Bridging the Divide: Practical Strategies for Overcoming Interdisciplinary Challenges in Bioethics Methodology
This article addresses the critical methodological challenges faced by researchers, scientists, and drug development professionals when navigating the interdisciplinary landscape of modern bioethics.
Bridging the Divide: Practical Strategies for Overcoming Interdisciplinary Challenges in Bioethics Methodology
Abstract
This article addresses the critical methodological challenges faced by researchers, scientists, and drug development professionals when navigating the interdisciplinary landscape of modern bioethics. As emerging technologies like Artificial Intelligence (AI) and biotechnology rapidly transform biomedical research, traditional ethical frameworks are often outpaced. This piece provides a comprehensive guide, moving from foundational concepts like principlism and casuistry to applied methods such as the Embedded Ethics approach. It offers practical solutions for troubleshooting pervasive issues like algorithmic bias and a lack of transparency, and validates these strategies through real-world case studies and comparative analysis of ethical frameworks. The goal is to equip researchers with the tools to integrate robust, interdisciplinary ethical analysis directly into their research and development lifecycle, fostering responsible innovation that aligns with both scientific and societal values.
The Roots of the Rift: Understanding Core Interdisciplinary Tensions in Bioethics
Technical Support Center: Troubleshooting Interdisciplinary Bioethics Methodology
This technical support center provides "troubleshooting guides" for researchers navigating the complex methodological challenges inherent in interdisciplinary bioethics research. The following FAQs address specific issues you might encounter, framed within the broader thesis of overcoming interdisciplinary barriers to strengthen methodological rigor.
Frequently Asked Questions and Troubleshooting Guides
1. FAQ: How do I resolve conflicting conclusions arising from different disciplinary methods in my bioethics research?
- Issue Description: Your research team includes members from philosophy, law, and sociology. Each applies their own disciplinary methods to a common research question (e.g., the ethics of genomic data sharing) and arrives at different, sometimes conflicting, normative conclusions. There is no agreed-upon standard to evaluate which conclusion is most valid [1].
- Troubleshooting Steps:
- Diagnose the Root Cause: Acknowledge that this conflict often stems from differing, often implicit, disciplinary standards of "rigor" and "validity" [1]. Philosophy may prioritize logical coherence, law may focus on precedent, and sociology may value empirical data.
- Isolate the Methodological Assumptions: Facilitate a team discussion to explicitly articulate the methodological assumptions and standards of evidence from each discipline. This makes the sources of conflict visible.
- Implement an Interdisciplinary Framework: Move beyond a simple multidisciplinary model (where disciplines work in parallel) towards an interdisciplinary one. Actively work to integrate perspectives, creating a synthesized analytical framework that acknowledges the strengths and limitations of each approach [1] [2]. The goal is not to find one "correct" answer, but to develop a more robust, nuanced understanding that is informed by multiple ways of knowing.
- Preventative Measures for Future Research: Establish a shared methodological framework at the project's inception. This framework should define how different types of evidence will be weighed and integrated to form normative conclusions.
2. FAQ: How can I ensure my interdisciplinary bioethics research is perceived as rigorous and credible during peer review?
- Issue Description: You are submitting a paper to a journal and are concerned that peer reviewers from a single discipline may dismiss your work as lacking rigor because it does not conform to their specific methodological standards [1].
- Troubleshooting Steps:
- Gather Contextual Information: Proactively identify potential points of methodological criticism by seeking feedback from colleagues representing each of the disciplines involved in your research before submission.
- Reproduce the Issue for Scrutiny: In the manuscript itself, explicitly justify your interdisciplinary approach. Detail the methods used from each discipline and explain how their integration strengthens the research, rather than obscuring it.
- Apply a Cross-Disciplinary Fix: Frame your work's contribution in terms that are recognized across disciplines, such as its "originality, quality, value, and validity," while carefully defining these terms within your interdisciplinary context [1].
- Solution for Widespread Impact: Advocate for and contribute to the development of field-wide standards for interdisciplinary rigor in bioethics. Support journals in recruiting interdisciplinary reviewer panels.
3. FAQ: My research team is struggling to make practical ethical recommendations for our clinical partners. Our theoretical analysis seems disconnected from the realities of the clinic. What is wrong?
- Issue Description: The ethical guidance your team has developed is theoretically sound but is failing to gain traction or provide practical decision-making support in a fast-paced clinical setting [1].
- Troubleshooting Steps:
- Practice Active Listening: Engage with clinical partners not just as subjects of study, but as collaborators. Spend time in the clinical environment to understand the pressures, constraints, and practical dilemmas they face daily.
- Ask Effective, Targeted Questions: Instead of asking purely theoretical questions, focus on context-specific ones. For example: "What specific information would be most helpful for you at the moment of decision?" or "What are the operational barriers to implementing this guidance?"
- Develop a Practical Workaround: Use empirical methods from the social sciences (e.g., qualitative interviews, ethnographic observation) to ground your normative analysis in the actual experiences and values of stakeholders [2]. This helps minimize biases like exceptionalism and reductionism, creating recommendations that are both ethically robust and practically applicable [2].
- Final Resolution: Co-design clinical ethics tools or guidelines with end-users (clinicians, patients, administrators) to ensure the output of your research is usable and directly addresses a documented need.
Experimental Protocol: An Interdisciplinary Methodology for Empirical Bioethics
This protocol outlines a structured approach for integrating empirical social science data with philosophical analysis to produce ethically robust and contextually relevant outputs.
1. Problem Identification & Team Assembly
- Objective: Define a pressing clinical ethics issue and assemble an interdisciplinary team.
- Materials: Experts from bioethics (philosophical), social science (e.g., sociology, anthropology), and clinical practice (medicine, nursing).
- Methodology:
- Hold a preliminary meeting to define the research question from multiple disciplinary viewpoints.
- Formally document the anticipated contributions and methodological standards from each discipline.
2. Empirical Data Collection & Analysis
- Objective: Gather qualitative data on stakeholder experiences and values.
- Materials: Interview guides, recording equipment, qualitative data analysis software.
- Methodology:
- Conduct semi-structured interviews or focus groups with relevant stakeholders (e.g., patients, clinicians).
- Transcribe interviews and analyze the data using established qualitative methods (e.g., thematic analysis) to identify key themes, values, and practical conflicts.
3. Normative-Philosophical Integration
- Objective: Integrate empirical findings into a structured ethical analysis.
- Materials: Output from Step 2 (empirical themes), philosophical frameworks (e.g., principlism, casuistry, virtue ethics).
- Methodology:
- Interpret the identified empirical themes through relevant philosophical frameworks.
- Critically assess how the lived reality of the clinic challenges, refines, or strengthens abstract ethical principles.
- Formulate ethical recommendations that are both philosophically sound and empirically grounded.
4. Output Co-Design & Dissemination
- Objective: Create and share a usable output.
- Materials: Draft recommendations, workshop materials.
- Methodology:
- Present the draft recommendations to a group of stakeholder representatives.
- Use a workshop format to refine the output based on feedback regarding its clarity, feasibility, and usefulness.
- Disseminate the final product through academic channels and tailored formats for practice (e.g., clinical guidelines, decision-making tools).
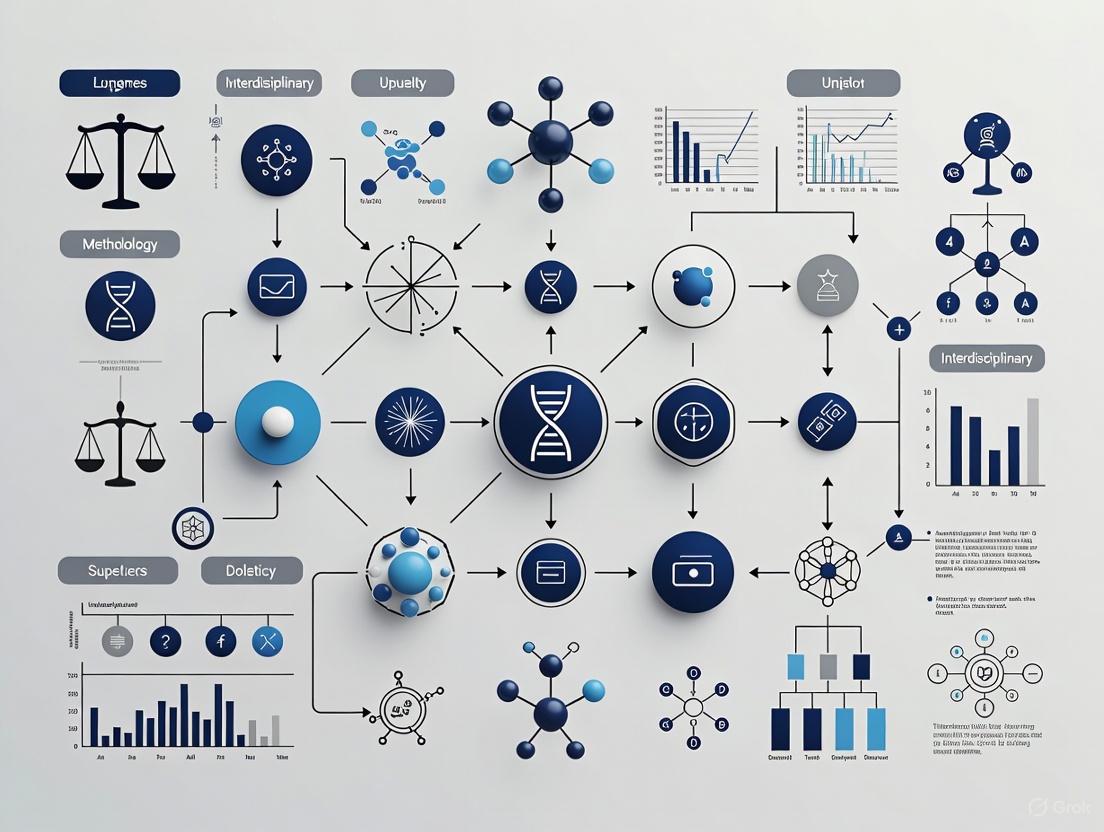
Visualizing the Interdisciplinary Workflow
The following diagram illustrates the integrated workflow of the empirical bioethics methodology, showing how different disciplinary contributions interact throughout the process.
The Researcher's Toolkit: Essential Reagents for Interdisciplinary Bioethics
The table below details key conceptual "reagents" and their functions in interdisciplinary bioethics research.
| Research Reagent | Function & Explanation |
|---|---|
| Qualitative Interview Guides | A structured protocol used to gather rich, narrative data on stakeholder experiences, values, and reasoning, grounding ethical analysis in empirical reality [2]. |
| Philosophical Frameworks | Conceptual tools (e.g., Principlism, Virtue Ethics) that provide a structured language and logical system for analyzing moral dilemmas and constructing normative arguments [1]. |
| Legal & Regulatory Analysis | The systematic review of statutes, case law, and policies to understand the existing normative landscape and legal constraints surrounding a bioethical issue [2]. |
| Collaborative Governance Model | A project management structure that explicitly defines roles for all disciplinary experts and stakeholders, ensuring equitable integration of perspectives from start to finish [2]. |
| Bias Mitigation Strategies | Deliberate techniques (e.g., reflexive journaling, devil's advocate) used to identify and challenge disciplinary biases like exceptionalism or reductionism within the research team [2]. |
Bioethics research inherently involves integrating diverse disciplinary perspectives, from philosophy and medicine to law and sociology [1]. This interdisciplinary nature creates methodological challenges, as there is no single, agreed-upon standard of rigor for evaluating ethical questions [1]. Researchers and clinicians must navigate these complexities when addressing moral dilemmas in biomedical contexts. This technical support framework provides structured guidance for applying three foundational ethical theories—Utilitarianism, Deontology, and Virtue Ethics—to practical research scenarios, thereby promoting methodological consistency and rigorous ethical analysis.
Frequently Asked Questions (FAQs): Core Ethical Concepts
Q1: What are the fundamental differences between these three major ethical theories?
- Virtue Ethics focuses on the agent or person, emphasizing character and the pursuit of moral excellence (arete) through virtues. It answers the question, "Who should I be?" [3].
- Deontology focuses on the act itself, concerned with moral duties, rules, and obligations regardless of consequences. It is rooted in principles like Kant's categorical imperative [3] [4].
- Utilitarianism (a form of consequentialism) focuses on the outcome or consequences of an action. It seeks to maximize happiness and minimize pain for the greatest number of people [3] [4].
Q2: How does the principle of justice manifest differently across these theories?
Q3: Can these ethical frameworks be combined in practice? Yes, in practice, these frameworks are often combined. Principlism in bioethics, for example, integrates aspects of these theories into a practical framework built on autonomy, beneficence, non-maleficence, and justice [4]. The challenge lies in balancing these perspectives, such as weighing deontology's patient-centered duties against utilitarianism's society-centered outcomes during a public health crisis [4].
Ethical Theory Troubleshooting Guide
This guide helps diagnose and resolve common ethical problems in biomedical research.
Problem: A conflict arises between patient welfare and collective public health interests.
| Ethical Theory | Diagnostic Questions | Proposed Resolution Pathway |
|---|---|---|
| Utilitarianism | - Which action will produce the best overall consequences?- How can we maximize well-being for the largest number of people?- Does the benefit to the majority outweigh the harm to a minority? | 1. Calculate the potential benefits and harms for all affected parties.2. Choose the course of action that results in the net greatest good. |
| Deontology | - What are my fundamental duties to this patient?- Does this action respect the autonomy and dignity of every individual?- Am I following universally applicable moral rules? | 1. Identify core duties (e.g., to tell the truth, not to harm).2. Uphold these duties, even if doing so leads to suboptimal collective outcomes. |
| Virtue Ethics | - What would a compassionate and just researcher do?- How can this decision reflect the character of a good medical professional?- Which action contributes to my eudaimonia (flourishing) as an ethical person? | 1. Reflect on the virtues essential to your role (e.g., integrity, empathy).2. Act in a way that embodies those virtues. |
Problem: Determining informed consent protocols for vulnerable populations.
Experimental Protocol: Analyzing an Ethical Dilemma
This protocol provides a systematic methodology for analyzing ethical dilemmas in biomedical research, ensuring a structured and interdisciplinary approach.
Materials and Reagents
Table: Essential Materials for Ethical Analysis
| Material | Function |
|---|---|
| Case Description Document | Provides a detailed, factual account of the ethical dilemma for analysis. |
| Stakeholder Map | Identifies all affected individuals, groups, and institutions and their interests. |
| Ethical Frameworks Checklist | A list of core questions from Utilitarian, Deontological, and Virtue Ethics perspectives. |
| Regulatory and Legal Guidelines | Reference materials (e.g., Belmont Report, Declaration of Helsinki) to ensure compliance [4] [5]. |
Methodology
- Case Formulation: Write a precise, neutral description of the case, outlining the facts, context, and the specific ethical conflict.
- Stakeholder Mapping: Identify all parties affected by the decision. For each stakeholder, note their interests, rights, and potential harms/benefits.
- Multi-Theoretical Analysis: Analyze the case sequentially through the lens of each ethical theory using the questions in the troubleshooting guide.
- Resolution Weighing: List potential resolutions. For each resolution, summarize the arguments for and against it based on the three ethical analyses.
- Reflective Equilibrium: Seek a coherent judgment by going back and forth between the case details, the ethical principles, and the proposed resolutions, refining each until a stable, justified outcome is reached.
Workflow Visualization
Conceptual Mapping of Ethical Theories
The following diagram illustrates the logical relationships and primary focus of each major ethical theory within a biomedical context.
Table: Comparative Analysis of Ethical Theories in Biomedical Contexts
| Feature | Utilitarianism | Deontology | Virtue Ethics |
|---|---|---|---|
| Primary Focus | Outcome / Consequence [3] | Act / Duty [3] | Agent / Character [3] |
| Core Question | What action maximizes overall well-being? | What is my duty, regardless of outcome? | What would a virtuous person do? |
| Key Proponents | Bentham, Mill [3] | Kant [3] | Aristotle [3] |
| Central Concept | Greatest Happiness Principle [3] | Categorical Imperative [3] | Eudaimonia (Human Flourishing) [3] |
| Strengths in Biomedicine | Provides a clear calculus for public health policy; aims for objective, collective benefit [4]. | Robustly defends individual rights and autonomy; provides clear rules [4]. | Holistic; integrates motive, action, and outcome; emphasizes professional integrity [3]. |
| Weaknesses in Biomedicine | May justify harming minorities for majority benefit; can be impractical to calculate all consequences [4]. | Can be rigid; may ignore disastrous outcomes of "right" actions [3]. | Can be vague; virtues may be interpreted differently; lacks specific action-guidance [3]. |
| Biomedical Example | Rationing a scarce drug to save the most lives during a pandemic. | Obtaining informed consent from every research participant, without exception. | A researcher displaying compassion when withdrawing a patient from a trial. |
Modern research, particularly in the drug development and biopharmaceutical fields, operates at the intersection of scientific innovation and profound ethical responsibility. Navigating the complex challenges that arise requires a robust and systematic framework. This technical support center is designed to help researchers, scientists, and drug development professionals identify, analyze, and resolve these interdisciplinary ethical dilemmas by applying the four core principles of bioethics: Autonomy (respect for individuals' right to self-determination), Beneficence (the obligation to do good), Non-maleficence (the duty to avoid harm), and Justice (ensuring fairness and equity) [6]. By framing common operational challenges within this structure, we provide a practical methodology for upholding ethical standards in daily research practice.
Ethical Troubleshooting Guides
Guide 1: Participant Recruitment and Informed Consent
This section addresses common ethical challenges in enrolling research participants and obtaining truly informed consent.
Problem: Inconsistent comprehension during the consent process.
- Ethical Principle Affected: Autonomy. A key component of informed consent is that the participant comprehends the disclosure [6].
- Root Cause: Complex scientific language, inadequate time for discussion, or cultural and health literacy barriers.
- Solution: Implement a multi-stage consent process. Provide consent documents well in advance, use teach-back methods to confirm understanding, and allow for a "cooling-off" period where participants can discuss with family or advisors. Ensure documents are translated and culturally adapted for the target population.
Problem: Selection bias leading to non-representative cohorts.
- Ethical Principle Affected: Justice. This principle demands a fair distribution of the benefits and burdens of research [6] [7].
- Root Cause: Over-reliance on convenient recruitment channels (e.g., single clinic sites) or overly restrictive eligibility criteria that are not scientifically justified.
- Solution: Utilize diverse recruitment strategies, including social media and community outreach, to reach underrepresented groups [7]. Employ randomization techniques to minimize selection bias and critically review eligibility criteria to ensure they are necessary [7].
Problem: Perceived therapeutic misconception.
- Ethical Principle Affected: Autonomy and Non-maleficence. Participants may incorrectly believe that the primary goal of the research is to provide them with therapeutic benefit, potentially leading to harm if they for proven treatments.
- Root Cause: Insufficient clarity in communication that distinguishes research from clinical care.
- Solution: Explicitly and repeatedly state the research nature of the intervention. Clearly explain the difference between diagnostic tests for clinical care and those for research data collection. Document these discussions within the consent form.
Guide 2: Data Integrity, Privacy, and Security
This guide focuses on ethical challenges related to the handling and protection of research data.
Problem: High background noise or non-specific binding in sensitive assays (e.g., ELISA).
- Ethical Principle Affected: Beneficence and Non-maleficence. Inaccurate data can lead to incorrect conclusions, potentially harming future patients who receive an unsafe or ineffective product [7].
- Root Cause: Contamination of kit reagents by concentrated sources of the analyte, improper washing techniques, or use of incompatible equipment [8].
