Bridging the Gap: A Practical Framework for Integrating Normative and Empirical Approaches in Bioethics
This article provides a comprehensive guide for researchers and drug development professionals on integrating normative and empirical methodologies in bioethics.
Bridging the Gap: A Practical Framework for Integrating Normative and Empirical Approaches in Bioethics
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on integrating normative and empirical methodologies in bioethics. It explores the foundational principles of this interdisciplinary field, critiques prevalent methodological challenges like the 'vagueness' of integration, and presents actionable strategies for selecting ethical frameworks and designing robust studies. By addressing key hurdles and offering comparative analysis of different approaches, the content aims to equip scientists with the tools to conduct ethically sound, methodologically rigorous, and socially relevant research in the biopharmaceutical sector and beyond.
The Foundations of Empirical Bioethics: Defining the Normative-Empirical Nexus
Empirical bioethics is an interdisciplinary research field that seeks to integrate empirical findings from the social sciences with normative philosophical analysis to address bioethical issues [1]. The growth of this field is largely attributed to a dissatisfaction with purely philosophical approaches, which were perceived as insufficient to address the complex reality of human practices in healthcare and biomedical research [1]. This integrative discipline fundamentally grapples with a central philosophical challenge: how can descriptive facts about the world (the "is") inform prescriptive ethical recommendations (the "ought")? [2] [3]. Empirical bioethics does not claim that empirical data alone can determine what is right or wrong, but rather that such data provides essential context, identifies practical challenges, and tests the feasibility of ethical ideals, thereby enriching normative analysis [4] [3].
Defining the Terrain: What Constitutes Empirical Bioethics?
Core Characteristics and Aims
Empirical bioethics is characterized by its commitment to interdisciplinary work. It centers on the integration of empirical research—which can be qualitative or quantitative—with ethical argument to arrive at normative conclusions [1]. The ultimate aim of this endeavor is not empirical research for its own sake, but to produce knowledge that can inform and improve real-world practices and policies [2] [5].
A key insight from the field is that ethically relevant empirical data are ubiquitous, often appearing in publications outside traditional ethics journals. Seminal studies that have influenced bioethical norms, such as analyses of tube feeding in advanced dementia or placebo use in antidepressant trials, were frequently conducted by researchers who do not identify as bioethicists and published in clinical journals without ethics-specific keywords [4]. This underscores the importance for bioethicists to engage with literature beyond their immediate discipline.
A Framework for Empirical Bioethics Research
One influential framework conceptualizes empirical bioethics research as comprising three hierarchical phases, conveyed through the metaphor of landscaping [5]:
Table 1: The Mapping-Framing-Shaping Framework for Empirical Bioethics Research
| Phase | Primary Aim | Typical Activities | Key Output |
|---|---|---|---|
| Mapping | Survey the existing terrain | Literature reviews; analysis of previous scholarship and data | Understanding of the "state of the art" and identification of knowledge gaps |
| Framing | Explore specific areas in depth | Qualitative or quantitative research with stakeholders to understand lived experiences | Fine-grained understanding of how issues are experienced and perceived |
| Shaping | Propose normative recommendations | Integrative analysis using a bridging methodology | Ethically robust recommendations for practice or policy |
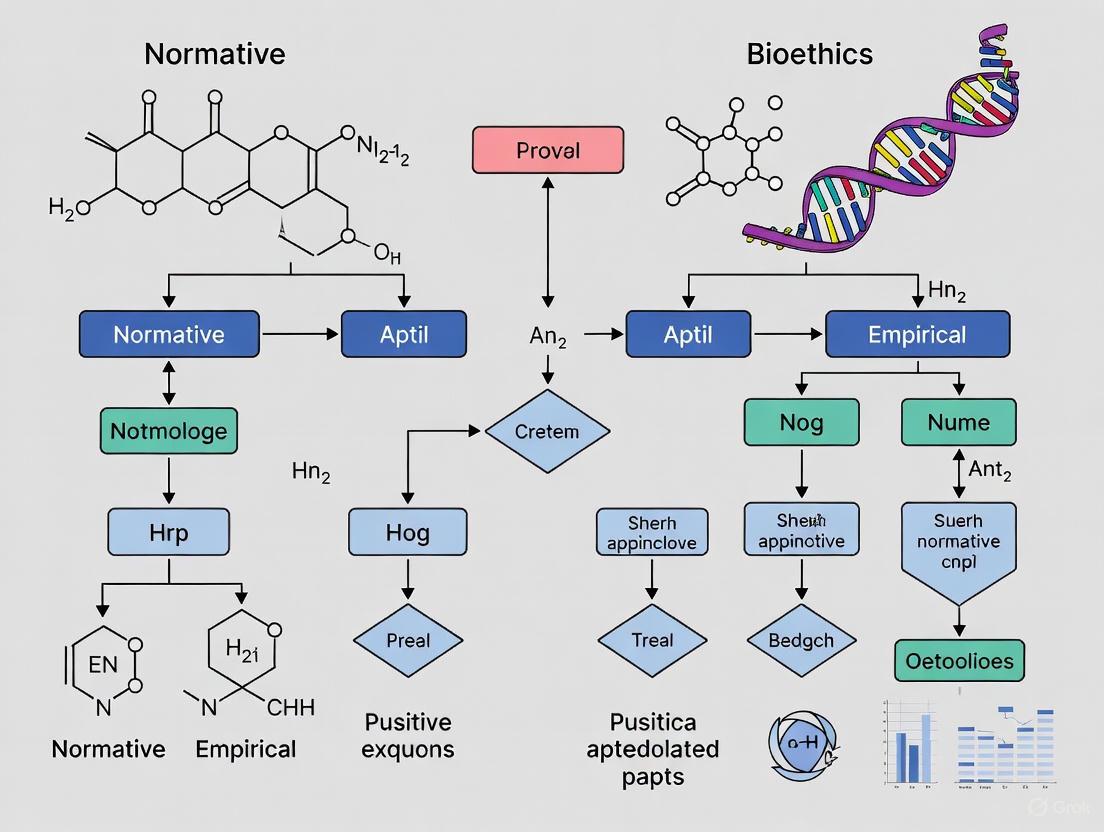
Figure 1: The three-phase empirical bioethics research workflow, highlighting integration as the definitive step.
The critical element that distinguishes empirical bioethics from merely conducting empirical research on an ethics-adjacent topic is the integration step, where methodology is explicitly used to bridge the empirical findings with normative analysis [5]. This integration is what allows the researcher to move from description to prescription.
Methodological Approaches and Integration Strategies
Classifying Empirical Research in Bioethics
Empirical research can inform bioethics at different levels. One prominent classification system identifies four hierarchical categories, from descriptive to normative [2]:
Table 2: A Hierarchical Classification of Empirical Research in Bioethics
| Category | Primary Question | Example | Normative Ambition |
|---|---|---|---|
| Lay of the Land | What are current practices, opinions, or beliefs? | Surveys of end-of-life care preferences among patients and providers [2] | Descriptive; sets the stage for further inquiry |
| Ideal vs. Reality | To what extent does practice match ethical ideals? | Studies documenting racial disparities in healthcare delivery [2] | Identifies ethical failures in practice |
| Improving Care | How can we bring practice closer to ethical ideals? | Interventions to improve informed consent comprehension [3] | Develops and tests practical interventions |
| Changing Ethical Norms | Should our ethical norms evolve based on evidence? | Using data on outcomes of tube feeding in dementia to reconsider norms [4] | Aims to refine or revise ethical norms |
Methodologies for Integration
A systematic review has identified at least 32 distinct methodologies for integrating empirical research with normative analysis [1]. These can be broadly categorized into three approaches:
Consultative Approaches: The researcher acts as an external thinker who independently analyzes empirical data and ethical theory to develop a normative conclusion. The most prominent example is reflective equilibrium (or "wide reflective equilibrium"), a process where the researcher moves back-and-forth between ethical principles, considered moral judgments, and empirical facts until a state of coherence ("equilibrium") is reached [1].
Dialogical Approaches: These methods rely on structured dialogue between stakeholders (including researchers, participants, and other relevant actors) to reach a shared understanding and normative conclusion. In these approaches, the ethicist often acts as a facilitator rather than the sole arbiter of the ethical analysis [1].
Combined Approaches: Some methodologies blend elements of both consultative and dialogical approaches, such as hermeneutical methods that interpret the meaning of practices through both engagement and reflection [1].
Despite this diversity, researchers in the field often report that the integration process remains somewhat vague in practice, representing both a strength (flexibility) and a weakness (potential obscurity) [1].
Experimental Protocols in Empirical Bioethics
A Generic Protocol for Qualitative Framing Studies
Objective: To explore and understand how a specific bioethical issue is experienced and framed by relevant stakeholders.
Methodology: This protocol employs a qualitative exploratory design, typically using semi-structured interviews or focus groups [6].
Table 3: Essential Research Reagents for Qualitative Framing Studies
| Item Category | Specific Examples | Function in the Research Process |
|---|---|---|
| Participant Recruitment | Systematic sampling from clinical populations; purposive sampling of experts | Ensures the inclusion of relevant perspectives and experiences |
| Data Collection Tools | Semi-structured interview guide; audio recording equipment; secure storage | Facilitates consistent, in-depth data collection while protecting participant confidentiality |
| Data Management | Qualitative data analysis software (e.g., MAXQDA, NVivo); transcription services | Enables systematic organization, coding, and analysis of complex qualitative data |
| Analytical Framework | Thematic analysis guide (e.g., Braun & Clarke, 2006) [1]; codebook | Provides a structured yet flexible method for identifying, analyzing, and reporting patterns (themes) within the data |
Procedure:
- Ethics Approval: Obtain approval from an accredited Research Ethics Committee or Institutional Review Board.
- Sampling: Identify and recruit a purposive sample of participants who have direct experience with the bioethical issue under investigation. Sample size is typically determined by the principle of saturation, where new data no longer yields new thematic insights [6].
- Data Collection: Conduct individual interviews or focus groups using a semi-structured guide. All sessions should be audio-recorded and transcribed verbatim to ensure accuracy.
- Data Analysis: Employ thematic analysis, which involves (a) familiarization with the data, (b) generating initial codes, (c) searching for themes, (d) reviewing themes, (e) defining and naming themes, and (f) producing the report [1] [7].
- Integration: The empirical findings (themes) are then integrated with normative analysis using a chosen methodology (e.g., reflective equilibrium) to develop ethical recommendations.
A Protocol for a "Changing Ethical Norms" Study
Objective: To use a body of empirical evidence to form the basis of an argument for refining or changing an established ethical norm.
Methodology: This approach involves a comprehensive evidence synthesis and normative analysis, often building on multiple existing studies rather than a single primary investigation [2] [8].
Procedure:
- Evidence Mapping: Conduct a systematic review of the literature to gather all relevant empirical data related to the ethical norm in question (e.g., clinical outcomes, patient experiences, stakeholder perspectives).
- Critical Appraisal: Assess the quality, consistency, and applicability of the gathered evidence. A single study is rarely sufficient to warrant a change in ethical norms; a body of credible evidence is required [8].
- Identify Normative Implications: Analyze how the empirical evidence challenges, supports, or complicates the assumptions underlying the current ethical norm. This involves testing whether what is "ought" is, in fact, possible ("ought implies can") [9] or examining the consequences of adhering to a norm in practice [3].
- Construct a Normative Argument: Develop a reasoned argument for how the ethical norm should be refined, contextualized, or changed in light of the evidence. This is not a direct derivation from facts to values, but a structured justification that gives appropriate weight to both empirical findings and ethical principles [2] [8].
- Propose Refined Norms or Applications: Articulate the proposed change to the norm or its application in specific contexts, clearly outlining the ethical reasoning that bridges the empirical evidence and the normative conclusion.
Current Trends and Digital Innovations
The field of empirical bioethics is increasingly embracing digital methods, giving rise to "digital bioethics." This involves using online and digital technologies to collect and analyze research data, such as analyzing discussions on social media platforms to understand public perspectives on emerging ethical issues [10].
These novel approaches leverage computational capabilities, including natural language processing (NLP) and machine learning, to handle large datasets. However, they also introduce a dependence on technical skills not typically part of a bioethicist's training. In response, platform prototypes are being developed to empower researchers without advanced programming expertise to leverage these digital methods, for instance, by providing modular components for data collection, filtering, and analysis that can be configured through a graphical interface [10]. This innovation aims to make digital bioethics more accessible and to foster methodological development.
Empirical bioethics represents a vital maturation of bioethical inquiry, moving beyond abstract theorizing to engage seriously with the realities of clinical practice and human experience. Its core contribution lies in its integrative imperative—the insistence that robust ethical analysis requires both empirical vigilance and normative sophistication. By systematically mapping the terrain, framing issues through the perspectives of those most affected, and leveraging methodological rigor to shape recommendations, empirical bioethics provides a powerful framework for addressing the most pressing challenges in healthcare and biomedical research. For researchers, scientists, and drug development professionals, engaging with this approach is not merely an academic exercise but a practical necessity for developing ethically sound and practically feasible policies and practices.
Integrating normative and empirical approaches represents a significant methodological frontier in contemporary bioethics research. This integration, however, is often characterized by substantial vagueness and a lack of clarity in practical execution. This article provides structured application notes and protocols to guide researchers in systematically disentangling and then purposefully reintegrating empirical data with normative analysis. By synthesizing established methodologies such as symbiotic empirical ethics, reflective equilibrium, and dialogical empirical ethics, we present a structured framework to enhance methodological rigor. The protocols include detailed workflows, reagent solutions for interdisciplinary research, and visualization tools designed to help researchers, scientists, and drug development professionals navigate the complexities of empirical bioethics research, ultimately leading to more transparent and defensible normative conclusions.
Empirical bioethics is an interdisciplinary field that centers on the integration of empirical findings with normative, philosophical analysis [1]. The growth of this field is largely attributed to a dissatisfaction with purely philosophical approaches, which are often perceived as insufficient for addressing the complex, real-world nuances of bioethical issues [1]. An empirically informed bioethics is better suited to deal with the complexity of human practices. Despite a consensus on the relevance of empirical research to bioethical argument, the process of integration remains challenging [1]. A systematic review has identified at least thirty-two distinct methodologies for integration, revealing a field rich with innovation but also struggling with uncertainty about the particular aims, content, and domain of application for these methods [1]. Many existing methodologies risk being "frustratingly vague and insufficiently determinate in practical contexts" [1]. This article aims to address this vagueness by providing clear, actionable protocols and tools for researchers seeking to untangle and then meaningfully weave together the normative and empirical threads of their work.
Core Methodologies in Empirical Bioethics
The first step in untangling normative and empirical components is to understand the primary methodological frameworks available. The choice of framework dictates how empirical data and ethical analysis will interact throughout the research process.
Table 1: Core Methodologies for Integrating Normative and Empirical Analysis
| Methodology | Key Feature | Process of Integration | Primary Application Context |
|---|---|---|---|
| Reflective Equilibrium [1] | A back-and-forth, coherence-seeking method performed by the researcher. | The researcher ("the thinker") iteratively revises ethical principles, empirical data, and considered judgements until moral coherence ("equilibrium") is achieved. | Consultative research where the researcher acts as an external analyst. |
| Symbiotic Empirical Ethics [11] | A naturalist approach viewing ethical theory and practice as symbiotically related. | A structured five-step process moving from empirical data to the refinement of ethical theory, ensuring practice informs theory and vice-versa. | Research aiming to develop or refine ethical theory based on concrete practical findings. |
| Dialogical Empirical Ethics [1] | Relies on stakeholder dialogue to reach a shared, normative understanding. | Collaboration and discourse between researchers, participants, and other stakeholders are the primary mechanism for developing normative conclusions. | Participatory action research and contexts where stakeholder buy-in is critical. |
| Ground Moral Analysis [1] | Integrates empirical data collection with normative analysis from the outset. | The normative and empirical are intertwined from the start of the research project, often using a grounded theory approach. | Exploratory research where ethical concepts are expected to emerge from the data. |
Application Protocol: Symbiotic Empirical Ethics
The symbiotic empirical ethics methodology, as developed by Frith, provides a structured, five-step protocol for moving from empirical findings to normative suggestions [11]. This approach is particularly valuable for making explicit the process of developing ethical theory based on practical data.
Detailed Experimental Protocol
Objective: To generate normative ethical solutions or theory refinements grounded in empirical qualitative data concerning a specific ethical challenge in healthcare or research settings.
Step-by-Step Workflow:
- Identify a Practice-Based Problem: Begin with a concrete ethical problem or challenge observed in clinical or research practice. For example, the Reset Ethics project began with the problem of how to ethically integrate Infection Prevention and Control (IPC) measures into routine maternity and paediatric services during the COVID-19 pandemic [11].
- Gather Qualitative Empirical Data: Collect rich, contextual data on the identified problem. This typically involves qualitative methods such as:
- Semi-structured interviews with key stakeholders (e.g., healthcare professionals, patients, administrators).
- Focus group discussions to explore shared and divergent experiences.
- The data should capture the lived experiences and ethical challenges of those directly involved.
- Conduct Thematic Analysis: Analyze the qualitative data using standard thematic analysis techniques. This involves:
- Transcribing interviews and focus groups verbatim.
- Systematically coding the data to identify recurring patterns and themes.
- Developing overarching themes that capture the core ethical tensions or insights present in the data. In the Reset project, a key theme was that IPC measures were experienced as "harmful barriers to the experience of receiving and offering care" [11].
- Analyze Themes Using Ethical Theory: This is the core integrative step. Take the emergent empirical themes and analyze them using the concepts and frameworks of relevant ethical theories. The Reset project, for instance, used relational ethical theory to analyze its findings, contrasting the relational reality of care with the atomistic, individual-patient focus of some clinical ethics frameworks [11].
- Refine/Develop Ethical Theory and Generate Normative Suggestions: Based on the analysis, refine the existing ethical theory or develop new normative suggestions that are informed by the empirical data. The conclusion of the Reset project was the normative suggestion that "clinical ethics should explicitly attend to the importance of relationships in clinical practice" and that organizational decision-making should account for the moral significance of caring relationships [11].
Research Reagent Solutions
In empirical bioethics, the "research reagents" are the conceptual tools and frameworks that enable the integration of data and theory.
Table 2: Essential Research Reagent Solutions for Empirical Bioethics
| Research 'Reagent' | Function/Explanation | Example Use Case |
|---|---|---|
| Semi-Structured Interview Guides | To collect rich, contextual qualitative data on lived experiences of ethical dilemmas while ensuring key topics are covered. | Exploring healthcare professionals' challenges in balancing visitor restrictions with family-centered care in paediatrics [11]. |
| Qualitative Data Analysis Software (e.g., MAXQDA) | To assist in the systematic management, coding, and thematic analysis of qualitative data (interview/focus group transcripts) [1]. | Identifying recurring themes and patterns across a large dataset of interviews, such as the theme of "relational care as an ethical imperative." |
| Established Ethical Frameworks (e.g., Principlism) | To provide the initial normative concepts and vocabulary for analyzing the empirical data. | Using the four principles (autonomy, beneficence, non-maleficence, justice) as a lens to code ethical conflicts described by participants. |
| Relational Ethical Theory | A theoretical framework that posits individuals are constituted by their networks of relationships, shifting the ethical focus from the atomistic individual [11]. | Arguing for a shift in clinical ethics to acknowledge the "patient-in-relationships" based on data showing the importance of relational interactions in care. |
| Reflective Equilibrium Framework | A methodological tool for testing and achieving coherence between ethical principles, empirical facts, and considered moral judgements [1]. | Revising one's initial normative position on visitor policies after being confronted with empirical data on the negative impacts of isolation. |
Data Presentation and Analysis Protocols
Clear data presentation is crucial for demonstrating the validity of the integration process. This involves both summarizing quantitative or categorical data and transparently outlining the analytical steps for qualitative data.
Table 3: Template for Research Protocol Sections as per Adapted SRQR Guidelines for Empirical Bioethics [12]
| Protocol Section | Key Content to Include | Rationale |
|---|---|---|
| Title and Abstract | Clearly describe the nature of the study and its empirical-normative approach. | Allows readers to immediately identify the methodological approach of the paper. |
| Problem Studied | Explain the importance of the problem and summarize the most significant existing literature. | Positions the research within the existing scholarly conversation and justifies its necessity. |
| Research Paradigm | Explicitly state and justify the methodological framework (e.g., qualitative, quantitative, mixed) and the theoretical framework (e.g., principlism, relational ethics) for integration [12]. | Provides critical transparency about the epistemological and normative foundations of the study. |
| Data Collection & Instruments | Detail the procedures and instruments used (e.g., interview guides, questionnaires). | Ensures the reliability and allows for the replication of the empirical component. |
| Data Analysis | For qualitative data, specify in sufficient detail how the data will be analyzed (e.g., thematic analysis). For normative analysis, describe the ethical framework applied. | Demonstrates methodological rigor in both the empirical and normative wings of the research. |
| Integration Method | Clearly articulate the chosen method for integration (e.g., symbiotic, reflective equilibrium) and justify its selection. Explain how the method was operationalized. | Addresses the core challenge of vagueness by making the integration process transparent and accountable. |
Untangling normative analysis from empirical data is not an end in itself; rather, it is a necessary step towards their more robust and transparent reintegration. By moving away from vague methodological descriptions and adopting structured protocols like the one detailed herein, researchers in bioethics, science, and drug development can significantly enhance the credibility, impact, and practical utility of their work. The explicit use of frameworks such as symbiotic empirical ethics, coupled with clear data presentation and a well-defined "toolkit" of research reagents, provides a roadmap for navigating the complexities of interdisciplinary research. This structured approach ensures that the resulting normative conclusions are not only philosophically sound but also deeply grounded in the empirical realities of practice.
The growing complexity of modern bioethical challenges, particularly in fast-evolving fields like healthcare artificial intelligence (AI) and drug development, has revealed the limitations of isolated research approaches. Purely philosophical methods risk becoming disconnected from the practical realities and complexities of clinical practice, while merely descriptive empirical approaches often fail to deliver the normative guidance needed for ethical decision-making [13] [7]. This protocol outlines the rationale and methodological framework for integrating normative and empirical approaches within bioethics research, providing researchers with structured pathways to produce findings that are both philosophically robust and empirically grounded.
The impetus for integration stems from recognition that ethical principles must be informed by the actual experiences, values, and constraints of stakeholders—including patients, researchers, clinicians, and drug development professionals [14]. Empirical bioethics has emerged precisely from "a dissatisfaction with a purely philosophical approach, perceived as being insufficient to address bioethical issues" and a belief that "an empirically informed bioethics is better suited to deal with the complexity of human practices" [7]. By systematically bridging these traditionally separate domains, researchers can develop ethical frameworks that are simultaneously conceptually sound, practically applicable, and contextually responsive.
Theoretical Foundations and Integration Rationale
Epistemological Underpinnings
Integrated empirical bioethics operates on the premise that ethical analysis gains validity and practical relevance when informed by systematic observation of real-world contexts, practices, and stakeholder perspectives [7]. This approach acknowledges that ethical dilemmas occur within specific socio-technical environments—such as clinical trials, research laboratories, or healthcare delivery systems—where organizational structures, professional norms, and resource constraints significantly shape moral decision-making.
The integration of normative and empirical components follows two primary epistemological pathways:
- Empirically-Informed Normativity: Empirical data about stakeholder experiences, values, and practices informs and shapes the development of ethical principles and recommendations.
- Normatively-Framed Empiricism: Ethical theories and frameworks guide the collection and interpretation of empirical data, ensuring research addresses morally significant questions.
This bidirectional relationship ensures that ethical analysis remains grounded in actual practices while empirical research addresses normatively significant questions [7]. As one study notes, "empirical research in empirical ethics is not an end in itself, but a required step towards a normative conclusion or statement with regard to empirical analysis, leading to a combination of empirical research with ethical analysis and argument" [7].
Comparative Advantages of Integrated Approaches
Table 1: Comparing Research Approaches in Bioethics
| Approach | Key Characteristics | Strengths | Limitations | Suitable Research Questions |
|---|---|---|---|---|
| Purely Philosophical | Deductive reasoning from ethical principles; conceptual analysis; limited empirical data | Conceptual clarity; logical consistency; identifies fundamental principles | May overlook practical constraints; potential disconnect from real-world contexts | Foundational ethical principles; conceptual clarification |
| Purely Descriptive | Observation and description of ethical phenomena; quantitative or qualitative data | Identifies actual practices and attitudes; contextual understanding | Limited normative guidance; descriptive rather than prescriptive | Mapping stakeholder perspectives; describing ethical practices |
| Integrated Empirical-Normative | Combines empirical data with ethical analysis; iterative processes | Contextually sensitive ethical guidance; pragmatic relevance; theoretically informed | Methodological complexity; requires interdisciplinary expertise | Developing practice-grounded ethical guidelines; policy formulation |
Methodological Framework and Integration Protocols
Core Integration Methodologies
Based on analysis of current practices in empirical bioethics, three prominent methodological approaches for integration have emerged, each with distinct procedures and applications [7].
