Empirical Bioethics Methodology: Assessing Rigor, Navigating Standards, and Implementing Best Practices
This article provides a comprehensive framework for assessing methodological rigor in empirical bioethics, tailored for researchers, scientists, and drug development professionals.
Empirical Bioethics Methodology: Assessing Rigor, Navigating Standards, and Implementing Best Practices
Abstract
This article provides a comprehensive framework for assessing methodological rigor in empirical bioethics, tailored for researchers, scientists, and drug development professionals. It explores the foundational challenges and consensus standards defining the field, details practical methodological approaches for integrating empirical and normative analysis, addresses common troubleshooting and optimization strategies for interdisciplinary work, and presents validation and comparative techniques for evaluating research quality. By synthesizing current evidence and established guidelines, this guide aims to enhance the design, conduct, and critical appraisal of empirical bioethics research within biomedical and clinical contexts.
Defining Rigor in Empirical Bioethics: Core Concepts and Consensus Standards
A fundamental challenge lies at the heart of empirical bioethics: the is-ought problem. First clearly articulated by the Scottish philosopher David Hume, this problem questions the logical validity of inferring prescriptive statements (about what ought to be) from purely descriptive, factual statements (about what is) [1]. Hume noted that authors of moral systems often make this leap imperceptibly, without explaining how these fundamentally different types of relations connect [1]. This creates a significant methodological challenge for empirical bioethics, a field that explicitly seeks to integrate empirical data from social science with normative ethical analysis to draw practical conclusions [2]. The problem is not merely academic; it strikes at the very validity of the field's conclusions. If normative claims cannot be logically derived from empirical observations, then the entire project of using patient preferences, clinical observations, or sociological data to inform ethical guidelines appears philosophically dubious. This guide compares how different methodological approaches within empirical bioethics attempt to bridge this divide, assessing their rigor and effectiveness in addressing this foundational challenge.
Methodological Frameworks for Integration
Philosophical Foundations and the Scope of the Challenge
The is-ought problem, also referred to as Hume's law or Hume's guillotine, posits that an ethical conclusion cannot be logically deduced from entirely non-ethical premises [1]. In modern research terms, this creates a gap between the empirical data collected about practices, attitudes, or experiences (the is) and the normative recommendations or ethical evaluations that bioethics seeks to produce (the ought). This gap is further complicated by what is known as the fact-value distinction in epistemology [1]. For bioethics researchers, this means that simply gathering robust data on, for example, how clinicians actually behave in difficult situations is not, in itself, sufficient to determine how they should behave. The challenge is to develop methodologies that can traverse this gap in a philosophically sound and methodologically rigorous manner.
Comparative Analysis of Key Methodological Approaches
Bioethics researchers have developed several innovative methodological frameworks to tackle this challenge. The table below provides a structured comparison of three prominent approaches, highlighting their core strategies for integration and their relative strengths and weaknesses.
| Methodological Approach | Core Integration Strategy | Key Strengths | Principal Weaknesses |
|---|---|---|---|
| Critical Interpretive Synthesis | Empirical data is used to critically interrogate and refine existing ethical concepts and theories, creating a new, empirically informed theoretical framework [2]. | Generates novel theoretical insights; avoids simply mapping data onto pre-existing categories; dynamic and iterative process [2]. | Can be theoretically complex; may be difficult to achieve transparency; requires high-level interpretive skill [2]. |
| Reflective Equilibrium | Seeks coherence between empirical data, ethical principles, and considered moral judgments through a process of continuous adjustment [2]. | Systematizes a process of moral justification familiar from everyday reasoning; allows for revision of principles in light of cases [2]. | Can be circular if not carefully practiced; may privilege certain intuitions; achieving equilibrium can be subjective [2]. |
| Procedure-Based Models | Uses structured deliberative procedures (e.g., expert panels, stakeholder dialogues) to interpret empirical findings and derive normative conclusions [2]. | Enhances legitimacy through participatory processes; makes the normative deliberation transparent and structured [2]. | Conclusions are only as good as the procedure itself; can be resource-intensive; risk of conflating consensus with correctness [2]. |
Experimental Protocols and Analytical Workflows
To ensure methodological rigor, researchers must carefully design their studies from inception to completion. The following workflow, formally outlined in consensus standards for empirical bioethics research, provides a structured pathway for integrating empirical and normative analysis [2]. This process is designed to make the bridging of the is-ought gap explicit, transparent, and systematic.
Detailed Protocol for Integrated Empirical-Normative Research
This protocol operationalizes the workflow above, providing concrete steps for researchers to follow.
Phase 1: Foundational Scoping & Question Formulation
- Step 1: Define an interdisciplinary aim that explicitly requires both empirical and normative components to answer [2]. The aim should explain why a mono-disciplinary approach is insufficient.
- Step 2: Formulate specific, interlinked empirical and normative research questions. Example: Empirical: "What are the lived experiences of patients in prolonged disorder of consciousness?" Normative: "What weight should patient biography, as narrated by families, hold in surrogate decision-making?" [2].
- Step 3: Select and justify a specific methodological framework for integration (e.g., from the comparison table above) that is appropriate for the research questions.
Phase 2: Interdisciplinary Conduct & Analysis
- Step 4: Conduct Empirical Work: Collect and analyze data using methods from social science (e.g., interviews, surveys, ethnography). Researchers must demonstrate methodological competence by adhering to established standards of rigor from the relevant empirical discipline (e.g., qualitative research trustworthiness criteria) [2].
- Step 5: Conduct Normative Analysis: Analyze the ethical issue using tools from moral philosophy (e.g., principle-based analysis, casuistry, virtue ethics). This must involve more than simply applying a pre-determined conclusion; it should be a robust analysis engaging with ethical theory and literature [2].
- Step 6: Integration: This is the crucial bridging phase. Apply the chosen methodological framework (e.g., Reflective Equilibrium, Critical Interpretive Synthesis) to interrelate the empirical findings and the normative analysis. This step must be made transparent, explaining how the data is informing the ethical evaluation and vice-versa [2].
Phase 3: Conclusion & Validation
- Step 7: Draw and articulate the normative conclusion, explicitly acknowledging the role the empirical data played in its formation and any limitations or constraints this places on the conclusion.
- Step 8: Disseminate findings in a way that is accessible to both empirical and normative disciplines and engage in critical reflection on the process itself, contributing to methodological advancement [2].
The Scientist's Toolkit: Essential Reagents for Rigorous Research
Successful navigation of the empirical-normative divide requires specific conceptual tools and methodological "reagents." The following table details key components necessary for conducting robust empirical bioethics research, as outlined in consensus standards [2].
| Research 'Reagent' | Function & Purpose | Application Example |
|---|---|---|
| Interdisciplinary Research Question | Forces the research to engage with both empirical and normative domains from the outset, preventing a mere "add-on" of one to the other [2]. | "How do neonatal intensive care unit staff conceptualize 'best interests' (empirical), and how should these conceptions inform a framework for resolving disagreements between staff and parents (normative)?" |
| Explicit Integration Framework | Provides the logical and methodological structure for combining empirical data and normative analysis, making the process transparent and defensible [2]. | Using the procedure of Reflective Equilibrium to adjust one's considered judgments about privacy in light of empirical data on public attitudes toward data sharing. |
| Transparent Normative Foundations | The ethical theories, principles, or concepts used in the analysis. Making them explicit allows for critical evaluation of the normative work [2]. | Stating that the analysis will employ a capabilities approach (as developed by Nussbaum and Sen) to evaluate the ethics of cognitive enhancement technologies. |
| Rigorously Generated Empirical Data | Data collected and analyzed according to the standards of the relevant social science discipline, ensuring the factual 'is' being incorporated is valid and reliable [2]. | Using thematic analysis with double-coding and consensus meetings to analyze interview transcripts about decision-making processes. |
| Deliberative Forum | A structured procedure (physical or virtual) that brings together diverse stakeholders to discuss and interpret the implications of empirical findings for normative questions [2]. | Convening a mixed panel of patients, clinicians, and ethicists to deliberate on the findings of a survey about the acceptability of novel genetic technologies. |
The is-ought gap remains a permanent feature of the philosophical landscape, but it is not an insurmountable barrier for empirical bioethics. As this guide has demonstrated, through the conscious application of rigorous methodological frameworks like Critical Interpretive Synthesis and Reflective Equilibrium, and by adhering to structured experimental protocols, researchers can build credible bridges across the divide. The validity of this interdisciplinary project no longer rests on claiming to have solved Hume's problem, but on transparently demonstrating how carefully gathered empirical evidence can inform and enrich robust normative reasoning. The future methodological rigor of the field depends on its practitioners continuing to refine these approaches, explicitly detailing their integrative strategies, and subjecting them to ongoing critical peer review.
Bioethics, since its emergence as a distinct field of inquiry, has been characterized by a fundamental tension: it addresses profoundly normative questions concerning life, health, and death, yet it does so by drawing upon a diverse array of disciplinary methods, from philosophy and law to sociology and empirical psychology. This inherent interdisciplinarity has fueled a long-standing debate about its very disciplinary status and, crucially, whether it possesses established, internal methodological rules [3]. While some refer to bioethics as a discipline in its own right, others label it a "field," "demi-discipline," or an "interdisciplinary" or "multidisciplinary" endeavor [3]. This terminological disagreement points to a more profound methodological uncertainty. The central challenge is that each discipline bioethics draws from—whether philosophy, medicine, or social science—comes with its own standard of rigor, its own criteria for determining valid and truthful results [3]. When these perspectives converge, as they must in bioethics, what constitutes methodological rigor? This question is not merely academic; it has serious implications for the legitimacy, authority, and practical impact of bioethical scholarship [3].
This article examines the ongoing discipline debate in bioethics by comparing the arguments for methodological plurality against the emerging consensus on standards of practice. It assesses the field's methodological rigor through the lens of a structured, comparative framework, presenting quantitative data on methodological trends and qualitative analysis of established protocols. By framing the discussion as a comparison between traditional philosophical inquiry and the rising paradigm of empirical bioethics, this guide provides researchers, scientists, and drug development professionals with a clear understanding of the methodological landscape and the tools to navigate it rigorously.
Comparative Analysis of Bioethics Methodological Frameworks
The table below summarizes the core positions in the debate regarding bioethics' methodological identity, highlighting the associated challenges and the evolving responses to them.
Table: Comparative Frameworks in the Bioethics Methodology Debate
| Framework | Core Tenets | Strengths | Weaknesses & Challenges |
|---|---|---|---|
| Traditional Philosophical Bioethics | Relies on classical philosophical methods: conceptual analysis, normative argumentation, and casuistry [4]. | Provides a strong foundation for normative reasoning and the development of ethical principles like autonomy and justice [4]. | Can be abstract; may lack grounding in the realities of clinical practice and stakeholder perspectives [4]. |
| Empirical Bioethics | Integrates data-driven research from social sciences (e.g., surveys, interviews) with ethical analysis to inform normative conclusions [4] [2]. | Grounds ethical reflection in actual practices, beliefs, and experiences, making it highly relevant to clinicians and patients [4]. | Faces the "is-ought" challenge; requires sophisticated methods for integrating descriptive data with normative reasoning [4] [2]. |
| Experimental Bioethics ("Bioxphi") | A subdiscipline using experiment-based designs from cognitive sciences (psychology, neuroscience) to understand how and why stakeholders make moral judgments [5]. | Offers high internal rigor and can reveal cognitive biases and psychological mechanisms underlying moral intuitions [5]. | Findings may be context-specific; the path from psychological findings to normative conclusions remains complex [5]. |
| The "Consensus" Movement | Seeks to establish agreed-upon Standards of Practice for empirical bioethics to ensure quality and rigor [2]. | Addresses the "quality crisis" directly; provides concrete guidance for researchers, funders, and journals [2]. | May be perceived as overly rigid; consensus is difficult to achieve in a fundamentally interdisciplinary field [2]. |
The Implications of Methodological Pluralism
The lack of a single, unifying methodology has spawned several significant challenges that undermine the field's credibility and effectiveness [3]:
- Theoretical & Epistemological Challenges: There are no clear, universally accepted standards for assessing competing normative conclusions derived from different methodological starting points [3].
- Peer Review Challenges: The criteria for "good scholarship"—originality, quality, validity—are interpreted differently across disciplines, creating inconsistency and confusion in the review process for bioethics journals [3].
- Sociological & Authority Challenges: The absence of agreed-upon standards can undermine the claims to authority, credibility, and legitimacy of bioethics researchers, particularly in the public sphere [3].
- Clinical Decision-Making Challenges: In healthcare settings, the lack of a clear framework for balancing different disciplinary perspectives can hinder effective and justified ethical decision-making [3].
- Institutional & Pedagogical Challenges: Uncertainty about the field's core methods complicates curriculum development, bioethics education, and its place within university structures [3].
Established Methodological Rules: The Emergence of Standards
In response to these challenges, significant efforts have been made to formalize methodological rules, particularly within the domain of empirical bioethics. A key consensus project, which utilized a modified Delphi process with 16 academics from five European countries, successfully established 15 standards of practice for empirical bioethics research. These standards are organized into six domains, providing a concrete framework for assessing methodological rigor [2].
Table: Consensus Standards for Empirical Bioethics Research
| Domain | Description of Standards |
|---|---|
| Aims | Research must clearly articulate its aims and the specific bioethical problem it addresses [2]. |
| Questions | The research questions must be framed to require both empirical and normative analysis for their answer [2]. |
| Integration | The methodology must explicitly describe and justify how the empirical and normative components will be integrated throughout the research process, rather than being merely juxtaposed [2]. |
| Conduct of Empirical Work | The empirical work must be designed, conducted, and reported according to the established quality criteria of the relevant social scientific discipline (e.g., qualitative or quantitative research standards) [2]. |
| Conduct of Normative Work | The normative analysis must be conducted and reported according to recognized standards of philosophical or ethical rigor, with transparent reasoning and engagement with relevant ethical theories and concepts [2]. |
| Training & Expertise | The research team must possess, or have access to, adequate expertise in both the empirical methods and the normative analysis required for the project [2]. |
This consensus represents a major step towards disciplining the field. It provides journals, funders, and researchers with a shared set of expectations, addressing the peer review and legitimacy challenges head-on. The standards emphasize that rigor in empirical bioethics is not just about doing good empirical work or good normative work, but about systematically integrating the two [2].
A Hierarchical Model for Empirical Research
Further structuring the empirical turn, one proposed framework classifies empirical research in bioethics into four hierarchical categories, each building upon the last [4]. This model provides a clear "experimental protocol" for designing and categorizing studies.
Diagram: The Hierarchical Progression of Empirical Bioethics Research
- Level 1: Lay of the Land - This foundational research describes current practices, opinions, or beliefs. Examples include surveys of what patients want in end-of-life care or studies examining the composition of hospital ethics committees [4].
- Level 2: Ideal Versus Reality - This research starts with an accepted ethical norm (e.g., "informed consent must be comprehended by research subjects") and tests whether reality aligns with this ideal. The vast body of work on racial disparities in healthcare is a prime example of this category [4].
- Level 3: Improving Care - Studies at this level develop and assess interventions to bring clinical practice closer to ethical ideals, such as testing a new communication tool to improve the informed consent process [4].
- Level 4: Changing Ethical Norms - The highest level of work, which synthesizes data from multiple empirical studies to inform, challenge, and potentially revise our ethical norms and principles [4].
The Scientist's Toolkit: Essential Methodological Reagents
For researchers embarking on a bioethics project, the following "reagents"—core methodological components and documents—are essential for ensuring rigor and ethical compliance.
Table: Essential Research Reagents for Methodologically Rigorous Bioethics
| Research Reagent | Function & Role in Ensuring Rigor |
|---|---|
| Study Protocol | Serves as the comprehensive blueprint for the study, detailing objectives, design, methodology, and statistical considerations. It is the foundational document for ethical and scientific review [6]. |
| Informed Consent Form (ICF) | The primary tool for upholding the ethical principle of autonomy. It must provide all necessary information in plain language, allowing potential participants to make a fully informed decision [6]. |
| Data Collection Tool (e.g., CRF) | A standardized tool, like a Case Report Form (CRF), ensures consistent, accurate, and unambiguous data collection across all study participants, which is crucial for data integrity [6]. |
| Integration Methodology | The explicit, pre-defined plan for how the empirical (descriptive) and normative (prescriptive) components of the research will be combined to produce coherent, justified conclusions [2]. |
| Ethics Committee (IRB/REC) Approval | Formal approval from a Research Ethics Committee (REC) or Institutional Review Board (IRB) is mandatory. It confirms that the study design respects participant rights, safety, and well-being [7]. |
The Global Ethics Review Landscape
For international research, understanding the variability in ethics review processes is a critical aspect of methodological rigor. A recent 2025 study of 17 countries highlights significant heterogeneity in the timelines and requirements for ethical approval, which can impact the feasibility of collaborative studies [7]. The following workflow visualizes the complex, multi-stage process researchers may face.
Diagram: Workflow for Navigating International Ethical Review
The quantitative data from this study reveals substantial disparities. For example, while some countries require formal ethical approval for all study types, others, like the UK and Slovakia, may waive this for audits or non-interventional studies. Timelines for approval also vary dramatically, from 1-3 months in many regions to over 6 months in countries like Belgium and the UK for interventional studies [7]. This variability underscores the importance of the "Determine Local Ethics Requirements" reagent in the scientist's toolkit.
The debate over whether bioethics has established methodological rules does not yield a simple "yes" or "no" answer. The evidence points to a field that is actively and successfully disciplining itself. While bioethics may never be a monolithic discipline with a single, unified method, the development of consensus standards [2] and the widespread adoption of structured frameworks for empirical research [4] demonstrate a clear trajectory toward methodological maturation.
The core strength of bioethics—its interdisciplinarity—is also the source of its greatest challenge. However, the emergence of explicit standards for integration, rigorous empirical work, and sound normative analysis provides a robust response to critiques about a lack of rigor. For researchers, scientists, and professionals in drug development, this means that conducting rigorous bioethics research is entirely possible, provided it is guided by these emerging rules. The methodology is no longer purely aspirational; it is increasingly concrete, demanding, and essential for producing scholarship that can legitimately claim to inform both policy and practice. The discipline debate is thus being resolved not through declaration, but through the progressive, collective establishment of methodological rules that honor the field's complex heritage while ensuring its scientific and ethical credibility.
Assessing Methodological Rigor in Empirical Bioethics Research
Empirical bioethics is an interdisciplinary field that integrates social scientific research with ethical analysis to arrive at normative conclusions. For years, the field has been characterized by a "broad variety of methodologies," which, while innovative, has made it challenging to present, defend, or critically assess the quality of research work [2]. The absence of a clear, agreed-upon standard of rigor poses serious threats to the field, undermining claims to authority, credibility, and legitimacy, and creating challenges for peer review and practical decision-making [3]. In response to these challenges, a group of 16 academics from five European countries convened at the Brocher Foundation in May 2015 with a specific goal: to generate and reach a consensus on standards of practice for empirical bioethics research [2] [8]. Through a modified Delphi process, this group established 15 standards of practice, organized into 6 domains, providing a critical framework for assessing methodological rigor [2]. This guide objectively compares this emerging consensus standard against the prior state of the field, providing researchers, scientists, and drug development professionals with the tools to implement rigorous empirical bioethics in their work.
The Experimental Protocol: Forging Consensus through a Modified Delphi Method
The development of the 15 standards was itself a rigorous scholarly exercise designed to build consensus among experts with diverse disciplinary backgrounds.
- Research Question: The primary aim was to establish a consensus on the core characteristics of empirical bioethics and to define minimum standards for methodological quality in its design, conduct, and reporting [2].
- Participant Selection: The process involved 16 academics from 5 different European countries, who were purposively selected to represent a range of disciplinary backgrounds and putatively opposing positions within empirical bioethics [2] [8]. This diversity was crucial for ensuring the resulting standards would be robust and widely applicable.
- Consensus Process: The team utilized a modified Delphi approach [2] [8] [9]. The classic Delphi method involves multiple rounds of anonymous questionnaires where panelists reassess their judgments based on summarized group feedback. The modification for this project involved replacing iterative questionnaires with structured group discussions, allowing for immediate clarification of ambiguous or controversial issues—a necessary adaptation given the linguistic and conceptual diversity of the participants [2].
- Outcome Measure: The explicit goal was to generate a set of standards precise enough to provide concrete guidance. Consensus was successfully reached on 15 individual standards, which were then logically grouped into 6 overarching domains of research practice [2].
The following diagram illustrates the structured process used to develop the consensus.
Comparative Analysis: The Brocher Consensus vs. The Pre-Consensus Landscape
The Brocher Consensus can be understood as a direct response to the methodological challenges that plagued the earlier development of empirical bioethics. The table below provides a point-by-point comparison of the research landscape before and after the formulation of these standards.
| Dimension of Comparison | Pre-Consensus Landscape | The Brocher Consensus Framework |
|---|---|---|
| Defining Rigor | No agreed-upon standard of rigor; criteria for truth and validity varied by contributor's home discipline [3]. | Establishes a shared framework for rigor across 6 domains, providing external validation for interdisciplinary work [2]. |
| Methodological Justification | Researchers had to justify every methodological choice "from first principles," a process that was lengthy and difficult [2]. | Provides legitimate starting points and agreed-upon assumptions, streamlining justification for funding and publication [2]. |
| Peer Review | Challenging due to reviewers applying different disciplinary norms; terms like "validity" interpreted inconsistently [3]. | Offers a common benchmark for journals and funders to assess quality, making peer review more consistent and fair [2]. |
| Interdisciplinary Integration | A known challenge with dozens of proposed methodologies, but no consensus on how to validly integrate empirical and normative work [2] [3]. | Makes integration a central domain, requiring researchers to explicitly justify how the empirical and normative parts of their work relate [2]. |
| Training & Expertise | Unclear what skills were essential for a bioethics researcher, leading to potential gaps in training [3]. | Explicitly addresses the need for appropriate training and expertise in both empirical and normative methods [2] [8]. |
The Researcher's Toolkit: Essential Components for Empirical Bioethics
Executing methodologically rigorous empirical bioethics research requires a suite of conceptual and practical tools. The following table details key "research reagent solutions" essential for this field.
| Tool / Component | Function in Empirical Bioethics Research |
|---|---|
| Modified Delphi Method | A structured communication technique used to achieve consensus among a panel of experts through iterative rounds of discussion and feedback [2]. |
| Explicit Normative Framework | The philosophical or ethical theory (e.g., principlism, consequentialism) that provides the foundation for the normative analysis in the research [2]. |
| Rigorously Designed Empirical Protocol | The detailed methodology for the empirical component (e.g., qualitative interviews, surveys), ensuring social scientific rigor and trustworthiness of the data [2] [4]. |
| Documented Integration Strategy | The clearly articulated procedure for combining empirical findings with normative reasoning, which is the defining core of empirical bioethics [2]. |
| Interdisciplinary Research Team | A collaboration of investigators with complementary expertise in both normative disciplines (e.g., philosophy, law) and empirical disciplines (e.g., sociology, epidemiology) [2] [3]. |
The Empirical-Normative Workflow in Action
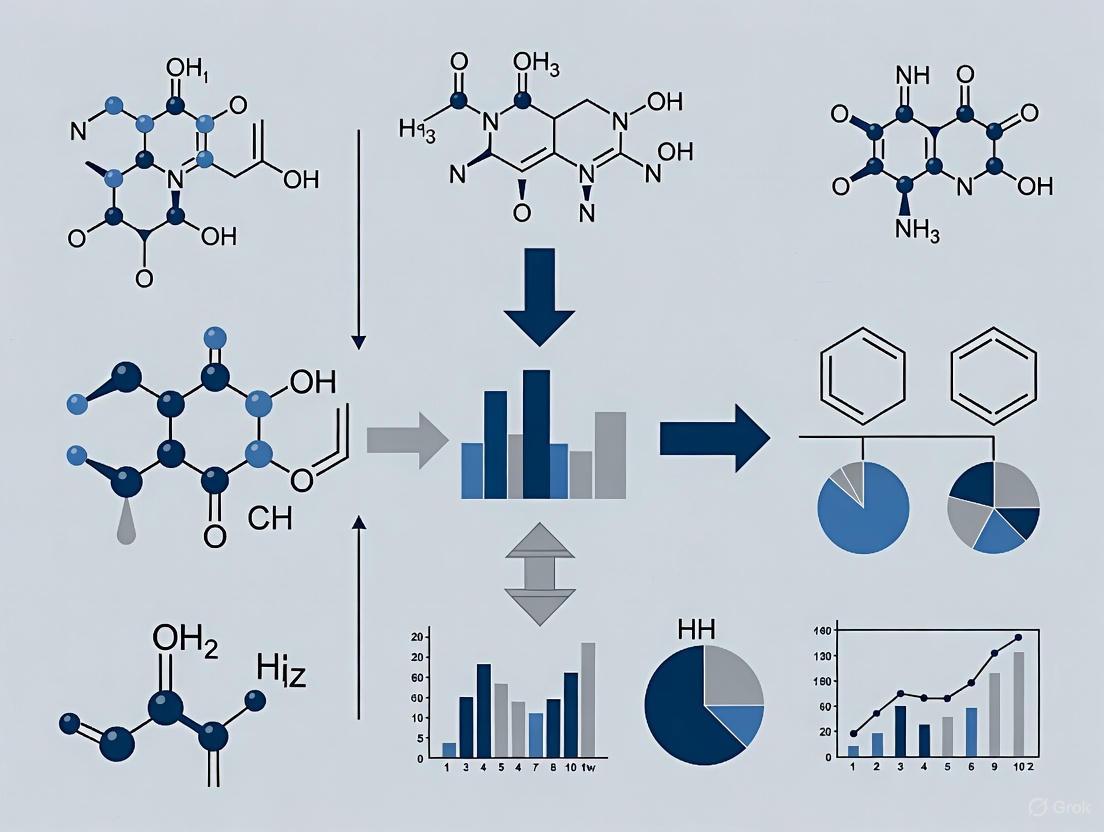
A core innovation of the Brocher Consensus is its emphasis on the integration of empirical and normative work. The following diagram maps the logical workflow of a rigorous empirical bioethics project, from its inception to its conclusion, highlighting how these two streams of inquiry interact.
