Agape Love as a Foundational Ethic in Christian Medical Practice and Research
This article explores the concept of agape love—a selfless, neighbor-regarding love—as a foundational principle for Christian medical ethics.
Agape Love as a Foundational Ethic in Christian Medical Practice and Research
Abstract
This article explores the concept of agape love—a selfless, neighbor-regarding love—as a foundational principle for Christian medical ethics. Tailored for researchers, scientists, and drug development professionals, it examines the theological and philosophical underpinnings of agape, its practical application in clinical and research settings, common challenges in its implementation, and its relationship with secular ethical frameworks. The analysis aims to provide a robust resource for integrating this virtue ethic into the complex decision-making processes of modern biomedical science, arguing that agape offers a unique, person-centered approach that complements and enriches principle-based bioethics.
Defining Agape: The Theological and Philosophical Bedrock of Christian Medical Ethics
The exploration of agape love—a selfless, sacrificial, and unconditional form of love—is central to Christian ethical frameworks, particularly in demanding fields like medical ethics and drug development research. This analysis traces the theological trajectory from the historical narrative of King Ahab in the Old Testament, who embodies a profound deficiency of this virtue, to the ultimate expression of agape in Christ's sacrifice. Ahab's reign (c. 874–853 BC) [1] [2] provides a powerful case study of leadership and personal morality divorced from agape principles, characterized by self-interest, injustice, and the rejection of prophetic correction. By examining Ahab's failures and contrasting them with the New Testament's definition of divine love, researchers can establish a robust biblical foundation for an agape-based ethic. This foundation is essential for guiding professional conduct in high-stakes scientific environments, where decisions profoundly impact human health and well-being.
Historical and Biblical Analysis of King Ahab
The Reign and Character of King Ahab
King Ahab, the son of Omri, reigned over the northern kingdom of Israel for 22 years. His reign is historically attested in extra-biblical sources, such as the Kurkh Monoliths of the Assyrian king Shalmaneser III, which record Ahab's contribution of 2,000 chariots to the coalition that fought the Assyrians at the Battle of Qarqar in 853 BC [1]. Biblically, his rule is depicted as a period of significant moral and spiritual decline. The author of 1 Kings states that "Ahab son of Omri did more evil in the eyes of the LORD than any of those before him" (1 Kings 16:30, NIV) [3].
His marriage to Jezebel, the daughter of the Sidonian king Ethbaal, was a pivotal political alliance that had deep religious consequences [1] [2]. Under her influence, Ahab actively sponsored the worship of the Canaanite god Baal and the goddess Asherah, erecting an altar and a temple for Baal in the capital city, Samaria [1] [2] [3]. This represented a direct abandonment of the worship of Yahweh and a state-sponsored move towards idolatry, which the biblical writers vehemently condemn.
Table: Key Aspects of Ahab's Reign as Described in 1 Kings
| Aspect of Reign | Description | Biblical Reference |
|---|---|---|
| Spiritual Standing | "Did more evil in the eyes of the LORD than any of those before him" | 1 Kings 16:30 |
| Major Political Alliance | Married Jezebel, daughter of King Ethbaal of Sidon | 1 Kings 16:31 |
| Primary Religious Failure | Served and worshiped Baal; built a temple and altar for Baal in Samaria | 1 Kings 16:31-32 |
| Character Flaw | Resisted prophetic correction; prone to moodiness and passivity | 1 Kings 18:17-18; 21:4-5 |
A Case Study in the Absence of Agape: The Naboth's Vineyard Incident
Ahab's character is most clearly revealed in the incident involving Naboth's vineyard (1 Kings 21) [1] [4] [3]. This episode serves as a powerful negative exemplar of agape love, demonstrating the consequences of self-interest, covetousness, and a failure to uphold justice.
- Selfish Desire vs. Selfless Love: Ahab coveted the vineyard belonging to Naboth, which was adjacent to the royal palace. When Naboth refused to sell or trade his ancestral inheritance, citing Israelite covenant law, Ahab did not respect his rights. Instead, he prioritized his own desire for immediate gratification over the welfare and legal protections of his subject [3].
- Passivity and Complicity in Injustice: Ahab's response to Naboth's refusal was one of passive aggression. He "went home, angry and sullen because of Naboth's answer... He lay on his bed sulking and refused to eat" (1 Kings 21:4, NLT) [3]. This emotional withdrawal created a vacuum that his wife, Jezebel, filled with ruthless action. She orchestrated a false accusation and judicial murder of Naboth to seize the vineyard for Ahab [1] [4]. Ahab's failure to lead justly and his complicity in this evil act by accepting the stolen property stand in direct opposition to the active, protective nature of agape love.
- Rejection of Prophetic Correction: Following the murder of Naboth, God sent the prophet Elijah to confront Ahab. Elijah pronounced a divine judgment upon Ahab and his household for their wickedness (1 Kings 21:17-24) [1]. A genuine expression of agape love would involve repentance and a turn toward justice. While Ahab did momentarily display signs of humility and remorse (1 Kings 21:27), leading God to postpone the full measure of judgment, his overall pattern was one of resistance to the prophetic calls for change [1] [3].
The Theological Transition to Agape Love
Defining Agape Love
In contrast to Ahab's self-centeredness, the New Testament presents agape as the highest form of love. While ancient Greek had several words for love (e.g., eros for romantic love, philia for brotherly friendship), agape is distinct in its nature and origin [5] [6] [7].
- Unconditional and Sacrificial: Agape love is characterized by its unconditional nature. It is not based on the worthiness, attractiveness, or response of the recipient. It is a love that gives and sacrifices based on the will of the lover, not the merits of the loved one [8] [6]. This is perfectly modeled in Christ's death: "God demonstrates his own love for us in this: While we were still sinners, Christ died for us" (Romans 5:8, NIV) [6].
- Active and Willful: Unlike a fleeting emotion, agape is a deliberate act of the will. It is a conscious commitment to seek the highest good of another, manifested in action [6] [7]. As 1 John 3:18 states, "Let us not love with words or speech but with actions and in truth."
- Moral and Enduring: Agape love is inextricably linked to a strong moral character. It is described in 1 Corinthians 13 with attributes such as patience, kindness, and a refusal to delight in evil. It "always protects, always trusts, always hopes, always perseveres" (1 Corinthians 13:7, NIV) [9] [6].
Table: Contrasting Ahab's Actions with the Qualities of Agape Love
| Quality of Agape Love | Manifestation in Christ's Sacrifice | Deficiency in King Ahab |
|---|---|---|
| Sacrificial (John 15:13) | Gave his life for humanity while they were still sinners. | Sought his own comfort; allowed an innocent man (Naboth) to be killed for personal gain. |
| Just & Righteous | Fulfilled God's justice through a perfect sacrifice. | Perverted justice through false accusations and judicial murder. |
| Obedient to God | Submitted to the Father's will, even unto death. | Disobeyed God by worshiping Baal and rejecting prophetic warnings. |
| Patient & Forbearing | Is patient, not wanting anyone to perish. | Was sullen, angry, and impatient when his desires were thwarted. |
The Pinnacle of Agape: Christ's Sacrifice
Christ's sacrifice on the cross is the ultimate historical and theological expression of agape love. It serves as the definitive answer to the moral failure exemplified by Ahab. Where Ahab took life to gain a piece of property, Christ gave his life to gain reconciliation for humanity [6]. This act is the foundation of Christian ethics, establishing a new paradigm for human relationships and moral reasoning. For researchers and medical professionals, this model mandates a commitment to the welfare of others that transcends personal convenience, financial incentive, or professional prestige. It calls for a sacrificial dedication to the patient's good, mirroring the self-giving love of Christ.
Agape Love as a Foundational Ethic for Research and Medicine
From Biblical Theology to Ethical Framework
The transition from the Ahab narrative to an agape-based ethical framework requires translating theological concepts into practical principles for scientific and medical practice. Agape love, as "neighbor-regarding love for others" that makes no distinction "between worthy and unworthy, friend and enemy," provides a robust foundation for the core principles of modern medical ethics [10].
This love moves beyond sentiment to become an active, guiding force. It demands non-maleficence by refusing to harm, beneficence by actively promoting good, justice by advocating for the vulnerable, and autonomy by respecting the God-given dignity of every person. In the context of drug development, this could manifest as a steadfast commitment to patient safety over profit, the inclusion of diverse populations in clinical trials to ensure equitable access to therapies, and a transparent communication of risks and benefits.
Practical Application: The Researcher's Toolkit
Integrating agape love into a research environment involves cultivating specific virtues and practices that align with this core ethic.
Table: Research Reagent Solutions for Cultivating an Agape Ethic
| Essential 'Reagent' | Function in Ethical Practice |
|---|---|
| Agape Motivation | Serves as the foundational catalyst for all actions, driving the researcher to prioritize patient welfare above self-interest. |
| Longsuffering (Makrothumia) | Provides the "long wick" needed for patient, persistent work through research setbacks and complex problems without giving up. [7] |
| Prophetic Confrontation | Acts as a corrective agent, allowing and encouraging colleagues to ethically challenge unsafe practices or biased interpretations of data. |
| Justice & Righteousness | Functions as a standard buffer, ensuring that all research protocols and outcomes are applied fairly and equitably across all patient populations. |
| Self-Sacrifice | Serves as the binding agent, enabling the researcher to willingly invest extra time and resources to ensure thoroughness and integrity. |
Conceptual Framework Linking Ahab Narrative to Agape Love
The biblical and historical journey from King Ahab to Christ's sacrifice delineates a critical ethical evolution: from self-serving leadership to self-giving love. Ahab's story serves as a perpetual warning of the societal and personal decay that ensues when power is divorced from agape love. In contrast, Christ's sacrifice establishes agape as the non-negotiable foundation for all Christian moral reasoning. For researchers, scientists, and medical professionals, this agape ethic provides a transformative framework. It calls for a commitment to rigorous, compassionate, and just scientific practice that mirrors the unconditional, sacrificial love of God. By rooting their work in this ethic, they can ensure that their contributions to human health are not only technically proficient but also morally profound, embodying the highest calling of their vocation.
This whitepaper provides a technical analysis of the four distinct Greek concepts of love—agape, eros, philia, and storge—within the framework of Christian medical ethics. While all four loves represent valid forms of human relationship, agape love stands apart as a uniquely theological and ethical concept characterized by unconditional, self-sacrificial commitment to the good of the other. This paper examines the defining attributes of each love, establishes a comparative framework for ethical application, and explores how agape love serves as a foundational presupposition for clinical decision-making, patient care, and biomedical research. Particular attention is given to agape's role in resolving ethical tensions in organ transplantation, end-of-life care, and the physician-patient relationship where other forms of love may prove insufficient or problematic.
Within Christian theological anthropology, human persons are created for relationship, with love constituting the fundamental mode of this relationality. The New Testament utilizes four distinct Greek terms to describe the multifaceted reality of love, each with specific characteristics, objects, and ethical implications. Understanding this taxonomy is essential for constructing a robust Christian bioethics, as different forms of love inform different aspects of medical practice and research.
The English word "love" suffers from significant semantic overload, being applied to relationships with God, spouses, friends, family, country, and even food. This conceptual ambiguity creates ethical confusion when applied to complex medical contexts. The Greek linguistic framework provides precise terminology to navigate these complexities: agape (unconditional, self-sacrificial love), philia (friendship love), eros (romantic love), and storge (familial affection) [11]. Christian medical ethics recognizes the proper place for each while acknowledging agape as the transcendent form that informs and sanctifies the others.
The fundamental thesis of this whitepaper is that agape love provides a unique ethical foundation for medical practice and research that cannot be reduced to or derived from other forms of love. Its distinctive characteristics—unconditional commitment, willful intentionality, and self-sacrificial orientation—make it particularly suited to address the vulnerability, dependency, and ethical challenges inherent in healthcare contexts [12].
Defining the Four Loves: Core Characteristics and Distinctions
Agape: Unconditional, Self-Sacrificial Love
Agape represents the highest form of love in Christian scripture, distinguished by its unconditional nature and intentional commitment to the good of the other, regardless of merit or reciprocity [6]. Unlike other loves that arise from emotional attraction or natural affinity, agape is primarily volitional rather than emotional, embodying a deliberate choice to seek another's welfare [13].
The essence of agape is self-sacrificial giving, most perfectly exemplified in Christian theology by God's sacrifice of His Son (John 3:16) and Christ's death for humanity [11] [14]. This love is not based on the worthiness or attractiveness of the recipient but flows from the character of the lover. As such, agape maintains its commitment even when feelings of affection wane or when the relationship becomes costly [13].
Key characteristics of agape love include:
- Unconditional nature: It is given freely, not contingent upon the qualities, actions, or response of the recipient [15]
- Self-sacrificial orientation: It willingly sacrifices self-interest for the benefit of others [14]
- Volitional commitment: It operates as an act of the will rather than being primarily emotion-driven [13]
- Moral character: It possesses ethical qualities and obligations distinct from other loves [13]
- Divine source: It originates from God's nature (1 John 4:8) and is poured into human hearts through the Holy Spirit (Romans 5:5) [6]
In medical ethics, agape provides the foundation for benevolence—the steadfast commitment to patient welfare regardless of patient characteristics, social value, or ability to reciprocate [12].
Eros: Romantic, Passionate Love
Eros refers to romantic or passionate love characterized by desire, attraction, and intimacy between partners [11]. This love encompasses the physical, emotional, and spiritual dimensions of romantic attraction and finds its proper expression within the covenant of marriage [15].
Unlike agape, which seeks to give, eros naturally seeks fulfillment through union with the beloved. While sometimes misconstrued as merely sexual attraction, authentic eros within marriage includes but transcends physical intimacy, representing a profound longing for complete union with another person [11].
In biblical literature, eros is celebrated in Song of Solomon, where the bride and groom exchange passionate declarations of love (Song of Solomon 1:2), and in Proverbs, which encourages spouses to "be intoxicated always in her love" (Proverbs 5:18-19) [11]. When informed and sanctified by agape, eros becomes more than mere desire—it becomes a committed, self-giving orientation toward one's spouse.
Philia: Friendship and Brotherly Love
Philia refers to the affectionate bond between friends, characterized by mutual affection, trust, camaraderie, and shared values [11] [15]. This love operates on the basis of reciprocity and common interests, flourishing within relationships of equality and mutual regard.
Biblical examples include:
- David and Jonathan: "the soul of Jonathan was knit to the soul of David, and Jonathan loved him as his own soul" (1 Samuel 18:1) [11]
- Jesus and his disciples: "I have called you friends" (John 15:15) [11]
- Early Christian community: "devoted themselves to the apostles' teaching and the fellowship" (Acts 2:42) [11]
Philia represents an essential component of human flourishing and community formation. In healthcare settings, philia manifests as the collegial relationships between healthcare professionals and the therapeutic alliances formed with patients [16].
Storge: Natural Familial Affection
Storge describes the natural affection and loyalty inherent in family relationships—between parents and children, siblings, and extended kin [11] [17]. This love is rooted in kinship bonds, shared experiences, and the familiarity developed through common life [15].
Biblical examples include:
- Jacob and Esau: Despite past conflict, Esau embraces Jacob and weeps upon their reunion (Genesis 33:4) [11]
- Ruth and Naomi: Ruth's devotion to her mother-in-law ("Your people shall be my people") demonstrates familial loyalty beyond blood ties (Ruth 1:16) [11]
- Mary and Jesus: Jesus' concern for his mother's welfare even during his crucifixion (John 19:26-27) [11]
Storge provides the natural foundation for caregiving within families, which forms the prototype for many healthcare relationships. The New Testament expands this concept to include the Christian community, urging believers to "be devoted to one another in love" using the compound word "philostorgos" (Romans 12:10) [18].
Table 1: Comparative Analysis of the Four Loves
| Characteristic | Agape | Eros | Philia | Storge |
|---|---|---|---|---|
| Primary Nature | Volitional, unconditional | Emotional, desire-based | Reciprocal, affinity-based | Instinctual, familiarity-based |
| Primary Object | All people, including enemies | Spouse/romantic partner | Friends, companions | Family members |
| Foundation | Commitment, sacrifice | Attraction, passion | Shared interests, values | Kinship, shared life |
| Biblical Examples | John 3:16; 1 Corinthians 13 | Song of Solomon; Proverbs 5:18-19 | David & Jonathan; Jesus & disciples | Ruth & Naomi; Mary & Jesus |
| Medical Ethical Application | Foundation of beneficence; care for difficult patients | Marital consent in healthcare decisions | Therapeutic alliance; professional collaboration | Family involvement in care decisions |
Agape Love as a Distinct Ethical Foundation in Medical Practice
Theological and Philosophical Distinctives of Agape
Agape love possesses several unique characteristics that distinguish it from other loves and make it particularly suited as a foundation for medical ethics:
3.1.1 Unconditional Regard Independent of Merit Unlike philia (which depends on shared values) or eros (which responds to desirable qualities), agape love is granted irrespective of the recipient's worthiness or characteristics [6]. This quality is essential in healthcare contexts where providers must care for patients regardless of their social status, personal characteristics, or role in their own illness.
3.1.2 Volitional Rather Than Emotional Foundation Agape operates as a "love of the will"—a conscious choice rather than being motivated primarily by emotional response [13]. This volitional character provides stability in long-term care relationships and in treating difficult patients where natural affection may be absent.
3.1.3 Source in Divine Nature Rather Than Human Capacity Christian theology identifies agape as originating in God's own nature (1 John 4:8) rather than emerging from human virtue [14]. This theological understanding acknowledges that sustaining such demanding love requires transcendent resources, particularly in emotionally draining healthcare environments [6].
3.1.4 Uniquely Christian Character Numerous scholars note that agape love represents a distinctive contribution of Christian revelation. As noted by the C.S. Lewis Institute, "No other approach gives a significant place to 'agape' or other-centered love" [14]. The radical notion that "God is love" finds no parallel in other religious systems, making agape a uniquely Christian contribution to ethics [14].
Agape Versus Alternative Ethical Foundations
Agape love provides a distinctive alternative to common ethical frameworks in healthcare:
3.2.1 Against Relativism: Agape as Grounded Moral Principle Unlike situational ethics which compromises moral principles when "love seems better served by doing so" [12], agape love operates within consistent moral boundaries. This protects against subjectivism where "love" becomes justification for any action based on individual preference [12].
3.2.2 Beyond Materialism: Agape as Transcendent Motivation Materialistic philosophies struggle to account for truly self-sacrificial love. As noted by evolutionary biologists, "disinterested altruism...is something that has no place in nature" from a purely materialistic perspective [14]. Agape thus provides a foundation for altruism in medicine that transcends biological determinism.
3.2.3 Contrasted with Other Loves: Agape as Supernatural Complement Agape does not eliminate other loves but transforms and completes them. In marriage, agape stabilizes eros when feelings fluctuate [13]. In professional relationships, agape extends philia beyond natural affinities. In family care, agape strengthens storge when resources are depleted.
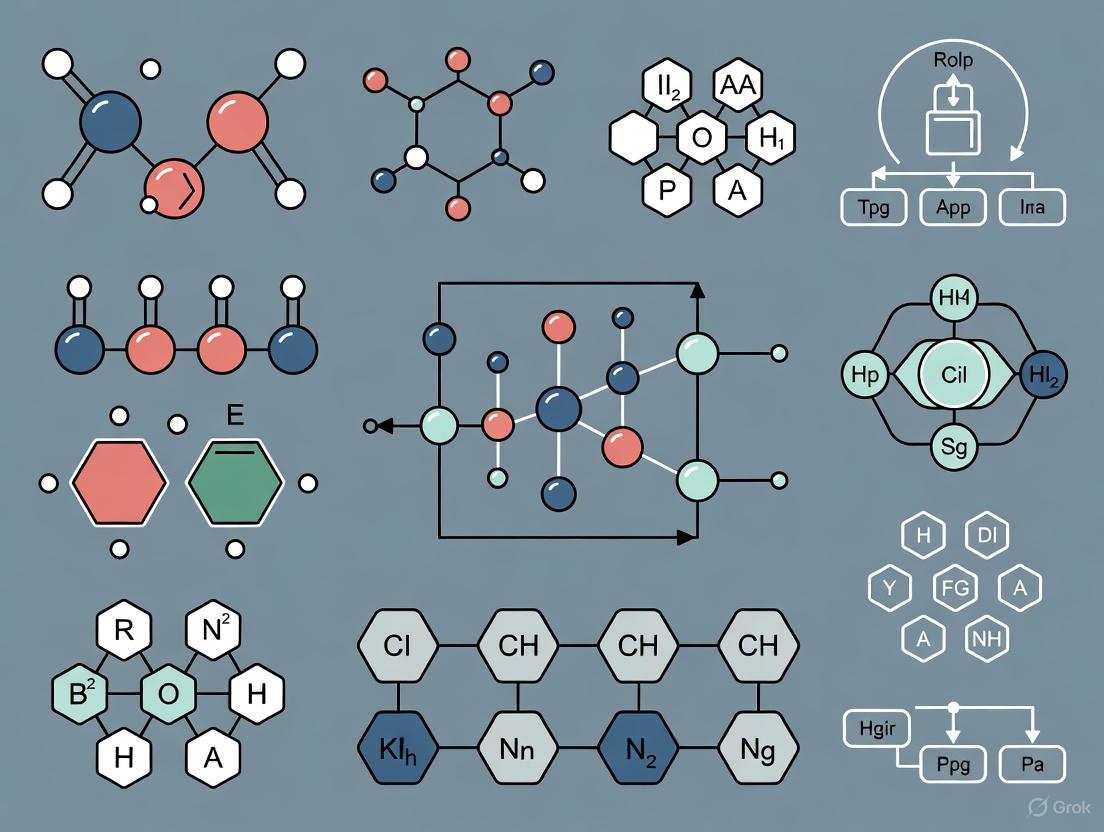
Diagram 1: Interrelationship of Loves in Medical Ethics
Applied Agape: Experimental Protocols and Research Methodologies
Research Protocol: Measuring Agape in Clinical Environments
4.1.1 Experimental Objective To quantify expressions of agapic behavior versus other love forms in clinician-patient interactions across diverse medical settings.
4.1.2 Methodology
- Setting: Tertiary care hospital with outpatient clinics, emergency department, and inpatient units
- Participants: 150 clinician-patient dyads (75 experimental, 75 control)
- Intervention: Ethics training emphasizing agape principles (experimental) versus standard ethics training (control)
- Measurement Tools:
- Behavioral Coding Scheme: Documented instances of:
- Agape indicators: Uncompensated time, care for hostile patients, sacrifice of personal convenience
- Philia indicators: Rapport-building, shared laughter, personal disclosure
- Storge indicators: Familial address patterns, protective behaviors
- Patient Surveys: Assess perceived commitment, trust, and unconditional regard
- Clinician Self-Reports: Measure motivations and emotional responses
- Behavioral Coding Scheme: Documented instances of:
4.1.3 Data Analysis Mixed-methods approach combining quantitative analysis of behavioral frequencies with qualitative analysis of interview data regarding motivational frameworks.
The Scientist's Toolkit: Research Reagents for Studying Agape
Table 2: Essential Methodological Frameworks for Love Research
| Research Tool | Function | Application in Love Studies |
|---|---|---|
| Motivational Analysis Framework | Distinguishes volitional from emotional motivations | Identifies agapic versus erotic/philic motivations in caregiving |
| Sacrificial Behavior Metrics | Quantifies cost-bearing actions | Measures agape through documented sacrifices (time, convenience, risk) |
| Unconditionality Index | Assesses consistency across patient characteristics | Tests agape stability with unappealing versus appealing patients |
| Virtue Ethic Assessment | Evaluates characterological foundations | Connects agape to virtue ethics versus principle-based approaches |
| Theological Anthropology | Provides metaphysical framework | Grounds agape in Christian concept of human dignity |
Case Study: Agape in Organ Transplantation Ethics
Organ transplantation presents a compelling case study for agape love in medical ethics. The practice inherently involves questions of sacrifice, gift-giving, and regard for strangers—all central to agape [19].
4.3.1 Agape as Ethical Foundation for Donation Living organ donation embodies agape principles when donors undergo significant risk and sacrifice with no medical benefit to themselves. This mirrors the agapic concept of "laying down one's life for another" (John 15:13) [15] [19]. Post-mortem donation similarly represents a final gift to strangers, extending care beyond natural affinities (storge) or relationships (philia).
4.3.2 Resolution of Ethical Tensions Agape love helps resolve key tensions in transplantation ethics:
- Between utility and dignity: Agape maintains respect for both donor and recipient while pursuing life-saving treatment [19]
- Between scarcity and need: Agape inspires equitable allocation systems that honor the sacrificial gift
- Between biological and spiritual: Agape affirms bodily resurrection without requiring physical intactness, addressing theological concerns [19]
4.3.3 Research Findings A 2025 study analyzing motivations of living organ donors found that those with explicit agapic frameworks (e.g., "I'm doing this because it's the right thing to do regardless of who receives it") demonstrated greater psychological resilience post-donation than those with primarily storgic motivations (family obligation) [19].
Diagram 2: Agape Love in Organ Transplantation Ethics
This technical analysis demonstrates that agape love provides a distinctive and essential foundation for Christian medical ethics that cannot be reduced to other forms of love. Its unique characteristics—unconditionality, volitional commitment, self-sacrificial orientation, and divine source—make it particularly suited to address the vulnerabilities and ethical challenges inherent in healthcare.
While eros, philia, and storge each contribute valuable dimensions to human flourishing and medical relationships, they remain subject to natural limitations—fluctuating emotions, reciprocal expectations, and familial boundaries. Agape love transcends these limitations, providing a stable ethical foundation for caring for the unappealing patient, making sacrificial professional commitments, and maintaining moral boundaries when other motivations fail.
For biomedical researchers and healthcare professionals, recognizing this distinction has practical implications. Ethics education should explicitly cultivate agapic motivations alongside technical competencies. Institutional policies should create environments where agapic commitments can flourish without being exploited. Research methodologies should develop more sophisticated tools for quantifying and studying agape's impact on patient outcomes and professional satisfaction.
Ultimately, agape love represents Christianity's unique contribution to medical ethics—a vision of care grounded not in contractual obligation, emotional affinity, or biological impulse, but in steadfast, willful commitment to the good of the other, reflecting the character of God Himself. As such, it deserves not only theoretical consideration but practical implementation across the spectrum of biomedical research and clinical practice.
In the field of Christian medical ethics, agape love serves as a foundational principle for guiding moral reasoning and clinical practice. This whitepaper delineates the three core characteristics of agape—selflessness, sacrifice, and unconditional regard—and explores their operationalization within biomedical contexts. Agape, distinct from other forms of love, is defined as a deliberate, neighbor-regarding love that makes no distinction between the worthy and unworthy, friend and enemy [10]. It provides a robust theological foundation for the secular ethical principles common in modern medicine, arguing that what the medical community often views as non-judgmental care finds its deepest justification in this Christian ethic [10].
The analysis is situated within the virtue ethics framework, which prioritizes the moral character of the individual over rigid adherence to rules or mere calculation of outcomes [20]. This approach asserts that right action in complex bioethical dilemmas flows from a character formed by the virtue of charity, or benevolent love [20]. By examining the theoretical underpinnings, empirical correlates, and practical applications of agape's core characteristics, this paper provides researchers and clinicians with a structured, interdisciplinary understanding of its significance for ethical medical practice.
Theoretical Foundations in Christian Ethics
The concept of agape love is deeply rooted in Christian Scripture and tradition, fundamentally shaping its application in bioethics. The biblical commandment to love God and neighbor as oneself lies at the heart of Christian ethics and provides the normative content for agape [21]. This love is not primarily an emotion but a habitual inward disposition to act, feel, and think in morally good ways, cultivated through practice and grace [20].
Selflessness (Agape as Kenosis): Agape is characterized by self-emptying, modeled on Christ's kenosis (self-emptying) in Philippians 2:5-8. It is an all-giving, selfless love that seeks the good of the other without regard for personal cost or merit [22] [20]. In medical practice, this translates to a consistent focus on the patient's welfare, setting aside the physician's personal biases, prejudices, or financial interests [10].
Sacrifice (Agape as Action): Agape finds its ultimate expression in concrete action, most profoundly in sacrifice. The Gospel of John states, "Greater love has no one than this: to lay down one's life for one's friends" (John 15:13) [19]. This sacrificial principle underpins acts ranging from organ donation, viewed as a manifestation of Christian love and solidarity, to the daily sacrifices healthcare workers make for their patients [19]. The internal disposition of agape must be expressed through the external virtue of benevolence, the attitude of intending and doing good for others [20].
Unconditional Regard (Agape as Gift): Agape is granted unconditionally, not based on the recipient's perceived worthiness. It is a grace-based love that mirrors God's love for humanity [20] [10]. This characteristic provides a robust foundation for the non-judgmental care essential to medical ethics, mandating compassionate treatment for all patients regardless of lifestyle, beliefs, or social status [10]. This stands in stark contrast to relativistic approaches where "love" is defined solely by the recipient's subjective desires, a view critiqued as potentially harmful [20].