Reflective Equilibrium Protocol
The reflective equilibrium approach, particularly in its "wide" form, involves an iterative process of adjustment between ethical principles, empirical findings, and considered moral judgments [7].
Protocol Steps:
- Initial Positioning: Clearly articulate relevant ethical theories, principles, and preliminary moral intuitions regarding the research question.
- Empirical Data Collection: Gather systematic data through methods appropriate to the research context (e.g., interviews, surveys, observational studies).
- Comparative Analysis: Identify points of coherence and tension between ethical principles, empirical findings, and considered moral judgments.
- Iterative Adjustment: Systematically adjust elements to achieve greater coherence, which may involve:
- Revising ethical principles to better account for empirical realities
- Reinterpreting empirical data through different theoretical lenses
- Modifying initial moral judgments in light of conflicting evidence
- Equilibrium Achievement: Establish a reflective equilibrium where principles, data, and judgments achieve maximal coherence.
- Normative Output: Formulate ethical guidance or recommendations based on the achieved equilibrium.
Application Context: Particularly suitable for research questions where established ethical principles require contextual refinement or when empirical findings challenge conventional moral wisdom.
Embedded Ethics Protocol
The Embedded Ethics approach involves integrating ethicists and social scientists directly into research and development teams, particularly in technology-driven domains like healthcare AI and drug development [14].
Protocol Steps:
- Integration Planning: Identify integration points in the research or development lifecycle where ethical input will be most valuable.
- Team Embedding: Position ethicists/social scientists within research teams with access to meetings, documentation, and decision-making processes.
- Continuous Monitoring: Employ ongoing observation and engagement to identify emerging ethical issues during technology development or research progression.
- Iterative Intervention: Introduce ethical analysis at multiple stages rather than solely as a pre- or post-development evaluation.
- Collaborative Deliberation: Facilitate structured discussions between technical experts and ethics researchers to co-develop solutions.
- Documentation and Reflexivity: Maintain detailed records of ethical issues identified, discussions held, and resolutions reached.
Application Context: Particularly valuable in interdisciplinary health research consortia, AI development projects, and innovative drug development where ethical implications emerge throughout the research process [14].
Dialogical Empirical Ethics Protocol
This approach emphasizes stakeholder engagement and dialogue as the primary mechanism for integrating empirical and normative dimensions [7].
Protocol Steps:
- Stakeholder Mapping: Identify all relevant stakeholders for the ethical issue under investigation.
- Empirical Data Collection: Gather initial data on stakeholder perspectives, experiences, and values through interviews, surveys, or observations.
- Structured Dialogue Facilitation: Organize and facilitate deliberative forums where stakeholders engage with ethical principles and empirical findings.
- Iterative Sense-Making: Support participants in collaboratively working through ethical dilemmas and developing shared understandings.
- Normative Refinement: Translate dialogical outcomes into ethical recommendations or frameworks.
- Validation and Feedback: Circulate findings back to stakeholders for confirmation and further refinement.
Application Context: Particularly appropriate for research questions involving diverse value perspectives, policy development, or community-engaged research.
Methodological Toolbox for Integration
Table 2: Empirical Methods for Integrated Bioethics Research
| Method Category | Specific Methods | Data Generated | Integration Function | Resource Requirements |
|---|---|---|---|---|
| Stakeholder Engagement | Interviews, focus groups, peer-to-peer interviews [14] | Perspectives, values, experiences | Informs ethical analysis with stakeholder viewpoints | Moderate time commitment; ethical approval needed |
| Observational Approaches | Ethnography, participant observation [14] | Contextual practices, organizational cultures | Grounds ethical analysis in actual practices | Significant time investment; researcher training needed |
| Deliberative Methods | Structured workshops, stakeholder dialogues [14] | Reflective judgments, negotiated outcomes | Generates ethical consensus through democratic processes | Facilitation expertise; diverse stakeholder recruitment |
| Analytical Methods | Bias analyses, literature reviews [14] | Systematic identification of ethical issues | Structures ethical assessment using conceptual frameworks | Research expertise; access to literature databases |
Practical Implementation and Research Reagents
Research Reagent Solutions
Table 3: Essential Analytical Tools for Integrated Bioethics Research
| Tool Category | Specific Tools/Platforms | Primary Function | Integration Application | Access Considerations |
|---|---|---|---|---|
| Qualitative Data Analysis | MAXQDA, NVivo [15] | Coding and analysis of textual, audio, visual data | Systematic analysis of interviews, focus groups, documents | Commercial licenses; training required |
| Quantitative Analysis | SPSS, Stata, R [15] [16] | Statistical analysis of numerical data | Analysis of survey data; descriptive and inferential statistics | Various licensing models; R is open-source |
| Mixed Methods Support | MAXQDA 2024 [15] | Integration of qualitative and quantitative data | Combined analysis of diverse data types for richer insights | Commercial license; specialized functionality |
| Data Collection | Qualtrics, LimeSurvey [16] | Survey design and distribution | Efficient gathering of empirical data from multiple participants | Various pricing tiers; cloud-based access |
Integration Workflow Protocol
Application Contexts and Adaptability
The integrated approaches outlined in this protocol have demonstrated particular utility in several bioethics research domains relevant to drug development professionals and health researchers:
Early-Phase Clinical Trials in Oncology
Integrated approaches enable researchers to examine ethical issues surrounding patient participation, informed consent processes, and risk-benefit assessments through combined analysis of stakeholder experiences (empirical) and ethical principles of autonomy, beneficence, and justice (normative) [13].
Artificial Intelligence in Healthcare
The Embedded Ethics approach has proven valuable in identifying and addressing ethical challenges during the development of AI technologies for healthcare, including issues of algorithmic bias, transparency, and accountability [14]. This enables proactive ethical integration rather than post-hoc analysis.
Genomic Research and Polygenic Risk Scores
Integrated methodologies facilitate examination of ethical implications of genetic risk prediction, including issues of privacy, psychological impact, and justice in access to emerging genomic technologies [14].
Implementation Considerations and Limitations
While integrated empirical-normative approaches offer significant advantages, researchers should acknowledge several implementation challenges:
Methodological Competence
Successful integration requires research teams to possess or develop competence in both empirical research methods and ethical analysis. This often necessitates interdisciplinary collaboration or additional training [7].
Resource Allocation
Integrated approaches typically require more time and resources than single-method studies, particularly for processes like reflective equilibrium that involve iterative analysis or Embedded Ethics requiring long-term engagement [14].
Theoretical and Methodological Transparency
Researchers must clearly articulate and justify their chosen integration methodology, as "the indeterminacy of integration methods is a double-edged sword. It allows for flexibility but also risks obscuring a lack of understanding of the theoretical-methodological underpinnings" [7].
Despite these challenges, the rigorous integration of empirical and normative approaches represents a scientifically robust and ethically responsive pathway for addressing complex bioethical challenges in contemporary health research and drug development.
The application of the four cornerstone principles of bioethics—autonomy, beneficence, nonmaleficence, and justice—is undergoing a significant transformation. Contemporary scholarship emphasizes the necessity of integrating traditional normative analysis with empirical research methodologies to address complex challenges in healthcare and biotechnology [17] [12]. This integrated approach strengthens the foundation for ethical decision-making by grounding theoretical principles in observable data concerning human behaviors, values, and systemic interactions. The burgeoning field of empirical bioethics reflects this synthesis, utilizing methods from social sciences to investigate ethical questions within medical practice and research [18] [12]. This document provides application notes and experimental protocols to guide researchers and drug development professionals in operationalizing the four principles within this integrated framework, with particular attention to emerging technologies and cross-cultural contexts.
Core Principles and Their Operationalization
The Principle of Autonomy
Theoretical Foundation: The principle of autonomy recognizes the intrinsic right of individuals to self-determination and to make decisions about their own lives and bodies without external coercion [19]. This principle provides the ethical foundation for informed consent, truth-telling, and confidentiality in clinical practice and research [19]. Its philosophical roots are often traced to Kant and Mill, emphasizing the unconditional worth of individuals and their capacity for rational decision-making [19].
Applied Contexts and Challenges:
- Informed Consent Protocols: Valid consent requires that the patient or research subject is competent, receives full disclosure, comprehends the information, acts voluntarily, and provides consent [19]. These requirements, while foundational in Western bioethics, may encounter resistance or require adaptation in non-Western cultures that emphasize family-centered or community-centered decision-making [19] [20].
- Relational Autonomy: Critics of a strictly individualistic interpretation of autonomy propose a broader concept of "relational autonomy," acknowledging that decisions are shaped by social relationships, culture, gender, and ethnicity [19].
- Emerging Technology Interface: The digital transformation of healthcare introduces new dimensions to autonomy, involving consent for the use of digital tools, data sharing, and AI-supported care [17]. Empirical studies are crucial for understanding patient preferences and comprehension in these novel contexts.
The Principles of Beneficence and Nonmaleficence
Theoretical Foundation: The principles of beneficence (the obligation to act for the benefit of others) and nonmaleficence (the obligation not to inflict harm, primum non nocere) are among the oldest in medical ethics, traceable to the Hippocratic Oath [19]. Beneficence supports moral rules to protect rights, prevent harm, and help persons with disabilities, while nonmaleficence supports rules against killing, causing pain, or incapacitating others [19].
Applied Contexts and Challenges:
- Risk-Benefit Analysis in Drug Development: A practical application of these principles involves the careful weighing of the benefits of an intervention against its potential burdens and risks [19]. This is central to the design of clinical trials and therapeutic regimens.
- End-of-Life Care: These principles guide difficult decisions regarding withholding or withdrawing life-sustaining treatment, medically administered nutrition and hydration, and pain management, where the doctrine of double effect may be applied [19].
- Digital Health and AI: In digital health, beneficence involves using technology to improve health outcomes, while nonmaleficence requires addressing risks like data breaches, algorithmic errors, or the amplification of health disparities [17]. Algorithmic bias represents a significant potential maleficence that requires empirical investigation and mitigation.
The Principle of Justice
Theoretical Foundation: The principle of justice demands fairness in the distribution of benefits, risks, and costs [19]. Philosopher John Rawls's theory, which argues for principles of justice chosen behind a "veil of ignorance," is highly influential in contemporary bioethics [17]. It is crucial to distinguish between equality (treating everyone the same), equity (allocating resources based on circumstance to achieve fair outcomes), and justice (addressing the root causes of inequality and removing structural barriers) [17].
Applied Contexts and Challenges:
- Distributive Justice in Healthcare Access: This concerns the fair allocation of scarce healthcare resources and access to innovative therapies. The failure of "trickle-down equity" in healthcare highlights the need for proactive justice-oriented approaches from the outset of technology development [21].
- Translational Justice: This emerging framework proposes "procedural and outcomes-based attention to how clinical technologies move from bench to bedside in a manner that equitably addresses the values and practical needs of affected community members" [21]. It argues that equity must be integrated from the basic science stage, not as an afterthought.
- Digital Determinants of Health (DDH): Factors such as access to digital infrastructure, digital literacy, and algorithmic bias are increasingly recognized as determinants of health outcomes. Justice requires actively reducing this digital divide through inclusive design and policy [17].
- Global and Cross-Cultural Frameworks: There is a growing movement to augment and enrich the bioethics canon with scholarly work on global frameworks of justice that reach beyond Eurocentric perspectives, particularly for emerging biotechnologies [22] [20].
Quantitative Landscape of Empirical Bioethics Research
Empirical research in bioethics has seen significant growth, providing a data-driven foundation for integrating normative and empirical approaches. The following table summarizes key trends in empirical bioethics publications based on a retrospective study of nine leading journals.
Table 1: Prevalence and Nature of Empirical Research in Bioethics (1990-2003)
| Aspect of Empirical Research | Findings | Statistical Significance |
|---|---|---|
| Overall Prevalence | 435 of 4,029 articles (10.8%) used an empirical design [18]. | N/A |
| Temporal Trend | Increase from 5.4% in 1990 to 15.3% in 2003. Period 1997-2003 (n=309) had more empirical studies than 1990-1996 (n=126) [18]. | χ² = 49.0264, p < .0001 [18] |
| Leading Journals (by % of empirical articles) | 1. Nursing Ethics (39.5%)2. Journal of Medical Ethics (16.8%)3. Journal of Clinical Ethics (15.4%) [18] | N/A |
| Methodological Paradigm | 64.6% (n=281) employed a quantitative paradigm [18]. | N/A |
| Geographic Distribution of Bioethics Publications | USA (59.3%), UK (13.5%), Canada (4.0%), and Australia (3.8%) dominated publications [23]. | Significant decrease in U.S. contribution from 1997-2003 (χ² = 90, p < .0001) [23] |
Table 2: Key Research Topics in Empirical Bioethics
| Research Topic | Frequency | Representative Research Subjects |
|---|---|---|
| Prolongation of Life and Euthanasia | 68 studies (Most frequent topic) [18] | Patients, healthcare providers |
| Patient Autonomy & Informed Consent | Numerous studies [18] [20] | Patients, surrogates |
| Cross-Cultural Understanding of Principles | Numerous studies [20] | Medical professionals, general public across different countries |
Experimental Protocols for Empirical Bioethics
General Protocol Template for Empirical Bioethics Research
The following protocol template, adapted for humanities and social sciences in health, is suitable for quantitative, qualitative, and mixed-methods research in empirical bioethics [12].
Table 3: Core Sections of an Empirical Bioethics Research Protocol
| Section Number | Section Title | Key Content Requirements |
|---|---|---|
| 1 | Title, short title and acronym | Concisely describe the nature and subject of the study and the methodological approach [12]. |
| 6 | Summary | Summarize the study's context, primary objective, and general method without bibliographic references [12]. |
| 7 | Problem studied | Explain the importance of the problem and summarize the most significant existing works [12]. |
| 8 | Objective(s) of the study | Present the specific research objectives and/or questions [12]. |
| 9 | Disciplinary field | Specify the principal disciplinary field(s) (e.g., empirical bioethics, medical anthropology) [12]. |
| 10 | Research paradigm of the study | Critical Section: Specify the methodological framework (qualitative/quantitative/mixed) and the theoretical normative framework (e.g., principlism, specific theory of justice) used to derive normative conclusions from empirical data [12]. |
| 12 | Characteristics of the investigator(s) | Specify investigator qualifications, experience, and potential relationships to participants that could bias the study [12]. |
| 13 | Characteristics of the participants/populations | Specify the characteristics of the study participants and the sample size justification [12]. |
| 15 | Consent and information | Specify and justify the type of informed consent and information notice used [12]. |
| 16 | Data collection | Present and justify the types of data, procedures, and instruments (e.g., interview guides, questionnaires) [12]. |
| 19 | Data analysis | Present and justify the analytical methods, including techniques for qualitative and/or quantitative data [12]. |
Workflow for an Integrated Normative-Empirical Study
The following diagram illustrates the sequential and iterative workflow for conducting a study that integrates empirical research with normative analysis.
Protocol for Evaluating AI in Medical Ethics Contexts
With the increasing use of artificial intelligence, empirical protocols are needed to evaluate its alignment with bioethical principles. The following methodology is adapted from a study on human-machine agreement in patient autonomy cases [24].
Objective: To evaluate and improve the alignment of Large Language Models (LLMs) with physician consensus on hypothetical cases involving patient autonomy.
Methodology:
- Case Development: Compose a set of hypothetical cases (e.g., 44 cases) covering key areas like capacity to consent, treatment refusal, and confidentiality. No real patient information should be used [24].
- Physician Panel: Establish a panel of board-certified physicians (e.g., 5 physicians) to establish a consensus (majority response) for each case [24].
- Evaluation Phase: Present cases to foundational LLMs (e.g., ChatGPT, LLaMA, Gemini) and compare their yes/no responses to the physician consensus using Cohen's κ statistic [24].
- Improvement Phase: Iteratively use prompt engineering techniques (e.g., chain-of-thought, N-shot prompting, question-refinement) to improve LLM responses. The goal is to achieve statistically significant improvement in agreement with the physician consensus, measured by the McNemar test [24].
The Scientist's Toolkit: Research Reagent Solutions
This section details key methodological "reagents" and their functions for designing and implementing robust empirical bioethics research.
Table 4: Essential Methodological Tools for Empirical Bioethics Research
| Tool / Method | Function / Application | Considerations for Use |
|---|---|---|
| Validated Surveys & Questionnaires | Quantitatively measure attitudes, beliefs, and experiences of stakeholders (patients, providers, public) regarding ethical issues. | Requires rigorous development, validation, and cross-cultural adaptation for international studies [18] [20]. |
| Semi-Structured Interview Guides | Facilitate in-depth, qualitative exploration of lived experiences, values, and ethical reasoning behind decisions. | Guides should be piloted. Interviewers require training to minimize bias [18] [12]. |
| Hypothetical Vignettes | Present standardized ethical scenarios to study decision-making patterns and evaluate interventions (e.g., AI ethics tools) under controlled conditions [24]. | Fidelity and realism of vignettes are critical for ecological validity. |
| Standardized Protocol Template | Provides a structured framework for planning, documenting, and ensuring rigor in humanities and social science health research [12]. | Must be flexible enough to accommodate diverse methodological and epistemological approaches [12]. |
| Cross-Cultural Comparative Framework | Systematically analyze and compare the interpretation and application of ethical principles across different cultural and national contexts [20]. | Must account for linguistic nuances, local norms, and dominant religious/philosophical traditions [20]. |
| Prompt Engineering Techniques (for AI Ethics) | A set of methods (e.g., chain-of-thought, role-playing) to improve the reliability and ethical alignment of LLM responses in bioethics tasks [24]. | Requires human expert oversight and validation against a gold standard (e.g., physician consensus) [24]. |
The integration of normative analysis with empirical research methodologies represents the forefront of modern bioethics. By systematically applying the principles of autonomy, beneficence, nonmaleficence, and justice through the protocols, tools, and frameworks outlined in this document, researchers and drug development professionals can generate robust, actionable evidence to guide ethical practice. This approach is essential for navigating the complex ethical terrain of digital health, biotechnology, and global health inequities, ensuring that advancements in medicine remain firmly rooted in a commitment to human dignity and justice. Future work must continue to broaden the scope of justice frameworks beyond traditional Western canon and refine empirical methods for capturing the nuanced reality of ethical decision-making in diverse contexts.
Application Note: Empirical Data and Normative Analysis in Clinical Research Appraisal
Background and Quantitative Landscape
The integration of empirical data with normative analysis begins with understanding the landscape of scientific commentary in clinical research. Analysis of PubMed data reveals that only 4.65% of published clinical research articles receive post-publication comments, with a total of 171,556 unique comments on 130,629 unique clinical studies [25]. This commentary ecosystem represents a crucial interface where empirical evidence meets interpretive, normative judgment.
Table 1: Characterization of Scientific Commentary on Clinical Research Studies
| Aspect | Overall Data | Editorials | Letters to Editor |
|---|---|---|---|
| Total Comments | 171,556 | 46,644 | 85,252 |
| Commented Articles | 130,629 | 48,370 | 62,919 |
| Temporal Distribution (2015-2018) | 29,027 comments (16.92%) | 7,442 comments (15.95%) | 12,494 comments (14.66%) |
| Supportive Tone Prevalence | 67% (from sample) | N/A | N/A |
| Top Journal (Frequency) | The New England Journal of Medicine (4.94% of comments) | The New England Journal of Medicine (4.25% of comments) | The New England Journal of Medicine (7.32% of comments) |
Protocol for Evidence Appraisal Integration
Objective: To establish a systematic methodology for integrating empirical clinical research findings with normative ethical analysis through critical commentary assessment.
Materials:
- PubMed/MEDLINE database access
- Citation management software (e.g., EndNote, Zotero)
- Qualitative data analysis tool (e.g., MAXQDA, NVivo)
- Ethical framework selection guide
Procedure:
- Identification: Query PubMed using Medical Subject Headings (MeSH) for clinical studies with comments via "hascommentin" filter [25]
- Metadata Extraction: Collect PubMed IDs, publication types, dates, journal names, and MeSH terms for articles and corresponding comments
- Full-Text Acquisition: Retrieve complete comments through NCBI Entrez Programming Utilities, PMC Open Access, and non-PMC journals with OA policies
- Content Analysis: Apply Latent Dirichlet Allocation (LDA) topic modeling with Gibbs sampling to identify dominant themes
- Sentiment Coding: Manually classify comments as "generally supportive," "neutral," or "generally critical" with interrater reliability assessment
- Normative Framework Application: Select appropriate ethical theories using adequacy, suitability, and theoretical background criteria [26]
- Integration: Employ reflective equilibrium or dialogical methods to synthesize empirical findings with normative analysis
Deliverables: Critical appraisal report with empirical summary and normative recommendations, thematic analysis of commentary patterns, and ethical guidance for clinical implementation.
Application Note: Normative-Empirical Integration in Biopharmaceutical Policy
Empirical Foundation for Policy Analysis
Biopharmaceutical policy represents a critical application area where empirical data on research and development (R&D) investment must inform normative decisions about drug pricing, innovation incentives, and public health priorities. Current policy models, including those used by the Congressional Budget Office (CBO), rely on outdated data that fail to capture complexities of modern drug development [27]. The relationship between financial returns and R&D investment demonstrates that $2.5 billion in additional revenue is needed to invent one new chemical entity, and a 1% increase in potential market size leads to a 4-6% increase in new drugs in that therapeutic area [27].
Table 2: Biopharmaceutical Policy Analysis Framework
| Policy Challenge | Current Data Limitations | Empirical Needs | Normative Considerations |
|---|---|---|---|
| Impact of price-setting | Outdated models; lack of analogs for US market | Updated investment data across therapeutic areas | Balance between immediate savings and future health benefits |
| Therapeutic area disparities | Shift to oncology not fully captured | Therapeutic area-specific impact analyses | Equity in drug development for rare diseases and common conditions |
| Post-market development | Overlooks R&D for existing drugs | Data on new indications and combination therapies | Patient access to improved treatments |
| Emerging modalities | Limited data on cell/gene therapies | Investment patterns in novel technologies | Just allocation of resources for transformative treatments |
| Global implications | US-centric models | International investment flow data | Global health equity and burden-sharing |
Protocol for Policy Impact Assessment
Objective: To evaluate the normative implications of biopharmaceutical policies using empirical data on R&D investment and clinical development outcomes.
Materials:
- Federal and private biopharmaceutical development datasets
- Investment trend analysis software
- Policy modeling tools
- Therapeutic area classification system
Procedure:
- Data Aggregation: Compile data on R&D investment, clinical trial outcomes, and market returns from FDA records, clinical trial registries, and industry reports
- Therapeutic Area Stratification: Analyze investment patterns across oncology, rare diseases, vaccines, and emerging modalities (gene/cell therapies)
- Policy Scenario Modeling: Project impacts of price regulations, intellectual property changes, and reimbursement policies on R&D investment
- Stakeholder Analysis: Identify varying risk tolerance among investors, large pharmaceutical companies, and small biotech firms
- Normative Framework Selection: Apply adequacy criteria to select ethical theories addressing justice, equity, and innovation incentives [26]
- Integration Methodology: Implement reflexive balancing between empirical data and normative principles [1]
- Impact Quantification: Estimate effects on new drug development, patient access, and global health outcomes
Deliverables: Policy impact assessment report, therapeutic area-specific investment recommendations, and ethical framework for balancing innovation incentives with affordability concerns.
Visualization: Integration Methodology for Empirical-Normative Research
Diagram 1: Empirical-Normative Integration Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Empirical-Normative Bioethics Research
| Research Tool | Function | Application Context |
|---|---|---|
| PubMed/MEDLINE Database | Identification of clinical studies and scientific commentary | Evidence base characterization and commentary analysis [25] |
| Qualitative Data Analysis Software | Topic modeling and content analysis of textual data | Identifying themes in scientific commentary and policy documents [25] |
| Ethical Framework Selection Guide | Systematic approach to choosing normative theories | Ensuring adequacy, suitability, and theoretical coherence [26] |
| Reflective Equilibrium Methodology | Structured process for normative-empirical integration | Balancing empirical data with ethical principles through iterative reflection [1] |
| Policy Modeling Tools | Projecting impacts of regulatory changes on innovation | Analyzing effects of price-setting on drug development investment [27] |
| Stakeholder Engagement Framework | Incorporating diverse perspectives in analysis | Ensuring inclusive dialogical empirical ethics approaches [1] |
Application Note: Methodological Approaches for Integration
Theoretical Foundations
The integration of empirical and normative approaches requires careful methodological consideration. Empirical bioethics centers around the integration of empirical findings with normative philosophical analysis, but the process often remains unclear despite numerous available methodologies [1]. Three primary methodological approaches have been identified: (1) consultative, where researchers independently analyze data to develop normative conclusions (e.g., reflexive balancing, reflective equilibrium); (2) dialogical, relying on stakeholder dialogue to reach shared understanding (e.g., inter-ethics); and (3) combined approaches that integrate both methods [1].
