frameworks.
Informed Consent Focus: Policy documents frequently define vulnerability in relation to informed consent capacity, echoing the Belmont Report's emphasis on persons with diminished autonomy [5] [13]. This consent-based account remains dominant in operational definitions.
Protection-Participation Tension: The review identified ongoing tension between protecting vulnerable populations from harm and ensuring their appropriate participation in research [5]. Historically, strict protectionist approaches sometimes resulted in exclusion from research and its potential benefits, perpetuating injustices [5].
Emerging Regulatory Trends for 2025
Analysis of forthcoming regulatory changes indicates continued evolution in the protection of vulnerable populations:
Enhanced Focus on Diverse Enrollment: Regulatory agencies are increasing emphasis on diverse participant enrollment, including vulnerable populations, to ensure treatments are effective across patient demographics [25]. This represents a practical application of the justice principle.
Single IRB Review for Multicenter Studies: Implementation of single IRB review for multicenter studies aims to streamline ethical review while maintaining protection standards [25]. This structural change may promote more consistent application of vulnerability assessments across research sites.
ICH E6(R3) Updates: New international standards for clinical trials emphasize data integrity and traceability, with implications for the ethical conduct of research involving vulnerable populations [25].
Methodological Framework: Implementing Ethical Principles in Research with Vulnerable Populations
Translating ethical principles into practical research methodologies requires systematic approaches to identifying and addressing vulnerability. The following section provides researchers with concrete frameworks for implementing Belmont-inspired ethics in contemporary studies.
Experimental Protocol for Vulnerability Assessment
Protocol Title: Comprehensive Vulnerability Assessment and Mitigation Framework for Human Subjects Research
Objective: To provide a systematic methodology for identifying, assessing, and addressing vulnerabilities in research participants throughout the study lifecycle.
Materials and Equipment:
- Vulnerability assessment checklist (context-specific)
- Informed consent evaluation toolkit
- Risk-benefit assessment matrix
- Cultural and linguistic appropriate communication resources
- Data protection and confidentiality protocols
Procedure:
Pre-Study Vulnerability Mapping
- Conduct stakeholder engagement with community representatives from potentially vulnerable groups
- Identify contextual factors that may create or exacerbate vulnerability in the specific research setting
- Document potential vulnerabilities in research protocol
Participant-Level Assessment
- Implement individualized evaluation of consent capacity using validated assessment tools
- Identify situational factors that may compromise voluntary participation (e.g., power differentials, economic pressures)
- Assess understanding of research concepts through teach-back methods
Continuous Monitoring and Reassessment
- Establish mechanisms for ongoing evaluation of participant vulnerability throughout study participation
- Implement procedures for dynamic consent where understanding may fluctuate
- Document and address emerging vulnerabilities through protocol modifications
Post-Study Evaluation
- Assess distribution of risks and benefits across participant subgroups
- Evaluate whether vulnerability protections resulted in equitable participation
- Incorporate lessons learned into future study designs
Validation: This protocol draws from systematic analysis of 79 policy documents [5] [13] and incorporates best practices identified in recent literature on engaging vulnerable populations in research [26]. The framework balances categorical and analytical approaches to vulnerability, acknowledging the regulatory requirement to address specific protected groups while remaining responsive to individual and contextual factors.
Research Reagent Solutions: Essential Materials for Ethical Research with Vulnerable Populations
Table: Essential Resources for Ethical Research with Vulnerable Populations
| Resource Category | Specific Tools/Components | Function in Protecting Vulnerable Populations |
|---|---|---|
| Consent Enhancement Tools | Simplified consent forms, Multimedia consent materials, Teach-back assessment protocols, Witness verification procedures | Enhance comprehension and ensure genuine informed consent for those with cognitive, educational, or linguistic vulnerabilities |
| Capacity Assessment Instruments | MacArthur Competence Assessment Tool, UBACC, SICIATRI | Objectively evaluate decision-making capacity and identify need for additional protections or proxy consent |
| Cultural and Linguistic Resources | Certified translators, Culturally validated assessment tools, Community navigators | Address vulnerabilities arising from language barriers or cultural differences |
| Data Protection Systems | Secure encrypted databases, Limited access protocols, Anonymization techniques | Protect vulnerable participants from privacy breaches and associated harms |
| Community Engagement Frameworks | Community Advisory Boards, Participatory research designs, Benefit-sharing agreements | Address justice-based vulnerabilities through meaningful community involvement |
Visualization of Ethical Framework Implementation
The following diagram illustrates the systematic application of Belmont Report principles to the protection of vulnerable populations in research, mapping the relationship between core ethical principles, their applications, and resulting protections.
Diagram: Ethical Framework for Vulnerable Population Protection. This visualization maps the evolution from Belmont Report principles to contemporary approaches for protecting vulnerable research populations, demonstrating the relationship between core ethical principles and their practical applications.
Discussion: Contemporary Challenges and Future Directions
The enduring influence of the Belmont Report presents both strengths and challenges for modern research ethics. The tension between categorical and analytical approaches to vulnerability reflects deeper philosophical questions about how best to operationalize ethical principles in diverse research contexts.
Implementation Challenges
Research ethics committees frequently maintain preference for the categorical approach to vulnerability as a "pragmatically simpler solution" despite theoretical recognition that the analytical approach is more nuanced and context-sensitive [5]. This creates practical challenges for researchers who must navigate sometimes inconsistent interpretations of vulnerability across different review boards.
Furthermore, the systematic review of policy documents reveals that research ethics committees often require statements about vulnerable population enrollment without providing specific guidance on implementation, potentially resulting in "differential treatment of vulnerable research subjects with potentially inequitable outcomes" [5]. This guidance gap may lead researchers to exclude traditionally vulnerable groups due to management difficulties rather than ethical considerations [5].
Balancing Protection and Participation
Contemporary ethical frameworks increasingly recognize that both exclusion and exploitation of vulnerable populations can constitute ethical failures [26]. As noted by experts in the field, "excluding the vulnerable is biased and unethical," yet inclusion requires sophisticated approaches to distinguish "between coercion and fair compensation while respecting the principles of informed consent" [26].
The evolution toward appropriate inclusion reflects a maturation beyond the protectionist paradigm that initially followed the Belmont Report. Where early implementations often emphasized restrictions on vulnerable population enrollment, modern approaches recognize that "individuals from all these populations may legitimately participate in clinical trials under ethical and well-managed conditions" [26].
Regulatory Innovation and Future Trends
Emerging regulatory trends for 2025 suggest continued refinement of vulnerability protections, with emphasis on diverse enrollment, streamlined ethical review processes, and enhanced data integrity requirements [25]. These developments represent practical implementations of the justice principle, ensuring equitable distribution of research benefits and burdens while maintaining appropriate safeguards.
Future directions likely include greater integration of community engagement in vulnerability assessment, development of more sophisticated consent models for fluctuating capacity, and increased attention to structural vulnerabilities arising from social determinants of health. The ongoing revision of international guidelines such as ICH E6(R3) indicates continued global convergence toward ethically robust yet practical frameworks for vulnerable population research [25].
The Belmont Report's enduring influence on modern research guidelines demonstrates the remarkable resilience of its ethical framework. Its three principles—Respect for Persons, Beneficence, and Justice—have successfully guided research ethics for over four decades while adapting to evolving understandings of vulnerability and protection. The contemporary landscape reflects a maturation from rigid categorical protections toward more nuanced, context-sensitive approaches that balance safeguarding against exploitation with appropriate inclusion.
For researchers, scientists, and drug development professionals, understanding this regulatory evolution is essential for designing ethically sound studies that both protect and appropriately include vulnerable populations. The systematic methodologies and frameworks presented in this whitepaper provide practical tools for implementing these ethical principles in current research environments. As regulatory standards continue to evolve, the Belmont Report's foundational principles remain remarkably relevant for addressing emerging ethical challenges in human subjects research.
Practical Protocols: Implementing Ethical Safeguards in Study Design and Conduct
In life science research and development, including diverse populations is critical for ensuring scientific rigor and generalizability of research findings. Historically, this has not been accomplished for many reasons, including racial and gender biases, differential access to medical care, and varied enrollment in clinical trials across different populations, geographical regions, and countries. For vulnerable populations specifically, these barriers compound existing health disparities, creating ethical challenges that demand systematic solutions. The scientific imperative is equally compelling; without adequate representation, research findings may lack external validity and fail to account for biological, genetic, and social factors that influence disease presentation and treatment response across different populations.
Advancing inclusive research (AIR) requires frameworks and metrics for assessing real-world data and measuring population science. Because different factors drive health inequities and variables in measuring population science, relying on one metric for measuring progress may have limitations. This technical guide presents a comprehensive framework for designing and implementing inclusive research protocols that ensure equitable participation and benefit distribution, with particular attention to vulnerable populations within research ethics. The principles and methodologies outlined herein address both the ethical obligations to ensure equitable access to research benefits and the methodological necessities for producing scientifically valid, generalizable results.
Theoretical Framework: Foundational Principles for Inclusive Research
The 5Ps Framework for Advancing Inclusive Research
The 5 Principles (5Ps) framework provides a conceptual foundation designed to ensure a study is representative to the extent possible—based on data availability, operational constraints, and regulatory requirements—and adheres to biomedical ethical principles. These five principles form the basis for a data-informed framework to measure and systematically define inclusive research to ensure rigor and benchmarking within organizations and across the broader sector [27].
The framework standardizes processes by which inclusive research and clinical trials can be conducted in an organization, allowing for benchmarking, performance assessments, and integration of health equity and inclusive research at a population level. For vulnerable populations, this systematic approach is particularly crucial as it provides measurable accountability for inclusion that has historically been neglected.
Table 1: The 5Ps Framework for Advancing Inclusive Research
| Principle | Core Focus | Key Considerations for Vulnerable Populations |
|---|---|---|
| Population Science | Biological, genetic, and demographic considerations | Responsible use of population descriptors; understanding social determinants of health; addressing underrepresentation in baseline data |
| Data-Informed Site Placement | Geographical distribution of research sites | Ensuring site locations align with disease burden in vulnerable communities; geographical proportionality in trial enrollment |
| Inclusive Trial Design | End-to-end inclusive protocol development | Removing unnecessary exclusion criteria; addressing practical barriers to participation; incorporating community feedback |
| Patient-Reported Data Standards | Integration of patient perspectives | Ensuring complete and consistent data collection across diverse populations; culturally appropriate measurement tools |
| Trial Access Enablement | Practical support for participation | Addressing financial, logistical, and trust barriers; patient navigation assistance; demonstrating trustworthiness to communities |
Measuring Representativeness: The Participation-to-Prevalence Ratio
A critical metric for assessing inclusion is the participation-to-prevalence ratio (PPR), calculated by dividing the percentage of a particular population among the study participants by the percentage of that population in the disease population. A range of 80–120% has been suggested as adequate representation, where each study should aim for zero error between these proportions [27]. For example, if women constitute 40% of a disease population but only 20% of a trial's participants, the PPR would be 50% (20/40), indicating significant underrepresentation.
This metric is particularly valuable for vulnerable populations as it provides a quantitative benchmark for evaluating inclusion and identifying disparities in enrollment. When applied systematically across multiple studies, it enables performance tracking and accountability in addressing historical underrepresentation.
Methodological Implementation: Protocols for Inclusive Research Design
Population Science Considerations in Protocol Development
The first principle anchors on the "Who," i.e., who is most affected by the disease or condition? Collecting diverse biological, genetic, and demographic data is essential for understanding patient outcomes, disease risk, and enrollment rates. Race and ethnicity are social constructs, with different interpretations that have led to the exclusion of certain populations in clinical research. Genetic ancestry is often oversimplified to broad continental categories, undermining scientific objectivity and potentially perpetuating harmful stereotypes linked to racial genetic determination [27].
For vulnerable populations, appropriate use of population descriptors is essential. The National Academies of Sciences, Engineering, and Medicine (NASEM) recommends the appropriate use of population descriptors in genetics and genomics research. The US Food and Drug Administration (FDA) has updated guidelines to standardize race and ethnicity data collection in clinical studies. These initiatives may enhance the understanding and enrollment of the diverse patient populations in clinical trials [27].
Experimental Protocol: Disease Area Population Analysis
Literature Review Implementation: Conduct a comprehensive literature review of the therapy area to summarize the epidemiology, risk factors, disparities in diagnosis, disease characteristics and progression, genetics, biomarkers, treatment patterns and outcomes, and quality of care in global patient populations with a focus on health equity.
Quality Assessment: Grade studies that meet the criteria using a quality assessment tool for the strength of evidence. Searches and summaries can be done manually or with natural language processing or augmented intelligence tools, keeping biases and limitations in mind.
Disease Burden Measurement: Measure disease burden using demographic-specific variables with standardized metrics, identifying demographic groups with granularity in geographical areas to enable precise benchmarking, while recognizing that most existing sources of data on disease prevalence are biased in the same direction as the problem.
Data-Informed Country and Site Placement Methodology
Once the patient population (biology, genetics, demographics) with the disease is understood, Principle 2 anchors on "Where" these patients are. The FDA issued draft guidance for the creation of Diversity Action Plans (DAPs) by sponsors of pivotal studies to increase enrollment of historically underrepresented populations to improve the strength of the evidence for the intended-use population [27].
Experimental Protocol: Geographical Site Selection
Epidemiological Data Identification: Identify preferred sources, such as the US Cancer Statistics (USCS) and the Institute for Health Metrics and Evaluation (IHME) Global Burden of Disease study, based on data quality, representativeness, and disease area coverage to provide epidemiology estimates at the indication or disease area level.
Global Burden Assessment: Use these sources to determine incidence or prevalence of the disease by region to determine the global burden of disease, as well as age and sex distribution to set overall global targets, and race and ethnicity distribution in the USA to set the US targets.
Subpopulation Analysis: Augment multiple data sources to generate epidemiologic estimates that closely approach the trial population when sources provide limited information about subpopulations (e.g., biomarker-driven subsets, stage, and evolution beyond the initial diagnosis).
Country-Specific Adaptation: For diversity outside the USA, use regional and/or country-specific enrollment by demographic variables to ensure that trial results are reflective of countries' diversity, as recorded per national statistical offices or census bureaus, rather than relying solely on US-specific demographic frameworks.
LMIC Considerations: Formalize assessments of accessibility for low- and middle-income countries (LMICs) to ensure efficient and diverse patient enrollment, recognizing that country-specific needs are very different in LMICs versus high-income countries.
Diagram 1: Inclusive Research Implementation Workflow
Inclusive Trial Design and Protocol Development
The updated SPIRIT 2025 statement provides evidence-based guidance for protocol development that now explicitly incorporates inclusive research considerations. The statement consists of a checklist of 34 minimum items to address in a trial protocol, along with a diagram illustrating the schedule of enrolment, interventions, and assessments for trial participants. Notable changes include additional emphasis on the assessment of harms and description of interventions and comparators, and a new item on how patients and the public will be involved in trial design, conduct, and reporting [28].
Experimental Protocol: SPIRIT 2025 Inclusive Protocol Development
Stakeholder Engagement: Implement plans for patient or public involvement in the design, conduct, and reporting of the trial, with specific attention to representation from vulnerable populations.
Outcome Selection: Define specific objectives related to both benefits and harms, ensuring that outcome measures are validated across diverse populations and are meaningful to vulnerable groups.
Accessibility Planning: Develop comprehensive plans to communicate trial results to participants, healthcare professionals, the public, and other relevant groups (e.g., reporting in trial registry, plain language summary, publication) in formats accessible to vulnerable populations.
Transparency Documentation: Clearly document names, affiliations, and roles of protocol contributors; name and contact information for the trial sponsor; and role of trial sponsor and funders in design, conduct, analysis, and reporting of trial, including any authority over these activities.
Table 2: SPIRIT 2025 Key Updates for Inclusive Research
| SPIRIT 2025 Section | Updated Item | Application to Vulnerable Populations |
|---|---|---|
| Open Science | Trial registration, protocol access, data sharing | Ensures transparency and accessibility of research protocols and results |
| Patient and Public Involvement | Details of patient/public involvement in design, conduct, reporting | Formalizes engagement of vulnerable populations in research planning |
| Dissemination Policy | Plans to communicate results to various groups | Addresses knowledge translation to participant communities |
| Roles and Responsibilities | Composition and roles of oversight committees | Promotes diverse representation in trial governance |
Research Reagent Solutions: Tools for Inclusive Research Implementation
Table 3: Essential Research Reagents and Resources for Inclusive Research
| Tool/Resource | Function | Application Context |
|---|---|---|
| Diversity Action Plans (DAPs) | Formal strategy to increase enrollment of underrepresented populations | Required for FDA submission; sets specific enrollment goals for underrepresented groups |
| Participation-to-Prevalence Ratio (PPR) | Quantitative metric for assessing representativeness | Benchmarking inclusion across demographic groups; target range: 80-120% |
| Global Burden of Disease Data | Epidemiological data for understanding disease distribution | Informing site selection based on geographical disease burden |
| SPIRIT 2025 Checklist | Protocol development framework | Ensuring comprehensive addressing of inclusive research considerations |
| Cultural Adaptation Frameworks | Methodologies for translating research materials | Ensuring consent forms, surveys, and educational materials are culturally appropriate |
| Patient Navigation Programs | Practical support for trial participation | Addressing logistical, financial, and educational barriers for vulnerable populations |
Data Visualization and Analysis Framework for Inclusive Research
Diagram 2: Inclusive Research Monitoring Cycle
Quantitative Benchmarks for Inclusive Research
The implementation of inclusive research principles requires rigorous data collection and analysis to assess progress and impact. The following table summarizes key quantitative metrics derived from empirical studies of diversity in research.
Table 4: Quantitative Benchmarks for Assessing Inclusive Research Outcomes
| Metric Category | Current Performance | Evidence Source | Implications for Vulnerable Populations |
|---|---|---|---|
| Leadership Diversity | Women hold only 23.3% of senior leadership positions globally | 2024 Report from Druthers [29] | Underrepresentation in decision-making limits attention to diverse health needs |
| DEI Program Effectiveness | 90% of companies lack ability to measure DE&I effectiveness | 2024 Industry Analysis [29] | Accountability gap for inclusion initiatives affecting vulnerable groups |
| Financial Impact | Inclusive cultures achieve 19% higher revenue growth | Harvard Business Review [29] | Business case for inclusion extends to research organizations |
| Talent Acquisition | 67% of job seekers consider DE&I policies when applying | Team Storage Survey [29] | Research institutions with strong DE&I attract broader talent pool |
| Market Expansion | Diverse teams 70% more likely to capture new markets | Doit 2024 Report [29] | Diverse research teams better address global health challenges |
The framework and methodologies presented provide a comprehensive approach to designing inclusive research that ensures equity in participation and benefit. For vulnerable populations, systematic implementation of these principles addresses both ethical imperatives for equitable access and methodological requirements for scientifically valid research. The 5Ps framework—encompassing population science, data-informed site placement, inclusive trial design, patient-reported data standards, and trial access enablement—provides a structured approach to embedding inclusion throughout the research lifecycle.
The integration of these principles with updated protocol guidance from SPIRIT 2025 creates a robust foundation for advancing inclusive research practices. By adopting measurable benchmarks, particularly the participation-to-prevalence ratio, research organizations can track progress and maintain accountability for including vulnerable populations. As the evidence demonstrates, inclusive research is not merely an ethical obligation but a scientific necessity for generating valid, generalizable knowledge that benefits all populations.
Within research ethics, the concept of vulnerability has evolved significantly beyond categorical definitions toward a more nuanced understanding of contextual factors that impair autonomous decision-making [5] [3]. This shift demands parallel evolution in informed consent processes, moving from standardized forms toward dynamic, relationship-centered approaches that acknowledge participants' lived experiences and cultural contexts. Vulnerability in research is no longer viewed merely as a characteristic of specific groups but as a condition that can arise from contextual circumstances, including power imbalances, communication barriers, or socioeconomic pressures that compromise voluntary participation [3] [30]. This whitepaper establishes a strategic framework for transforming consent from a transactional event into an ethical practice grounded in cultural humility and continuous engagement, particularly when working with vulnerable populations.
Contemporary ethical frameworks recognize that traditional consent processes often fail to address the complex realities of vulnerable populations. A systematic review of policy documents reveals that vulnerability is predominantly conceptualized in relation to impaired consent capacity, with significant attention to barriers affecting understanding and voluntary agreement [5]. The contextual approach to vulnerability allows researchers to identify specific situational factors that may undermine authentic consent and implement targeted safeguards accordingly [3]. This paper synthesizes evidence-based methodologies and practical tools to address these challenges through culturally responsive and ethically robust consent practices.
Conceptual Foundations: Vulnerability and Consent Capacity
Evolving Conceptualizations of Vulnerability
The ethical imperative for special protections for vulnerable populations originated with The Belmont Report (1979), which identified them as persons with "compromised capacity to free consent" [5]. Contemporary ethics frameworks have since developed three distinct analytical approaches to understanding vulnerability:
- Consent-based accounts: Focus on limitations in capacity to provide free and informed consent due to conditions such as undue influence or reduced autonomy [5]
- Harm-based accounts: Emphasize increased probability of incurring harm during research participation [5]
- Justice-based accounts: Highlight unequal conditions and opportunities for research subjects as sources of vulnerability [5]
Current policy documents show a persistent tendency to identify vulnerable groups rather than provide a general definition of vulnerability [5]. This categorical approach typically includes children, prisoners, pregnant women, economically disadvantaged persons, and those with impaired decision-making capacity [31]. However, a more nuanced contextual approach recognizes that vulnerability can be situational rather than inherent, affecting individuals across multiple dimensions including cognitive, communicative, institutional, and deferential vulnerabilities [3].
Intersectional Vulnerabilities in Research
Vulnerability often arises from the intersection of multiple social determinants. Research participants from racial and ethnic minority groups, those living in poverty, and individuals with low educational attainment frequently face compounded barriers to genuine informed consent [30]. These intersecting factors create what has been termed structural exclusion, where vulnerable individuals are systematically underrepresented in research or inadequately protected during participation [30].
The digitalization of health research introduces new dimensions of vulnerability, particularly concerning data privacy, technological access, and digital literacy [32] [33]. Participants with limited digital access or literacy may be excluded from research opportunities or unable to provide meaningful consent for complex digital health technologies [32]. These emerging vulnerabilities necessitate updated consent frameworks that address both traditional and technology-mediated research contexts.
Foundational Strategies for Culturally Sensitive Consent
Building Cultural Responsiveness into Consent Processes
Culturally sensitive consent requires moving beyond translation toward meaningful engagement with participants' cultural frameworks. Research in Lebanon demonstrated that utilizing a Design Thinking framework combined with Participatory Action Research enabled development of consent guidelines that genuinely reflected local cultural norms and communication patterns [34]. This approach emphasized trust-building, appropriate timing, and community involvement as critical yet often overlooked aspects of consent processes.