Table 1: Theological Foundations of Agape's Core Characteristics
| Core Characteristic | Theological Model | Key Scriptural Reference | Moral Expression |
|---|---|---|---|
| Selflessness | Kenosis (Self-emptying) | Philippians 2:5-8 | All-giving, selfless love (Agape) |
| Sacrifice | Voluntary Self-giving | John 15:13 | Laying down one's life for another |
| Unconditional Regard | Grace & Gift | Romans 5:8 | Love for enemy and unworthy |
A critical theoretical distinction exists between agape implemented through benevolence versus relativism. Situational ethics, a form of relativism, argues that love is the primary factor in moral decision-making and should be defined by the recipient's perceived needs, even if it requires setting aside ethical maxims [20]. A virtue ethics approach, however, contends that true love is guided by the confines of moral character and interdependent moral absolutes, not subjective desire alone. This ensures that "love" remains grounded in objective truth and the genuine good of the other [20].
Quantitative Analysis and Empirical Correlates
While agape is a theological virtue, its psychological and behavioral manifestations can be empirically studied. Research on attachment styles and love attitudes provides a quantitative lens through which to view relational dynamics relevant to agape's expression.
Love Attitudes and Their Correlates
The Love Attitudes Scale (LAS) categorizes six love styles, among which Agape is defined as a selfless, all-giving love [22]. Quantitative studies, particularly in populations like nursing students who are training for caring professions, reveal significant correlations between secure attachment and healthy love attitudes, while insecure attachment is linked to more possessive or pragmatic love styles.
Table 2: Correlation Analysis Between Attachment Styles and Love Attitudes
| Attachment Style | Self-Model | Other-Model | Correlated Love Attitude(s) | Correlation Direction |
|---|---|---|---|---|
| Secure | Positive | Positive | Storge (Friendship love) [22] | Positive |
| Preoccupied | Negative | Positive | Mania (Possessive, dependent love) [22] | Positive |
| Dismissive | Positive | Negative | Pragma (Logical, 'shopping list' love) [22] | Positive |
| Fearful | Negative | Negative | Mania (Possessive, dependent love) [22] | Positive |
Psychological and Neurobiological Underpinnings
The practice of agape love is associated with measurable positive health outcomes, which can be framed as a secondary benefit of this primary ethical obligation.
- Neurobiological Activation: Loving behaviors activate the neurotransmitter dopamine, associated with reward and stress reduction, and oxytocin, the "bonding hormone" that helps relieve anxiety [22].
- Mental Health and Well-being: Secure attachment, a foundation for healthy self-giving, is positively linked to life satisfaction and self-esteem, and negatively linked to depression, anxiety, and loneliness [22].
- Longevity and Health Behaviors: The experience of love, particularly in stable relationships, is associated with longer life and encourages individuals to prioritize their well-being [22].
These empirical findings suggest that a life oriented toward agape love, while potentially involving cost and sacrifice, is correlated with a foundation of psychological security and contributes to holistic health.
Experimental and Methodological Frameworks
Studying a virtue like agape requires innovative methodologies that bridge theology, social science, and medical ethics. The following section outlines a proposed experimental workflow and the necessary "tools" for this interdisciplinary research.
Research Workflow for Agape in Medical Ethics
The diagram below outlines a conjunctive methodology for investigating agape in bioethical contexts, integrating theoretical, empirical, and practical phases.
The Researcher's Toolkit: Key Methodologies and Instruments
To conduct rigorous research on agape in medical ethics, investigators should be familiar with the following key methodological tools and concepts.
Table 3: Essential Research Reagents and Methodologies
| Item / Concept | Category | Function / Definition | Application Example |
|---|---|---|---|
| Love Attitudes Scale (LAS) [22] | Psychometric Tool | Measures six love styles (Eros, Ludus, Storge, Pragma, Mania, Agape). | Quantifying agape attitudes in healthcare professional cohorts. |
| Relationship Scales Questionnaire (RSQ) [22] | Psychometric Tool | Assesses four adult attachment styles (Secure, Fearful, Preoccupied, Dismissive). | Investigating links between attachment security and capacity for selfless care. |
| Virtue Ethics Framework [20] | Philosophical Methodology | Focuses on the moral character of the individual rather than just acts or outcomes. | Grounding bioethical analysis in the cultivation of charitable character. |
| Benevolence [20] | Ethical Principle | The virtue of doing good; the active expression of charitable love. | Guiding clinical decisions to seek the patient's genuine good, distinct from subjective desire. |
| Case Study Analysis | Qualitative Method | In-depth examination of complex, real-world ethical dilemmas. | Analyzing how selflessness is navigated in cases of organ transplantation [19]. |
Application in Biomedical Contexts
The core characteristics of agape love translate into specific ethical orientations and practices within medicine and biomedical research.
Agape as a Guide for Clinical Practice and Research
- Championing the Vulnerable: Agape's unconditional regard mandates the protection of vulnerable populations in research and clinical trials, learning from historical atrocities like the Tuskegee studies [20]. It frames public bioethics as fundamentally concerned with human "vulnerability, dependence, frailty, and finitude" [20].
- Navigating Organ Transplantation: The Orthodox Christian stance on organ donation exemplifies a balanced application of agape. It encourages organ donation as an act of Christian love and solidarity, yet calls for a careful approach that respects the sacredness of the body and the potential harm to the donor [19]. This represents a real-world balance of selfless giving with ethical caution.
- Informing Global Health Justice: Agape love, when understood as transformative political action, provides the moral impetus for addressing systemic inequalities in global health, pushing for equitable access to medical resources and care [21].
- Grounding Environmental Ethics: The "love for nature" extends the object of agape's regard to the non-human world, creating a Christian environmental ethic that acknowledges humanity's responsibility as stewards of creation [21].
The diagram below illustrates how the core characteristics of agape logically flow into foundational principles of modern medical ethics, providing them with a theological and motivational foundation.
Selflessness, sacrifice, and unconditional regard are not merely abstract ideals but are the core characteristics of agape love that provide a robust framework for Christian medical ethics. Grounded in theological virtue and expressed through the principle of benevolence, agpe offers a compelling alternative to both rigid legalism and subjective relativism in bioethical reasoning. By integrating theoretical understanding with empirical study and practical application, medical researchers and practitioners can cultivate a professional ethic that faithfully embodies this foundational concept, ensuring that technological advancement and clinical care remain rooted in the unwavering commitment to love one's neighbor as oneself.
The concept of agape, or selfless neighbor-love, represents a cornerstone of Christian ethical thought. Within the specialized domain of medical ethics, this theological virtue transcends mere sentiment to become a foundational principle for moral reasoning and professional practice. This whitepaper examines the distinctive contributions of two pivotal 20th-century figures—theologian Paul Ramsey and activist-theologian Martin Luther King Jr.—in articulating and applying agape as a rigorous ethical norm. Their work, though developed in different contexts, converges on the conviction that agape provides a robust framework for understanding human dignity, obligation, and community in the face of complex moral challenges.
For researchers, scientists, and drug development professionals, this exploration offers a critical resource. It delineates how a values-based framework, rooted in the concept of agape, can inform and enrich the ethical deliberation inherent to healthcare innovation and clinical practice. By understanding the theoretical underpinnings and practical implications of agapeic ethics, professionals can better navigate the moral dimensions of their work, from prioritizing research goals to engaging with patients and communities.
Theoretical Foundations of Agape
The ethical architecture of agape, as advanced by Ramsey and King, is built upon a specific theological and philosophical foundation. Understanding its core characteristics is essential for appreciating its application to medical ethics.
Defining Agape and Its Key Characteristics
Agape is distinguished from other forms of love, such as eros (passionate or desire-based love) or philia (friendship or brotherly love), by its particular qualities [23]. It is a disinterested, unconditional love that is directed toward the neighbor for their own sake, without expectation of return [24] [25] [26]. Ramsey described it as a "neighbor-regarding love" that "makes no distinction between worthy and unworthy, friend and enemy" [10].
The table below summarizes the core characteristics of agape that form the basis of this ethical framework.
Table 1: Core Characteristics of Agape Love
| Characteristic | Description | Theological/Ethical Significance |
|---|---|---|
| Disinterestedness | Expects nothing in return; not contingent on the recipient's worth or actions [24] [25]. | Establishes an objective moral obligation independent of subjective feelings or mutual benefit. |
| Unconditional | Bestowed regardless of the recipient's identity, status, or actions (friend/enemy, worthy/unworthy) [10]. | Grounds human dignity in something other than merit, performance, or social standing. |
| Other-Regarding | Primarily directed toward the well-being of the neighbor [26]. | Fosters an ethic of responsibility and care for the other, central to care-giving professions. |
| Community-Building (King) | Seeks to create, preserve, and enhance community [24] [25]. | Positions ethical action as a social force aimed at reconciliation and the creation of a "Beloved Community." |
| Value-Creating (King) | In reaching out, it imbues the object with value [25]. | Affirms and protects the intrinsic worth of every person, especially the vulnerable. |
Agape in Philosophical and Theological Context
The agapeic ethics of Ramsey and King consciously situate themselves against other ethical systems. Ramsey, for instance, critiqued situational ethics, which, while also emphasizing love, argued that moral rules could be set aside if love seemed better served by doing so [12]. Ramsey and others, like bioethicist Edmund Pellegrino, contended that this approach was dangerously unmoored from stable moral principles and the virtue of the individual [12]. Instead, agape is best expressed through the virtue of benevolence—a habitual disposition to do good that is shaped by moral character and principles [12]. This aligns with virtue ethics, which focuses on the character of the moral agent rather than solely on rules (deontology) or outcomes (utilitarianism) [12].
The following diagram illustrates the logical relationship between agape and other key concepts in Ramsey's and King's ethical frameworks.
The Ethical Work of Paul Ramsey
Paul Ramsey was a pioneering figure who brought theological ethics into direct conversation with the emerging field of bioethics. His work established agape as a fundamental norm for medical morality.
Ramsey's Core Formulation: Agape as Disinterested Neighbor-Love
At the heart of Ramsey's ethics is the concept of agape as a disinterested love of neighbor for her or his own sake [24] [26]. This love is not a mere emotion but a steadfast commitment to the other, rooted in the covenant faithfulness of God. For Ramsey, this implied that every human life is both a gift and a trust given by God [24]. This perspective has profound implications for medicine, framing the patient not as a problem to be solved but as a person to be honored, whose life has inviolable worth.
Ramsey's exploration of "covenant" was crucial in refining his account of the relation between love and justice [26]. Covenant faithfulness provides a stable, principled foundation for neighbor-love, moving it beyond mere feeling and grounding it in a relational obligation. In the clinical context, this translates to the physician's covenant with the patient—a faithful promise to always act for the patient's good, a concept later developed by bioethicist Edmund Pellegrino [12].
Application to Medical Ethics and Bioethics
Ramsey's thought provides a powerful framework for addressing core issues in medical morality. The following table outlines key methodological applications of his agapeic ethic.
Table 2: Methodological Applications of Ramsey's Agapeic Ethic in Medical Ethics
| Methodological Principle | Description | Implication for Research & Practice |
|---|---|---|
| The Patient as Person | Upholds the inherent dignity of patients, loved ones, and staff [24]. | Challenges utilitarian approaches that might sacrifice individual well-being for collective outcomes; mandates informed consent. |
| Covenant Fidelity | Emphasizes faithfulness and promise-keeping in the caregiver-patient relationship [26]. | Fosters trust and ensures that the patient's good remains the primary end of medicine, even in profit-driven environments. |
| Love Transforming Justice | Agape works through and transforms natural justice, ensuring care for the marginalized [26]. | Demands scrutiny of systemic health disparities and prioritizes equitable access to healthcare and the benefits of research. |
| Life as a Gift and a Trust | Recognizes human life as a sacred trust, not a commodity to be engineered [24]. | Imposes moral limits on technological manipulation of human life (e.g., certain genetic enhancements) and mandates care at all life stages. |
The Ethical Work of Martin Luther King Jr.
While Martin Luther King Jr. is renowned as a civil rights leader, his thought was deeply theological, and his theory of nonviolent social change was explicitly grounded in the Christian concept of agape.
King's Formulation: Agape as a Social and Transformative Force
King was profoundly influenced by Ramsey's work on agape, particularly the idea of disinterested neighbor-love [24] [25]. He integrated this with the concept of the Beloved Community—the ultimate goal of nonviolent activism, which is a global community in which reconciliation and justice prevail [24]. For King, agape was "the heartbeat of the moral cosmos" [25]—a redemptive force that loves both because of and in spite of the neighbor's qualities, thereby having the power to transform enemies into friends [25].
This love is not passive. It is a "very stern love" that organizes itself into collective action to confront injustice, taking on suffering without inflicting it [25]. King referred to this as a "dangerous and costly altruism" [25], which directly challenges complacency and systemic evil. He famously argued that we are "caught in an inescapable network of mutuality," meaning that our fates are intertwined, and our ethical responsibilities extend to all members of the human family [24].
Application to Public Health and Social Justice
King's agape-driven ethics provide a critical lens for evaluating public health and medical research. His focus on the Beloved Community and the "network of mutuality" forces a shift from a purely individualistic bioethics to one that considers communal and social responsibilities. It raises fundamental questions about how medical research and healthcare delivery can either build up or tear down human community.
This perspective makes the pursuit of health equity a moral imperative. Agape requires confronting the "deep health and health care disparities, and increased incidents of mortality that exist between communities divided along racial and socioeconomic lines" [24]. It challenges researchers and healthcare professionals to ask not only "what does it mean to value life at the end of life?" but also "what does it mean to value life before the end of life?" for those on the margins of society [24]. This principle is visualized in the workflow of King's agape-based social action below.
Agape in Contemporary Medical Ethics Research
The framework established by Ramsey and King continues to find resonance in modern healthcare, providing a robust foundation for values-based practice and inspiring concrete ethical action.
Agape as a Foundational Ethic for Clinical Practice
In contemporary secular medical spaces, the principle of non-judgmental care for all ill persons is widely accepted. Anna Berry argues that Ramsey's and King's concept of agape provides a "robust account" for why this is obligatory, forming "a lens through which to practice medicine" that undergirds modern principles of medical ethics [10]. This "neighbor regarding love for others" offers a deeper theological rationale for duties like beneficence and justice.
Recent research has begun to empirically investigate related concepts. A 2025 systematic literature review examined "humanitarian love"—a term used to capture the value of altruistic, non-erotic love in healthcare [27]. The review found that when healthcare professionals direct this love towards patients, it helps reduce feelings of burnout, emotional exhaustion, and compassion fatigue [27]. Furthermore, when directed towards themselves, it fosters positive emotions, enhancing their ability to provide high-quality care [27]. This suggests that the agapeic ethic, far from being a burdensome ideal, may be a vital component of sustainable and humane medical practice.
The Scientist's Toolkit: Key Conceptual Frameworks
For the researcher seeking to apply these principles, the following table details essential conceptual "reagents" derived from the agapeic ethics of Ramsey and King.
Table 3: Essential Conceptual Frameworks for Agape-Informed Research Ethics
| Conceptual Framework/Value | Function in Ethical Analysis | Key Proponent |
|---|---|---|
| The Patient as Person | Serves as a foundational axiom, ensuring that research protocols and clinical applications consistently uphold the inherent dignity of every human subject. | Ramsey [24] |
| Beloved Community | Functions as a guiding teleology, orienting the long-term goals of research and healthcare policy toward inclusion, reconciliation, and universal flourishing. | King [24] [25] |
| Network of Mutuality | Acts as a systemic lens, revealing the interconnectedness of human beings and demanding that research consider broad social impacts and equitable distribution of risks/benefits. | King [24] |
| Covenant Fidelity | Provides a meta-ethical foundation, framing the researcher's and clinician's role as one of promise-keeping and faithful service to humanity, beyond mere contractual obligation. | Ramsey [26] |
| Love Transforming Justice | Serves as an operational principle, guiding the translation of the abstract ideal of love into concrete, fair policies and practices within institutions and systems. | Ramsey [26] |
The ethical work of Paul Ramsey and Martin Luther King Jr. demonstrates that agape is far more than a private religious virtue. It is a rigorous and demanding ethical norm capable of structuring moral reasoning in medicine and medical research. Ramsey's emphasis on covenant faithfulness and the patient as person provides a stable foundation for the clinical encounter and bioethical deliberation. King's vision of agape as a transformative, community-building force expands this foundation, compelling the field to address systemic injustice and to work toward a healthcare ecosystem that reflects the "Beloved Community."
For researchers, scientists, and drug development professionals, engaging with this tradition offers a profound opportunity. It challenges the reduction of bioethics to a mere set of procedural rules or cost-benefit analyses. Instead, it calls for an ethic rooted in the unconditional acknowledgment of human dignity, a commitment to the common good, and the pursuit of justice. In an era of rapid technological advancement and persistent health disparities, the synthesis of Ramsey's and King's thought on agape love remains an indispensable resource for guiding innovation toward truly humane ends.
Within the framework of Christian medical ethics, the concept of agape love provides a profound foundation for understanding human life as both a gift from God and a sacred trust. This whitepaper explores the implications of this foundation for a sanctity of life ethic, particularly as it guides researchers, scientists, and drug development professionals. The perception of life as a gift and trust confers inviolable dignity and immeasurable worth on every human being, irrespective of stage, state, or condition [28]. This conviction directly shapes ethical decision-making in biomedical research, demanding that practices honor the intrinsic value of the human person, from the earliest stages of life to its natural end.
Agape love, characterized as non-preferential, self-giving, and willful delight in the other, operates as a fundamental moral norm within Christian ethics [5] [6]. It is not merely an emotion but a determined act of the will, a joyful resolve to put the welfare of others above one's own [6]. When applied to the biomedical field, this love ethic necessitates a commitment to uphold the sanctity of life even—and especially—when such a commitment challenges research efficiency, economic pressures, or prevailing cultural norms.
Theological and Philosophical Foundations
Human Life as a Created Gift
The starting point for a Christian anthropology relevant to bioethics is the doctrine of creation. The belief that "God created mankind in his own image" (Gen 1:27) establishes the surpassing dignity and value of every human life [29] [30]. This divine image (Imago Dei) is not contingent upon an individual's characteristics, capabilities, or social utility; it is a privileged status conferred upon all humanity by the Creator [30] [31]. As articulated in the Apostles' Creed, this understanding is deeply personal: God is the active creator and sustainer of each individual, providing "my body and soul, eyes, ears, and all my members, my reason and all my senses" [31]. This relationship is fundamentally one of grace: God is the giver, and humanity is the recipient.
This worldview stands in stark contrast to atheistic materialism, which reduces the human person to "nothing more than the behavior of a vast assembly of nerve cells and their associated molecules" [31]. The metaphysical assertion of humanity's created purpose is the bedrock for resisting the objectification of human beings in research and medicine. Human life is not an aimless biological accident but is endowed with a telos—a purpose to live in perfect fellowship with God [31]. This inherent purpose confers a value that transcends human capacity to measure [28].
The Stewardship Model of Life as a Trust
If human life is a gift, then it is also a trust. The concept of stewardship flows directly from the recognition that "You are not your own; you were bought at a price. Therefore honor God with your bodies" (1 Corinthians 6:19-20) [32]. God is the "Lord of life from its beginning until its end," and therefore, "no one can under any circumstance claim for himself the right directly to destroy an innocent human being" [29]. This understanding positions researchers and clinicians not as ultimate masters of human life, but as responsible stewards who are accountable to God for how they treat the object of His love.
This stewardship model has direct implications for medical ethics. It challenges the notion of absolute autonomy, instead framing human authority over life as a delegated and limited trust. The body and life itself are understood as property on loan from God, and as such, must be treated with reverence and respect [32]. This perspective provides a powerful basis for opposing practices that directly destroy innocent human life but also for guiding the ethical development of new therapies, where the question is not merely "Can we?" but "Ought we?".
Agape Love as the Normative Framework for Bioethics
Agape love is the active expression of the sanctity of life ethic. Distinguished from erotic love (eros) or friendship (philia), agape is universal, unconditional, and motivated by the interest and welfare of all others [5]. It is a love that is chosen and cultivated, often requiring a conscious decision to act for the good of another, regardless of their characteristics or one's personal feelings [5] [32].
In the context of medical research, agape love manifests as a commitment to the principle of neighbor-welfare, which always treats humanity as an end in itself and never as a mere means to an end [32]. This stands in critical tension with utilitarian approaches that might justify compromising the well-being of a few for the benefit of the many. For the Christian researcher, agape love is not sufficient as the only source of ethics in a way that bypasses other moral norms; rather, it is the fulfilling spirit of the moral law, which includes upholding the sanctity of life as a divine command [32]. Agape love, properly understood, will therefore never violate the intrinsic dignity of a human person, because to do so would be a failure to love both the neighbor and the God who created and redeemed that neighbor.
Table 1: Core Concepts of Agape Love in Christian Ethics
| Concept | Definition | Implication for Biomedical Research |
|---|---|---|
| Universal Scope | Love extends to all people, regardless of relationship or merit [5]. | The ethical protection of research subjects must be universal, inclusive of embryos, the cognitively disabled, and other marginalized groups. |
| Active Benevolence | Love is a willful commitment to the good of the other, demonstrated by action [6]. | Ethics moves beyond non-maleficence to a proactive commitment to the flourishing of research subjects and patients. |
| Non-Preferential | Love is not based on desirable characteristics of the recipient [5]. | The value of a research subject is not determined by their intelligence, physical ability, or potential contribution to society. |
| Source in God | God's nature is love, and human agape is a response to His prior love [6] [31]. | The motivation for ethical research is not merely compliance, but a response to the grace and love of God. |
Practical Applications in Research and Drug Development
Ethical Challenges in Novel Therapeutic Development
The development of novel therapeutics, particularly for rare diseases, presents growing tensions between the desire to accelerate patient access to breakthrough therapies and the need to generate robust evidence of safety and efficacy [33]. Accelerated approval pathways, while addressing urgent patient needs, create specific ethical challenges that must be navigated through the lens of the sanctity of life and agape love.
Vulnerable patient populations, desperate for treatment, may overestimate benefits and underestimate risks, compromising the integrity of informed consent [33]. From a sanctity of life perspective, this challenges researchers to exercise exceptional care in communicating the true state of evidence, protecting patients from false hope or unproven claims. Furthermore, agape love demands a keen attention to equity in access to experimental therapies. These therapies often favor "a motivated, informed, and well-connected subset of the patient population," exacerbating existing injustices [33]. A commitment to universal love requires actively working to make access fair and inclusive.
The following diagram illustrates the key ethical tensions and commitments arising at the intersection of agape love and drug development.
Agape-Inspired Responses to Ethical Challenges
In the face of these challenges, an ethic grounded in the sanctity of life and agape love proposes tangible strategies and commitments.
- Reinforcing Informed Consent as a Covenantal Act: The consent process should be understood not as a mere legal transaction but as a communication of respect for the patient's God-given autonomy and intellect. This involves creating comprehensible materials, allowing ample time for questions, and openly acknowledging the limitations of the available data, especially in accelerated approval contexts [33].
- Advocating for Inclusive Trial Design and Access: Agape love's universal scope compels researchers and companies to design trials that are as inclusive as possible, minimizing barriers for disadvantaged populations. Furthermore, it advocates for pricing and reimbursement models that ensure life-saving therapies are accessible, not just to the wealthy or well-insured, but to all who need them [33].
- Maintaining a Commitment to Scientific Rigor: The stewardship of patient trust and well-being requires a steadfast commitment to generating high-quality evidence. While accelerated pathways are valuable, the ultimate goal is therapies that are both safe and effective. Agape love does not settle for "good enough" when patient lives are at stake but pursues the highest standards of scientific excellence as an expression of love for neighbor.
Table 2: Ethical Challenges and Agape-Informed Mitigation Strategies in Drug Development
| Ethical Challenge | Description | Agape-Informed Mitigation Strategy |
|---|---|---|
| Compromised Informed Consent | Patients/caregivers may overestimate benefit and minimize risk due to vulnerability and lack of treatment options [33]. | - Implement enhanced consent protocols with independent patient advocates.- Use plain-language, visual aids to communicate uncertainty and evidence quality. |
| Health Equity Concerns | Access to novel therapies often favors motivated, informed, and well-connected patients, exacerbating disparities [33]. | - Design clinical trials with inclusive enrollment criteria and logistical support.- Engage community representatives in trial design and planning. |
| Data Generation Under Acceleration | Accelerated approval may lead to drugs on the market with limited long-term safety and efficacy data [33]. | - Commit to robust post-market surveillance and long-term follow-up studies.- Maintain scientific integrity by resisting political or commercial pressure to overstate early findings. |
For the research professional seeking to operationalize the sanctity of life ethic, the following frameworks and concepts are essential tools.
Table 3: Essential Ethical Frameworks for the Research Scientist
| Framework/Concept | Function | Application in Research |
|---|---|---|
| Theological Anthropology | Provides a clear definition of the human person as a unity of body and soul, created in God's image with inherent dignity [29] [31]. | Serves as the foundational basis for all research ethics, guiding the treatment of human subjects, human biological samples, and human embryos. |
| The Sanctity of Life Ethic | The belief that all human beings, at every stage and in every condition, possess immeasurable worth and inviolable dignity [28]. | Demands the protection of human life from deliberate harm and underpins opposition to practices like abortion, embryo destruction, and euthanasia. |
| Agape Love Principle | The normative command to actively seek the welfare of all others, unconditionally and self-sacrificially [5] [6]. | Guides interpersonal conduct with research subjects and colleagues, and shapes the ultimate goal of research as service to human flourishing. |
| Stewardship Model | Recognizes that human life is a gift from God, held in trust, and that humans are accountable to God for their use of this gift [30] [32]. | Fosters a sense of responsibility and accountability in research, countering a "can we, therefore we should" technological imperative. |
The conceptualization of human life as a gift from God and a sacred trust provides a robust and transcendent foundation for the sanctity of life ethic within Christian medical ethics. When this foundation is animated by the principle of agape love—a willful, active, and universal commitment to the good of the other—it becomes a powerful guide for researchers, scientists, and drug development professionals. This ethic challenges the reduction of the human person to mere biological material or a means to a scientific end. It calls for a research culture characterized by profound respect, rigorous protection of the vulnerable, relentless pursuit of justice, and a stewardship that recognizes our ultimate accountability to the Giver of all life. In an era of rapid biomedical advancement, this worldview offers a critically needed compass for navigating the complex ethical terrain, ensuring that the pursuit of scientific progress remains firmly rooted in the service of human dignity.
From Principle to Practice: Implementing Agape in Clinical Care and Research Design
Agape, a selfless and sacrificial form of love, provides a robust theological and ethical framework for Christian healthcare professionals. This whitepaper explores the integration of agape love into medical practice, demonstrating its alignment with values-based practice (VBP) and its capacity to foster non-judgmental, culturally sensitive care. Through a systematic review of current literature and conceptual analysis, we establish that agape love enhances patient care and serves as a critical protective factor against burnout and compassion fatigue among providers. The paper presents practical methodologies for cultivating and applying agape, structured data on its impacts, and visual models for its operationalization, offering researchers and clinicians a definitive guide for implementing this core Christian ethic.
Within Christian medical ethics, the concept of agape love represents a foundational yet often underexplored principle for guiding clinical practice. Distinguished from other forms of love by its unconditional, self-giving, and sacrificial nature, agape is characterized by a deliberate commitment to the well-being of others without expectation of reciprocation [22]. This paper positions agape as a critical lens through which to view and enact non-judgmental care for all patients, aligning professional conduct with a biblical worldview that commands "love your neighbor as yourself" [19].
The modern healthcare landscape, with its emphasis on efficiency and technical proficiency, often marginalizes the relational aspects of care. This has led to a recognized gap in the healthcare literature, where the value of love is either overlooked or treated as a transgressive element, sometimes referred to as the "L" word [27]. However, a growing body of evidence suggests that what is systematically defined as humanitarian love—helping others, alleviating suffering, and promoting growth—has a tangible positive impact. When healthcare professionals direct this love towards patients, it helps reduce feelings of burnout, emotional exhaustion, and compassion fatigue [27]. Grounding this humanitarian imperative in the theological certainty of agape provides a powerful motivation for Christian practitioners, transforming a clinical duty into a sacred vocation.
This paper contends that agape love is not an abstract spiritual ideal but a practical, actionable principle that can be systematically integrated into values-based practice. It offers a framework for navigating complex patient interactions, particularly in situations involving diverse cultural backgrounds, deeply held personal beliefs, or conditions that might trigger bias. By defining agape, outlining its measurable outcomes, and providing concrete tools for its implementation, this guide aims to equip researchers and clinicians to embody this core Christian ethic in their professional lives faithfully.