Protocol for Reflective Equilibrium Integration
Objective: To implement Wide Reflective Equilibrium as a methodology for integrating empirical data with normative analysis.
Materials:
- Empirical research findings
- Documented moral intuitions and principles
- Background ethical theories
- Iterative analysis framework
Procedure:
- Empirical Premise Formation: Collect and analyze relevant empirical data (e.g., clinical research patterns, investment trends)
- Normative Premise Articulation: Identify relevant moral principles, values, and ethical theories for the research question
- Initial Considered Judgments: Document reasoned moral intuitions about specific cases
- Iterative Reconciliation: Systematically move back and forth between empirical data, ethical principles, and considered judgments
- Coherence Assessment: Evaluate whether all elements form a coherent network of beliefs
- Equilibrium Achievement: Reach temporary equilibrium where all elements support one another
- Application: Apply the achieved equilibrium to the specific research question or case
Deliverables: Reflective equilibrium report documenting the iterative process, identified points of tension and resolution, and normative conclusions supported by empirical evidence.
The scope of application from clinical research to biopharmaceutical policy and public health demonstrates the critical importance of integrating empirical data with normative analysis. This integration requires systematic methodologies that make the selection of ethical frameworks transparent and the process of combining empirical findings with normative reasoning explicit. Through structured approaches like reflective equilibrium and dialogical ethics, researchers can develop more robust, justified conclusions that advance both scientific understanding and ethical practice in medicine and health policy.
Methodologies in Action: Selecting Frameworks and Applying Integrative Models
Empirical bioethics is an interdisciplinary field that seeks to integrate empirical findings with normative (philosophical) analysis to draw substantive conclusions about how we ought to act in healthcare and life sciences contexts [7] [28]. This integration is particularly crucial for drug development professionals and researchers who must navigate complex ethical terrain that spans basic science, clinical research, clinical care, and public health [29]. Despite the availability of numerous methodological approaches, the process of integration often remains opaque and challenging, with researchers reporting an "air of uncertainty and overall vagueness" about how to effectively combine empirical data with normative reasoning [7]. This application note provides structured guidance on three prominent methodological approaches, complete with practical protocols and visual frameworks designed for immediate application in research settings.
Methodological Frameworks: Principles and Applications
The table below summarizes three principal methodologies employed in empirical bioethics research, each offering distinct approaches to integrating empirical observations with normative analysis.
Table 1: Core Methodologies in Empirical Bioethics Research
| Methodology | Primary Integration Mechanism | Typical Applications | Key Characteristics |
|---|---|---|---|
| Reflective Equilibrium | Back-and-forth adjustment between principles and judgements [7] [30] | Policy development, ethical analysis of clinical guidelines [7] | Researcher-driven deliberation; seeks coherence across beliefs; can be narrow (principles-judgements) or wide (includes background theories) [30] |
| Dialogical Models | Structured stakeholder dialogue [7] | Technology ethics, clinical ethics consultation, guideline development [7] [31] | Collaborative deliberation; ethicist as facilitator; generates shared understanding [7] |
| Grounded Moral Analysis | Systematic analysis of empirical data to identify and refine ethical concepts [7] | Research ethics, emerging technology ethics, clinical practice ethics [7] | Inductive approach; moral concepts emerge from data; iterative data collection and analysis [7] |
Reflective Equilibrium: Protocol and Application
Reflective Equilibrium (RE), particularly in its "wide" form, represents a sophisticated approach to ethical justification that extends beyond mere coherence-seeking to aim for systematic coherence among an interconnected network of commitments [30]. The methodology is characterized by its iterative process of adjustment between considered judgments about particular cases and ethical principles, seeking mutual alignment and support.
Experimental Protocol: Implementing Wide Reflective Equilibrium
Research Question Formulation
- Define the specific ethical problem or question requiring normative guidance
- Example: "What ethical framework should guide the use of gamification in digital mental health technologies for adolescents?" [31]
Initial Commitment Elicitation
- Document considered judgments: Gather pre-theoretical ethical intuitions about specific cases or scenarios
- Articulate relevant principles: Identify applicable ethical principles (e.g., autonomy, beneficence, justice)
- Identify background theories: Note relevant philosophical, political, or scientific theories that inform the domain
Process of Equilibration
- Test principles against judgments: Assess whether principles consistently generate the considered judgments in specific cases
- Identify discrepancies: Note where principles and judgments conflict or where judgments are inconsistent
- Revise and refine: Make adjustments to principles, judgments, or background theories to eliminate inconsistencies
- Seek systematic coherence: Aim for relationships of mutual support across the belief network, not mere consistency
Equilibrium Assessment
- Evaluate whether the revised set of commitments provides a defensible, coherent framework that justifies the normative conclusions
- Assess whether the framework satisfies epistemic virtues such as explanatory power, simplicity, and fruitfulness [30]
The following diagram illustrates this iterative process:
Diagram 1: Reflective Equilibrium Iterative Process
Dialogical Models: Protocol and Application
Dialogical empirical ethics relies on structured dialogue between stakeholders to reach a shared understanding of ethical issues and collaboratively develop normative guidance [7]. This approach is particularly valuable in contexts involving multiple perspectives or where ethical analysis benefits from direct engagement with lived experience.
Experimental Protocol: Implementing Dialogical Integration
Stakeholder Identification and Recruitment
- Identify all relevant stakeholder groups (patients, clinicians, researchers, industry representatives, etc.)
- Ensure diverse representation within stakeholder groups
- Obtain informed consent for participation, clarifying the normative (not just research) nature of the dialogue
Dialogue Facilitation
- Establish dialogue ground rules emphasizing respect, confidentiality, and open exchange
- Deploy facilitation techniques that ensure equitable participation
- Frame discussion around concrete cases or scenarios to ground abstract principles
- Encourage explicit articulation of values and reasoning
Iterative Dialogue Process
- Initial value exploration: Elicit stakeholder perspectives without imposing theoretical frameworks
- Principle articulation: Collaboratively identify and define relevant ethical principles
- Case-principle testing: Examine how principles apply to specific cases
- Normative refinement: Jointly refine principles and judgments through discussion
Consensus Building
- Identify areas of agreement and disagreement
- Work toward shared normative conclusions when possible
- Document persistent disagreements and their foundations
The following diagram illustrates the collaborative structure of dialogical models:
Diagram 2: Dialogical Model Collaborative Structure
Grounded Moral Analysis: Protocol and Application
Grounded moral analysis employs a systematic, inductive approach to ethical analysis where moral concepts and frameworks emerge from empirical data rather than being imposed upon it [7]. This approach is particularly valuable when investigating novel ethical territories or when seeking to avoid premature theoretical closure.
Experimental Protocol: Implementing Grounded Moral Analysis
Data Collection Design
- Employ qualitative methods (interviews, focus groups, observations) appropriate to the research question
- Develop data collection instruments that allow ethical dimensions to emerge naturally
- Include diverse participants to capture a range of moral perspectives
Iterative Data Analysis
- Initial coding: Identify and label morally relevant concepts in the data
- Axial coding: Group initial codes into broader ethical categories and themes
- Theoretical coding: Develop relationships between categories to build a conceptual framework
- Constant comparison: Continuously compare new data with emerging framework
Normative Framework Development
- Refine ethical concepts through iterative data collection and analysis
- Develop substantive ethical positions grounded in the data
- Test emerging framework against new cases or data
Integration and Validation
- Assess coherence and justifiability of the grounded framework
- Examine relationship with existing ethical theories
- Refine framework to address discrepancies or limitations
Standards of Practice in Empirical Bioethics
The consensus on standards of practice in empirical bioethics research provides crucial guidance for ensuring methodological rigor [28]. The table below summarizes key standards across six domains of research practice.
Table 2: Empirical Bioethics Standards of Practice
| Domain | Standard | Application Guidance |
|---|---|---|
| Aims | Clearly articulate the aims of the research and its intended contribution | Distinguish between conceptual, instrumental, and symbolic aims; specify intended normative outcomes [28] |
| Questions | Formulate research questions that reflect the interdisciplinary nature of the project | Ensure questions require both empirical and normative analysis; avoid reduction to purely empirical or purely normative questions [28] |
| Integration | Justify the method of integration and demonstrate its execution | Select appropriate integration method (e.g., RE, dialogical, grounded); document how empirical and normative elements interact [7] [28] |
| Empirical Work | Design and conduct empirical work to bioethics standards | Meet quality standards of social science research; ensure methodological appropriateness for normative aims [28] |
| Normative Work | Design and conduct normative work to bioethics standards | Employ rigorous normative methodologies; articulate and justify normative frameworks [28] |
| Training & Expertise | Ensure research team possesses appropriate interdisciplinary expertise | Include both empirical and normative expertise; foster mutual understanding across disciplinary divides [28] |
The Scientist's Toolkit: Essential Research Reagents
The table below details key methodological "reagents" essential for conducting rigorous empirical bioethics research.
Table 3: Essential Research Reagents for Empirical Bioethics
| Research Reagent | Function | Application Notes |
|---|---|---|
| Semi-structured Interview Guides | Elicit rich qualitative data on moral experiences and reasoning | Include open-ended questions; allow follow-up probes; pilot-test for clarity [7] |
| Case Vignettes | Present concrete scenarios for ethical analysis | Ensure relevance to research question; systematically vary key parameters; maintain realism [7] |
| Deliberative Dialogue Frameworks | Structure stakeholder engagement | Establish ground rules; define facilitator role; create balanced participant mix [7] [28] |
| Coding Manuals | Systematize qualitative data analysis | Define code definitions; establish inclusion/exclusion criteria; ensure intercoder reliability [7] |
| Normative Analysis Frameworks | Structure ethical reasoning and argumentation | Apply established frameworks (e.g., principlism) or develop grounded frameworks; ensure logical rigor [29] [28] |
| Integration Protocols | Guide the combining of empirical and normative elements | Specify sequence and weighting of empirical and normative components; document adjustment processes [7] [28] |
Application Contexts in Pharmaceutical Research and Development
The methodological approaches outlined above find specific application across multiple domains of pharmaceutical research and development:
Clinical Trials Ethics
- Application of reflective equilibrium to balance competing ethical principles in trial design
- Dialogical engagement with patients, researchers, and regulators to establish ethically sound protocols
- Grounded analysis of participant experiences to identify previously unrecognized ethical issues [32]
Data Ethics and Digital Health
- Normative framework development for emerging technologies using wide reflective equilibrium
- Stakeholder dialogue addressing ethical tensions in data use, privacy, and benefit-sharing [33]
- Grounded moral analysis of developer perspectives on ethical challenges in digital mental health [31]
Biopharmaceutical Bioethics
- Specification of ethical principles for industry contexts through deliberative processes
- Development of ethics roadmaps for iterative technology development projects [29] [31]
- Ethical analysis spanning research, development, supply, commercialization, and clinical use of healthcare products [29]
The landscape of methods in empirical bioethics offers diverse yet complementary approaches to integrating empirical research with normative analysis. Reflective equilibrium provides a rigorous framework for individual researcher deliberation, dialogical models leverage collective wisdom through structured engagement, and grounded moral analysis ensures ethical frameworks remain connected to lived experience. For researchers, scientists, and drug development professionals, mastering these methodologies enables more nuanced and effective navigation of the complex ethical challenges inherent in pharmaceutical research and development. By adhering to established standards of practice and selecting methodologies appropriate to their specific research questions, bioethics researchers can produce work that is both empirically robust and normatively defensible, ultimately contributing to more ethical healthcare innovation.
The integration of normative ethical analysis with empirical data is a cornerstone of contemporary bioethics research, particularly in fields like healthcare artificial intelligence (AI) and clinical drug development. This interdisciplinary approach, often termed Embedded Ethics or empirical bioethics, relies on the collaboration between ethicists, social scientists, and domain specialists to address ethical and social challenges as they emerge during research and development processes [14]. The core challenge lies in selecting an ethical theory that is both philosophically adequate and contextually suitable, while also being capable of productive interrelation with empirical data to generate normative conclusions. This document provides application notes and detailed protocols to guide researchers, scientists, and drug development professionals in this critical selection process, framed within the broader thesis that robust bioethics requires a synergistic, rather than parallel, approach to normative and empirical inquiry.
Foundational Concepts and Selection Criteria
Defining Adequacy and Suitability
The selection of an ethical theory for a bioethics research project should be guided by two principal criteria: adequacy and suitability.
- Adequacy refers to the theory's conceptual robustness and its capacity to address the normative dimensions of the research problem. An adequate theory provides a coherent framework for identifying, analyzing, and justifying moral principles and conclusions [34].
- Suitability concerns the theory's practical fit for the specific research context, including the domain of application (e.g., pragmatic clinical trials, AI in healthcare), the nature of the empirical data to be collected, and the intended outcome of the research (e.g., practical recommendations, conceptual framework) [7].
The interrelation with empirical data is the dynamic process through which the selected ethical theory and the gathered data inform and refine one another. This is not a sequential process but an iterative dialogue, essential for grounding normative analysis in the reality of human practices and experiences [7].
Major Ethical Theories and Their Application
Bioethics research often draws upon several established normative theories. The table below summarizes the key features, strengths, and weaknesses of three major approaches, providing a basis for initial theory selection.
Table 1: Comparison of Major Ethical Theories in Bioethics Research
| Feature | Utilitarianism | Deontology | Virtue Ethics |
|---|---|---|---|
| Focus | Consequences of actions [34] | Duties and rules [34] | Character of the moral agent [34] |
| Key Principle | Greatest happiness principle [34] | Categorical imperative [34] | Cultivation of virtues [34] |
| Notable Philosophers | Jeremy Bentham, John Stuart Mill [34] | Immanuel Kant [34] | Aristotle, Elizabeth Anscombe [34] |
| Strengths | Practical in policy-making; focuses on outcomes [34] | Provides clear moral guidelines; emphasizes rights and duties [34] | Emphasizes moral development and context [34] |
| Weaknesses | Can justify harmful actions; requires quantifying the "good" [34] | Rigid; may lead to moral dilemmas when duties conflict [34] | Challenges in universal application; can be vague [34] |
| Best Suited For | Health policy analysis, resource allocation, risk-benefit assessment | Informed consent processes, privacy protection, protocol development | Professional ethics training, stakeholder engagement, understanding clinician moral stress |
Application Notes for Theory Selection
Aligning Theory with Research Context and Question
The choice of an ethical theory must be directly responsive to the research question and context.
- For research on systemic or policy-level interventions (e.g., implementing a new AI-based diagnostic tool across a hospital system), a utilitarian approach may be suitable for evaluating the overall impact on patient outcomes, efficiency, and resource distribution [34].
- For studies involving rights, autonomy, and strict protocols (e.g., obtaining informed consent in a pragmatic clinical trial where traditional consent is impractical), a deontological framework can provide the necessary emphasis on duties and respect for persons [35].
- For inquiries into professional conduct and moral character (e.g., investigating sources of moral stress in physicians during a public health crisis), virtue ethics offers a lens to explore the character, intentions, and practical wisdom of the moral agents involved [36].
Navigating the Challenge of Integration
A common challenge in empirical bioethics is the vagueness surrounding the integration of empirical findings with normative analysis [7]. Researchers report using methods like "back-and-forth" reflective equilibrium or collaborative dialogical approaches, yet often describe the process as uncertain [7]. To mitigate this, the selection of an ethical theory should be explicit and its proposed role in integration clearly justified at the protocol stage. This involves deciding whether the theory will be used to frame the empirical data collection, to analyze the data, or to interpret the findings in a structured dialogical process with stakeholders [7].
Experimental Protocols for Empirical Bioethics
Protocol I: Embedded Ethics for AI Health Technology Development
This protocol adapts the Embedded Ethics approach for integrating ethics and social science into AI-related healthcare projects, such as those in drug development or medical device innovation [14].
Aim: To proactively identify and address ethical and social issues at every stage of technology development.
Workflow Overview:
Detailed Methodology:
- Embedding Researchers: Integrate trained ethicists and/or social scientists as core members of the interdisciplinary research and development team. They should participate in regular team meetings and work in the same physical or virtual venue to build a profound understanding of the project [14].
- Stakeholder Analysis: Systematically identify all individuals and groups affected by the technology (e.g., patients, clinicians, developers, regulators). Use this analysis to guide subsequent empirical data collection [14].
- Iterative Data Collection and Normative Analysis: Deploy a combination of empirical methods from the social sciences, selected based on the research question. The embedded researcher continuously moves between the collected data and established ethical debates to identify and analyze emerging concerns.
- Methods: Include (but are not limited to) ethnographic approaches, peer-to-peer interviews, focus groups, interviews with affected groups, and bias analyses of algorithms or data sets [14].
- Integration: The selected ethical theory (e.g., deontology for privacy concerns, utilitarianism for resource allocation) provides the normative framework for analyzing the empirical data. For instance, interview data on user trust can be analyzed through a virtue ethics lens to understand the character traits of a trustworthy AI system.
- Collaborative Reflection and Guidance: The embedded researcher facilitates workshops and discussions with the broader team to present findings, stimulate reflexivity, and collaboratively develop ethically sound solutions that are fed back into the technology development cycle [14].
Protocol II: Reflective Equilibrium for Pragmatic Clinical Trial Ethics
This protocol employs the Wide Reflective Equilibrium method to address ethical issues in Pragmatic Clinical Trials (PCTs), such as alternatives to informed consent and risk assessment [7] [35].
Aim: To achieve a coherent alignment between ethical principles, considered moral judgements, relevant facts, and background theories regarding a specific ethical dilemma in a PCT.
Workflow Overview:
Detailed Methodology:
- Articulate Initial Positions: Clearly state the initial ethical principles (P) and considered moral judgements (J) about the issue. For example:
- Principle (P): Respect for patient autonomy requires explicit, written informed consent.
- Judgement (J): In a PCT comparing standard-of-care treatments with minimal risk, an opt-out consent model may be ethically acceptable to ensure trial feasibility and generalizability [35].
- Gather Relevant Facts (F): Collect empirical data to inform the dilemma. This can involve:
- Conducting surveys or interviews with potential participants to understand their values and preferences regarding consent models [35].
- Reviewing empirical literature on the comprehension and attitudes of patients in opt-out versus opt-in studies.
- Analyzing data on the operational burdens and implementation barriers of different consent models from previous trials [35].
- Seek Reflective Equilibrium: Engage in an iterative process of adjustment and revision. The researcher, acting as "the thinker," moves back and forth between the principles (P), judgements (J), and facts (F) [7].
- If empirical data shows that patients in an opt-out model feel equally respected and adequately informed, it may challenge the initial principle, leading to its revision (e.g., autonomy can be respected through broad notification and easy opt-out mechanisms, not just written consent).
- Conversely, a strong philosophical argument might lead the researcher to re-evaluate an initial judgement in light of a principle.
- Reach a Normative Conclusion: The process concludes when a state of coherence—a "reflective equilibrium"—is achieved among all elements. This equilibrium provides the justified normative output for the research, such as a framework for ethical consent in PCTs [7].
The Scientist's Toolkit: Research Reagent Solutions
This table details key methodological "reagents" for conducting empirical bioethics research, explaining their primary function in the research process.
Table 2: Essential Methodologies for Empirical Bioethics Research
| Research Reagent | Function in Empirical Bioethics |
|---|---|
| Stakeholder Analysis | A systematic method to identify and characterize all relevant parties (e.g., patients, clinicians, developers) affected by a technology or intervention, ensuring that ethical analysis is inclusive and contextually grounded [14]. |
| Semi-Structured Interviews | A qualitative data collection method that uses a flexible interview guide to explore participants' perspectives, experiences, and values in depth. Essential for gathering rich, narrative data on moral dilemmas and ethical reasoning [14] [36]. |
| Focus Groups | A facilitated group discussion used to generate data through the interaction of participants on a specific topic. Useful for exploring collective views, cultural norms, and the social dimensions of an ethical issue [14]. |
| Ethnographic Approaches | Involves immersive observation of practices in real-world settings (e.g., clinics, labs). Helps uncover tacit ethical challenges and the practical contexts in which ethical decisions are made, which may not be captured through interviews alone [14]. |
| Reflective Equilibrium | A core methodological "tool" for integration. It provides a structured, albeit iterative, process for moving between empirical data (facts), moral intuitions (judgements), and ethical principles to achieve a coherent normative position [7]. |
| Bias Analysis | A methodological framework, often adapted from AI ethics and social science, for proactively identifying and assessing potential biases in datasets, algorithms, or research protocols that could lead to discriminatory outcomes or unfair distribution of benefits and burdens [14]. |
Within the interdisciplinary field of empirical bioethics, a central challenge is the integration of empirical findings with normative analysis. This document outlines specific application notes and protocols for one dominant methodological approach: the consultative approach, where the researcher acts as an external thinker to analyze data and develop normative conclusions independently. This method is contrasted with dialogical approaches, which rely on stakeholder dialogue to reach shared understanding. The consultative model is characterized by the researcher taking primary responsibility for the integrative process, functioning as a facilitator who applies ethical theory to enrich decision-making, often using a methodology known as reflexive balancing [1].
Theoretical Framework and Key Concepts
Reflexive Balancing and Related Methodologies
Reflexive balancing is a specific consultative method where the researcher, as the external thinker, engages in a deliberative process to achieve coherence among various moral considerations. It is closely related to, and often used interchangeably with, the method of reflective equilibrium [1].
- Reflective Equilibrium: This is a two-way dialogue between ethical principles, values, or judgments and practice (empirical data). The researcher, "the thinker," goes back and forth between normative underpinnings and empirical facts until they achieve moral coherence, an "equilibrium" [1]. In a consultative framework, this process is carried out by the researcher independently.
- The Researcher's Role: In this model, the researcher is not a mere observer but an active, external thinker who collects empirical data and then, through a structured process of reflection, integrates it with normative theories to arrive at a justified ethical position or recommendation [1].
Comparison of Integrative Empirical Bioethics Methodologies
The table below summarizes the key methodological categories in empirical bioethics, highlighting the consultative approach in contrast to other common methods.
Table 1: Categories of Integrative Methodologies in Empirical Bioethics
| Methodology Category | Description | Key Example Method(s) | Role of the Researcher |
|---|---|---|---|
| Consultative | Analysis of data by the researcher, who works independently as an external thinker to develop a normative conclusion [1]. | Reflexive Balancing, Reflective Equilibrium [1] | External thinker and analyst |
| Dialogical | Relies on dialogue between stakeholders (e.g., researchers and participants) to reach a shared understanding and conclusion [1]. | Inter-ethics [1] | Facilitator of dialogue |
| Combined | Hybrid approaches that incorporate elements of both consultative and dialogical methods [1]. | Hermeneutics [1] | Interpreter and facilitator |
Application Notes: Implementing Reflexive Balancing
The following protocol provides a detailed, step-by-step methodology for conducting a research project using the reflexive balancing approach.
Experimental Protocol for Reflexive Balancing
Protocol Title: A Multi-Stage Protocol for Conducting Reflexive Balancing in Empirical Bioethics Research
Objective: To systematically integrate empirical data with normative analysis through a structured process of reflection and adjustment performed by the researcher, with the goal of achieving a coherent ethical position.
Materials and Reagent Solutions: Table 2: Essential Research Reagents for Reflexive Balancing
| Item | Function/Description |
|---|---|
| Qualitative Data Analysis Software (e.g., MAXQDA) | Facilitates the organization, coding, and analysis of large volumes of qualitative empirical data (e.g., interview transcripts) [1]. |
| Structured Interview/Focus Group Guides | Semi-structured or structured protocols used for consistent data collection from participants, ensuring relevance to the research question [1]. |
| Normative Framework Checklist | A predefined list of relevant ethical principles, theories, and concepts (e.g., autonomy, beneficence, justice, utilitarianism, deontology) to guide the normative analysis. |
| Reflexive Journal | A digital or physical log for the researcher to document iterations, challenges, and insights throughout the back-and-forth process of achieving equilibrium. |
Methodology:
Phase 1: Normative Preparation
- Step 1.1: Conduct a thorough literature review to identify and articulate the relevant ethical principles, theories, and considered moral judgments pertinent to the research topic. This forms the initial normative framework.
- Step 1.2: Formulate a set of preliminary, hypothetical ethical positions or questions based on this normative groundwork.