This workflow demonstrates that empirical bioethics is not a simple linear process where data collection merely "informs" ethics. Instead, it is an integrative and often iterative practice where empirical findings and normative analysis are in constant dialogue [2] [4]. The "Integration Process" is the crucial, active component where researchers synthesize the two strands, using methods such as dialectical reflection or case-based reasoning to arrive at justified normative conclusions.
The Brocher Foundation Consensus on 15 standards across 6 domains represents a pivotal achievement in the maturation of empirical bioethics. By moving the field from a state of methodological heterogeneity and contested rigor to one with a shared framework for quality, it directly addresses fundamental challenges related to credibility, peer review, and training [2] [3]. For researchers, scientists, and professionals in drug development, engaging with these standards is no longer optional but essential for producing work that can withstand interdisciplinary scrutiny. The consensus is not a final word but an invitation for the community of practice to "develop and evolve further" [2]. The continued adoption and critical engagement with these standards by researchers, funders, and journals will be the ultimate measure of their success in strengthening the methodological rigor of bioethics research.
Empirical bioethics represents an innovative, interdisciplinary field that integrates empirical social scientific research with normative ethical analysis to address complex problems in medicine and the life sciences. This integration aims to ground ethical recommendations in the realities of clinical practice and stakeholder experiences while maintaining philosophical rigor. However, this interdisciplinary nature presents significant methodological challenges, primarily concerning how to establish and maintain rigor when combining descriptive (empirical) and normative (ethical) approaches [3]. The field has been described as both exciting and frustrating—"exciting, because it potentially 'promises a great deal', but also frustrating 'because the emerging field threatens to be so multifarious and vague that making sense of it is a challenge for even the most seasoned researcher'" [10]. This guide objectively compares emerging frameworks and standards designed to enhance methodological rigor in empirical bioethics research, providing researchers with evidence-based guidance for conducting and evaluating quality in this complex field.
The fundamental challenge stems from what theorists identify as the "is-ought problem"—the philosophical challenge of deriving normative 'ought' claims from empirical 'is' data [10]. Without clear standards, bioethics research faces five serious practical challenges: (1) no clear standards for answering bioethical questions, (2) problems for peer review processes, (3) undermined claims to authority and legitimacy, (4) difficulties in clinical decision-making, and (5) questions about its proper institutional setting [3]. This comparison guide examines how current methodological frameworks address these challenges through formal, cognitive, and ethical norms.
Comparative Analysis of Quality Criteria Frameworks
Established Standards and Consensus Approaches
A significant development in empirical bioethics methodology emerged from a consensus project involving 16 academics from five European countries using a modified Delphi approach. This project established 15 discrete standards of practice organized into six domains, creating a comprehensive framework for methodological rigor [10].
Table 1: Consensus Standards for Empirical Bioethics Research
| Domain | Number of Standards | Focus Areas |
|---|---|---|
| Aims | Not specified | Clarifying research purposes and interdisciplinary goals |
| Questions | Not specified | Formulating research questions amenable to integration |
| Integration | Not specified | Methodological approaches for combining empirical and normative elements |
| Conduct of Empirical Work | Not specified | Application of appropriate social science methods |
| Conduct of Normative Work | Not specified | Application of appropriate ethical analysis methods |
| Training & Expertise | Not specified | Ensuring researcher competence across disciplines |
The consensus approach argues that establishing agreed-upon standards helps cement empirical bioethics as a distinct 'community of practice' with specific methodological norms, which in turn improves research quality, provides guidance for training, and offers validation for methodological choices during peer review of publications and grant applications [10]. Proponents note that these standards are particularly valuable in an interdisciplinary field where "there is no standard approach to cite, there is no accepted methodology or set of methods to fall back on" [10].
The "Road Map" Framework for Interdisciplinary Research
An alternative but complementary approach has been proposed by Mertz and colleagues, who developed what they term a "road map" for quality criteria in empirical ethics research [11]. This framework organizes criteria into five key domains, presented as reflective questions to guide researchers:
Table 2: Road Map Quality Criteria Framework
| Domain | Key Focus | Sample Reflective Questions |
|---|---|---|
| Primary Research Question | Appropriate scope and interdisciplinary nature | Does the question require both empirical and normative analysis? |
| Theoretical Framework & Methods | Coherent methodological integration | Are empirical methods adequate? Are normative approaches justified? |
| Relevance | Practical significance and impact | Does the research address a pressing ethical problem? |
| Interdisciplinary Research Practice | Collaborative team composition | Does the team have appropriate interdisciplinary expertise? |
| Research Ethics & Scientific Ethos | Ethical conduct of the research itself | Are standard ethical principles for research being followed? |
This framework emphasizes that poor methodology in empirical ethics "results in misleading ethical analyses, evaluations or recommendations" which "not only deprives the study of scientific and social value, but also risks ethical misjudgement" [11]. The road map approach is presented as a heuristic tool to provoke systematic reflection during research planning and composition, positioning quality assurance as an ethical imperative in itself.
Distinguishing Norm Types in Research Practice
Theoretical work on norms provides essential context for understanding different categories of standards applicable to empirical bioethics. Research in cognitive psychology distinguishes between constitutive norms (which define what a practice is) and regulative norms (which guide how the practice should be conducted) [12].
Table 3: Norm Types in Empirical Bioethics Research
| Norm Type | Definition | Research Application |
|---|---|---|
| Formal Norms | Standards for research writing and dissemination | Reporting standards, publication formats, structural requirements |
| Cognitive Norms | Methodological commitments and analytical approaches | Criteria for valid inference, appropriate methods, analytical rigor |
| Ethical Norms | Moral conduct of research activities | Participant protection, integrity in analysis, responsible reporting |
This distinction helps clarify that methodological rigor in empirical bioethics requires attention to multiple dimensions of quality simultaneously. Formal norms ensure proper research reporting, cognitive norms guarantee the intellectual integrity of the approach, and ethical norms safeguard the moral dimensions of the research process [11]. The psychology of normative cognition suggests that humans develop specialized cognitive mechanisms for learning, complying with, and enforcing norms—a capacity that underpins the methodological standardization now emerging in empirical bioethics [13].
Experimental Protocols and Methodological Implementation
Consensus Development Methodology
The 15-standards framework was developed using a modified Delphi approach that adapted traditional consensus methods to address the conceptual diversity of empirical bioethics [10]. The methodological protocol involved:
- Participant Selection: 16 academics from 5 European countries with diverse disciplinary backgrounds were purposively selected to represent different and potentially opposing positions in empirical bioethics.
- Process Adaptation: Instead of multiple iterative questionnaires typical of Delphi methods, the process used iterative discussion groups with regular feedback sessions.
- Rationale for Adaptation: The modification was justified by "the pressing need to have clear and robust direct verbal communication through discussion that allowed disagreements to be aired and mutually understood" [10].
- Consensus Validation: The process sought to generate standards "precise enough to provide concrete guidance for (a) identifying the core characteristics of empirical bioethics, (b) planning empirical bioethics, (c) conducting empirical bioethics, and (d) reporting empirical bioethics" [10].
This methodological approach recognized that linguistic and conceptual diversity in the field made questionnaire-based approaches problematic, requiring instead a process that allowed immediate clarification of ambiguous or controversial issues.
Implementation Evaluation Methodology
A different methodological approach was used to evaluate how ethical recommendations are translated into practice, employing a cross-sectional mapping study of 400 recent publications from four bioethics journals [14]. The experimental protocol included:
- Sample Identification: The latest 100 publications from each of four bioethics journals (Journal of Medical Ethics, Nursing Ethics, AJOB Empirical Bioethics, BMC Medical Ethics) were identified through PubMed searches.
- Categorization Framework: Publications were categorized as (1) evaluative empirical research (assessing implementation of ethical recommendations), (2) non-evaluative empirical research, or (3) borderline cases using predefined criteria.
- Analysis Method: For evaluative studies, researchers analyzed which types of norms or recommendations were being evaluated, using a framework that distinguished between aspirational norms, specific norms, and best practices.
- Inter-rater Reliability: Screening and categorization were performed independently by two reviewers with disagreements resolved by consensus, and interrater agreement was measured on a random subsample using Cohen's kappa.
This methodology revealed that among recent empirical bioethics publications, 36% (84 of 234 included studies) constituted evaluative empirical research, while 54% were non-evaluative empirical studies, and 10% were borderline cases [14]. This provides quantitative evidence about current research practices and the relative emphasis on different types of empirical approaches in the field.
Visualization of Methodological Integration
The following diagram illustrates the integrated relationship between different norm types and research components in empirical bioethics, showing how quality criteria interact across the research lifecycle:
Diagram 1: Integration of Norm Types in Research
Successful empirical bioethics research requires specific methodological competencies and resources. The following table details essential components of the empirical bioethics research toolkit:
Table 4: Research Reagent Solutions for Empirical Bioethics
| Tool Category | Specific Methods/Approaches | Function in Research Process |
|---|---|---|
| Empirical Data Collection | Qualitative interviews, focus groups, surveys, observational studies, systematic reviews | Generates robust empirical data about ethical issues in practice |
| Normative Analysis Frameworks | Principlism, casuistry, consequentialist analysis, deontological approaches, virtue ethics | Provides structured methods for ethical analysis and argument development |
| Integration Methodologies | Reflective equilibrium, symbiotic ethics, triangulation approaches, iterative integration | Bridges empirical findings and normative reasoning |
| Interdisciplinary Collaboration Structures | Mixed teams, cross-disciplinary supervision, integrated project designs | Facilitates genuine interdisciplinary exchange and expertise sharing |
| Quality Assessment Tools | Consensus standards, road map criteria, reporting guidelines | Ensures methodological rigor across all research phases |
Each component addresses specific methodological challenges in empirical bioethics. For example, integration methodologies specifically target the fundamental "is-ought" challenge by providing systematic approaches to combining descriptive and normative elements [10] [11]. The toolkit metaphor emphasizes that successful research requires selecting appropriate methodological "reagents" for the specific research question at hand, much as laboratory scientists select appropriate physical reagents for their experiments.
This comparison of frameworks demonstrates significant progress in establishing methodological standards for empirical bioethics research. The consensus-based 15-standards approach and the reflective road map criteria represent complementary strategies for enhancing quality—the former providing specific benchmarks, the latter offering heuristic guidance for research planning and execution. Quantitative evidence shows that evaluative empirical research constitutes a substantial minority (36%) of current empirical bioethics publications, indicating growing attention to how ethical recommendations translate into practice [14].
The distinction between formal, cognitive, and ethical norms provides a valuable conceptual framework for understanding different dimensions of quality in interdisciplinary bioethics research. By adopting these emerging standards and frameworks, researchers can address fundamental challenges to the field's credibility while enhancing the practical impact and scholarly excellence of their work. Future methodological development should focus on validating and refining these criteria across diverse research contexts while maintaining the productive tension between empirical and normative approaches that defines this innovative field.
Empirical bioethics is navigating a critical juncture in its development as a field. Born from the necessity to address complex societal challenges posed by advances in life sciences and biotechnology, bioethics has increasingly embraced interdisciplinary approaches over the past quarter-century [15]. This evolution from traditional single-discipline methodologies toward integrative frameworks represents a fundamental shift in how bioethical inquiry is structured and validated. The growing recognition that ethical decision-making in healthcare requires multiple perspectives has fueled this transformation, moving the field beyond the limitations of traditional disciplinary boundaries [3].
The central challenge facing contemporary bioethics lies in establishing itself as a distinct community of practice while navigating its inherently interdisciplinary nature. Disciplines are characterized partly by their methods and standards of rigor, but when bioethics research draws on diverse methods from philosophy, law, medicine, theology, sociology, and other fields, determining what constitutes rigor becomes complex [3]. This methodological pluralism has led to significant disagreement about bioethics' disciplinary status—variously described as a discipline, applied discipline, multidisciplinary endeavor, interdisciplinary field, or simply a field of study [3]. This terminology debate reflects deeper uncertainties about the methods and standards that should govern bioethical inquiry and how various disciplinary perspectives can be integrated to produce valid, reliable normative conclusions.
Comparative Analysis of Interdisciplinary Approaches
The bioethics landscape encompasses several distinct models of interdisciplinary practice, each with characteristic methodologies, strengths, and limitations. The table below provides a systematic comparison of these primary approaches.
Table 1: Comparative Analysis of Interdisciplinary Approaches in Bioethics
| Approach | Definition | Key Characteristics | Strengths | Limitations |
|---|---|---|---|---|
| Critical Interdisciplinarity | Exemplified by the Nuffield Council, focuses on autonomous ethical inquiry and problematizing foundational assumptions [15] | Develops public-facing "non-expert discourse of experts"; emphasizes situated reflection [15] | Challenges disciplinary biases; fosters novel insights | Difficulties deriving positive normative conclusions; challenges generalizing from situated contexts [15] |
| Integrated Empirical Bioethics | Systematic integration of empirical social scientific analysis with ethical analysis to draw normative conclusions [2] | Explicit methodology for combining empirical and normative elements; transparent about integration process [2] | Grounds normative conclusions in empirical reality; enhances practical relevance | Faces "is-ought" challenge; requires sophisticated methodological expertise [2] |
| Multidisciplinary | Multiple disciplines work side-by-side without significant integration [3] | Additive rather than integrative; maintains disciplinary boundaries | Respects disciplinary standards; easier to evaluate by traditional criteria | Limited synthesis; potential for fragmented conclusions [3] |
| Anticipatory Bioethics | Focuses on ethical analysis of emerging technologies before widespread implementation [16] | Future-oriented; attempts to inform technology development proactively [16] | Potential for practical impact before technological lock-in; addresses timing challenges | Risk of speculation; limited empirical evidence for validation [16] |
Methodological Rigor: Protocols and Standards
Consensus Standards for Empirical Bioethics Research
A significant development in establishing methodological rigor is the emergence of consensus standards for empirical bioethics research. Through a modified Delphi process involving 16 academics from five European countries, researchers have identified 15 standards of practice organized into six domains [2]. These standards provide a framework for ensuring quality and rigor in interdisciplinary bioethics research.
Table 2: Domains and Standards for Empirical Bioethics Research
| Domain | Key Standards | Practical Applications |
|---|---|---|
| Aims | Clear statement of research aims and purpose of empirical component [2] | Explicit justification for interdisciplinary approach; definition of target outcomes |
| Questions | Formulation of research questions requiring both empirical and normative analysis [2] | Questions that cannot be adequately addressed within single disciplines |
| Integration | Transparent description of how empirical and normative elements are connected [2] | Methodological clarity about integration process; justification for chosen approach |
| Conduct of Empirical Work | Appropriate application of social science methods; reflection on limitations [2] | Rigorous data collection and analysis; awareness of disciplinary norms |
| Conduct of Normative Work | Transparent normative framework; clear justification for normative claims [2] | Philosophical rigor; acknowledgement of value premises |
| Training & Expertise | Research team possesses appropriate combination of empirical and normative expertise [2] | Collaborative teams with complementary skills; interdisciplinary training |
Experimental Protocols for Interdisciplinary Integration
Several specific methodological protocols have been developed to facilitate rigorous integration of disciplinary perspectives in bioethics research:
The Dialogue Method: This approach structures facilitated discussions between stakeholders from different disciplinary backgrounds, creating what has been described as "akin to a philosophy seminar" [2]. The protocol involves: (1) identification of relevant disciplinary perspectives and stakeholders; (2) structured dialogue sessions with explicit methodological rules; (3) iterative development of ethical frameworks; (4) validation through application to specific cases. This method transforms standard data collection techniques like focus groups into more interrogative and challenging forums suitable for ethical analysis.
Systematic Integration Methodology: Developed to address the challenge of deriving normative conclusions from empirical data, this protocol includes: (1) parallel empirical and normative analysis; (2) identification of points of convergence and divergence; (3) development of integrated conclusions through iterative reflection; (4) transparency about limitations in the integration process [2]. This methodology explicitly addresses the "is-ought" challenge that often troubles interdisciplinary bioethics research.
Validation Framework for Anticipatory Bioethics: Specifically designed for analyzing emerging technologies, this protocol involves: (1) explicit clarification of implicit assumptions; (2) validation of assumptions through evidence from interdisciplinary scholarly literature; (3) broad perspective analysis to contextualize findings; (4) systematic assessment of potential impacts and ethical implications [16]. This framework aims to enhance methodological rigor in future-oriented bioethical analysis.
Visualization of Interdisciplinary Processes
The following diagram illustrates the conceptual framework and workflow for interdisciplinary integration in bioethics research, mapping the relationship between different elements and processes:
Successful interdisciplinary work in bioethics requires specific methodological resources and competencies. The table below outlines essential components of the interdisciplinary bioethics toolkit.
Table 3: Essential Methodological Resources for Interdisciplinary Bioethics
| Tool Category | Specific Tools/Methods | Function/Purpose |
|---|---|---|
| Empirical Methods | Qualitative interviews, focus groups, surveys, ethnographic observation [2] | Generate data about stakeholder perspectives, practices, and contexts |
| Normative Analysis Frameworks | Principle-based approaches, casuistry, virtue ethics, consequentialist analysis [2] | Provide structured methods for ethical analysis and justification |
| Integration Methodologies | Dialogical methods, reflective equilibrium, embedded research models [2] | Facilitate combination of empirical and normative elements |
| Quality Assessment Tools | Consensus standards, peer review protocols, validation frameworks [2] | Ensure methodological rigor and appropriate application of methods |
| Interdisciplinary Communication Aids | Conceptual clarification protocols, terminology guides [17] | Bridge disciplinary language and conceptual differences |
Institutional Models and Global Variations
Exemplary Institutional Approaches
Several institutions have developed distinctive models for fostering interdisciplinary bioethics practice:
The Nuffield Council on Bioethics exemplifies the model of critical interdisciplinarity, emphasizing autonomous ethical inquiry that problematizes foundational assumptions rather than taking them as given [15]. This approach has developed a public-facing "non-expert discourse of experts" that makes complex ethical discussions accessible while maintaining scholarly rigor. The Council's methodology involves situating ethical reflection in specific contexts while grappling with the challenge of deriving positive normative conclusions from this situated approach [15].
Yale Interdisciplinary Center for Bioethics adopts a comprehensive approach that extends beyond biomedical ethics to include environmental ethics, animal ethics, scientific research ethics, business ethics, and emerging technologies [18]. Their model combines academic research with practical engagement through institutional review boards and hospital ethics committees, creating bridges between theoretical reflection and practical application.
University of Toronto's Interdisciplinary Bioethics Working Group brings together healthcare practitioners, academic philosophers, clinical ethicists, students, and resident physicians to address fundamental questions about what "doing bioethics" means across different professional contexts [17]. This model explicitly tackles communication gaps between groups with different assumptions about bioethics' purpose and methods.
Global Variations in Ethical Review Processes
The institutionalization of bioethics is reflected in global variations in research ethics review processes. A recent study of 17 countries revealed significant heterogeneity in ethical approval requirements and timelines, illustrating how interdisciplinary bioethics interfaces with regulatory frameworks [7]. For example, while European countries like Belgium and the UK have processes described as particularly arduous (often exceeding six months for interventional studies), countries like Vietnam and Hong Kong have streamlined mechanisms for certain study types [7]. These variations present both challenges and opportunities for interdisciplinary bioethics operating in international contexts.
Challenges and Future Directions
Persistent Methodological Challenges
Despite progress in developing interdisciplinary methodologies, bioethics continues to face several persistent challenges:
The Rigor Challenge: The absence of clear, universally accepted standards for answering bioethical questions remains problematic [3]. With researchers from different disciplinary backgrounds applying different methods and having different goals, determining how to assess normative conclusions is complex. This challenge affects practical decision-making in clinical settings, where integrating various disciplinary perspectives continues to be difficult [3].
The Legitimacy Challenge: The lack of clarity regarding disciplinary status and standards of rigor undermines bioethics researchers' "claims to authority, credibility and legitimacy" [3]. Without agreed-upon criteria for determining valid knowledge, the field's influence on policy and practice may be limited.
The Integration Challenge: Effectively integrating diverse disciplinary perspectives remains methodologically difficult. Each discipline brings its own standards of rigor, methodological approaches, and epistemological assumptions, creating challenges for generating coherent, defensible conclusions [3].
Future Directions for Interdisciplinary Bioethics
The future development of bioethics as a distinct community of practice will likely focus on several key areas:
Methodological Consolidation: There is growing momentum toward developing more precise methodological standards for interdisciplinary work, particularly regarding how empirical and normative elements should be integrated [2]. This includes clearer frameworks for validating interdisciplinary approaches and assessing the quality of resulting research.
Enhanced Training Models: As the field matures, developing more sophisticated training approaches that equip researchers with both empirical and normative competencies becomes increasingly important [2]. This includes creating pathways for developing "dual expertise" or fostering more effective collaborative models.
Global Engagement: Bioethics is increasingly developing frameworks for globally resonant ethics that can guide powerful scientific developments while respecting cultural and contextual variations [15]. This involves navigating tensions between universal ethical principles and culturally situated values.
Anticipatory Methodology: There is growing emphasis on strengthening methodological rigor in anticipatory bioethics to distinguish it from mere speculation while maintaining its future-oriented, proactive character [16]. This includes developing better evidence-based approaches to analyzing emerging technologies.
Interdisciplinarity has transformed bioethics from a theoretical subfield into a distinct community of practice with its own methodological approaches, standards of rigor, and institutional structures. While challenges remain in fully integrating diverse disciplinary perspectives and establishing universally accepted standards of quality, the field has made significant progress in developing frameworks for rigorous interdisciplinary inquiry. The consolidation of methodological standards, exemplified by the consensus around empirical bioethics practices, represents a crucial step in bioethics' maturation as a field capable of addressing complex ethical challenges in healthcare and biotechnology.
As bioethics continues to evolve, its future as a distinct community of practice will depend on maintaining its commitment to methodological rigor while remaining adaptable to new challenges and responsive to the needs of multiple stakeholders. By embracing its interdisciplinary character while continuing to develop its unique methodological identity, bioethics can strengthen its contribution to both scholarly discourse and practical decision-making in increasingly complex biomedical contexts.
Implementing Methodological Frameworks: From Theory to Practice
In the rigorous field of bioethics, the selection of appropriate research methodologies is paramount for generating robust, credible, and actionable knowledge. The scholarly landscape is broadly divided into two methodological paradigms: empirical research, which is grounded in observed and measured phenomena, and non-empirical research, which derives knowledge from theoretical analysis, argumentation, and the synthesis of existing work [19] [20]. Empirical research answers questions about "how the world is" through direct experience, relying on concrete, verifiable evidence gathered via observation or experimentation [19]. Its origins trace back to ancient Greek practitioners who shifted from dogmatic principles to dependence on observed phenomena, with the term "empirical" stemming from the Greek "empeirikos," meaning "experienced" [19].
Conversely, non-empirical research does not involve the firsthand collection of data [20]. Instead, it analyzes and summarizes existing research, theories, and beliefs to advance conceptual understanding, critique ethical frameworks, or develop normative positions. In bioethics, this often takes the form of philosophical inquiry, theoretical essays, and literature reviews. The tension and potential for synergy between these approaches form a central theme in contemporary bioethics, raising critical questions about how the "is" of empirical observation can inform the "ought" of normative ethics [4]. This guide provides a structured comparison of these approaches, offering researchers a framework for assessing methodological rigor and selecting the optimal path for their investigative objectives.
Comparative Analysis: Core Characteristics and Applications
Empirical Research: Measurement and Observation
Empirical research is defined by its exclusive derivation of conclusions from concrete, verifiable evidence [19]. It functions to create new knowledge about the way the world actually works by systematically investigating a particular problem using methodologies rooted in the social or natural sciences [21]. A key hallmark of an empirical study is that it presents a new set of findings from original data collection, and its methodology is described in such detail that the study could be recreated and its results tested [20].