Conceptual Framework: Defining Agape in a Healthcare Context
Agape in Theological and Psychological Context
Agape love occupies a distinct space in both theological and psychological typologies. Theologically, it is most clearly exemplified by Christ's sacrifice, embodying the principle that "greater love has no one than this: to lay down one's life for one's friends" [19]. This aligns with the agape love style defined by Lee (1973) and operationalized in the Love Attitudes Scale (LAS) as an all-giving, selfless love [22]. In healthcare, this translates to a commitment to act for the patient's good, prioritizing their needs and well-being above the provider's convenience, prejudice, or personal gain.
Psychologically, agape is characterized by several core attributes that distinguish it from other emotional states like empathy or compassion:
- Unconditional Regard: Agape extends care and respect regardless of a patient's background, lifestyle, or health choices. It is not contingent on the patient being "likable" or "compliant."
- Intentional Action: Unlike a fleeting emotion, agape is a conscious choice and a sustained commitment, often manifested through deliberate, caring behaviors [27].
- Sacrificial Commitment: It involves a willingness to expend personal resources—time, emotional energy, advocacy—for the patient's benefit, mirroring the Christian ethical teaching of selfless, sacrificial love for others [19].
Agape vs. Related Concepts in Clinical Practice
To avoid conceptual confusion, it is essential to differentiate agape from other valued qualities in healthcare.
- Agape vs. Empathy: While empathy involves understanding and sharing the feelings of another, agape goes further by committing to act for that person's good, even in the absence of shared feeling.
- Agape vs. Compassion: Compassion is the response to suffering coupled with a desire to help. Agape provides the underlying, sustained motivational foundation that makes compassion possible, even in the face of burnout.
- Agape vs. Professional Detachment: Professional detachment protects the clinician, but can sometimes lead to impersonal care. Agape offers a third way—engaged, personal care that is grounded in purpose rather than emotional fusion, thereby preventing exhaustion [27].
The following table summarizes these key distinctions for clarity and comparison.
Table 1: Distinguishing Agape from Other Clinical Concepts
| Concept | Definition | Primary Focus | Role in Healthcare |
|---|---|---|---|
| Agape Love | Selfless, sacrificial, and unconditional commitment to the good of another. | The patient's well-being, independent of reciprocation. | Foundational motivation for sustained, non-judgmental care. |
| Empathy | The ability to understand and share the feelings of another. | Affective and cognitive connection with the patient's experience. | Builds rapport and understanding; a component of patient-centered care. |
| Compassion | The recognition of and desire to alleviate another's suffering. | Responding to and reducing patient suffering. | Drives caring actions in response to immediate need. |
| Professional Detachment | Maintaining emotional distance to ensure objective judgment. | Self-protection and clinical objectivity. | Prevents burnout and poor judgment but risks impersonal care if over-emphasized. |
Agape in Practice: Operationalizing Love in Patient Care
The Psychosocial Impact and Protective Benefits
Empirical research underscores that integrating agape, or humanitarian love, into practice has significant benefits for both the patient and the healthcare professional. A systematic literature review found that humanitarian love fosters positive emotions in healthcare workers, enhancing their ability to provide high-quality care and effectively support patient needs [27]. Furthermore, directing this love towards patients is a protective factor, helping to reduce feelings of burnout, emotional exhaustion, and compassion fatigue among healthcare professionals [27]. This positions agape not merely as an ethical luxury but as a crucial component of sustainable clinical practice.
Practical Strategies for Cultivation and Application
Operationalizing agape requires translating the abstract concept into measurable behaviors and attitudes. The following methodologies provide a framework for its cultivation.
Methodology 1: Cultivating Cultural Humility through Self-Reflection Cultural humility is a practical expression of agape, emphasizing an interpersonal stance that is open to the patient's cultural identity [34]. It moves beyond the static goal of "cultural competence" and involves lifelong learning and self-critique.
- Procedure: Implement a structured self-reflection protocol following complex or ethically fraught patient encounters. Practitioners should document their initial judgments, identify potential biases based on patient characteristics (e.g., accent, health literacy, lifestyle), and consciously reframe their perspective to prioritize the patient's self-understanding and values.
- Application: This practice aligns with the biblical exhortation to "in humility value others above yourselves, not looking to your own interests but each of you to the interests of others" (Philippians 2:3-4) [34]. It minimizes cultural superiority and makes space for the patient's expertise on their own life.
Methodology 2: Conscientious Practice and Trust-Building Agape love is expressed through conscientious practice—meticulous, honest, and integrity-filled care [34]. This builds trust, which is essential for a therapeutic relationship.
- Procedure: Focus on consistent, reliable actions: using plain language, actively listening without interruption, following through on promises, and demonstrating respect for patient autonomy in all interactions.
- Application: This strategy directly fulfills the Christian principle of treating patients as we would want to be treated [34]. Trust is the tangible outcome of selfless, consistent action.
Methodology 3: Implementing a Values-Based Practice (VBP) Framework VBP is a sister framework to Evidence-Based Practice that explicitly integrates the values of service users and healthcare professionals [27]. Agape serves as the foundational value within this framework.
- Procedure: In clinical decision-making, formally incorporate discussions about patient values alongside medical evidence. Use open-ended questions to explore what matters most to the patient, and consciously apply the principle of agape to navigate value conflicts, always seeking the course of action that best serves the patient's well-being as they define it.
- Application: This systematizes the Christian ethic of love, ensuring it is not an afterthought but a central component of the clinical reasoning process.
The following diagram illustrates the dynamic relationship between the cultivation of agape and its outcomes in clinical practice.
Research and Clinical Toolkit
For researchers aiming to study agape in clinical settings and for practitioners seeking to implement its principles, the following tools and frameworks are essential.
Table 2: Key Research Reagents and Methodological Tools
| Tool / Reagent | Function / Definition | Application in Research and Practice |
|---|---|---|
| Love Attitudes Scale (LAS) | A validated psychometric scale that measures six love styles, including Agape (all-giving, selfless love) [22]. | Quantifies the propensity for selfless love in healthcare professionals; can be used as a variable in correlation studies with patient outcomes or provider burnout. |
| Cultural Humility Framework | An interpersonal stance that is "open in relation to aspects of cultural identity that are most important to the patient" [34]. | Provides a qualitative and quantitative framework for assessing non-judgmental care and its development through interventions like training modules. |
| Values-Based Practice (VBP) | A process that engages with the experiences, principles, and moral beliefs of service users and professionals [27]. | Serves as an operational framework for integrating agape into clinical decision-making protocols and evaluating its impact on care quality. |
| Self-Reflection Protocols | Structured guides for critical self-assessment of one's judgments, biases, and actions following patient interactions. | A key intervention for cultivating agape; data from reflection journals can be coded and analyzed for qualitative research on attitude transformation. |
Data Synthesis and Analysis
The quantitative and conceptual data derived from the research tools above can be synthesized to provide a clear evidence base for the impact of agape love. The following tables summarize key findings and conceptual relationships.
Table 3: Documented Psychosocial Impacts of Humanitarian Love (Agape) on Health Professionals [27]
| Impact Domain | Documented Effect | Implication for Clinical Practice |
|---|---|---|
| Emotional Well-being | Fosters positive emotions and enhances the ability to provide high-quality care. | Agape is a sustainable source of professional fulfillment that counteracts cynicism. |
| Burnout & Fatigue | Reduces feelings of burnout, emotional exhaustion, and compassion fatigue. | Functions as a protective factor, promoting career longevity and consistent care quality. |
| Therapeutic Efficacy | Improves the ability to effectively support patient's most important needs. | Directly correlates selfless care with improved patient-centered outcomes. |
Table 4: Relating Agape Love to Foundational Christian Medical Ethics
| Christian Ethical Principle | Relationship to Agape Love | Practical Application in Clinical Care |
|---|---|---|
| Sanctity of Life [19] | Agape is the active expression of respect for the sacred worth of each individual. | Provides meticulous and respectful care to every patient, regardless of prognosis or social status. |
| Stewardship | Agape motivates the responsible and compassionate use of medical resources for the good of others. | Advocates for just resource allocation and provides cost-effective, necessary care. |
| Sacrificial Giving [19] | Agape is defined by self-giving, mirroring Christ's sacrifice. | Going beyond the minimum duty: spending extra time, providing emotional support, and advocating fiercely for patients. |
This whitepaper examines the empirical and theoretical debate between virtue ethics and situationism, arguing for the cultivation of benevolence as a robust character trait. Framed within Christian medical ethics, the thesis posits agape love as a foundational principle that enables healthcare professionals to develop cross-situational consistency in moral behavior. The analysis integrates contemporary psychological research, philosophical argumentation, and theological ethics to provide a robust framework for moral development in healthcare contexts, particularly relevant for researchers and drug development professionals facing complex ethical challenges.
Virtue ethics, with its origins in Aristotelian philosophy, emphasizes the cultivation of moral character traits, or virtues, as the foundation for ethical behavior. A virtuous agent acts from a "firm and unchangeable character," discerning what a situation calls for (e.g., compassion, honesty) and acting accordingly [35]. This view presupposes that individuals possess robust character traits—stable dispositions that produce consistent behavior across different situations [36].
Situationism, a challenge arising from empirical psychology, contends that this view of character is empirically untenable. Situationists argue that seemingly insubstantial situational factors often have a substantial, and sometimes disquieting, effect on behavior [35] [37]. The well-known "dime in the phone booth" experiment is frequently cited: the minor good fortune of finding a dime made subjects 84% more likely to help a woman who dropped her papers, suggesting that a trivial situational factor powerfully influenced helping behavior more than stable dispositions [35] [37]. Other classic studies, such as the Milgram obedience experiments and the Princeton Theological Seminary "Good Samaritan" study, further illustrate the power of situations to override presumed character traits [35] [36] [37].
This situationist critique presents a significant challenge to the project of virtue ethics. If moral behavior is overwhelmingly determined by situational pressures rather than internal character, then the central endeavor of virtue ethics—cultivating a virtuous character—may be misguided. For Christian medical ethics, which emphasizes agape love as a selfless, sacrificial commitment to the well-being of others, this challenge is particularly acute [38] [19] [10]. If virtues are as situationally fragile as situationists suggest, can healthcare professionals truly develop a stable disposition of benevolence? This paper argues that they can, and that the Christian concept of agape love provides a unique resource for doing so.
Theoretical Framework: Agape Love as a Foundational Ethic
The Nature of Agape Love
In the New Testament, agape love represents the highest form of love, characterized by its unconditional, self-sacrificial, and volitional nature [38] [13] [39]. Unlike other forms of love—such as epithumia (physical desire), eros (romantic love), or philia (friendship)—agape is not based on emotional attraction, personal benefit, or sentimental relationship [13] [39]. Instead, it is a love of choice, a deliberate commitment to seek the greater good of others without expecting anything in return [38] [13].
Theologically, agape is understood as the love that God is (1 John 4:8), the love that God shows (John 3:16), and the love that God gives as a manifestation of the Holy Spirit's work in the heart of a believer (Galatians 5:22) [13]. This divine love is exemplified in Jesus Christ's self-sacrificial death on the cross, regarded as the quintessential demonstration of agape for humanity [38].
Agape Love in Medical Ethics
In medical ethics, agape love provides a robust foundation for the non-judgmental care of ill persons, a central tenet of excellent and ethical medicine [10]. Dr. Anna Berry articulates this as a "neighbor regarding love for others" that makes no distinction between worthy and unworthy, friend and enemy [10]. This approach aligns with the unconditional compassion required in healthcare, such as the treatment of bacterial endocarditis in a person who struggles with IV drug use or caring for those who forego preventive measures only to find themselves severely ill [10].
Agape love, when adopted as a foundational ethic, moves beyond a mere principle to become a habitual disposition that guides clinical decision-making and patient interactions. It challenges healthcare professionals to practice a steadfast, self-denying, and sacrificial form of care, prioritizing patient needs over personal convenience or bias [38] [13] [10]. Recent systematic reviews have begun to empirically investigate this concept, often under the term "humanitarian love," and have found it enhances healthcare professionals' psychosocial well-being and reduces burnout [27].
Table 1: Key Characteristics of Agape Love in Healthcare Contexts
| Characteristic | Description | Clinical Application |
|---|---|---|
| Unconditional | Not based on the merit or attractiveness of the recipient | Providing the same standard of care to all patients, regardless of background or behavior |
| Sacrificial | Willing to incur cost for the benefit of another | Going beyond minimal duties for patient welfare, even when inconvenient |
| Volitional | A conscious choice rather than mere feeling | Maintaining compassion in challenging cases where empathy might be difficult |
| Enduring | Consistent across time and situations | Providing reliable, faithful care throughout the treatment relationship |
| Transformative | Has the power to heal and restore | Creating a therapeutic environment that promotes healing beyond physical treatment |
Empirical Evidence: Testing the Virtue Ethics Response
Reconceptualizing the Situationist-Virtue Ethics Debate
Recent empirical philosophy has attempted to move beyond the conceptual impasse between situationism and virtue ethics by representing their disagreement as a testable claim about the correlation between situational pressure and virtuous behavior [36].
Situationists can be interpreted as positing a steep, monotone decreasing linear relation: as situational pressure increases, virtuous behavior decreases steadily. Virtue ethicists, conversely, predict a tilde-shaped curvilinear relation: virtuous behavior remains stable and consistent across mid-range, standard situations of varying pressure, decreasing only in more extreme situations [36].
This empirical model grants the situationist that virtue theory entails particular empirical consequences, and then tests whether the evidence actually supports virtue ethics. A 2023 study conducted precisely this test, with results offering tentative support for eudaemonist and agent-based varieties of virtue ethics [36]. The findings suggest that while extreme situations can disrupt virtuous behavior, individuals with cultivated virtues demonstrate significant cross-situational consistency in ordinary circumstances.
Humanitarian Love in Healthcare Research
A 2024 systematic literature review examined the role of "humanitarian love" (conceptualized similarly to agape) and its psychosocial impact on health professionals [27]. The review of 16 studies comprising 2045 participants found that:
- Humanitarian love directed toward patients helps reduce feelings of burnout, emotional exhaustion, and compassion fatigue among healthcare professionals.
- Humanitarian love directed toward self fosters positive emotions, enhancing professionals' ability to provide high-quality care and effectively support patient needs [27].
These findings provide empirical support for the claim that agape love, when cultivated as a professional value, enhances both practitioner well-being and patient care quality—key concerns for researchers and drug development professionals operating in high-stress environments.
Table 2: Key Experiments in the Situationism-Virtue Ethics Debate
| Experiment | Methodology | Key Findings | Virtue Ethics Interpretation |
|---|---|---|---|
| Dime in the Phone Booth (Isen & Levin, 1972) | Researchers placed a dime in a phone booth; confederate dropped papers nearby | Those who found dime were 84% more likely to help | Minor situational factors can facilitate or hinder virtue expression without disproving robust traits [35] |
| Princeton Theological Seminary (Darley & Batson, 1973) | Seminary students told to give talk on Good Samaritan; encountered distressed person en route | Those in a hurry were less likely to help; topic of talk had no effect | Practical wisdom includes properly prioritizing time; virtue requires attentional resources [35] [36] |
| Milgram Obedience (Milgram, 1974) | Participants instructed to administer increasingly severe shocks to confederate | 65% administered maximum voltage despite protests | Extraordinary situational pressure can overwhelm ordinary virtue; highlights need for specific virtue of moral courage [35] [37] |
| Empirical Test of Correlation (2023) | Tested shape of correlation between situational pressure and virtuous behavior | Found tilde-shaped curvilinear relation supporting virtue ethics | Supports virtue ethics claim that behavior is consistent across ordinary situational variations [36] |
Cultivating Benevolence: An Integrated Model for Healthcare Professionals
The empirical and theoretical evidence suggests that benevolence, grounded in agape love, can be cultivated as a robust disposition. This cultivation requires intentional practices that engage the cognitive, affective, and behavioral dimensions of the person.
The Agape Transformation Model
The following model illustrates how agape love transforms character and influences ethical decision-making in healthcare contexts:
Diagram 1: Agape Transformation Model for Ethical Decision-Making
Practical Protocols for Cultivating Benevolence
For healthcare researchers and professionals, cultivating benevolence as a habitual disposition requires intentional practices. The following protocols, drawn from virtue ethics and Christian spiritual formation, provide a framework for development:
Cognitive Rehearsal and Moral Imagination
- Regular reflection on exemplars of agape love in medical practice, such as caregivers who show extraordinary compassion to difficult patients or researchers who prioritize participant dignity over convenience.
- Case study analysis of ethically complex situations, deliberately considering how agape love would inform decisions rather than relying solely on principle-based ethics.
- Scriptural engagement with texts that define agape love (e.g., 1 Corinthians 13, John 13:34-35) specifically reflecting on their application to healthcare contexts [13] [32].
Habituation Through Intentional Practice
- Conscious implementation of agape love characteristics (patience, kindness, trust, hope, perseverance) in specific professional interactions [13].
- Developing "if-then" plans for challenging situations, pre-committing to benevolent responses when situational pressures are anticipated.
- Self-examination routines to identify and address personal biases that hinder agape love, particularly toward certain patient populations or research subjects.
Community Accountability and Formation
- Participation in professional communities that explicitly value and discuss agape love in practice, providing both support and accountability.
- Mentorship relationships that foster character development alongside technical skill development.
- Structured feedback mechanisms on how well one embodies agape love in professional practice, similar to other competency assessments.
Research Reagents for Ethical Practice
Table 3: Essential Resources for Cultivating Benevolence in Research and Healthcare
| Resource Type | Specific Examples | Function in Cultivating Benevolence |
|---|---|---|
| Exemplar Narratives | Case studies of ethical excellence; biographies of compassionate researchers | Provides concrete models for moral imagination and aspiration |
| Reflective Practices | Structured ethical debriefing; examen of consciousness; journaling | Develops self-awareness and habit of learning from experience |
| Community Structures | Ethics consultation services; virtue ethics reading groups; peer mentoring | Creates accountability and shared language for character development |
| Educational Resources | 1 Corinthians 13 analysis; virtue ethics frameworks; situationism research | Builds theoretical understanding of agape love and its challenges |
| Assessment Tools | Burnout scales; compassion satisfaction measures; 360-degree feedback | Monitors progress and identifies areas for growth |
The situationist critique rightly highlights the profound influence of situational factors on moral behavior. However, empirical evidence and philosophical refinement of virtue theory suggest that robust character traits are both possible and cultivable. For healthcare researchers and professionals, the Christian concept of agape love provides a particularly powerful foundation for developing benevolence as a habitual disposition.
This whitepaper has argued that agape love—understood as unconditional, sacrificial, and volitional—can transform character and enable cross-situational consistency in ethical behavior. By intentionally engaging in practices that cultivate this virtue, healthcare professionals can better navigate the complex moral challenges of research and patient care, reducing burnout while promoting both personal well-being and patient dignity.
The integration of agape love as a foundational ethic offers a robust response to situationism while providing a comprehensive framework for moral formation in healthcare contexts. For Christian researchers and medical professionals, this approach represents not merely an ethical theory but a lived expression of faith that aligns with the deepest commitments of Christian medical ethics.
The persistent and critical shortage of organs for transplantation represents a paramount global public health challenge [40]. Within the context of modern healthcare systems, ethical frameworks that motivate and justify organ donation are essential. This case study posits agape love, a selfless, unconditional Christian love, as a robust ethical groundwork for organ donation and transplantation. The concept of agape, which emphasizes altruism and the welfare of others without expectation of return, provides a compelling moral foundation that can address ethical concerns and potentially increase donation willingness [41]. This paper explores the intersection of this theological virtue with the practical realities of organ donation, examining empirical data on knowledge and attitudes, the complex role of religious beliefs, and the potential for agape-inspired altruism to shape both individual behavior and systemic policy.
The Ethical Landscape of Organ Donation
The Global Organ Shortage Crisis
The disparity between the supply of and demand for transplantable organs is a worldwide issue. Current metrics, such as donors per million population (PMP), reveal significant international variability, but this measurement is flawed as it fails to account for critical differences in underlying population demographics, such as age distributions of deaths [40]. A more nuanced analysis using age-stratified data highlights a 4-fold difference in overall donation rates between countries, with far greater variability within specific age strata. For instance, donation rates in the oldest age group (70 years and older) can differ by as much as 10-fold [40]. This suggests that many healthcare systems possess a significant, untapped potential to increase donation. The United States, for example, has the potential to gain over 8,000 increased donors per year if it matched the performance of the highest-performing countries across all age groups [40].
Predominant Ethical Models and Public Perception
The ethical discourse surrounding organ donation often navigates a tension between pure altruism and the perceived commodification of the human body [42]. Altruism remains a primary motivation for donation, with research consistently showing that individuals who perceive organ donation as a selfless act are more inclined to consent [42]. Public perceptions, however, are easily swayed by misconceptions, particularly regarding brain death and religious permissibility, which can severely hinder willingness to donate [42]. Legal frameworks, such as opt-in versus opt-out systems of consent, also shape donation rates. Opt-out systems, which presume consent unless an individual explicitly refuses, have been demonstrated to yield higher donation rates, as evidenced by the successful implementation of such a system in Wales [42]. The Spanish model, which has achieved 40 deceased organ donors PMP, is another prominent example of an effective, system-wide approach that combines an opt-out framework with robust infrastructure and public awareness campaigns [40].
Table 1: Key Factors Influencing Organ Donation Decisions
| Factor Category | Specific Factor | Impact on Donation Willingness |
|---|---|---|
| Socio-demographic | Urban Residence [43] | Positive Predictor |
| Number of Extended Family [43] | Negative Predictor (More family = less willingness) | |
| Knowledge & Awareness | Understanding of Brain Death [42] | Critical Positive Predictor |
| Information from Medical Providers [43] | Strong Positive Predictor | |
| Religious & Cultural | Belief in Religious Compatibility [42] | Strong Positive Predictor |
| Perception of Conflict with Tradition [43] | Strong Negative Predictor | |
| Psychological | Emotional Openness [43] | Positive Predictor |
| Emotional Aversion to Bodily Loss [43] | Negative Predictor |
Agape Love as a Theoretical Framework
Theological Foundations of Agape
Agape (ἀγάπη) is a central tenet of Christian ethics, denoting a self-sacrificial, unconditional love that seeks the good of the neighbor. It is distinguished from other forms of love (eros, philia) by its fundamentally other-oriented nature. This love is exemplified in the Christian narrative of Jesus Christ's self-giving and is commanded as the guiding principle for relationships. Within medical ethics, agape provides a powerful impetus for altruistic action, framing the act of organ donation not as a duty or an exchange, but as a free, generous gift of oneself for the benefit of another person's life and health.
Agape in the Context of Organ Transplantation
The application of agape to organ transplantation was historically advanced by theologians like Joseph Fletcher, who saw in this new medical technology a practical opportunity to express all-encompassing, utilitarian love [41]. Fletcher and others presented organ donation as both an expression of agape and a means of "updating" Christianity through Utilitarian ethics [41]. This perspective was developed at a unique historical moment in the United States when traditional reserve about corpse mutilation had weakened, creating a "window of opportunity" for the acceptance of organ transplantation as an ethical and even praiseworthy practice [41]. This framing directly counters ethical concerns about the commodification of the human body. The Catholic Church, for instance, while strongly supporting organ donation as a noble and charitable act, simultaneously insists that any commercial trading of organs is "morally unacceptable" because it violates human dignity by treating the body as a mere object [44]. Thus, agape preserves the dignity of both donor and recipient by grounding the act in gratuitous love.
Empirical Data on Knowledge, Attitudes, and Beliefs
Insights from a Postgraduate Student Cohort
Empirical research is critical to understanding how ethical concepts translate into public attitudes and behaviors. A recent 2025 survey-based cross-sectional study of 324 postgraduate students at Inonu University in Türkiye provides revealing data [42]. The study, which utilized the validated Organ Donation Attitude Scale (ODAS) with a high Cronbach's alpha of 0.841, found that while 96.5% of respondents recognized the necessity of organ donation, only 16.9% were registered donors [42]. This gap between approval and action is a critical area for intervention.
Religious beliefs were significant for the vast majority (92.5%) and influenced major life decisions for 62.2% [42]. However, a key finding was that the strength of religious belief, while important in life, did not significantly alter ODAS scores [42]. This suggests that religiosity per se may not be the primary barrier. Instead, specific misconceptions were the stronger determining factors: students who had not donated were significantly more likely to believe that brain death is reversible (p < 0.001) and to consider organ donation incompatible with Islam (p < 0.001) [42]. This highlights that it is not religious faith itself, but particular interpretations and knowledge gaps within that faith, which require addressing.
The Role of Religious and Cultural Beliefs
The influence of religion on donation attitudes is complex and varies across cultural contexts. While major monotheistic religions generally support organ donation in principle, practical willingness is often low due to varying interpretations and cultural practices [42]. A study of donor families in Guangxi, China, identified cultural beliefs and religious views as significant barriers, with 53.3% of participants feeling that donation conflicted with traditional culture [43]. This was particularly pronounced in the group that refused donation [43]. This contrasts with the official stance of many religious authorities. For example, no religion formally forbids donation or receipt of organs, and no religion formally obliges one to donate or refuse organs [44]. The challenge, therefore, lies in bridging the gap between high-level theological acceptance and grassroots-level cultural and religious apprehensions, a task for which the concept of agape, as a motivating and clarifying force, is well-suited.
Table 2: Religious Stances on Organ Donation and Key Concerns
| Religion/Group | General Stance on Donation | Notable Concerns or Conditions |
|---|---|---|
| Catholicism | Morally acceptable, encouraged as an act of charity [44] | Against commodification; donor's death must be fully ascertained [44]. |
| Islam | Generally considered compatible by many scholars [42] | Some scholars oppose due to body as "amanat" (trust from God); questions on Muslim to non-Muslim donation [42] [44]. |
| Judaism | Generally supported [42] | Some Orthodox Jews may have religious objections to "opting in" or may request directed donation [44]. |
| Buddhism/Confucianism/Shinto | May be discouraged by traditional reserve about corpse mutilation [44] [41]. |
Agape in Action: Experimental and Interventional Approaches
Methodologies for Assessing Attitudes and Knowledge
To effectively design interventions rooted in agape, robust methods for assessing the current landscape are essential. The following workflow outlines a standard methodology for this research, as utilized in recent studies [42] [43].
Diagram 1: Research Workflow for Assessing Donation Attitudes
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Materials for Social Science Research in Organ Donation
| Item/Tool | Function in Research |
|---|---|
| Structured Demographic Questionnaire | Collects baseline socio-demographic data (age, gender, residency, education) to identify correlation with donation willingness [42] [43]. |
| Organ Donation Knowledge Assessment Form | A custom set of questions (e.g., on brain death, religious compatibility) to quantify participants' understanding and identify key misconceptions [42]. |
| Validated Attitude Scale (e.g., ODAS) | A psychometrically validated instrument like the Organ Donation Attitude Scale (ODAS) to reliably measure positive/negative perceptions toward donation [42]. |
| Semi-structured Interview Guide | A flexible guide for qualitative interviews to explore deeper cultural, emotional, and religious factors behind decision-making [43]. |
| Statistical Software (e.g., SPSS) | Software used for performing statistical tests (chi-square, t-tests, logistic regression) to analyze data and identify significant predictors [43]. |
An Agape-Informed Intervention Model
Based on the identified barriers and motivators, a multi-faceted intervention model can be proposed. This model leverages the concept of agape to reframe the donation narrative while systematically addressing knowledge gaps and cultural concerns. The logical flow of this intervention is shown below.
Diagram 2: Agape-Informed Intervention Model
Discussion and Synthesis
The integration of agape love as an ethical groundwork for organ donation provides a cohesive and motivating framework that can address several persistent challenges. This case study demonstrates that the primary barriers to donation are often not outright rejection but rather a combination of specific misconceptions (e.g., about brain death), cultural and religious apprehensions, and a lack of empathetic, clear communication [42] [43]. Agape directly addresses these by offering a positive, proactive narrative that frames donation as a profound act of selfless love.
The empirical data from Türkiye shows that while religiosity is high, it does not automatically translate into donation action unless accompanied by accurate knowledge [42]. This underscores the necessity of targeted educational programs that are co-developed with religious authorities to clarify theological stances and reassure potential donors. The success of such an approach relies on moving beyond abstract doctrine to practical, community-based dialogue, effectively bridging the gap between official religious positions and grassroots beliefs.
Furthermore, the agape framework reinforces the ethical imperative for systemic reforms, such as the adoption of opt-out consent models that have proven effective in increasing donation rates in countries like Spain and Wales [42] [40]. These policies can be viewed as structural expressions of a communal ethic of care, creating a default environment of generosity while preserving individual choice. For healthcare professionals, an agape-informed ethos necessitates training in sensitive communication and family support, recognizing that the decision to donate is often made in moments of profound grief and emotional distress [43]. Ultimately, uniting the motivational power of agape with strategic, evidence-based interventions presents a promising path toward alleviating the global organ shortage and upholding the dignity of every human person involved in the transplant process.