- Solution: Strictly segregate pre- and post-sample analysis workspaces. Clean all surfaces and equipment before use, and employ pipette tips with aerosol filters. Use only the recommended wash buffers and techniques to avoid introducing artifacts [8].
Problem: Inappropriate data interpolation from non-linear assay results.
- Ethical Principle Affected: Beneficence and Non-maleficence. Using an incorrect curve-fitting model (e.g., linear regression for an inherently non-linear immunoassay) introduces inaccuracies, especially at the critical low and high ends of the standard curve [8].
- Root Cause: Reliance on R-squared values without validating the model's accuracy across the analytical range.
- Solution: Use robust curve-fitting routines like Point-to-Point, Cubic Spline, or 4-Parameter logistics. Validate the model by "back-fitting" the standards as unknowns; the model should report their nominal values accurately [8].
Problem: Risk of participant re-identification from shared data.
- Ethical Principle Affected: Autonomy (Confidentiality) and Non-maleficence. Breaching confidentiality violates the trust established in the informed consent process and could cause harm to the participant [6] [7].
- Root Cause: Data sharing without proper de-identification protocols or insufficient data security measures.
- Solution: Store personal identifiers and scientific data separately. Limit data access through role-based controls and establish data use agreements with all external partners. Implement strong cybersecurity measures for electronic data, especially with the rise of wearables and EHRs [7].
Guide 3: Risk-Benefit Analysis and Post-Trial Responsibilities
This section tackles challenges in evaluating risks and benefits and upholding responsibilities after a trial concludes.
Problem: Difficulty quantifying and communicating uncertain risks.
- Ethical Principle Affected: Autonomy and Non-maleficence. Participants cannot make an autonomous decision without a realistic understanding of potential risks.
- Root Cause: Inherent scientific uncertainties in early-phase research and the use of vague, non-quantitative language.
- Solution: Conduct a thorough risk-benefit assessment that considers the severity, frequency, and preventability of adverse reactions [7]. Communicate risks using clear, quantitative terms where possible (e.g., "this side effect was seen in approximately 1 in 10 patients at this dose level") and acknowledge uncertainties explicitly.
Problem: Ensuring continued access to beneficial treatment post-trial.
- Ethical Principle Affected: Justice and Beneficence. It is unjust if only participants in certain regions or from wealthy backgrounds can continue a life-saving treatment after the trial ends [7].
- Root Cause: Lack of pre-trial planning and funding for post-trial access, particularly in globalized trials.
- Solution: Address post-trial access plans during the study design and ethics review phase. Develop transparent policies for providing continued treatment, detailing eligibility and duration. Facilitate a seamless transition for participants back to the standard healthcare system [7].
Problem: Managing incidental findings.
- Ethical Principle Affected: Beneficence and Autonomy. Researchers have an obligation to act on potentially clinically significant findings discovered during research, but must also respect the participant's right not to know.
- Root Cause: Advances in diagnostic technologies that reveal information beyond the primary research objectives.
- Solution: Establish a clear protocol before the study begins. This should define what constitutes a reportable incidental finding, outline the process for clinical confirmation, and detail how participants will be offered the option to receive or decline such information during the consent process.
Frequently Asked Questions (FAQs)
Q1: How can we apply the principle of autonomy in cultures with a family- or community-centered decision-making model? A1: Respecting autonomy does not necessarily mean imposing a Western individualistic model. The principle can be upheld through relational autonomy, which acknowledges that decisions are often made within a social context [6]. The consent process should involve engaging with the family or community leaders as the patient desires, while still ensuring that the individual participant's values and preferences are respected and that they provide their ultimate agreement [9].
Q2: What are the emerging ethical concerns with using AI and Machine Learning in drug development? A2: The primary concerns revolve around accountability, transparency, and bias [7]. While AI can automate tasks and save time, algorithmic decision-making without human oversight may perpetuate or amplify existing biases in training data, leading to unjust outcomes. There is also a risk of a "black box" effect where the rationale for a decision is unclear, challenging the principles of beneficence and non-maleficence. Ensuring human-in-the-loop validation and auditing algorithms for bias are critical steps [7].
Q3: How can a values-based framework, like the TRIP & TIPP model, help in daily R&D decisions? A3: A structured model, such as the one using values (Transparency, Respect, Integrity, Patient Focus) and contextual factors (Timing, Intent, Proportionality, Perception), provides a practical, prospective decision-making tool [10]. It engages employees as moral agents by asking specific framing questions (e.g., "How does this solution put the patient's interests first?" or "Is the solution proportional to the situation?") to assess options against the organization's core values before a decision is finalized, reducing the need for top-down rules [10].
Q4: How does the principle of justice apply to environmental sustainability in pharmaceutical research? A4: Environmental ethics is an increasingly important aspect of justice. It involves the responsible use of resources and minimizing the environmental impact of drug manufacturing [7]. This aligns with global justice, as pollution and climate change disproportionately affect vulnerable populations. Furthermore, justice requires ensuring equitable distribution of treatments for global health emergencies, rather than focusing only on profitable markets [7].
Quantitative Data in Ethical Research
The following table summarizes key quantitative considerations for ensuring ethical compliance in clinical trials, directly supporting the principles of justice and beneficence.
Table 1: Key Quantitative Benchmarks for Ethical Clinical Trial Management
| Aspect | Quantitative Benchmark | Ethical Principle & Rationale |
|---|---|---|
| Informed Consent Comprehension | > 80% score on a comprehension questionnaire post-consent discussion. | Autonomy: Ensures participants have adequate understanding to exercise self-determination. |
| Participant Diversity | Recruitment goals should aim to reflect the demographic prevalence of the disease, including racial, ethnic, and gender diversity. | Justice: Ensures fair burden and benefit sharing; data on drug efficacy and safety are representative. |
| Data Quality Control | Spike-and-recovery experiments for sample diluents should yield recoveries of 95% to 105% [8]. | Beneficence/Non-maleficence: Ensures data integrity, which is foundational to making correct conclusions about safety and efficacy. |
| Data Monitoring Committee (DMC) Review | Interim safety reviews triggered by pre-defined thresholds (e.g., specific serious adverse event rates). | Non-maleficence: Protects current participants from undue harm by allowing for early trial termination if risks outweigh benefits. |
| Post-Trial Access Transition | Plan for seamless transition, with a defined timeframe (e.g., supply of investigational product for 30-60 days post-trial). | Justice/Beneficence: Prevents abrupt cessation of care for participants who benefited from the investigational product. |
Experimental Protocol: An Ethics-Based Risk Assessment
This protocol provides a methodology for prospectively evaluating a research study's ethical soundness.
Objective: To systematically identify, assess, and mitigate ethical risks in a research protocol before implementation.
Materials: Research protocol document, multidisciplinary team (e.g., clinical researcher, bioethicist, patient representative, data manager).
Methodology:
- Stakeholder Mapping: Identify all stakeholders (e.g., participants, researchers, sponsors, the community) and how the research impacts them.
- Principle-by-Principle Review:
- Autonomy: Walk through the informed consent process. Is the language accessible? Is there a plan to assess comprehension? How are cultural preferences for decision-making incorporated?
- Beneficence/Non-maleficence: List all potential benefits and harms (physical, psychological, social, economic). Quantify their likelihood and severity. Justify that the potential benefits outweigh the risks.
- Justice: Scrutinize the participant selection criteria. Is the population inclusive of those who will use the drug? Are there groups being excluded without scientific justification?
- Contextual Factor Analysis (TIPP): Evaluate the proposal using the TIPP framework [10]:
- Timing: Is this the right time for this research, considering public health needs and available standard of care?
- Intent: Is the primary aim scientific communication and patient benefit, or are there conflicting commercial or promotional intentions?
- Proportionality: Is the scale of the research (number of participants, resources) proportionate to the question it seeks to answer?
- Perception: How would the research plan be perceived by the public or a skeptical audience? Is it transparent and trustworthy?
- Mitigation Planning: For each identified ethical risk, develop a specific mitigation strategy (e.g., enhanced consent process, revised eligibility criteria, a DMC charter).
Visualizing the Ethical Decision-Making Workflow
The following diagram illustrates the structured, five-step process for applying ethical principles to resolve complex research dilemmas, integrating company values and contextual factors [10].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Materials and Their Ethical Significance
| Item | Function | Ethical Principle Connection |
|---|---|---|
| Validated & De-identified Biobank Samples | Provides biological specimens for research while protecting donor identity. | Autonomy/Respect: Requires proper informed consent for storage and future use. Justice: Promotes equitable resource sharing. |
| Accessible Data Visualization Tools | Software with built-in, colorblind-friendly palettes (e.g., Viridis, Cividis) and perceptually uniform color gradients [11] [12]. | Justice: Ensures scientific information is accessible to all colleagues and the public, regardless of visual ability. Prevents exclusion and misinterpretation. |
| Role-Based Electronic Data Capture (EDC) System | Securely collects and manages clinical trial data with tiered access levels. | Confidentiality (Autonomy): Protects participant privacy. Integrity: Ensures data accuracy and traceability, supporting beneficence and non-maleficence. |
| Contamination-Free Assay Reagents | Highly sensitive ELISA kits and related reagents for accurate impurity detection [8]. | Beneficence/Non-maleficence: Accurate data is fundamental to ensuring product safety and efficacy. Preventing contamination is a technical and ethical imperative. |
| Multilingual Consent Form Templates | Standardized consent documents that can be culturally and linguistically adapted. | Autonomy: Empowers participants by providing information in their native language, facilitating true understanding and voluntary agreement. |
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: Our predictive model for patient health risks performs well overall but shows significantly lower accuracy for our minority patient populations. What are the first steps we should take to investigate this?
A1: This pattern suggests potential data bias. Begin your investigation by auditing your training data for representation disparities and label quality across different demographic groups [13]. You should also analyze the model's feature selection process to determine if it is disproportionately relying on proxies for sensitive attributes [14]. Technically, you can employ adversarial de-biasing during training, which involves jointly training your predictor and an adversary that tries to predict the sensitive attribute (e.g., race) from the model's representations. If the adversary fails, it indicates the representation does not encode bias [15].
Q2: We are developing an early warning system for use in a clinical nursing setting. What are the primary ethical risks we should address in our design phase?
A2: The key ethical risks can be categorized into five dimensions [16]:
- Data- and Algorithm-Related Risks: Including data privacy breaches and algorithmic unfairness.
- Professional Role Risks: Ambiguity in responsibility attribution when algorithm-driven decisions lead to errors.
- Patient Rights Risks: Potential dehumanization of care and threats to patient autonomy.
- Governance Risks: Lack of transparency and potential for misuse of the system.
- Accessibility Risks: Barriers to the technology's adoption and social acceptance.
Q3: A fairness audit has revealed that our algorithm exhibits bias. What are some algorithmic techniques we can use to mitigate this bias without scrapping our entire model?
A3: Several technical approaches can be implemented [15]:
- Adversarial De-biasing: As described above, this technique protects sensitive attributes by making it impossible for an adversary to predict them from the model's internal representations.
- Variational Fair Autoencoders (VFAE): This is a semi-supervised method that learns an invariant representation of the data by explicitly separating sensitive attributes (
s) from other latent variables (z). It uses a Maximum Mean Discrepancy (MMD) penalty to ensure the distributions ofzare similar across different groups of the sensitive attribute. - Dynamic Upsampling: This technique involves intelligently upsampling underrepresented groups in the training data based on learned latent representations.
- Distributionally Robust Optimization: This method prevents disparity amplification by optimizing the model for worst-case subgroup performance.
Q4: Our interdisciplinary team, comprising computer scientists, bioethicists, and clinicians, often struggles with aligning on a definition of "fairness." How can we navigate this challenge?
A4: This is a core interdisciplinary challenge. Facilitate a series of workshops to explicitly define and document the operational definition of fairness for your specific project context. You should map technical definitions (e.g., demographic parity, equalized odds) to clinical and ethical outcomes. Furthermore, establish a continuous monitoring framework to assess the chosen fairness metric's real-world impact, acknowledging that definitions may need to evolve [16] [14].
Troubleshooting Common Experimental Issues
| Issue | Symptom | Potential Cause | Solution |
|---|---|---|---|
| Performance Disparity | Model accuracy/recall is significantly lower for a specific demographic subgroup [14]. | Non-representative Training Data, Feature Selection Bias, or Temporal Bias where disease patterns have changed [13]. | 1. Audit and rebalance training datasets.2. Apply algorithmic fairness techniques like adversarial de-biasing [15].3. Implement continuous monitoring and model retraining protocols. |
| Feedback Loop | The model's predictions over time reinforce existing biases and reduce accuracy [14]. | Development Bias where the model is trained on data reflecting past human biases, creating a self-reinforcing cycle. | Design feedback mechanisms that collect ground truth data independent of the model's predictions. Regularly audit model outcomes for reinforcing patterns. |
| "Black Box" Distrust | Clinical end-users (e.g., nurses) do not trust the model's recommendations and override them [16]. | Lack of Transparency and Explainability, leading to a conflict with professional autonomy. | Integrate Explainable AI (XAI) techniques to provide rationale for predictions. Involve end-users in the design process and provide digital literacy training [16]. |
| Responsibility Gaps | Uncertainty arises when the model makes an erroneous recommendation; it is unclear who is accountable [16]. | Unclear Governance and Accountability frameworks for shared human-AI decision-making. | Develop clear organizational policies that delineate responsibility between developers, clinicians, and institutions. Establish an ethical review board [16]. |
Quantitative Analysis of Algorithmic Bias
Table 1: Categorization and Prevalence of Bias in Medical AI
| Bias Category | Source / Sub-type | Description | Example in a Medical Context |
|---|---|---|---|
| Data Bias | Historical Data Bias | Training data reflects existing societal or health inequities [14]. | An algorithm trained on healthcare expenditure data unfairly allocates care resources because it fails to account for different access patterns among racial groups [14]. |
| Reporting Bias | Certain events or outcomes are reported at different rates across groups. | Under-reporting of symptoms in a specific demographic leads to a model that is less accurate for that group. | |
| Development Bias | Algorithmic Bias | The model's objective function or learning process inadvertently introduces unfairness [13]. | A model optimized for overall accuracy may sacrifice performance on minority subgroups. |
| Feature Selection Bias | Chosen input variables act as proxies for sensitive attributes [13]. | Using "postal code" as a feature, which is highly correlated with race and socioeconomic status. | |
| Interaction Bias | Temporal Bias | Changes in clinical practice, technology, or disease patterns over time render the model obsolete or biased [13]. | A model trained pre-pandemic may be ineffective for post-pandemic patient care. |
| Feedback Loop | Model predictions influence future data collection, reinforcing initial biases [14]. | A predictive policing algorithm leads to over-policing in certain neighborhoods, generating more arrest data that further biases the model [14]. |
Table 2: Governance Pathways for Ethical AI in Healthcare
| Governance Pathway | Concrete Measures | Key Objective |
|---|---|---|
| Technical–Data Governance [16] | Privacy-preserving techniques (e.g., federated learning), bias monitoring dashboards, fairness audits. | To ensure data security and algorithmic fairness through technical safeguards. |
| Clinical Human–Machine Collaboration [16] | Nurse and clinician training in AI literacy, designing transparent interfaces, interdisciplinary co-creation teams. | To foster trust and effective collaboration between healthcare professionals and AI systems. |
| Organizational-Capacity Building [16] | Establishing AI ethics review boards, creating clear accountability frameworks, investing in continuous staff training. | To build institutional structures that support the ethical deployment and use of AI. |
| Institutional–Policy Regulation [16] | Developing and enforcing clinical guidelines for AI use, promoting standardised reporting of model performance and fairness. | To create a regulatory environment that ensures safety, efficacy, and equity. |
Experimental Protocols
Protocol 1: Adversarial De-biasing for Fair Representation Learning
Objective: To train a predictive model that learns a representation of the input data which is maximally informative for the target task (e.g., predicting patient risk) while being minimally informative about a protected sensitive attribute (e.g., race or gender).
Methodology:
- Model Architecture: Construct a multi-head neural network.
- A shared encoder network,
g(X), that learns a representation of the input data. - A predictor head,
f(g(X)), which is trained to minimize the prediction loss for the target labelY. - An adversary head,
a(g(X)), which is trained to minimize the prediction loss for the sensitive attributeZfrom the shared representationg(X).
- A shared encoder network,
- Training Procedure: The overall optimization is a minimax game with the following objective [15]:
- Minimize the predictor's loss
L_y(f(g(X)), Y). - Maximize (or minimize the negative of) the adversary's loss
L_z(a(g(X)), Z). - This is achieved by using a gradient reversal layer (
J_λ) between the shared encoder and the adversary. During backpropagation, this layer passes gradients to the encoder with a negative factor (-λ), encouraging the encoder to learn features that confuse the adversary.
- Minimize the predictor's loss
- Hyperparameters: The trade-off between prediction accuracy and fairness is controlled by the hyperparameter
λ.
Protocol 2: Bias Audit using Variational Fair Autoencoder (VFAE)
Objective: To learn a latent representation of the data that is invariant to a specified sensitive attribute, and to use this representation for downstream prediction tasks to reduce bias.
Methodology:
- Architecture: Employ a Variational Autoencoder (VAE) framework with a specific structure designed for fairness.
- The model assumes a data generation process where an input
xis generated from a sensitive variablesand a latent variablez1that encodes the remaining, non-sensitive information. - To prevent
z1from becoming degenerate, a second latent variablez2is introduced to capture noise not explained by the labely.
- The model assumes a data generation process where an input
- Loss Function: The model is trained by maximizing a penalized variational lower bound. The key component for fairness is the Maximum Mean Discrepancy (MMD) penalty, which is added to the standard VAE loss [15].
- MMD Penalty: This term explicitly encourages the distributions of the latent representation
z1to be similar across different values of the sensitive attributes(e.g.,q_φ(z1|s=0)andq_φ(z1|s=1)). It measures the distance between the mean embeddings of these two distributions in a reproducing kernel Hilbert space (RKHS). - Semi-supervised Application: This architecture can naturally handle both labelled and unlabelled data, making it suitable for real-world clinical settings where labels may be scarce.
Visualizations
Adversarial De-biasing Workflow
VFAE Architecture for Invariant Representations
Five Ethical Risks and Four Governance Pathways
The Scientist's Toolkit: Research Reagent Solutions
| Item / Solution | Function in Bias Mitigation |
|---|---|
| Adversarial De-biasing Framework | A neural network architecture designed to remove dependence on sensitive attributes by using a gradient reversal layer to "confuse" an adversary network [15]. |
| Variational Fair Autoencoder (VFAE) | A semi-supervised generative model that learns an invariant data representation by leveraging a Maximum Mean Discrepancy (MMD) penalty to ensure latent distributions are similar across sensitive groups [15]. |
| AI Fairness 360 (AIF360) Toolkit | An open-source library containing a comprehensive set of metrics for measuring dataset and model bias, and algorithms for mitigating bias throughout the ML pipeline. |
| Fairness Auditing Dashboard | A custom software tool for continuously monitoring model performance and fairness metrics (e.g., demographic parity, equalized odds) across different subgroups in a production environment [16]. |
| Interdisciplinary Review Board (IRB) | A governance structure, not a technical tool, but essential for evaluating the ethical implications of AI systems. It should include bioethicists, clinicians, data scientists, and legal experts [16]. |
Welcome to the Interdisciplinary Support Center
This support center provides troubleshooting guides and FAQs to help researchers, scientists, and drug development professionals overcome common interdisciplinary communication challenges in bioethics methodology research. The resources below address specific issues that arise when translating technical jargon across domains.
Frequently Asked Questions
Q: Why do my protocol descriptions frequently get misinterpreted when shared with ethics review boards?
A: This is a common interdisciplinary challenge. Ethics board members may lack the specific technical context you possess. To mitigate this:
- Pre-define all acronyms and technical terms in a shared glossary at the beginning of your document.
