A Comprehensive Guide to Obtaining Valid Informed Consent in Clinical Trials: Principles, Procedures, and Best Practices
This article provides a complete framework for researchers and clinical trial professionals to ethically and effectively obtain valid informed consent.
A Comprehensive Guide to Obtaining Valid Informed Consent in Clinical Trials: Principles, Procedures, and Best Practices
Abstract
This article provides a complete framework for researchers and clinical trial professionals to ethically and effectively obtain valid informed consent. Covering foundational ethical principles, step-by-step methodological application, solutions for complex scenarios including vulnerable populations, and processes for regulatory validation, this guide synthesizes current regulations and health literacy best practices to ensure participant autonomy and data integrity.
The Ethical and Regulatory Bedrock of Informed Consent
Informed consent serves as a cornerstone of ethical clinical research, representing a fundamental shift from paternalistic practices to respect for participant autonomy. Historically, the concept emerged from landmark legal cases and responses to unethical medical experiments, establishing the principle that patients must agree to medical procedures and research interventions [1]. In our modern ethical conception, informed consent is defined as a process by which "a subject voluntarily confirms his or her willingness to participate in a particular trial, after having been informed of all aspects of the trial that are relevant to the subject's decision to participate" [2]. This definition underscores the dual nature of informed consent as both an ethical imperative and a communicative process.
Contemporary understanding positions informed consent at the intersection of accurate factual information and effective communication [3]. This framework recognizes that merely providing information is insufficient; how that information is conveyed, understood, and processed by potential participants is equally critical. The process begins the moment researchers start soliciting participants and continues until no further use is made of the participant's information or biospecimens [4]. This ongoing nature distinguishes true informed consent from the simplistic act of signing a form, which merely documents the process at one point in time.
Essential Elements: Information and Communication Components
Core Informational Elements
The informational components of informed consent must provide comprehensive details enabling an autonomous decision. Based on regulatory requirements and ethical guidelines, these essential elements include [3] [5]:
- Purpose and Nature: A clear statement that the study involves research, description of the research purpose, expected duration of participation, and study procedures
- Risks and Benefits: Description of any reasonably foreseeable risks, discomforts, and potential benefits to participants or others
- Alternatives and Voluntariness: Disclosure of appropriate alternative procedures or courses of treatment, and a clear statement that participation is voluntary
- Protections and Contacts: Information about confidentiality protections, compensation for injury, contacts for questions about research and participant rights, and the conditions under which participation may be terminated
The following table summarizes the quantitative findings from studies evaluating how these elements are typically addressed in consent processes:
Table 1: Quantitative Evaluation of Informed Consent Processes
| Evaluation Aspect | Finding | Source/Study |
|---|---|---|
| Documentation of 4 core elements (nature, risks, benefits, alternatives) | Documented only 26.4% of the time on consent forms | Bottrell et al. as cited in [1] |
| Participant satisfaction with consent process | Majority "positive" about their experience (169 participants surveyed) | Study in Trials Journal [6] |
| Research staff confidence in facilitating consent | 74.4% felt "very confident" or "confident" | Same survey of 115 staff [6] |
| Staff concerns about participant understanding | 56% expressed concern about whether participants understood complex information | Same survey [6] |
| Phase I consent quantitative assessment | ~80% of patients received complete information about drug characteristics and treatment modalities | Study of 32 taped conversations [7] |
Essential Communication Elements
Effective communication transcends mere information disclosure. The quality of the interaction significantly influences participant understanding and autonomy. Based on communication models adapted to clinical research, essential communication elements include [3]:
- Building Rapport: Establishing trust and equality in the researcher-participant exchange
- Assessing Understanding: Actively checking for comprehension through techniques like "playback" where participants repeat details in their own words
- Using Accessible Language: Avoiding medical jargon, using easy-to-understand language appropriate to the population
- Encouraging Questions: Creating an environment where participants feel comfortable seeking clarification
- Emotional Responsiveness: Recognizing and addressing indirectly expressed anxieties and emotional concerns
Research evaluating the qualitative aspects of consent discussions has revealed specific patterns in communication effectiveness:
Table 2: Qualitative Assessment of Communication Dimensions in Informed Consent
| Communication Dimension | Performance Assessment | Identified Pitfalls |
|---|---|---|
| Information Dimension | Most items scored ≥3.5 (5-point scale) | Assessment of patient understanding scored <3 in 53% of consultations [7] |
| Emotional Dimension | All items scored >3.5 | Generally well-handled by clinicians [7] |
| Interactive Dimension | Lowest mean scores recorded | Difficulty recognizing indirectly expressed anxieties [7] |
| Overall Successful Consultation | 71% of consultations had all three dimensions scoring >3 and balancing one another | Meerwein's model applied to 32 conversations [7] |
Experimental Protocols and Assessment Methodologies
The Process and Quality of Informed Consent (P-QIC) Tool
The P-QIC instrument was developed specifically to quantitatively measure the quality of informed consent encounters through direct observation. The methodology for developing and validating this tool involved [3]:
Instrument Development Protocol:
- Initial Source: Adapted from an observer checklist developed by the Institutional Review Board at Columbia University Medical Center consisting of 25 items
- Theoretical Framework: Based on the model positioning informed consent at the intersection of factual information and effective communication
- Information Elements: Derived from CIOMS guidelines and U.S. Department of Health and Human Services Federal Regulation Title 45
- Communication Elements: Derived from the Kalamazoo Consensus Statement, the Conversation Model of Informed Consent, and Delphi consensus-building methods
Psychometric Testing Protocol:
- Sample: 63 students enrolled in health-related programs participated in psychometric testing; 16 students participated in test-retest reliability; 5 investigator-participant dyads were observed for actual consent encounters
- Stimuli Development: Professionally filmed, simulated consent encounters designed to vary in process and quality
- Testing Procedure: Participants watched and rated videotaped simulations of four consent encounters intentionally varied in process and content
- Reliability Assessment: Test-retest reliability established by raters watching videotaped simulations twice; inter-rater reliability demonstrated by two simultaneous but independent raters observing actual consent encounters
- Setting: Conducted at a major urban teaching hospital in the northeastern United States
Validation Outcomes:
- The initial testing demonstrated reliable and valid psychometric properties in both simulated standardized consent encounters and actual consent encounters in hospital settings
- The tool provides a quick assessment of areas of strength and those needing improvement in consent encounters
- Applications include training new investigators and ongoing quality improvement programs for informed consent
Teach-Back and Comprehension Assessment Protocols
The teach-back method is a critical evidence-based technique for assessing and enhancing participant understanding during consent discussions. The protocol involves [1]:
Implementation Steps:
- Explanation: The researcher explains a concept using plain language
- Assessment Request: The researcher asks the participant to explain the concept in their own words
- Clarification: If the participant demonstrates misunderstanding, the researcher re-explains using alternative wording
- Reassessment: The participant again attempts to explain the concept
- Repetition: This cycle continues until understanding is verified
Effectiveness Data:
- Studies implementing health literacy-based consent forms combined with teach-back techniques demonstrated improved patient-provider communication
- Participants reported increased comfort in asking questions when teach-back was employed
- The method helps both patients and clinicians concentrate on essential aspects of the information
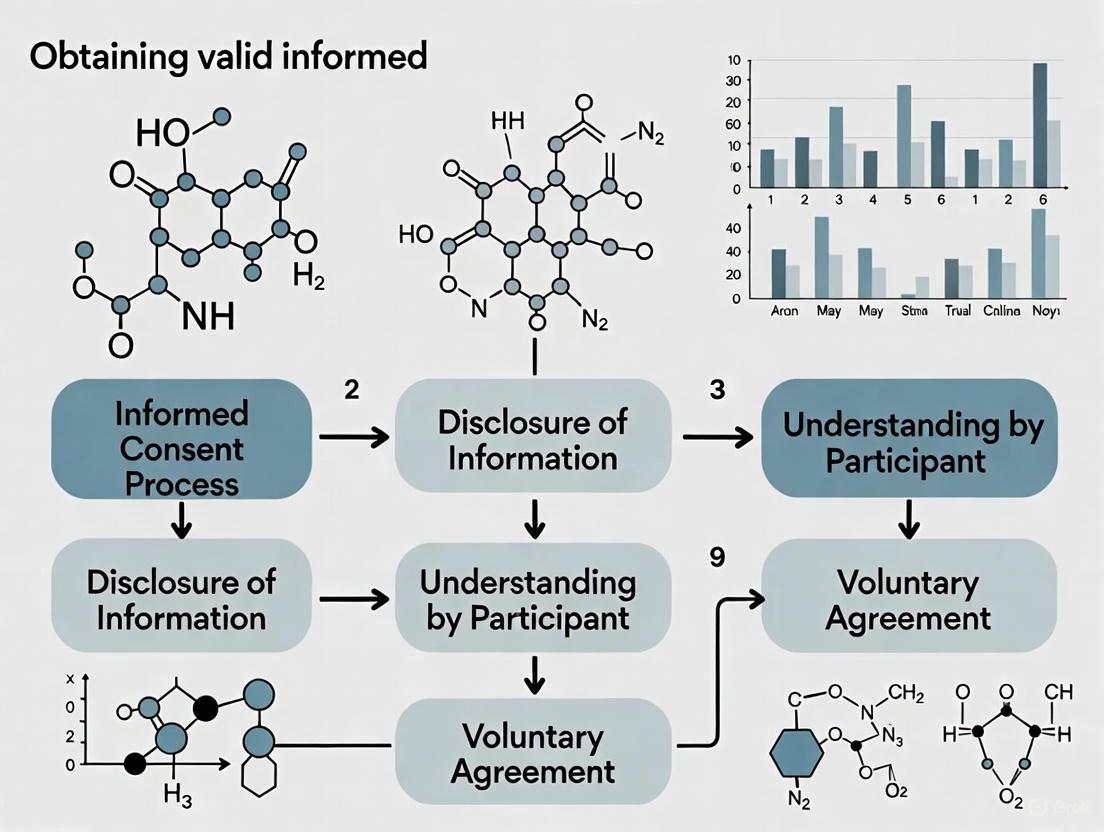
Visualizing the Informed Consent Process
The following diagram illustrates the comprehensive nature of informed consent as an ongoing process rather than a single event:
Informed Consent as an Ongoing Process
Table 3: Research Reagent Solutions for Informed Consent Processes
| Tool/Resource | Function/Purpose | Application Context |
|---|---|---|
| P-QIC Instrument | Observational tool measuring process and quality of consent encounters | Training new investigators; quality improvement programs; research on consent effectiveness [3] |
| Teach-Back Method | Verification of participant understanding through playback technique | During consent discussions; assessing comprehension of complex concepts; health literacy adaptation [1] |
| Health Literacy Assessment | Evaluation of readability and comprehension level of consent materials | During consent form development; plain language adaptation; regulatory compliance [4] |
| Essential Elements Checklist | Verification that all required informational components are included | Protocol development; IRB/ethics committee submissions; regulatory compliance [3] [5] |
| Vulnerable Population Protocols | Specialized procedures for participants with diminished autonomy | Research with children, cognitively impaired, prisoners, emergency settings [2] |
Implementation Framework and Procedural Protocols
Structured Consent Discussion Protocol
Based on analysis of successful consent consultations, the following structured protocol is recommended for implementing valid consent processes:
Pre-Consent Preparation Phase:
- Timing and Setting: Schedule dedicated time in a quiet, private setting without interruptions [1]
- Participant Preparation: Provide consent forms in advance, allowing sufficient time for review and consultation with family or advisors [6]
- Support Persons: Encourage participants to bring family members or friends to the discussion when appropriate [6]
- Staff Training: Ensure research staff receive specific training on facilitating informed consent discussions [6]
Consent Discussion Execution:
- Introduction and Rapport: Begin by establishing trust and emphasizing the voluntary nature of participation [3]
- Key Information First: Present a concise and focused presentation of key information most relevant to the participation decision [4]
- Staged Information Delivery: Divide complex information into manageable segments with pauses for questions [7]
- Comprehension Verification: Systematically employ teach-back techniques after explaining critical concepts [1]
- Emotional Awareness: Monitor for indirect expressions of anxiety and address them explicitly [7]
- Documentation: After ensuring understanding, document the consent with appropriate signatures [5]
Post-Consent Continuation:
- Ongoing Availability: Maintain availability for questions throughout the study period [4]
- Reconsent Procedures: Implement procedures for reconsent if new information emerges or study parameters change [1]
- Results Communication: Provide study results to participants in an accessible format after study completion [6]
Special Circumstances Protocol
Vulnerable Populations Adaptation: Research with vulnerable populations requires additional safeguards and adapted procedures [2]:
- Cognitive Impairment: Assess decision-making capacity using standardized tools; involve legally authorized representatives with continued assent from participants when possible
- Emergency Settings: Follow exception from informed consent (EFIC) regulations for emergency research; implement community consultation and public disclosure requirements
- Children: Obtain parental permission with age-appropriate assent from children; tailor information to developmental level
- Language Barriers: Use certified medical interpreters rather than family members; translate consent materials and certify translation accuracy
Waiver of Consent Conditions: Under strict conditions, research without consent may be permissible when [2]:
- Impracticability: Obtaining consent is not feasible due to time, resource, or validity constraints
- Self-Respect: The research does not infringe the principle of self-determination
- Clinical Relevance: The research provides significant clinical relevance justifying the waiver
Valid informed consent represents a sophisticated integration of comprehensive information, effective communication, and ongoing participant engagement. Moving beyond the signed form as an isolated event to conceptualize consent as a dynamic process requires researchers to develop both knowledge and skills in information delivery, interpersonal communication, and comprehension assessment. The experimental protocols and assessment tools detailed in this application note provide evidence-based methodologies for implementing this process-oriented approach. By adopting these structured protocols and utilizing the included researcher toolkit, clinical trial professionals can enhance participant understanding, respect autonomy, and strengthen the ethical foundation of human subjects research.
This document provides detailed application notes and experimental protocols for implementing the three core ethical principles of informed consent—voluntariness, information disclosure, and comprehension—in clinical trial research. These principles form the ethical foundation required by international regulations including ICH-GCP, the Declaration of Helsinki, and U.S. FDA guidelines [8] [9]. Robust implementation is critical for protecting participant autonomy, ensuring regulatory compliance, and maintaining the integrity of research data. This guide outlines standardized methodologies for translating ethical theory into verifiable practice, complete with quantitative assessment tools and procedural workflows designed for researchers, scientists, and drug development professionals.
Informed consent is a foundational ethical and legal requirement in clinical research, transforming the participant from a passive subject into an autonomous partner [8] [9]. Its validity rests not on the mere signing of a form but on the successful implementation of a continuous process built on three core principles: information disclosure, comprehension, and voluntariness [9] [10]. These principles are operationalized through the Informed Consent Form (ICF), a document that must balance regulatory completeness with participant understanding [8].
The historical evolution of informed consent, driven by past abuses such as the Nazi experiments and the Tuskegee Syphilis Study, underscores its non-negotiable status in modern research [8]. Contemporary regulations, including ICH-GCP E6(R2) and 21 CFR Part 50, enshrine these principles into law, requiring documented evidence that consent was obtained ethically and validly [8] [11]. This document provides the practical framework for meeting these stringent requirements, ensuring that participant welfare and autonomy remain at the center of clinical research.
Quantitative Data on Informed Consent Practices
Empirical studies highlight significant challenges in the practical application of informed consent principles. The following tables summarize key quantitative findings on compliance and readability, which inform the protocols in subsequent sections.
Table 1: Good Clinical Practice (GCP) Compliance of Informed Consent Forms (ICFs) in a Multicenter Analysis [12]
| GCP-Mandated Information Item | Industry Sponsored Studies (% Compliance) | Non-Sponsored Studies (% Compliance) |
|---|---|---|
| Purpose of the study | >90% | <50% |
| Risks or discomforts | >90% | <50% |
| Benefits | >90% | <50% |
| Voluntary participation & right to withdraw | >90% | <50% |
| Randomization probability | >90% | <50% |
| Investigator contact information | >90% | <50% |
| Subject rights and responsibilities | 33% | 16% |
| Anticipated out-of-pocket expenses | 24% | <20% |
| Overall GCP Compliance | 79.5% | 55.8% |
Table 2: Readability Analysis of Informed Consent Forms Using Flesch-Kincaid Scale [12]
| Readability Metric | Industry Sponsored Studies (Mean ± SD) | Non-Sponsored Studies (Mean ± SD) | Target Value |
|---|---|---|---|
| Reading Ease Score | 48.9 ± 4.8 | 38.5 ± 8.0 | >60 [12] [10] |
| Grade Level Score | 9.7 ± 0.7 | 12.2 ± 1.3 | ~8th Grade [10] |
| Categorization (based on Reading Ease) | 51% Difficult, 49% Fairly Difficult | 83% Difficult, 17% Very Confusing | "Standard" or "Fairly Easy" |
Application Notes & Protocols for Core Principles
Principle 1: Information Disclosure
3.1.1 Protocol for Comprehensive Information Disclosure
The goal of this protocol is to ensure all regulatory-required information is completely and accurately disclosed to the prospective participant.
- Step 1: Develop the ICF Draft. Using the current study protocol and Investigator's Brochure, create the ICF. It must include all basic elements stipulated by relevant regulations (e.g., FDA 21 CFR 50.25, ICH-GCP) [10].
- Step 2: Integrate Additional and Specific Elements. Append any additional elements required by the IRB or applicable due to the study's nature. These may include statements on:
- Unforeseeable risks.
- Circumstances for investigator-terminated participation.
- Additional costs to the participant.
- Consequences of withdrawal.
- Disclosure of significant new findings [10].
- Step 3: Cross-Reference and Validate Content. Systematically cross-reference the ICF with the study protocol to ensure all procedures, visits, and experimental interventions are accurately described. Verify that all risks listed in the Investigator's Brochure are included in the ICF's "Risks" section [10].
- Step 4: IRB/EC Submission and Revision. Submit the draft ICF and study protocol to the Institutional Review Board (IRB) or Ethics Committee (EC) for review. Incorporate all feedback and secure final approval before any participant is consented [8] [11].
3.1.2 The Scientist's Toolkit: Reagents for Information Disclosure
| Essential Material | Function in Protocol |
|---|---|
| Approved Study Protocol & Investigator's Brochure | Serves as the source of truth for all study procedures, risks, and investigational product details to be disclosed [10]. |
| Regulatory Checklist (e.g., 21 CFR 50.25 Checklist) | Ensures every mandated basic and additional element of informed consent is included in the ICF draft [10]. |
| IRB/EC Application Package | Formalizes the ethical review process, providing the committee with all necessary documents to assess the adequacy of subject protection [8]. |
Principle 2: Comprehension
3.2.1 Protocol for Assessing and Ensuring Participant Comprehension
This protocol outlines a systematic approach to verify that the disclosed information is understood by the participant, moving beyond mere document delivery to an interactive process.
- Step 1: Pre-Consent Readability Assessment. Before IRB submission, assess the ICF's readability using a validated tool like the Flesch-Kincaid scale. The target is a Reading Ease score >60 and a Grade Level of 8th grade or lower [12] [10]. Use plain language and avoid technical jargon.
- Step 2: The Interactive Consent Discussion. The investigator or a qualified designee must conduct a structured discussion with the potential participant. This is not a passive reading exercise but a two-way dialogue [9].
- Step 3: Comprehension Verification via Teach-Back Method. After explaining a key concept (e.g., randomization, risks, right to withdraw), ask the participant to explain it back in their own words [9]. Document the participant's questions and the investigator's answers. This step is critical for validating understanding.
- Step 4: Assessment and Documentation. Use open-ended questions to gauge understanding (e.g., "Can you tell me what might happen if you decide to leave the study early?"). The investigator must make a professional judgment that the participant has understood the information before proceeding to signature [11]. Document the process, including the use of any translated materials or interpreters.
The following workflow diagrams the comprehensive comprehension verification process.
Principle 3: Voluntariness
3.3.1 Protocol for Ensuring Voluntary Decision-Making
This protocol is designed to create an environment free of coercion and undue influence, allowing for a choice made purely of the participant's own free will.
- Step 1: Environment Setup. Conduct the consent discussion in a private setting, free from distractions and outside pressure. The participant should be given adequate time to consider the information [9] [13].
- Step 2: Explicit Verbal and Written Statements. The investigator must explicitly state, both verbally and within the ICF, that:
- Step 3: Mitigate Perceived Coercion. For participants with whom the investigator has a pre-existing relationship (e.g., patient-physician), explicitly address that their clinical care will not be affected by their decision. Avoid any language that could be perceived as persuasive or incentivizing beyond the disclosed benefits [9].
- Step 4: Facilitate Unpressured Deliberation. Actively encourage the participant to discuss the study with family, friends, or independent advisors. Avoid rushing the decision. For vulnerable populations, ensure additional safeguards are in place, such as the involvement of a neutral third party or legally authorized representative [9] [11].
The logical relationship between environmental factors, investigator actions, and the outcome of a voluntary decision is shown below.
Integrated Workflow and Advanced Considerations
The following diagram synthesizes the protocols for all three principles into a single, integrated workflow for obtaining valid informed consent.
Table 3: Protocol for Special Population Considerations
| Participant Population | Core Consideration | Protocol Requirement |
|---|---|---|
| Non-English Speakers | Linguistic comprehension | Use IRB-approved translated ICFs. For unforeseen scenarios, use a short-form consent with an interpreter and a written summary [10]. |
| Minors (Children) | Legal consent & developmental understanding | Obtain permission from parent/guardian. Obtain assent from the child using age-appropriate language and documentation (e.g., simplified forms, stickers) [13]. |
| Incapacitated Adults | Legal consent & diminished autonomy | Obtain consent from a Legally Authorized Representative (LAR). The LAR must be qualified, without conflicts of interest, and familiar with the participant's wishes [13]. |
| Adults with Low Literacy | Comprehension | Rely more heavily on the interactive discussion and verbal teach-back methods. An impartial witness may be required to attest that information was fairly presented [13]. |
The protocols outlined in this document provide a actionable roadmap for embedding the core ethical principles of voluntariness, information disclosure, and comprehension into every stage of the informed consent process. By treating consent as a continuous, interactive dialogue rather than a singular administrative task, researchers can fulfill both the letter and the spirit of international regulations. The quantitative data presented reveals clear areas for improvement, particularly in enhancing the readability of ICFs and ensuring consistent GCP compliance across all study types. The rigorous application of these standardized methodologies is the ultimate safeguard for participant autonomy and the cornerstone of ethically sound and legally defensible clinical research.
Obtaining valid informed consent is a fundamental ethical and regulatory requirement in clinical research. This process is governed by robust frameworks designed to protect participant autonomy, safety, and rights. The Common Rule (45 CFR Part 46) in the United States and the International Council for Harmonisation's Good Clinical Practice (ICH-GCP) guidelines are two pivotal regulatory systems that set the standard for this process. While the Common Rule provides the foundational federal policy for the ethical conduct of human subjects research, ICH-GCP offers an internationally recognized quality standard that ensures data credibility and participant protection across global trials. This application note details the specific requirements of these frameworks, provides protocols for their implementation, and situates them within the critical practice of securing valid informed consent.
Regulatory Framework Analysis
The Common Rule: Core Principles and Consent Requirements
The Common Rule outlines the basic provisions for Institutional Review Boards (IRBs), informed consent, and the protection of human subjects in research. Its provisions for informed consent are both procedural and substantive, mandating that consent must be informed, comprehensible, and voluntary [1].
- Key Elements: The regulations stipulate specific elements that must be included in the informed consent document and process. These include a clear explanation of the research purpose, procedures, foreseeable risks, potential benefits, alternative procedures, and a statement of confidentiality [14] [1].
- Comprehension: A core tenet of the Common Rule is that the information presented to the potential subject must be in a language and at a level of complexity that is understandable to the subject or their legally authorized representative. The process must facilitate the participant's understanding and voluntary decision-making [14].
- Documentation: Informed consent must be documented by a written form that the participant has signed, unless this requirement is specifically waived by the IRB under narrow circumstances, such as when the signed consent form would be the only record linking the subject to the research and a breach of confidentiality would be the primary risk [1].
