Bridging the Is-Ought Gap: Methodologies and Applications in Empirical Bioethics Research
This article provides a comprehensive guide for biomedical researchers and professionals on navigating the is-ought gap in empirical bioethics.
Bridging the Is-Ought Gap: Methodologies and Applications in Empirical Bioethics Research
Abstract
This article provides a comprehensive guide for biomedical researchers and professionals on navigating the is-ought gap in empirical bioethics. It explores the foundational debate surrounding Hume's Law, presents practical methodological frameworks for integrating empirical data with normative analysis, addresses common implementation challenges, and validates approaches based on current researcher consensus. By synthesizing theoretical insights with applied strategies, this resource aims to empower interdisciplinary teams in drug development and clinical research to conduct ethically robust and methodologically sound empirical bioethics research.
Demystifying Hume's Law: The Foundation of the Is-Ought Problem in Bioethics
Understanding Hume's Law and its Historical Influence on Bioethics
Frequently Asked Questions (FAQs)
1. What is Hume's Law or the Is-Ought Problem? Hume's Law, also known as the Is-Ought Problem, is the thesis that an ethical or judgmental conclusion (a statement about what ought to be) cannot be logically inferred from purely descriptive, factual statements (statements about what is) [1]. David Hume argued that authors often make this transition imperceptibly and that this new relation of "ought" needs to be observed and explained, as it cannot be a simple deduction from entirely different relations [1].
2. Is Hume's Law a valid argument against empirical bioethics? No, current scholarship argues that Hume's Law is not a definitive argument against empirical bioethics [2] [3]. The interpretation of Hume's Law as creating an unbridgeable logical gulf between facts and morality is dependent on a specific, non-cognitivist meta-ethical stance. Other interpretations are possible, and conflating meta-ethics with applied ethics is problematic [2]. A non-cognitivist interpretation challenges not just empirical bioethics, but all bioethics situated within ethical cognitivism [2].
3. What is the difference between Hume's Law, the fact-value distinction, and the naturalistic fallacy? These are three distinct but often conflated concepts [2]:
- Hume's Law: Concerns the logical relationship between descriptive ("is") and prescriptive ("ought") statements.
- Naturalistic Fallacy: An expression introduced by G.E. Moore to refute ethical naturalism, broadly meaning it is a logical fallacy to define "good" in terms of natural properties [2].
- Fact-Value Distinction: The view that factual statements and value statements are distinct, sometimes extended to the positivist idea that science is value-free [2].
4. How can empirical research be integrated into normative bioethics? Integration is possible through shared meta-ethical postulates. The "bridge postulate" states that a bridge between facts and values is both possible and foundational to bioethics, though its exact nature remains open for discussion. The "ethical cognitivism" postulate states that bioethics generally operates on the assumption that ethical statements are truth-apt and that knowledge is possible in ethics [2].
5. What was the 'empirical turn' in bioethics? The "empirical turn" refers to a shift in the 1990s where social scientists began confidently contributing to bioethics, outlining how sociological and ethnographic perspectives could benefit the field [4]. This shifted bioethics from a field dominated by philosophical application of principles to a "dynamic, changing, multi-sited field" involving multiple disciplines [4].
Troubleshooting Guide: Common Methodological Issues
Problem: Deriving a normative conclusion directly from an empirical dataset.
- Symptoms: A research conclusion states what should be done based solely on descriptive data (e.g., "Our survey found that 80% of clinicians do X, therefore this is the ethical practice.").
- Solution: Explicitly state the normative premise that links your empirical finding to the ethical conclusion. The reasoning should be: (1) Empirical finding: "80% of clinicians do X"; (2) Normative premise: "Clinical practice Y is ethically good because it aligns with the principle of beneficence"; (3) Therefore, the empirical finding is evaluated against an explicit ethical standard.
Problem: Conflating widespread practice (what "is") with ethical justification (what "ought" to be).
- Symptoms: Justifying an action by stating "it's always been done this way," "it's natural," or "everyone else is doing it" without further ethical reasoning [5].
- Solution: Treat common practices as descriptive starting points for ethical reflection, not as normative conclusions. Use empirical data to inform the context and potential consequences of an action, but evaluate those consequences against explicit ethical principles.
Problem: Confusing Hume's Law with the Naturalistic Fallacy.
- Symptoms: Using the terms "Hume's Law" and "Naturalistic Fallacy" interchangeably in research methodology or literature reviews.
- Solution: Differentiate the concepts clearly. Hume's Law deals with the "is-ought" inference, while the Naturalistic Fallacy, in its original Moorean sense, deals with defining "good" in terms of natural properties. Precise terminology strengthens methodological rigor [2].
Research Reagent Solutions: Conceptual Toolkit
| Item | Function in Empirical Bioethics Research |
|---|---|
| Ethical Principles (e.g., Autonomy, Beneficence) | Provide the necessary normative premises for building a bridge from empirical facts ("is") to ethical conclusions ("ought") [4]. |
| Empirical Methods (e.g., surveys, ethnography) | Generate the descriptive, factual data ("is") about human behavior, beliefs, and contexts in healthcare and the life sciences [4]. |
| Bridge Postulate | Serves as the foundational meta-ethical assumption that a connection between facts and values is possible, justifying the entire empirical-normative research enterprise [2]. |
| Ethical Cognitivism Postulate | Provides the underlying assumption that ethical statements can be truth-apt, making rational discourse and knowledge in bioethics possible [2]. |
| Interdisciplinary Dialogue | The methodological framework that allows empirical data and normative analysis to inform and refine each other, creating a coherent justification for conclusions. |
Experimental Protocol: Bridging the Is-Ought Gap
This protocol provides a structured methodology for integrating empirical findings with normative analysis, creating a justified bridge across the is-ought gap.
1. Problem Identification & Literature Review
- Identify a specific ethical dilemma in biomedicine or research (e.g., informed consent for a new genetic therapy).
- Conduct a systematic review of both (a) relevant empirical literature (e.g., studies on patient comprehension of genetic information) and (b) relevant normative literature (e.g., ethical analyses of autonomy and consent).
2. Empirical Data Collection & Analysis
- Objective: To gather robust descriptive data ("is") related to the identified problem.
- Methodology Selection: Choose an appropriate empirical method (e.g., qualitative interviews with stakeholders, quantitative surveys, observational ethnography).
- Execution: Collect and analyze data according to the standards of the chosen methodological discipline (e.g., thematic analysis for interviews, statistical analysis for surveys).
3. Normative Analysis & Premise Articulation
- Objective: To make explicit the ethical values and principles ("ought") relevant to the problem.
- Methodology: Conduct a philosophical analysis to identify and justify the key ethical principles at stake (e.g., respect for persons, justice, well-being). This step involves articulating the normative premises that are often left unstated.
4. Integrative Synthesis
- Objective: To logically connect the empirical findings with the normative framework.
- Methodology: Do not present data and ethics as separate sections. Instead, synthesize them. For example: "Our empirical finding (F) interacts with ethical principle (P) in the following way... Therefore, to uphold principle (P) in light of finding (F), we ought to consider action (A)." This creates a coherent argument where the "ought" is derived from the normative principle, informed and shaped by the empirical facts.
5. Conclusion & Recommendation Formulation
- Formulate specific, actionable recommendations that are logically supported by the integrative synthesis. The conclusion should be a prescriptive statement that is transparently justified by both the empirical evidence and the articulated normative premises.
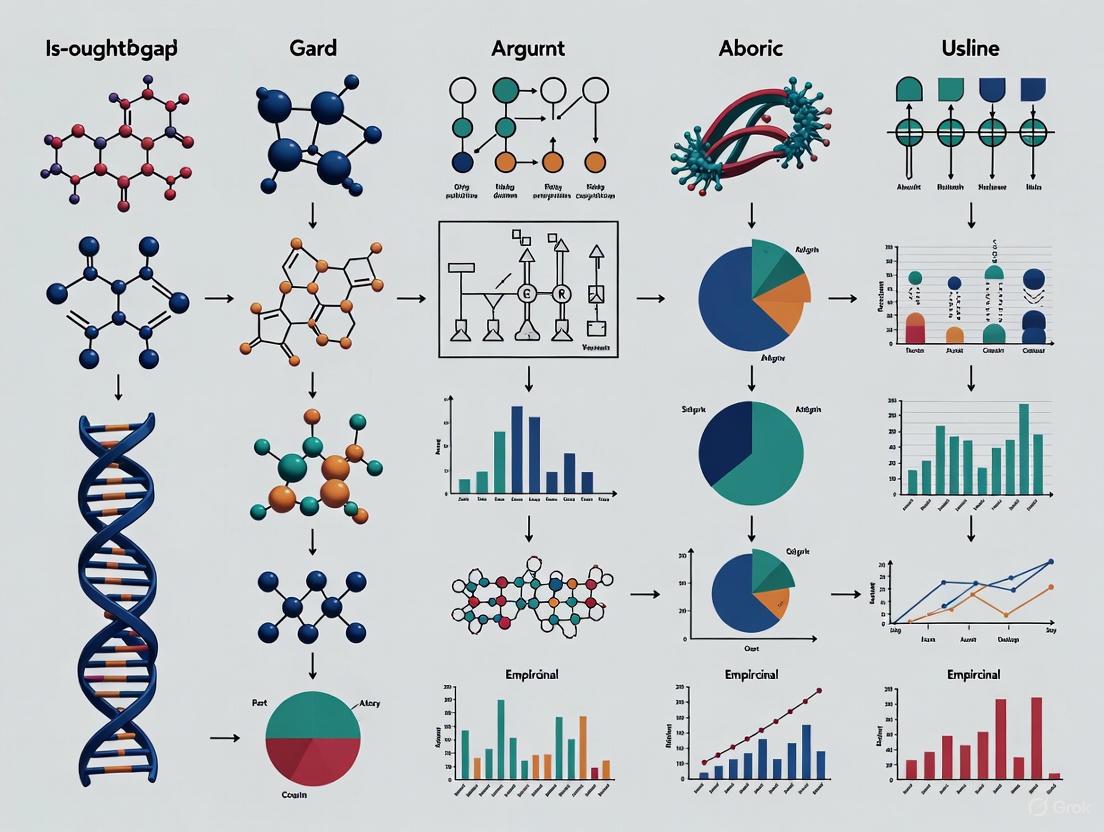
Workflow Diagram
Technical Support Center: Troubleshooting Meta-Ethical Concepts in Empirical Bioethics
This guide helps researchers navigate common conceptual errors when integrating empirical data with normative reasoning. Correctly distinguishing these ideas is foundational to robust and defensible empirical bioethics research.
Troubleshooting Guides
Problem: My empirical data describes what is happening in practice, but reviewers say I cannot conclude what we ought to do.
- Potential Cause: Attempting to directly derive a normative conclusion from purely descriptive premises, which invokes the Is-Ought Problem [1] [2].
- Solution:
- Explicitly state your normative premise. All ethical argumentation requires at least one foundational value judgment [1] [2]. For example: "If a practice causes demonstrable harm to patient well-being (empirical claim), and if we ought to prevent patient harm (normative premise), then we ought to change this practice."
- Use empirical data to test normative assumptions. Data cannot generate an "ought" from nothing, but it can test the feasibility, consequences, and real-world application of existing ethical principles [6] [7].
- Reframe your conclusion. Instead of making a sweeping normative statement, position your finding as identifying an ethical issue, informing the context of a debate, or testing how a known norm functions in practice [6].
Problem: A colleague claims that because a behavior is "natural" or biological, it is therefore ethically justified.
- Potential Cause: Committing the Naturalistic Fallacy, which is the error of defining "good" solely in terms of natural properties or of equating what is natural with what is good [8] [9].
- Solution:
- Challenge the definition. Question whether "natural" is being clearly defined and whether that definition logically entails "good." G.E. Moore's Open-Question Argument is useful here: "Yes, this trait evolved, but is it good?" The very possibility of this question shows the terms are not equivalent [1] [9].
- Provide counterexamples. Identify clear cases where a natural fact (e.g., a disease) is not considered good, or a valued thing (e.g., a vaccine) is not strictly "natural."
- Separate description from evaluation. Clearly differentiate the empirical claim ("This behavior occurs in nature") from the separate, required value judgment ("This behavior is morally desirable") [5].
Problem: My team cannot agree on whether a study finding is an objective fact or a value-laden observation.
- Potential Cause: Confusion around the Fact-Value Distinction, which holds that statements about what is the case (descriptive) are logically different from statements about what ought to be the case (evaluative/prescriptive) [10] [9].
- Solution:
- Perform a language test. Look for value-laden words like "good," "bad," "should," "unjust," or "harmful." Their presence often signals an evaluative claim [9].
- Apply the distinction pragmatically. While some philosophers argue for a strict dichotomy, for practical research purposes, treat it as a warning to be critically aware of when you are reporting data versus when you are interpreting it through a moral framework [2] [10].
- Document the transition. In your research write-up, make a clear and justified connection between the factual evidence you present and the value-based interpretation or recommendation you make [2].
Frequently Asked Questions (FAQs)
Q1: Are the Is-Ought Problem and the Naturalistic Fallacy the same thing? A1: No, they are distinct but related concepts. The Is-Ought Problem, identified by David Hume, is a broader logical challenge about the validity of inferring prescriptive statements ("ought") from descriptive statements ("is") [1] [2]. The Naturalistic Fallacy, coined by G.E. Moore, is a specific instance of this problem where one incorrectly defines "good" in terms of some natural property (like "pleasurable" or "evolutionarily successful") [2] [8] [9]. All instances of the naturalistic fallacy violate the is-ought rule, but not all is-ought violations are naturalistic fallacies.
Q2: How can the Fact-Value Distinction be a problem for scientific research? A2: A strict interpretation of the distinction suggests that science, which deals in empirical facts, is fundamentally separate from ethics and values [10]. This would seem to invalidate the project of empirical bioethics from the start. However, most contemporary approaches reject a rigid dichotomy. Instead, they recognize that while facts and values are different, they are deeply intertwined in practice. Values influence what research questions we ask, how we interpret data, and what we deem a "good" outcome, while facts are essential for understanding the real-world implications of our values [2] [10] [9].
Q3: If we can't derive an "ought" from an "is," how can empirical research possibly inform bioethics? A3: This is the central challenge for empirical bioethics. The solution is not to attempt a direct, logical derivation but to use empirical data in more nuanced ways. Researchers report that data is most useful for:
- Understanding context and identifying ethical issues in practice [6].
- Testing the feasibility and consequences of ethical norms [6] [7].
- Informing the specification of general principles [7]. The "is-ought gap" thus acts not as a barrier, but as a critical warning to reflect carefully on how we integrate facts with our value judgments [2] [6].
Conceptual Comparison Table
The table below summarizes the core differences and relationships between these three key concepts.
| Concept | Core Definition | Primary Proponent | Key Question | Role in Empirical Bioethics |
|---|---|---|---|---|
| Is-Ought Problem [1] [2] | The logical challenge of deriving prescriptive conclusions ("ought") from purely descriptive premises ("is"). | David Hume | How can a statement about what should be validly inferred from statements about what is? | A foundational logical rule warning against unjustified leaps from data to policy. |
| Fact-Value Distinction [10] [9] | An epistemological distinction between statements of fact (descriptive, based on observation) and statements of value (prescriptive, based on ethics/aesthetics). | Derived from Hume; emphasized by Max Weber | How do claims about the world (facts) differ from claims about what is good or right (values)? | A heuristic to maintain awareness of when a researcher is reporting data versus making a value judgment. |
| Naturalistic Fallacy [8] [9] | The specific error of defining "good" in terms of natural properties or inferring that something is good because it is natural. | G.E. Moore | Can the moral quality "good" be defined without remainder by any set of natural properties? | A common pitfall to avoid, particularly when appealing to biology, evolution, or "human nature" in ethical arguments. |
The Researcher's Toolkit: Key Conceptual Reagents
Just as an experiment requires specific materials, clear reasoning in empirical bioethics requires these conceptual tools.
| Tool | Function | Application Example |
|---|---|---|
| Explicit Normative Premise | Provides the necessary ethical foundation for an argument, bridging the is-ought gap [1] [2]. | "Given our commitment to justice (normative premise), and data showing this policy disproportionately harms a vulnerable group (empirical fact), we ought to revise the policy." |
| The Open-Question Test | A mental model to detect the naturalistic fallacy by questioning any definition of "good" [9]. | "You say 'good' is 'what is pleasurable.' But is pleasure always good?" The possibility of this question shows the terms are not synonymous. |
| Descriptive/Evaluative Language Filter | A writing and review check to ensure clarity about when a statement is a fact versus a value judgment [9]. | Flagging words like "should," "unjust," or "harmful" in a manuscript and verifying that the shift from descriptive to evaluative is explicitly justified. |
Logical Workflow for Navigating the Is-Ought Gap
The following diagram maps the logical pathway from empirical observation to an ethically robust conclusion, showing where these conceptual distinctions come into play.
Experimental Protocol: Testing a Normative Claim with Empirical Data
This methodology outlines a robust approach for using empirical research to inform, without improperly deriving, ethical conclusions.
Objective: To evaluate how a specific ethical norm (e.g., "patients ought to be fully informed before consent") functions in a real-world clinical context.
Background: The Is-Ought Problem forbids creating a norm from data alone, but data can test a norm's application and consequences [6] [7].
Procedure:
- Normative Specification: Begin with a clear, general ethical principle (e.g., "Respect for persons requires informed consent") [7].
- Operationalization: Define measurable empirical indicators for the norm. For informed consent, this could be:
- Indicator 1: Patient recall of procedural risks.
- Indicator 2: Patient understanding of alternative treatments.
- Indicator 3: Patient perception of coercion.
- Data Collection: Employ mixed methods (e.g., surveys to quantify understanding, in-depth interviews to qualify patient experience) to gather data on these indicators [6].
- Integration & Analysis:
- Compare the empirical findings against the ideal expressed by the norm.
- Identify barriers (e.g., complex medical language, time constraints) that cause the "is" (practice) to diverge from the "ought" (norm) [6] [7].
- Use these findings not to create a new norm, but to specify or refine how the original norm can be better enacted (e.g., "The principle of informed consent necessitates the use of plain-language guides and dedicated consent counselors") [7].
Expected Outcome: The research provides an evidence-based justification for specific practices and policies that uphold a core ethical principle, thereby bridging the "is-ought" gap through specification and application rather than faulty derivation.
Frequently Asked Questions
Q1: What are Hume's Law and the Is-Ought Problem, and why are they relevant to my empirical bioethics research?
Hume's Law, originating from philosopher David Hume, is the thesis that an ethical or judgmental conclusion (an "ought") cannot be logically inferred from purely descriptive, factual statements (an "is") [1]. This is also known as the Is-Ought Problem. For empirical bioethics, which integrates empirical data with normative analysis, this poses a potential foundational challenge: if "no ought from is," how can bioethics be empirical? [2] However, this is often seen not as an insurmountable barrier, but as a critical warning sign to carefully reflect on the normative implications of empirical results [11].
Q2: Aren't Hume's Law, the fact-value distinction, and the naturalistic fallacy the same thing?
No, this is a common conflation in bioethics literature [2]. They are distinct though interrelated concepts:
- Hume's Law deals with the logical relationship between descriptive ("is") and prescriptive ("ought") statements [2] [1].
- The Naturalistic Fallacy, a term coined by G.E. Moore, is the claim that it is a fallacy to define "good" in terms of natural properties, representing a meta-ethical refutation of ethical naturalism [2].
- The Fact-Value Distinction is the view that facts and values are distinct, sometimes encompassing the idea that science is value-free [2].
Q3: What practical challenges might I face when integrating empirical data with normative analysis?
Researchers often report an "air of uncertainty and overall vagueness" during integration [12]. Key challenges include:
- Methodological Indeterminacy: While many methodologies exist (e.g., reflective equilibrium, dialogical ethics), their practical steps are often unspecific, leading to flexibility but also potential obscurity [12].
- Weighting Evidence: It can be difficult to determine how much weight to give empirical data versus ethical theory during the analytic process [12].
- Ethical Disruption: The research process itself can be disruptive, as it may require participants to critically explore settled moral views, potentially leaving them feeling unsettled or that they are "in the wrong" [13].
Q4: What are the acceptable objectives for conducting empirical research in bioethics?
A qualitative study of bioethics researchers found varying levels of agreement on different objectives [11]. The most and least supported objectives are summarized in the table below.
Table 1: Acceptability of Objectives for Empirical Research in Bioethics
| Objective of Empirical Research | Level of Acceptance |
|---|---|
| Understanding the context of a bioethical issue | Unanimous agreement [11]. |
| Identifying ethical issues in practice | Unanimous agreement [11]. |
| Striving to draw normative recommendations | Highly contested [11]. |
| Developing and justifying moral principles | Highly contested [11]. |
Troubleshooting Common Experimental Issues
Problem: Uncertainty in choosing a methodology for integrating empirical and normative analysis.
Solution: Familiarize yourself with established methodological families. Select a method that aligns with your research question and epistemological stance, and be prepared to justify your choice transparently [12].
Table 2: Methodologies for Integrating Empirical and Normative Analysis
| Methodology | Core Approach | Key Characteristics |
|---|---|---|
| Reflective Equilibrium [12] | A "back-and-forth" process of adjustment by the researcher. | The researcher ("the thinker") iteratively moves between ethical principles, empirical data, and considered judgments until a state of moral coherence ("equilibrium") is achieved. A consultative model. |
| Dialogical Empirical Ethics [12] | Relies on structured discourse between stakeholders. | Integration occurs through collaboration and dialogue between researchers, participants, and other stakeholders to reach a shared understanding. A dialogical model. |
| Grounded Moral Analysis [12] | Develops normative conclusions directly from empirical data. | The empirical and normative elements are intertwined from the start of the research project, with moral principles being developed or refined through the analysis of data. An inherent integration model. |
Problem: Navigating the Is-Ought gap when deriving normative recommendations from data.