The integration of agape love—a selfless, sacrificial love for others—into clinical practice represents a paradigm shift toward more holistic and ethical patient care. This whitepaper provides a technical framework for quantifying, implementing, and measuring love within clinical protocols and patient interactions. Drawing upon established psychometric instruments, healthcare relationship models, and the ethical principles of Christian medical ethics, we present methodologies for operationalizing agape love as a tangible component of therapeutic interventions. Supported by quantitative data, visualized workflows, and practical toolkits, this guide equips researchers and clinicians to leverage this fundamental human experience as a variable in drug development and patient-centered care.
The evolving healthcare landscape increasingly emphasizes whole-person health, recognizing that health and disease are influenced by a complex interplay of biological, behavioral, social, and environmental factors [45]. Within this paradigm, the patient-provider relationship is increasingly recognized as a critical point of therapeutic intervention, capable of optimizing health outcomes, enhancing patient satisfaction, and improving adherence to treatment plans [45]. Concurrently, the field of psychology has made significant strides in quantifying the abstract construct of love through validated psychometric scales, enabling its study as a measurable variable [46].
Framed within Christian medical ethics, agape love provides a robust philosophical and ethical foundation for this endeavor. Agape is characterized as a selfless, sacrificial, and unconditional love for others. In a bioethical context, this principle strongly aligns with medical actions intended to save or profoundly improve the lives of others, such as organ donation, which can be viewed as a manifestation of Christian charity and solidarity [19]. This paper posits that the operationalization of such love extends beyond dramatic acts to the daily fabric of clinical interactions, forging effective partnerships between patients and healthcare teams [47]. The challenge, therefore, is not to argue for its importance, but to provide researchers and clinicians with the tools to systematically integrate it into their work.
Quantitative Foundations: Measuring Love
To transition love from an abstract concept to a usable variable in research and clinical assessment, validated measurement tools are essential. Several psychometric instruments have been developed to deconstruct love into measurable components.
The Triangular Theory of Love and its Measurement
Robert Sternberg's Triangular Theory of Love is a prominent model that defines love as consisting of three core elements: intimacy (feelings of closeness, connection, and bondedness), passion (the drives that lead to romance, physical attraction, and sexual consummation), and commitment (the decision to maintain the relationship) [46]. The Sternberg Triangular Love Scale (STLS) is a 45-item instrument that measures these dimensions, each rated on a 9-point Likert scale [46]. The three components are separable but interactive, and their combination results in different types of love experiences [48].
The Short Love Scale (SLS-12)
For research settings where questionnaire length is a constraint, the Short Love Scale (SLS-12) offers a concise, reliable alternative. Developed and validated in Poland in 2022, the SLS-12 is a 12-item instrument designed to assess love in romantic relationships across three dimensions [46]. It includes items directly related to sexual life, an aspect often missing from earlier scales, recognizing it as an important component of a close love relationship [46].
Table 1: Psychometric Properties of the Short Love Scale (SLS-12)
| Property | Value/Result | Interpretation |
|---|---|---|
| Model Fit (CFI) | 0.981 | Excellent fit (values >0.95 are excellent) |
| Model Fit (TLI) | 0.973 | Excellent fit |
| Model Fit (RMSEA) | 0.067 | Acceptable fit (value < 0.08 is acceptable) |
| Diagnostic Cut-offs | 12-44: Poor Relationship45-52: Moderately Good Relationship53-60: Very Good Relationship | Based on ROC curve analysis |
The SLS-12 demonstrates that love can be measured with high psychometric reliability and validity, providing researchers with a feasible tool for inclusion in broader studies [46].
Clinical Protocols: Integrating Love into Patient Interactions
The measurement of love in close relationships provides a model for how caring constructs can be assessed within the clinical environment. The following section outlines protocols for fostering healing relationships, informed by qualitative research with healthcare providers.
The Healing Pathway Model
A qualitative study involving 52 conventional and Complementary and Integrative Health (CIH) providers identified a conceptual Healing Pathway Model, which outlines how providers can leverage patient relationships to facilitate healing [45]. The model is structured around three core domains:
- Provider Approach for Facilitating Healing: The specific attitudes and behaviors exhibited by the provider.
- Foundations of a Healing Pathway: The underlying principles that make the approach effective.
- Observation of Healing Outcomes: The tangible results observed in patients and the relationship.
Table 2: Core Domains of the Healing Pathway Model
| Domain | Key Components | Clinical Manifestation |
|---|---|---|
| Provider Approach | Authentic presence, mutual participation, compassionate communication | The provider acts as an "expert helper," engaging the patient as an active partner in their own care [45]. |
| Foundation of Healing | Trust, safety, co-creation of care plans | The relationship is built on Watson's core principles, such as the practice of loving-kindness and enabling a deep belief in the patient [45]. |
| Healing Outcomes | Improved patient engagement, self-efficacy, and clinical outcomes | Patients report greater satisfaction, better adherence, and improved quality of life [45]. |
Protocol for Mutual Participation and Shared Decision-Making
A key operationalization of agape love in the clinic is the Mutual Participation Model, where the provider and patient are in mutually supportive roles with shared responsibility [45]. This aligns with the ethical tenet of honoring the patient's God-given dignity and autonomy [19].
Workflow for Implementing Mutual Participation: The following diagram illustrates a continuous workflow for establishing and maintaining a mutual participation model in clinical practice.
Operationalizing love in research and clinical practice requires a set of defined "reagents" — reliable tools and methods for measurement and intervention.
Table 3: Research Reagent Solutions for Operationalizing Love
| Tool/Reagent | Function | Application Context |
|---|---|---|
| Short Love Scale (SLS-12) | Quantifies the intensity and quality of love in a relationship. | Research: As an outcome variable in studies on patient-clinician bonding or family caregiver dynamics. |
| Sternberg Triangular Love Scale (STLS) | Provides a detailed profile of intimacy, passion, and commitment. | Research: For in-depth psychological studies on the nature of therapeutic alliances. |
| Semi-Structured Interview Scripts | Elicits rich qualitative data on experiences of caring and healing. | Qualitative Research: To gather provider and patient narratives on healing relationships [45]. |
| Healing Pathway Model Framework | Serves as a conceptual map for designing patient-centered care interventions. | Clinical Practice: Guides the training of clinicians in fostering healing relationships [45]. |
| Mutual Participation Model | Provides a structural template for shared decision-making. | Clinical Protocols: Informs the design of clinical workflows that honor patient autonomy and partnership [45] [47]. |
Application in Bioethics: A Case Study in Organ Transplantation
The operationalization of agape love finds a profound application in the field of organ transplantation, where Christian ethics provide a clear framework for evaluating the practice. The principle of agape love — selfless, sacrificial love for others — is central to this analysis, aligning with the scriptural tenet to "love your neighbor as yourself" and the concept that "greater love has no one than this: to lay down one's life for one's friends" [19].
The Orthodox Church's stance on transplantation is one of cautious support, grounded in deep theological principles. It encourages organ donation as an act of charity and solidarity but calls for a careful approach that respects key considerations [19]. The following diagram models the ethical decision-making process for organ donation from a Christian ethical perspective.
This framework demonstrates how an abstract ethical concept (agape) can be operationalized into a structured protocol for guiding patients, families, and medical professionals through complex bioethical decisions.
Love, particularly in the form of agape, is not merely a sentimental ideal but a potent, operationalizable component of ethical clinical practice and research. Through the use of validated psychometric instruments, structured clinical protocols like the Healing Pathway and Mutual Participation models, and clear ethical frameworks, the abstract concept of love can be translated into tangible actions and measurable outcomes. For researchers, this opens new avenues for exploring the impact of human connection on health. For clinicians, it provides a roadmap for forging the effective partnerships that patients desire and that lead to better care. For the field of Christian medical ethics, it grounds the lofty principle of agape love in the daily reality of healing, affirming that the respectful, self-giving care for the whole person is not only good ethics but also good medicine.
Fostering the Beloved Community in Healthcare Teams and Research Laboratories
The healthcare and scientific research sectors stand at a critical juncture. While remarkable advances have been made in medical technology and treatment, a parallel crisis has emerged within the workforce itself. Health workers experience worse mental health outcomes than any other segment of the U.S. workforce, with only 38% of distressed health workers seeking care despite severe symptoms [49]. This environment, characterized by burnout, systemic barriers to mental healthcare, and hierarchical structures, directly impacts the quality of patient care and the integrity of scientific research. In response to this crisis, this whitepaper proposes a transformative framework: the intentional cultivation of the "Beloved Community" within healthcare teams and research laboratories, grounded in the Christian medical ethics concept of agape love.
This concept of agape love, defined as a "neighbor-regarding love for others" that makes no distinction between worthy and unworthy, friend and enemy, provides a robust ethical foundation for modern medical practice and scientific collaboration [10]. Dr. Martin Luther King Jr., who popularized the term "Beloved Community," envisioned it not as a utopian ideal but as a realistic, achievable goal where "poverty, hunger and homelessness will not be tolerated because international standards of human decency will not allow it" and where "racism and all forms of discrimination, bigotry and prejudice will be replaced by an all-inclusive spirit of sisterhood and brotherhood" [50]. Within scientific and medical contexts, this translates to environments where excellence is pursued not through competition and domination, but through mutual respect, radical hospitality, and a shared commitment to the common good.
Conceptual Foundations: Agape Love and the Beloved Community
Agape Love as a Foundational Ethic
Agape love represents a distinct form of love that differs significantly from other love types. Unlike eros (romantic love) or philia (friendship), agape is unconditional, selfless, and seeks the welfare of others without expectation of return [5] [51]. In the Christian tradition, it symbolizes the love God has for people and the love humans should have for God and, by extension, for all others simply because they are created in the divine image [5]. In a secular professional context, this translates to what Dr. Albert Schweitzer termed "Reverence for Life"—the ethical principle that all living creatures deserve respect and care [51].
For researchers and healthcare professionals, agape love provides a lens through which to practice science and medicine. It is a love that is "spontaneous, unselfish, and creative" [50], and it forms the core value upon which the Beloved Community is built [50] [52]. In practical terms, it means treating every colleague, research subject, and patient with unconditional positive regard, recognizing their inherent worth and dignity regardless of their role, background, or characteristics.
The Beloved Community Mindset
The Beloved Community is the tangible outcome of a consistent practice of agape love and nonviolence. It is a community that manifests and protects agape love as its guiding principle [52]. According to The King Center, the Beloved Community is not devoid of conflict but resolves conflicts peacefully through "a mutual, determined commitment to nonviolence" [50]. This framework is particularly relevant to high-stakes environments like research laboratories and healthcare teams where conflict, competition for resources, and high-pressure deadlines can create fertile ground for systemic dysfunction.
The Beloved Community mindset requires a "radical revolution of values," shifting from a "thing-oriented" society to a "person-oriented" one [53]. In the context of drug development and medical research, this means measuring success not only by publication metrics, grant funding, and patent approvals but also by the quality of collaboration, the well-being of the research team, and the ultimate impact on human flourishing.
Table 1: Core Principles of the Beloved Community Framework in Scientific Contexts
| Core Principle | Definition | Application in Research & Healthcare |
|---|---|---|
| Radical Hospitality [52] | Offers inclusive welcome to everyone; an inclusive family rather than exclusive club. | Creating inclusive teams that value diverse backgrounds and disciplines; ensuring all team members have a voice. |
| Win Friendship & Understanding [50] | Seeks to redeem and reconcile rather than defeat opponents. | Transforming competitive, zero-sum lab cultures into collaborative ones where shared goals are prioritized. |
| Defeat Injustice, Not People [50] | Focuses energy on removing evil forces (unjust systems), not destroying persons [52]. | Systematically identifying and reforming policies that cause burnout, inequality, or hinder scientific progress. |
| Unyielding Persistence for Justice [52] | Unwavering commitment to justice and equity. | Advocating for equitable access to research opportunities and challenging discriminatory practices in authorship or promotion. |
| Network of Mutuality [52] | Acknowledges the inescapable interdependence of the human family. | Recognizing that drug discovery and patient care depend on seamless collaboration across multiple specialties and roles. |
Operationalizing the Framework: Methodologies for Healthcare and Research
A Protocol for Cultivating a Beloved Community Mindset
Transforming a team or laboratory requires intentional, structured effort. The following protocol, adapted from the principles of Beloved Community Labs and the Six Steps of Nonviolent Social Change, provides a methodological approach [54] [50].
Phase 1: Information Gathering and Education
- Objective: To develop a deep, shared understanding of the current state and the vision for change.
- Methodology:
- Conduct a Psychological Safety Audit: Utilize anonymous surveys and facilitated focus groups to assess current levels of psychological safety, belonging, and well-being. The Mental Health Access Survey can be adapted to gauge team members' comfort in seeking support without fear of professional repercussions [49].
- Map the Ecosystem: Identify all formal and informal policies, power structures, and cultural norms that impact team dynamics. This includes authorship guidelines, mentorship structures, and performance review criteria.
- Shared Education: Convene the team to review the gathered data and jointly educate themselves on the principles of the Beloved Community and agape love. This establishes a common language and shared framework for change.
Phase 2: Personal Commitment and Negotiation
- Objective: To build individual buy-in and co-create a new social contract for the team.
- Methodology:
- Articulate a Shared Vision: Facilitate a workshop where team members collaboratively answer: "What would our lab/team look like if it were a true Beloved Community?"
- Draft a Community Compact: Based on the vision, draft a written compact that outlines shared values and behavioral commitments. This should include specific, measurable pledges related to communication, conflict resolution, and mutual support.
- Formalize Commitment: Each team member publicly signs the compact, making a personal commitment to uphold its principles.
Phase 3: Direct Action and Reconciliation
- Objective: To implement new structures and practices, and to create processes for continuous reconciliation.
- Methodology:
- Implement Structural Changes: Act on the findings from Phase 1. This may include establishing a confidential peer support system, revising lab policies that contribute to burnout, or creating rotating leadership roles for projects.
- Establish Reconciliation Circles: Implement a regular (e.g., monthly) practice where team members can safely address conflicts, misunderstandings, or harms in a spirit of truth-telling and reconciliation, not punishment.
- Create a "Re-Entry" Pathway: Develop a supportive, non-punitive protocol for team members returning from leave (e.g., medical, mental health) to ensure their successful reintegration [49].
The following diagram illustrates the cyclical, iterative nature of this protocol:
The Scientist's Toolkit: Essential Reagents for Cultural Transformation
Building a Beloved Community requires concrete tools and resources. The table below details key "reagents" necessary for this cultural transformation.
Table 2: Research Reagent Solutions for Cultivating Beloved Community
| Item / Solution | Function / Purpose | Implementation Example |
|---|---|---|
| Confidential Peer Support [49] | Provides a safe, non-judgmental space for health workers and researchers to seek support without fear of professional stigma or repercussions. | Establish a trained peer support network with guaranteed confidentiality, separate from reporting lines to leadership. |
| Community Compact | Serves as a co-created social contract that articulates shared values, expectations, and commitments to agape love and radical hospitality. | Draft and sign a compact during a team retreat; display it prominently in the lab and include it in onboarding materials. |
| Trained Facilitators | To guide teams through difficult conversations, conflict resolution, and reconciliation processes with emotional intelligence and neutrality. | Engage a neutral third-party facilitator from outside the immediate team to lead initial reconciliation circles and training sessions. |
| Restorative Justice Circles | A structured process for addressing harm, conflict, or policy violations in a way that repairs relationships and reintegrates individuals into the community. | Use circles to address authorship disputes or interpersonal conflicts, focusing on the impact of actions and collective healing. |
| Psychological Safety Audit Tool | A diagnostic instrument to quantitatively and qualitatively measure the current state of psychological safety, belonging, and well-being. | Administer a standardized survey (e.g., based on the TIS-PS scale) anonymously every 6 months to track progress over time. |
Practical Applications and Impact
Application in Healthcare Teams
In clinical settings, the Beloved Community framework directly addresses the systemic crises of burnout and mental health stigma. The "Health Workers Have The Right, Too" campaign aligns perfectly with this ethos, advocating for six key actions that operationalize agape love [49]:
- Ensuring accessible and affordable mental health care.
- Committing to equal privacy in mental health care.
- Strengthening access to confidential Professional Health Program support.
- Guaranteeing confidential peer support.
- Encouraging education and training on mental health and professional wellbeing.
- Advancing a supportive pathway for re-entry.
These actions embody the Beloved Community trait of "speaking truth in love, always considering ways to be compassionate with one another" [52]. By implementing these measures, healthcare organizations move beyond superficial wellness programs to fundamentally restructure systems so that caregivers can receive the care they need without fear, thereby sustaining their capacity to provide compassionate, excellent patient care.
Application in Research Laboratories
In research environments, the hyper-competitive "publish or perish" culture often undermines collaboration and ethical conduct. The Beloved Community framework offers a corrective model. The Agape Model of nursing practice, which is based on the agape love and characteristics of Christ, provides a template for a Christ-centered approach to professional relationships that can be adapted for scientific teams [55]. This includes:
- Affirmation of Differences: Building a community that practices "recognition and affirmation, not eradication, of differences" [52], which is essential for fostering the cognitive diversity that drives scientific innovation.
- Shared Power: Actively "sharing power" and acknowledging the "inescapable network of mutuality" [52] by implementing shared authorship guidelines, rotating leadership of lab meetings, and ensuring all contributors are recognized.
- Unyielding Persistence for Justice: Applying this principle [52] to champion rigorous, ethical research practices and to challenge unethical pressures that prioritize speed or sensationalism over truth and safety.
The ultimate aim is to create a lab culture where the focus shifts from individual achievement to collective discovery, freeing scientists to do their most creative and impactful work.
The crises facing healthcare and scientific research—burnout, attrition, ethical failures—are not merely operational problems to be solved with technical solutions. They are spiritual and moral crises stemming from a culture of extraction, competition, and domination [54]. The framework of the Beloved Community, grounded in the Christian ethic of agape love, provides a powerful, transformative alternative.
This shift requires more than intellectual assent; it demands what Beloved Community Labs call "deep embodiment"—the practice of stepping into the future by "generating and experiencing a new world here and now by practicing and embodying a new set of values" [54]. For researchers, scientists, and healthcare professionals, this means having the courage to restructure our teams and laboratories around the values of radical hospitality, relentless reconciliation, and reverential care for one another. By doing so, we not only enhance the wellbeing of our workforce but also improve the quality of our science and the integrity of the healing arts, creating a future where both caregivers and patients can thrive.
Navigating Ethical Challenges: Balancing Agape with Modern Medical Realities
In the field of bioethics, the proper definition of "love" holds profound implications for clinical practice, research ethics, and healthcare policy. Relativistic frameworks that define love based on individual preference or situational factors have gained significant influence, particularly through systems like situation ethics, which posits love as the primary moral factor while rejecting fixed moral absolutes [12]. This approach, pioneered by thinkers like Joseph Fletcher, argues that ethical maxims should be "compromised or set aside in the situation if love seems better served by doing so" [12]. Such relativistic conceptions stand in direct opposition to the classical Christian understanding of agape love, creating a critical point of tension for researchers and practitioners in Christian medical ethics who seek to ground their work in a robust moral framework.
This paper argues that agape love, properly understood within the Christian tradition, constitutes an objective moral reality rather than a subjective preference. We will demonstrate how agape provides a necessary foundation for biomedical ethics that respects human dignity, maintains moral consistency, and offers resistance to utilitarian calculations that might otherwise sacrifice individual welfare for collective benefit. Through theological examination, empirical analysis, and practical application, we will establish that agape love serves as an indispensable resource for addressing complex ethical challenges in contemporary medicine and research.
Theological Foundations: Defining Agape Love
The Distinctive Nature of Agape
Agape represents a distinctive form of love that differs fundamentally from emotional affection or preferential regard. Biblical agape love is unconditional, sacrificial love that Biblically refers to a love that God is, that God shows, and that God gives as a manifestation of His Spirit's bearing fruit in the heart of a yielded saint [13]. Unlike emotional forms of love that respond to attractive qualities in the beloved, agape is characterized by several definitive features:
Volitional rather than emotional: Agape is "the love of choice, the love of serving with humility, the highest kind of love, the noblest kind of devotion, the love of the will (intentional, a conscious choice) and not motivated by superficial appearance, emotional attraction, or sentimental relationship" [13]. This stands in contrast to phileo (brotherly love) which is based on emotional connection and shared interests.
Self-sacrificial in nature: Agape "is a love that impels one to sacrifice one's self for the benefit of the object loved" and "speaks of a love which is awakened by a sense of value in the object loved, an apprehension of its preciousness" [13]. This finds its ultimate expression in the Christian concept of Christ's sacrifice.
Unconditional and enduring: Agape "does not depend on the world's criteria for love, such as attractiveness, emotions, or sentimentality" but rather persists regardless of changing circumstances or feelings [13].
Agape Versus Subjective Love
The fundamental distinction between agape and relativistic conceptions of love becomes evident in their respective foundations. Relativistic approaches, such as Fletcher's situation ethics, though using the language of love, ultimately ground moral decisions in subjective assessments of what appears loving in a given situation, "making no ethical demands upon the person loving" [13]. By contrast, agape love "is a love of devotion" with "ethical qualities about it, obligations, responsibilities" that flow from the character of God Himself [13].
This distinction has profound implications for medical ethics. Agape "always treats human beings as ends in themselves and never as mere means" [32], providing a foundation for human dignity that cannot be overridden by utilitarian calculations. This stands in direct opposition to Fletcher's "agapeic calculus," which resembles utilitarianism in seeking "the greatest amount of neighbour-welfare for the largest number of neighbours possible" [32].
Empirical Investigation: Quantitative and Qualitative Evidence
Research Methodology on Love Constructs
Contemporary research on love has developed rigorous methodological approaches for investigating different love styles and their correlates. The following table summarizes key methodological frameworks employed in empirical studies of love:
Table 1: Methodological Approaches in Love Research
| Method Component | Description | Application in Research |
|---|---|---|
| Love Attitudes Scale (LAS) | Measures six love styles: Eros (passionate), Ludus (game-playing), Storge (friendship), Pragma (logical), Mania (possessive), and Agape (all-giving) [22] | Quantitative assessment via 5-point Likert scale; subscales show Cronbach's alpha 0.62-0.88 [22] |
| Relationship Scales Questionnaire (RSQ) | Assesses four attachment styles: secure, fearful, obsessive, and indifferent [22] | 17-item Turkish version showed internal consistency 0.27-0.61 and test-retest reliability 0.78 [22] |
| Mixed-Methods Approach | Combines quantitative surveys with qualitative focus groups and interviews [56] | Provides triangulation; offers both statistical trends and nuanced understanding |
| Personality Assessment | Links love styles to personality traits using Five Factor model or DSM-derived traits [57] | Reveals connections between personality pathology and maladaptive love styles |
Empirical Findings on Agape and Relativism
Recent empirical investigations have yielded significant data regarding the impact of relativistic frameworks on agape love. A 2024 phenomenological study conducted within Ethiopian Evangelical Churches employed both quantitative and qualitative methods to assess the influence of postmodern relativism on agape love [56]. The quantitative findings revealed concerning trends:
Table 2: Quantitative Findings on Postmodernism's Influence on Agape Love
| Survey Item | Response Distribution | Interpretation |
|---|---|---|
| "Postmodernism is heresy according to the Bible" | 55% agreed, 34% neutral, 12% strongly disagreed [56] | Significant portion of respondents influenced by relativistic thinking |
| "Teachings on earthly prosperity have affected love toward God" | Nearly 90% agreed [56] | Materialistic focuses correlate with diminished divine love |
| Qualitative Findings | Ministers reported congregants increasingly adopting "deceptive ways of postmodernism" [56] | Relativism seen as actively undermining traditional agape |
These empirical findings demonstrate that relativistic frameworks exert a statistically significant negative influence on the understanding and practice of agape love within religious communities. The research concluded that "postmodernism has negatively influenced agape love of contemporary Evangelical Churches" [56], highlighting the very confrontation between agape and relativism that this paper addresses.
Agape in Bioethical Application: Beyond Situation Ethics
Critical Analysis of Situation Ethics
In biomedical ethics, the confrontation between agape and relativism becomes particularly acute in the evaluation of situation ethics. Developed by Joseph Fletcher, situation ethics proposes love as the sole moral principle while rejecting moral absolutes, arguing that Christians should do "whatever the other person wants, as that is the most loving thing to do" [12]. This approach suffers from critical flaws when examined from a Christian ethical perspective:
Definitional ambiguity: Fletcher's system provides no objective standard for defining love, leaving it vulnerable to subjective interpretation. Without such a standard, "human feelings and emotions can be deceptive" [12], potentially justifying actions that violate human dignity under the guise of love.
Neglect of moral formation: Situation ethics "does not relate the situation to the virtue of the individual and to moral principles that cannot be violated" [12]. It focuses exclusively on actions and outcomes while ignoring character development.
Theological inconsistency: Fletcher's approach "conflicts with the Bible's long list of prescriptive commandments and suggests that agape is instead of the law rather than a fulfilment of it, as Jesus taught" [32]. It thus separates love from the broader moral framework of Christian scripture.
Agape as Ground for Medical Morality
In contrast to situation ethics, agape love provides a robust foundation for medical morality that affirms both the objective value of human persons and the necessary virtues for ethical practice. The virtue of charity shapes "the whole of Christian medical morals, as it does every other aspect of moral life" [12]. This approach, championed by bioethicists like Edmund Pellegrino, emphasizes that patients are best cared for "when the caregiver seeks the best for them, and what is best must come from various interdependent absolutes that work together to care well for others" [12].
Agape-informed medical ethics recognizes that "technological advancement has come under increasingly significant evaluation" precisely because "how people are treated matters" [12]. This perspective acknowledges human vulnerability, dependence, and finitude as central concerns of bioethics, rather than viewing them as problems to be eliminated through technological mastery [12].
Theoretical Framework: Diagramming the Conflict
The essential conflict between agape love and relativistic approaches can be visualized through their opposing foundational principles and consequent ethical applications. The following diagram illustrates the logical relationships and decisional pathways that distinguish these two approaches:
This conceptual framework illustrates how agape love begins from objective foundations—the character of God, universal human dignity, and moral absolutes—and moves toward ethical decisions that respect persons as ends in themselves. By contrast, relativistic approaches begin from subjective preferences and situational factors, potentially leading to the instrumentalization of persons. The diagram highlights the essential conflict between these paradigms and their profoundly different implications for medical ethics.
Research Reagents: Methodological Tools for Investigation
The empirical study of agape love and its ethical applications requires specific methodological tools and assessment instruments. The following table details essential "research reagents"—conceptual tools and methodologies—that enable rigorous investigation in this field:
Table 3: Essential Research Methodologies for Investigating Agape in Ethics
| Research Tool | Function | Application in Bioethics |
|---|---|---|
| Love Attitudes Scale (LAS) | Quantifies preferences for six love styles; particularly identifies agapic orientation [22] | Measures correlation between agape scores and ethical positions in healthcare contexts |
| DSM-Five Factor Model Assessment | Evaluates personality traits (psychoticism, antagonism, disinhibition, negative affect, detachment) [57] | Investigates connections between personality pathology and receptivity to agape versus relativistic ethics |
| Mixed-Methods Protocol | Combines quantitative Likert-scale surveys with qualitative focus groups and interviews [56] | Provides comprehensive understanding of how abstract love concepts translate to ethical decision-making |
| Virtue Ethics Assessment Framework | Evaluates moral character and virtue development rather than just specific actions [12] | Assesses formation of agape as character trait rather than merely compliance with rules |
| Triangulation Validation | Uses multiple data sources and methods to verify findings [56] | Ensures research conclusions about agape's influence are methodologically robust |
These methodological tools enable researchers to move beyond theoretical speculation to empirical investigation of how agape love functions in practical ethical reasoning. They facilitate the gathering of quantitative data that can be analyzed statistically (e.g., using IBM SPSS Statistics software) while also capturing qualitative dimensions through focused group discussions and key informant interviews [56].
The confrontation between agape love and relativism represents a critical fault line in contemporary bioethics. The evidence examined in this paper—drawn from theological analysis, empirical research, and ethical application—demonstrates that agape love provides an objective moral foundation that cannot be reduced to subjective preference. Agape stands in necessary opposition to relativistic frameworks like situation ethics, which despite using the language of love, ultimately ground moral decisions in subjective assessments and utilitarian calculations.
For researchers, scientists, and drug development professionals working within Christian medical ethics, agape love offers a robust framework for addressing complex challenges. It provides a foundation for human dignity that resists instrumentalization, affirms the importance of moral absolutes while allowing for nuanced application, and prioritizes the development of virtuous character in healthcare professionals. Rather than representing one optional perspective among many, agape love constitutes an essential resource for preserving medicine's moral core in an increasingly relativistic age.