- Use analogies that relate complex biological processes to more familiar concepts.
- Structure your methodology using visual workflows (see diagrams below) to make the process flow logically clear, even to non-specialists.
Q: How can I ensure the ethical implications of my technical work are accurately understood by a diverse research team?
A: Foster a shared conceptual framework.
- Develop cross-disciplinary lexicons: Create a living document of key terms with definitions from both technical and ethical perspectives.
- Implement structured communication protocols: Hold kickoff meetings where each discipline explains their core concepts and potential ethical red flags to the others.
- Use scenario-based planning: Walk through the experimental protocol step-by-step as a group to identify and discuss potential ethical decision points.
Q: What is the most effective way to present quantitative data on drug efficacy to an audience that includes bioethicists, scientists, and regulators?
A: Clarity and context are paramount. Present data in clearly structured tables that allow for easy comparison. Always pair quantitative results with a qualitative interpretation that explains the significance of the data from both a scientific and an ethical standpoint. Avoid presenting data without this crucial narrative framing.
Troubleshooting Common Experimental Workflow Gaps
Problem: Critical communication breakdowns occur at handoff points between molecular biology teams and clinical research teams.
Solution: Implement the standardized Interdisciplinary Experimental Workflow.
Interdisciplinary Research Workflow
Problem: A key ethical consideration is overlooked in the early stages of experimental design, causing delays and protocol revisions later.
Solution: Utilize the Ethical Risk Assessment Pathway to embed ethics throughout the research lifecycle.
Ethical Risk Assessment Pathway
Data Presentation Standards
| Metric | Molecular Biology Data | Clinical Application Data | Bioethics Significance |
|---|---|---|---|
| Drug Efficacy Rate | 95% Target Protein Inhibition | 70% Patient Response Rate | Informs risk/benefit analysis for vulnerable populations. |
| Adverse Event Incidence | 5% High-grade in model | 2% Occurrence in Phase II trial | Critical for informed consent documentation clarity. |
| Statistical Significance (p-value) | p < 0.001 | p < 0.01 | Determines threshold for claiming effectiveness versus overstating results. |
Table 2: Research Reagent Solutions for Cross-Disciplinary Studies
| Reagent / Material | Function in Experiment | Interdisciplinary Consideration |
|---|---|---|
| CRISPR-Cas9 Gene Editing System | Precise genomic modification for creating disease models. | Raises ethical questions on genetic alteration boundaries; requires clear explanation for non-specialists. |
| Primary Human Cell Lines | Provides a more physiologically relevant experimental model. | Sourcing and informed consent documentation are paramount for ethics review; provenance must be unambiguous. |
| Polymerase Chain Reaction (PCR) Kits | Amplifies specific DNA sequences for detection and analysis. | Technical "cycle threshold" values must be translated into clinical detectability/likelihood concepts. |
| Informed Consent Form Templates | Legal and ethical requirement for human subjects research. | Language must be translated from legalese into technically accurate yet comprehensible layperson's terms. |
Experimental Protocol: Assessing Cross-Disciplinary Comprehension
Objective
To quantitatively and qualitatively measure the effectiveness of jargon-translation strategies in conveying a complex experimental methodology to an interdisciplinary audience.
Methodology
- Participant Recruitment: Form three groups: (1) technical specialists, (2) bioethicists, and (3) drug development professionals.
- Material Preparation: Develop two versions of a complex experimental protocol:
- Version A: Uses standard, domain-specific technical language.
- Version B: Incorporates a glossary, visual aids (see workflows above), and translated jargon.
- Procedure: Randomly assign participants to review either Version A or Version B. Following review, all participants complete a standardized assessment measuring:
- Accuracy: Comprehension of the protocol's core steps and objectives.
- Efficiency: Time taken to complete the assessment.
- Perceived Clarity: Self-reported rating of the material's understandability.
- Data Analysis: Compare assessment scores, completion times, and clarity ratings between groups and between the two protocol versions using statistical analysis (e.g., ANOVA).
Expected Outcome
It is hypothesized that Version B of the protocol will yield significantly higher comprehension accuracy, faster reading times, and higher perceived clarity across all three professional groups, demonstrating the efficacy of structured communication tools in bridging interdisciplinary gaps.
From Theory to Practice: Implementing Integrated Ethical Methodologies
Introducing the Embedded Ethics and Social Science Approach
Core Concepts and Workflow
The Embedded Ethics and Social Science (EESS) approach integrates ethicists and social scientists directly into technology development teams. This interdisciplinary collaboration proactively identifies and addresses ethical and social concerns throughout the research lifecycle, moving beyond after-the-fact analysis to foster responsible, inclusive, and ethically-aware technology innovation in healthcare and beyond [17].
Key Characteristics of the EESS Approach
| Characteristic | Description |
|---|---|
| Integration | Ethics and social science researchers are embedded within the project team, participating in regular meetings and day-to-day work [17]. |
| Interdisciplinarity | Fosters collaboration between ethicists, social scientists, AI researchers, and domain specialists (e.g., clinicians) from the project's outset [17]. |
| Proactivity | Aims to anticipate ethical and social concerns before they manifest as real-world harm, shaping responsible technology innovation [17]. |
| Contextual Sensitivity | Develops a profound understanding of the project's specific technological details and application context [17]. |
Implementation Workflow
The diagram below illustrates the continuous and iterative workflow for implementing the Embedded Ethics approach:
The Researcher's Toolkit: EESS Methodologies
The EESS approach employs a toolbox of empirical and normative methods. The table below details these key methodologies and their primary functions in the research process.
Methodological Toolbox
| Method | Primary Function in EESS |
|---|---|
| Stakeholder Analyses [17] | Identifies all relevant parties affected by the technology to understand the full spectrum of impacts and values. |
| Literature Reviews [17] | Establishes a foundation in existing ethical debates and empirical social science research relevant to the project. |
| Ethnographic Approaches [17] | Provides deep, contextual understanding of the practices and cultures within the development and deployment environments. |
| Peer-to-Peer Interviews [17] | Elicits insider perspectives and unarticulated assumptions within the interdisciplinary project team. |
| Focus Groups [17] | Generates data on collective views and normative stances regarding the technology and its implications. |
| Bias Analyses [17] | Systematically examines datasets and algorithms for potential discriminatory biases or unfair outcomes. |
| Workshops [17] | Facilitates collaborative problem-solving and interdisciplinary inquiry into identified ethical concerns. |
Troubleshooting Common Implementation Challenges
Problem 1: Lack of Team Engagement
The Challenge: The embedded ethics team is not adequately involved in core project meetings or strategic discussions, limiting their understanding and impact.
The Solution:
- Secure leadership buy-in from the outset to mandate participation in regular team meetings [18].
- Clarify roles and responsibilities for all team members, including embedded ethicists, within the project protocol [19].
- Foster a collaborative culture by having the embedded researcher spend time in the team's environment and participate in day-to-day work on a social level [17].
Problem 2: Identifying Relevant Ethical Issues
The Challenge: The project team struggles to anticipate potential ethical and social concerns during the planning and early development stages.
The Solution:
- Conduct a structured ethical walkthrough at the project's start. Use key questions to scope potential issues [18]:
- Perform an initial stakeholder analysis to map all parties affected by the technology and anticipate issues of justice and fairness [17].
Problem 3: Managing Interdisciplinary Communication
The Challenge: Communication barriers between ethicists, social scientists, and technical staff hinder effective collaboration.
The Solution:
- Establish a shared vocabulary and encourage team members to clarify technical details and ethical concepts during meetings [17].
- Use iterative feedback loops. Present initial ethical analyses and refine them based on technical feedback, moving between established debates and specific development problems [17].
- Employ visual aids, such as workflow diagrams, to make complex ethical considerations and project relationships accessible to all disciplines [19].
Problem 4: Integrating Ethics into Technical Workflows
The Challenge: Ethical reflections remain theoretical and are not translated into practical changes in the technology's design or deployment.
The Solution:
- Focus on "bias analyses" as a concrete method to collaborate with technical teams on a well-defined problem, leading to tangible improvements in algorithms or datasets [17].
- Develop a publication policy early on that clarifies how results will be disseminated, which can serve as a concrete framework for discussing responsible communication [19].
- Co-design solutions. The embedded ethicist should not only identify problems but also work directly with developers to advise on and help design ethically-informed technical solutions [17].
Essential Research Reagent Solutions
In the context of EESS, "research reagents" are the conceptual tools and frameworks used to conduct the analysis. The table below lists essential items for this methodological approach.
EESS Research Reagents
| Item / Framework | Function in EESS |
|---|---|
| Research Protocol [19] | The master document outlining the project's rationale, objectives, methodology, and ethical considerations. Serves as a common reference. |
| Informed Consent Forms [19] | Ensures that research participants, and potentially other stakeholders, are provided with the information they need to make an autonomous decision. |
| Data Management Plan [19] | Details how research data (both technical and qualitative) will be handled, stored, and analyzed, ensuring integrity and compliance. |
| Stakeholder Map [17] | A visual tool that identifies all individuals, groups, and organizations affected by the technology, used to guide engagement and analysis. |
| Interview & Focus Group Guides [17] | Semi-structured protocols used to collect qualitative data from various stakeholders, ensuring methodological standardization. |
Technical Support Center: FAQs & Troubleshooting Guides
This support center provides resources for researchers and scientists to navigate technical and ethical challenges in bioethics methodology research.
Frequently Asked Questions (FAQs)
Q1: What is the core function of an "Embedded Ethicist" in a research project? The Embedded Ethicist is not an external auditor but a integrated team member who facilitates ethical reflection throughout the research lifecycle. They move ethics beyond a compliance checklist ("research ethics") to become a substantive research strand ("ethical research") that scrutinizes the moral judgments, values, and potential conflicts inherent in the project's goals and methodologies [20].
Q2: How can I structure a troubleshooting process to be both efficient and thorough? Adopt a logical "repair funnel" approach. Start with the broadest potential causes and systematically narrow down to the root cause [21]. Key areas to isolate initially are:
- Method-related issues: Verify all parameters and procedures.
- Mechanical-related issues: Inspect instrumentation and hardware.
- Operation-related issues: Review human factors and execution.
Q3: Why is it critical to change only one variable at a time during experimental troubleshooting? Changing multiple variables simultaneously causes confusion and delays by making it impossible to determine which change resolved the issue. Always isolate variables and test them one at a time to correctly identify the root cause [22].
Q4: How can our team proactively identify ethical blind spots in our technology development? Utilize structured approaches like the Ethical, Legal, and Social Implications (ELSI) framework. This involves integrating ethical analysis right from the project's beginning, rather than as an after-the-fact evaluation. This can include ethics monitoring throughout the project cycle and formulating specific ethical research questions about the underlying values of the technology being developed [20].
Q5: What is the most important feature for a digital help center or knowledge base? Robust search functionality. A prominent, AI-powered search bar is essential for users to find answers quickly. An intuitive search reduces frustration and empowers users to resolve issues independently, which is a core goal of self-service [23] [24].
Troubleshooting Guides
Guide 1: Troubleshooting Experimental Protocol Failures
This guide outlines a systematic protocol for diagnosing failed experiments.
Required Materials:
| Research Reagent / Material | Function |
|---|---|
| Positive Control Samples | Verifies the protocol is functioning correctly by using a known positive outcome. |
| Negative Control Samples | Confirms the absence of false positives and validates the assay's specificity. |
| Fresh Reagent Batches | Isolates reagent degradation as a failure source. |
| Lab Notebook | Documents all steps, observations, and deviations for traceability. |
| Equipment Service Records | Provides historical performance data for instrumentation. |
Step-by-Step Methodology:
- Repeat the Experiment: Unless cost or time-prohibitive, repeat the experiment to rule out simple human error [22].
- Validate the Result: Critically assess if the unexpected result constitutes a failure. Revisit the scientific literature—could the result be biologically plausible? A dim signal, for instance, might indicate a protocol problem or low protein expression [22].
- Verify Controls: Ensure you have included appropriate positive and negative controls. A valid positive control helps determine if the problem lies with the protocol itself [22].
- Inspect Equipment & Reagents: Check for improper storage or expired reagents. Visually inspect solutions for cloudiness or precipitation. Confirm compatibility of all components (e.g., primary and secondary antibodies) [22].
- Change Variables Systematically: Generate a list of potential failure points (e.g., concentration, incubation time, temperature). Change only one variable at a time, starting with the easiest to test [22].
- Document Everything: Meticulously record every step, variable changed, and the corresponding outcome in your lab notebook. This creates a valuable reference for your team [21] [22].
The workflow below visualizes this structured troubleshooting process:
Guide 2: Resolving Instrument Performance Issues
Apply the "repair funnel" logic to narrow down instrument problems.
Step-by-Step Methodology:
- Gather Preliminary Information: Ask: What was the last action before the issue? How frequent is the problem? Check the instrument logbook and software error logs. Establish what "normal" looks like from historical data [21].
- Reproduce the Issue: Can you modify parameters to reliably reproduce the problem? Consistent reproduction is key to understanding the root cause [21].
- Isolate the System:
- Confirm Parameters: Meticulously verify that all method parameters match the intended protocol. Software updates or accidental saves can alter locked-down methods [21].
- Use "Half-Splitting": For modular instruments, isolate whether the problem lies in one major subsystem (e.g., the chromatography side vs. the mass spec side) to focus repair efforts [21].
- Perform the Repair:
- Document and Propose Prevention: Before concluding, fully document the issue and resolution. Include any service records. Propose adjustments to preventative maintenance schedules to avoid recurrence [21].
The following diagram illustrates the isolation and diagnosis process:
Key Performance Indicators for Research Support
Track the following metrics to measure the efficiency of your support structures, whether for technical or ethical guidance [23] [25].
| Support Metric | Definition | Target Goal |
|---|---|---|
| First Contact Resolution | Percentage of issues resolved in the first interaction. | > 70% |
| Average Resolution Time | Mean time taken to fully resolve a reported issue. | Minimize Trend |
| Self-Service Usage Rate | Percentage of users who find answers via knowledge base/FAQs without submitting a ticket. | Increase Trend |
| Customer Satisfaction (CSAT) | User satisfaction score with the support received. | > 90% |
| Ticket Deflection Rate | Percentage of potential tickets prevented by self-service resources. | Increase Trend |
Troubleshooting Guide: Common Interdisciplinary Methodology Challenges
This guide addresses frequent methodological problems encountered in interdisciplinary bioethics research, providing practical solutions to ensure rigor and credibility.
1. Problem: How to resolve conflicting conclusions from different disciplinary methods. A philosopher and a sociologist on the same team reach different normative conclusions from the same data.
- Solution: Implement a structured deliberation framework.
- Action: Facilitate a meeting where each researcher explicitly states their research question, methodological approach, key assumptions, and standards of evidence.
- Goal: To map the points of divergence and identify if the conflict is factual (disagreement on data), methodological (disagreement on how to interpret), or foundational (disagreement on core values) [1].
- Outcome: Foster mutual understanding and work towards an integrated conclusion that acknowledges the strengths and limitations of each perspective.
2. Problem: How to establish legitimacy and authority for interdisciplinary bioethics research. Research is criticized for lacking rigor because it doesn't conform to the standards of a single, traditional discipline [1].
- Solution: Proactively define and justify the research framework.
- Action: In publications and proposals, clearly articulate the chosen interdisciplinary model (multidisciplinary, interdisciplinary, transdisciplinary), the rationale for the selected methods, and the integrated standard of rigor being applied [1].
- Goal: To preempt criticism by demonstrating a self-aware and systematic approach to interdisciplinary work.
- Outcome: Enhance the research's credibility with funders, journals, and peers.
3. Problem: How to conduct a bias audit on a dataset or algorithm. A machine learning model, used to classify historical archival images, is found to perpetuate historical under-representation of certain social groups [26].
- Solution: Implement a multi-stage bias mitigation protocol.
- Action:
- Interdisciplinary Scrutiny: Assemble a team with domain experts (e.g., historians, ethicists) and technical experts (data scientists) to review the data and model outputs [26].
- Technical Interrogation: Use techniques like data augmentation (e.g., balancing dataset representation) and adversarial debiasing to reduce algorithmic unfairness [26].
- Continuous Monitoring: Establish a plan for ongoing auditing and refinement of the model after deployment [26].
- Goal: To identify and mitigate bias at multiple stages, from data selection and annotation to algorithmic design [26].
- Outcome: Develop a more fair, accurate, and ethically sound model.
- Action:
4. Problem: How to integrate diverse stakeholder values into ethical analysis. A clinical ethics consultation struggles to balance the perspectives of hospital administrators, clinicians, patients, and family members.
- Solution: Employ structured stakeholder analysis and ethnographic methods.
- Action:
- Stakeholder Mapping: Identify all relevant parties and their respective interests, influence, and ethical stakes.
- Ethnographic Engagement: Use methods like targeted interviews and direct observation to understand the lived experiences, values, and decision-making processes of these stakeholder groups.
- Goal: To ensure all relevant voices are identified and their values are genuinely understood, not just assumed.
- Outcome: A more robust, inclusive, and practical ethical analysis that is grounded in the real-world context.
- Action:
Frequently Asked Questions (FAQs)
Q1: What constitutes rigor in interdisciplinary bioethics research? Rigor is not about adhering to the standards of a single discipline but about the justified and transparent application of multiple methods to a research question. This involves clearly explaining the choice of methods, how they are integrated, and the criteria used to evaluate the validity of the resulting conclusions [1].
Q2: What are the core challenges of interdisciplinary work in bioethics? Key challenges include: the lack of clear, unified standards for answering bioethical questions; difficulties in the peer-review process due to disciplinary differences; undermined credibility and authority; challenges in practical clinical decision-making; and questions about the field's proper institutional setting [1].
Q3: Why is a bias audit important in bioethics research? Bias audits are crucial because bioethical decisions often rely on data and algorithms that can inherit and amplify existing societal prejudices. Mitigating bias ensures more inclusive, accurate, and ethically sound outcomes, which is a core objective of bioethics [26].
Experimental Protocols & Data Presentation
Table 1: Standards for Text Contrast in Accessible Visual Design This table outlines the minimum contrast ratios required by the Web Content Accessibility Guidelines (WCAG) for Level AAA, which helps ensure diagrams and text are readable for a wider audience, including those with low vision or color deficiencies [27] [28].
| Text Type | Definition | Minimum Contrast Ratio | Example |
|---|---|---|---|
| Large Text | Text that is at least 18.66px or 14pt in size, or bold text at least 14px or 10.5pt in size [29]. | 4.5:1 | A large, bolded heading. |
| Standard Text | Text that is smaller than 18.66px and not bold. | 7:1 | The main body text of a paragraph. |
Table 2: Key Research Reagent Solutions for Methodological Rigor
| Item | Function in the Research Process |
|---|---|
| Structured Deliberation Framework | A protocol for facilitating discussion between disciplines to map conflicts and work towards integrated conclusions [1]. |
| Stakeholder Mapping Tool | A systematic process for identifying all relevant parties, their interests, and their influence in an ethical issue. |
| Bias Mitigation Techniques | Technical methods (e.g., data augmentation, adversarial debiasing) used to identify and reduce unfair bias in datasets and algorithms [26]. |
| Ethnographic Interview Guide | A semi-structured set of questions used to understand the lived experiences and values of stakeholders in a real-world context. |
Methodological Workflow Diagrams
The following diagram illustrates the core process for conducting rigorous, interdisciplinary research in bioethics, integrating the tools discussed in this guide.
Interdisciplinary Research Workflow
This diagram details the specific steps involved in the critical "Bias Audit" phase of the research workflow.