Empirical studies in bioethics have seen a statistically significant increase over recent decades, rising from 5.4% of bioethics publications in 1990 to 15.4% in 2003, a trend that is expected to continue [21]. This growth underscores the field's growing recognition of the value of evidence-based inquiry. Empirical research can be categorized hierarchically by its objectives, ranging from foundational descriptive work to studies that aspire to change ethical norms [4].
Table 1: Hierarchical Categories of Empirical Research in Bioethics
| Category | Primary Objective | Exemplary Research Questions | Bioethics Application Example |
|---|---|---|---|
| Lay of the Land | To define current practices, opinions, or beliefs; describes the status quo [4]. | What do physicians think about X? How do patients perceive Y? [4] | Surveying the composition and procedures of hospital ethics committees [4]. |
| Ideal vs. Reality | To assess the extent to which actual clinical practice reflects established ethical ideals [4]. | Does reality match our ethical norms? Where are the gaps? | Investigating disparities in healthcare delivery across racial or socioeconomic groups [4]. |
| Improving Care | To develop and test interventions that bring clinical practice closer to ethical ideals [4]. | How can we improve care to align with ethical norms? | Designing and evaluating a new informed consent process to enhance patient comprehension [4]. |
| Changing Ethical Norms | To synthesize empirical data from multiple studies to inform, refine, or challenge existing ethical principles [4]. | Should our ethical norms change based on accumulated evidence? | Using long-term quality of life data from patients with chronic illnesses to reconceptualize "benefit" in end-of-life decisions [4]. |
Non-Empirical Research: Theory and Synthesis
Non-empirical research serves as the backbone of theoretical and conceptual development in bioethics. It is characterized by the analysis, interpretation, and synthesis of existing knowledge, rather than the generation of new, primary data [20]. This approach is indispensable for clarifying concepts, constructing ethical arguments, critiquing underlying assumptions, and providing comprehensive overviews of a field.
Common outputs of non-empirical research include theoretical articles, conceptual analyses, literature reviews, and position papers. These works are typically structured around logical argumentation and the critical engagement with existing literature and philosophical traditions. A key characteristic is the absence of sections such as "Methods (and Materials)" or "Results," as the author(s) did not conduct original research [20]. Instead, they bring together relevant, useful articles on a general topic to provide a synthesized perspective [20].
In bioethics, non-empirical research addresses fundamental questions of value, principle, and justification that are not always amenable to empirical measurement. It provides the normative framework—the "ought"—that guides ethical deliberation and policy formation.
Direct Comparison of Methodological Features
The choice between empirical and non-empirical methods shapes every aspect of a research project, from its initial design to the nature of its conclusions. The table below provides a point-by-point comparison of their defining features.
Table 2: Feature Comparison of Empirical and Non-Empirical Research
| Feature | Empirical Research | Non-Empirical Research |
|---|---|---|
| Basis of Knowledge | Actual experience, observation, and measurement [19] [20] | Theory, belief, and logical analysis [20] |
| Primary Output | New, primary data and findings [20] | Synthesis, critique, or theoretical development based on existing work [20] |
| Data Form | Numerical (quantitative) or textual/visual (qualitative) data collected firsthand [19] | Existing texts, theories, and published literature |
| Common Formats | Journal articles with IMRaD structure; studies using surveys, experiments, interviews [20] | Theoretical articles, literature reviews, essays, critical commentaries [20] |
| Research Question | Often "what," "how many," "how," or "why" (exploratory) questions | Often "should," "what ought," or conceptual "what is the meaning of" questions |
| Role in Bioethics | Describes reality, identifies ethical problems in practice, tests feasibility of norms, informs policy with evidence [22] [4] | Develops and justifies moral principles, provides normative recommendations, clarifies concepts, synthesizes fields [22] |
Experimental Protocols and Data Analysis in Empirical Research
Qualitative Empirical Methodologies
Qualitative research methods are utilized for gathering non-numerical data to determine underlying reasons, views, or meanings from study participants [19]. This approach is more descriptive and is particularly useful for exploring complex concepts, social interactions, and cultural phenomena [23]. It allows researchers to gain a better understanding of "how" or "why" things occur [23].
- Interview Method: This is a widely used conversational approach where in-depth data is obtained through structured, semi-structured, or unstructured formats [19] [23]. It is exclusively qualitative and allows researchers to obtain precise, relevant information by asking the correct questions. Interviews are commonly used in the social sciences and humanities, such as for interviewing resource persons on bioethical issues [19].
- Focus Groups: A focus group is a thoroughly planned discussion guided by a moderator and designed to derive opinions on a designated topic [19]. This method, essentially a group interview, is valuable for thinking through particular issues or concerns and is widely used to answer "how," "what," and "why" questions [19]. In applied settings, focus groups are frequently employed by consumer product producers for designing and improving products based on user preferences.
- Case Study: This method is used to identify extensive information through an in-depth analysis of existing cases [19]. It is typically used to obtain empirical evidence for investigating complex problems in business studies or bioethics. When conducting case studies, the researcher must carefully perform the empirical analysis, ensuring the variables and parameters in the current case are similar to the case being examined.
- Observational Method: This involves observing and gathering data from study subjects in a personal and time-intensive manner [19]. It is often used in ethnographic studies to obtain empirical evidence and is part of the ethnographic research design. While commonly used for qualitative purposes, observation can also be utilized for quantitative research when observing measurable variables.
Quantitative Empirical Methodologies
Quantitative research methods gather numerical data that can be ranked, measured, or categorized through statistical analysis [19] [23]. This approach is useful for uncovering patterns or relationships, making generalizations, and determining how many, how much, how often, or to what extent a phenomenon occurs [23].
- Survey Research: Survey research is designed to generate statistical data about a target audience and can involve large, medium, or small populations [19]. This quantitative method uses predetermined sets of closed questions that are easy to answer, thus enabling the gathering and analysis of large data sets. While traditionally expensive and time-consuming, advancements in technology have made surveys easier and cheaper to administer through email and social media [19].
- Experimental Research: Experiments involve testing hypotheses in controlled conditions by manipulating variables [23]. This method helps determine cause-and-effect relationships and testing outcomes when variables are altered or removed. Traditionally laboratory-based, experimental research is used to advance knowledge in the physical and life sciences, and increasingly in social sciences [19] [23].
- Causal-Comparative Research: This method leverages the strength of comparison to determine cause-and-effect relationships among variables where manipulation is not possible [19]. For example, a causal-comparative study might measure the productivity of employees in an organization that allows remote work compared to staff in an organization that does not offer work-from-home arrangements.
- Longitudinal Study: A longitudinal method researches the traits or behavior of a subject under observation after repeatedly testing over a certain period [19]. Data collected can be qualitative or quantitative. A prominent example is the British Doctors Study initiated in 1951, which compared smokers and non-smokers and provided undeniable proof of the direct link between smoking and lung cancer by 1956 [19].
Data Analysis Techniques
Data analysis methods vary significantly between qualitative and quantitative research, each requiring specific analytical approaches and tools.
Table 3: Data Analysis Methods in Empirical Research
| Method Type | Data Analysis Approach | Common Tools & Techniques | Outputs |
|---|---|---|---|
| Quantitative Analysis | Statistical analysis of numerical data [23] | Descriptive statistics (mean, median, mode, SD) [24]; Inferential statistics (hypothesis testing) [24] | Statistical significance, p-values, correlations, generalizable findings [23] |
| Qualitative Analysis | Interpretive analysis of non-numerical data [23] | Thematic analysis, textual analysis, coding, searching for patterns [19] [25] | Themes, insights, descriptions of multiple realities, conceptual understanding [25] |
For quantitative data, descriptive statistics summarize or describe the characteristics of a dataset, including measures of central tendency (mean, median, mode) and variability (range, standard deviation) [24]. Inferential statistics are used to test research hypotheses and make inferences or predictions about a population based on sample data, involving objective criteria to decide whether a hypothesis should be accepted or rejected [24].
For qualitative data, analysis tends to be more creative, iterative, and holistic [25]. Techniques like thematic analysis involve searching for recurring themes and patterns across qualitative datasets, while textual analysis involves describing, interpreting, and understanding textual content by connecting it to broader artistic, cultural, political, or social contexts [19].
Empirical Research Methodology Selection and Analysis Pathways
Essential Research Reagents and Tools
Conducting rigorous research in bioethics requires both conceptual and practical tools. The following table details key "research reagent solutions" and essential materials used across different methodological approaches.
Table 4: Essential Research Reagents and Methodological Tools
| Tool/Reagent | Primary Function | Application Context |
|---|---|---|
| Structured Interview Protocol | Ensures consistency in qualitative data collection by using predetermined questions [23]. | Qualitative studies seeking in-depth personal perspectives on ethical dilemmas. |
| Validated Survey Instrument | Provides reliable and consistent measurement of constructs across a sample population [25]. | Quantitative studies measuring attitudes, beliefs, or practices regarding bioethical issues. |
| Statistical Analysis Software (e.g., SAS, R) | Performs descriptive and inferential statistical analyses on numerical data [21] [24]. | Quantitative empirical research for data management, hypothesis testing, and determining significance. |
| Qualitative Data Analysis Software (e.g., NVivo) | Facilitates coding, thematic analysis, and management of non-numerical data [25]. | Qualitative studies handling large volumes of interview transcripts, field notes, or documents. |
| Ethics Committee Approval | Provides formal ethical oversight and ensures participant protection in research [26]. | All empirical research involving human subjects, ensuring adherence to autonomy, beneficence, justice. |
| Theoretical Framework | Provides a structured conceptual foundation for analyzing ethical problems [22]. | Non-empirical research developing normative arguments or synthesizing ethical concepts. |
| Systematic Literature Search Protocol | Ensures comprehensive, unbiased identification of relevant existing literature [22]. | Literature reviews and non-empirical research requiring thorough knowledge of existing scholarship. |
The selection between empirical and non-empirical approaches is not a matter of choosing a superior methodology, but rather of aligning research methods with specific investigative goals. As this guide demonstrates, each approach offers distinct strengths and addresses different types of research questions within bioethics.
Empirical methods excel at describing realities, identifying ethical issues in practice, and testing the feasibility and consequences of ethical norms [22] [4]. They provide the essential evidence base for understanding how ethical principles manifest in real-world contexts. Non-empirical methods, particularly philosophical and theoretical analysis, remain crucial for developing and justifying moral principles, providing normative recommendations, and engaging in conceptual clarification [22].
The most contested, yet potentially most fruitful, applications of empirical research in bioethics occur at the intersection of "is" and "ought," where empirical findings inform, and sometimes challenge, existing ethical norms [22] [4]. The hierarchical model presented in this guide—from Lay of the Land to Changing Ethical Norms—provides a framework for understanding the potential scope and ambitions of empirical work [4].
For researchers in bioethics and drug development, methodological rigor requires careful consideration of the research question, appropriate selection from the methodological toolkit, and transparent reporting of methods and limitations. Whether through systematic data collection or rigorous philosophical analysis, the ultimate goal remains the same: to produce knowledge that enhances ethical understanding and improves human health and wellbeing.
The integration of social science methods with ethical analysis, a field often termed empirical bioethics, represents a growing and methodologically innovative area of research. This interdisciplinary approach seeks to ground normative ethical conclusions in robust empirical evidence concerning stakeholder values, lived experiences, and social contexts. However, the combination of these distinct paradigms—the empirical "is" and the normative "ought"—presents significant challenges for establishing methodological rigor [3]. The field has been characterized by a "systematic lack of clarity" regarding its primary methods and standards of rigor, which in turn creates challenges for peer review, undermines claims to authority, and complicates practical decision-making [3]. This guide provides a comparative analysis of predominant structured integration techniques, assessing their protocols, applications, and methodological rigor to inform researchers, scientists, and drug development professionals engaged in this complex interdisciplinary space.
Comparative Analysis of Integration Methodologies
The following structured techniques represent the most clearly articulated approaches to integrating social science with ethical analysis, each offering distinct pathways to methodological rigor.
Table 1: Structured Integration Techniques in Empirical Bioethics
| Methodology | Core Integration Mechanism | Primary Applications | Key Strengths | Documented Limitations |
|---|---|---|---|---|
| Structured Ethics Appendix [27] | A predefined set of prompts guiding ethical reflection throughout research, reported in an appendix. | Social science experiments, randomized controlled trials (RCTs), primary data collection. | Promotes transparency, sparks reflective practice, improves communication of ethical considerations. | Can be treated as a bureaucratic checklist rather than a reflective process; relatively new approach. |
| Consensus Standards for Empirical Bioethics [2] | A Delphi-derived consensus on 15 standards of practice across 6 research domains, providing a shared framework. | Planning, conducting, and reporting interdisciplinary empirical bioethics research. | Provides concrete guidance for quality assessment; benefits funders, journals, and peer review. | May constrain methodological innovation; requires broad buy-in from the research community. |
| Digital Bioethics Methods [28] | Computational social science techniques (e.g., automated analysis of online discourse) to study bioethical issues. | Investigating novel digital phenomena; tracing the articulation of bioethical issues in online spaces. | Accesses large-scale, naturally occurring data; studies discourse in a "digital agora." | Raises new ethical questions about digital research ethics; requires technical computational skills. |
| The Ethical Interface & STS Approach [29] | Views science, technology, and society as co-produced; integrates normative analysis throughout innovation. | Analyzing technoscientific controversies; policy development for emerging technologies. | Anticipatory and inclusive; addresses power dynamics and cultural pluralism; strong theoretical foundation. | Conceptually complex; can be difficult to operationalize into a standard research protocol. |
Experimental Protocols and Workflows
This section details the specific methodologies for implementing the key integration techniques, providing a roadmap for researchers to apply them in practice.
Protocol for Developing a Structured Ethics Appendix
The structured ethics appendix is designed to move beyond procedural ethics (e.g., IRB approval) toward a more substantive ethical communication [27]. The protocol involves addressing a series of core questions during research design and reporting:
- Policy Equipoise Assessment: Researchers must determine whether there is genuine uncertainty regarding the net benefits of each study arm relative to others and to the best possible, morally attainable alternative policy. This justifies randomization beyond simple scarcity [27].
- Role of the Researcher: Explicitly define the researcher's relationship to the intervention (e.g., impartial observer vs. active participant) and the implications for informed consent [27].
- Harms Identification: Systematically identify potential harms to both participants and non-participants, stemming from either the interventions or the data collection methods themselves [27].
- Conflict of Interest Disclosure: Declare financial and reputational conflicts that could influence research design or interpretation [27].
- Foreseeable Misuse: Consider and articulate potential ways research results could be misused and by whom, demonstrating anticipatory ethics [27].
Structured Ethics Appendix Workflow
Protocol for Implementing Consensus Standards
The consensus on standards for empirical bioethics research, developed through a modified Delphi process with European experts, provides a framework for ensuring quality [2]. The protocol mandates addressing six domains:
- Aims & Questions: Clearly state the research aims and the interdisciplinary research question(s), explaining why an empirical bioethics approach is required [2].
- Integration: Provide a clear and justified methodology for integrating empirical and normative elements, specifying how the empirical data will inform the normative analysis [2].
- Conduct of Empirical Work: Justify the chosen empirical methods (e.g., surveys, interviews, ethnography) and demonstrate their rigorous application, adhering to social scientific standards [2].
- Conduct of Normative Work: Justify the chosen normative approach (e.g., deontology, utilitarianism, virtue ethics) and demonstrate its rigorous application, adhering to philosophical standards [2].
- Training & Expertise: Research teams should possess, or actively cultivate, expertise in both the relevant empirical methods and normative analysis [2].
Protocol for Digital Bioethics Analysis
Digital bioethics employs methods from computational social science to study ethical discourse online [28]. A typical workflow includes:
- Research Question Formulation: Define a bioethical issue for investigation (e.g., public discourse on CRISPR gene editing).
- Data Sourcing: Identify and collect data from relevant digital platforms (e.g., Twitter/X, specialized forums, news comments).
- Computational Processing: Use automated techniques such as natural language processing, sentiment analysis, or network analysis to structure and analyze the data.
- Normative Integration: Interpret the computational findings through normative ethical frameworks to draw bioethically significant conclusions.
Digital Bioethics Methodology Flow
Successful integration of social science and ethical analysis requires both conceptual and practical tools. The following table details key "research reagents" for this interdisciplinary work.
Table 2: Essential Reagents for Integrated Empirical-Normative Research
| Research Reagent | Function & Purpose | Application Context |
|---|---|---|
| Policy Equipoise Framework [27] | Justifies randomization in studies by assessing uncertainty of net benefits relative to the best morally attainable alternative policy. | Designing ethical randomized controlled trials (RCTs) in social science and public health. |
| Delphi Consensus Method [2] | A structured communication technique used to reach consensus among experts, often on quality standards or normative guidelines. | Developing practice standards in emerging fields; resolving complex ethical-policy questions. |
| Computational Social Science Tools [28] | Software and algorithms (e.g., for NLP, network analysis) to collect and analyze large-scale digital data on public discourse. | Studying the emergence and evolution of ethical debates in online spaces (digital bioethics). |
| Moral Philosophy Frameworks [30] [29] | Provides the foundational normative lenses (deontology, utilitarianism, virtue ethics) for structured ethical reasoning. | Analyzing empirical findings to draw normative conclusions; justifying ethical recommendations. |
| Co-production Model (STS) [29] | An analytical lens viewing scientific knowledge and social order as mutually constitutive, highlighting embedded values. | Critically assessing how technologies and scientific practices shape, and are shaped by, societal values. |
The structured integration of social science with ethical analysis is maturing, with several robust methodologies now available to researchers. The Structured Ethics Appendix offers a practical tool for enhancing transparency in experimental social science [27], while the Consensus Standards provide a broader framework for assuring the quality of interdisciplinary empirical bioethics research [2]. Emerging approaches like Digital Bioethics significantly expand the empirical toolbox by turning the online space into a site for rigorous research [28]. Underpinning all these methods is the foundational principle, drawn from Science and Technology Studies, that science, technology, and ethics are not separate domains but are co-produced within a dynamic "ethical interface" [29]. For drug development professionals and scientists, selecting and rigorously applying one of these structured techniques is critical for generating work that is methodologically sound, ethically informed, and capable of withstanding interdisciplinary scrutiny.
In the realm of empirical bioethics and healthcare research, many complex questions cannot be answered by quantitative data alone. Problems characterized by uncertainty, emerging evidence, and ethical complexity require methodologies that can synthesize expert judgment into reliable consensus. The Modified Delphi method has emerged as a systematic approach to this challenge, offering a structured process for developing collective intelligence on complex issues where statistical evidence is limited, conflicting, or ethically difficult to obtain [31].
Originally developed by the RAND Corporation during the Cold War for military forecasting, the Delphi technique has since been adapted for diverse healthcare applications [31] [32]. The modified version retains the core strengths of traditional Delphi—anonymity, iteration, and controlled feedback—while introducing pragmatic adaptations that make it particularly valuable for contemporary health research, including drug development and bioethics [32]. This method enables researchers to navigate complex problems where human expert judgment provides superior insights to individual opinion or where research evidence remains incomplete [31].
As methodological rigor becomes increasingly crucial in empirical bioethics, understanding the applications, protocols, and comparative strengths of the Modified Delphi method is essential for researchers, scientists, and drug development professionals seeking to establish best practices, develop clinical guidelines, or identify future research priorities in their respective fields.
Understanding the Modified Delphi Method
Definition and Core Principles
The Modified Delphi method is a systematic, structured process designed to help a group of experts reach consensus on a particular topic through a combination of iterative surveys and controlled feedback [33]. Unlike traditional qualitative methods that rely on face-to-face discussions, this approach uses repeated rounds of anonymous voting to provide focus and prioritization to complex problem-solving processes [33].
The methodology is particularly valuable for complex healthcare problems that require collective intelligence, such as developing key performance indicators for telemedicine [34], defining disease progression in polycythemia vera [35], or establishing quality indicators for virtual care [36]. By leveraging structured communication and statistical aggregation of group responses, the Modified Delphi method transforms individual opinions into collective judgment while minimizing the psychological biases inherent in group interactions.
Key Modifications from Traditional Delphi
While preserving the fundamental Delphi principles, the modified version introduces several pragmatic adaptations that enhance its efficiency and applicability to healthcare research:
Structured Starting Point: Instead of beginning with completely open-ended questions, modified Delphi typically presents panelists with preliminary information derived from literature reviews, existing evidence, or prior research [32]. For instance, in developing quality indicators for virtual care, researchers conducted a comprehensive scoping review that identified 140 potential indicators before the first Delphi round [36].
Streamlined Process: Modified Delphi often employs fewer rounds than traditional approaches, typically two to four iterations rather than the potentially unlimited rounds of classical Delphi [32]. This adaptation respects the time constraints of expert panelists while maintaining methodological integrity.
Integration of Discussion Elements: Some modified Delphi approaches incorporate controlled discussion elements, such as virtual panel meetings between voting rounds [36]. These discussions allow experts to clarify reasoning while maintaining the anonymity of subsequent voting stages.
Experimental Protocol and Implementation
Standardized Workflow
The implementation of a Modified Delphi study follows a structured, multi-stage process that ensures methodological rigor while allowing for contextual adaptation. The workflow diagram below illustrates this standardized approach:
Phase 1: Problem Identification and Structuring
The initial phase involves clearly defining the research problem and establishing the methodological framework. Researchers must document the criteria used to identify the problem area, which may include extensive systematic literature searches, group discussions among a steering committee, or open-ended discussions with potential panel members [31]. During this phase, the research team establishes the consensus criteria, closing criteria for rounds, and analytical approaches that will be used throughout the study [31].
Phase 2: Expert Panel Selection
Panel member selection is arguably the most crucial aspect of Delphi research quality [31]. The panel composition directly influences the validity and generalizability of results. Key considerations include:
Homogeneity vs. Heterogeneity: A diverse panel provides broader perspectives, while a homogenous group may offer more specialized insights on focused problems [31]. For a study defining disease progression in polycythemia vera, a homogeneous panel of hematologist-oncologists was appropriate [35], whereas developing virtual care quality indicators required a heterogeneous panel including clinicians, patients, policymakers, and administrators [36].
Expertise Criteria: Clear, predefined criteria for "expertise" should be established, such as years of experience, publications in the field, or specific professional qualifications [31]. For example, a study on health professions education required panelists to have postgraduate qualifications and at least two years of teaching experience [37].
Panel Size: While traditional Delphi panels can range from 10 to 100 members, modified Delphi typically employs smaller panels (e.g., 10-20 experts) for practical management [31] [38]. A virtual care study successfully used a 19-member pan-Canadian panel [36], while a sustainability measure development study involved 10 experts [38].
Phase 3: Iterative Rating Rounds with Controlled Feedback
The core of the Modified Delphi process involves iterative rounds of voting with interspersed controlled feedback:
Round 1 - Initial Rating: Panelists receive the preliminary materials (e.g., statements, indicators, or scenarios) and rate them using established measurement scales (typically Likert scales of 3 to 10 points) [36] [34] [37]. In a virtual care quality indicator study, panelists used a 9-point Likert scale based on Agency for Healthcare Research and Quality measure attributes [36].
Controlled Feedback: After each round, the research team analyzes responses and provides panelists with statistical summaries (means, medians, percentages, measures of dispersion) and sometimes anonymous comments [31]. This feedback allows experts to see the group's perspective while maintaining anonymity.
Subsequent Rounds: Panelists reconsider their ratings in light of the group feedback. The process typically continues for 2-4 rounds until predetermined consensus thresholds are met [33] [32]. Each iteration provides opportunities for refining statements, clarifying interpretations, and converging toward agreement.
Phase 4: Consensus Assessment and Stability Analysis
The final phase involves determining whether sufficient consensus has been achieved based on predefined criteria. Common approaches include:
Statistical Thresholds: Many studies define consensus as a specific percentage of responses falling within a predetermined range (e.g., ≥75% agreement) [36] [35] [38]. The virtual care study required 75% or more of panelists' responses in the top tertile (scores of 7-9) with a median composite score of 7 or greater [36].
Stability Assessment: Some methodologies incorporate tests for response stability between rounds, such as McNemar's test for dichotomous responses [37], ensuring that consensus is not merely transient.
Qualitative Integration: Final analysis often incorporates qualitative insights from open-ended comments to contextualize the statistical consensus and identify remaining areas of divergence [37].