Solution: Do not treat empirical data as a direct source of moral "oughts." Instead, use it to test, refine, and inform the application of normative principles within a specific context [11]. The following workflow, often used in Reflective Equilibrium, visualizes this process.
Problem: My research team has different disciplinary backgrounds, leading to confusion about the role of empirical findings.
Solution: Establish clear objectives and theoretical positioning early in the research process [12]. Use the following chart to clarify how empirical research functions within the broader bioethical inquiry and to identify potential sources of interdisciplinary confusion.
The Scientist's Toolkit: Key Research Reagents
This toolkit outlines essential conceptual "reagents" for designing and executing a rigorous empirical bioethics study.
Table 3: Essential Conceptual Tools for Empirical Bioethics Research
| Tool Name | Function | Application Notes |
|---|---|---|
| Bridge Postulate [2] | Foundational assumption that a connection between facts and values is possible. | A necessary meta-ethical starting point that justifies the entire empirical bioethics endeavor. |
| Ethical Cognitivism Postulate [2] | Assumption that ethical statements can be truth-apt and that ethical knowledge is possible. | Positions your research within a mainstream meta-ethical framework, countering non-cognitivist interpretations of Hume's Law. |
| "Reasonable Person" Standard [14] | A normative benchmark for interpreting empirical data on participant preferences. | Used, for example, to determine what information should be provided during informed consent by referencing what a "reasonable person" would want to know. |
| Transparency in Integration [12] | The practice of explicitly stating and justifying how empirical data and normative analysis are combined. | A crucial standard for methodological rigor. Researchers must clearly explain their chosen method of integration and how it was executed. |
Empirical bioethics faces a fundamental challenge: how can researchers legitimately integrate descriptive statements about what is (facts derived from empirical data) with prescriptive statements about what ought to be (moral values and norms)? This problem, known as the is-ought gap or Hume's Law, presents a significant methodological hurdle [2]. The Bridge Postulate addresses this challenge directly by asserting that a bridge between facts and values is not only possible but foundational to the entire bioethics endeavor [2]. This technical framework provides researchers, scientists, and drug development professionals with practical methodologies and troubleshooting guidance for implementing this postulate in their experimental research, enabling them to navigate the complex terrain between empirical observation and normative recommendation without committing logical fallacies.
Understanding the Conceptual Framework
Defining the Is-Ought Problem and Its Implications
The is-ought problem, derived from David Hume's philosophical work, highlights the logical distinction between descriptive statements (what "is") and prescriptive statements (what "ought" to be) [2]. In contemporary terminology, this means that no set of purely descriptive statements can entail an evaluative statement without additional evaluative premises [2]. For bioethics researchers, this creates a significant methodological challenge when attempting to derive ethical recommendations from empirical data alone.
Three distinct concepts are often conflated in this discussion but must be carefully distinguished:
- Hume's Law: Concerns the logical relationship between "is" and "ought" statements
- Naturalistic Fallacy: A term introduced by G.E. Moore referring to defining "good" in terms of natural properties
- Fact-Value Distinction: The view that factual statements and value statements have different truth conditions [2]
The Bridge Postulate: Core Principles
The Bridge Postulate rests on two foundational principles that guide empirical bioethics research:
Bridge Possibility Principle: A bridge between facts and values is both possible and foundational to bioethics, though the nature of this bridge remains open to methodological discussion and refinement [2].
Ethical Cognitivism Principle: Unless explicitly stated otherwise, bioethics operates within ethical cognitivism - the view that ethical statements are truth-apt and that knowledge is possible in ethics [2].
These principles enable researchers to proceed with empirical-normative integration while maintaining philosophical rigor, providing a framework for developing methodologies that explicitly address the is-ought challenge rather than ignoring it.
Methodological Framework: Mapping, Framing, Shaping
The Mapping-Framing-Shaping framework provides a structured approach to empirical bioethics research projects, offering a comprehensive methodology for implementing the Bridge Postulate in practice [15].
Phase 1: Mapping the Terrain
The mapping phase involves surveying existing knowledge to understand the current state of research and identify gaps [15].
Experimental Protocol: Systematic Literature Mapping
Objective: To comprehensively identify and analyze existing literature, policies, and empirical data relevant to the bioethical issue under investigation.
Methodology:
- Conduct systematic searches across relevant databases (e.g., PubMed, SCOPUS, specialized ethics databases)
- Identify and analyze key concepts, controversies, and consensus positions in the literature
- Map relationships between different stakeholder perspectives and evidence types
- Identify knowledge gaps and methodological limitations in existing research
Technical Requirements:
- Access to comprehensive academic databases
- Reference management software (e.g., EndNote, Zotero)
- Qualitative data analysis software for thematic analysis (e.g., NVivo, Atlas.ti)
Troubleshooting Guide:
- Problem: Overwhelming volume of irrelevant literature in search results.
- Solution: Refine search strategy using Boolean operators, field-specific filters, and iterative search techniques.
- Problem: Inconsistent terminology across disciplines.
- Solution: Develop a comprehensive taxonomy of relevant terms and conduct synonym searches.
Phase 2: Framing Stakeholder Perspectives
The framing phase involves in-depth exploration of how stakeholders experience and perceive the ethical issues identified in the mapping phase [15].
Experimental Protocol: Qualitative Stakeholder Framing
Objective: To understand how ethical issues are framed, experienced, and perceived by relevant stakeholders.
Methodology:
- Identify and recruit diverse stakeholders through purposive sampling
- Conduct in-depth interviews, focus groups, or ethnographic observations
- Analyze qualitative data using established techniques (thematic analysis, grounded theory)
- Identify patterns in how stakeholders frame ethical problems and potential solutions
Technical Requirements:
- Interview/focus group guides tailored to different stakeholder groups
- Audio recording equipment and transcription services
- Qualitative data analysis software
- Ethical approval for research involving human participants
Troubleshooting Guide:
- Problem: Stakeholders provide socially desirable responses rather than genuine perspectives.
- Solution: Establish rapport, ensure anonymity, use indirect questioning techniques.
- Problem: Conflicting perspectives between different stakeholder groups.
- Solution: Maintain detailed records of contextual factors influencing different perspectives.
Phase 3: Shaping Ethical Recommendations
The shaping phase involves developing normative recommendations informed by the preceding mapping and framing phases [15].
Experimental Protocol: Integrative Ethical Analysis
Objective: To develop ethically justified recommendations that are informed by both empirical evidence and normative analysis.
Methodology:
- Explicitly articulate the method of integration between empirical findings and normative reasoning
- Identify points of convergence and divergence between different evidence sources
- Develop recommendations through reflective equilibrium, balancing principles, evidence, and case judgments
- Specify limitations and conditions for application of recommendations
Technical Requirements:
- Documentation of the entire research process for transparency
- Framework for assessing the strength and quality of different types of evidence
- Method for addressing residual uncertainty and disagreement
Troubleshooting Guide:
- Problem: Empirical data appears to conflict with established ethical principles.
- Solution: Re-examine interpretation of data and application of principles; consider mid-level principles to mediate between abstract theory and empirical facts.
- Problem: Difficulty in justifying why certain empirical findings should influence normative conclusions.
- Solution: Explicitly articulate the relevance of specific facts to ethical values through "bridging premises."
The following diagram illustrates the overall workflow and the critical integration points in this methodology:
Research Reagent Solutions: Methodological Tools
Table 1: Essential Methodological Tools for Empirical Bioethics Research
| Tool Category | Specific Methods/Techniques | Primary Function | Application Context |
|---|---|---|---|
| Data Collection | Semi-structured interviews | Elicit rich, nuanced stakeholder perspectives | Framing phase: understanding lived experiences |
| Focus groups | Identify group dynamics and shared understandings | Framing phase: exploring collective perspectives | |
| Systematic surveys | Quantify attitudes, beliefs, and preferences | Mapping phase: establishing prevalence of views | |
| Data Analysis | Thematic analysis | Identify, analyze, and report patterns in qualitative data | Framing phase: analyzing interview/focus group data |
| Content analysis | Systematically categorize textual content | Mapping phase: analyzing literature and documents | |
| Ethical matrix | Structure evaluation of options against ethical principles | Shaping phase: comparative ethical analysis | |
| Integration Methods | Reflective equilibrium | Achieve coherence between principles, cases, and judgments | Shaping phase: developing justified recommendations |
| Mid-level principles | Mediate between abstract theory and empirical facts | Shaping phase: bridging theory and practice | |
| Case-based reasoning | Use paradigm cases to inform new situations | Shaping phase: analogical reasoning in ethics |
Frequently Asked Questions: Troubleshooting Common Challenges
Conceptual and Methodological Challenges
Q: How can we avoid deriving "ought" directly from "is" when making recommendations based on empirical data?
A: The key is to explicitly include normative premises that justify why specific facts are morally relevant. For example, instead of moving directly from "patients prefer X" to "we should do X," include the bridging premise: "patient preferences should be respected in contexts Y and Z, with exceptions A, B, and C." Document these bridging premises transparently in your methodology [2] [11].
Q: What is the difference between doing ethics by opinion poll and legitimate empirical bioethics research?
A: Ethics by opinion poll merely aggregates and reports what people think should be done. Legitimate empirical bioethics uses empirical data to inform ethical analysis by:
- Illuminating the context of ethical decisions
- Testing empirical assumptions in ethical arguments
- Understanding how ethical principles are interpreted and applied in practice
- Identifying unanticipated ethical challenges [11] [16]
Q: How should we handle conflicting values or perspectives identified through empirical research?
A: Value conflicts should not be suppressed or ignored. Instead:
- Map the conflicts systematically using value taxonomy
- Analyze the sources and nature of disagreements
- Explore possibilities for resolution or accommodation
- Develop recommendations that acknowledge persistent disagreements where they exist
- Consider procedural solutions when substantive agreement is impossible [17]
Implementation and Analytical Challenges
Q: What sample sizes are appropriate for qualitative research in empirical bioethics?
A: Sample size in qualitative research is determined by the principle of saturation rather than statistical power. Typically, researchers continue data collection until no new themes or insights are emerging. For interview studies, this often occurs between 15-30 participants per stakeholder group, but can vary based on the diversity of perspectives and complexity of the topic [11].
Q: How can we ensure methodological rigor in qualitative empirical bioethics?
A: Ensure rigor through:
- Transparency about methods and limitations
- Triangulation of data sources and methods
- Member checking (validating interpretations with participants)
- Peer debriefing and independent analysis where possible
- Clear audit trails of analytical decisions [11] [15]
Q: What is the appropriate role of quantitative methods in empirical bioethics?
A: Quantitative methods are valuable for:
- Establishing prevalence of practices, attitudes, or experiences
- Identifying patterns and correlations in large datasets
- Testing hypotheses about factors influencing ethical decision-making
- Generalizing findings from qualitative research to larger populations However, quantitative data still requires normative interpretation and should not be viewed as mechanically determining ethical conclusions [16].
Advanced Integration Techniques and Validation
Digital Methods for Empirical Bioethics
Emerging digital methods offer new approaches for implementing the Bridge Postulate:
Table 2: Digital Methods for Empirical Bioethics Research
| Method | Description | Application Example | Technical Requirements |
|---|---|---|---|
| Computational text analysis | Automated analysis of large text corpora | Identifying themes in social media discussions of bioethical issues | Natural language processing libraries, programming skills |
| Network analysis | Mapping relationships between concepts or stakeholders | Analyzing policy networks or conceptual relationships in ethics literature | Network analysis software, data visualization tools |
| Sentiment analysis | Automated classification of emotional valence in text | Tracking public sentiment about emerging technologies | Text analysis algorithms, validated dictionaries |
These digital methods can enhance traditional approaches by enabling analysis of larger datasets and identifying patterns that might not be apparent through manual methods alone [18].
Validation Framework for Empirical Bioethics Methods
Robust validation of methodological approaches is essential for ensuring the reliability of empirical bioethics research:
Validation Protocol: Methodological Quality Assessment
Objective: To establish that the chosen methodology reliably produces knowledge relevant to the research questions.
Methodology:
- Preliminary Development: Define method scope, endpoints, and analytical requirements
- Feasibility Testing: Verify that methods can be implemented as designed and produce useful data
- Internal Validation: Establish that methods produce consistent, reliable results within a single research context
- External Validation: Demonstrate that methods can be successfully implemented across different research contexts [19]
Quality Indicators:
- Transparency about methodological choices and limitations
- Appropriate handling of conflicting evidence and perspectives
- Explicit documentation of the integration process between empirical and normative elements
- Critical reflection on researcher positionality and potential biases
The Bridge Postulate provides a foundational principle for empirical bioethics research: while facts alone cannot determine values, and values alone cannot determine facts, a disciplined methodological bridge between them is both possible and essential for addressing complex bioethical challenges. The frameworks, methods, and troubleshooting guides presented here offer researchers practical approaches for implementing this postulate while maintaining philosophical rigor. By transparently documenting their bridging methodologies and critically reflecting on their integrative approaches, researchers can produce work that simultaneously respects the logical distinction between facts and values while building constructive pathways between them. This enables empirical bioethics to fulfill its potential of developing normative recommendations that are both philosophically sound and empirically informed.
Ethical Cognitivism as a Shared Meta-Ethical Postulate in Bioethics
FAQs: Navigating Meta-Ethical Foundations and Research Practice
FAQ 1: What is ethical cognitivism and why is it a foundational postulate in bioethics? Ethical cognitivism is the meta-ethical view that ethical sentences (e.g., "informed consent is obligatory") express propositions and can therefore be true or false (they are truth-apt) [20]. This stands in direct opposition to non-cognitivism, which denies that moral sentences express beliefs that can be true or false, instead viewing them as expressions of emotion, attitudes, or prescriptions [21].
Within bioethics, ethical cognitivism serves as a core shared postulate. This means that unless explicitly stated otherwise, bioethical discourse operates on the assumption that ethical statements are truth-apt and that knowledge is possible in ethics [2]. This foundational stance makes rational deliberation and argument about ethical issues possible, as it allows for the existence of correct and incorrect answers to ethical questions, which is crucial for guiding clinical practice and policy.
FAQ 2: How does cognitivism relate to the classic 'Is-Ought Problem' in empirical bioethics? The 'Is-Ought Problem' (Hume's Law) questions the logical derivation of normative claims ("ought") from descriptive facts ("is") and is often raised as a challenge to empirical bioethics [2]. The force of this challenge, however, is heavily dependent on one's meta-ethical stance.
A non-cognitivist interpretation of Hume's Law establishes a strict logical gulf between facts and values, making the integration of empirical data into normative reasoning particularly problematic [2]. In contrast, a cognitivist framework provides a different landscape. Cognitivism allows for the possibility that ethical propositions can be objectively true, even if not through a direct correspondence with physical entities [20]. This opens the door for more nuanced ways of bridging the "is-ought" gap, such as through coherence theories of truth or by viewing normative reasoning as analogous to other normative domains like mathematics [20]. Therefore, adopting ethical cognitivism as a postulate mitigates the logical threat of Hume's Law and supports the project of integrating empirical research with normative ethics.
FAQ 3: What are the practical implications of adopting a cognitivist stance for a research team? Adopting a cognitivist stance has direct consequences for research design and team discourse:
- Rational Resolution of Disagreements: Team members can operate on the premise that ethical disagreements are subject to rational argument and evidence, rather than being mere clashes of subjective preference. This encourages deliberation aimed at finding the most justified position.
- Clarity in Argumentation: It mandates that normative claims (e.g., "this trial design is unethical") be supported by reasons and evidence that purport to be truth-tracking, rather than being asserted as simple expressions of approval or disapproval.
- Framework for Empirical-Normative Integration: It provides a philosophical foundation for methodologies that seek to use empirical data (e.g., on patient preferences or quality of life) to inform normative conclusions, as it holds that such conclusions can be validly true or false [2].
FAQ 4: Our team is facing a disagreement on an ethical judgment. How can a shared cognitivist postulate guide our deliberation? A shared commitment to cognitivism provides a structured pathway for conflict resolution:
- Articulate Competing Propositions: Frame the disagreement as a conflict between two or more potentially truth-apt propositions (e.g., "Proposition A: Providing treatment X is obligatory" vs. "Proposition B: Providing treatment X is not obligatory").
- Identify Supporting Evidence and Principles: For each proposition, require advocates to present their supporting evidence, including relevant empirical data, ethical principles (e.g., beneficence, autonomy), and analogies to paradigm cases [22].
- Seek a Coherent Conclusion: Deliberate on which proposition forms the most coherent and justified conclusion based on the totality of the evidence and principles, with the goal of identifying the position most likely to be true.
FAQ 5: How can we methodologically bridge the "is-ought" gap when designing empirical bioethics research? The "Ought-Is" problem—translating established norms into practice—can be addressed by integrating principles from implementation science into the ethics research process [7]. The following workflow outlines a structured approach to bridge this gap.
Diagram 1: A framework for translating ethical norms into practice, integrating implementation science principles [7].
Troubleshooting Guides: Common Scenarios and Solutions
Scenario 1: Handling Non-Cognitivist Challenges
- Problem: A colleague argues that a specific ethical recommendation is "just your opinion" and not objectively defensible, reflecting a non-cognitivist challenge.
- Diagnosis: This is a fundamental meta-ethical disagreement that can stall productive discussion.
- Solution:
- Re-affirm Shared Goal: Clarify that the team's default operating principle (postulate) is that ethical claims can be more or less justified based on reasons and evidence.
- Shift to Reasons: Ask the colleague to provide reasons why they disagree with the recommendation, thereby implicitly engaging in cognitivist practice.
- Appeal to Paradigm Cases: Reference clear, widely accepted ethical precedents (e.g., "It is wrong to experiment on humans without consent") to demonstrate that not all ethical judgments are merely subjective [22].
- Problem: A researcher is uncertain how to use descriptive data from a survey (an "is") to make a policy recommendation (an "ought").
- Diagnosis: This is a direct encounter with the Is-Ought problem in research practice.
- Solution:
- Make Normative Premises Explicit: The inference from data to recommendation requires at least one implicit normative premise. State it clearly.
- Empirical Finding (Is): 95% of patients in the study desire detailed information about all treatment risks.
- Explicit Normative Premise (Ought): Clinical practices ought to respect the autonomous preferences of patients where possible.
- Normative Conclusion (Ought): Therefore, clinicians ought to provide detailed information about all treatment risks.
- Use a Structured Framework: Employ a structured framework, like the "four boxes" method, to organize the empirical facts and their relationship to key ethical principles [22]. This makes the normative reasoning process transparent and systematic.
- Make Normative Premises Explicit: The inference from data to recommendation requires at least one implicit normative premise. State it clearly.
Scenario 3: Managing Disagreement on Risk-Benefit Analysis
- Problem: The research team is deadlocked over whether the potential benefits of a novel drug outweigh its risks in a clinical trial.
- Diagnosis: Disagreement may stem from different weightings of the same facts or from differing interpretations of incomplete data.
- Solution:
- Deconstruct the Analysis: Break down the risk-benefit judgment into its component propositions using a structured table.
- Systematic Deliberation: Use the table to isolate the precise points of disagreement, focusing deliberation on the evidence for each component.
Table 1: Framework for Deconstructing a Risk-Benefit Disagreement
| Component Proposition | Evidence (Facts/ 'Is') | Conflicting Interpretations / Weightings ('Ought' Judgments) |
|---|---|---|
| Benefit is clinically significant. | Phase II data shows 40% tumor reduction in 30% of participants. | View A: This represents a meaningful therapeutic benefit for a severe condition. View B: The effect is not robust enough to be considered significant. |
| Risks are manageable. | 15% of participants experienced severe but reversible side effects. | View A: The reversibility makes these risks acceptable. View B: A 15% rate of severe events is unacceptably high. |
| The risk-benefit profile is favorable. | Synthesis of the above data. | View A: The potential for significant benefit justifies the known risks. View B: The severity and frequency of risks outweigh the uncertain benefit. |
Table 2: Essential Meta-Ethical and Methodological "Reagents" for Empirical Bioethics Research
| Conceptual Tool | Function in Research | Key Characteristics |
|---|---|---|
| Ethical Cognitivism [20] [2] | Provides the foundational postulate that ethical statements can be true or false, enabling rational argument and knowledge accumulation in ethics. | Truth-apt, belief-expressing, encompasses both realism and error theory. |
| The Four-Topics Method [22] | A structured clinical ethics tool for case analysis; organizes facts of a case into Medical Indications, Patient Preferences, Quality of Life, and Contextual Features to facilitate ethical decision-making. | Practical, case-based, promotes systematic and comprehensive analysis. |
| Implementation Science Framework [7] | Provides a disciplined approach to translating established ethical norms ("ought") into widespread practice ("is"), addressing the "Ought-Is" problem. | Focused on sustainability, assesses barriers and facilitators (e.g., via CFIR). |
| Aspirational vs. Specific Norms [7] | Distinguishes between broad, inspirational ethical goals and concrete, actionable rules, guiding the development of feasible research interventions. | Aspirational: General, "true North." Specific: Directed, incremental, feasible. |
| Paradigm Case [22] | A clear, precedent-setting case where there is broad agreement on the ethical resolution; used as an analogical reference point for analyzing novel cases. | Provides reference, aids in pattern recognition, and grounds ethical reasoning. |
From Theory to Practice: Methodological Frameworks for Integration
Reflective equilibrium is a state of balance or coherence among a set of beliefs arrived at by a process of deliberative mutual adjustment among general principles and particular judgements [23]. Philosopher John Rawls, who coined the term, proposed this method to address concerns that our moral judgments alone may not justify the moral views they express, as they can be "fraught with idiosyncrasy and vulnerable to vagaries of history and personality" [24]. The method provides a systematic approach to moral reasoning that allows us to generate considered moral judgments from a wide variety of initial beliefs and intuitions [25].