Phase 2: Empirical Data Collection
- Step 2.1: Design and implement an empirical study (e.g., using qualitative methods such as interviews or focus groups) to gather data on the lived experiences, attitudes, and moral reasoning of stakeholders (e.g., clinicians, patients, researchers) regarding the ethical issue [1].
- Step 2.2: Transcribe and anonymize the collected data in preparation for analysis.
Phase 3: Data Analysis and Reflexive Balancing
- Step 3.1: Systematically code and analyze the empirical data using thematic analysis. Identify key themes, conflicts, and patterns in the stakeholders' moral experiences.
- Step 3.2 (The Balancing Loop): Initiate the iterative process of reflexive balancing. Actively compare the emergent empirical themes (from Step 3.1) with the initial normative framework (from Phase 1).
- Step 3.3: Identify points of coherence and tension. For example, an empirical finding may challenge a pre-held considered judgment, or a normative principle may offer a new interpretation of an empirical theme.
- Step 3.4: Adjust either the interpretation of the empirical data, the weighting of the normative principles, or the initial considered judgments to achieve greater coherence across all elements. Document each iteration and rationale in the reflexive journal.
- Step 3.5: Repeat Steps 3.2-3.4 until a stable, reflective equilibrium is achieved, resulting in a well-considered, empirically-informed normative conclusion.
Diagram 1: Reflexive Balancing Workflow
Case Study Application and Advanced Considerations
Illustrative Case: Proactive Clinical Ethics Consultation
The proactive model of Clinical Ethics Consultation Services (CECS) serves as a practical example of a consultative approach in action. In this model, the ethics consultation team actively engages with healthcare professionals through methods like inter-professional ethics rounds and patient note reviews, rather than waiting for a consultation request [37].
- The Researcher/Consultant as External Thinker: In ethics rounds, the consultation team visits staff stations, asks about ethical concerns, and then works with staff to collectively articulate the problem, its ethical dimensions, and potential ways to address it [37]. The team's role is to offer guidance and facilitate a better decision-making process by considering various ethical aspects, while final decisions remain with the medical team. This mirrors the consultative research model, where the ethicist acts as a facilitator applying ethical theory to concrete situations [37] [1].
- Data and Balancing: The "empirical data" in this case is the lived experience and moral distress of the clinical team. The ethics consultants must balance this data against established normative frameworks (principles of bioethics, institutional policies) to provide reasoned guidance.
Advanced Methodological Considerations
Researchers should be aware of ongoing debates and challenges within the consultative paradigm:
- The Challenge of Vagueness: Scholars have reported an "air of uncertainty and overall vagueness" surrounding integration methods like reflective equilibrium [1]. Pressing issues include how much weight to give empirical data versus ethical theory, and the subjective appreciation of the ethicist. This vagueness allows for flexibility but also risks obscuring a lack of methodological rigor [1].
- Algorithmic Bioethics and Complex Ethics: Emerging discussions point towards formalizing consultative processes. One proposal is "Collective Reflective Equilibrium" as a methodology for deciding among conflicting ethical approaches (e.g., egalitarian vs. utilitarian), which can then be used to create ethical algorithms for specific problems like resource allocation [38]. This represents a more structured and potentially scalable application of the consultative approach to complex, multi-faceted problems.
Application Note: Theoretical Foundations in Bioethics Integration
Context within Normative-Empirical Bioethics Research
Dialogical and collaborative methods represent a critical methodological strand within empirical bioethics, addressing the persistent challenge of integrating normative analysis with empirical data [1]. This approach stands in contrast to purely consultative models (like reflective equilibrium, conducted by the researcher alone) by emphasizing that shared understanding emerges through the process of stakeholder dialogue itself [1] [11]. The fundamental thesis is that ethical analysis is not merely applied to practice but is developed and refined with practitioners and stakeholders, creating a symbiotic relationship between theory and practice [11].
Key Methodological Approaches
- Symbiotic Empirical Ethics: This methodology uses a structured, five-step approach to refine ethical theory based on empirical findings, positing that practice and theory are symbiotically related [11].
- Dialogical Empirical Ethics: Relies on structured dialogue between stakeholders (researchers, participants, professionals) to reach a shared understanding and normative conclusion [1].
- Principle-Based Empirically Grounded Roadmap Approach (PERA): Integrates normative principles from literature with empirical data on "ethics in practice" from developers and stakeholders, using abductive reasoning to create practical guidance [39].
Protocol: Implementing Symbiotic Empirical Ethics
Scope and Application
This protocol provides a systematic framework for using symbiotic empirical ethics, a specific dialogical method, to explore ethical challenges in healthcare settings and generate normative conclusions. It is particularly effective for studying everyday ethical dilemmas in clinical practice and organizational decision-making [11].
Procedural Steps
Step 1: Identify Ethical Issues from Practice
- Objective: Gather rich qualitative data on ethical challenges as experienced by healthcare professionals and stakeholders in real-world contexts.
- Procedure:
- Conduct semi-structured interviews and focus group discussions with a diverse range of participants (e.g., clinicians, nurses, patients, administrators) [11].
- Focus questioning on specific ethical dilemmas, decision-making processes, and perceived barriers to ethical practice.
- Record and transcribe discussions verbatim for analysis.
Step 2: Analyse Data for Ethical Themes
- Objective: Identify recurrent ethical themes and concerns within the qualitative data.
- Procedure:
- Employ thematic analysis to code transcripts and identify patterns related to ethical values, conflicts, and reasoning [11].
- Focus on participants' own ethical language and conceptual frameworks.
Step 3: Reflect on Ethical Theory
- Objective: Contextualize empirical findings within relevant ethical theories and principles.
- Procedure:
- Analyze identified themes against established ethical frameworks (e.g., principism, relational ethics, care ethics) [11].
- Identify points of convergence and divergence between empirical data and theoretical norms.
Step 4: Develop a Normative Conclusion
- Objective: Generate a refined normative suggestion that addresses the empirical findings.
- Procedure:
Step 5: Suggest Possible Solutions
- Objective: Translate normative conclusions into practical, actionable recommendations for policy and practice.
- Procedure:
Workflow Visualization
Application Note: A Model for Meaningful Stakeholder Dialogue
Core Principles for Effective Engagement
The SER (Social and Economic Council) model for meaningful stakeholder dialogue provides a theoretical foundation comprising nine key elements organized into three categories, essential for preparing, executing, and concluding dialogue in bioethics research [40].
Table 1: Core Elements of a Meaningful Stakeholder Dialogue Model
| Category | Element | Description | Practical Application in Bioethics |
|---|---|---|---|
| Criteria | Motivation | Reasons for engaging in dialogue; clarity of intentions [40]. | Articulate the specific bioethical question or dilemma prompting the dialogue. |
| Commitment | Genuine dedication to engaging and incorporating results [40]. | Allocate time, resources, and integrate stakeholder feedback into research design and conclusions. | |
| Inclusion | Engaging with the right stakeholders and supporting their participation [40]. | Identify all relevant parties (patients, providers, ethicists) and remove barriers to their engagement. | |
| Implementation | Transparency | Openness about decisions, actions, and processes [40]. | Clearly communicate the dialogue's scope, limitations, and how input will be used. |
| Personal Contact | Building mutual trust through open, sincere interaction and active listening [40]. | Foster a safe environment for discussion, being mindful of power dynamics and cultural differences. | |
| Organising Dialogue | Substantive and practical preparation to meet objectives [40]. | Choose appropriate formats (e.g., multi-stakeholder meetings) and skilled facilitation. | |
| Support | Internal Processes | Embedding stakeholder engagement into business operations and securing senior management support [40]. | Secure institutional buy-in and define internal responsibilities for the engagement process. |
| Collaboration | Working with other parties (NGOs, knowledge networks) [40]. | Partner with patient advocacy groups or professional associations to enhance credibility and reach. | |
| Knowledge | Understanding of legal, political, cultural, and social contexts [40]. | Ground the dialogue in factual and contextual understanding of the bioethics issue. |
Stakeholder Engagement Champion Model
For large-scale or long-term research programs, designating in-country Stakeholder Engagement Champions is an effective model to ensure meaningful, context-driven engagement [41].
- Role: Locally-based professionals with strong communication skills and deep contextual understanding of the health system and stakeholders [41].
- Function: They autonomously design context-specific engagement strategies, allocate resources, and lead interactions with stakeholders throughout the research lifecycle [41].
- Support: Champions are supported through mentorship, peer exchange, and capacity-building activities from a central platform [41].
Protocol: Multi-Stakeholder Dialogue for Ethical Roadmapping
Scope and Application
This protocol adapts the Principle-based Empirically Grounded Roadmap Approach (PERA) for use in a multi-stakeholder setting. It is designed for projects, such as developing digital mental health technologies, where ethical guidance is needed for a largely predetermined technology with embedded co-development practices and planned future iterations [39].
Procedural Steps
Step 1: Integrative Evidence Gathering
- Objective: Collate diverse forms of evidence to inform the ethical roadmap.
- Procedure:
- a) Map Normative Principles: Conduct a literature review to identify relevant ethical principles from bioethics literature [39].
- b) Scoping Review of Moral Intuitions: Systematically review publications or conduct interviews with developers of comparable technologies to understand "ethics in practice" and how they navigate ethical moments [39].
- c) Collect Original Empirical Data: Gather qualitative data (interviews, observations) on the specific use case, focusing on stakeholder values and ethical concerns [39].
Step 2: Facilitated Multi-Stakeholder Dialogue
- Objective: Generate shared understanding and co-create ethical guidance.
- Procedure:
- Convene a diverse group of stakeholders (e.g., developers, ethicists, end-users, healthcare professionals).
- Use a skilled facilitator to guide discussions on the evidence gathered in Step 1 [40].
- Employ techniques like Participatory Decision-Making to grant stakeholders a genuine voice and influence over the roadmap's content, fostering shared ownership [42].
Step 3: Abductive Synthesis and Roadmap Formulation
- Objective: Synthesize insights into a tangible ethics roadmap.
- Procedure:
- Use abductive reasoning (inference to the best explanation) to integrate the normative principles, empirical findings on moral intuitions, and stakeholder input from the dialogue [39].
- Draft an "ethics roadmap" that presents practical, actionable guidance for developers. This output is designed to be portable and adaptable for future project iterations [39].
Step 4: Continuous Feedback and Implementation
- Objective: Ensure the roadmap remains a living document.
- Procedure:
- Establish a Continuous Feedback and Monitoring System [42]. Use pulse surveys, feedback portals, and regular check-ins to gather stakeholder input on the roadmap's utility and challenges in implementation.
- Iteratively refine the roadmap based on this feedback.
Logical Framework Visualization
The Scientist's Toolkit: Essential Reagents for Dialogical Research
Table 2: Key Research Reagent Solutions for Dialogical Bioethics
| Item / Tool | Function | Application Context |
|---|---|---|
| Stakeholder Mapping Matrix | A visual tool to identify and categorize stakeholders based on their influence and interest [42]. | Used during project planning to ensure all relevant voices are included and to tailor engagement strategies [42]. |
| Semi-Structured Interview Guide | A flexible script of open-ended questions to gather rich qualitative data on ethical experiences [11]. | Employed in Symbiotic Empirical Ethics (Step 1) to explore ethical issues from the perspective of practitioners and stakeholders [11]. |
| Multi-Channel Communication Plan | A strategy for using a coordinated mix of platforms (email, social media, town halls) to deliver tailored messages [42]. | Ensures consistent and accessible communication with diverse stakeholder groups throughout the research lifecycle [42]. |
| Facilitator's Guide & Ground Rules | A set of protocols to ensure balanced, respectful, and productive dialogue in multi-stakeholder meetings [40]. | Critical for managing group dynamics, ensuring equitable participation, and maintaining focus on the dialogical objectives [40]. |
| Continuous Feedback System | Formal channels (e.g., pulse surveys, feedback portals) for collecting and acting on stakeholder input in near real-time [42]. | Used to iteratively refine ethical frameworks and tools like the ethics roadmap, demonstrating responsiveness to stakeholder concerns [42]. |
| Ethics Roadmap Template | A tangible output format that synthesizes normative and empirical insights into actionable guidance for developers [39]. | Serves as the key deliverable of the PERA protocol, designed to be a portable and adaptable tool for future project iterations [39]. |
The increasing complexity of clinical trials, coupled with heightened demands for ethical rigor and patient-centricity, necessitates a more integrated approach to protocol development and review. This case study presents a practical framework for combining normative and empirical approaches in bioethics research within the context of clinical trial design. The proposed integrative model bridges theoretical ethical reasoning with practical evidence-gathering, ensuring trials are both scientifically valid and ethically robust [13] [43].
Normative methods in bioethics, such as reflective equilibrium, provide a structured way to resolve ethical dilemmas by striving for coherence between our ethical beliefs about cases and overarching moral principles [43]. When these are systematically combined with empirical data—such as stakeholder perspectives and feasibility evidence—the resulting framework offers a comprehensive method for addressing complex ethical challenges in clinical research [13].
Theoretical Foundation: The Integrative Bioethics Framework
Core Components
The integrative framework rests on two complementary pillars:
- Normative Pillar: Serves as the foundation for ethical justification, employing established methods like reflective equilibrium to create coherence among moral principles, case judgments, and relevant facts [43]. Principlism—often using the four principles of autonomy, beneficence, non-maleficence, and justice—provides a complementary structure for identifying and weighing ethical obligations [43].
- Empirical Pillar: Informs the normative process by gathering systematic evidence about stakeholder values, practical contexts, and potential consequences of design choices. This ensures that ethical analysis is grounded in real-world conditions and participant experiences [13].
Operationalizing the Framework
The following diagram illustrates the dynamic interaction between these components throughout the trial lifecycle, demonstrating how normative and empirical elements inform one another iteratively.
Application Notes: Implementing the Framework in Trial Design
Phase 1: Integrated Protocol Development
The initial protocol development phase systematically applies the integrative framework to key trial design elements:
- Stakeholder-Informed Endpoint Selection: Combine empirical data from patient focus groups and community advisory boards with normative analysis of the clinical value of proposed endpoints. This ensures measured outcomes reflect both scientific relevance and patient priorities [44].
- Risk-Benefit Assessment Enhancement: Move beyond technical risk calculation by incorporating qualitative data on how potential participants perceive and weigh risks against potential benefits, creating a more nuanced understanding of the trial's risk-benefit profile from the participant perspective [45].
- Informed Consent Process Design: Develop consent materials and processes that transparently address ethical issues identified through normative analysis, while using empirical testing (e.g., readability assessments, comprehension interviews) to ensure information is truly accessible and understandable [13] [45].
Phase 2: Ethics Review Integration
Ethics committees can strengthen their review process by adopting this integrative approach:
- Systematic Protocol Evaluation: Apply structured checklists that explicitly include both normative ethical criteria and empirical evidence requirements. The updated SPIRIT 2025 statement, which includes a new item on patient and public involvement, provides a valuable foundation for this [46].
- Evidence-Based Deliberation: Request and review empirical data on stakeholder perspectives and local context as part of the ethical evaluation, ensuring committee judgments are informed by relevant factual evidence about the participant population and implementation environment [13].
- Dynamic Tracking Review: Implement a proactive review process that continues throughout the trial lifecycle, monitoring accumulated empirical data (e.g., participant experiences, emerging safety signals) and reassessing earlier ethical judgments as new evidence emerges [45].
Experimental Protocols and Methodologies
Protocol 1: Stakeholder Values Assessment
This protocol generates empirical data on stakeholder perspectives to inform the normative analysis of key trial design questions.
- Objective: To systematically identify and analyze the ethical priorities and concerns of key stakeholder groups (patients, investigators, community representatives) regarding a proposed clinical trial design.
- Methodology: Employ mixed methods combining focus groups and structured surveys with cross-sectional analysis of different stakeholder perspectives.
- Participant Recruitment: Use purposive sampling to ensure representation of relevant stakeholder groups, including patients with the condition under study, referring clinicians, research coordinators, and community advocates.
- Data Collection:
- Conduct separate focus groups for each stakeholder category using semi-structured discussion guides.
- Perform thematic analysis of discussion transcripts to identify key value themes and ethical concerns.
- Develop and administer a quantitative survey based on emergent themes to assess the relative importance of identified values across a larger sample.
- Data Integration: Create a structured values framework that maps areas of consensus and divergence among stakeholder groups, providing a evidence base for subsequent normative analysis of trial design options.
Protocol 2: Ethical Impact Assessment
This protocol provides a systematic approach for projecting and evaluating the potential ethical consequences of different trial design choices.
- Objective: To identify and assess potential ethical impacts of specific trial design elements before protocol finalization, enabling proactive ethical optimization.
- Methodology: Structured application of a modified ethical impact assessment framework adapted from technology assessment methodologies.
- Procedure:
- Stakeholder Mapping: Identify all parties potentially affected by the trial design, with particular attention to vulnerable groups.
- Impact Identification: Systematically assess how each major design element (e.g., eligibility criteria, comparator selection, endpoint choice) might affect different stakeholder rights and interests.
- Normative Evaluation: Apply principlism framework to analyze identified impacts in relation to established ethical principles [43].
- Mitigation Planning: Develop specific protocol modifications to prevent, minimize, or compensate for identified negative ethical impacts.
- Output: An ethical impact assessment report documenting the analysis and justifying the selected design choices through both empirical evidence and normative reasoning.
Quantitative Data Synthesis
Table 1: SPIRIT 2025 Checklist Integration with Ethical Framework
| SPIRIT 2025 Section | Key Ethical Considerations | Empirical Assessment Methods | Normative Analysis Methods |
|---|---|---|---|
| Background & Rationale (Item 9) | Justification for comparator choice; addressing unmet needs | Analysis of treatment gaps; stakeholder priority assessment | Principle of justice; beneficence analysis |
| Patient & Public Involvement (Item 11) | Authentic engagement; avoiding tokenism | Documentation of involvement methods and influence | Respect for autonomy; democratic legitimacy |
| Risk-Benefit Assessment | Proportionality; equitable risk distribution | Quantitative risk estimation; qualitative risk perception studies | Principlism analysis; reflective equilibrium |
| Informed Consent | Comprehension; voluntariness; ongoing process | Readability testing; comprehension assessments; withdrawal rate monitoring | Respect for autonomy; right to self-determination |
Table 2: Ethics Review Assessment Metrics
| Review Dimension | Quantitative Indicators | Qualitative Indicators | Integrated Assessment Framework |
|---|---|---|---|
| Scientific & Ethical Balance | Sample size justification; statistical power calculations | Therapeutic misconception assessment; value of research question | Risk-benefit proportionality analysis |
| Participant Selection Justice | Eligibility criteria analysis; demographic representativeness plans | Vulnerability assessment; exclusion justification | Principle of justice application; inclusive trial design |
| Informed Consent Quality | Readability scores; comprehension test results | Process voluntariness assessment; cultural appropriateness | Respect for autonomy implementation |
| Ongoing Safety Oversight | Frequency of scheduled safety reviews; stopping rule specifications | Participant experience monitoring plans | Beneficence and non-maleficence in trial conduct |
Research Reagent Solutions
Table 3: Essential Resources for Integrative Bioethics Research
| Resource Category | Specific Tool/Method | Primary Function | Application Context |
|---|---|---|---|
| Protocol Development Tools | SPIRIT 2025 Checklist [46] | Ensures comprehensive protocol content covering key scientific and ethical elements | Trial planning phase; protocol writing |
| Stakeholder Engagement | Modified SRQR Template [13] | Provides structured approach for qualitative and mixed-methods research on stakeholder perspectives | Empirical ethics data collection |
| Ethical Analysis Framework | Principlism/Reflective Equilibrium [43] | Offers systematic method for identifying and resolving ethical dilemmas | Normative analysis of trial design choices |
| Regulatory Compliance | WHO Best Practices Guidance [44] | Provides international standards for ethical trial conduct | Ethics review; protocol development |
| Ethics Review Enhancement | Tracking Review Protocol [45] | Enables ongoing ethical oversight throughout trial implementation | Dynamic ethics committee review |
Implementation Workflow
The practical implementation of the integrative framework follows a structured workflow from initial concept to final protocol approval, with iterative refinement based on continuous feedback.
This case study demonstrates how an integrative framework combining normative and empirical approaches can enhance both the ethical quality and practical implementation of clinical trials. By systematically incorporating stakeholder perspectives through empirical methods while maintaining rigorous ethical analysis through normative approaches, researchers and ethics committees can develop trials that are more responsive to participant needs and more robust in their ethical justification.
The structured methodologies and tools provided here offer practical guidance for implementing this integrative approach, supporting the development of clinical trials that successfully balance scientific rigor with ethical excellence. This framework aligns with evolving international standards [44] and addresses the growing emphasis on patient-centered research and ethical innovation in clinical trial design [46] [45].
Navigating Challenges: Overcoming Vagueness and Ethical Pitfalls in Integration
Application Notes: Principles and Practices for Empirical Bioethics Integration
The Integration Challenge in Empirical Bioethics
Empirical bioethics constitutes an interdisciplinary field centered on integrating empirical findings with normative philosophical analysis to address complex bioethical issues [1]. This integration promises more contextually relevant ethical guidance but presents significant methodological challenges. A systematic review identified 32 distinct methodologies for integrating empirical and normative approaches, revealing considerable heterogeneity and uncertainty about aims, content, and domain of application [28]. This methodological diversity, while fostering innovation, often results in frustrating vagueness and insufficiently determinate practical guidance [1].
The Double-Edged Sword of Methodological Indeterminacy
The indeterminacy of integration methods presents a dual character. On one hand, it provides essential flexibility needed to address diverse research questions and contexts, allowing researchers to adapt approaches to specific needs [1]. On the other hand, it risks obscuring insufficient understanding of theoretical-methodological underpinnings and can lead to inadequately justified normative conclusions [1]. This vagueness particularly manifests in approaches like reflective equilibrium, where pressing issues include determining how much weight should be given to empirical data versus ethical theory [1].
Standards for Quality Integration
In response to these challenges, consensus has emerged around standards of practice for empirical bioethics research [28]. These standards provide guidance for ensuring methodological rigor while acknowledging the field's interdisciplinary nature. Key requirements include clearly stating how theoretical positions were chosen for integration, explaining and justifying how integration methods were carried out, and maintaining transparency in reporting how integration was executed [1].
Table 1: Core Standards for Empirical Bioethics Research
| Domain | Standard Description | Practical Application |
|---|---|---|
| Aims | Clearly articulate research aims and questions | Explicitly state how integration will address the research problem |
| Integration | Justify methodological approach and theoretical position | Explain rationale for chosen integration method and its appropriateness |
| Empirical Work | Conduct empirical work to disciplinary standards | Ensure empirical data collection and analysis meet relevant quality criteria |
| Normative Work | Conduct normative analysis to disciplinary standards | Ensure ethical analysis demonstrates philosophical rigor |
| Training & Expertise | Ensure research team possesses requisite skills | Assemble interdisciplinary team with complementary expertise |
Experimental Protocols for Integration Methods
Reflective Equilibrium Protocol
The reflective equilibrium method represents a "back-and-forth" approach where researchers engage in iterative deliberation between ethical principles/values/judgments and empirical data [1].
Workflow Diagram:
Step-by-Step Procedure:
- Initial Mapping: Identify relevant normative elements (principles, values, theories) and considered judgments about the ethical issue
- Empirical Data Collection: Gather relevant empirical data through qualitative or quantitative methods appropriate to the research question
- Comparative Analysis: Systematically compare normative positions with empirical findings, identifying areas of alignment and tension
- Iterative Adjustment: Engage in back-and-forth revision of normative commitments and interpretation of empirical data to achieve coherence
- Equilibrium Assessment: Determine when sufficient coherence between normative and empirical elements has been achieved
- Output Generation: Articulate normative conclusions that reflect the achieved equilibrium
Dialogical Empirical Ethics Protocol
Dialogical approaches rely on structured dialogue between stakeholders to reach shared understanding and normative conclusions [1].
Workflow Diagram:
Step-by-Step Procedure:
- Stakeholder Identification: Identify and recruit diverse stakeholders relevant to the ethical issue
- Dialogical Framework: Establish ground rules and structure for ethical dialogue
- Facilitated Discussion: Conduct structured dialogues exploring ethical dimensions, with researchers as facilitators
- Content Analysis: Systematically analyze dialogue content for emerging ethical themes and considerations
- Normative Synthesis: Develop ethically justified positions through collaborative sense-making
- Output Validation: Verify synthesized positions with participants to ensure faithful representation
Joint Display Integration Protocol for Mixed Methods
The joint display approach provides visual means to integrate qualitative and quantitative data, drawing out new insights through structured comparison [47].