Essential Research Reagents: The Modified Delphi Toolkit
Table 1: Key Methodological Components in Modified Delphi Studies
| Component | Function | Implementation Examples |
|---|---|---|
| Expert Panel | Provides specialized knowledge and judgment | 19-member pan-Canadian panel (clinicians, patients, administrators, policymakers) [36]; 7 US-based clinical physicians specializing in polycythemia vera [35] |
| Rating Instrument | Quantifies expert opinions | 9-point Likert scale based on AHRQ measure attributes [36]; 10-point Likert scale for telemedicine KPIs [34]; 3-point importance scale for medical education topics [37] |
| Consensus Threshold | Determines when agreement is reached | ≥75% agreement with median score ≥7 [36]; ≥80% consensus for medical education topics [37]; 70% agreement level for telemedicine indicators [34] |
| Feedback Mechanism | Allows refinement of opinions | Statistical summaries (means, percentages, measures of dispersion) after each round [31]; virtual panel meetings between rounds [36] |
| Stability Measure | Assesses consistency of responses between rounds | McNemar's test for dichotomous responses [37]; Cohen's Kappa for inter-round agreement [34] |
Comparative Analysis: Modified Delphi vs. Alternative Consensus Methods
Table 2: Methodological Comparison of Consensus Techniques
| Method Characteristic | Modified Delphi | Traditional Delphi | Nominal Group Technique (NGT) | Consensus Development Conference |
|---|---|---|---|---|
| Anonymity | Maintained throughout voting process | Maintained throughout | Limited during discussion | Typically not anonymous |
| Geographical Flexibility | High (electronic administration) | High | Low (typically in-person) | Moderate (possible virtual) |
| Time Requirements | Moderate (2-4 rounds) | Potentially extensive (multiple rounds) | Low (single session) | Low to moderate |
| Resource Intensity | Moderate | Moderate to high | Low | High |
| Risk of Dominant Individuals | Minimal | Minimal | Moderate | High |
| Structured Feedback | Controlled, statistical | Controlled, statistical | Immediate, qualitative | Varied, often qualitative |
| Exploration of Rationale | Limited through comments | Limited through comments | Extensive during discussion | Extensive during discussion |
| Typical Applications | Healthcare indicators, guideline development, policy recommendations | Forecasting, long-range planning | Problem identification, solution generation | Clinical guidelines, policy statements |
Advantages of Modified Delphi
The Modified Delphi method offers several distinct advantages that explain its widespread adoption in healthcare research:
Reduced Bias: Anonymous responses prevent dominance by influential individuals and reduce conformity pressures (groupthink) [32] [39]. Ideas are judged on merit rather than the authority or personality of contributors.
Geographical Flexibility: Electronic administration enables global participation, accessing diverse expertise without logistical constraints [32] [39]. A telemedicine study in Egypt successfully implemented an electronic modified Delphi approach [34].
Iterative Consensus-Building: The structured feedback process allows participants to refine their thinking while maintaining methodological rigor [32]. The repetition with controlled feedback facilitates convergence toward agreement.
Documentation of Process: The method produces a transparent record of how consensus was reached, supporting justification of decisions in policy-making or clinical guideline development [32].
Limitations and Mitigation Strategies
Despite its strengths, researchers should acknowledge and address several limitations:
Limited Open Discussion: The controlled feedback mechanism may restrict rich qualitative exchange [39]. Some modified Delphi approaches incorporate discussion rounds or use preliminary Nominal Group Techniques to mitigate this limitation [37].
Participant Attrition: Multiple rounds can lead to dropout, potentially biasing results [39]. Well-designed studies maintain high engagement through efficient processes and respectful use of experts' time [36].
Dependence on Expert Competence: Results are only as valid as the panel's expertise [39]. Rigorous selection criteria and clear definition of expertise domains are essential safeguards [31].
Artificial Consensus: The structured process might create premature or superficial agreement [31]. Stability measures and analysis of dissent help preserve methodological integrity [37].
Applications in Healthcare and Bioethics
The Modified Delphi method has demonstrated particular utility across diverse healthcare applications:
Clinical Guideline and Indicator Development
In developing quality indicators for virtual care, Mukerji et al. used a three-round modified Delphi process to curate 25 indicators from an initial list of 140 potential measures [36]. The structured process allowed integration of diverse perspectives from clinicians, patients, administrators, and policymakers, resulting in a balanced scorecard aligned with the Quintuple Aim framework.
Disease Definition and Classification
For complex conditions like polycythemia vera, where disease progression criteria remain uncertain, a US-modified Delphi consensus achieved 95% agreement (39/41 statements) on defining disease progression and modification [35]. The method enabled specialists to converge on standardized definitions essential for clinical trial design and treatment evaluation.
Educational Framework Development
In medical education, a modified e-Delphi study reached consensus on 17 key topics for integrating health professions education into undergraduate medical curricula [37]. The process engaged 69 experts across Pakistan, demonstrating the method's scalability and adaptability to diverse educational contexts.
Measurement Tool Development
The development of the Sustainability Measure for Healthcare utilized a modified Delphi technique to create a 37-item scale for assessing the sustainability of complex healthcare interventions [38]. The iterative process successfully captured varying expert perceptions of sustainability while identifying commonalities translatable into a valid measurement instrument.
The Modified Delphi method represents a sophisticated tool for achieving expert consensus on complex issues characterized by uncertainty or limited evidence. Its structured yet flexible approach balances methodological rigor with practical implementation, making it particularly valuable for researchers and drug development professionals addressing multifaceted problems in bioethics and healthcare.
By providing a systematic framework for synthesizing collective intelligence while minimizing psychological biases, the Modified Delphi method enhances the transparency, reliability, and credibility of consensus processes. The documented protocols, quantitative assessment criteria, and stability measures address key methodological concerns in empirical bioethics, supporting the development of rigorously constructed guidelines, indicators, and conceptual frameworks.
As healthcare challenges grow increasingly complex and interdisciplinary, the Modified Delphi method offers a validated approach for harnessing diverse expertise to establish best practices, define emerging concepts, and prioritize future research directions—all essential components for advancing evidence-based healthcare and ethical drug development.
Applying the Reflective Equilibrium Method for Coherentist Analysis
Empirical bioethics faces a fundamental challenge: establishing methodological rigor when integrating normative analysis with empirical social science research [3]. This interdisciplinary field draws from philosophy, sociology, medicine, and law, each with distinct standards of validity and truth [3]. The resulting methodological pluralism has created five significant challenges: (1) no clear standards for answering bioethical questions, (2) problems in peer review, (3) undermined claims to authority and legitimacy, (4) difficulties in clinical decision-making, and (5) questions about bioethics' proper institutional setting [3].
Within this context, the reflective equilibrium (RE) method has emerged as a prominent approach to justification. Originally developed by John Rawls, RE offers a systematic process for achieving coherence among moral beliefs, principles, and relevant background theories [40]. This guide provides a comprehensive comparison of RE applications, experimental protocols, and implementation frameworks to assist researchers in selecting appropriate methodological approaches for empirical bioethics research.
Understanding Reflective Equilibrium: Core Concepts and Variants
Theoretical Foundations
Reflective equilibrium is a coherentist method of justification that involves mutual adjustment between different types of beliefs until coherence is achieved [40]. The process begins with considered moral judgments—those judgments made under conditions conducive to ethical reasoning where individuals have adequate information, are free from distress, and are motivated to make correct decisions [40]. These judgments are then systematically reconciled with general moral principles and relevant background theories through iterative refinement [41].
The method is "reflective" because practitioners understand how their judgments conform to principles and the premises of their derivation [41]. The resulting "equilibrium" is inherently temporary, as new information or perspectives can disrupt the coherence at any time [41]. This dynamic nature makes RE particularly suitable for complex bioethical dilemmas where scientific advancements continuously evolve the landscape of moral considerations.
Narrow vs. Wide Reflective Equilibrium
Table 1: Comparison of Reflective Equilibrium Variants
| Characteristic | Narrow Reflective Equilibrium | Wide Reflective Equilibrium |
|---|---|---|
| Scope | Matches principles to existing judgments with minor adjustments | Incorporates all plausible moral and philosophical considerations |
| Elements | Considered judgments + Moral principles | Considered judgments + Moral principles + Background theories |
| Revision Scope | Limited revision of initial judgments | Comprehensive revision allowed, including radical changes |
| Theoretical Support | Minimal theoretical justification | Robust incorporation of relevant philosophical arguments |
| Application Complexity | Relatively straightforward | Methodologically demanding |
The distinction between narrow and wide reflective equilibrium represents a central differentiation in methodological approach. Narrow reflective equilibrium (NRE) seeks coherence between a person's initial moral judgments and moral principles, allowing only minor adjustments to resolve inconsistencies [40]. In contrast, wide reflective equilibrium (WRE) incorporates background theories and philosophical arguments, permitting substantial revision of initial beliefs, including what Michael DePaul characterizes as "moral conversion" experiences where one's moral outlook undergoes fundamental transformation [40].
Norman Daniels famously defended WRE as a more robust justificatory method precisely because it draws on background theories that can independently support ethical principles against alternatives [41]. For empirical bioethics, this distinction has practical implications: NRE may suffice for refining established ethical frameworks, while WRE proves necessary when confronting novel dilemmas requiring fundamental reconsideration of moral commitments.
Comparative Analysis of Reflective Equilibrium Applications
Current Application Landscape
A 2024 systematized review of explicit WRE applications provides revealing data about how this method is actually employed in ethical research [41]. The review identified only 19 studies containing 23 explicit applications where WRE was systematically applied according to Daniels' definition (containing three levels, naming their elements, and providing connections between levels) [41]. This surprisingly low number suggests that while frequently discussed as a theoretical justification method, RE's structured application remains limited.
Table 2: Application Analysis of Wide Reflective Equilibrium
| Application Dimension | Findings | Significance |
|---|---|---|
| Total Explicit Applications | 23 across 19 studies | Method remains rarely implemented in structured form |
| Reported Success Rate | 19 equilibria reached | High success when properly applied |
| Disciplinary Distribution | Various disciplines including bioethics, business ethics, law | Broad interdisciplinary applicability |
| Purpose Variation | Different purposes and topics addressed | Methodological flexibility |
| Procedural Consistency | Considerable variation in adjustment process and criteria | Lack of standardization in implementation |
The review further analyzed 50 equilibria discussed within these applications, finding that researchers reached a reported equilibrium state in 19 instances [41]. Applications differed considerably in procedural specifics, particularly regarding the presentation of adjustment processes and criteria used to determine when equilibrium had been achieved [41]. This heterogeneity underscores the need for more standardized reporting of RE methodologies in empirical bioethics research.
Comparative Methodological Frameworks
When comparing RE to other methodological approaches in empirical bioethics, several distinctive features emerge. A 2018 consensus project developed 15 standards of practice organized into 6 domains: aims, questions, integration, conduct of empirical work, conduct of normative work, and training & expertise [2]. These standards emphasize the importance of transparently reconciling the empirical "is" with the normative "ought"—a challenge that RE directly addresses through its structured process of mutual adjustment [2].
Survey data reveals that among bioethics researchers who use empirical methods, only 35% reported having successfully integrated empirical data with normative analysis, though 59.8% planned to do so in current projects [42]. This intention-implementation gap highlights the methodological difficulties inherent in interdisciplinary bioethics research—difficulties that RE specifically aims to mitigate through its systematic approach to coherence-building.
Experimental Protocol: Implementing Reflective Equilibrium
Core Workflow Process
The following diagram illustrates the iterative workflow for implementing wide reflective equilibrium in empirical bioethics research:
Implementation Protocol Details
Phase 1: Element Identification
- Considered Moral Judgments: Collect judgments under conditions that minimize distortion (adequate information, emotional calm, impartiality) [40]. Apply confidence constraints by prioritizing judgments held with conviction [40].
- Moral Principles: Identify relevant general principles across all levels of generality, from specific case rules to abstract theoretical commitments [40].
- Background Theories: Select relevant philosophical arguments, social theories, and empirical research that bear on the ethical question [41].
Phase 2: Coherence Assessment
- Systematic Comparison: Map relationships between all three element types, identifying points of agreement and conflict.
- Inconsistency Documentation: Catalog specific discrepancies requiring resolution, noting their relative significance to the overall framework.
Phase 3: Mutual Adjustment
- Iterative Revision: Modify elements to resolve inconsistencies, granting no element immunity from revision [41].
- Theoretical Consultation: Use background theories to guide revision decisions between competing coherence strategies [41].
- Comprehensive Justification: Document reasons for each adjustment, creating an audit trail of the reasoning process.
Phase 4: Equilibrium Verification
- Stability Check: Confirm that no further adjustments are required to maintain coherence among all elements.
- Robustness Testing: Assess how the equilibrium withstands potential counterexamples and alternative interpretations.
This protocol typically requires multiple iterations, with the average study reporting equilibrium after several adjustment cycles [41]. Researchers should document both the final equilibrium and the revision process that led to it, as this justificatory trail forms a crucial component of methodological rigor.
Research Reagent Solutions: Essential Methodological Components
Table 3: Essential Methodological Components for Reflective Equilibrium Research
| Component Category | Specific Elements | Function in RE Process |
|---|---|---|
| Data Collection Tools | Semi-structured interview protocols; Case vignettes; Systematic literature review frameworks | Capturing considered judgments; Identifying relevant principles and theories |
| Analytical Frameworks | Coherence mapping matrices; Consistency assessment rubrics; Priority hierarchy templates | Identifying inconsistencies; Guiding adjustment decisions |
| Theoretical Resources | Philosophical argument databases; Empirical research repositories; Conceptual analysis tools | Providing background theories; Supporting principle justification |
| Validation Instruments | Peer review checklists; Stakeholder feedback instruments; Counterexample testing protocols | Verifying equilibrium stability; Testing robustness |
These methodological "reagents" serve as essential tools for implementing rigorous RE processes. The coherence mapping matrices, for instance, help researchers visualize relationships between elements, while the priority hierarchy templates assist in resolving conflicts when multiple coherence strategies are available. The theoretical resources are particularly crucial for WRE, as background theories provide independent justification for moral principles beyond their ability to explain existing judgments [41].
The reflective equilibrium method offers empirical bioethics researchers a systematic approach to justifying normative conclusions through coherentist reasoning. The comparative analysis presented here suggests several strategic considerations for method selection:
First, the distinction between narrow and wide RE has significant implications for justificatory strength. While NRE may be more straightforward to implement, WRE provides stronger justification through its incorporation of background theories [41]. Researchers should select their approach based on the novelty and complexity of the ethical question at hand.
Second, the documented variation in RE application procedures indicates a need for greater methodological standardization [41]. Researchers should transparently report their specific adjustment processes and equilibrium criteria to facilitate evaluation and replication.
Finally, the relatively sparse explicit application of structured RE suggests significant opportunity for methodological advancement in empirical bioethics [41]. As the field continues to grapple with challenges of interdisciplinary integration, RE offers a promising framework for achieving methodological rigor while respecting the distinctive contributions of both empirical and normative inquiry.
Within contemporary bioethics and related applied fields, methodological rigor is not merely an academic concern but a foundational requirement for credible practice. Principlism, an approach utilizing mid-level principles such as autonomy, beneficence, non-maleficence, and justice, has become a dominant framework for addressing ethical problems in medicine and research [43]. However, its application occurs within a contentious landscape where the very disciplinary status of bioethics is debated—described variably as a discipline, an interdisciplinary field, or a multidisciplinary endeavor [3]. This disagreement fundamentally impacts methodological standards, as disciplines are characterized in part by their shared methods and criteria for rigor [3]. When bioethics research draws on multiple methods from philosophy, law, sociology, and medicine, establishing consistent standards for evaluating normative claims becomes complex [3] [42]. This guide objectively compares principlism's operationalization against emerging methodological alternatives, examining their procedural frameworks, empirical support, and applicability to decision-making contexts faced by researchers and drug development professionals.
Comparative Frameworks: Principlism and Its Alternatives
The table below provides a systematic comparison of principlism against two significant alternative approaches: ethics of care and empirical bioethics. Each framework offers distinct methodological commitments and operational procedures.
Table 1: Comparative Analysis of Ethical Frameworks in Applied Ethics
| Framework Attribute | Principlism | Ethics of Care | Empirical Bioethics |
|---|---|---|---|
| Primary Focus | Application of mid-level ethical principles | Relationships and responsive care practices | Integration of empirical data with normative analysis |
| Core Operational Units | Autonomy, Beneficence, Non-maleficence, Justice | Attentiveness, Responsibility, Competence, Responsiveness [43] | Empirical findings (qualitative/quantitative), ethical principles, integration methodology |
| Methodological Approach | Casuistry and principled reasoning | Contextual narrative and relationship preservation | Interdisciplinary methods combining social science research with philosophical ethics [2] [42] |
| Strength of Application | Provides structured, replicable analytical process | Acknowledges fundamental human dependence and asymmetry [43] | Grounds normative analysis in observable realities and stakeholder perspectives |
| Documented Limitations | Can prioritize abstract reasoning over contextual nuances | May lack clear decision procedures for resource allocation | Challenges in validly integrating empirical "is" with normative "ought" [2] [42] |
Expanding the Methodological Landscape
Beyond the frameworks compared above, applied ethics also draws upon virtue ethics (focusing on moral character), casuistry (case-based reasoning), and communicative ethics (procedural deliberation). The development of hybrid methodologies is increasingly common, with one systematic review identifying 32 distinct methodologies within empirical bioethics alone [2]. This heterogeneity reflects the field's ongoing effort to develop rigorous methods that can address complex, real-world ethical problems without oversimplification. The choice of framework often depends on the specific context—clinical consultation, policy formation, or research ethics review—and the nature of the ethical question being addressed.
Quantitative Assessment of Methodological Integration
Empirical studies reveal how ethical frameworks are actually operationalized within research practice. The data below summarizes findings from a survey of European bioethics researchers, illustrating current practices in methodological training and application.
Table 2: Empirical Assessment of Research Practices in Bioethics (Survey of 200 Researchers)
| Research Practice Dimension | Metric | Percentage of Researchers |
|---|---|---|
| Use of Empirical Methods | Use or have used empirical methods in their work | 87.5% [42] |
| Methodological Training | Received training in qualitative methods | 61.0% [42] |
| Received training in quantitative methods | 59.0% [42] | |
| Used empirical methods without methodological training | 22.9% [42] | |
| Self-Assessed Expertise | Self-identified as experts in methods they used | ≤6.0% [42] |
| Normative-Empirical Integration | Have integrated empirical data with normative analysis | 35.0% [42] |
| Plan integration in current projects | 59.8% [42] |
Interpreting the Metrics
The relatively high usage of empirical methods coupled with limited methodological training and self-assessed expertise highlights a significant challenge for methodological rigor in the field. This training gap potentially compromises the quality of empirical work and the validity of its integration with normative analysis [42]. Furthermore, the substantial increase in researchers planning integration (59.8%) compared to those who have previously achieved it (35.0%) suggests both growing recognition of integration's importance and possible uncertainty about how to execute it effectively. This data underscores the need for enhanced methodological training and clearer standards for interdisciplinary work.
Experimental Protocols for Ethical Framework Assessment
Protocol 1: Randomized Evaluation of Ethical Decision-Making Processes
Objective: To quantitatively compare the outcomes and participant experiences of different ethical frameworks when applied to standardized clinical cases.
Design:
- Randomized controlled design with three parallel groups (Principlism, Ethics of Care, Empirical Bioethics)
- Blinding: Participants are blinded to the specific framework being tested; analysts are blinded to group assignment
- Control: Case analysis without structured framework
Participant Recruitment:
- Sample: 150 professionals (clinicians, researchers, ethicists)
- Inclusion: Minimum 2 years experience in clinical or research ethics
- Stratification: By professional background and years of experience
Intervention:
- Training Phase: 2-hour standardized training on assigned ethical framework
- Application Phase: Analysis of 3 standardized clinical cases with ethical challenges
- Assessment: Evaluation of decision quality, time to decision, and stakeholder consideration
Outcome Measures:
- Primary: Consensus with expert panel judgment (measured on 7-point Likert scale)
- Secondary: Time to reach decision; Comprehensiveness of stakeholder consideration; Participant satisfaction with framework
Ethical Considerations: Approved by Institutional Review Board with waiver of documented consent [44]
Protocol 2: Longitudinal Assessment of Framework Implementation
Objective: To evaluate the sustainability and practical implementation challenges of different ethical frameworks in organizational settings.
Design:
- Mixed-methods longitudinal design with quarterly assessments over 2 years
- Sites: 6 academic medical centers implementing different ethics frameworks
Data Collection:
- Quantitative: Ethics consultation metrics, satisfaction surveys
- Qualitative: Semi-structured interviews with framework users
- Document Analysis: Ethics committee minutes and case documentation
Analysis:
- Integration: Convergent design with triangulation of quantitative and qualitative data
- Framework Assessment: Implementation fidelity, adaptability to novel cases, resource requirements
This protocol exemplifies the empirical bioethics approach by systematically collecting and integrating observational data with normative analysis of implementation outcomes [2] [42].
Visualizing Methodological Integration in Empirical Bioethics
The diagram below illustrates the conceptual architecture and procedural workflow for integrating empirical research with normative analysis, a core methodological challenge in contemporary bioethics.
This workflow highlights the critical integration point where empirical findings and normative reasoning must be synthesized—a process that requires careful methodological consideration to avoid the naturalistic fallacy of deriving "ought" directly from "is" without proper justification [2].
The table below details key methodological components and their functions for conducting rigorous research in applied ethics.
Table 3: Essential Methodological Resources for Applied Ethics Research
| Tool or Resource | Primary Function | Application Context |
|---|---|---|
| Semi-Structured Interview Guides | Elicit rich qualitative data on ethical perspectives | Exploring stakeholder values and experiences in clinical or research settings |
| Standardized Case Scenarios | Provide consistent stimuli for comparative analysis | Testing ethical frameworks under controlled conditions with different participant groups |
| Normative Analysis Framework | Structure ethical reasoning process | Systematic application of principles, care considerations, or other ethical theories |
| Integration Methodology | Bridge empirical findings and normative conclusions | Explicit procedures for connecting descriptive data with prescriptive claims [2] |
| Mixed-Methods Research Designs | Combine quantitative and qualitative approaches | Comprehensive understanding of complex ethical phenomena [42] |
| Consensus Development Procedures | Establish agreement on ethical guidance | Delphi techniques, nominal group processes for policy development |
Comparative Performance in Decision Contexts
The application of different ethical frameworks produces varying outcomes across decision contexts. The following table synthesizes performance data based on experimental and observational studies.
Table 4: Framework Performance Across Decision Contexts
| Decision Context | Principlism Performance | Ethics of Care Performance | Empirical Bioethics Performance |
|---|---|---|---|
| Clinical Ethics Consultation | Provides clear structure; may overlook relational dynamics | Excels in relational contexts; may lack procedural clarity | Grounded in stakeholder perspectives; methodologically complex |
| Research Ethics Review | Systematic coverage of key ethical considerations | Identifies power imbalances in researcher-participant relationships | Incorporates empirical data on participant experiences and comprehension |
| Organizational Policy Development | Ensures consistent application across cases | May struggle with resource allocation at scale | Policies informed by operational realities and stakeholder values |
| Emergency Clinical Decision-Making | Can be overly time-consuming for rapid response | Adapts to contextual urgency while preserving care orientation | Requires pre-established empirical foundation for immediate application |
Evidence Base and Validation
The performance characteristics outlined above are drawn from multiple sources: (1) comparative case analysis studies where different frameworks are applied to standardized ethical dilemmas; (2) systematic observation of ethics consultation processes and outcomes; and (3) participant-reported experiences with different deliberative approaches. Principlism demonstrates particular strength in contexts requiring transparent justification and consistent application, such as institutional policy development and research ethics review, where its structured approach facilitates accountability. Conversely, ethics of care shows superior performance in relationship-intensive settings such as pediatric ethics, geriatric care, and chronic illness management, where preserving relational bonds is a central ethical concern [43]. Empirical bioethics, while methodologically demanding, provides the most comprehensive approach for developing ethics guidance that is both philosophically sound and practically implementable, as it incorporates actual stakeholder perspectives and contextual realities [2] [42].
In the evolving field of empirical bioethics, the integration of social-scientific research with normative ethical analysis presents unique methodological challenges. Without transparent reporting, the rigor and validity of such interdisciplinary work can be difficult to assess. This guide compares the current state of methodological reporting against emerging standards, providing researchers with a clear framework for documenting their approach. The adoption of explicit reporting standards is critical for ensuring transparency, facilitating proper evaluation, and strengthening the scholarly foundation of empirical bioethics research.
The Imperative for Standards in Empirical Bioethics
Empirical bioethics is a broad field characterized by significant methodological diversity. A systematic review identified 32 distinct methodologies attempting to integrate empirical and normative approaches, leading to a landscape where justifying methodological choices from first principles is often necessary but space-consuming in publications [10]. This heterogeneity threatens the field's credibility as a distinct community of practice.
The call for standards is driven by several needs:
- Quality Assurance: Establishing a baseline for methodological quality and transparency [10].
- Efficient Communication: Providing researchers with a shared framework for justifying methodological choices, which is especially useful when seeking funding or publication [10].
- Training and Pedagogy: Offering clear guidance for teaching students and early-career researchers [10].
A consensus project among European experts led to the development of 15 standards of practice, organized into six domains, providing a foundational framework for the field [10].