In empirical bioethics research, reflective equilibrium offers a crucial methodological framework for addressing the is-ought gap—the philosophical challenge of deriving normative claims ("ought") from empirical facts ("is") [7]. By providing a structured process for moving between empirical observations and normative principles, reflective equilibrium helps researchers navigate this traditional divide in a principled manner.
The Three Levels of Moral Inquiry
The process of reflective equilibrium involves reflecting on three interconnected levels of moral thinking [25]:
- Level 1: Particular Case Judgments: Intuitive moral responses to specific situations or cases
- Level 2: General Moral Principles: Mid-level rules that guide decision-making across multiple cases
- Level 3: Theoretical Considerations: Broader philosophical theories and background considerations
The Iterative Process
Reaching reflective equilibrium requires continuous adjustment among these three levels [24] [25]. When conflicts arise between different levels—for instance, when a general principle conflicts with multiple considered judgments about particular cases—we must adjust our views at each level until we achieve coherence. This process continues until our principles, judgments, and background theories form a stable, coherent set [23].
Troubleshooting Common Implementation Challenges
FAQ: Frequently Encountered Problems
Q: What should I do when my general principles consistently conflict with my intuitions about specific cases? A: This indicates a need to refine your principles. Don't automatically discard either element—instead, examine whether your principles are overly broad or whether your intuitions might be influenced by bias. Consider formulating exception clauses or intermediate principles that can accommodate the conflicting judgments while maintaining theoretical coherence [24] [25].
Q: How do I handle situations where I have low confidence in my moral judgments? A: Rawls suggests we can "discard those judgments made with hesitation, or in which we have little confidence" [24]. However, an alternative view suggests that lack of confidence alone shouldn't exclude judgments from consideration, as they may represent important but underdeveloped moral commitments that could find support during the reflective process [24].
Q: What happens when background theories from different disciplines provide conflicting guidance? A: This is common in interdisciplinary bioethics research. The solution is to engage in "wide reflective equilibrium," which involves considering all relevant philosophical arguments and scientific evidence, then seeking the most coherent combination of these elements, even if this requires revising initial commitments [24] [23].
Q: How can I address the is-ought gap when applying reflective equilibrium in empirical bioethics? A: Rather than viewing the is-ought gap as an insurmountable barrier, treat it as a warning sign to critically reflect on the normative implications of empirical results [11]. The iterative process of reflective equilibrium allows for normative principles to be tested against empirical reality and empirical observations to be interpreted through normative frameworks.
Common Implementation Errors and Solutions
Table 1: Troubleshooting Common Reflective Equilibrium Implementation Problems
| Problem Scenario | Root Cause | Recommended Solution | Prevention Strategy |
|---|---|---|---|
| Consistent inability to reach coherence between principles and judgments | Overly rigid adherence to initial principles | Consider "radical" reflective equilibrium allowing comprehensive revision of initial beliefs [24] | Adopt a provisional attitude toward all moral beliefs at the outset |
| Circular justification where principles simply restate judgments | Lack of critical distance from initial intuitions | Introduce new cases or theoretical perspectives to break the circularity | Systematically seek out counterexamples and challenging cases |
| Disregard of relevant empirical evidence | Artificial separation of empirical and normative inquiry | Actively incorporate scientific background theories into wide reflective equilibrium [23] | Form interdisciplinary teams with both empirical and normative expertise |
| Paralysis from constant revision | Lack of provisional fixed points | Identify "considered judgments" that serve as relatively stable reference points [24] | Recognize that reflective equilibrium is always provisional and can be revisited |
Research Protocols for Empirical Bioethics Applications
Protocol 1: Establishing Wide Reflective Equilibrium in Bioethics Research
Purpose: To develop morally coherent positions on bioethical issues through systematic integration of considered judgments, moral principles, and relevant background theories [23].
Methodology:
- Identify Considered Judgments: Collect moral intuitions about specific cases under conditions conducive to moral deliberation (adequate information, emotional calm, impartiality) [24]
- Articulate Candidate Principles: Formulate general principles that potentially explain the considered judgments
- Gather Background Theories: Collect relevant scientific facts, philosophical arguments, and practical constraints
- Test for Coherence: Identify conflicts between judgments, principles, and theories
- Engage in Mutual Adjustment: Revise elements at all levels to achieve greater coherence
- Achieve Equilibrium: Continue process until arriving at a stable, coherent set of beliefs
Validation Measure: The robustness of the resulting position is measured by its ability to withstand challenging counterexamples and explain a wide range of moral judgments [24].
Protocol 2: Bridging the Is-Ought Gap Through Implementation Science
Purpose: To translate ethical norms into practice by integrating implementation science principles with reflective equilibrium [7].
Methodology:
- Develop Aspirational Norms: Formulate broad ethical ideals (e.g., "No one should die of hunger")
- Specify Actionable Norms: Develop specific, implementable norms through reflective equilibrium (e.g., "Physicians should screen for food insecurity")
- Design Interventions: Create practical interventions to enact the specific norms
- Measure Outcomes: Implement interventions and assess their effectiveness
- Refine Through Reflection: Use empirical results to refine norms and principles through reflective equilibrium
Validation Measure: Successful implementation of ethical norms in practice, measured through both ethical coherence and practical effectiveness [7].
Analytical Framework for Assessing Moral Coherence
Quantitative Measures of Reflective Equilibrium
Table 2: Metrics for Evaluating Progress Toward Reflective Equilibrium
| Metric Category | Specific Measures | Interpretation Guidelines | Data Sources |
|---|---|---|---|
| Coherence Indicators | Number of unresolved conflicts between principles and judgments | Fewer conflicts indicate progress toward equilibrium | Documentation of reasoning process |
| Scope of cases explained by principle set | Broader explanatory scope indicates more robust equilibrium | Case analysis records | |
| Stability Measures | Frequency of revision required for core principles | Decreasing revision frequency suggests approaching equilibrium | Version control of principle formulations |
| Resilience to new counterexamples | Resistance to disruption by new cases indicates mature equilibrium | Testing with novel cases | |
| Empirical-Normative Integration | Number of empirical facts successfully incorporated into normative framework | Higher integration indicates successful wide reflective equilibrium [23] | Interdisciplinary research documentation |
Key Conceptual Tools for Implementing Reflective Equilibrium
Table 3: Essential Methodological Resources for Reflective Equilibrium Research
| Tool Category | Specific Tool | Function in Research Process | Application Example |
|---|---|---|---|
| Judgment Refinement Tools | "Considered judgment" criteria [24] | Identifies which moral intuitions to include in the process | Filtering out judgments made under emotional distress |
| Confidence assessment | Prioritizes judgments based on certainty level | Focusing adjustment efforts on low-confidence areas | |
| Theoretical Integration Tools | Wide reflective equilibrium framework [23] | Incorporates background theories and philosophical arguments | Integrating scientific facts about pain perception into end-of-life ethics |
| Principles-judgments-case triads | Structures the relationship between different belief levels | Mapping connections between autonomy principle and specific consent decisions | |
| Implementation Tools | Consolidated Framework for Implementation Research (CFIR) [7] | Identifies barriers and facilitators for translating norms to practice | Assessing organizational readiness for new ethical guidelines |
Advanced Application: Addressing the Is-Ought Gap in Bioethics
The method of reflective equilibrium provides a systematic approach to addressing the fundamental is-ought challenge in empirical bioethics research. Rather than attempting to derive normative conclusions directly from empirical facts, reflective equilibrium creates a structured process for mutual adjustment between empirical observations and normative principles [11].
Research with bioethics scholars reveals that the most accepted objectives for empirical research in bioethics include "understanding the context of a bioethical issue" and "identifying ethical issues in practice" [11]. These objectives align well with the reflective equilibrium method, which uses empirical findings to test, refine, and develop moral principles through an iterative process of reflection and adjustment.
The implementation science framework complements this approach by providing a pathway from normative reflection to practical action, creating a complete cycle from empirical observation to normative refinement to practical implementation and back to empirical assessment [7]. This integrated approach acknowledges that "ethical statements that pose as short-term action items but cannot be implemented might foster guilt, cynicism, or despondency and inaction" [7], thus emphasizing the importance of feasible normative guidance.
Frequently Asked Questions
| Question | Answer |
|---|---|
| What is the primary goal of Dialogical Empirical Ethics? | To address ethical issues by setting up structured dialogues with stakeholders, using their concrete experiences as a source for moral learning and developing normative conclusions together, rather than the ethicist working in isolation [26]. |
| How can this method help bridge the "is-ought" gap? | It tackles the is-ought problem by treating empirical data not as a direct source of norms, but as a crucial element for reflection within a dialogical process. This process helps test and develop normative stances that are grounded in the reality of practice [12] [6]. |
| What is a common challenge when integrating empirical data with normative analysis? | The process is often experienced as vague or unclear. Methodologies like reflective equilibrium and dialogical approaches can be frustratingly indeterminate in practice, risking a lack of theoretical rigor [12]. |
| What is the role of the ethicist in this process? | The ethicist acts as a facilitator of the dialogical process, guiding the exchange of experiences and reflection among stakeholders to shape normative conclusions, rather than being the sole analyst [26]. |
| Which objectives of empirical research in bioethics are most acceptable to researchers? | Understanding the context of a bioethical issue and identifying ethical issues in practice receive strong support. Objectives like drawing direct normative recommendations or justifying moral principles are more contested [6]. |
Troubleshooting Common Experimental Challenges
Problem: Unclear Methodological Path for Integration
- Symptoms: Uncertainty about how to combine empirical findings (the "is") with ethical analysis (the "ought"); confusion between different methodologies like reflective equilibrium and dialogical ethics.
- Solution:
- Clearly State Theoretical Position: Justify why a particular methodological approach (e.g., dialogical, consultative) was chosen for your project [12].
- Choose a Structured Dialogical Method: Adopt a framework like Responsive Evaluation, which involves eliciting stakeholder stories, exchanging experiences in homogeneous and heterogeneous groups, and collectively drawing normative conclusions [26].
- Document the Process: Be transparent about how the integration was carried out step-by-step to mitigate vagueness [12].
- Symptoms: Criticism that the research is attempting to derive normative claims directly from descriptive data; difficulty in defending the normative weight of the study's outcomes.
- Solution:
- Frame the Gap as a Warning, Not a Barrier: Treat the is-ought gap as a critical signpost to reflect on the limits of your empirical data, not as an insurmountable obstacle [6].
- Use Empirical Data as a Testing Ground: Position your empirical findings as a way to test, challenge, and refine existing elements of normative theory, rather than as the sole foundation for new norms [6].
- Facilitate Normative Dialogue: Do not let stakeholders' experiences be the final word. Use facilitated dialogue to critically reflect on these experiences and co-develop justified normative positions [26].
Problem: Stakeholder Consensus is Elusive
- Symptoms: Dialogues reach an impasse because of conflicting values or perspectives among participants; inability to draw a coherent normative conclusion.
- Solution:
- Shift the Goal from Consensus to Learning: Frame the primary output of the dialogue as mutual moral learning and a deeper understanding of the problem, which can be valuable even without full consensus [26].
- Use Homogeneous Groups: Before bringing all stakeholders together, first facilitate dialogues within homogeneous groups (e.g., patients only, clinicians only) to build confidence and clarify internal perspectives [26].
- The Ethicist's Normative Contribution: As a facilitator, you can enrich the process by carefully introducing ethical concepts and theories to help participants navigate their disagreements and structure their reflections [26] [12].
The Scientist's Toolkit: Essential Research Reagents
| Item | Function in Dialogical Empirical Ethics |
|---|---|
| Structured Dialogue Protocol | A pre-defined format (e.g., from Responsive Evaluation) to guide discussions, ensuring they are productive and systematically capture all relevant experiences and normative reflections [26]. |
| Stakeholder Maps | A visual or descriptive tool identifying all relevant parties (patients, clinicians, policymakers) and their relationships, which is crucial for inclusive and representative sampling [26]. |
| Semi-Structured Interview Guides | A set of open-ended questions used to elicit detailed stories and perspectives from participants, providing the rich, qualitative empirical data for the dialogical process [26]. |
| Ethical Framework Primer | A simplified overview of key ethical principles (e.g., autonomy, beneficence) and theories, used by the facilitating ethicist to inform and enrich stakeholder discussions without imposing conclusions [12]. |
| Integration Methodology Handbook | A reference document detailing methods like Wide Reflective Equilibrium or Hermeneutic analysis, helping researchers navigate the back-and-forth between empirical data and normative reasoning [12]. |
Experimental Protocol: Implementing a Dialogical Ethics Study
Objective: To develop and implement normative guidelines for improving the practice concerning coercion and compulsion in psychiatry through stakeholder collaboration [26].
Step-by-Step Methodology:
Project Scoping and Stakeholder Mapping
- Identify all key stakeholder groups (e.g., patients with lived experience, psychiatrists, nurses, hospital administrators, family advocates).
- Define the specific ethical issue and the scope of the desired normative guidelines.
Empirical Data Elicitation
- Conduct in-depth, semi-structured interviews with individuals from each stakeholder group.
- Focus on collecting concrete, detailed narratives about their experiences with and perspectives on coercion and compulsion in psychiatric care.
Structured Dialogical Exchange
- Homogeneous Dialogues: Convene separate focus groups for each stakeholder type (e.g., a patient-only group). Present anonymized data and facilitate discussion to develop group-specific insights.
- Heterogeneous Dialogue: Bring representatives from all stakeholder groups together. Facilitate a structured conversation where experiences from the homogeneous dialogues are shared and debated.
Normative Analysis and Conclusion Drawing
- The facilitating ethicist guides the heterogeneous group in a reflective process to identify common values, resolve conflicts, and draft normative guidelines that are informed by the shared dialogue.
- This involves a continuous "back-and-forth" between the collected experiences (empirical data) and ethical principles (normative analysis) [12].
Implementation and Reflexivity
- Present the co-created guidelines back to the broader practice community for feedback.
- Plan for the implementation of the guidelines and establish methods for ongoing monitoring and reflexive evaluation of their impact and ethical soundness in practice.
Methodological Pathways for Empirical Bioethics
The following diagram illustrates the primary methodological approaches for integrating empirical data with normative analysis, as identified in recent research [12].
The Dialogical Empirical Ethics Workflow
This workflow outlines the key phases of a project using dialogical ethics, from initial problem identification to the implementation of co-created normative guidance [26].
Empirical bioethics faces a fundamental challenge: how to integrate descriptive empirical data ("what is") into normative ethical reasoning ("what ought to be") without committing logical fallacies. This dilemma, often referred to as Hume's Law or the is-ought problem, establishes that no set of purely descriptive statements can logically entail an evaluative statement without at least one evaluative premise [2]. Symbiotic empirical ethics offers a practical methodology that addresses this challenge by creating a reciprocal relationship between ethical theory and practice, where each informs and refines the other in an iterative process [27].
This technical support guide provides researchers, scientists, and drug development professionals with practical frameworks for implementing symbiotic empirical ethics within their work, enabling them to navigate the is-ought gap while developing ethically robust research practices and interventions.
Theoretical Foundations: Understanding the Is-Ought Problem
Key Concepts and Distinctions
The is-ought problem is frequently conflated with two other distinct concepts in bioethics literature. The table below clarifies these essential distinctions:
Table 1: Key Meta-ethical Concepts in Empirical Bioethics
| Concept | Definition | Primary Proponent | Relevance to Empirical Bioethics |
|---|---|---|---|
| Hume's Law (Is-Ought Problem) | No set of descriptive statements alone can entail an evaluative statement without at least one evaluative premise [2] | David Hume | Creates logical limitations for deriving norms directly from empirical data |
| Naturalistic Fallacy | The logical fallacy of defining "good" in terms of natural properties [2] | G.E. Moore | Represents a meta-ethical refutation of ethical naturalism |
| Fact-Value Distinction | The view that factual statements and value statements have different truth-aptness [2] | Various | Suggests science is value-free, though this is contested |
The "Ought-Is" Problem: Implementing Ethical Norms
A complementary challenge to the traditional is-ought problem is the "ought-is" problem: how to implement ethical rules or norms to ensure they fulfill their primary purpose once developed [7]. This implementation challenge requires an "implementation mindset" where ethicists consider whether norms can feasibly be enacted, as ethical statements that cannot be implemented may foster "guilt, cynicism, or despondency and inaction" [7].
The Symbiotic Empirical Ethics Methodology: A Step-by-Step Guide
Symbiotic empirical ethics is based on a naturalistic conception of ethical theory that sees practice as informing theory just as theory informs practice [27]. The methodology uses ethical theory both to explore empirical data and to draw normative conclusions through a structured process.
Table 2: The Five-Step Symbiotic Empirical Ethics Process
| Step | Process | Key Activities | Theoretical-Practice Relationship |
|---|---|---|---|
| 1 | Define Ethical Question & Select Normative Framework | Identify concrete ethical problem; Select appropriate ethical theory based on adequacy for issue and research design [28] | Theoretical foundation guides empirical inquiry |
| 2 | Collect Empirical Data | Qualitative/quantitative data gathering on real-world ethical challenges and stakeholder experiences [29] | Practice generates evidence about actual ethical phenomena |
| 3 | Analyze Data Through Theoretical Lens | Apply selected ethical framework to interpret empirical findings; Identify tensions between theory and practice [27] | Theory provides interpretive structure for understanding practice |
| 4 | Refine Ethical Theory | Modify theoretical framework based on empirical insights; Develop new normative concepts addressing practice gaps [27] | Practice reveals limitations in theory, driving theoretical development |
| 5 | Develop Practical Recommendations | Formulate specific, implementable ethical guidelines and interventions informed by refined theory [29] | Refined theory generates more practically adequate norms |
Workflow Diagram: Symbiotic Ethics Process
Troubleshooting Common Implementation Challenges
Frequently Encountered Problems and Solutions
Table 3: Troubleshooting Guide for Symbiotic Ethics Implementation
| Problem | Possible Causes | Data to Collect | Solution Approach |
|---|---|---|---|
| Difficulty integrating empirical findings with normative analysis | Conflation of Hume's Law with naturalistic fallacy; Underdeveloped ethical framework [2] | Document precise nature of disjunct between data and theory; Map argumentative structure of inferences | Explicitly articulate evaluative premises; Adopt "bridge postulate" that facts-values connection is possible [2] |
| Ethical recommendations are not implemented in practice | "Ought-is" gap: failure to consider implementation feasibility during norm development [7] | Stakeholder engagement data; Resource constraints; Organizational barriers | Apply implementation science principles during norm development; Develop "specific norms" rather than only "aspirational norms" [7] |
| Stakeholder resistance to ethical recommendations | Theory selection mismatch with practical context; Inadequate attention to relational dimensions [28] [29] | Qualitative data on stakeholder values and concerns; Analysis of relational networks in practice context | Select ethical theory based on adequacy for issue and research design; Foreground relational aspects of ethics [28] [29] |
| Uncertainty about which ethical theory to select | Pluralism of ethical theories; Lack of clear selection criteria [28] | Map specific requirements of research question; Identify theoretical commitments of stakeholders | Apply systematic criteria: adequacy for issue, suitability for research design, alignment with empirical approaches [28] |
Research Reagent Solutions: Essential Methodological Tools
Table 4: Essential Methodological Components for Symbiotic Ethics Research
| Methodological Component | Function | Examples from Literature |
|---|---|---|
| Qualitative Data Collection Methods | Gather rich, contextual data on ethical experiences and challenges | Interviews, focus groups with healthcare professionals on resetting services during pandemic [29] |
| Implementation Science Frameworks | Support enactment and sustainability of ethical interventions | Consolidated Framework for Implementation Research (CFIR) assessing intervention characteristics, settings [7] |
| Ethical Theory Selection Criteria | Provide systematic approach to choosing appropriate normative framework | Criteria of adequacy, suitability, and empirical alignment [28] |
| Translational Ethics Framework | Guide movement from abstract norms to concrete practices | Sisk et al.'s framework: Aspirational Norms → Specific Norms → Best Practices [7] |
| Mixed Judgment Analysis | Structure integration of normative and empirical propositions | Explicitly tracing normative and descriptive premises in ethical conclusions [28] |
Detailed Experimental Protocol: Implementing Symbiotic Ethics
Phase 1: Study Design and Theory Selection
- Define Concrete Ethical Problem: Formulate specific, practice-based ethical question rather than abstract theoretical problem
- Select Ethical Theory: Apply three criteria for theory selection [28]:
- Adequacy: Theory must appropriately address the specific ethical issue
- Suitability: Theory must align with research purposes and design
- Empirical Alignment: Consider interrelation between ethical theory and theoretical backgrounds of socio-empirical research
- Develop Data Collection Protocols: Design empirical methods that will generate data relevant to both theoretical refinement and practical application
Phase 2: Data Collection and Integration
- Gather Empirical Data: Collect qualitative and/or quantitative data on actual ethical practices, challenges, and stakeholder perspectives
- Initial Theoretical Analysis: Apply selected ethical framework as interpretive lens for preliminary data analysis
- Identify Theory-Practice Tensions: Document specific points where empirical findings challenge, extend, or refine existing theoretical framework
Example: The Reset Ethics project collected data through interviews and focus groups with healthcare professionals about ethical challenges in resetting maternity and paediatric services during COVID-19, finding that infection prevention measures created harmful barriers to relational care [29].