Table 2: Joint Display Implementation Framework
| Display Type | Design Application | Integration Approach | Analytic Strategy |
|---|---|---|---|
| Statistics-by-Themes | Explanatory sequential; Convergent | Merging quantitative results with qualitative themes | Side-by-side comparison to generate inferences |
| Side-by-Side Comparison | Convergent; Intervention | Merging parallel quantitative and qualitative datasets | Narrative weaving of complementary findings |
| Instrument Development | Exploratory sequential | Building quantitative instruments from qualitative findings | Linking qualitative dimensions to scale items |
| Theoretical/Conceptual Lens | Explanatory sequential | Explaining quantitative results using qualitative data | Framing results within conceptual frameworks |
Step-by-Step Procedure:
- Design Determination: Identify appropriate mixed methods design (exploratory sequential, explanatory sequential, or convergent)
- Data Collection: Implement complementary quantitative and qualitative data collection procedures
- Separate Analysis: Conduct initial separate analysis of quantitative and qualitative datasets
- Display Construction: Create visual joint display that arrays quantitative and qualitative results together
- Integration Analysis: Draw meta-inferences by analyzing relationships between datasets in the display
- Interpretation: Develop integrated conclusions that reflect both empirical evidence and normative considerations
The Scientist's Toolkit: Essential Research Reagents for Empirical Bioethics
Table 3: Core Methodological Resources for Integrated Bioethics Research
| Tool Category | Specific Method/Approach | Function and Application |
|---|---|---|
| Integration Frameworks | Reflective Equilibrium [1] | Iterative coherence-building between normative and empirical elements |
| Dialogical Ethics [1] | Structured stakeholder engagement for shared normative understanding | |
| Principle-Based Roadmap (PERA) [39] | Ethics roadmap development for guiding technology development | |
| Mixed Methods Tools | Joint Displays [47] | Visual integration of quantitative and qualitative datasets |
| Connecting Approaches [48] | Using one database to inform sampling for another | |
| Building Approaches [48] | Using one database to inform data collection approach of the other | |
| Quality Standards | Consensus Standards [28] | Benchmarks for rigorous empirical bioethics research design and reporting |
| Formal, Cognitive & Ethical Norms [28] | Comprehensive criteria for research quality and integrity |
Advanced Integration Frameworks
The PERA Approach for Technology Ethics
The Principle-Based Empirically Grounded Roadmap Approach (PERA) represents an advanced methodology developed for digital mental health technologies but applicable more broadly [39]. This approach responds to contexts where technology is largely predetermined, co-development practices are embedded, and future iterations are anticipated.
Workflow Diagram:
Embedded Ethics Implementation
Embedded ethics approaches integrate ethics researchers within development teams, emphasizing early collaboration and shared responsibilities [39]. This methodology employs "ethics parallel research" that accompanies but maintains reflective distance from technological development.
Implementation Protocol:
- Team Integration: Embed ethics researchers within development teams from project inception
- Parallel Investigation: Conduct simultaneous empirical and normative investigation alongside development processes
- Iterative Feedback: Provide ongoing ethical feedback at critical development milestones
- "Ethically Important Moments" Documentation: Identify and analyze spontaneous ethical decision points during development
- Structured Outputs: Generate practical guidance tailored to development context and constraints
The methodological vagueness surrounding integration in empirical bioethics presents both challenges and opportunities. By adopting structured approaches like those outlined in these application notes and protocols, researchers can harness the flexibility of interdisciplinary methods while maintaining scholarly rigor. The continued development and refinement of integration methodologies remains essential for empirical bioethics to fulfill its promise of generating ethically robust, empirically grounded normative guidance.
The transition from descriptive statements (what is) to prescriptive statements (what ought to be) constitutes one of the most fundamental philosophical challenges for interdisciplinary research in bioethics. First articulated by Scottish philosopher David Hume, the is-ought problem highlights a logical difficulty in deriving ethical conclusions from purely factual premises [49]. In contemporary bioethics, this problem manifests when researchers attempt to integrate empirical data from social science with normative ethical analysis [50] [1]. The field of empirical bioethics has emerged precisely to address this methodological challenge, developing structured approaches to bridge the fact-value divide without committing logical fallacies [51] [52].
This problem presents particular difficulties for researchers, scientists, and drug development professionals who operate in evidence-based domains yet must make normative recommendations. Direct inferences from descriptive data to normative conclusions remain problematic for theoretical, methodological, and pragmatic reasons [50]. Understanding why such direct inference fails logically, and what methodological alternatives exist, provides crucial foundation for robust bioethical analysis in scientific and clinical contexts.
Table: Core Concepts in the Is-Ought Problem
| Concept | Definition | Bioethics Relevance |
|---|---|---|
| Is-Statements | Descriptive claims about factual reality | Empirical data on practices, attitudes, behaviors |
| Ought-Statements | Prescriptive claims about moral obligations | Ethical recommendations, guidelines, policies |
| Direct Inference | Attempt to derive ought from is without justification | Logically problematic; commits naturalistic fallacy |
| Indirect Methodologies | Structured approaches to connect facts and values | Empirical bioethics methods; justified integration |
The Philosophical Foundation: Hume's Guillotine
Historical Origin and Definition
David Hume first identified the is-ought problem in his 1739 work "A Treatise of Human Nature," noting a troubling pattern in moral systems where authors seamlessly transition from descriptive to prescriptive language without explanation or justification [49]. This observation led to what is now termed Hume's law or Hume's guillotine – the thesis that ethical conclusions cannot be logically inferred from purely descriptive factual statements alone [49]. The central issue lies in the categorical difference between statements about what exists in the world and statements about what should be valued or pursued.
Logical Structure of the Problem
The logical problem emerges because moral statements contain an element that cannot be found in purely descriptive statements. As Hume observed, ought statements "express some new relation or affirmation" that requires explanation [49]. In modern terms, moral language typically includes a prescriptive force that factual language lacks. While descriptive statements can be verified through observation or measurement, prescriptive statements invoke values, duties, or ideals that transcend mere description. This creates a logical gap that cannot be crossed without additional moral premises.
Contemporary Manifestations in Bioethics Research
The Empirical Turn in Bioethics
Bioethics has witnessed a significant empirical turn in recent decades, with a substantial increase in the use of qualitative and quantitative social science methods to investigate ethical questions [51]. One survey of bioethics researchers across twelve European countries found that 87.5% use or have used empirical methods in their work [51]. This interdisciplinary approach promises more context-sensitive and practically relevant ethics, but simultaneously intensifies the methodological challenge of integrating empirical findings with normative analysis.
The Integration Challenge
The fundamental challenge in empirical bioethics lies in the integration problem – how to meaningfully connect empirical data with normative reasoning without committing logical fallacies [1]. Research indicates this integration remains methodologically vague in practice. A 2023 qualitative study of bioethics scholars revealed significant uncertainty about integration methods, with approaches often described as frustratingly vague and insufficiently determinate in practical contexts [1]. This vagueness represents a double-edged sword, allowing flexibility while potentially obscuring poor methodological rigor.
Table: Survey Data on Empirical Methods in Bioethics (n=200 Researchers)
| Research Practice | Percentage | Significance |
|---|---|---|
| Use empirical methods | 87.5% | Widespread adoption of empirical approaches |
| Received methodological training | ~60% | Substantial portion lack formal training |
| Self-identify as expert in methods used | ≤6% | Limited methodological confidence |
| Attempted empirical-normative integration | 35% | Minority actively address the core challenge |
Why Direct Inference Fails: Theoretical and Practical Barriers
Logical and Theoretical Barriers
Direct inference from empirical data to normative conclusions fails for several theoretical reasons. First, it violates the logical principle that conclusions cannot contain information not present in the premises [49]. Second, it ignores the diversity of moral frameworks that might interpret the same facts differently [50]. For example, the same data about end-of-life decision-making might be interpreted differently through utilitarian, deontological, or virtue ethics frameworks [50]. Third, direct inference typically commits the naturalistic fallacy, erroneously deriving moral properties from natural properties without justification [49].
Epistemological Differences
The failure of direct inference also stems from fundamental epistemological differences between empirical and normative inquiry. Empirical research typically aims for descriptive accuracy, while normative ethics concerns prescriptive justification [50]. These different aims require different forms of reasoning and evidence. As one analysis notes, philosophical-ethical theories "do not primarily aim to fit the world as it is, but to guide human agency," creating a reverse "direction of fit" compared to empirical theories [50].
Pluralism of Ethical Theories
The plurality of competing ethical theories further complicates direct inference. Different theoretical frameworks (consequentialist, deontological, virtue-based, etc.) may generate divergent practical recommendations from the same empirical data [50]. This pluralism creates what one researcher describes as a problem of "theory selection" in empirical-ethical research [50]. Without explicit justification for why one theoretical framework is more appropriate than others for a given context, any direct inference from facts to values remains theoretically arbitrary.
Methodological Alternatives: Beyond Direct Inference
Reflective Equilibrium
Reflective equilibrium represents one prominent methodological alternative to direct inference. This coherence-seeking approach involves iterative adjustment between ethical principles, intuitive judgments about cases, and relevant empirical facts until a state of equilibrium is reached [1] [53]. Rather than deriving ought from is, this method treats empirical data as one element in a broader process of ethical reflection. In practice, this often takes the form of "back-and-forth" methods where researchers move between empirical data and normative analysis [1].
Dialogical Approaches
Dialogical empirical ethics represents another alternative methodology that engages stakeholders directly in ethical deliberation. This approach relies on structured dialogues between researchers, practitioners, and other stakeholders to reach shared understanding and normative conclusions [1] [53]. Unlike direct inference, dialogical approaches treat ethical norms as emerging from collaborative reasoning processes rather than being derived from empirical data. These methods position participants as co-investigators in the normative analysis [1].
Implementation Science Framework
A more recent approach applies implementation science to bridge the ought-is gap through what has been termed the "ought-is problem" – how to implement ethical norms in practice [54]. This framework recognizes that moving from normative claims to practical implementation requires systematic attention to intervention characteristics, contextual factors, and implementation processes [54]. The Consolidated Framework for Implementation Research (CFIR) offers one structured approach to address these challenges [54].
Experimental Protocols for Empirical Bioethics Research
Protocol 1: Reflective Equilibrium in Practice
Purpose: To achieve coherence between empirical findings and normative analysis through iterative reflection.
Procedure:
- Data Collection: Gather empirical data through qualitative or quantitative methods relevant to the ethical question.
- Initial Coding: Systematically code and analyze empirical data using standard social science methods.
- Formulate Preliminary Normative Framework: Identify relevant ethical principles, theories, and considered judgments.
- Test Coherence: Examine how well the preliminary framework aligns with empirical findings.
- Iterative Adjustment: Revise either the normative framework or interpretation of empirical data to achieve greater coherence.
- Achieve Equilibrium: Continue adjustment until no further revisions are needed to maintain coherence.
Methodological Considerations: This approach requires transparency about which elements were revised during the process and why. Researchers should document the reasoning behind each adjustment [1] [53].
Protocol 2: Dialogical Integration Method
Purpose: To generate normative conclusions through structured stakeholder dialogue.
Procedure:
- Participant Selection: Identify and recruit diverse stakeholders with relevant perspectives and experiences.
- Data Generation: Conduct focus groups or interviews to elicit stakeholder views and experiences.
- Structured Dialogue: Facilitate deliberative discussions where stakeholders engage with ethical dimensions of the issue.
- Collaborative Analysis: Work with participants to identify ethically significant themes and patterns.
- Normative Development: Support stakeholders in developing shared normative positions.
- Validation: Return to participants to verify interpretations and conclusions.
Methodological Considerations: This method positions the researcher as a facilitator rather than external analyst. Quality criteria include representativeness of participants, quality of deliberation, and transparency about power dynamics [1].
Protocol 3: Implementation Science Approach
Purpose: To translate ethical norms into practice through implementation principles.
Procedure:
- Norm Specification: Transform aspirational norms into specific, actionable norms.
- Intervention Design: Develop concrete interventions to enact the specific norms.
- Context Analysis: Identify barriers and facilitators across intervention characteristics, outer setting, inner setting, and individual characteristics.
- Implementation Process: Develop a systematic process for introducing and sustaining the intervention.
- Evaluation: Measure implementation outcomes including feasibility, fidelity, and sustainability.
- Dissemination: Share successful implementation strategies and best practices.
Methodological Considerations: This approach requires early attention to feasibility during norm specification and collaboration with implementation experts [54].
Table: Research Reagent Solutions for Empirical Bioethics
| Tool/Resource | Function | Application Context |
|---|---|---|
| Qualitative Analysis Software (e.g., NVivo, MAXQDA) | Facilitates systematic coding and analysis of qualitative data | Thematic analysis of interview/focus group data [1] |
| Consolidated Framework for Implementation Research | Identifies barriers/facilitators to implementing ethical norms | Translating ethical guidelines into practice [54] |
| Delphi Method Protocols | Structured communication for achieving expert consensus | Developing standards of practice in emerging areas [52] |
| Mixed-Methods Research Designs | Integrates qualitative and quantitative approaches | Comprehensive understanding of complex ethical issues [51] |
| Reflective Equilibrium Templates | Guides iterative normative-empirical alignment | Achieving coherence between data and ethical theory [1] [53] |
Standards of Practice for Empirical Bioethics Research
In response to methodological challenges in empirical bioethics, consensus projects have developed standards of practice to ensure methodological rigor. One such project reached agreement on 15 standards organized into 6 domains [52]:
- Aims: Clear specification of research aims and how empirical and normative components interrelate.
- Questions: Research questions should reflect the interdisciplinary nature of the inquiry.
- Integration: Explicit description and justification of integration methodology.
- Conduct of Empirical Work: Appropriate empirical methods with quality measures.
- Conduct of Normative Work: Rigorous normative analysis with philosophical justification.
- Training & Expertise: Research team should possess or develop both empirical and normative expertise.
These standards emphasize that successful empirical bioethics requires more than simply combining empirical data with ethical speculation. It demands systematic methodology and transparent reasoning about how empirical and normative elements interrelate [52].
The problem of direct inference from 'is' to 'ought' remains a fundamental challenge for bioethics research, but not an insurmountable one. By recognizing the logical limits of direct inference and adopting structured methodological alternatives, researchers can produce ethically robust and empirically informed analyses. The field has moved beyond simple dualisms to develop sophisticated integration methodologies that respect the distinctive contributions of both empirical and normative inquiry.
For researchers, scientists, and drug development professionals, these methodological insights offer practical pathways to address ethical questions without committing logical fallacies. The continued development and refinement of these approaches represents one of the most important frontiers for advancing bioethics as a discipline that is both philosophically rigorous and empirically grounded.
The field of bioethics is increasingly characterized by its embrace of both normative ethical analysis and empirical research. This interdisciplinary approach recognizes that complex ethical challenges in healthcare and drug development require an understanding of both theoretical principles and real-world contexts. However, a significant tension persists regarding how much weight should be given to empirical data versus ethical theory when these approaches yield different perspectives [1]. The integration of these seemingly disparate approaches remains methodologically challenging, with many scholars reporting uncertainty and vagueness in their attempts to combine empirical findings with normative analysis [1].
This application note addresses these challenges by providing structured frameworks and practical protocols for researchers navigating the complex relationship between empirical evidence and ethical theory. The guidance is particularly relevant for professionals in pharmaceutical development, clinical research, and bioethics who must balance rigorous empirical investigation with robust ethical analysis throughout the research lifecycle.
Theoretical Foundations: From Tension to Integration
The Philosophical Landscape
The relationship between empirical data and ethical theory has long been dominated by the is-ought problem, which questions whether empirical facts ("is") can directly determine ethical prescriptions ("ought") [6]. This philosophical challenge has significant practical implications for bioethics research, as it creates methodological uncertainty about how empirical findings should inform normative conclusions.
Recent analysis of empirical research integrity from 2015 to 2023 reveals a noteworthy shift in how ethical problems are conceptualized. The previously dominant "Bad Apple" hypothesis, which focuses on individual transgressions, has declined from 54% to 30%, while the "Wicked System" hypothesis, which emphasizes systemic flaws, has increased from 46% to 52% [55]. This trend reflects growing recognition that ethical challenges often require systemic solutions rather than merely addressing individual misconduct.
Current Methodological Approaches
Several methodological frameworks have emerged to facilitate the integration of empirical and normative approaches:
- Reflective Equilibrium: A back-and-forth process where researchers move between ethical principles and empirical data to achieve moral coherence [1]
- Dialogical Empirical Ethics: Relies on stakeholder dialogue to reach shared understanding of analysis and conclusions [1]
- Consultative Approaches: Feature independent researcher analysis of data to develop normative conclusions [1]
Despite these frameworks, qualitative studies reveal that researchers experience significant vagueness and uncertainty about integration methods, which can obscure understanding of theoretical-methodological underpinnings [1]. This methodological ambiguity represents a critical challenge for the field.
Table: Key Ethical Theories and Their Application to Empirical-Normative Integration
| Ethical Theory | Core Principle | Relevance to Integration | Primary Limitations |
|---|---|---|---|
| Utilitarianism | Maximizing net utility | Supports using empirical data to calculate consequences | Difficult to quantify all relevant values |
| Deontology | Adherence to moral duties | Emphasizes normative principles as constraints | Potential conflict between obligations |
| Virtue Ethics | Moral character development | Focuses on researcher virtues in interpretation | Less specific action guidance |
Hierarchical Framework for Empirical Bioethics Research
A hierarchical construct for classifying empirical research in bioethics provides a structured approach to integration [2]. This framework organizes research into four progressive categories, each with distinct objectives and methodological considerations.
The Four-Level Hierarchy
Table: Hierarchical Levels of Empirical Research in Bioethics
| Level | Category | Primary Research Question | Example Studies | Normative Weight |
|---|---|---|---|---|
| 1 | Lay of the Land | What are current practices, opinions, or beliefs? | Attitudes toward end-of-life care; ethics committee composition | Low: Primarily descriptive |
| 2 | Ideal vs. Reality | To what extent does practice match ethical ideals? | Healthcare disparities research; informed consent comprehension | Medium: Identifies gaps |
| 3 | Improving Care | How can practice be aligned with ethical ideals? | Interventions to reduce disparities; consent process improvements | High: Informs interventions |
| 4 | Changing Ethical Norms | Should ethical norms be revised based on evidence? | Syntheses of multiple studies challenging existing norms | Highest: Challenges principles |
Research Protocols for Each Level
Protocol 3.2.1: Lay of the Land Studies
- Objective: Describe current practices, opinions, or beliefs regarding a bioethical issue
- Methodology Options: Cross-sectional surveys, qualitative interviews, focus groups
- Sample Size Determination: Power analysis for quantitative studies; saturation model for qualitative approaches
- Data Analysis: Descriptive statistics for quantitative data; thematic analysis for qualitative data
- Normative Considerations: Ensure question framing does not presuppose ethical positions
Protocol 3.2.2: Ideal Versus Reality Studies
- Objective: Assess the alignment between actual practices and established ethical norms
- Methodology Options: Comparative analysis, audit studies, structured observation
- Key Measures: Gap analysis metrics, compliance rates, discrepancy measures
- Confounding Control: Multivariate analysis, propensity scoring, matched designs
- Normative Considerations: Clearly articulate the ethical ideal being assessed
Visualizing the Integration Process
The following diagram illustrates the dynamic process of integrating empirical research with normative analysis, highlighting key decision points and feedback mechanisms:
This workflow emphasizes the iterative nature of integration, where empirical findings and normative analysis inform and refine each other through multiple cycles of reflection and testing. The feedback loop from Normative Refinement back to Empirical Testing represents the critical process of empirically testing refined ethical norms [2].
Researcher Perspectives on Acceptable Objectives
Understanding how researchers view the objectives of empirical bioethics research is essential for developing realistic integration protocols. A qualitative exploration of researchers' views revealed varying levels of acceptance for different objectives [6].
Consensus and Controversy in Research Objectives
- Highly Accepted Objectives: Understanding the context of bioethical issues and identifying ethical issues in practice received unanimous agreement among researchers [6]
- Moderately Accepted Objectives: Using empirical research to test ethical recommendations and evaluate how they work in practice
- Contested Objectives: Using empirical research to draw normative recommendations and develop/justify moral principles generated significant disagreement [6]
Protocol for Managing Divergent Perspectives
Protocol 5.2.1: Interdisciplinary Team Management
- Team Composition: Include empirical researchers, normative ethicists, and domain experts
- Communication Framework: Establish shared vocabulary and respect for different epistemological traditions
- Conflict Resolution: Develop protocols for addressing methodological disagreements
- Authorship Guidelines: Clearly define contributions across empirical and normative dimensions
Application to Pharmaceutical Ethics and Drug Development
The integration of empirical data and ethical theory has particular significance in pharmaceutical development, where ethical decisions have profound implications for patient safety, public trust, and regulatory compliance.
Ethical Frameworks for Clinical Trial Design
Recent updates to clinical trial protocols, including the SPIRIT 2025 statement, emphasize transparency and ethical considerations in trial design [46]. These guidelines incorporate greater attention to patient and public involvement, data sharing policies, and detailed harm assessment protocols.
Protocol 6.1.1: Ethical Clinical Trial Protocol Development
- Stakeholder Engagement: Involve patient representatives throughout protocol development
- Risk-Benefit Analysis: Systematically assess and document potential harms and benefits
- Data Transparency: Develop clear plans for data sharing and results dissemination
- Ethics Review: Submit to research ethics committees for independent review
Regulatory Compliance and Ethical Integration
The 2025 FDAAA 801 Final Rule introduces stricter requirements for clinical trial registration and results reporting [56]. These regulatory changes reflect growing emphasis on transparency and accountability in pharmaceutical research.
Table: Key Regulatory Changes and Their Ethical Implications
| Regulatory Change | Implementation Timeline | Ethical Principle | Data Requirement |
|---|---|---|---|
| Shortened Results Submission | 9 months (previously 12) | Timeliness | Primary completion date documentation |
| Real-Time Noncompliance Notification | Immediate upon implementation | Accountability | Compliance monitoring systems |
| Mandatory Informed Consent Posting | Phase-in period | Transparency | Redacted consent documents |
| Expanded ACT Definition | Specific effective date | Justice | Broader trial classification |
The Scientist's Toolkit: Essential Research Reagents
Successful integration of empirical and normative approaches requires specific methodological tools and frameworks. The following table details essential "research reagents" for this interdisciplinary work.
Table: Essential Reagents for Empirical-Normative Integration Research
| Tool Category | Specific Tool/Technique | Primary Function | Application Context |
|---|---|---|---|
| Empirical Methods | Semi-structured interviews | Explore stakeholder perspectives | Lay of the Land studies |
| Structured surveys | Quantify attitudes and practices | Ideal vs. Reality studies | |
| Systematic observation | Document actual behaviors | Improving Care studies | |
| Normative Frameworks | Principlism | Apply mid-level principles | Clinical ethics consultation |
| Reflective equilibrium | Achieve coherence between theory and data | All integration contexts | |
| Casuistry | Case-based reasoning | Protocol development | |
| Integration Methods | Dialogical workshops | Facilitate stakeholder dialogue | Controversial ethical issues |
| Joint analysis sessions | Collaborative interpretation | Interdisciplinary teams | |
| Scenario testing | Test normative frameworks | Policy development |
The integration of empirical data and ethical theory remains a challenging but essential endeavor for contemporary bioethics research, particularly in pharmaceutical development and clinical research. By applying the structured frameworks, explicit protocols, and visual guides presented in this application note, researchers can navigate the complex terrain between "is" and "ought" with greater methodological rigor and transparency.
The field continues to evolve toward more sophisticated integration approaches that recognize the complementary strengths of empirical and normative methods. Future development should focus on creating more precise guidelines for weighting empirical evidence in normative conclusions, while maintaining the distinctive contributions of ethical theory to bioethical analysis.
Collaborative bioethics research, which integrates empirical findings with normative analysis, presents distinct challenges in authorship ethics. The growth of this interdisciplinary field, where empirical data informs ethical argumentation, necessitates transparent and fair authorship practices to maintain scientific integrity and accountability [1] [18]. The International Committee of Medical Journal Editors (ICMJE) has established criteria for authorship that are widely adopted across health sciences journals, requiring substantial contributions to: (1) conception/design or data acquisition/analysis/interpretation; (2) drafting or critically revising the work; (3) final approval; and (4) accountability for all aspects of the work [57]. However, practical application of these criteria in bioethics collaborations is complicated by disciplinary diversity, power differentials, and the integrative nature of empirical-normative research [58] [59]. This document provides application notes and experimental protocols to navigate these complexities, ensuring accountability and fairness in authorship practices specific to collaborative bioethics research.
