The Evolution of Bioethics in the United States: From Historical Foundations to Modern Institutionalization
This article provides a comprehensive analysis of the historical emergence and institutionalization of bioethics in the United States, tailored for researchers, scientists, and drug development professionals.
The Evolution of Bioethics in the United States: From Historical Foundations to Modern Institutionalization
Abstract
This article provides a comprehensive analysis of the historical emergence and institutionalization of bioethics in the United States, tailored for researchers, scientists, and drug development professionals. It explores the foundational scandals and socio-political forces that shaped the field, details the development of key ethical frameworks and regulatory bodies like IRBs, examines persistent challenges in human subject protection and policy, and compares the distinct professionalization of bioethics in the U.S. versus other national contexts. The synthesis offers critical insights for navigating contemporary ethical dilemmas in biomedical research and clinical practice.
Origins and Catalysts: The Historical Forces that Forged American Bioethics
The period between the adoption of the American Medical Association's (AMA) Code of Ethics in 1847 and the promulgation of the Nuremberg Code in 1947 represents a foundational epoch in the history of medical ethics and the emergence of modern bioethics. This two-century span witnessed a profound transformation in the ethical governance of medicine, shifting from a framework of internal professional etiquette toward one encompassing universal human rights and explicit protections for individuals in the context of scientific research. This evolution was driven by unprecedented scientific advances, egregious ethical failures in human experimentation, and significant socio-legal challenges to medical paternalism. This whitepaper traces these key historical precedents, situating them within the broader thesis of bioethics' institutionalization in the United States. For researchers, scientists, and drug development professionals, understanding this historical trajectory is crucial for appreciating the ethical underpinnings of contemporary regulatory frameworks governing human subjects research.
The AMA Code of Medical Ethics (1847): Codifying Professional Conduct
The Code of Medical Ethics adopted at the inaugural meeting of the American Medical Association in 1847 marked the first formal attempt to codify medical ethics in the United States [1]. Its creation was a primary objective for the newly formed professional body, reflecting a desire to establish medicine as a self-regulating profession with defined standards of conduct.
Historical Context and Founding Principles
The 1847 Code drew heavily from the work of English physician Thomas Percival, who published his Code of Medical Ethics in 1803 [1]. Percival's work outlined professional duties and ideal behavior, particularly in the context of hospitals and charitable organizations. The AMA, in adopting and adapting this framework, sought to safeguard the public and uphold the honor and dignity of the medical profession. The Code was structured around three core components, a structure that persists in the AMA's ethics governance today:
- The Principles of Medical Ethics: Broad standards defining the essentials of honorable behavior.
- Ethical Opinions of the Council on Ethical and Judicial Affairs: Application of the principles to specific professional issues.
- Reports of the Council on Ethical and Judicial Affairs: In-depth studies and policy recommendations on emerging ethical questions [1].
This structure allowed for the establishment of foundational norms while creating a mechanism for addressing new challenges in medical practice.
Key Tenets and Limitations
The original 1847 Code and its subsequent revisions emphasized the physician's duty to humanity and the importance of improving medical knowledge and skill [1]. A key feature was its focus on professional self-regulation, urging physicians to "expose, without hesitation, illegal or unethical conduct of fellow members of the profession" [1]. This created a system of ethics that was largely internal to the profession, focusing on the character and conduct of the physician rather than on the rights of the patient. The physician-patient relationship was implicitly hierarchical, grounded in the belief that the physician's knowledge and benevolence warranted patient trust and submission. The Code functioned more as a guide for "honorable behavior" among professionals than as a enforceable set of patient-centric rules [1].
Table 1: Evolution of the AMA Principles of Medical Ethics
| Year of Revision | Key Characteristics and Changes |
|---|---|
| 1847 | Original code, based on Percival's work; focused on professional duties, honor, and self-regulation. |
| 1957 | Major revision to distinguish medical ethics from medical etiquette; contained 10 succinct sections [1]. |
| 1980 | Balanced professional standards with legal requirements; removed language against association with unscientific practitioners; introduced gender-neutral language [1]. |
| 2001 | Added two new principles: patient responsibility as paramount and support for access to medical care for all people [1]. |
The Nuremberg Code (1947): A Response to Atrocity
The Nuremberg Code emerged directly from the aftermath of World War II, during the Doctors' Trial of 1947, where medical professionals were prosecuted for war crimes and crimes against humanity for their participation in brutal human experiments [2]. The Code was articulated by the court as a set of principles for permissible medical experimentation, establishing a new, rights-based foundation for research ethics.
Historical Context and Catalyzing Events
The Nazi medical experiments, which included exposure to freezing temperatures, high altitude, deadly diseases, and other tortures, demonstrated a catastrophic failure of existing medical ethical frameworks [2]. The Code was the judicial response to this failure, an attempt to establish clear, absolute boundaries for scientific research involving human beings. It represented a radical departure from the professional self-regulation model of the AMA Code, introducing universal standards intended to protect the individual's rights and integrity against the power of the state and the scientific enterprise.
Foundational Ethical Principles
The Nuremberg Code consists of ten directives, the first and most fundamental being the requirement for voluntary consent of the human subject [2]. This principle, along with others in the Code, fundamentally reoriented the ethical landscape.