Phase 3: Theory Refinement and Recommendation Development
- Modify Ethical Theory: Adjust theoretical framework to better account for empirical findings
- Develop Specific Norms: Formulate concrete, implementable ethical recommendations rather than only aspirational norms
- Design Implementation Strategies: Create specific interventions, policies, or practices to enact ethical recommendations
Example: Based on their findings about the importance of relationships, the Reset Ethics project suggested explicitly acknowledging "the importance of the relationships within which the patient is held" in clinical ethics practice [29].
FAQs: Addressing Common Researcher Questions
Q1: How does symbiotic empirical ethics avoid violating Hume's Law against deriving 'ought' from 'is'?
A: Symbiotic ethics does not claim to directly derive normative conclusions from purely empirical data. Instead, it uses empirical findings to inform, test, and refine existing ethical theories that already contain normative content. The empirical data helps identify where theories need extension or revision, but always within a framework that includes evaluative premises [2] [27].
Q2: What types of empirical data are most useful in a symbiotic ethics approach?
A: Useful data includes qualitative research on stakeholder experiences and ethical challenges [29], implementation studies on existing ethical practices [30], and evaluative research on how ethical recommendations are translated into practice [30]. The key is collecting data that reveals both the practical ethical challenges and the factors affecting implementation of ethical norms.
Q3: How do I select an appropriate ethical theory for my empirical ethics research?
A: Theory selection should be based on three main criteria [28]:
- Adequacy: The theory must appropriately address your specific ethical issue
- Suitability: The theory must fit your research purposes and design
- Empirical Alignment: Consider how the theory relates to theoretical backgrounds of your socio-empirical research
Q4: How can symbiotic ethics address the "ought-is" problem of implementing ethical recommendations?
A: By integrating implementation science principles throughout the process, including during norm development [7]. This involves considering feasibility during the formulation of specific norms, engaging stakeholders early, and using implementation frameworks like the Consolidated Framework for Implementation Research (CFIR) to identify potential barriers and facilitators.
Q5: What is the role of relationships in symbiotic empirical ethics?
A: Relationships are crucial both as a subject of ethical analysis and as part of the methodology. Empirical research has shown that healthcare professionals experience relational interactions as ethically important dimensions of care [29]. Methodologically, attention to relationships helps bridge the theory-practice gap by recognizing that ethical decisions occur within networks of relationships.
{#conceptual-overview}
Bridging the Ethical Divide: From Theory to Practice
A significant challenge in empirical bioethics is the "is-ought" problem (Hume's Law), which questions how one can derive prescriptive "ought" statements from descriptive "is" statements about the world [1]. This creates a gap between developing ethical norms and actually implementing them in practice. Implementation science, a discipline dedicated to supporting the sustained enactment of interventions, provides a framework to bridge this gap, addressing what can be termed the "ought-is" problem: how to implement an ethical rule or norm to ensure it fulfills its purpose [7].
This technical support content guides researchers in applying implementation science strategies to translate ethical norms into measurable, real-world practices.
{chart}
Implementation Science Framework for Ethical Norms
{chart}
{table}
Key Implementation Science Frameworks
| Framework/Purpose | Core Components | Application in Ethical Translation |
|---|---|---|
| Consolidated Framework for Implementation Research (CFIR) [7] [31]: Understand barriers/facilitators | Five domains: intervention characteristics, outer/inner settings, individuals involved, implementation process [7] | Diagnosing context for ethical interventions; selecting implementation strategies |
| Process Models [31]: Guide planning and evaluation | Steps from pre-implementation through sustainment; often use mixed methods [31] | Structuring the translation of a specific norm into a sustained practice |
| Theories, Models, and Frameworks (TMFs) [31]: Inform data collection and analysis | Five types: process models, determinant frameworks, classic/implementation theories, evaluation frameworks [31] | Explaining causal mechanisms; guiding qualitative/quantitative analysis |
{table}
{faq}
Frequently Asked Questions: Implementation Science & Ethics
What is the "ought-is" problem in bioethics? While the traditional "is-ought" problem questions deriving moral conclusions from factual statements, the "ought-is" problem is the challenge of implementing an established ethical norm or rule in real-world practice to ensure it leads to ethical actions [7]. It focuses on the translation from principle to action.
Why is implementation science relevant to ethical research? Evidence-based medicine takes an average of 17 years to be incorporated into routine practice [7] [32]. Implementation science provides a structured, multidisciplinary approach to close this gap for ethical practices, ensuring that proven interventions are sustainably and effectively enacted [7].
How can I select an implementation science framework for my ethics project? Selection depends on your research question. Use determinant frameworks like CFIR to identify contextual barriers. Use process models to guide the sequence of activities from planning to sustainment. Use evaluation frameworks to measure the success of your implementation effort [31]. The framework should help you understand, plan, or evaluate the process of enacting your specific ethical norm.
What are common barriers to implementing ethical norms? Barriers can exist at multiple levels [7] [32]:
- Intervention Characteristics: The ethical norm itself may be too complex or costly to implement.
- Inner Setting: An organization's culture, resources, or workflows may resist the new ethical practice.
- Outer Setting: External policies, regulations, or patient needs may create friction.
- Individuals Involved: Lack of knowledge, self-efficacy, or trust among practitioners or patients.
- Process: Poor planning, engagement, or execution of the implementation.
Can implementation science be applied before a drug or intervention is approved? Yes. While historically focused post-approval, there is a growing push to integrate implementation science earlier in the development life cycle (e.g., during clinical trial Phases I-III) to proactively address barriers to future adoption, equity, and sustainability [32] [33]. {faq}
{troubleshooting}
Troubleshooting Guide: Solving Common Implementation Problems
Problem: Slow or Incomplete Uptake of an Ethical Guideline This guide uses a top-down and divide-and-conquer approach to diagnose issues. [34] [35]
Q: My team has developed an ethical guideline (e.g., a new informed consent process), but it's not being consistently adopted in our clinical trials. What should I do?
1. Identify the Symptom and Gather Data
- Symptom: Low adoption rates, inconsistent application, or stakeholder complaints.
- Action: Collect quantitative data (e.g., adoption metrics) and qualitative feedback from stakeholders (researchers, clinicians, patients) to understand the nature of the resistance [34].
2. Diagnose the Root Cause Using a Structured Framework Apply the CFIR domains to categorize barriers [7] [31]:
- Intervention Characteristics: Is the new consent process perceived as too complex or time-consuming compared to the old one?
- Inner Setting: Do clinic workflows or IT systems not support the new process? Is there a lack of leadership buy-in?
- Individuals Involved: Are research staff adequately trained and do they believe in the value of the new process?
- Outer Setting: Are there regulatory or institutional review board (IRB) concerns we haven't addressed?
- Process of Implementation: Was the rollout rushed, or were key stakeholders not engaged in the planning?
3. Establish Realistic Solutions Based on the root cause, prioritize solutions [34] [36]:
- If complexity is the issue: Simplify the intervention. Use plain language and graphics in consent forms [7].
- If workflow is the issue: Collaborate with frontline staff to co-design a process that integrates into their routine.
- If knowledge is the issue: Develop and deliver targeted training sessions and quick-reference guides.
- If engagement is the issue: Create a stakeholder engagement plan that includes patients, providers, and leadership early in the process [32].
4. Implement, Document, and Test the Solution
- Action: Pilot the refined ethical intervention with a small, supportive team.
- Documentation: Create a clear, step-by-step guide with visual aids for the new process [35] [36].
- Testing: Have a colleague who was not involved in the development follow the guide to ensure it is clear and effective [36].
5. Evaluate and Refine
- Action: Measure the key outcomes again after the pilot (e.g., adoption rates, user satisfaction).
- Refinement: Use the data to make further adjustments before scaling the implementation more broadly [33].
{chart}
Troubleshooting Workflow for Ethical Implementation
{chart}
{toolkit}
The Scientist's Toolkit: Key Reagents for Implementation Research
{table}
| Research Reagent / Tool | Function in Implementation Science |
|---|---|
| Theories, Models, and Frameworks (TMFs) [31] | Provide conceptual maps to understand, plan, and evaluate the implementation process. |
| Stakeholder Engagement Plans [7] [32] | Ensure the perspectives of patients, providers, and health systems are incorporated to co-develop feasible solutions. |
| Mixed-Methods Approaches [33] [31] | Combine quantitative (e.g., surveys, metrics) and qualitative (e.g., interviews, focus groups) data to fully understand implementation context and outcomes. |
| Logic Models [33] | Visually map out the hypothesized relationships between inputs, activities, outputs, and outcomes of an implementation effort. |
| Implementation Strategy Bundles [32] [33] | A coordinated set of actions (e.g., training, audit/feedback, workflow redesign) designed to overcome specific barriers to implementation. |
| Hybrid Trial Designs [32] | Study designs that simultaneously assess both the clinical effectiveness of an intervention and the success of its implementation in a real-world context. |
{table}
The COVID-19 pandemic created unprecedented ethical challenges for healthcare systems worldwide, particularly in balancing infection control with the delivery of compassionate, relational care. This case study explores the application of symbiotic empirical ethics—a methodology that integrates empirical research with normative ethical analysis—to address these challenges within maternity and paediatric services during the pandemic. The core problem illuminated by this crisis was the collision between established clinical ethics focused on individual patient relationships and public health ethics prioritizing community safety [37] [29]. This case study provides researchers and healthcare professionals with a practical framework for navigating such ethical tensions through a methodological approach that directly addresses the is-ought gap in bioethics research—the philosophical challenge of deriving normative conclusions ("ought") from empirical data ("is") [2].
Theoretical Framework & Methodology
Understanding Symbiotic Empirical Ethics
Symbiotic empirical ethics (SEE) is a specific methodological approach within empirical bioethics that uses a five-step process to refine and develop ethical theory based on a naturalist account of ethics where practice and theory are symbiotically related [37] [29]. This methodology explicitly addresses the is-ought problem by:
- Rejecting non-cognitivist interpretations of Hume's Law that would completely forbid deriving normative statements from empirical data [2]
- Embracing ethical cognitivism—the position that ethical statements are truth-apt and that knowledge is possible in ethics [2]
- Creating a bridge postulate that acknowledges the necessity of connecting factual observations with value judgments [2]
Table: Core Components of Symbiotic Empirical Ethics
| Component | Description | Role in Addressing Is-Ought Gap |
|---|---|---|
| Ethical Cognitivism | View that ethical statements can be true or false | Provides philosophical foundation for deriving normative insights from data |
| Bridge Postulate | Acknowledgement that facts and values must be connected | Creates methodological pathway from empirical observations to ethical recommendations |
| Five-Step Process | Systematic approach to integrating data and theory | Offers replicable structure for moving from "is" to "ought" |
The Reset Ethics Study Design
The NHS Reset Ethics project employed SEE methodology to investigate the ethical challenges of resetting England's NHS maternity and paediatric services during the COVID-19 pandemic [37] [29]. The study design included:
- Data Collection: Interviews and focus group discussions with healthcare professionals and members of the public between November 2020 and July 2021 [37]
- Qualitative Analysis: Thematic analysis of healthcare experiences using Frith's symbiotic empirical ethics methodology [29]
- Normative Development: Working from empirical findings toward normative suggestions for clinical ethics practice [37]
The methodology flowchart below illustrates the systematic process of moving from empirical data to ethical recommendations:
Troubleshooting Guide: Common Methodological Challenges
FAQ: Addressing Key Research Challenges
Table: Frequently Asked Questions on Symbiotic Ethics Methodology
| Question | Challenge Description | Recommended Solution |
|---|---|---|
| How do we validate normative claims derived from qualitative data? | Risk of drawing unsubstantiated ethical conclusions from limited empirical findings | Employ methodological triangulation: combine interviews with document analysis and expert consultation [38] |
| What if participants' experiences suggest contradictory ethical norms? | Empirical data may reveal conflicting perspectives on what constitutes ethical practice | Use constant comparison method to identify patterns while acknowledging ethical complexity and ambiguity [38] |
| How can we ensure our ethical recommendations are implementable? | Risk of developing theoretically sound but practically unworkable normative suggestions | Apply implementation science principles during normative development to assess feasibility [7] |
| How do we maintain methodological rigor when working across disciplines? | Tension between empirical social science and philosophical ethics approaches | Establish clear quality criteria from both traditions: credibility + philosophical coherence [37] [38] |
Implementation Framework: From Ought to Is
A critical challenge in empirical bioethics is ensuring that normative recommendations can be successfully implemented—what has been termed the "ought-is problem" [7]. The following framework adapts implementation science principles to ethical practice:
Key Findings: Relational Ethics in Pandemic Care
The Reset Ethics project revealed significant tensions between infection control measures and relational aspects of care. The table below summarizes key empirical findings from the study:
Table: Impact of IPC Measures on Relational Care (Reset Ethics Study)
| IPC Measure | Impact on Care Delivery | Ethical Tension Identified | Proposed Ethical Solution |
|---|---|---|---|
| Visitor Restrictions | Limited family presence; increased patient isolation; compromised support systems | Autonomy vs. community safety | Allow designated support persons with safety protocols |
| Personal Protective Equipment (PPE) | Created communication barriers; reduced non-verbal cues; impeded relationship-building | Beneficence vs. healthcare worker protection | Transparency about PPE necessity; supplemented communication strategies |
| Virtual Consultations | Increased access but decreased personal connection; technological barriers for some | Justice vs. efficiency | Hybrid models; technology support for vulnerable patients |
| Workflow Reorganization | Disrupted established care relationships; team fragmentation | Fidelity vs. operational necessity | Consistent team assignments where possible; relationship continuity planning |
Conceptual Model: Relational Ethics Framework
Based on the study findings, the researchers developed a conceptual framework for relational ethics in healthcare. This framework re-conceptualizes the patient not as an isolated individual but as embedded within networks of relationships that are ethically significant [37] [29]:
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Methodological Resources for Symbiotic Empirical Ethics Research
| Research Tool | Function | Application in Reset Study |
|---|---|---|
| Semi-Structured Interview Protocols | Elicit rich qualitative data on ethical experiences | Adapted to explore specific tensions between IPC measures and relational care [38] |
| Constant Comparison Method | Analyze qualitative data through systematic coding and categorization | Used to identify recurring themes in healthcare professionals' ethical challenges [38] |
| Frith's Symbiotic Ethics Methodology | Five-step approach to integrating empirical and normative work | Provided structured process for moving from data to ethical recommendations [37] [29] |
| Implementation Science Frameworks (CFIR) | Assess contextual factors affecting implementation success | Informed development of feasible ethical recommendations [7] |
| Triangulation Procedures | Enhance validity through multiple data sources/methods | Combined healthcare professional and patient perspectives [38] |
Experimental Protocols & Methodologies
Protocol: Applying Symbiotic Empirical Ethics
For researchers seeking to replicate or adapt this methodology, the following detailed protocol outlines the key steps:
Objective: To investigate ethical challenges in healthcare settings and develop normative recommendations through symbiotic empirical ethics methodology.
Materials:
- Interview/focus group guides
- Audio recording equipment
- Qualitative data analysis software
- Ethical framework documents
Procedure:
Study Design & Ethical Approval
- Define research questions focusing on ethical challenges in specific healthcare contexts
- Obtain institutional ethical approval
- Develop recruitment strategies for healthcare professionals and patients [38]
Data Collection
Qualitative Analysis
- Apply constant comparison method to transcribed data
- Develop initial codes and categories through independent review by multiple researchers
- Refine categories through iterative discussion and comparison
- Identify recurring themes and ethical tensions [38]
Normative Analysis
Validation & Refinement
- Conduct methodological triangulation
- Present preliminary findings to stakeholders for feedback
- Refine normative recommendations based on feedback [38]
Quality Control:
- Maintain detailed audit trail of analytical decisions
- Document researcher positions and potential biases
- Ensure philosophical coherence of normative claims [37] [38]
Workflow: Integrated Empirical-Normative Analysis
The following workflow diagram illustrates the iterative process of moving between empirical data and normative analysis:
This case study demonstrates how symbiotic empirical ethics provides a robust methodological approach for addressing the is-ought gap in bioethics research. By systematically integrating empirical findings from healthcare professionals' pandemic experiences with normative ethical analysis, the Reset Ethics project developed feasible recommendations for preserving relational aspects of care while maintaining necessary infection control measures [37] [29].
The methodological framework presented here offers researchers a structured approach to:
- Collect rich qualitative data on ethical challenges in healthcare
- Analyze this data through both empirical and philosophical lenses
- Develop normative recommendations that are both ethically sound and practically implementable
- Address the is-ought problem through transparent methodological bridging
For future research, this case study highlights the importance of maintaining focus on relational dimensions of healthcare ethics, particularly in crisis situations where there is pressure to prioritize efficiency over human connection. The tools, protocols, and frameworks provided here can be adapted to investigate ethical challenges across diverse healthcare contexts and contribute to developing more relationally-attuned clinical ethics practices.
Navigating Methodological Uncertainty: Solutions for Common Integration Challenges
A persistent challenge in empirical bioethics is the vagueness surrounding integration methods—the process of combining normative analysis with empirical data. While this flexibility can be advantageous, it often obscures a lack of understanding of the theoretical-methodological underpinnings, creating uncertainty about how to validly move from empirical findings ("is") to normative recommendations ("ought") [39]. This technical support center provides practical guidance for addressing this vagueness, offering concrete methodologies to strengthen the rigor of your integrative empirical bioethics research.
Troubleshooting Guide: Common Integration Challenges
Problem: The "Leaky Pipeline" - Norms That Fail to Translate to Practice
- Symptoms: Ethical recommendations are published but show minimal uptake in clinical or research practice; interventions fail to sustain beyond initial implementation.
- Diagnosis: This "ought-is" problem occurs when normative claims are developed without considering implementation feasibility from the outset [7].
- Solution: Adopt an implementation mindset during normative development. Utilize the Consolidated Framework for Implementation Research (CFIR) to identify potential barriers across five domains: intervention characteristics, outer setting, inner setting, characteristics of individuals, and implementation process [7].
- Symptoms: Uncertainty about whether empirical data validly supports ethical recommendations; concerns about committing the naturalistic fallacy.
- Diagnosis: This reflects the philosophical challenge that no set of descriptive statements alone entails an evaluative statement without at least one evaluative premise [2].
- Solution: Implement systematic integration frameworks from the outset. Explicitly document and justify your "bridge premises" that connect empirical findings to normative claims. Utilize established methodologies like reflective equilibrium or dialogical methods that create structured processes for moving between empirical data and normative reasoning [39].
Problem: Unclear Methodological Path - Vagueness in Integration Approach
- Symptoms: Difficulty articulating exactly how empirical and normative components relate in your research; methodological descriptions lack specificity.
- Diagnosis: Researchers report "an air of uncertainty and overall vagueness" about integration methods, even when using familiar approaches like reflective equilibrium [39].
- Solution: Pre-specify and document your integration protocol. The table below summarizes acceptable objectives for empirical research in bioethics based on researcher consensus:
Table: Acceptable Objectives for Empirical Research in Bioethics [11]
| Objective | Acceptance Level | Key Characteristics |
|---|---|---|
| Understanding Context | High | Exploring the real-world circumstances surrounding a bioethical issue |
| Identifying Ethical Issues | High | Detecting ethical concerns as they manifest in practice |
| Evaluating Interventions | Medium | Assessing how ethical recommendations perform in reality |
| Informing Normative Recommendations | Medium | Using empirical data to suggest changes to specific ethical norms |
| Developing/Justifying Moral Principles | Low | Using empirical data to establish or validate foundational moral principles |
Problem: Disconnected Collaboration - Insufficient Interdisciplinary Dialogue
- Symptoms: Tension between empirical and normative researchers; failure to appreciate different methodological approaches; missed opportunities for genuine integration.
- Diagnosis: Researchers from different disciplines may work in parallel rather than through truly integrated collaboration [39].
- Solution: Implement structured dialogical methods that facilitate genuine interdisciplinary exchange. Create formal processes for empirical and normative researchers to collaboratively analyze data and develop ethical insights, treating integration as inherent to the research design rather than a final step [39].
Frequently Asked Questions
Q1: Is Hume's Law a valid argument against empirical bioethics?
No. While Hume's Law (the "is-ought problem") is often raised as a concern, it does not invalidate empirical bioethics when properly understood [2]. The version of Hume's Law that poses problems stems from ethical non-cognitivism (the view that ethical statements aren't truth-apt), but most bioethics operates within ethical cognitivism (the view that ethical knowledge is possible). The key is recognizing that establishing a "bridge" between facts and values is both possible and foundational to bioethics [2].
Q2: What are the most and least acceptable objectives for empirical bioethics research?
Based on qualitative exploration of researchers' views [11]:
- Most accepted: Understanding the context of bioethical issues and identifying ethical issues in practice (unanimous agreement).
- Most contested: Striving to draw normative recommendations and developing/justifying moral principles. The pattern shows researchers favor objectives that produce empirical results over those making strong normative claims.
Q3: How can we implement ethical norms more effectively in healthcare settings?
Apply principles from implementation science to ethics. Develop specific (not just aspirational) norms, create targeted interventions to enact them, measure outcomes, identify best practices, and disseminate widely. Consider feasibility during normative development—if a norm cannot be implemented, it fails ethics' practical purpose [7].
Q4: What methodologies help overcome vagueness in integration?
Three approaches show particular promise [39]:
- Back-and-forth methods: Using reflective equilibrium to continuously adjust between empirical data and normative principles.
- Dialogical methods: Structured collaboration between empirical and normative researchers throughout the research process.
- Inherent integration approaches: Designing research where empirical and normative elements are intertwined from the start.