Quantitative Landscape of Empirical Bioethics Research
Historical Growth and Methodological Approaches
Empirical research in bioethics has demonstrated significant growth, indicating the expanding relevance of empirical-normative integration. The table below summarizes the prevalence and methodological characteristics of empirical studies in nine leading bioethics journals from 1990-2003:
Table 1: Empirical Research in Bioethics Journals (1990-2003) [18]
| Journal | Total Empirical Articles (1990-2003) | Percentage of Total Content | Primary Research Paradigm |
|---|---|---|---|
| Nursing Ethics | 145 | 39.5% | Quantitative (64.6% across all journals) |
| Journal of Medical Ethics | 128 | 16.8% | Mixed Methods |
| Journal of Clinical Ethics | 93 | 15.4% | Qualitative |
| Cambridge Quarterly of Healthcare Ethics | 21 | 6.9% | Not Specified |
| Bioethics | 22 | 6.6% | Not Specified |
| Hastings Center Report | 14 | 3.3% | Not Specified |
| Kennedy Institute of Ethics Journal | 5 | 2.2% | Not Specified |
| Theoretical Medicine and Bioethics | 4 | 1.9% | Not Specified |
| Christian Bioethics | 3 | 1.5% | Not Specified |
| Total Across All Journals | 435 | 10.8% | Quantitative predominates |
The data reveal a statistically significant increase (χ² = 49.0264, p<0.0001) in empirical studies between 1990-1996 (n=126) and 1997-2003 (n=309), confirming the growing importance of empirical approaches in bioethics [18]. This expansion necessitates clear authorship frameworks to manage the complexities of collaborative empirical-normative research.
Foundational Ethical Framework for Authorship
Core Authorship Criteria and Responsibilities
The ICMJE criteria provide the foundational framework for ethical authorship. The following workflow outlines the sequential application of these criteria in collaborative bioethics research:
Figure 1: Authorship Determination Workflow for Collaborative Bioethics Research
Role-Specific Responsibilities in Collaborative Teams
Collaborative bioethics research benefits from clearly defined role expectations, which should be established early in the research process:
Table 2: Author Role Responsibilities in Collaborative Bioethics Research [60] [61]
| Role | Primary Responsibilities | Empirical-Normative Considerations |
|---|---|---|
| First Author | Leads design, execution, data collection/analysis; drafts manuscript; coordinates revisions; ensures data accuracy | Must bridge empirical and normative domains; integrate methodological approaches; address is-ought distinctions |
| Middle Authors | Contribute to specific aspects (methodology, analysis, interpretation); review drafts; approve final manuscript | Provide specialized expertise in either empirical or normative methods; facilitate integration between approaches |
| Senior/Last Author | Provides conceptual guidance, funding, resources; ensures research integrity; supervises junior researchers | Oversees integrative approach; ensures ethical coherence; manages power dynamics in collaboration |
| Corresponding Author | Handles journal communication; ensures administrative completeness; post-publication responses | Coordinates interdisciplinary team input; manages divergent disciplinary expectations and timelines |
| Non-Author Contributors | Technical support, data collection, language editing (acknowledged but not authors) | May include empirical research assistants, philosophical consultants, or specialized editors |
Application Notes for Bioethics-Specific Challenges
Addressing Language and Power Imbalances
Global health research partnerships between low-middle income countries (LMICs) and high-income countries (HICs) present particular ethical challenges in authorship attribution [59]. The requirement for English-language drafting and revision (ICMJE Criterion #2) may systematically exclude non-English speaking researchers who have made substantial intellectual contributions to the conception, design, or data interpretation [59]. To promote equity:
- Provide professional translation services for colleagues who draft sections in their native language
- Establish writing mentorship partnerships between native and non-native English speakers
- Allocate specific budgetary resources for language support in grant proposals
- Recognize that linguistic disadvantage should not preclude authorship eligibility when substantive intellectual contributions exist
Navigating Empirical-Normative Integration Methods
The methodological pluralism in empirical-ethical research creates unique authorship considerations. Researchers should transparently report their integration approach, which may include:
- Reflective Equilibrium: Back-and-forth justification between ethical principles and empirical data [1]
- Dialogical Empirical Ethics: Stakeholder dialogue to reach shared understanding [1]
- Inherent Integration: Normative and empirical dimensions intertwined from project inception [1]
Each method implies different forms of intellectual contribution, which should be explicitly documented in authorship contribution statements.
Experimental Protocols for Authorship Determination
Protocol 1: Establishing Authorship Expectations at Project Initiation
Purpose: To prevent authorship disputes through transparent early communication and agreement.
Materials: Project description document; ICMJE criteria; discipline-specific standards; authorship discussion tool.
Procedure:
- Initial Team Meeting: Convene all potential collaborators during project conceptualization
- Criteria Review: Distribute and discuss ICMJE authorship criteria [57] and discipline-specific norms
- Contribution Forecasting: Identify anticipated substantive contributions from each team member
- Authorship Planning: Develop provisional authorship list and order based on projected contributions
- Documentation: Record agreements in written document circulated to all team members [61]
- Revision Mechanism: Establish process for modifying agreements as project evolves
Validation: A study of authorship practices found that teams implementing structured early discussions reported fewer disputes and fairer attribution of credit [62].
Protocol 2: Managing Authorship Across Empirical-Normative Divides
Purpose: To ensure appropriate credit for interdisciplinary contributions in bioethics research.
Materials: Contribution taxonomy template; integration methodology documentation; regular meeting schedule.
Procedure:
- Methodology Mapping: Explicitly document how empirical and normative elements will be integrated [26]
- Contribution Tracking: Maintain records of substantive intellectual contributions from all team members using standardized taxonomies (e.g., CRediT) [61]
- Integration Documentation: Specifically record contributions to the empirical-normative integration process
- Regular Review: Schedule quarterly authorship reviews to assess contribution alignment with projections
- Barrier Identification: Proactively identify and address obstacles to equitable participation (e.g., language barriers, methodological unfamiliarity)
- Final Verification: Prior to submission, confirm all authors meet ICMJE criteria and approve manuscript
Validation: Research indicates that explicit methodology documentation and regular communication reduce interdisciplinary conflicts and promote attributional equity [1] [26].
Table 3: Research Reagent Solutions for Authorship Ethics [60] [61]
| Tool/Resource | Function | Application Context |
|---|---|---|
| ICMJE Criteria Document | Defines universal standards for authorship | Baseline reference for all collaborative research projects; journal requirements |
| CRediT Taxonomy | Standardized classification of 14 contributor roles | Precise documentation of specific contributions beyond basic authorship criteria |
| Authorship Discussion Tool | Structured questionnaire to facilitate authorship conversations | Early project stages and when resolving disputes; ensures comprehensive consideration |
| Contribution Tracking System | Documented record of intellectual inputs | Ongoing documentation throughout project lifecycle; evidence for authorship decisions |
| Institutional Authorship Guidelines | Discipline-specific standards and processes | Contextualizing universal principles to specific research domains and methodologies |
| AI Use Disclosure Framework | Guidelines for reporting AI-assisted technology | Transparent acknowledgment of AI contributions without qualifying for authorship |
Ensuring accountability and fairness in collaborative bioethics research requires deliberate implementation of structured authorship protocols that address the field's unique empirical-normative integration challenges. By adopting the application notes and experimental protocols outlined above, research teams can navigate the complexities of interdisciplinary collaboration while maintaining ethical integrity. The increasing prominence of empirical approaches in bioethics [18] makes such frameworks essential for promoting equitable practices that respect all forms of intellectual contribution, whether empirical or normative in nature.
The biopharmaceutical industry operates at the complex intersection of life sciences, clinical research, clinical care, public health, and business, presenting distinct ethical challenges that demand more than theoretical analysis [63]. Operationalizing ethics requires the successful integration of normative bioethics (concepts, principles, and rules) with empirical research (data on practices, outcomes, and contexts) to create actionable guidance for industry professionals [64] [63]. This integration is essential for navigating the "gray areas" that lack specific policy guidelines, such as clinical trial diversity, use of big data, access to medicines, and managing drug shortages [63].
Despite consensus on the importance of empirical bioethics, methodological vagueness often surrounds the integration process, creating both flexibility and theoretical obscurity [64] [7]. This document provides structured Application Notes and Protocols to bridge this gap, translating ethical norms into practical frameworks tailored to the biopharmaceutical context. Through clearly defined processes, decision-making models, and evaluation metrics, we establish a reproducible methodology for implementing ethics across the research, development, supply, commercialization, and clinical use of biopharmaceutical products [63].
Theoretical Foundation and Integration Methodology
Conceptual Framework for Biopharmaceutical Bioethics
Biopharmaceutical bioethics is defined as "the application of bioethics norms (concepts, principles, and rules) to the research, development, supply, commercialization, and clinical use of biopharmaceutical healthcare products" [63]. This definition establishes a scope comprehensive enough to address the full product lifecycle yet specific enough to provide meaningful guidance. The application of bioethics norms occurs at two levels: (1) company guidance level (policies and positions) and (2) case-specific level (individual project decisions) [63].
Table 1: Bioethics Specification Across Domains
| Ethics Domain | Primary Focus | Key Specifications for Biopharmaceutical Context |
|---|---|---|
| Research Ethics | Well-being of research participants | Adaptive trial designs, diversity in participant selection, data transparency |
| Clinical Ethics | Individual patient treatment | Risk-benefit assessment, patient-focused development, quality of life considerations |
| Public Health Ethics | Societal health interventions | Access to medicines, responsible pricing, drug shortage management, global equity |
Empirical-Normative Integration Methods
Three primary methodological approaches for integrating empirical findings with normative analysis have been identified in bioethics research [64] [7]:
Consultative Methods (e.g., Reflective Equilibrium): The researcher acts as an external thinker who engages in a "back-and-forth" process between ethical principles and empirical data to achieve moral coherence [7]. This approach positions the researcher as the primary integrator who balances ethical theories with observed practices and outcomes.
Dialogical Methods: Collaboration among multiple stakeholders is viewed as the optimal integration mechanism. Through structured dialogue, researchers, industry professionals, patients, and other stakeholders collectively develop ethical guidance [64] [7]. This approach embraces the view that ethical understanding emerges from multi-stakeholder deliberation.
Inherent Integration Approaches: The normative and empirical dimensions are intertwined from a project's inception, with data collection and ethical analysis occurring concurrently rather than sequentially [64]. This method seeks to overcome the artificial separation between facts and values throughout the research process.
Diagram 1: Empirical-Normative Integration
Contextual Framework for Biopharmaceutical Applications
Industry-Specific Contextual Factors
The application of bioethics norms to the biopharmaceutical industry requires careful consideration of five contextual factors that distinguish this environment from other healthcare settings [63]:
Dual Missions: Balancing patient health priorities with business sustainability imperatives creates unique ethical tensions that require explicit acknowledgment and management.
Timely and Pragmatic Guidance: The rapid pace of innovation and competitive markets necessitates ethics frameworks that provide practical direction within operational timeframes.
Resource Stewardship: Responsible management of finite resources (financial, human, manufacturing) represents an ethical imperative that must be balanced against other considerations.
Multiple Stakeholders: Ethical decisions must account for diverse perspectives including patients, healthcare professionals, regulators, payers, investors, and communities.
Operational Complexity: Global operations with varying regulatory requirements, cultural norms, and healthcare systems create implementation challenges for standardized ethical frameworks.
Values-Based Decision-Making Protocol
A values-based decision-making model provides a structured approach for addressing ethical questions in the biopharmaceutical context [65]. This five-step process integrates company values with contextual factors to guide prospective decision-making:
Table 2: Five-Step Decision-Making Protocol
| Step | Process | Key Actions | Output |
|---|---|---|---|
| 1. Problem Definition | Articulate the specific ethical question | Identify stakeholders, gather background information, frame the decision point | Clear problem statement with context |
| 2. Option Generation | Develop potential solutions | Brainstorm multiple approaches, consult diverse perspectives | 3-5 viable decision options |
| 3. Values Assessment | Evaluate options against core values | Apply TRIP values (Transparency, Respect, Integrity, Patient-focus) and TIPP contextual factors | Values-based ranking of options |
| 4. Decision & Implementation | Select and execute optimal path | Choose best option, develop implementation plan, assign responsibilities | Action plan with timeline and metrics |
| 5. Evaluation & Learning | Assess outcomes and refine approach | Monitor implementation, evaluate results, document lessons learned | Continuous improvement of decision framework |
Application Notes: Implementing Ethics Frameworks
Values Specification and Operationalization
Corporate values must be explicitly defined and translated into practical guidance to ensure consistent application. The following table demonstrates how abstract values can be operationalized through specific framing questions [65]:
Table 3: Values Operationalization Framework
| Value | Definition | Framing Questions for Application | Contextual Factors (TIPP) |
|---|---|---|---|
| Transparency | Ensuring communications are fair, honest, and not misleading; providing timely, relevant, accurate information | How will we inform relevant stakeholders and share this decision? How will we document the solution? | Timing, Perception |
| Respect | Actively seeking, valuing, and drawing on differing knowledge, perspectives, experience; creating atmosphere of trust | Have all perspectives/stakeholders been considered? How does this solution build trust? | Proportionality, Perception |
| Integrity | Acting legally and fairly within spirit of laws and policies; making realistic commitments and keeping promises | Would you be comfortable discussing this solution with family/in public? Is it compliant with regulations and policies? | Intent, Proportionality |
| Patient Focus | Prioritizing patient and consumer needs in research; ensuring safety is paramount | How does this solution put patient/trial participant interests first? How are potential risks managed? | Intent, Proportionality, Timing |
Case Study Application: Clinical Trial Diversity
Protocol 1: Enhancing Representation in Clinical Trials
Background: Despite ethical mandates and scientific necessity, many clinical trials fail to adequately represent diverse populations, limiting generalizability and equity in access to innovative therapies.
Integration Methodology: Dialogical empirical ethics approach combining stakeholder engagement with normative analysis of justice principles.
Procedure:
- Empirical Data Collection:
- Conduct systematic audit of recent trial demographics compared to disease epidemiology
- Survey trial sites to identify structural barriers to diverse participation
- Interview underrepresented communities to understand participation concerns
Stakeholder Dialogue:
- Convene multi-stakeholder panel including patients, investigators, regulators, community representatives
- Facilitate structured discussions using the values-based decision framework
- Identify specific barriers and potential solutions through collaborative problem-solving
Normative Analysis:
- Apply principle of justice to evaluate current practices and proposed solutions
- Assess alignment with respect for persons through enhanced informed consent processes
- Evaluate beneficence through potential improvements in drug safety and efficacy across populations
Implementation Strategy:
- Develop specific diversity targets based on disease epidemiology
- Implement community engagement protocols prior to trial initiation
- Address practical barriers (transportation, compensation, cultural sensitivity)
- Establish monitoring and reporting mechanisms for diversity metrics
Evaluation Metrics:
- Percentage increase in underrepresented population enrollment
- Reduction in barrier severity ratings from site surveys
- Improvement in diversity of patient advisory board composition
Experimental Protocols and Assessment Tools
Ethics Integration Assessment Protocol
Objective: Systematically evaluate the effectiveness of ethics integration in decision-making processes across the organization.
Materials:
- Pre-defined evaluation rubric
- Stakeholder feedback mechanisms
- Decision documentation templates
- Ethics integration dashboard
Procedure:
- Baseline Assessment:
- Document current decision-making processes for 3-5 recent projects
- Identify where and how ethical considerations were incorporated
- Map stakeholders involved in each decision point
Intervention Implementation:
- Introduce values-based decision framework through targeted workshops
- Establish ethics consultation service for complex cases
- Implement standardized documentation for ethical decision rationale
Post-Intervention Evaluation:
- Track application of framework in subsequent projects
- Measure time from problem identification to resolution
- Assess stakeholder satisfaction with decision processes
- Evaluate consistency of value application across similar cases
Continuous Improvement:
- Establish regular review cycles for ethics framework application
- Create mechanism for updating values specification based on experience
- Develop case library of ethical decisions for organizational learning
Analysis: Compare pre- and post-intervention metrics for decision quality, stakeholder satisfaction, and alignment with organizational values.
Multi-Stakeholder Consensus Framework
Objective: Establish a reproducible process for achieving ethical alignment across diverse stakeholders on contentious issues.
Integration Methodology: Combined dialogical and consultative approach with iterative refinement.
Procedure:
- Stakeholder Mapping:
- Identify all relevant stakeholders for the specific ethical question
- Categorize by perspective (patients, clinicians, researchers, business, regulators)
- Ensure representation of minority and vulnerable viewpoints
Structured Dialogue:
- Facilitate initial stakeholder meeting to frame the ethical question
- Employ neutral facilitation to ensure balanced participation
- Use case studies to ground abstract principles in practical realities
Draft Framework Development:
- Synthesize stakeholder input into draft guidance document
- Clearly articulate areas of agreement and remaining分歧
- Specify implementation considerations and potential challenges
Iterative Refinement:
- Circulate draft framework for stakeholder feedback
- Modify based on substantive input while maintaining ethical coherence
- Conduct second stakeholder meeting to refine and finalize
Implementation and Review:
- Establish governance structure for framework application
- Set review timeline based on issue volatility and emerging evidence
- Create amendment process for framework evolution
Diagram 2: Consensus Framework Development
Table 4: Research Reagent Solutions for Ethics Integration
| Tool/Resource | Function | Application Context | Implementation Considerations |
|---|---|---|---|
| Values Specification Guide | Translates abstract values into practical questions | Decision-making at all levels; policy development | Requires organizational commitment; needs periodic updating |
| Stakeholder Mapping Template | Identifies relevant stakeholders and their perspectives | New project initiation; ethical issue resolution | Should include internal and external stakeholders; assess influence and interest |
| Ethics Integration Dashboard | Tracks ethics metrics and framework application | Organizational monitoring; compliance reporting | Must balance transparency with practical constraints; avoid reductionism |
| Case Library | Documents previous ethical decisions and rationales | Organizational learning; new employee training | Requires careful anonymization; should include diverse case types |
| Multi-Stakeholder Dialogue Protocol | Facilitates structured engagement across diverse groups | Contentious issues; policy development | Needs skilled facilitation; requires time investment; cultural sensitivity |
| Normative-Empirical Integration Rubric | Assesses quality of ethics integration in projects | Research evaluation; continuous improvement | Should be validated across different project types and contexts |
Operationalizing ethics in the biopharmaceutical industry requires moving beyond theoretical compliance to embedded ethical practice. The Application Notes and Protocols presented here provide a structured approach for contextualizing normative bioethics principles through empirical engagement with the realities of drug development and commercialization. By implementing these frameworks, organizations can navigate complex ethical terrain while maintaining alignment with their mission to serve patients and society.
Successful implementation requires commitment to ongoing evaluation and refinement of ethics integration processes. Organizations should establish clear metrics for assessing the effectiveness of their ethics frameworks, create mechanisms for organizational learning from both successes and challenges, and maintain openness to external perspectives through transparent stakeholder engagement. Through such systematic approaches, the biopharmaceutical industry can fulfill its ethical obligations while advancing medical innovation.
Evaluating Success: Validating Integrated Approaches and Comparative Framework Analysis
The integration of normative (ethical) analysis with empirical (descriptive) data constitutes the defining methodology and central challenge for contemporary empirical bioethics research [1]. This interdisciplinary endeavor seeks to generate normative conclusions that are both philosophically sound and empirically grounded in the realities of clinical practice and human experience [52]. Despite the proliferation of methodological approaches, the process of integration often remains opaque, with researchers reporting significant uncertainty and vagueness in their methodological practices [1]. This document establishes clear benchmarks for achieving rigor, transparency, and justification in the integration process, providing actionable standards for researchers, scientists, and drug development professionals working at the intersection of ethics and empirical science.
Foundational Standards for Research Practice
A consensus project involving European bioethics scholars established foundational standards for empirical bioethics research, organized into six key domains [52]. These standards provide the essential framework upon which transparent integration methodologies must be built.
Table 1: Core Domains of Research Practice Standards in Empirical Bioethics
| Domain | Key Standards | Application to Integration |
|---|---|---|
| Aims | Clearly articulate the research goals and the role of integration. | Justify why an integrative approach is necessary to address the specific research question. |
| Questions | Formulate research questions that inherently require both empirical and normative investigation. | Ensure questions cannot be adequately answered by either empirical data or normative analysis alone. |
| Integration | Specify the methodological approach for combining empirical and normative elements [52]. | Clearly state, explain, and justify the chosen method of integration and its execution. |
| Conduct of Empirical Work | Apply rigorous social scientific methods appropriate to the research question. | Ensure empirical data collection and analysis meet disciplinary standards for validity and reliability. |
| Conduct of Normative Work | Employ systematic ethical analysis with justified theoretical foundations [26]. | Make explicit the normative framework (theories, principles) used and the rationale for its selection. |
| Training & Expertise | Possess or collaborate to obtain competency in both empirical and normative methodologies. | Ensure the research team collectively holds the required expertise for credible integration. |
Methodological Approaches and Their Application
The field has developed numerous methodological pathways for integration, each with distinct procedures and epistemological commitments. Researchers must select and report their chosen approach with precision.
Predominant Integration Methodologies
Table 2: Common Methodological Approaches for Integration in Empirical Bioethics
| Methodology | Classification | Core Integrative Mechanism | Key Characteristics |
|---|---|---|---|
| Reflective Equilibrium | Consultative | Researcher-driven back-and-forth reflection between empirical data and ethical principles to achieve moral coherence [1]. | The researcher ("the thinker") systematically adjusts ethical judgments, principles, and empirical data until equilibrium is reached. |
| Dialogical Empirical Ethics | Dialogical | Structured dialogue among stakeholders (e.g., researchers, participants, professionals) to reach a shared normative understanding [1]. | Relies on collaborative discourse and deliberation to co-construct normative conclusions; ethicist often acts as a facilitator. |
| Grounded Moral Analysis | Combined | Iterative-inductive process where ethical analysis is developed directly from, and constantly checked against, empirical data [1]. | Normative concepts and frameworks emerge from the empirical data rather than being fully pre-defined. |
Experimental Protocol: Implementing Wide Reflective Equilibrium
The following protocol provides a detailed methodology for conducting integration via Wide Reflective Equilibrium, one of the most frequently cited approaches.
Objective: To achieve a coherent alignment between an individual's considered moral judgments, relevant moral principles/rules, and background empirical theories through a structured, iterative process. Primary Applications: Ethical analysis of clinical practices, policy development, and normative framework refinement.
Materials and Reagents:
- Ethical Theory Compendium: A collection of foundational and contemporary texts in moral philosophy relevant to the research topic.
- Empirical Dataset: Qualitative and/or quantitative data pertaining to the moral experience, beliefs, or practices of relevant stakeholders (e.g., interview transcripts, survey results, observational field notes).
- Coding and Analysis Software: Qualitative data analysis software (e.g., MAXQDA, NVivo) for organizing empirical data and theoretical concepts.
- Analytical Memoing System: A structured log (digital or physical) for documenting the iterative steps of reflection and adjustment.
Procedure:
- Initial Preparation: a. Articulate Considered Judgments: Identify and document a set of initial, stable moral judgments about the research topic. These should be judgments held with high confidence after careful reflection (e.g., "Informed consent is a prerequisite for this trial"). b. Formulate Candidate Principles: Systematically assemble a set of moral principles and rules that potentially explain and justify the initial considered judgments. c. Compile Background Theories: Gather relevant empirical and philosophical background theories (e.g., theories of autonomy, sociological studies of doctor-patient communication, clinical outcome data).
Iterative Reconciliation Phase: a. Test for Coherence: Systematically check for coherence among the three sets of elements: considered judgments, moral principles, and background theories. Identify points of tension and conflict. b. Make Adjustments: To achieve coherence, make revisions to any of the elements. This may involve: i. Revising a considered judgment in light of a principle that has strong justificatory power. ii. Modifying or rejecting a principle that generates counter-intuitive judgments or clashes with well-supported empirical facts. iii.Re-evaluating the relevance or interpretation of background theories based on normative reasoning. c. Document Rationale: For every adjustment made, document the precise reason for the change in the analytical memo. This is critical for transparency.
Stabilization and Output: a. Achieve Equilibrium: Continue the iterative process until a stable, coherent network of beliefs is achieved. This represents the reflective equilibrium for the research question. b. Articulate Normative Conclusion: Clearly state the justified normative position that has emerged from the process. c. Report the Process: In the research output, report not only the conclusion but also the path taken, including key adjustments and the rationale behind them, to allow for critical evaluation.
Diagram 1: Workflow for Wide Reflective Equilibrium Integration
The Scientist's Toolkit: Research Reagent Solutions
Successful integration requires specific conceptual and methodological tools. The following table details the essential "research reagents" for conducting rigorous empirical bioethics research.