Bias Audit Process
Frequently Asked Questions (FAQs)
FAQ 1: What are the core types of research collaboration, and how do they differ?
Research collaboration exists on a spectrum of integration [30]:
| Collaboration Type | Definition | Key Characteristics |
|---|---|---|
| Unidisciplinary | An investigator uses models and methods from a single discipline [30]. | Traditional approach; single perspective. |
| Multidisciplinary | Investigators from different disciplines work on a common problem, but from their own disciplinary perspectives [30]. | Additive approach; work is done in parallel. |
| Interdisciplinary | Investigators from different disciplines develop a shared mental model and blend methods to address a problem in a new way [30]. | Integrative approach; interdependent work. |
| Transdisciplinary | An interdisciplinary collaboration that evolves into a new, hybrid discipline (e.g., neuroscience, bioengineering) [30]. | Creates a new field of study. |
FAQ 2: What are the common phases of an interdisciplinary science team?
Interdisciplinary teams typically progress through four key phases, each with distinct tasks [30]:
- Development: Team assembly, problem definition, and establishing a shared mental model and team identity [30].
- Conceptualization: Defining specific research questions, design, communication practices, and team roles [30].
- Implementation: Executing and coordinating the research plan, managing conflict, and integrating findings [30].
- Translation: Applying the team's knowledge to address the real-world problem, which may include forming partnerships with industry, government, or the public [30].
FAQ 3: What methodological challenges does interdisciplinary bioethics research face?
Bioethics draws on diverse disciplines, each with its own standards of rigor, leading to several challenges [1]:
| Challenge Area | Specific Issue |
|---|---|
| Theoretical Standards | No clear, agreed-upon standards for assessing normative conclusions from different disciplinary perspectives [1]. |
| Peer Review | Difficulty in interpreting criteria like "originality" and "validity" across disciplines, and a lack of awareness of other disciplines' methods [1]. |
| Credibility & Authority | The absence of a unified standard can undermine the perceived legitimacy of the research and researchers [1]. |
| Practical Decision-Making | In clinical settings, effectively integrating diverse disciplinary perspectives for ethical decision-making remains difficult [1]. |
FAQ 4: How can our team effectively manage social interactions and knowledge integration?
Successful teamwork requires managing social transactions to foster knowledge integration [30]. Key practices include:
- Schedule Time for Team Development: Dedicate time to build a shared vision, common goals, and direct communication about the science [30].
- Discuss Credit Early: Have explicit conversations about how recognition and credit will be shared among collaborators [30].
- Build Trust and Psychological Safety: Cultivate an environment of trust, which enables team members to blend their competencies openly [30].
Troubleshooting Guides
Problem 1: Experiments or collaborative processes are yielding unexpected or inconsistent results.
This is a common issue in both wet-lab experiments and the "social experiments" of collaboration. A systematic approach to troubleshooting is essential [31] [32].
- Step 1: Define the Problem. Clearly articulate what was expected versus what occurred. For collaborative issues, identify the specific friction point (e.g., "ethicists and scientists disagree on risk assessment criteria") [32].
- Step 2: Analyze the Design. Scrutinize the experimental or team protocol [32]. Key elements to assess are shown in the table below:
| Element to Assess | Key Questions |
|---|---|
| Controls | Were appropriate controls in place? In collaboration, are there agreed-upon guidelines or moderators? [32] |
| Sample & Representation | Was the sample size sufficient? Does the team include all necessary disciplinary and stakeholder perspectives? [32] |
| Methodology & Communication | Was the methodology valid? Are team communication structures and practices effective? [30] |
| "Randomization" & Bias | Were subjects assigned randomly to minimize bias? Have team roles been assigned fairly to avoid disciplinary dominance? [32] |
- Step 3: Identify External Variables. Consider factors outside the immediate design that could be causing the failure, such as environmental conditions, timing, or unaccounted-for stakeholder interests [32].
- Step 4: Implement Changes. Modify the design based on your analysis. This could involve generating detailed Standard Operating Procedures (SOPs) for experiments or re-establishing team communication practices [32].
- Step 5: Test the Revised Design. Retest the experiment or implement the new collaborative process to validate that the changes have addressed the issues [32].
Problem 2: The team is struggling to integrate knowledge from different disciplines.
This often stems from a lack of a shared mental model [30].
- Action: Facilitate a dedicated session where each discipline explains their core models, methods, and standards of "rigor" using accessible language [1]. Use a facilitator to help the group develop a shared framework for the specific project, acknowledging that a single standard of rigor may need to be negotiated [1].
Problem 3: Disagreements arise over post-trial responsibilities in high-risk clinical research.
This is a complex, real-world bioethical challenge where interdisciplinary input is critical [33].
- Action: Proactively assemble a broad range of stakeholders, including lab researchers, bioethicists, clinicians, participants, insurance experts, and policy makers, to discuss post-trial support before the trial begins [33]. Focus on defining the specific attributes of the irreversible treatment and the corresponding obligations, moving beyond theoretical debates to practical planning [33].
The Scientist's Toolkit: Key Reagents for Interdisciplinary Collaboration
| Tool / Concept | Function / Purpose |
|---|---|
| Shared Mental Model | A unified understanding of the research problem and approach that bridges disciplinary jargon and perspectives, enabling true integration [30]. |
| Field Guide for Collaboration | A living document that outlines the team's shared vision, goals, communication plans, and agreements on credit and authorship [30]. |
| Stakeholder Mapping | A process to identify all relevant parties (scientists, ethicists, community members, policy makers) who are impacted by or can impact the research [30]. |
| Participatory Team Science | An approach that formally engages public stakeholders (community members, patients) as active collaborators on the research team, providing essential lived experience and context [30]. |
Technical Support Center: Embedded Ethics FAQs & Troubleshooting
This guide provides practical solutions for researchers, scientists, and drug development professionals implementing embedded ethics in AI-driven healthcare projects.
Frequently Asked Questions
Q1: What is Embedded Ethics and how does it differ from traditional ethics review processes?
A1: Embedded Ethics is an approach that integrates ethicists and social scientists directly into technology development teams to address ethical issues iteratively throughout the entire development lifecycle, rather than through a single-point ethics review [17] [34]. Unlike traditional ethics reviews that often occur at specific milestones, embedded ethics involves continuous collaboration where ethicists participate in regular team meetings, develop deep understanding of technical details, and work alongside developers from project planning through implementation [17]. This approach aims to anticipate ethical concerns proactively rather than addressing them after development is complete.
Q2: What are the most effective methods for identifying ethical issues in early-stage AI diagnostic development?
A2: Research indicates several effective methods for early-stage ethical issue identification [17]:
- Conducting stakeholder analyses to map all affected parties
- Performing bias analyses on training data and algorithms
- Implementing ethnographic approaches to understand clinical contexts
- Facilitating interdisciplinary workshops with diverse perspectives
- Conducting literature reviews of similar ethical challenges
These methods help teams anticipate issues related to algorithmic fairness, data provenance, explainability, and clinical deployment before they become embedded in the technology [17] [35].
Q3: How can we address interdisciplinary communication barriers between ethicists and AI developers?
A3: Successful teams implement several strategies to bridge communication gaps [17] [34]:
- Establish regular cross-disciplinary meetings with structured agendas
- Create shared glossaries of technical and ethical terms
- Implement peer-to-peer interviews to build mutual understanding
- Develop prototyping sessions where ethical concerns can be visualized technically
- Facilitate joint problem-solving on concrete implementation challenges
These approaches help transform cultural differences between fields from obstacles into productive sources of innovation [34].
Q4: What practical steps can we take to mitigate algorithmic bias in genomic risk prediction tools?
A4: For genomic AI applications, particularly concerning in child psychiatry [36]:
- Diversify training data by including populations beyond European ancestry
- Validate models across diverse demographic groups before deployment
- Implement continuous bias monitoring during clinical use
- Contextualize predictions with psychosocial and environmental factors
- Establish multidisciplinary review boards to interpret results
These steps are particularly crucial for polygenic risk scores, which have demonstrated reduced accuracy for underrepresented populations [36].
Troubleshooting Common Implementation Challenges
Problem: Resistance from technical team members who view ethics as a development barrier
| Symptoms | Possible Causes | Solution Approaches |
|---|---|---|
| - Missed ethics meetings- Superficial engagement with ethical concerns- Perception that ethics slows innovation | - Unclear value proposition- Previous negative experiences with ethics processes- Lack of understanding of ethical risk | - Demonstrate concrete value through case studies- Co-develop ethical specifications with technical team- Show how ethics prevents future rework- Include ethics in success metrics |
Problem: Ineffective integration of ethical analysis into technical development cycles
| Symptoms | Possible Causes | Solution Approaches |
|---|---|---|
| - Ethical feedback comes too late for implementation- Recommendations are too abstract for technical application- Ethics perceived as separate from core development | - Lack of shared processes- Insufficient technical understanding by ethicists- Poor timing of ethical review | - Embed ethicists in agile sprints- Create "ethics tickets" in development backlog- Develop concrete implementation patterns for ethical principles- Establish joint design sessions |
Problem: Difficulty managing ethical uncertainties in rapidly evolving AI technologies
| Symptoms | Possible Causes | Solution Approaches |
|---|---|---|
| - Paralysis in decision-making- Inconsistent handling of emerging ethical questions- Lack of clarity on risk thresholds | - Absence of decision frameworks- Unclear accountability for ethical risk decisions- Rapidly changing technical capabilities | - Develop ethics risk assessment matrix- Establish clear escalation paths- Create living ethics documentation- Implement regular ethics review checkpoints |
Experimental Protocols for Embedded Ethics
Protocol 1: Embedded Ethics Integration for AI Diagnostic Development
Purpose: To systematically integrate ethical considerations throughout the development of AI-driven diagnostic tools [37] [34].
Materials:
- Interdisciplinary team (ethicists, AI developers, clinicians, legal experts)
- Ethical-legal assessment framework
- Documentation system for ethical decisions
- Stakeholder engagement plan
Methodology:
- Project Scoping Phase
Data Collection & Preparation Phase
Algorithm Development Phase
Validation & Testing Phase
Implementation & Monitoring Phase
Troubleshooting:
- If team collaboration is ineffective: Implement structured communication protocols and peer interviews [17]
- If ethical issues emerge late: Increase frequency of ethics reviews and integrate into development sprints [34]
- If cultural resistance persists: Demonstrate value through case studies of ethical failures in similar projects [37]
Protocol 2: Ethical Integration in Genomic AI Research
Purpose: To address ethical challenges in AI-driven genomic research for psychiatric applications [36].
Materials:
- Genomic and clinical datasets
- AI/ML infrastructure
- Ethical oversight committee
- Patient engagement resources
Methodology:
- Research Design Phase
Data Processing Phase
Model Development Phase
Clinical Translation Phase
Troubleshooting:
- If models show demographic bias: Augment training data from underrepresented groups and apply bias mitigation techniques [36]
- If clinical misinterpretation occurs: Develop improved decision support and clinician education [36]
- If privacy concerns arise: Consider distributed learning approaches that minimize data sharing [35]
Embedded Ethics Methods Comparison
Table: Embedded Ethics Methods and Applications
| Method | Primary Use Case | Implementation Effort | Key Outputs |
|---|---|---|---|
| Stakeholder Analysis [17] | Early project scoping | Medium | Map of affected parties, key concerns, value conflicts |
| Bias Assessment [17] | Data preparation and algorithm development | High | Identification of discriminatory patterns, mitigation strategies |
| Ethnographic Approaches [17] | Understanding clinical context and workflows | High | Deep contextual understanding, unidentified use cases |
| Interdisciplinary Workshops [17] | Collaborative problem-solving | Medium | Shared understanding, co-designed solutions |
| Iterative Ethical Review [34] | Ongoing development process | High | Continuous ethical refinement, early issue identification |
Table: Ethical Challenges in AI-Driven Genomic Medicine
| Ethical Challenge | Risks | Mitigation Strategies |
|---|---|---|
| Equity and Access [36] | Perpetuation of health disparities, limited applicability to diverse populations | Diversify genomic datasets, validate across populations, ensure equitable access |
| Informed Consent [36] | Inadequate understanding of complex AI-genomic implications, privacy risks | Dynamic consent models, clear communication, ongoing consent processes |
| Privacy and Data Protection [35] | Re-identification risk, unauthorized data use, loss of control | Distributed learning approaches, strong governance, technical safeguards |
| Determinism and Stigmatization [36] | Genetic essentialism, self-fulfilling prophecies, discrimination | Contextualize genetic risk, avoid labels, emphasize modifiable factors |
Research Reagent Solutions: Embedded Ethics Toolkit
Table: Essential Methodological Tools for Embedded Ethics Research
| Tool/Resource | Function | Application Context |
|---|---|---|
| Interdisciplinary Collaboration Framework [17] [34] | Establishes protocols for cross-disciplinary teamwork | Facilitating effective communication between ethicists, developers, clinicians |
| Stakeholder Analysis Template [17] | Systematically identifies affected parties and concerns | Early project scoping to anticipate ethical issues |
| Bias Assessment Protocol [17] | Detects discriminatory patterns in data and algorithms | AI development phases to ensure fairness and equity |
| Iterative Review Process [34] | Enables continuous ethical refinement throughout development | Ongoing project oversight and course correction |
| Distributed Machine Learning Methods [35] | Enables analysis without centralizing sensitive data | Genomic research and healthcare applications with privacy concerns |
Workflow Visualization
Embedded Ethics AI Development Integration
Genomic AI Ethics Workflow
Distributed ML Privacy Approach
Navigating Roadblocks: Solving Common Pitfalls in Interdisciplinary Ethics
Identifying and Mitigating Bias in AI and Data Sets
FAQs on AI Bias Fundamentals
What is AI bias and how does it occur? AI bias refers to systematic and unfair discrimination in AI system outputs, resulting from biased training data, algorithmic design, or human assumptions [38]. Bias can enter the AI pipeline at multiple stages: during data collection if data isn't representative, during data labeling through human annotator biases, during model training if architectures favor majority groups, and during deployment when systems encounter real-world scenarios not reflected in training data [39].
How can we distinguish between real-world patterns and harmful bias in AI outcomes? Not all disparities in AI outcomes constitute bias; some may accurately reflect real-world distributions [40]. For example, an AI predicting higher diabetes risk in a specific demographic group based on genuine health trends is not necessarily biased—it may reflect actual population health patterns. The key is conducting thorough analysis to determine if outcome differences stem from technical bias or underlying societal realities, which requires examining data context and broader societal factors [40].
Why is bias in healthcare AI particularly concerning? In healthcare, biased AI can worsen existing health disparities [41]. For instance, an algorithm affecting over 200 million patients in the U.S. significantly favored white patients over Black patients when predicting healthcare needs because it used healthcare spending as a proxy for need, ignoring that Black patients historically have less access to care and spend less [38]. This reduced Black patients identified for extra care by more than 50% despite equal or greater health needs [38].
Troubleshooting Guides
Problem: Suspected Demographic Bias in Model Performance
Symptoms: Model performs significantly worse for specific demographic groups (e.g., higher error rates for darker-skinned individuals in facial recognition) [39] [38].
Diagnosis Protocol:
- Disaggregate Evaluation: Test model performance across different demographic groups using comprehensive benchmarking datasets like Sony's FHIBE (Fair Human-Centric Image Benchmark), which includes consensually-sourced images from subjects in over 81 countries with extensive annotations [42].
- Identify Bias Type: Determine if bias stems from:
Mitigation Strategies:
- Pre-processing: Balance datasets through re-sampling or re-weighting [43] [44]
- In-processing: Implement fairness constraints during training [43] [44]
- Post-processing: Adjust decision thresholds for different groups to ensure equitable outcomes [43]
AI Bias Mitigation Workflow
Problem: AI System Reinforcing Gender Stereotypes
Symptoms: AI associates specific professions with genders (e.g., "nurse" with female pronouns, "engineer" with male pronouns) or generates stereotypical imagery [39] [45].
Case Study: Amazon's recruiting tool was scrapped after discovering it penalized resumes containing the word "women's" (like "women's chess club") and graduates of all-women's colleges because it was trained on historical hiring data that favored men in a male-dominated industry [43] [38].
Mitigation Approach:
- Audit Training Data: Identify and address representation imbalances and stereotypical associations [39]
- Implement Balanced Sampling: Ensure equal representation across genders in training data for profession-related tasks [39]
- Use De-biasing Techniques: Apply adversarial training to remove gender correlations from embeddings [43]
- Continuous Monitoring: Regularly test for stereotypical outputs across different prompt types [39]
Problem: Racial Disparities in Healthcare Algorithms
Symptoms: Algorithm shows significantly different accuracy or recommendation patterns across racial groups [41] [38].
Case Study: A widely used healthcare risk-prediction algorithm demonstrated racial bias by relying on healthcare costs as a proxy for medical needs. Since less money is historically spent on Black patients with the same level of need, the algorithm mistakenly assigned them lower risk scores, disproportionately excluding them from care programs [45] [38].
Mitigation Framework:
- Identify Flawed Proxies: Audit features for potential biases (e.g., using cost rather than direct health indicators) [41]
- Incorporate Clinical Validation: Ensure medical experts from diverse backgrounds validate model recommendations [46]
- Implement Fairness Metrics: Use statistical measures like demographic parity difference to quantify disparities [44]
Healthcare Algorithm Bias Audit
Quantitative Analysis of AI Bias
Table 1: Performance Disparities in Facial Recognition Systems [38]
| Demographic Group | Error Rate (%) | Notes |
|---|---|---|
| Light-skinned males | 0.8-1.0 | Highest accuracy across all systems |
| Dark-skinned females | 34.7 | Up to 35% misclassification rate in some systems |
| Overall white males | ≤1.0 | Consistently high performance |
| Overall black women | Up to 35.0 | Significant performance gaps |
Table 2: AI Bias Prevalence Across Domains [47]
| Domain | Bias Incidence | Key Findings |
|---|---|---|
| Neuroimaging AI models | 83.1% high risk of bias | 555 models assessed for psychiatric disorders |
| Marketing AI tools | 34% produce biased information | Second most common challenge after inaccurate data |
| AI recruitment | 30% more likely to filter candidates over 40 | Compared to younger candidates with identical qualifications |
| ChatGPT political bias | 72.4% agreement with green views | Compared to 55% for conservative statements |
Experimental Protocols for Bias Detection
Protocol 1: Intersectional Bias Assessment in Human-Centric Computer Vision
Objective: Systematically evaluate model performance across intersecting demographic attributes [42].
Materials:
- FHIBE dataset or similar diverse benchmarking data [42]
- Model inference infrastructure
- Statistical analysis software (Python/R)
Methodology:
- Stratified Evaluation: Test model across demographic intersections (gender × skin tone × age)
- Performance Disaggregation: Calculate precision, recall, and F1 scores for each subgroup
- Bias Magnitude Quantification: Compute disparity ratios between best-performing and worst-performing groups
- Root Cause Analysis: Identify specific failure patterns (e.g., hairstyle variability affecting gender classification) [42]
Protocol 2: Healthcare Algorithm Equity Audit
Objective: Detect and quantify disparities in clinical AI systems [41] [46].