ICH-GCP Guidelines: A Global Benchmark
The ICH-GCP guidelines provide an international ethical and scientific quality standard for designing, conducting, recording, and reporting trials that involve the participation of human subjects. The principles of ICH-GCP have been adopted by regulatory authorities in the U.S., the European Union, Japan, and many other countries, making it a cornerstone for global drug development [15].
- Participant Protection: The primary focus of ICH-GCP is to ensure that the rights, safety, and well-being of trial subjects are protected and that the clinical trial data are credible [15].
- Informed Consent Process: ICH-GCP emphasizes that informed consent is a process that begins before a subject's participation and continues throughout the trial. The investigator, not a delegate, has a direct responsibility to ensure that this process is conducted properly and that the subject has ample opportunity to ask questions and receive satisfactory answers [16].
- Ongoing Consent: The guidelines underscore that subjects must be informed of any new information that becomes available during the trial which may be relevant to their willingness to continue participation. Re-consent is required when this new information is significant [16].
The forthcoming E6(R3)* update, announced for September 2025, marks a significant evolution of these guidelines. It incorporates more flexible, risk-based approaches and embraces innovations in trial design and technology, while maintaining a strong focus on participant protection and data reliability [15].
Comparative Analysis of Framework Requirements
The table below summarizes and compares the key informed consent requirements as outlined by the Common Rule and ICH-GCP guidelines.
Table 1: Key Informed Consent Requirements in the Common Rule vs. ICH-GCP
| Feature | The Common Rule | ICH-GCP Guidelines |
|---|---|---|
| Primary Focus | Protection of human subjects in research; ethical principles [1] | Credibility of data and protection of participant rights, safety, and well-being [15] |
| Core Consent Elements | Nature of research, risks, benefits, alternatives, confidentiality, voluntary participation, contact information [14] | Detailed trial information, including trial treatment(s), purpose, procedures, allocation of treatment, and compensation [15] |
| Process Emphasis | Ensuring comprehension and voluntariness; information must be understandable [14] [1] | A continuing process, initiated prior to consent; investigator-responsibility for ensuring understanding [16] |
| Documentation | Typically a signed consent form, with specific waivers possible [1] | A signed and dated written consent form prior to participation [16] |
| Ongoing Consent | Implied through the right to withdraw; specific re-consent for protocol changes is an IRB decision | Explicitly required when new relevant information becomes available [16] |
| Key Update (as of 2025) | - | E6(R3): Promotes flexibility, risk-based approaches, and use of technology [15] |
Experimental Protocols for Valid Informed Consent
Protocol 1: The Pre-Consent Preparation and Assessment Workflow
This protocol ensures all foundational work is complete before approaching a potential participant.
Table 2: Essential Research Reagents for Valid Informed Consent
| Reagent/Material | Function in the Consent Process |
|---|---|
| Protocol Summary (Lay Language) | Serves as the foundation for creating an understandable consent form; explains the study's purpose and procedures simply [14]. |
| IRB-Approved Informed Consent Form (ICF) | The legal document that structures the consent discussion and ensures all regulatory elements are addressed [14] [16]. |
| Visual Aids & Multimedia Tools | Enhances comprehension of complex procedures (e.g., randomization, blinding) and helps communicate risks and benefits effectively [1]. |
| Health Literacy Assessment Tool | Aids in screening for potential barriers to understanding, allowing the research team to tailor their communication approach [1]. |
| Teach-Back Method Script | Provides a structured method for assessing participant understanding by asking them to explain the study in their own words [1]. |
Procedure:
- IRB Submission and Approval: Submit the final clinical trial protocol, the informed consent form (ICF), and all participant-facing materials to the IRB or Ethics Committee for review and approval. Do not proceed until written approval is obtained [14].
- Team Training and Delegation: Train all research staff involved in the consent process on the study protocol, the approved ICF, and principles of health literacy. Document this training. The principal investigator retains ultimate responsibility [1].
- Participant Pre-Screening: Identify potential participants who meet the preliminary eligibility criteria for the study. This assessment should be documented in the study records.
- Environment Preparation: Schedule a dedicated meeting in a private, quiet setting free from distractions to conduct the informed consent discussion. Allow for sufficient time (typically 30-60 minutes).
Protocol 2: The Informed Consent Discussion and Documentation Process
This protocol details the step-by-step procedure for conducting and documenting a valid informed consent discussion.
Procedure:
- Initial Introduction and Purpose: Introduce yourself and your role. Clearly state that the conversation is about a research study and distinguish research from standard clinical care [14] [1].
- Presentation of the ICF: Provide the participant with a copy of the IRB-approved ICF. Use the document as a guide for the discussion, but explain the content using simple, everyday language. Avoid or thoroughly define medical jargon [14].
- Systematic Review of Key Elements:
- Nature and Purpose: Explain the research purpose, duration, and procedures. Describe any experimental procedures clearly [14].
- Risks and Discomforts: Discuss all reasonably foreseeable risks (physical, psychological, social, financial) and the steps taken to minimize them [14] [1].
- Benefits: Describe any potential benefits to the participant or to society. Be clear if there is no direct benefit to the participant [14].
- Alternatives: Explain the alternatives to participation, which may include other treatments or no treatment at all [14] [1].
- Confidentiality: Explain how records will be protected, who will have access (including the possibility of regulatory agency review), and how data will be stored and eventually destroyed [14].
- Voluntary Participation: Explicitly state that participation is voluntary and that refusal or withdrawal will not result in penalty or loss of benefits to which the participant is otherwise entitled. Explain the process for withdrawal and any potential consequences of early withdrawal (e.g., need for a safe taper of investigational product) [14] [16].
- Assessment of Understanding (Teach-Back): Use the teach-back method to confirm comprehension. Ask open-ended questions such as, "Can you tell me in your own words what the main risks of this study are?" or "What would you do if you wanted to stop being in the study?" [1].
- Answering Questions: Encourage and answer all questions the participant or their family members may have. Avoid rushing the process and offer the opportunity to take the ICF home and discuss it with family, friends, or their personal physician [14] [16].
- Documentation of Consent: Once all questions are answered and the participant demonstrates understanding, proceed with signing the ICF. The participant and the individual conducting the consent discussion should sign and date the form. The participant receives a copy of the signed document [16].
Protocol 3: Maintaining Valid Consent Throughout the Trial
Informed consent is a continuous process, not a single event. This protocol ensures consent remains valid for the study's duration.
Procedure:
- Ongoing Communication: Maintain regular, open communication with the participant throughout their involvement in the trial. Check in about their well-being and reinforce that they can withdraw at any time without penalty [16].
- Monitoring for New Information: Monitor for any new safety information or significant changes to the protocol that arise during the trial. This includes new risks identified in other study participants or in the scientific literature.
- Re-Consent Process: If new information is deemed relevant to the participant's willingness to continue in the study, prepare an amended ICF and submit it to the IRB for approval. Once approved, schedule a meeting with the participant to discuss the new information and obtain their re-consent using the same rigorous process as the initial consent. Document the re-consent with a new signed ICF [16].
- Documenting Withdrawal: If a participant decides to withdraw, document the date and reason for withdrawal (if provided). Ensure that any procedures for safe termination of participation are followed (e.g., a final safety assessment) [14].
Visualization of the Informed Consent Process
The following diagram illustrates the complete, continuous workflow for obtaining and maintaining valid informed consent, from preparation through trial completion, as detailed in the experimental protocols.
Diagram 1: The Informed Consent Workflow
Discussion
The process of obtaining valid informed consent is a dynamic and multifaceted responsibility for researchers. The regulatory frameworks of the Common Rule and ICH-GCP provide the essential structure, but the application requires critical thinking, cultural competence, and a genuine commitment to participant partnership.
A significant challenge is ensuring true comprehension, not just a signature. The use of validated health literacy tools and the teach-back method are evidence-based strategies to bridge the comprehension gap [1]. Furthermore, the increasing globalization of clinical trials necessitates sensitivity to cultural and linguistic differences. What constitutes voluntary consent in one culture may not in another, and reliance on professional interpreters is non-negotiable for non-native speakers [1] [17].
The future of informed consent is being shaped by technological innovation and regulatory evolution. The ICH E6(R3) guidelines encourage the use of electronic consent (eConsent) platforms, which can incorporate interactive modules, videos, and embedded comprehension checks to enhance understanding [15]. These tools, aligned with a risk-based approach, allow for a more proportional and efficient consent process, focusing greater resources on higher-risk studies while maintaining rigorous ethical standards.
Valid informed consent is the ethical and legal bedrock of clinical research. The Common Rule and ICH-GCP guidelines provide a comprehensive, complementary set of requirements that, when implemented faithfully through detailed protocols, ensure that participants' autonomy is respected and their welfare is protected. As the clinical trial landscape evolves with new technologies and global collaborations, the principles of clear communication, ongoing dialogue, and participant-centered care remain paramount. By adhering to these frameworks and employing robust methodologies, researchers can build the trust necessary for successful and ethical clinical research.
Informed consent is a foundational ethical and regulatory requirement in clinical research. It is a process by which a subject voluntarily confirms their willingness to participate in a particular trial, after having been informed of all aspects of the trial that are relevant to their decision to participate [2]. This process is documented through a written, signed, and dated informed consent form, which serves as evidence that the consent conversation took place and that the participant agreed to join the study [2]. For researchers and drug development professionals, understanding the precise elements required in a consent form is critical not only for regulatory compliance but also for ensuring participant autonomy, safety, and understanding. A properly executed informed consent process respects the participant's right to self-determination and establishes the ethical foundation for the entire clinical investigation.
Regulatory Foundation & Core Components
The content of an informed consent form is not arbitrary; it is strictly defined by national and international regulations. In the United States, the Food and Drug Administration (FDA) regulations at 21 CFR 50.25 and the Department of Health and Human Services (HHS) regulations at 45 CFR 46.116 delineate the basic and additional elements that must be included to make a consent form legally effective [18] [19]. Furthermore, the International Council for Harmonisation (ICH) Good Clinical Practice (GCP) guidelines provide an international standard, defining informed consent as the process whereby a subject voluntarily confirms his or her willingness to participate after being informed of all relevant trial aspects [2].
The following workflow outlines the structured process of developing and obtaining a legally valid informed consent, from foundational regulations to participant understanding.
The Eight Basic Required Elements
The following table synthesizes the eight basic elements of informed consent as mandated by FDA regulations (21 CFR 50.25(a)), which must be present in every consent form for clinical research [18] [20] [19].
Table 1: Basic Required Elements of a Legally Valid Informed Consent Form
| Element Number | Element Description | Key Considerations for Researchers |
|---|---|---|
| 1 | Statement of Research & Procedures: A statement that the study involves research, an explanation of the purposes, expected duration of participation, a description of procedures, and identification of any experimental procedures [18] [19]. | Clearly distinguish research procedures from standard care. Specify the total number of subjects involved [20]. |
| 2 | Description of Foreseeable Risks: A description of any reasonably foreseeable risks or discomforts to the subject [18] [19]. | Include physical, psychological, social, and economic risks. Describe measures to minimize risks [19]. |
| 3 | Description of Potential Benefits: A description of any benefits to the subject or to others that may reasonably be expected from the research [18] [19]. | Avoid unproven claims. Clearly state if there is no direct benefit to the subject [19]. |
| 4 | Disclosure of Alternatives: A disclosure of appropriate alternative procedures or courses of treatment, if any, that might be advantageous to the subject [18] [20]. | Identify the subject's alternatives, including the alternative of not receiving therapy [19]. |
| 5 | Statement on Confidentiality: A statement describing the extent to which confidentiality of records will be maintained, noting that the FDA may inspect the records [18] [20]. | Explain who will have access to the data (e.g., sponsor, IRB, FDA) and the steps taken to ensure confidentiality [19]. |
| 6 | Compensation for Injury: For research involving more than minimal risk, an explanation of whether any compensation and medical treatments are available if injury occurs and, if so, what they consist of [18] [20]. | Provide details on how to obtain further information about research-related injury. Note that consent cannot waive a subject's legal rights [20]. |
| 7 | Contacts for Questions: An explanation of whom to contact for answers to pertinent questions about the research and research subjects' rights, and whom to contact in the event of a research-related injury [18] [20]. | Provide the names and contact information of the principal investigator and an independent contact (e.g., IRB) [21]. |
| 8 | Voluntary Participation: A statement that participation is voluntary, refusal to participate will involve no penalty or loss of benefits, and the subject may discontinue participation at any time [18] [20]. | Emphasize that the decision will not affect the quality of medical care received [2] [22]. |
Additional Elements of Informed Consent
Under certain circumstances, one or more additional elements of information must be provided to the subject. The IRB determines which of these elements are appropriate based on the nature of the research and its context [18] [20].
Table 2: Additional Elements of Informed Consent (as required by the IRB)
| Element | Description | Typical Use Cases |
|---|---|---|
| Unforeseeable Risks | A statement that the treatment or procedure may involve risks to the subject (or embryo/fetus) that are currently unforeseeable [18] [20]. | Early-phase trials, novel interventions. |
| Termination by Investigator | Anticipated circumstances under which the subject's participation may be terminated by the investigator without the subject's consent [18] [19]. | Protocol non-compliance, intercurrent illness. |
| Additional Costs | Any additional costs to the subject that may result from participation in the research [18] [19]. | Procedures not covered by the sponsor or insurance. |
| Consequences of Withdrawal | The consequences of a subject's decision to withdraw and procedures for orderly termination [18] [20]. | Long-term follow-up studies, data handling post-withdrawal. |
| Significant New Findings | A statement that significant new findings developed during the research that may relate to the subject's willingness to continue will be provided [18] [20]. | All clinical trials, especially those of long duration. |
| ClinicalTrials.gov Statement | For applicable clinical trials, a statement that a description of the trial will be available on ClinicalTrials.gov [18]. | FDA-regulated clinical trials. |
Experimental Protocol: Implementing a Legally Valid Consent Process
Protocol for Developing and Obtaining Informed Consent
Objective: To ensure every research participant (or their legally authorized representative) provides legally effective, ethically valid, and voluntary informed consent prior to initiating any study-related procedures.
Materials & Reagents:
- Final IRB/EC-approved informed consent document: The definitive version of the consent form, including all required elements.
- Study protocol and Investigator's Brochure: Reference documents to ensure accurate information is conveyed.
- A private, quiet setting: To facilitate an open discussion without coercion or undue influence.
- eConsent platform or paper forms: For documentation, as approved by the IRB/EC [22].
- Certified translation(s): For non-English speaking participants, ensuring the consent form is in a language understandable to the subject [21].
Methodology:
- Preparation and Documentation:
Information Disclosure Process:
- Conduct a structured discussion with the participant/LAR in a setting that minimizes distractions [2].
- Explain the study using lay language, avoiding technical jargon. Address all basic and applicable additional elements from Tables 1 and 2 [19] [21].
- Specifically highlight key information: the purpose, procedures, risks, benefits, alternatives, voluntary nature of participation, and the right to withdraw [2] [22].
- Encourage and answer all questions thoroughly. Use interactive methods like "teach-back" where the participant explains the study in their own words to verify comprehension [21].
Assessment of Understanding and Voluntariness:
Documentation of Consent:
- Provide the participant/LAR with a copy of the signed and dated consent form [2].
- For paper-based consent, ensure the participant and the person obtaining consent sign and date the form simultaneously. For electronic consent (eConsent), use a system that captures electronic signatures and timestamps and provides a copy to the participant [22].
- Document the entire process in the participant's study record, including the date, time, and any questions raised and answered [21].
Ongoing Consent (Re-consent):
- Monitor the study for significant new findings or protocol changes that might affect a participant's willingness to continue.
- If such events occur, obtain re-consent using an IRB/EC-approved revised consent form or consent addendum [22].
Researcher's Toolkit: Essential Materials for the Consent Process
Table 3: Essential Materials and Reagents for the Informed Consent Process
| Item | Function/Application |
|---|---|
| IRB/EC-Approved ICF | The legally vetted document containing all required elements and information for the participant. |
| Protocol Summary/Visual Aids | Simplified summaries, diagrams, or videos to enhance participant understanding of complex study designs [21]. |
| eConsent Platform | A digital system for presenting consent information, facilitating electronic signatures, and managing version control [22]. |
| Comprehension Assessment Tool | A short questionnaire or a set of verbal questions to objectively verify the participant's understanding of key study aspects [21]. |
| Certified Translation Services | To provide legally accurate translations of the ICF for participants who do not speak the primary study language [21]. |
| Legally Authorized Representative (LAR) Guidelines | Institutional policies and checklists to guide interactions with LARs for subjects unable to consent for themselves [20]. |
Critical Considerations for Valid Implementation
Ensuring Participant Comprehension
The consent form must be written in language that is easily understood by the subjects [2]. This involves using a second-person writing style (e.g., "you" and "we"), explaining technical terms, and avoiding complex legalistic language [19]. The use of multimedia components in eConsent, such as video and audio, can further break down complex information to ensure true understanding [22].
Prohibited Language and Practices
Informed consent forms must never include exculpatory language, which is any language through which the subject is made to waive their legal rights or that releases the investigator, sponsor, or institution from liability for negligence [20] [19]. Furthermore, consent forms should not contain unproven claims of effectiveness or certainty of benefit, as this can be misleading and constitute undue influence [19].
Special Circumstances and Vulnerable Populations
Research involving vulnerable populations—such as children, incapacitated adults, or prisoners—requires additional safeguards [2]. For children, consent must be obtained from a parent or guardian (LAR), and the child's assent should be sought when appropriate [20]. For adults who lack decision-making capacity, consent must be obtained from a legally authorized representative [2] [20]. The IRB provides specific guidance on consent procedures for these populations.
Informed consent serves as a cornerstone of ethical clinical research, yet under specific low-risk circumstances, regulatory frameworks permit exceptions to the standard requirement for individual written consent. The waiver of informed consent represents a critical ethical and methodological consideration for researchers designing pragmatic clinical trials, quality assurance activities, and comparative effectiveness studies [23]. These research approaches aim to embed clinical investigation within routine healthcare practices to generate generalizable evidence relevant to real-world settings.
The fundamental ethical discordance addressed by consent waivers stems from the observation that while rigorous research requires consent for practice evaluation, routine clinical decision-making often lacks similar formal consent processes for equivalent treatments [23]. This ethical framework recognizes that traditional written informed consent models can create significant barriers to research feasibility and inclusiveness, potentially resulting in study populations that differ substantially from broader patient populations in important characteristics such as age, comorbidity burden, and prognosis [23]. For research evaluating interventions that will affect all patients within a system, waiver of consent models may minimize selection bias and enhance generalizability.
Regulatory Framework and Ethical Justification
International and National Guidelines
Global research organizations have established specific guidelines governing the circumstances under which waiver of consent may be ethically permissible. Our analysis identifies key regulatory frameworks across international and national jurisdictions, summarized in Table 1 below.
Table 1: International and National Guidelines for Waiver of Consent in Clinical Research
| Governing Organization | Guideline Name | Year | Key Waiver Provisions |
|---|---|---|---|
| Council for International Organisations of Medical Sciences (CIOMS) | International Ethical Guidelines for Health-related Research Involving Humans | 2016 | Guideline 10 addresses waiver of consent for health-related research, identifiable data/biological specimens, non-identifiable data, and research involving vulnerable populations [23] |
| US Department of Health & Human Services | Code of Federal Regulations (The Common Rule) | 2019 | IRB waiver or alteration permitted for clinical investigations involving no more than minimal risk [23] |
| Canadian Institutes of Health Research | Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans | 2018 | Articles 3.7A and 3.7B outline waiver conditions for various research types including social sciences and public health research [23] |
| European Parliament and Council | Regulation No 536/2014 On Clinical Trials on Medicinal Products for Human Use | 2014 | Paragraph 33 and Article 30 specifically address cluster randomized trials where groups rather than individuals are allocated to interventions [23] |
| National Health and Medical Research Council (Australia) | National Statement on Ethical Conduct in Human Research | 2018 | Chapter 2.3.10 addresses research using personal information or personal health information [23] |
Ethical Principles and Justification
The ethical justification for waiving informed consent rests on several interconnected principles. Low-risk pragmatic clinical research, such as learning health system research and comparative effectiveness studies, aims to evaluate interventions in real-world settings, often comparing medical treatments already in common use [23]. When the risks inherent in research participation approximate those encountered in routine clinical care, the requirement for individual consent may be ethically modified.
The increasing recognition of healthcare services' impact on clinical outcomes, coupled with digital advancements facilitating previously impossible research, has stimulated interest in appropriate utilization of consent waivers in minimal-risk clinical research [23]. The waiver of consent is particularly relevant for comparative effectiveness studies and health-service interventions designed to affect broad patient populations, where traditional consent models would limit generalizability and introduce selection bias.
Table 2: Core Ethical Criteria for Waiver of Consent
| Criterion | Ethical Rationale | Application in Research Context |
|---|---|---|
| Minimal Risk | Research risks do not exceed those encountered in routine clinical care | Protects participants from harm while facilitating research in real-world settings [23] |
| Practical Impracticability | Obtaining consent would make the research impossible or methodologically invalid | Preserves scientific validity when researching system-level interventions or including representative populations [23] |
| Respect for Persons | Notification processes maintain acknowledgment of participant dignity | Provides information about research participation even when formal consent is waived [24] |
| Social Value | Research addresses important questions that could not be answered without waiver | Ensures that risks to autonomy are proportionate to potential knowledge gains [23] |
Experimental Protocols for Implementing Consent Waivers
Protocol 1: Ethics Review and Approval Process
Objective: To establish a standardized procedure for obtaining institutional review board (IRB) or research ethics committee (REC) approval for waiver of consent in eligible clinical studies.
Materials and Reagents:
- IRB/REC application forms
- Study protocol document
- Risk assessment matrix
- Data management plan
- Participant information materials (for notification when applicable)
Procedure:
- Study Design Phase: Determine whether the research qualifies as minimal risk according to regulatory definitions. Document how risks are not greater than those encountered in routine clinical care [23].
- Feasibility Assessment: Evaluate whether obtaining individual consent would be impracticable due to methodological requirements (e.g., cluster randomization, need for representative population) [23].
- Protocol Documentation: Explicitly describe in the study protocol the justification for consent waiver, including how the research meets regulatory criteria.
- Ethics Submission: Submit complete application to the relevant IRB/REC, highlighting how the research satisfies the following criteria:
- Research involves no more than minimal risk to participants
- Waiver will not adversely affect participant rights and welfare
- Research could not practicably be carried out without the waiver
- Whenever appropriate, participants will be provided with additional pertinent information after participation [23]
- Committee Engagement: Be prepared to address committee questions regarding risk categorization and alternative consent approaches.
- Approval Documentation: Obtain and file formal approval of the consent waiver before initiating any research procedures.
Protocol 2: Participant Notification Procedures
Objective: To implement ethical participant notification processes for studies conducted under waiver of consent, promoting respect for persons and maintaining trust in research institutions.
Materials and Reagents:
- Notification templates (letters, emails, posters)
- Contact information for eligible participants
- Educational materials about the research
- Procedures for addressing participant inquiries
- Opt-out mechanisms (when applicable)
Procedure:
- Notification Design:
- Develop participant-friendly notification materials explaining the research purpose, procedures, and data usage
- Tailor communication methods to the specific population and healthcare context
- Include information about participant rights and contact information for questions [24]
Implementation Strategy:
- Deploy multi-modal notification approaches (e.g., letters, emails, waiting room posters, clinician conversations)
- Sequence notifications to maximize reach while minimizing burden
- For cluster randomized trials, consider presentations at staff meetings and institutional communications [24]
Content Optimization:
- Determine the appropriate amount of information to disclose, ranging from general statements about institutional research to detailed study information
- Balance comprehensiveness with accessibility and readability
- Include information about how to opt out of data use when feasible [24]
Response Management:
- Establish procedures for addressing participant questions and concerns
- Train staff to respond appropriately to inquiries
- Document and address participant objections promptly
Effectiveness Evaluation:
- Monitor reach of notification efforts
- Solicit feedback on notification clarity and comprehensiveness
- Adjust approaches based on participant and stakeholder input
Visualization of Waiver Decision Pathway
The following diagram illustrates the logical decision process for determining when a waiver of informed consent may be appropriate for a clinical study:
Waiver of Consent Decision Pathway
Research Reagent Solutions for Ethical Implementation
Table 3: Essential Research Reagents for Implementing Consent Waiver Studies
| Reagent/Resource | Function | Application Notes |
|---|---|---|
| IRB/REC Application Templates | Standardized documentation for ethics review | Pre-formatted templates specific to waiver requests improve review efficiency and compliance [23] |
| Risk Assessment Matrix | Systematic evaluation of study risks | Visual tool comparing research risks to routine clinical care risks; supports minimal risk determination [23] |
| Participant Notification Materials | Communication of research information | Letters, emails, posters, and educational materials tailored to participant literacy and accessibility needs [24] |
| Data Protection Protocols | Safeguarding of participant data | Encryption, anonymization, and access control measures for research with waived consent [23] |
| Accessibility Resources | Support for diverse participant needs | Adapted materials for participants with communication, hearing, or visual disabilities [25] |
| Opt-Out Mechanism Framework | Respect for participant autonomy | Structured processes allowing participants to exclude their data from research when feasible [24] |
The waiver of informed consent represents a carefully circumscribed exception within clinical research ethics, reserved for specific minimal-risk situations where traditional consent processes would compromise study feasibility or validity. International guidelines demonstrate broad consensus on the core principles governing such waivers, emphasizing minimal risk, practicability, and protection of participant rights [23].