Key strategies for enhancing cultural responsiveness include:
- Community involvement in design: Engaging community members as partners in developing consent processes and materials [34]
- Culturally appropriate communication: Adapting communication styles to local norms, which may prioritize oral discussions over written documents [34]
- Trust-building through sustained relationships: Recognizing that trust develops over time through consistent, respectful engagement [34]
- Addressing power imbalances: Implementing procedures that mitigate hierarchical relationships between researchers and participants [34] [30]
Language and literacy barriers present significant challenges that can be mitigated by involving trained interpreters and developing materials appropriate for participants' educational levels [34] [30]. Consent forms should typically be written at a 6th-8th grade reading level and use plain language strategies to enhance comprehension [35] [33].
Addressing Structural and Communicative Barriers
Vulnerable populations often face structural barriers that impede genuine consent. Research with marginalized communities highlights how power differentials, historical trauma, and socioeconomic pressures can undermine voluntary participation [30]. Researchers must recognize that autonomy is constrained by contextual factors and implement additional safeguards accordingly.
Effective approaches to addressing these barriers include:
- Comprehensive consent assessment: Evaluating potential participants' understanding through teach-back methods or simple questionnaires [31]
- Culturally tailored materials: Developing consent materials that reflect community values, concerns, and communication styles [34]
- Supplementary educational measures: Using audio-visual tools, illustrations, and interactive discussions to enhance understanding [34] [31]
- Independent consent monitors: Involving community representatives or patient advocates to oversee consent procedures [31]
Table 1: Quantitative Assessment of Consent Communication Preferences in Digital Health Research [33]
| Factor | Impact on Preference | Statistical Significance |
|---|---|---|
| Character length | Longer text reduced preference for original by factor of 1.20x | P=.04 |
| Age | Older participants preferred original by factor of 1.95x | P=.004 |
| Content type | Risk explanations showed strongest preference for modified versions | P=.03 |
| Physical activity level | Active participants showed different preferences for consent communication | Significant |
Implementing Continuous Consent Processes
From Transactional Event to Relational Process
Traditional consent often represents a single transactional event at study initiation, but ethical practice with vulnerable populations requires continuous consent throughout the research relationship. This approach recognizes that understanding, willingness, and circumstances may change over time, necessitating ongoing communication and reaffirmation of participation [35].
Continuous consent frameworks include:
- Staged consent: Presenting information in manageable blocks at different time points to facilitate understanding [3]
- Ongoing check-ins: Regularly verifying continued willingness to participate and addressing new questions or concerns [35]
- Dynamic consent: Using digital platforms to maintain engagement and allow participants to adjust permissions over time [32]
- Re-consent procedures: Formal reaffirmation of consent when study procedures change or new risks emerge [31]
The relational nature of continuous consent is particularly important when working with populations experiencing cognitive fluctuations, evolving capacities, or changing life circumstances [3] [31]. This approach acknowledges consent as a process rather than an event, embedding it within an ongoing researcher-participant relationship.
Digital Innovations for Ongoing Engagement
Digital health technologies introduce both challenges and opportunities for continuous consent. Electronic platforms can facilitate dynamic consent models that enable participants to track their data, adjust permissions, and receive updates throughout the research process [32] [33]. However, these approaches must address digital literacy barriers and ensure equitable access.
Key elements of digital continuous consent include:
- Interactive platforms: Providing accessible interfaces for participants to manage their engagement preferences [32]
- Just-in-time information: Delivering relevant consent information at decision points rather than overwhelming participants initially [33]
- Granular permission options: Allowing participants to choose levels of involvement and data sharing [32]
- Ongoing communication: Maintaining regular contact to ensure continued understanding and willingness [35]
Research indicates that digital consent platforms must be carefully designed to avoid exacerbating existing disparities. Participants with varying demographic characteristics show different preferences for consent communication formats, emphasizing the need for responsive design [33].
Experimental Protocols and Methodological Approaches
Participatory Action Research for Guideline Development
A study in Lebanon demonstrated the efficacy of combining Design Thinking with Participatory Action Research to develop culturally relevant consent guidelines [34]. This methodology actively engaged affected communities as partners in identifying problems and designing solutions.
Table 2: Experimental Protocol for Participatory Consent Guideline Development [34]
| Research Phase | Methodological Approach | Stakeholder Engagement |
|---|---|---|
| Problem Framing | Design Thinking workshops | Researchers and community members collaboratively define consent barriers |
| Solution Ideation | Participatory Action Research cycles | Community members generate and refine potential solutions |
| Guideline Development | Iterative co-design sessions | Diverse stakeholders draft and revise consent guidelines |
| Implementation Testing | Pilot studies with vulnerable populations | Researchers and participants assess guideline feasibility and effectiveness |
The experimental protocol emphasized cultural adaptation rather than universal application, recognizing that consent processes must respond to local contexts and community norms [34]. This approach generated insights about the importance of motivations for participation, trust-building, and timing in consent processes—factors often overlooked in standardized approaches.
Framework Development for Digital Health Consent
A systematic approach to developing comprehensive consent frameworks for digital health research involved qualitative analysis of National Institutes of Health guidance and real-world informed consent forms [32]. The methodology followed a rigorous multi-phase process:
- Data Familiarization: Repeated review of guidance documents to understand structure and intentions [32]
- Code Generation: Descriptive labeling of consent-related requirements, expectations, and values [32]
- Attribute Formation: Grouping related codes into broader consent attributes and subattributes [32]
- Framework Testing: Iterative refinement through application to real-world consent forms [32]
- Validation: Assessment of framework completeness and relevance through expert deliberation [32]
This process identified significant gaps in current consent practices, particularly regarding technology-specific risks. The resulting framework organized consent elements across multiple domains, including researcher permissions, obligations, and technology-specific considerations [32].
Diagram 1: Continuous Consent Process Flow - This diagram illustrates the cyclical nature of continuous consent, moving from initial agreement through ongoing engagement.
The Researcher's Toolkit: Practical Implementation Frameworks
Research Reagent Solutions for Ethical Consent
Table 3: Essential Tools for Culturally Sensitive Consent Processes
| Tool Category | Specific Methods | Application Context |
|---|---|---|
| Comprehension Assessment | Teach-back method, Simple questionnaires, Interactive quizzes | Verifying understanding across literacy levels |
| Communication Enhancement | Audio-visual aids, Illustrated materials, Plain language writing | Making complex information accessible |
| Cultural Mediation | Trained interpreters, Cultural brokers, Community ambassadors | Bridging cultural and linguistic gaps |
| Process Documentation | Dynamic consent platforms, Staged consent records, Ongoing assent documentation | Maintaining ethical transparency |
| Capacity Support | Decision aids, Supported decision-making frameworks, Independent advocates | Assisting participants with cognitive or communicative vulnerabilities |
Implementation Framework for Vulnerable Population Research
Implementing culturally sensitive and continuous consent requires systematic approaches tailored to specific vulnerabilities. The following framework provides a structured methodology:
Diagram 2: Vulnerability Assessment and Safeguard Implementation Cycle - This process emphasizes continuous evaluation and improvement of consent protocols.
Implementation should be guided by two critical questions: (1) Is inclusion of vulnerable individuals necessary? and (2) If so, are safeguards adequate? [3]. This framework ensures that vulnerability considerations are integrated throughout the research lifecycle rather than addressed as an afterthought.
Culturally sensitive and continuous consent represents a fundamental shift from regulatory compliance to ethical engagement. This approach recognizes that genuine consent requires ongoing attention to power dynamics, cultural contexts, and evolving participant understanding. By implementing the strategies outlined in this whitepaper, researchers can transform consent from a bureaucratic hurdle into a meaningful ethical practice that respects the dignity and autonomy of vulnerable populations.
The future of ethical research with vulnerable populations depends on moving beyond standardized forms toward responsive, relationship-centered consent processes. As digital health technologies and precision medicine initiatives advance, researchers must develop increasingly sophisticated approaches to ensure that vulnerable individuals are neither excluded from research benefits nor exposed to exploitation. The frameworks presented here provide a foundation for this evolution, emphasizing cultural humility, continuous engagement, and contextual sensitivity as cornerstones of ethical practice.
The integration of clinical care and research responsibilities creates a complex ethical terrain, particularly when investigating vulnerable populations. Clinician-researchers navigate inherent tensions between therapeutic obligations and research imperatives, where professional responsibilities to provide care can conflict with methodological requirements to maintain scientific rigor and objectivity [36]. This dual positioning generates significant ethical challenges around informed consent, therapeutic boundaries, and emotional involvement, especially when urgent clinical needs emerge during data collection activities [36]. Within the broader context of research ethics concerning vulnerable populations, these challenges become increasingly pronounced, as power differentials and potential for coercion are amplified.
The concept of vulnerability in research ethics was first formally introduced in The Belmont Report (1979), which defined vulnerable people as those in a "dependent state and with a frequently compromised capacity to free consent" [5] [13]. Contemporary scholarship has evolved toward recognizing both categorical (group-based) and analytical (context-dependent) sources of vulnerability, with particular relevance to clinician-researchers who must identify and respond to vulnerability factors throughout the research process [5]. This guide addresses these complexities by providing evidence-based ethical frameworks and practical strategies to support clinician-researchers in maintaining integrity while conducting valuable research with vulnerable populations.
Ethical Challenges and Tensions in Dual Roles
Foundational Ethical Dilemmas
Clinician-researchers operating in sensitive research contexts regularly encounter several interconnected ethical challenges. These tensions are particularly acute in resource-limited settings where healthcare gaps may amplify participants' needs and where clinician-researchers are often viewed as trusted authorities [36].
Role Conflict and Boundary Management arises when professional obligations to intervene clinically conflict with research neutrality requirements. This dilemma becomes starkly evident when, for example, a clinician-researcher observes unsafe care practices during home visits but must decide whether documenting the situation for research purposes takes precedence over immediate intervention [36]. The dual role can blur therapeutic boundaries and complicate decisions about when—and whether—to intervene, creating significant ethical distress for the researcher [36].
Emotional Labor and Vulnerability represents another substantial challenge. Sensitive research with vulnerable populations—such as men living with advanced prostate cancer—inevitably raises complex emotional demands [36]. Emotional tensions emerge when participants' distress risks overwhelming the researcher's composure, requiring considerable emotional labor [36]. This vulnerability is bidirectional, affecting both participants and researchers, particularly in emotionally charged, culturally sensitive contexts [36].
Informed Consent Complications frequently occur in dual-role contexts. The clinician-researcher's identity, while potentially fostering rapport and facilitating participant access, may inadvertently create perceived therapeutic misconceptions [36]. Patients participating in research led by their clinicians may struggle to distinguish between routine care and research procedures, potentially compromising the voluntary nature of consent, especially when capacity fluctuates due to illness or medication [36].
Vulnerability Considerations in Research Ethics
Understanding vulnerability is essential for clinician-researchers navigating dual roles. Systematic analyses of research ethics policy documents reveal several approaches to conceptualizing vulnerability [5] [13]:
Table: Conceptual Approaches to Vulnerability in Research Ethics
| Approach | Definition | Focus | Examples |
|---|---|---|---|
| Categorical (Group-Based) | Vulnerability based on group membership | Identifying vulnerable populations | Children, prisoners, pregnant women, economically disadvantaged [5] [13] |
| Consent-Based | Vulnerability stemming from compromised capacity for autonomous consent | Decision-making process | Undue influence, reduced autonomy, therapeutic misconception [5] [13] |
| Harm-Based | Vulnerability as increased probability of incurring research-related harm | Risk-benefit profile | Higher susceptibility to exploitation or adverse outcomes [5] [13] |
| Justice-Based | Vulnerability arising from unequal conditions or opportunities | Distributive justice | Exclusion from research benefits, unfair resource distribution [5] [13] |
Each approach carries distinct implications for clinician-researchers, who must remain alert to both categorical vulnerabilities (e.g., working with terminally ill patients) and context-dependent vulnerabilities that may emerge during the research process [5].
Practical Frameworks and Mitigation Strategies
Proactive Ethical Preparation and Boundary Protocols
Successful navigation of dual roles requires systematic preparation and clear boundary management strategies. Research demonstrates that enhanced ethical preparation and emotional resilience building are crucial for nurse researchers and clinician-investigators working with vulnerable populations [36]. Structured approaches should include:
- Pre-Research Boundary Planning: Establishing explicit protocols for handling clinical issues that arise during research activities, including predetermined referral pathways and intervention thresholds [36].
- Structured Reflexive Journaling: Maintaining detailed field notes and reflexive memos documenting emotional reactions, ethical uncertainties, and internal deliberations about emerging clinical concerns [36].
- Regular Peer Debriefing: Creating formal opportunities for externalizing ethical reflections through scheduled consultations with mentors or peer ethics groups, helping mitigate over-identification with participants [36].
These practices help maintain methodological integrity while responding ethically to participants' needs, particularly in resource-constrained environments where support services may be limited [36].
Ethical Engagement of Vulnerable Populations
Contemporary research ethics emphasizes appropriate inclusion rather than blanket exclusion of vulnerable populations. As noted by research ethics experts, "While vulnerable populations are considered at higher risk of harm or injustice in research, since they often cannot protect themselves through valid informed consent, they are also underrepresented and underserved in clinical research" [26]. Exclusion creates its own ethical problems by perpetuating inequities in evidence-based care [26].
Clinician-researchers should implement specific safeguards when engaging vulnerable participants:
- Enhanced Consent Processes: Utilizing iterative consent discussions, capacity assessments when indicated, and involving legally authorized representatives where appropriate while respecting the participant's assent or dissent [36] [26].
- Distinguishing Compensation from Coercion: Developing fair compensation structures that recognize participants' contributions without creating undue influence, particularly for economically disadvantaged groups [26].
- Cultural and Contextual Sensitivity: Practicing awareness and respect for research participants' cultures and conducting research procedures in ways that acknowledge cultural norms and values [36] [37].
The Association of Clinical Research Professionals' Code of Ethics emphasizes that clinical research professionals must "respect and safeguard the rights and welfare of all individuals with whom they interact professionally" and "never use coercion or undue influence when recruiting research participants" [37].
Methodological Approaches and Tools
Reflexive Methodologies for Ethical Engagement
Adopting appropriate methodological frameworks is essential for maintaining ethical integrity in clinician-researcher role duality. A reflective narrative approach provides a valuable methodological foundation for critically engaging with personal experiences, ethical dilemmas, and emotional complexities in sensitive research contexts [36]. This approach acknowledges the situated nature of the clinician-researcher role and creates space for systematic examination of how dual-role tensions influence data collection and interpretation [36].
Dyadic interview techniques can reveal relational dynamics and co-constructed narratives but require particular sensitivity to disclosure patterns and emotional protection [36]. These methods capture important interpersonal dimensions of healthcare experiences while introducing additional ethical considerations regarding confidentiality and potentially conflicting perspectives within caregiver-patient dyads [36].
Table: Essential Methodological Tools for Ethical Clinician-Researcher Practice
| Tool | Function | Ethical Application |
|---|---|---|
| Reflexive Journaling | Documents researcher reactions, ethical uncertainties, and decision rationales | Creates audit trail of ethical decision-making; mitigates projection bias [36] |
| Peer Debriefing Protocols | Structured consultation with ethics-aware colleagues | Provides external perspective on role conflicts; reduces isolation in ethical decision-making [36] |
| Boundary Planning Framework | Pre-established thresholds for clinical intervention during research | Maintains research integrity while ensuring participant safety; clarifies role expectations [36] |
| Iterative Consent Processes | Ongoing consent discussions throughout research participation | Respects participant autonomy; accommodates fluctuating capacity in vulnerable populations [36] [26] |
Ethical Analysis and Decision-Making Framework
The following diagram illustrates a systematic approach to ethical decision-making when dual-role conflicts arise during research activities:
This framework emphasizes both immediate response protocols and essential reflective processes for maintaining ethical integrity across multiple research encounters.
Implementation in Specific Research Contexts
Research in Resource-Limited Settings
Resource-constrained environments present distinctive challenges for clinician-researchers, where healthcare system limitations may intensify dual-role tensions. In these contexts, the ethical obligation to address clinical needs observed during research may be heightened by limited access to alternative care providers [36]. Research in Ghanaian palliative care settings demonstrates how clinician-researchers must balance rigorous data collection with responding to urgent clinical concerns, such as unsafe wound-care practices observed during home visits [36].
Essential adaptations for resource-limited settings include:
- Contextual Vulnerability Assessment: Identifying how systemic resource constraints create or exacerbate participant vulnerabilities beyond individual characteristics [36].
- Collaborative Partnership Models: Engaging local healthcare providers and systems in research planning to establish sustainable referral pathways that outlive individual research projects [36].
- Culturally Attuned Communication: Developing culturally competent, flexible engagement strategies to foster trust and authenticity when discussing sensitive topics [36].
Technological and Bias Considerations in Modern Research
Contemporary clinician-researchers must also navigate emerging ethical challenges related to technology and artificial intelligence in research. As artificial intelligence and machine learning systems become integrated into medical research, new dimensions of bias and ethical consideration emerge that clinician-researchers must address [38]. These technologies can introduce or amplify biases through multiple mechanisms, including data bias (unrepresentative training data), development bias (algorithmic design choices), and interaction bias (how systems are implemented in real-world contexts) [38].
Clinician-researchers utilizing these technologies should implement:
- Bias Auditing Protocols: Regular assessment of AI/ML tools for potential biases that might disproportionately affect vulnerable populations [38].
- Transparency Documentation: Clear documentation of how automated systems are employed in research processes and how their limitations might impact vulnerable participants [38].
- Technological Competence Development: Pursuing appropriate education to understand the ethical implications of research technologies being employed [38].
Navigating the clinician-researcher dual role requires ongoing attention to ethical complexities, particularly when working with vulnerable populations. By implementing structured reflective practices, establishing clear boundary protocols, and maintaining focus on the nuanced manifestations of vulnerability, clinician-researchers can conduct ethically sound research that respects participant autonomy and welfare while generating valuable knowledge.
The ethical imperative extends beyond mere compliance with regulations toward cultivating a research practice that remains responsive to both clinical responsibilities and scientific integrity. Through thoughtful engagement with these guidelines, clinician-researchers can contribute to a research culture that appropriately includes vulnerable populations while implementing robust safeguards against exploitation or harm.
Community Engagement and Trust-Building with Marginalized Groups
The concept of vulnerability is a cornerstone of the theoretical basis and practical application of ethics in human subjects research [3]. Within research ethics, vulnerable populations are defined as groups or individuals with an increased likelihood of being wronged or incurring additional harm, often due to a diminished ability to protect their own interests [3]. This vulnerability can stem from intrinsic factors (e.g., cognitive impairment, age) or situational circumstances (e.g., poverty, institutional setting, language barriers) that limit the capacity to provide voluntary, informed consent or increase the risk of exploitation [3] [39].
Engaging these communities is not merely an ethical nicety but a scientific and moral imperative. The generalizability and applicability of clinical research findings depend on the inclusion of diverse populations [40]. Furthermore, persistent health disparities often disproportionately affect marginalized groups, making their participation essential for developing effective, equitable health interventions [41] [42]. This guide provides a technical framework for researchers seeking to build authentic, trust-based partnerships with marginalized communities, positioning such engagement as a fundamental requirement within a broader research ethics framework.
Theoretical Foundations: Understanding Vulnerability and Trust
Conceptualizing Vulnerability
A nuanced understanding of vulnerability moves beyond a simple categorical checklist. Two primary approaches inform ethical research design:
- Categorical Vulnerability: This approach identifies specific groups as vulnerable (e.g., children, prisoners, pregnant women, economically disadvantaged persons) [3]. While this is operationalized in regulations like the Common Rule (45 CFR §46), it is a blunt instrument. It may not account for individuals with multiple vulnerabilities, variations within a group, or the context-specific nature of vulnerability [3].
- Contextual Vulnerability: This more fluid approach identifies situations that render an individual vulnerable [3]. For example, an affluent executive is not typically vulnerable but may become so when experiencing a medical emergency. This approach allows for more tailored safeguards. Contextual vulnerabilities can be classified as:
- Cognitive or Communicative: Difficulty comprehending information or making decisions [3].
- Institutional: Being under the formal authority of others (e.g., prisoners, military personnel) [3].
- Deferential: Being under informal authority or influence (e.g., due to race, class, or a doctor-patient relationship) [3].
A modern ethical framework recognizes that vulnerability occurs along a spectrum and is sensitive to the specific research context [3]. This requires investigators and Institutional Review Boards (IRBs) to ask two key questions: (1) Is the inclusion of potentially vulnerable individuals scientifically necessary? and (2) If so, are the safeguards adequate to protect their rights and welfare? [3].
The Centrality of Trust and Historical Mistrust
Trust is the foundational element upon which successful community-engaged research is built. For many marginalized communities, historical mistrust of research institutions is a significant barrier, rooted in a legacy of exploitation and unethical treatment [43] [42]. This is particularly true for Native American communities, who have often been over-researched without benefiting from the results, and Black American communities, whose mistrust is fueled by historical events like the Tuskegee syphilis study [43] [42].
Building trust requires a paradigm shift from conducting research "on a community" to partnering "with a community" [42]. This involves acknowledging past harms, demonstrating cultural humility, and ceding control over the research agenda to ensure it provides genuine value to the community [43].
A Methodological Framework for Engagement and Trust-Building
Foundational Principles for Partnership
The following principles, derived from successful long-term partnerships, should guide the research process [43].
Table 1: Foundational Principles for Community-Engaged Research
| Principle | Core Question | Key Actions |
|---|---|---|
| Getting It Right | Do we accurately understand the community's structure, history, and culture? | Learn the political and historical evolution of the community, including tribal structures for Native communities [43]. |
| Working With What You Got | How do we identify and leverage existing community resources and assets? | Identify and use local resources; compensate community members for their time and expertise; conduct activities in accessible, community-preferred locations [43]. |
| Creating Co-Ownership | Does the community have genuine ownership and control over the research process? | Develop memoranda of understanding; involve community partners in instrument design, data interpretation, and dissemination; ensure community benefits from the research [43]. |
| Playing by the (Cultural) Rules | Are we respecting and adhering to cultural norms and worldviews? | Recognize that cultural norms supersede research agendas; adapt linear research processes to be more circular or dynamic to align with community worldviews [43]. |
Community-Based Participatory Research (CBPR) as a Core Methodology
Community-Based Participatory Research (CBPR) is an evolving research approach that emphasizes developing meaningful and equitable partnerships between researchers and community partners [41]. It is an ideal methodology for engaging marginalized populations as it prioritizes long-term commitments, knowledge-sharing, and community empowerment [41]. The CBPR process is often visualized as a cycle of look, think, and act, though these phases are dynamic and overlapping [43].