Comparative Analysis: Current Practices vs. Reporting Standards
The table below contrasts common methodological reporting challenges with the explicit standards proposed to address them.
| Aspect of Methodological Reporting | Common Challenges and Gaps | Proposed Reporting Standards and Solutions |
|---|---|---|
| Defining Research Aims | Failing to articulate how the research addresses a concrete normative issue oriented toward practice [10]. | Research should explicitly state its normative aim and explain its practical orientation [10] [45]. |
| Integration of Empirical & Normative Elements | Treating empirical data and ethical analysis as separate, parallel components without explaining their interaction [10] [46]. | Researchers must articulate and justify their methodology for "integrating" empirical research and ethical argument, with an expansive understanding of what integration can entail [10] [45]. |
| Articulating Philosophical Stance | Omitting or obscuring underlying epistemological and meta-ethical commitments that shape the research approach [10]. | Researchers should state their broad philosophical position and explain how it informs their specific project methodology, without the burden of defending all foundational assumptions in every paper [10] [46]. |
| Conduct of Empirical Work | Applying empirical methods without justifying their selection or adapting them to the unique context of bioethical inquiry [10]. | The choice and implementation of empirical methods must be justified and executed with reference to established disciplinary standards [10]. |
| Clarity of Reporting | Presenting complex, mixed-methods research in a way that obscures the integration process due to word count limitations or unclear writing [47]. | Researchers should transparently communicate the methods, findings, and unique insights from integration, making the process accessible to readers within publication constraints [47]. |
Experimental Protocols for Establishing Methodological Rigor
The following protocols are adapted from consensus-building and systematic review methodologies relevant to developing and assessing reporting standards.
Protocol 1: Modified Delphi Consensus Process
This protocol outlines the steps for establishing expert-based reporting standards, as used in developing empirical bioethics standards [10].
- Expert Panel Assembly: Convene a diverse group of scholars (e.g., 16 academics from 5 countries) with a range of disciplinary backgrounds and methodological commitments.
- Initial Drafting: Generate a preliminary set of standards based on a review of existing methodologies and quality criteria.
- Iterative Discussion Rounds: Conduct a series of structured group discussions (e.g., 4 rounds over 2.5 days). Unlike traditional anonymous Delphi, this adapted method uses direct dialogue to immediately clarify linguistic and conceptual disagreements.
- Consensus Seeking: After each round, refine the standards based on group feedback. The goal is to reach a consensus on the final set of standards.
- Documentation and Dissemination: Publish the agreed-upon standards with a clear account of the process and areas of disagreement to invite broader community response [10].
Protocol 2: Systematic Review of Benchmarking Impact
This protocol is designed to evaluate the relationship between benchmarking activities (a form of standardized comparison) and quality improvement, providing a model for assessing the impact of standards [48].
- Search Strategy: Systematically search three major databases (PubMed, Web of Science, Scopus) using defined keywords related to benchmarking and quality improvement.
- Study Selection: Apply pre-defined inclusion and exclusion criteria. For example, include only articles that empirically assess the relationship between benchmarking and clinical outcomes/processes across at least two entities over time.
- Data Extraction and Quality Assessment: Use a standardized tool to extract data on authors, year, clinical area, effect on quality, and type of interventions used alongside benchmarking. Assess study quality with an appropriate tool for diverse research designs.
- Data Synthesis: Synthesize the evidence according to established guidelines (e.g., PRISMA). Categorize results by process and outcome domains to determine if benchmarking stimulates quality improvement [48].
Visualizing the Development and Application of Reporting Standards
The following diagrams illustrate the workflow for creating reporting standards and the logical structure of their core components.
This table details key conceptual tools and frameworks essential for conducting and reporting rigorous empirical bioethics research.
| Tool or Framework | Function in Empirical Bioethics Research |
|---|---|
| Consensus Standards (e.g., Ives et al.) | Provides a set of 15 agreed-upon standards across 6 domains (Aims, Integration, Conduct etc.) to guide research design, execution, and reporting, thereby ensuring transparency and scholarly rigor [10]. |
| Modified Delphi Method | Offers a structured process for building consensus among experts on complex topics like methodology, balancing diverse viewpoints to establish legitimate and inclusive guidelines [10]. |
| Mixed Methods Research (MMR) Guidelines | Provides frameworks for effectively integrating quantitative and qualitative components, which is a core challenge in empirical bioethics. These guidelines help in transparently reporting how integration was achieved [47]. |
| Quality Assessment Tool (QATSDD) | A critical appraisal tool for reviewing studies with diverse designs, allowing for the systematic evaluation of the methodological quality of empirical research included in reviews or used as a model [48]. |
| Ethical Benchmarking Frameworks | Tools like the Moral Foundations Questionnaire (MFQ) and moral dilemma scenarios, adapted from moral psychology, provide structured methods for evaluating the ethical reasoning and alignment of research outputs or AI systems used in research [49]. |
Navigating Methodological Pitfalls and Enhancing Research Quality
The integration of empirical data with normative analysis represents a core challenge in advancing methodological rigor in empirical bioethics research. Over the last few decades, bioethics has witnessed a significant "empirical turn," with the proportion of empirical publications in bioethics journals increasing from 5.4% in 1990 to 17.8% by 2015 [50]. This trend reflects growing recognition that abstract philosophical principles require grounding in real-world contexts and experiences. Despite this growth, fundamental tensions persist in bridging the methodological divide between descriptive research (what is) and normative inquiry (what ought to be).
This guide examines the common integration failures that undermine methodological rigor in empirical bioethics research, providing researchers with evidence-based frameworks for identifying and resolving these gaps. By comparing predominant integration approaches and their failure patterns, we aim to equip bioethics researchers with practical methodologies for strengthening their research designs and achieving more robust ethical analyses.
The Landscape of Empirical-Normative Integration
Defining the Integration Challenge
Empirical bioethics is an interdisciplinary activity that centers around the integration of empirical findings with normative philosophical analysis [51]. This integration aims to inform abstract principles with workable practices and ensure bioethicists remain connected to the actual experiences of those affected by ethical decisions [50]. The fundamental challenge lies in reconciling two distinct epistemological traditions: the descriptive orientation of social science research methods with the prescriptive nature of ethical analysis [3].
A survey of bioethics scholars across twelve European countries revealed that while most respondents (87.5%) used or had used empirical methods in their work, only approximately one-third (35%) reported having successfully integrated empirical data with normative analysis [42]. This indicates a significant implementation gap between methodological aspiration and execution.
Prevalence of Empirical Approaches in Bioethics
Table 1: Growth of Empirical Research in Bioethics Journals
| Time Period | Percentage of Empirical Papers | Key Trends |
|---|---|---|
| 1990 | 5.4% | Early stage of empirical turn |
| 2003 | 15.4% | Significant increase noted |
| 2004-2015 | 18.1% | Stabilization of empirical presence |
| 2004 | 14.9% | Baseline for recent period |
| 2015 | 17.8% | Current prevalence |
Analysis of nine prominent bioethics journals between 2004-2015 found that 18.1% of original papers collected and analyzed empirical data [50]. The Journal of Medical Ethics and Nursing Ethics collectively accounted for 89.4% of all empirical papers, with the former publishing significantly more quantitative studies and the latter favoring qualitative approaches [50].
Common Integration Failures: Identification and Analysis
Failure 1: Poorly Defined Methodological Requirements
The most fundamental integration failure stems from inadequately specified requirements for how empirical and normative components will interrelate within a research design. This mirrors system integration failures where "overlooked or poorly defined requirements" lead to solutions that don't meet stakeholder expectations [52].
In bioethics, this manifests as:
- Unclear epistemological relationships between descriptive data and normative claims
- Insufficient specification of how empirical findings will inform ethical analysis
- Ambiguity regarding the weight given to empirical evidence versus philosophical reasoning
This failure mode is particularly prevalent in early-career researchers, with surveys indicating that more than a fifth (22.9%) of empirical researchers in bioethics had not received any methodological training [42].
Failure 2: Methodological Design Weaknesses
Integration designs often suffer from flaws influenced by disciplinary biases or methodological limitations. As noted in system integration, design weaknesses can create solutions with "hidden flaws that only surface when tested in real-world conditions" [52].
In empirical bioethics, these design flaws include:
- Choosing inappropriate methodological approaches for the research question
- Facing technical constraints with qualitative or quantitative platforms
- Deploying inefficient architectures that cannot handle the complexity of empirical-normative integration
- Creating methodological frameworks that cannot adapt to unexpected findings
These design weaknesses reflect what one scholar identifies as the absence of "clear standards for answering bioethical questions" due to researchers having "different goals and apply[ing] different methods" [3].
Failure 3: Insufficient Methodological Training and Expertise
The interdisciplinary nature of empirical bioethics creates unique personnel-related challenges. Surveys reveal significant training deficiencies, with only 6% or less of empirical researchers considering themselves experts in the methods they used [42]. This skills gap directly impacts integration quality, as success "depends on the resources allocated to it" [52].
Key personnel-related integration failures include:
- Limited availability of researchers with dual methodological expertise
- Insufficient technical competence in both empirical and normative methods
- Self-imposed constraints due to limited methodological experiences
- The rarity of researchers capable of rigorous interdisciplinary work
Failure 4: Procedural Vagueness in Integration Processes
Perhaps the most distinctive failure mode in empirical bioethics is the procedural vagueness surrounding how integration actually occurs. Despite the availability of many empirical bioethics methodologies, the integration process often remains obscure [51]. Researchers describe an "air of uncertainty and overall vagueness" that surrounds integration methods [51].
This vagueness manifests as:
- Unclear steps for moving between empirical data and normative analysis
- Ambiguity about how much weight to give empirical data versus ethical theory
- Lack of transparency in how integration methods are executed
- Insufficient documentation of the back-and-forth process between components
A systematic review identified thirty-two distinct methodologies for integrating empirical and normative approaches, yet many lack specificity in their practical application [51].
Failure 5: Inadequate Validation and Quality Assurance
Integration failures frequently occur during the validation phase, where there is insufficient testing of the relationship between empirical findings and normative conclusions. This parallels system integration where "insufficient testing" and "lack of governance" lead to undetected flaws [52].
In bioethics, this includes:
- Failure to establish criteria for validating integrated conclusions
- Inadequate peer review processes for interdisciplinary work
- Lack of consensus on quality standards for integrated research
- Unvalidated assumptions about the relationship between facts and values
This challenge is compounded by what scholars identify as the absence of "agreed-upon criteria to determine when the application of methods to inquire into a particular question can be said to yield truthful and valid results" [3].
Experimental Protocols for Assessing Integration Methodologies
Protocol 1: Reflective Equilibrium Testing
Reflective equilibrium represents a commonly cited though often vaguely implemented integration methodology. The following protocol provides a structured approach for implementation:
Objective: To systematically test the use of reflective equilibrium for integrating empirical findings with normative principles.
Procedures:
- Initial Normative Framework Establishment: Document pre-existing ethical principles, theories, and considered judgments relevant to the research question.
- Empirical Data Collection: Gather empirical data through qualitative or quantitative methods appropriate to the ethical issue.
- Iterative Comparison Process: Systematically compare empirical findings with normative framework, identifying areas of alignment and tension.
- Adjustment Phase: Modify either normative judgments or interpretation of empirical data to achieve coherence.
- Equilibrium Assessment: Evaluate whether sufficient coherence has been achieved between revised normative framework and empirical observations.
- Validation: Test the resulting equilibrium against novel cases or counterexamples.
Validation Metrics:
- Transparency of documentation at each phase
- Systematic handling of discrepant data
- Credibility of resulting coherence to interdisciplinary reviewers
- Practical applicability to original ethical problem
Protocol 2: Dialogical Integration Assessment
Dialogical methods emphasize stakeholder engagement in the integration process rather than researcher-driven analysis:
Objective: To evaluate the effectiveness of structured stakeholder dialogues in integrating empirical and normative perspectives.
Procedures:
- Stakeholder Mapping: Identify relevant stakeholders representing empirical, normative, and affected party perspectives.
- Dialogue Framework Development: Create structured discussion protocols that explicitly address empirical-normative intersections.
- Facilitated Dialogue Sessions: Conduct moderated discussions focusing on tensions between observed practices and ethical standards.
- Iterative Reflection: Engage participants in reflecting on how empirical insights challenge or reinforce normative positions.
- Consensus Building: Work toward mutually acceptable resolutions that incorporate both empirical realities and ethical commitments.
- Output Documentation: Record the process of negotiation and justification for integrated outcomes.
Validation Metrics:
- Inclusivity of stakeholder representation
- Depth of engagement with empirical-normative tensions
- Credibility of outcomes to all stakeholder groups
- Actionability of resulting ethical guidance
Visualization of Integration Relationships and Failure Points
Diagram 1: Empirical-Normative Integration Failure Pathways. This workflow maps relationships between empirical and normative components, highlighting common failure points in the integration process.
Research Reagent Solutions: Methodological Tools for Integration
Table 2: Essential Methodological Resources for Empirical-Normative Integration
| Methodological Tool | Function | Application Context |
|---|---|---|
| Reflective Equilibrium Protocol | Provides structured process for achieving coherence between empirical data and normative judgments | Suitable for researcher-driven integration projects |
| Dialogical Engagement Framework | Facilitates stakeholder participation in integration process | Appropriate for practice-oriented research with multiple stakeholders |
| Mixed Methods Research Design | Enables coordinated collection and analysis of both qualitative/quantitative and normative data | Useful for complex research questions requiring multiple evidence types |
| Integration Validation Checklist | Systematically assesses quality of empirical-normative integration | Applicable across methodologies as quality assurance mechanism |
| Transparency Documentation Template | Standardizes reporting of integration processes and decisions | Essential for peer review and methodological replication |
Comparative Analysis of Integration Approaches
Table 3: Methodological Comparison of Empirical-Normative Integration Approaches
| Integration Method | Failure Rate Indicators | Training Requirements | Implementation Complexity | Output Robustness |
|---|---|---|---|---|
| Reflective Equilibrium | High (vagueness in application) | Moderate philosophical training | Medium | Variable |
| Dialogical Models | Medium (stakeholder selection bias) | High facilitation skills | High | Context-dependent |
| Grounded Moral Analysis | Medium (theoretical grounding) | Mixed methods expertise | High | Moderate-high |
| Consultative Approaches | Low-Medium (researcher bias) | Discipline-specific mastery | Low-Medium | Consistent |
| Hybrid Methodologies | Variable (integration points) | Advanced interdisciplinary training | Very High | Potentially High |
The resolution of empirical-normative integration failures requires systematic attention to methodological rigor at each stage of the research process. Based on our analysis of common failure patterns, successful integration depends on: (1) explicit specification of epistemological relationships between empirical and normative components; (2) investment in interdisciplinary methodological training; (3) implementation of structured validation processes; and (4) enhanced transparency in reporting integration procedures.
Future methodological development should focus on creating more determinate guidelines for integration processes while maintaining the flexibility needed to address diverse research questions. Additionally, bioethics education programs must implement more rigorous training in both empirical methods and integration methodologies to ensure researchers possess the necessary skills to navigate the complex terrain between empirical evidence and normative analysis [42]. By addressing these core integration failures, the field can strengthen its methodological foundations and enhance its capacity to generate ethically robust, empirically informed guidance for complex healthcare challenges.
Empirical bioethics is an interdisciplinary field that integrates empirical findings with normative (philosophical) analysis to address complex ethical issues in biomedicine and healthcare [51]. Despite the proliferation of methodologies—a systematic review identified 32 distinct empirical bioethics methodologies—the process of integrating empirical research with normative analysis often remains opaque and frustratingly vague [51] [2]. This methodological ambiguity presents significant challenges for researchers, funders, and journals seeking to conduct, evaluate, and publish rigorous empirical bioethics research [2].
The fundamental challenge centers on how to validly move from empirical "is" to normative "ought" claims, navigating ontological and epistemological questions while bridging disciplinary divides [2]. Many researchers attempting to integrate normative and empirical approaches report experiencing uncertainty about appropriate methodologies, with existing frameworks often providing insufficient practical guidance for implementation [51]. This article examines these methodological challenges and provides structured approaches for justifying research choices, offering comparative analysis of predominant methodologies, practical protocols, and visualization of workflows to enhance methodological rigor and transparency in empirical bioethics research.
Comparative Analysis of Empirical Bioethics Methodologies
Predominant Methodological Approaches
Table 1: Comparison of Primary Integration Methodologies in Empirical Bioethics
| Methodology | Core Integration Mechanism | Primary Strengths | Documented Limitations |
|---|---|---|---|
| Reflective Equilibrium | Back-and-forth process until moral coherence achieved [51] | Familiar to ethicists; systematic approach | Vagueness in weighting empirical vs. theoretical elements [51] |
| Dialogical Empirical Ethics | Stakeholder dialogue to reach shared understanding [51] | Incorporates multiple perspectives; collaborative | Risk of subjective application of ethical theories [51] |
| Reflexive Balancing | Researcher-driven analysis of data [51] | Clear researcher responsibility | Dependent on researcher's analytical skills |
| Symbiotic Ethics | Intertwining empirical and normative from project start [51] | Avoids artificial separation; more natural integration | Requires sophisticated understanding of both domains |
| Grounded Moral Analysis | Normative analysis emerges from empirical data [51] | Grounded in practical realities | Risk of insufficient theoretical foundation |
The systematic review by Davies et al. (2015) categorized these methodologies into three primary types: (1) dialogical approaches that rely on dialogue between stakeholders to reach shared understanding; (2) consultative approaches where researchers analyze data independently to develop normative conclusions; and (3) hybrid approaches that combine both dialogical and consultative elements [51]. Each approach presents different advantages and challenges regarding implementation, with significant variation in how much weight is given to empirical data versus ethical theory [51].
Consensus Standards for Empirical Bioethics Research
Table 2: Domains and Standards for Empirical Bioethics Research Practice
| Domain | Standard Number | Standard Description | Implementation Guidance |
|---|---|---|---|
| Aims | 1 | Address a normative issue oriented toward practice [2] | Clearly articulate the practical ethical problem being addressed |
| Questions | 2 | Integrate empirical methods with ethical argument [2] | Explicitly connect research questions to both empirical and normative goals |
| Integration | 3 | Justify method of integration and theoretical position [2] | Provide transparent rationale for chosen integrative methodology |
| Empirical Work | 4-7 | Appropriate design, recruitment, data collection, and analysis [2] | Follow disciplinary standards for empirical research quality |
| Normative Work | 8-10 | Rigorous analysis, argumentation, and justification [2] | Employ philosophical rigor in ethical analysis and reasoning |
| Training & Expertise | 11-15 | Relevant expertise in both empirical and normative methods [2] | Ensure research team possesses necessary interdisciplinary competencies |
A consensus project involving 16 academics from 5 European countries established 15 standards of practice organized into these 6 domains, providing a framework for assessing methodological rigor in empirical bioethics research [2]. These standards emphasize that high-quality empirical bioethics must clearly state how theoretical positions are chosen for integration, explain and justify how integration methods are carried out, and maintain transparency in reporting how integration was executed [2].
Experimental Protocols and Workflows
Protocol for Reflective Equilibrium Implementation
The reflective equilibrium methodology, while commonly referenced, requires careful implementation to avoid vagueness. The following protocol provides a structured approach:
Phase 1: Initial Ethical Framework Establishment
- Document initial ethical principles, values, and considered judgments relevant to the research question
- Identify potential conflicts or tensions between these elements
- Establish preliminary weighting of different ethical considerations based on theoretical foundations
Phase 2: Empirical Data Collection and Analysis
- Design empirical study specifically to inform identified ethical considerations
- Collect data using appropriate qualitative or quantitative methods
- Analyze empirical findings with specific attention to implications for initial ethical framework
Phase 3: Iterative Reconciliation Process
- Systematically compare empirical findings with initial ethical framework
- Identify where empirical data challenges, supports, or complicates initial judgments
- Modify either initial judgments or theoretical commitments to achieve greater coherence
- Document all modifications with justifications for each adjustment
Phase 4: Equilibrium Assessment
- Evaluate whether achieved coherence represents defensible moral positions
- Test equilibrium against hypothetical cases and potential counterarguments
- Determine whether further iterations are needed or equilibrium has been sufficiently achieved
This protocol addresses the documented vagueness in traditional reflective equilibrium approaches by providing explicit structure to the "back-and-forth" process researchers described [51].
Consensus Development Protocol for Standards Establishment
The modified Delphi approach used to develop empirical bioethics standards provides a replicable protocol for methodological development:
Diagram 1: Consensus development workflow for methodological standards
This structured consensus process enabled diverse academics with different methodological commitments to reach agreement on standards of practice, demonstrating how collaborative approaches can address methodological ambiguity [2]. The process was particularly valuable for navigating the linguistic and conceptual diversity of an interdisciplinary field, allowing immediate clarification and response to ambiguous or controversial issues [2].
Visualization of Methodological Relationships
Interdisciplinary Integration Pathways
Diagram 2: Interdisciplinary integration pathways in empirical bioethics
This visualization illustrates the primary pathways through which empirical and normative elements interact in different methodological approaches, highlighting both the distinct processes and shared goals of integration.
Table 3: Research Reagent Solutions for Empirical Bioethics Methodology
| Tool Category | Specific Method/Approach | Primary Function | Implementation Considerations |
|---|---|---|---|
| Integration Frameworks | Reflective Equilibrium | Achieve coherence between empirical data and normative claims [51] | Requires explicit weighting of elements; document iterations |
| Dialogical Methods | Stakeholder Deliberation | Incorporate multiple perspectives in normative analysis [51] | Ensure representative participation; manage power dynamics |
| Consensus Development | Modified Delphi Technique | Establish methodological standards through expert input [2] | Balance anonymity with needed clarification opportunities |
| Empirical Quality Standards | Disciplinary Best Practices | Ensure empirical component meets methodological rigor [2] | Adapt standards from relevant social scientific disciplines |
| Normative Quality Standards | Philosophical Argumentation | Ensure rigorous ethical analysis and justification [2] | Maintain logical consistency; address counterarguments |
| Transparency Mechanisms | Explicit Methodological Reporting | Document integration process for assessment and replication [2] | Pre-register integration approach; report deviations |
These methodological "reagents" provide researchers with essential tools for designing, implementing, and reporting empirical bioethics research that successfully navigates the challenges of interdisciplinary integration.
Discussion: Navigating Methodological Ambiguity
The persistence of methodological ambiguity in empirical bioethics reflects both the inherent challenges of interdisciplinary work and the field's ongoing development [51] [45]. This analysis demonstrates that while no single methodology has emerged as universally superior, researchers can employ several strategies to enhance methodological rigor and justification of research choices.
First, the conscious selection and explicit justification of integration methodologies is essential. Researchers should carefully consider whether dialogical, consultative, or hybrid approaches best suit their research questions and theoretical commitments, then transparently document this choice [51] [2]. Second, adherence to established standards—such as the 15 consensus standards—provides a framework for ensuring methodological rigor across multiple domains of research practice [2]. Third, structured implementation of chosen methodologies, using detailed protocols like those outlined in this article, addresses the vagueness that often characterizes integration approaches [51].
The flexibility of empirical bioethics methodologies is both a strength and a challenge [51]. While it allows researchers to tailor approaches to specific research questions and contexts, it also creates ongoing ambiguity about appropriate methodological choices. By employing the comparative frameworks, experimental protocols, and methodological tools presented here, researchers can more confidently navigate this ambiguity while producing empirically grounded and normatively justified research outcomes that advance both theory and practice in bioethics.
Interdisciplinary research integrates methods, concepts, and theories from multiple disciplines to address complex problems that cannot be adequately resolved within a single disciplinary framework [3]. In empirical bioethics and drug development, this approach is increasingly essential for addressing multifaceted challenges that span scientific, ethical, and social dimensions [2]. The integration of diverse epistemological frameworks—the underlying beliefs about what constitutes valid knowledge, appropriate evidence, and rigorous methods—presents both significant opportunities and substantial challenges for research teams [53]. When disciplinary perspectives with different epistemological systems collaborate, the potential for innovative solutions increases, but so does the risk of misunderstanding, conflict, and the predominance of one disciplinary perspective over others, a phenomenon known as disciplinary capture [53].
The management of diverse epistemologies is particularly crucial in empirical bioethics, where researchers must navigate the methodological tensions between empirical research (which describes what "is") and normative analysis (which determines what "ought" to be) [2]. Successfully addressing these epistemological divides requires deliberate strategies to create conditions where diverse forms of disciplinary expertise can contribute meaningfully to shared research goals [54]. This guide compares approaches to managing epistemological diversity, examines their relative effectiveness, and provides practical frameworks for optimizing collaborative research practices in scientific and drug development contexts.
Comparative Analysis of Collaboration Challenges and Solutions
Epistemological Obstacles in Interdisciplinary Collaboration
Interdisciplinary collaborations frequently encounter specific, predictable challenges rooted in fundamental differences in how disciplines conceptualize research problems and validate knowledge. These challenges can undermine collaboration effectiveness if not properly addressed [55].