Experimental Protocols for Integration Methods
Protocol 1: Structured Reflective Equilibrium for Data-Norm Integration
Title: Reflective Equilibrium Process
Purpose: To systematically integrate empirical findings with normative reasoning through an iterative adjustment process.
Materials Needed:
- Empirical dataset (qualitative or quantitative)
- Documentation of initial normative positions
- Relevant ethical frameworks/theories
- Analysis tools appropriate to data type
Procedure:
- Document Initial Positions: Clearly articulate starting normative judgments about the ethical issue.
- Collect Empirical Data: Gather relevant empirical evidence about the issue in practice.
- Identify Background Theories: Specify the ethical frameworks informing the analysis.
- Conduct Iterative Analysis: Systematically adjust between elements to achieve coherence:
- Test normative judgments against empirical findings
- Modify judgments that conflict with robust data
- Reinterpret data through different theoretical lenses
- Continue until stable equilibrium achieved
- Document the Process: Record all adjustments and justifications for transparency.
Validation: The process is valid when all elements cohere without significant tension, and adjustments are rationally justified.
Protocol 2: CFIR-Informed Norm Implementation Framework
Title: CFIR Implementation Pathway
Purpose: To develop and implement ethical norms with explicit consideration of implementation barriers and facilitators.
Materials Needed:
- Consolidated Framework for Implementation Research (CFIR) guide
- Stakeholder mapping tools
- Implementation feasibility assessment checklist
- Outcome measurement instruments
Procedure:
- CFIR Barrier Assessment: Prior to finalizing norms, systematically assess potential implementation barriers across all five CFIR domains.
- Stakeholder Engagement: Identify and engage key stakeholders who will be affected by or responsible for implementing the norm.
- Norm Specification: Develop specific, actionable norms informed by the barrier assessment and stakeholder input.
- Intervention Design: Create targeted interventions to enact the specific norms, considering:
- Educational components
- System-level changes
- Measurement approaches
- Pilot Testing: Implement interventions in controlled settings to assess feasibility and effectiveness.
- Outcome Measurement: Track predefined outcomes to determine intervention success.
- Best Practice Identification: Refine approaches based on outcome data and disseminate successful models.
Validation: Successful implementation is demonstrated through sustained enactment of the norm and achievement of predefined ethical outcomes.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Methodological Resources for Empirical Bioethics Integration
| Research Reagent | Function | Application Context |
|---|---|---|
| Reflective Equilibrium Protocol | Creates structured process for iterative adjustment between data and norms | When seeking to justify normative positions in light of empirical evidence |
| CFIR Framework | Identifies implementation barriers during normative development | When creating ethical guidelines intended for real-world application |
| Dialogical Integration Methods | Facilitates genuine collaboration between empirical and normative experts | When conducting interdisciplinary research teams |
| Stakeholder Engagement Protocols | Ensures relevant perspectives inform normative development | When addressing ethical issues affecting multiple stakeholder groups |
| Implementation Science Principles | Supports translation of ethical norms into sustained practice | When moving from theoretical ethics to practical application |
| Bridge Premise Documentation | Explicitly states the normative principles connecting facts to values | When defending against charges of committing the naturalistic fallacy |
The Consolidated Framework for Implementation Research (CFIR) represents a comprehensive meta-theoretical framework developed to guide systematic assessment of multi-level implementation contexts by identifying barriers and facilitators that influence implementation success [40] [41]. Originally published in 2009 and updated in 2022 based on extensive user feedback, this framework synthesizes constructs from numerous implementation theories and models across multiple disciplines [40] [41]. For researchers in empirical bioethics addressing the is-ought gap—the challenge of bridging descriptive empirical findings with normative ethical recommendations—CFIR provides a structured approach to contextualize ethical interventions within complex healthcare systems. The framework helps bioethicists understand why certain ethical guidelines succeed or fail in practice and identifies leverage points for improving the implementation of ethically-informed interventions [41].
CFIR serves as a determinant framework that aims to predict or explain barriers and facilitators (determinants) to implementation effectiveness (the outcome) [42]. Its structured approach to identifying multi-level contextual factors makes it particularly valuable for bioethics researchers seeking to translate normative ethical frameworks into practical, real-world applications. By systematically accounting for the complex interplay between interventions, individuals, internal settings, external contexts, and implementation processes, CFIR provides a methodology to navigate the is-ought divide in empirical bioethics research [42].
CFIR Domain Structure and Framework Components
The updated CFIR comprises 48 constructs and 19 subconstructs organized across five major domains that collectively provide a comprehensive mapping of implementation determinants [42]. These domains form an interconnected ecosystem of factors that influence how successfully an innovation or intervention is implemented within a given context.
Table 1: CFIR Domains and Core Components
| Domain | Description | Key Constructs |
|---|---|---|
| Innovation Domain | Characteristics of the intervention being implemented | Evidence strength & quality, Innovation-design, Adaptability, Cost |
| Outer Setting | The external context surrounding the implementing organization | Patient needs & resources, External policies & incentives, Peer pressure |
| Inner Setting | The internal context of the implementing organization | Culture, Implementation climate, Readiness for implementation |
| Individuals: Roles & Characteristics | Attributes of individuals involved in implementation | Knowledge & beliefs, Self-efficacy, Individual stage of change |
| Implementation Process | Activities and strategies used to implement the innovation | Planning, Engaging, Executing, Reflecting & evaluating |
The framework's comprehensive structure enables bioethics researchers to systematically investigate why ethically-sound interventions may fail in practice and how implementation can be improved. For example, when implementing a new ethical protocol for informed consent in clinical trials, researchers can use CFIR to identify potential barriers across all five domains—from the design of the consent process itself (Innovation) to clinician attitudes (Individuals), organizational resources (Inner Setting), regulatory requirements (Outer Setting), and rollout strategies (Process) [43] [42].
Figure 1: CFIR Domain Relationships and Interactions
Technical Support Center: CFIR Troubleshooting Guides
Frequently Asked Questions (FAQs)
FAQ 1: How do I determine if CFIR is appropriate for my bioethics research project?
CFIR is particularly well-suited for projects where understanding contextual determinants is essential for explaining implementation success or failure [42]. If your bioethics research involves implementing an ethical intervention, guideline, or protocol and you need to understand the factors affecting its adoption, CFIR provides a comprehensive framework. The framework is most valuable when you have access to stakeholders who can provide insights across multiple domains and when your research timeline allows for systematic data collection and analysis across different contextual levels [42].
FAQ 2: What are the most common challenges when applying CFIR and how can I address them?
The complexity and comprehensiveness of CFIR, while beneficial for thorough analysis, can present challenges for researchers [41]. Common issues include framework complexity, resource-intensive data collection, and difficulties in defining domain boundaries specific to each project [41] [42]. Based on user feedback, 58% of experienced CFIR users felt the framework was more complicated than necessary, while only 16% felt it was easy to use for non-researchers [41]. To address these challenges, researchers have developed pragmatic adaptations, including: (1) focusing on a subset of constructs most relevant to the specific research context; (2) clearly defining domain boundaries at the outset of the project; and (3) using rapid analysis techniques while maintaining methodological rigor [44] [42].
FAQ 3: How can I adapt CFIR for community-based bioethics interventions?
When applying CFIR to community-based settings, particularly in bioethics research involving vulnerable populations, adaptations may be necessary to better capture relevant contextual factors [45]. Successful adaptations documented in implementation studies include: promoting "patient needs and resources" to a more prominent position within the framework; modifying construct definitions to better fit community contexts; and adding domains specific to community partnerships [44] [45]. For example, a study in Burkina Faso adapting CFIR for a community tuberculosis program added "characteristics of associations involved" as a new domain to account for organizational capacity of community partners, and included a "support system" domain to capture training and technical assistance structures [45].
FAQ 4: How do I use CFIR to select implementation strategies for ethics interventions?
CFIR serves as a diagnostic tool to identify key barriers and facilitators that then inform the selection of implementation strategies [42]. The process involves: (1) systematically assessing determinants across all five CFIR domains; (2) prioritizing determinants that are both important and changeable; (3) mapping these prioritized determinants to implementation strategies using established matching tools; and (4) designing strategies that address multiple determinants simultaneously [42]. This approach ensures that implementation strategies are specifically tailored to address the contextual barriers identified through CFIR analysis.
Troubleshooting Common CFIR Application Issues
Table 2: CFIR Application Challenges and Solutions
| Challenge | Symptoms | Recommended Solutions | Bioethics Application Example |
|---|---|---|---|
| Framework Complexity | Difficulty applying all constructs; data overload; overwhelmed researchers | Select 5-8 key constructs a priori; use CFIR coding guide; employ matrix analysis for focused examination [44] [42] | When implementing ethics consultation services, focus on: Innovation Adaptability, Patient Needs, Organizational Culture, Knowledge & Beliefs, and Engaging |
| Retrospective vs Prospective Application | Confusion about timing; uncertain data collection points | Use prospectively to predict barriers; use retrospectively to explain outcomes; mixed approaches acceptable [42] [46] | Apply prospectively when designing new informed consent protocols; retrospectively when analyzing failed ethics committee initiatives |
| Defining Domain Boundaries | Overlap between domains; difficulty attributing determinants | Clearly define innovation scope; distinguish between inner/outer setting; separate innovation from implementation process [42] | Clearly delineate between the ethical intervention (e.g., advance care planning tool) and implementation strategies (training, workflow integration) |
| Resource-Intensive Data Collection | Limited time; budget constraints; stakeholder fatigue | Use rapid ethnography; leverage existing documents; employ targeted rather than comprehensive data collection [44] | Use existing ethics committee minutes, consultation records, and policy documents as data sources before conducting new interviews |
Methodological Protocols for CFIR Applications
Step-by-Step CFIR Implementation Guide
The CFIR Leadership Team has established a structured five-step approach for applying the framework in implementation research [42]. This methodology provides bioethics researchers with a systematic process for investigating the is-ought gap in empirical ethics research.
Step 1: Study Design
- Define research questions and implementation outcomes
- Determine CFIR domains and construct boundaries specific to the project
- Identify whether the application is prospective (predicting outcomes) or retrospective (explaining outcomes) [42]
- For bioethics applications, clearly define the ethical innovation or intervention and distinguish it from implementation strategies
Step 2: Data Collection
- Determine data collection approach (qualitative, quantitative, or mixed methods)
- Develop data collection instruments guided by CFIR constructs
- Implement sampling strategy that captures multiple perspectives across relevant stakeholder groups [42]
- In bioethics research, ensure representation of diverse stakeholder views, including patients, clinicians, ethics committee members, and administrators
Step 3: Data Analysis
- Code data using CFIR constructs as a coding framework
- Analyze patterns across cases or settings
- Identify prominent determinants and their interactions [42]
- For bioethics applications, pay particular attention to value conflicts and normative considerations that emerge as barriers or facilitators
Step 4: Data Interpretation
- Interpret findings in relation to implementation outcomes
- Identify "difference-maker" determinants that distinguish between success and failure
- Develop explanatory models about how determinants interact to influence outcomes [42]
- In bioethics research, connect these practical determinants to theoretical ethical frameworks
Step 5: Knowledge Dissemination
- Report findings using CFIR-informed terminology and structure
- Share results with stakeholders to inform future implementation efforts
- Contribute to refinement of CFIR through critique and feedback [42]
Figure 2: CFIR Application Methodology Workflow
Data Collection and Analysis Protocols
Effective application of CFIR requires systematic approaches to data collection and analysis. The framework can guide both qualitative and quantitative methods, though qualitative approaches are more commonly used for in-depth determinant identification [42].
Qualitative Data Collection Protocol:
- Conduct semi-structured interviews using CFIR-informed interview guides
- Include questions that probe each relevant CFIR construct
- Ensure representation across different stakeholder groups and organizational levels
- Supplement interviews with document review and observation where possible [42]
- For bioethics applications, include questions that specifically explore ethical dimensions and value considerations
Analysis Protocol:
- Use deductive coding based on CFIR constructs while remaining open to emergent themes
- Employ team-based coding with regular consensus meetings to enhance reliability
- Utilize qualitative data analysis software to manage and organize coded data
- Assess the valence (barrier/facilitator) and strength of each determinant [42]
- For comparative analysis, create determinant matrices across cases or sites
Table 3: CFIR Data Collection Methods and Applications
| Method | Description | CFIR Application | Strength for Bioethics Research |
|---|---|---|---|
| Semi-structured Interviews | Guided conversations using CFIR-informed questions | Elicit detailed perspectives on implementation determinants | Captures nuanced ethical reasoning and value conflicts |
| Focus Groups | Structured group discussions with stakeholders | Identify shared and contrasting perceptions across groups | Reveals collective ethical norms and organizational culture |
| Document Review | Analysis of existing documents (policies, minutes, reports) | Provides contextual understanding and historical perspective | Identifies formal ethical frameworks and institutional values |
| Observation | Systematic observation of implementation contexts | Reveals actual practices versus stated procedures | Uncovers practical ethics versus theoretical frameworks |
| Surveys with Open-ended Questions | Structured instruments with qualitative components | Broad data collection with some qualitative depth | Efficiently captures diverse stakeholder perspectives |
Implementation researchers have developed various tools and resources to support effective application of CFIR. These "research reagents" provide practical support for studying the is-ought gap in bioethics implementation.
Table 4: Essential CFIR Research Tools and Resources
| Tool/Resource | Function | Application in Bioethics Research | Source/Availability |
|---|---|---|---|
| CFIR Construct Coding Guide | Provides definitions and examples for consistent coding | Ensures systematic analysis of ethical implementation barriers | CFIR Technical Assistance Website [40] |
| CFIR Interview Guide Templates | Standardized questions aligned with CFIR constructs | Facilitates comprehensive data collection on ethics implementation | Published implementation studies [43] [45] |
| Inner Setting Memo Template | Structured format for documenting organizational context | Captures institutional ethics infrastructure and climate | CFIR User Guide [42] |
| Construct Rating Guidelines | Criteria for assessing strength and valence of determinants | Enables prioritization of key barriers to ethical implementation | Adaptation of existing implementation tools [42] |
| CFIR Implementation Research Worksheet | Comprehensive planning document for CFIR studies | Guides design of ethics implementation research projects | CFIR User Guide [42] |
Case Application: CFIR in Bioethics Research
The practical application of CFIR in bioethics research is illustrated through real-world examples that demonstrate how the framework helps bridge the is-ought gap by systematically identifying implementation determinants.
Case Example 1: Home Rehabilitation Care for Older Adults A study applying CFIR to home-based rehabilitation care for older adults with disabilities identified 29 implementation determinants, including 16 barriers and 13 facilitators [43]. These factors aligned with 15 of the 26 CFIR constructs across all domains. More barriers were identified in the Characteristics of Individuals, Intervention Characteristics, and Outer Setting domains, while fewer barriers were identified in the Inner Setting [43]. This systematic identification of determinants provides crucial insights for implementing ethically-sound care models that respect elderly patients' autonomy while ensuring safety and quality.
Case Example 2: Community Tuberculosis Program in Burkina Faso Research on TB program implementation adapted CFIR to community settings by modifying constructs to better fit the context [45]. Researchers added "characteristics of associations involved" as a new domain and included a "support system" domain to capture training and technical assistance structures [45]. This adaptation demonstrates CFIR's flexibility for global health ethics applications, where resource constraints and cultural factors create unique implementation challenges for ethical care delivery.
Case Example 3: Patient-Centered Care Transformation A study of primary care transformation made three key adaptations to CFIR: (1) promoted "patient needs and resources" to its own domain; (2) divided the inner setting domain into three hierarchical layers; and (3) tailored construct definitions to fit patient-centered care contexts [44]. These adaptations highlight how CFIR can be modified to address specific ethical imperatives such as patient-centeredness and autonomy in healthcare delivery.
Through these and similar applications, CFIR provides bioethics researchers with a structured methodology for investigating the complex interplay between ethical ideals and practical implementation challenges, ultimately helping to bridge the is-ought gap in empirical bioethics research.
Empirical bioethics is a hybrid field that integrates descriptive, empirical research with normative, philosophical analysis to address practical problems in medicine and healthcare. This interdisciplinary approach seeks to ground ethical guidance in the realities of clinical practice and stakeholder experiences. However, this integration raises a fundamental philosophical challenge: the is-ought problem [1]. First articulated by David Hume, this problem highlights the logical difficulty of deriving prescriptive "ought" statements from purely descriptive "is" statements of fact.
This technical support center addresses the methodological challenges that emerge from navigating this divide. Researchers in empirical bioethics must balance ambitious normative goals with methodological feasibility while maintaining philosophical rigor. The following sections provide practical guidance, troubleshooting, and frameworks for designing and implementing robust empirical bioethics research that respects both empirical and normative demands.
Conceptual Framework: Understanding the Implementation Pathway
The Is-Ought Problem in Bioethics Research
The is-ought problem presents a significant challenge for empirical bioethics research [1]. It arises when researchers attempt to make claims about what ought to be based solely on statements about what is. Hume observed that ethical conclusions cannot be logically inferred from purely descriptive factual statements alone [1]. This creates a fundamental gap between empirical observations (what we discover about practices, attitudes, or experiences) and normative recommendations (what we should do ethically).
From Ought to Is: An Implementation Science Framework
Moving from establishing ethical norms to implementing them in practice presents a parallel challenge—the "ought-is problem" [7]. This refers to the difficulty of translating ethical rules or norms into actual changes in practice to ensure they fulfill their purpose. A proposed framework incorporates implementation science into ethics to guide this translation process [7].
Framework for Implementing Ethical Norms in Practice
Troubleshooting Guide: Common Methodological Challenges
Systematic Review Limitations
Problem: Attempts to conduct systematic reviews of ethical arguments in bioethics are often fundamentally misguided [47]. Bioethical arguments are evaluative rather than quantitative, making standard notions of quality assessment and bias inapplicable.
Solution: Consider alternative review methodologies:
- Focused literature reviews with transparent inclusion criteria
- Concept analysis approaches that acknowledge the argumentative nature of classification
- Interpretive review methods from social sciences rather than aggregative systematic review models [47]
Qualitative Data Collection Issues
Problem: Interviews may produce superficial data that lacks contextual depth or reproduces dominant cultural narratives without critical examination [48].
Solution: Adopt narrative approaches to interviewing:
- Use open-ended questioning that allows participants to construct narratives
- Attend to narrative construction occurring at personal, interpersonal, and cultural levels
- Analyze the form and structure of stories in addition to their content [48]
- Be transparent about how interviewer background and positionality shape data collection
Normative Recommendation Challenges
Problem: Researchers encounter difficulties when moving from empirical findings to normative recommendations, facing criticism for attempting to bridge the is-ought gap [6].
Solution: Implement transparent reasoning processes:
- Explicitly state the ethical framework guiding normative analysis
- Document how empirical findings inform but don't determine ethical conclusions
- Use reflective equilibrium methods to balance empirical data with ethical principles
- Acknowledge limitations in generalizing from specific contexts to broader norms
Frequently Asked Questions (FAQs)
Q1: What objectives are most acceptable for empirical bioethics research?
A: Research shows that understanding the context of a bioethical issue and identifying ethical issues in practice receive nearly unanimous agreement from researchers in the field [6]. The most contested objectives include striving to draw normative recommendations and developing/justifying moral principles [6].
Q2: How can I ensure my empirical bioethics research is methodologically rigorous?
A: Ensure methodological transparency and align your methods with your epistemological stance [48]. Consider adopting a "diagnostic attitude" marked by continuous re-examination of your questions, participants' stories, and analytical frames rather than a purely problem-solving approach [48].
Q3: What is the role of stakeholder engagement in empirical bioethics?
A: Stakeholder engagement is crucial throughout the research process, particularly when formulating specific norms and developing interventions [7]. Engagement helps ensure that ethical guidance is feasible and contextually appropriate.
Q4: How can implementation science principles improve ethical practice?
A: Implementation science provides frameworks for addressing barriers to implementing ethical norms, including intervention characteristics, outer and inner settings, individual characteristics, and implementation processes [7]. Applying these principles can help bridge the "ought-is" gap.
Experimental Protocols & Methodologies
Narrative Interviewing Protocol
Based on narrative approaches in empirical bioethics [48], this protocol enables researchers to gather rich, contextualized data:
Preparation Phase:
- Define research question with attention to ethical and empirical dimensions
- Conduct ethical review considering sensitive nature of bioethics topics
- Develop interview guide with open-ended questions and potential probes
Interview Phase:
- Create environment conducive to storytelling
- Use minimal prompts to encourage narrative flow
- Attend to nonverbal cues and emotional content
- Document contextual factors and researcher reflections
Analysis Phase:
- Transcribe interviews with attention to paralinguistic features
- Analyze data using both thematic and narrative approaches
- Consider personal, interpersonal, and cultural levels of narrative construction
- Validate interpretations through member checking or peer debriefing
Implementation Assessment Protocol
This protocol helps assess the feasibility of implementing ethical norms [7]:
Feasibility Testing:
- Identify potential barriers using the Consolidated Framework for Implementation Research (CFIR)
- Engage stakeholders in assessing practical constraints
- Pilot test interventions in limited settings
- Measure both process and outcome indicators
Adaptation Process:
- Refine specific norms based on feasibility assessment
- Modify intervention strategies to address contextual barriers
- Develop implementation supports tailored to setting characteristics
Table: Acceptable Objectives in Empirical Bioethics Research
| Research Objective | Acceptance Level | Key Considerations | Methodological Approaches |
|---|---|---|---|
| Understanding context of bioethical issues | High agreement [6] | Requires deep immersion in setting | Ethnography, qualitative interviews, document analysis |
| Identifying ethical issues in practice | High agreement [6] | Distinguish between perceived and actual ethical issues | Mixed methods, observation, focus groups |
| Informing policy development | Moderate agreement [6] | Balance ideal vs. practical considerations | Delphi methods, stakeholder engagement, policy analysis |
| Developing normative recommendations | Contested [6] | Must address is-ought gap explicitly | Reflective equilibrium, reasoned justification |
| Justifying moral principles | Most contested [6] | Requires philosophical rigor alongside empirical data | Integrated empirical-ethical methodologies |
Table: Implementation Science Framework Applied to Bioethics
| Implementation Domain | Application to Bioethics | Assessment Methods |
|---|---|---|
| Intervention Characteristics | Adapt ethical norms to specific contexts | Feasibility testing, pilot studies |
| Outer Setting | Consider external policies, regulations | Environmental scanning, stakeholder analysis |
| Inner Setting | Address organizational culture, resources | Organizational readiness assessment |
| Individual Characteristics | Account for stakeholder values, capabilities | Surveys, interviews, assessment of ethical sensitivity |
| Process of Implementation | Develop structured approach to implementing ethical norms | Process mapping, implementation tracking |
Visualizing the Empirical-Normative Integration Process
Integrating Empirical and Normative Approaches in Bioethics
Interdisciplinary collaboration, defined as people from different disciplines working together from a project's inception to completion, has become a necessity in academic institutions and research [49]. In bioethics, this involves bridging the gap between normative expertise (focused on ethical principles and what "ought" to be) and empirical expertise (focused on gathering evidence about what "is") [16] [7]. This collaboration is essential for addressing complex bioethical issues that require both ethical analysis and empirical investigation of real-world practices, stakeholders' experiences, and clinical contexts [16] [11].