The following diagram illustrates the key stages and iterative nature of building a community partnership.
Operationalizing Engagement: Phases and Protocols
Phase 1: Preparation and Partnership Formation
- Establish a Community Partnership Steering Committee (CPSC): Form a committee with representative members from the community. Their role includes reviewing materials, selecting culturally appropriate measurements, and providing cultural guidance [43].
- Build a Demographically Representative Research Team: A research team that shares demographic characteristics with the community can enhance trust and cultural competence [42].
- Negotiate a Memorandum of Understanding (MOU): A formal MOU between the academic institution and community entities (e.g., tribes) can clarify roles, expectations, and data ownership [43].
Phase 2: Community Entry and Trust-Building
- Identify "Community Champions": Leverage trusted individuals within the community, such as religious leaders or respected elders, to vouch for the research and facilitate introductions [42].
- Ensure Transparency and Clarity: From the outset, be transparent about the research goals, what participation involves, how data will be used, and how the community will benefit [42].
- Employ Effective Recruitment Modes: Use trusted channels like community-based organizations (CBOs), churches, and cultural centers for recruitment. Materials should be in plain language and accessible formats [42].
Phase 3: Data Collection with Cultural Sensitivity
Engagement must be tailored to the community's preferences and logistical realities. A recent scoping review of CBPR with marginalized pediatric populations identified the following common methodologies, though their application varies widely [41].
Table 2: Common Engagement Methods in CBPR with Marginalized Pediatric Populations [41]
| Method Category | Specific Methods Cited | Reported Effectiveness & Challenges |
|---|---|---|
| Community Partnership | Forming steering committees; partnering with CBOs | Foundational for relevance and trust; requires significant time investment. |
| Qualitative Engagement | Focus groups; in-depth interviews; digital storytelling | Effective for exploring sensitive topics; can be challenging with youth. |
| Advisory Structures | Youth advisory boards; community advisory boards | Provides ongoing guidance; requires careful management of power dynamics. |
| Electronic Participation | Online surveys; mobile phone diaries; virtual meetings | Increases reach; may exclude those with limited tech access or literacy. |
Considerations for Online Research with Vulnerable Populations: Online methods can offer participants privacy and comfort. Key protocols include [39]:
- Allowing extra time to cultivate rapport and trust in virtual settings.
- Permitting participants to choose their preferred communication tools (e.g., audio-only vs. video).
- Partnering with service agencies to provide technical support, ensuring participants without digital literacy are not excluded.
Phase 4: Dissemination and Sustaining Partnerships
- Disseminate Findings Back to the Community: This is a critical, often overlooked step. Share results in accessible formats and languages, through community forums, briefs, and infographics [42]. This demonstrates respect and completes the ethical circle of communication.
- Ensure Ongoing Benefit to the Community: The partnership should not end with publication. Researchers should volunteer expertise, engage in cultural exchanges, and support community-driven health initiatives to build a lasting, reciprocal relationship [43].
This table details key resources and their functions for planning and conducting ethical research with marginalized groups.
Table 3: Research Reagent Solutions for Community-Engaged Research
| Item / Solution | Function in the Research Process |
|---|---|
| Community Advisory Board (CAB) | Provides ongoing, strategic guidance on all research phases; ensures cultural and contextual relevance; helps navigate community dynamics [42]. |
| Memorandum of Understanding (MOU) | A formal contract clarifying roles, responsibilities, data ownership, and dissemination rights; foundational for establishing co-ownership [43]. |
| Culturally-Translated & Plain-Language Consent | Ensures truly informed consent by presenting information in a language, literacy level, and format that is understandable to participants [3] [40]. |
| Stipends for Community Member Time | Compensates community members (e.g., CPSC members) for their expertise, time, and travel; recognizes the value of their contribution [43]. |
| Digital Storytelling Kits | An arts-based method that empowers participants to share their experiences through narrative and video; can be particularly effective for mental health research [39]. |
| Mobile Data Collection Tools | Tools like mobile phone diaries allow for data collection in the context of participants' daily lives, useful for engaging transient or "hard-to-reach" groups [39]. |
Ethical and Regulatory Safeguards
Engaging vulnerable populations requires adherence to a stringent ethical and regulatory framework designed to protect participants.
- Informed Consent: The process must be tailored to capacity and context. For children, this involves parental consent and the child's assent. For the cognitively impaired, consent from a legally authorized representative is required, with the individual's involvement to the greatest extent possible. Using clear, non-technical language and multimedia aids is essential for all vulnerable groups [40].
- Risk-Benefit Assessment: Regulatory bodies require that potential benefits outweigh the risks. Researchers must minimize risks through protocol design and ensure vulnerable populations are selected for scientifically valid reasons, not merely convenience [3] [40].
- Independent Review: IRBs or Ethics Committees must scrutinize protocols involving vulnerable populations to ensure additional safeguards are in place [3] [40].
Community engagement and trust-building with marginalized groups is a sophisticated, iterative process that demands a fundamental reorientation of the researcher's role. It requires moving from being an "expert" extracting data to a "partner" generating knowledge with a community. By grounding work in the ethical concepts of contextual vulnerability and justice, adhering to foundational principles of partnership, and implementing rigorous, flexible CBPR methodologies, researchers can overcome historical mistrust. This approach not only ensures ethical compliance but also enhances the scientific rigor, relevance, and ultimate impact of research, contributing to the reduction of health disparities and the promotion of equitable health outcomes for all.
The protection of participant privacy is a foundational ethical imperative in scientific research, becoming critically important when studies involve vulnerable populations. The concept of vulnerability in research was formally introduced in The Belmont Report (1979), which defined vulnerable individuals as those in a "dependent state and with a frequently compromised capacity to free consent" [13]. Modern research ethics recognizes that vulnerability can stem from various factors including age, socio-economic status, cognitive impairment, or situational contexts that may compromise autonomous decision-making [10].
Within this framework, robust data management and confidentiality protocols serve as essential mechanisms for upholding the ethical principles of respect for persons, beneficence, and justice. These protocols ensure that the increased risks of privacy breaches, stigmatization, or exploitation that vulnerable populations may face are systematically mitigated throughout the research lifecycle [13] [10]. This technical guide provides comprehensive methodologies for implementing these critical protections, with particular attention to the specialized considerations required when researching vulnerable groups.
Foundational Concepts and Regulatory Framework
Defining Confidentiality in Research Contexts
In research ethics, confidentiality encompasses distinct but related concepts for protecting participant information [44]:
- Confidentiality: Personal identifiers are collected and known to the researcher but are protected from unauthorized access or disclosure. Security measures are implemented to safeguard the link between the data and the individual's identity.
- Anonymity: No identifiers are collected, and no one, including the researcher, can link the data to the individual who provided it. This represents the highest standard of privacy protection.
- Pseudonymization: Identifiers are replaced with a code key. The data can potentially be re-identified using this key, which must be stored separately and securely.
Ethical Justifications for Enhanced Protections
The imperative for stringent data protection in research with vulnerable populations is grounded in several ethical considerations. Vulnerability is often conceptualized through consent-based accounts, where individuals may have diminished capacity to provide fully autonomous informed consent due to undue influence or compromised autonomy [13]. Additionally, justice-based accounts highlight that vulnerable groups may experience unequal social conditions, thereby warranting special provisions to ensure equitable treatment and avoid exploitation in research settings [13]. Furthermore, research involving vulnerable populations frequently addresses sensitive topics (e.g., health status, illegal activities, trauma), where accidental disclosure of private information could result in significant social, psychological, or legal harm to participants [10] [44].
Pre-Research Planning: Establishing a Confidentiality Framework
Data Responsibility Matrix
Before collecting any data, researchers must establish a clear chain of responsibility for handling participant information. The following table outlines essential roles and responsibilities [44]:
| Role | Primary Responsibilities | Access Level |
|---|---|---|
| Data Controller | Determines how and why personal data is processed; oversees collection methods, storage duration, and sharing protocols [44]. | Full access to all data and documentation. |
| Data Processor | Handles specific tasks such as data transcription, analysis, or cleaning based on assigned protocols [44]. | Restricted to data necessary for their specific task. |
| Data Protection Officer | Oversees compliance with confidentiality protocols; acts as primary contact for participant concerns; conducts internal audits [44]. | Full access for monitoring and compliance purposes. |
Participant Notices and Informed Consent Protocols
Transparent communication with potential participants is a cornerstone of ethical research. Consent forms and informational notices should be crafted using accessible, jargon-free language that the participant can easily understand and recall [44].
These documents must explicitly address [44]:
- The specific types of data being collected (e.g., name, audio recordings, health history).
- The purpose of data collection and all potential future uses (e.g., publication, secondary analysis).
- The data retention timeline, specifying how long data will be stored and the method of secure destruction afterward.
- Withdrawal rights, clearly stating that participants can leave the study at any time and request data deletion, including the process and contact person for doing so.
- For research with vulnerable groups, consider implementing additional consent layers, such as separate agreements for audio recording or the use of anonymized quotes [10].
Data Minimization Strategy
The principle of data minimization involves collecting only the personal data absolutely necessary to achieve the research objectives [44]. This reduces privacy risks and simplifies data management.
Implementation steps include [44]:
- Systematically reviewing each planned data point against the research questions.
- Using broad categories (e.g., age range instead of exact age) where sufficient.
- Planning for progressive data deletion (e.g., deleting contact information after communication is complete).
- Designing data collection tools to avoid gathering extraneous personal details.
Data Collection and Management Protocols
Secure Data Collection Workflow
The following diagram illustrates a secure workflow for handling data from collection to analysis, emphasizing the separation of identifiers from the outset.
Secure Data Handling Workflow
Secure Data Collection Tools and Practices
During the data collection phase, researchers must employ technically secure methods to prevent unauthorized access or data breaches [44].
- Tool Selection and Configuration: Utilize enterprise-grade platforms with end-to-end encryption for video interviews, surveys, or data transfers. Before deployment, test all tools with dummy data to identify potential security gaps, disabling unnecessary features like IP address collection. For mobile data collection, ensure devices have screen locks, encryption, and are dedicated solely to research purposes [44].
- Informed Consent as a Process: The initial signing of a form is one component. Researchers should begin each data collection session with a verbal recap of key data protection information and confirm the participant's continued consent. All consent must be thoroughly documented, including the time, date, and method. Crucially, procedures must be in place for the immediate cessation of data collection and execution of data deletion requests if a participant withdraws consent [44].
- Handling Sensitive Disclosures: Despite planning, participants may reveal unexpectedly sensitive information. Researchers should be trained to identify and gently interrupt to suggest the use of a general term instead of a specific identifier. A protocol for documenting these redactions is essential. For data requiring processing (e.g., transcription), use secure temporary storage with automatic deletion dates [44].
Post-Collection Data Management and Analysis
Data Anonymization and Aggregation Techniques
Once data is collected, the primary technical task is to de-identify it for analysis while preserving its utility and statistical integrity.
- Separation of Identifiers: The first step is to create at least two distinct datasets: one containing the identifiers linked to a secure, random participant code, and another containing the research data linked only by that same code. These datasets must be stored separately with different access controls. The identifier file should have the most restricted access, ideally limited to one or two team members responsible for participant communication [44].
- Aggregation and Suppression for Publication: When preparing data for reports or publications, use aggregation (e.g., presenting summary statistics for groups) to prevent re-identification. In tables or graphs, employ cell suppression by withholding data in any cell that contains a number of participants below a pre-defined threshold (e.g., below 5) to prevent the deduction of individual responses [44].
Data Storage and Disposal Protocol
A clear and enforced policy for the retention and destruction of research data is a critical component of confidentiality [44].
- Secure Storage Solutions: All electronic data should be stored on encrypted drives or secure, password-protected university/enterprise servers. Cloud storage solutions used must have robust security agreements and encryption in transit and at rest. Physical data (e.g., signed consent forms) must be kept in locked filing cabinets in access-controlled rooms.
- Scheduled Data Disposal: The research plan must specify a data retention schedule. Data should not be kept indefinitely. Once the retention period (justified by the research purpose) has expired, data must be disposed of securely. Electronic data should be deleted using software that overwrites the data, making it unrecoverable. Physical documents should be cross-cut shredded [44].
Essential Research Reagent Solutions for Data Security
The following table details key tools and methodologies that constitute the modern researcher's toolkit for ensuring data confidentiality [44].
| Tool Category | Specific Examples | Function & Application |
|---|---|---|
| Encrypted Collection Platforms | Enterprise-grade video conferencing (e.g., Zoom for Healthcare); encrypted survey tools (e.g., Qualtrics); secure data transfer services (e.g., SFTP servers). | Protects data in transit during collection and transfer, preventing interception by unauthorized parties. |
| Secure Storage Systems | Encrypted hard drives (e.g., BitLocker, FileVault); institutional secure servers; access-controlled cloud storage with strong security agreements. | Safeguards data at rest against unauthorized access, theft, or hardware loss. |
| Pseudonymization Software | Custom spreadsheet scripts; dedicated data management software (e.g., REDCap); random code generators. | Systematically replaces direct identifiers with codes, facilitating the separation of identity from research data. |
| Secure Disposal Tools | Certified data-wiping software (e.g., DBAN); professional document shredding services. | Ensures the permanent and irretrievable destruction of data after the retention period expires, closing the data lifecycle securely. |
Implementing rigorous data management and confidentiality protocols is a non-negotiable standard for all research, but it carries particular moral and practical weight in studies involving vulnerable populations. By moving beyond a simple compliance checklist and embracing a comprehensive framework—from pre-research planning and secure data collection to responsible analysis and final disposal—researchers can honor their ethical commitment to participant autonomy and justice. This proactive approach not only mitigates the risk of harm but also actively builds the trust that is essential for conducting meaningful and respectful research with vulnerable communities.
Navigating Ethical Dilemmas: Solutions for Common and Complex Challenges
Identifying and Mitigating Undue Influence and Coercion in Recruitment
The ethical conduct of human subjects research rests upon the foundational principle of respect for persons, which requires that participation be voluntary and based on adequately informed consent. Within the context of vulnerable populations research ethics, this principle demands vigilant identification and mitigation of coercion and undue influence during participant recruitment. These compromising influences undermine autonomy and represent significant ethical breaches that can harm participants, compromise data integrity, and erode public trust in research. A nuanced understanding of these concepts is therefore essential for researchers, scientists, and drug development professionals committed to upholding the highest ethical standards.
The Belmont Report, a cornerstone of research ethics, first formalized concerns for vulnerable individuals, defining them as those in a "dependent state and with a frequently compromised capacity for free consent" [5] [13]. Modern ethics frameworks have evolved from strictly prohibiting enrollment of vulnerable groups toward ensuring their appropriate involvement with additional safeguards, thereby balancing the ethical duty of protection with the imperative of justice and inclusion [5] [26]. This whitepaper provides a technical guide for operationalizing these principles, offering a detailed roadmap for identifying and mitigating coercion and undue influence throughout the recruitment lifecycle.
Core Concepts: Distinguishing Coercion and Undue Influence
Definitions and Key Distinctions
Precise differentiation between coercion and undue influence is a prerequisite for effective mitigation. While both undermine voluntary participation, they operate through distinct mechanisms.
- Coercion occurs when an overt or implicit threat of harm is intentionally presented by one person to another to obtain compliance [45] [46]. It involves the prospect of a negative consequence for non-participation. For example, a clinical trial participant might be led to believe that refusing enrollment could limit their access to routine medical care, or a student might fear academic repercussions from a professor-investigator for declining to take part in research [45].
- Undue Influence arises through an excessive or inappropriate offer of an attractive or desirable benefit that clouds a potential participant's judgment, leading them to make decisions against their better judgment or without adequate consideration of risks [45] [46]. Unlike coercion, it exploits a power imbalance or a person's circumstances. A classic example is offering disproportionately high financial compensation to economically disadvantaged individuals, potentially compelling them to enroll despite potential risks [45].
The following table summarizes the core differences:
Table 1: Distinguishing Coercion from Undue Influence
| Feature | Coercion | Undue Influence |
|---|---|---|
| Core Mechanism | Threat of harm or negative consequence | Excessive or manipulative offer of a benefit |
| Participant Perception | Avoidance of a penalty | Pursuit of an inappropriate reward |
| Typical Context | Explicit or implicit power dynamics (e.g., institutional authority) | Situational vulnerability (e.g., economic disadvantage) |
| In Research Settings | Fear of reprisal from an authority figure | Compensation or incentives that overshadow risk assessment [46] |
The Concept of Vulnerability
Vulnerability is a situational or inherent state that increases the risk of being subjected to coercion or undue influence. Policy documents and ethics committees often use two primary approaches to conceptualize vulnerability:
- The Group-Based (Categorical) Approach: This method identifies entire groups as vulnerable based on shared characteristics. It is pragmatically simpler for Institutional Review Boards (IRBs) to implement but can be over-inclusive and stigmatizing [5] [13]. Commonly listed groups include children, prisoners, pregnant women, individuals with cognitive impairments, and the economically or educationally disadvantaged [5] [26] [47].
- The Analytical (Contextual) Approach: This more nuanced framework focuses on the potential sources of vulnerability within a specific research context. It is increasingly considered theoretically preferable and includes three primary accounts [5] [13]:
- Consent-based accounts: Vulnerability stems from a compromised capacity to provide voluntary, informed consent.
- Harm-based accounts: Vulnerability arises from a higher probability of incurring harm or injury during research.
- Justice-based accounts: Vulnerability results from systemic inequalities and unfair distribution of the burdens and benefits of research.
Identifying Vulnerable Populations and Risk Factors
A systematic approach to identifying vulnerability is the first step in preventing unethical recruitment. The following table synthesizes common vulnerable populations, their specific risks, and the primary type of influence they are most susceptible to, as identified in policy documents and ethical guidelines [5] [47] [46].
Table 2: Vulnerable Populations and Associated Recruitment Risks
| Population | Characteristics & Context | Susceptibility to | Specific Recruitment Risks |
|---|---|---|---|
| Children & Adolescents | Limited capacity for understanding; parental authority. | Undue Influence | Incentives (toys, gift cards) may overwhelm a child's judgment; compensation to parents may cloud their assessment of the child's best interest [46]. |
| Prisoners | Incarcerated setting; limited autonomy and economic opportunities. | Coercion & Undue Influence | Perceived pressure from prison authorities; compensation is disproportionately attractive due to limited earning options [47] [46]. |
| Individuals with Cognitive Impairments | Diminished capacity to understand research information. | Undue Influence | Difficulty comprehending risks and benefits, making them susceptible to appealing offers they may not fully contextualize [47]. |
| Economically Disadvantaged | Financial hardship; limited access to healthcare. | Undue Influence | Disproportionately high financial incentives may compel participation despite risks [45] [5]. |
| Students | Power imbalance with faculty-investigators; grade dependency. | Coercion | Fear of academic repercussions if they decline to participate, especially when recruited by their own instructors [45] [48]. |
| Racial/Ethnic Minorities | Historical mistrust; language or cultural barriers. | Coercion & Undue Influence | May not feel free to refuse participation to authority figures; may not fully understand consent forms, making incentives more influential [48]. |
This workflow diagram illustrates the logical process for identifying vulnerability and associated risks of coercion and undue influence during recruitment planning and screening:
A Framework for Mitigation: Strategies and Protocols
Foundational Ethical Principles
Mitigation strategies must be grounded in the three core principles of research ethics established by the Belmont Report:
- Respect for Persons: Recognizing the autonomy of individuals and protecting those with diminished autonomy [45] [10].
- Beneficence: The obligation to maximize possible benefits and minimize potential harms [45].
- Justice: Ensuring the fair distribution of the burdens and benefits of research [45] [26].
Proactive Mitigation Strategies
A comprehensive mitigation plan involves proactive measures across the recruitment and consent process.
Table 3: Proactive Mitigation Strategies for Recruitment
| Strategy Domain | Specific Actions | Target Outcome |
|---|---|---|
| Transparent Communication & Consent | Use accessible language; ensure comprehension through quizzes or teach-back methods; disclose all risks and the voluntary nature of participation. | Truly informed consent; reduced misunderstanding. |
| Managing Power Imbalances | Avoid recruiting dependent populations (e.g., one's own students) where possible; use neutral third parties for recruitment; ensure refusal has no consequences. | Voluntary participation free from fear of reprisal [45] [48]. |
| Structuring Payments Ethically | Differentiate between reimbursement, compensation, and incentives; ensure amounts are reasonable and not excessive; prorate compensation. | Minimizes undue influence from financial incentives [46]. |
| Team Training & Competency | Train all research staff on ethics, identifying vulnerability, and communication skills; conduct mock recruitment sessions. | Consistent, ethical implementation of protocols. |
| IRB Collaboration & Review | Engage the IRB early; submit detailed recruitment plans and consent materials; seek guidance on specific vulnerable groups. | Independent ethical oversight and approval [45]. |
Ethical Payment Structures
Financial compensation is a common area of concern for undue influence. The following table breaks down acceptable payment types and their ethical considerations, based on guidance from leading research institutions [46].
Table 4: Ethical Framework for Research Participant Payments
| Payment Type | Purpose | Ethical Justification | Examples & Best Practices |
|---|---|---|---|
| Reimbursement | To cover out-of-pocket expenses (travel, parking, meals). | Restores participant to pre-enrollment financial baseline; no net benefit, thus minimal risk of undue influence. | Provide $5 for clinic parking; reimburse airfare and lodging for out-of-state participants [46]. |
| Compensation | To offset time and burden associated with participation. | Makes research participation as attractive as other ways of spending time; generally not unduly influential if reasonable. | Pay at local average wage (e.g., $15/hour) for time spent in study procedures [46]. |
| Incentives | To improve recruitment and retention rates. | Carries the highest risk of undue influence, as it is intended to positively influence the decision to enroll. | Offer a modest bonus for completing all study visits. Should be used cautiously and reviewed carefully by the IRB [46]. |
Monitoring and Oversight: Ensuring Ongoing Compliance
Ethical vigilance must extend beyond initial recruitment into the entire trial duration. Continuous monitoring is essential to detect and rectify any emergent coercion or undue influence.
Experimental Protocols for Monitoring
The following methodologies provide a framework for systematic monitoring:
Protocol for Consent Process Audits
- Objective: To verify that the informed consent process is conducted properly and without pressure.
- Methodology: An independent auditor (e.g., a Quality Assurance monitor or a member of the Data and Safety Monitoring Board) reviews a random sample of consent forms and conducts brief, confidential interviews with a subset of recent participants. The interview script includes questions such as, "Did you feel any pressure to join this study?" and "Were you able to ask all the questions you wanted?"
- Data Analysis: Qualitative analysis of interview responses for themes of pressure or misunderstanding; quantitative tracking of consent form completion errors.
Protocol for Monitoring Drop-Out Rates
- Objective: To identify potential undisclosed coercion or undue influence that manifests after enrollment.