When implemented appropriately with proper ethical oversight, waiver of consent enables important research on healthcare delivery and comparative effectiveness that would otherwise be impossible, ultimately strengthening the evidence base for routine clinical care. Even when formal consent is waived, researchers should default to providing participants with information about the research [24], thereby respecting the ethical principle of respect for persons and maintaining trust in the research enterprise.
This protocol provides researchers, scientists, and drug development professionals with a structured framework for evaluating and implementing consent waivers when scientifically and ethically justified, advancing the goal of a learning health system while maintaining rigorous ethical standards.
Executing the Consent Process: A Step-by-Step Operational Blueprint
Within the framework of obtaining valid informed consent in clinical trials, the creation of a comprehensible consent document is not merely an administrative task—it is an ethical imperative. The informed consent form (ICF) serves as the foundational record of the participant's agreement and a reference source throughout the study. Its effectiveness hinges on the participant's ability to read, understand, and reflect upon its content. Regulatory bodies, including the FDA, and ethical principles outlined in the Belmont Report, emphasize that true informed consent depends on comprehension, which is severely compromised if the document is written in complex, technical language [10] [26]. This document outlines the application notes and protocols for developing ICFs that adhere to the recommended 8th-grade reading level, thereby fostering valid informed consent.
The Rationale for Plain Language and Readability
The transition towards participant-centric clinical research has solidified the role of clear communication as a cornerstone of ethical practice.
- Ethical Foundations: The Belmont Report's principle of Respect for Persons requires that subjects be given the opportunity to choose what will or will not happen to them. This autonomy is meaningless if the information provided to facilitate choice is incomprehensible [10].
- Comprehension Gap: Empirical evidence consistently reveals a significant gap between the intended meaning of ICFs and participant understanding. A 2021 survey of research staff found that 56% were concerned about whether participants had understood complex information [27]. Studies evaluating readability have demonstrated that many consent forms are written at a grade level of 10-11 or higher, far exceeding the recommended 8th-grade level and the average reading ability of the public [26] [28].
- Regulatory Guidance: U.S. regulatory agencies explicitly recommend that written ICFs contain "easy-to-read and understandable information so a lay person can make an informed decision about participating in a study" [10]. The Johns Hopkins Medicine IRB, for instance, recommends the ICF reading level be no higher than 8th grade [29].
Quantitative Readability Assessments
To ensure compliance with readability standards, objective metrics should be employed. The following table summarizes the common readability indices and their target values for ICFs.
Table 1: Readability Indices for Informed Consent Form Assessment
| Index | Target for ICFs | Interpretation of Scores | Formula Basis |
|---|---|---|---|
| Flesch Reading Ease (FRES) | 60-70 (Standard) or higher [30] | Scores 0-29: Very Confusing; 30-49: Difficult; 50-59: Fairly Difficult; 60-69: Standard; 70-79: Fairly Easy [30] | Word length and sentence length [26] |
| Flesch-Kincaid Grade Level | ≤ 8th Grade [29] | Translates the FRES into a U.S. school grade level (e.g., 8.0 = 8th grade) [26] | Word length and sentence length [26] |
| Gunning Fog Index | 7 or 8 [26] | The result indicates the years of formal education needed to understand the text on first reading. A score above 12 is too hard for most readers. [26] | Sentence length and complex words (3+ syllables) [26] |
Experimental Protocol: Readability Analysis
Purpose: To objectively determine the reading grade level of a draft informed consent document. Methodology:
- Document Preparation: Compile the complete text of the ICF in a word processing software like Microsoft Word. Omit headers, footers, and page numbers for analysis.
- Software Configuration:
- In Microsoft Word, navigate to: File > Options > Proofing.
- Under "When correcting spelling and grammar in Word," ensure "Check grammar with spelling" is selected.
- Select the "Show readability statistics" check box [29].
- Analysis Execution: Run a full spelling and grammar check on the document. Upon completion, a Readability Statistics dialog box will appear.
- Data Recording: Record the Flesch Reading Ease score and the Flesch-Kincaid Grade Level.
- Interpretation: Compare the obtained scores to the targets in Table 1. If the grade level exceeds 8.0, iterative revisions are required.
A Protocol for Drafting and Simplifying Consent Documents
Achieving an 8th-grade reading level requires a systematic approach to writing. The following workflow and detailed tips provide a concrete protocol for researchers.
Diagram 1: ICF Plain Language Development Workflow. This diagram outlines the iterative process of drafting, revising, and validating an informed consent form for readability.
Application Notes for Plain Language:
Word Choice:
- Use common, short words (≤ 3 syllables) [29] [30]. For example, use "about" instead of "approximately," "use" instead of "utilize," and "help" instead of "facilitate" [30].
- Replace medical jargon with plain language. Do not provide the jargon and the definition in parentheses; simply use the plain term [30]. For instance, use "high blood pressure" instead of "hypertension."
- Be consistent with terminology (e.g., use "study drug" consistently, not alternating with "investigational medication") [29].
Sentence Structure:
Document Formatting:
- Use a 12-point sans-serif font (e.g., Arial, Calibri) [30].
- Ensure margins are at least 1 inch to provide ample white space [30].
- Use left-justified, right-ragged text alignment to give readers visual cues [30].
- Keep paragraphs short and focused on one idea [29].
- Use bulleted or numbered lists for three or more items [30].
- Highlight critical points using bold or italics, but avoid using ALL CAPS or excessive highlighting, which can reduce readability [29] [30].
Table 2: Research Reagent Solutions for Consent Document Development
| Tool / Resource Name | Function / Utility | Specific Application in ICF Development |
|---|---|---|
| Microsoft Word Readability Statistics | Built-in software tool to calculate Flesch-Kincaid Grade Level and Flesch Reading Ease. | Provides an immediate, quantitative assessment of a draft ICF's reading difficulty [29]. |
| Online Readability Checkers | Web-based platforms (e.g., Automatic Readability Checker) that analyze text passages. | Offers an alternative or verification method for readability scores independent of word processing software [30]. |
| Layperson Reviewer | A non-exist, non-colleague who represents the potential study population. | Performs a "comprehension check" by reading the ICF and explaining the study back in their own words; identifies confusing jargon or concepts [29] [30]. |
| Plain Language Thesaurus/Websites | Online glossaries (e.g., "Everyday Words for Public Health Communication" from CDC) that suggest simple alternatives for complex terms. | Aids in the systematic replacement of scientific and technical jargon with language accessible to a lay audience [29] [30]. |
| "Teach Back" Method | A communication protocol wherein the participant is asked to state what they have learned in their own words. | Used during the consent process (post-document development) to verify and confirm understanding of the study information [27]. |
Advanced Considerations and Protocol Validation
- Comprehension vs. Readability: Readability scores are a measure of reading difficulty, not a direct measure of understanding. A document can be written at a low grade level but still address concepts that are difficult to grasp [28]. Therefore, readability must be paired with techniques that verify conceptual comprehension, such as the Teach Back method [27].
- Electronic Informed Consent (eIC): Digital platforms for consent are increasingly common. Studies show that eIC can support comprehension comparable to paper, enhance the completeness of required fields, and does not impose a significant technology burden on participants [31]. eIC platforms can integrate multimedia elements (videos, interactive quizzes) that may further improve understanding.
- Protocol for Non-English Speaking Participants: For participants who do not speak English, a simple translation of a complex English form is insufficient. The short-form consent process, which involves an interpreter and an impartial witness, can be used for initial enrollment under certain conditions. However, for FDA-regulated studies, a fully translated consent form in the participant's language must be provided promptly after the short form is used [32].
Preparing an informed consent document using plain language at an 8th-grade reading level is a critical and achievable component of obtaining valid informed consent. By adhering to a structured protocol that involves iterative drafting guided by plain language principles, objective readability testing, and validation through layperson review, researchers can create documents that truly honor the ethical principle of respect for persons. This rigorous approach to communication minimizes the gap between disclosure and comprehension, thereby strengthening the integrity of the entire clinical research process.
Obtaining valid informed consent is a cornerstone of ethical clinical research, serving as the primary mechanism for protecting participant autonomy and rights. The process transcends mere regulatory compliance, representing a fundamental ethical commitment to participant understanding and voluntary participation. The complexity of modern clinical trials, however, presents significant challenges to achieving genuine comprehension. The Key Information Section (KIS) has emerged as a critical structured approach to enhancing participant understanding by presenting core information in a clear, concise, and accessible format. This mandate represents a paradigm shift from legalistic documentation to participant-centered communication, requiring systematic implementation within the clinical trial protocol framework.
International guidelines, including the International Council for Harmonisation Good Clinical Practice (ICH-GCP) principles, emphasize that the investigator's fundamental duty is to ensure the welfare of participants under their care, which inherently includes guaranteeing that consent is properly informed and voluntarily given [33]. The updated SPIRIT 2025 statement, which provides evidence-based guidance for clinical trial protocols, reinforces this ethical foundation through enhanced reporting requirements for participant-facing materials [34]. Within this evolving regulatory landscape, the KIS functions not as another administrative hurdle but as a scientifically-validated tool for improving information retention and promoting meaningful consent.
Regulatory Framework and Core Components
Evolving Regulatory Standards
The mandate for a Key Information Section aligns with global regulatory trends emphasizing transparency and participant engagement. The SPIRIT 2025 statement introduces systematic requirements for protocol content, including explicit attention to how participants will be informed throughout the trial process [34]. This updated guidance consists of a 34-item checklist that serves as a foundational framework for protocol development, emphasizing completeness and transparency in describing trial procedures and participant interactions.
Regulatory authorities recognize that traditional consent documents often exceed reasonable comprehension levels for many participants. The KIS addresses this discrepancy by distilling complex trial information into essential elements that facilitate understanding. According to ICH-GCP perspectives, the sponsor holds ultimate responsibility for trial quality and participant safety, while investigators bear direct responsibility for proper consent acquisition [33]. This shared accountability necessitates careful attention to how key information is structured and presented throughout the consent process.
Essential Elements of the Key Information Section
The Key Information Section must present the most critical information that a prospective participant needs to make an informed decision. Based on regulatory guidance and human factors research, the following core components represent the minimum required elements:
- Purpose Statement: Clear explanation that the activity is research, what the study is designed to investigate, and who is being invited to participate.
- Trial Duration and Commitment: Realistic description of the expected time commitment, including the total study duration, number of study visits, and procedures involved at each visit.
- Foreseeable Risks and Discomforts: Prominent disclosure of the most serious and most frequent risks associated with the investigational product and study procedures.
- Potential Benefits: Balanced presentation of any potential direct benefits to participants, along with a clear statement that there may be no direct benefit.
- Alternative Options: Description of appropriate alternative procedures or courses of treatment that might be advantageous to the participant outside the research context.
- Voluntary Participation and Withdrawal Rights: Explicit statements that participation is voluntary, that refusal to participate involves no penalty or loss of benefits, and that the participant may discontinue participation at any time.
- Compensation and Treatment for Injury: Clear information about whether any compensation or medical treatment is available for research-related injuries.
Quantitative Analysis of KIS Implementation
SPIRIT 2025 Protocol Requirements for Participant Communication
The updated SPIRIT 2025 statement provides specific checklist items relevant to structuring information for participants and obtaining valid consent. The following table summarizes the key protocol requirements:
Table 1: SPIRIT 2025 Checklist Items Relevant to Informed Consent and Participant Communication
| Section | Item No. | Checklist Item Description | Relevance to KIS Implementation |
|---|---|---|---|
| Administrative Information | 1b | Structured summary of trial design and methods | Provides foundation for KIS content development |
| Open Science | 8 | Plans to communicate trial results to participants | Extends transparency beyond initial consent process |
| Introduction | 9a | Scientific background and rationale, including benefits and harms | Informs risk-benefit communication in KIS |
| Methods | 11 | Details of patient or public involvement in design, conduct, and reporting | Supports participant-centered KIS development |
| Ethics and Dissemination | 31 | Plans for seeking informed consent | Requires description of consent process including KIS |
| Ethics and Dissemination | 33 | How and by whom informed consent will be obtained | Ensures proper implementation of KIS in consent process |
Research Reagent Solutions for Consent Comprehension Assessment
Validating the effectiveness of the Key Information Section requires methodological rigor. The following table details essential methodological tools and approaches for developing and testing KIS comprehensibility:
Table 2: Essential Methodological Tools for KIS Development and Validation
| Tool Category | Specific Instrument/Approach | Function in KIS Implementation |
|---|---|---|
| Readability Metrics | Flesch-Kincaid Grade Level, SMOG Index | Quantifies reading level and identifies complex language requiring simplification |
| Comprehension Assessment | Validated questionnaires, Teach-back method | Measures actual understanding of key trial concepts after KIS review |
| Participant Engagement Tools | eConsent platforms with embedded multimedia | Enhances KIS presentation through interactive elements and visual aids |
| Quality Assurance Systems | Electronic Case Report Forms (eCRF) | Ensures consent documentation integrity; EDC systems provide audit trails for consent data [35] |
| Regulatory Documentation | Annotated Case Report Forms (aCRF) | Documents where consent information maps to data collection points in trial documentation [36] |
Experimental Protocol: Implementing and Validating the KIS
KIS Development and Testing Workflow
The following diagram illustrates the systematic approach to developing, testing, and implementing an effective Key Information Section:
KIS Development and Testing Workflow
Detailed Methodological Approach
Phase 1: Content Development and Readability Assessment Begin by extracting core trial information from the protocol, focusing specifically on elements listed in Table 1. Draft the initial KIS using plain language principles, aiming for a 6th-8th grade reading level. Apply validated readability metrics (e.g., Flesch-Kincaid) to quantify reading level and identify problematic phrasing. Research indicates that traditional consent forms often exceed a 12th grade reading level, creating significant comprehension barriers that the KIS specifically aims to address.
Phase 2: Multi-stakeholder Review and Cognitive Testing Convene a review panel including at least two investigators, one ethics committee representative, and three patient representatives. Incorporate feedback regarding medical accuracy, ethical concerns, and participant perspective. Subsequently, conduct cognitive interviews with 10-15 individuals representing the target participant population, using verbal probing to assess understanding of key concepts. This iterative process ensures the KIS addresses actual rather than perceived participant information needs.
Phase 3: Implementation and Validation Train all consenting personnel on the proper use of the KIS within the overall consent process, emphasizing its role as a discussion aid rather than a replacement for conversation. Implement a structured assessment of comprehension following the consent discussion, using a brief validated instrument to measure understanding of core concepts. Document the entire development process and comprehension outcomes in the trial master file, creating evidence of the systematic approach to supporting valid informed consent.
Integration with Broader Trial Documentation Systems
The Key Information Section does not exist in isolation but must integrate seamlessly with broader clinical trial documentation systems. The Case Report Form (CRF), whether paper-based or electronic (EDC), serves as the primary tool for collecting and recording trial data, including documentation of the consent process [35]. The annotated CRF (aCRF) provides critical metadata that maps data points from source documents to submission datasets, creating a transparent chain of documentation that supports data integrity [36].
Electronic data capture systems enhance this integration by providing automated checks and audit trails. Modern EDC systems should include functionality for "automatic checks, data query management, source data verification, electronic signature, database locking, and data export" [35]. These features provide the technical infrastructure supporting compliant consent documentation, particularly when the KIS is implemented within electronic consent platforms.
The principles of structured information presentation extend beyond the initial consent document. The Clinical Study Data Reviewer's Guide (cSDRG) and Define-XML documents provide standardized metadata that support regulatory review by comprehensively describing dataset structures and relationships [36]. This ecosystem of structured documentation works in concert to enhance transparency, facilitate understanding at multiple levels, and ultimately support the ethical conduct of clinical research.
The mandate for a Key Information Section represents a significant advancement in the ethical conduct of clinical research. By systematically structuring essential information to enhance comprehension, the KIS moves beyond procedural compliance toward meaningful participant engagement. Successful implementation requires methodological rigor, multi-stakeholder collaboration, and seamless integration with broader trial systems. When properly developed and implemented, the KIS serves as both an ethical imperative and a practical tool for fostering genuine understanding, ultimately strengthening the foundation of trust upon which clinical research depends. As the field continues to evolve, the principles of structured information presentation will undoubtedly expand to other participant-facing materials, further advancing the goal of truly participant-centered clinical research.
Within the framework of obtaining valid informed consent in clinical trials, the process itself is recognized as a cornerstone of ethical research, safeguarding participant autonomy and ensuring patient-centered care [1]. It is a dynamic communication process, far exceeding the act of merely signing a form [1]. The validity of this consent is profoundly influenced by the conditions under which it is obtained. This application note provides detailed protocols focused on three critical, yet often undervalued, dimensions of the consent process: the environment where the discussion occurs, the timing of the conversation, and the qualifications of the personnel involved. Optimizing these factors is essential for moving beyond a culture of simple compliance to one of ethical commitment and robust participant understanding [37].
Quantitative Data on Consent Process Factors
Empirical research highlights significant disparities between research staff and participant experiences, underscoring the need for improved protocols. The following table synthesizes key quantitative findings from recent studies.
Table 1: Quantitative Data on Consent Process Experiences from Research Staff and Participants
| Aspect of Consent Process | Research Staff Perspective | Research Participant Perspective | Source |
|---|---|---|---|
| Confidence in Facilitation | 74.4% felt confident or very confident. | (Not directly measured in participant-facing studies) | [6] |
| Concern for Participant Understanding | 56% were concerned about participants' understanding of complex information. | (Contrast: Participants are often overwhelmingly positive about their experience.) | [6] |
| Adequacy of Information Leaflets | 63% felt information leaflets were too long and/or complicated. | (Correlates with findings on health literacy and comprehension.) | [6] |
| Time as a Barrier | 40% felt that time constraints were a barrier to an effective process. | Highlighted the importance of having sufficient time as a key positive factor. | [6] |
| Impact of Health Literacy | (Associated with lower comprehension) | Limited health literacy was associated with significantly lower overall comprehension scores (β -9.02, p<.001). | [38] |
| Impact of Language (Spanish vs. English) | (Associated with lower comprehension) | Use of Spanish for medical communication was associated with significantly lower overall comprehension (β -5.30, p=.01). | [38] |
Experimental Protocols for Assessing and Optimizing the Consent Discussion
To ensure the consent process is valid and meaningful, researchers should implement structured protocols. The following sections detail methodologies for evaluating and improving the environment, timing, and personnel involved.
Protocol for Evaluating the Consent Environment and Participant Comprehension
This protocol is designed to assess the physical and psychological setting of the consent discussion and measure its effectiveness on participant understanding [6] [39].
Table 2: Key Reagents and Tools for Consent Evaluation
| Research Reagent / Tool | Function / Explanation |
|---|---|
| Quality of Informed Consent (QuIC) Instrument | A validated 20-item questionnaire to objectively measure participant comprehension of the informed consent, including domains of purpose, procedures, risks, benefits, and voluntariness. Scores range from 0-100 [38]. |
| Participant Satisfaction Survey | A customized survey using Likert scales and open-ended questions to quantify participant perceptions of the time, timing, location, and level of explanation provided during the consent process [6]. |
| Health Literacy Assessment Tool | A brief screening tool, such as a subset of questions from established measures, to identify participants who may need additional communication support. Examples include the Newest Vital Sign or single-item screeners [38]. |
| Teach-Back Method Guide | A structured protocol for research staff to ask participants to explain key study information in their own words. This is used not as a test of the participant, but to confirm the staff's explanation was clear [1] [39]. |
| Standardized Consent Environment Checklist | A checklist to ensure each consent discussion occurs in a location that meets all protocol-defined criteria for privacy, minimal noise, and freedom from interruptions. |
Procedure:
- Preparation: Prior to the consent discussion, the research staff should confirm the availability of a private room or space. The QuIC questionnaire and satisfaction survey should be prepared in the participant's primary language.
- Consent Discussion: Conduct the informed consent process in the designated environment, following the institution's standard operating procedure.
- Comprehension Assessment: Immediately following the discussion and before signing the consent form, administer the QuIC instrument to the participant.
- Teach-Back Validation: For key concepts (e.g., randomization, primary risks, right to withdraw), the research staff will employ the teach-back method, using a script such as: "To make sure I explained everything clearly, could you please tell me in your own words what you understand about [key concept]?"
- Satisfaction Assessment: After the participant completes the QuIC, administer the satisfaction survey.
- Data Analysis: Analyze QuIC scores overall and by domain. Correlate comprehension scores with satisfaction data and environmental variables (e.g., location type, duration of discussion). A significant proportion of participants scoring below a pre-defined threshold (e.g., < 80% on the QuIC) indicates a need for process improvement.
Protocol for Establishing Optimal Timing and Personnel Criteria
This protocol outlines a methodology for defining and auditing the timing of the consent approach and the training requirements for personnel obtaining consent [37] [16].
Procedure:
- Define Timing Parameters:
- Establish a standard that potential subjects must not be approached for consent during periods of high emotional distress, such as immediately after a life-altering diagnosis. A guideline of allowing a week to accept a diagnosis before discussing trial enrollment has been recommended [37].
- Mandate that the initial consent discussion must occur in an unhurried atmosphere, allowing participants ample time to review the document and ask questions. The process must be presented as a non-rushed interaction [37].
- Implement a policy that participants are encouraged to take the consent document home, discuss it with family, friends, or their primary care physician, and return after a reflection period (e.g., 24-48 hours) to provide their final decision [16].
- Establish Personnel Qualifications:
- Define that only individuals with appropriate credentials, qualifications, and experience in the field of study are permitted to obtain consent. This ensures they can adequately answer participant questions [37].
- Require all personnel who obtain consent to complete structured, ongoing training on facilitating informed consent discussions. This training must cover GCP guidelines, institutional IRB requirements, and communication techniques for complex concepts [6].
- Incorporate specific training on working with interpreters and utilizing translated consent documents, including the process of translation and back-translation to ensure accuracy and comprehensibility [38] [37].
- Audit and Monitoring:
- Conduct routine audits of consent forms to ensure the correct, approved versions are used and that documentation is complete.
- Track the time allocated for consent discussions and monitor for correlations with participant comprehension scores and satisfaction.
- Perform direct observation of consent discussions by trained auditors to assess staff adherence to timing, environment, and communication protocols.
Visualization of Workflows
Consent Environment Setup Protocol
The following diagram illustrates the logical workflow for preparing the optimal environment and process for a valid consent discussion.
Personnel Qualification and Training Workflow
This diagram outlines the logical relationships and decision process for qualifying personnel to conduct informed consent discussions.
Employing the Teach-Back Method to Verify Participant Understanding
Within the ethical and regulatory framework of clinical trials research, obtaining valid informed consent is a foundational requirement. Valid consent transcends the mere signing of a document; it requires that participants possess a genuine understanding of the trial's purpose, procedures, risks, and benefits [22]. However, studies consistently reveal a significant gap in participant comprehension. Research indicates that patients immediately forget between 40% and 80% of the medical information provided, and nearly half of the information they do retain is incorrect [40]. A systematic review of informed consent measures further highlights that the primary focus of most assessment tools is on understanding, underscoring its central role in ethical research conduct [41].