Materials:
- Diverse patient dataset with comprehensive demographic information
- Clinical outcome validation data
- Fairness assessment toolkit (Fairlearn, Aequitas)
Methodology:
- Outcome Disparity Measurement: Compare false positive/negative rates across racial, gender, and socioeconomic groups
- Clinical Impact Assessment: Evaluate whether accuracy differences translate to meaningful care disparities
- Proxy Variable Identification: Test if input features serve as biased proxies for protected attributes
- Mitigation Intervention: Apply appropriate pre-processing, in-processing, or post-processing techniques based on audit findings [43]
Research Reagent Solutions
Table 3: Essential Tools for AI Bias Research
| Tool Name | Type | Function | Reference |
|---|---|---|---|
| FHIBE Dataset | Benchmark Data | Consensual, globally diverse images for fairness evaluation | [42] |
| Google's What-If Tool | Analysis Tool | Visual, interactive model performance analysis without coding | [38] |
| Fairlearn | Python Library | Implements fairness metrics and mitigation algorithms | [44] |
| Demographic Parity | Metric | Measures whether predictions are independent of protected attributes | [44] |
| Equalized Odds | Metric | Ensures similar true positive and false positive rates across groups | [43] |
| AI Fairness 360 | Comprehensive Toolkit | Includes multiple metrics and algorithms for bias detection and mitigation | - |
| ConversationBufferMemory | Technical Implementation | Manages conversation history in LangChain for consistent context | [44] |
| ThresholdOptimizer | Algorithm | Adjusts decision thresholds for different groups to achieve fairness | [44] |
Troubleshooting Guides and FAQs
FAQ: Core Concepts
What is the difference between AI transparency and explainability?
Transparency and explainability are related but distinct concepts crucial for building trustworthy AI. Transparency focuses on providing general information about the AI system's design, architecture, data sources, and governance structure to a broad audience. It answers the question: "How does this AI system work in general?" In contrast, explainability seeks to clarify the reasons behind specific, individual decisions or outputs. It answers the question: "Why did the AI make this particular decision?" [48].
Why are transparency and explainability particularly important in bioethics research?
Bioethics is an inherently interdisciplinary field, drawing on medicine, law, philosophy, sociology, and more [1] [49]. Each discipline has its own standards of rigor and methods for validating knowledge [1]. When AI systems are used in bioethical decision-making, a lack of transparency and explainability can exacerbate existing interdisciplinary challenges. It can undermine the credibility of the research, create confusion in peer review, and hinder effective collaboration and practical decision-making in clinical settings [1]. Transparent and explainable AI helps establish a common framework for evaluating AI-driven insights across different disciplinary perspectives.
How can I tell if my AI model's explanations are understandable to non-technical stakeholders?
A key element of explainability is Human Comprehensibility. The explanation provided by the AI must be in a format that is easily understood by humans, including non-experts like legal, compliance, and clinical professionals. This requires translating complex AI operations into simple, clear language, avoiding technical jargon like code or complex mathematical notations [48]. Test this by presenting the explanation to representatives from the various disciplines involved in your research and assessing their ability to understand the reasoning.
Troubleshooting Guide: Common Issues and Solutions
| Problem | Possible Cause | Solution |
|---|---|---|
| Stakeholders distrust AI outputs. | Lack of system transparency; perceived as a "black box." | Implement transparency by documenting and sharing information on the AI's design, data sources, and accountability structure [48]. |
| Difficulty understanding why a specific decision was made. | Poor model explainability; complex internal mechanics. | Utilize explainability techniques (e.g., LIME, SHAP) to generate reason codes or highlight key factors for each decision [48]. |
| AI explanations are not actionable for clinicians or ethicists. | Explanations are too technical and not human-comprehensible. | Translate the AI's reasoning into natural language and ethical justifications that align with interdisciplinary frameworks [48]. |
| Peer review of AI-assisted research is challenging. | Lack of agreed-upon standards of rigor for AI in bioethics [1]. | Proactively document and disclose the AI methodologies used, fostering a common understanding across disciplinary boundaries [1]. |
Experimental Protocols for Transparency and Explainability
Protocol 1: Implementing a Transparency Framework
Objective: To systematically document and disclose key elements of an AI system used in bioethics research.
Methodology:
- Design and Development Disclosure: Document the AI's architecture (e.g., GAN, CNN), the algorithms used, and the training process [48].
- Data and Input Transparency: Catalog the sources and types of data used for training and operation. Disclose any data preprocessing or transformation steps applied [48].
- Governance and Accountability: Clearly define and publish the roles and responsibilities of individuals or teams accountable for the AI system's development, deployment, and ongoing governance [48].
Protocol 2: Generating Human-Comprehensible Explanations
Objective: To create understandable justifications for individual AI decisions tailored to an interdisciplinary audience.
Methodology:
- Decision Justification: For a specific output, detail the primary factors and data points that most influenced the decision. This is akin to "showing your work" in a logical proof [48].
- Model Interpretability: Employ techniques that make the model's mechanics accessible. This could involve using simpler, interpretable models where possible or post-hoc explanation tools for complex models [48].
- Output Translation: Render the explanation in a clear, concise format using natural language. Avoid technical code or hexadecimal outputs, ensuring it is readable for all stakeholders, including those from law, philosophy, and clinical practice [48].
Visualizing the Strategy
Diagram: Framework for Trustworthy AI in Bioethics
Diagram: Workflow for an Explainable AI Decision
The Scientist's Toolkit: Research Reagent Solutions
| Item / Solution | Function in AI Transparency & Explainability |
|---|---|
| Model Cards | A transparency tool that provides a short document detailing the performance characteristics of a trained AI model, intended for a broad audience [48]. |
| SHAP (SHapley Additive exPlanations) | A game theory-based method used in explainability to quantify the contribution of each input feature to a specific model prediction. |
| LIME (Local Interpretable Model-agnostic Explanations) | An explainability technique that approximates a complex "black box" model with a simpler, interpretable model to explain individual predictions. |
| Algorithmic Audits | Independent reviews of AI systems to assess their fairness, accountability, and adherence to transparency and ethical guidelines. |
| Documentation & Governance Frameworks | Structured protocols for documenting data provenance, model design, and accountability structures, fulfilling transparency requirements [48]. |
Balancing Data Needs with Patient Privacy and Informed Consent in the Age of Big Data
Technical Support Center: Troubleshooting Data Ethics
This support center provides practical guidance for researchers, scientists, and drug development professionals navigating the interdisciplinary challenges of bioethics in the era of big data and AI.
Frequently Asked Questions (FAQs)
What is the primary purpose of bioethics pipeline troubleshooting? The primary purpose is to identify and resolve errors or inefficiencies in data workflows, ensuring accurate and reliable data analysis while maintaining ethical compliance [50].
How can I ensure the accuracy of a bioinformatics pipeline while preserving patient privacy? Validate results with known datasets, cross-check outputs using alternative methods, and maintain detailed documentation. For privacy, implement data governance frameworks that separate identifying information from clinical data [50].
What are the most common ethical challenges in health-related big data projects? Common challenges include maintaining meaningful informed consent with complex AI systems, preventing discrimination in data uses, handling data breaches appropriately, and ensuring equitable benefits from data research [51].
How do I handle informed consent for evolving AI models that use patient data? Even if a patient consents to sharing their data for a specific purpose, AI models usually incorporate data into all future predictions, evolving with it and blurring the limits of the use cases to which the patient agreed. Consider implementing tiered consent processes that allow for periodic re-consent for higher-risk applications [52].
What industries benefit the most from bioinformatics pipeline troubleshooting with ethical safeguards? Healthcare, environmental studies, agriculture, and biotechnology are among the industries that rely heavily on bioinformatics pipelines and benefit from robust ethical frameworks [50].
Troubleshooting Guides
Problem: Obtaining Meaningful Informed Consent for AI-Driven Research
Symptoms
- Patients cannot comprehend how their data will be used in complex AI systems
- Consent forms become lengthy, technical documents that function as checkboxes rather than genuine informed consent
- Uncertainty about how to handle consent for AI models that continuously learn and evolve beyond their initial training data
Diagnosis and Resolution
| Step | Action | Ethical Principle | Tools/Resources |
|---|---|---|---|
| 1 | Identify the Specific AI Use Case | Transparency | Document the AI's purpose, data requirements, and potential impacts [52] |
| 2 | Implement Tiered Risk Assessment | Proportionality | Classify AI applications by risk level using frameworks like the EU AI Act [52] |
| 3 | Develop Layered Consent Materials | Comprehension | Create simplified summaries with visual aids alongside detailed technical documents |
| 4 | Establish Ongoing Consent Mechanisms | Ongoing Autonomy | Implement processes for re-consent when AI applications significantly evolve [52] |
| 5 | Validate Understanding | Genuine Agreement | Use teach-back methods or understanding checks with participants |
Problem: Managing Privacy Risks in Large-Scale Health Data Analysis
Symptoms
- Difficulty anonymizing complex datasets while maintaining research utility
- Concerns about re-identification risks in genomic and clinical data
- Uncertainty about legal compliance across different jurisdictions (e.g., HIPAA, GDPR)
Diagnosis and Resolution
| Step | Action | Ethical Principle | Technical Approach |
|---|---|---|---|
| 1 | Conduct Privacy Impact Assessment | Prevention | Map data flows and identify potential privacy vulnerabilities [51] |
| 2 | Implement Differential Privacy | Data Minimization | Add calibrated noise to queries to prevent individual identification |
| 3 | Use Federated Learning | Local Processing | Train AI models across decentralized devices without sharing raw data |
| 4 | Establish Data Governance | Accountability | Create clear protocols for data access, use, and security breaches [51] |
| 5 | Monitor for Discrimination | Justice | Regularly audit algorithms for biased outcomes across demographic groups [51] |
Research Reagent Solutions: Ethical Framework Components
| Component | Function | Application Context |
|---|---|---|
| Contextual Integrity Framework | Evaluates appropriate information flow based on specific contexts and relationships [51] | Assessing whether data use violates contextual norms |
| Differential Privacy Tools | Provides mathematical privacy guarantees while allowing aggregate data analysis | Sharing research data with external collaborators |
| Federated Learning Platforms | Enables model training across decentralized data sources without data movement | Multi-institutional research collaborations |
| Tiered Consent Templates | Adapts consent complexity based on project risk level | Studies involving AI/ML components with uncertain future uses |
| Algorithmic Auditing Tools | Detects discriminatory patterns in AI decision-making | Validating fairness in predictive healthcare models |
Experimental Protocol: Ethical Data Governance Implementation
Purpose To establish a reproducible methodology for implementing ethical data governance in big health data research projects.
Materials
- Data classification framework
- Risk assessment matrix
- Privacy-preserving technologies (encryption, anonymization tools)
- Documentation system for consent tracking
- Ethical oversight committee
Procedure
Data Mapping and Classification
- Catalog all data elements collected and generated
- Classify by sensitivity level and regulatory requirements
- Document data flows and access points
Risk-Benefit Analysis
- Identify potential benefits to individuals, communities, and society
- Assess risks of privacy violations, discrimination, and other harms
- Implement proportional safeguards based on risk level
Consent Architecture Design
- Develop multi-layered consent processes matching data use complexity
- Establish mechanisms for ongoing communication and re-consent
- Implement withdrawal procedures that respect participant autonomy
Technical Safeguards Implementation
- Deploy appropriate privacy-enhancing technologies
- Establish access controls and audit trails
- Create data breach response protocols
Continuous Monitoring and Evaluation
- Regularly assess ethical compliance and emerging risks
- Solicit participant feedback on consent processes
- Adapt frameworks based on technological and regulatory changes
Workflow Visualization
Ethical Data Governance Workflow
Tiered Consent Framework
Regulatory Compliance Table
| Regulation/Jurisdiction | Key Requirements | Applicability to Health AI | Compliance Challenges |
|---|---|---|---|
| HIPAA (U.S.) | Limits use/disclosure of protected health information; requires safeguards [51] | Applies to healthcare providers, plans, clearinghouses | Limited coverage for health data outside traditional healthcare settings [51] |
| GDPR (EU) | Requires purpose limitation, data minimization; special category for health data [51] | Broad application to all health data processing | Tension with evolving AI systems that blur use case boundaries [52] |
| EU AI Act | Risk-based approach; quality and safety requirements for high-risk AI systems [52] | Specific requirements for medical AI devices | Focuses on product safety rather than fundamental rights protection [52] |
| State Laws (U.S.) | Varied protections (e.g., CCPA); often broader than HIPAA | Patchwork of requirements across states | Compliance complexity for multi-state research initiatives |
Troubleshooting Common Experimental Scenarios
Scenario: Unexpected Algorithmic Bias Detection
Problem During validation of a predictive model for patient outcomes, you discover the algorithm performs significantly worse for minority demographic groups.
Troubleshooting Steps
Repeat the Analysis
- Confirm the bias pattern persists across multiple data splits
- Verify data quality and completeness across demographic groups
Investigate Root Causes
- Examine training data for representation imbalances
- Analyze feature importance across different populations
- Check for proxy variables that correlate with protected attributes
Implement Mitigation Strategies
- Apply algorithmic fairness techniques (reweighting, adversarial debiasing)
- Collect more representative data where feasible
- Adjust model decision thresholds by demographic group if justified
Document and Disclose
- Record the bias discovery and mitigation approach
- Include limitations in model documentation
- Establish ongoing monitoring for performance disparities
Scenario: Data Breach Incident Response
Problem You discover that a research dataset containing identifiable health information has been potentially accessed by unauthorized parties.
Troubleshooting Steps
Immediate Containment
- Isolate affected systems and preserve evidence
- Assess scope and nature of breached data
- Activate incident response team
Regulatory and Ethical Obligations
- Notify appropriate authorities per legal requirements (varies by jurisdiction)
- Inform affected individuals where necessary
- Consult with institutional review board and privacy officer
Remediation and Prevention
- Identify and address vulnerability that enabled breach
- Enhance security controls based on lessons learned
- Review and update data governance policies
Transparency and Accountability
- Document the incident and response thoroughly
- Communicate appropriately with stakeholders
- Implement additional safeguards to prevent recurrence
This technical support center provides resources for researchers and drug development professionals to navigate accountability and liability challenges when using AI systems in interdisciplinary bioethics research.
Diagnostic Troubleshooting Guide
Use the following questions to identify potential accountability gaps in your AI-driven research projects.
| Diagnostic Question | Likely Accountability Gap | Recommended Next Steps |
|---|---|---|
| Can you trace and explain the AI's decision for a specific output? | Explainability Gap [53] | Check system documentation for explainable AI (XAI) features; proceed to Guide 1. |
| Do contracts with the AI vendor waive their liability for system errors or bias? | Contractual Liability Gap [54] | Review vendor agreements for liability caps and warranties; proceed to Guide 2. |
| Is there a clear, documented chain of human oversight for the AI's decisions? | Human Oversight Gap [55] [56] | Review operational protocols for Human-in-the-Loop (HITL) checkpoints; proceed to Guide 3. |
| If the AI causes harm (e.g., biased data), can you prove your team used it responsibly? | Governance Gap [54] [56] | Audit internal governance protocols for documentation and bias testing. |
Step-by-Step Troubleshooting Guides
Guide 1: Addressing the AI "Black Box" – Explainability Gap
Problem: An AI tool used to analyze patient data for a research study produces a concerning recommendation, but the reasoning is opaque, making it impossible to explain or defend in a publication or ethics review.
Solution: Implement a multi-layered explainability protocol.
- Quick Fix (5 minutes): Check the AI system's interface for built-in explainability features. Look for a "Why?" button, confidence scores, or feature importance charts that highlight the primary data factors influencing the decision [55].
- Standard Resolution (15 minutes): If the quick fix is insufficient, apply a post-hoc explanation technique. Use a model-agnostic tool like LIME (Local Interpretable Model-agnostic Explanations) or SHAP (Shapley Additive exPlanations) to generate a local approximation of the model's behavior for that specific decision [55]. Document the tool used and the explanation generated.
- Root Cause Fix (Ongoing): For critical research applications, proactively choose AI models that are inherently interpretable (e.g., decision trees, rule-based systems) where possible [55]. During vendor selection, prioritize those who provide transparency into their model's architecture and data sources and offer robust explanation capabilities [53].
Guide 2: Addressing Unfair Contracts – Contractual Liability Gap
Problem: Your team wants to use a powerful AI tool for drug discovery, but the vendor's contract limits their liability to the value of the subscription and disclaims all warranties for compliance with ethical guidelines.
Solution: Aggressive and informed contract negotiation.
- Quick Fix (Immediate): Before signing, conduct a specific gap analysis of the vendor's terms. Highlight clauses related to: liability caps, compliance warranties (especially for ethics and anti-discrimination), indemnification for third-party claims, and audit rights [54].
- Standard Resolution (Negotiation): Negotiate for mutual liability caps rather than one-sided vendor protection. Demand explicit warranties that the tool complies with relevant regulations (e.g., HIPAA, GDPR). Crucially, seek the right to audit the algorithm for bias and fairness upon a trigger event [54].
- Root Cause Fix (Strategy): Integrate legal counsel into the technical procurement process for AI systems. Develop a standardized checklist of minimum acceptable contract terms for AI vendors to ensure accountability is baked in from the start [54].
Guide 3: Addressing Automated Decisions – Human Oversight Gap
Problem: An AI system used to screen biomedical literature for research ethics approval begins automatically rejecting studies based on a poorly justified criterion, with no human reviewer catching the error.
Solution: Design and enforce a formal Human-in-the-Loop (HITL) protocol.
- Quick Fix (Immediate): Immediately halt any fully automated decision-making processes for critical research functions. Redirect all AI-generated outputs to a designated human reviewer for approval before any action is taken [55].
- Standard Resolution (15 minutes): Define and document clear HITL thresholds. This specifies when human review is required (e.g., for all negative outcomes, low-confidence scores, or decisions affecting human subjects). Implement this as a mandatory step in your workflow [55] [56].
- Root Cause Fix (Ongoing): Integrate HITL requirements into the core design of your research workflows using MLOps practices. This ensures version control, creates audit trails of all human overrides, and facilitates continuous monitoring for anomalous AI behavior [56].
Frequently Asked Questions (FAQs)
Q1: In an interdisciplinary research setting, who is ultimately accountable for a harmful decision made by an AI tool—the biologist using it, the computer scientist who built it, or the ethicist on the team? A: Ultimately, the organization and the principal investigator deploying the AI are accountable. The Mobley v. Workday precedent suggests that entities using AI for delegated functions (like screening) are acting as agents and share liability [54]. Accountability must be clearly assigned through governance structures that define roles for all stakeholders involved in the AI's lifecycle [55] [56].
Q2: Our AI model is a proprietary "black box" from a vendor. How can we fulfill ethical obligations for explainability in our published research? A: You must employ external explainability techniques (like LIME or SHAP) and rigorously document the process [55]. Furthermore, this limitation should be explicitly disclosed in your research methods as a potential source of bias or error. Your vendor due diligence should also prioritize partners who provide greater transparency [53].
Q3: What is the minimum standard for human oversight of an AI system in a clinical research context? A: There is no single universal standard, but best practices dictate that human oversight must be "meaningful and effective." This means the human reviewer must have the authority, competence, and contextual information to override the AI's decision. They should not be a mere rubber stamp [55]. Regulatory frameworks like the EU AI Act mandate human oversight for high-risk AI systems, which would include many clinical applications [57].
Q4: What are the key elements we need to document to prove we are using an AI system responsibly? A: Maintain a comprehensive audit trail that includes:
- Model Details: Version, source, and intended use case.
- Data Provenance: Records of training data sources and pre-processing steps.
- Testing Results: Documentation of bias audits, performance metrics, and validation studies.
- Operational Logs: Records of human reviews, overrides, and incident reports [54] [56].
- Governance Records: Meeting minutes from ethics reviews and protocol updates.
The Scientist's Toolkit: AI Accountability & Governance
| Tool / Resource | Function in Addressing AI Accountability |
|---|---|
| Model Audit Framework | A structured protocol for conducting internal or third-party audits of AI systems to assess fairness, accuracy, and explainability. |
| Bias Assessment Tool | Software (e.g., AI Fairness 360) used to proactively identify and mitigate unwanted biases in training data and model outputs [55]. |
| MLOps Platform | Integrated platform for managing the machine learning lifecycle, ensuring version control, audit trails, and continuous monitoring to promote accountability [56]. |
| Contractual Checklist | A standardized list of non-negotiable terms for AI vendor agreements, focusing on liability, warranties, and audit rights [54]. |
| Incident Response Plan | A documented procedure for containing, assessing, and rectifying harms caused by an AI system failure, including communication protocols. |
AI Accountability Framework
The diagram below outlines a systematic workflow for establishing accountability in AI-driven research, integrating key principles from technical and governance perspectives.