- Methodology: Track participant withdrawal rates by recruitment source and recruiter. Investigate any significant deviations from the average. High drop-out rates from a specific subgroup or site may indicate that participants felt pressured to enroll initially but later sought to exit.
- Data Analysis: Statistical process control (e.g., Shewhart charts) to identify non-random patterns in withdrawal data.
Protocol for Interim Ethical Analysis
- Objective: To proactively assess participant welfare and the ethical climate of the trial.
- Methodology: The Trial Monitoring Committee reviews aggregated, anonymized data from safety reports, drop-out rates, and any participant feedback surveys. They specifically look for patterns that suggest participant discomfort or lack of voluntariness [47].
- Data Analysis: Trend analysis over time to ensure that ethical metrics remain stable and acceptable.
Table 5: Key Research Reagent Solutions for Ethical Recruitment
| Tool or Resource | Function in Ethical Recruitment | Application Example |
|---|---|---|
| Institutional Review Board (IRB) | Provides independent ethical review and approval of all recruitment materials and strategies before study initiation [45] [10]. | Submitting flyers, advertisement scripts, and the informed consent document for IRB approval. |
| Digital Consent Platforms | Streamlines the consent process; can incorporate multimedia (videos, quizzes) to enhance understanding; ensures version control and audit trails. | Using an iPad-based app to walk a participant with low literacy through an interactive consent module. |
| Anonymous Reporting Hotline | Provides a safe channel for participants or research staff to report observed coercive practices or ethical concerns without fear of reprisal [47]. | A phone number listed on the consent form that participants can call to voice concerns directly to the ethics committee. |
| Data Safety and Monitoring Board (DSMB) | An independent group of experts that monitors participant safety and treatment efficacy data during a clinical trial, which can include review of ethical metrics [47]. | The DSMB reviews aggregate data on participant withdrawals and reasons for withdrawal as part of their safety review. |
| Cultural/Linguistic Validated Tools | Translated and culturally adapted consent forms and study instruments ensure comprehension for non-native speakers and diverse populations. | Using a consent form that has been translated by a certified professional and validated through cognitive interviewing with the target population. |
The identification and mitigation of coercion and undue influence are not regulatory hurdles but fundamental components of ethical and scientifically valid research. For researchers and drug development professionals, this demands a shift in perspective—from viewing vulnerability merely as a checklist for IRB approval to embracing a continuous, analytical process of ethical vigilance. By integrating the frameworks, protocols, and tools outlined in this whitepaper—grounded in the analytical approach to vulnerability and a justice-based framework for inclusion—the research community can uphold its commitment to participant dignity. This ensures that the pursuit of knowledge and innovative therapies is built upon a foundation of unwavering respect for all individuals who contribute to scientific progress.
Managing the Emotional Labor and Boundary Tensions in Sensitive Research
Engaging in research with vulnerable populations places significant affective demands on researchers, necessitating a structured approach to managing the associated emotional labor and boundary tensions. Emotional labor, defined as the process of managing one's feelings and expressions to fulfill the emotional requirements of a job, is a fundamental, yet often overlooked, component of sensitive research [49] [50]. Within the specific context of a broader thesis on research ethics with vulnerable populations, this in-depth guide addresses the critical need to recognize and institutionalize support for the emotional and psychological well-being of researchers. The aim is to move beyond individual coping strategies and toward an ethical imperative for organizations to build a sustainable and equitable research culture that proactively mitigates the risks of burnout, vicarious trauma, and emotional exhaustion [51].
Theoretical Foundations: Emotional Labor and Boundary Spanning
Conceptualizing Emotional Labor in Research
Emotional labor is the effort invested in evoking or suppressing feelings to present a professionally appropriate outward demeanor, a task that is particularly salient when a researcher's genuine emotions are not concordant with the demands of the situation [50]. This labor involves two key aspects:
- Adherence to Display Rules: Researchers must often follow unwritten rules governing their outward emotional expression, which may require suppressing reactions of distress, anger, or frustration during interactions with participants or when engaging with traumatic data [49].
- Building and Maintaining Trust: A core part of the research relationship, especially with vulnerable groups, involves fostering perceptions of competence and trust, making participants feel heard and treated fairly [49].
This labor can be performed through surface acting (showing a "fake" emotion that is not genuinely felt) or deep acting (making an effort to actually feel and show a genuine emotion aligned with one's values). Surface acting is known to be more mentally taxing and depleting than deep acting [50].
Boundary Tensions as Spanning Roles
Researchers working with vulnerable populations often act as boundary spanners. This role involves operating across the borders between their own institutional context, the lived reality of the participant community, and often, multiple other service sectors (e.g., health, social services) [49]. The boundary spanner must filter and transfer information across these domains, communicate with different "masters," and develop interpersonal trust across boundaries [49]. This role is fraught with tension, as the researcher must be sensitive to the social cues and normative expectations of these different groups, constantly adapting their emotional presentation and navigating complex relational dynamics [49].
Table: Types of Emotional Labor in Sensitive Research
| Type of Labor | Definition | Research Context Example |
|---|---|---|
| Surface Acting | Displaying an emotion that is not genuinely felt by suppressing true feelings. | A researcher feels frustrated with a participant's account but maintains a neutral and patient expression. |
| Deep Acting | Making an effort to genuinely feel and exhibit the expected emotion, often aligned with personal values. | A researcher consciously cultivates empathy to provide a supportive presence for a distressed participant. |
| Boundary Spanning | Managing relationships and information across different organizational or professional domains. | A health researcher coordinates a participant's care with social services and clinical providers, navigating different institutional logics. |
Impacts and Institutional Imperatives
The Cost of Unsupported Emotional Labor
The cumulative effect of unacknowledged and unsupported emotional labor can be severe, both for the individual researcher and the research enterprise. Adverse outcomes include [51] [50]:
- Psychological & Physical Health: Emotional exhaustion, burnout, insomnia, depersonalization, and heightened risk for conditions like hypertension and heart disease.
- Cognitive & Performance Impacts: Depletion of cognitive energy leading to more mistakes, longer task completion times, and reduced job satisfaction.
- Organizational Damage: High staff turnover, loss of experienced researchers, and a deterioration of the overall research culture.
The risks are particularly acute for individuals from groups often expected to perform unpaid emotional labor, such as women and people of color, potentially exacerbating existing inequities in the research field [50].
A Strategic Institutional Framework
A proactive, institutional-level strategy is required to ethically manage emotionally challenging research. This can be conceptualized in three escalating stages of implementation [51]:
- Bronze Stage: Focused on awareness and foundational policies. This involves raising awareness of emotional labor and its impacts, developing guidance that is integrated into ethical review procedures, and ensuring basic legal health and safety risk assessments are in place.
- Silver Stage: Involves active support and project-level integration. This includes establishing training for researchers and supervisors, creating clear referral pathways for professional support, and mandating funded, project-specific "Researcher Wellbeing Plans."
- Gold Stage: Represents a holistic, transformative cultural response. At this stage, policies, processes, and daily practices are all proactively attentive to the prevention of and provision for research-related distress, creating a supportive and sustainable research environment.
Experimental Protocols and Methodological Considerations
Protocol for Studying Emotional Labor
To systematically investigate the emotional labor of researchers, a mixed-methods approach can be employed, drawing on validated methodologies.
Workplace Assessment Protocol (Informed by Pines et al., 2024): A study design to investigate emotional labor and workplace violence management can be adapted for the research context [52].
- Participant Recruitment: Recruit a purposive sample of researchers (e.g., 26 participants) across various disciplines and career stages who work with vulnerable populations.
- Data Collection: Conduct in-depth, semi-structured interviews to explore:
- Specific strategies used to de-escalate challenging interactions with participants.
- Perceptions of how institutional context shapes their ability to manage affective demands.
- Initial perceptions that shape engagement with aggressive or distressed participants.
- Experiences of emotional labor and its connection to burnout.
- Data Analysis: Employ thematic analysis, using emotional labor constructs (surface acting, deep acting, display rules) as a framework for coding the interview transcripts. This allows for the investigation of how researchers use emotion management to smooth communication and build relationships.
Workflow for Studying Emotional Labor in Research Teams The following diagram illustrates the sequential and cyclical process for a research team engaging with emotionally challenging data, highlighting points of emotional risk and necessary support interventions.
The Researcher's Wellbeing Toolkit
Effectively managing emotional labor requires both personal and institutional tools. The following table details essential components of a support system for researchers.
Table: Essential Support Systems for Managing Emotional Labor
| Support Category | Specific Tool / Mechanism | Function & Rationale |
|---|---|---|
| Organizational Policy | Researcher Wellbeing Plan | A proactive, project-specific document created before research begins, outlining potential emotional risks and planned coping strategies [51]. |
| Modified Ethics Protocols | Ethics committee guidelines explicitly include consideration of mental health impacts on researchers and require plans to address them [51]. | |
| Training & Development | Emotional Agility Training | Teaches researchers skills for naming, expressing, and discussing emotions, moving beyond assumptions that these skills are innate [50]. |
| Recognition of Emotional Labor | Affirming that emotional labor matters through formal conversations and team meetings, helping to reduce stigma and encourage sharing [50]. | |
| Interventional Support | Independent Wellbeing Supervision | Regular, confidential meetings with a paid counselor/therapist independent of the employer, focused solely on researcher wellbeing [51]. |
| Peer Support Networks | A formal or informal network of experienced and novice researchers to share advice and normalize experiences of emotional challenge [51]. | |
| Practical Research Management | Task Rotation & Exposure Limits | Reducing exposure to traumatic data by rotating tasks among team members and limiting the number of emotionally intense interviews per day [51]. |
| Scheduled Recovery Time | Ensuring researchers take regular, mandated breaks to allow for mental and emotional recovery, preventing cumulative exhaustion [50]. |
Visualization of Support Systems and Workflows
A Tiered Model for Institutional Response
The following diagram maps the strategic, three-stage institutional framework (Bronze, Silver, Gold) for supporting researcher wellbeing, detailing the key initiatives and responsible parties at each level.
Managing the emotional labor and boundary tensions inherent in sensitive research is not a peripheral concern but a central pillar of ethical research practice, particularly within a thesis focused on vulnerable populations. A comprehensive approach that combines individual emotional agility with robust, institutional support structures is essential for protecting researcher well-being and ensuring the integrity and sustainability of the research itself. The frameworks, protocols, and tools outlined in this guide provide a roadmap for transforming research culture from one that tacitly expects emotional labor to one that explicitly recognizes, values, and supports it, thereby fostering a more humane, equitable, and rigorous scientific enterprise.
The premature closure of a clinical trial is a significant event that extends beyond a simple operational halt; it represents a critical ethical juncture requiring meticulous management to protect participant welfare and maintain scientific integrity. This is particularly paramount when trials include vulnerable populations—individuals with diminished autonomy or those especially susceptible to coercion or undue influence [3]. The ethical foundation for managing these closures is rooted in the core principles of research ethics: respect for persons, beneficence, and justice [53]. An abrupt termination, if managed poorly, can violate each of these principles, leading to harm, distrust, and the exploitation of those participants who require the greatest protection.
Vulnerability in research is not a simple binary classification but occurs along a spectrum and can be contextual [3]. Individuals may be vulnerable due to cognitive or communicative limitations, institutional constraints (such as being a prisoner), or deferential relationships (such as in a doctor-patient dynamic) [3]. When a trial involving such participants ends abruptly, these vulnerabilities can be exacerbated. Participants may experience therapeutic misconception, where they confuse research with clinical care, and their sudden discontinuation from an investigational product can lead to physical harm and psychological distress. Furthermore, the failure to properly manage the termination process can unjustly burden these populations, violating the principle of distributive justice. Therefore, a structured, ethical approach to study termination is not merely an administrative task but a moral obligation for researchers, sponsors, and ethics committees.
Vulnerable Populations and Contextual Risks in Trial Discontinuation
Understanding vulnerability is essential for anticipating and mitigating the unique risks that arise during trial termination. The categorical approach to vulnerability identifies specific groups, such as children, pregnant women, prisoners, and the economically disadvantaged, who are automatically afforded additional regulatory protections [3]. However, a more nuanced contextual approach recognizes that any individual's vulnerability is sensitive to their specific situation [3]. A chief executive officer, for instance, is not typically considered vulnerable but may become so when experiencing a medical emergency [3].
For these individuals, an abrupt trial closure presents distinct threats. The National Bioethics Advisory Commission (NBAC) defines vulnerability as a condition that puts individuals at "greater risk of being used in ethically inappropriate ways in research" [3]. This risk materializes during termination in several ways. Participants with cognitive or communicative vulnerabilities may struggle to understand why the trial is ending and what will happen next, leading to anxiety and confusion. Those with institutional or deferential vulnerability may be reluctant to seek clarification or express distress, fearing to disappoint the investigators they perceive as authority figures [3]. The sudden end of a structured trial environment and the relationship with the research team can also remove a crucial source of social and medical support, particularly for socio-economically disadvantaged groups.
Table: Types of Vulnerability and Associated Risks During Trial Termination
| Type of Vulnerability | Description | Risks During Abrupt Termination |
|---|---|---|
| Cognitive/Communicative | Difficulty comprehending information or making decisions about participation [3]. | Inability to understand the reason for termination or post-trial care options; increased anxiety and distress. |
| Institutional | Persons under formal authority of others (e.g., prisoners, military) [3]. | Perceived coercion to remain silent about adverse effects; inability to freely seek post-trial care. |
| Deferential | Persons under informal authority (e.g., due to gender, class, or doctor-patient relationships) [3]. | Unwillingness to ask questions or report termination-related issues for fear of displeasing the investigator. |
| Economic/Educational | Persons who are economically or educationally disadvantaged [3]. | Loss of access to study-related medical care and support; potential financial hardship from ended participation stipends. |
Quantitative Data: Pre-Randomization Predictors of Study Discontinuation
Proactive identification of participants at higher risk of dropping out is a crucial component of ethical trial design and can inform retention strategies that may prevent premature discontinuation. Recent research from the Anti-Amyloid treatment in Asymptomatic AD (A4) Study provides valuable, quantitative insights into the factors that predict study discontinuation. In this large, preclinical Alzheimer's trial, 29% of randomized participants (339 of 1169) discontinued during the blinded period, with a median follow-up time of 759 days [54]. The primary reason for dropout, in 56.3% of cases, was that the participant was "unwilling or unable to continue" [54].
A multivariate analysis revealed specific pre-randomization characteristics that were significantly associated with dropout status. This data allows research teams to identify potentially vulnerable participants early and develop targeted support mechanisms to mitigate attrition risk, thereby protecting both participant welfare and data integrity.
Table: Pre-Randomization Predictors of Study Discontinuation in the A4 Trial [54]
| Predictor Variable | Association with Discontinuation | Odds Ratio (OR) and 95% Confidence Interval | P-value |
|---|---|---|---|
| Screening Anxiety (STAI score) | Positive association; higher anxiety predicted higher dropout. | OR = 1.07 [1.02; 1.12] | 0.002 |
| Age | Positive association; older age predicted higher dropout. | OR = 1.06 [1.03; 1.09] | <0.001 |
| Family History of Dementia | Negative association; protective effect against dropout. | OR = 0.75 [0.55; 1.01] | 0.063 |
| APOE ε4 Carrier Status | Negative association; protective effect against dropout. | OR = 0.79 [0.6; 1.04] | 0.094 |
Methodologies and Protocols for Ethical Termination
A Structured Protocol for Trial Termination
Managing a trial closure ethically requires a pre-defined, systematic protocol that is activated immediately upon the decision to terminate. This protocol must prioritize participant safety, transparency, and continuity of care. The following workflow outlines the critical steps from the termination decision through to final data analysis, highlighting key actions and stakeholder responsibilities.
Communicating with Vulnerable Populations
The communication step is particularly critical and must be adapted to the needs of vulnerable participants. The Institutional Review Board (IRB) must ensure that additional safeguards are in place to protect their rights and welfare [3]. Communication should not be a one-time event but a process. For participants with cognitive vulnerabilities, this may involve using plain-language materials, supplementary educational aids, and involving a trusted surrogate or advocate in the conversation [3]. The process of consent, or in this case "debriefing," may need to be modified, for example through staged consent where information is presented in manageable blocks to facilitate understanding [3]. The essential elements of this critical communication are detailed below.
Table: Essential Elements of Termination Communication for Vulnerable Populations
| Communication Element | Key Considerations | Adaptations for Vulnerability |
|---|---|---|
| Reason for Termination | Provide an honest, clear explanation in lay terms. | Use interpreters, pictograms, or simplified language for cognitive or communicative vulnerability. |
| Immediate Implications for Care | Explain what will happen at the next visit and the discontinuation process for the investigational product. | Use multimedia aids (videos, audio) to reinforce understanding [40]. |
| Post-Trial Care Options | Outline plans for follow-up medical care, referrals to primary care, or transition to standard therapy. | For deferential vulnerability, have an independent patient advocate present to empower questions. |
| Emotional & Psychological Support | Acknowledge potential distress and provide resources for counseling or support. | Proactively schedule follow-up calls to check on participants with high anxiety, a known risk factor for dropout [54]. |
| Access to Final Results | Inform participants how and when they can learn about the study's overall findings. | Commit to providing results in an accessible format, respecting the principle of honesty and reciprocity [53]. |
The Scientist's Toolkit: Research Reagent Solutions for Safety Monitoring
Robust safety monitoring is a cornerstone of participant protection, especially during the unstable period of trial termination. The following toolkit details key methodological components for effectively eliciting and managing adverse event data, which is crucial for ensuring participant safety during the trial closure phase.
Table: Key Methodologies for Eliciting and Managing Participant-Reported Adverse Events
| Tool or Method | Function & Description | Application in Termination Phase |
|---|---|---|
| Open-Ended Elicitation | A general, non-leading question (e.g., "How have you been feeling since your last visit?") to capture overall health changes and bothersome symptoms [55]. | Essential for identifying the most severe or clinically relevant adverse events and unexpected symptoms following treatment discontinuation. |
| Structured Checklist | A comprehensive list of specific potential adverse events (e.g., headache, nausea, dizziness) for the participant to review [55]. | Ensures systematic ascertainment of known or anticipated withdrawal effects; prevents under-detection of less severe but important events. |
| Participant Interview | A structured or semi-structured interview conducted by a clinician to probe deeply into the participant's health status [55]. | Critical for complex cases or vulnerable participants; allows for clarification and a more nuanced understanding of emerging symptoms. |
| Patient-Reported Outcome (PRO) Measures | Validated instruments that directly capture the patient's perspective on their health, function, and quality of life. | Provides quantitative data on the impact of trial termination on participant well-being; useful for longitudinal tracking after transition. |
| Data Safety and Monitoring Board (DSMB) | An independent committee of experts that reviews accumulating trial data, including safety data, at intervals [53]. | Can be tasked with overseeing the termination wind-down phase, reviewing all serious adverse events to ensure participant safety is prioritized. |
Regulatory and Oversight Framework
Ethics Committees (ECs) or Institutional Review Boards (IRBs) are central to the oversight of ethical trial termination. Their role, defined by historical milestones like the Nuremberg Code and the Belmont Report, is to protect the rights and welfare of research subjects [53]. During termination, this role expands from pre-approval review to ongoing monitoring. ECs must ensure that the termination plan submitted by the investigator adequately addresses the six basic principles of ethics: autonomy, justice, beneficence, nonmaleficence, confidentiality, and honesty [53].
The IRB is charged with ensuring that additional safeguards to protect the rights and welfare of subjects who are likely to be vulnerable are included [3]. When reviewing a termination plan, the IRB should consider: 1) Is the communication plan appropriate for the participant population, including those who are vulnerable? 2) Are the plans for safety monitoring and transition to care adequate to minimize harm (nonmaleficence) and act in the participant's benefit (beneficence)? 3) Is the plan for disseminating the trial results, including to participants, fair and honest? [53]. Regulatory bodies like the FDA and EMA also provide guidelines for protecting vulnerable populations during research, which extend to the closure phase, emphasizing the need for valid informed consent and a favorable risk-benefit assessment [40]. The following diagram illustrates the key stakeholders and their interactions in the oversight of an ethical trial termination.
The abrupt closure of a clinical trial presents a complex interplay of ethical, methodological, and interpersonal challenges. These challenges are magnified when the trial includes participants whose vulnerabilities require additional protections. A proactive, participant-centric approach is not merely a regulatory checkbox but a fundamental component of ethical research. The fallout from poor termination management can erode trust in the research institution, exacerbate health disparities, and, most importantly, cause lasting harm to individuals who volunteered for the benefit of science and society.
To mitigate these risks, stakeholders should adopt the following best practices:
- Integrate Termination Planning into Protocol Design: Develop a comprehensive, pre-approved termination and participant transition plan as part of the initial trial protocol, with special consideration for the needs of identified vulnerable populations.
- Prioritize Transparent and Compassionate Communication: Use a multi-modal, accessible communication strategy to ensure all participants, regardless of their vulnerability or health literacy, understand the reasons for termination and the subsequent steps.
- Ensure Continuity of Care: Establish clear pathways for participants to transition back to standard healthcare, providing referrals and support to avoid therapeutic abandonment, particularly for those from socio-economically disadvantaged backgrounds.
- Uphold the Principle of Honesty through Disclosure: Commit to sharing the study results with participants in an understandable format, honoring their contribution and upholding the ethical completion of the research contract.
- Leverage Data for Proactive Retention: Use predictive data, such as baseline anxiety levels and age, to identify participants at higher risk of dropout and implement targeted support strategies early to improve retention and prevent distress [54].
By rigorously applying these practices, the research community can navigate the difficult process of trial termination in a way that respects participant autonomy, minimizes harm, and fulfills the moral contract between science and society.
Optimizing Consent Processes for Participants with Fluctuating or Impaired Capacity
The ethical conduct of research hinges on the principle of respect for persons, which recognizes an individual's autonomy and right to self-determination. For potential research participants with fluctuating or impaired decision-making capacity, this principle necessitates special protections to ensure their rights and welfare are safeguarded [56]. Such individuals may include those with psychiatric, developmental, or organic disorders such as dementia or stroke, conditions that can impair the mental or emotional functions required for providing informed consent [57]. Within the broader thesis on vulnerable populations in research ethics, it is critical to understand that vulnerability is not merely a label applied to groups, but often a condition arising from a compromised capacity for free consent, which can be temporary, situational, or permanent [5] [13]. The overarching goal is not to exclude these individuals from research—as their participation is often vital for developing treatments for their conditions—but to identify vulnerabilities and implement robust, ethical processes that enable their safe and respectful participation [56] [57].
This guide provides a technical roadmap for researchers and drug development professionals to optimize consent processes for this population. It moves beyond regulatory checklists to address the core ethical challenges: assessing capacity accurately, designing a consent process that is truly informative and participatory, and implementing ongoing safeguards that respect the potential for a participant's capacity to change.