The Teach-Back method emerges as a robust, evidence-based solution to this challenge. It is a structured communication technique where investigators assess a participant's understanding by asking them to explain, in their own words, the information that has just been conveyed [40] [42]. This process creates a feedback loop, allowing for the immediate identification and correction of misunderstandings. This application note details how clinical researchers can integrate Teach-Back into the informed consent process to fulfill the ethical imperative of ensuring participant comprehension, thereby strengthening the validity of the consent obtained.
Core Principles and Empirical Support for Teach-Back
Definition and Key Mechanisms
Teach-Back, also known as "closing the loop," is a health literacy universal precaution founded on active learning principles. It shifts the responsibility for clear communication from the participant to the researcher [43]. The core mechanism involves a cyclical process of:
- Explanation: Providing information in plain, jargon-free language.
- Assessment: Asking the participant to restate the key points in their own words.
- Clarification: Re-explaining any misremembered or misunderstood concepts.
- Re-assessment: Repeating the cycle until the information is accurately understood [44].
This method moves beyond the ineffective question, "Do you understand?" which often elicits a perfunctory "yes" regardless of actual comprehension [40]. Instead, it uses open-ended questions to objectively verify understanding.
Evidence of Effectiveness in Healthcare and Research
Extensive evidence supports the effectiveness of Teach-Back in improving patient outcomes, which provides a strong rationale for its application in clinical trial consent.
Table 1: Empirical Evidence Supporting the Teach-Back Method
| Outcome Area | Findings | Citation |
|---|---|---|
| Patient Understanding & Knowledge | Patients who received Teach-back after discharge from an emergency department had significantly higher knowledge scores regarding their diagnosis, symptoms, and follow-up care. | [42] |
| Clinical Outcomes | A systematic review and meta-analysis demonstrated that discharge education using Teach-back significantly reduced readmission rates for patients with heart failure. | [44] |
| Patient Satisfaction | Studies show patients prefer the Teach-back method and report higher satisfaction with communication when it is used. | [40] [42] |
| Comprehension Verification | Teach-back allows researchers to verify that they have explained information clearly and identifies exactly which concepts require re-teaching. | [40] [45] |
Furthermore, a study focusing on informed consent measures identified core domains essential for valid consent, including Autonomy, Consequences, and Expectations [41]. The Teach-back method directly addresses these domains by ensuring participants understand the implications of their participation (Consequences) and the nature of the research (Expectations), thereby supporting a truly autonomous (Autonomy) decision.
Application Protocol: Integrating Teach-Back into the Informed Consent Process
This protocol provides a step-by-step guide for clinical researchers to implement Teach-back during the informed consent discussion for a clinical trial.
Pre-Consent Preparation
- Develop a Teach-Back Guide: Prior to the consent meeting, identify 3-5 critical concepts from the informed consent form that are essential for decision-making. These typically include:
- The research purpose and experimental nature of the intervention.
- Key procedures and the participant's time commitment.
- Potential risks and anticipated benefits.
- The randomization process (if applicable).
- The right to withdraw at any time without penalty.
- Formulate Open-Ended Questions: For each critical concept, craft open-ended questions that cannot be answered with "yes" or "no."
- Instead of: "Do you understand the risks?"
- Use: "To make sure I explained everything clearly, could you describe in your own words what the possible side effects of this new treatment might be?"
- Instead of: "Is that clear?"
- Use: "I know this can be complex. How would you explain the difference between the two study groups to your family member?"
Conducting the Consent Discussion with Teach-Back
- Set the Stage: Begin by explaining that you want to ensure you have been clear and that the information is understandable. Normalize the process by saying, "I want to be sure I've done a good job explaining this. So, after we go through each part, I'm going to ask you to explain it back to me in your own words. This helps me make sure I'm being clear." This frames Teach-back as a check on your communication skills, not a test of the participant's intelligence [40].
- Explain a Single Concept: Present one piece of information using plain language, avoiding medical jargon. Break down complex ideas into manageable segments.
- Request a Teach-Back: Ask one of your pre-prepared, open-ended questions related to the concept you just explained.
- Listen and Assess: Listen carefully to the participant's response. Assess for accuracy and completeness.
- Clarify and Re-teach if Necessary: If the response is incorrect or incomplete, respond with, "Thank you. I realize I didn't explain that quite right. Let me try again." Then, re-explain the information using different words or methods (e.g., a simple diagram).
- Repeat the Cycle: Ask the participant to Teach-back the concept again. Continue this loop of explaining, assessing, and clarifying until the participant can accurately articulate the information.
- Document the Process: Note in the study records that Teach-back was used to verify understanding of key consent elements. This provides evidence of your commitment to ensuring valid informed consent. The use of an electronic consent (eConsent) platform can facilitate the tracking of this process [22].
- Proceed Through All Concepts: Repeat steps 2-6 for each of the critical concepts you identified.
This workflow can be adapted for eConsent platforms by incorporating interactive checkpoints where participants are prompted to summarize information before proceeding.
Table 2: Key Resources for Implementing Teach-Back in Clinical Research
| Resource / Tool | Function / Purpose | Example / Notes |
|---|---|---|
| Plain Language Consent Forms | Foundation for understanding; reduces cognitive load. | Use active voice, short sentences, and define technical terms. Required by ICH GCP guidelines. |
| Pre-Defined Open-Ended Questions | Standardizes the assessment of comprehension across study sites and staff. | Questions tailored to the study's critical consent concepts (e.g., risks, randomization). |
| eConsent Platform | Enhances the consent process with multimedia and tracking. | Platforms like Castor eConsent can integrate Teach-back prompts, record participant interactions, and manage version control [22]. |
| Observation Tool (T-BOT) | Aids in training and quality assurance by assessing researcher competency. | The refined Teach-back Observation Tool (T-BOT) provides a validated means to score and improve the use of Teach-back skills [45]. |
| AHRQ Teach-Back Training Toolkit | Provides comprehensive training materials for researchers. | Includes videos, a self-evaluation log, and learning modules from the Agency for Healthcare Research and Quality [40]. |
The integration of the Teach-Back method into the clinical trial informed consent process is a pragmatic and powerful strategy to bridge the gap between information disclosure and genuine participant understanding. By adopting this participant-centered approach, researchers can move beyond a procedural formality to a meaningful ethical dialogue. This not only strengthens the validity of the consent obtained and upholds the principle of respect for persons but also enhances participant trust and engagement throughout the trial. In an era demanding higher standards for research transparency and ethics, Teach-back provides a simple, evidence-based tool to ensure that informed consent is truly informed.
In the ethical framework of clinical research, obtaining a participant's informed consent is a process, but the documentation of that consent serves as its critical, verifiable record. Proper documentation is not merely an administrative task; it is the tangible evidence that the consent process adhered to ethical and regulatory standards, thereby protecting participant rights and data integrity. Within a broader thesis on obtaining valid informed consent, this article addresses the specific protocols for signature requirements and the subsequent secure storage of consent documents. These procedures ensure that the foundational principle of respect for persons is upheld not just in conversation, but in durable, accountable practice. Failure to correctly execute and store consent documentation can compromise an entire study, leading to regulatory sanctions and the invalidation of research data [46] [9].
Signature and Documentation Requirements
The signature on an informed consent form (ICF) is the culmination of a successful consent process. It must be obtained under specific conditions to be considered valid.
Core Elements of Consent Documentation
For a consent form to be legally and ethically sound, it must contain specific core elements that provide comprehensive information to the participant. Based on an analysis of regulatory requirements, a 2025 guideline identified 75 core elements for consent forms, grouped into several key categories [47].
Table: Core Categories for Informed Consent Documentation
| Category | Description | Key Inclusions |
|---|---|---|
| Participant Rights | Information on the voluntary nature of participation and participant rights [47] [48]. | Right to withdraw without penalty, voluntary participation statement [47]. |
| Study Overview | Details what participation in the study involves [47] [48]. | Study purpose, procedures, duration, and experimental design (e.g., randomization) [47]. |
| Risks and Benefits | outlines the potential harms and benefits of participation [47] [48]. | Description of reasonably foreseeable risks and reasonable expected benefits [47]. |
| Data Protection | Explains how participant confidentiality will be maintained [47]. | Data handling, privacy measures, and use of biological samples [47]. |
| Consent Execution | The section where agreement is formally documented [47]. | Signatures, dates, and, if applicable, assent procedures [47]. |
Signature Protocols and Best Practices
The act of signing the document must be performed in accordance with strict standards to ensure its authenticity and reliability.
- Attributable and Contemporaneous Signing: The signature, date, and time must be recorded by the person obtaining consent at the time the process occurs, not added later [49] [46]. This practice ensures the documentation is attributable and contemporaneous [49].
- Correcting Errors: If an error is made on a paper consent form, the correction must be made by drawing a single line through the incorrect entry, then initialing and dating the correction. It is strictly forbidden to obliterate the entry or use whiteout [49].
- Comprehension Verification: The individual obtaining consent must assess the participant's understanding, often using the "teach-back" method, where the participant explains the study in their own words. This verification should be documented in the source notes [46] [1].
- Version Control: Researchers must use the most current IRB-approved version of the ICF. Using an outdated form is a common audit finding and can invalidate consent [46].
Storage and Retention Protocols
Once properly executed, the consent document becomes a vital research record that must be stored securely and retained for a defined period.
Electronic Storage Best Practices
The transition to electronic storage for research documents is common, but it requires specific protocols to ensure the copies are certified and secure [50].
- Certified Copies: A certified copy is defined as a copy verified by a dated signature as an exact copy possessing all the same attributes and information as the original [50]. The certification process must confirm that:
- All pages are present and legible.
- The copy is an exact replica of the original.
- For consent documents, each is bookmarked appropriately [50].
- Secure Storage Locations: Electronic files should be stored on secure, backed-up institutional servers (e.g., WUSTL Box, REDCap, Research Storage Project) rather than on individual desktops or laptops, which are more vulnerable [50].
- IRB Approval and Sponsor Permission: Converting paper documents to electronic files typically requires prior approval from the Institutional Review Board (IRB). For sponsored trials, written permission from the sponsor must also be obtained and filed with the study documents [50].
Retention Requirements and Destruction
Regulatory bodies mandate minimum retention periods for research documents, including ICFs.
- Retention Period: Electronic files of research documents should be kept for a minimum of 6 years following the formal closure of the study, or longer if required by institutional policy or the study sponsor [50].
- Destruction of Paper Originals: After all records are scanned and certified, the paper copies can be destroyed, reducing physical storage burdens [50].
The following workflow diagram illustrates the complete lifecycle of a consent document, from creation through to final storage, integrating the key requirements and protocols discussed.
The Researcher's Toolkit: Essential Materials for Consent Documentation
Table: Essential Reagents and Solutions for Consent Documentation
| Tool/Solution | Function | Key Features & Compliance |
|---|---|---|
| IRB-Approved Informed Consent Form (ICF) | The legally approved document presented to the participant. | Contains all required elements [47] [48]; has a valid version number and date [46]. |
| Electronic Consent (eConsent) Platform | A digital system for presenting consent information and capturing signatures. | Must be 21 CFR Part 11 compliant [46]; provides an audit trail and version control [46] [50]. |
| Secure Electronic Storage System | A protected digital environment for storing certified copies of consent documents. | Institutional servers (e.g., WUSTL Box) [50]; provides data backup and access controls [50]. |
| Document Certification Form | A form used to verify that a scanned electronic copy is an exact and complete replica of the original paper document. | Dated signature of the certifier [50]; confirms all pages are present and legible [50]. |
| Readability Assessment Tool | Software or formula to evaluate the reading level of the consent document. | Flesch-Kincaid Grade Level [51] [52]; ensures language is at an 8th-grade level or lower [51] [48]. |
The meticulous documentation and storage of informed consent are non-negotiable components of valid consent in clinical research. Adherence to precise signature requirements and robust storage protocols provides a verifiable chain of custody for consent documents, thereby upholding the ethical integrity of the research process and ensuring regulatory compliance. By implementing these detailed application notes and protocols, researchers and drug development professionals can fortify the foundation of trust with participants and safeguard the legitimacy of their scientific endeavors.
Navigating Complex Scenarios and Enhancing Participant Understanding
Strategies for Consent with Vulnerable Populations (Children, Cognitively Impaired)
Within the context of clinical trials, the principle of informed consent serves as the ethical foundation, ensuring participants autonomously agree to partake after understanding the purpose, risks, and benefits of the study [9]. However, obtaining valid informed consent becomes particularly complex when involving vulnerable populations, defined as groups whose limited decision-making ability, disadvantaged status, or lack of power increases their susceptibility to coercion, manipulation, or harm by unscrupulous researchers [53]. These groups include, but are not limited to, children and individuals with cognitive impairments. The historical exclusion of these populations from clinical research has led to a critical gap in evidence regarding the safety and efficacy of treatments for these groups [53] [54]. Conversely, historical abuses have also occurred where vulnerable populations were targeted because they were accessible and unprotected [53]. Therefore, modern clinical research faces the dual imperative of including these populations to ensure generalizability of findings while implementing rigorous, ethically sound strategies to protect their rights and welfare [55] [54].
This document outlines specific application notes and protocols for engaging two key vulnerable populations—children and cognitively impaired individuals—within the informed consent process. The goal is to provide researchers, scientists, and drug development professionals with actionable methodologies that align with regulatory requirements and ethical principles, thereby supporting the broader thesis that valid consent is achievable even in challenging contexts.
Defining Vulnerability and Regulatory Framework
Conceptualizing Vulnerability
Vulnerability in research is not an inherent trait but rather a condition stemming from various sources. Policy documents and ethical guidelines often operationalize vulnerability through a categorical or group-based approach, identifying specific populations such as children, prisoners, and cognitively impaired individuals as vulnerable [54]. A more nuanced, analytical approach identifies the sources of vulnerability, which can be categorized into three accounts:
- Consent-based accounts: Vulnerability arises from a compromised capacity to provide free and informed consent due to undue influence, reduced autonomy, or impaired decision-making ability [54].
- Harm-based accounts: Vulnerability is characterized by a higher probability of incurring harm or injury during the course of research [54].
- Justice-based accounts: Vulnerability stems from unequal conditions and systemic barriers that limit opportunities for fair participation in research [54].
For children and cognitively impaired individuals, the challenges are primarily rooted in consent-based and harm-based accounts, necessitating tailored strategies to address their specific needs.
Key Regulatory and Ethical Guidelines
Researchers must adhere to a robust framework of international and national regulations. Key documents include the Declaration of Helsinki, the Belmont Report (which first formally introduced the concept of vulnerability), and the International Council for Harmonisation (ICH) guidelines [55] [54] [9]. Regulatory bodies like the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) provide specific guidance, such as ICH E11 for pediatric populations and ICH E7 for geriatric populations [55]. In the United States, the FDA's 21 CFR Part 50 provides the specific regulations for the protection of human subjects, with Subpart D offering additional protections for children [9]. Central to this framework is the oversight by an Institutional Review Board (IRB) or Ethics Committee (EC), which must review and approve all protocols involving vulnerable subjects to ensure that adequate safeguards are in place [55].
Table 1: Core Regulatory Bodies and Guidelines for Vulnerable Populations
| Regulatory Body/Guideline | Core Focus | Relevance to Vulnerable Populations |
|---|---|---|
| Declaration of Helsinki [9] | Foundational ethical principles for human subject research. | Emphasizes special protections for vulnerable groups. |
| Belmont Report [54] [9] | Ethical principles: Respect for Persons, Beneficence, Justice. | Identifies vulnerable populations and justifies protective measures. |
| FDA 21 CFR Part 50 [9] | Protection of human subjects in U.S. clinical trials. | Subpart D outlines specific requirements for children. |
| ICH E6(R2) Good Clinical Practice [9] | Global standard for clinical trial conduct. | Requires protocols to justify inclusion of vulnerable subjects and detail safeguards. |
| ICH E11 [55] | Clinical trials in pediatric populations. | Provides a framework for the ethical conduct of pediatric clinical trials. |
Quantitative Evidence on Consent Practices
Empirical research on the informed consent process reveals significant insights from both research participants and staff, highlighting areas for improvement. A 2021 survey of 169 research participants and 115 research staff in Ireland and the UK quantified perceptions of the consent process [27].
Table 2: Research Staff and Participant Perspectives on the Informed Consent Process [27]
| Metric | Research Participant Perspective (n=169) | Research Staff Perspective (n=115) |
|---|---|---|
| Overall Experience | Overwhelmingly positive about their experience. | N/A |
| Key Participant Concern | The importance of having sufficient time for the consent discussion. | N/A |
| Staff Confidence | N/A | 74.4% felt very confident or confident facilitating consent discussions. |
| Information Comprehension | N/A | 56% were concerned about whether participants understood complex information. |
| Consent Documentation | N/A | 63% felt Participant Information Leaflets were too long and/or complicated. |
| Barriers to Effective Consent | N/A | 40% felt that time constraints were a significant barrier. |
| Requested Improvements | Value in receiving follow-up, such as study results. | Dominant theme: the importance of adequate time and resources. |
This data underscores the critical need for allocating sufficient time, simplifying consent documents, and actively verifying understanding—practices that are even more crucial when working with vulnerable populations.
Strategic Approaches for Pediatric Consent and Assent
Engaging children in research requires a dual process: obtaining permission from parents or legal guardians and seeking assent from the child. Assent is defined as the child's affirmative agreement to participate, distinct from mere failure to object [56] [9].
Application Notes
The approach must be tailored to the child's age, maturity, and psychological state. The process should be ongoing, reaffirmed throughout the study duration. The primary challenge is presenting information in a developmentally appropriate manner to ensure the child comprehends what participation entails. Furthermore, researchers must clearly differentiate the roles of the parent (who provides legal consent) and the child (who provides ethical assent) and be prepared to respect a child's decision to dissent or withdraw, even if the parent has given permission [56].
Experimental Protocol: Tiered Assent Process
Aim: To obtain meaningful and developmentally appropriate assent from pediatric participants in a clinical trial. Materials: Research Reagent Solutions as listed in Table 3. Table 3: Research Reagent Solutions for Pediatric Consent
| Item | Function in Protocol |
|---|---|
| Illustrated Assent Booklet | Uses age-appropriate visuals and simple language to explain procedures, risks, and benefits; improves comprehension. |
| Child-Friendly Assent Form | A short, simple form for the child to sign or mark; signifies their agreement. |
| Witness (e.g., Child Life Specialist) | An independent observer to ensure the process is conducted without coercion and to support the child. |
| Teach-Back Tool (e.g., Dolls/Diagrams) | A physical or visual aid to help the child explain back the study procedures in their own words. |
Methodology:
- Pre-Assent Preparation: Develop multiple versions of assent materials tailored to different age groups (e.g., 6-9, 10-12, 13-17 years). These must be reviewed and approved by the IRB/EC.
- Initial Discussion with Parent/Legal Guardian: First, conduct the full informed consent discussion with the parent(s) or guardian(s) without the child present. This allows adults to ask questions freely and make an informed decision.
- Child Assent Session: In a child-friendly environment, a trained researcher conducts the assent session.
- Use the prepared, age-appropriate materials.
- Clearly explain the study's purpose, what will happen, what is expected of them, and that they can stop at any time.
- Emphasize that their decision (to participate or not) will not get them or their parents into trouble.
- Employ the "teach-back" method: ask the child to explain what they understood in their own words.
- Documentation: Obtain the parent's signed informed consent form. Document the child's assent or dissent on the appropriate form. If the child is verbal, record their affirmative agreement. For non-verbal children, document behavioral cues indicating willingness.
- Ongoing Re-affirmation: At the beginning of each subsequent study visit, briefly re-explain the procedures and confirm the child's continued willingness to participate.
The following workflow diagram illustrates this multi-step protocol:
Strategic Approaches for Cognitively Impaired Populations
For individuals with cognitive impairments (e.g., dementia, intellectual disabilities), the capacity to provide fully independent informed consent may be limited or fluctuate. The ethical imperative is to involve them in the decision-making process to the greatest extent possible while ensuring their protection [56] [55].
Application Notes
Capacity is decision-specific and should not be viewed as an all-or-nothing state. A person may lack the capacity to understand complex trial designs but retain the capacity to understand basic procedures and express their feelings. The process often requires obtaining proxy consent from a legally authorized representative (LAR) while simultaneously seeking assent from the individual [55]. Researchers must be trained to identify and interpret verbal and non-verbal dissent, which can include behaviors like saying "no," pulling away, showing signs of distress, or a lack of cooperation [56]. The key is to create an accessible and supportive communication environment.
Experimental Protocol: Capacity-Adjusted Consent Process
Aim: To ethically enroll individuals with cognitive impairments in clinical research by integrating capacity assessment, proxy consent, and participant assent. Materials: Research Reagent Solutions as listed in Table 4. Table 4: Research Reagent Solutions for Consent with Cognitive Impairment
| Item | Function in Protocol |
|---|---|
| Brief Capacity Assessment Tool | A validated, short tool to gauge the participant's understanding of key study elements. |
| Legally Authorized Representative (LAR) | The individual legally empowered to provide informed consent on behalf of the participant. |
| Communication Training Manual for Staff | Guidelines on using simple language, identifying behavioral cues, and avoiding coercion. |
| Multimedia Consent Aids (Audio/Video) | Accessible formats to present information, supplementing written documents. |
Methodology:
- Pre-Screening and Identification: Identify potential participants who may have cognitive impairments through medical record review or clinician referral. The protocol must be pre-approved by an IRB/EC for this population.
- Initial Capacity Assessment: A qualified researcher administers a brief, standardized capacity assessment tool focused on the participant's ability to understand the nature of the research, its risks and benefits, and the alternatives.
- Triadic Consent Discussion: Conduct a joint discussion involving the researcher, the participant, and their LAR.
- Use clear, simple language and avoid technical jargon.
- Utilize multimedia aids to support comprehension.
- The researcher must directly and patiently engage the participant, checking for understanding and seeking their opinion.
- Determine Consent/Assent Pathway:
- If the participant is deemed to have capacity, proceed with standard informed consent.
- If capacity is impaired, obtain informed consent from the LAR. Simultaneously, seek assent from the participant. Crucially, respect any sign of dissent from the participant, which would override the LAR's consent.
- Documentation and Monitoring: Document the capacity assessment outcome, the LAR's signed consent form, and the participant's assent or dissent. Continuously monitor the participant's willingness and comfort level throughout the study, re-evaluating capacity if necessary.
The following diagram illustrates the decision-making pathway within this protocol:
Engaging vulnerable populations, specifically children and individuals with cognitive impairments, in clinical research is both a scientific necessity and an ethical obligation. As demonstrated, valid consent is not only achievable but also methodologically rigorous when using structured, population-specific strategies. The core principles underpinning these strategies include an unwavering commitment to respect for persons, which involves honoring the autonomy of individuals to the extent possible and protecting those with diminished autonomy; transparency in communication through plain language and accessible formats; and ongoing engagement that treats consent as a process rather than a single event. By implementing the detailed application notes and experimental protocols outlined herein, researchers can generate robust, generalizable data while upholding the highest ethical standards, ensuring that the benefits of clinical research are extended to all segments of the population.
Adapting the Process for Emergency and Critical Care Research
Clinical research in emergency and critical care settings presents fundamental ethical challenges in obtaining valid informed consent. In the intensive care unit (ICU), only approximately 10% of patients possess decisional capacity due to conditions such as trauma, shock, sedation, or the administration of mechanical ventilation [57]. This high prevalence of decisional incapacity creates significant barriers to enrolling critically ill patients in research, which can prolong study implementation, limit the generalizability of results, and ultimately delay the identification of effective treatments for life-threatening conditions [58]. The ethical principle of autonomy, which requires individuals to understand research and provide voluntary consent, conflicts with the practical realities of emergency medical research where therapeutic time windows are narrow and patients are rarely able to comprehend or communicate clearly [57] [58].
This application note addresses these challenges by providing evidence-based protocols and decision frameworks for adapting consent processes to critical care environments. These approaches balance the protection of participant autonomy with the practical necessities of conducting rigorous research in emergency settings, ensuring that critically ill patients are not denied opportunities to benefit from clinical research participation while maintaining ethical integrity [58].