The central challenge in this interdisciplinary endeavor is the is-ought problem—the philosophical difficulty of deriving ethical prescriptions (what "ought" to be) solely from empirical facts (what "is") [1]. This problem creates a significant barrier to integrating empirical research findings into normative ethical frameworks [16] [7] [11]. Despite this challenge, empirical research in bioethics has grown substantially, with researchers recognizing its value for understanding the context of bioethical issues and identifying ethical issues in practice [11]. Successful collaboration requires specific strategies to navigate the methodological and communicative challenges that arise when bridging these different epistemological traditions [49] [50].
Understanding the Is-Ought Gap and Implementation Challenge
The Nature of the Is-Ought Problem
The is-ought problem, first articulated by philosopher David Hume, represents a significant challenge in moral philosophy. It arises when claims about what "ought" to be are based solely on statements about what "is" [1]. Hume noted a fundamental difference between descriptive statements (about facts) and prescriptive statements (about values), observing that it is not logically valid to derive moral conclusions from purely factual premises without additional moral premises [1].
In contemporary bioethics, this problem manifests in debates about the proper relationship between empirical research and normative analysis [16] [11]. While empirical research can describe current practices, beliefs, and attitudes, it cannot alone determine what is ethically required or prohibited [16]. This creates a significant challenge for interdisciplinary collaboration between empirical researchers and normative scholars in bioethics.
From Ought to Is: The Implementation Challenge
Beyond the traditional is-ought problem, bioethics faces a corresponding "ought-is" problem—the challenge of implementing ethical norms in practice [7]. Once normative claims are developed, there exists an ethical imperative to effect changes based on these norms, yet this implementation process often encounters significant barriers [7].
Implementation science offers valuable insights for addressing this challenge. This discipline studies methods to promote the systematic uptake of research findings into routine practice [7]. The Consolidated Framework for Implementation Research (CFIR) identifies five domains that can serve as barriers or facilitators to successful implementation: (1) intervention characteristics, (2) outer setting, (3) inner setting, (4) characteristics of the individuals involved, and (5) implementation process [7].
Table: Domains of the Consolidated Framework for Implementation Research (CFIR)
| Domain | Description | Application to Bioethics |
|---|---|---|
| Intervention Characteristics | Features of the ethical norm or intervention being implemented | Assessing how complex, testable, and adaptable ethical norms are for practical contexts |
| Outer Setting | External influences on the organization | Economic, political, and cultural factors affecting ethical implementation |
| Inner Setting | Internal organizational context | Structural, cultural, and implementation climate within healthcare institutions |
| Characteristics of Individuals | Attributes of those involved | Knowledge, beliefs, and self-efficacy of professionals implementing ethical norms |
| Process of Implementation | How implementation is accomplished | Planning, engaging, executing, and reflecting on implementation efforts |
The framework above demonstrates that successfully navigating from normative "ought" to practical "is" requires systematic attention to multiple contextual factors beyond the ethical justification itself [7].
Effective Collaboration Strategies and Frameworks
Foundational Strategies for Interdisciplinary Teams
Research on successful interdisciplinary collaborations has identified several key strategies that facilitate effective teamwork across disciplinary boundaries [49]:
Define Shared Goals and Objectives: Collaborators should explicitly articulate shared objectives and clarify member responsibilities from the project's beginning, making adjustments as necessary throughout the collaboration [49].
Develop a Shared Language: Teams should conduct workshops to improve communication and reduce disciplinary jargon, creating a common conceptual framework that all members understand [49].
Create Knowledge Exchange Mechanisms: Teams should develop environments that encourage members to share their expertise and epistemological approaches [49].
Establish Conflict Resolution Protocols: Teams should create clear processes for resolving disagreements that inevitably arise from different disciplinary perspectives and methodologies [49].
Foster an Inclusive Collaborative Environment: Teams should actively promote diversity and inclusion while creating shared learning communities that foster creativity [49].
Implement Progress Evaluation Systems: Teams should establish regular assessment processes to monitor progress and make necessary adjustments to collaboration strategies [49].
These strategies help interdisciplinary teams overcome common challenges such as communication barriers, different methodological approaches, and disciplinary cultural differences [49] [50].
The Hierarchical Framework for Empirical Bioethics Research
Empirical research in bioethics can be conceptualized as operating at different levels of abstraction and normative significance. One proposed framework categorizes empirical bioethics research into four hierarchical levels [16]:
Table: Hierarchical Framework for Empirical Research in Bioethics
| Level | Category | Description | Examples |
|---|---|---|---|
| 1 | Lay of the Land | Defines current practices, opinions, beliefs or other aspects of the status quo | Surveys of physician attitudes on end-of-life care; studies of ethics committee composition [16] |
| 2 | Ideal Versus Reality | Assesses the extent to which actual clinical practice reflects ethical ideals | Research demonstrating disparities in healthcare delivery across racial groups; studies showing inadequate understanding in informed consent for research [16] |
| 3 | Improving Care | Develops and tests approaches to bring clinical practice closer in line with ethical ideals | Interventions to improve informed consent processes; programs to reduce healthcare disparities [16] [7] |
| 4 | Changing Ethical Norms | Synthesizes empirical findings from multiple studies to inform and potentially modify ethical principles | Using accumulated evidence on end-of-life decision-making to refine concepts of patient autonomy; incorporating empirical findings on cultural variations in truth-telling to contextualize disclosure norms [16] |
This framework demonstrates how empirical research can contribute to bioethics at different levels, with higher levels involving greater integration of empirical findings with normative analysis [16]. Most researchers find the first three levels less controversial than the fourth, which directly addresses the is-ought gap by suggesting empirical research can inform the development and justification of moral principles [11].
Empirical Bioethics Research Hierarchy
Technical Support: Troubleshooting Common Collaboration Challenges
Frequently Asked Questions (FAQs)
Q1: How can we effectively communicate across disciplinary boundaries when our fields use the same terms with different meanings?
A: Establish a shared glossary at the beginning of your collaboration and schedule regular "jargon-busting" sessions where team members explain key concepts from their disciplines in accessible language [49]. Document these definitions in a shared repository that all members can reference throughout the project.
Q2: What should we do when empirical findings appear to contradict established ethical norms?
A: First, carefully examine the methodological assumptions and limitations of the empirical research [16] [11]. Then, analyze whether the ethical norms might require specification or contextualization rather than outright rejection. Use these moments of tension as opportunities for conceptual refinement rather than seeing them as threats to either discipline [16] [11].
Q3: How can we allocate credit fairly in publications when our interdisciplinary team includes both empirical and normative researchers?
A: Discuss authorship criteria and order early in the collaboration process, using established guidelines such as the Vancouver Protocol. Consider the value of publishing companion pieces in specialized journals when a single interdisciplinary journal is not feasible [49].
Q4: What strategies can help bridge different methodological approaches between empirical and normative research?
A: Develop a shared methodology that explicitly integrates both approaches, such as "embedded ethics" where ethicists are integrated into empirical research teams, or "iterative integration" where normative and empirical work inform each other in repeated cycles [11].
Q5: How can we secure funding for truly interdisciplinary work that may not fit neatly into traditional disciplinary categories?
A: Craft proposals that explicitly address the added value of the interdisciplinary approach, document successful prior collaborations, include team members with established interdisciplinary track records, and carefully explain your integration strategy to reviewers who may represent different disciplinary perspectives [49].
Troubleshooting Guide for Common Collaboration Problems
Table: Troubleshooting Common Interdisciplinary Collaboration Challenges
| Problem | Symptoms | Possible Solutions | Prevention Strategies |
|---|---|---|---|
| Communication Breakdown | Meetings dominated by one discipline; persistent misunderstandings; side conversations about "what they really mean" | Implement facilitated dialogues; create a shared glossary; use visual mapping of concepts [49] | Establish communication norms early; include communication training in team development [49] |
| Methodological Tensions | Disagreements about what counts as evidence; conflicts about research design; questioning of each other's approaches | Develop a shared methodology document; invite outside methodological consultants; design pilot studies [11] | Discuss methodological assumptions during team formation; educate members about each other's methods [49] |
| Power Imbalances | One discipline dominates decision-making; certain perspectives consistently marginalized; authorship disputes | Implement rotating leadership; create explicit criteria for decision-making; use external facilitators [49] [50] | Establish shared governance structures; clearly define roles and responsibilities [49] |
| Integration Failures | Parallel research streams that never connect; final product looks like separate reports stapled together | Schedule regular integration sessions; create conceptual maps linking components; assign integration facilitators [49] [11] | Build integration into project timeline; designate responsibility for integration [49] |
The troubleshooting approach for interdisciplinary collaborations shares similarities with methodological troubleshooting in laboratory science, which emphasizes systematic problem identification, controlled variable testing, and thorough documentation [51] [52]. Both contexts require structured approaches to diagnosing and addressing problems when expected outcomes are not achieved.
Systematic Troubleshooting Approach
Essential Research Reagent Solutions for Interdisciplinary Bioethics
Successful interdisciplinary collaboration in bioethics requires both conceptual and methodological "reagents" that facilitate the integration of normative and empirical approaches.
Table: Essential Methodological Reagents for Interdisciplinary Bioethics Research
| Research Reagent | Function | Application Examples |
|---|---|---|
| Shared Conceptual Glossary | Creates common definitions for terms used differently across disciplines | Defining "autonomy" in ways meaningful to both philosophers and social scientists [49] |
| Iterative Integration Framework | Structures repeated cycles of normative and empirical work | Empirical findings inform ethical analysis, which generates new research questions for empirical investigation [11] |
| Stakeholder Engagement Protocols | Ensures relevant perspectives are included in research process | Engaging patients, clinicians, and policymakers in research on healthcare allocation [49] [7] |
| Mixed Methods Design | Combines qualitative and quantitative approaches | Using surveys to establish frequencies and interviews to understand meanings and experiences [16] [11] |
| Implementation Science Frameworks | Supports translation of ethical norms into practice | Applying CFIR to implement new informed consent processes in healthcare systems [7] |
| Ethical Deliberation Methods | Structures normative analysis in response to empirical findings | Using specified principlism or casuistry to interpret empirical results [16] [11] |
These methodological reagents provide the necessary tools for conducting rigorous interdisciplinary research that respects both normative and empirical traditions while generating integrated insights [49] [16] [7].
Case Study: Implementing Improved Informed Consent Processes
The challenge of improving informed consent for research participation illustrates how interdisciplinary collaboration can address the is-ought gap through systematic approaches [16] [7]. The ethical norm that "researchers should obtain informed consent from competent adults before enrolling them in a research project" is well-established but often imperfectly implemented [7].
Empirical research has demonstrated that many research subjects fail to understand basic aspects of clinical trials, including the purpose of the study, its voluntary nature, and the distinction between research and therapy [16]. This discrepancy between ethical ideal (valid informed consent) and empirical reality (deficient understanding) creates an imperative for interdisciplinary collaboration [16] [7].
An interdisciplinary team might address this challenge by:
Conducting Lay of the Land Research: Documenting current consent processes and identifying specific areas of misunderstanding [16].
Developing Interventions: Creating revised consent forms that use plain language, graphics, and improved formatting to enhance comprehension [7].
Testing Interventions: Implementing the revised consent processes and measuring their impact on understanding using validated instruments [16] [7].
Disseminating Findings: Sharing successful approaches broadly and advocating for policy changes based on empirical evidence [7].
This approach bridges normative and empirical expertise by using empirical methods to implement and refine ethical norms, while using ethical analysis to interpret empirical findings and guide practical recommendations [16] [7] [11].
Successfully bridging normative and empirical expertise in bioethics requires thoughtful strategies for interdisciplinary collaboration that directly address the is-ought problem [49] [16] [7]. By implementing structured approaches to communication, methodology, and integration, interdisciplinary teams can generate insights that neither discipline could produce alone [49] [50]. The frameworks, troubleshooting guides, and reagent solutions presented here provide practical resources for researchers embarking on these essential collaborations.
As bioethics continues to address complex challenges at the intersection of healthcare, technology, and society, the ability to effectively integrate normative and empirical approaches will become increasingly crucial [16] [7] [11]. By viewing the is-ought relationship as an opportunity for creative tension rather than an insurmountable barrier, interdisciplinary teams can develop ethically grounded and empirically informed approaches to pressing bioethical challenges [16] [11].
Technical Support Center
Troubleshooting Guides
Problem: Your research conclusions seem to over-privilege either empirical findings or theoretical norms, creating an imbalance that fails to truly bridge the is-ought gap.
Underlying Cause: This often occurs when the integration methodology—the process of combining empirical data with normative analysis—is poorly defined or inconsistently applied [12].
Troubleshooting Steps:
Diagnose the Imbalance: Systematically check your research process against the following table to identify where the drift occurs:
Phase Check Indicator of Empirical Over-weighting Indicator of Normative Over-weighting Framing Research Question Question is purely descriptive (e.g., "What are the attitudes?") with no inherent normative goal. Question is purely theoretical; empirical data is an afterthought. Data Collection Role of Data Data is treated as a direct source of moral truth ("is" directly implies "ought"). Data is used anecdotally or selectively to support a pre-existing theoretical conclusion [53]. Integration Methodology Use of vague, undefined "back-and-forth" methods without theoretical justification [12]. No clear method for allowing empirical findings to challenge or refine normative premises. Shaping Conclusion Recommendations simply mirror the majority view in the data ("ethics by opinion poll"). Recommendations ignore relevant empirical realities about stakeholder experiences. Select and Justify an Integration Method: Choose a explicit methodology for integration and transparently report its use. Common methods include [12]:
- Reflective Equilibrium: A "back-and-forth" process of adjusting ethical judgments, principles, and empirical data until they cohere.
- Dialogical Empirical Ethics: Using structured dialogue between researchers and stakeholders to develop shared normative understandings.
Conduct a "Limitation Prominence Assessment": To guard against unconscious normative bias, critically evaluate your study's limitations. Ask not just what the limitations are, but how significantly they could affect the interpretation of your data in light of the ethical question. Give prominent discussion to limitations that most risk leading to a misreading of the results [53].
Guide 2: Addressing "Vagueness" in Integration Methodology
Problem: The process of how empirical data and normative analysis were combined is described as a "dialogue" or "iterative process," but the specific steps, decision points, and influences remain opaque to reviewers and readers [12].
Underlying Cause: A lack of explicit, structured frameworks for conducting and reporting the integration process.
Troubleshooting Steps:
Adopt a Structured Framework: Implement the Mapping-Framing-Shaping framework to structure your entire project [15]. The workflow for this framework is illustrated below, ensuring a logical progression from understanding the landscape to issuing recommendations.
Document the Integration Rigorously: For the "Integration Process" node in the diagram, maintain an audit trail that records:
- Which specific empirical finding challenged which specific normative premise.
- How the conflict was resolved (e.g., was the premise revised, or was the finding re-interpreted?).
- How different weighting given to data points (e.g., from different stakeholders) influenced the final normative outcome [54].
Frequently Asked Questions (FAQs)
FAQ 1: What is the single most common cause of a failed empirical bioethics study?
The most common cause is not a technical failure in data collection, but a failure to adequately articulate and execute the method of integration between the empirical and the normative [12]. Without a transparent and defensible integration method, the study risks being perceived as either poor social science or poor philosophy, and its conclusions will lack persuasive force for bridging the is-ought gap.
FAQ 2: How can I prevent my own ethical views from biasing the presentation of empirical data?
This is a risk known as normative bias [53]. Mitigation strategies include:
- Reflexivity: Continuously critically reflect on your own presuppositions and how they might shape the research.
- Peer Debriefing: Have colleagues, particularly those with different viewpoints, review your interpretation of the data.
- Prominent Limitations Reporting: Use the "Limitation Prominence Assessment" to ensure the most critical limitations of your study—especially those that could lead to misinterpretation in favor of your hypothesis—are discussed prominently, not buried [53].
FAQ 3: When combining data from different sources (e.g., patients, clinicians), should all data be weighted equally?
Not necessarily. The appropriate weighting of data is a normative decision itself and should be justified based on the research question [54]. For example, if studying the ethical implementation of a new therapy, the experiences of patients receiving that therapy might be given more weight than those of other stakeholders. The key is to be transparent about why certain data or perspectives were given more influence in shaping the final normative conclusion.
The Scientist's Toolkit: Essential Methodological Reagents
The following table details key methodological components essential for conducting rigorous empirical bioethics research.
| Item | Function in Empirical Bioethics |
|---|---|
| Integration Methodology (e.g., Reflective Equilibrium) | Provides the theoretical framework for combining descriptive "is" data with normative "ought" analysis, directly addressing the core challenge of the field [12]. |
| Structured Research Framework (e.g., Mapping-Framing-Shaping) | Offers a high-level blueprint for the entire research project, ensuring each phase builds logically toward normative recommendations [15]. |
| Weighting Strategy | A pre-defined plan for handling different data types and sources, used to correct for bias and reflect the relative importance of various empirical inputs in the final normative analysis [54]. |
| Limitation Prominence Assessment | A reflexive tool to evaluate and prominently report study limitations based on their potential to mislead the ethical debate, thereby guarding against normative bias [53]. |
| Transparency Protocol | A commitment to clearly stating how the integration method was chosen, justified, and executed, which is a key standard of practice for the field [12]. |
Researcher Perspectives and Validated Approaches in Contemporary Practice
FAQ: Understanding Empirical Bioethics Research
Q1: What is the fundamental challenge of integrating empirical research into bioethics? The fundamental challenge is navigating the is-ought gap, a philosophical problem articulated by David Hume. This principle states that one cannot logically infer a prescriptive statement about what "ought" to be from purely descriptive statements about what "is" [1]. In empirical bioethics, this raises questions about how factual data about the world can be used to derive normative, ethical conclusions [11].
Q2: What are the most widely accepted objectives for empirical research in bioethics? According to a 2022 qualitative study exploring researchers' views, two objectives received unanimous agreement from scholars [11] [55]:
- Understanding the context of a bioethical issue.
- Identifying ethical issues in practice. These objectives are considered the least contested because they focus on producing empirical results that inform the ethical debate without making a direct leap to normative conclusions.
Q3: Which objectives in empirical bioethics are more contested among researchers? The same study found that the most contested objectives are the more ambitious ones that directly engage with normative conclusions [11] [55]. These are:
- Striving to draw normative recommendations.
- Developing and justifying moral principles. Researchers expressed that while empirical data can provide a "testing ground" for normative theory, these ambitious objectives require careful integration of empirical facts into normative inquiry, often guided by normative expertise [11].
Q4: Can empirical research ever lead to changing ethical norms? Yes, but this process is complex. Empirical research can reveal a gap between established ethical norms and real-world practice, or provide data showing that the outcomes of certain practices do not align with ethical goals. This is often a precursor to re-evaluating and changing specific ethical norms (e.g., guidelines for practice) rather than overarching moral principles [56] [7]. This process is most robust when it involves stakeholder engagement and considers feasibility [7].
Q5: What is the "Ought-Is" problem? While the classic "Is-Ought" problem concerns deriving ethical norms from facts, the "Ought-Is" problem focuses on the challenge of implementing established ethical norms into practice. It asks: how does one ensure that an ethical "ought" is actually enacted and sustained in the real world? This problem has led to calls for using implementation science—a discipline dedicated to supporting the sustained enactment of interventions—within ethics [7].
Troubleshooting Common Research Challenges
Problem: My empirical findings are dismissed as irrelevant to the normative debate.
- Potential Cause: The research is perceived as merely describing facts without clearly connecting them to a relevant ethical principle or argument.
- Solution: Proactively frame your research. Explicitly state which ethical concepts (e.g., autonomy, justice, well-being) your data illuminates. Position your work as informing the empirical premises of an ethical argument, not as directly generating a moral conclusion [11].
Problem: I am unsure how to move from my data to a normative recommendation.
- Potential Cause: This is the core is-ought challenge. A direct logical deduction is impossible; a normative framework is required for the transition.
- Solution: Do not work in isolation. Collaborate with normative ethicists or engage deeply with normative theory. Use your data to test, challenge, or refine the empirical assumptions within existing ethical theories or principles [11]. Clearly delineate between your empirical findings and the subsequent normative interpretation.