Core Concepts: Decisional Capacity and Vulnerability
Defining Decisional Capacity in the Research Context
Decisional capacity to consent to research is the ability of a potential subject to understand, appreciate, reason with, and express a choice regarding the information presented about a clinical study [56]. It is crucial to recognize that capacity is not a global state but is decision-specific; an individual may have the capacity to make simple daily decisions but lack the capacity to comprehend the complexities of a research protocol [56]. Furthermore, capacity is not static; it may fluctuate over time due to the natural progression of a disease, medication effects, or emotional state [56] [57].
A robust assessment of capacity extends beyond mere comprehension or recall of facts. It involves evaluating four key thought domains [56]:
- Understanding: The ability to comprehend the disclosed information regarding the research study's purpose, procedures, risks, and potential benefits.
- Appreciation: The ability to recognize how the research involvement (or lack thereof) applies to and affects one's own personal situation and condition.
- Reasoning: The ability to process information logically by comparing alternatives (participation vs. non-participation) and their consequences.
- Expression of a Choice: The ability to communicate a clear and stable decision.
Conceptualizing Vulnerability
Vulnerability in research refers to a susceptibility to research-related harm or risk due to a compromised ability to protect one's own interests [56]. A systematic review of policy guidelines reveals a tendency to define vulnerability through a "group-based notion" (e.g., children, prisoners, the elderly) [5] [13]. However, a more nuanced "analytical approach" is increasingly favored, focusing on the sources of vulnerability, which can be contextual and temporary [13]. These sources are categorized in the table below.
Table 1: Categories and Examples of Vulnerability in Research
| Category | Description | Examples |
|---|---|---|
| Group Membership [56] [13] | Vulnerability ascribed by membership in a specific population. | Children, prisoners, pregnant women, racial minorities, refugees, institutionalized persons [56]. |
| Situational Vulnerability [56] | Vulnerability provoked by temporary circumstances or the environment. | Severe pain, sedation, being non-English speaking, fear of negative consequences, power differentials (e.g., student of the investigator) [56]. |
| Research-Induced Vulnerability [56] | Vulnerability created by the design or conduct of the research itself. | Poorly designed study, inadequate consent discussion, misrepresentation of risks/benefits, complex language, pressure to consent quickly [56]. |
For individuals with impaired capacity, vulnerability often stems from a consent-based account (lack of capacity for autonomous consent) but can be compounded by justice-based concerns (risk of underrepresentation or unfair exclusion from research) and harm-based accounts (higher probability of incurring harm) [13].
Assessment of Decisional Capacity
Determining When and How to Assess
A foundational rule is that all adults should be presumed competent to consent unless there is evidence of a serious disability that would impair reasoning or judgment [57]. Assessment should be triggered by the study's population and risk level. For example, research on conditions like dementia or schizophrenia inherently warrants a planned assessment strategy.
The method of assessment should be commensurate with the level of risk, complexity, and duration of the research [57]. The following workflow outlines a standardized procedure for integrating capacity assessment into the recruitment process.
Diagram 1: Capacity Assessment and Consent Workflow
Standardized Assessment Tools and Methodologies
For studies greater than minimal risk, or when impairment is suspected, using a validated tool is recommended. The choice of tool depends on the need for a brief screen or a comprehensive evaluation.
Table 2: Standardized Tools for Assessing Capacity to Consent to Research
| Tool Name | Type | Key Domains Assessed | Application & Interpretation |
|---|---|---|---|
| UBACC [56] | Brief Screening Tool | Understanding, Appreciation | 10-item scale. Quickly identifies subjects who require a more in-depth assessment. It is not a definitive measure of incapacity. |
| MacCAT-CR [56] | Structured Interview | Understanding, Appreciation, Reasoning, Expression of Choice | Provides a nuanced profile of strengths and weaknesses across domains. No single cut-off score; interpretation is context-dependent, weighing domains based on study risk. |
Table 3: Essential Toolkit for Consent Capacity Research
| Tool/Resource | Function/Brief Explanation |
|---|---|
| MacCAT-CR Manual & Protocol | Provides the standardized interview script and scoring guidelines tailored to a specific research study. |
| UBACC Questionnaire | Serves as a rapid, reliable screening instrument to flag potential incapacity. |
| Consent Monitor/Participant Advocate | An independent individual who ensures the consent process is conducted thoroughly and without coercion. |
| Enhanced Informational Materials | Storyboards, simplified documents, and videos used to improve comprehension during the consent discussion. |
| Digital Audio Recorder | To document the consent conversation for later verification of process integrity (with appropriate permissions). |
Optimizing the Informed Consent Process
From Document to Process: A Dynamic Interaction
Informed consent must be treated as an ongoing process of communication, not a one-time signature on a document [56]. This is especially critical for populations with impairments. Key strategies include:
- Enhanced Communication: Use plain language, teach-back methods, and visual aids (storyboards, videos) to convey complex information [57].
- Assessing Understanding: Integrate open-ended questions to gauge comprehension. Example questions include [57]:
- "What will happen to you if you agree to take part in this study?"
- "What might be a bad thing about being in this study for you?"
- "What should you do if you want to stop later?"
- Managing Therapeutic Misconception: Clearly and repeatedly emphasize the differences between research and clinical care, and the uncertainty of direct benefit [57].
Protocols for Fluctuating Capacity and Surrogate Decision-Making
For participants with fluctuating or diminishing capacity, a single assessment at enrollment is insufficient. The following workflow details a protocol for ongoing management.
Diagram 2: Managing Fluctuating Capacity During a Study
When a participant is found to lack capacity, the following procedures must be activated:
- Surrogate Consent: A legally authorized representative (LAR) must provide permission for continued participation. Researchers must be aware of state-specific laws governing surrogate consent for research [57].
- Participant Assent: Even when a LAR provides consent, the potential participant's affirmative agreement (assent) must be sought whenever possible. Mere failure to object should not be construed as assent. For research posing more than minimal risk, the participant's objection should be binding, barring specific court authorization [57].
Additional Safeguards and IRB Considerations
Implementing Additional Protective Measures
The University of Nevada, Reno policy outlines several key safeguards that can be adapted for various research contexts [57]:
- Independent Assessment: Utilizing a clinician or professional independent of the research team to evaluate capacity.
- Waiting Periods: Building in a mandatory reflection period between the initial consent discussion and the final decision to participate.
- Participant Advocates: Appointing an individual to support the potential participant's interests and understanding throughout the process.
- Ongoing Monitoring: Implementing data safety and monitoring boards (DSMBs) or similar oversight for higher-risk studies.
Justification and Protocol Development for IRB Submission
Institutional Review Boards (IRBs) require a detailed justification for involving individuals with impaired decision-making capacity. Researchers must provide [57]:
- A scientific rationale for why this population is the only appropriate group for the study.
- A detailed plan for assessing capacity, including the tools and criteria to be used.
- A protocol for obtaining surrogate consent and participant assent.
- A description of procedures to minimize risks.
- A justification that the research meets one of the following criteria:
- Presents no greater than minimal risk.
- Presents greater than minimal risk but offers the prospect of direct benefit to the participant.
- Presents a minor increase over minimal risk without direct benefit but is likely to yield vital knowledge about the participant's condition.
Optimizing consent processes for participants with fluctuating or impaired capacity is a critical and achievable goal in ethical research. It requires a shift from a static, document-centric view of consent to a dynamic, process-oriented, and participant-centered approach. By integrating systematic capacity assessments, utilizing validated tools, designing accessible communication strategies, and implementing robust safeguards for fluctuating capacity and surrogate decision-making, researchers can ensure that this vulnerable population is neither unjustly excluded from the benefits of research nor exposed to undue harm. This commitment to ethical rigor is fundamental to upholding the principle of respect for persons and advancing scientifically valid and inclusive research.
Balancing Scientific Rigor with Participant Well-being in Resource-Limited Settings
Conducting clinical research in resource-limited settings (RLS) is not merely a logistical challenge but a profound ethical undertaking. The globalization of research has made international collaboration a necessity for addressing widespread health issues, from infectious diseases like HIV and malaria to the growing burden of chronic non-communicable diseases (CNCDs) [58]. This expansion of research into RLS brings to the forefront critical tensions between maintaining scientific rigor and ensuring the well-being of vulnerable participants who may have limited access to healthcare and face numerous socioeconomic challenges [58]. The fundamental ethical dilemma rests on conducting research that generates valid, reliable data while simultaneously providing appropriate protection and care for participants whose vulnerability may be exacerbated by poverty, limited education, and underdeveloped healthcare systems [3] [59].
This guide addresses these complex intersections through a framework grounded in both ethical principles and practical implementation strategies. It recognizes that vulnerability in research is not merely a categorical designation but a contextual state that requires nuanced understanding and tailored safeguards [3]. By examining specific ethical challenges, methodological considerations, and practical tools, we provide researchers with a comprehensive approach to conducting ethically sound and scientifically valid research in settings where resources are constrained but scientific need is great.
Understanding Vulnerability in Research Ethics
Conceptualizing Vulnerability: Beyond Categorical Approaches
Vulnerability in human subjects research is a cornerstone concept that necessitates additional protections for participants. Traditional approaches have often relied on categorical classifications, identifying specific groups as vulnerable populations, including children, prisoners, pregnant women, fetuses, mentally disabled persons, and economically or educationally disadvantaged individuals [3]. While this approach has regulatory utility, it presents significant limitations as it fails to account for persons with multiple vulnerabilities, variations in degree of vulnerability within groups, and the fundamental reality that vulnerability is often situation-dependent rather than inherent [3].
A more sophisticated contextual approach allows for a nuanced understanding of vulnerability as occurring along a spectrum of seriousness and as a consequence of specific situations and environments [3]. This perspective recognizes that even typically autonomous individuals can become vulnerable in certain contexts, such as a corporate executive experiencing chest pain in an emergency department [3]. The National Bioethics Advisory Commission (NBAC) defines vulnerability as "a condition, either intrinsic or situational, of some individuals that puts them at greater risk of being used in ethically inappropriate ways in research" [3].
A Framework of Vulnerability Categories
The IRB-SBS identifies eight distinct categories of vulnerability that provide a comprehensive framework for assessing participant risk in research settings [59]:
Table: Categories of Vulnerability in Research Participants
| Vulnerability Category | Description | Examples | Potential Safeguards |
|---|---|---|---|
| Cognitive/Communicative | Inability to process, understand, or reason through consent information | Mental limitations, language barriers, illiteracy | Translated documents, plain language, capacity assessment, surrogate consent |
| Institutional | Subject to formal authority structures that may coerce participation | Prisoners, military personnel, employee/employer relationships | Third-party consent procedures, insulation from hierarchical pressure |
| Deferential | Informal subordination to authority figures | Doctor/patient relationships, abuse victims, spousal dynamics | Sensitive recruitment plans, voluntary consent opportunities |
| Medical | Medical conditions that cloud decision-making capacity | Serious illness where research may be misconstrued as treatment | Clear separation of research from treatment, careful presentation |
| Economic | Economic circumstances that unduly influence participation | Poverty, payment amounts that encourage risk-taking | Appropriate payment levels, avoidance of undue inducement |
| Social | Risk of discrimination based on personal characteristics | Race, gender, ethnicity, age-based discrimination | Non-discriminatory practices, cultural sensitivity |
| Legal | Lack of legal consent capacity or fear of legal repercussions | Minors, undocumented immigrants, illegal behaviors | Legal representative consent, certificates of confidentiality |
| Study Vulnerability | Vulnerability created by the research design itself | Deception studies, incomplete disclosure | Full debriefing, post-study disclosure |
This framework helps researchers identify potential vulnerabilities specific to their study population and implement appropriate, targeted safeguards rather than relying on one-size-fits-all protections [59].
Ethical Challenges in Resource-Limited Settings
Systemic and Infrastructural Barriers
Research in RLS confronts significant systemic challenges that impact both scientific rigor and ethical conduct. The single most important challenge is the lack of a skilled workforce to support both healthcare delivery and clinical research [58]. This shortage is exacerbated by the "brain drain" of qualified academic staff and healthcare professionals migrating from resource-poor countries to more advanced industrialized nations [58]. The disparity in healthcare spending creates dramatic differences in research infrastructure—whereas developed countries may spend thousands per capita on health, some sub-Saharan African countries spend as little as $20 per person annually [58].
Additional infrastructural challenges include deficient research facilities, inefficient healthcare systems to support clinical research, poor data management capabilities, inadequately structured institutional ethics boards, and poor regulatory oversight [58]. Epileptic power supply in many regions further complicates the maintenance of research equipment and integrity of samples [58]. These limitations directly impact the researcher's ability to maintain scientific rigor while simultaneously creating environments where participants may be more vulnerable to exploitation or harm.
Clinician-Researcher Dual Role Dilemmas
A particularly complex ethical challenge arises when healthcare providers assume dual roles as researchers in RLS. This dual positioning can generate significant ethical tensions around consent, therapeutic boundaries, and emotional involvement, particularly when clinical needs arise during data collection [36]. The clinician-researcher may face conflicts between professional obligations to intervene and the methodological imperative to maintain research neutrality [36].
Reflective research involving men with advanced prostate cancer and their caregivers in Ghana demonstrated several key ethical challenges, including substantial emotional labor, professional role conflicts, and difficulty managing therapeutic boundaries [36]. The clinician-researcher dual role significantly shaped participant consent, data collection, and interpretation of findings, highlighting the vulnerability of both participants and researchers in emotionally charged, culturally sensitive contexts [36]. Ethical tensions often emerged between maintaining professional objectivity and addressing immediate care needs, especially when encountering clinically concerning situations like unsafe wound-dressing practices in home settings [36].
Informed Consent in Culturally Diverse Contexts
The capacity of participants to give truly informed consent often presents significant challenges in RLS [58]. Modern medical terms frequently lack exact translations in local languages, and understanding of disease causes and pathology varies considerably with cultural context and educational background [58]. Additionally, potential participants in clinical trials may otherwise have no access to treatment, creating vulnerability and raising ethical concerns about future access to trial medications after study completion [58].
Cultural factors such as social taboos surrounding death, disease-related stigma, and collective decision-making processes can profoundly influence both the conduct of data collection and participants' willingness to share information openly [36]. Dyad interviews in sensitive research contexts reveal the influence of collective meaning-making and necessitate sensitivity to culturally embedded reticence, particularly regarding topics like death and illness disclosure [36].
Methodological Framework and Protocols
Ethical Preparedness and Reflexivity Framework
A structured approach to ethical preparedness is essential for navigating the complex terrain of research in RLS. The following workflow outlines key components for maintaining both ethical integrity and scientific rigor:
Diagram: Ethical Framework for Research in RLS
This framework emphasizes the cyclical nature of ethical practice, where reflection and adaptation occur throughout the research process rather than merely as a pre-study consideration.
Structured Reflexive Protocol for Researcher Preparation
Engaging in structured reflexivity is particularly critical when researching vulnerable populations in RLS. The following protocol provides a methodological approach to maintaining ethical awareness:
Objective: To enhance researcher self-awareness, identify potential ethical dilemmas before they arise, and process emotional labor encountered during fieldwork.
Materials: Reflective journal (digital or physical), audio recorder (optional), peer debriefing partner or group.
Procedure:
- Pre-fieldwork reflection: Before commencing research, document expectations, biases, and concerns regarding the research context and relationships.
- Daily reflective practice: Following each research interaction, record detailed notes capturing:
- Emotional reactions to participant encounters
- Ethical uncertainties or dilemmas encountered
- Internal deliberations about navigating clinical concerns
- Non-verbal cues and contextual observations
- Structured memoing: Weekly, synthesize reflections into analytical memos addressing:
- Patterns in dual-role tensions
- Cultural or contextual factors influencing consent
- Power dynamics in researcher-participant relationships
- Peer debriefing: Regularly discuss reflections with research team or peers to externalize ethical analysis and mitigate over-identification with participants [36].
Outcome Assessment: The reflective process should generate tangible modifications to research practice, such as adjusted consent procedures, additional safeguards, or protocol modifications responsive to emergent ethical concerns.
Participant Vulnerability Assessment Protocol
A systematic approach to assessing and addressing participant vulnerability helps ensure appropriate safeguards are implemented:
Objective: To identify situational and categorical vulnerabilities within the research population and implement targeted protections.
Materials: Vulnerability assessment checklist, cultural liaison (if applicable), appropriate consent documents.
Procedure:
- Contextual assessment: Evaluate the research environment for factors that may create or exacerbate vulnerability, including:
- Healthcare access limitations
- Economic constraints within population
- Literacy levels and language barriers
- Cultural norms regarding authority and consent
- Individual screening: During recruitment, assess for presence of multiple vulnerability categories using the framework in Section 2.2.
- Safeguard implementation: Based on assessment findings, implement appropriate protections such as:
- Enhanced consent procedures (staged consent, plain language documents)
- Involvement of cultural liaisons or translators
- Independent consent monitors for power differential concerns
- Assessment of decision-making capacity when indicated
- Ongoing evaluation: Continuously monitor for emergent vulnerabilities throughout research participation.
Documentation: Maintain detailed records of vulnerability assessments and corresponding safeguard implementations for IRB review and study replication.
Data Analysis and Visualization in Resource-Constrained Environments
Quantitative Data Comparison Methods
Appropriate data analysis and visualization techniques are essential for maintaining scientific rigor while working within resource constraints. The selection of appropriate comparison methods depends on the nature of the variables being examined and the specific research question.
Table: Quantitative Data Comparison Methods for Research in RLS
| Comparison Scenario | Appropriate Graph Types | Statistical Summary | Use Case Example |
|---|---|---|---|
| Single quantitative variable across 2 groups | Back-to-back stemplot, 2-D dot chart, boxplot | Difference between means/medians, standard deviation, IQR | Comparing chest-beating rates between younger and older gorillas [60] |
| Single quantitative variable across >2 groups | 2-D dot charts, parallel boxplots | Differences between group means/medians with reference level | Comparing push-out forces across three dental cement types [60] |
| Distribution of quantitative variable within groups | Histograms, boxplots | Five-number summary (min, Q1, median, Q3, max), frequency | Showing frequency of numerical data within specific intervals [61] |
| Trends over time | Line charts, overlapping area charts | Mean values at time points, trend lines | Monthly revenue of a company over a year [61] |
| Part-to-whole comparisons with limited categories | Pie charts, doughnut charts | Percentages, proportions | Operating system market share [61] |
When comparing quantitative variables in different groups, the data should be summarized for each group separately, then differences between groups should be calculated [60]. For two groups, the difference between the means and/or medians should be computed; for more than two groups, differences between one group (reference level) and the others are typically calculated [60].
Visual Protocol Development for Standardization
Graphic protocols provide a valuable method for standardizing procedures and reducing errors in resource-limited settings where training may be variable and supervision limited [62]. Clearly documented, step-by-step graphic protocols help ensure all research team members use consistent methods, thereby enhancing methodological rigor [62].
Development Process:
- Protocol breakdown: Deconstruct each research procedure into discrete, sequential steps
- Visual representation: Create standardized visual representations for each step using consistent iconography
- Integration: Combine visual elements with concise textual instructions
- Validation: Test protocol clarity with diverse team members
- Version control: Maintain detailed version history to track modifications and ensure reproducibility [62]
Implementation Benefits:
- Reduced procedural errors at the bench
- Streamlined onboarding of new research staff
- Enhanced consistency across multiple research sites
- Facilitated knowledge transfer regardless of language barriers [62]
Essential Research Reagent Solutions
Conducting rigorous research in resource-limited settings often requires creative solutions to reagent and material constraints. The following toolkit highlights essential categories with specific considerations for RLS contexts:
Table: Research Reagent Solutions for Resource-Limited Settings
| Reagent Category | Specific Considerations for RLS | Alternative Approaches | Ethical Dimensions |
|---|---|---|---|
| Point-of-Care Diagnostics | Temperature stability, minimal equipment requirements, visual readouts | CRISPR-based detection (e.g., for melioidosis), lateral flow assays | Rapid diagnosis enables appropriate participant care in remote settings |
| Sample Preservation | Electricity-independent storage, transport stability | Chemical preservatives, dried blood spots, ambient temperature storage | Maintains sample integrity despite infrastructural limitations |
| Cultural-appropriate Consent Materials | Visual aids, plain language, local language translation | Pictorial consent forms, witnessed oral consent, community leader involvement | Enhances genuine comprehension and voluntary participation |
| Data Collection Tools | Offline capability, low literacy interfaces, power-efficient devices | Mobile data collection with synchronization, paper forms with digital backup | Protects participant data while accommodating technical constraints |
| Essential Laboratory Reagents | Extended shelf life, minimal refrigeration, local production | Lyophilized reagents, centralized testing hubs, regional supply chains | Ensures research continuity despite supply chain vulnerabilities |
Balancing scientific rigor with participant well-being in resource-limited settings requires both philosophical commitment and practical methodologies. The approach must be rooted in a nuanced understanding of vulnerability as contextual rather than merely categorical, recognizing that ethical practice demands continuous reflexivity and adaptation to specific circumstances [3]. By implementing structured ethical frameworks, maintaining rigorous reflective practices, and employing appropriate methodological adaptations, researchers can generate scientifically valid knowledge while fully honoring their ethical obligations to vulnerable participants.
The dual role of clinician-researcher in these settings presents particular challenges that must be navigated through clear boundary protocols, structured reflexive journaling, and regular peer debriefing [36]. These practices help maintain ethical integrity when research and clinical responsibilities intersect, especially in emotionally charged contexts involving serious illness or limited healthcare access.
Ultimately, ethical research in resource-limited settings is not achieved through rigid application of rules, but through cultivated sensitivity to context, power dynamics, and cultural factors that influence participant vulnerability. By embracing both methodological rigor and ethical mindfulness, researchers can contribute to reducing global health disparities while respecting the dignity and rights of all research participants.
Ethics in a Changing World: Validating Approaches Against Modern Realities
The globalization of clinical trials to Low- and Middle-Income Countries (LMICs) represents a significant shift in biomedical research, offering both tremendous opportunities and substantial ethical challenges. This whitepaper examines the complex landscape of international research within the context of vulnerable populations, addressing the fine-tuned balance required between scientific advancement and protection against exploitation. While global trials can accelerate drug development and build healthcare capacity in LMICs, they also raise critical concerns regarding informed consent, standard of care, and fair benefit distribution. This analysis provides researchers, scientists, and drug development professionals with ethical frameworks and practical methodologies to ensure trials conducted in LMICs adhere to the highest ethical standards, protect vulnerable participants, and promote equitable collaboration between high-income countries and LMIC partners.