Key Challenges in Emergency and Critical Care Consent
Patient-Related Challenges
The primary challenge in critical care research stems from the near-universal lack of patient decision-making capacity. Multiple factors contribute to this decisional incapacity, creating a complex ethical landscape for researchers [57]:
- Medical Conditions: The underlying illness causing ICU admission (e.g., trauma, shock, coma) directly impairs cognitive function and consciousness.
- Iatrogenic Factors: Sedative medications and analgesics administered for mechanical ventilation or pain management cloud judgment and consciousness.
- Psychological Stress: Extreme pain, anxiety, and fear of imminent death render patients unreceptive to information and unwilling to consider research participation.
- Undetected Impairment: Delirium affects up to one-third of ICU patients, with physicians recognizing less than one-third of these cases without specialized diagnostic instruments [57].
Even when patients appear competent, studies demonstrate poor recall of research information. One investigation found that only 32% of consenting ICU patients could recall the purpose of a trial and its related risks 10-12 days after providing consent [57].
Surrogate Decision-Maker Challenges
When patients lack capacity, surrogate decision makers (SDMs) become the primary source of consent, involved in over 90% of consent encounters in critical care settings [57]. However, this surrogate consent paradigm presents substantial challenges [57] [58]:
- High Stress Levels: SDMs experience significant emotional distress, with up to two-thirds suffering anxiety or depression when a loved one is hospitalized in the ICU.
- Impaired Decision-Making: Emotional suffering may compromise a surrogate's ability to process complex research information and rationally evaluate benefits and risks.
- Inaccurate Substituted Judgment: SDMs predict patients' treatment preferences with only 68% accuracy, with similar inaccuracies extending to research participation decisions [58].
- Psychological Burden: Being asked to provide consent for research associates with post-traumatic stress symptoms in 35% of family members of critically ill patients [58].
Table 1: Challenges with Surrogate Decision-Makers in Critical Care Research
| Challenge Category | Specific Issues | Impact on Research |
|---|---|---|
| Cognitive-Emotional | Anxiety, depression, information overload | Impaired comprehension and decision-making quality |
| Representation Accuracy | Limited knowledge of patient preferences | Decisions may not reflect patient's true wishes |
| Logistical | Difficulty identifying legal representative, availability | Recruitment delays, selection bias |
| Psychological Morbidity | Post-traumatic stress symptoms | Ethical concerns about surrogate welfare |
Systemic and Workflow Challenges
Research staff face significant operational barriers in obtaining valid consent in emergency settings. Surveys of research professionals reveal that 40% consider time constraints a major barrier, while 56% express concern about participant understanding of complex information [27]. Additionally, 63% of research staff report that informed consent documents are too long and complicated for effective use in emergency settings [27]. These challenges are compounded by the narrow therapeutic windows characteristic of critical care research, where delays in enrollment can directly impact patient outcomes and study validity.
Alternative Consent Models: Frameworks and Applications
Several alternative consent models have been developed and implemented to address the unique challenges of emergency and critical care research. The following decision pathway provides a structured approach to selecting the appropriate consent model based on study characteristics and patient circumstances:
Exception from Informed Consent (EFIC)
The Exception from Informed Consent (EFIC) model represents a carefully regulated approach for emergency research where obtaining prospective consent is not feasible. Regulated under 21 CFR 50.24 in the United States, EFIC permits research without explicit consent when specific conditions are met [59]:
- Life-Threatening Condition: Patients must have a life-threatening medical condition for which available treatments are unproven or unsatisfactory.
- Narrow Therapeutic Window: The investigation must be necessary to determine the safety and effectiveness of particular interventions.
- Infeasibility of Consent: Obtaining informed consent must not be feasible because the patient's condition prevents communication and there is insufficient time to contact a legal representative.
- Potential for Direct Benefit: The intervention must hold out the prospect of direct benefit to the patient.
- Community Consultation: Researchers must engage in community consultation and public disclosure before initiating the study [59].
EFIC requires intensive oversight by Institutional Review Boards (IRBs) and continuous monitoring of the research process to protect participant rights and welfare [59].
Deferred Consent Model
The deferred consent model involves enrolling patients in research without initial consent, then seeking consent from the patient or surrogate at the earliest appropriate opportunity. This approach is particularly valuable when the therapeutic window is too narrow to locate surrogates but the research involves ongoing interventions or data collection [59]. Key considerations include:
- Post-Enrollment Authorization: Consent is obtained specifically for the patient's continued participation in research after initial emergency interventions.
- Data Integrity Concerns: If consent for data review is not granted, missing data may introduce bias into the analysis [59].
- Ethical Questions: Philosophical concerns exist about whether subjects can meaningfully consent to procedures that have already occurred [59].
Evidence from critical care trials demonstrates general acceptance of deferred consent models. In one randomized controlled trial of pulmonary artery catheter use, only 3% of survivors approached for retrospective consent after regaining competency declined participation [58].
Prospective Consent Approach
Prospective consent involves identifying at-risk populations and obtaining consent before an emergency occurs. This model mirrors approaches used in organ donation and other predictable medical scenarios [59]. Implementation challenges include:
- Recruitment Difficulties: The low likelihood that any individual will develop the specific emergency condition complicates recruitment of adequate sample sizes.
- Comprehension Concerns: Questions remain about whether consent can be truly informed when the chance of actual participation is minimal.
- Operational Logistics: Robust systems must differentiate between patients who have consented, refused, or not been approached [59].
Hybrid and Two-Tiered Consent Models
Hybrid models combine elements of different consent approaches tailored to specific study risks and individual patient circumstances. These adaptive frameworks acknowledge that a single consent model may not suffice for all critical care research scenarios [58]. A two-tiered approach categorizes studies by risk level:
- Lower-Risk Studies: Utilize deferred consent, two-physician consent, or request for 'objection to consent' models.
- Higher-Risk Studies: Require more rigorous consent procedures, including surrogate consent or EFIC with enhanced safeguards.
Table 2: Comparative Analysis of Alternative Consent Models in Critical Care Research
| Consent Model | Regulatory Basis | Key Applications | Advantages | Limitations |
|---|---|---|---|---|
| Exception from IC (EFIC) | 21 CFR 50.24 (FDA) | Life-threatening conditions; narrow therapeutic windows | Enables vital emergency research; regulatory clarity | Requires community consultation; complex implementation |
| Deferred Consent | Various national regulations | Ongoing interventions after initial emergency; longitudinal data collection | More ethical than no consent; maintains research integrity | Ethical concerns about authorizing past actions |
| Prospective Consent | Institutional policy approval | Identifiable at-risk populations (e.g., pre-surgical) | Preserves autonomy; aligns with elective procedures | Limited applicability; low actual participation rate |
| Proxy Consent | Common law and statutes | Routine critical care research with available surrogates | Respects patient autonomy through representation | Surrogate stress; inaccuracy in predicting patient wishes |
| Two-Physician Consent | Specific national laws (e.g., UK) | Emergency situations without available surrogates | Practical solution for time-sensitive interventions | Limited to specific jurisdictions; potential conflicts |
Implementation Protocols and Practical Applications
Protocol for Exception from Informed Consent (EFIC) Implementation
The EFIC protocol requires meticulous planning and execution to meet regulatory requirements while maintaining ethical integrity [59]:
Pre-Study Phase:
- Protocol Design: Ensure the research addresses a life-threatening condition with potential for direct benefit and cannot practically be conducted without a consent waiver.
- Community Consultation: Engage in two-way communication with the communities from which subjects will be drawn, educating them about the research and the need for consent exceptions.
- Public Disclosure: Publicly disclose the study design, risks, and benefits before initiation and throughout the trial.
- IRB Approval: Obtain approval from a dedicated IRB that will provide intensive oversight throughout the study.
Study Execution Phase:
- Data Safety Monitoring: Implement an independent data monitoring committee to review accumulating data.
- Attempt Surrogate Contact: Make continued efforts to contact legal representatives during the study period.
- Patient/SDM Notification: Inform patients or their representatives at the earliest feasible opportunity of the patient's inclusion in the research.
- Request Consent for Continued Participation: Seek consent for any ongoing study procedures beyond the initial emergency intervention.
Post-Enrollment Phase:
- Debriefing: Provide comprehensive information to patients or surrogates about the research after initial stabilization.
- Consent for Data Use: Obtain consent for continued use of collected data and specimens when feasible.
- Outcome Reporting: Inform participants and the community about study results in an accessible format.
Protocol for Deferred Consent Implementation
The deferred consent protocol addresses both ethical and methodological concerns in critical care research [59]:
- Ethical Review: Obtain approval from the Research Ethics Board/IRB specifically for the deferred consent process, demonstrating that initial consent is not feasible and the research poses no more than minimal risk beyond standard care.
- Documentation: Clearly document in the research record the reasons why prospective consent could not be obtained, including time constraints and unavailability of surrogates.
- Timely Approach: Approach the patient (if capacity is regained) or SDM at the earliest feasible opportunity, typically within 48-72 hours of enrollment.
- Comprehensive Disclosure: Provide complete information about the study, including all procedures that have already occurred and those planned for the future.
- Authorization Decision: Present three clear options:
- Consent to continued participation and use of data already collected
- Consent only to use of data already collected with no future participation
- Refuse both continued participation and use of already collected data
- Data Management Plan: Pre-establish protocols for handling data if participants decline to provide retrospective consent, including statistical plans to address potential bias from missing data.
Validation and Quality Assessment Tools
Implementation of valid consent processes requires systematic quality assessment. Recent research has developed and validated specific instruments to evaluate the formal quality of informed consent documents [60]:
- Structured Checklists: Validated checklists for Patient Information Sheets (PIS) and Informed Consent Forms (ICF) containing specific items and sub-items aligned with regulatory requirements.
- Reliability Metrics: These instruments demonstrate very good inter-observer concordance (Kappa index ≥ 0.81, p < 0.001), providing reliable tools for ethics committees and sponsors [60].
- Comprehensive Evaluation: The checklist for Patient Information Sheets covers 5 sections, 16 items, and 46 sub-items, while the Informed Consent Form checklist contains 11 key items [60].
The Scientist's Toolkit: Essential Materials and Reagents
Table 3: Research Reagent Solutions for Consent Process Implementation
| Tool Category | Specific Instrument | Primary Function | Implementation Guidance |
|---|---|---|---|
| Regulatory Documents | 21 CFR 50.24 (FDA EFIC Rule) | Legal framework for exception from informed consent | Required for US-based emergency research; consult for compliance |
| Quality Assessment | Validated PIS/ICF Checklists | Evaluate formal quality of consent documents | Use for protocol development and ethics committee review [60] |
| Comprehension Verification | Teach-Back Method | Assess participant understanding of consent information | Ask participants to explain key concepts in their own words [27] |
| Remote Consent | eConsent Platforms | Facilitate consent process through digital means | Implement multimedia explanations; particularly useful for prospective consent [22] |
| Community Engagement | Community Consultation Framework | Facilitate two-way communication with potential communities | Develop tailored materials for different stakeholder groups [59] |
| Capacity Assessment | Decisional Capacity Evaluation | Determine patient's ability to provide informed consent | Use standardized assessment tools; document findings thoroughly |
| Ethical Oversight | IRB/EC Review Procedures | Ensure research complies with ethical standards | Engage early in protocol development; seek specific guidance on consent approach |
Adapting the informed consent process for emergency and critical care research requires a nuanced approach that balances ethical imperatives with practical realities. The updated SPIRIT 2025 statement emphasizes comprehensive protocol reporting, including clear descriptions of consent processes for vulnerable populations [34]. Future directions in this field should focus on:
- Hybrid Consent Models: Developing adaptive frameworks that apply different consent approaches based on specific study risks and patient circumstances [58].
- Technology Integration: Implementing eConsent platforms with multimedia capabilities to enhance understanding, particularly for prospective consent scenarios [22].
- Stakeholder Engagement: Increasing patient and public involvement in the design of consent processes for emergency research [34].
- Empirical Research: Conducting further studies to better understand the decisional burden experienced by surrogate decision-makers and to validate alternative consent models across diverse cultural and clinical contexts [58].
The continued refinement of ethical frameworks for emergency and critical care research ensures that critically ill patients receive appropriate access to potentially beneficial research while maintaining rigorous protections for autonomy, welfare, and rights.
Overcoming Language and Cultural Barriers to True Informed Consent
Informed consent serves as a cornerstone of ethical clinical research, rooted in the principles of respect for persons, beneficence, and justice. True informed consent represents more than a signature on a form; it constitutes an ongoing process that ensures research participants autonomously make decisions based on a comprehensive understanding of the research purpose, procedures, risks, benefits, and alternatives [61] [62]. Despite international guidelines mandating that consent information be delivered in a language understandable to the participant, significant barriers persist that compromise the quality and validity of this process, particularly for ethnic minority populations and those participating in global clinical trials [63] [64].
Language proficiency and cultural interpretation fundamentally affect participant comprehension. A systematic review and meta-analysis of informed consent understanding revealed that comprehension levels vary dramatically across different consent components, with particularly poor understanding of complex methodological concepts like randomization and placebo controls [61]. These challenges are exacerbated in global trial contexts where regulatory documents must navigate multiple official languages, regional dialects, and cultural interpretations of medical concepts [64]. This document outlines evidence-based protocols and application notes to help researchers overcome these barriers and achieve truly informed consent.
Quantitative Assessment of Current Understanding Gaps
Comprehensive analysis of participant understanding reveals significant gaps in informed consent comprehension. The following table synthesizes findings from systematic reviews and meta-analyses quantifying these understanding deficits across key consent components.
Table 1: Participant Understanding of Informed Consent Components
| Consent Component | Level of Understanding | Number of Studies/ Participants | Key Influencing Factors |
|---|---|---|---|
| Confidentiality | 75.8% [61] - 97.5% [65] | 100 studies [65] | Educational level, study location |
| Nature of Study | 74.7% [61] - 91.4% [65] | 135 cohorts [61] | Age, critical illness, study phase |
| Voluntary Participation | 74.7% [61] - 67.3% [65] | 135 cohorts [61] | Cultural context, trust in healthcare system |
| Potential Benefits | 74.0% [61] | 135 cohorts [61] | Therapeutic misconception |
| Study Purpose | 69.6% [61] | 135 cohorts [61] | Educational level, language proficiency |
| Potential Risks & Side-Effects | 67.0% [61] | 100 studies [65] | Complexity of information, health literacy |
| Ability to Name One Risk | 54.9% [61] | 135 cohorts [61] | Interview method, timing of assessment |
| Alternative Treatment if Withdrawn | 64.1% [61] | 135 cohorts [61] | Clarity of explanation, document length |
| Randomization | 52.1% [61] - 39.4% [65] | 135 cohorts [61] | Methodological complexity, educational level |
| Placebo Concept | 53.3% [61] - 4.8% [65] | 135 cohorts [61] | Cultural perceptions, linguistic equivalence |
Experimental Protocols for Assessing and Improving Understanding
Protocol 1: Multilingual Consent Process with Comprehension Verification
Application Note: This protocol implements a sequential approach to consent that combines accurate translation with active comprehension verification, moving beyond simple document translation.
Materials & Reagents:
- Certified Translation Memory (TM): An archive of preferred clinical trial terminology and accepted medical terms in the target language [64].
- Back-Translation Protocol: A systematic process for independent reverse translation to verify meaning preservation [64] [66].
- Teach-Back Assessment Tool: A structured questionnaire or interview guide to assess participant understanding after consent discussions [6] [67].
- Audio-Visual Aids: Culturally adapted multimedia materials explaining complex concepts in the participant's native language [63] [66].
Methodology:
- Transcreation of Materials: Adapt informed consent documents and materials through transcreation that considers both language and cultural context of the target population. Replace culturally specific metaphors and examples with locally relevant equivalents [63] [64].
- Back-Translation Verification: Execute formal translation and back-translation process using independent, qualified translators fluent in both source and target languages. Resolve discrepancies through expert consensus [64] [66].
- Structured Consent Discussion: Conduct the consent discussion using trained bilingual staff or certified medical interpreters. Ensure the interpreter receives training in medical terminology and quality healthcare interpretation [63] [62].
- Comprehension Assessment: Implement a structured teach-back method where participants explain key concepts in their own words. Focus assessment on higher-risk concepts with traditionally lower understanding (randomization, placebo, risks) [6] [67].
- Iterative Clarification: Provide additional explanation for misunderstood concepts and re-assess understanding until all critical components are comprehended. Document the process and number of clarification cycles required [6].
Protocol 2: Community-Engaged Consent for Oral Cultures
Application Note: This protocol addresses challenges in regions with predominantly oral traditions and low literacy rates, such as West Africa, where written documents have limited utility [66].
Materials & Reagents:
- Audio-Recorded ICF: Informed consent form recordings in the participant's primary language using culturally appropriate narration [66].
- Community Engagement Framework: A structured approach for collaborating with community leaders and cultural brokers to ensure cultural appropriateness [68] [66].
- Impartial Witness Protocol: Guidelines for engaging independent witnesses to verify that oral presentations accurately reflect written documents [62] [66].
- Visual Aids: Culturally representative diagrams, pictures, and 3D objects to explain medical procedures and concepts [62] [67].
Methodology:
- Community Partnership: Engage community leaders and cultural experts early in the consent development process to review materials for cultural appropriateness and comprehension [68] [66].
- Audio Documentation: Develop and ethics committee-approved audio recording of the entire informed consent form in the local language. Submit both written and audio formats for approval [66].
- Group Briefing Sessions: Conduct initial consent discussions in group settings in the local language, creating an environment where participants feel comfortable asking questions and expressing concerns [66].
- Individual Verification Sessions: Follow group sessions with private meetings where participants can ask questions confidentially. Assess individual understanding through open-ended questioning [66].
- Witness-Verified Consent: For illiterate participants, employ an impartial witness fluent in both languages to verify that oral information aligns with written documents. Ensure the witness is unrelated to the research subject and remains independent from the research team [62] [66].
Technological Solutions and Regulatory Framework
Digital and Multimedia Approaches
Technology offers promising solutions for enhancing understanding across language and cultural barriers. The FDA has endorsed electronic informed consent (eConsent) systems that incorporate multimedia elements, video explanations, and interactive comprehension checks [62]. Research demonstrates that audio-visual interventions in a participant's preferred language can increase knowledge of clinical trials and positive intention to participate [63]. TrialX's Diversity, Equity, and Inclusion (DEI) Toolkit provides an example of an end-to-end multilingual solution that creates study websites, pre-screeners, and patient notifications in multiple languages [63]. These systems can be particularly valuable for explaining complex medical devices through animations and interactive diagrams [67].
Regulatory Considerations and Best Practices
Recent FDA guidance (2023) clarifies that Institutional Review Boards (IRBs) do not need to review and approve every translated version of consent forms but should establish reasonable procedures for ensuring quality translation and interpretation assistance [62]. The guidance emphasizes:
- Using qualified translators rather than relying on family members (especially children) for interpretation [62].
- Incorporating pictures, diagrams, videos, and other visual aids to enhance understanding [62].
- Providing reasonable modifications and auxiliary aids to meet the specific needs of study populations [62].
- Ensuring that individuals obtaining consent are knowledgeable, well-trained, and preferably healthcare professionals who can adequately address medical questions [62].
Table 2: Comparison of Solution Effectiveness for Barriers
| Solution Approach | Best For | Key Advantages | Implementation Challenges |
|---|---|---|---|
| Bilingual Staff | High-prevalence language groups in study region | Direct communication, builds rapport | Resource intensive, limited scalability |
| Certified Medical Interpreters | Low-prevalence language groups | Medical terminology accuracy, quality assurance | Cost, availability for rare languages |
| Transcreated Audio-Visual Materials | Low literacy populations, standardized messaging | Consistency, cultural adaptation | Upfront development cost, technology access |
| Technology Platforms (eConsent) | Multicenter trials, diverse populations | Scalability, built-in comprehension checks | Digital literacy requirements, regulatory approval |
| Community-Engaged Approach | Oral cultures, indigenous populations | Cultural legitimacy, trust building | Time intensive, requires deep community relationship |
Integrated Workflow for Comprehensive Informed Consent
The following diagram illustrates a comprehensive workflow for obtaining informed consent that integrates multiple strategies to overcome language and cultural barriers:
Table 3: Essential Resources for Implementing Enhanced Consent Protocols
| Tool/Resource | Function | Application Notes |
|---|---|---|
| Translation Memory (TM) | Maintains consistency in translated terminology across documents and studies | Create study-specific glossaries; essential for multicenter trials [64] |
| Back-Translation Protocol | Validates accuracy and completeness of translated materials | Requires independent translators not involved in initial translation [64] [66] |
| Cultural Adaptation Framework | Guides modification of content to ensure cultural relevance | Involves replacing examples, metaphors, and images with culturally appropriate equivalents [63] [64] |
| Teach-Back Assessment Guide | Standardizes measurement of participant understanding | Should focus on concepts with historically low comprehension rates [6] [67] |
| Audio Recording Equipment | Creates verifiable audio versions of consent forms | Essential for oral cultures and low-literacy populations [66] |
| Multimedia Development Tools | Produces explanatory videos, animations, and visual aids | Particularly valuable for complex medical device trials [63] [67] |
| Community Advisory Board | Provides cultural guidance and builds community trust | Should be established early in protocol development [68] [66] |
Overcoming language and cultural barriers to achieve true informed consent requires a multifaceted approach that moves beyond simple translation to embrace cultural adaptation, community engagement, and technological innovation. The protocols and frameworks presented here provide researchers with evidence-based methodologies to enhance participant understanding, particularly for complex concepts like randomization and placebo controls. By implementing these strategies, researchers can fulfill the ethical imperative of true informed consent while simultaneously improving trial participation and diversity, ultimately leading to more generalizable research findings and advancing health equity.
Obtaining valid informed consent is a cornerstone of ethical clinical research. True comprehension of trial information by participants is fundamental to this process. This document provides detailed application notes and protocols for integrating health literacy assessment and usability testing into the informed consent workflow to optimize participant understanding. The guidance is framed within the broader thesis that valid consent is not merely a signed form but a process of genuine comprehension, which can be compromised by complex materials and navigational barriers [2] [22]. Researchers have an obligation to ensure information is not only provided but also understood by participants, a principle central to ethical codes and regulations for human subject research [2]. These protocols are designed to assist researchers, scientists, and drug development professionals in systematically enhancing consent materials and processes.
Health Literacy Assessment Tools
Health literacy is an individual's capacity to obtain, process, and understand basic health information needed to make appropriate health decisions. Assessing the health literacy of a target population is a critical first step in developing comprehensible consent materials. The following table summarizes key validated tools for this purpose.
Table 1: Health Literacy Assessment Tools for Clinical Research
| Tool Name | Description | Administration Time | Key Features | Primary Use Case |
|---|---|---|---|---|
| The Newest Vital Sign (NVS) [69] | A bilingual (English/Spanish) screening tool that uses a nutrition label to assess literacy and numeracy. | ~3 minutes | Identifies patients at risk for low health literacy; Easy to administer in clinical settings. | Quick screening in busy research settings to identify participants who may need additional support. |
| REALM-SF (Rapid Estimate of Adult Literacy in Medicine, Short Form) [69] | A 7-item word recognition test that measures ability to pronounce common medical terms. | ~2 minutes | Provides a quick assessment of health literacy; Excellent agreement with the full 66-item REALM. | Rapidly assigning a grade-level estimate to a patient's health literacy in diverse research settings. |
| Health Literacy Tool Shed [69] | An online database of health literacy measures, including their psychometric properties. | N/A | A resource for researchers to compare and select the most appropriate measurement instrument based on peer-reviewed literature. | Identifying and selecting a validated health literacy instrument tailored to a specific study's needs and population. |
Protocol for Integrating Health Literacy Assessment
Objective: To identify potential participants who may struggle with standard consent materials and to adapt communication strategies accordingly.
Materials: Chosen health literacy assessment tool (e.g., NVS), private room, information sheet explaining the purpose of the assessment.
Procedure:
- Pre-Screening Consideration: Determine the appropriateness of pre-consent health literacy screening based on the study's target population and IRB guidance. Waiver of consent for the screening itself may be required.
- Administration: A trained member of the research team administers the chosen tool in a private, comfortable setting.