Table 3: Essential Research Reagents for Empirical Bioethics Integration
| Reagent / Tool | Function / Purpose | Key Considerations |
|---|---|---|
| Normative Framework Selector | Aids in the systematic selection of an ethical theory (e.g., deontology, consequentialism, virtue ethics) to serve as the normative background [26]. | Selection should be justified based on the topic's adequacy, project design suitability, and coherence with empirical research's theoretical background [26]. |
| Data Interrogation Protocol | A set of pre-defined questions to analyze empirical data for its normative relevance and implications. | Questions might include: "What values are expressed in this data?" "What moral conflicts are evident?" "How do contextual factors shape moral reasoning?" |
| Integration Methodology Checklist | Ensures the chosen integration method (e.g., Reflective Equilibrium, Dialogical) is applied completely and transparently [52]. | The checklist should verify that the researcher has explained the method's theoretical basis, step-by-step execution, and how it bridges the empirical-normative divide. |
| Transparency Log (Analytical Memoing) | A real-time diary documenting key decisions, rationale for methodological shifts, and reflexive observations during the integration process. | Serves as an audit trail, providing evidence of rigor and allowing peers to trace the derivation of normative conclusions from the raw data and initial premises. |
| Stakeholder Engagement Framework | A structured plan for incorporating perspectives from relevant stakeholders (patients, clinicians, developers) in the normative deliberation [1]. | Particularly crucial for dialogical methods; defines who is involved, at what stage, and how their input is integrated into the ethical analysis. |
Visualization of Methodological Selection and Application
Selecting an appropriate methodology is a critical first step. The following diagram outlines the decision pathway for choosing and applying a primary integration method, highlighting the points of transparency and justification required by rigorous standards.
Diagram 2: Methodology Selection and Justification Pathway
The integration of normative and empirical approaches represents a central challenge in contemporary bioethics research. This comparative analysis examines two prominent methodological frameworks: Reflective Equilibrium (RE) and Dialogical Ethics. As the field grapples with complex issues ranging from clinical practice to algorithmic decision-making, researchers require robust methodological guidance that bridges theoretical justification with practical application [51]. Reflective Equilibrium, particularly in its wide form, offers a systematic approach for achieving coherence among moral judgments, principles, and background theories [66]. In contrast, Dialogical Ethics emphasizes procedural deliberation among stakeholders as the pathway to ethical resolution [67]. This analysis provides researchers, scientists, and drug development professionals with structured application notes and experimental protocols for implementing these methodologies within empirical bioethics research, focusing on their distinctive strengths, limitations, and appropriate contexts of application.
Theoretical Foundations and Key Concepts
Reflective Equilibrium: A Coherence-Based Approach
Reflective Equilibrium (RE) is a method of ethical justification that aims to produce coherence among different types of beliefs held by a moral agent [68]. Originally developed by John Rawls in "A Theory of Justice," the method involves a process of mutual adjustment between "considered moral judgments" and "moral principles" [66]. The method begins with an initial set of moral judgments about particular cases, which are then systematically compared with relevant moral principles and background theories. Through an iterative process of reflection and revision, these elements are adjusted until a state of "equilibrium" is achieved where all components cohere satisfactorily [68].
The methodology has evolved into two primary variants: Narrow Reflective Equilibrium (NRE) and Wide Reflective Equilibrium (WRE). NRE seeks coherence specifically between moral judgments and moral principles, while WRE expands this coherence relationship to include "a set of relevant background theories" [66]. This wider approach incorporates philosophical arguments, empirical data, and theoretical considerations that can independently support ethical principles, making it particularly valuable for addressing complex bioethical dilemmas where multiple forms of evidence and reasoning are relevant [69]. The equilibrium reached is considered "reflective" because the moral agent understands how their judgments and principles interrelate and can provide reasoned justifications for this coherent structure [66].
Dialogical Ethics: A Procedural-Deliberative Approach
Dialogical Ethics offers a fundamentally different approach to ethical justification, focusing on intersubjective deliberation rather than individual coherence. As a procedural alternative to substantive ethical frameworks, Dialogical Ethics does not establish goods in advance but rather determines them through a structured dialogue process involving the actual parties affected by an ethical dilemma [67]. The approach is "dialogical" in that it institutes empathic critical discussion and negotiation among stakeholders, regulated by appropriate rules of order that are reciprocally agreed upon [67].
This methodological framework has proven particularly valuable in bioethics for resolving situations where substantive ethical theories reach an impasse, such as in cases of medical futility [67]. The fundamental tenet of Dialogical Ethics is that ethical validity emerges from the quality of the dialogical process itself, rather than from its conformity to pre-established moral truths. This process typically involves facilitation, structured exchange of perspectives, and collaborative development of ethical resolutions that account for the diverse values and interests of all relevant stakeholders [70]. Unlike RE, which operates primarily through individual reflection, Dialogical Ethics is inherently relational and communicative, positioning ethical justification as a social achievement rather than an individual cognitive accomplishment.
Comparative Analysis: Structured Evaluation
Table 1: Core Conceptual and Procedural Comparison
| Aspect | Reflective Equilibrium | Dialogical Ethics |
|---|---|---|
| Primary Focus | Coherence among beliefs of an individual moral agent [66] | Procedure of dialogue among affected parties [67] |
| Epistemological Basis | Coherentist justification through mutual adjustment [68] | Procedural legitimacy through inclusive deliberation [67] |
| Key Elements | Considered judgments, moral principles, background theories [66] | Stakeholders, facilitation, rules of dialogue, empathic discussion [67] |
| Scope of Application | Individual moral reasoning; theoretical justification [68] | Collective decision-making; practical resolution of dilemmas [70] |
| Temporal Dimension | Potentially extended individual reflection | Time-bounded deliberative events [70] |
| Outcome | Justified coherent belief system | Contextually appropriate resolution [67] |
Table 2: Strengths and Limitations Analysis
| Dimension | Reflective Equilibrium | Dialogical Ethics |
|---|---|---|
| Key Strengths | Systematic justification; Handles complexity through background theories; Compatible with empirical data [69] | Resolves substantive impasses; Incorporates diverse stakeholder values; Promotes practical implementation [67] |
| Methodological Limitations | Potential subjectivism; Underspecified adjustment process; Risk of conserving biases [69] [7] | Challenging with incompetent parties; Conflicts of interest; Resource intensive [67] |
| Evidentiary Requirements | Considered judgments; Relevant principles; Background theories (in WRE) [66] | Inclusive stakeholder representation; Appropriate facilitation; Agreed procedural rules [70] |
| Validation Criteria | Coherence; Comprehensive-ness; Reflective acceptance [66] | Procedural fairness; Stakeholder acceptance; Practical workability [67] |
Application Notes for Bioethics Research
Reflective Equilibrium Implementation Framework
The successful application of Wide Reflective Equilibrium (WRE) in bioethics research requires systematic execution across three interconnected levels. Researchers should begin by compiling the initial data set of "considered moral judgments" on the issue under investigation. These judgments must be rendered under conditions conducive to moral deliberation—where researchers are well-informed, free from distorting influences, and motivated by moral concerns [68]. In practice, this involves gathering case intuitions, professional consensus statements, and well-established ethical assessments relevant to the research context, such as judgments about acceptable risk thresholds in clinical trials or appropriate standards of informed consent.
The second level involves identifying candidate moral principles that potentially systematize these considered judgments. For drug development professionals, this typically includes principles of beneficence, non-maleficence, autonomy, and justice, alongside field-specific ethical guidelines [71]. The third level incorporates relevant background theories, which may include scientific evidence, sociological data, philosophical accounts, and theoretical frameworks that bear on the ethical issue [66]. The distinctive feature of WRE is the mutual adjustment process among these three levels, where conflicts are addressed through revisions at any level—judgments may be revised in light of principles, principles modified or rejected based on judgments, and background theories employed to guide these adjustments. This process continues until researchers achieve a stable equilibrium where all elements cohere satisfactorily [69].
Dialogical Ethics Implementation Framework
Implementing Dialogical Ethics in bioethics research requires careful attention to procedural elements that ensure legitimate outcomes. The process begins with comprehensive stakeholder mapping to identify all parties affected by or involved in the ethical issue, including researchers, clinicians, patients, industry representatives, and community members [70]. For drug development contexts, this might include research participants, regulators, ethics committee members, and patient advocacy groups. The next critical step establishes clear rules of order to regulate the dialogue, ensuring reciprocal communication, empathic engagement, and balanced participation [67].
A skilled facilitator should guide the deliberative process, creating conditions for respectful exchange and managing power differentials that might distort communication [70]. The dialogue itself should integrate both empathic critical discussion—aimed at mutual understanding—and negotiation—focused on reaching practical resolutions [67]. Unlike RE, which prioritizes cognitive coherence, Dialogical Ethics emphasizes relational dynamics and communicative processes as the foundation for ethical justification. Successful implementation typically results in contextually appropriate resolutions that acknowledge multiple value perspectives and generate stakeholder buy-in, particularly valuable for addressing controversial issues in research ethics where substantive agreement has proven elusive [67].
Experimental Protocols and Workflows
Protocol for Applying Reflective Equilibrium in Bioethics Research
Table 3: Research Reagent Solutions for Reflective Equilibrium
| Research 'Reagent' | Function in Methodological Protocol |
|---|---|
| Considered Judgment Inventory | Provides initial moral data points; captures pre-reflective ethical intuitions about cases [68] |
| Principles Repository | Supplies candidate systematizing principles; offers competing normative frameworks [66] |
| Background Theory Database | Contains relevant scientific, philosophical, and theoretical resources; informs adjustment process [69] |
| Coherence Tracking System | Documents conflicts and adjustments; maps justificatory relationships among elements [66] |
| Equilibrium Validation Tool | Tests stability of achieved equilibrium; identifies potential sources of instability [69] |
Figure 1: Reflective Equilibrium Workflow: This diagram illustrates the iterative process of achieving reflective equilibrium through mutual adjustment among moral judgments, principles, and background theories.
Protocol for Applying Dialogical Ethics in Bioethics Research
Table 4: Research Reagent Solutions for Dialogical Ethics
| Research 'Reagent' | Function in Methodological Protocol |
|---|---|
| Stakeholder Mapping Tool | Identifies relevant participants; analyzes stakes and interests [70] |
| Deliberative Protocol | Establishes rules of engagement; structures dialogue process [67] |
| Facilitation Framework | Guides impartial process management; ensures participatory equality [70] |
| Empathic Engagement Method | Fosters mutual understanding; encourages perspective-taking [67] |
| Resolution Documentation | Captures deliberative outcomes; records value trade-offs [70] |
Figure 2: Dialogical Ethics Workflow: This diagram outlines the structured process of dialogical ethics, from stakeholder mapping through facilitated dialogue to negotiated resolution.
Integration and Hybrid Approaches
Collective Reflective Equilibrium and Algorithmic Bioethics
Recent methodological innovations have explored hybrid approaches that integrate strengths from both RE and Dialogical Ethics. Collective Reflective Equilibrium (CRE) expands the traditional RE framework beyond individual reasoning to incorporate multiple perspectives through deliberative processes [72]. This approach is particularly promising for addressing complex policy dilemmas in bioethics where multiple stakeholders hold legitimate but conflicting values. CRE seeks to resolve ethical conflicts by balancing moral intuitions with theoretical principles across a collective, rather than within an individual [72].
When combined with algorithmic bioethics, CRE offers a structured approach to ethical decision-making in contexts such as resource allocation during pandemics or ethical AI implementation in healthcare [72]. This integration formalizes ethical reasoning into decision trees that incorporate key ethical considerations, enabling researchers and policymakers to apply coherentist reasoning to complex, multi-stakeholder scenarios. For drug development professionals, this hybrid approach offers methodological resources for addressing ethical challenges that involve competing values from scientific, commercial, clinical, and patient perspectives while maintaining systematic justificatory standards.
Empirical Bioethics Integration Frameworks
The integration of empirical research with normative analysis represents a growing edge of methodological innovation in bioethics [51]. Survey data indicates that most bioethics researchers (87.5%) use or have used empirical methods in their work, yet only about one-third of these scholars report having successfully integrated empirical data with normative analysis [51]. This gap highlights the need for more robust methodological frameworks that bridge the empirical-normative divide.
Both RE and Dialogical Ethics offer distinct pathways for this integration. RE can incorporate empirical data as part of the "background theories" that inform the reflective process [69], while Dialogical Ethics can utilize empirical findings to inform stakeholder deliberations [70]. However, researchers report significant challenges in implementation, with interviews revealing "an air of uncertainty and overall vagueness" surrounding integration methods [7]. This suggests a need for more precise protocols and validation criteria for empirical-normative integration in both approaches.
Reflective Equilibrium and Dialogical Ethics offer complementary rather than competing methodological resources for bioethics research. RE provides superior tools for systematic justification and theoretical coherence, making it particularly valuable for developing ethical frameworks, justifying principles, and addressing foundational questions in bioethics [66]. Dialogical Ethics offers more effective approaches for resolving practical dilemmas, incorporating diverse stakeholder perspectives, and generating legitimate outcomes in contested policy contexts [67].
For researchers, scientists, and drug development professionals, the strategic selection between these approaches should be guided by research context and objectives. RE is recommended for projects requiring robust justificatory structures and theoretical defense, such as establishing ethical guidelines for novel technologies or analyzing conceptual foundations of research ethics [69]. Dialogical Ethics is more appropriate for addressing context-specific dilemmas, resolving stakeholder conflicts, and developing policies requiring broad acceptance, such as institutional ethics protocols or community-engaged research guidelines [70]. Emerging hybrid approaches like Collective Reflective Equilibrium offer promising avenues for complex challenges that demand both systematic justification and inclusive deliberation [72]. By understanding the distinctive strengths, limitations, and implementation requirements of each methodology, bioethics researchers can more effectively select and adapt these approaches to advance the integration of empirical and normative analysis in their scientific contexts.
In contemporary bioethics, a significant methodological shift is underway, moving from abstract theorizing to integrated approaches that combine normative analysis with empirical research. This fusion addresses a critical gap in traditional ethics, which often struggled to provide actionable, context-sensitive guidance for complex, real-world challenges in healthcare and technology development [14] [39]. Integrated approaches ensure that ethical frameworks are not only theoretically sound but also practically relevant and responsive to the nuances of their application contexts.
The core premise of this integration is that robust ethical guidance emerges from the iterative dialogue between foundational ethical principles and evidence gathered from the very situations and stakeholders these principles are meant to serve. This article explores several leading integrated methodologies—Embedded Ethics and Social Science (EESS), the Principle-Based Empirically Grounded Roadmap Approach (PERA), and others—detailing their protocols and demonstrating how their application leads to more impactful and resilient ethical oversight.
Integrated Approaches in Practice: Methodologies and Impact
Embedded Ethics and Social Science (EESS)
The Embedded Ethics and Social Science (EESS) approach involves integrating ethicists and social scientists directly into interdisciplinary research and development teams from a project's outset. This deep integration allows for the proactive identification and mitigation of ethical and social concerns throughout the technology development lifecycle, rather than addressing them as an afterthought [14].
- Core Protocol: The EESS methodology is operationalized through a dynamic toolbox of empirical methods tailored to the project phase and specific ethical questions. The table below summarizes the key methods and their primary functions in generating robust ethical guidance.
Table 1: EESS Toolbox of Methods for Integrated Ethics
| Method | Primary Function in Ethical Analysis | Stage of Application |
|---|---|---|
| Stakeholder Analyses [14] | Identifies affected parties and power dynamics, ensuring inclusive and just outcomes. | Project Initiation & Scoping |
| Ethnographic Approaches [14] | Uncovers unarticulated values and "ethics in practice" within development contexts. | Early & Mid-Development |
| Focus Groups & Interviews [14] | Elicits nuanced stakeholder perspectives on benefits, risks, and value conflicts. | Mid-Development & Evaluation |
| Bias Analyses [14] | Systematically evaluates algorithms and datasets for potential discriminatory effects. | Data Curation & Model Validation |
| Interdisciplinary Workshops [14] | Fosters shared understanding and co-design of ethical solutions among diverse experts. | Ongoing & Critical Decision Points |
- Workflow and Logical Relationship: The following diagram visualizes the continuous, iterative workflow of the EESS approach, illustrating how ethical reflection is woven into the fabric of project development.
The Principle-Based Empirically Grounded Roadmap Approach (PERA)
Developed for contexts where technology is somewhat predetermined but requires ethical guidance for future iterations, PERA provides a structured methodology to create a portable "ethics toolkit." This approach is particularly valuable in digital mental health and other domains with established co-development practices [39].
- Core Protocol: PERA integrates multiple data sources to build a practical ethics roadmap. The protocol involves three sequential but interlinked phases of inquiry, followed by a synthesis stage.
Table 2: Phases of the PERA Protocol for an Ethics Roadmap
| Phase | Description | Data Output |
|---|---|---|
| Principle Mapping | Systematic review of ethical principles from the academic literature on comparable technologies. | A set of candidate normative principles (e.g., autonomy, justice, non-maleficence). |
| Scoping Review | Investigation of the "moral intuitions" and "ethics in practice" of developers working on similar technologies. | Insights into real-world ethical dilemmas and how they are navigated by practitioners. |
| Original Empirical Data Collection | Gathering project-specific data through methods like interviews or observations within the use case. | Context-rich, localized understanding of emerging ethical issues. |
| Abductive Synthesis | Integration of findings from all phases to refine principles and generate actionable recommendations. | A finalized "Ethics Roadmap" document to guide future development. |
- Logical Workflow: The PERA process is a funnel, moving from broad principles to a specific, actionable roadmap, as shown below.
Protocolization in Empirical Bioethics
To ensure rigor and transparency, integrated ethics research requires robust protocols. A newly formalized template addresses this need by adapting standards from qualitative health research to be suitable for all types of humanities and social sciences investigations in health, including empirical bioethics [13].
This protocol template emphasizes key sections that are crucial for integrated studies:
- Epistemological Positioning: Forces investigators to clarify the theoretical foundations bridging normative and empirical domains [13].
- Management of Bias: Requires a explicit plan for identifying and mitigating biases in both empirical data collection and normative reasoning [13].
- Adapted Consent and Data Protection: Recognizes that strict, traditional consent forms can sometimes bias participant responses in ethics research, and allows for context-appropriate adaptations while safeguarding fundamental rights [13].
The Scientist's Toolkit: Key Reagents for Integrated Ethics Research
Successfully implementing integrated ethics requires specific "reagents" or tools. The table below details essential components for setting up a robust integrated ethics research program.
Table 3: Research Reagent Solutions for Integrated Ethics
| Reagent / Solution | Function in the Integrated Ethics Process |
|---|---|
| Embedded Ethicist | An ethics researcher fully integrated into the development team to facilitate real-time, contextual ethical reflection [14]. |
| Stakeholder Mapping Template | A structured tool for identifying all parties affected by a technology, ensuring their perspectives are considered [14]. |
| Interview & Focus Group Guides | Semi-structured protocols for eliciting in-depth perspectives from users, developers, and affected communities on ethical dimensions [14] [73]. |
| Bias Assessment Framework | A checklist or algorithmic tool for systematically scanning for discriminatory biases in datasets and models [14]. |
| Interdisciplinary Workshop Format | A designed session plan to facilitate knowledge exchange and collaborative problem-solving between ethicists, technical staff, and other stakeholders [14]. |
| Reflective Journal | A tool for researchers and participants to document "ethically important moments" and personal reflections, enriching the empirical data [74]. |
| Ethics Roadmap Document | The tangible output of processes like PERA, providing adaptable, practical guidance for future project iterations [39]. |
Case Studies and Applications
Reporting Back Research Results (RBRR)
The ethical obligation to report research results to participants is well-established, but the question of how to do this effectively, particularly with sensitive or uncertain findings, requires an integrated approach. An expert panel applied the principles of bioethics (respect for autonomy, beneficence, non-maleficence, and justice) to this practical challenge [73].
Their work revealed that standardized terminology was a foundational need, without which coherent guidance was impossible. Their integrated deliberation led to concrete recommendations, including developing centralized resources, actively engaging participants to maintain trust, and recognizing community-level harms and benefits [73]. This demonstrates how normative principles, when confronted with empirical logistical challenges, yield more precise and actionable guidance.
Adaptive Clinical Trial Designs
Innovative clinical trial designs, such as Bayesian adaptive trials, raise novel ethical and methodological questions. A multi-stakeholder workshop brought together statisticians, ethicists, regulators (e.g., FDA, WHO), industry representatives, and patient advocates to address these [75].
This integrated forum allowed for a simultaneous examination of ethical assumptions (e.g., what constitutes fairness in a dynamically changing trial) and methodological performance (e.g., whether designs compromise reliability). The goal was to foster public awareness, provide regulatory guidance, and address stakeholder concerns, ensuring that the evolution of trial design is guided by a balanced consideration of scientific efficiency and ethical imperatives [75].
The integrated approaches detailed in this article—EESS, PERA, and robust protocolization—provide a powerful framework for producing ethical guidance that is both principled and practical. The consistent theme across all methodologies is that impact is maximized when ethics is not a peripheral audit but an embedded, continuous process of reflection and adaptation.
For researchers and drug development professionals, adopting these protocols means building a more reflexive and responsible research practice. The presented tools and case studies offer a starting point for translating the theory of integrated bioethics into tangible action, ultimately leading to technologies and therapies that are not only innovative but also socially robust, trustworthy, and just.
Application Notes: Integrating Empirical Data and Normative Analysis in Bioethics
The integration of empirical data with normative analysis is essential for developing bioethical frameworks that are both philosophically sound and practically applicable. These application notes outline protocols for systematically incorporating empirical evidence into bioethics research, using COVID-19 vaccine equity as a primary case study. This approach enables researchers to ground normative claims in observable reality, test ethical principles against practical outcomes, and specify the conditions under which ethical frameworks apply.
Empirical data informs normative claims by revealing the real-world contexts, stakeholder perspectives, and practical constraints that ethical frameworks must address. It tests the validity and applicability of established ethical principles by examining their consequences and acceptability in practice. Furthermore, it helps specify the precise scope and implementation details of normative recommendations, moving from abstract principles to concrete, actionable guidance. A systematic mapping of recent literature on COVID-19 vaccine equity reveals how empirical research can enrich bioethical discourse by identifying underrepresented populations, contextual factors, and epistemic disparities that normative analysis might otherwise overlook [76].
Empirical Data Synthesis: COVID-19 Vaccine Equity Analysis
The following tables synthesize findings from a systematic mapping of 51 articles from leading bioethics and science communication journals published between March 2020 and July 2022 [76]. This empirical data provides a foundation for informing, testing, and specifying normative claims regarding global vaccine distribution.
Table 1: Populations Identified in COVID-19 Vaccine Equity Literature
| Population Category | Specific Groups Mentioned | Frequency in Bioethics Literature | Frequency in Science Communication Literature |
|---|---|---|---|
| Broadly Vulnerable | General "vulnerable populations" | High | Low |
| Age-Specific | Children/adolescents, older adults | Medium | Low |
| Racial/Ethnic Minorities | Various racial/ethnic groups | High | Medium |
| Occupational Groups | Essential workers | Medium | Low |
| Intersectionally Marginalized | First Nation communities, incarcerated individuals, people with developmental disabilities, low SES children in LMICs | Low | Low |
Table 2: Scale and Context of Vaccine Equity Discussions
| Analytical Scale | Focus of Discourse | Bioethics Publications | Science Communication Publications |
|---|---|---|---|
| Global | Disparities between high-income and low-middle-income countries | High | Medium |
| National | Domestic allocation policies and priority groups | Medium | Low |
| Local | Community-specific access and outreach | Low | Low |
Table 3: Types of Equity Issues Addressed
| Equity Dimension | Specific Concerns | Bioethics Focus | Science Communication Focus |
|---|---|---|---|
| Allocation & Access | Vaccine distribution, priority groups, supply chains | High | Medium |
| Knowledge & Communication | Health literacy, misinformation, accessible information | Low | High |
| Research & Development | Trial participation, representative research | Medium | Low |
| Political Economy | Global power dynamics, intellectual property, diplomacy | Medium | Low |
Experimental Protocols
Protocol 1: Systematic Literature Mapping for Bioethical Analysis
Purpose: To identify and categorize empirical data relevant to normative bioethical claims through systematic literature mapping.
Materials:
- Journal databases (e.g., Scimago, Clarivate, Google Scholar)
- Reference management software (e.g., Zotero, EndNote)
- Qualitative data analysis software (e.g., NVivo, Dedoose)
Methodology:
- Journal Selection: Identify 5-10 leading journals in bioethics and related empirical fields (e.g., science communication) [76].