Clinical research has followed the broader trend of globalization, with a significant migration of trial sites from traditional locations in North America and Europe to LMICs in Asia, Latin America, and Africa [63]. Table 1 illustrates the growth patterns across different regions. This transition is driven by multiple factors including lower operational costs, faster patient recruitment, and large pools of treatment-naïve patients in LMICs [63]. From 2005-2012, the largest average annual growth in clinical trials occurred in Asian (30%) and Latin American/Caribbean (12%) regions, substantially exceeding the world average growth rate of 8% [64].
Table 1: Global Growth Patterns of Clinical Trials (2005-2012)
| Geographic Region | Average Annual Growth Rate | Key Contributing Countries |
|---|---|---|
| Asian Regions | 30% | Iran, China, South Korea, Japan, India |
| Latin American/Caribbean | 12% | Brazil |
| Lower-Middle Income Regions | 33% | Iran, China, Egypt |
| Low-Income Regions | 21% | - |
Beyond economic motivations, legitimate scientific reasons exist for conducting trials in LMICs, particularly for diseases that predominantly affect these populations, such as malaria and tuberculosis [63]. However, this geographic shift raises fundamental ethical questions about whether economically disadvantaged populations are being exploited for the benefit of patients in wealthy nations [63]. The central challenge lies in ensuring that the interests of vulnerable populations in LMICs are protected while simultaneously advancing medical knowledge and improving global health outcomes.
Ethical Frameworks and Vulnerability Concepts
Theoretical Foundations of Vulnerability
The concept of vulnerability serves as a cornerstone for protecting research participants in global trials. Vulnerability in research contexts has been defined as "a condition, either intrinsic or situational, of some individuals that puts them at greater risk of being used in ethically inappropriate ways in research" [3]. This encompasses both difficulties in providing voluntary informed consent and increased risk of exploitation [3].
The Belmont Report established the principle that "persons with diminished autonomy are entitled to protection," forming the basis for special safeguards for vulnerable populations [3]. International guidelines like the Declaration of Helsinki further characterize vulnerable groups as those who "may have an increased likelihood of being wronged or of incurring additional harm" [3]. The Council for International Organizations of Medical Sciences (CIOMS) notes that vulnerable persons are "relatively (or absolutely) incapable of protecting their own interests" due to personal characteristics or life circumstances [3].
Approaches to Understanding Vulnerability
Two distinct approaches help conceptualize vulnerability in research settings:
Categorical Approach: This method identifies specific groups as vulnerable, including children, prisoners, pregnant women, fetuses, mentally disabled persons, and economically or educationally disadvantaged persons [3]. While this approach provides clear regulatory categories, it has limitations in addressing individuals with multiple vulnerabilities and variations in vulnerability degree within groups.
Contextual Approach: This framework recognizes that vulnerability is sensitive to context, with individuals potentially vulnerable in one situation but not another [3]. This nuanced understanding allows for more targeted safeguards. Key vulnerability categories in this approach include:
- Cognitive or Communicative Vulnerability: Difficulty comprehending information or making decisions about participation [3]
- Institutional Vulnerability: Being under formal authority of others (e.g., prisoners, military personnel) [3]
- Deferential Vulnerability: Being under informal authority based on gender, race, class, or professional inequalities [3]
The following diagram illustrates the relationship between these vulnerability concepts and their implications for research ethics:
Historical Context and Regulatory Evolution
Historical Cases Shaping Research Ethics
Several historical cases have fundamentally shaped modern research ethics and regulations:
The Tuskegee Syphilis Study (1932-1972): U.S. physicians denied penicillin treatment to African American men with syphilis to study the disease's natural progression, despite the availability of effective treatment [12]. This study led to the passage of the National Research Act in 1974 and the creation of the Belmont Report, which established respect for persons, beneficence, and justice as fundamental ethical principles [63] [12].
Nazi Medical Experiments: Non-consensual and often fatal experiments on concentration camp prisoners during World War II resulted in the Nuremberg Code (1947), establishing voluntary consent as essential for ethical research [12].
Willowbrook Hepatitis Study (1956-1970): Researchers intentionally infected children with intellectual disabilities with hepatitis, raising serious ethical concerns about coercion and vulnerability [12].
Key Regulatory Frameworks and Guidelines
Multiple international guidelines provide ethical direction for global clinical research:
Declaration of Helsinki (DoH): First adopted in 1964 by the World Medical Association and regularly updated, this document sets forth ethical principles for medical research involving human subjects [63]. The 2000 revision significantly limited placebo use in response to HIV studies in developing countries that denied effective medication to placebo control groups [63].
ICH-GCP Guidelines: Created by regulatory authorities from Europe, Japan, and the United States in collaboration with the pharmaceutical industry, these guidelines differ from the DoH, particularly regarding placebo use and post-trial access [63].
CIOMS International Guidelines: Provide specific guidance for biomedical research involving human subjects in international contexts [63].
Table 2: Key Regulatory Frameworks for Global Clinical Trials
| Guideline/Framework | Year Established | Key Ethical Contributions | Limitations in Global Context |
|---|---|---|---|
| Nuremberg Code | 1947 | Established voluntary consent as essential | Limited applicability to vulnerable populations |
| Declaration of Helsinki | 1964 (with 7 revisions) | International ethical principles for physicians; limited placebo use | FDA abandoned reference to it in 2008 |
| Belmont Report | 1979 | Principles of respect for persons, beneficence, justice | U.S.-centric framework |
| ICH-GCP | 1996 | Standardized clinical practice across regions | More permissive on placebos than DoH |
Current Ethical Challenges in Global Trials
Informed Consent and Cultural Context
Informed consent presents particular challenges in global trials due to cultural differences in understanding autonomy and decision-making. The Western concept of individual autonomy "does not always translate well to other countries" where Eastern philosophies may prioritize community or family decision-making [63]. This creates tension between universal ethical standards and culturally specific applications.
Community-based participatory research (CBPR) has emerged as an approach to address these challenges by involving local communities in setting research agendas, designing protocols, and determining appropriate consent processes [63]. However, as Sandra Alfano, Chair of Yale's Institutional Review Board, notes, "CBPR is really the focus on everyone's mind, but it is very difficult to achieve" [63].
Standard of Care and Placebo Controls
The use of placebo controls in LMICs when effective treatment exists in HICs represents one of the most contentious ethical issues. This practice was prominently challenged during HIV trials in the 1990s, where studies on mother-to-child transmission of HIV in developing countries denied effective medication to participants in placebo control arms [63]. This controversy led to significant revisions in the Declaration of Helsinki, which now greatly limits placebo use [63].
The standard of care debate highlights the tension between scientific validity and ethical obligations to research participants. ICH-GCP regulations are more permissive than the Declaration of Helsinki, stating that "the standard of care required to be provided to the control group depends on the population," meaning control group subjects are only entitled to the standard of care they would otherwise receive in their local context [63].
Post-Trial Benefits and Fairness
A critical ethical concern in global trials is ensuring that host populations benefit from research outcomes. The "10/90 gap" illustrates this disparity: less than 10% of global research resources address health problems affecting 90% of the world's population [65]. This represents a massive imbalance in research priorities, with only about 5% of the world's research expenditures occurring in LMICs where approximately 93% of preventable mortality occurs [65].
Ethical frameworks emphasize that "the primary goal of conducting clinical trials in developing countries should be to address the health needs of the host population" [63]. This includes ensuring successful interventions become available to the host community after trial completion and building sustainable research and healthcare capacity.
Methodological Considerations and Safeguards
Vulnerability Assessment Protocol
Implementing systematic vulnerability assessments is essential for ethical trial conduct. The following workflow outlines a comprehensive approach:
Institutional Review Boards (IRBs) can use a two-question framework when reviewing protocols involving potentially vulnerable populations: (1) is inclusion necessary? and (2) if so, are safeguards adequate? [3]. This ensures careful justification for involving vulnerable groups and implementation of appropriate protections.
Ethical Toolbox for Researchers
Table 3: Essential Methodologies for Ethical Global Trials
| Methodology Category | Specific Tools & Approaches | Application Context | Key Considerations |
|---|---|---|---|
| Informed Consent Enhancements | Staged consent, plain-language forms, supplementary education, interpreters, community leaders involvement | All research contexts, particularly with low literacy or different language speakers | Balance universal standards with cultural appropriateness; avoid mechanistic approaches |
| Capacity Building | Local investigator training, research ethics education, infrastructure development | Long-term partnerships with LMIC institutions | Sustainable programs beyond single trials; equitable collaboration |
| Community Engagement | Community Advisory Boards (CABs), community-based participatory research (CBPR) | All research in unfamiliar cultural contexts | Genuine partnership rather than tokenism; early involvement in research design |
| Vulnerability Protections | Independent advocates, capacity assessment tools, delayed enrollment for transient vulnerability | Research involving potentially vulnerable populations | Avoid over-protectionism that excludes groups from research benefits |
Regulatory Harmonization and Oversight
Strengthening regulatory capacity in LMICs is essential for sustainable ethical oversight. This includes developing robust national ethics committees, building inspectorate capabilities for Good Clinical Practice monitoring, and creating context-appropriate regulatory frameworks [64]. The Pan American Health Organization and World Health Organization have developed regional harmonization initiatives, such as the "Good Clinical Practices: Document of the Americas" to strengthen ethical oversight across regions [64].
Case Studies and Applications
HIV Trials in Mother-to-Child Transmission
The HIV trials in developing countries during the 1990s represent a pivotal case study in research ethics. These studies investigated regimens to prevent mother-to-child HIV transmission using placebo controls, despite the existence of proven effective treatment in high-income countries [63]. This raised fundamental questions about whether different ethical standards should apply in resource-poor settings and sparked international debate that led to significant revisions of the Declaration of Helsinki in 2000 [63].
COVID-19 Vaccine Trials
The rapid globalization of COVID-19 vaccine trials demonstrated both advances and persistent challenges in ethical research conduct. While these trials generally complied with regulatory expectations, critiques emerged regarding representativeness of trial populations and informed consent processes in high-stakes, rapidly evolving situations [12]. The pandemic context highlighted the delicate balance between urgent public health needs and maintaining rigorous ethical standards.
The globalization of clinical trials presents both unprecedented opportunities and profound ethical challenges. When conducted ethically, research in LMICs can address pressing health needs, build local capacity, and contribute to reducing global health disparities. However, without careful attention to vulnerability, consent, and fairness, such research risks exploiting those most in need of protection.
Future efforts must focus on developing more nuanced approaches to vulnerability that recognize its contextual and spectrum-based nature rather than treating it as a binary classification [3]. Genuine community engagement and capacity building should become standard practice rather than aspirational goals. Furthermore, ethical frameworks must continue to evolve to address emerging challenges including digital health technologies, genomic research, and increasing complexity in global research partnerships.
By embedding ethical principles into every aspect of clinical research—from design to implementation—researchers, sponsors, and regulators can ensure that scientific advancement proceeds with appropriate respect for human dignity and promotes equitable health benefits for all populations, regardless of economic circumstance or geographic location.
The integration of artificial intelligence (AI), genomics, and digital health tools into research and clinical practice represents a paradigm shift in biomedical science. While these technologies promise unprecedented advances in personalized medicine and healthcare delivery, they introduce complex ethical challenges, particularly for vulnerable populations. Vulnerable populations—including individuals with severe mental illness, older adults in care settings, and those affected by disasters or conflicts—face disproportionate risks from these technologies, ranging from compromised consent processes to algorithmic bias and privacy violations. The ethical imperative is clear: to harness the benefits of emerging technologies while implementing robust safeguards that protect those most susceptible to harm. This technical guide examines the critical ethical considerations and proposes structured frameworks for the ethical integration of these technologies in research involving vulnerable groups.
Ethical Challenges of AI in Healthcare
Synthetic Data and Research Integrity
The use of synthetic data generated by AI presents both opportunities and significant ethical risks for research integrity. Synthetic data, which mimics real-world data without originating from actual measurements, offers valuable applications for modeling phenomena and creating digital twins while protecting privacy [66]. However, bioethicists have raised concerns about its potential to corrupt the scientific record through both accidental misuse, where synthetic data is mistaken for real data, and deliberate misconduct, where fabricated data is passed as genuine [66]. The potential for generative AI to create highly realistic fake data has been characterized as a "ticking time bomb" that could undermine trust in science, particularly when such data infiltrates research involving vulnerable populations who may be less able to identify or challenge such inaccuracies [66].
Algorithmic Bias and Fairness
AI and machine learning systems in healthcare are susceptible to multiple forms of bias that can perpetuate and exacerbate health disparities among vulnerable populations. These biases can be categorized into three primary types:
- Data Bias: Arises from unrepresentative training data, missing data, or historical inequalities embedded in datasets
- Development Bias: Occurs during feature selection, model engineering, and algorithm design
- Interaction Bias: Emerges from deployment contexts, clinical practice variations, and temporal changes in technology or disease patterns [38]
The deployment of biased AI systems in healthcare settings raises critical ethical concerns regarding justice and fairness, as these systems may produce unfair or detrimental outcomes for populations already experiencing health disparities [38]. This is particularly problematic for vulnerable groups who may have less access to alternative care options or resources to challenge algorithmic decisions.
Public Perception and Trust
Understanding public perspectives on AI in healthcare is crucial for developing ethically sound implementations. A 2023 nationwide survey in South Korea (n=1,002) revealed that while 84.5% of respondents expressed optimism about AI's positive impacts in healthcare over the next five years, significant concerns persisted regarding data privacy (54.0%), potential AI errors causing harm (52.0%), and ambiguous legal responsibilities (42.2%) [67]. Willingness to share data varied by type, with genetic data being the least preferred (64.1%) compared to electronic medical records (72.8%) and lifestyle data (72.3%) [67]. These findings highlight the nuanced public acceptance of AI in healthcare and the particular sensitivity around genetic information.
Table 1: Public Willingness to Share Health Data for AI Applications
| Data Type | Willingness to Share | Key Concerns |
|---|---|---|
| Electronic Medical Records | 72.8% | Privacy violations, security breaches |
| Lifestyle Data | 72.3% | Potential misuse, commercial exploitation |
| Biometric Data | 71.3% | Unauthorized access, identification risks |
| Genetic Data | 64.1% | Discrimination, familial implications, re-identification |
Genomic Research and Digital Health Tools: Specific Vulnerabilities
Consent Challenges in Genomic Research
Obtaining meaningful informed consent represents a fundamental ethical challenge in genomic research involving vulnerable populations. Traditional consent practices often fail to address the unique implications of genomic data, including its permanence, familial implications, and potential for future re-identification [68]. These challenges are compounded when working with vulnerable groups who may have diminished decision-making capacity or face barriers to comprehension.
Research involving individuals with severely treatment-resistant psychotic symptoms (TRS) highlights these complexities. Historical practices of blanket exclusion from research have been challenged by evidence demonstrating that cognitive impairment, rather than severity of psychopathology, poses the greatest threat to decisional capacity [69]. Empirical studies using validated assessment tools like the MacArthur Competence Assessment Tool-Clinical Research (MacCAT-CR) have shown that some individuals with chronic and severe psychotic illness retain adequate decisional capacity for informed consent, particularly when support and remediation are provided [69].
Digital Health Tools in Crisis Settings
Digital health interventions, including telemedicine, mobile health platforms, and remote monitoring technologies, are increasingly deployed in natural disaster and conflict settings to support vulnerable populations. A 2025 scoping review identified eight studies examining such implementations, revealing both opportunities and significant ethical challenges [70]. These technologies can enhance healthcare access and continuity during crises but frequently fail to adequately include persons with disabilities in their design and implementation [70].
Common barriers to effective digital health implementation in these settings include infrastructure damage, digital literacy gaps, and weak governance structures, while key enablers include public-private partnerships, trained staff, and scalable technologies [70]. Most interventions were characterized as reactive, with limited evidence of long-term integration or inclusive design, raising ethical concerns about the sustainability and equity of such approaches [70].
Digital Health Twins and Older Adults
Digital health twins (DHTs)—sophisticated virtual representations that simulate individual health profiles—present novel ethical considerations, particularly for older adults in care settings. A 2025 scoping review on DHTs identified five key ethical challenges: (1) data security and privacy concerns; (2) equity and accessibility of healthcare; (3) effectiveness variations across contexts; (4) implications for autonomy, consent, and overdiagnosis; and (5) impacts on healthcare workflows and provider workload [71].
The continuous and urgent influx of personal health information required for DHTs, combined with their complex interconnected nature, creates heightened privacy and security risks compared to other digital health technologies [71]. These risks are particularly acute for older adults, who may be more susceptible to data breaches and less familiar with digital technologies [71].
Methodological Frameworks and Experimental Approaches
Ethical Framework Development for Digital Health Consent
Recent research has developed comprehensive frameworks to address ethical gaps in digital health consent processes. A 2025 study created and validated a consent framework through analysis of 25 real-world informed consent forms from digital health studies [32]. The methodology involved:
- Thematic Analysis: Six-step process to extract and categorize consent elements from NIH guidance documents
- Framework Development: Identification of 63 attributes and 93 subattributes across four domains (Consent, Grantee Permissions, Grantee Obligations, and Technology)
- Iterative Testing: Multiple rounds of review and refinement using actual consent forms until thematic saturation was achieved [32]
The results demonstrated significant gaps in current practices, with the highest completeness for required attributes reaching only 73.5% across the reviewed consent forms [32]. The study also identified four ethically salient consent elements not present in current national guidance: commercial profit sharing, study information disclosure, during-study result sharing, and data removal requests [32].
Digital Health Consent Framework Development Workflow: This diagram illustrates the systematic process for developing and validating an ethical consent framework for digital health research, from initial guidance analysis to final framework implementation.
Capacity Assessment in Psychiatric Research
Research on decision-making capacity in individuals with severely treatment-resistant psychotic symptoms has yielded important methodological insights. The Pennsylvania State Hospital (PASH) study implemented a comprehensive protocol for assessing and supporting capacity in this vulnerable population over a four-year period [69]. Key methodological components included:
- Structured Assessment: Use of validated tools including the MacArthur Competence Assessment Tool-Clinical Research (MacCAT-CR) and the 10-item Brief Assessment of Capacity to Consent
- Individualized Evaluation: Movement beyond categorical exclusion to personalized capacity assessments
- Capacity Remediation: Implementation of strategies to enhance understanding and decision-making abilities
- Ongoing Monitoring: Continuous evaluation of capacity throughout research participation [69]
This approach demonstrated that with appropriate safeguards, carefully selected involuntarily committed individuals can ethically participate in research regarding the mental illnesses that profoundly shape their lives [69].
Table 2: Key Assessment Tools for Decision-Making Capacity in Research
| Assessment Tool | Primary Application | Key Domains Measured | Administration Time |
|---|---|---|---|
| MacArthur Competence Assessment Tool-Clinical Research (MacCAT-CR) | Psychiatric research | Understanding, appreciation, reasoning, expression of choice | 15-20 minutes |
| Brief Assessment of Capacity to Consent (BACC) | Rapid screening in diverse populations | Understanding of key research concepts | 5-10 minutes |
| Evaluation to Sign Consent (ESC) | Clinical trials with impaired populations | Understanding of study procedures and risks | 10-15 minutes |
Implementation Framework for Digital Health in Crisis Settings
A systematic methodology for implementing digital health technologies in disaster and conflict settings was developed through a scoping review following the Arksey and O'Malley framework and PRISMA-ScR guidelines [70]. The research process included:
- Comprehensive Search Strategy: Multi-database search (PubMed, EBSCOhost, Cochrane Library) combined with gray literature review from WHO, UNDRR, UNICEF, and NGO sources
- Systematic Screening: Two-stage title/abstract and full-text review process with predefined inclusion/exclusion criteria
- Data Charting: Structured extraction capturing study characteristics, population details, intervention types, outcomes, and contextual factors
- Thematic Analysis: Identification of patterns across studies regarding implementation barriers, enablers, and equity considerations [70]
This methodology provided insights into how digital health interventions can support Sustainable Development Goals 3 (good health and well-being), 10 (reduced inequalities), 11 (sustainable cities and communities), and 13 (climate action) in crisis-affected populations [70].
Research Reagent Solutions: Ethical Tools and Frameworks
Table 3: Essential Research Reagents for Ethical Implementation of Emerging Technologies
| Reagent/Framework | Primary Function | Application Context | Key Features |
|---|---|---|---|
| MacArthur Competence Assessment Tool-Clinical Research (MacCAT-CR) | Assess decision-making capacity | Research with cognitively impaired populations | Validated semi-structured interview measuring understanding, appreciation, reasoning, and choice |
| Digital Health Consent Framework | Comprehensive consent for technology studies | Digital health research involving vulnerable groups | 63 attributes across consent, permissions, obligations, and technology domains |
| Ethical, Legal and Social Implications (ELSI) Framework | Identify and address broader implications | Genomic and AI research | Programmatic assessment of ethical, legal, and social consequences of research |
| WHO AI Ethics Guidelines | Governance of AI applications | Healthcare AI implementation | Over 40 recommendations for ethical AI use across government, industry, and healthcare |
| Dynamic Consent Platforms | Ongoing consent management | Longitudinal genomic studies | Digital platforms enabling continuous participant engagement and consent updates |
Mitigation Strategies and Ethical Safeguards
Technical and Governance Approaches
Addressing the ethical challenges of emerging technologies requires multi-layered strategies spanning technical solutions, governance frameworks, and educational initiatives. For AI systems, these include:
- Technical Safeguards: Watermarking of synthetic data to prevent accidental misuse [66], advanced encryption methods for genetic data protection [68], and bias detection algorithms to identify discriminatory patterns in AI models [38]
- Governance Structures: Development of specialized oversight committees for research involving vulnerable populations, implementation of data transparency protocols, and establishment of clear accountability mechanisms for AI system outcomes [71]
- Regulatory Compliance: Proactive engagement with evolving regulatory landscapes, including international standards for genetic data protection and AI governance [68]
Capacity Building and Community Engagement
Ethical implementation of emerging technologies in research with vulnerable populations requires investment in capacity building and meaningful community engagement. Key strategies include:
- Targeted Education: Prioritizing ethics training for developers (70.7%), medical institution managers (68.2%), and researchers (65.6%), as identified in public surveys [67]
- Community Partnership: Building research teams that include relevant communities affected by and interested in the proposed research [72]
- Workforce Development: Creating opportunities for early career scholars, research team members, and project staff from underrepresented institutions [72]
Multi-Layer Ethical Safeguard System: This diagram illustrates the continuous process of identifying ethical risks and implementing overlapping safeguards throughout the research lifecycle, incorporating technical, governance, and educational components.
The ethical integration of AI, genomics, and digital health tools in research with vulnerable populations requires thoughtful implementation of specialized frameworks, assessment tools, and mitigation strategies. Key findings from current research indicate that blanket exclusion of vulnerable groups from research is ethically problematic and scientifically counterproductive [69]. Instead, a balanced approach incorporating individualized capacity assessment, comprehensive consent processes, and multilayered safeguards can enable ethical research participation while protecting against exploitation and harm. The rapid evolution of these technologies necessitates equally adaptive ethical frameworks that can address emerging challenges while upholding fundamental principles of respect for persons, justice, and beneficence. Future work should focus on developing standardized implementation guidelines, enhancing digital literacy among vulnerable populations, and establishing international consensus on ethical standards for emerging technologies in research contexts.