Problem: My research on an ethical topic is not recognized as "bioethics" by journals.
- Potential Cause: A significant amount of empirically-informed ethics research is published in clinical or scientific journals without explicit ethics keywords, making it "hidden" from the bioethics community [56].
- Solution: If publishing in a non-ethics journal, proactively include ethics-related keywords and a discussion of the ethical implications of your findings. This makes the work more discoverable for bioethicists conducting literature reviews [56].
Problem: An ethical intervention or guideline, while sound in theory, fails to be adopted in practice.
- Potential Cause: This is a failure of implementation, falling into the "Ought-Is" gap. The norm or intervention may not be feasible, or key barriers to its adoption were not addressed [7].
- Solution: Adopt an "implementation mindset" from the outset. Utilize frameworks from implementation science, such as the Consolidated Framework for Implementation Research (CFIR), to diagnose barriers and facilitators related to the intervention itself, the inner and outer settings, and the individuals involved [7].
Experimental Protocols & Methodological Pathways
Protocol 1: A Framework for Integrating Empirical Data into Normative Analysis
This protocol outlines a systematic approach to using empirical research to inform bioethical analysis without committing a naturalistic fallacy.
- Step 1: Define the Ethical Question. Clearly state the normative question (e.g., "Ought we to use placebo controls in trials for antidepressants?").
- Step 2: Identify Empirical Premises. Identify the factual claims that underpin existing arguments about the question (e.g., "Placebo groups in antidepressant trials are exposed to substantial morbidity and mortality.") [56].
- Step 3: Gather Empirical Data. Conduct or locate rigorous empirical research to test these premises (e.g., a review of safety data from clinical trial databases) [56].
- Step 4: Analyze Normative Implications. Interpret the empirical findings in the context of the ethical question. Do they challenge, support, or complicate the existing empirical premises of the debate? (e.g., Data showing no significant increase in harm in placebo groups challenges the premise that such trials are inherently high-risk.) [56].
- Step 5: Refine the Ethical Argument. Re-formulate the ethical argument using the updated empirical premises. The normative conclusion is based on a revised understanding of the facts, not derived from them directly.
The logical workflow of this protocol is depicted below, showing how empirical and normative inquiry interact iteratively.
Protocol 2: A Framework for Implementing Ethical Norms ("Ought-Is")
This protocol uses principles from implementation science to bridge the gap between establishing an ethical norm and ensuring its sustained enactment in practice [7].
- Step 1: Formulate an Aspirational Norm. Start with a broad, agreed-upon ethical goal (e.g., "No patient should suffer preventable pain.").
- Step 2: Specify the Norm. Develop a specific, actionable norm (e.g., "All physicians in our hospital should regularly assess pain and offer relief to patients who seek it.").
- Step 3: Develop an Intervention. Design a concrete intervention to enact the specific norm (e.g., a mandatory pain assessment tool in electronic health records coupled with staff training).
- Step 4: Study and Evaluate. Implement the intervention and measure outcomes (e.g., rates of pain assessment, patient-reported pain scores) to determine its success.
- Step 5: Identify and Disseminate Best Practices. Share the successful intervention broadly and, if effective, support it with policy changes to ensure sustained implementation.
The following diagram visualizes this multi-stage translation process from a broad ideal to concrete, disseminated practice.
The following table details key conceptual "tools" and frameworks essential for conducting rigorous empirical bioethics research.
| Tool/Framework | Primary Function | Key Consideration |
|---|---|---|
| Qualitative Methods (e.g., interviews, focus groups) [11] | To gain in-depth understanding of the context and lived experience of ethical issues from stakeholder perspectives. | Critical for achieving the most accepted objective of "understanding context." |
| Systematic Reviews [56] | To rigorously synthesize existing empirical data relevant to an ethical debate (e.g., on outcomes of tube feeding in dementia). | Helps establish a reliable evidence base to test the empirical premises of ethical arguments. |
| Implementation Science Frameworks (e.g., CFIR) [7] | To diagnose barriers and facilitators for implementing an ethical norm or intervention in a specific setting. | Directly addresses the "Ought-Is" problem by providing a structured approach to enactment. |
| Stakeholder Engagement [7] | To ensure the perspectives of all affected parties (patients, clinicians, etc.) are incorporated into both normative and empirical work. | Improves the feasibility, relevance, and legitimacy of the research and its outcomes. |
| Normative Ethical Theory [11] | To provide the logical framework and principles needed to move from empirical data to ethical justification. | An essential tool for navigating the is-ought gap; collaboration with normative experts is recommended. |
FAQs: Core Concepts and Common Challenges
FAQ 1.1: What does "Understanding Context" mean in empirical bioethics research, and why is it a highly supported objective? Understanding context refers to the process of investigating the real-world circumstances, stakeholder perspectives, and situational factors that surround a bioethical issue. This objective is highly supported because ethical principles cannot be applied in a vacuum; they must be informed by the specific realities of clinical practice, research settings, and patient experiences. Research shows this objective receives unanimous agreement from bioethics scholars because it grounds normative inquiry in actual facts and conditions, helping to bridge the "is-ought" gap by ensuring ethical analysis is relevant to practice [6].
FAQ 1.2: Why is "Identifying Ethical Issues in Practice" considered a foundational objective for empirical bioethics? This objective involves using empirical methods to detect and describe ethical problems as they naturally occur in healthcare and research settings, rather than relying solely on theoretical deduction. It is foundational because it ensures that bioethics research addresses genuine, rather than hypothetical, moral challenges. This empirical approach reveals how ethical principles are navigated in complex real-world situations, making it a crucial first step before developing normative recommendations [6].
FAQ 1.3: How do these objectives help address the "is-ought" gap in bioethics? The "is-ought" gap describes the philosophical challenge of deriving ethical prescriptions ("ought") from empirical facts ("is"). Understanding context and identifying ethical issues in practice address this gap by:
- Providing a testing ground for normative theory with real-world data [6]
- Ensuring ethical recommendations are feasible and relevant to actual practice [7]
- Creating a feedback loop where empirical findings can challenge and refine ethical principles [7]
FAQ 1.4: What are common methodological challenges when pursuing these objectives? Researchers commonly encounter:
- Integration Vagueness: Uncertainty about how to systematically combine empirical findings with normative analysis [57]
- Theoretical-Methodological Alignment: Ensuring chosen research methods align with epistemological commitments [58]
- Stakeholder Engagement: Adequately incorporating perspectives of all relevant parties while maintaining methodological rigor [7]
FAQ 1.5: What ethical safeguards are necessary when conducting empirical bioethics research? When studying sensitive bioethical issues in practice, researchers must:
- Implement special protections for vulnerable populations (e.g., children, patients) following regulatory requirements [59]
- Secure appropriate informed consent that acknowledges the dual role of researcher and ethicist [7]
- Obtain IRB/IEC approval that addresses both empirical and normative dimensions of the research [59]
- Consider justice implications, especially in international research contexts [59]
Troubleshooting Guides for Empirical Bioethics Research
Troubleshooting Guide 2.1: Addressing Integration Challenges Between Empirical Data and Normative Analysis
Problem: Researchers struggle to meaningfully integrate empirical findings with normative ethical analysis.
Symptoms:
- Research results in parallel streams of empirical data and ethical theory that never fully connect
- Peer reviewers note that the paper "doesn't bridge the is-ought divide"
- Uncertainty about how much weight to give empirical findings versus ethical principles
Step-by-Step Solution:
- Select an Explicit Integration Framework Early
- Choose a specific methodological approach (e.g., Reflective Equilibrium, Dialogical Empirical Ethics) during study design [57]
- Document how this framework will guide both data collection and normative analysis
- Justify this choice based on your research question and theoretical commitments
Implement Back-and-Forth Analysis
- Use iterative cycles between empirical data and normative concepts [57]
- Create a structured process for challenging ethical principles with empirical findings
- Allow empirical data to reveal limitations in existing ethical frameworks
Engage in Deliberative Dialogue
- Organize structured discussions with stakeholders (clinicians, patients, policymakers) [57]
- Use these dialogues to test emerging normative conclusions against practical experience
- Document how stakeholder input shaped final ethical analysis
Document the Integration Process Transparently
- Clearly describe in publications how integration was achieved
- Acknowledge limitations and challenges in the integration process
- Explicitly state how empirical findings informed normative conclusions [57]
Troubleshooting Guide 2.2: Overcoming Contextual Understanding Barriers
Problem: Research fails to adequately capture the context of ethical issues.
Symptoms:
- Findings seem abstract or disconnected from real-world practice
- Research participants indicate that results don't reflect their lived experiences
- Difficulty translating findings into practical recommendations
Step-by-Step Solution:
- Employ Immersive Methodologies
- Use ethnographic approaches to observe ethical issues in natural settings
- Implement longitudinal designs to understand how contexts change over time
- Consider purpose-built digital tools (e.g., virtual scenarios) to study ethical decision-making in simulated contexts [58]
Triangulate Data Sources
- Combine interviews with observation and document analysis
- Seek perspectives from multiple stakeholder groups
- Use mixed methods to capture both breadth and depth of context
Adopt a "Design Bioethics" Approach
Troubleshooting Guide 2.3: Enhancing Ethical Issue Identification in Complex Environments
Problem: Research misses subtle or systemic ethical issues in practice.
Symptoms:
- Only surface-level or obvious ethical concerns are identified
- Participants struggle to articulate ethical dimensions of their experiences
- Research reveals individual-level issues but misses organizational or systemic concerns
Step-by-Step Solution:
- Implement Sensitizing Procedures
- Use contrastive vignettes to help participants recognize ethical dimensions [58]
- Employ ethical incident technique, asking participants to describe situations that "didn't feel right"
- Incorporate reflexive exercises where participants consider alternative perspectives
Leverage Experimental Survey Methods
Apply Systematic Ethical Frameworks
- Use established ethical frameworks (e.g., principlism) as heuristic devices during data analysis
- Look for ethical tensions between different principles in practice
- Identify how organizational structures create predictable ethical challenges
Conceptual Framework for Addressing the Is-Ought Gap
Research Reagent Solutions for Empirical Bioethics
Table: Essential Methodological Tools for Empirical Bioethics Research
| Research 'Reagent' | Function | Application Examples | Key Considerations |
|---|---|---|---|
| Reflective Equilibrium Framework | Enables iterative refinement between empirical data and ethical principles [57] | Testing how empirical findings about patient preferences challenge principles of autonomy | Requires transparent documentation of the reflective process; addresses is-ought gap through coherence building |
| Structured Dialogical Methods | Facilitates co-creation of normative positions through stakeholder dialogue [57] | Developing ethical guidelines for emerging technologies with multiple stakeholder groups | Demands skilled facilitation; produces contextually-grounded normative outputs |
| Contrastive Vignettes | Reveals how contextual factors influence moral judgments [58] | Studying how resource allocation decisions change with different patient characteristics | Controls for extraneous variables while testing specific contextual influences |
| Implementation Science Framework | Supports translation of ethical norms into sustainable practices [7] | Implementing and sustaining informed consent improvements in research practice | Addresses the "ought-is" problem by focusing on feasibility and sustainability |
| Purpose-Built Digital Tools | Creates controlled but contextualized environments for studying ethical decision-making [58] | Using serious games to study privacy decisions in mental health care | Balances ecological validity with experimental control; enables research at scale |
| Consolidated Framework for Implementation Research (CFIR) | Identifies barriers and facilitators to implementing ethical practices [7] | Diagnosing why ethical guidelines fail to change clinical behavior | Provides comprehensive assessment across intervention characteristics, settings, and processes |
Methodological Workflow for Contextual Understanding
Quantitative Support for Research Objectives
Table: Researcher Agreement with Objectives of Empirical Bioethics Research (Adapted from Empirical Studies)
| Research Objective | Level of Support | Key Rationales | Methodological Preferences |
|---|---|---|---|
| Understanding Context of Bioethical Issues | Unanimous agreement among researchers [6] | Essential for relevant and applicable ethical analysis; grounds normative inquiry in actual practice | Mixed methods; immersive ethnography; stakeholder engagement; digital context simulation [58] |
| Identifying Ethical Issues in Practice | Unanimous agreement among researchers [6] | Reveals actual rather than theoretical ethical challenges; ensures research addresses genuine concerns | Observational studies; ethical incident technique; practice-based ethnography; contrastive vignettes [58] |
| Informing Policy Development | High support with varying agreement levels [6] | Increases practical impact of bioethics research; connects ethical analysis to real-world decision-making | Deliberative dialogues; stakeholder engagement; policy analysis; implementation science approaches [7] |
| Drawing Normative Recommendations | Contested support among researchers [6] | Concerns about is-ought gap; challenges in justifying move from descriptive to prescriptive | Reflective equilibrium; reasoned justification; transparent normative reasoning; collaborative approaches [57] |
| Developing/Justifying Moral Principles | Most contested objective [6] | Significant methodological challenges; requires robust philosophical justification alongside empirical data | Wide reflective equilibrium; coherentist approaches; foundational philosophical analysis complemented by empirical insights [57] |
Troubleshooting Guides and FAQs for Empirical Bioethics Research
Troubleshooting Common Research Challenges
Issue: Navigating the Is-Ought Gap in Analysis Problem: Researchers are uncertain how to move from empirical data (what "is") to normative recommendations (what "ought" to be) without committing a naturalistic fallacy.
- Solution: Treat the is-ought gap not as an insurmountable obstacle, but as a critical warning sign. Use it to prompt reflection on the normative implications of your empirical results rather than treating empirical data as a direct source of morality [6].
- Methodology: Implement the Mapping-Framing-Shaping framework. In the "shaping" phase, explicitly articulate how your normative recommendations are informed by—but not directly derived from—the empirical findings from previous phases [61].
- Validation: Ensure your research team includes both empirical and normative expertise to guide this integrative process appropriately [6].
Issue: Defending Ambitious Normative Claims Problem: Drawing normative recommendations and developing/justifying moral principles are the most contested objectives of empirical bioethics research [6].
- Solution: Position empirical data as a "testing ground" for elements of normative theory rather than a direct justificatory basis. This provides firm ground for integrating empirical facts into normative inquiry while maintaining philosophical rigor [6].
- Documentation: Clearly document your integrative methodology in publications, explaining how you bridged empirical and normative elements to arrive at recommendations [61].
Issue: Achieving Interdisciplinary Integration Problem: Research fails to genuinely integrate empirical and normative approaches, instead treating empirical work as merely illustrative.
- Solution: Adopt explicit standards of practice for interdisciplinary work. The consensus standards for empirical bioethics research provide guidance across six domains: Aims, Questions, Integration, Conduct of Empirical Work, Conduct of Normative Work, and Training & Expertise [62].
- Implementation: Utilize methodologies like reflective equilibrium that provide structured approaches for moving between empirical observations and normative principles [61].
Frequently Asked Questions
Q1: What are the most and least accepted objectives for empirical research in bioethics? A: According to qualitative research with bioethics scholars, the objectives receiving unanimous agreement were:
- Understanding the context of a bioethical issue
- Identifying ethical issues in practice
The most contested objectives were:
- Striving to draw normative recommendations
- Developing and justifying moral principles [6]
Q2: What framework can help structure my empirical bioethics research project? A: The Mapping-Framing-Shaping framework provides a three-phase approach:
- Mapping: Survey the existing terrain through literature reviews to understand the state of knowledge
- Framing: Explore specific areas in depth through qualitative research with stakeholders
- Shaping: Develop recommendations informed by findings from previous phases [61]
Q3: What standards exist for conducting high-quality empirical bioethics research? A: A European consensus project established 15 standards of practice across 6 domains. These standards help ensure rigorous interdisciplinary work that properly integrates empirical and normative elements while maintaining methodological transparency [62].
Q4: How can I address reviewer concerns about the is-ought gap in my research? A: Proactively acknowledge this challenge in your methodology section. Explain how your approach uses empirical data to inform rather than directly justify normative claims. Cite literature that positions the is-ought gap as a critical checkpoint rather than a prohibition [6].
Experimental Protocols and Methodologies
Protocol 1: Mapping-Framing-Shaping Framework Implementation
Three-Phase Research Workflow
Phase 1: Mapping
- Objective: Comprehensively survey existing scholarship and identify knowledge gaps
- Methods: Systematic literature reviews, analysis of previous scholarship from multiple disciplines
- Outcome: Refined research questions and identification of areas requiring deeper exploration [61]
Phase 2: Framing
- Objective: Develop deep understanding of how issues are experienced by stakeholders
- Methods: Qualitative research (interviews, focus groups), analysis of lived experiences
- Outcome: Rich perspectival data on stakeholder perceptions and judgments [61]
Phase 3: Shaping
- Objective: Formulate normative recommendations informed by empirical findings
- Methods: Integrative methodologies (e.g., reflective equilibrium), interdisciplinary analysis
- Outcome: Justified normative claims that are richly informed by empirical reality [61]
Quantitative Data on Researcher Perspectives
Table 1: Acceptability of Empirical Bioethics Research Objectives Among Researchers
| Research Objective | Acceptance Level | Key Rationales |
|---|---|---|
| Understanding context of bioethical issues | Unanimous | Essential for relevant ethical analysis [6] |
| Identifying ethical issues in practice | Unanimous | Grounds ethics in real-world challenges [6] |
| Drawing normative recommendations | Highly Contested | Concerns about is-ought gap; requires careful integration [6] |
| Developing/justifying moral principles | Highly Contested | Most ambitious objective; requires firm theoretical grounding [6] |
Table 2: Key Methodological Resources for Empirical Bioethics Research
| Resource | Function | Application in Research |
|---|---|---|
| Mapping-Framing-Shaping Framework | Provides overarching research structure | Guides project design through three iterative phases [61] |
| Reflective Equilibrium | Integration methodology | Systematically moves between empirical data and ethical principles [61] |
| Qualitative Interview Guides | Data collection | Elicits rich stakeholder experiences and perspectives [6] |
| Standards for Practice | Quality assurance | Ensures rigorous interdisciplinary research conduct [62] |
| Thematic Analysis | Data interpretation | Identifies patterns in qualitative empirical data [61] |
Integration Methodology for Normative Recommendations
Frequently Asked Questions
What is the most supported reasoning pattern for integrating empirical data into bioethics? Empirical research is most supported when it serves as a testing ground for elements of normative theory [11]. This pattern involves using empirical findings to critically examine, validate, or challenge the assumptions and practical implications of existing ethical frameworks. It is widely accepted because it directly connects factual observations to normative deliberation without making an invalid logical leap from "is" to "ought" [11].
How does this reasoning pattern help bridge the is-ought gap? This pattern does not claim that empirical data alone can justify a moral principle. Instead, it treats the is-ought gap as a critical warning sign [11]. It uses empirical data to test whether a normative theory holds up in the real world, examining its practical consequences, identifying unforeseen ethical issues, and ensuring that the resulting norms are feasible and contextually grounded [11] [7].
What are common pitfalls when using this pattern, and how can I avoid them? A major pitfall is attempting to draw direct normative recommendations solely from empirical results, which is one of the most contested objectives in empirical bioethics [11]. To avoid this:
- Maintain a critical perspective: Use data to inform and test normative claims, not to replace normative reasoning [11].
- Engage stakeholders early: Collaborate with those affected by the norms to ensure the research questions and interventions are feasible and relevant [7].
- Integrate implementation science: Consider how a norm will be enacted in practice from the very beginning of your research design [7].
What methodological considerations are crucial for this approach? Your methodology must be rigorous and transparent to ensure the empirical data is a reliable testing ground.
- Mixed-Methods Design: Combine quantitative and qualitative approaches to both measure outcomes and understand lived experiences [11].
- Stakeholder Engagement: Actively involve communities, practitioners, and patients throughout the research process to ensure the findings are relevant and the resulting norms are practicable [7].
- Implementation-Focused Analysis: From the outset, analyze potential barriers and facilitators to implementing any norm derived from your research, using established frameworks like the Consolidated Framework for Implementation Research (CFIR) [7].
Troubleshooting Guide: Common Experimental Challenges
| Challenge | Symptom | Solution |
|---|---|---|
| The Is-Ought Leap | Peer reviewers or colleagues note that your conclusions make an unsupported logical jump from descriptive data to a prescriptive claim [11]. | Reframe the conclusion. Position your empirical findings as testing, challenging, or informing an existing normative claim, rather than definitively establishing a new one [11]. |
| Non-Generalizable Results | Findings from your specific study sample are questioned for their broader relevance to bioethical discourse [11]. | Explicitly discuss the limitations of your study's context and sample. Use your results to generate hypotheses for future research rather than claiming broad applicability [11] [63]. |
| Unfeasible Norms | A normative recommendation derived from your research is dismissed as impractical or impossible to implement in real-world settings [7]. | Adopt an "implementation mindset" during the research phase. Use implementation science frameworks like CFIR to assess the feasibility of potential norms before finalizing them [7]. |
| Lack of Interdisciplinary Integration | The empirical and normative sections of your work feel disconnected, failing to form a cohesive argument [11]. | Structure your research around a feedback loop where empirical findings directly question or support specific aspects of a normative theory, leading to its refinement [11]. |
Experimental Protocols
Protocol 1: Testing a Normative Theory with Qualitative Data This protocol is ideal for exploring how ethical principles are experienced in practice and identifying unforeseen issues.
- Select a Normative Framework: Choose a well-established ethical principle or guideline relevant to your field (e.g., informed consent, respect for autonomy).
- Study Design: Employ a qualitative study design, such as semi-structured interviews or focus groups, with stakeholders who have direct experience with the issue (e.g., patients, clinicians) [11].