Table 1: Epistemological Obstacles in Interdisciplinary Research
| Obstacle Category | Description | Impact on Collaboration |
|---|---|---|
| Differing Causal Concepts | Disciplines vary in how they conceptualize causation (mechanistic, intentional, emergent) [53] | Leads to conflicting explanations of phenomena; natural scientists may prefer mechanistic causes while social scientists incorporate social norms and intentions |
| Evidentiary Standards | Disagreements about what constitutes sufficient evidence and proper methods [3] [53] | Creates tension over research design; laboratory-based controls vs. field-based observations; case studies vs. generalized claims |
| Research Goals & Values | Varying conceptions of what research should accomplish and what makes it meaningful [53] | Results in misaligned expectations about outcomes; theoretical knowledge vs. practical application; publication vs. implementation |
| Communication Barriers | Disciplinary jargon, conceptual frameworks, and implicit assumptions [54] | Hinders effective communication and mutual understanding; team members talk past each other using discipline-specific terminology |
| Integration Difficulties | Challenges in combining insights from different epistemological frameworks [55] | Leads to superficial collaboration where disciplines work in parallel without genuine integration of perspectives |
Disciplinary Capture: Mechanisms and Consequences
A significant risk in interdisciplinary work is disciplinary capture, where research decisions—about relevant facts, methods, standards of evidence, causes, and research goals—default to the epistemological framework of a single dominant discipline [53]. This often occurs unintentionally through rational decision-making processes, such as adopting the framework of better-funded disciplines or making early methodological choices that constrain later decisions [53]. The consequences are particularly evident in collaborations between natural and social scientists, where social scientists frequently report feeling ineffective in shaping project outcomes despite their formal inclusion [53].
Quantitative Assessment of Collaboration Frameworks
Research has evaluated various approaches to managing epistemological diversity in interdisciplinary teams. The table below summarizes the effectiveness of different frameworks based on empirical studies of interdisciplinary collaborations.
Table 2: Comparison of Interdisciplinary Collaboration Frameworks
| Collaboration Framework | Key Principles | Effectiveness Metrics | Limitations |
|---|---|---|---|
| Epistemic Control Framework [54] | Develops metacognitive understanding through sequenced steps: epistemic awareness, humility, empathy, and control | Enhanced communication; creative problem-solving; meaningful epistemic shifting | Requires significant time investment; depends on facilitator skill |
| Engineering Paradigm [55] | Emphasizes practical problem-solving; constructs knowledge for specific epistemic tasks | Effective for localized projects with clear research questions; accommodates pluralism | May sacrifice theoretical depth for practical utility |
| Consensus Standards Approach [2] | Establishes agreed-upon standards of practice through modified Delphi method | Improves research quality; provides clear evaluation criteria; strengthens community of practice | May constrain methodological innovation; difficult to achieve broad buy-in |
| Trading Zones Concept [53] | Creates shared spaces for collaboration without requiring full epistemological integration | Facilitates short-term cooperation; allows boundary-crossing communication | Risk of superficial engagement; may not achieve deep integration |
Experimental Protocols and Methodological Standards
Establishing Methodological Rigor in Interdisciplinary Research
The development of methodological standards for interdisciplinary research in empirical bioethics provides a valuable case study in managing epistemological diversity. A consensus project utilizing a modified Delphi approach with 16 academics from 5 European countries established 15 standards of practice organized into 6 domains [2]. This rigorous methodology involved iterative rounds of discussion and feedback, allowing experts from different disciplinary backgrounds to articulate shared standards while respecting epistemological differences.
The consensus process addressed fundamental challenges of interdisciplinary quality assessment, including how to evaluate research that integrates diverse methodological approaches with different standards of rigor [3]. The resulting standards provide a framework for ensuring methodological rigor without imposing a single epistemological perspective, thus maintaining the rich diversity of disciplinary approaches while establishing shared quality benchmarks [2].
Detailed Experimental Protocol: Modified Delphi Method for Standard-Setting
The modified Delphi method used in establishing empirical bioethics standards offers a replicable protocol for managing epistemological diversity in interdisciplinary teams [2]:
Participant Selection: Assemble a diverse group of experts (16 academics from 5 countries with different disciplinary backgrounds) to ensure representation of multiple epistemological perspectives.
Structured Discussion: Conduct facilitated group discussions (2.5 days) that allow immediate response and clarification of ambiguous or controversial issues, essential when participants have different conceptual understandings.
Consensus Building: Iteratively refine positions through structured feedback that summarizes group views and identifies areas of agreement and disagreement.
Standard Articulation: Develop precise, concrete guidance for (a) identifying core characteristics, (b) planning, (c) conducting, and (d) reporting interdisciplinary research.
Implementation Framework: Create mechanisms for ongoing engagement and refinement of standards by the broader research community.
This protocol successfully addressed the challenge of "conceptual and linguistic diversity" in interdisciplinary work by prioritizing direct verbal communication and immediate clarification over anonymous questionnaires typically used in Delphi methods [2].
Visualization of Epistemological Management Frameworks
Sequential Development of Epistemic Control
The epistemic control framework provides a structured pathway for developing collaborative capacity across epistemological boundaries [54]. This sequenced approach enables researchers to progressively build the metacognitive skills necessary for effective interdisciplinary work.
Interdisciplinary Research Workflow with Epistemological Safeguards
Effective management of epistemological diversity requires integrating specific checkpoints throughout the research process to prevent disciplinary capture and ensure meaningful inclusion of diverse perspectives.
Successful navigation of epistemological diversity requires specific conceptual tools and resources. The following table details essential "research reagents" for interdisciplinary collaboration, analogous to laboratory reagents in experimental science.
Table 3: Essential Resources for Managing Epistemological Diversity
| Tool Category | Specific Resource | Function & Application |
|---|---|---|
| Conceptual Frameworks | Epistemic Control Framework [54] | Provides sequenced pathway for developing metacognitive understanding across disciplines |
| Communication Protocols | Modified Delphi Method [2] | Structured approach for achieving consensus among diverse epistemological perspectives |
| Integration Mechanisms | Engineering Paradigm of Science [55] | Emphasizes practical problem-solving and knowledge construction for specific tasks |
| Analytical Tools | Disciplinary Capture Diagnostics [53] | Identifies when one discipline's epistemological framework dominates collaboration |
| Institutional Supports | Extended Funding Timelines [53] | Provides necessary time for deep epistemological integration and relationship building |
| Training Resources | Epistemic Empathy Development [54] | Builds capacity to understand and appreciate different epistemic frameworks |
Effectively managing diverse epistemologies in interdisciplinary research requires deliberate strategies that go beyond simply assembling experts from different fields. The most successful approaches combine structured frameworks for developing epistemic awareness and control with practical safeguards against disciplinary capture [54] [53]. Quantitative assessment of collaboration models demonstrates that approaches emphasizing metacognitive development, explicit attention to epistemological differences, and systematic integration processes yield significantly better outcomes in terms of research innovation, participant satisfaction, and practical impact [54] [2].
For researchers, scientists, and drug development professionals, implementing these evidence-based approaches to epistemological management can transform interdisciplinary collaborations from frustrating exercises in cross-disciplinary translation into generative spaces for creative problem-solving. By treating epistemological diversity as a resource rather than an obstacle, research teams can more effectively address the complex challenges at the intersection of science, ethics, and society.
A critical challenge in empirical bioethics research is the integration of empirical data with normative analysis. This guide compares methodological approaches based on their adherence to principles of theoretical transparency, a core component of methodological rigor. The evaluation focuses on how different frameworks explicitly state their philosophical assumptions and justify the integration of descriptive and ethical reasoning.
The following data on researcher practices and methodological characteristics were synthesized from empirical studies on bioethics and mixed methods research. This comparison highlights the current state of theoretical transparency in the field.
Table 1: Empirical Research Practices in Bioethics
A survey of bioethics researchers across 12 European countries (n=200) revealed the following practices and training related to empirical-normative integration [56]:
| Practice or Characteristic | Percentage of Researchers |
|---|---|
| Use or have used empirical methods | 87.5% |
| Received at least some qualitative methods training | 61.0% |
| Received at least some quantitative methods training | 59.0% |
| "Empirical researchers" with no methodological training | 22.9% |
| Self-identified experts in methods they have used | ≤6.0% |
| Reported integration of empirical data with normative analysis in past work | 35.0% |
| Plan integration in current projects | 59.8% |
Table 2: Methodological Characteristics for Assessing Theoretical Transparency
This table compares key methodological features that contribute to methodological rigor, based on analysis of reporting standards in mixed methods research [47].
| Methodological Feature | High Transparency | Common Deficiencies |
|---|---|---|
| Stating Philosophical Assumptions | Explicitly states normative framework (e.g., Principlism) and its influence on research questions. | Assumptions remain implicit or unstated, leading to unclear justification for moral claims. |
| Describing Integration Procedures | Clearly details how and at what stage quantitative and qualitative findings are integrated. | Integration process is mentioned but not described transparently, making it difficult to evaluate. |
| Communicating Unique Insights | Articulates how integration generated meta-inferences not possible with a single method. | Fails to communicate the added value of the mixed methods approach within word count limitations. |
| Reporting Methodological Rigor | Reports steps taken to ensure reliability and validity for both quantitative and qualitative components. | Omits reporting of key steps in the research process, compromising evaluability of findings. |
Detailed Experimental Protocols
To ensure methodological rigor and theoretical transparency, the following protocols outline standardized procedures for key research activities in empirical bioethics.
Protocol 1: Framework Justification and Assumption Documentation
This protocol ensures that the ethical framework guiding a study is explicitly stated and justified.
- Framework Selection: Prior to study design, researchers must document the selection of a specific normative framework (e.g., Beauchamp and Childress's four principles, Utilitarianism, Deontology) [57] [58]. The documentation must include the rationale for its selection over alternative frameworks.
- Assumption Elicitation: Research teams will conduct structured brainstorming sessions to identify and record all underlying assumptions about the research topic, the chosen framework, and the potential relationship between empirical data and normative analysis.
- Stakeholder Review: The documented framework and assumptions will be reviewed by a multi-disciplinary panel, including at least one expert in philosophical ethics and one in social science research methods, to challenge and refine the assumptions.
- Study Design Integration: The final, documented assumptions will be used to explicitly shape the research questions, data collection instruments (e.g., ensuring survey questions can generate data relevant to the chosen ethical principles), and the plan for analysis.
Protocol 2: Integrated Data Analysis for Empirical Bioethics
This protocol details the process for integrating quantitative and qualitative data to generate normative insights, a defining feature of rigorous mixed methods research [47].
- Independent Analysis: Quantitative and qualitative data are analyzed separately using standard statistical and thematic analysis techniques, respectively.
- Data Transformation for Integration: Create a "joint display" table. This table places findings from the quantitative analysis (e.g., "85% of respondents agreed with statement X") directly adjacent to related qualitative findings (e.g., "Interview themes revealed that agreement was driven by value Y").
- Normative Interrogation: Systematically compare the two columns of data in the joint display. The documented ethical framework from Protocol 1 is used to interrogate the findings. For example: "How does the principle of autonomy help us interpret the tension between the high survey agreement and the qualitative expressions of coercion?"
- Inference Development: Formulate "meta-inferences"—conclusions that draw on both the empirical data and the normative framework. The research report must clearly trace how each meta-inference was generated from this integrative process.
Logical Workflow and Signaling Pathways
The following diagram illustrates the sequential logic and critical decision points for establishing theoretical transparency in a research study.
The Scientist's Toolkit: Research Reagent Solutions
This table details essential conceptual "reagents" and their functions in constructing methodologically rigorous and theoretically transparent empirical bioethics research.
Table 3: Essential Conceptual Tools for Empirical Bioethics
| Tool Name | Function in Research |
|---|---|
| Defined Ethical Framework | Provides the normative structure for the study. Examples include Principlism (Beneficence, Nonmaleficence, Autonomy, Justice) or a Social Justice framework [57] [58]. Its primary function is to justify the normative claims made from empirical data. |
| Joint Display Analysis Table | A methodological tool used during data integration. Its function is to visually juxtapose quantitative and qualitative findings, facilitating direct comparison and the generation of meta-inferences [47]. |
| Meta-Inference Validation Checklist | A quality control tool. Its function is to ensure that conclusions drawn from the integrated data are coherent, logically derived from both data types, and address potential divergent findings [47]. |
| Color-Accessible Visualization Palette | A communication tool. Its function is to ensure that all data charts and conceptual diagrams are interpretable by audiences with color vision deficiencies, adhering to WCAG guidelines for contrast (e.g., 4.5:1 minimum) [59] [60] [61]. |
| Methodological Rigor Reporting Checklist | A standardized reporting tool, often based on guidelines like the MIRRI. Its function is to ensure transparent reporting of all key research process steps, allowing readers to evaluate the validity and reliability of the study's inferences [47]. |
Empirical bioethics has emerged as a distinct interdisciplinary field that integrates empirical social scientific research with ethical analysis to draw normative conclusions [2]. This integration aims to resolve real-world bioethics dilemmas in clinical, biomedical, and public health decision-making, policy, and practice [62]. The field promises significant contributions to addressing pressing health care challenges but faces fundamental challenges related to ontological, epistemological, and methodological questions about how to bridge the empirical "is" and the normative "ought" [2].
The complexity of contemporary bioethics problems, particularly those involving digital technologies, artificial intelligence in health care, and innovative drug development, necessitates robust approaches to training and expertise development [63]. As the field continues to evolve, consensus on standards of practice becomes increasingly important for establishing empirical bioethics as a distinct community of practice with specific methodological norms and aims [2]. This article examines current approaches to building interdisciplinary competence, comparing methodological frameworks and training strategies that enhance methodological rigor in empirical bioethics research.
Comparative Analysis of Disciplinary Contributions
Table 1: Disciplinary Contributions to Empirical Bioethics Research
| Discipline | Core Methodological Approaches | Contributions to Empirical Bioethics | Training Requirements |
|---|---|---|---|
| Philosophical Ethics | Conceptual analysis, normative reasoning, reflective equilibrium | Provides frameworks for ethical analysis and normative justification; clarifies value concepts | Advanced training in moral theory, ethical frameworks, analytical philosophy |
| Social Sciences | Qualitative interviews, focus groups, ethnographic observation, quantitative surveys | Generates empirical data on stakeholder perspectives, contextual factors, ethical dilemmas | Methodological training in data collection, analysis, interpretation of social phenomena |
| Clinical/ Biomedical Research | Clinical trials, outcome measurement, biomarker validation | Provides understanding of medical contexts, patient experiences, clinical realities | Clinical knowledge, understanding of healthcare systems and research methodologies |
| Legal Studies | Legal analysis, case review, regulatory assessment | Informs policy recommendations, analyzes regulatory frameworks, assesses legal implications | Training in health law, regulatory frameworks, policy analysis |
The integration of these diverse disciplines creates a complex training landscape. Researchers must develop T-shaped expertise – deep knowledge in one primary discipline coupled with broad understanding of related fields and the skill to facilitate collaborative integration [2]. This expertise enables teams to specify bioethics problems that clinicians, researchers, policymakers, and others face in their daily work and facilitate practical resolutions [62].
Methodological Frameworks for Interdisciplinary Research
Consensus Standards for Empirical Bioethics
A consensus finding project utilizing a modified Delphi approach with 16 academics from 5 European countries established 15 standards of practice for empirical bioethics research, organized into 6 domains [2]. Within training and expertise, these standards emphasize that researchers must possess:
- Methodological competence in both empirical and normative approaches
- Interdisciplinary understanding of how different disciplines conceptualize and approach bioethical issues
- Reflective capacity to understand the relationship between empirical findings and normative conclusions
The consensus process highlighted that because there is no standard approach to cite and no accepted methodology or set of methods to fall back on, researchers must provide justification for every methodological choice from first principles [2]. This places additional importance on comprehensive training that enables such justification.
Experimental Protocols for Integrated Methodology
Table 2: Research Reagent Solutions for Empirical Bioethics
| Research Component | Essential Methodological Tools | Function in Empirical Bioethics |
|---|---|---|
| Empirical Data Collection | Semi-structured interview guides, focus group protocols, survey instruments, observational frameworks | Captures stakeholder perspectives, contextual factors, and practical realities of ethical dilemmas |
| Normative Analysis | Ethical frameworks (e.g., principlism), case-based reasoning, reflective equilibrium | Provides structured approach to ethical analysis and justification of normative conclusions |
| Integration Methods | Iterative analysis protocols, deliberative workshops, joint interpretation sessions | Facilitates meaningful integration of empirical findings with ethical reasoning |
| Quality Assessment | Intercoder reliability measures, validity checks, peer debriefing, transparency documentation | Ensures methodological rigor and trustworthiness of both empirical and normative components |
Diagram 1: Empirical Bioethics Research Workflow. This diagram illustrates the parallel development and subsequent integration of empirical and normative components in empirical bioethics research.
Training Models and Competency Development
Structured Training Approaches
Multiple training models have emerged to address the complex competency requirements in empirical bioethics. The Australasian Association of Bioethics and Health Law has developed a specific Empirical Ethics stream that includes live debates, critical dialogues, podcast series, reading groups, and resource development for 'how to do empirical bioethics' launching in 2025 [64]. This structured approach provides multiple pathways for skill development.
Mentored projects represent another effective training model, in which postdoctoral fellows or early-career faculty work closely with experienced bioethics scholars [62]. These relationships facilitate knowledge transfer and development of practical skills through guided experience. Such mentorship is particularly valuable for navigating the challenges of interdisciplinary work, where standard approaches to data collection may need to be altered to generate data that can address specific bioethical aims [2].
Core Competency Domains
Successful training programs address four interconnected competency domains:
Methodological Competence: Development of skills in both empirical research methods and ethical analysis, with understanding of their respective quality standards.
Epistemological Awareness: Understanding of different forms of knowledge and how they contribute to addressing bioethical questions.
Integration Skills: Ability to meaningfully connect empirical findings with normative reasoning through appropriate methodologies.
Translational Capacity: Skill in disseminating research results to both academic and non-academic audiences, including policymakers, clinicians, and community stakeholders [62].
Training that addresses these competencies enables researchers to overcome the communication gaps that often exist between different disciplinary communities, such as those between pharmaceutical and computational science communities in AI-driven drug development [65].
Applications in Emerging Bioethics Domains
Digital Health and AI Ethics
The application of empirical bioethics to digital technologies in medicine, health care, and public health requires specific methodological adaptations [63]. Research in this domain must address emerging challenges such as algorithmic bias, data privacy, and the ethical implications of AI-driven clinical decision-making. Non-empirical methods commonly employed include conceptual analysis, reflective equilibrium, and principle-based approaches [63].
Training for digital health ethics must incorporate understanding of the technologies themselves, alongside their ethical implications. This requires collaboration between ethicists, computer scientists, clinicians, and policymakers to ensure comprehensive understanding of both technical and ethical dimensions.
Pharmaceutical Research and Development Ethics
Empirical bioethics plays a crucial role in addressing ethical challenges in pharmaceutical research and development, particularly as AI transforms drug discovery and clinical trials [65] [66]. Training for professionals in this domain must include understanding of clinical trial methodologies, regulatory frameworks, and the specific ethical challenges posed by innovative approaches such as digital twin technology [65].
The growth of AI in pharmaceutical research (with over 75 AI-derived molecules reaching clinical stages by the end of 2024) creates urgent need for ethical oversight that balances innovation with patient safety and welfare [66]. Empirical bioethics researchers working in this space require understanding of both the technical aspects of AI-driven drug development and the ethical frameworks for evaluating its implications.
Building competence across disciplines in empirical bioethics requires ongoing commitment to developing robust training frameworks, mentorship opportunities, and supportive institutional structures. As the field continues to evolve in response to emerging technologies and complex health care challenges, the development of researchers with T-shaped expertise – deep disciplinary knowledge combined with broad interdisciplinary understanding – becomes increasingly important.
The establishment of consensus standards for training and expertise provides a foundation for quality assurance in empirical bioethics research [2]. However, ongoing attention to methodological innovation, training program development, and supportive research infrastructure is necessary to ensure that the field can effectively address the complex bioethical challenges of contemporary health care and biomedical research.
Evaluating and Validating Empirical Bioethics Research Quality
Establishing Quality Assessment Criteria for Empirical Bioethics
The field of bioethics has undergone a significant transformation over recent decades, characterized by a pronounced "empirical turn" [21]. This evolution reflects a growing recognition that robust ethical analysis must be informed by reliable data about real-world contexts, practices, and experiences. Empirical bioethics is broadly defined as an interdisciplinary activity that integrates empirical social scientific analysis with ethical analysis to draw normative conclusions [2]. As the field has expanded, so too has the pressing need to establish clear, consensus-based standards for assessing the methodological rigor and quality of empirical bioethics research.
Quantitative analyses demonstrate this trend clearly. Between 1990 and 2003, the proportion of empirical studies in nine leading bioethics journals increased significantly from 5.4% to 15.4%, with this growth being statistically significant (χ2 = 49.0264, p<.0001) [21]. This rise underscores the necessity for quality assessment criteria tailored to the unique challenges of interdisciplinary work that bridges the normative and the empirical. This guide examines established and emerging quality standards, providing structured comparisons to aid researchers, reviewers, and funders in evaluating and conducting rigorous empirical bioethics research.
Established Quality Criteria for Bioethics Research
Before delving into standards specific to empirical bioethics, it is crucial to understand the foundational criteria for quality in broader bioethics scholarship. Analysis of exemplary articles has identified key markers of methodological rigor [67].
Table 1: Core Quality Criteria for Bioethics Scholarship
| Criterion Category | Specific Quality Markers |
|---|---|
| Argumentative Quality | Presenting clear objectives; refraining from drawing conclusions beyond premises; making underlying theoretical assumptions explicit [67]. |
| Empirical Foundation | Assessing the truth of premises accurately through rigorous quality assessment of empirical evidence; distinguishing empirical and normative arguments clearly [67]. |
| Dialectical Rigor | Presenting counterarguments in a manner opponents can accept; challenging conventional stereotypes and attitudes; not taking crucial or controversial premises for granted [67]. |
These general criteria form a bedrock upon which more specific standards for empirical bioethics have been built. They emphasize clarity, rigor in argumentation, and the proper use of evidence—all essential when integrating empirical data into normative reasoning.
Consensus Standards for Empirical Bioethics Research
A significant milestone in quality assessment was a consensus project that brought together 16 academics from five European countries, resulting in 15 standards of practice organized into six domains [2]. These standards were developed through a modified Delphi process, ensuring they represent agreed-upon norms within a diverse expert community.
Table 2: Consensus Standards for Empirical Bioethics Research [2]
| Research Domain | Core Standards of Practice |
|---|---|
| Aims | Clearly articulate the research aim and its relevance to an empirical bioethics approach. |
| Questions | Formulate research questions that are answerable and require an integrated empirical-normative approach. |
| Integration | Justify the methodology for integrating empirical and normative analysis; ensure the integration is explicit and purposeful. |
| Conduct of Empirical Work | Design and execute empirical work according to relevant quality standards for the chosen methods (e.g., social science). |
| Conduct of Normative Work | Design and execute normative work according to relevant quality standards for the chosen methods (e.g., philosophical analysis). |
| Training & Expertise | Ensure the research team possesses, or has access to, appropriate expertise in both empirical and normative methods. |
The consensus highlights that the primary challenge of empirical bioethics lies in the integration of the "is" of empirical data with the "ought" of normative evaluation [2]. This integration must be methodologically sound and transparent rather than superficial or post hoc. Furthermore, the standards affirm that simply collocating empirical and normative work is insufficient; the research design must require their interaction to address the core question.
Diagram 1: Interrelation of consensus standards in empirical bioethics. The central role of Integration requires inputs from both empirical and normative work, guided by clear aims and supported by expertise [2].
Methodological Procedures and Reporting Quality
Systematic Reviews in Empirical Bioethics
Systematic reviews are increasingly used to synthesize empirical bioethical literature, particularly in fields like nursing ethics. A meta-review of 76 systematic reviews of empirical bioethical literature revealed important trends and reporting quality issues [68].
- Methodological Diversity: The reviewed syntheses incorporated qualitative studies (13%), quantitative studies (32%), or a mix of both (55%) [68]. This reflects the range of empirical data relevant to bioethical inquiry.
- Ethical Engagement: A significant majority (72%) of the systematic reviews included the authors' own ethical reflections on the findings, and 59% provided explicit ethical recommendations [68]. This demonstrates a move beyond mere description to active normative engagement.
- Reporting Quality: The meta-review found heterogeneous reporting quality. However, reviews that used the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guideline tended to score better, highlighting the value of established reporting frameworks [68].
Mixed-Method Synthesis
For complex questions involving both intervention effects and contextual implementation factors, mixed-method syntheses are particularly valuable. These approaches combine quantitative and qualitative evidence to understand not just "what works," but how, for whom, and under what circumstances [69].
Table 3: Common Designs for Mixed-Method Synthesis [69]
| Synthesis Design | Description | Application in Bioethics |
|---|---|---|
| Segregated Design | Quantitative and qualitative evidence are synthesized separately first. | Findings are brought together at the interpretation stage, e.g., using an evidence-to-decision framework. |
| Sequential Synthesis | The findings of one synthesis (e.g., qualitative) inform the design or questions of the next (e.g., quantitative). | Qualitative evidence on patient preferences can shape the outcomes evaluated in a subsequent quantitative review. |
| Convergent Design | Quantitative and qualitative evidence are integrated during the analysis phase. | Used to develop a more comprehensive understanding of a phenomenon by weaving different data types together. |
These designs provide structured ways to handle the complexity inherent in many bioethical issues, ensuring that empirical data meaningfully informs normative conclusions.