Within the broader context of a thesis on vulnerable populations in research ethics, this technical guide provides a systematic analysis of how international ethics guidelines conceptualize and operationalize vulnerability. The concept of vulnerability serves as a cornerstone of research ethics, signaling to researchers and ethics committees that some participants may be at higher risk of harm or wrong [20]. Since its formal introduction in The Belmont Report (1979), the notion of vulnerability has been both universally adopted and persistently contested across the research ethics landscape [5] [20]. Despite widespread agreement that some research participants require special protections, substantial disagreement exists regarding its precise definition, underlying justification, and practical application across international policy frameworks [5] [13] [20].
This guidance responds to the pressing need to balance protection against exclusion of vulnerable populations in research. Historically, stringent protections led to the systematic exclusion of vulnerable groups from clinical research, consequently limiting their access to innovative treatments and perpetuating health inequities [5] [13]. Contemporary approaches increasingly recognize that ethical research requires not only protecting vulnerable individuals from harm but also ensuring their equitable participation in research [5] [10]. This whitepaper examines how major international guidelines navigate this complex terrain, offering researchers, scientists, and drug development professionals a practical framework for applying these principles in practice.
Analytical Methodology for Guideline Comparison
Systematic Approach to Policy Analysis
The comparative analysis presented in this whitepaper employs methodology adapted from recent systematic reviews of research ethics policy documents [5] [13] [20]. This approach enables a structured examination of how vulnerability is conceptualized and operationalized across international guidelines.
Table: Core Components for Policy Analysis
| Analytical Component | Description | Application Example |
|---|---|---|
| Definitional Analysis | Examination of explicit and implicit definitions of vulnerability | Identifying whether guidelines provide abstract definitions or rely on group classifications |
| Normative Justification | Analysis of ethical principles invoked to justify special protections | Determining if protections are grounded in consent, harm, or justice-based concerns |
| Group Identification | Cataloging populations specifically designated as vulnerable | Comparing lists of vulnerable groups across different guidelines |
| Operational Provisions | Examination of practical safeguards prescribed for vulnerable populations | Assessing specificity of procedural requirements for different vulnerable groups |
Document Selection and Evaluation Framework
The methodology for selecting and analyzing guidelines follows PRISMA-Ethics guidance for systematic reviews in research ethics [5] [13]. Authoritative policy documents were identified through comprehensive searches of established compilations including the International Compilation of Human Research Standards, Listing of Social-behavioral Research Standards, and ethics frameworks from authoritative bodies such as the World Medical Association and Council for International Organizations of Medical Sciences (CIOMS) [5] [73]. Analysis proceeds through structured examination of four interrelated domains: (1) definition of vulnerability, (2) identification of vulnerable groups/sources of vulnerability, (3) normative justifications for protection, and (4) specific provisions or safeguards required [20].
Diagram: Analytical Framework for Guideline Comparison. This workflow illustrates the systematic approach to analyzing policy documents across four key domains to generate conceptual, taxonomic, and practical outputs.
Conceptual Foundations of Vulnerability
Definitional Approaches Across Guidelines
International research ethics guidelines demonstrate considerable diversity in their definitional approaches to vulnerability. Analysis reveals that few policies provide explicit abstract definitions of vulnerability, instead relying predominantly on implicit definitions conveyed through the enumeration of vulnerable groups and specific sources of vulnerability [20]. This definitional ambiguity presents significant challenges for consistent application across research contexts and settings.
The Belmont Report established the foundational understanding of vulnerable persons as those in a "dependent state and with a frequently compromised capacity to free consent" [5] [13]. Subsequent guidelines have expanded upon this conception, with the National Bioethics Advisory Commission (NBAC) defining vulnerability as "a condition, either intrinsic or situational, of some individuals that puts them at greater risk of being used in ethically inappropriate ways in research" [3]. The Declaration of Helsinki characterizes vulnerable groups and individuals as those who "may have an increased likelihood of being wronged or of incurring additional harm" [3]. These definitions reflect what scholars have identified as three distinct accounts of vulnerability in research ethics: (1) consent-based accounts focusing on compromised capacity for autonomous decision-making; (2) harm-based accounts emphasizing increased susceptibility to research-related injuries; and (3) justice-based accounts concerned with unfair distribution of research burdens and benefits [5] [13].
Normative Justifications for Protection
The ethical justifications for providing additional protections to vulnerable research participants vary across international guidelines, reflecting different philosophical foundations and historical concerns.
Table: Normative Justifications for Protecting Vulnerable Participants
| Guideline Source | Primary Ethical Principle | Conceptualization of Vulnerability |
|---|---|---|
| Belmont Report (1979) | Respect for Persons | Diminished autonomy and compromised capacity for free consent |
| Declaration of Helsinki | Non-maleficence/ Beneficence | Increased likelihood of being wronged or incurring additional harm |
| NBAC Guidelines | Prevention of Exploitation | Increased risk of being used in ethically inappropriate ways |
| CIOMS Guidelines | Justice/Protection of Interests | Relative incapability of protecting one's own interests |
Analysis indicates that most guidelines incorporate multiple ethical justifications rather than relying on a single principle [20]. The integration of autonomy-based, harm-based, and justice-based concerns reflects recognition that vulnerability manifests in different forms across research contexts and may require correspondingly diverse protective measures [5] [20].
Comparative Analysis of International Guidelines
Categorical versus Contextual Approaches
International guidelines vary considerably in their approach to identifying vulnerable populations, with two predominant models emerging: the categorical approach and the contextual approach [3].
The categorical approach identifies specific groups presumed to be vulnerable, such as children, prisoners, pregnant women, and economically disadvantaged persons [3]. This approach is exemplified by the U.S. Common Rule (45 CFR §46), which enumerates vulnerable groups and in some cases provides specific regulatory subparts with additional protections (Subparts B-D) [3]. Similarly, the Declaration of Helsinki and CIOMS Guidelines provide extensive lists of populations typically considered vulnerable [3]. The primary strength of this approach lies in its practical clarity for researchers and ethics committees, while its limitation is the potential for both over-inclusion and under-inclusion of individuals who do not fit neatly within designated categories [3].
In contrast, the contextual approach recognizes vulnerability as arising from specific situations, relationships, or environments rather than group membership alone [3]. This approach acknowledges that vulnerability is often dynamic and multi-layered, resulting from interactions between individual characteristics and external circumstances [20]. The NBAC guidelines notably advocate for this perspective, emphasizing that "vulnerability is sensitive to context, and individuals may be vulnerable in one situation but not in another" [3]. Contemporary scholarship increasingly favors this nuanced understanding, though research ethics committees often prefer the categorical approach for its pragmatic simplicity [5] [13].
Typology of Vulnerabilities in Research Ethics
Synthesizing across international guidelines reveals a consistent typology of vulnerabilities that manifest in research contexts:
- Cognitive or Communicative Vulnerability: Encompasses persons with difficulty comprehending information or making decisions about participation, including those with limited decision-making capacity, those in situations that impair decision-making (e.g., medical emergencies), and those with communication barriers [3].
- Institutional Vulnerability: Includes persons under formal authority structures that may compromise voluntary choice, such as prisoners, military personnel, and students [3].
- Deferential Vulnerability: Arises from informal power imbalances based on gender, socioeconomic status, knowledge differentials (e.g., doctor-patient relationships), or other hierarchical relationships [3].
- Medical Vulnerability: Applies to persons with serious health conditions for which no satisfactory standard treatment exists, potentially compromising voluntary decision-making through desperation [13] [74].
- Economic Vulnerability: Stems from poverty or limited resources that may make financial incentives unduly influential [5] [3].
- Social Vulnerability: Affects marginalized groups experiencing discrimination, stigma, or limited social protections [5] [13].
Diagram: Categorical vs. Contextual Vulnerability Approaches. This visualization contrasts the group-based categorical approach with the situational contextual approach to identifying vulnerability in research.
Provisions and Safeguards for Vulnerable Populations
International guidelines prescribe various provisions and safeguards to protect vulnerable participants, though the specificity of these requirements varies considerably across documents.
Table: Protective Provisions for Vulnerable Populations
| Vulnerability Type | Common Safeguards | Guideline Sources |
|---|---|---|
| Cognitive/Communicative | Assessment of capacity, use of surrogates, simplified consent forms, staged consent, interpreters, delayed enrollment | [3] |
| Institutional | Alternative consent processes, independent recruiters, exclusion of those unable to refuse voluntarily | [3] |
| Deferential | Minimization of power differentials in consent process, independent oversight, careful evaluation of incentives | [3] |
| All Vulnerable Groups | Additional scrutiny by research ethics committees, justification for inclusion, assessment of risks and benefits | [5] [3] [10] |
A critical consideration across guidelines is the principle of proportionality – safeguards should be commensurate with the level and nature of vulnerability, avoiding both inadequate protection and excessive paternalism that might unjustly exclude populations from research participation [3]. The Declaration of Helsinki emphasizes that particular attention must be given to specific populations who are "vulnerable to coercion or undue influence" [3]. Meanwhile, CIOMS guidelines note that special justification is required for research involving vulnerable persons, and such research should be "exceptionally responsive to the health needs or priorities of these groups" [20].
Practical Implementation Framework
Decision-Making Protocol for Researchers
For researchers and drug development professionals navigating the complex landscape of vulnerability protections, a structured decision-making protocol emerges from comparative guideline analysis:
- Vulnerability Assessment: Identify potential vulnerabilities using both categorical and contextual approaches, considering individual characteristics, research design, and environmental factors [3].
- Necessity Determination: Justify the inclusion of vulnerable participants based on scientific necessity and responsiveness to the health needs of the vulnerable group [3] [20].
- Safeguard Selection: Implement safeguards proportionate to the identified vulnerabilities, drawing from established protections for specific vulnerability types [3] [10].
- Ethics Review Engagement: Seek early consultation with research ethics committees regarding vulnerability assessments and proposed protections [5] [73].
- Continuous Monitoring: Maintain ongoing evaluation of participant vulnerability throughout the research process, with particular attention to changing circumstances [3] [10].
Research Reagent Solutions: Ethical Tools for Vulnerability Protection
Table: Essential Methodological Tools for Ethical Research with Vulnerable Populations
| Research Tool | Function | Application Context |
|---|---|---|
| Capacity Assessment Protocols | Objective evaluation of decision-making capacity | Research involving persons with cognitive impairments, mental illness, or acute medical conditions |
| Cultural/Linguistic Adaptation Frameworks | Ensure comprehension across diverse populations | Research with linguistic minorities, indigenous communities, or cross-cultural settings |
| Tiered Consent Procedures | Facilitate understanding through staged information disclosure | Complex research protocols or populations with fluctuating capacity |
| Independent Participant Advocates | Protect interests of participants with institutional or deferential vulnerability | Research involving prisoners, institutionalized persons, or significant power imbalances |
| Contextual Vulnerability Assessment Checklists | Systematic identification of situational vulnerability factors | All research protocols during ethics review and ongoing monitoring |
This comparative analysis demonstrates that while international ethics guidelines share a common commitment to protecting vulnerable research participants, they diverge significantly in their conceptualization, identification, and management of vulnerability. The tension between categorical and contextual approaches reflects a fundamental challenge in research ethics: balancing the need for clear, practicable standards against the ethical imperative to recognize the nuanced and dynamic nature of vulnerability in real-world research contexts [5] [3] [20].
For researchers, scientists, and drug development professionals, effective ethical practice requires moving beyond mechanical compliance with categorical classifications toward a more nuanced, process-oriented approach that carefully considers how specific research contexts may create or exacerbate vulnerabilities [3]. This approach aligns with emerging trends in research ethics that emphasize proportional protections – safeguards that adequately protect vulnerable participants without unnecessarily excluding them from research participation and its potential benefits [5] [13].
The evolving landscape of international guidelines suggests a growing recognition that vulnerability is not a fixed property of certain groups, but rather a potential condition that may arise through the interaction of individual characteristics, research design, and social context [3] [20]. This understanding places responsibility on researchers and ethics committees to conduct context-sensitive vulnerability assessments and implement appropriately tailored safeguards throughout the research process. As policy continues to develop in this area, the challenge remains to provide sufficient guidance to ensure consistent ethical practice while allowing the flexibility needed to respond to the unique vulnerabilities that arise across diverse research contexts.
Ethical rigor forms the cornerstone of valid and trustworthy clinical research. This analysis examines recent ethical successes and failures within the specific context of vulnerable populations, framing them within the enduring principles of research ethics established by foundational documents like the Belmont Report [12]. Vulnerable populations—including those facing serious illness, economic disadvantage, or marginalization—are at heightened risk of exploitation, making stringent ethical safeguards not merely a regulatory requirement but a moral imperative [36] [75] [12]. This paper synthesizes evidence from contemporary case studies, detailing both commendable ethical practices and concerning lapses. It provides a technical guide for researchers and drug development professionals, complete with structured data, methodological protocols, and practical tools to navigate the complex ethical terrain of modern clinical research, particularly when working with vulnerable groups.
Analysis of Recent Ethical Failures
The Termination of Federally Funded Clinical Trials
A significant contemporary ethical challenge involves the premature termination of thousands of National Institutes of Health (NIH) grants connected to ongoing clinical trials as of July 2025 [75]. This decision impacted over 200 trials and approximately 689,000 participants, about 20% of whom were infants, children, and adolescents. Many of these studies focused on health challenges in populations that identify as Black, Latinx, or sexual and gender minority [75].
Ethical Analysis and Violated Principles
This mass termination represents a systemic ethical failure on multiple fronts, directly conflicting with the core principles of the Belmont Report:
- Violation of Respect for Persons: The abrupt cessation of studies challenges the very foundation of informed consent. Participants were not informed that their studies might be defunded for political reasons, thereby invalidating the autonomy of their decision to participate [75].
- Violation of Beneficence: The termination disrupts or ends benefits that research participation provides, potentially denying participants access to promising interventions. In some cases, funding disruption has "resulted in contamination of the study design," forcing participant withdrawal and rendering their data unusable [75].
- Violation of Justice: This action disproportionately affects marginalized populations who are already underrepresented in research yet bear a higher burden of disease. Halting these studies reverses progress toward health equity and perpetuates historical injustices [75] [12].
Table 1: Quantitative Impact of Recent Clinical Trial Terminations
| Metric | Impact Scope | Population Details |
|---|---|---|
| Number of Grants Cut | Approximately 4,700 [75] | - |
| Clinical Trials Affected | More than 200 [75] | - |
| Total Participants Affected | Roughly 689,000 [75] | - |
| Young Participants Affected | ~20% (Infants, Children, Adolescents) [75] | Conditions included HIV, substance use, depression [75] |
Historical Context of Ethical Violations
Contemporary failures are best understood alongside historical violations that shaped modern research ethics. Key cases include:
- The Tuskegee Syphilis Study (1932-1972): Researchers from the U.S. Public Health Service withheld treatment from African American men with syphilis and deliberately denied them life-saving penicillin even after it became the standard treatment. The study's legacy includes profound and lasting mistrust of medical research within Black communities [12].
- Nazi Medical Experiments (WWII): Non-consensual, often fatal experiments on concentration camp prisoners led to the Nuremberg Code, which established voluntary consent as an absolute ethical cornerstone [12].
- Willowbrook Hepatitis Study (1956-1970): Researchers intentionally infected children with intellectual disabilities with hepatitis, exploiting a vulnerable population and a coercive environment for parental consent [12].
Analysis of Ethical Successes and Frameworks for Navigating Challenges
Ethical Praxis in Sensitive Qualitative Research
A reflective narrative from a qualitative study in Ghana involving men with advanced prostate cancer and their caregivers provides a model for ethical success in complex, sensitive research settings [36]. The study, which explored home-based care dynamics, exemplifies how a clinician-researcher can navigate a dual role ethically through heightened reflexivity and structured practices.
Experimental Protocol and Methodology
The methodological framework for this ethically conscious research is detailed below.
Table 2: Methodological Protocol for Ethical Sensitive Research
| Component | Implementation in the Prostate Cancer Care Study |
|---|---|
| Research Design | Qualitative design employing individual interviews, dyadic interviews, and focus group discussions [36]. |
| Methodological Approach | Reflective narrative approach to critically engage with the researcher's personal experiences and ethical dilemmas [36]. |
| Data Sources | Interview transcripts, detailed field notes, reflexive memos, and a field diary documenting emotional reactions and ethical uncertainties [36]. |
| Reflexive Process | Inductive analysis of reflective material; regular debriefing with peers and mentors to externalize reflections and mitigate over-identification [36]. |
| Ethical Safeguards | Enhanced ethical preparation, clear boundary protocols, structured reflexive journaling, and regular peer debriefing [36]. |
Success Analysis and Implemented Principles
This case study demonstrates the successful application of ethical principles in a resource-limited setting:
- Upholding Respect for Persons: The researcher maintained ongoing, informed consent and respected cultural sensitivities around stigma and taboos related to prostate cancer, fostering trust and authenticity [36].
- Exercising Beneficence and Non-maleficence: The reflective approach allowed the researcher to manage emotional labor and navigate the ethical tension between intervening in clinical needs (e.g., observing unsafe wound-dressing practices) and maintaining research integrity [36].
- Promoting Justice: The study focused on a vulnerable population in a global south context, contributing valuable knowledge on a culturally specific healthcare experience and working to avoid their erasure from scientific discourse [36].
An Integrated Workflow for Ethical Decision-Making
The following diagram maps the logical workflow and critical decision points for managing ethical dilemmas, as illustrated in the clinician-researcher case study.
Upholding ethical standards requires not only principled judgment but also the consistent application of proven tools and materials. The following table details key resources for conducting ethically sound research with vulnerable populations.
Table 3: Research Reagent Solutions for Ethical Practice
| Research 'Reagent' | Function in Ethical Research |
|---|---|
| Informed Consent Forms | Documents the voluntary agreement of a participant to take part in research after being fully informed of the purpose, procedures, risks, and benefits [12]. |
| Protocols for Reflexive Journaling | A structured method for researchers to document their positionality, emotional responses, and ethical uncertainties, enhancing self-awareness and critical engagement [36]. |
| Institutional Review Board (IRB) Protocol | The formal research plan submitted for ethical and scientific review to an independent body to ensure participant safety and ethical conduct [12]. |
| Peer Debriefing Framework | A structured process for discussing ethical challenges with disinterested peers to mitigate bias and emotional involvement, validating the researcher's interpretive process [36]. |
| Data Anonymization Tools | Software and procedures to remove or encrypt personally identifiable information from research data, safeguarding participant confidentiality and privacy [12]. |
| Community Engagement Plan | A strategy for involving the community from which participants are drawn in the design and conduct of research, ensuring cultural relevance and respect [12]. |
The recent cases of clinical trial termination and the reflective model of ethical research in palliative care underscore a critical duality. On one hand, systemic and political decisions can perpetuate historical ethical failures, eroding trust and violating the core principles of respect, beneficence, and justice, particularly for vulnerable groups. On the other hand, individual researchers and teams can successfully navigate profound ethical complexities through deliberate, structured, and reflexive practices. For researchers, scientists, and drug development professionals, the path forward must involve a renewed commitment to these proactive frameworks. This includes advocating for policies that protect ongoing research, integrating ethical planning from a study's inception, and embracing reflexivity not as an ancillary task but as a central component of rigorous, respectful, and ultimately successful research with vulnerable populations.
The systematic underrepresentation of specific populations in scientific and clinical research is not merely a statistical discrepancy; it constitutes a fundamental flaw that compromises the scientific integrity, generalizability, and ethical foundation of medical advancements. This whitepaper examines the multifaceted costs of this exclusion, focusing on both the scientific consequences, such as biased data and non-generalizable findings, and the profound ethical implications, particularly for vulnerable and marginalized populations. Despite increased awareness, global data indicate persistent gaps. For instance, women now account for only 33% of researchers globally, a figure that remains far from parity [76]. In clinical trials, Black and Hispanic populations frequently account for less than 10% of participants, despite often bearing a higher burden of diseases like diabetes and certain cancers [77]. This underrepresentation threatens the validity of research findings and perpetuates long-standing health inequities. The following sections will quantify the current state of representation, detail the scientific and ethical costs of exclusion, analyze the barriers to inclusion, and propose a framework of actionable solutions for researchers and drug development professionals.
Representation in scientific research and clinical trials remains uneven across geographic regions, disciplines, and demographic groups. The data reveal a landscape of progress in some areas juxtaposed with persistent, deep-rooted disparities in others.
Global and Regional Representation in STEM
The global participation of women in science, technology, engineering, and mathematics (STEM) fields serves as one barometer for inclusion. As of 2025, women comprise approximately 28% of the overall STEM workforce, with men constituting the remaining 72% [76]. This global average, however, masks significant regional variations and disciplinary imbalances. The table below summarizes key regional data for women in research.
Table 1: Regional Comparison of Women in Research (2025)
| Region | Percentage of Women Researchers | Key Disciplinary Notes |
|---|---|---|
| Latin America | 44% | Leads in participation but struggles with mid-career retention [76]. |
| Europe | 35% | Strong in biology and medicine; underrepresentation in engineering [76]. |
| North America | ~30% | Well-represented in health/life sciences; under 20% in computing/engineering [76]. |
| Africa | <30% (average) | Wide national variation; improved representation with targeted policies [76]. |
| Asia and Pacific | 27% | Contrasts between high graduation rates and poor long-term retention [76]. |
Disciplinary representation is equally skewed. According to OECD data, while women have reached parity in life sciences (50%), they remain severely underrepresented in engineering (18%) and computer science (20%) [76]. This phenomenon, often described as the "leaky pipeline," sees the proportion of women declining at successive career stages, from undergraduate studies to senior leadership positions [76].
Representation in Clinical Research
In clinical trials, the underrepresentation of racial and ethnic minorities is a long-standing challenge. An analysis of FDA-approved drugs in 2020 revealed that 75% of trial participants were White, despite White people constituting only 62% of the U.S. population according to the 2020 Census [78]. A review of 53 new molecular entities approved by the FDA in 2020 found that only 8% of trial participants were Black and 11% were Hispanic, proportions that lag behind their share of the U.S. population [79]. This disparity exists despite evidence that members of underrepresented ethnic groups express a willingness to participate in research that is equal to or greater than that of majority groups [80]. A 2014 national review of cancer trials, for example, found equal willingness to participate across racial and ethnic groups [80].
Scientific Consequences of Underrepresentation
The exclusion of diverse populations from research has direct and detrimental effects on the quality of scientific data, the safety and efficacy of medical products, and the pace of innovation.