- Interpretation: Score the assessment according to the tool's guidelines. For example, with the NVS, a score of 0-1 suggests high likelihood of limited literacy, while a score of 2-3 indicates the possibility of limited literacy [69].
- Adaptation: Based on the results:
- For participants with limited health literacy, employ enhanced communication techniques: teach-back method, simplified language, and visual aids.
- Use the findings to refine the informed consent form and process for future participants, ensuring materials are understandable by individuals with low health literacy.
Usability Testing for Consent Processes and Platforms
Usability testing evaluates how easily users can interact with a system, whether it is a paper-based form, an eConsent platform, or a clinical trial search engine. Research indicates that users with low health literacy have significant difficulty forming queries and navigating standard web-based clinical trial search tools [70]. The following protocol outlines a method for testing the usability of these critical interfaces.
Protocol for Usability Testing of Consent Tools
Objective: To identify navigational and comprehension barriers within informed consent materials and digital platforms.
Materials: Prototype of the consent material or digital platform (e.g., eConsent system, trial search engine), quiet testing environment, audio/video recording equipment, pre- and post-test questionnaires, task list.
Procedure:
- Participant Recruitment: Recruit 5-8 participants representing a spectrum of health and computer literacy levels, reflecting the intended study population [70]. Ensure diversity in age, education, and technological proficiency.
- Pre-Test Questionnaire: Administer a brief questionnaire to gather demographic data and baseline computer/health literacy.
- Task-Based Testing: Provide participants with a list of key tasks while using a "think-aloud" protocol. Tasks for an eConsent platform may include:
- "Find the section that describes the potential risks of this study."
- "Use the glossary to look up the term 'randomization'."
- "Navigate to the page where you can ask the researcher a question."
- "Locate the information about withdrawing from the study at any time."
- Data Collection: Record success/failure rates for each task, time-on-task, participant's verbal feedback, and any observed frustrations or confusion.
- Post-Test Interview: Conduct a semi-structured interview to gather subjective feedback on the clarity, ease of use, and overall experience. Ask participants to rate the difficulty of tasks and provide suggestions for improvement.
- Data Analysis: Thematically analyze qualitative feedback and quantify task performance metrics. Prioritize identified issues based on frequency and severity.
Diagram: Usability Testing and Iterative Design Workflow
The Scientist's Toolkit: Research Reagent Solutions
This section details essential tools and materials for implementing the protocols described in this document.
Table 2: Essential Reagents for Health Literacy and Usability Research
| Item | Function/Brief Explanation |
|---|---|
| Validated Health Literacy Screeners (e.g., NVS, REALM-SF) | Tools to objectively assess a participant's ability to understand health information, allowing for tailored communication [69]. |
| Readability & Suitability Assessment Tools (e.g., CDC Clear Communication Index, PEMAT, SAM) | Instruments to evaluate the clarity, understandability, and actionability of written patient education and consent materials [69]. |
| Audio/Video Recording Equipment | For capturing complete data during usability testing sessions, including participant actions, verbal feedback, and non-verbal cues. |
| eConsent or Digital Platform Prototype | An interactive version of the digital consent tool or search engine used for testing navigation, design, and information architecture before full deployment [22]. |
| Task List Script | A standardized set of instructions and scenarios given to participants during usability testing to evaluate the effectiveness and efficiency of the tool. |
Integration with the Informed Consent Process
The ultimate goal of these assessments and tests is to integrate their findings into a more robust and ethical informed consent process. The diagram below illustrates how health literacy and usability principles are embedded throughout this process.
Diagram: Informed Consent Process Optimized for Comprehension
The optimized process emphasizes:
- Pre-emptive Optimization: Using health literacy data and usability findings to design materials and platforms before they are used with participants [69] [70].
- Information Disclosure: Providing all relevant information about the trial in an accessible manner, using simplified language, visual aids, and multimedia components as seen in eConsent solutions [22].
- Assessment of Understanding: Actively verifying comprehension through techniques like the teach-back method, where participants explain the information in their own words [22]. This addresses the ethical requirement that researchers ensure information is understood, not just disclosed [2].
- Voluntariness and Ongoing Process: Confirming that consent is given freely and reinforcing that participants can withdraw at any time. The process continues throughout the trial, requiring re-consent if new significant information emerges or at regular intervals in long-term studies [2] [22].
By adopting these application notes and protocols, researchers can move beyond a procedural view of informed consent and toward a process that genuinely respects participant autonomy through demonstrable comprehension.
Addressing Common Participant Questions and Misconceptions
Within the framework of obtaining valid informed consent in clinical trials, addressing participant questions and misconceptions is not merely an administrative task but a fundamental ethical imperative. Informed consent serves as a cornerstone of patient autonomy and a critical safeguard in clinical research, governed by principles outlined in the Belmont Report—respect, beneficence, and justice [71]. Misconceptions can severely undermine the validity of consent, exposing participants to unforeseen risks and compromising data integrity. This document provides detailed application notes and protocols to assist researchers, scientists, and drug development professionals in proactively identifying and clarifying common participant uncertainties, thereby ensuring a robust, ethical, and compliant informed consent process.
Application Notes: Participant Concerns and Evidence-Based Clarifications
Effective communication requires anticipating and resolving common participant questions. The following table synthesizes frequent misconceptions and provides evidence-based guidance for researcher responses, drawing from FDA guidance and established ethical codes [72] [71].
Table 1: Common Participant Questions and Evidence-Based Clarifications
| Participant Question/Misconception | Underlying Concern | Recommended Clarification & Researcher Talking Points | Regulatory & Ethical Basis |
|---|---|---|---|
| "Does my signing mean I am guaranteed to get better?" (Therapeutic Misconception) | Confusion between the goals of clinical research (generating knowledge) and individualized therapeutic care. | Clearly state: "The primary purpose of this research is to gather scientific knowledge that may help future patients, not to provide direct therapeutic benefit to you. The treatment may not, and in some cases, will not, benefit you personally." Emphasize standard treatment alternatives [72]. | FDA ICF Guidance: Must clarify that participation is primarily for contributing to research, not for individual treatment [72]. Helsinki Declaration: The well-being of the human subject should take precedence over the interests of science and society [71]. |
| "What happens if I get sick or injured because of the trial?" | Fear of being left with medical and financial burdens from a research-related injury. | Provide a direct, unambiguous statement. Example: "The sponsor will cover the cost of medical treatment for any injury directly caused by the study drug or procedures. This does not constitute a waiver of your legal rights. For full details, please refer to section [X] of the consent form." | ICH-GCP: Sponsors must provide insurance or compensate for trial-related injury [33]. FDA ICF Guidance: Requires a statement on compensation and treatment for injuries beyond minimal risk [72]. |
| "Can I leave the study if I change my mind?" | Fear of being locked in and facing penalties or loss of rights. | Reassure the participant: "Your participation is entirely voluntary. You can withdraw from the study at any time, for any reason, without any penalty or loss of benefits to which you are otherwise entitled." Explain what data may be retained post-withdrawal [72] [73]. | FDA ICF Guidance: Must explicitly state that participation is voluntary and that refusal or withdrawal will not incur penalty or loss of benefits [72]. |
| "Will my personal information be kept private?" | Concerns about confidentiality and who will access sensitive health data. | Explain: "Your personal health information will be collected and stored securely. It will be accessible to the research team, the sponsor, the Institutional Review Board (IRB), and regulatory agencies like the FDA to verify the data. Your name will not be used in any public reports from this study." | FDA ICF Guidance: Must describe confidentiality and the parties who may access records, including the FDA [72]. |
| "If I agree now, do I have to keep participating forever?" | Misunderstanding that consent is a one-time, binding event. | Clarify: "Informed consent is a continuing process. We will inform you of any new, relevant information that emerges during the study that might affect your willingness to participate. You may be asked to re-sign a consent form if there are significant changes, and you can always ask questions at any time." | FDA ICF Guidance: Consent is an ongoing process, not just a form signature [72]. Significant new findings must be provided to subjects [72]. |
Experimental Protocols: Methodologies for Valid Consent
Protocol: Comprehensive Pre-Consent Preparation
A valid consent process begins long before a participant encounters the consent form.
ICF Design and Review:
- Plain Language Writing: Draft the Informed Consent Form (ICF) at an 8th-grade reading level or lower. Avoid complex medical jargon; use "high blood pressure" instead of "hypertension." If technical terms are unavoidable, include simple explanations [71].
- Content Validation: Ensure the ICF includes all eight basic elements required by 21 CFR 50.25(a), such as a description of the research, risks, benefits, alternatives, and confidentiality [72]. For Applicable Clinical Trials, include the mandatory statement about trial registration on ClinicalTrials.gov [72].
- Regulatory Approval: Submit the final ICF draft to the Independent Ethics Committee (IEC)/Institutional Review Board (IRB) for review and approval. Use only the IRB-approved, most current version of the ICF [74] [73].
Researcher Training and Delegation:
- Formal Training: All study team members involved in the consent process must undergo documented training on the protocol, the ICF, GCP principles, and effective communication techniques with diverse populations.
- Delegation of Authority: The Principal Investigator (PI) must formally delegate the task of obtaining informed consent to qualified, trained personnel using a Delegation of Authority Log. The PI retains ultimate responsibility for the process [33].
Protocol: Executing the Initial Consent Interaction
This protocol details the structured interaction for obtaining initial consent.
Environment and Setting:
- Conduct the discussion in a private, quiet, and comfortable setting that encourages relaxation and open dialogue. Avoid conducting the process in noisy hallways or busy clinic rooms [74].
- Allocate sufficient, uninterrupted time for the discussion, typically 30-60 minutes, depending on the study's complexity.
Structured Information Disclosure:
- Use the IRB-approved ICF as a guide, but deliver the information in a conversational manner.
- Systematically cover all key aspects of the study: purpose, duration, procedures, experimental and standard-of-care interventions, and the voluntary nature of participation.
- Discuss Risks and Benefits Objectively: Present all reasonably foreseeable risks and discomforts, their likelihood, and any mitigating measures. Describe any direct benefits to the participant and/or societal benefits. Avoid overly optimistic language [72].
- Disclose Alternatives: Explain the alternatives to participation, such as standard available treatments or supportive care [72].
Assessment of Understanding and Question Handling:
- Employ the "teach-back" method: Ask the participant to explain the study's purpose, key procedures, main risks, and the fact that participation is voluntary in their own words. This assesses comprehension more effectively than simply asking "Do you understand?" [71].
- Encourage and patiently answer all questions. The researcher's responses must be consistent with the protocol and ICF content. Any question asked and its answer should be documented in the source documents [74].
Documentation of Consent:
- Once the participant has no further questions and provides agreement, proceed with signing the ICF.
- Signatures: The participant (or their legally authorized representative) and the researcher who conducted the consent discussion must sign and date the ICF [73].
- Copy Provision: Immediately provide a signed copy of the ICF to the participant and retain the original in the study records [74].
- Source Documentation: The consent process must be documented in the participant's medical or research record, noting the date, time, version of the ICF used, and the fact that a copy was provided [74].
Protocol: Managing Ongoing Consent and Special Populations
Table 2: Protocols for Special Consent Scenarios
| Scenario | Protocol Requirements & Workflow | Key Considerations |
|---|---|---|
| Ongoing Consent Process | 1. Provide Updates: Inform participants of any significant new findings (e.g., new risks identified) that may affect their willingness to continue [72].2. Re-consent: If the study protocol or risks change significantly, obtain a new ICF using the latest IRB-approved version [73].3. Re-affirm Willingness: At key study visits, briefly confirm the participant's continued willingness to participate. | Consent is not a single event. Maintaining an open channel of communication builds trust and ensures continued validity. |
| Participants with Limited Literacy | 1. Oral Presentation: Read the entire ICF aloud to the participant [71].2. Use of a Witness: Engage an impartial, literate witness to observe the entire consent process. The witness attests that the information was accurately explained and that consent was freely given, and signs the ICF [73]. | The witness must be independent of the research team. The use of multimedia (e.g., eConsent platforms with audio/video) can be highly effective [75]. |
| Pediatric Participants | 1. Parental Permission: Obtain written informed consent from the child's parent or legal guardian [73].2. Child Assent: Seek the willing agreement ("assent") from the child, appropriate to their age and maturity. For children aged 8-18, this should be a signed assent form. For younger children, a verbal agreement is sufficient [73].3. Respect Dissent: If a child objects to participation, their decision should typically be respected, even if the parent has given permission [73]. | The language and process must be adapted to the child's developmental level. |
| Adults Unable to Consent | 1. Legally Authorized Representative (LAR): Identify the individual legally empowered to provide consent on behalf of the subject (varies by jurisdiction) and obtain their informed consent [71].2. Witness Requirements: Follow procedures for witnesses as needed.3. Assent from Subject: If the subject has some understanding, their assent should still be sought where possible. | The definition of an LAR is specific to national and local laws. Researchers must know the applicable regulations [71]. |
Visualizing the Consent Process and Materials Toolkit
The following diagram illustrates the logical workflow and decision points in a comprehensive informed consent process, integrating the key protocols outlined above.
Diagram: Workflow for a Valid Informed Consent Process
The Scientist's Toolkit: Essential Materials for Consent Research
Table 3: Essential Reagents and Solutions for Informed Consent Research
| Tool / Material | Function / Purpose in Consent Research |
|---|---|
| IRB-Approved Informed Consent Form (ICF) | The foundational document ensuring regulatory compliance (e.g., with 21 CFR 50.25) and serving as the primary guide for the consent discussion. It must include all basic and applicable additional elements [72]. |
| Plain Language Guide & Readability Assessment Tool | Tools (e.g., Flesch-Kincaid) used to evaluate and ensure the ICF is written at an appropriate comprehension level (e.g., ≤8th grade) to facilitate participant understanding [71]. |
| Electronic Consent (eConsent) Platform | Technology solutions (e.g., Medidata Consent) that use multimedia (text, audio, video) to present information in a more engaging and understandable way, potentially improving comprehension and streamlining documentation [75]. |
| Specialized ICF Translation Solution | Professional tools and services (e.g., X-doc.ai) that ensure accurate, culturally adapted, and compliant translation of ICFs for multi-regional clinical trials, maintaining medical and legal precision [76]. |
| Delegation of Authority Log | A critical trial master file document that formally records which study team members are authorized by the Principal Investigator to conduct the informed consent process [33]. |
| Source Documentation Template | Standardized forms (within the Electronic Health Record or on paper) for consistently recording the details of every consent interaction, including date, time, attendees, questions asked, and answers given [74]. |
Ensuring Regulatory Adherence and Process Integrity
The Role of IRBs/Ethics Committees in Reviewing and Approving Consent
An Institutional Review Board (IRB) is an appropriately constituted group formally designated to review and monitor biomedical research involving human subjects [77]. The fundamental purpose of IRB review of informed consent is to assure that the rights and welfare of subjects are protected, while also ensuring the institution has complied with applicable regulations [77]. This review serves as a critical safeguard in clinical research, ensuring that individuals voluntarily participate only after demonstrating adequate understanding of the research purposes, procedures, risks, and benefits.
IRBs use a group process to review research protocols and related materials, including informed consent documents and investigator brochures [77]. This collaborative review helps ensure that the informed consent process meets both ethical standards and regulatory requirements before research begins and through periodic monitoring during the study's progression.
Ethical Foundations and Regulatory Framework
Core Ethical Principles
The National Institutes of Health (NIH) outlines seven main principles to guide ethical research, with informed consent representing a central pillar [78]. According to these principles, potential participants should make their own autonomous decisions about whether to participate or continue participating in research through a robust process of informed consent [78]. This requires that individuals (1) are accurately informed of the purpose, methods, risks, benefits, and alternatives to the research; (2) understand this information and how it relates to their own clinical situation or interests; and (3) make a voluntary decision without coercion or undue influence.
Regulatory Authorities and Requirements
Multiple regulatory frameworks govern IRB operations and informed consent processes:
- FDA Regulations: Apply to research involving products regulated by the FDA (21 CFR Parts 50 and 56) regardless of federal funding [77]
- HHS Regulations (45 CFR Part 46): Apply to research conducted or supported by HHS [77]
- Single IRB Policy: For NIH-funded multi-site studies, a single IRB must provide ethical review [79]
IRBs must register with the federal government if they review FDA-regulated studies, with registration information maintained in an Internet-based system by HHS [77]. While FDA regulations do not require an "assurance" document, institutions conducting HHS-supported research must provide written assurance of compliance with HHS protection of human subjects regulations [77].
Table: Key Regulatory Bodies Governing IRB Operations
| Agency | Jurisdiction | Key Requirements |
|---|---|---|
| FDA | Research involving FDA-regulated products (drugs, devices, biologics) | IRB registration required; compliance with 21 CFR Parts 50 & 56 [77] |
| HHS/OHRP | HHS-conducted or supported research | Federalwide Assurance; compliance with 45 CFR Part 46 [77] |
| NIH | NIH-funded research | Single IRB review for multi-site studies [79] |
IRB Composition and Organizational Structure
Membership Requirements
FDA regulations mandate that IRBs maintain diverse membership to provide comprehensive review of research protocols [77]. The membership requirements include:
- Scientific Members: At least one member with primary concerns in scientific areas (typically physicians or PhD-level scientists) [77]
- Non-Scientific Members: At least one member with primary concerns in non-scientific areas [77]
- Unaffiliated Members: At least one member not otherwise affiliated with the institution [77]
- Diverse Backgrounds: Members with varying backgrounds and representative capacities to promote complete review of research activities
IRBs should strive for membership that represents diverse disciplines and perspectives, though one individual may satisfy more than one membership category [77]. When research involves specialized scientific areas beyond the expertise of members, IRBs may use consultants to assist in review [77].
Management of Conflicts of Interest
The FDA regulations explicitly address conflicts of interest within IRB membership [77]. While clinical investigators may serve as IRB members, the regulations prohibit any member from participating in the IRB's initial or continuing review of any study in which the member has a conflicting interest, except to provide information requested by the IRB [77]. This safeguard ensures that reviews remain objective and focused on subject protection rather than institutional, professional, or financial interests.
The Consent Review Process: Procedures and Criteria
Elements of Valid Informed Consent
IRBs evaluate consent documents against established regulatory criteria to ensure all required elements are present and adequately described. The following table summarizes the core components IRBs assess during document review.
Table: Essential Elements of Informed Consent Documents
| Element Category | Specific Requirements | IRB Assessment Criteria |
|---|---|---|
| Study Description | Purpose, duration, procedures, experimental interventions | Clear explanation of research nature; identification of experimental procedures [78] |
| Risks & Discomforts | Physical, psychological, social, economic risks | Comprehensive listing; reasonable risk minimization strategies [78] |
| Benefits | Direct and societal benefits | Realistic description; distinction from standard care [78] |
| Alternatives | Standard treatments or procedures | Viable clinical alternatives to research participation [78] |
| Confidentiality | Privacy protections, data handling, information security | Adequate safeguards for personal data; disclosure of limits to confidentiality [78] [80] |
| Compensation | Arrangements for research-related injuries | Clear statement about compensation availability or absence; no waiver of rights [77] |
| Voluntary Participation | Right to refuse or withdraw without penalty | Explicit statements affirming voluntary participation [78] |
| Contact Information | Research team and IRB contact details | Appropriate contacts for questions, rights concerns, and research-related injuries [78] |
IRB Workflow for Consent Review
The following diagram illustrates the comprehensive workflow IRBs follow when reviewing and approving informed consent documents and processes:
Types of IRB Review
IRBs employ different review procedures based on the risk level presented by the research:
- Full Committee Review: Required for research presenting more than minimal risk to human subjects, involving discussion and consensus decision by the convened IRB [81]
- Expedited Review: For research procedures presenting no more than minimal harm to participants, conducted by designated IRB members without full committee convening [81]
- Continuing Review: Periodic reassessment of previously approved research at intervals appropriate to the degree of risk, but not less than once per year [81]
The expedited review process typically completes within 10 working days, while full committee review occurs at regularly scheduled meetings, usually monthly [81]. The length of time for final approval depends on the promptness of investigator responses to IRB concerns [81].
Special Considerations in Consent Review
Vulnerability and Fair Subject Selection
The NIH guiding principles emphasize fair subject selection, stating that "the primary basis for recruiting participants should be the scientific goals of the study — not vulnerability, privilege, or other unrelated factors" [78]. IRBs must pay special attention to protocols involving potentially vulnerable populations who may have diminished autonomy or increased susceptibility to coercion. Specific groups (e.g., women, children, prisoners, cognitively impaired individuals) should not be excluded from research opportunities without a good scientific reason or particular susceptibility to risk [78].
Compensation and Injury Policies
IRB review must ensure that institutional policies regarding compensation for research-related injuries are clearly communicated in consent documents [77]. According to FDA regulations, for research involving more than minimal risk, the subject must be told whether any compensation and medical treatments are available if injury occurs, and if so, what they consist of, or where further information may be obtained [77]. Any statement that compensation is not offered must avoid waiving or appearing to waive any of the subject's rights [77].
Data Privacy and Confidentiality
With increasing emphasis on data protection, IRBs must evaluate protocols for adequate privacy safeguards [80]. This includes ensuring datasets minimize exposure of personally identifiable information unless informed consent is provided, implementing secure data storage practices, and using anonymization protocols to reduce risk of data leakage [80]. For AI and machine learning research, additional considerations include copyright compliance, dataset representativeness, and appropriate data licensing [80].
Research Reagent Solutions: Essential Materials for Consent Research
Table: Key Research Tools for Validating Consent Processes
| Research Tool | Function/Purpose | Application in Consent Research |
|---|---|---|
| Validated Comprehension Assessments | Quantitative measurement of participant understanding | Objectively evaluates consent comprehension; identifies problematic consent elements [78] |
| Readability Analytics Software | Analyzes reading level and complexity of documents | Ensures consent forms match target population literacy levels [78] |
| Digital Consent Platforms | Electronic consent presentation and documentation | Facilitates multimedia consent; enables interactive comprehension checks [80] |
| IRB Submission Management Systems | Streamlines protocol submission and tracking | Manages consent document version control; documents review decisions [81] |
| Participant Survey Instruments | Collects feedback on consent experience | Assesses perceived coercion, understanding, and satisfaction with consent process [78] |
Experimental Protocol: Assessing Consent Comprehension
Objective
To quantitatively evaluate participant understanding of key informed consent elements following the consent discussion and document review, identifying areas where comprehension fails and interventions are needed.
Materials
- Final IRB-approved informed consent document
- Validated comprehension assessment tool tailored to specific study
- Digital or paper-based data collection instrument
- Environment ensuring participant privacy and confidentiality
Methodology
- Participant Recruitment: Recruit representative sample from target population (N=30-50)
- Standardized Consent Process: Conduct consent discussion using IRB-approved document
- Comprehension Assessment: Administer validated comprehension tool immediately after consent discussion
- Data Analysis: Calculate comprehension scores for each consent element and overall
- Qualitative Feedback: Collect participant feedback on confusing or unclear consent elements
- Iterative Refinement: Modify consent materials based on findings and re-test if necessary
Outcome Measures
- Percentage of participants understanding key risk elements
- Identification of consistently misunderstood concepts
- Time required for adequate comprehension
- Correlation between demographic factors and comprehension levels
Emerging Challenges and Future Directions
Oversight Gaps and IRB Effectiveness
Recent Government Accountability Office (GAO) reports identify significant challenges in IRB oversight, noting that federal agencies inspect relatively few IRBs annually [82]. OHRP aims to conduct only three to four routine inspections annually, while FDA conducts an average of 133 inspections annually [82]. Neither agency has conducted a risk-based assessment of their IRB inspection programs to determine if they are inspecting adequate numbers of IRBs to protect human subjects [82]. Additionally, OHRP and FDA have not assessed to what extent IRB reviews are effective in protecting human subjects because they have not determined the best approaches for evaluation [82].
Evolving Ethical Standards
Ethical frameworks continue to evolve with technological advancements. The updated SPIRIT 2025 statement emphasizes enhanced protocol transparency, including open science practices and greater patient involvement in trial design [34]. Similarly, conferences like NeurIPS and ICML have established detailed ethics guidelines addressing algorithmic fairness, privacy protection, and responsible research practices that extend beyond traditional biomedical concerns [80] [83]. These developments indicate a broadening scope of ethical considerations that IRBs must incorporate into their review processes.