- Search Strategy: Define relevant time periods (e.g., March 2020-July 2022 for COVID-19 studies) and search terms combining subject matter ("COVID", "vaccin") with equity concepts ("equit", "just", "disparit", "marginal*") [76].
- Screening Process: Review titles, abstracts, keywords, and full texts to confirm relevance to both the subject matter and equity dimensions.
- Data Extraction: Code included articles for:
- Scale of analysis (local, national, global)
- Populations discussed
- Types of equity issues addressed
- Methodological approaches
- Key findings and recommendations [76]
- Synthesis: Identify patterns, gaps, and intersections between normative claims and empirical evidence across the literature.
Validation: Independent coding by multiple researchers with discussion to reach consensus on final coding [76].
Protocol 2: Stakeholder Engagement for Normative Framework Development
Purpose: To empirically inform normative claims through direct engagement with affected communities and stakeholders.
Materials:
- Interview/focus group guides
- Recording and transcription equipment
- Ethical approval documentation
- Collaborative workshop materials
Methodology:
- Stakeholder Identification: Purposefully sample diverse stakeholders representing affected populations, healthcare providers, policymakers, and community leaders.
- Data Collection:
- Conduct semi-structured interviews exploring values, experiences, and ethical concerns
- Facilitate focus groups to identify shared perspectives and divergences
- Organize deliberative workshops for co-development of ethical recommendations [76]
- Analysis: Employ thematic analysis to identify recurring values, ethical tensions, and contextual factors that should inform normative frameworks.
- Integration: Systematically incorporate stakeholder-identified values and concerns into the development or refinement of ethical guidelines.
Ethical Considerations: Obtain informed consent, ensure confidentiality, provide opportunities for participant feedback, and address power imbalances in the research process.
Conceptual Framework Visualization
Diagram 1: Conceptual framework showing the dynamic relationship between empirical data and normative claims in bioethics research. The visualization illustrates how empirical data informs normative claims by providing contextual understanding, tests established principles through validation processes, and specifies implementation guidance for ethical frameworks.
Research Workflow Visualization
Diagram 2: Research workflow for integrating empirical and normative approaches. This diagram outlines the systematic process of gathering empirical data through multiple methods, conducting integrated analysis, and producing refined ethical frameworks that are informed, tested, and specified through empirical engagement.
Research Reagent Solutions
Table 4: Essential Research Materials for Empirical Bioethics
| Research Tool | Function | Application in Empirical Bioethics |
|---|---|---|
| Qualitative Data Analysis Software (e.g., NVivo, Dedoose) | Facilitates coding and thematic analysis of interview transcripts, focus groups, and documentary sources | Identifies recurring values, ethical concerns, and contextual factors from stakeholder engagement data |
| Reference Management Software (e.g., Zotero, EndNote) | Organizes literature sources, manages citations, and supports systematic review processes | Enables comprehensive literature mapping and integration of diverse scholarly sources into normative analysis |
| Structured Interview Guides | Provides consistent framework for semi-structured interviews with stakeholders | Ensures systematic exploration of ethical values and experiences while allowing emergence of unanticipated themes |
| Deliberative Workshop Protocols | Outlines structured processes for facilitated group discussions and co-development of ethical guidance | Enables collaborative refinement of normative frameworks with diverse stakeholders, minimizing paternalism [76] |
| Systematic Review Databases (e.g., PubMed, Scopus) | Provides comprehensive access to scholarly literature across disciplines | Supports identification of relevant empirical studies and theoretical works for integrative analysis |
| Data Visualization Tools (e.g., Tableau, Graphviz) | Creates diagrams, charts, and conceptual maps to represent complex relationships | Illustrates connections between empirical findings and normative claims, enhancing communication to diverse audiences |
The rapid integration of artificial intelligence (AI) and emerging technologies into healthcare and biomedical research presents unprecedented ethical challenges that demand methodological evolution in bioethics. This convergence necessitates a deliberate fusion of normative ethical analysis with empirical research approaches to create robust, future-proof methodological frameworks. Bioethics serves as a moral compass for emerging technologies like AI, ensuring that technological advancements align with human values and dignity, while AI can aid bioethical analysis by processing complex datasets to identify patterns in ethical decision-making [77]. The fundamental challenge lies in developing bioethics methodologies that remain relevant amidst accelerating technological change while maintaining rigorous ethical standards for healthcare and drug development contexts.
This protocol paper establishes structured approaches for integrating AI ethics considerations into bioethics methodological frameworks, with particular emphasis on bridging the normative-empirical divide in bioethics research. The frameworks presented address both the ethical implications of AI in biomedicine and the use of AI tools to enhance bioethics methodology itself, creating a bidirectional relationship that strengthens the entire research ecosystem.
Theoretical Foundation: Integrating Normative and Empirical Approaches
Normative Methodological Frameworks
Normative methods in bioethics provide systematic approaches for determining ethically acceptable and defensible outcomes when confronted with ethical dilemmas [78]. These methods are prescriptive rather than descriptive—they aim to guide how ethical decisions should be made rather than describing how they are made in practice:
Reflective Equilibrium: This process, popularized by John Rawls and applied to bioethics by scholars like DeGrazia and Millum, involves starting with existing ethical beliefs about cases and principles, weeding out unreliable beliefs, and adjusting the remaining set to achieve maximum coherence. The end goal is "a set of principles that fit together as a single theory and which, along with the relevant empirical facts, entail the moral judgments about cases that we think are correct" [43].
Principlism: This approach utilizes foundational principles (typically beneficence, nonmaleficence, autonomy, and justice) as primary action-guidance for dealing with particular cases [43]. When integrated with AI ethics, these principles require operationalization into measurable parameters.
Argument-Based Medical Ethics: McCullough, Coverdale, and Chervenak provide a formal framework for critically appraising normative medical ethics literature through a structured checklist that assesses focused ethics questions, argument robustness, analytical quality, and practical applicability [43].
Empirical Bioethics Protocols
Empirical bioethics integrates descriptive research about what people believe, do, and experience with normative inquiry into what ought to be done [13]. The protocol template for empirical bioethics investigations includes several distinctive sections that differ from pure clinical research protocols:
- Epistemological Positioning: Researchers must explicitly state their epistemological framework and methodological approach (qualitative, quantitative, mixed methods) [13].
- Normative-Empirical Loop: The protocol should detail how empirical data will inform normative analysis and vice versa, including the ethical theory or theories that will guide the normative analysis [13].
- Contextualized Consent Procedures: Recognizing that traditional informed consent approaches may influence participant behavior and responses in empirical ethics research, the protocol allows for careful modification of consent processes while maintaining ethical standards [13].
- Data Protection Flexibility: The protocol acknowledges that excessive anonymization may limit analytical depth, permitting responsible pseudonymization where justified by research objectives [13].
Table 1: Normative-Empirical Integration Framework
| Component | Normative Elements | Empirical Elements | Integration Mechanism |
|---|---|---|---|
| Problem Identification | Ethical theory analysis; Principle identification | Stakeholder interviews; Ethnographic observation | Iterative refinement of research questions through theory-practice dialogue |
| Data Collection | Conceptual analysis; Logical argument construction | Surveys; Focus groups; Case studies | Embedded ethical reflection during data collection; Real-time normative assessment |
| Analysis | Coherence testing; Principle application | Qualitative coding; Statistical analysis | Alternating between empirical findings and normative frameworks; Seeking reflective equilibrium |
| Output Development | Ethical recommendations; Policy guidelines | Validation testing; Stakeholder feedback | Normative outputs grounded in empirical reality; Empirical findings normatively contextualized |
Application Note 1: AI Ethics Assessment Protocol for Biomedical Research
This protocol provides a structured approach for identifying, assessing, and addressing ethical implications of AI technologies in biomedical research and drug development contexts. It adapts the BrainSwarming and Generic Parts Technique (GPT)—Innovation Enhancing Techniques (IETs) originally developed for engineering contexts—to bioethical analysis [79].
Methodology
BrainSwarming for Ethical Analysis
BrainSwarming creates a visual problem-solving graph that facilitates simultaneous identification of ethical concerns and potential solutions:
Goal Definition: Place the primary ethical goal at the top of the graph (e.g., "Ensure justice and fairness in AI-based patient selection for clinical trials").
Resource Identification: Place available resources at the bottom (e.g., "AI algorithm," "patient data," "regulatory frameworks").
Goal Refinement: Iteratively refine the primary goal downward into more specific subgoals (e.g., "Identify bias in training data," "Ensure representative sampling," "Establish accountability mechanisms").
Resource Decomposition: Decompose resources upward into components and features using the Generic Parts Technique (e.g., "AI algorithm" → "decision rules," "training data," "validation metrics," "output interpretations").
Solution Pathway Identification: Create connections between refined goals and resource components where interactions represent potential ethical solutions or concerns [79].
Generic Parts Technique for Ethical Analysis
The GPT helps overcome psychological obstacles to innovation by systematically decomposing and re-describing resources:
Decomposition: Ask "Can this AI component be broken down further?" and decompose it into constituent parts.
Functional Neutralization: Ask "Does this description imply a use?" and reframe the description neutrally to prevent functional fixedness.
Iterative Application: Repeat the process until no further meaningful decomposition is possible [79].
Implementation Workflow
The following diagram illustrates the AI Ethics Assessment Protocol workflow:
Application Case Study: Blockchain for Bioethical Goals
In a demonstrated application of these techniques to identify uses of blockchain technology to further bioethical goals, researchers successfully generated 100 solution pathways connecting blockchain components with ethical principles [79]. For example:
Conditional Informed Consent: Blockchain's smart contract functionality was connected to the ethical principle of autonomy to create dynamic consent mechanisms that allow research participants to modify consent preferences over time.
Transparent Research Auditing: Blockchain's immutable audit trail was connected to the principle of beneficence to create transparent records of clinical trial data management.
Equitable Resource Allocation: Blockchain's distributed ledger was connected to the principle of justice to create verifiable and fair systems for allocating scarce medical resources.
Application Note 2: Normative-Empirical Integration Protocol
This protocol provides a systematic methodology for integrating normative ethical analysis with empirical research approaches, creating a rigorous framework for bioethics research that remains relevant in the context of emerging technologies.
Methodology
Sequential Mixed-Methods Design
The protocol employs a sequential mixed-methods approach with four distinct phases:
Normative Framework Development: Establish preliminary ethical frameworks using established normative methods (reflective equilibrium, principlism, casuistry).
Empirical Data Collection: Gather qualitative and quantitative data on stakeholder perspectives, technological impacts, and practical manifestations of ethical issues.
Integrative Analysis: Systematically compare and contrast normative frameworks with empirical findings, identifying areas of alignment and tension.
Refined Framework Development: Modify and refine ethical frameworks based on empirical insights, then validate through iterative stakeholder engagement.
Reflective Equilibrium Process
The reflective equilibrium process is operationalized through these specific steps:
Initial Moral Judgments: Document reasoned initial judgments about specific cases involving AI and emerging technologies.
Principle Formulation: Articulate ethical principles that explain and justify these judgments.
Coherence Testing: Identify and address inconsistencies between judgments, principles, and background theories.
Adjustment and Refinement: Revise judgments and principles to achieve greater coherence while retaining those convictions in which confidence is highest.
Empirical Integration: Incorporate relevant empirical facts about technology capabilities, impacts, and stakeholder perspectives [43].
Implementation Workflow
The following diagram illustrates the Normative-Empirical Integration Protocol:
Quality Assessment Framework
The quality of normative-empirical bioethics research should be evaluated against these criteria adapted from argument-based medical ethics [43]:
- Focused Ethics Question: Does the research address a clearly stated ethical issue or problem?
- Argument Robustness: Is the literature search complete? Are analysis and arguments clearly reported?
- Analytical Quality: Is the argument valid and sound? Are key concepts clearly defined?
- Practical Application: Will the results help in practice? How should thinking or practices change based on the results?
Research Reagent Solutions: Essential Methodological Tools
Table 2: Bioethics Methodology Research Reagents
| Methodological Tool | Function | Application Context |
|---|---|---|
| BrainSwarming Framework | Visual problem-solving technique that facilitates simultaneous identification of ethical concerns and solutions | Ethical technology assessment; Stakeholder engagement; Interdisciplinary collaboration |
| Generic Parts Technique | Systematic decomposition and neutral redescription of resources to overcome functional fixedness | Analysis of AI systems; Identification of novel ethical implications; Innovation in ethical solutions |
| Reflective Equilibrium Protocol | Structured process for achieving coherence between moral judgments, principles, and empirical facts | Normative framework development; Resolution of ethical conflicts; Integration of diverse perspectives |
| Normative-Empirical Integration Matrix | Framework for systematically combining normative analysis with empirical data | Mixed-methods bioethics research; Policy development; Technology ethics assessment |
| Ethical Impact Assessment Template | Structured tool for anticipating and evaluating ethical impacts of emerging technologies | Research ethics committees; Technology development teams; Regulatory review |
Protocol Validation and Implementation Guidelines
Validation Framework
The methodological frameworks presented in this paper should be validated through these implementation steps:
Case Application: Apply protocols to diverse bioethical dilemmas involving AI and emerging technologies.
Stakeholder Feedback: Engage researchers, ethicists, technology developers, and affected communities in evaluating framework utility.
Iterative Refinement: Modify protocols based on implementation experience and emerging ethical challenges.
Interdisciplinary Review: Submit methodologies for critique across relevant disciplines (philosophy, computer science, medicine, law).
Implementation Considerations
Successful implementation of these protocols requires attention to several practical considerations:
Research Ethics Committee Education: Ethics review boards must develop understanding of both empirical bioethics methodologies and AI ethics considerations to provide appropriate oversight [13] [80].
Dynamic Consent Approaches: Traditional informed consent models may require adaptation for empirical bioethics research and AI-driven studies, potentially incorporating blockchain-based dynamic consent systems [13] [79].
Policy Integration: Research outputs should be translated into accessible formats for policy developers, leveraging implementation research ethics frameworks [81].
Global Equity Framework: Methodologies must incorporate considerations of global justice and structural inequities as emphasized in the 2024 Declaration of Helsinki revisions [82].
The integration of AI ethics and emerging technologies into bioethics methodological frameworks requires both theoretical sophistication and practical adaptability. The protocols presented in this paper provide structured approaches for maintaining bioethical relevance amidst rapid technological change while preserving the normative foundation essential to the discipline. By combining rigorous normative analysis with empirical investigation and innovative problem-solving techniques, bioethicists can develop frameworks that not only address current ethical challenges but remain capable of evolving to meet future technological developments. The essential imperative is creating methodologies with sufficient structure to ensure rigor while maintaining enough flexibility to adapt to unpredictable technological landscapes.
Conclusion
The successful integration of normative and empirical approaches is paramount for bioethics to maintain its relevance and rigor in addressing complex challenges in biomedical research and drug development. This synthesis of key takeaways reveals that overcoming methodological vagueness through transparent, reasoned theory selection and robust integration frameworks is essential. The future of the field hinges on developing more determinate methodologies that retain flexibility, fostering interdisciplinary collaboration, and proactively applying these integrated approaches to emerging areas such as artificial intelligence, genomics, and global health equity. By embracing these practices, bioethics researchers and drug development professionals can ensure that their work is not only scientifically valid but also ethically defensible and impactful for patients and society.
References
- 1. The Vagueness of Integrating the Empirical and the Normative [https://pmc.ncbi.nlm.nih.gov/articles/PMC11288993/]
- 2. The Role of Empirical Research in Bioethics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2826359/]
- 3. The Relevance of Empirical Research in Bioethics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2632190/]
- 4. What Counts as Empirical Research in Bioethics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2838431/]
- 5. a framework for empirical bioethics research projects [https://link.springer.com/article/10.1186/s12910-019-0428-0]
- 6. Acceptable objectives of empirical research in bioethics [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-022-00845-1]
- 7. Researchers' Views on Doing Empirical Bioethics [https://link.springer.com/article/10.1007/s11673-023-10286-z]
- 8. Categorizing Empirical Research in Bioethics: Why Count ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3098471/]
- 9. How Can Empirical Bioethics Research Legitimately Inform ... [https://philosophicalbioethics.com/?page_id=763]
- 10. A Platform to Develop and Apply Digital Methods for Empirical ... [https://formative.jmir.org/2022/5/e28558/]
- 11. Using symbiotic empirical ethics to explore the significance of ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-024-01053-9]
- 12. Health research protocols: a template for empirical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12183882/]
- 13. Health research protocols: a template for empirical bioethics ... [https://health-policy-systems.biomedcentral.com/articles/10.1186/s12961-025-01362-4]
- 14. Embedded Ethics in Practice: A Toolbox for Integrating the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11668859/]
- 15. Top Quantitative Analysis Tools 2025: Unlock Data Insights [https://airbyte.com/top-etl-tools-for-sources/top-quantitative-analysis-tools-unlock-data-insights]
- 16. 8 Best Research Analysis Tools for Quantitative Data in 2025 [https://www.displayr.com/best-survey-analysis-tools/]
- 17. Applying the principle of justice in digital health [https://www.nature.com/articles/s41746-025-01877-8]
- 18. Empirical research in bioethical journals. A quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2565792/]
- 19. Principles of Clinical Ethics and Their Application to Practice [https://pmc.ncbi.nlm.nih.gov/articles/PMC7923912/]
- 20. Ethical principles across countries: does 'ethical' mean the ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1579778/full]
- 21. Translational Justice and the Quest for Equity in US Healthcare [https://pmc.ncbi.nlm.nih.gov/articles/PMC12143965/]
- 22. Spotlight: Launch of the Justice Dialogues Initiative [https://www.mhe.cuimc.columbia.edu/news/spotlight-launch-justice-dialogues-initiative]
- 23. How international is bioethics? A quantitative retrospective study [https://bmcmedethics.biomedcentral.com/articles/10.1186/1472-6939-7-1]
- 24. Human-Machine Agreement in Medical Ethics: Patient ... [https://medinform.jmir.org/2025/1/e77061]
- 25. Understanding the nature and scope of clinical research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7025356/]
- 26. The normative background of empirical-ethical research [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-015-0016-x]
- 27. Evidence to inform biopharmaceutical policy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11631377/]
- 28. Standards of practice in empirical bioethics research [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-018-0304-3]
- 29. Considerations for applying bioethics norms to a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7992125/]
- 30. Reflective equilibrium, aesthetic appreciation, and ... [https://link.springer.com/article/10.1007/s11229-025-04928-5]
- 31. Integrating ethics in digital mental healthcare technologies [https://pubmed.ncbi.nlm.nih.gov/40736629/]
- 32. The Ethics of Clinical Trials in the Drug Development Process [https://www.meetlifesciences.com/media-hub/blog/the-ethics-of-clinical-trials-in-the-drug-development-process/]
- 33. The evolution of data ethics in clinical research and drug ... [https://www.sciencedirect.com/science/article/pii/S2352552520300554]
- 34. Ethical theories, governance models, and strategic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12307427/]
- 35. October 16, 2025: New Article Surveys Landscape of ... [https://rethinkingclinicaltrials.org/news/october-16-2025-new-article-surveys-landscape-of-empirical-ethics-research-related-to-pragmatic-clinical-trials/]
- 36. How to Write Empirical and Normative Aims and Methods in ... [https://philosophicalbioethics.com/?page_id=769]
- 37. Two Approaches of 'Proactive Consultation': Towards Well- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11785846/]
- 38. Collective Reflective Equilibrium, Algorithmic Bioethics and ... [https://www.cambridge.org/core/journals/cambridge-quarterly-of-healthcare-ethics/article/collective-reflective-equilibrium-algorithmic-bioethics-and-complex-ethics/E74F24C1A48271D9A9E67B360179ABC5]
- 39. Integrating ethics in digital mental healthcare technologies [https://link.springer.com/article/10.1007/s11019-025-10283-6]
- 40. Theory of meaningful stakeholder dialogue [https://www.ser.nl/en/themes/irbc/meaningful-dialogue/theory]
- 41. Stakeholder engagement champions: a locally-driven model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12143356/]
- 42. 8 Essential Stakeholder Engagement Strategies for 2025 [https://trandev.net/stakeholder-engagement-strategies/]
- 43. Normative Methods in Bioethics [https://philosophicalbioethics.com/?page_id=766]
- 44. Guidance for best practices for clinical trials [https://www.who.int/our-work/science-division/research-for-health/implementation-of-the-resolution-on-clinical-trials/guidance-for-best-practices-for-clinical-trials]
- 45. Guideline for ethics review of clinical trials [https://link.springer.com/article/10.1007/s44178-024-00122-8]
- 46. SPIRIT 2025 statement: Updated guideline for protocols of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037212/]
- 47. Integrating Quantitative and Qualitative Results in Health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4639381/]
- 48. Achieving Integration in Mixed Methods Designs—Principles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4097839/]
- 49. Is–ought problem [https://en.wikipedia.org/wiki/Is%E2%80%93ought_problem]
- 50. The normative background of empirical-ethical research [https://pmc.ncbi.nlm.nih.gov/articles/PMC4404235/]
- 51. The use of empirical research in bioethics - BMC Medical Ethics [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-017-0239-0]
- 52. Standards of practice in empirical bioethics research [https://pmc.ncbi.nlm.nih.gov/articles/PMC6038185/]
- 53. Experimental philosophical bioethics and normative ... [https://link.springer.com/article/10.1007/s11017-021-09546-z]
- 54. The “Ought-Is” Problem: An Implementation Science ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7164659/]
- 55. From 2015 to 2023, eight years of empirical research on ... [https://researchintegrityjournal.biomedcentral.com/articles/10.1186/s41073-025-00163-1]
- 56. 2025 FDAAA 801 Final Rule Changes Impacting Clinical ... [https://prorelixresearch.com/2025-fdaaa-801-clinical-trial-rule-impact/]
- 57. Defining the Role of Authors and Contributors [https://www.icmje.org/recommendations/browse/roles-and-responsibilities/defining-the-role-of-authors-and-contributors.html]
- 58. The ethics of collaborative authorship - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3166465/]
- 59. Authorship ethics in global health research partnerships ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/1472-6939-15-42]
- 60. Guidelines on Authorship in Scholarly or Scientific ... [https://division-research.brown.edu/research-cycle/conduct-research/ethics-research/guidelines-authorship-scholarly-or-scientific]
- 61. Guidelines on Authorship and Acknowledgement [https://facultyresources.fas.harvard.edu/guidelines-authorship-and-acknowledgement]
- 62. Researchers' Perceptions of Ethical Authorship Distribution in ... [https://pubmed.ncbi.nlm.nih.gov/31165383/]
- 63. Considerations for applying bioethics norms to a ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-021-00600-y]
- 64. The Vagueness of Integrating the Empirical and the Normative ... [https://pubmed.ncbi.nlm.nih.gov/37938498/]
- 65. Ethical decision-making in biopharmaceutical research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7482740/]
- 66. Applications of the Wide Reflective Equilibrium [https://link.springer.com/article/10.1007/s10892-023-09458-1]
- 67. The ground of dialogical bioethics [https://pubmed.ncbi.nlm.nih.gov/12814286/]
- 68. Reflective Equilibrium - Stanford Encyclopedia of Philosophy [https://plato.stanford.edu/entries/reflective-equilibrium/]
- 69. Reflective equilibrium in logic | Synthese [https://link.springer.com/article/10.1007/s11229-023-04480-0]
- 70. An ethical analysis of policy dialogues [https://health-policy-systems.biomedcentral.com/articles/10.1186/s12961-023-00962-2]
- 71. Ethics review, reflective equilibrium and reflexivity - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8866750/]
- 72. Collective Reflective Equilibrium and algorithmic bioethics [https://www.antitheses.net/blog/collective-reflective-equilibrium-and-algorithmic-bioethics-a-new-approach-to-complex-ethical-dilemmas]
- 73. Not whether but how: the ethics and Language of reporting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12560451/]
- 74. Transformative Learning in Digital Bioethics Education [https://www.mdpi.com/2076-2615/15/23/3398]
- 75. Ethics and Innovative Clinical Trial Designs [https://www.cmu.edu/ethics-ai/events/adaptive-trials-2025.html]
- 76. PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12306670/]
- 77. Bioethics, AI Politics, and a New World Order [https://bioethicseducation.org/bioethics-ai-politics-and-a-new-world-order-2/]
- 78. The Status of Normative Ethical Decision-Making Models [https://link.springer.com/article/10.1007/s10551-025-06094-7]
- 79. BrainSwarming, blockchain, and bioethics: applying ... [https://www.nature.com/articles/s41598-023-50232-y]
- 80. Artificial intelligence policies in bioethics and health humanities [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-025-01239-9]
- 81. Developing the ethics of implementation research in health [https://implementationscience.biomedcentral.com/articles/10.1186/s13012-016-0527-y]
- 82. The 2024 Revision of the Declaration of Helsinki and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11893356/]