The empirical findings presented here indicate that relativistic frameworks already exert significant influence in religious communities, with nearly 12% of evangelical respondents strongly disagreeing that postmodern relativism constitutes heresy [56]. This underscores the urgency of clearly articulating and defending agape love as an objective moral reality. For Christian medical ethics to maintain its distinctive contribution to healthcare and research, it must boldly confront relativism by championing agape love as the necessary foundation for honoring human dignity, pursuing genuine flourishing, and respecting the sacredness of life at all stages.
The integration of artificial intelligence (AI) and machine learning (ML) into drug development represents a paradigm shift, offering the potential to reduce development timelines from a decade to under two years and generate enormous economic value [58] [59]. However, this reliance on data-intensive AI models introduces a new category of vulnerability: deliberate data poisoning. "Nightshade," a tool developed by researchers at the University of Chicago's SAND Lab, exemplifies this threat. It works by adding "barely perceptible" pixel-level perturbations to images, causing AI models to misclassify them fundamentally—for example, interpreting a dog as a cat [60]. In the context of biomedical research, where AI is used for critical tasks such as compound screening, efficacy prediction, and clinical trial design, a successful "Shade Poisoning" attack could corrupt models, leading to faulty drug candidates, erroneous toxicity predictions, and compromised clinical trials [58] [59].
This technical guide examines the risk of "Shade Poisoning" through the lens of agape love, a core principle of Christian medical ethics. Agape is defined as a non-preferential, self-sacrificial love that seeks the good of the other, fundamentally orienting ethical action toward the protection of patient well-being and the pursuit of justice [32] [14]. This stands in stark contrast to a purely profit-driven or complacent approach that might prioritize speed to market over robust security and ethical diligence. By framing the technical response within this ethical imperative, this paper provides drug development professionals with methodologies to safeguard their AI systems, thereby fulfilling the agapeic duty to protect patients from harm.
Technical Foundations of Data Poisoning
The Mechanics of Nightshade and Its Analogues
Tools like Nightshade represent an offensive deterrent against the non-consensual scraping of data for AI training. Their operational principle lies in the manipulation of an AI model's feature space—the internal representation where the model learns to distinguish between different categories of data.
The algorithm identifies the features that define a specific concept (e.g., a "dog") and then applies minimal perturbations to the image pixels. These changes are virtually invisible to the human eye but are significant enough to shift the image's representation in the AI's feature space toward a different, target concept (e.g., a "cat"). When these "poisoned" samples are ingested during the model's training phase, they cause the model to learn incorrect feature associations. The integrity of the AI model is compromised, leading to persistent and often irreversible misclassification behaviors. Research indicates that only a relatively small number of poisoned samples can cause permanent damage to a generative AI model's output capabilities [60].
Vulnerability of Drug Development Pipelines
The drug development lifecycle is particularly vulnerable to such attacks due to its growing dependence on large, often publicly sourced or multi-institutional, datasets for training AI models. Key vulnerable stages include:
- Drug Discovery: AI models that screen vast chemical or genomic datasets to identify drug candidates could be misled by poisoned data, resulting in the pursuit of ineffective or unsafe compounds [58] [59].
- Preclinical Testing: Predictive models for pharmacokinetics and toxicity that are trained on poisoned data could provide a false sense of a compound's safety, leading to costly failures in later stages or, worse, patient harm [59].
- Clinical Trial Optimization: AI used for patient stratification and recruitment relies on accurate data. Data poisoning could introduce bias, skewing trial populations and compromising the validity of trial results [61] [58].
The following table summarizes the potential impact across the drug development lifecycle.
Table 1: Potential Impacts of Data Poisoning Across the Drug Development Lifecycle
| Development Stage | Primary AI Application | Potential Impact of Data Poisoning |
|---|---|---|
| Drug Discovery [58] [59] | Compound screening, target identification | Pursuit of ineffective drug candidates; misidentification of biological targets |
| Preclinical Testing [59] | Toxicity and pharmacokinetic prediction | Failure to identify toxic compounds; inaccurate dosing predictions |
| Clinical Trial Management [61] [58] | Patient stratification, trial design optimization | Introduction of bias; unrepresentative trial populations; invalid efficacy results |
| Pharmacovigilance [59] | Adverse drug event (ADE) detection | Failure to detect safety signals; compromised post-market patient safety |
An Ethical Framework: Agape Love in Christian Medical Ethics
The technical challenge of data poisoning is, at its core, an ethical one. Agape love, as articulated in Christian ethics, provides a robust framework for a response. This love is not an emotion but a principle of action characterized by its other-centeredness and self-sacrificial nature [14]. It is the love that "seeks the good of the other" unconditionally.
In the context of medical research, agape love manifests as an unwavering commitment to patient safety and well-being. It directly opposes a utilitarian "greatest good for the greatest number" calculus that might justify cutting corners on security [32]. This principle demands that researchers and corporations see patients not as mere data points or means to a profitable end, but as persons whose dignity and safety are paramount. This aligns with the philosophical argument of Immanuel Kant, who asserted that humanity must always be treated as an end in itself, and never as a mere means [32].
Therefore, the agape-driven imperative is to proactively protect the data and AI models that underpin modern medicine. Overcoming complacency in advocacy and care means investing in robust security measures, even when they are costly or slow down development, because the ultimate goal is "the speed to the patient," not just the market, ensuring the therapy delivered is both effective and safe [62].
Experimental Protocols for Poisoning Risk Mitigation
To operationalize the duty of care, researchers must implement rigorous experimental and data-handling protocols. The following methodologies provide a defensive framework.
Protocol 1: Data Provenance and Integrity Verification
Objective: To ensure the authenticity and integrity of all data used to train critical AI models in the drug development pipeline.
Detailed Methodology:
- Provenance Logging: Create an immutable, blockchain-based or other secure ledger to track every dataset's origin, custody, and modifications. Each entry must include the data source, date of acquisition, and any entities that have handled the data.
- Checksum Verification: Apply cryptographic hash functions (e.g., SHA-256) to original data sources. Before training, re-compute the hash of the dataset and verify it against the stored value to detect any tampering or corruption.
- Data Lineage Analysis: Use automated tools to map the flow of data from its source through all transformation processes. This helps identify any point where unvetted or potentially poisoned data could have been introduced.
- Cross-Referencing: Where possible, validate datasets against independent, trusted sources to confirm biological or chemical consistency.
Protocol 2: Adversarial Robustness Stress Testing
Objective: To proactively identify a model's vulnerability to data poisoning and other adversarial attacks before deployment.
Detailed Methodology:
- Poisoned Data Synthesis: Generate a controlled set of poisoned data samples following known attack vectors, such as applying Nightshade-style perturbations or introducing label noise.
- Red Team Exercise: Integrate the synthesized poisoned data into a copy of the training pipeline. Retrain the model and monitor for significant performance degradation or behavioral changes.
- Robustness Metrics: Quantify the model's resilience using metrics such as Adversarial Accuracy (performance on poisoned data) and Loss Divergence (difference in training loss between clean and poisoned data).
- Continuous Monitoring: Implement this protocol not as a one-time pre-deployment check, but as a recurring part of the model's lifecycle management, especially when new data is incorporated.
Protocol 3: Pre-clinical Dual-Track Verification
Objective: To prevent the omission of critical safety signals, such as long-term toxicity, that could be missed by an AI model compromised by poisoned data or inherent bias [58].
Detailed Methodology:
- Parallel Pathways: For all critical safety and efficacy assessments (e.g., intergenerational toxicity), run two parallel tracks.
- AI Track: Utilize the AI-powered virtual model for rapid prediction.
- Empirical Track: Conduct traditional in vitro or in vivo animal experiments as a control.
- Synchronized Comparison: Systematically compare the outcomes from both tracks at predetermined milestones. Any significant discrepancy must trigger a "hard stop" and a root-cause investigation.
- Bias Auditing: Analyze the AI model's training data for representativeness, specifically checking for under-representation of certain demographic or genetic groups that could lead to biased outcomes [61] [58]. This workflow ensures that the speed offered by AI does not come at the cost of patient safety, a key concern of agapeic ethics.
The following diagram illustrates this essential dual-track verification workflow.
The Scientist's Toolkit: Key Research Reagent Solutions
Implementing these protocols requires a suite of specialized tools and reagents. The following table details essential components for building a poisoning-resistant research pipeline.
Table 2: Key Research Reagent Solutions for Poisoning-Resistant AI Research
| Tool/Reagent Category | Specific Examples | Function & Explanation |
|---|---|---|
| Data Integrity Tools [60] | Cryptographic hashing libraries (e.g., OpenSSL), Blockchain-based provenance trackers | Verifies data authenticity and creates an immutable audit trail from source to model, preventing undetected tampering. |
| Adversarial Testing Suites [60] | CleverHans, IBM Adversarial Robustness Toolbox, Custom Nightshade-style poison generators | Simulates real-world poisoning attacks to stress-test model robustness and identify vulnerabilities before deployment. |
| Model Explainability (XAI) Platforms [58] [59] | SHAP, LIME, DeepLift | Provides interpretability into AI model decisions, helping researchers identify if an output is based on legitimate features or potentially poisoned artifacts. |
| Bias Detection Frameworks [61] [58] | AI Fairness 360, Fairlearn, Demographic parity analyzers | Audits training data and model outputs for unfair biases that could be exacerbated by data poisoning, ensuring justice in patient representation. |
| Dual-Track Validation Assets [58] | In vitro assay kits, Animal model cohorts, High-quality public datasets (e.g., BRENDA) | Serves as the empirical ground truth in the dual-track protocol, providing a crucial reality check for AI-generated predictions. |
Regulatory and Compliance Landscape
Regulatory bodies are acutely aware of the risks and opportunities presented by AI. The FDA's 2025 draft guidance on AI in drug development emphasizes a risk-based credibility assessment framework, requiring developers to establish trust in their AI models for a specific "context of use" [59]. This inherently includes evaluating a model's resilience to data corruption. Similarly, the European Medicines Agency (EMA) stresses data integrity, traceability, and human oversight [59]. Proactive poisoning mitigation is not just a technical best practice but is becoming a regulatory expectation. Demonstrating robust adversarial testing and data integrity controls will be crucial for successful regulatory submissions. Furthermore, if a poisoned model leads to patient harm, companies could face significant liability under product safety and tort law [59].
The threat of "Shade Poisoning" is a tangible and serious risk to the integrity of AI-driven drug development. Addressing this threat requires more than just technical fixes; it demands a foundational ethical commitment. The principle of agape love—with its insistence on self-sacrificial care for the other—provides the necessary imperative to overcome corporate and scientific complacency. By implementing rigorous defensive protocols, conducting continuous adversarial testing, and embracing a regulatory framework that prioritizes patient safety above all else, the drug development community can faithfully uphold its duty to protect those it serves. The journey from data to drug must be guarded with both technical excellence and ethical vigilance.
The integration of advanced technological interventions in medicine presents a complex ethical challenge at the intersection of Christian theology, medical science, and human dignity. Within Christian medical ethics, the concept of agape love—selfless, sacrificial love for others—serves as a critical foundation for navigating these tensions [19] [12]. This principled approach to love differs significantly from situational ethics, which prioritizes individual circumstances over defined moral character [12]. As technological capabilities in areas such as organ transplantation, nanotechnology, and experimental therapies advance, the Christian ethical framework must balance the sanctity of the human body, created in God's image, with the call to express compassion through medical intervention [19] [63].
This paper examines how agapeic ethics provides a coherent framework for resolving apparent conflicts between bodily integrity, resurrection beliefs, and technological intervention. We explore the theological foundations of these concepts and present quantitative data on emerging technologies, experimental protocols for assessing interventions, and ethical guidelines grounded in Christian virtue ethics. By synthesizing theological principles with scientific analysis, we provide researchers and drug development professionals with a robust framework for evaluating technological interventions through the lens of Christian love and responsibility.
Theological Foundations: Agape Love in Christian Bioethics
The Concept of Agape as a Ground Norm
Agape love represents a distinctive ethical framework within Christian thought, characterized by its volitional nature and sacrificial quality [23]. Unlike eros (passionate desire) or philia (friendship), agape embodies a deliberate choice to seek the good of others regardless of personal cost [23]. This concept finds its ultimate expression in Christ's sacrifice, providing a theological model for self-giving love in medical contexts [19]. In bioethics, agape manifests as the virtue of benevolence—the attitude of intending and doing good toward others through beneficence (charity) [12].
The operationalization of agape love in medical ethics requires moving beyond relativism, where love is defined by individual preference, toward a virtue ethics approach that roots moral decisions in defined character qualities [12]. As Pellegrino emphasizes, "It is the virtue of charity that above all shapes the whole of Christian medical morals, as it does every other aspect of moral life" [12]. This approach prioritizes the development of moral character in healthcare providers and researchers, ensuring that technological applications reflect both compassion and moral integrity.
Human Dignity and the Imago Dei
The Christian understanding of human dignity originates from the creation narrative in Genesis, which establishes that humans are created in God's image (Imago Dei) [19] [63]. This theological concept confers unique worth to every human person and establishes the body as deserving respect beyond its functional capacity. The doctrine of Imago Dei provides a crucial foundation for evaluating technological interventions, as it affirms the inherent value of human life regardless of health status, cognitive ability, or physical capacity [63].
The principle of respect for persons flows directly from this understanding, attaching greater proportional value to human life than to autonomy or privacy alone [63]. This contrasts with secular bioethical frameworks that often prioritize autonomy as the preeminent value, sometimes justifying procedures such as abortion or euthanasia based solely on self-determination [63]. Within the Christian framework, respect for human dignity limits autonomous choices that would violate the fundamental worth of the human person.
Bodily Resurrection and Physical Integrity
Orthodox Christian theology affirms the belief in bodily resurrection, which has historically raised questions about the compatibility of organ donation and other physical interventions with Christian doctrine [19]. Modern theological interpretations generally resolve this tension by emphasizing that bodily resurrection is not dependent on physical completeness at death [19]. This perspective acknowledges God's ability to restore the body in resurrection regardless of what transpires in earthly life, thereby allowing for medical procedures that involve bodily alteration when undertaken for morally legitimate purposes.
The body is understood not as a possession to be manipulated at will but as a sacred trust to be stewarded responsibly. This stewardship paradigm allows for therapeutic interventions that promote health and alleviate suffering while rejecting modifications that would undermine human dignity or treat the body as mere raw material [19] [63].
Ethical Tensions in Technological Intervention
The Principle of Double Effect in Medical Applications
The principle of double effect, derived from the work of St. Thomas Aquinas, provides an important ethical tool for evaluating medical interventions that have both beneficial and harmful consequences [63]. According to this principle, an action with both good and bad effects may be morally permissible if: (1) the action itself is morally good or neutral; (2) the bad effect is not the means by which the good effect is achieved; (3) the intention is solely for the good effect; and (4) there is proportionality between the good and bad effects [63].
A classic application of this principle in medical ethics involves a pregnant woman with uterine cancer whose treatment requires removal of the uterus, resulting in the unintended death of the fetus [63]. The death of the fetus, while foreseen, is not the means by which the mother's life is saved, making the procedure morally permissible within this framework. Similarly, this principle can be applied to evaluate emerging technologies where therapeutic benefits may involve unintended consequences for bodily integrity.
Agape Versus Autonomy in Medical Decision-Making
Christian bioethics emphasizes the principle of respect for persons over absolute autonomy [63]. While secular bioethics has increasingly elevated autonomy to "the preeminent value governing the actions of healthcare providers," Christian ethics recognizes that human dignity imposes limits on self-determination [63]. This distinction becomes particularly significant in contexts such as end-of-life decisions, reproductive technologies, and enhancements that may compromise fundamental aspects of human nature.
The agapeic framework redirects the ethical question from "What does the individual want?" to "What does love require in this situation?" This reorientation acknowledges our relational responsibility toward others within the human community, particularly toward the most vulnerable [12] [63]. For researchers and drug development professionals, this implies considering not only patient autonomy but also the broader impact of technological interventions on human flourishing and social relationships.
Table 1: Comparative Ethical Frameworks in Bioethics
| Ethical Framework | Central Principle | View of the Body | Approach to Technological Intervention |
|---|---|---|---|
| Agapeic Ethics | Benevolence and sacrificial love | Sacred trust created in God's image | Cautious support grounded in preservation of life and dignity |
| Principiism | Respect for autonomy, nonmaleficence, beneficence, justice | Subject of rights and preferences | Balance of competing principles through rational deliberation |
| Utilitarianism | Maximization of overall benefit | Instrument for achieving well-being | Support for interventions that produce net benefit |
| Virtue Ethics | Development of moral character | Locus of virtue and moral practice | Evaluation based on character qualities expressed |
Quantitative Analysis of Technological Interventions
Biodistribution of Nanoparticles in Medical Applications
Emerging medical technologies, particularly those involving nanotechnology, present new questions about bodily integrity and the ethical implications of internal distribution of synthetic materials. Quantitative analysis of nanoparticle biodistribution provides crucial data for evaluating the physical impact of these interventions.
Research on nanoparticle pharmacokinetics reveals distinct patterns of tissue distribution that vary by nanoparticle composition and size. Analysis of 2018 datasets characterizing graphene oxide, lipid, polymeric, silica, iron oxide, and gold nanoparticles demonstrates consistent accumulation patterns, with the highest concentrations typically found in the liver and spleen [64].
Table 2: Nanoparticle Biodistribution Coefficients (%ID/g) by Tissue Type
| Tissue Type | NBC Value (%ID/g) | Standard Deviation | Key Considerations |
|---|---|---|---|
| Liver | 17.56 | ± 4.32 | Primary clearance organ, high accumulation |
| Spleen | 12.10 | ± 3.85 | Immune function implications |
| Tumor | 3.40 | ± 1.25 | Targeted therapy potential |
| Kidney | 3.10 | ± 0.95 | Renal clearance pathway |
| Lungs | 2.80 | ± 1.15 | First-pass accumulation |
| Intestine | 1.80 | ± 0.65 | Enterohepatic circulation |
| Heart | 1.80 | ± 0.55 | Cardiovascular risk assessment |
| Pancreas | 1.20 | ± 0.45 | Endocrine function implications |
| Stomach | 1.20 | ± 0.40 | Limited absorption |
| Skin | 1.00 | ± 0.35 | Dermal exposure concerns |
| Muscle | 0.60 | ± 0.25 | Low perfusion tissues |
| Bones | 0.90 | ± 0.30 | Marrow interactions |
| Brain | 0.30 | ± 0.15 | Blood-brain barrier penetration |
Advanced quantification techniques using PET/MRI imaging with radiolabeled nanoparticles (e.g., 89Zr-IONP) enable precise tracking of distribution patterns, providing researchers with critical data for evaluating both efficacy and potential tissue toxicity [65]. These quantitative approaches allow for evidence-based assessment of how technological interventions interact with bodily systems at the molecular level.
Ethical Assessment Framework for Biodistribution Data
From a Christian ethical perspective, biodistribution data must be evaluated through the lens of agape love and respect for human dignity. Key considerations include:
- Potential for harm to vulnerable tissues: High accumulation in organs with limited regenerative capacity (e.g., brain, heart) warrants particular caution [64]
- Long-term effects on bodily integrity: Persistence of nanoparticles in tissues raises questions about chronic impacts on physiological function [64]
- Informed consent implications: Complex distribution patterns complicate comprehensive disclosure of risks [63]
The agapeic framework would support interventions demonstrating favorable distribution profiles with minimal impact on organs essential to human flourishing, while questioning technologies with unpredictable or potentially harmful distribution patterns that could compromise the functional integrity of the person.
Experimental Protocols for Ethical Technological Assessment
Quantitative Imaging Protocol for Intervention Tracking
The following detailed methodology enables precise quantification of interventional distribution, providing essential data for ethical evaluation:
Materials and Equipment:
- 89Zr-radiolabeled nanoparticles (50-100 nm diameter) [65]
- 3.0T PET/MR scanner with head and neck coil (12 channels) [65]
- 3D multi-echo gradient echo UTE sequence with cones k-space trajectory [65]
- Image processing software (MATLAB 2016a with MEDI toolbox) [65]
Experimental Procedure:
- Radiolabeling: Combine iron oxide nanoparticles (16.75 mg, 200 μL DI water) with 89Zr (1.01 mCi, 2 μL) in 1M oxalic acid and 2 μL of 1M Na2CO3 [65]
- Purification: Heat mixture at 120°C for 2 hours, purify using magnetic separation [65]
- Phantom Preparation: Construct gelatin cylinder with embedded plastic spheres containing increasing nanoparticle concentrations (2.5, 5, 10, 20, 30 mg/L) [65]
- Image Acquisition: Simultaneously acquire 10-minute time-of-flight static PET and MR data using specified parameters (TE = [0.148, 3.3, 5.6, 7.9] ms, TR = 13.2 ms, flip angle 12°, matrix 128×128, slice thickness 3 mm) [65]
- Data Analysis:
- Reconstruct PET images using TOF ordered subsets expectation maximization algorithm [65]
- Manually draw regions of interest on MR image slices [65]
- Calculate R2* using mono-exponential fit of magnitude images [65]
- Reconstruct quantitative susceptibility maps using Morphology Enabled Dipole Inversion toolbox [65]
This protocol enables correlation between nanoparticle concentration and multiple imaging parameters (89Zr-PET signal, R2*, quantitative susceptibility), providing comprehensive data on distribution patterns [65].
In Vivo Validation Protocol
For translational applications, the following in vivo protocol provides critical data on real-world distribution:
Materials and Equipment:
- Swine model (45-50 kg) [65]
- 5 French catheter (Slip-Cath Beacon Tip) [65]
- X-ray guidance system (Cios Alpha) [65]
- 89Zr-IONPs in saline (3.05 mCi per 25 mg IONPs in 10 ml total volume) [65]
Experimental Procedure:
- Catheter Placement: Under X-ray guidance, place catheter into common hepatic artery of supine swine [65]
- Baseline Imaging: Acquire pre-infusion PET/MR images [65]
- Infusion Protocol:
- Image Analysis:
This protocol validates the relationship between imaging parameters and actual nanoparticle concentration in living tissue, essential for predicting human distribution patterns [65].
Research Reagent Solutions for Ethical Technological Development
Table 3: Essential Research Materials for Ethical Technological Assessment
| Research Reagent | Function | Ethical Considerations | Example Application |
|---|---|---|---|
| 89Zr-radiolabeled nanoparticles | Enables precise quantification of biodistribution through PET imaging | Radiation exposure must be justified by potential benefit | Tracking tissue distribution of therapeutic nanoparticles [65] |
| Multi-echo gradient echo UTE sequences | Provides quantitative magnetic susceptibility mapping | Non-invasive nature respects bodily integrity | Quantifying iron oxide nanoparticle concentration in tissues [65] |
| Morphology Enabled Dipole Inversion (MEDI) toolbox | Reconstructs quantitative susceptibility maps from MR phase data | Open-source tool promotes transparency and collaboration | Calculating magnetic susceptibility values for concentration correlation [65] |
| Iron oxide nanoparticles (50-100 nm) | Serves as model system for magnetic drug carriers | Biocompatibility and clearance pathways must be established | Developing endovascular magnetic filtration devices for targeted chemotherapy [65] |
| 3.0T PET/MR systems | Enables simultaneous acquisition of metabolic and anatomical data | Combined radiation/MR exposure requires ethical justification | Correlating anatomical location with metabolic activity in intervention studies [65] |
Resolution Framework: Integrating Agape Ethics with Technological Advancement
Decision Matrix for Technological Interventions
The following conceptual framework provides researchers with a practical tool for evaluating specific technologies through the lens of agape ethics:
Applications to Specific Technological Domains
Organ Transplantation Ethics
Organ transplantation represents a paradigmatic case where agape ethics provides resolution to apparent tensions between bodily integrity and technological intervention. The Orthodox Church offers a nuanced position on organ transplantation, recognizing its life-saving potential while cautioning against reducing the process to a purely mechanical act [19]. This balance reflects the agapeic principle of honoring the dignity of both donor and recipient.
The Church's stance of cautious support for organ donation manifests Christian love and solidarity, while calling for careful, spiritually mindful approaches that respect both the sacredness of the body and individual conscience [19]. This framework acknowledges organ donation as a commendable expression of agape love—"Greater love has no one than this: to lay down one's life for one's friends" (John 15:13)—while maintaining that such acts must be voluntary, informed, and respectful of the divine gift of the body [19].
Emerging Nanotechnologies
For emerging nanotechnologies, the agapeic framework emphasizes the precautionary principle coupled with ongoing evaluation of distribution patterns and potential impacts on human flourishing. The quantitative biodistribution data presented in Section 4.1 enables researchers to make evidence-based assessments about the degree of bodily invasion and potential long-term consequences.
Christian ethics would support nanotechnology applications that demonstrate:
- Favorable distribution profiles with minimal accumulation in vulnerable tissues [64]
- Clear therapeutic benefits that outweigh potential risks [63]
- Reversibility or limited persistence in the body [64]
- Transparency in disclosure for informed consent [63]
This paper has presented a framework for resolving tensions between bodily integrity, resurrection beliefs, and technological intervention through the application of agape love in Christian medical ethics. By integrating theological principles with quantitative scientific assessment, we provide researchers and drug development professionals with practical tools for ethical evaluation.
The agapeic approach recognizes technological intervention as a legitimate expression of Christian love when directed toward healing and flourishing, while maintaining appropriate boundaries that respect the body as created in God's image. This framework neither uncritically embraces nor reflexively rejects technological advancement, but rather evaluates each intervention based on its capacity to promote genuine human good while respecting the fundamental dignity of the person.
As biomedical technology continues to advance, the Christian research community has an essential role in developing and applying ethical frameworks that balance innovation with responsibility, technological capability with moral wisdom, and individual benefit with communal good. Through this integration of agape ethics with scientific excellence, we honor both the calling to heal and the sacredness of the human person.
Agape love, a selfless, all-giving love distinct from romantic or familial affection, presents a transformative but often neglected framework for Christian medical ethics. In an era marked by significant health disparities, this foundational Christian virtue mandates a proactive commitment to justice and the common good within healthcare systems and research. The concept of agape, or compassionate love, is characterized by free choice for the other, cognitive understanding, valuing the other, and a responsive heart [66]. In the context of health disparities, agape love extends beyond individual clinical encounters to address systemic inequities in health outcomes, access to care, and the social determinants of health. This whitepaper establishes the theological and ethical foundation for agape as a core principle in medical research and practice, provides quantitative evidence of its impact, proposes methodologies for its integration, and outlines practical applications for researchers and drug development professionals committed to biblical justice in health.
Theoretical Framework: Agape as a Foundational Principle
Agape love represents a commitment to loving all persons—the oppressed and the oppressor, the victim and the perpetrator—reflecting Dr. Martin Luther King Jr.'s interpretation, which required recognizing evil acts without seeing any person as inherently evil [67]. This aligns with the "love ethic" described by scholar bell hooks, which utilizes all dimensions of love—care, commitment, trust, responsibility, respect, and knowledge—in daily life and actions for the collective good [66]. This ethic is applicable at a societal, whole-population level, making it particularly relevant for addressing systemic health disparities.
Within healthcare, this concept has been operationalized as "humanitarian love," understood as altruistic, non-erotic love that forms the basis for caring professions and enables inner healing and self-realization for patients [27]. Similarly, "social love" describes the motivation and actions of a system, organization, or institution, and the people working within them, aimed at increasing the wellbeing of another, self, community, and the environment [66]. For researchers and drug development professionals, this translates into a research ethic that prioritizes the health needs of the most marginalized communities, ensures equitable access to medical advancements, and consciously challenges systems of power that perpetuate health inequities.
Quantitative Evidence: The Impact of Love-Based Frameworks
Empirical research, though limited, demonstrates the tangible effects of integrating love-based frameworks into healthcare systems and professional practice. The psychosocial benefits for healthcare professionals and the potential for systemic transformation are particularly noteworthy.
Table 1: Psychosocial Impact of Humanitarian Love on Health Professionals
| Impact Dimension | Findings | Implication for Research |
|---|---|---|
| Professional Well-being | Fosters positive emotions, reduces burnout, emotional exhaustion, and compassion fatigue [27]. | Enhances sustainability of research teams working on health disparities. |
| Care Quality | Enhances ability to provide high-quality care and effectively support patient needs [27]. | Improves community engagement and trust in research initiatives. |
| Relational Capacity | Secure attachment styles in nursing students correlate with healthy love attitudes (e.g., storge, friendship love) [22]. | Informs team composition and leadership development for ethical research. |
A systematic literature review analyzing 16 studies with 2,045 participants confirmed that when healthcare professionals direct humanitarian love towards themselves, it fosters positive emotions, enhancing their ability to provide high-quality care. Conversely, directing this love towards patients helps reduce feelings of burnout and emotional exhaustion [27]. Furthermore, studies on attachment styles and love attitudes among healthcare students reveal a negative correlation between secure attachment and manic, possessive love, and a positive correlation between secure attachment and storge (friendship love) [22]. This suggests that cultivating secure relational capacities is foundational for expressing agape in professional contexts.