Optimizing Community and Stakeholder Engagement to Build Trust and Ensure Equity
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: What are the first steps to engaging community members in health equity research? Begin by identifying a focused, community-relevant topic to make the concept of partnership tangible [58]. Initial efforts should include conducting targeted outreach to community organizations and removing practical barriers to participation, such as registration fees and parking costs [58].
Q2: How can I formulate a strong, actionable research question for community-engaged studies? A strong research question should be focused, researchable, feasible, specific, and complex enough to develop over the space of a paper or thesis [59]. It is often developed by choosing a broad topic, doing preliminary reading to learn about current issues, and then narrowing your focus to a specific niche or identified gap in knowledge [59] [60].
Q3: Our research team is struggling with tokenistic community involvement. How can we center authentic community voices? A proven strategy is to feature a panel of community experts as a core part of your event or research design [58]. Partner with existing community workgroups to identify and invite panelists, and structure the session as an interactive discussion moderated by a trusted figure to elevate experiential knowledge [58].
Q4: What is the difference between quantitative and qualitative research questions in this context?
- Quantitative questions are precise and typically include the population, variables, and research design. They aim to prove or disprove a hypothesis and are often categorized as descriptive, comparative, or relationship-based [60] [61].
- Qualitative questions are more adaptable and non-directional, seeking to discover, explain, or explore. They can be exploratory, interpretive, or evaluative, often focusing on understanding experiences and behaviors in a natural setting [60] [61].
Q5: How do we evaluate the success of our community engagement initiatives? Evaluation can be conducted via post-event surveys. Success indicators include an improved understanding of health disparities among attendees, increased knowledge of best practices for community engagement, and greater motivation to foster these connections in their own work. Qualitative feedback can also provide valuable insights [58].
Common Challenges and Solutions
| Challenge | Description | Proposed Solution |
|---|---|---|
| Tokenistic Engagement | Community input is sought but not meaningfully incorporated, leading to power imbalances and mistrust [58]. | Center lived experiences by involving community partners in research design and featuring community expert panels [58]. |
| Lack of Researcher Skills | Faculty and researchers feel under-resourced or insufficiently trained to conduct community-engaged research [58]. | Build institutional capacity through symposiums, workshops, and internal grants that support and showcase community-engaged work [58]. |
| Poor Attendance & Participation | Even well-designed initiatives fail to attract a diverse mix of academic and community stakeholders. | Implement targeted, barrier-reducing outreach: waive fees, provide parking/vouchers, and use a hybrid format [58]. |
| Unfocused Research Questions | Questions are too broad, not researchable, or irrelevant to the community's actual needs [59]. | Use structured frameworks like PICO(T) and the FINER criteria to develop focused, feasible, and novel questions [60] [61]. |
| Sustaining Collaboration | Engagements are one-off events that fail to create lasting change or ongoing partnerships [58]. | Move beyond one-time events by conducting landscape analyses and developing longitudinal projects to build capacity for the long term [58]. |
Experimental Protocols and Methodologies
Protocol 1: Designing a Community-Engaged Research Symposium
This methodology outlines the key steps for organizing an academic symposium designed to foster genuine community engagement, based on a successfully implemented model [58].
1. Focused Topic Selection
- Objective: Ground the event in a concrete health equity challenge relevant to the community.
- Methods: Partner with community liaisons and clinical workgroups to identify a priority area (e.g., Sickle Cell Disease). This makes the need for partnership tangible for researchers [58].
2. Call for Community-Engaged Abstracts
- Objective: Showcase projects with meaningful community involvement.
- Methods:
- Disseminate an open call for abstracts through university and community partner listservs.
- Form a review committee to score submissions using a rubric that prioritizes projects demonstrating authentic community partnership in their design, implementation, or evaluation [58].
3. Centering Community Voices via an Expert Panel
- Objective: Elevate the knowledge of those with lived experience.
- Methods:
- Collaboratively identify and invite community panelists (e.g., patients, advocates).
- Hold pre-panel meetings with each participant to align on goals.
- Structure the panel as an interactive discussion moderated by a trusted keynote speaker [58].
4. Targeted Outreach and Accessibility
- Objective: Ensure diverse attendance from both academic and community sectors.
- Methods:
- Conduct intentional outreach through local organizations and personal invitations to community leaders.
- Remove participation barriers by waiving registration fees for community members, providing free parking, and offering a hybrid event format [58].
Protocol 2: Developing a Research Question Using the FINER Criteria
A framework for formulating a sound research question that is feasible, interesting, novel, ethical, and relevant [60].
1. Start with a Broad Topic
- Use brainstorming and concept mapping to explore a general area of interest, considering both personal interest and current discussions in the research community [60].
2. Conduct Preliminary Research
- Perform an initial literature review to understand the current state of the field and identify gaps or limitations in existing knowledge [60].
3. Narrow the Focus and Draft Questions
- Use "gap-spotting" to construct questions that address identified limitations, or "problematization" to challenge existing assumptions in the literature [60].
4. Evaluate Using FINER Criteria
- Assess each potential question against the following criteria [60]:
- Feasible: Adequate resources, time, and technical expertise to investigate.
- Interesting: Engaging to the researcher and the broader community.
- Novel: Confirms, refutes, or extends previous findings.
- Ethical: Will receive approval from relevant review boards.
- Relevant: Important to the scientific community and public interest.
Research Reagent Solutions
This table details key methodological components, or "research reagents," essential for conducting community-engaged health equity research.
| Item / Solution | Function & Explanation |
|---|---|
| Community Advisory Board (CAB) | A group of community stakeholders that provides ongoing guidance, ensures cultural relevance, and helps shape research priorities and methods from inception to dissemination. |
| Structured Engagement Framework (e.g., PICO(T)) | Provides a methodological structure (Patient/Problem, Intervention, Comparison, Outcome, Time) to formulate focused, answerable research questions [61]. |
| Barrier-Reduction Toolkit | A set of practical resources (e.g., fee waivers, parking vouchers, translation services, hybrid participation options) designed to actively enable diverse community participation [58]. |
| Partnership Rubric | A scoring tool used by review committees to evaluate and select research abstracts based on demonstrated depth of community involvement, moving beyond tokenistic inclusion [58]. |
| Post-Engagement Evaluation Survey | A data collection instrument (e.g., a Continuing Medical Education survey) used to measure the impact of an initiative on attendees' understanding, knowledge, and motivation [58]. |
Workflow Visualizations
Community Engagement Symposium Workflow
Research Question Development Pathway
Measuring Success: Validating and Comparing Ethical Frameworks
Frequently Asked Questions
What are the most common reasons an interdisciplinary ethics strategy fails? Strategies often fail due to a lack of clear, shared goals among team members from different disciplines and insufficient communication protocols [62]. Other critical failures include the use of evaluation benchmarks that are misaligned with real-world outcomes or that contain inherent biases, which can misdirect the strategy's development and undermine trust in its results [63].
How can we establish shared goals with team members from different disciplinary backgrounds? Begin by collaboratively defining the ethical framework for your project. This involves discussing and agreeing upon the core moral principles that will guide your work, such as autonomy, beneficence, non-maleficence, and justice [64]. Facilitate discussions where each discipline can express its primary ethical concerns and methodologies, aiming to find common ground and establish a unified purpose [65].
Our team is experiencing a conflict between ethical frameworks. How can we resolve this? Adopt a structured approach to ethical analysis. Methodologies like principlism, which balances multiple ethical principles, or case-based methods (casuistry), which draws parallels to precedent-setting cases, can provide a neutral structure for deliberation [64]. The focus should be on applying these structured methods to the specific case at hand rather than debating theoretical differences.
What is a key sign that our ethics strategy is working? A key benchmark of success is the effective mitigation of foreseeable ethical risks and the absence of harm to research participants or end-users [66]. Furthermore, success is demonstrated when the strategy proactively identifies and navigates novel ethical dilemmas arising from technological innovations, rather than reacting to problems after they occur [64].
How do we evaluate the real-world impact of our ethics strategy beyond checking compliance boxes? Move beyond one-time testing logic [63]. Evaluation should be continuous and should consider the strategy's practical consequences on healthcare practice and policy [65]. This can involve analyzing how the strategy influences decision-making, ensures equitable access to benefits, and addresses the needs of underserved populations [64].
Troubleshooting Guides
Problem: Inconsistent Ethical Decisions Across the Team
Different team members are applying different ethical standards, leading to inconsistent project guidance and outcomes.
Step 1: Diagnose the Cause
- Organize a facilitated meeting to review recent case decisions.
- Identify if inconsistencies stem from differing core principles (e.g., utilitarianism vs. deontology), varying risk tolerances, or a simple lack of a shared decision-making protocol [64].
Step 2: Implement a Unified Framework
- Develop a standard operating procedure (SOP) for ethical review that all disciplines must follow.
- This SOP should incorporate a multi-principle framework that requires team members to explicitly consider and weigh principles like autonomy, justice, and non-maleficence for every major decision [64].
Step 3: Create a Decision-Making Artifact
- Introduce a structured worksheet or digital form that logs each ethical query, the principles considered, the arguments made, and the final rationale. This creates consistency and a valuable institutional record [62].
Problem: Breakdown in Communication with External Partners
Miscommunication with external IRBs, cultural consultants, or international collaborators is delaying project approval.
Step 1: Formalize Reliance Agreements
- Ensure that a formal written agreement is in place between collaborating institutions. This agreement must define the respective authorities, roles, responsibilities, and methods of communication between the IRB of record and your team [66].
Step 2: Proactively Engage Cultural and Regulatory Expertise
- For international research, proactively inform your IRB of local regulations and cultural norms regarding recruitment and consent. The IRB can then obtain a cultural consultant to provide written comments on protocols involving subjects from a foreign culture [66].
Step 3: Verify Credentials and Training
- Before ceding review to an external IRB, verify that the IRB is accredited by a body like the Association for the Accreditation of Human Research Protection Programs (AAHRPP) and that all investigators have documented, up-to-date human subjects protection training [66].
Evaluation Benchmarks and Methodologies
The following table outlines core benchmarks and methods for evaluating your interdisciplinary ethics strategy, highlighting common pitfalls identified in AI benchmarking that are equally relevant to ethics evaluation [63].
Table 1: Benchmarks for Evaluating an Interdisciplinary Ethics Strategy
| Benchmark Category | Specific Metric | Evaluation Methodology | Common Pitfalls to Avoid |
|---|---|---|---|
| Framework Robustness | • Adherence to declared ethical principles (e.g., Belmont) [66].• Use of a structured ethical analysis method (e.g., Principlism, Casuistry) [64]. | • Audit a sample of project decisions against the framework.• Conduct peer-review of ethical analyses. | • Over-focus on performance: Prioritizing speed of decision-making over quality of ethical reasoning [63].• Construct validity issues: Using a framework that doesn't actually measure real-world ethical outcomes [63]. |
| Interdisciplinary Collaboration | • Documented input from all relevant disciplines in final decisions.• Survey scores on team communication and trust. | • Analyze meeting minutes and decision logs.• Administer anonymous team health surveys. | • Cultural/commercial dynamics: Allowing one dominant discipline (e.g., commercial interests) to silence others [63]. |
| Societal & Practical Impact | • Equity of benefits distribution to underserved populations [64].• Successful navigation of IRB/regulatory review [66].• Public perception and media discourse analysis [65]. | • Analyze participant demographic data.• Track protocol approval timelines.• Conduct systematic analysis of media debates [65]. | • Inadequate documentation: Failing to document the rationale for trade-offs, making the strategy opaque and unaccountable [63].• Gaming the system: Optimizing for IRB approval at the expense of genuine ethical rigor [63]. |
Table 2: The Researcher's Toolkit: Essential Formulation and Evaluation Frameworks
| Tool Name | Function | Brief Explanation & Application |
|---|---|---|
| PICO/SPICE Framework [67] | Formulating Research Questions | A structured tool to define the Population, Intervention, Comparison, and Outcome (or Setting, Perspective, Intervention, Comparison, Evaluation) of a study, ensuring the research question is well-defined and testable. |
| FINER Criteria [67] | Evaluating Research Questions | A checklist to assess if a research question is Feasible, Interesting, Novel, Ethical, and Relevant. Crucial for evaluating the practical and ethical viability of a research direction. |
| Principlism [64] | Ethical Analysis | A pluralistic approach that balances the four core principles of autonomy, beneficence, non-maleficence, and justice to resolve specific moral dilemmas. |
| Media Debate Analysis [65] | Assessing Societal Impact | A methodological approach to systematically analyze media coverage, providing insights into public perceptions, emerging moral problems, and the societal context of your work. |
Experimental Protocol: Evaluating Strategy Effectiveness with a Simulated Case
This protocol provides a methodology for stress-testing your interdisciplinary ethics strategy using a simulated, high-fidelity case study.
1. Objective To evaluate the robustness, consistency, and interdisciplinary cohesion of an ethics strategy when confronted with a complex, novel ethical dilemma.
2. Materials and Reagents
- Case Study: A detailed, written scenario involving a cutting-edge technology (e.g., an AI diagnostic tool with biased training data, a gene-editing therapy) that presents clear conflicts between ethical principles (e.g., justice vs. beneficence).
- Participant Briefing Pack: Including the team's own ethics framework, SOPs, and any relevant regulatory guidelines.
- Observation Checklist: For facilitators to record metrics like time to decision, invocation of core principles, and frequency of cross-disciplinary communication.
- Post-Simulation Survey: To capture participant perceptions of the process.
3. Procedure
- Step 1: Team Assembly & Briefing Convene a representative, interdisciplinary team. Provide the briefing pack and the detailed case study. Assign a facilitator to manage the process without influencing the outcome.
- Step 2: Ethical Analysis Phase The team works through the case using its established ethics strategy and decision-making protocols. The facilitator records observations against the checklist.
- Step 3: Decision and Rationale Documentation The team must reach a consensus decision or a formal dissenting opinion. The final rationale, including all ethical principles weighed and rejected, must be documented in the standard worksheet.
- Step 4: Debrief and Analysis Facilitate a debriefing session focusing on the process, not just the outcome. Discuss points of friction, communication breakdowns, and ambiguities in the framework. Administer the post-simulation survey.
- Step 5: Strategy Iteration Use the collected data (observation notes, decision artifact, survey results) to identify weaknesses in the ethics strategy and refine the frameworks, SOPs, and communication plans accordingly.
4. Data Analysis Analyze the results to answer key evaluation questions:
- Consistency: Would two different teams reach a similar conclusion using the same strategy?
- Robustness: Did the strategy adequately guide the team through the novel dilemma?
- Efficiency: Was the process unnecessarily cumbersome?
- Interdisciplinary Integration: Did all disciplines feel their viewpoint was adequately heard and considered?
Visual Workflow: Interdisciplinary Ethics Strategy Evaluation
The diagram below outlines the logical workflow for developing, implementing, and iteratively improving an interdisciplinary ethics strategy.
Overcoming interdisciplinary challenges is a central problem in bioethics methodology research. The field is characterized by the integration of diverse disciplines, from philosophy and law to the social, natural, and medical sciences [49]. This interdisciplinary setting, while a source of creative collaboration and innovation, presents significant methodological challenges, particularly regarding establishing a common standard of rigor when each contributing discipline possesses its own accepted criteria for truth and validity [1]. This paper analyzes two predominant methodological approaches for addressing ethical issues in technological and scientific development: the traditional After-the-Fact Review and the emerging Embedded Ethics model.
Embedded Ethics, specifically defined as "the practice of integrating the consideration of social and ethical into the entire development process in a deeply integrated, collaborative and interdisciplinary way," represents a proactive attempt to bridge these methodological divides [17]. In contrast, Traditional After-the-Fact Review often occurs post-implementation and has been criticized for lacking forward-looking strategies to effectively avoid harm before it occurs [17]. This analysis compares these two paradigms within the context of interdisciplinary bioethics research, providing researchers and developers with a practical framework for selecting, implementing, and troubleshooting these methodologies.
Core Concepts and Definitions
Traditional After-the-Fact Review
This model involves ethical and social analysis conducted after a technology has been largely developed or deployed. It is often characterized by external assessment and aims to mitigate adverse effects once they have been identified, though it often struggles to prevent harm proactively [17].
Embedded Ethics Approach
This is a dynamic, integrative approach where trained ethicists and/or social scientists are embedded within research and development teams. They conduct empirical and normative analysis iteratively throughout the development process to help teams recognize and address ethical concerns as they emerge [17]. The approach is designed to "stimulate reflexivity, proactively anticipate social and ethical concerns, and foster interdisciplinary inquiry" at every stage of technology development [17].
Interdisciplinary Bioethics Methodology
Bioethics is defined as the "systematic study of the moral dimensions – including moral vision, decisions, conduct, and policies – of the life sciences and health care, employing a variety of methodologies in an interdisciplinary setting." [49] This methodology broadens horizons and favors the cross-pollination of ideas, though it must navigate challenges related to integrating diverse disciplinary standards of rigor [1] [49].
Comparative Analysis: Embedded Ethics vs. Traditional After-the-Fact Review
The following table summarizes the key quantitative and qualitative differences between the two methodological approaches.
Table 1: Methodological Comparison of Embedded Ethics and Traditional After-the-Fact Review
| Feature | Embedded Ethics | Traditional After-the-Fact Review |
|---|---|---|
| Timing of Integration | Integrated from the outset and throughout the R&D lifecycle [17] | Post-development or post-implementation analysis [17] |
| Primary Objective | Proactively anticipate concerns and shape responsible innovation [17] | Mitigate identified adverse effects and harms [17] |
| Position of Ethicists | Embedded within the research team; collaborative [17] | External to the project team; often advisory or auditing |
| Nature of Output | Iterative feedback, dynamic guidance, and stimulated team reflexivity [17] | Retrospective reports, compliance checks, and ethical audits |
| Key Advantage | Prevents harm by design; fosters interdisciplinary sensitivity [17] | Clear separation of roles; leverages established review procedures |
| Key Challenge | Requires deep, ongoing collaboration and resource commitment | "After-the-fact analysis is often too late" to prevent harm [17] |
| Suitability | Complex, fast-moving fields like AI and healthcare with high ethical stakes [17] | Projects with well-defined endpoints and stable ethical frameworks |
Experimental Protocols and Workflows
Protocol for Implementing an Embedded Ethics Approach
The following workflow outlines the key stages for integrating Embedded Ethics into a research and development project, such as in AI-related healthcare consortia.
Figure 1: Workflow for implementing the Embedded Ethics approach in a project lifecycle.
Protocol Steps:
- Integration: Embed trained ethics and social science researchers as core members of the interdisciplinary project team from the very beginning [17].
- Immersion: The embedded researchers participate in regular team meetings and, when possible, work in the same venue to develop a profound understanding of the project's technical details and standard practices [17].
- Iterative Analysis: The embedded researchers continuously move between established ethical debates in the literature and the specific, emerging problems of the development project [17].
- Method Application: Employ a combination of empirical and normative methods (e.g., stakeholder analyses, ethnographic approaches, bias analyses, workshops) to identify and address issues [17].
- Dialogue: Maintain active, ongoing one-on-one and group discussions with technical team members to clarify details and discuss ongoing analyses [17].
- Refinement: Use the insights from the ethical analysis to proactively refine the technology's design, deployment plan, and research questions.