Conducting high-quality empirical bioethics research requires familiarity with a suite of methodological tools and concepts. The following table outlines key "research reagents" for the empirical bioethicist.
Table 4: Essential Methodological Resources for Empirical Bioethics
| Tool or Concept | Function in Empirical Bioethics | Key Considerations |
|---|---|---|
| PRISMA Guidelines | To ensure comprehensive and transparent reporting of systematic reviews [68]. | Improves reproducibility and critical appraisal; particularly useful for literature-synthesizing studies. |
| Delphi Method | To structure group communication and achieve consensus among experts on complex issues [2]. | Used for developing quality standards and defining core ethical concepts or practices; values anonymity to reduce conformity bias. |
| Mixed-Methods Synthesis Framework | To integrate quantitative and qualitative evidence in a single review [69]. | Addresses complexity by explaining how interventions work in context; requires careful planning of integration strategy. |
| Epistemic Trust Framework | To analyze the dynamics of trust in clinical research relationships [70]. | Useful for studies on informed consent, patient participation, and research ethics; incorporates dimensions like trustworthiness and transparency. |
Establishing robust quality assessment criteria is fundamental to the maturation of empirical bioethics as a rigorous interdisciplinary field. The move from abstract theoretical debate to consensus-based standards, such as those detailed in this guide, marks significant progress. These standards provide a scaffold for designing, conducting, and evaluating research that meaningfully integrates empirical inquiry with normative analysis.
The continued development and application of these criteria will rely on collective engagement from the research community. As called for by leaders in the field, researchers, funders, and journals should actively engage with proposed standards, using them to refine methodologies and strengthen the overall quality of empirical bioethics scholarship [2]. Through such concerted efforts, the field can better fulfill its promise of providing ethically nuanced and empirically grounded guidance for complex practice and policy challenges.
In the evolving landscape of empirical bioethics research, methodological rigor remains both a paramount objective and a persistent challenge. As an interdisciplinary field, bioethics draws upon diverse methodological approaches from philosophy, social sciences, and biomedical research, creating a complex tapestry of integrative frameworks [3]. This comparative analysis examines the strengths, limitations, and applications of prominent methodological frameworks in empirical bioethics, with particular attention to their capacity to generate normatively robust conclusions. The increasing prominence of empirical methods in bioethics—rising from approximately 5.4% of bioethics publications in 1990 to 15.3% by 2003—underscores the urgency of establishing clear standards for evaluating methodological quality [42]. Contemporary bioethics research must navigate the fundamental challenge of integrating empirical "is" with normative "ought" claims while maintaining disciplinary integrity [2]. This analysis provides researchers, scientists, and drug development professionals with a structured framework for selecting and implementing methodological approaches that meet evolving standards of scholarly excellence and practical relevance.
Comparative Analysis of Core Methodological Approaches
Typology of Methodological Frameworks
Empirical bioethics encompasses a spectrum of methodological approaches characterized by distinct epistemological commitments and implementation procedures. Table 1 summarizes three primary analytical approaches for comparative trend analysis, illustrating how each addresses fundamental research questions.
Table 1: Comparative Analytical Approaches for Trend Analysis
| Analytical Approach | Core Characteristics | Research Questions Addressed | Key Limitations |
|---|---|---|---|
| Stratified Approach | Conducts separate regression analyses for each country or subgroup; uses common model specification across units [71]. | Describes trends within specific subgroups or populations [71]. | Does not provide statistical inference on variation between groups; limited capacity for cross-group comparison [71]. |
| Fixed Effect Approach | Models average trends and group differences through main and interaction effects; uses contrast coding for group comparisons [71]. | Tests overall trends and specific between-group differences in trends [71]. | Complex interpretation with multiple groups; does not model variance components explicitly [71]. |
| Random Effects Approach | Models average trend as fixed effect with group differences parameterized as random variance components; uses multi-level modeling [71]. | Quantifies between-group variation in trends; analyzes hierarchical data structures [71]. | Requires sufficient groups for variance estimation; more complex model specification [71]. |
A survey of bioethics researchers reveals that 87.5% use or have used empirical methods in their work, yet more than 22% of these "empirical researchers" had not received any methodological training [42]. This training gap underscores the need for clear methodological standards and comparative frameworks.
Qualitative Comparative Analysis (QCA) and Emerging Frameworks
Beyond traditional statistical approaches, bioethics researchers have adapted methodological frameworks from social sciences, including Qualitative Comparative Analysis (QCA) and its variants (crisp-set, multi-value, and fuzzy-set QCA) [72]. These case-based methods examine configurations of causally relevant conditions to outcomes, allowing for multiple causation pathways and reducing empirical complexity through Boolean logic [72]. Unlike variable-oriented approaches that seek generalizable patterns, QCA embraces causal complexity and asymmetrical relationships, making it particularly valuable for studying nuanced ethical phenomena across different contexts [72].
The proliferation of methodological approaches in empirical bioethics has been substantial, with one systematic review identifying 32 distinct methodologies that integrate empirical and normative dimensions [2]. This heterogeneity presents both opportunities and challenges, as researchers must navigate diverse methodological options without established standards for evaluation.
Methodological Rigor in Empirical Bioethics: Consensus Standards
Domain-Based Standards of Practice
A landmark consensus project involving 16 academics from 5 European countries established 15 standards of practice for empirical bioethics research, organized into 6 domains [2]. These standards, developed through a modified Delphi process, provide a framework for ensuring methodological quality:
- Aims: Research should clearly articulate its purposes, questions, and intended contributions to scholarship and practice.
- Questions: Research questions must be framed to facilitate meaningful integration of empirical and normative approaches.
- Integration: Studies should explicitly describe and justify how empirical and normative dimensions interrelate throughout the research process.
- Conduct of Empirical Work: Empirical components must adhere to methodological standards of relevant disciplines (e.g., social sciences) with appropriate design, sampling, data collection, and analysis.
- Conduct of Normative Work: Normative analysis should employ rigorous ethical reasoning with transparent justification for theoretical frameworks and conclusions.
- Training & Expertise: Researchers should possess or seek appropriate methodological training in both empirical and normative approaches [2].
These consensus standards address fundamental challenges in bioethics methodology, including the "is-ought problem" of deriving normative conclusions from empirical data and the disciplinary identity of bioethics as a field [2].
Comparative Evaluation of Methodological Rigor
Table 2 presents a comparative analysis of methodological rigor across different research approaches, highlighting key criteria for evaluation.
Table 2: Methodological Rigor Assessment Across Research Approaches
| Research Approach | Empirical Rigor Criteria | Normative Rigor Criteria | Integration Quality | Typical Applications |
|---|---|---|---|---|
| Stratified Trend Analysis | High internal validity within groups; standardized measurement [71]. | Limited explicit normative framework; descriptive focus [71]. | Minimal integration; primarily descriptive [71]. | Documenting health behavior trends; subgroup comparisons [71]. |
| Fixed/Random Effects Models | Strong statistical inference; handles hierarchical data structures [71]. | Dependent on theoretical framing; not inherent to method [71]. | Can be coupled with normative analysis; quantitative focus [71]. | Cross-national policy analysis; identifying variation sources [71]. |
| Qualitative Comparative Analysis (QCA) | Case-oriented approach; identifies necessary/sufficient conditions [72]. | Compatible with ethical reasoning patterns; contextual analysis [72]. | Strong potential through configurational thinking [72]. | Complex intervention studies; multi-site ethics consultation [72]. |
| Empirical Bioethics (Integrated) | Meets social science standards; appropriate method selection [2]. | Rigorous ethical analysis; transparent justification [2]. | Explicit integration methodology; reflexive process [2]. | Clinical ethics support; policy development; technology assessment [2]. |
Experimental Protocols and Implementation Frameworks
Protocol for Comparative Trend Analysis in Bioethics
The following protocol, adapted from a multinational adolescent health study, provides a structured approach for implementing comparative methodological analysis [71]:
Research Question Formulation: Define clear comparative questions addressing both descriptive trends (e.g., "Did toothbrushing show an overall linear time trend 2006-2022?") and variation questions (e.g., "Did countries/regions show different time trends?") [71].
Data Source Identification: Select appropriate datasets with repeated measures across multiple units (countries, institutions, populations). The Health Behaviour in School-aged Children study exemplifies a design with independent samples from the same countries measured at 4-year intervals [71].
Model Specification:
- For stratified analysis: Specify a common regression model (e.g., logistic regression with time as predictor) to be run separately for each country or subgroup.
- For fixed effects analysis: Develop a single model with main effects of time and group, plus interaction terms.
- For random effects analysis: Specify a multi-level model with fixed time effect and random intercepts and slopes at the country level [71].
Model Estimation and Interpretation: Execute models using appropriate statistical software, then interpret fixed effects for overall trends and variance components for between-group differences.
Integration with Normative Analysis: Contextualize statistical findings within relevant ethical frameworks, policy contexts, or theoretical perspectives to derive normative implications.
Workflow Visualization for Comparative Methodological Analysis
The following diagram illustrates the sequential and iterative process for conducting comparative methodological analysis in empirical bioethics:
Figure 1: Workflow for Comparative Methodological Analysis in Empirical Bioethics
Analytical Frameworks and Implementation Tools
Successful implementation of comparative methodological analysis requires familiarity with key conceptual frameworks and analytical tools. Table 3 outlines essential resources for researchers conducting methodological comparisons in bioethics.
Table 3: Essential Methodological Resources for Comparative Analysis
| Resource Category | Specific Tools/Frameworks | Primary Function | Application Context |
|---|---|---|---|
| Statistical Modeling | Multi-level regression models; Generalized Linear Mixed Models (GLMM) [71]. | Quantifies variation within and between groups; handles hierarchical data. | Cross-national studies; institutional comparisons; longitudinal analysis. |
| Comparative Methodology | Qualitative Comparative Analysis (QCA); Fuzzy-set analysis [72]. | Identifies necessary/sufficient condition configurations for outcomes. | Complex intervention ethics; multi-site policy analysis; case-based ethics. |
| Integration Frameworks | 32 distinct empirical bioethics methodologies [2]; Reflective equilibrium [3]. | Structures combination of empirical data and normative reasoning. | Interdisciplinary bioethics research; policy development; clinical ethics. |
| Rigor Assessment | Consensus standards (6 domains, 15 standards) [2]; Quality criteria roadmaps [2]. | Evaluates methodological quality; ensures comprehensive approach. | Study design; peer review; funding applications; research training. |
| Specialized Software | R, Stata (statistical models); fsQCA software (configurational analysis) [71] [72]. | Implements complex analytical procedures; visualizes relationships. | Data analysis phase of research projects; results validation. |
This comparative framework analysis demonstrates that methodological selection in empirical bioethics involves consequential trade-offs between analytical precision, interpretive depth, and practical feasibility. The stratified approach offers descriptive clarity but limited inferential capacity, while fixed and random effects models provide robust statistical inference about variation sources. Qualitative Comparative Analysis excels in identifying complex causal configurations but requires careful case selection and measurement [71] [72].
The consensus standards for empirical bioethics research offer a critical foundation for enhancing methodological rigor across these approaches [2]. As the field continues to develop, researchers must explicitly justify methodological selections based on research questions, available data, and intended contributions to both empirical understanding and normative reasoning. For drug development professionals and scientific researchers, this comparative framework provides guidance for evaluating bioethics research quality and for designing studies that generate both empirically valid and normatively robust conclusions.
The ongoing methodological refinement in empirical bioethics represents not merely a technical exercise, but a fundamental commitment to generating knowledge that can legitimately inform ethical practice in healthcare, research, and policy development. Through conscious attention to methodological rigor and transparent reporting, bioethics researchers can strengthen their contributions to addressing complex ethical challenges in rapidly evolving scientific domains.
Empirical bioethics is an interdisciplinary field that integrates empirical social scientific research with ethical analysis to arrive at normative conclusions [2]. This hybrid nature is its greatest strength, allowing it to address complex biomedical challenges with both descriptive and prescriptive insights. However, this interdisciplinarity also presents a fundamental challenge: the absence of universally agreed-upon standards of methodological rigor. Unlike established disciplines with clear criteria for evaluating research quality, empirical bioethics has struggled with how to assess the validity and reliability of its findings, a problem that undermines the field's authority and credibility [3]. This guide examines how community-driven peer review platforms, exemplified by Peer Community In (PCI), are establishing a new paradigm for validating research quality through transparent, community-based standards, thereby offering a model for reinforcing methodological rigor in empirical bioethics.
The core challenge lies in the integration of disparate epistemological traditions. When research draws on multiple disciplines, each with its own "criteria to determine when the application of methods to inquire into a particular question can be said to yield truthful and valid results," establishing a unified standard of rigor becomes complex [3]. This has led to practical difficulties in peer review, where terms like "originality, quality, value, and validity" may be interpreted differently by reviewers from different disciplinary backgrounds [3]. Community-based peer review models address this challenge by refocusing validation on the scientific content of articles rather than the prestige of the publication venue, creating a framework where methodological rigor is paramount [73].
Community-Based Peer Review: The PCI Model
Core Principles and Operational Framework
Peer Community In (PCI) is a non-profit organization of researchers that provides a diamond open access platform for peer review and recommendation of scientific preprints free of charge [73]. Its operational model bypasses traditional journal structures, instead creating a community-driven validation system where recommenders—acting as editors—manage the peer review of preprints within their specialized fields. The process culminates in a decision to recommend preprints that pass rigorous evaluation, transforming them into complete, reliable, and citable articles without the need for publication in traditional journals [73].
The PCI framework operates on several foundational principles that directly support methodological rigor:
- Stimulating: Each PCI recommends remarkable articles within its specific scientific field, focusing on intrinsic scientific quality [73].
- Open: The entire process is transparent, with open access to recommended articles, evaluation reports (reviews, author responses, and editorial decisions), and typically the associated data, scripts, and code [73].
- Free and Independent: The process is free for all users and managed by scientists for scientists, eliminating financial conflicts of interest [73].
- Reliable: Recommendations are based on sound evaluations by at least two reviewers, with the Managing Board checking the quality of reviews, decisions, and recommendations [73].
Table 1: Key Features of the PCI Peer Review Model
| Feature | Description | Impact on Methodological Rigor |
|---|---|---|
| Preprint-Based Review | Evaluation begins with preprints, not submitted manuscripts | Accelerates dissemination and focuses review on content rather than publication venue |
| Recommender System | Thematic experts manage review and recommend high-quality preprints | Distributes editorial workload while maintaining subject-specific expertise |
| Transparent Review | Open access to reviews, responses, and decisions | Creates accountability and allows public scrutiny of methodological critiques |
| Multi-form Output | Recommended articles can remain as preprints or be submitted to partner journals | Decouples validation from formal publication, emphasizing methodological soundness |
Comparative Analysis: PCI vs. Traditional Journal Review
When compared to traditional journal-based peer review, the PCI model presents distinct advantages for validating methodological approaches, particularly in interdisciplinary fields like empirical bioethics.
Table 2: PCI vs. Traditional Journal Peer Review
| Characteristic | PCI Model | Traditional Journal Model |
|---|---|---|
| Speed of Publication | Rapid; review begins immediately with preprint posting | Often slow; multiple submission rounds delay dissemination |
| Financial Model | Free diamond open access (no fees to authors or readers) | Typically requires subscription fees or article processing charges |
| Review Transparency | Open reviews, responses, and decisions | Most often closed, confidential peer review |
| Evaluation Focus | Scientific content and methodological rigor | Often influenced by journal impact factor and perceived novelty |
| Output Flexibility | Multiple publication pathways after recommendation | Restricted to journal's specific publication format |
| Researcher Control | Managed by working scientists for the community | Often controlled by commercial publishers |
The PCI model directly addresses what has been termed the "five challenges" in bioethics research, particularly the problems of unclear standards for answering bioethical questions and difficulties in the peer review process arising from interdisciplinary methodological differences [3]. By making the review process transparent and focusing on methodological soundness rather than disciplinary conformity, PCI provides a validation mechanism that can accommodate the methodological diversity inherent to empirical bioethics.
Establishing Methodological Rigor in Empirical Bioethics
Consensus Standards for Empirical Bioethics Research
The need for methodological standards in empirical bioethics has prompted deliberate consensus-building efforts. One significant project gathered 16 academics from 5 European countries with diverse disciplinary backgrounds to establish standards of practice using a modified Delphi approach [2]. This process resulted in 15 agreed-upon standards organized into 6 domains of research practice, providing a framework for assessing methodological rigor:
- Aims: Research should have clearly defined aims that justify the interdisciplinary approach.
- Questions: Research questions should be formulated to reflect both empirical and normative components.
- Integration: The research must demonstrate explicit integration of empirical and normative approaches.
- Conduct of Empirical Work: Empirical methods should be appropriate, rigorous, and transparently reported.
- Conduct of Normative Work: Normative analysis should be systematic, transparent, and connected to empirical findings.
- Training & Expertise: The research team should possess or cultivate appropriate interdisciplinary expertise [2].
These standards emphasize that in empirical bioethics, "the theoretical assumptions behind one's approach need to be stated, explained or fully justified" rather than taken for granted as they might be within established disciplinary silos [2]. This aligns perfectly with PCI's focus on transparent methodological justification.
Experimental Approaches and Validated Measures
Methodological rigor in empirical bioethics can be enhanced through experimental approaches that treat proposed ethical norms as "hypotheses which guide experimentation and observation of results" [74]. This experimentalist stance acknowledges that ethical frameworks must be tested against real-world contexts and complexities.
Several validated measures have been developed specifically for assessing ethical reasoning and decision-making in biomedical contexts, providing tools for strengthening the empirical component of bioethics research:
Table 3: Validated Measures for Empirical Bioethics Research
| Measure | Description | Application in Empirical Bioethics |
|---|---|---|
| Professional Decision-Making in Research (PDR) | 16-item vignette-based measure assessing strategies for addressing challenging research ethics issues [75] | Evaluates decision-making in contexts with human/animal subjects protections, integrity concerns |
| Professional Decision-Making in Medicine (PDM) | Parallel form to PDR adapted for clinical contexts and ethical dilemmas in healthcare [75] | Assesses physician decision-making when managing competing interests and patient values |
| How I Think about Research (HIT-Res) | Measures cognitive distortions used to justify compliance and integrity violations [75] | Identifies reasoning patterns that may predispose to research misconduct |
| Values in Scientific Work (VSW) | 35-item measure assessing importance scientists attach to intrinsic, extrinsic, and social values [75] | Examines value systems that influence ethical behavior in research environments |
These instruments provide empirically validated approaches to measuring constructs relevant to bioethical inquiry, strengthening the methodological foundation of research that seeks to bridge empirical observation and normative analysis.
Visualizing the Peer Review and Validation Workflow
The following diagram illustrates the complete workflow of the community-based peer review process, from initial preprint submission to final recommendation and publication pathways, highlighting how methodological rigor is assessed at each stage:
Community Peer Review Workflow
Essential Research Reagent Solutions for Empirical Bioethics
Conducting methodologically rigorous empirical bioethics research requires specific "research reagents" – conceptual tools and frameworks that facilitate the integration of empirical and normative analysis. The following table details key methodological solutions for addressing the field's unique challenges:
Table 4: Essential Research Reagent Solutions for Empirical Bioethics
| Research Reagent | Function | Application Context |
|---|---|---|
| Delphi Method | Structured communication technique for achieving consensus among experts [2] | Establishing methodological standards; resolving normative questions where empirical data on expert views is needed |
| Vignette-Based Instruments | Controlled scenarios measuring decision-making processes and ethical reasoning [75] | Assessing professional decision-making in research (PDR) and clinical (PDM) contexts |
| Cognitive Interviewing | Method for testing and refining survey instruments by understanding respondents' thought processes [75] | Developing validated measures for ethical constructs; ensuring question validity in interdisciplinary research |
| Factor Analysis | Statistical method for identifying underlying dimensions or factors in measurement instruments [75] | Validating multi-dimensional constructs in ethics research; developing robust measurement tools |
| Transparent Integration Frameworks | Explicit methodologies for combining empirical findings with normative analysis [2] | Ensuring rigorous connection between "is" and "ought" in empirical bioethics research |
Comparative Evaluation of Validation Mechanisms
The validation of research quality in empirical bioethics occurs through multiple mechanisms, each with distinct strengths and limitations for ensuring methodological rigor:
Table 5: Validation Mechanisms for Empirical Bioethics Research
| Validation Mechanism | Process | Strengths | Limitations |
|---|---|---|---|
| Community Peer Review (PCI) | Open review of preprints by community recommenders [73] | Focus on methodological rigor; transparent process; free access | Limited brand recognition in traditional evaluation systems |
| Traditional Journal Peer Review | Confidential peer review organized by journal editors | Established credibility; disciplinary standards | Often slow; limited transparency; influenced by journal prestige |
| Consensus Standards | Adherence to agreed-upon methodological standards [2] | Provides quality benchmarks; supports interdisciplinary rigor | May constrain methodological innovation; emerging framework |
| Instrument Validation | Psychometric validation of research measures [75] | Ensures reliability and validity of empirical components | Time-consuming development process; may narrow research focus |
The movement toward community-based peer review models like PCI represents a significant shift in how methodological rigor is established and recognized in research fields characterized by methodological diversity, such as empirical bioethics. By leveraging community standards through transparent, expert-driven evaluation, these models address fundamental challenges of interdisciplinary research while promoting open science practices. For empirical bioethics specifically, the combination of community peer review with emerging consensus standards on methodological quality offers a pathway toward greater credibility, authority, and impact. As the field continues to develop, such community-driven validation mechanisms will be essential for establishing empirical bioethics as a rigorous and distinctive "community of practice" capable of addressing complex ethical challenges in biomedicine and research.
Empirical bioethics is an exciting but challenging field that integrates social scientific research with normative ethical analysis to address complex moral questions in healthcare and the life sciences [76]. The fundamental aim of this interdisciplinary approach is to produce scholarship that has "real-world purchase"—genuine practical relevance for clinicians, researchers, and policymakers navigating ethical dilemmas [76]. However, this integration of empirical and normative approaches has historically faced significant theoretical and practical challenges, including epistemological tensions between descriptive "is" and normative "ought" claims, and methodological questions about how to validly combine different disciplinary perspectives [3] [2].
The core problem lies in bioethics' contested disciplinary status. As one analysis notes, bioethics has been variably described as "a discipline, an applied discipline, a demi-discipline, a sub-discipline, and a second-order discipline," while others consider it "multidisciplinary, interdisciplinary, or transdisciplinary" [3]. This lack of consensus has practical consequences: without agreed-upon standards of rigor, bioethics research faces challenges in peer review, claims to authority and legitimacy, and practical decision-making in clinical settings [3].
In response to these challenges, a significant consensus-finding project was undertaken, culminating in a set of 15 standards of practice for empirical bioethics research [2]. This checklist represents a crucial step toward establishing methodological rigor while respecting the field's inherent interdisciplinary nature. This guide provides researchers with a framework for benchmarking their work against these emerging consensus standards, enabling more systematic planning, conduct, and reporting of empirical bioethics research.
The Empirical Bioethics Landscape
Current Practices and Training Gaps
Recent surveys of European bioethics researchers reveal both the growing prevalence of empirical methods and significant training deficits in the field. A 2017 study found that 87.5% of bioethics researchers reported using or having used empirical methods in their work [42]. However, among these 'empirical researchers,' 22.9% had received no formal methodological training, and only 6% or fewer considered themselves experts in the qualitative or quantitative methods they employed [42]. This training gap underscores the urgent need for clear methodological standards and training resources.
The same study found that while only 35% of scholars who had used empirical methods reported having integrated empirical data with normative analysis, 59.8% planned to do so in their current projects [42]. This indicates a growing recognition of the importance of genuine integration, not just parallel execution of empirical and normative work.
Theoretical Foundations and Challenges
The methodological challenges in empirical bioethics are not merely practical but deeply theoretical. Research must satisfy two distinct quality standards: those of normative conceptual analysis and the epistemological standards of the parent disciplines from which empirical methodologies are borrowed [42]. This requires navigating what has been termed the "fact/value distinction" while developing approaches that can generate both empirically informed and philosophically justified normative conclusions [76].
Different methodological approaches have emerged to address these challenges. These range from more consultative approaches (where researchers consult data while conducting normative analysis separately) to more dialogical approaches (where researchers and participants co-develop understandings and solutions to moral questions) [76]. Each approach offers distinct advantages for achieving different research objectives while maintaining methodological rigor.
The 15-Point Consensus Checklist: Standards for Empirical Bioethics Research
Through a modified Delphi process involving 16 academics from 5 European countries with diverse disciplinary backgrounds, consensus was reached on 15 standards of practice for empirical bioethics research [2]. These standards are organized into six domains of research practice, providing a comprehensive framework for ensuring methodological rigor.