Table 2: Public Health System Challenges Addressed by Social Love
| Systemic Challenge | Current Neglect | Potential of Social Love |
|---|---|---|
| Provider Experience | Underfunding, technological demands, compassion fatigue, burnout [66]. | Re-imagining systems to promote generative relationships and reduce burnout. |
| Population Health | Entrenched health inequalities, poor life trajectories, burden of chronic disease [66]. | Acting as a lens for public health policymaking to improve population wellbeing. |
| Violence as a Health Issue | A public health approach often neglects relational and communal dimensions [66]. | Disrupting pathways to violence through community connection and justice. |
The prevailing biomedical model often neglects these relational concepts to the detriment of both providers and recipients of care [66]. For researchers, this evidence underscores that integrating agape is not merely an ethical imperative but a pragmatic strategy for sustaining the workforce and improving the efficacy of health interventions.
Methodological Integration: Experimental Protocols and Research Design
Integrating agape into medical research requires rigorous methodologies that blend quantitative, qualitative, and community-engaged approaches. Below are detailed protocols for key research areas.
Protocol 1: Measuring the Physiological Impact of Agape-Informed Care
This protocol quantifies how agape-informed clinical interactions affect patient physiology and stress biomarkers.
- Objective: To determine if clinical care from providers trained in agape principles reduces biomarkers of stress and inflammation in patients from disparity populations.
- Population: 200 patients from racially/ethnically marginalized communities with hypertension, recruited from community health centers.
- Intervention Group: Receives care from clinicians who have undergone a 4-week "Agape in Practice" curriculum focusing on compassionate communication, empathy, and patient empowerment [27].
- Control Group: Receives standard care from clinicians without this training.
- Primary Outcomes:
- Biomarkers: Serum cortisol, C-reactive protein (CRP), and interleukin-6 (IL-6) measured at baseline, 3, and 6 months.
- Psychosocial Scales: Perceived empathy (Consultation and Relational Empathy Scale), trust in provider, and self-efficacy measured via validated scales.
- Data Analysis: Linear mixed models to assess group differences in biomarker trajectories over time, controlling for baseline covariates.
Protocol 2: Community-Based Participatory Research (CBPR) for Drug Development
This protocol ensures agape love—through respect, commitment, and knowledge—is operationalized in the research process itself, prioritizing community voice.
- Phase 1: Community Identification & Partnership
- Action: Identify a community experiencing a significant health disparity (e.g., higher diabetes prevalence).
- Method: Form a Community Advisory Board (CAB) comprising patients, faith leaders, and community health workers. The research team and CAB co-sign a partnership covenant outlining principles of shared power, accountability, and mutual respect [66].
- Phase 2: Priority Setting & Research Co-Design
- Action: Define the most pressing research question.
- Method: Conduct facilitated dialogue sessions using the "Check and Challenge" model [66] to ensure the research addresses the community's definition of the "common good." Research protocols and consent forms are co-developed and reviewed for cultural and linguistic appropriateness.
- Phase 3: Implementation & Capacity Building
- Action: Conduct the research.
- Method: Employ and train community members as research staff. Data collection respects community norms and schedules.
- Phase 4: Dissemination & Benefit Sharing
- Action: Share results and ensure benefits.
- Method: Results are first shared with the community in accessible formats. Profits from any discoveries are partially reinvested into community health infrastructure, fulfilling the "justice" component of agape.
The following workflow diagram visualizes this agape-informed CBPR process:
The Scientist's Toolkit: Research Reagents for Ethical Engagement
Table 3: Essential Materials and Tools for Agape-Informed Research
| Item/Tool | Function in Research | Ethical Rationale |
|---|---|---|
| Community Advisory Board (CAB) | A structured group of community stakeholders that provides oversight and guidance throughout the research process. | Embeds commitment, trust, and knowledge (hooks' love ethic) into project governance [66]. |
| Validated Psychosocial Scales | Tools like the Compassionate Love Scale [66] or LAS [22] to measure relational variables. | Provides quantitative data on the impact of agape, moving it from abstract concept to measurable variable. |
| Partnership Covenant | A formal document co-signed by researchers and the CAB outlining shared principles, data ownership, and benefit-sharing. | Operationalizes responsibility and respect, preventing exploitation and ensuring justice [66]. |
| Cultural & Linguistic Translation Services | Professional services to ensure all research materials are accessible and appropriate for the target population. | Demonstrates care and values the other by honoring the community's language and context [27]. |
Practical Applications and Implementation Roadmap
For researchers and drug development professionals, translating the principle of agape into action involves concrete steps across the research continuum.
- 5.1. Research Priority Setting: Advocate for and allocate internal research funds to diseases that predominantly affect disadvantaged populations, even if market returns are lower. This embodies agape's self-giving nature.
- 5.2. Clinical Trial Design: Implement inclusive trial protocols that reduce barriers to participation (e.g., providing transportation, conducting visits in community settings). This actively works against systemic injustice in healthcare access.
- 5.3. Data Interpretation and Dissemination: Analyze data through an equity lens, explicitly reporting outcomes by race, ethnicity, socioeconomic status, and other relevant disparity indicators. Share findings with participants and communities in accessible formats, honoring the "knowledge" dimension of hooks' love ethic [66].
The following pathway outlines the strategic implementation of agape principles from discovery to public health impact:
Agape love, far from being a vague spiritual ideal, provides a robust and actionable mandate for addressing health disparities through justice and the pursuit of the common good. By integrating this principle into the core of medical ethics, research design, and professional practice, scientists and drug development professionals can contribute to a more equitable and compassionate healthcare landscape. The empirical evidence suggests that such an approach not only fulfills an ethical imperative rooted in Christian tradition but also enhances the effectiveness and sustainability of healthcare systems. As articulated in the prophetic mandate, the requirement is clear: "to do justice, and to love kindness, and to walk humbly with your God" (Micah 6:8). For the research community, this means building systems and generating knowledge that actively dismantles disparities, honoring the inherent worth of every individual through a committed, strategic, and selfless love.
In the context of Christian medical ethics, the concept of agape love represents a selfless, sacrificial, and unconditional love that intentionally desires another's highest good [68]. This profound ethical foundation often compels healthcare professionals and researchers to operate with a level of commitment that can paradoxically lead to burnout, a state of emotional exhaustion, depersonalization, and reduced personal accomplishment [69]. For those in demanding fields like drug development, where the pursuit of healing aligns with missional purpose, the tension between sacrificial care and sustainable practice becomes particularly acute. This whitepaper provides an in-depth technical analysis of evidence-based strategies to mitigate burnout while maintaining the ethical imperative of agape love, which is characterized by its willful nature as a choice rather than merely an emotion [68]. The systematic implementation of these protocols ensures that those engaged in the noble work of healing can persist in their vocations without depleting the very resources that enable their compassionate service.
The Burnout Crisis in Healthcare and Research
Prevalence and Impact
Burnout has reached alarming levels in healthcare and research environments, with recent data indicating that approximately 63% of practitioners experienced burnout in 2022, a significant increase from 44% in 2017 [70]. This syndrome extends beyond subjective distress to produce measurable detrimental effects on both professional performance and patient outcomes. Research demonstrates that burnout leads to reduced patient satisfaction, increased medical errors, and decreased quality of care [69]. For the individual professional, consequences include physical and mental health problems, poor social relationships, reduced job satisfaction, and increased absenteeism [69].
Table 1: Burnout Prevalence and Impact in Healthcare
| Metric | Findings | Source |
|---|---|---|
| Burnout Prevalence (2022) | 63% of healthcare practitioners | [70] |
| Burnout Prevalence (2017) | 44% of healthcare practitioners | [70] |
| Projected Clinician Shortage (by 2034) | 37,800 to 124,000 fewer clinicians | [70] |
| Key Burnout Dimensions | Exhaustion, cynicism, reduced professional efficacy | [71] |
| Impact on Patient Care | Reduced satisfaction, increased errors, decreased quality | [69] |
Root Causes and Contributing Factors
The etiology of burnout is multifactorial, emerging from systemic organizational structures and individual vulnerabilities. Key contributing factors include excessive workload, inadequate support, lack of control and autonomy, stressful work environments, and moral injury from the inability to meet patient needs and demands [69]. A longitudinal study of Swedish teachers—another high-touch profession with parallels to healthcare—identified low self-efficacy [OR 0.42; CI 0.26–0.68] and high job demands [OR 1.97; CI 1.02–3.8] as the strongest explanatory variables for burnout development [71]. This research further found that increased job demands during follow-up were associated with an increased level of burnout [OR 3.41; CI 1.73–6.69], while increased decision latitude was associated with a decreased level of burnout [OR 0.51; CI 0.30–0.87] [71].
Theological Foundation: Agape Love as Sustainable Ethic
Defining Agape Love
Agape love represents the highest form of unconditional love in Christian theology, distinguished from other forms of love by its selfless, sacrificial, and unconditional nature [68] [72]. The United States Conference of Catholic Bishops defines agape as "the expression of love turned outward toward concern for others" [72]. Unlike emotional affection (storge), romantic love (eros), or friendship (philia), agape is fundamentally volitional rather than emotional—a deliberate striving for another's highest good demonstrated through action [68]. This theological concept finds its ultimate expression in the Christian narrative of Jesus's sacrificial death, embodying unconditional love given freely without expectation of return [72].
Implications for Sustainable Care
Properly understood, agape love provides a theological framework for sustainable care practices rather than justification for self-destruction. As 1 Corinthians 13:4-7 describes, "Love is patient, love is kind... it is not self-seeking" [68]. This characterization suggests that authentic agape requires wisdom, boundaries, and sustainability rather than impulsive self-sacrifice that leads to depletion. The distinction is crucial: while agape love is fundamentally sacrificial, it is not destructive of the caregiver's core capacity to continue loving. From an ethical perspective, agape love serves as the foundation for Christian morality, fostering humility, forgiveness, and reconciliation while driving movements for justice and inspiring action against suffering [73]. This theological understanding informs the ethical imperative for implementing sustainable practices that enable perseverant, rather than temporary, sacrificial service.
Evidence-Based Interventions: A Multi-Level Approach
Organizational-Level Interventions
Organizational factors represent the most significant contributors to burnout and thus require systematic intervention. Evidence suggests that managing workload through limitation of duty hours, adequate staffing levels, and flexible work schedules effectively reduces burnout [69]. A structured approach to workload management should include:
- Duty Hour Limitations: Implementation of reasonable shift durations with mandatory rest periods between shifts, particularly in research environments with time-sensitive experiments [69].
- Adequate Staffing Models: Utilization of predictive analytics to align staffing with workload demands, preventing chronic understaffing [69].
- Flexible Scheduling: Accommodation of individual circadian rhythms and personal commitments through flexible work arrangements where feasible [69].
Beyond workload management, organizational culture transformation is essential. This includes developing supportive leadership, fostering peer support communities, and creating a culture of openness where practitioners can seek help without fear of stigma or negative consequences [69]. Research indicates that doctors who rated their supervisor's leadership behavior highly showed lower levels of burnout, intention to leave their job, and higher levels of professional fulfilment [69]. Practical implementations include:
- Leadership Development Programs: Training for principal investigators and research directors in supportive leadership practices.
- Structured Peer Support: Establishment of mentoring programs, virtual book clubs, and regular wellness activities that build community [69].
- Psychological Safety Initiatives: Creation of confidential reporting systems for burnout symptoms without professional repercussions.
Table 2: Organizational-Level Interventions for Burnout Prevention
| Intervention Category | Specific Strategies | Evidence of Effectiveness |
|---|---|---|
| Workload Management | Duty hour limitations, adequate staffing, flexible schedules | Systematic review shows limitation of duty hours is effective [69] |
| Leadership Development | Supportive leadership training, responsive management | Physicians rating supervisors highly had lower burnout [69] |
| Peer Support | Mentoring programs, virtual book clubs, group activities | Being part of a community beneficial; mentoring effective [69] |
| Work Culture | Regular meal breaks, paid time off, personal/professional balance | Culture encouraging balanced life vital [69] |
Individual-Level Interventions
While systemic factors predominate, individual practices play a complementary role in burnout resilience. The emerging field of lifestyle medicine offers evidence-based approaches that directly impact burnout metrics. Research demonstrates that healthcare professionals who extensively practiced lifestyle medicine had a 43% lower chance of experiencing burnout [70]. Specific interventions include:
- Physical Activity: Regular moderate-intensity exercise, with a target of 150 minutes per week, significantly reduces stress and improves resilience.
- Whole-Food, Plant-Predominant Eating Patterns: Nutritional interventions focused on anti-inflammatory foods that support neurological health and stress response systems.
- Restorative Sleep: Implementation of sleep hygiene protocols ensuring 7-8 hours of quality sleep, critical for emotional regulation and cognitive function.
- Stress Management Techniques: Mindfulness meditation, breath work, and other contemplative practices that modulate physiological stress responses [70].
Additionally, cognitive-behavioral approaches that enhance self-efficacy demonstrate significant protective effects against burnout. The longitudinal study of teachers found that low self-efficacy was the strongest explanatory factor for burnout, remaining significant after adjustment for baseline burnout [71]. This suggests that interventions targeting perceived self-efficacy—such as mastery experiences, vicarious learning, and positive feedback—may substantially impact burnout trajectories.
The Lifestyle Medicine Protocol
The American College of Lifestyle Medicine (ACLM) has developed a structured approach that demonstrates exceptional efficacy in reducing burnout among healthcare professionals [70]. Of 482 surveyed ACLM members, 90% reported that integrating lifestyle medicine into their practice positively impacted their professional satisfaction [70]. Key elements include:
- Therapeutic Lifestyle Interventions: Utilizing lifestyle changes as primary treatment modalities for chronic conditions, creating greater professional meaning and effectiveness [70].
- Holistic Patient Engagement: Addressing patients' emotional and lifestyle dimensions alongside physical complaints, creating more fulfilling clinician-patient relationships [70].
- Personal Practice: Implementing lifestyle medicine principles in one's own life, with practitioners reporting significant improvements in well-being from increased physical activity, plant-based nutrition, and stress management [70].
This approach enables healthcare professionals to recapture the meaningful aspects of their vocation while modeling healthy behaviors for their patients.
Experimental Design for Burnout Research
Methodological Framework
Rigorous investigation of burnout interventions requires sophisticated experimental designs that can identify effective components and their interactions. The Design of Experiments (DoE) methodology provides a systematic approach to optimize interventions by simultaneously testing multiple factors rather than the traditional one-factor-at-a-time approach [74] [75]. This methodology is particularly valuable for complex phenomena like burnout, where multiple interacting elements contribute to outcomes.
The fundamental steps in DoE include:
- Define the Objective: Clearly articulate the research question and primary outcome measures (e.g., reduction in Maslach Burnout Inventory scores) [75].
- Define the Experimental Domain: Identify factors to be investigated and their ranges based on prior knowledge [75].
- Select the Experimental Design: Choose appropriate factorial designs (full, fractional, or Plackett-Burman) that balance comprehensiveness with feasibility [74] [75].
- Develop the Statistical Model: Formulate a mathematical model representing the relationship between input variables and response outcomes [75].
- Run the Design and Perform Statistical Analysis: Execute the experimental protocol and analyze results using ANOVA and other statistical methods to identify significant effects [75].
Sample Experimental Protocol
To illustrate the application of DoE in burnout intervention research, consider this sample protocol adapted from pharmaceutical development methodology [75]:
Table 3: Experimental Factors and Levels for Burnout Intervention Study
| Input Factor | Unit | Lower Limit | Upper Limit |
|---|---|---|---|
| Workload Intensity | % of current | -20% (-1) | Baseline (+1) |
| Peer Support Sessions | sessions/month | 1 (-1) | 4 (+1) |
| Autonomy Enhancement | level | Low (-1) | High (+1) |
| Mindfulness Training | minutes/day | 10 (-1) | 20 (+1) |
| Sleep Extension | hours/night | 6 (-1) | 7.5 (+1) |
A fractional factorial design (2^5-2^III) would enable efficient screening of these factors with eight experimental runs, each representing a unique combination of factor levels [75]. The response variable would be measured using standardized burnout metrics, such as the Maslach Burnout Inventory, with additional measures of professional efficacy and job satisfaction.
Implementation Framework and Visualization
Integrated Burnout Prevention System
The following workflow diagram illustrates the systematic integration of agape ethics with evidence-based burnout prevention strategies:
Research Reagent Solutions for Burnout Studies
Table 4: Essential Methodological Tools for Burnout Intervention Research
| Research Tool | Function | Application Example |
|---|---|---|
| Maslach Burnout Inventory (MBI) | Gold standard assessment of burnout dimensions | Primary outcome measure in intervention studies [69] [71] |
| Design of Experiments (DoE) | Systematic optimization of multiple intervention factors | Simultaneously test workload, autonomy, support interventions [74] [75] |
| Fractional Factorial Designs | Efficient screening of multiple factors with minimal runs | Identify most impactful elements from multi-component interventions [75] |
| Response Surface Methodology | Modeling complex relationships between variables and outcomes | Optimize intervention dosage and timing [74] |
| Self-Efficacy Scales | Assessment of perceived capability in work domains | Measure impact on burnout vulnerability [71] |
| Longitudinal Cohort Design | Tracking burnout trajectories over extended periods | Assess intervention sustainability [71] |
The integration of agape love ethics with evidence-based burnout prevention strategies creates a sustainable framework for sacrificial care in medical research and practice. By implementing systematic organizational changes, individual resilience practices, and lifestyle medicine principles, healthcare professionals can maintain their vocational commitment while preserving their capacity for compassionate service. The experimental methodologies outlined provide rigorous tools for developing and optimizing these interventions, ensuring that those who dedicate themselves to the healing mission can do so with enduring effectiveness and personal well-being. This alignment of ethical commitment with scientific evidence offers a promising path forward for addressing the burnout crisis while honoring the sacred calling of healthcare service.
Agape in Dialogue: Validating its Role Alongside Secular Bioethical Frameworks
Within the landscape of clinical bioethics, principlism offers a dominant framework for decision-making, built upon the four tenets of autonomy, beneficence, nonmaleficence, and justice. However, from the perspective of Christian medical ethics, this framework can appear fragmented, potentially overlooking the spiritual good of the person. This whitepaper posits that the Christian concept of agape—self-giving, unconditional love—serves not merely as a fifth principle, but as a foundational virtue that informs, integrates, and transcends the four principles. Agape provides a coherent moral identity for the healthcare professional, reorients the goals of patient care toward authentic human flourishing, and offers a robust, person-centered framework for navigating complex ethical dilemmas in research and clinical practice, particularly where principles conflict.
Principlism, as articulated by Beauchamp and Childress, provides a widely adopted framework for biomedical ethics, particularly in pluralistic societies [76]. Its four principles offer a common language for ethical deliberation:
- Respect for Autonomy: Acknowledges the patient's right to self-determination and requires informed consent without controlling influences [77] [76].
- Beneficence: The obligation to act for the patient's benefit, promoting welfare and positive requirements to help [77] [78].
- Nonmaleficence: The duty to "do no harm," avoiding actions that may injure the patient, either through commission or omission [77] [78].
- Justice: The principle of fairness, requiring that persons be treated equally and without discrimination in the distribution of benefits and risks [77] [78].
While these principles provide valuable action guides, they are often presented as prima facie duties, meaning they are binding unless they conflict with a stronger obligation [76]. In clinical reality, such conflicts are frequent (e.g., a patient's autonomous choice may conflict with a physician's view of what is beneficial). Principlism itself offers no meta-framework for resolving these conflicts, which can lead to an ad-hoc balancing act that risks reducing ethics to a technical calculus [77] [76]. This approach can commodify healthcare, viewing patients as "containers of disease" rather than whole persons on a spiritual journey [79]. A technical, principle-driven approach may secure a biomedical good but can fail to achieve the patient's spiritual good—knowing, loving, and serving God, which is central to human flourishing in the Christian tradition [79].
Agape as the Foundational Virtue
In contrast to a rule-based system, agapism proposes that love is the single absolute and guiding principle in Christian ethics [80]. Rooted in Jesus's teaching that the greatest commandment is to "love your neighbour as yourself" (Matthew 22:39), agape is a self-sacrificial, unconditional love that wills the good of the other, regardless of personal liking [80]. Joseph Fletcher's situation ethics, though not without theological critique, brought this concept to modern bioethics, arguing that all moral rules are only relative to love and should be set aside if love is better served [80] [12].
Agape functions not merely as a principle but as a virtue—a habitual inward disposition to act, feel, and think in morally good ways [12]. Edmund Pellegrino, a renowned Catholic bioethicist, argued that the virtue of charity (caritas) shapes the whole of Christian medical morality, integrating moral character with action [12]. This virtue-based approach, or aretaic ethics, focuses on the substance of a person's morality, asserting that right action flows from a character formed by love [12] [81]. The following diagram illustrates how agape serves as the foundational virtue from which the four principles are derived and applied.
A key differentiator between agapism and secular principlism is the foundational source of moral authority. Secular ethics often seeks an objective foundation in human reason, sentiment, or consensus [82]. Theological ethics, however, grounds its foundation in the nature and character of God. This resolves the Euthyphro Dilemma—whether God commands something because it is good, or it is good because God commands it—by asserting that God's will is controlled by God's nature, which is essentially loving and good [82]. Therefore, obligations flow from a divine nature of love, providing a non-arbitrary foundation for human rights and dignity, often articulated as humans being created in God's image or as bestowed with worth by being loved by God [82].
How Agape Informs and Transforms the Four Principles
Agape love does not discard the four principles but rather fills them with deeper meaning and provides a telos, or ultimate end, for their application. The following table summarizes how agape reorients each principle.
Table 1: The Transformation of Ethical Principles through Agape
| Ethical Principle | Secular Principlist Application | Application Informed by Agape |
|---|---|---|
| Autonomy | Respect for self-determination; obtaining informed consent as a legal and ethical procedure [77] [76]. | Love-driven respect: Autonomy is respected as a reflection of the God-given dignity of the person. Consent becomes part of a covenantal dialogue, honoring the patient's spiritual journey and ultimate good [77] [79]. |
| Beneficence | Acting to provide a "medical benefit," often defined in biomedical terms (e.g., prolonging life, curing disease) [77] [76]. | Seeking the spiritual good: The ultimate benefit is the patient's holistic well-being and human flourishing (beatitudo), which may involve accepting palliative care to "seek the Face of Jesus" rather than pursuing futile treatments [79]. |
| Nonmaleficence | Avoiding physical or psychological harm; a calculus of risks and benefits [77] [76]. | Expanded horizon of harm: The greatest harm is separation from God. Actions consider spiritual harm, and the principle of double effect is applied with love as the primary intention [77] [12]. |
| Justice | Fair distribution of scarce resources and treatments based on need, merit, or social contribution [77] [78]. | Love distributed: Justice is "love distributed" [80]. It demands a preferential option for the vulnerable, recognizing the intrinsic worth bestowed on every person by God's love, not their capacities [80] [82]. |
Autonomy Transformed by Love
From an agape perspective, respect for autonomy springs from the intrinsic and unconditional worth of every person, who is created in the image of God [82]. This moves informed consent beyond a transactional, legalistic event to a covenantal dialogue within a healing relationship [79]. The clinician, motivated by love, seeks to understand the patient's values, fears, and spiritual goals. The classic case of a Jehovah's Witness refusing a life-saving blood transfusion demonstrates this shift. Principlism frames this as a conflict between autonomy and beneficence [76]. Agape, while respecting the patient's autonomous choice, frames it through a broader understanding of harm and benefit, engaging the patient's deeply held religious convictions with compassion and seeking their spiritual good even in the face of physical death [76].
Beneficence and Nonmaleficence Guided by Spiritual Good
Agape redefines what constitutes a true "benefit." The biomedical good is subordinate to the spiritual good. In end-of-life care, the most beneficent action may not be the most technologically aggressive one, but the one that allows a patient to achieve what the narrative of Mary exemplifies: to peacefully "center all of my attention and prayers on seeking the Face of Jesus" [79]. Similarly, nonmaleficence expands to consider spiritual harm. Fletcher's extreme example of a family killing a crying baby to save the group from bandits is logically consistent with his situation ethics but is theologically problematic [80] [12]. A virtue-based agapism would operate within moral boundaries, ensuring that the intention of love is guided by a formed character and respect for the sanctity of life [12]. The doctrine of double effect, used to justify actions with a foreseen but unintended harmful effect (e.g., high-dose opioids for pain that may hasten death), finds its moral coherence when the primary intention is the loving act of alleviating suffering [77].
Justice as Love Distributed
Fletcher explicitly stated that "love and justice are the same, for justice is love distributed" [80]. A secular approach to justice might allocate resources based on utilitarian calculations. An agape-informed justice, however, is inherently biased toward the vulnerable, the dependent, and the marginalized, because it sees in them the bestowed worth of being loved by God [82]. This perspective challenges researchers and drug developers to consider not only the market potential of a therapy but also its impact on underserved populations and those with rare diseases. Justice becomes the systematic expression of love across a community, ensuring that the benefits of medical progress are distributed with a particular care for the "least of these."
An Integrated Model for Ethical Decision-Making
The following diagram and protocol outline a methodology for applying an agape-informed ethical framework to clinical and research dilemmas. This model integrates the assessment of principles with the foundational virtue of agape and the telos of human flourishing.
Experimental/Ethical Analysis Protocol:
- Situation Assessment: Gather all relevant medical, psychosocial, and spiritual facts. Identify the key stakeholders and their values.
- Principlist Analysis: Analyze the case using the four principles of autonomy, beneficence, nonmaleficence, and justice. Clearly identify where principles align and where they conflict (e.g., patient autonomy vs. physician's duty of beneficence).
- Agape Intervention: Apply the virtue of agape as the foundational lens. This step involves:
- Virtue Examination: The healthcare professional reflects on their own character and intentions, asking, "What does a disposition of self-giving love require here?"
- Telos Reframing: Shift the focus from resolving the principle conflict to a broader question: "What course of action best serves the patient's ultimate good and human flourishing (beatitudo)—their knowing, loving, and serving God, even in illness and death?" [79].
- Spiritual Discernment: Engage the patient (if possible) and family in a dialogue about their spiritual needs and goals, viewing them as persons with intrinsic dignity, not problems to be solved.
- Integrated Re-evaluation: Reconsider the four principles in light of the insights gained from the agape lens. Autonomy becomes respect for the person's spiritual journey; beneficence is defined by the spiritual good; nonmaleficence considers spiritual harm; justice ensures the care plan reflects a fair and loving distribution of resources and attention.
- Action and Reflection: Choose the course of action that best coheres with an agape-informed integration of the principles. After implementation, reflect on the outcome to further cultivate the virtue of charity in future practice.
The Scientist's Toolkit: Research Reagents for Ethical Analysis
For researchers and drug development professionals engaging with this framework, the following "reagents" are essential conceptual tools.
Table 2: Essential Research Reagents for Agape-Informed Ethical Analysis
| Research Reagent | Function in Ethical Analysis |
|---|---|
| The Healing Relationship Model [79] | Serves as the primary culture medium for analysis, framing the clinical encounter as a covenant between a vulnerable patient and a healer who promises to care, moving beyond a transactional contract. |
| Virtue Ethics Framework [12] [81] | The catalyst for moving from rule-based ethics to character-based ethics. It focuses on cultivating the virtues (e.g., compassion, integrity) necessary to consistently act with agape. |
| Principle of Double Effect [77] [76] | An analytical tool for distinguishing between intended and merely foreseen consequences of an action, ensuring that the primary intention remains loving (e.g., pain relief) even when a negative effect (e.g., respiratory depression) is foreseen. |
| Human Flourishing (Eudaimonia/Beatitudo) Telos [79] | The defined endpoint or goal of all ethical decision-making. It ensures that the "success" of an intervention is measured not merely by biomarker data but by its contribution to the patient's holistic well-being and spiritual journey. |
| Narrative Ethics Methodology | A qualitative assay for understanding patient values. It involves actively listening to the patient's story to comprehend their understanding of illness, dignity, and what constitutes a good life and death, thereby informing the application of agape. |
In an era of advanced medical technology and complex care, the four principles of bioethics remain necessary but insufficient for a holistic practice of medicine. They provide a valuable checklist but lack a unifying soul. Agape love, understood as the foundational theological virtue of charity, provides that soul. It informs the principles by giving them a Christ-centered meaning, integrates them when they conflict by providing a telos of human flourishing, and ultimately transcends them by shifting the focus from solving ethical problems to serving persons in their totality. For the Christian researcher, clinician, or administrator, embracing this framework transforms professional practice from a technical occupation into a healing ministry—a participation in the love of Christ that accompanies the sick and the vulnerable on their journey, protecting their dignity and promoting their ultimate good.