Limited Generalizability and Biased Data
When clinical trials fail to enroll participants who reflect the demographics of the real-world population that will use a medical product, the generalizability of the results is severely compromised. This limits researchers' ability to examine therapy responses across different racial, ethnic, gender, and age groups [79]. The consequence is a medical evidence base that may not be applicable to all patients, leading to uncertainties for clinicians and patients from underrepresented groups. As noted by one analysis, "Without adequately representing the populations most affected by a disease, clinical trial data risks being biased, potentially resulting in treatments that are less effective—or even harmful—for underrepresented groups" [77]. This scientific shortcoming directly fuels health disparities, as treatments and interventions end up being tailored primarily to the majority population [81].
Compromised Safety and Efficacy
Differences in medical product safety and effectiveness can emerge based on factors such as age, ethnicity, sex, and race [77]. A homogeneous participant pool can obscure these variations, potentially leading to the approval of drugs that have unanticipated side effects or reduced potency in certain populations. For example, the failure to understand sexually dimorphic effects between genders can contribute to disparities in respective treatment outcomes [79]. This lack of diverse data poses a direct risk to patient safety and public health.
Table 2: Key Scientific Consequences of Underrepresentation
| Scientific Dimension | Consequence of Underrepresentation | Example/Impact |
|---|---|---|
| Data Generalizability | Findings cannot be reliably applied to broader, diverse populations. | Physicians may be less likely to prescribe drugs to Black patients if trials were unrepresentative [82]. |
| Safety & Efficacy Profiling | Incomplete understanding of drug response variability. | Risk of unforeseen adverse events or reduced effectiveness in underrepresented groups [77]. |
| Innovation & Discovery | Limits the scope of scientific inquiry and problem-solving. | Lack of diverse perspectives can stifle creativity and lead to solutions that fail to meet all needs [83]. |
| Precision Medicine | Hinders the development of tailored treatments. | Inability to identify genetic, metabolic, or social factors that influence disease and treatment across groups [77]. |
Ethical Consequences of Underrepresentation
Beyond the scientific imperative, the exclusion of specific populations from research raises profound ethical concerns that challenge the core principles of research ethics, particularly when involving vulnerable populations.
Violation of Ethical Principles
The abrupt termination of clinical trials, especially those involving marginalized groups, highlights acute ethical dilemmas. Such actions conflict with the long-standing ethical principles of the Belmont Report: respect for persons, beneficence, and justice [75]. When studies enrolling young people dealing with serious health challenges like HIV or depression are cut short for political or funding reasons, it violates the trust between researchers and participants and challenges the notion of true informed consent [75]. Participants accept the risks of research with the understanding that their contribution will advance knowledge and public health; terminating a study prematurely negates the value of their contribution and disrespects their autonomy.
Breach of Trust and Social Justice
The historical legacy of abuse and exploitation in medical research, such as the Tuskegee syphilis study, has engendered a deep-seated mistrust of the healthcare system and research institutions among many marginalized communities [80] [81]. Continued underrepresentation and exclusion perpetuate this mistrust, creating a vicious cycle where past exclusion leads to reluctance to participate, which in turn leads to continued lack of representation. This constitutes a breach of the ethical principle of justice, which demands a fair distribution of the benefits and burdens of research. When certain groups are consistently excluded from the potential benefits of participating in research, such as access to cutting-edge therapies, and are also subject to the risks of treatments tested only on other populations, a profound injustice occurs [81] [75].
Impact of Recent Policy Shifts
Recent executive orders in the United States banning diversity, equity, and inclusion (DEI) initiatives in the federal government threaten to reverse progress and exacerbate these ethical concerns. These orders have led to the termination of programs designed to promote equitable access for LGBTQIA+ populations and other groups underrepresented in research [82]. Furthermore, cuts to thousands of federal grants for clinical trials "threaten to upend the progress made in the past few decades" in understanding and treating the health challenges of marginalized populations [75]. Such policy shifts risk further alienating vulnerable communities and undermining the ethical foundation of clinical research.
Barriers and Facilitators to Inclusion
Addressing the cost of exclusion requires a clear understanding of the barriers that limit participation and the facilitators that can promote it. The socio-ecological framework offers a multi-level perspective on these factors.
Multifaceted Barriers to Participation
The barriers to inclusive research are not primarily due to a lack of willingness among underrepresented groups. Evidence consistently shows that Asian, Black, Latinx, and American Indian/Alaska Native individuals are no less likely, and in some cases more likely, to participate in research if asked [80]. The barriers are more systemic and operational:
- Trust and Historical Legacy: Mistrust of healthcare professionals, research, and researchers due to historical and contemporary abuses is a significant barrier [80] [81].
- Socioeconomic and Logistical Challenges: Practical obstacles include lack of transportation, competing work and caregiving responsibilities, and the direct costs of participation [78] [81].
- Institutional and Research Design Flaws: A frequent barrier is the simple failure of researchers to ask underrepresented individuals to participate [80]. Other institutional barriers include language barriers, unavailability of translated study materials, and study locations that are inaccessible to certain communities [78] [81].
- Implicit Bias among Research Staff: Clinical research coordinators (CRCs) may demonstrate unconscious biases that affect recruitment. One study found that CRCs reported greater success in recruiting participants from groups that are not underrepresented in research, though implicit bias vignettes did not show a direct link to approach intentions [78].
Table 3: Barriers and Facilitators Across the Socio-Ecological Framework
| Level | Barriers | Facilitators |
|---|---|---|
| Individual | Mistrust, lack of awareness about trials, fear [81]. | Transparent communication, providing summary results post-trial [82]. |
| Interpersonal | Lack of culturally competent staff; language barriers [78] [81]. | Hiring diverse staff; cultural competency training; translated materials [78] [82]. |
| Institutional | Study designs with rigid, exclusionary criteria; inconvenient study locations and visit schedules [77] [78]. | Community-oriented research; flexible visit schedules; decentralized trials [78] [82]. |
| Community/Societal | Historical abuses; legacies of discrimination; policy environments hostile to DEI [80] [82]. | Community engagement and partnerships; trusted community leaders as ambassadors [81] [79]. |
Evidence-Based Facilitators and Strategies
Research has identified several effective strategies to improve the recruitment and retention of underrepresented groups:
- Community Engagement and Personalized Approaches: Building long-term, authentic relationships with communities and engaging patient and public involvement (PPI) groups are critical [81] [79]. This includes working with community leaders and using targeted, culturally relevant advertising [79].
- Culturally and Linguistically Appropriate Materials: Providing translated study documents and consent forms, as well as employing bilingual staff, are key facilitators identified by both research participants and clinical research coordinators [78] [81].
- Reducing Participant Burden: Strategies that improve recruitment include providing incentives to compensate for time and travel, and reducing the number of required in-person study visits [78].
- Diversifying the Research Workforce: Recruiting research staff who reflect the communities they serve is a powerful tool for building trust and improving enrollment. The diversity of patients enrolled at a site is often proportionate to the diversity of the site personnel [82].
Methodologies and Experimental Protocols for Inclusive Research
To move from identifying barriers to implementing solutions, researchers require concrete methodological tools and protocols. The following section outlines established and emerging approaches for designing inclusive studies.
Community-Engaged Recruitment Protocol
This protocol is designed to be integrated during the early planning stages of a clinical trial to ensure recruitment strategies are centered on community needs and input.
- Objective: To establish a participatory framework for trial design and recruitment that builds trust and aligns study procedures with community context.
- Materials:
- Community Advisory Board (CAB): A group of community stakeholders, patient advocates, and trusted local leaders.
- Culturally Translated Materials: Study advertisements, informed consent forms, and participant surveys translated and back-translated for cultural and linguistic appropriateness.
- Dedicated Budget: Resources for compensating CAB members, covering translation services, and implementing community-suggested logistical support (e.g., transportation vouchers, childcare).
- Procedure:
- Community Mapping (Months 1-2): Identify and map key community organizations, clinics, and trusted leaders in areas with high disease prevalence and underrepresented populations.
- CAB Formation (Month 3): Recruit and formally constitute a CAB, outlining roles, responsibilities, and compensation.
- Collaborative Protocol Review (Month 4): Present the draft study protocol to the CAB for feedback on eligibility criteria, visit schedules, and outcome measures. Revise the protocol based on CAB input to reduce unnecessary barriers.
- Co-Development of Materials (Month 5): Work with the CAB and professional translators to develop and refine all participant-facing materials.
- Ongoing Engagement (Throughout Trial): Hold regular CAB meetings to review recruitment progress, discuss challenges, and adapt strategies as needed.
Experimental Workflow for Inclusive Trial Design
The following diagram visualizes the key stages of embedding equity and inclusion throughout the clinical trial lifecycle, from initial design to post-trial dissemination.
The Scientist's Toolkit: Research Reagent Solutions for Equity
Advancing research equity requires not only methodological shifts but also specific "reagents" or tools. The following table details key resources essential for conducting inclusive research.
Table 4: Essential Research Reagent Solutions for Inclusive Studies
| Tool/Reagent | Function in Promoting Equity | Application Notes |
|---|---|---|
| Translated & Culturally Adapted Consent Forms | Ensures true informed consent by making complex study information comprehensible and relevant to participants of diverse linguistic and cultural backgrounds. | Requires professional translation and back-translation, plus review by cultural experts for contextual appropriateness beyond literal meaning [78] [81]. |
| Diversity Action Plan (DAP) | A formal document, now required by the FDA for Phase III trials, outlining goals and strategies for enrolling a participant population that reflects the demographics of the disease population [77] [82]. | Serves as a strategic roadmap for sponsors, forcing early consideration of eligibility criteria, site selection, and recruitment tactics. |
| Community Advisory Board (CAB) | Provides ongoing, grounded insight into community norms, concerns, and effective communication channels, acting as a bridge between the research institution and the community. | Critical for building trust and ensuring study acceptability. Members must be compensated for their time and expertise [81] [79]. |
| Digital Patient Recruitment Platforms | Expands the reach of trial advertising to diverse audiences through targeted social media campaigns and partnerships with community-focused websites. | Must be used ethically and in conjunction with traditional community engagement to avoid perpetuating digital divides [79]. |
| Implicit Bias Training Modules | Educates research staff (PIs, CRCs) about unconscious attitudes and stereotypes that can affect interactions with potential participants and decisions about eligibility. | Training should be mandatory and skill-based, focusing on practical strategies to mitigate bias in recruitment and consent processes [78]. |
The cost of exclusion in scientific research is both scientifically untenable and ethically indefensible. The consequences—from non-generalizable data and compromised patient safety to the perpetuation of health inequities and violation of core ethical principles—impose a heavy burden on society and the scientific enterprise. The evidence is clear: the problem is not a lack of willingness among diverse populations to participate, but rather a failure of research systems to adequately invite, include, and value them. As the global community faces complex health challenges, the need for scientific solutions that work for everyone has never been greater. Researchers, sponsors, and regulators have a collective responsibility to implement the known facilitators of inclusion: engaging communities as authentic partners, diversifying the research workforce, reducing practical barriers to participation, and designing studies with equity as a core objective. The future validity of science and the just distribution of its benefits depend on this critical evolution.
Conclusion
Ethical research with vulnerable populations is not an obstacle to scientific progress but a fundamental prerequisite for it. The key takeaways underscore that a nuanced, analytical understanding of vulnerability—moving beyond simple checklists—is essential. This must be coupled with robust, participant-centered methodologies that prioritize genuine informed consent and community partnership. Furthermore, the research community must develop resilient frameworks to navigate modern challenges, from globalized trials and new technologies to the ethical management of study terminations. The future of credible and impactful biomedical research depends on our collective commitment to these principles, ensuring that scientific advancement is both inclusive and just, ultimately benefiting all segments of society.
References
- 1. Research Ethics - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK459281/]
- 2. Ethical Considerations When Vulnerable Populations are ... [https://rethinkingclinicaltrials.org/news/grand-rounds-ethics-and-regulatory-series-january-13-2023-ethical-considerations-when-vulnerable-populations-are-subjects-in-pragmatic-trials-emily-a-largent-jd-phd-rn/]
- 3. Vulnerability in Research: Basic Ethical Concepts and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7122263/]
- 4. Guiding Principles for Ethical Research [https://www.nih.gov/health-information/nih-clinical-research-trials-you/guiding-principles-ethical-research]
- 5. Vulnerability in research ethics: A systematic review of policy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12212517/]
- 6. Ethics and Consent in Research with Vulnerable Participants [https://researchmethodscommunity.sagepub.com/blog/ethics-and-consent-in-research-with-vulnerable-participants]
- 7. Principles of Clinical Ethics and Their Application to Practice [https://pmc.ncbi.nlm.nih.gov/articles/PMC7923912/]
- 8. Ethics and integrity in uncertain times [https://www.nature.com/articles/s41591-025-03795-4]
- 9. ORI is Updating its Policies on Research Integrity to Meet ... [https://ori.hhs.gov/blog/ori-updating-its-policies-research-integrity-meet-demands-modern-research-environment]
- 10. Ethics in Vulnerable Population Research [https://www.solutionsirb.com/ethics-in-vulnerable-population-research/]
- 11. Evolution of protections of human participants in research [https://uwaterloo.ca/research/office-research-ethics/research-human-participants/frequently-asked-questions/evolution-protections-human-participants-research]
- 12. Ethical Violations in Clinical Research: Lessons from the ... [https://acrpnet.org/2025/06/16/ethical-violations-in-clinical-research-lessons-from-the-past-challenges-for-the-future]
- 13. Vulnerability in research ethics: A systematic review of policy ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0327086]
- 14. Research Ethics Timeline [https://www.niehs.nih.gov/research/resources/bioethics/timeline]
- 15. The Nuremberg Code Does Not Apply to Licensed ... [https://historyofvaccines.org/blog/the-nuremberg-code-does-not-apply-to-licensed-approved-and-authorized-vaccinations-only-to-the-research-that-led-to-that-licensure-approval-and-authorization/]
- 16. About The Untreated Syphilis Study at Tuskegee [https://www.cdc.gov/tuskegee/about/index.html]
- 17. Willowbrook State School: Institutional Abuse, Medical Ethics ... [https://criticaldebateshsgj.scholasticahq.com/article/141852-willowbrook-state-school-institutional-abuse-medical-ethics-and-the-rise-of-disability-rights-in-the-united-states]
- 18. Vulnerable population and methods for their safeguard [https://pmc.ncbi.nlm.nih.gov/articles/PMC3601707/]
- 19. Vulnerable Populations Research Core | Cizik Nursing ... [https://www.uth.edu/nursing-research/cores/vulnerable-populations-research/]
- 20. The concept of 'vulnerability' in research ethics: an in-depth ... [https://health-policy-systems.biomedcentral.com/articles/10.1186/s12961-016-0164-6]
- 21. Chasing 'vulnerability' across six decades of the ... [https://link.springer.com/article/10.1007/s40592-025-00235-4]
- 22. 2025 Code of Ethics for Nurses Provision 7.2 [https://codeofethics.ana.org/provision-7-2]
- 23. Belmont Report - Human Research Protection Program [https://irb.wisc.edu/regulatory-information/belmont-report/]
- 24. The creation of the Belmont Report and its effect on ethical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9700634/]
- 25. 10 Clinical Trial Regulatory Changes Coming in 2025 [https://en.ennov.com/blog/clinical-blog/trial-regulatory-changes-coming-2025/]
- 26. With the Right Approach, Vulnerable Populations Can and ... [https://acrpnet.org/2025/10/29/with-the-right-approach-vulnerable-populations-can-and-should-be-engaged-in-research]
- 27. Five Data-Informed Principles for Advancing Inclusive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474690/]
- 28. SPIRIT 2025 statement: Updated guideline for protocols of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037212/]
- 29. Diversity, equity, and inclusion in 2025: 10 DE&I trends all ... [https://www.etu.co/resources/2025-dei]
- 30. Seeing Beyond the Margins: Challenges to Informed Inclusion of Vulnerable Populations in Research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6077979/]
- 31. Vulnerable population and methods for their safeguard - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3601707/]
- 32. Bridging ethical gaps in digital health research: a framework ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12509369/]
- 33. Factors Influencing Informed Consent Preferences in ... [https://www.jmir.org/2025/1/e63349/]
- 34. Developing guidelines for culturally relevant informed consent: an example from Lebanon | PLOS Mental Health [https://journals.plos.org/mentalhealth/article?id=10.1371/journal.pmen.0000174]
- 35. The Requirements for Informed Consent (Series #1) [https://www.tc.columbia.edu/institutional-review-board/irb-blog/2025/informed-consent-the-requirements-for-informed-consent-series-1/]
- 36. Ethical challenges in sensitive research: a reflective narrative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12275307/]
- 37. Code of Ethics [https://acrpnet.org/about-acrp/code-of-ethics]
- 38. Ethical and Bias Considerations in Artificial Intelligence ... [https://www.sciencedirect.com/science/article/pii/S0893395224002667]
- 39. Online research with vulnerable populations [https://researchmethodscommunity.sagepub.com/blog/online-research-vulnerable-populations]
- 40. Considerations for enrolling Vulnerable Populations in ... [https://tfscro.com/resources/regulatory-considerations-for-enrolling-vulnerable-populations-in-clinical-trials/]
- 41. Methods for engaging vulnerable and marginalized children ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12392517/]
- 42. Building Trust for Community-Engaged Research [https://jprm.scholasticahq.com/article/131692-building-trust-for-community-engaged-research-recommendations-from-a-qualitative-study]
- 43. Principles for Establishing Trust When Developing a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3103821/]
- 44. Checklist for Ensuring Participant Confidentiality [https://www.upskillist.com/blog/checklist-for-ensuring-participant-confidentiality/]
- 45. Preventing Coercion and Influence in Research Consent [https://www.solutionsirb.com/preventing-coercion-and-influence-in-research-consent/]
- 46. Subject Payment - UW Research [https://www.washington.edu/research/hsd/guidance/subject-payment/]
- 47. Monitoring Coercion and Undue Influence in Vulnerable ... [https://www.clinicaltrials101.com/monitoring-coercion-and-undue-influence-in-vulnerable-participant-recruitment/]
- 48. The Ethics of College Students as Research Participants [https://link.springer.com/article/10.1007/s10805-025-09670-8]
- 49. The emotional labour of boundary spanning - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5868552/]
- 50. Emotional Labor in the Workplace: The Disproportionate ... [https://www.stkate.edu/academics/women-in-leadership-degrees/empowering-women/emotional-labor-in-the-workplace]
- 51. Coping with Emotionally Challenging Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC12457521/]
- 52. Healthcare Professionals' Emotional Labor and ... [https://pubmed.ncbi.nlm.nih.gov/37331974/]
- 53. Ethics Committees: Structure, Roles, and Issues - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10293659/]
- 54. Pre-Randomization Predictors of Study Discontinuation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11266258/]
- 55. Eliciting adverse effects data from participants in clinical trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC7098080/]
- 56. Capacity, Vulnerability, and Informed Consent for Research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6035898/]
- 57. 240. Research Involving Adults with Impaired Decision-Making Capacity | Research Integrity & Security | University of Nevada, Reno [https://www.unr.edu/research-integrity/program-areas/human-research/human-research-protection-policy-manual/240-research-involving-adults-with-impaired-decision-making-capacity]
- 58. Issues and Challenges for Clinical Research in International ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7150258/]
- 59. Vulnerable Participants [https://hrpp.research.virginia.edu/teams/irb-sbs/researcher-guide-irb-sbs/vulnerable-participants]
- 60. 14 Comparing quantitative data between individuals [https://bookdown.org/pkaldunn/SRM-Textbook/BetweenQuantData.html]
- 61. 7 Types of Comparison Charts for Effective Data Visualization [https://ninjatables.com/types-of-comparison-charts/?srsltid=AfmBOopTtFkE9FEI_IDqDyds6dHtlfaMv-j51WHv4L8yWM3CqwNJ2nGd]
- 62. Graphic Protocols [https://www.biorender.com/features/graphic-protocols]
- 63. The ethics of global clinical trials - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4428044/]
- 64. Globalization of clinical trials: ethical and regulatory ... [https://www.ijclinicaltrials.com/index.php/ijct/article/view/103]
- 65. The ethics of clinical research in low- and middle-income ... [https://www.sciencedirect.com/science/article/abs/pii/B9780444535016000251]
- 66. Synthetic data created by generative AI poses ethical challenges [https://www.niehs.nih.gov/news/factor/2025/4/feature/ai-data-ethics]
- 67. Advancing artificial intelligence ethics in health and ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1563544/full]
- 68. The 2025 Guide to Ethical Standards in Personalized ... [https://www.laboratoriosrubio.com/en/ethical-personalized-medicine/]
- 69. Obstacles, Opportunities, and Ethical Considerations for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12496010/]
- 70. Digital Health for Vulnerable and Disabled Populations in ... [https://www.medrxiv.org/content/10.1101/2025.09.15.25335819v1.full-text]
- 71. Ethical and Quality of Care–Related Challenges of Digital ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12560958/]
- 72. Ethical, Legal and Social Implications Research Program [https://www.genome.gov/Funded-Programs-Projects/ELSI-Research-Program-ethical-legal-social-implications]
- 73. Ensuring ethical standards and procedures for research ... [https://www.who.int/activities/ensuring-ethical-standards-and-procedures-for-research-with-human-beings]
- 74. 1. Fundamental Ethical Principles [https://www.isscr.org/guidelines/fundamental-ethical-principles]
- 75. Researchers Highlight Ethical Concerns When Clinical ... [https://www.bu.edu/sph/news/articles/2025/researchers-highlight-ethical-concerns-when-clinical-trials-are-cut-short/]
- 76. Latest Women In STEM Statistics For 2025 [https://womeninstemnetwork.com/women-stem-statistics-2025/]
- 77. Diversity in Clinical Trials: A Scientific Imperative for 2025 [https://www.wcgclinical.com/insights/diversity-in-clinical-trials-a-scientific-imperative-for-2025/]
- 78. Barriers and facilitators to recruitment of underrepresented ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10514687/]
- 79. Barriers to diversification in recruitment, minority ... [https://www.sciencedirect.com/science/article/abs/pii/S0165178121006284]
- 80. Barriers to Representation of Underrepresented and Excluded ... [https://www.ncbi.nlm.nih.gov/books/NBK584407/]
- 81. Barriers and facilitators for engaging underrepresented ethnic ... [https://equityhealthj.biomedcentral.com/articles/10.1186/s12939-025-02431-4]
- 82. The Impact of DEI Ban On Clinical Research Ecosystem [https://www.appliedclinicaltrialsonline.com/view/the-impact-of-dei-ban-on-clinical-research-ecosystem]
- 83. UNESCO launches ''Imagine a world with more women in ... [https://www.unesco.org/en/articles/unesco-launches-imagine-world-more-women-science-campaign]