Table 1: The 15 Consensus Standards for Empirical Bioethics Research
| Domain | Standard Number | Standard Description |
|---|---|---|
| Aims | 1 | Research aims and objectives must be clearly stated. |
| 2 | The research question must be fit for purpose. | |
| Questions | 3 | Research questions must be answerable. |
| 4 | Research questions must be relevant to the field. | |
| Integration | 5 | Methodology must be appropriate to the research question. |
| 6 | The approach to integration must be explained and justified. | |
| 7 | The purpose of the empirical work must be explained and justified. | |
| 8 | Limitations must be acknowledged and addressed. | |
| Conduct of Empirical Work | 9 | The conduct of the empirical work must be explained and justified. |
| 10 | The empirical work must be quality-assured. | |
| Conduct of Normative Work | 11 | The conduct of the normative work must be explained and justified. |
| 12 | The normative work must be quality-assured. | |
| Training & Expertise | 13 | The research team must be competent and credible. |
| 14 | The research team must be appropriately constituted. | |
| 15 | The research context must be appropriately resourced. |
Domain 1: Aims (Standards 1-2)
The first domain addresses the foundational elements of any research project. Standard 1 requires that research aims and objectives must be clearly stated, ensuring transparency about what the study intends to achieve. Standard 2 emphasizes that the research question must be fit for purpose, meaning it should be appropriately scoped and designed to address the identified ethical problem [2].
These standards respond to the identified challenge that without clear aims, bioethics research struggles to establish its authority and legitimacy [3]. Well-defined aims help position the research within the broader bioethics landscape and clarify its potential contribution to both scholarship and practice.
Domain 2: Questions (Standards 3-4)
This domain focuses on the formulation of the research questions themselves. Standard 3 requires that research questions must be answerable through the chosen methodological approach, while Standard 4 emphasizes that research questions must be relevant to the field of bioethics [2].
These standards address the criticism that some bioethics research generates questions that cannot be meaningfully answered through empirical-normative integration, or that fail to engage with core concerns of the bioethics community. Relevance ensures the research has potential "real-world purchase" in clinical, research, or policy settings [76].
Domain 3: Integration (Standards 5-8)
The integration domain contains the core standards that distinguish empirical bioethics from separate empirical or normative projects. Standard 5 requires that the methodology must be appropriate to the research question, while Standard 6 emphasizes that the approach to integration must be explained and justified [2]. This explicit justification is crucial given the numerous documented approaches to integration—one systematic review identified 32 distinct methodologies for integrating empirical and normative elements in bioethics research [2].
Standard 7 requires researchers to explain and justify the purpose of the empirical work within the broader normative project, and Standard 8 addresses the need to acknowledge and address limitations in both empirical and normative dimensions [2]. This reflects the understanding that all research methods have inherent limitations that must be transparently acknowledged.
Domain 4: Conduct of Empirical Work (Standards 9-10)
These standards address the execution of the empirical component. Standard 9 requires that the conduct of the empirical work must be explained and justified, including details about data collection and analysis methods appropriate to the empirical tradition being employed. Standard 10 emphasizes that the empirical work must be quality-assured according to standards appropriate to its methodology [2].
These standards respond to concerns about the quality of empirical work in bioethics, ensuring that empirical components meet the epistemological standards of the parent disciplines from which methods are borrowed [42]. This is particularly important given the identified training gaps in empirical methods among bioethics researchers [42].
Domain 5: Conduct of Normative Work (Standards 11-12)
These parallel standards address the normative component. Standard 11 requires that the conduct of the normative work must be explained and justified, including the ethical framework or approach being employed. Standard 12 emphasizes that the normative work must be quality-assured according to standards of rigorous ethical analysis [2].
These standards ensure that the normative analysis meets the standards of philosophical rigor while remaining appropriately connected to the empirical findings. This addresses concerns that empirical bioethics might prioritize empirical findings at the expense of normative depth [76].
Domain 6: Training & Expertise (Standards 13-15)
The final domain addresses the human and institutional resources required for quality empirical bioethics research. Standard 13 requires that the research team must be competent and credible to conduct the proposed research, while Standard 14 emphasizes that the research team must be appropriately constituted with the necessary range of expertise [2]. Standard 15 notes that the research context must be appropriately resourced to support the project [2].
These standards respond to the interdisciplinary nature of empirical bioethics, which often requires combining expertise from philosophy, social science, clinical practice, and other fields. The training gaps identified in survey research make these standards particularly important for ensuring research quality [42].
Methodological Approaches and Workflow
The consensus standards provide a framework for evaluating research quality, but researchers must still select specific methodological approaches appropriate to their research questions. The field has developed numerous distinct methodologies for integrating empirical and normative work, which can be visualized as a sequential workflow with iterative elements.
Key Methodological Approaches
Several methodological approaches have gained prominence in empirical bioethics research, each offering distinct strategies for integrating empirical and normative elements:
Reflective Equilibrium: This approach, adapted from political philosophy, involves moving back and forth between empirical findings about moral intuitions and ethical principles to achieve coherence in moral reasoning [76]. Researchers systematically examine and refine their ethical judgments in light of both empirical data and theoretical considerations.
Deliberative Democracy: This methodology uses structured democratic deliberation among stakeholders to address ethical questions and develop legitimate policies [76]. It is particularly valuable for questions involving value conflicts where legitimate decision-making processes are needed.
Dialogical Practice: This approach emphasizes moral learning through dialogue between researchers and stakeholders, with direct improvement to practice as a primary goal [76]. It often involves facilitated conversations that resemble "philosophy seminars" more than traditional social science data collection [2].
Feminist Approaches: These methodologies explicitly address power dynamics and oppression in healthcare and research contexts, bringing a commitment to equality-based norms to both empirical and normative dimensions [76].
Each approach requires different expertise and resources, making the choice of methodology a critical decision that must be aligned with research questions, team composition, and intended outcomes.
The Empirical Bioethics Research Toolkit
Successful empirical bioethics research requires both conceptual frameworks and practical tools. The following table outlines essential "research reagent solutions"—key methodological components and their functions in empirical bioethics research.
Table 2: Empirical Bioethics Research Reagent Solutions
| Tool Category | Specific Method | Primary Function in Empirical Bioethics |
|---|---|---|
| Data Collection Methods | In-depth interviews | Explore stakeholder moral experiences and reasoning processes |
| Focus groups | Generate collective moral deliberation on specific ethical dilemmas | |
| Ethnographic observation | Understand ethical decision-making in natural contexts | |
| Surveys | Measure prevalence of specific moral attitudes or experiences | |
| Integration Frameworks | Reflective equilibrium | Systematically reconcile moral intuitions with ethical principles |
| Dialogical methods | Co-construct moral understanding with stakeholders | |
| Case deliberation | Analyze specific cases through structured ethical reflection | |
| Analysis Techniques | Thematic analysis | Identify patterns in qualitative moral experience data |
| Ethical framework analysis | Apply specific ethical theories to empirical findings | |
| Discourse analysis | Examine how ethical arguments are constructed in practice |
Each tool serves specific functions within the broader empirical bioethics methodology. For example, deliberative democracy approaches might combine focus groups with ethical framework analysis, while feminist approaches might prioritize in-depth interviews with discourse analysis to highlight power dynamics [76]. The key is selecting tools that align with both the research question and the chosen approach to integration.
Implementation Guidance and Best Practices
Practical Application of the Checklist
Implementing the 15-point checklist requires more than mechanical compliance. Researchers should use the standards as a framework for reflexive practice throughout the research process. This includes:
- Project Planning: Use the checklist during research design to ensure all domains are adequately addressed in proposals and protocols.
- Team Composition: Carefully consider the expertise needed (Standard 14) and identify training gaps (Standard 13) early in the process.
- Transparent Reporting: Use the standards to structure research publications, explicitly addressing each relevant domain to enhance transparency and credibility.
Anticipating Challenges
Empirical bioethics research faces several predictable challenges that researchers should anticipate:
- Interdisciplinary Communication: Different disciplinary traditions may use similar terminology with different meanings. Regular, structured communication helps build shared understanding.
- Methodological Innovation: Standard approaches to data collection may need modification to generate data suitable for normative analysis [2]. Such innovations require clear justification.
- Peer Review Challenges: Research may face appraisal according to different disciplinary norms [2]. Explicit reference to the consensus standards can help justify methodological choices.
The development of consensus standards represents significant progress in establishing empirical bioethics as a distinct "community of practice" with its own methodological norms and aims [2]. Widespread adoption of these standards has the potential to improve research quality, enhance credibility with stakeholders, and strengthen the field's contribution to addressing pressing ethical challenges in healthcare and the life sciences.
Empirical bioethics is an interdisciplinary field that integrates empirical social scientific research with ethical analysis to draw normative conclusions [2]. This integration promises to address complex healthcare challenges with nuanced understanding, but the field is characterized by significant methodological heterogeneity. A central, ongoing debate concerns whether bioethics qualifies as a discipline with defined methodological rules, or if its lack of a unifying methodology hinders its consolidation and the assessment of its scholarly impact [77]. This guide examines the methodologies and standards shaping empirical bioethics research, providing a comparative analysis of their application and rigor.
The fundamental challenge lies in the "methodological rigor gap." As Hofmann (2025) argues, bioethics often lacks explicit methodological reporting and consensus, with very few articles in normative bioethics containing methods sections or explicitly declaring their methods [77]. Conversely, a consensus project detailed by Ives et al. (2018) developed 15 standards of practice organized into 6 domains specifically to address this gap and enhance methodological quality in empirical bioethics research [2]. This tension between methodological diversity and the need for assessed rigor forms the critical framework for evaluating the field's impact and relevance.
Comparative Analysis of Methodological Approaches
Table 1: Key Methodological Approaches in Bioethics
| Approach Type | Core Focus | Typical Applications | Inherent Strengths | Documented Limitations |
|---|---|---|---|---|
| Theoretical/Philosophical | Conceptual analysis and normative reasoning | Developing ethical frameworks, analyzing moral concepts | Conceptual clarity, logical rigor | Often disconnected from practical contexts and empirical data [77] |
| Empirical Bioethics | Integrating empirical data with normative analysis | Understanding practitioner experiences, patient perspectives | Grounds ethical reflection in real-world practices and attitudes [2] | Challenges in methodological integration; "how an empirical 'is' can inform a normative 'ought' claim" [2] |
| Procedural/Policy-Oriented | Developing processes for decision-making | Clinical ethics committees, policy development | Practical focus, facilitates stakeholder input | May prioritize process over substantive ethical analysis [77] |
| Mixed Methods Research | Integrating quantitative and qualitative approaches | Investigating complex educational psychology issues [47] | Provides more complete understanding than single methods [47] | Reporting challenges, word count limitations in journals, difficulty clearly representing integration [47] |
Table 2: Prevalence and Rigor of Phenomenological Research in Health Contexts (2015-2025)
| Aspect of Rigor | Descriptive Phenomenology (23.2% of studies) | Interpretive Phenomenology (52.2% of studies) | Key Findings from Review |
|---|---|---|---|
| Philosophical Foundation | Rarely clearly indicated | Rarely clearly indicated | 77.9% of studies did not clearly indicate philosophical underpinnings [78] |
| Reporting Guidelines | Low adherence | Low adherence | 94.2% did not follow established reporting guidelines [78] |
| Data Collection | Primarily semi-structured interviews | Primarily semi-structured interviews | 78.3% used semi-structured interviews; 15.9% used focus groups [78] |
| Sample Size | Generally smaller samples | Generally smaller samples | Significantly smaller than non-phenomenological studies (p < 0.001) [78] |
Experimental Protocols in Empirical Bioethics Research
Consensus Development Protocol for Standards of Practice
The consensus process used in developing standards for empirical bioethics research employed a modified Delphi approach [2]. This methodological protocol involved:
Expert Panel Assembly: 16 academics from 5 European countries with diverse disciplinary backgrounds were selected to represent different and putatively opposing empirical bioethics positions [2].
Modified Delphi Process: Unlike traditional anonymous Delphi methods, this adaptation utilized structured group discussions at the Brocher Foundation in May 2015. This allowed immediate clarification of ambiguous or controversial issues, essential given linguistic and conceptual diversity within the field [2].
Consensus Generation: Through iterative discussion, participants reassessed initial judgments based on group feedback, working toward agreement on standards of practice without the conformity pressure typical of open group settings [2].
Output Formulation: The process yielded consensus on 15 standards of practice organized into 6 domains: Aims, Questions, Integration, Conduct of Empirical Work, Conduct of Normative Work, and Training & Expertise [2].
Methodological Review Protocol for Assessing Rigor
Systematic methodological reviews in mixed methods research (MMR-SMR) follow a rigorous protocol to assess methodological quality [47]:
Systematic Search: Comprehensive screening of all articles in five prominent educational psychology journals over a seven-year period (2016-2022) [47].
Identification of Trends: Analysis of prevalence and reporting quality of mixed methods articles (n = 57 identified) using systematic screening criteria [47].
Quality Assessment: Evaluation of methodological rigor based on explicit criteria, including reporting of integration procedures, methodological transparency, and adherence to reporting guidelines [47].
Synthesis: Identification of strengths and areas for improvement in reporting quality, with provision of suggestions for promoting high reporting quality in mixed methods articles [47].
Visualization of Research Processes
Research Methodology Selection in Bioethics
Methodological Rigor Assessment Framework
Essential Research Reagent Solutions
Table 3: Methodological Tools for Empirical Bioethics Research
| Research 'Reagent' | Function | Application Context | Considerations for Use |
|---|---|---|---|
| Modified Delphi Technique | Structured consensus finding process among experts | Developing field standards, establishing methodological guidelines [2] | Balances structured input with immediate clarification opportunities; adapted from traditional anonymous Delphi |
| Systematic Methodological Review (MMR-SMR) | Summarizes trends in how mixed methods research is used within a field [47] | Evaluating prevalence and quality of methodological approaches | Uses systematic identification to create pool of studies for analysis of methodological rigor |
| Reporting Guidelines (e.g., COREO, MIRRI) | Ensure transparent and complete reporting of methodological details | Manuscript preparation, study design phase | Addresses word count limitations; enhances reproducibility; often underutilized [78] |
| Qualitative Interview Protocols | Collect in-depth descriptive data on lived experiences | Phenomenological research, understanding practitioner perspectives [78] | Semi-structured formats most common (78.3%); requires alignment with philosophical underpinnings |
| Integration Procedures | Explicit methods for combining empirical and normative components | Mixed methods research, empirical bioethics studies [2] [47] | Defining feature of MMR; requires clear description of how quantitative and qualitative findings are combined |
| Perceptually Uniform Color Maps | Accurate data representation in visualizations | Scientific figures, data presentation [79] | Prevents visual distortion of data; ensures accessibility for color-vision deficient readers |
The assessment of methodological rigor in empirical bioethics reveals a field in dynamic development, characterized by ongoing efforts to standardize practices while respecting methodological diversity. The consensus on 15 standards of practice represents significant progress in establishing empirical bioethics as a distinct "community of practice" [2]. However, persistent gaps in methodological reporting—particularly unclear philosophical foundations and insufficient description of integration procedures—continue to challenge the field's credibility and practical application [78].
Future methodological development should focus on three key areas: (1) enhancing explicit methodological reporting in published research, (2) addressing the challenges of integration between empirical and normative components, and (3) developing discipline-specific quality criteria that respect the interdisciplinary nature of bioethics inquiry. As the field continues to mature, this focus on methodological rigor will strengthen both the theoretical foundations and practical relevance of empirical bioethics research, ultimately supporting its critical role in addressing complex ethical challenges in healthcare and medicine.
Conclusion
Assessing methodological rigor in empirical bioethics requires careful attention to established standards, deliberate integration of empirical and normative components, and transparent reporting of methodological choices. The consensus-developed standards of practice provide a crucial foundation for ensuring research quality, while the diversity of available methods allows for tailored approaches to specific research questions. For biomedical and clinical research, enhanced methodological rigor in empirical bioethics promises more robust ethical analyses of emerging technologies and complex healthcare challenges. Future directions should focus on developing more refined validation metrics, expanding training in interdisciplinary methodologies, and adapting these frameworks to address novel ethical dilemmas in drug development and clinical practice. By strengthening methodological rigor, empirical bioethics can increase its academic impact and practical relevance in guiding ethical decision-making across the biomedical research spectrum.
References
- 1. Is–ought problem [https://en.wikipedia.org/wiki/Is%E2%80%93ought_problem]
- 2. Standards of practice in empirical bioethics research [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-018-0304-3]
- 3. Disciplining Bioethics: Towards a Standard of Methodological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3413904/]
- 4. The Role of Empirical Research in Bioethics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2826359/]
- 5. Bioethics, Experimental Approaches. [https://philarchive.org/rec/LEWBEA]
- 6. List of Essentials Documents in Research Ethics [https://www.infonetica.net/articles/research-ethics-essential-documents]
- 7. Global comparison of research ethical review protocols [https://pmc.ncbi.nlm.nih.gov/articles/PMC11975204/]
- 8. Standards of practice in empirical bioethics research [https://pubmed.ncbi.nlm.nih.gov/29986689/]
- 9. Standards of practice in empirical bioethics research [https://ora.ox.ac.uk/objects/uuid:da48e195-1ebd-4a20-8e8e-13b354b4bb75]
- 10. Standards of practice in empirical bioethics research [https://pmc.ncbi.nlm.nih.gov/articles/PMC6038185/]
- 11. Research across the disciplines: a road map for quality criteria ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/1472-6939-15-17]
- 12. The empirical study of norms is just what we are missing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4202778/]
- 13. The Psychology of Normative Cognition [https://plato.stanford.edu/entries/psychology-normative-cognition/]
- 14. Empirical studies on how ethical recommendations are ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9835353/]
- 15. Institutional Bioethics: From Critical Interdisciplinarity to ... [https://pubmed.ncbi.nlm.nih.gov/40397099/]
- 16. The methodological rigor of anticipatory bioethics [https://link.springer.com/article/10.1007/s11019-014-9578-5]
- 17. Interdisciplinary Bioethics | Jackman Humanities Institute [https://www.humanities.utoronto.ca/programs-research/research/working-groups/interdisciplinary-bioethics]
- 18. Yale Interdisciplinary Center for Bioethics: Welcome [https://bioethics.yale.edu/welcome]
- 19. What Is Empirical Research? Definition, Types & Samples ... [https://research.com/research/what-is-empirical-research]
- 20. Empirical v. Non-Empirical Research - BY 499 - Senior ... [https://libguides.brenau.edu/c.php?g=684143&p=4834482]
- 21. Empirical research in bioethical journals. A quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2565792/]
- 22. Acceptable objectives of empirical research in bioethics [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-022-00845-1]
- 23. Types of Research - Research Methods [https://semo.libguides.com/c.php?g=1296240&p=9634655]
- 24. 30. Data analysis methods in quantitative research [https://uq.pressbooks.pub/quality-in-healthcare/chapter/data-analysis-methods-quantitative-research/]
- 25. Quantitative vs. Qualitative - Empirical & Non- ... [https://library.piedmont.edu/c.php?g=1277355&p=9373002]
- 26. Ethics in medical research: A quantitative analysis of the ... [https://www.medrxiv.org/content/10.1101/2024.06.23.24309373v1]
- 27. A call for structured ethics appendices in social science ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8307908/]
- 28. Digital bioethics: introducing new methods for the study of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10646908/]
- 29. Reframing the Ethical Interface: A Critical STS Approach to ... [https://rsisinternational.org/journals/ijrias/articles/reframing-the-ethical-interface-a-critical-sts-approach-to-science-technology-and-society/]
- 30. A Structural Approach to Ethical Reasoning [https://www.abacademies.org/articles/a-structural-approach-to-ethical-reasoning-the-integration-of-moral-philosophy-6525.html]
- 31. Delphi methodology in healthcare research: How to decide its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8299905/]
- 32. The Delphi method: A comprehensive guide for group ... [https://www.1000minds.com/decision-making/delphi-method]
- 33. Modified Delphi Process | Family & Preventive Medicine [https://medicine.utah.edu/dfpm/public-health/research/research-groups/ohleh/research/phepr/modified-delphi-process]
- 34. Development of key performance indicators for a telemedicine ... [https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-025-12733-6]
- 35. Results from a US modified Delphi consensus to define ... [https://pubmed.ncbi.nlm.nih.gov/41091181/]
- 36. Modified Delphi Panel Process [https://www.jmir.org/2025/1/e38657]
- 37. Building the 8-star doctor: a modified Delphi study to define ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-025-07694-7]
- 38. The development of the sustainability measure for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465213/]
- 39. Delphi Consensus: Advantages and Disadvantages [https://triducive.com/2022/10/14/advantages-and-disadvantages-delphi-consensus/]
- 40. Reflective Equilibrium - Stanford Encyclopedia of Philosophy [https://plato.stanford.edu/entries/reflective-equilibrium/]
- 41. Applications of the Wide Reflective Equilibrium [https://link.springer.com/article/10.1007/s10892-023-09458-1]
- 42. The use of empirical research in bioethics: a survey of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5741864/]
- 43. Fundamentals of an Ethics of Care - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK543745/]
- 44. Ethical Guidelines for Statistical Practice [https://www.amstat.org/your-career/ethical-guidelines-for-statistical-practice]
- 45. Setting standards for empirical bioethics research: a response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6044088/]
- 46. a commentary on standards of practice in empirical bioethics [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-018-0303-4]
- 47. Reporting of Methodological Rigor in Empirical Mixed ... [https://link.springer.com/article/10.1007/s10648-025-10090-8]
- 48. The contribution of benchmarking to quality improvement in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8812166/]
- 49. LLM ethics benchmark: a three-dimensional assessment ... [https://www.nature.com/articles/s41598-025-18489-7]
- 50. An update on the “empirical turn” in bioethics: analysis of ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-018-0246-9]
- 51. The Vagueness of Integrating the Empirical and the Normative [https://pmc.ncbi.nlm.nih.gov/articles/PMC11288993/]
- 52. 7 Most Common Issues & Integration | Multishoring Failures [https://multishoring.com/blog/7-most-common-integration-issues-aka-why-system-integration-projects-fail/]
- 53. Epistemological obstacles to interdisciplinary research [https://i2insights.org/2017/10/31/epistemology-and-interdisciplinarity/]
- 54. Creativity, interdisciplinary collaboration and epistemic ... [https://www.sciencedirect.com/science/article/pii/S1871187120302236]
- 55. Reflections on interdisciplinary research in practice [https://pmc.ncbi.nlm.nih.gov/articles/PMC12594677/]
- 56. The use of empirical research in bioethics - BMC Medical Ethics [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-017-0239-0]
- 57. Principles of Clinical Ethics and Their Application to Practice [https://pmc.ncbi.nlm.nih.gov/articles/PMC7923912/]
- 58. Public Health Ethics: Importance, Frameworks, and Examples [https://publichealth.tulane.edu/blog/public-health-ethics/]
- 59. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 60. Chapter 5.4: Color Theory and Accessibility in Data Visualization [https://express.excelsior.edu/datascience/chapter/5-4-color-theory-and-accessibility-in-data-visualization/]
- 61. Understanding WCAG 2 Contrast and Color Requirements [https://webaim.org/articles/contrast/]
- 62. Making a Difference Request for Proposals - Fall 2025 [https://greenwall.org/making-a-difference-grants/request-for-proposals-MAD-fall-2025]
- 63. Non-empirical methods for ethics research on digital ... [https://link.springer.com/article/10.1007/s11019-024-10222-x]
- 64. Empirical Ethics [https://aabhl.org/stream/empirical-ethics/]
- 65. How AI will reshape pharma in 2025 [https://www.drugtargetreview.com/article/154981/how-ai-will-reshape-pharma-by-2025/]
- 66. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 67. In pursuit of goodness in bioethics : analysis of an exemplary article [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-018-0299-9]
- 68. Systematic reviews of empirical literature on bioethical topics: Results... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7323745/]
- 69. Synthesising quantitative and qualitative evidence to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6350750/]
- 70. Building trust in clinical research: a systems approach to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12307415/]
- 71. Methodological Approaches to Comparative Trend Analyses [https://www.ssph-journal.org/journals/international-journal-of-public-health/articles/10.3389/ijph.2024.1607669/full]
- 72. Comparative Analysis Methodologies in Nursing Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC12417324/]
- 73. Peer Community In - free peer review & validation of preprints ... [https://peercommunityin.org/]
- 74. Experimentalism in bioethics research [https://pubmed.ncbi.nlm.nih.gov/6886573/]
- 75. Testing Services [https://bioethicsresearch.org/research-services/testing-services/]
- 76. Empirical Bioethics: Theoretical and Practical Perspectives [https://script-ed.org/article/empirical-bioethics-theoretical-and-practical-perspectives/]
- 77. Bioethics: No Method—No Discipline? [https://www.ovid.com/journals/cqhe/pdf/10.1017/s0963180124000136~bioethics-no-methodno-discipline]
- 78. Evaluating the rigour and application of phenomenological ... [https://www.sciencedirect.com/science/article/pii/S1078817425001634]
- 79. The misuse of colour in science communication [https://www.nature.com/articles/s41467-020-19160-7]