The concept of agape love, rooted in Christian theology and ethics, represents a selfless, sacrificial, and unconditional commitment to the flourishing of others. This paper argues for the intentional integration of agape as a complementary ethical framework within public health ethics, particularly in domains of community health and ecological care. Agape provides a motivational foundation and relational paradigm that extends beyond conventional bioethical principles, framing health not merely as the absence of disease but as the holistic well-being of persons and the planetary systems they inhabit. Within Christian medical ethics research, agape offers a theological grounding for understanding health responsibilities as manifestations of divine love expressed through human action [12].
Contemporary public health faces dual challenges: addressing persistent health disparities within human populations and responding to the growing ecological crisis that threatens health determinants. Agape love, conceptualized as "neighborly love" and a "disinterested love of neighbor for her or his own sake," provides a moral framework for addressing these interconnected challenges by creating and preserving community [24]. This paper explores how agape love informs both the goals of public health and the means by which they are pursued, with particular relevance for researchers, scientists, and drug development professionals seeking to align their work with broader commitments to human dignity and ecological flourishing.
Theoretical Foundations of Agape Love
Conceptual Definitions and Distinctions
Agape love represents a distinctive moral framework characterized by several core features:
- Unconditional Regard: Agape entails a disinterested love of neighbor for their own sake, not contingent upon personal characteristics, merit, or reciprocity [24].
- Volitional Commitment: Unlike emotional affections, agape operates as a willed commitment to seek the good of others, reflecting the Hebrew concept of 'ahab with its volitional element [23].
- Comprehensive Scope: Agape extends beyond interpersonal relationships to encompass care for the broader creation, recognizing that "both human and non-human others share in divine creationism" [23].
This understanding contrasts with other forms of love in Greek philosophy—eros (passionate desire), philia (friendship), and storge (familial affection)—through its emphasis on self-giving rather than fulfillment or mutual advantage [23] [48]. In bioethical contexts, agape finds expression through the virtue of benevolence, defined as "the attitude of intending or the action of doing good toward others," which guides ethical action through moral character rather than subjective preference alone [12].
Agape in Theological and Ethical Traditions
Agape love finds resonance across multiple religious traditions that inform global health ethics:
- Christian theology positions agape as the "integrating centre of the whole of Christian faith and ethics," essential to any conceivable Christian ecological ethic [23].
- Jewish tradition emphasizes Tikkun Olam (repairing the world) as a sacred duty reflecting the partnership between God and humanity in caring for the earth [23].
- Islamic tradition views the natural world as signs (ayah) of God's existence and wisdom, with environmental care representing an expression of gratitude for divine gifts [23].
These traditions collectively affirm that caring for creation constitutes a "morally and divinely imposed duty" that bears practical testimony to love for God, fellow humans, and non-human others [23].
Table 1: Conceptual Frameworks of Love in Ethical Traditions
| Concept | Definition | Ethical Application | Tradition |
|---|---|---|---|
| Agape | Selfless, sacrificial love for others without expectation of return | Grounds obligation to neighbor and creation | Christian Ethics |
| Tikkun Olam | "Repairing the world" through human partnership with God | Environmental responsibility as sacred duty | Jewish Tradition |
| Ayah | Natural world as signs of God's existence and wisdom | Respect and protection of creation | Islamic Tradition |
| Benevolence | Virtue of intending and doing good toward others | Guides ethical action through moral character | Virtue Ethics |
Agape Love in Community Health Practice
Operationalizing Agape in Healthcare Delivery
Community health organizations explicitly grounded in agape principles demonstrate practical models for integrating this ethic into healthcare delivery. Agape Family Health exemplifies this approach through its commitment to "health for all," which translates agape love into concrete institutional practices [83]:
- Inclusive Access: Providing healthcare services "regardless of socio-economic status" with particular outreach to "underserved and vulnerable populations" [83].
- Comprehensive Care: Delivering integrated services spanning "primary care, behavioral health services, women's health, pediatric services, preventive care, vaccinations, chronic disease management, to substance abuse services" [83].
- Patient-Centered Approach: Fostering "personalized care based on unique needs" through collaborative relationships that encourage "active participation" in health journeys [83].
Similarly, Agape Health Services implements this ethic through its mission to provide "high quality, comprehensive, coordinated primary healthcare" with special attention to patients regardless of "ability to pay and without judgement" [84]. These operational models demonstrate how agape love moves beyond abstract principle to shape service delivery structures, clinical relationships, and institutional priorities.
Addressing Structural Inequities through Agape
Agape love provides a critical lens for identifying and responding to structural injustices that produce health disparities. As Dr. Patrick Smith observes in his Paul Ramsey Award lecture, agape compels attention to the ways "a significant indicator of health outcomes is based on zip codes" and the "deep health and health care disparities" that divide communities "along racial and socioeconomic lines" [24]. This recognition frames health equity not as a technical problem alone but as a moral imperative rooted in the "inescapable network of mutuality" that binds human communities [24].
Agape-informed public health ethics thus directs attention to the social determinants of health and advocates for policies that promote health equity. This includes actively engaging "in health policy discussions at the local and state level" to "influence policies that promote health equity, improve access to healthcare services, and address the social determinants of health" [83]. The relational anthropology underlying agape love recognizes that human flourishing depends upon social conditions that enable health, positioning healthcare professionals as advocates for systemic change.
Agape Love in Ecological Care
Theological Foundations for Environmental Ethics
Agape love provides a compelling theological foundation for environmental ethics by reconceptualizing the relationship between humanity and the natural world. Drawing upon ecological liberation hermeneutics, this perspective recognizes "the mutual interactions between social systems and ecological systems and the inseparability of social justice and injustice from ecological justice and injustice" [23]. Leonardo Boff extends the "option for the poor" to include the environment, contending that "spirituality embodies an attitude which places life at the centre and defends and promotes life against reductionism and death in all its forms" [23].
This framework employs the eco-justice principles of interconnectedness and purpose to articulate humanity's moral relationship with creation. It recognizes that "both human and non-human others share in divine creationism" and are "interconnected by a common origin and experience in which both humans and nature are oppressed and share the common hope of redemption" [23]. Agape love thus expands the moral community beyond human persons to encompass the broader creation, affirming the intrinsic value of non-human life and ecosystems.
Practical Applications in Ecological Stewardship
The integration of agape love into ecological ethics finds concrete expression in practices of environmental care. Research in Rivers State, Nigeria demonstrates how Christian communities can operationalize agape through "proper waste management, keeping both private and public spaces clean" as a "morally and divinely imposed duty" [23]. This practical environmental stewardship represents a "testimonial of love for God, fellow human beings, and non-human others" and fulfills the mission where "Christian love (agape) serves as an ethical principle of inflicting 'no harm' to humans or non-human others" [23].
Bruce Jennings' concept of "ecological care" further develops this integration, emphasizing "caring about and for the health and integrity of the ecosystemic condition of life" while also requiring "a social, cultural, and political ecology of care-giving practices" [85]. This dual approach recognizes that effective environmental care necessitates both ethical commitment to natural systems and social structures that sustain caring practices. Ecological care thus conceived "seeks a natural ecology well cared for and a cultural ecology in which care is well done" [85].
Diagram 1: Agape Love in Community and Ecological Care Framework
Quantitative Research on Agape Love
Empirical Assessment of Agape in Communities
Recent empirical research provides quantitative insights into the understanding and influence of agape love within religious communities. A 2024 phenomenological study conducted in contemporary Evangelical Churches in Ethiopia employed a mixed-methods approach to assess the impact of postmodern thought on agape love [56]. The research utilized:
- Quantitative Surveys: 128 evangelical respondents completed Likert-scale surveys, with data analyzed using IBM SPSS Statistics Version 29 Software.
- Qualitative Components: Focus Group Discussions (FGD) and Key Informant Interviews (KII) with ministers using probing questions.
- Triangulation: Integration of quantitative and qualitative data with quality assurance measures.
The findings revealed significant challenges to agape-centered ethics, with approximately 55% of respondents identifying postmodernism as biblically heretical, while nearly 12% strongly disagreed with this assessment, indicating the influence of relativistic frameworks [56]. Notably, almost 90% of participants agreed that "teachings focusing on earthly prosperity have affected the love of the believers towards God" [56]. These findings demonstrate the vulnerability of agape ethics to cultural and philosophical shifts while highlighting the need for intentional moral formation in communities of faith.
Table 2: Quantitative Findings on Agape Love in Ethiopian Evangelical Churches
| Research Variable | Respondent Percentage | Interpretation | Methodological Tool |
|---|---|---|---|
| Postmodernism as heresy | 55% agreement | Recognizes tension with agape | Likert-scale survey |
| Neutral on postmodernism | 34% neutral position | Limited conceptual clarity | Likert-scale survey |
| Rejects heresy designation | 12% strong disagreement | Acceptance of postmodern thought | Likert-scale survey |
| Prosperity teachings affect love | 90% agreement | Identified threat to agape ethics | Quantitative and qualitative triangulation |
Research Methodologies for Studying Agape
The study of agape love requires innovative methodological approaches that bridge theological ethics, social sciences, and biomedical research. Effective protocols include:
- Non-Participant Observation: Systematic documentation of practices reflecting agape love, such as waste management in religious communities, care practices in clinical settings, or community health outreach [23].
- Mixed-Methods Design: Combining quantitative measures (e.g., scales assessing altruistic behaviors, resource allocation patterns) with qualitative approaches (e.g., narrative interviews, focus groups) to capture both behavioral and motivational dimensions [56].
- Ecological Liberation Hermeneutics: Interpretive framework analyzing "the nexus between the cry of the oppressed and the cry of the earth" through examination of ethical and social dimensions of ecological crises [23].
These methodologies enable researchers to move beyond theoretical abstraction to investigate the practical manifestation and impact of agape love in diverse contexts, from clinical encounters to environmental practices.
Implementation Framework for Researchers and Professionals
Integrating Agape into Research and Development
For researchers, scientists, and drug development professionals, agape love provides an ethical framework that complements established principles of research ethics. This integration occurs at multiple levels:
- Research Priority Setting: Directing attention to diseases and conditions that disproportionately affect marginalized populations and contribute to global health disparities.
- Resource Allocation: Ensuring equitable access to research benefits, including successful therapeutic interventions, across socioeconomic strata.
- Community Engagement: Adopting participatory research models that respect the agency and dignity of research participants and affected communities.
- Environmental Responsibility: Minimizing the ecological impact of research activities and industrial processes in pharmaceutical development.
These applications reflect the understanding of agape as "neighborly love" that seeks to "uncover or identify the neighbor in people we meet having deep regard and concern for them" [24]. In professional contexts, this entails recognizing research participants, patients, and affected ecosystems as neighbors deserving of moral consideration.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Methodological Resources for Agape-Informed Research
| Research Tool | Function | Application Context |
|---|---|---|
| SPSS Statistical Software | Quantitative data analysis | Measuring attitudes and behaviors related to agape love [56] |
| FICA Spiritual History Tool | Assessing spiritual needs | Integrating spirituality into patient care and research [86] |
| Love Attitudes Scale | Measuring manifestations of love | Research on agape and other love forms in communities [48] |
| Ecological Liberation Hermeneutics | Interpretive framework for eco-justice | Analyzing interconnection of social and ecological systems [23] |
| Triangulation Protocols | Integrating quantitative and qualitative data | Mixed-methods research on agape in practice [56] |
Diagram 2: Agape-Informed Research Implementation Workflow
Agape love provides an essential complement to existing frameworks in public health ethics by grounding moral responsibility in a theological anthropology of relationality, extending concern to the most vulnerable, and framing health as holistic flourishing of persons within planetary ecosystems. For researchers and healthcare professionals, this paradigm offers a motivational foundation that transcends instrumental rationality and technical efficiency, directing attention to the fundamental question of what constitutes truly compassionate and equitable care.
The integration of agape love into public health ethics and practice requires both conceptual clarity and practical implementation. As Daniel Sulmasy argues, responsible healthcare must attend to "the spiritual aspects of patients' lives and identities," recognizing that failure to do so "divorces medical practice from a fundamental mode of patient experience and coping" [86]. This approach, extended to ecological contexts, enables a comprehensive ethic of care that addresses the interconnected challenges of health equity and environmental sustainability.
Future research should continue to develop rigorous methodological approaches for studying agape love in health contexts, assess the outcomes of agape-informed interventions, and explore the implications of this framework for emerging ethical challenges in biotechnology, global health, and planetary health. Through such work, the healthcare community can more fully realize the vision of agape love as both a guiding principle and practical commitment to the flourishing of all creation.
Within the framework of Christian medical ethics, the concept of agape love represents a foundational, selfless, and unconditional virtue. This whitepaper examines two critical expressions of agape—philia (brotherly love and friendship) and forgiveness—and synthesizes the empirical evidence for their effects on human health. While agape provides the theological and ethical foundation, its manifestations in philia relationships and forgiveness practices represent tangible pathways through which this love influences physiological and psychological well-being. A growing body of scientific literature now provides robust data on the health correlates of these virtues, offering evidence-based insights for researchers and healthcare professionals working at the intersection of spirituality, ethics, and medicine.
Philia Love: Health Outcomes and Biological Mechanisms
Defining Philia in a Health Context
Philia, distinguished from erotic or familial love, constitutes the accepting love of good friendship and strong social bonds between equals [87]. This form of affection is characterized by its voluntary nature, mutual respect, and the provision of social support. From a biomedical perspective, philia relationships represent a potentially modifiable social determinant of health with measurable biological consequences.
Documented Health Correlates of Philia
Multiple studies have demonstrated that philia love and social connectedness are associated with significant health benefits across physiological systems. The touch of a loved one, a physical manifestation of philia, has been shown to lower blood pressure [87]. Individuals in loving, supportive relationships experience fewer doctor visits, shorter hospital stays, less pain, and more positive emotions compared to their socially isolated counterparts [87]. These positive consequences collectively enhance psychological resilience during difficult times [87].
Table 1: Documented Health Outcomes Associated with Philia Relationships
| Health Domain | Specific Outcomes | Proposed Mechanisms |
|---|---|---|
| Cardiovascular | Lower blood pressure; Reduced risk of heart disease | Stress buffering; Neurohormonal regulation |
| Healthcare Utilization | Fewer doctor visits; Shorter hospital stays | Enhanced immune function; Faster recovery |
| Psychological | Increased positive emotions; Greater resilience | Social support; Meaning and purpose |
| Pain Perception | Reduced experience of pain | Endorphin release; Distraction; Coping enhancement |
Forgiveness as an Expression of Agape: Empirical Health Correlates
Conceptual Framework of Forgiveness
Forgiveness, particularly when spiritually motivated, constitutes a behavioral expression of agape love through the conscious replacement of negative feelings toward wrongdoers with neutral or positive ones [88] [89]. Research distinguishes between forgiveness of others, self-forgiveness, and the perception of divine forgiveness [90], each with potential health implications. The process involves abandoning resentment and developing goodwill toward transgressors [91], representing a voluntary, prosocial transformation rather than condoning, excusing, or forgetting wrongdoing [88].
Mental Health Outcomes
Strong, consistent evidence links forgiveness to improved mental health across diverse populations. Longitudinal studies demonstrate that forgiveness is associated with reduced depressive symptoms, lower anxiety, and decreased psychological distress [90] [88]. A large-scale outcome-wide analysis found that forgiveness of others was prospectively associated with improved psychosocial well-being, including higher positive affect, greater social integration, and reduced hopelessness and loneliness [88]. Forgiveness interventions have shown effectiveness even among clinical populations, including incest survivors, those who experienced spousal abuse, and terminally ill cancer patients [91].
Physical Health Correlates
While evidence for forgiveness impacting physical health is less extensive than for mental health, several significant correlations have been documented. Research has linked forgiveness to improved cardiovascular health, including better heart functioning and reduced hypertension [91] [92]. Studies among patients with chronic pain conditions, such as fibromyalgia, have demonstrated that forgiveness interventions can improve physical functionality, reduce pain, and decrease fatigue [91]. Other research has connected forgiveness to better sleep quality and strengthened immune function [91].
Table 2: Health Outcomes Associated with Forgiveness in Empirical Studies
| Health Domain | Specific Outcomes | Study Characteristics |
|---|---|---|
| Mental Health | Reduced depression, anxiety, hostility; Increased life satisfaction | Large longitudinal studies (N=54,703 nurses; N=6,994 young adults) [90] [88] |
| Cardiovascular | Improved heart health; Reduced hypertension; Lower stress | RCTs; 5-week dynamic longitudinal study [91] [92] |
| Chronic Conditions | Reduced pain and fatigue in fibromyalgia; Improved physical function | Randomized controlled trials [91] |
| Health Behaviors | Reduced nicotine dependence; Lower substance abuse | Observational and intervention studies [88] |
Key Methodological Approaches and Experimental Protocols
Longitudinal Cohort Designs
Large-scale longitudinal studies provide some of the most compelling evidence for forgiveness-health connections. The Nurses' Health Study II (N=54,703 female nurses) assessed spiritually motivated forgiveness in 2008 and examined subsequent health outcomes over 7 years [88]. Researchers used validated scales including the Brief Multidimensional Measure of Religiousness/Spirituality to measure forgiveness, with outcomes assessed through standardized measures of psychological well-being, distress, health behaviors, and physical health conditions [88]. Statistical analyses employed linear, logistic, and Poisson regression models with extensive covariate adjustment for sociodemographic factors, prior religious service attendance, and baseline values of outcome variables [88].
Dynamic Longitudinal Models
Shorter-term dynamic studies capture the temporal relationships between forgiveness, stress, and health. One 5-week community-based study (N=332) measured state forgiveness, perceived stress, and mental and physical health symptoms weekly using the Rye Forgiveness Scale and standardized health measures [92]. The study employed parallel process latent growth curve modeling to test whether changes in forgiveness predicted changes in stress, which in turn predicted changes in health symptoms [92]. This methodology allowed researchers to establish temporal precedence and examine weekly fluctuations in these constructs.
Randomized Controlled Trials of Forgiveness Interventions
Forgiveness intervention studies employ structured protocols typically delivered over multiple sessions. One evidence-based approach involves 12-session forgiveness therapy incorporating process models that guide participants through phases of uncovering negative effects, deciding to forgive, working toward understanding, and discovering emotional release [91]. These interventions measure outcomes using standardized psychological measures (e.g., Beck Depression Inventory, State-Trait Anxiety Inventory) and in some cases physiological parameters (e.g., blood pressure, heart rate variability) at pre-intervention, post-intervention, and follow-up periods [91].
Biological and Psychological Mediating Pathways
Stress and Coping Pathways
The stress-and-coping model of forgiveness proposes that unforgiveness creates stressful states that negatively impact health, while forgiveness serves as an emotion-focused coping strategy that reduces stress perceptions [92]. Research has confirmed that increases in forgiveness are associated with decreases in perceived stress, which in turn mediate improvements in mental health outcomes [92]. This pathway operates both between persons (people who forgive more experience less stress) and within persons (weeks when individuals report higher forgiveness are followed by lower stress) [92].
Anger and Rumination Reduction
Forgiveness appears to improve health by resolving anger and reducing rumination—the repetitive focus on transgressions and negative emotions [91] [93]. Anger mediates the relationship between forgiveness and psychological health, with forgiveness interventions significantly reducing anger levels [91]. Similarly, rumination serves as a maladaptive cognitive process that forgiveness interrupts, thereby improving mental health outcomes [93]. This mediating effect appears more prominent in women, who generally demonstrate higher tendencies to ruminate [93].
Hope and Meaning Restoration
Forgiveness can foster hope—defined as the perceived capability to derive pathways to desired goals and motivate oneself to use those pathways [91]. Hope serves as a significant mediator between forgiveness and improved psychological health, particularly for outcomes like self-esteem and depressive symptoms [91]. By abandoning resentment, individuals may discover new meaning in suffering and develop a more optimistic future orientation [91].
Diagram 1: Forgiveness Health Pathway Mediators
Essential Research Reagents and Methodological Tools
Table 3: Essential Research Instruments and Measures for Studying Love and Forgiveness
| Instrument/Tool | Construct Measured | Application in Research | Psychometric Properties |
|---|---|---|---|
| Brief Multidimensional Measure of Religiousness/Spirituality | Forgiveness of others, self, and divine | Large-scale cohort studies (NHSII, GUTS) [90] [88] | Validated in diverse populations |
| Rye Forgiveness Scale | State forgiveness of others | Weekly assessments in dynamic longitudinal studies [92] | 15 items; Good reliability (α>.80) |
| Heartland Forgiveness Scale | Dispositional forgiveness (positive forgiveness & reduced unforgiveness) | Mediation studies examining psychological mechanisms [93] | Measures positive and negative dimensions |
| Rumination-Reflection Questionnaire | Self-consciousness (rumination & reflection) | Mediator between forgiveness and health [93] | Distinguishes adaptive and maladaptive self-focus |
The empirical evidence demonstrates that philia relationships and forgiveness—as tangible expressions of agape love—correlate with significant health benefits across multiple domains. Philia love associates with improved cardiovascular outcomes, reduced healthcare utilization, and enhanced psychological resilience. Forgiveness consistently predicts better mental health, and emerging evidence suggests potential physical health benefits, particularly for cardiovascular function and chronic pain conditions. Key biological and psychological mechanisms include stress reduction, anger and rumination resolution, and hope restoration. These findings offer valuable insights for researchers and healthcare professionals developing integrative approaches to whole-person care within ethical frameworks that acknowledge the importance of relational and spiritual dimensions in health and healing.
The integration of deeply held religious doctrines with the pragmatic demands of secular healthcare systems represents one of the most significant challenges in contemporary bioethics. For Christian researchers, clinicians, and drug development professionals, this tension is particularly acute when navigating medical necessity determinations, resource allocation frameworks, and technological innovation pathways. The concept of agape love—selfless, sacrificial love for others—emerges as a potentially transformative unifying norm that can bridge these seemingly disparate domains. This technical guide explores the methodological frameworks, practical applications, and experimental protocols for implementing agape as an integrative principle within medical ethics and research contexts.
Agape provides a theological foundation for navigating complex bioethical decisions by reframing them through the lens of selfless regard for the flourishing of others. Where secular medical ethics often relies on principles of autonomy, beneficence, non-maleficence, and justice, agape introduces a distinctive motivational framework that both complements and challenges these established norms [94]. This integration is particularly relevant for Christian professionals working in research and drug development, where decisions about resource allocation, technology adoption, and clinical priorities regularly intersect with value-based considerations.
Theological and Theoretical Foundations of Agape
Biblical and Theological Framework
Agape love finds its roots in the Christian narrative of a God who creates human beings in His image and demonstrates love through sacrificial action [19]. This concept is distinguished from other forms of love (eros, philia) by its volitional character and other-oriented focus [23]. The New Testament establishes agape as the central ethical norm for Christian life, exemplified in Jesus's teaching to "love your neighbor as yourself" (Matthew 22:37-40) and his definition of ultimate love: "to lay down one's life for one's friends" (John 15:13) [19].
This theological foundation establishes human dignity as inherent rather than contingent upon functionality or social utility. Every human being possesses infinite value by virtue of being created in God's image (imago Dei), which generates corresponding ethical obligations toward their care and protection [95]. This perspective directly informs biomedical ethics by challenging purely utilitarian calculations and affirming the protection of vulnerable populations, including embryos, disabled persons, and those with diminished cognitive capacity [95].
Agape as a Bioethical Norm
Within Christian medical ethics, agape functions as an integrating center that shapes both the principles and practices of healthcare [23]. It provides a motivational framework that transforms professional obligations into expressions of moral commitment, going beyond mere rule-following to embody the character of Christ in medical contexts [94]. This approach aligns with the call for Christians to "imitate God" (Ephesians 5:2) and "walk as Christ walked" (1 John 2:6) in all domains of life, including professional practice [94].
The operationalization of agape in medical ethics involves four key elements: sharing the mind of Christ (adopting a Christian worldview of creation, fall, redemption, and future hope), holding the commands of Christ (following biblical ethical principles), showing the character of Christ (demonstrating virtues like compassion and integrity), and carrying the cross of Christ (embracing sacrificial service and truth-telling despite costs) [94].
Methodological Framework for Integration
Conceptual Integration Model
The integration of agape ethics with secular medical frameworks requires a structured methodological approach. The following conceptual model illustrates the integration pathway:
Analytical Methodology for Ethical Decision-Making
Christian medical professionals can employ a systematic methodology for applying agape ethics in complex situations. This approach combines theological reflection with rigorous ethical analysis:
Situation Analysis: Define the medical, social, and ethical dimensions of the specific case or policy question, including all relevant stakeholders and their interests.
Theological Reflection: Identify relevant biblical principles, theological concepts, and historical Christian positions that inform understanding of the situation [94] [95].
Secular Ethical Mapping: Analyze the situation using standard medical ethical frameworks (principilism, consequentialism, virtue ethics) to understand prevailing secular perspectives.
Agape Integration: Apply agape as a unifying norm to identify areas of convergence and divergence between theological and secular perspectives, seeking solutions that honor both commitments.
Practical Implementation: Develop specific protocols, policies, or actions that reflect the integrated ethical position while remaining operable within secular constraints.
This methodology enables professionals to navigate complex scenarios such as resource allocation decisions, where agape prioritizes the needs of the most vulnerable while working within systemic constraints [95].
Experimental Protocols and Research Methodologies
Research Protocol for Evaluating Agape-Based Interventions
The following detailed methodology provides a framework for studying the implementation and outcomes of agape-based ethical approaches in healthcare settings:
Research Question: How does the explicit incorporation of agape ethics influence decision-making processes and outcomes in medical resource allocation?
Hypothesis: Healthcare systems that intentionally integrate agape principles will demonstrate more equitable resource distribution to vulnerable populations while maintaining operational efficiency.
Materials and Equipment:
- Electronic health record systems with appropriate data extraction capabilities
- Survey instruments measuring patient-reported outcomes and satisfaction
- Structured interview protocols for healthcare providers and administrators
- Ethical climate assessment tools validated for healthcare settings
- Statistical analysis software (R, SPSS, or SAS) for multivariate analysis
Procedure:
- Participant Recruitment: Identify and recruit three comparable healthcare organizations with varying levels of integration of faith-based ethics.
- Baseline Assessment: Collect quantitative data on current resource allocation patterns, patient outcomes, and stakeholder satisfaction.
- Intervention Implementation: Introduce agape ethics educational modules and decision-making frameworks to the experimental group.
- Data Collection: Implement mixed-methods data collection over 12 months, including:
- Quantitative metrics on resource distribution
- Qualitative interviews with key decision-makers
- Patient and family satisfaction surveys
- Data Analysis: Employ comparative statistical analysis and thematic coding to identify significant differences between groups.
Ethical Considerations: This protocol must maintain standards of informed consent, confidentiality, and scientific integrity while respecting the religious commitments of participants [95].
Research Reagent Solutions for Ethical Analysis
The following table details key methodological tools and approaches for implementing agape-based ethical analysis in medical contexts:
Table 1: Research Reagent Solutions for Agape-Based Ethical Analysis
| Research Component | Function | Application Example |
|---|---|---|
| Biblical Theological Analysis | Provides foundational understanding of agape love | Examining New Testament teachings on sacrificial love [19] [94] |
| Ecological Liberation Hermeneutics | Interpretative framework emphasizing justice for marginalized | Analyzing resource allocation impacts on vulnerable populations [23] |
| Principalism Integration Framework | Bridges theological and secular ethical systems | Applying agape to inform principles of justice and beneficence [95] |
| Mixed-Methods Assessment | Measures practical outcomes of ethical frameworks | Evaluating patient and provider experiences with agape-informed care |
| Trinitarian Relational Model | Conceptualizes community and interconnectedness | Designing healthcare systems that reflect mutual participation [23] |
Application to Medical Necessity and Resource Allocation
Agape-Informed Framework for Resource Allocation
The application of agape ethics to resource allocation decisions requires concrete principles that can be operationalized within secular healthcare systems. The following diagram illustrates the decision-making pathway:
Christian healthcare professionals have a responsibility to participate in resource allocation decisions rather than ceding this territory to purely utilitarian or materialistic frameworks [95]. Agape ethics supports allocation principles that:
Prioritize Vulnerable Populations: Direct resources toward patients with limited advocacy capacity or social disadvantage, reflecting Christ's concern for the marginalized [95].
Balance Immediate and Long-Term Needs: Make stewardship decisions that address both urgent medical needs and sustainable healthcare infrastructure [95].
Transcend Economic Reductionism: Resist reducing human value to economic metrics while acknowledging real resource constraints [95].
Promote Proportional Burden-Sharing: Distribute the sacrifices required by limited resources in a manner that protects the most vulnerable.