The following diagram illustrates the ethical assessment framework IRBs should apply when reviewing consent processes and research protocols:
IRBs play an indispensable role in protecting human research subjects through comprehensive review of informed consent processes and documents. This responsibility requires careful evaluation of both the ethical foundations and practical implementation of consent, ensuring participants make truly informed and voluntary decisions. As research methodologies evolve and new ethical challenges emerge, IRBs must adapt their review processes while maintaining focus on the core principles of respect for persons, beneficence, and justice. By employing structured approaches to consent review, maintaining diverse expertise in membership, and implementing robust oversight mechanisms, IRBs fulfill their critical function in upholding the integrity of human subjects research and preserving public trust in the research enterprise.
Within the broader thesis of obtaining valid informed consent in clinical trials, the audit function serves as a critical verification mechanism. It ensures that the ethical and regulatory principles of respect for persons, beneficence, and justice are operationalized in practice. An effective audit moves beyond document review to assess the entire consent ecosystem, evaluating whether the process truly supports a participant's autonomous decision-making [24] [46]. This application note provides a structured framework and specific metrics for auditing the informed consent process to ensure both regulatory compliance and high-quality, ethical participant engagement.
Key Compliance Metrics
Auditing for compliance verifies adherence to regulations such as Good Clinical Practice (GCP) and 21 CFR Part 50. The following table summarizes essential quantitative compliance metrics and their data sources.
Table 1: Key Compliance Metrics for Auditing the Informed Consent Process
| Metric Category | Specific Metric | Data Source | Target/Benchmark |
|---|---|---|---|
| Documentation Integrity | % of consent forms using the correct, IRB-approved version | Regulatory Binder, eConsent system logs | 100% [46] |
| % of consent forms with complete signatures, dates, and initials | Subject Source Documents | 100% [84] | |
| Process Adherence | % of participants consented prior to any trial-related procedures | Subject Source Documents, Study Logs | 100% [84] |
| % of required re-consents completed following protocol amendments | Consent Tracker, Regulatory Binder | 100% [46] | |
| Regulatory Oversight | Evidence of timely IRB submission and approval for all consent documents | IRB Correspondence File | 100% [84] |
| % of audit findings related to consent closed per CAPA timeline | Quality Management System (QMS) | >95% [85] |
Experimental Protocol: Compliance Document Review
Objective: To systematically verify the completeness, accuracy, and proper versioning of Informed Consent Forms (ICFs) for all study participants.
Materials:
- IRB Approval Records: Master list of all approved ICF versions with dates.
- Subject Identification Log: De-identified list of all enrolled participants.
- Source Documents: The complete, signed ICF for each participant.
- Regulatory Binder: Site file containing protocol, IRB communications, and essential documents.
- Electronic Consent (eConsent) System Audit Trail: (If applicable) Digital log of consenting activities.
Methodology:
- Create a Master ICF Log: Generate a log listing every enrolled participant. For each, record the ICF version and date stipulated in the protocol and IRB approval records as the correct version for their enrollment period.
- Verify ICF Version for Each Participant: For each participant, retrieve their signed ICF from the source documents. Compare the version number and date on the signed form against the "correct" version in your master log. Record any discrepancies.
- Check Execution Completeness: Examine each signed ICF to ensure the participant (and legally authorized representative, if applicable) has signed and dated the form. Verify that any required witness signatures are present and that all pages have been initialed as per IRB and protocol requirements.
- Confirm Consent Timing: Cross-reference the date and time of the participant's signature on the ICF with the date of the first protocol-mandated procedure (e.g., first dose of investigational product, first screening lab). The consent must be documented prior to any trial-related procedures.
- Review Amendment Implementation: Identify all protocol amendments that required a revised ICF. For each, determine the cohort of participants who required re-consent. Verify via the source documents and consent tracker that the re-consent was performed with the updated ICF before continuing participants in the amended study.
Key Quality Metrics
While compliance is foundational, a high-quality consent process ensures genuine participant understanding and engagement. The following table outlines metrics for assessing quality.
Table 2: Key Quality Metrics for Auditing the Informed Consent Process
| Metric Category | Specific Metric | Data Source | Target/Benchmark |
|---|---|---|---|
| Participant Understanding | Score on a validated post-consent comprehension assessment | Participant Comprehension Test | >90% correct on key elements [3] |
| Documentation of "teach-back" or participant paraphrasing in source notes | Subject Source Notes | >95% of participants [46] | |
| Process Quality | Observer scores using a validated tool (e.g., P-QIC) | Direct observation, Scored Checklists | >90% on communication items [3] |
| % of participants reporting a positive consent experience | Participant Experience Survey (e.g., SPFQ) | Net Positive Feedback [86] | |
| Stakeholder Engagement | % of trials where patient insights were implemented in consent design | Protocol, Patient Engagement Logs | Positive Trend [86] |
| Healthcare professional knowledge scores on informed consent policies | AHRQ HCP Survey or equivalent | >80% correct [87] |
Experimental Protocol: Direct Observation with the P-QIC Tool
Objective: To objectively assess the quality of the interaction during the informed consent encounter using a standardized, validated observational instrument.
Materials:
- Process and Quality of Informed Consent (P-QIC) Tool: A validated checklist integrating essential elements of information and communication [3].
- Audio/Video Recording Equipment (optional): To allow for later review and calibration between raters.
- Quiet, Private Room: The standard environment for consent discussions.
Methodology:
- Train Auditors/Raters: Ensure all auditors are trained on the P-QIC tool and its scoring criteria. The tool measures both the delivery of required information (e.g., research nature, risks, benefits, alternatives) and the quality of communication (e.g., use of plain language, checking for understanding, encouraging questions) [3].
- Conduct Calibration Session: Prior to the audit, have raters independently score the same recorded or live consent encounter. Compare scores and discuss discrepancies to ensure consistent application of the tool.
- Execute Direct Observation: The auditor observes the live consent discussion between the investigator/designee and the potential participant. The auditor does not participate in the discussion.
- Score the Encounter: Using the P-QIC tool, the auditor scores each item related to information provision and communication behaviors as they occur.
- Calculate Composite Scores: After the encounter, calculate scores for the "Information" and "Communication" domains, as well as an overall quality score. These scores provide a quantitative basis for identifying strengths and weaknesses in the consent process and for measuring improvement over time [3].
The Auditor's Toolkit
A robust consent process audit requires specific tools and reagents to assess both documentation and interactive quality effectively.
Table 3: Research Reagent Solutions for Consent Process Auditing
| Tool / Reagent | Primary Function | Application in Audit |
|---|---|---|
| Validated Consent Checklists (e.g., from [60]) | Standardized assessment of ICF content and regulatory elements. | Ensures every required informational element is present in the ICF document as per GCP and local regulations. |
| P-QIC Observational Tool [3] | Quantitative measurement of the consent interaction quality. | Objectively scores the investigator's communication skills and completeness of the verbal explanation. |
| Participant Comprehension Assessment | Directly measures participant understanding post-consent. | Validates the effectiveness of the consent process; can be a simple quiz on key study aspects (e.g., purpose, risks, randomization). |
| AHRQ HCP Survey [87] | Assesses healthcare professional knowledge and attitudes on consent. | Evaluates the site team's foundational understanding of informed consent principles and policies, a key contributor to process quality. |
| eConsent Platform Audit Logs | Digital record of participant interaction with consent materials. | Provides verifiable data on time spent reviewing materials, questions asked, and version control, supporting remote or hybrid audit activities. |
Integrated Audit Workflow
A comprehensive audit of the informed consent process should follow a logical sequence, moving from system-level reviews to direct observation and culminating in data synthesis and reporting. The diagram below illustrates this integrated workflow.
A modern, effective audit of the informed consent process must transcend a simple check for signatures. It requires a dual focus on strict regulatory compliance and meaningful participant engagement. By implementing the structured metrics, detailed protocols, and integrated workflow outlined in this document, auditors, researchers, and drug development professionals can transform the consent audit from a compliance exercise into a powerful tool for quality improvement. This rigorous approach directly contributes to the broader thesis of obtaining valid informed consent by ensuring the process is not only legally defensible but also ethically sound, thereby strengthening participant trust and the integrity of clinical research as a whole.
Informed consent serves as a cornerstone of ethical clinical research, ensuring that participants autonomously agree to partake in studies based on comprehension of relevant risks and benefits. However, traditional consent models face significant practical challenges in real-world research scenarios, particularly in pragmatic trials aiming to generate evidence under routine care conditions. This article examines three distinct approaches—Zelen's design, cluster randomized controlled trials (RCTs), and pragmatic trials—that modify conventional consent processes to address specific methodological and ethical challenges. These innovative frameworks attempt to balance the ethical imperative of informed consent with the practical necessities of conducting research that is generalizable, efficient, and reflective of real-world clinical practice. The following sections provide a detailed comparison of these models, their applications, and practical protocols for implementation, framed within the broader context of obtaining valid informed consent in clinical research.
Comparative Analysis of Consent Models
The table below summarizes the key characteristics, ethical considerations, and applications of Zelen's design, cluster RCTs, and pragmatic trials, highlighting their distinct approaches to informed consent.
Table 1: Comparison of Consent Models in Clinical Trial Designs
| Feature | Zelen's Design | Cluster RCTs | Pragmatic Trials |
|---|---|---|---|
| Core Concept of Consent Modification | Randomization occurs before seeking consent; participants are informed of and consent only to their assigned intervention [88]. | Randomization and intervention are applied at the group level (e.g., clinic, community); individual consent may be infeasible or sought for data collection only [89]. | Aims to integrate research into routine care; may use alterations or waivers of consent when the intervention is low-risk and embedded in practice [90]. |
| Primary Rationale | To minimize disappointment bias and increase participation rates by avoiding pre-randomization discussion of a potentially desirable treatment the participant may not receive [88]. | To avoid contamination (e.g., in public health interventions) and to evaluate interventions that can only be implemented at a group level [89]. | To enhance external validity and generalizability by studying interventions in real-world settings with diverse, representative populations [90] [91]. |
| Common Consent Approach | Single-consent design: Only the experimental group is informed of the study [88].Double-consent design: Both groups are asked to consent after randomization [88] [92]. | Cluster-cluster: Individual consent is often not feasible for the intervention [89].Individual-cluster: Individuals may consent to the intervention but not to cluster-level randomization [89]. | Consent may be waived or altered for low-risk interventions compared to usual care, or an opt-out process may be used [90]. |
| Key Ethical Justification | The scientific need to assess real-world consequences of an intervention and the minimal risk imposed, especially in single-consent designs where control subjects receive usual care [88]. | The intervention is delivered at a community level, mirroring public health practice where individual consent is not always sought [89]. | The research poses no more than minimal risk, and obtaining consent is impracticable. The waiver does not adversely affect participants' rights and welfare [2] [90]. |
| Typical Applications | Evaluating outreach or engagement interventions for stigmatized conditions; comparing treatments where patient preference is strong [88]. | Public health interventions (e.g., community education), studies of practice change among healthcare providers [89]. | Comparing standard-of-care treatments, evaluating quality improvement initiatives, and embedded research within healthcare systems [90] [91]. |
Detailed Methodological Protocols
Protocol 1: Implementing a Zelen Single-Consent Design
The Zelen single-consent model is particularly useful for trials where introducing the concept of a new, potentially desirable treatment to all eligible patients could cause disappointment bias in those not receiving it, thereby skewing the results.
Table 2: Protocol for a Zelen Single-Consent Trial
| Protocol Step | Detailed Procedure | Example from KOA Trial [93] |
|---|---|---|
| 1. Identification & Eligibility | Identify potential participants automatically from existing records (e.g., electronic health records) based on pre-defined inclusion/exclusion criteria. Avoid active recruitment that discloses the study [88]. | Patients with knee osteoarthritis (KOA) were identified from hospital outpatient departments. Eligibility was confirmed based on ACR criteria, age, pain scores, and KL grade. |
| 2. Randomization | Eligible individuals are randomly assigned to either the experimental or control group before any contact is made regarding the study [88] [93]. | After enrollment assessment, 74 eligible participants were randomized 1:1 to either the Infrared Laser Moxibustion (ILM) or Traditional Moxibustion (TM) group. |
| 3. Seeking Consent & Intervention | Experimental Group: Contacted and provided with full information about the assigned intervention. Their consent is sought specifically for that treatment [88].Control Group: Not informed of the study and continue to receive usual care without any contact or disruption [88]. | ILM Group: Asked if they were willing to comply with the randomized ILM treatment. If they agreed, they were enrolled.TM Group: Directly enrolled without any questioning or consent process regarding the study and received traditional moxibustion. |
| 4. Outcome Assessment | Outcomes are assessed using routinely collected data (e.g., electronic records) or through blinded outcome assessors to minimize bias [88]. | Primary outcome (pain score on NRS) was assessed at baseline and week 6. Outcome evaluators, data collectors, and analysts were blinded to group assignment. |
| 5. Data Analysis | Analysis follows the intention-to-treat principle, comparing outcomes based on the original random assignment, regardless of whether participants in the experimental group accepted the treatment [88]. | The analysis will compare the mean change in pain scores between the ILM and TM groups as they were originally randomized. |
Protocol 2: Managing Consent in a Cluster Pragmatic Trial
This protocol is adapted from the Hyperlink 3 hypertension trial, which successfully implemented a pragmatic design with a waiver of informed consent [90].
Table 3: Protocol for a Cluster Pragmatic Trial with Altered Consent
| Protocol Step | Detailed Procedure | Example from Hyperlink 3 Trial [90] |
|---|---|---|
| 1. Study Design & IRB Approval | Design the trial as a cluster-randomized study where the unit of randomization is a clinic, hospital, or community. Seek IRB approval for a partial or full waiver of informed consent under the Revised Common Rule criteria, arguing that the research is low-risk and impracticable without a waiver [89] [90]. | 21 primary care clinics were cluster-randomized. The IRB granted a partial waiver of consent for enrollment because the telehealth intervention was low-risk and the study was impracticable if written consent was required beforehand. |
| 2. Integrated Recruitment | Integrate participant identification and enrollment into routine clinical workflows. Use automated electronic health record (EHR) algorithms to flag eligible patients during clinical encounters [90]. | A real-time EHR algorithm identified eligible adults (18-85) with uncontrolled hypertension during primary care visits. A "best practice alert" prompted clinic staff to action. |
| 3. Enrollment Procedure | Enrollment is defined by a clinical action, such as a physician signing a referral order for the study intervention. This occurs without a formal research consent process at the point of enrollment [90]. | Enrollment was defined by the primary care professional signing a hypertension follow-up referral order (defaulting to pharmacist care in intervention clinics). The date of this encounter was the enrollment date. |
| 4. Subsequent Information & Data Collection | After enrollment, participants may be contacted for data collection (e.g., surveys). The cover letter or phone script for such activities should include elements of informed consent, and completion implies consent for data use [90]. | Enrolled patients were later mailed a survey. The cover letter included information about the study, and returning the survey implied consent to use the data. |
| 5. Outcome Ascertainment | Rely primarily on data collected through routine care within the health system (e.g., EHR data on blood pressure, hospitalizations) to assess the primary outcome [90]. | The primary outcome (blood pressure control) was assessed using data extracted directly from the EHR, minimizing additional research-specific procedures. |
Logical Workflow and Decision Pathway
The following diagram illustrates the logical relationship between the different trial designs and their associated consent models, highlighting key decision points for researchers.
The Scientist's Toolkit: Essential Research Reagents and Methodological Tools
Successful implementation of these advanced consent models requires specific methodological "reagents" and tools beyond traditional clinical trial supplies.
Table 4: Essential Methodological Tools for Implementing Alternative Consent Models
| Tool / Reagent | Function & Application | Key Considerations |
|---|---|---|
| PRECIS-2 Tool [90] | A framework to score a trial's design across nine domains on a continuum from explanatory (very controlled) to pragmatic (very real-world). | Justifies pragmatic design choices, including alterations to consent, to reviewers and IRBs by visually demonstrating the trial's real-world intent. |
| Institutional Review Board (IRB) Waiver Criteria [88] [2] | The regulatory basis (e.g., Revised Common Rule) for requesting a waiver or alteration of informed consent. | Researchers must prepare a robust application demonstrating the research is impracticable without the waiver and poses no more than minimal risk. |
| Electronic Health Record (EHR) System with Alert Functionality [90] | Enables automated, real-time identification and enrollment of eligible participants during routine care, as used in pragmatic trials. | Requires close collaboration with IT and clinical stakeholders. Algorithms must be rigorously validated to correctly identify the target population. |
| Robust Data Warehouses & Linkage Systems | Allows for the collection of primary outcome data from routine sources (e.g., claims data, registries), minimizing research-specific procedures for participants [88] [91]. | Ensures data quality and completeness are sufficient for analysis. Addresses data privacy and security concerns. |
| Community Engagement & Advisory Boards | Provides a mechanism for "community-level consent" or consultation, which is particularly valuable in cluster RCTs and Zelen designs where individual consent is not obtained [89]. | Helps ensure the research is acceptable to the affected community, builds trust, and can advise on ethical and practical challenges. |
Obtaining valid informed consent is a fundamental ethical and regulatory requirement in clinical research, representing more than a signature on a form. It constitutes a comprehensive, ongoing process that begins at the first interaction with a potential participant and continues through to their eventual withdrawal or study completion. This process safeguards the autonomy of research participants and ensures the integrity of clinical data. Framed within the broader thesis of obtaining valid consent, this document provides detailed application notes and protocols for researchers, scientists, and drug development professionals, emphasizing meticulous documentation at every stage to uphold the principles of Good Clinical Practice (GCP).
Core Principles of Valid Informed Consent
The informed consent process is built upon three critical ethical pillars that must be present for consent to be considered valid: voluntarism, information disclosure, and decision-making capacity [94].
- Voluntarism: The participant's decision must be made freely, independently, and without coercion, undue influence, or pressure. Factors such as the psychological effects of illness, cultural beliefs, or dependency on caregivers can compromise voluntarism, particularly in vulnerable populations [94].
- Information Disclosure: Researchers must provide all information necessary for a reasonable person to make an informed decision. This includes the study's purpose, procedures, risks, benefits, alternatives, and the rights of the participant [14] [94]. The information must be presented in a manner that is easily understood, using lay language appropriate to the participant's comprehension level [14] [4].
- Decision-Making Capacity: The potential participant must possess the cognitive ability to understand the disclosed information, appreciate its consequences for their own situation, reason through the options, and communicate a clear choice [94]. Capacity is distinct from legal competence, which is a formal judicial determination [94].
Table 1: Core Elements of Informed Consent as per Regulatory Guidelines [14] [5]
| Element Category | Specific Requirement |
|---|---|
| Study Overview | Title, investigator names, research purpose, expected duration, and procedures [5]. |
| Risks & Benefits | Description of reasonably foreseeable risks, discomforts, and potential benefits (if any) [14] [5]. |
| Alternatives & Rights | Disclosure of alternative procedures/treatments; clarity that participation is voluntary and withdrawal is allowed without penalty [14] [5]. |
| Data & Confidentiality | Statements on privacy, data confidentiality, future use of data or biospecimens, and, if applicable, whole genome sequencing [14] [5]. |
| Contacts & Injury | Contact information for questions about the study and research-related injuries [14] [5]. |
The Informed Consent Workflow: A Visual Guide
The following diagram maps the entire informed consent process, from initial contact through to ongoing participation and potential withdrawal, highlighting key documentation and decision points.
Informed Consent Workflow - The complete process from initial contact to study conclusion, showing key stages and feedback loops for participant understanding.
Detailed Experimental Protocols
Protocol 1: Pre-Consent Readiness and Participant Assessment
Objective: To ensure the potential participant is in a suitable cognitive and emotional state to engage in the informed consent process, thereby upholding the principle of voluntarism.
Methodology:
- Environment Setup: Conduct the initial discussion in a quiet, private, and distraction-free setting to minimize external pressures [46]. Allow ample time for the conversation, avoiding rushed interactions immediately before study procedures.
- Cognitive and Emotional Evaluation: The CRC or investigator should verbally assess the participant's focus and comprehension. This involves observing for signs of stress, confusion, or impairment that could affect decision-making capacity [46].
- Eligibility Pre-Screening: Briefly review key inclusion/exclusion criteria to confirm preliminary eligibility before delving into the detailed consent form, ensuring the process is respectful of the participant's time.
Documentation: Create a contemporaneous note in the participant's source record confirming the environment was appropriate, the participant appeared capable of engaging, and no undue influence was applied [94] [46].
Protocol 2: Delivering Information and Assessing Comprehension
Objective: To verify genuine understanding of the study using structured communication techniques, rather than assuming comprehension from a signature.
Methodology:
- Plain Language Delivery: Present the informed consent form using short paragraphs, bullet points, and subheadings. Replace complex scientific or legal jargon with plain language (e.g., "by chance" instead of "randomized") [5] [4] [46]. The form should ideally be written at an 8th-grade reading level [46].
- Interactive Teach-Back Method: After explaining a section, ask the participant open-ended questions to restate the information in their own words [4] [46]. Example prompts include:
- "Can you tell me what you understand this study will involve for you?"
- "What are the main risks that stand out to you?"
- "What would you do if you wanted to stop being in the study?"
- Iterative Clarification: If misunderstanding is detected, rephrase the information, use analogies or visuals, and re-assess until comprehension is confirmed. Document the use of teach-back and any necessary re-explanation in the source notes [46].
Documentation: Source notes must detail the questions asked, the participant's responses demonstrating understanding, and any educational tools or aids used.
Table 2: Comprehension Verification Checklist
| Concept to Assess | Sample Teach-Back Question | Acceptable Response Indicator |
|---|---|---|
| Study Purpose | "Can you explain why we are doing this study in your own words?" | Articulates the research goal beyond "to help science." |
| Procedures | "What are the main things you'll be asked to do during the study?" | Identifies key activities like specific tests, visits, or logs. |
| Risks | "What are the potential downsides or discomforts you remember?" | Mentions specific, foreseeable risks described in the ICF. |
| Voluntarism | "What happens if you decide you don't want to be in the study anymore?" | States they can quit at any time without penalty to their medical care. |
Protocol 3: Managing Consent Updates and Participant Withdrawal
Objective: To maintain the validity of consent throughout the study lifecycle and manage participant withdrawal in an ethically and procedurally sound manner.
Methodology:
- Re-consent Trigger Protocol: Implement a standardized process to identify participants requiring re-consent when a protocol amendment introduces new procedures, risks, or benefits [46]. Pause any new study activities affected by the amendment until the updated IRB-approved consent form is signed.
- Orderly Withdrawal Process: When a participant expresses a desire to withdraw, clarify the level of withdrawal:
- Withdrawal from study intervention only: Participant stops treatment but allows continued data collection.
- Full withdrawal: Participant stops all study activities and revokes permission for future use of their data [5].
- Exit Communication: Conduct a final discussion to explain any required safety follow-up, the plan for returning standard care to the primary physician (with permission), and express gratitude for their contribution. Provide a copy of the signed withdrawal documentation.
Documentation: For re-consent, file the newly signed ICF and update the consent version log. For withdrawal, complete a "Withdrawal of Consent" form or a dedicated study case report form (eCRF) page, noting the date, reason (if given), and the scope of withdrawal.