Protocol for Conducting a Traditional After-the-Fact Review
Figure 2: Sequential workflow of a Traditional After-the-Fact Review process.
Protocol Steps:
- Commissioning: An external body (e.g., an ethics review board, regulatory agency, or internal audit committee) is commissioned to conduct the review after a technology is deployed or a project is completed.
- Scoping: The review body defines the scope of its inquiry, often focusing on specific, identified harms or compliance with existing regulations and guidelines.
- Evidence Collection: Gathering retrospective data, which may include user complaints, adverse event reports, performance metrics, and internal project documentation.
- Framework Analysis: The collected evidence is analyzed against pre-existing ethical frameworks, principles, or regulatory standards to identify breaches or shortcomings.
- Reporting: A report is generated detailing the findings and providing recommendations for corrective actions, policy changes, or future safeguards.
- Mitigation: The project team or responsible organization implements the recommended mitigating measures to address the identified issues.
The Scientist's Toolkit: Essential Methods & Reagents for Embedded Ethics
For researchers implementing an Embedded Ethics approach, the following table details key methodological "reagents" and their functions, as derived from successful applications in health AI projects [17].
Table 2: Research Reagent Solutions for Embedded Ethics Methodology
| Method/Tool | Primary Function | Application Context |
|---|---|---|
| Stakeholder Analyses | To identify all parties affected by the technology and map their interests, power, and vulnerabilities. | Informing project scope; ensuring inclusive design. |
| Ethnographic Approaches | To understand the cultural practices, workflows, and unspoken norms of the development team and end-users. | Gaining deep contextual insight into how technology will be used and its social impact. |
| Bias Analyses | To proactively identify and assess potential sources of algorithmic, data, or design bias. | Critical for AI/ML projects to ensure fairness and avoid discrimination. |
| Peer-to-Peer Interviews | To facilitate open discussion and knowledge sharing about ethical concerns within the project team. | Building trust and uncovering latent concerns among technical colleagues. |
| Focus Groups | To gather structured feedback from specific, pre-defined groups (e.g., potential user groups). | Exploring attitudes, perceptions, and reactions to technology concepts or prototypes. |
| Interdisciplinary Workshops | To collaboratively brainstorm, problem-solve, and develop ethical solutions with the entire team. | Synthesizing diverse expertise to address complex ethical-technical trade-offs. |
| Interviews with Affected Groups | To directly capture the experiences and values of those who will be most impacted by the technology. | Ensuring that the technology serves the needs of vulnerable or marginalized populations. |
Troubleshooting Guides and FAQs for Embedded Ethics Implementation
Q1: We tried to integrate an ethicist, but the technical team sees them as an obstacle to rapid development. How can we improve collaboration?
- Diagnosis: This indicates a preliminary failure in establishing shared goals and mutual respect. The ethicist may be perceived as an external auditor rather than a collaborative partner.
- Solution: Facilitate joint problem-solving sessions. The embedded researcher should focus on understanding the technical challenges and constraints first, then frame ethical considerations as integral to solving the core problem well, not as a separate hurdle. Co-authoring a project charter that explicitly includes ethical goals can align the team [17].
Q2: How can we maintain methodological rigor when our embedded ethics work must blend insights from philosophy, social science, and computer science?
- Diagnosis: This is a core interdisciplinary challenge. Rigor is not about adopting a single standard but about being transparent and systematic in how multiple methods are applied and integrated [1].
- Solution: Document the methodological approach meticulously. For example, when making a normative claim, reference the ethical framework (e.g., deontological, consequentialist) being applied [68]. When using empirical data from interviews, adhere to established qualitative research standards. Explicitly justify how the combination of methods provides a more robust answer than any one could alone [17].
Q3: Our embedded ethicist is struggling to understand the technical details of our AI model. Is this a fatal flaw?
- Diagnosis: This is a common challenge, not a fatal flaw. The goal is not for the ethicist to become a machine learning engineer, but to achieve sufficient mutual understanding for productive collaboration [17].
- Solution: Implement "tutorial" sessions where technical team members explain key concepts. Conversely, the ethicist should explain their core concepts and methods to the technical team. This bidirectional knowledge exchange fosters the "shared language" necessary for interdisciplinarity and builds the trust required for tackling complex problems [1] [17].
Q4: The recommendations from our embedded ethics analysis are too abstract to implement in code. What went wrong?
- Diagnosis: There is a translation gap between the normative ethical analysis and the practical engineering requirements.
- Solution: Shift from abstract principles to concrete design requirements via iterative prototyping. Use methods like the "Ethics Bowl" or "red teaming" exercises where developers actively critique each other's projects from a moral standpoint [69]. This forces the translation of abstract values into tangible system features and design choices.
The comparative analysis demonstrates that the Embedded Ethics model offers a transformative pathway for addressing the inherent interdisciplinary challenges in bioethics methodology. Unlike the Traditional After-the-Fact Review, which is often limited to mitigating harm that has already occurred, Embedded Ethics fosters a proactive, reflexive, and integrative practice. By embedding ethical and social inquiry directly into the research and development process, this approach empowers scientists and developers to anticipate concerns, navigate ethical trade-offs, and ultimately shape more responsible and socially just technologies. For the field of bioethics to effectively overcome its methodological challenges and guide innovation in complex domains like AI and healthcare, moving beyond after-the-fact review to deeply integrated, collaborative models is not just beneficial—it is essential.
Technical Support Center
Frequently Asked Questions (FAQs)
Q1: Our federated learning model performs well on the aggregated test set but fails to outperform a local model on its own dataset. Is this a failure? A1: Not necessarily. This is a recognized characteristic of federated learning (FL) in real-world settings. The global FL model is optimized for generalizability across all institutional data distributions. A local model, trained exclusively on its own data, may achieve superior performance on that specific dataset but likely will not generalize as well to external data sources. The value of the FL model lies in its robust, aggregated knowledge. [70]
Q2: Our collaborative experiments are taking too long due to system and data heterogeneity among partners. How can we speed this up? A2: Experiment duration is a common challenge. One effective strategy is to optimize the number of local training epochs on each client before aggregation. Balancing the number of local epochs is critical; too few can slow convergence, while too many may cause local models to diverge. Start with a lower number of epochs (e.g., 1-5) and adjust based on performance. [70]
Q3: We are facing network restrictions from hospital firewalls and corporate security policies. How can we establish a connection for the federated learning server? A3: This is a major practical hurdle. A documented solution is to deploy the central FL server on a cloud infrastructure, such as Amazon Web Services (AWS), within a semi-public network. This server must then have an open port to which the various institutional clients can connect, bypassing the need to alter highly restrictive hospital network policies. [70]
Q4: What are the primary interdisciplinary challenges in bioethics that impact collaborative research? A4: Bioethics research inherently draws on multiple disciplines (e.g., philosophy, law, medicine, sociology), each with its own methods and standards of rigor. Key challenges include: [1]
- The absence of clear, universal standards for evaluating normative conclusions.
- Difficulties in the peer-review process due to differing disciplinary interpretations of "rigor."
- Challenges in integrating diverse perspectives for practical clinical decision-making.
Q5: What is the fundamental hypothesis of radiogenomics? A5: Radiogenomics is founded on several core hypotheses, including: [71]
- Normal tissue radiosensitivity is a complex trait dependent on the combined influence of variations in several genes.
- Single Nucleotide Polymorphisms (SNPs) account for a proportion of the genetic basis for differences in clinical normal tissue radiosensitivity.
Troubleshooting Guides
Issue: Federated Learning Model Underperforms Locally
Symptoms:
- The global FL model shows strong average performance across all test sets.
- On a specific client's test set, the global model's performance is lower than that client's locally trained model.
| Diagnostic Step | Action | Expected Outcome |
|---|---|---|
| Performance Analysis | Calculate performance metrics (e.g., AUC, accuracy) for both the global and local models on the local test set. | Confirm the performance gap is real and not an artifact of measurement. |
| Data Distribution Check | Analyze the data distribution (e.g., feature means, label ratios) of the local dataset compared to other consortium members. | Identify significant data heterogeneity that may explain the global model's relative performance. |
| Evaluate Generalizability | Test the local model on other clients' test data or an external validation set. | The local model will likely show a steeper performance decline than the global FL model, demonstrating the FL model's strength in generalizability. |
Resolution: This is often an expected outcome, not a bug. The solution is to reframe the success criteria of the FL project from "beating every local model" to "building a robust, generalizable model that performs well across diverse, unseen datasets without sharing private data." [70]
Issue: Managing Interdisciplinary Collaboration and Methodological Rigor
Symptoms:
- Disagreements on what constitutes valid evidence or a rigorous argument.
- Peer reviews from different disciplines provide conflicting feedback.
- Difficulty integrating diverse perspectives into a single, coherent research output.
| Diagnostic Step | Action | Expected Outcome |
|---|---|---|
| Methodology Mapping | Explicitly list the methodological standards of rigor from each discipline represented in the consortium (e.g., philosophical, clinical, statistical). | Create a clear map of the different epistemological frameworks at play. |
| Identify Conflict Points | Pinpoint where the disciplinary standards conflict or are incommensurate in evaluating the research. | Isolate the specific sources of disagreement to move from a theoretical to a practical problem. |
| Develop a Hybrid Framework | Establish a project-specific framework that explicitly defines how different types of evidence and argumentation will be weighted and integrated. | Creates a shared, transparent standard of rigor for the specific project, mitigating interdisciplinary conflicts. [1] |
Resolution: Adopt an explicit interdisciplinary methodology. This involves creating a collaborative framework that does not privilege one discipline's methods over another by default but seeks a "creative collaboration" and "cross-pollination of ideas" to address the bioethical challenge. [49]
Experimental Protocols & Data
Protocol 1: Implementing a Real-World Federated Learning Network for Computational Pathology
Objective: To collaboratively train a deep learning model for digital immune phenotyping in metastatic melanoma across multiple international institutions without centralizing patient data. [70]
Methodology:
- Infrastructure Setup: A central server is deployed on an Amazon Web Services (AWS) instance in a semi-public network with an open port. Each participating institution (client) requires the IT expertise and network permissions to allow their system to connect to this server.
- Software Framework: Utilize the NVIDIA Federated Learning Application Runtime Environment (NVIDIA FLARE).
- Training Configuration:
- The model architecture is defined and distributed to all clients.
- Clients train the model locally on their private data for a predetermined number of epochs.
- Locally trained model weights are sent to the central server.
- The server aggregates the weights (e.g., using Federated Averaging) to update the global model.
- The updated global model is distributed back to clients for the next round of training.
- Optimization: To manage experiment duration, the number of local training epochs is a key hyperparameter to tune.
Protocol 2: Conducting a Radiogenomics Genome-Wide Association Study (GWAS)
Objective: To identify germline genetic variants (Single Nucleotide Polymorphisms or SNPs) associated with susceptibility to radiation-related toxicities. [71]
Methodology:
- Cohort Assembly: Pool individual patient cohorts from multiple research groups, often coordinated by a consortium like the International Radiogenomics Consortium (RGC).
- Phenotyping: Precisely define and grade specific radiation toxicity endpoints (e.g., proctitis, xerostomia) using standardized scales.
- Genotyping: Perform genome-wide genotyping on patient DNA samples to identify millions of SNPs.
- Quality Control: Filter out low-quality SNPs and subjects based on call rate, deviation from Hardy-Weinberg equilibrium, and other metrics.
- Association Analysis: For each SNP, perform a statistical test (e.g., logistic regression) for association with the toxicity phenotype, typically adjusting for clinical covariates (e.g., dose, age, gender).
- Multiple Hypothesis Testing Correction: Apply stringent correction methods (e.g., Bonferroni) to account for the millions of statistical tests performed and reduce false positives.
- Validation: Seek to replicate significant findings in an independent patient cohort.
Table 1: Characteristics of Featured Research Consortia
| Consortium / Field | Primary Collaborative Goal | Key Quantitative Challenge | Technical Infrastructure |
|---|---|---|---|
| Computational Pathology (FL) [70] | Train a model for digital immune phenotyping. | FL model did not outperform all local models on their native data; long experiment duration. | NVIDIA FLARE, AWS server, 3 clients in 4 countries. |
| Radiogenomics (RGC) [71] | Identify genetic variants linked to radiation toxicity. | Risk of spurious SNP associations due to multiple hypothesis testing; requirement for large, pooled cohorts (e.g., 5,300 in REQUITE). | Centralized biobanking and genotyping with distributed clinical data collection. |
| Bioethics Methodology [1] | Develop rigorous cross-disciplinary ethical analysis. | No agreed-upon primary method or standard of rigor; encompasses "dozens of methods." | Interdisciplinary teams, collaborative frameworks. |
Table 2: Troubleshooting Approaches for Common Challenges
| Challenge | Root Cause | Proposed Solution | Key Reference |
|---|---|---|---|
| FL Model Local Performance | Data heterogeneity; goal of generalizability. | Re-define success metrics; value global model performance. | [70] |
| Network/Firewall Restrictions | Hospital IT security policies. | Deploy central server on cloud (AWS) with an open port. | [70] |
| Interdisciplinary Methodological Conflict | Differing standards of "rigor" across disciplines. | Develop explicit, project-specific hybrid methodological frameworks. | [1] [49] |
| Spurious Genetic Associations | Multiple hypothesis testing in GWAS. | Apply stringent statistical corrections (e.g., Bonferroni); independent validation. | [71] |
Visualizations
Diagram 1: Federated Learning Workflow for Medical Data
Diagram 2: Interdisciplinary Bioethics Methodology
Diagram 3: Radiogenomics GWAS Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Item / Solution | Function | Application Context |
|---|---|---|
| NVIDIA FLARE | A software development kit for building and deploying federated learning applications. | Enables collaborative model training across distributed medical datasets while preserving data privacy. [70] |
| Cloud Compute Instance (e.g., AWS) | Provides a centrally accessible, scalable server environment. | Hosts the aggregation server in a federated learning network, mitigating institutional firewall issues. [70] |
| GWAS Genotyping Array | A microarray designed to assay hundreds of thousands to millions of SNPs across the human genome. | Used in radiogenomics to perform genome-wide scans for genetic variants associated with radiation toxicity. [71] |
| Standardized Phenotyping Scales | Common Terminology Criteria for Adverse Events (CTCAE) or similar. | Provides consistent and reproducible grading of radiation toxicity phenotypes across different clinical centers in a consortium. [71] |
| Interdisciplinary Framework | A structured methodology for integrating knowledge from different disciplines. | Provides the "systematic study" needed to address moral dimensions in healthcare and life sciences, ensuring rigor in bioethics research. [49] |
Troubleshooting Guides
Guide 1: My AI system is for drug discovery. Is it considered "high-risk" under the EU AI Act?
Problem: Determining the correct risk classification for an AI system used in scientific research and development.
Diagnosis: The EU AI Act uses a risk-based approach. Many AI systems in the life sciences, especially those impacting human health, are likely to be classified as high-risk, which triggers specific legal obligations [72] [73].
Solution: Follow this diagnostic flowchart to determine your AI system's status.
Next Steps: If your system is high-risk, you must comply with requirements in areas of risk management, data governance, technical documentation, and human oversight before placing it on the market [72].
Guide 2: How do I validate a General-Purpose AI (GPAI) model for use in our high-risk research pipeline?
Problem: Integrating a foundation model (e.g., a large language model for literature analysis) into a regulated research environment.
Diagnosis: The EU AI Act places specific obligations on both providers of GPAI models and the downstream providers who integrate them into high-risk systems [72] [74].
Solution: Ensure you and your GPAI model provider meet the following requirements.
Next Steps: Cooperate closely with your GPAI provider. As an integrator, you need their documentation to understand the model's capabilities and limitations to ensure your final high-risk AI system is compliant [72].
Frequently Asked Questions (FAQs)
Q1: What are the most critical deadlines I need to know for compliance? The EU AI Act is being implemented in phases [73] [75]:
- Prohibited AI Practices & AI Literacy: In effect since February 2025.
- General-Purpose AI (GPAI) Model Rules: Apply from August 2025.
- High-Risk AI Systems Rules: Apply from August 2026.
- High-Risk AI Systems embedded in regulated products: Apply from August 2027.
Q2: Our research AI only creates preliminary data for scientist review. Is it still high-risk? Possibly not. The AI Act provides exceptions for AI systems that perform "a narrow procedural task," "improve the result of a previously completed human activity," or perform "a preparatory task" to an assessment [72]. Document your assessment that the system is not high-risk before deployment.
Q3: What are the consequences of non-compliance? Penalties are severe and tiered based on the violation [76]:
- Prohibited AI Practices: Up to €35 million or 7% of global annual turnover.
- Non-compliance with Data/Transparency rules: Up to €15 million or 3% of global annual turnover.
- Other violations: Up to €7.5 million or 1% of global annual turnover.
Q4: How does the EU AI Act address the use of AI in generating research content to prevent misconduct? The Act emphasizes transparency. Furthermore, academic literature highlights that AI can introduce new forms of misconduct, such as data fabrication and text plagiarism [77]. The scientific community is advised to strengthen ethical norms, enhance researcher qualifications, and establish rigorous review mechanisms to ensure responsible and transparent research processes [77].
Q5: Are there simplified rules for startups and academic spinoffs? Yes. The AI Act includes support measures for SMEs and startups [76]. These include priority access to regulatory sandboxes (controlled testing environments), tailored awareness-raising activities, and reduced fees for conformity assessments.
Research Reagent Solutions: EU AI Act Compliance
This table details key "reagents" – the essential documentation and procedural components required to validate your AI system under the EU AI Act.
| Research Reagent | Function in Experimental Validation |
|---|---|
| Technical Documentation | Demonstrates compliance with regulatory requirements; provides authorities with information to assess the AI system's safety and adherence to the law [72]. |
| Instructions for Use | Provides downstream deployers (researchers) with the necessary information to use the AI system correctly and in compliance with the Act [72]. |
| Risk Management System | Plans, instantiates, and documents ongoing risk management throughout the AI lifecycle, aiming to identify and mitigate potential risks [72]. |
| Fundamental Rights Impact Assessment | A mandatory assessment for deployers of certain high-risk AI systems to evaluate the impact on fundamental rights before putting the system into use [76]. |
| Code of Practice (GPAI) | A voluntary tool for providers of General-Purpose AI models to demonstrate compliance with transparency, copyright, and safety obligations before formal standards are adopted [74]. |
In an increasingly interconnected research landscape, cross-cultural ethical validation has become a critical imperative for ensuring that bioethical frameworks remain globally relevant and inclusive. This process involves establishing shared moral principles applicable across diverse cultural backgrounds while respecting legitimate cultural variations [78]. For researchers, scientists, and drug development professionals, this represents both a methodological challenge and an ethical necessity.
The fundamental tension in this domain lies between cultural relativism (the perspective that ethical standards are determined by individual cultures) and ethical universalism (the view that universal ethical principles apply to all cultures) [78]. Navigating this tension requires sophisticated approaches that acknowledge cultural differences while upholding fundamental ethical commitments.
Theoretical Foundations: Understanding Cross-Cultural Ethical Frameworks
Key Theoretical Perspectives
Several theoretical frameworks provide foundation for understanding cross-cultural ethics:
- Integrative Social Contracts Theory (ISCT): Attempts to reconcile ethical universalism and cultural relativism by suggesting ethical standards derive from both macrosocial contracts (universal moral norms) and microsocial contracts (specific to particular communities) [78].
- Stakeholder Theory in Global Context: Emphasizes ethical responsibilities to all stakeholders, with the understanding that stakeholder identification and prioritization may vary across cultures [78].
- Virtue Ethics Across Cultures: Recognizes that while virtues like honesty might be universally valued, their practical expression differs across cultural contexts [78].