Quantitative Assessment Framework
The implementation of agape-based allocation principles can be evaluated using specific metrics across multiple dimensions:
Table 2: Metrics for Assessing Agape-Informed Resource Allocation
| Ethical Dimension | Quantitative Metrics | Data Collection Method |
|---|---|---|
| Equity in Access | Treatment rates across socioeconomic strata; Gap between most and least advantaged | EHR analysis; Population health data |
| Protection of Vulnerable | Resource allocation to disabled, elderly, cognitively impaired | Institutional budget analysis; Service utilization reviews |
| Stakeholder Experience | Patient and family satisfaction; Provider moral distress | Validated survey instruments; Structured interviews |
| Systemic Impact | Uncompensated care provision; Community benefit investment | Financial analysis; Community health needs assessment |
Agape in Emerging Medical Technologies
Ethical Framework for Technology Assessment
The rapid advancement of medical technologies, including artificial intelligence (AI) and human genome editing, presents critical ethical challenges that demand intentional integration of agape principles [96]. The Christian academic and research community bears particular responsibility for addressing the ethical dimensions of these technologies rather than ceding this territory to purely secular frameworks [96].
The following protocol provides a structured approach for evaluating emerging medical technologies through an agape-informed lens:
Technology Assessment Protocol:
Purpose Analysis: Examine whether the technology primarily serves to heal, enhance, or transform human nature beyond its created boundaries.
Benefit Distribution Evaluation: Assess whether the technology is likely to be accessible to marginalized populations or will exacerbate existing health disparities.
Human Dignity Impact Assessment: Evaluate potential effects on the understanding of human beings as created in God's image.
Relational Integrity Check: Analyze how the technology might affect human relationships, community bonds, and care for vulnerable persons.
Stewardship Analysis: Consider the appropriate use of created resources and technological capabilities within a framework of responsibility before God.
Application to Genome Editing Technologies
The emergence of CRISPR-based gene editing technologies illustrates the urgent need for agape-informed ethical analysis [96]. These technologies present both tremendous potential for alleviating genetic disorders and significant ethical concerns regarding equitable access, genetic enhancement, and permanent alteration of the human gene pool [96].
An agape-based approach to genome editing would:
- Strongly support therapeutic applications that alleviate suffering from genetic disorders
- Exercise caution regarding enhancements that could exacerbate social inequalities
- Prioritize development paths that ensure equitable access across socioeconomic boundaries
- Maintain the fundamental dignity of all persons regardless of genetic characteristics
This approach reflects the agape principle of "bearing one another's burdens" (Galatians 6:2) by directing technological development toward the relief of human suffering while maintaining ethical boundaries that protect human dignity [94] [96].
The integration of agape love as a unifying norm in medical ethics provides a robust framework for Christian researchers, clinicians, and drug development professionals to navigate the complex intersection of doctrinal commitment and secular medical necessity. This approach moves beyond simple rule-based compliance to transform the motivation, character, and practical reasoning of healthcare professionals.
Successful implementation requires both conceptual clarity and practical methodologies. The frameworks, protocols, and assessment tools presented in this technical guide provide a foundation for further development and application across diverse medical contexts. As Christian professionals work to embody agape love in their research and practice, they contribute to a healthcare ecosystem that more fully respects human dignity, promotes justice, and embodies the sacrificial love at the heart of the Christian faith.
The urgent ethical challenges presented by emerging technologies and resource constraints demand the distinctive contribution of Christian scholars and practitioners who can draw from the rich tradition of Christian ethical thought to inform contemporary medical practice [96]. By bringing agape ethics into dialogue with secular frameworks, Christian professionals play a vital role in shaping a medical ecosystem that honors both scientific excellence and moral commitment.
This whitepaper delineates the critical distinctions between agapeic benevolence as a foundational Christian virtue and Fletcher's Situation Ethics as a methodological framework. Within Christian medical ethics, agape represents an unconditional, intrinsic love that is the telos of the moral life, whereas situation ethics employs love as a pragmatic calculus for decision-making in contextual dilemmas. For researchers and drug development professionals, this distinction is paramount: agape provides a stable characterological foundation for upholding the sanctity of human life, while situation ethics offers a flexible procedure for navigating specific, novel moral conflicts. Understanding this dichotomy ensures that the relentless pursuit of technological advancement, from CRISPR to artificial intelligence, remains anchored in a consistent, person-centered ethic rather than being subject to ad hoc, consequentialist justifications [27] [96].
The Christian medical ethic is fundamentally a virtue ethic, wherein the cultivation of a moral character disposed toward agapeic love is the ultimate goal. Agape (from the Greek ἀγάπη) is a "neighbor regarding love for others" that is unconditional, makes no distinction between worthy and unworthy, and is the core disposition of excellent, ethical medical practice [10]. It is not merely an emotion but an attitude and act of will that desires and works for the neighbor's good, regardless of whether the neighbor is a friend or enemy [97] [98].
In an era of rapid technological progress, Christian academics face an unprecedented urgency to contribute theologically informed analyses to fields like human genome editing and artificial intelligence [96]. The application of CRISPR technology, for instance, presents profound questions about equity, human dignity, and the potential creation of "post-human subspecies." Resolving these issues requires a stable ethical foundation, which agape provides, to prevent policy from being shaped solely by secular, consequentialist frameworks. Agape is the bedrock principle that gives rise to and justifies the rules of medical ethics, ensuring that the principles of beneficence, nonmaleficence, autonomy, and justice are exercised with unconditional regard for the patient's well-being [99] [10].
Defining the Two Frameworks
Fletcher's Situation Ethics
Joseph Fletcher's Situation Ethics, articulated in his 1966 work Situation Ethics: The New Morality, proposes a moral methodology that navigates between the extremes of Legalism (blind adherence to rules) and Antinomianism (lawless moral anarchy) [100]. Fletcher's "Situationism" posits that moral decisions must be made contextually, within the entirety of a situation, with all normative features viewed as a whole [101].
Core Tenets of Situation Ethics
Fletcher's framework is structured around four working principles and six fundamental propositions, summarized in the table below.
Table 1: The Structural Framework of Fletcher's Situation Ethics
| Component | Description |
|---|---|
| Four Working Principles [97] | |
| Pragmatism | Actions must be practical and work in a given situation, based on experience rather than theory. |
| Relativism | The absolute laws of Christian ethics are made relative to the situation; terms like "never" and "always" are rejected. |
| Positivism | The theory begins with a belief in the reality and importance of love, a commitment not derived from reason alone. |
| Personalism | Persons are the center of moral concern, not laws or rules. |
| Six Fundamental Propositions [97] [98] | |
| 1. Intrinsic Good | Only one 'thing' is intrinsically good: love (agape), and nothing else. |
| 2. Ruling Norm | The ruling norm of Christian decision is love, which replaces all other laws. |
| 3. Love and Justice | Love and justice are the same, for justice is love distributed. |
| 4. Love for Neighbor | Love wills the neighbor's good, whether we like them or not. |
| 5. Ends and Means | Love is the end goal that justifies any means to achieve it. |
| 6. Contextual Decision | Love decides on each situation as it arises, without a predetermined set of laws. |
The operational engine of Situation Ethics is the agapeic calculus, where the right action is that which produces the "greatest amount of neighbor welfare for the largest number of neighbors possible" [98]. This makes it a teleological (end-based) and consequentialist theory, where the rightness of an act is determined by its loving outcome. Fletcher argued that in a complex situation, a generally "wrong" action like lying or killing could become the right action if it resulted in the most loving consequence [101] [102]. The following diagram illustrates this decision-making workflow.
The Concept of Agapeic Benevolence
In contrast, agapeic benevolence is not a calculus but a character disposition. It is a theological virtue, which, unlike the cardinal virtues (e.g., courage, temperance), is only fully possible for believers through divine grace [81]. It is a neighbor regarding love for others that makes no distinction between worthy and unworthy, friend and enemy [10].
Key Characteristics of Agapeic Benevolence
- Unconditional and Self-Giving: Agape does not depend on the merit or attractiveness of the recipient. It is a willed commitment to the good of the other, exemplified by Christ's love for humanity [10] [98].
- Intrinsically Good: Agape is good in and of itself, irrespective of consequences. Its value is not instrumental but inherent [97] [98].
- Foundational to Other Virtues: In a Christian ethical synthesis, agape is the foundation that gives rise to moral rules and inspires the development of other virtues like justice, courage, and hope [81].
- Focus on the Moral Agent: The primary focus is on the kind of person one is—a person whose character is shaped by agape. The right action then flows naturally from this virtuous character [81].
This virtue-based approach creates a different logical structure for moral reasoning, as shown below.
Critical Distinctions: A Comparative Analysis
The following table provides a systematic, side-by-side comparison of these two ethical approaches, highlighting their fundamental differences.
Table 2: A Comparative Analysis of Agapeic Benevolence and Fletcher's Situation Ethics
| Parameter | Agapeic Benevolence | Fletcher's Situation Ethics |
|---|---|---|
| Primary Nature | A virtue/disposition (a trait of character) [81]. | A method/calculus (a procedure for decision-making) [100] [98]. |
| Moral Foundation | The being of the moral agent; "Is the agent the right kind of person?" [81]. | The action and its consequences in a situation; "What is the most loving thing to do here?" [97] [102]. |
| Role of Love | Love is the intrinsic good that is the telos (goal) of the moral life [81] [98]. | Love is the extrinsic norm; a principle used to judge the rightness of an action [97] [101]. |
| View of Moral Rules | Rules are foundational guidelines that are grounded in and express the virtue of love (Rule Agapism) [81]. | Rules are maxims or guidelines that can be set aside if love's need demands it [97] [100]. |
| Theological Center | Theological virtue dependent on God's grace, shaping the soul into the likeness of Christ [81]. | Pragmatic principle that can operate independently of theological belief; "it has...nothing special to do with theological...faith" [100]. |
| Outcome | The right kind of character, from which right actions flow. The focus is on the moral agent. | The most loving consequence, which justifies any means. The focus is on the situation and outcome [97] [98]. |
Implications of the Distinction
The distinction has profound implications. For example, consider a healthcare professional caring for a person with advanced dementia.
- An ethic of agapeic benevolence would focus on the inherent worth of the person, affirming that their relationship with Jesus and their salvation are not contingent on their cognitive abilities. The professional's care flows from a character disposed to love this person unconditionally [99].
- A Situation Ethics approach would calculate the most loving action in the context—perhaps considering the patient's perceived quality of life, the family's distress, and resource allocation—which could lead to different conclusions depending on the calculated "greatest good" [99] [102].
Furthermore, in cutting-edge medical research, agape provides a stable foundation for upholding human dignity. It can, for instance, inform a precautionary principle regarding germline gene editing out of unconditional respect for the human person. Situation Ethics, by contrast, could more easily be used to justify such editing if the consequences were deemed sufficiently beneficial for the "greatest number," potentially leading to a slippery slope toward transhumanism [96].
Application in Medical Research: A Case Study on Spiritual Care
The systematic review by G. et al. (2025) on "Humanitarian Love" (a secular correlate of agape) in values-based practice provides quantitative and qualitative data on the impact of love as a core value in healthcare [27]. This research offers a model for studying the role of agapeic virtue in professional settings.
Research Methodology and Protocols
The review followed a rigorous systematic literature review methodology based on the PRISMA-S checklist [27].
- Search Databases: CINAHL, PubMed Central (PMC), and Elsevier/Scopus.
- Search Timeline: From the earliest records to September 8, 2024.
- PEO Framework: The search strategy was built using the PEO framework:
- P (Population): Health professionals (nurses, doctors, therapists, etc.)
- E (Exposure): Humanitarian love
- O (Outcome): Psychosocial impact
- Inclusion/Exclusion: Included observational and qualitative studies in English; excluded case reports and series.
- Screening and Bias Assessment: Conducted by two independent reviewers, with a third consulted for consensus. Cohen's Kappa (κ) was calculated to assess inter-judge agreement [27].
Key Experimental Findings and Data Synthesis
The review identified 16 studies that met the inclusion criteria, comprising 2,045 participants. The findings are synthesized in the table below.
Table 3: Synthesis of Findings on Humanitarian Love in Healthcare (G. et al., 2025) [27]
| Outcome Category | Key Finding | Implication for Practice |
|---|---|---|
| Impact on Healthcare Professionals | Fosters positive emotions and enhances the ability to provide high-quality care. | Investing in the cultivation of love reduces burnout and improves professional resilience. |
| Impact on Patient Care | Enables inner healing and self-realization for patients; reduces suffering. | Directing humanitarian love towards patients is a core component of effective, holistic care. |
| Psychosocial Well-being | Reduces feelings of burnout, emotional exhaustion, and compassion fatigue among professionals. | Humanitarian love should be established as a core value in Values-Based Practice (VBP) frameworks. |
The Scientist's Toolkit: Research Reagent Solutions
The following table details key conceptual "reagents" and their functions for researchers designing studies in this field.
Table 4: Research Reagent Solutions for Studying Agape in Medical Ethics
| Research Reagent | Function/Application in Research |
|---|---|
| PEO Framework | A structured tool for formulating a focused clinical question by defining Population, Exposure, and Outcome [27]. |
| PRISMA-S Checklist | A standardized protocol for ensuring a comprehensive and reproducible systematic literature search [27]. |
| Values-Based Practice (VBP) | A sister framework to Evidence-Based Practice that integrates the values of service users and practitioners into care decisions [27]. |
| FACIT-Sp12 Scale | A validated instrument (Functional Assessment of Chronic Illness Therapy—Spiritual Well-being) for measuring spiritual well-being, which can be adapted to assess aspects of agapeic care [99]. |
| Cohen's Kappa (κ) | A statistical measure used to evaluate the level of agreement between independent reviewers during the study selection process, ensuring methodological rigor [27]. |
The distinction between agapeic benevolence and Fletcher's Situation Ethics is not merely academic. For the Christian researcher and medical professional, it is the difference between an ethic that is rooted in the being of the moral agent and one that is consumed with the consequences of a particular act. Agape provides the unchanging, person-affirming foundation upon which a truly Christian medical ethic can be built, especially when confronting the novel challenges of 21st-century technology. Situation Ethics, while useful as a tool for navigating complex situational dilemmas, remains a procedural calculus that, unmoored from the stable virtue of agape, risks reducing love to a mere factor in a utilitarian equation. The future of ethical medical research depends on the ability to champion the former while critically employing the latter.
Conclusion
Agape love provides a profound and indispensable foundation for Christian medical ethics, moving beyond a rule-based or purely consequentialist approach to center on the inherent dignity of every person as bearing the image of God. This virtue ethic, characterized by selfless sacrifice and a commitment to the 'Beloved Community,' offers a robust framework for guiding clinical practice, shaping research priorities, and navigating complex bioethical dilemmas. For the biomedical research community, integrating agape presents a paradigm that champions the whole person over mere data points and fosters a culture of compassion within scientific inquiry. Future directions should include developing concrete ethical benchmarks for agape in drug development, fostering interdisciplinary dialogue between theologians and scientists, and conducting empirical studies on the impact of virtue-based ethics on patient outcomes and research integrity. The pursuit of medical advancement, when grounded in agape, becomes not just a technical endeavor, but a sacred vocation aimed at holistic healing.
References
- 1. Ahab [https://en.wikipedia.org/wiki/Ahab]
- 2. Ahab | Biography & Facts [https://www.britannica.com/biography/Ahab]
- 3. King Ahab and The Emotions of Change [https://deepspirituality.com/king-ahab/]
- 4. Bad Guys of the Bible: Ahab, Weak in Character and Faith [https://www.momentsofhopechurch.org/post/bad-guys-of-the-bible-ahab-weak-in-character-and-faith]
- 5. What Is Love? Ethics Explainer on Agape and Universal Love [https://ethics.org.au/ethics-explainer-agape/]
- 6. What is agape love? [https://www.gotquestions.org/agape-love.html]
- 7. The Agape Love of God [https://renner.org/article/the-agape-love-of-god/]
- 8. Sacrificial, Agape Love in Marriage [https://www.focusonthefamily.com/marriage/sacrificial-love/]
- 9. Love (Word Study) [https://www.bibleodyssey.org/articles/love-word-study/]
- 10. Agape Love- A Foundational Ethic for the Faithful Practice ... [https://www.medicineandreligion.com/agape-love--a-foundational-ethic-for-the-faithful-practice-of-medicine.html]
- 11. What Are the Four Types of Love in Scripture? - Christianity [https://www.christianity.com/wiki/christian-terms/what-are-agape-storge-phileo-and-eros-love-in-scripture.html]
- 12. The Doctrine of Love and Bioethics | Dignitas Vol. 31, No. 3 ... [https://cbhd.org/dignitas-articles/the-doctrine-of-love-and-bioethics]
- 13. Love-Agape (Greek Word Study) [https://www.preceptaustin.org/love-agape]
- 14. Argument from Agape [https://www.cslewisinstitute.org/resources/argument-from-agape/]
- 15. Types of Love in the Bible: Agape, Philia, Eros, and Storge Love [https://www.advancethefaithacademy.com/blog/types-of-love-in-the-bible-understanding-agape-philia-eros-and-storge-love]
- 16. When Words Fail: Love's Rightful Place in Medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9199038/]
- 17. The 4 Types of Love: Storge, Philia, Eros & Agape [https://www.wikihow.com/4-Types-of-Love]
- 18. Defining Love: Agape, Phileo, Eros, Storge - God\'s Word First [https://godswordfirst.org/defining-love-agape-phileo-eros-storge/]
- 19. Christian ethos and ethics as presuppositions for organ ... [https://www.sciencedirect.com/science/article/abs/pii/S2352552525000441]
- 20. The Doctrine of Love and Bioethics | Dignitas Vol. 31, No. 3-4 (Fall/Winter 2024) [https://www.cbhd.org/dignitas-articles/the-doctrine-of-love-and-bioethics]
- 21. Love and Christian Ethics [https://press.georgetown.edu/Book/Love-and-Christian-Ethics]
- 22. The Relationship Between Attachment Styles and Love ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12476884/]
- 23. Perspective on Agapeic Ethic and Creation Care [https://www.mdpi.com/2077-1444/16/1/21]
- 24. Agape Love, The Beloved Community, and Our Collective ... [https://cbc-network.org/2019/05/agape-love-the-beloved-community-and-our-collective-work-in-bioethics/]
- 25. How Christian Love Stirred Martin Luther King, Jr.'s Theory ... [https://www.logos.com/grow/martin-luther-king-jr-nonviolence/]
- 26. Christian Love and Covenant Faithfulness. [https://philpapers.org/rec/WERCLA]
- 27. Humanitarian Love in Values‐Based Practice and Health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12215605/]
- 28. The Sanctity of Life | The Bioethics Podcast [https://cbhd.org/podcast/the-sanctity-of-life]
- 29. THE ETHICS of BEGINNING-OF-LIFE HEALTH CARE, ... [https://www.healthcareministry.org/the-beginning-of-human-life/]
- 30. The Sanctity of Life Ethic [https://www.focusonthefamily.com/pro-life/the-sanctity-of-life-ethic/]
- 31. Theological Anthropology for Bioethics | Dignitas Vol. 30 ... [https://cbhd.org/dignitas-articles/theological-anthropology-for-bioethics]
- 32. Assess the claim that love (agape) is sufficient as the only ... [https://divinityphilosophy.net/2025/01/06/assess-the-claim-that-love-agape-is-sufficient-as-the-only-source-of-christian-ethics-40/]
- 33. Ethical challenges and opportunities in the development and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10262601/]
- 34. Strategies for Providing Culturally Sensitive: CARE TO ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9976714/]
- 35. Situationism and Virtue Ethics [https://1000wordphilosophy.com/2014/03/10/situationism-and-virtue-ethics/]
- 36. Pitting Virtue Ethics Against Situationism: An Empirical ... [https://link.springer.com/article/10.1007/s10677-023-10381-5]
- 37. The situationist critique of virtue ethics [https://www.philosophie.ch/2021-08-16-kohler]
- 38. Exploring the Power of Agape Love and Its Impact [https://bayareacbtcenter.com/agape-love/]
- 39. Is Agape Love The Highest? 5 Greek Loves & Biblical ... [https://www.kenboa.org/five-loves-greatest-agape/]
- 40. Age-stratified Data Highlight Worldwide Variability in Organ ... [https://pubmed.ncbi.nlm.nih.gov/41195981/]
- 41. William R. LaFleur, From Agape to Organs: Religious ... [https://philpapers.org/rec/LAFFAT]
- 42. Assessment of the relationship between organ donation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12312222/]
- 43. Analysis of Decision-making Behavior and Influencing ... [https://www.sciencedirect.com/science/article/abs/pii/S0041134525005251]
- 44. Religious aspects of organ transplantation [https://pubmed.ncbi.nlm.nih.gov/18555116/]
- 45. Enhancing patient-provider relationships with a whole person ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12070668/]
- 46. The Measurement of Love: Psychometric Properties and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9603604/]
- 47. Patients and Health Care Teams Forging Effective ... [https://nam.edu/perspectives/patients-and-health-care-teams-forging-effective-partnerships/]
- 48. A Quantitative Look at Love [https://sites.lsa.umich.edu/qmss/2023/02/14/a-quantitative-look-at-love/]
- 49. Press Release: New Initiative Brings Healthcare ... [https://drlornabreen.org/new-initiative-brings-healthcare-community-together/]
- 50. The King Philosophy - Nonviolence365® [https://thekingcenter.org/about-tkc/the-king-philosophy/]
- 51. Seven Love Types (Part 7) LOVE #6: Agape (Giving-love) [https://www.drchristianheim.com/blog/2020/8/28/seven-love-types-part-7-love-6-agape-giving-love]
- 52. 25 Traits of The Beloved Community [https://www.interfaithmissionservice.org/about-us/vision-and-mission/25-traits-of-the-beloved-community/]
- 53. Cultivating a Beloved Community Mindset to Transform ... [https://uwmedicine.shorthandstories.com/cultivating-a-beloved-community-mindset-to-transform-unjust-systems/]
- 54. Beloved Community Labs [https://belovedcommunitiesnetwork.org/transition-labs/]
- 55. A Nursing Practice Model Based on Christ: The Agape Model [https://pubmed.ncbi.nlm.nih.gov/28594653/]
- 56. STATISTICAL INFLUENCE OF POSTMODERNISM ON ... [https://biblicalstudies.in/index.php/pub/article/view/17]
- 57. Personality traits, love styles, and social rejection [https://www.sciencedirect.com/science/article/abs/pii/S0191886922005736]
- 58. Exploring the ethical issues posed by AI and big data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12581208/]
- 59. Regulating the Use of AI in Drug Development: Legal ... [https://www.fdli.org/2025/07/regulating-the-use-of-ai-in-drug-development-legal-challenges-and-compliance-strategies/]
- 60. The AI lab waging a guerrilla war over exploitative AI [https://www.technologyreview.com/2024/11/13/1106837/ai-data-posioning-nightshade-glaze-art-university-of-chicago-exploitation/]
- 61. Top challenges with clinical trial ethics in 2025 [https://clinicaltrialrisk.org/clinical-trial-design/top-challenges-with-clinical-trial-ethics/]
- 62. Ethical Dilemmas in Pharma: Pharma's Toughest Decisions [https://pda.org/pda-letter-portal/home/full-article/ethical-dilemmas-in-pharma-pharma's-toughest-decisions]
- 63. Principles of Bioethics for Christian Physicians: Autonomy and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11298101/]
- 64. Nanoparticle biodistribution coefficients: A quantitative ... [https://www.sciencedirect.com/science/article/pii/S0169409X23000236]
- 65. Quantification of 89Zr-Iron Oxide Nanoparticle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6235733/]
- 66. What's love got to do with it? Exploring social love and public ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11103914/]
- 67. Love, Intellect & Higher Order Empathy | Age of Awareness [https://medium.com/age-of-awareness/love-intellect-higher-order-empathy-9d6c30563c2e]
- 68. What is Agape ? Bible Meaning and Examples | Love .com Christianity [https://www.christianity.com/wiki/christian-terms/what-does-agape-love-really-mean-in-the-bible.html]
- 69. Strategies and Interventions to Improve Healthcare ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10233581/]
- 70. How lifestyle medicine can prevent burnout in healthcare ... [https://lifestylemedicine.org/healthcare-professional-burnout/]
- 71. Burnout among school teachers: quantitative and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6542045/]
- 72. : The Highest Form Of Unconditional Agape | Dennis McIntyre Love [https://www.patheos.com/blogs/faith4today/2025/06/agape-the-highest-form-of-unconditional-love/]
- 73. The Morality of Christian : A Theological and Love Perspective Ethical [https://ideas.repec.org/a/smo/journl/v9y2024i2p53-64.html]
- 74. Experimental Design: Approaches and Applications in ... [https://jddtonline.info/index.php/jddt/article/view/4908]
- 75. Design of Experiments in Pharmaceutical Development [https://www.spcforexcel.com/knowledge/experimental-design-techniques/design-experiments-pharmaceutical-development/]
- 76. Principles of Bioethics [https://depts.washington.edu/bhdept/ethics-medicine/bioethics-topics/articles/principles-bioethics]
- 77. Principles of Clinical Ethics and Their Application to Practice [https://pmc.ncbi.nlm.nih.gov/articles/PMC7923912/]
- 78. Ethical Principles [https://www.cdc.gov/niosh/learning/safetyculturehc/module-5/11.html]
- 79. Human Flourishing in Christ: A Journey of Hope in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8033492/]
- 80. Situation Ethics [https://alevelphilosophyandreligion.com/situation-ethics/]
- 81. The Virtue Ethic and Agapism - Ronald Nash [https://www.biblicaltraining.org/learn/institute/et501-christian-ethics/et501-04-the-virtue-ethic-and-agapism]
- 82. How Do Theological and Secular Ethics Relate and ... [https://www.mdpi.com/2077-1444/13/10/971]
- 83. Community Health Advocacy | Agape [https://www.agapefamilyhealth.org/about/community/advocacy/]
- 84. Home | Agape Health Services | Health Clinic Washington NC [https://www.agapechc.org/]
- 85. Ecological Care [https://humansandnature.org/ecological-care/]
- 86. Patients benefit from attending to spirituality in health care ... [https://kennedyinstitute.georgetown.edu/news-releases/patients-benefit-from-attending-to-spirituality-in-health-care-says-georgetown-university-bioethics-expert/]
- 87. The Four Types of Love: Some Are Healthy, Some Are Not [https://healthcare.utah.edu/the-scope/health-library/all/2023/02/four-types-of-love-some-are-healthy-some-are-not]
- 88. Forgiveness of others and subsequent health and well-being ... [https://bmcpsychology.biomedcentral.com/articles/10.1186/s40359-020-00470-w]
- 89. 10 Limits to Forgiveness in Health Care [https://link.springer.com/article/10.1007/s10728-025-00518-1]
- 90. Religiously or Spiritually-Motivated Forgiveness and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6662928/]
- 91. Indirect Effects of Forgiveness on Psychological Health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10120569/]
- 92. Forgiveness, Stress, and Health: a 5-Week Dynamic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5055412/]
- 93. Forgive, Let Go, and Stay Well! The Relationship between ... [https://www.mdpi.com/1660-4601/20/13/6229]
- 94. A Christian framework for medical ethical decision-making [https://www.cmf.org.uk/a-christian-framework-for-medical-ethical-decision-making/]
- 95. Position Statements [https://cmda.org/policy-issues-home/position-statements/]
- 96. A Call to Christian Academics Regarding Medical and ... [https://christianscholars.com/a-call-to-christian-academics-regarding-medical-and-technological-ethics/]
- 97. Fletcher's Situation Ethics - Religious Studies: OCR A Level [https://senecalearning.com/en-GB/revision-notes/a-level/religious-studies/ocr/2-2-1-fletchers-situation-ethics]
- 98. 1.5.5: The Six Propositions of Situation Ethics [https://human.libretexts.org/Courses/Folsom_Lake_College/PHIL_310%3A_Introduction_to_Ethics_(Bauer)/01%3A_Evaluate_a_variety_of_concepts/1.05%3A_Fletcher's_Situation_Ethics/1.5.05%3A_The_Six_Propositions_of_Situation_Ethics]
- 99. Ethics of Spiritual Care in the Midst of Dementia – Rev Ben ... [https://lukesjournalcmdfa.com/2025/04/17/ethics-of-spiritual-care-in-the-midst-of-dementia-rev-ben-boland/]
- 100. 5: Fletcher's Situation Ethics [https://human.libretexts.org/Bookshelves/Philosophy/Ethics/Ethics_(Fisher_and_Dimmock)/5%3A_Fletcher's_Situation_Ethics]
- 101. Situation ethics | Definition, Joseph F. Fletcher, & Moral ... [https://www.britannica.com/topic/situation-ethics]
- 102. Ethics - Introduction to ethics: Situation ethics [https://www.bbc.co.uk/ethics/introduction/situation_1.shtml]