Table 3: Key Research Reagent Solutions for the Informed Consent Process
| Tool / Resource | Function & Application | Regulatory Consideration |
|---|---|---|
| Version-Controlled ICF Templates | Pre-approved, plain-language consent form templates that can be adapted for specific studies, ensuring consistency and regulatory compliance [4] [95]. | Must be approved by the IRB/IEC; each version must have a unique identifier and date [46]. |
| Electronic Consent (eConsent) Platforms | Digital systems for delivering consent information, facilitating signatures, and managing the consent lifecycle (e.g., Medidata eConsent, REDCap) [46]. | Must be 21 CFR Part 11 compliant, with audit trails, user authentication, and version control [46]. |
| Consent Tracking Log | A centralized log (digital or paper-based) that records the consent version and date for every participant, crucial for audit trails and managing re-consent [46]. | A critical document for monitoring and audit; must be maintained in the regulatory binder [46]. |
| Health Literacy Assessment Tools | Readability software and participant feedback mechanisms (e.g., usability testing) to ensure consent forms are comprehensible to the target population [4]. | The FDA requires forms to be "understandable to the participant"; IRBs determine appropriateness for the population [95]. |
| Teach-Back Scripts & Aids | Standardized question guides, visual aids, and glossaries to assist research staff in explaining complex concepts and verifying understanding [4] [46]. | Documentation of their use in source notes demonstrates a good-faith effort to ensure comprehension. |
Documenting the entire informed consent process—from the initial contact through the decision to withdraw—is a dynamic and participant-centered endeavor. It transcends regulatory compliance, forming the ethical foundation of clinical research. By adhering to the detailed protocols and utilizing the tools outlined in this document, researchers can ensure that consent is not merely a signed form, but a meaningful, ongoing dialogue. This rigorous approach protects participant autonomy, enhances the quality and validity of research data, and ultimately strengthens the public's trust in the clinical research enterprise.
Informed consent serves as the ethical cornerstone of clinical research, yet evidence consistently demonstrates deficiencies in participant understanding and engagement. The traditional approach to informed consent—often characterized by lengthy, complex documents and a one-time signature event—has proven inadequate for ensuring genuine participant comprehension [96] [6]. A paradigm shift is underway, recognizing informed consent not as a bureaucratic hurdle but as an ongoing, interactive process that benefits substantially from structured participant feedback [96] [97]. This application note establishes why and how clinical researchers should systematically incorporate participant feedback to develop more effective, ethical consent materials that respect participant autonomy and enhance research quality.
Broad consensus among sponsors, research staff, and participants indicates significant room for improvement in current consent processes [97]. Research staff have expressed particular concern about participant comprehension, with 56% of staff worried about whether participants understood complex information and 63% finding information leaflets too long and/or complicated [6]. Quantitative evidence demonstrates that how information is presented significantly impacts consent decisions; one randomized controlled trial showed consent rates of 67% when benefits were framed positively versus 42% when identical information was framed negatively [98] [99]. This evidence underscores the critical importance of optimizing consent materials through direct participant input.
Quantitative Evidence: The Case for Improvement
Recent studies provide compelling quantitative evidence supporting the need for enhanced consent processes. The table below summarizes key findings from research evaluating current consent practices and the impact of various improvements.
Table 1: Quantitative Evidence on Consent Process Effectiveness
| Study Focus | Sample Size | Key Findings | Statistical Significance |
|---|---|---|---|
| Staff confidence in consent process [6] | 115 research staff | 74.4% felt confident facilitating discussions; 63% found leaflets too long/complicated | Descriptive statistics |
| Participant satisfaction [6] | 169 research participants | Majority positive about experience; highlighted need for adequate time and follow-up | Descriptive statistics |
| Impact of quantitative framing [98] | 100 participants | Consent rate 67% (positive frame) vs. 42% (negative frame) | p < 0.01 |
| Symptom severity effect [98] | 100 participants | Lower consent rates with minimal/severe symptoms vs. mid-range symptoms | χ²(2) = 8.35, p = 0.015 |
| Guideline recommendation validation [96] | Expert panel | 43 of 53 recommendations deemed appropriate; median scores 6.5-9/9 | Descriptive statistics |
Research participants themselves have identified specific areas for improvement, with emphasis on sufficient time for decision-making and the value of receiving study results after completion [6]. The i-CONSENT project validation demonstrated strong expert support for participant-centered approaches, with all recommended guidelines receiving median appropriateness scores between 6.5-9 on a 1-9 scale [96]. These findings collectively build a compelling evidence base for systematically integrating participant feedback into consent material development.
Methodological Framework: Structured Approaches for Feedback Integration
Design Thinking Methodology
The i-CONSENT guidelines recommend Design Thinking methodology to tailor information to the specific audience [96]. This human-centered approach involves representatives of the target population in all development steps, including designing and co-creating documents, implementing the consent process, and providing feedback for improvement [96]. The methodology enables two-way, seamless interaction that allows researchers to detect and clarify concepts likely to be misunderstood, particularly by people with low health literacy [96].
Layered Information Approach
A key innovation in participant-centric consent is the strategy of providing information in layers, allowing participants to decide for themselves how much detail they receive about a research study [96]. This approach respects individual differences in information preferences and prevents overwhelming potential participants with excessive information all at once. The layered approach typically includes:
- Level 1: Essential information for decision-making (1-2 pages)
- Level 2: Key study details and procedures (3-5 pages)
- Level 3: Comprehensive technical information (full protocol)
This structure was successfully implemented in the VIGIRA study on influenza vaccine effects in children, where materials were designed "WITH and FOR parents of children who could potentially participate in the study" [96]. The co-creation process involved interviews with parents of potential participants and incorporated feedback from researchers and participants from previous seasons [96].
Multi-Format Presentation
Contemporary consent processes should accommodate diverse preferences and needs by presenting information in different formats that may be combined with new technologies [96]. Research indicates that today's reading and learning habits have changed, with written texts increasingly incorporating elements such as hyperlinks, multimedia, images, and infographics [96]. By offering format choices, researchers respect participant autonomy while enhancing comprehension across diverse populations.
Experimental Protocols for Feedback Collection
Protocol 1: Comprehension Assessment Using Teach-Back Methods
Objective: To evaluate and improve participant understanding of key study concepts through interactive verification.
Table 2: Comprehension Assessment Protocol
| Step | Procedure | Duration | Data Collected |
|---|---|---|---|
| 1. Structured Explanation | Present study information using standardized script | 15-20 minutes | Baseline understanding |
| 2. Teach-Back Implementation | Ask participant to explain concepts in their own words | 10-15 minutes | Comprehension accuracy |
| 3. Clarification | Address misunderstandings immediately | 5-10 minutes | Specific knowledge gaps |
| 4. Documentation | Record responses and areas needing clarification | 5 minutes | Qualitative and quantitative metrics |
| 5. Material Revision | Modify consent materials based on identified issues | Variable | Version improvements |
This protocol directly addresses research findings that staff are concerned about participant understanding but seldom confirm comprehension levels during consent discussions [6]. The teach-back method has demonstrated effectiveness in improving understanding in informed consent contexts [6].
Protocol 2: Co-Creation Workshops for Consent Material Development
Objective: To collaboratively develop and refine consent materials with representative participants.
Materials and Setup:
- Diverse participant group (8-12 individuals)
- Draft consent materials and visual aids
- Neutral facilitation by trained staff
- Recording equipment for documentation
- Iterative prototyping tools
Procedure:
- Recruitment: Purposefully sample potential participants representing various literacy levels, ages, and backgrounds relevant to the study population.
- Orientation: Explain workshop goals and the importance of participant feedback.
- Content Review: Present draft materials section by section, soliciting initial reactions.
- Comprehension Checking: Use open-ended questions to assess understanding of key concepts.
- Redesign Collaboration: Work together to rewrite problematic sections, create visual aids, or reorganize content.
- Validation: Test revised materials with the group using teach-back methods.
- Documentation: Meticulously record all suggestions, changes, and rationales.
The i-CONSENT project successfully employed similar approaches, conducting design thinking sessions with potential participants to co-create consent forms for hypothetical clinical trials [96]. In some cases, surveys were conducted to learn the needs and preferences of potential participants when direct co-creation wasn't feasible [96].
Implementation Toolkit and Accessibility Standards
Research Reagent Solutions
Table 3: Essential Tools for Effective Consent Material Development
| Tool Category | Specific Examples | Function | Implementation Tips |
|---|---|---|---|
| Comprehension Verification | Teach-back checklist, Understanding assessment questions | Verify genuine understanding beyond signature | Adapt questions to study complexity; use open-ended format |
| Accessibility Enhancement | Contrast checkers, Readability analyzers, Translation services | Ensure materials accessible to diverse populations | Use plain language (<8th grade level); verify color contrast ratios |
| Multi-format Tools | Interactive PDFs, Audio versions, Infographic creators | Cater to different learning preferences | Offer choices; avoid one-size-fits-all approach |
| Feedback Collection | Structured interviews, Focus group guides, Surveys | Gather systematic participant input | Include both quantitative and qualitative measures |
| Documentation Aids | Consent process templates, Recording equipment, Version control systems | Maintain audit trail of development process | Document all changes and rationales |
Accessibility and Design Standards
Effective consent materials must adhere to accessibility standards to accommodate diverse participants. The Web Content Accessibility Guidelines (WCAG) specify minimum contrast ratios of 4.5:1 for normal text and 3:1 for large text (Level AA) [100]. Enhanced contrast requirements (Level AAA) specify ratios of 7:1 for normal text and 4.5:1 for large text [101]. These standards ensure readability for participants with visual impairments or other disabilities.
Additional design considerations include:
- Using plain language equivalent to 8th grade reading level or lower
- Incorporating visual aids and infographics to explain complex concepts
- Providing information in multiple languages when needed
- Offering both paper and electronic formats (eConsent) [97]
- Ensuring compatibility with screen readers and other assistive technologies
Validation and Continuous Improvement Framework
The ultimate validation of improved consent materials comes from demonstrated enhancements in participant understanding and experience. The i-CONSENT project used the RAND/UCLA method for validating clinical guidelines, having an external evaluation panel comprising patient representatives, investigators, ethics experts, pharmaceutical industry representatives, and regulators assess recommendations [96]. This rigorous approach ensures that innovations in consent materials genuinely improve the process rather than merely changing formats.
Continuous improvement requires establishing feedback loops throughout the research lifecycle. This includes:
- Pre-study material development with participant input
- Ongoing comprehension checking during enrollment
- Post-consent interviews to identify residual misunderstandings
- Exit interviews when participants complete study or withdraw
- Systematic analysis of feedback to inform future consent processes
The Clinical Trials Transformation Initiative (CTTI) emphasizes that the ideal informed consent process involves "an ongoing, interactive conversation between the participant and knowledgeable, responsive research staff" supported by tiered consent documents that provide critically relevant information [97]. This approach better meets participant needs while benefiting the clinical trial enterprise by promoting a research culture that encourages informed participation.
Incorporating participant feedback into consent materials represents both an ethical imperative and a practical necessity for modern clinical research. Evidence demonstrates that current processes often fail to ensure genuine understanding, while structured approaches to feedback integration significantly improve both comprehension and participant experience. By adopting design thinking methodologies, implementing layered information approaches, utilizing multi-format presentations, and establishing rigorous validation protocols, researchers can develop consent materials that truly respect participant autonomy and enhance research quality. The tools and frameworks presented in this application note provide actionable guidance for researchers committed to achieving valid informed consent through continuous improvement based on meaningful participant engagement.
Conclusion
Obtaining valid informed consent is a cornerstone of ethical clinical research, requiring a meticulous blend of regulatory knowledge, clear communication, and respect for participant autonomy. This guide synthesizes that it is not a single event but a continuous process that begins before signature and continues through study closure. Success hinges on creating comprehensible materials, conducting meaningful conversations, and adapting to complex scenarios like vulnerable populations and emergency settings. As clinical trials grow more complex and global, future directions must emphasize greater participant engagement, technological integration for the consent process, and ongoing commitment to the ethical principles that protect all research participants.
References
- 1. Informed Consent - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK430827/]
- 2. How to obtain informed consent for research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5980471/]
- 3. Measuring the Process and Quality of Informed Consent for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3638913/]
- 4. Consent Guide - Health Literacy in Clinical Research [https://mrctcenter.org/health-literacy/tools/overview/consent-guide/]
- 5. Elements of Informed Consent [https://www.brandeis.edu/ora/hrpp/special-topics/consent/elements-informed-consent.html]
- 6. An evaluation of the process of informed consent - Trials [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-021-05493-1]
- 7. Informed consent for phase I studies: Evaluation of quantity ... [https://www.sciencedirect.com/science/article/pii/S092375341961197X]
- 8. Informed Consent Forms: A Guide to Ethics & Regulation [https://intuitionlabs.ai/articles/informed-consent-clinical-trial-ethics]
- 9. Informed Consent: What Every Clinical Researcher Must ... [https://ccrps.org/clinical-research-blog/informed-consent-what-every-clinical-researcher-must-know]
- 10. Informed Consent Writing Tip Sheet [https://www.advarra.com/blog/informed-consent-writing-tip-sheet/]
- 11. GCP Expectations for Informed Consent and Subject ... [https://www.clinicaltrials101.com/gcp-expectations-for-informed-consent-and-subject-protection-at-site-level/]
- 12. GCP compliance and readability of informed consent forms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4394576/]
- 13. What is Informed Consent in Clinical Trials [https://www.allclinicaltrials.com/blog/what-is-informed-consent]
- 14. Consent Requirements - Toolkit - NIH [https://toolkit.ncats.nih.gov/module/prepare-for-clinical-trials/giving-input-on-the-informed-consent-process/consent-requirements/]
- 15. E6(R3) Good Clinical Practice (GCP) September 2025 [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/e6r3-good-clinical-practice-gcp]
- 16. Informed Consent: When, Why, and How It's Obtained [https://www.advarra.com/blog/informed-consent-when-why-and-how-its-obtained/]
- 17. Comparing Clinical Trial Regulations: USA vs. APAC [https://tfscro.com/resources/comparing-clinical-trial-regulations-usa-vs-apac/]
- 18. 21 CFR 50.25 -- Elements of informed consent. [https://www.ecfr.gov/current/title-21/chapter-I/subchapter-A/part-50/subpart-B/section-50.25]
- 19. Elements Required on the Consent Form [https://hrpp.research.virginia.edu/teams/irb-hsr/researcher-guide-irb-hsr/elements-required-consent-form]
- 20. Informed Consent: The Elements of ... [https://www.tc.columbia.edu/institutional-review-board/irb-blog/2025/informed-consent-the-elements-of-informed-consent-documents-series-2/]
- 21. Informed Consent Process in Clinical Trials [https://ccrps.org/clinical-research-blog/informed-consent-process-in-clinical-trials]
- 22. The Nuances of Informed Consent in Clinical Trials | Castor [https://www.castoredc.com/blog/nuances-of-informed-consent-clinical-trials/]
- 23. Waiver of informed consent in clinical research [https://pmc.ncbi.nlm.nih.gov/articles/PMC11927427/]
- 24. April 22, 2025: New Report Highlights Value of Informing ... [https://rethinkingclinicaltrials.org/news/april-22-2025-new-report-highlights-value-of-informing-participants-about-research-conducted-under-a-waiver-of-consent/]
- 25. Complex and alternate consent pathways in clinical trials [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-023-07159-6]
- 26. Readability of informed consent forms in clinical trials ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4958927/]
- 27. An evaluation of the process of informed consent [https://pmc.ncbi.nlm.nih.gov/articles/PMC8371296/]
- 28. Informed Consent: Reading and Understanding Are Not ... [https://www.appliedclinicaltrialsonline.com/view/informed-consent-reading-and-understanding-are-not-same]
- 29. How to Prepare a Readable Consent Form [https://www.hopkinsmedicine.org/institutional-review-board/guidelines-policies/guidelines/informed-consent-ii]
- 30. Top 10 Tips for Improving Readability of Informed Consent ... [https://www.hrpo.pitt.edu/top-10-tips-improving-readability-informed-consent-documents]
- 31. Digitalizing the Clinical Research Informed Consent Process [https://pmc.ncbi.nlm.nih.gov/articles/PMC10022878/]
- 32. Short Form Consent Process - Stanford IRB [https://irb.stanford.edu/for-researchers/consent-process/short-form-consent-process]
- 33. ICH视角下GCP合规的责任主体与监管机制 [https://www.zhonglun.com/research/articles/54855.html]
- 34. SPIRIT 2025 statement: Updated guideline for protocols of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037212/]
- 35. 病例报告表CRF、EDC的哪些事-临床试验120 [http://lcsy120.com/linchuangshiyan-wenda/3194.html]
- 36. 临床试验研究数据列表模型元数据递交指南(CDISC SDTM-MSG v2.0)-CSDN博客 [https://blog.csdn.net/Bowen_Wu/article/details/141639832]
- 37. Guidelines for Obtaining Informed Consent for Clinical ... [https://www.appliedclinicaltrialsonline.com/view/guidelines-obtaining-informed-consent-clinical-research]
- 38. Social Determinants of Health and Informed Consent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10714248/]
- 39. Informed consent process: A step further towards making it ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5543760/]
- 40. Teach-Back: A Simple Technique to Enhance Patients ... [https://www.aafp.org/pubs/fpm/issues/2018/0700/p20.html]
- 41. Patient reported measures of informed for consent ... clinical trials [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0199775]
- 42. Use and Effectiveness of the Teach-Back Method in Patient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6590951/]
- 43. The teach-back method: Communicating more effectively ... [https://webmdignite.com/blog/teach-back-method-communicating-more-effectively-patients-improve-health-outcomes]
- 44. Effectiveness of discharge education using teach-back ... [https://www.sciencedirect.com/science/article/abs/pii/S0738399122008254]
- 45. A Refined Teach-back Observation Tool: Validity Evidence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10561624/]
- 46. Informed Consent for CRCs – Best Practices, Tools, and ... [https://ccrps.org/clinical-research-blog/informed-consent-essentials-crcs-guide-to-best-practices]
- 47. Core elements of consent documentation for clinical research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12448764/]
- 48. Informed Consent Guidelines & Templates [https://hrpp.umich.edu/irb-health-sciences-and-behavioral-sciences-hsbs/informed-consent-guidelines-templates/]
- 49. Good Clinical Practice Study Documentation [https://medicine.duke.edu/research/scholarly-culture-and-accountability/good-clinical-practice-study-documentation]
- 50. Electronic Storage of Human Research Study Documents [https://research.washu.edu/electronic-storage-research-study-documents/]
- 51. Best Practices for Writing Informed Consent Forms in ... [https://clinixir.com/blog/best-practices-for-writing-informed-consent-forms-in-clinical-research]
- 52. The Requirements for Informed Consent (Series #1) [https://www.tc.columbia.edu/institutional-review-board/irb-blog/2025/informed-consent-the-requirements-for-informed-consent-series-1/]
- 53. With the Right Approach, Vulnerable Populations Can and ... [https://acrpnet.org/2025/10/29/with-the-right-approach-vulnerable-populations-can-and-should-be-engaged-in-research]
- 54. Vulnerability in research ethics: A systematic review of policy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12212517/]
- 55. Considerations for enrolling Vulnerable Populations in ... [https://tfscro.com/resources/regulatory-considerations-for-enrolling-vulnerable-populations-in-clinical-trials/]
- 56. Informed Consent or Assent Strategies for Research With ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8212005/]
- 57. Ethical challenges involved in obtaining consent for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5750252/]
- 58. The 'Consent to Research' paradigm in critical care [https://link.springer.com/article/10.1007/s00134-009-1562-9]
- 59. Best Practices for Handling Informed Consent in ... [https://acrpnet.org/2024/12/13/best-practices-for-handling-informed-consent-in-emergency-medical-cases]
- 60. [Translated article] Design and validation of two ... [https://www.sciencedirect.com/science/article/pii/S1130634323000028]
- 61. Participants' understanding of informed consent in clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4371493/]
- 62. FDA Finalizes Guidance for IRBs, Clinical Investigators ... [https://perkinscoie.com/insights/article/fda-finalizes-guidance-irbs-clinical-investigators-and-sponsors-informed-consent]
- 63. Language Barriers in Clinical Trials Participation [https://trialx.com/language-barriers-in-clinical-trials-participation-can-innovation-bridge-the-gaps-improve-diversity/]
- 64. Language & Culture in Global Clinical Trials [https://www.appliedclinicaltrialsonline.com/view/language-culture-global-clinical-trials]
- 65. Participants' understanding of informed consent in clinical trials [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0295784]
- 66. Informed Consent in West Africa: Bridging Regulatory ... [https://globalforum.diaglobal.org/issue/april-2025/informed-consent-in-west-africa-bridging-regulatory-compliance-and-cultural-diversity/]
- 67. Enhancing Informed Consent Forms for Medical Devices [https://pmc.ncbi.nlm.nih.gov/articles/PMC12311233/]
- 68. Understanding Barriers and Facilitators for Ethnic Minority ... [https://pubmed.ncbi.nlm.nih.gov/40098296/]
- 69. Health Literacy Resources: Assessment - Guides [https://guides.hshsl.umaryland.edu/healthliteracy/assessment]
- 70. Health literacy and usability of clinical trial search engines [https://pubmed.ncbi.nlm.nih.gov/25315593/]
- 71. 公共卫生研究中的伦理问题处理 [https://jphe.amegroups.org/article/view/4312/10865]
- 72. HPC Intelligence FDA法规培训 - 美国汉佛莱医药顾问有限公司 [http://www.humphriespcc.com/resources/training_72.html]
- 73. 如何获得知情同意书,解释试验情况后的必要步骤。 [http://www.jccro.com/anli/1381.html]
- 74. 【技术】要点速记!知情与知情同意监查常见问题 [https://www.clin-nov.com.cn/xwzx/html/509.html]
- 75. Consent | Medidata官网| Medidata Solutions [https://www.medidata.com/cn/clinical-trial-products/patient-centric-clinical-trials/consent/]
- 76. 终极指南- 2025年最佳知情同意书(ICF)翻译工具 [https://x-doc.ai/articles/zh-Hans/the-best-informed-consent-form-translator]
- 77. Institutional Review Boards Frequently Asked Questions [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/institutional-review-boards-frequently-asked-questions]
- 78. Guiding Principles for Ethical Research [https://www.nih.gov/health-information/nih-clinical-research-trials-you/guiding-principles-ethical-research]
- 79. Institutional Review Board [http://orwh.od.nih.gov/toolkit/human-subjects-protections/institutional-review-board]
- 80. Ethics Guidelines [https://neurips.cc/public/EthicsGuidelines]
- 81. Research Ethics Review Committee (ERC) [https://www.who.int/groups/research-ethics-review-committee/review-process]
- 82. Institutional Review Boards: Actions Needed to Improve ... [https://www.gao.gov/products/gao-23-104721]
- 83. Publication Ethics [https://icml.cc/Conferences/2025/PublicationEthics]
- 84. Clinical Investigator Site Audits: A Guide and Checklist ... [https://www.thefdagroup.com/blog/clinical-trial-investigator-site-audits]
- 85. GxP Audits Guide for Successful Clinical Trials [https://www.advarra.com/blog/gxp-audits-guide-for-successful-clinical-trials/]
- 86. CTTI's Metrics Framework [https://ctti-clinicaltrials.org/about/transforming-trials-2030/cttis-metrics-framework/]
- 87. Content Validity of the AHRQ Health Care Professional ... [https://opennursingjournal.com/VOLUME/16/ELOCATOR/e187443462205300/FULLTEXT/]
- 88. Zelen design clinical trials: why, when, and how | Full Text [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-021-05517-w]
- 89. Informed Consent and Cluster-Randomized Trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3487664/]
- 90. Comparison of explanatory and pragmatic design choices in a ... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-022-06611-3]
- 91. Experimental Designs and Randomization Schemes [https://rethinkingclinicaltrials.org/chapters/design/experimental-designs-and-randomization-schemes/experimental-designs-introduction/]
- 92. Optimizing clinical scientific research: the cohort intervention ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12580914/]
- 93. study protocol for a Zelen-design randomized controlled non ... [https://josr-online.biomedcentral.com/articles/10.1186/s13018-023-04408-x]
- 94. Informed consent in clinical research: Revisiting few ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3601699/]
- 95. Ways to Streamline Informed Consent Process in Clinical ... [https://www.advarra.com/blog/ways-to-streamline-informed-consent-process-in-clinical-trial-startup/]
- 96. Keys to improving the informed consent process in research [https://pmc.ncbi.nlm.nih.gov/articles/PMC9327854/]
- 97. Paving the way to a more effective informed consent process [https://www.sciencedirect.com/science/article/pii/S1551714416300854]
- 98. A randomized controlled trial comparing quantitative ... [https://pubmed.ncbi.nlm.nih.gov/1941028/]
- 99. A randomized controlled trial comparing quantitative ... [https://www.sciencedirect.com/science/article/abs/pii/089543569190129W]
- 100. Understanding WCAG 2 Contrast and Color Requirements [https://webaim.org/articles/contrast/]
- 101. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]