- Data Collection: Gather detailed narratives on how the normative principle is understood, enacted, and challenged in real-world situations.
- Analysis: Use thematic analysis to identify consistencies and, more importantly, tensions between the lived experiences of stakeholders and the assumptions of the normative framework.
- Interpretation: Refine or critique the normative theory based on the empirical tensions identified. The data acts as a testing ground for the theory's practical validity [11].
Protocol 2: An Implementation-Focused Path from "Ought" to "Is" This protocol provides a structured, interdisciplinary process for moving from an abstract norm to an enacted practice [7].
- Aspirational Norm: Begin with a broad, agreed-upon ethical goal (e.g., "No patient should experience preventable harm").
- Specific Norm: Through applied ethics deliberation, develop a specific, actionable norm (e.g., "Clinicians should use a validated checklist for high-risk procedures").
- Intervention Development: Collaborate with implementation scientists, clinicians, and system engineers to design a feasible intervention to enact the specific norm.
- Pilot Testing & Measurement: Implement the intervention on a small scale and measure predefined outcomes to determine its success or failure.
- Identification of Best Practices: Analyze the data to identify which intervention strategies most effectively enact the norm.
- Dissemination: Broadly share the successful interventions and support their widespread adoption, potentially through policy changes [7].
Research Reagent Solutions: Essential Methodological Tools
| Research Reagent | Function in Empirical Bioethics |
|---|---|
| Consolidated Framework for Implementation Research (CFIR) | A meta-theoretical framework used to guide systematic assessment of the context in which an intervention (or norm) will be implemented. It helps identify barriers and facilitators across multiple domains [7]. |
| Stakeholder Engagement Panels | A structured forum for involving patients, community members, and practitioners throughout the research process. This ensures the research remains grounded in practical realities and ethical priorities [7]. |
| Qualitative Interview Guides | A pre-defined set of open-ended questions used to gather rich, narrative data on the lived experiences, values, and reasoning patterns of individuals facing a bioethical issue [11]. |
| Process Reward Models (PRMs) | A tool adapted from AI research that provides stepwise evaluation of reasoning quality. In bioethics, this concept can be analogous to establishing criteria to evaluate the quality of ethical deliberation at each stage of a study [64]. |
| Thematic Analysis | A method for analyzing qualitative data by identifying, analyzing, and reporting patterns (themes) within the data. It is essential for distilling complex narratives into findings that can test normative theories [11]. |
Workflow and Conceptual Diagrams
The path from a broad ethical principle to an implemented practice relies on empirical data as a critical testing ground. [7]
Empirical data tests normative theories through multiple, reinforcing pathways without making a direct 'is-ought' leap. [11]
In empirical bioethics research, a central challenge is the is-ought gap—the philosophical problem of deriving normative conclusions ("what ought to be") from purely empirical data ("what is"). This technical support center provides practical guidance for researchers navigating this challenge through three key methodological approaches: consultative, dialogical, and combined methods. These frameworks help integrate empirical findings with ethical reasoning to produce robust, contextually-grounded normative guidance.
The following sections provide troubleshooting guides, frequently asked questions, and practical resources to support scientists, researchers, and drug development professionals in implementing these methodologies effectively within their empirical bioethics research.
Methodological Approaches: Definitions and Comparative Analysis
Defining the Core Methodologies
Consultative Approach: A strategic method used in client interactions where individuals engage in active listening and dialogue to understand needs and offer tailored solutions. This approach fosters trust, builds long-term relationships, and leads to more effective and personalized outcomes by focusing on collaboration and understanding [65]. In empirical bioethics, this involves actively seeking and considering opinions, feedback, and suggestions of stakeholders affected by bioethical decisions [65].
Dialogical Approach: An interpretative methodology that analyzes spoken or written utterances or actions for their embedded communicative significance based on the theory of dialogism [66]. This approach assumes human communication entails the interaction of diverse perspectives and is embedded in a socio-historical context, with meaning potentially differing for various participants [66]. It examines how participants orient to each other's orientations and how multiple voices (multivoicedness) manifest in communication.
Combined Methodological Approaches: Often implemented through mixed methods research, these designs strategically integrate quantitative and qualitative research methods to draw on the strengths of each [67] [68]. This integration facilitates a more comprehensive understanding of research issues through complementary data that offsets the limitations of exclusively quantitative or qualitative approaches [68].
Comparative Analysis of Methodological Features
Table 1: Key Characteristics of Consultative, Dialogical, and Combined Approaches
| Feature | Consultative Approach | Dialogical Approach | Combined Methods |
|---|---|---|---|
| Primary Focus | Understanding stakeholder needs to offer tailored solutions [65] | Analyzing communicative significance in utterances and actions [66] | Integrating qualitative and quantitative data for comprehensive insights [67] |
| Theoretical Foundations | Business consulting, stakeholder theory | Bakhtinian dialogism, Mead's symbolic interactionism [66] | Pragmatism, multiple paradigms |
| Role in Addressing Is-Ought Gap | Gathers stakeholder perspectives to inform normative conclusions [11] | Reveals multiple moral perspectives through discourse analysis | Provides methodological triangulation to bridge factual and normative claims [67] |
| Data Collection Methods | Structured meetings, surveys, focus groups [65] | Analysis of conversations, texts, interactions [66] | Simultaneous or sequential qualitative and quantitative data collection [67] |
| Analytical Emphasis | Problem-solving through collaborative solution development [65] | Understanding multiple voices, perspectives, and their interactions [66] | Integration of different data types to produce robust findings [68] |
| Outcome Orientation | Practical, actionable solutions tailored to specific contexts [65] | Thick description of moral perspectives and their relationships | Contextualized generalizable knowledge [67] |
Methodological Positioning in Empirical Bioethics Research
Table 2: Application of Methodologies to Empirical Bioethics Research
| Research Aspect | Consultative | Dialogical | Combined Methods |
|---|---|---|---|
| Addressing Is-Ought Gap | Uses stakeholder input to ground normative claims in lived experience [11] | Examines how moral positions are constructed through discourse | Employs triangulation to validate normative interpretations [67] |
| Epistemological Stance | Practical wisdom through engagement | Constructed knowledge through dialogue | Pragmatic knowledge through multiple perspectives |
| Primary Strengths | Builds trust and stakeholder buy-in for ethical recommendations [65] | Reveals implicit normativity in practices and discourse [66] | Offsets limitations of single-method designs [68] |
| Common Challenges | Potential delays in decision-making from process management [65] | Complexity in analyzing multiple perspectives and voices | Significant workload and potential conflicting results [67] |
| Appropriate Research Questions | "How can we develop ethically grounded policies that address stakeholder concerns?" | "How do different participants construct moral positions in healthcare discourse?" | "How can we both generalize and contextualize findings about ethical dilemmas?" |
Technical Support: Troubleshooting Guides and FAQs
Methodological Selection and Implementation
Q: How do I select the most appropriate methodological approach for my empirical bioethics study?
A: Your selection should align with your research questions, epistemological commitments, and the kind of normative conclusions you wish to generate [69]. Consider these factors:
- For research needing diverse stakeholder input to develop contextually appropriate normative guidance, the consultative approach offers structured processes for engagement [65].
- For studies examining how moral positions are constructed in discourse or navigating disagreements among stakeholders, the dialogical approach provides appropriate analytical tools [66].
- When seeking both generalizable patterns and contextual depth, combined mixed methods designs are particularly valuable [67].
Begin by explicitly articulating what kinds of normative claims you want to make and how you intend to justify them, then select methodologies that align with these goals [69].
Q: What are effective strategies for managing the significant workload of combined methodological approaches?
A: Mixed methods research is notoriously labor-intensive [67]. Consider these practical strategies:
- Implement an embedded design where one type of data plays a secondary role to the primary methodology, conserving resources while maintaining integration benefits [67].
- Utilize interdisciplinary teams rather than working individually to distribute the methodological expertise required [67].
- Limit scope strategically by focusing integration efforts on the most critical research questions rather than attempting comprehensive data combination.
Data Collection and Integration Challenges
Q: How can I effectively integrate qualitative and quantitative data when they produce conflicting results about an ethical issue?
A: Conflicting results present analytical challenges but also opportunities for deeper insight [67]. Consider these approaches:
- Return to stakeholders through additional consultative engagement to explore why discrepancies might exist between different data types.
- Employ dialogical analysis to examine how different methodologies might be capturing different aspects of a complex ethical phenomenon.
- Explicitly document and analyze the conflicts in your reporting, treating them as findings rather than failures, as they may reveal important tensions in the ethical landscape.
Q: What specific techniques help uncover unstated or implicit stakeholder values in consultative approaches?
A: Effective discovery requires more than simply asking direct questions [70]:
- Use scenario-based discussions that allow stakeholders to respond to concrete situations rather than abstract principles.
- Implement iterative questioning techniques that progressively deepen exploration of initial responses.
- Pay careful attention to disconnects between stated priorities and decision-making behaviors, which often reveal implicit value structures.
Addressing the Is-Ought Gap in Practice
Q: What practical steps can I take to explicitly address the is-ought gap when drawing normative conclusions from empirical data?
A: Researchers report that the is-ought gap should not be considered an absolute barrier but rather a warning sign to critically reflect on normative implications [11]. Implement these practices:
- Maintain transparency by explicitly documenting how you move from empirical findings to normative recommendations in your analytical process.
- Use intermediate reasoning principles that help bridge empirical observations and normative claims, making your logical pathway visible.
- Engage in explicit justification of why certain empirical facts should influence normative frameworks in your specific context.
Q: Which objectives for empirical research in bioethics are most widely accepted by researchers in the field?
A: A qualitative exploration of researchers' views found that understanding the context of a bioethical issue and identifying ethical issues in practice received unanimous agreement [11]. The most contested objectives were striving to draw normative recommendations and developing and justifying moral principles [11]. This suggests that while empirical research is widely valued for descriptive and contextual work, its role in direct norm-generation remains debated.
Experimental Protocols and Workflows
Standardized Protocol for Consultative Engagement in Bioethics
Objective: To systematically gather and integrate stakeholder perspectives to inform ethical analysis.
Materials Needed:
- Stakeholder identification matrix
- Interview/focus group protocols
- Recording and transcription equipment
- Qualitative data analysis software
- Ethical framework mapping template
Procedure:
- Stakeholder Identification: Identify all parties impacted by or having influence over the bioethical issue [65].
- Engagement Design: Select appropriate consultative methods (surveys, interviews, focus groups) based on research questions and stakeholder characteristics [65].
- Data Collection: Conduct engagements using semi-structured approaches that balance consistency with flexibility.
- Data Analysis: Transcribe and code responses, identifying key themes, values, and concerns.
- Integration with Ethical Analysis: Map stakeholder input against relevant ethical frameworks and principles.
- Solution Development: Collaborate with stakeholders to develop ethically grounded approaches that incorporate their perspectives.
Troubleshooting Notes:
- If stakeholders express reluctance to share perspectives, create safer environments by using neutral third-party facilitators.
- If conflicting stakeholder values emerge, employ dialogical techniques to foster mutual understanding before seeking resolution.
Methodological Workflow Visualization
Diagram 1: Methodological Workflow for Empirical Bioethics
Data Integration Protocol for Combined Methods
Objective: To systematically integrate qualitative and quantitative data to address bioethical questions.
Materials Needed:
- Quantitative data collection instruments
- Qualitative data collection protocols
- Data management system
- Integration matrix template
- Analytical triangulation framework
Procedure:
- Design Phase: Select appropriate mixed methods design (convergent, explanatory sequential, exploratory sequential, or embedded) based on research questions [67].
- Simultaneous Data Collection: Gather both quantitative and qualitative data according to their respective methodological standards.
- Preliminary Analysis: Analyze each dataset separately using appropriate techniques.
- Data Integration: Use joint displays, triangulation protocols, or following a thread techniques to identify points of convergence and divergence.
- Interpretation: Develop meta-inferences that draw on both data types to create comprehensive understanding.
- Normative Analysis: Use integrated findings to inform ethical analysis while explicitly addressing the is-ought gap.
Troubleshooting Notes:
- If quantitative and qualitative data conflict, return to field to collect additional data or re-examine analytical assumptions.
- If integration proves conceptually challenging, use visual mapping techniques to identify relationships between different data types.
Research Reagent Solutions for Methodological Implementation
Table 3: Essential Methodological Resources for Empirical Bioethics Research
| Resource Category | Specific Tools & Techniques | Primary Function | Application Context |
|---|---|---|---|
| Stakeholder Engagement | Focus groups, structured interviews, Delphi techniques [65] | Gather diverse perspectives on ethical issues | Consultative approach; identifying ethical issues in practice [11] |
| Dialogical Analysis | Conversation analysis, discourse analysis, narrative analysis [66] | Examine how ethical positions are constructed in language | Dialogical approach; understanding moral reasoning patterns |
| Data Integration | Joint displays, triangulation protocols, following a thread [67] | Combine qualitative and quantitative insights | Combined methods; developing comprehensive understanding |
| Ethical Framework Analysis | Principle-based analysis, casuistry, ethics assessment tools | Structure normative analysis of empirical findings | All approaches; moving from facts to norms while addressing is-ought gap |
| Mixed Methods Designs | Convergent parallel, explanatory sequential, exploratory sequential, embedded [67] | Provide structure for combining methodological approaches | Combined methods; achieving both generalizability and contextual depth |
Visualizing Methodological Integration Pathways
Diagram 2: Methodological Integration Pathways
Conclusion
Successfully addressing the is-ought gap in empirical bioethics requires moving beyond viewing Hume's Law as an insurmountable barrier and instead adopting sophisticated methodological frameworks that acknowledge the necessary bridge between facts and values. The most effective approaches combine philosophical rigor with empirical investigation through methods like reflective equilibrium, dialogical ethics, and symbiotic empirical ethics, while maintaining clear-eyed awareness of implementation challenges. Future progress in biomedical and clinical research depends on embracing interdisciplinary collaboration, where normative expertise guides the integration of empirical data to develop ethically sound recommendations that are both philosophically justified and practically feasible. By adopting these validated approaches, researchers can ensure their empirical bioethics work makes meaningful contributions to both ethical theory and healthcare practice.
References
- 1. Is–ought problem [https://en.wikipedia.org/wiki/Is%E2%80%93ought_problem]
- 2. Is Hume's Law a valid argument against empirical bioethics? [https://pmc.ncbi.nlm.nih.gov/articles/PMC12053791/]
- 3. Is Hume's Law a valid argument against empirical bioethics? [https://pubmed.ncbi.nlm.nih.gov/39865433/]
- 4. WHAT CAN HISTORY DO FOR BIOETHICS? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3654172/]
- 5. Is-Ought Gap: From Facts to Values - Academy 4SC [https://learn.academy4sc.org/video/is-ought-gap-from-facts-to-values/]
- 6. Acceptable objectives of empirical research in bioethics [https://pmc.ncbi.nlm.nih.gov/articles/PMC9794471/]
- 7. The “Ought-Is” Problem: An Implementation Science ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7164659/]
- 8. Naturalistic Fallacy - (Intro to Philosophy) [https://fiveable.me/key-terms/intro-philosophy/naturalistic-fallacy]
- 9. 8.1 The Fact-Value Distinction - Introduction to Philosophy [https://openstax.org/books/introduction-philosophy/pages/8-1-the-fact-value-distinction]
- 10. Fact–value distinction [https://en.wikipedia.org/wiki/Fact%E2%80%93value_distinction]
- 11. Acceptable objectives of empirical research in bioethics [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-022-00845-1]
- 12. The Vagueness of Integrating the Empirical and the Normative [https://pmc.ncbi.nlm.nih.gov/articles/PMC11288993/]
- 13. Ethical issues in the conduct of empirical bioethics research [https://aabhlconference.com/4743/]
- 14. The Relevance of Empirical Research in Bioethics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2632190/]
- 15. Mapping, framing, shaping: a framework for empirical ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-019-0428-0]
- 16. The Role of Empirical Research in Bioethics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2826359/]
- 17. The is and ought of the Ethics of Neuroenhancement [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2015.01998/full]
- 18. A Platform to Develop and Apply Digital Methods for Empirical ... [https://formative.jmir.org/2022/5/e28558/]
- 19. A bioassay method validation framework for laboratory and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10540336/]
- 20. Cognitivism (ethics) [https://en.wikipedia.org/wiki/Cognitivism_(ethics)]
- 21. Moral Cognitivism vs. Non-Cognitivism [https://plato.stanford.edu/entries/moral-cognitivism/]
- 22. Bioethics Tools [https://depts.washington.edu/bhdept/ethics-medicine/bioethics-tools]
- 23. Reflective equilibrium [https://en.wikipedia.org/wiki/Reflective_equilibrium]
- 24. Reflective Equilibrium - Stanford Encyclopedia of Philosophy [https://plato.stanford.edu/entries/reflective-equilibrium/]
- 25. Two Methods for Applying Ethics - Office of the Provost [https://www.smu.edu/provost/ethics/resources/ethicstoolbox/puttingethicsintopractice/twomethodsforapplyingethics]
- 26. Empirical ethics as dialogical practice [https://pubmed.ncbi.nlm.nih.gov/19338524/]
- 27. Symbiotic empirical ethics: a practical methodology [https://pubmed.ncbi.nlm.nih.gov/21039690/]
- 28. The normative background of empirical-ethical research [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-015-0016-x]
- 29. Using symbiotic empirical ethics to explore the significance of ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-024-01053-9]
- 30. Empirical studies on how ethical recommendations are ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9835353/]
- 31. The use of implementation science theories, models, and ... [https://health-policy-systems.biomedcentral.com/articles/10.1186/s12961-024-01102-0]
- 32. Why the Pharmaceutical Industry Needs Implementation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12126355/]
- 33. PPD Evidera Implementation Science [https://www.ppd.com/our-solutions/clinical/real-world-evidence/implementation-science/]
- 34. How to create a Troubleshooting Guide for your business [https://document360.com/blog/troubleshooting-guide/]
- 35. Troubleshooting Guide: Definition & Examples [https://www.bolddesk.com/blogs/troubleshooting-guide]
- 36. How to Create a Troubleshooting Guide [+ Free Template] [https://scribe.com/library/troubleshooting-guide]
- 37. Using symbiotic empirical ethics to explore the significance of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11131179/]
- 38. Perceptions of COVID-19 patients in the use of bioethical ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-024-01009-z]
- 39. The Vagueness of Integrating the Empirical and the Normative... [https://pubmed.ncbi.nlm.nih.gov/37938498/]
- 40. The Consolidated Framework for Implementation Research ... [https://cfirguide.org/]
- 41. The updated Consolidated Framework for Implementation ... [https://implementationscience.biomedcentral.com/articles/10.1186/s13012-022-01245-0]
- 42. The Consolidated Framework for Implementation Research ... [https://implementationscience.biomedcentral.com/articles/10.1186/s13012-025-01450-7]
- 43. Exploring barriers to and facilitators of the implementation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10183114/]
- 44. CFIR simplified: Pragmatic application of and adaptations ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6971122/]
- 45. Using CFIR framework for understanding barriers and ... [https://www.frontiersin.org/journals/health-services/articles/10.3389/frhs.2023.1294176/full]
- 46. Overview [https://cfirguide.org/evaluation-design/overview/]
- 47. Fallacious, misleading and unhelpful: The case for removing... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9321889/]
- 48. Developing new ways to listen: the value of narrative approaches in... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-021-00691-7]
- 49. Strategies for Successful Interdisciplinary Collaborations [https://etd.gatech.edu/2023/11/22/strategies-for-successful-interdisciplinary-collaborations/]
- 50. The Case for Understanding Interdisciplinary Relationships ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10262946/]
- 51. Troubleshooting Protocols - Biological Sciences: Summer ... [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 52. Teaching troubleshooting skills to graduate students - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11407763/]
- 53. The risk of normative bias in reporting empirical research [https://link.springer.com/article/10.1007/s11017-023-09639-x]
- 54. Weights of survey data [https://dmeg.cessda.eu/Data-Management-Expert-Guide/3.-Process/Weights-of-survey-data]
- 55. Acceptable objectives of empirical research in bioethics [https://pubmed.ncbi.nlm.nih.gov/36575520/]
- 56. What Counts as Empirical Research in Bioethics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2838431/]
- 57. Researchers' Views on Doing Empirical Bioethics [https://link.springer.com/article/10.1007/s11673-023-10286-z]
- 58. Design Bioethics: A Theoretical Framework and Argument for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8676709/]
- 59. Ethical Issues in Pediatric Drug Studies - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK202037/]
- 60. Using surveys with experimental designs in bioethics and ... [https://smdm.org/hub/page/using-surveys-with-experimental-designs-in-bioethics-and-health-policy-rese]
- 61. Mapping, framing, shaping: a framework for empirical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6880497/]
- 62. Standards of practice in empirical bioethics research [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-018-0304-3]
- 63. Empirical Research: Defining, Identifying, & Finding [https://libguides.memphis.edu/empirical-research/identifying/discussion]
- 64. Toward large reasoning models: A survey of reinforced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12546433/]
- 65. Consultative Approach: Meaning & Definition | Vaia [https://www.vaia.com/en-us/explanations/business-studies/sales-in-business/consultative-approach/]
- 66. Dialogical analysis [https://en.wikipedia.org/wiki/Dialogical_analysis]
- 67. Mixed Methods Research | Definition, Guide & Examples [https://www.scribbr.com/methodology/mixed-methods-research/]
- 68. Mixed Methods Research [https://catalyst.harvard.edu/community-engagement/mmr/]
- 69. A systematic review of empirical bioethics methodologies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4357052/]
- 70. Behavioral Interview Questions for Consultative Approach [https://yardstick.team/interview-questions/consultative-approach]