The Ethical, Cultural, and Transnational (ECT) Competence Framework
Recent research has identified three essential competencies for navigating cross-cultural ethical challenges [79]:
Table: Core Competencies for Cross-Cultural Ethical Practice
| Competency Domain | Key Components | Application in Bioethics |
|---|---|---|
| Ethical Competence | Accountability, transparency, integrity in decision-making | Understanding how ethical principles translate across different regulatory environments |
| Cultural Competence | Acknowledging, respecting, and responding effectively to diverse cultural backgrounds | Recognizing how cultural values shape health beliefs and practices |
| Transnational Competence | Analytical, emotional, and creative capacities to work across national contexts | Interpreting complex international research collaborations and their ethical implications |
Common Cross-Cultural Ethical Challenges: A Troubleshooting Guide
Frequently Encountered Ethical Dilemmas
Table: Common Cross-Cultural Ethical Challenges in Research
| Challenge Category | Specific Manifestations | Potential Impact |
|---|---|---|
| Informed Consent Practices | Differing cultural interpretations of autonomy and individual decision-making versus family/community involvement | Compromised research integrity and participant protection |
| Data Privacy and Ownership | Varied cultural norms regarding individual privacy versus collective benefit; disparate legal frameworks | Ethical and legal compliance issues; loss of community trust |
| Resource Allocation | Questions about equitable access to research benefits across different economic contexts | Perpetuation of global health inequities |
| Gift-Giving and Relationships | Cultural traditions of gift-giving conflicting with anti-bribery policies | Ethical violations and legal consequences |
| Communication Styles | Direct versus indirect communication affecting how ethical guidelines are conveyed and interpreted | Misunderstandings and unintended ethical breaches |
Troubleshooting FAQs: Addressing Specific Cross-Cultural Ethical Issues
FAQ: How should our research team handle situations where local cultural practices conflict with our institutional ethical guidelines?
Solution: Implement a middle-ground approach that respects local customs while maintaining ethical integrity. For example, when gift-giving is culturally expected but potentially problematic, establish clear limits allowing modest, culturally appropriate gifts that wouldn't influence outcomes or violate anti-bribery laws [80]. Engage cultural advisors to help determine appropriate boundaries.
FAQ: What approach should we take when operating in regions with differing data privacy standards?
Solution: Adopt the highest global standards for data privacy regardless of local regulations, as demonstrated by leading global tech companies [80]. Provide comprehensive training to research team members on implementing these standards consistently across all research sites.
FAQ: How can we ensure truly informed consent when working in cultures with different communication norms and decision-making structures?
Solution: Adapt consent processes to respect cultural decision-making patterns while maintaining ethical essentials. This may involve community leaders or family members in the consent process where culturally appropriate, while still seeking individual agreement. Ensure consent materials are linguistically and culturally appropriate, not merely translated [79].
Experimental Protocols for Cross-Cultural Ethical Validation
Protocol: Cultural Validation of Ethical Frameworks
Purpose: To systematically evaluate and adapt ethical frameworks for cross-cultural applicability in research settings.
Materials:
- Draft ethical framework or guidelines
- Cultural advisors from relevant communities
- Multidisciplinary review team (including members from different cultural backgrounds)
- Structured evaluation tool
Procedure:
- Initial Framework Analysis: Identify culture-specific assumptions in existing ethical frameworks.
- Stakeholder Mapping: Identify all relevant stakeholders across cultural contexts, including community representatives.
- Cultural Translation: Adapt framework language and concepts to ensure cultural relevance while maintaining ethical principles.
- Scenario Testing: Apply the framework to culturally-specific case scenarios to identify potential conflicts or gaps.
- Iterative Refinement: Modify the framework based on feedback while ensuring core ethical principles are maintained.
- Implementation Planning: Develop culturally-appropriate implementation strategies and training materials.
Validation: The adapted framework should be tested with diverse focus groups and refined until it demonstrates both ethical robustness and cultural appropriateness.
Protocol: Ethical Climate Assessment in Multinational Research
Purpose: To evaluate and improve the ethical climate across multinational research collaborations.
Materials:
- Validated ethical climate survey instrument
- Cross-cultural interview protocols
- Multilingual research team members
- Data analysis framework capable of identifying cultural patterns
Procedure:
- Survey Administration: Distribute ethical climate surveys in appropriate languages and cultural contexts.
- Structured Interviews: Conduct in-depth interviews with stakeholders from different cultural backgrounds.
- Comparative Analysis: Identify patterns, convergences, and divergences in ethical perceptions across cultures.
- Intervention Development: Create targeted interventions to address identified ethical climate challenges.
- Impact Evaluation: Assess the effectiveness of interventions through follow-up assessment.
Visualizing Cross-Cultural Ethical Validation: Workflow Diagrams
Cross-Cultural Ethical Framework Development Process
Ethical Dilemma Resolution Protocol
Research Reagent Solutions: Essential Tools for Cross-Cultural Ethical Research
Table: Essential Methodological Tools for Cross-Cultural Ethical Validation
| Tool Category | Specific Instruments | Application & Function |
|---|---|---|
| Assessment Tools | Cross-cultural ethical climate surveys, Cultural value assessment instruments | Measure perceptions of ethical practices across different cultural contexts |
| Analytical Frameworks | Integrative Social Contracts Theory (ISCT), Ethical, Cultural, and Transnational (ECT) framework | Provide structured approaches for analyzing cross-cultural ethical dilemmas |
| Stakeholder Engagement Methods | Cultural advisory panels, Community engagement protocols | Ensure inclusive participation of diverse cultural perspectives |
| Training Resources | Case studies with cultural variations, Ethical decision-making simulations | Build capacity for navigating cross-cultural ethical challenges |
| Implementation Tools | Localized code of conduct templates, Cross-cultural communication guides | Support application of ethical frameworks in specific cultural contexts |
Best Practices for Cross-Cultural Ethical Validation
Evidence-Based Implementation Strategies
Research indicates several effective strategies for implementing cross-cultural ethical frameworks [80] [79]:
Conduct Comprehensive Cultural Due Diligence: Before engaging in cross-cultural research, invest significant time in understanding cultural norms, values, and ethical perspectives of involved cultures [78].
Establish Clear Core Ethical Principles: Define a set of core ethical principles broad enough for cross-cultural application yet specific enough to provide clear direction. Examples include integrity, respect, fairness, and responsibility [78].
Promote Open Communication and Dialogue: Create structured channels for cross-cultural communication about ethical issues, including active listening and seeking to understand different cultural viewpoints [78].
Implement Continuous Ethics Training: Provide ongoing training on cross-cultural ethics that moves beyond awareness to practical decision-making skills using case studies and simulations [78].
Localize Ethical Frameworks: Develop global ethical standards that allow for localization to address specific cultural contexts while maintaining fundamental ethical intent [78].
Measuring Effectiveness: Key Performance Indicators
Table: Metrics for Evaluating Cross-Cultural Ethical Framework Effectiveness
| Evaluation Dimension | Specific Metrics | Data Collection Methods |
|---|---|---|
| Cultural Relevance | Perceived appropriateness across cultural groups, Identification of cultural conflicts | Focus groups, Structured interviews |
| Implementation Fidelity | Consistency of application across sites, Adherence to core principles | Ethical audits, Process documentation |
| Stakeholder Satisfaction | Perception of fairness and respect among diverse stakeholders | Satisfaction surveys, Grievance reporting |
| Ethical Outcomes | Reduction in cross-cultural ethical incidents, Improvement in ethical decision-making | Incident reporting, Case review analysis |
Cross-cultural validation of ethical frameworks is not merely an academic exercise but a practical necessity for researchers, scientists, and drug development professionals operating in global contexts. By implementing systematic approaches to cross-cultural ethical validation, the research community can develop frameworks that are both ethically robust and culturally inclusive.
The ongoing disruption in bioethics methodology [81] presents an opportunity to move beyond Western-centric frameworks and embrace the social, political, and philosophical plurality that characterizes our global research environment. Through deliberate preparation, continuous learning, and authentic engagement with diverse cultural perspectives, we can build ethical frameworks capable of guiding research that is both scientifically rigorous and culturally respectful.
Conclusion
Overcoming interdisciplinary challenges in bioethics is not merely an academic exercise but a fundamental prerequisite for responsible scientific progress. By moving beyond siloed approaches and adopting integrated methodologies like Embedded Ethics, researchers and drug developers can proactively address ethical concerns from the outset. The key takeaways underscore the necessity of continuous collaboration between ethicists, scientists, and the community; the critical importance of transparency and fairness in algorithmic systems; and the need for dynamic, adaptable ethical frameworks. The future of biomedical research demands that ethical rigor keeps pace with technological innovation. This involves developing new metrics for ethical impact, fostering greater public engagement, and building regulatory environments that support, rather than stifle, responsible and equitable innovation. Embracing these interdisciplinary strategies will ultimately ensure that scientific breakthroughs translate into trustworthy and just healthcare solutions for all.
References
- 1. Disciplining Bioethics: Towards a Standard of Methodological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3413904/]
- 2. Normative Stakes of Interdisciplinarity in Bioethics [https://www.academia.edu/125453867/Overcoming_Biases_Together_Normative_Stakes_of_Interdisciplinarity_in_Bioethics]
- 3. Deontology, utilitarianism, and virtues ethical theories [https://www.heartforkingdom.com/2024/05/05/deontology-utilitarianism-and-virtues-ethics/]
- 4. Deontological or Utilitarian? An Eternal Ethical Dilemma in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8391290/]
- 5. (PDF) Biomedical - opportunities and research ethical challenges [https://www.academia.edu/73926641/Biomedical_research_opportunities_and_ethical_challenges]
- 6. Principles of Clinical Ethics and Their Application to Practice [https://pmc.ncbi.nlm.nih.gov/articles/PMC7923912/]
- 7. The Ethics of Clinical Trials in the Drug Development Process [https://www.meetlifesciences.com/media-hub/blog/the-ethics-of-clinical-trials-in-the-drug-development-process/]
- 8. Troubleshooting & FAQs [https://www.cygnustechnologies.com/resources/guidelines?srsltid=AfmBOoovuS42NdWfIDQgyaOkmWi2KBnMU3982H_nUnjBGF_2rJDGaIWd]
- 9. Ethical principles across countries: does 'ethical' mean the ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1579778/full]
- 10. Ethical decision-making in biopharmaceutical research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7482740/]
- 11. Chapter 5.4: Color Theory and Accessibility in Data Visualization [https://express.excelsior.edu/datascience/chapter/5-4-color-theory-and-accessibility-in-data-visualization/]
- 12. Navigating color integrity in data visualization - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11117063/]
- 13. Ethical and Bias Considerations in Artificial Intelligence ... [https://www.sciencedirect.com/science/article/pii/S0893395224002667]
- 14. How to Tackle Algorithmic Bias: Top 4 Challenges and ... [https://emeritus.org/blog/what-is-algorithmic-bias/]
- 15. Algorithmic Solutions to Algorithmic Bias: A Technical Guide [https://medium.com/data-science/algorithmic-solutions-to-algorithmic-bias-a-technical-guide-aef59eaf6565]
- 16. Ethical challenges in the algorithmic era: a systematic rapid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574269/]
- 17. Embedded Ethics in Practice: A Toolbox for Integrating the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11668859/]
- 18. Ethical considerations in quality improvement: key ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8372876/]
- 19. Recommended format for a 'research protocol' [https://www.who.int/groups/research-ethics-review-committee/recommended-format-for-a-research-protocol]
- 20. An Example of Integrating Ethics in R&I Research [https://link.springer.com/article/10.1007/s41125-023-00096-0]
- 21. Teaching Your Lab Staff to Successfully Troubleshoot [https://www.labmanager.com/teaching-your-lab-staff-to-successfully-troubleshoot-32784]
- 22. Troubleshooting Protocols - Biological Sciences: Summer ... [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 23. 6 tips for building a thriving help center [https://www.zendesk.com/blog/6-tips-for-building-a-thriving-help-center/]
- 24. Help Center Best Practices for Better Customer Self-Service [https://document360.com/blog/help-center-best-practices/]
- 25. Top 17 Help Desk Best Practices for 2025 [https://www.desk365.io/blog/help-desk-best-practices/]
- 26. AI, cultural heritage and bias-mitigating in practice [https://link.springer.com/article/10.1007/s00146-025-02349-z]
- 27. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 28. Text has enhanced contrast - Rules - Siteimprove [https://alfa.siteimprove.com/rules/sia-r66]
- 29. Contrast requirements for WCAG 2.2 Level AA [https://www.makethingsaccessible.com/guides/contrast-requirements-for-wcag-2-2-level-aa/]
- 30. Interdisciplinary Team Science and the Public: Steps Towards ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5973546/]
- 31. Teaching troubleshooting skills to graduate students - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11407763/]
- 32. A Guide to Effective Troubleshooting in Experimental Design ... [https://www.bioprecisioncrafted.ca/post/uncovering-the-root-causes-a-guide-to-effective-troubleshooting-in-experimental-design-failures]
- 33. Journal of Medical Ethics blog [https://blogs.bmj.com/medical-ethics/2024/06/18/interdisciplinary-collaboration-to-identify-and-address-ethical-issues-arising-from-the-development-of-irreversible-high-risk-medical-treatments/]
- 34. Embedded ethics: a proposal for integrating ethics into the ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-022-00746-3]
- 35. Ethical challenges and solutions in AI-driven medical data ... [https://link.springer.com/article/10.1007/s44163-025-00266-0]
- 36. Ethics and Innovation: Artificial Intelligence and Genomics ... [https://jaacapconnect.org/article/143206-ethics-and-innovation-artificial-intelligence-and-genomics-in-child-psychiatric-risk-and-intervention]
- 37. Embedding ethical and legal principles in AI-driven clinical ... [https://www.sciencedirect.com/science/article/pii/S2666659625000290]
- 38. 14 Real AI Bias Examples & Mitigation Guide [https://www.crescendo.ai/blog/ai-bias-examples-mitigation-guide]
- 39. Bias in AI [https://www.chapman.edu/ai/bias-in-ai.aspx]
- 40. Addressing AI bias: a human-centric approach to fairness [https://www.ey.com/en_us/insights/emerging-technologies/addressing-ai-bias-a-human-centric-approach-to-fairness]
- 41. Algorithmic bias in public health AI: a silent threat to equity in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12325396/]
- 42. Groundbreaking Fairness Evaluation Dataset From ... [https://ai.sony/articles/Groundbreaking-Fairness-Evaluation-Dataset-From-Sony%20AI%20/]
- 43. Building AI Fairness by Reducing Algorithmic Bias [https://tepperspectives.cmu.edu/all-articles/building-ai-fairness-by-reducing-algorithmic-bias/]
- 44. Comprehensive Guide to AI Fairness and Bias Mitigation [https://sparkco.ai/blog/comprehensive-guide-to-ai-fairness-and-bias-mitigation]
- 45. Bias in AI: Examples and 6 Ways to Fix it [https://research.aimultiple.com/ai-bias/]
- 46. Evaluating accountability, transparency, and bias in AI ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-025-01243-z]
- 47. 50+ Must-Know Statistics on Bias in AI for 2025/26 [https://www.aiprm.com/bias-in-ai/]
- 48. Crucial Concepts in AI: Transparency and Explainability [https://www.f5.com/company/blog/crucial-concepts-in-ai-transparency-and-explainability]
- 49. BIOETHICS IN THE CONTEMPORARY CONTEXT ... [https://oapub.org/soc/index.php/EJSSS/article/view/1119]
- 50. Bioinformatics Pipeline Troubleshooting [https://www.meegle.com/en_us/topics/bioinformatics-pipeline/bioinformatics-pipeline-troubleshooting]
- 51. Privacy in the Age of Medical Big Data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6376961/]
- 52. Informed Consent, Redefined: How AI and Big Data Are ... [https://petrieflom.law.harvard.edu/2025/04/11/informed-consent-redefined-how-ai-and-big-data-are-changing-the-rules/]
- 53. AI accountability [https://carnegiecouncil.org/explore-engage/key-terms/ai-accountability]
- 54. AI Vendor Liability Squeeze: Courts Expand Accountability ... [https://www.joneswalker.com/en/insights/blogs/ai-law-blog/ai-vendor-liability-squeeze-courts-expand-accountability-while-contracts-shift-r.html?id=102l4ta]
- 55. 7 actions that enforce responsible AI practices [https://www.huronconsultinggroup.com/insights/seven-actions-enforce-ai-practices]
- 56. Responsible AI – Accountability [https://infusedinnovations.com/blog/responsible-ai-accountability]
- 57. When intelligent systems fail: a case study in AI liability and ... [https://www.taylorwessing.com/en/insights-and-events/insights/2025/10/ai-disputes-in-action---when-intelligent-systems-fail]
- 58. Lessons Learned from a Research in Health Equity Symposium [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399814/]
- 59. Writing Strong Research Questions | Criteria & Examples [https://www.scribbr.com/research-process/research-questions/]
- 60. How to Write a Research Question for 2026: Types, Steps, ... [https://research.com/research/how-to-write-a-research-question]
- 61. Types of Research Questions - Literature Searching [https://libguides.umn.edu/c.php?g=1337354&p=9854776]
- 62. Ethical Considerations for Interdisciplinary Collaboration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5459773/]
- 63. Can We Trust AI Benchmarks? An Interdisciplinary Review ... [https://ojs.aaai.org/index.php/AIES/article/view/36595]
- 64. Global Bioethics: Addressing Current Challenges ... [https://www.intechopen.com/chapters/1217243]
- 65. Bioethics at the intersection of politics, society, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12231874/]
- 66. Human Research Question and Answer Guide [https://research.uky.edu/office-research-integrity/faqs/human-research-question-answer-guide]
- 67. Back to the basics: guidance for formulating good research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11129835/]
- 68. A Review of How Different Views on Ethics Shape ... [https://link.springer.com/article/10.1007/s10796-025-10596-0]
- 69. Redesign 2025 – Tiles – Draft 4 – Embedded EthiCS @ Harvard [https://embeddedethics.seas.harvard.edu/draft-modules-redesign-2025-tiles-draft-4/]
- 70. Navigating real-world challenges: A case study on ... [https://www.sciencedirect.com/science/article/pii/S2153353925000501]
- 71. Machine Learning and Radiogenomics: Lessons ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2018.00228/full]
- 72. High-level summary of the AI Act [https://artificialintelligenceact.eu/high-level-summary/]
- 73. AI Act | Shaping Europe's digital future - European Union [https://digital-strategy.ec.europa.eu/en/policies/regulatory-framework-ai]
- 74. An Introduction to the Code of Practice for General ... [https://artificialintelligenceact.eu/introduction-to-code-of-practice/]
- 75. EU AI Act 2025 Update: GPAI Rules & Compliance [https://digital.nemko.com/insights/eu-ai-act-rules-on-gpai-2025-update]
- 76. EU AI Act Compliance Checker | EU Artificial Intelligence Act [https://artificialintelligenceact.eu/assessment/eu-ai-act-compliance-checker/]
- 77. Research integrity in the era of artificial intelligence [https://pmc.ncbi.nlm.nih.gov/articles/PMC11224801/]
- 78. Cross-Cultural Ethical Standards → Term [https://pollution.sustainability-directory.com/term/cross-cultural-ethical-standards/]
- 79. Exploring Ethical, Cultural, and Transnational Competence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11910911/]
- 80. Cross-Cultural Ethical Practices: Challenges and Best ... [https://www.jointhecollective.com/article/cross-cultural-ethical-practices-challenges-and-best-practices/]
- 81. PGBC 2025 - Disruption in Bioethics - Call for abstracts [https://ime-uk.org/pgbc-2025-disruption-in-bioethics-call-for-abstracts/]