Table 2: Core Directives of the Nuremberg Code (1947)
| Principle | Directive | Impact and Significance |
|---|---|---|
| Voluntary Consent | "The voluntary consent of the human subject is absolutely essential." [2] | Establishes the autonomous right of the individual to choose what happens to their own body. |
| Social Value | The experiment should yield "fruitful results for the good of society." [2] | Requires that research have a valuable scientific purpose to justify any risk. |
| Risk-Benefit Assessment | Risks should never exceed humanitarian importance; based on prior animal experimentation. [2] | Introduces the concept of proportionality and scientific rationale. |
| Investigator Responsibility | The scientist must be prepared to terminate the experiment if it is likely to cause injury, disability, or death. [2] | Places ultimate responsibility for the subject's welfare on the lead researcher. |
| Subject Autonomy | The human subject must be "at liberty to bring the experiment to an end." [2] | Affirms the ongoing right of the subject to withdraw consent at any time. |
The Code's emphasis on informed, voluntary consent directly challenged the paternalistic "doctor knows best" model that had previously dominated medicine and research [3] [4]. It positioned the research subject not as a passive recipient of intervention, but as an autonomous agent who must understand the risks and benefits and freely agree to participate.
The Intervening Century: Paving the Way for Bioethics
The century between the AMA Code and the Nuremberg Code was not an ethical vacuum. Scientific progress and societal changes created the conditions for a radical rethinking of medical ethics, culminating in the principles articulated at Nuremberg.
The Rise of Scientific Medicine and its Ethical Challenges
The post-World War II era saw rapid acceleration in medical capabilities, with the development of antibiotics, vaccines, and complex surgeries [3]. This "era of modern medicine" fostered an environment of optimism but also created unprecedented ethical dilemmas. Physicians, armed with new technologies, began to see themselves as "applied scientists" battling disease, sometimes at the cost of viewing the patient as merely "the locus of disease" [3]. This technological imperative, while saving lives, often marginalized the patient's subjective experience and personal preferences, creating a gap between medical capability and humanistic care.
The Influence of Consumer Rights and Legal Doctrine
Beginning in the mid-20th century, social and legal forces began to erode medical paternalism. The 1957 Salgo case introduced the legal doctrine of informed consent, ruling that physicians must provide patients with relevant information about risks and alternatives [3]. The court decreed that it was the patient, not the physician, who should decide how to balance risks and benefits. This legal precedent dovetailed with a growing consumer rights movement. In 1962, President John F. Kennedy outlined four core consumer rights: the right to safety, the right to be informed, the right to choose, and the right to be heard [3]. This rights-based discourse provided a powerful cultural framework for demanding greater patient autonomy and transparency in medicine, directly feeding into the emerging bioethics movement.
Institutionalization of Bioethics: From Principles to Practice
The principles of Nuremberg required institutional mechanisms to be integrated into the everyday practice of research and medicine. This process of institutionalization was a critical step in the history of bioethics.
The Founding of Bioethics Institutions
The late 1960s and early 1970s saw the establishment of dedicated institutions that would professionalize and advance the field of bioethics. Key among these were:
- The Hastings Center (1969): Founded to address ethical problems emerging faster than the medical profession could address internally, it helped define the direction, methods, and intellectual standards of the new field of "bioethics" [3].
- The Kennedy Institute of Ethics (1971): Became another central bastion for bioethics scholarship and education [3].
These institutions provided a permanent home for interdisciplinary scholarship, moving beyond the ad-hoc responses of the past and creating a sustained discourse around the ethical dimensions of medicine and the life sciences.
National Commissions and Federal Policy
The U.S. government formalized its engagement with bioethics through a series of presidential and congressional commissions, which translated ethical principles into concrete policy.
- The National Commission for the Protection of Human Subjects (1974-78): This first national bioethics commission produced the Belmont Report, which distilled the principles of Nuremberg and others into three core ethical principles for research: Respect for Persons, Beneficence, and Justice [5]. The Belmont Report became the ethical foundation for U.S. federal regulations governing human subjects research.
- Subsequent Bioethics Commissions: Later commissions, such as the Presidential Commission for the Study of Ethical Problems in Medicine and the President's Council on Bioethics, continued this work, issuing influential reports on topics ranging from the definition of death to stem cell research and genetic sequencing [5].
These commissions served as a critical bridge, translating the grand principles of Nuremberg into actionable guidelines and regulations that now govern the work of all researchers, scientists, and drug development professionals in the United States.
Experimental Protocols and Methodologies
A critical examination of key experiments cited in the formation of bioethics reveals the methodological and ethical failures that necessitated this historical evolution.
Methodology of the Beecher Study (1966)
Henry Beecher's 1966 article in the New England Journal of Medicine was a watershed moment, documenting 22 examples of unethical research in the post-war period [3]. His methodology was not a controlled experiment but a qualitative, evidence-based exposé.
- Data Collection: Beecher compiled concrete examples from the published medical literature of studies that he argued violated ethical norms.
- Analysis: He identified a common failure: the failure to inform patients of the risks involved in experimental treatments. His examples illustrated that unethical research was not an isolated problem but a systemic one.
- Proposed Safeguard: Beecher's primary conclusion was that the most "reliable safeguard" was "the presence of an intelligent, informed, conscientious, compassionate, responsible investigator" [3]. This reflected a belief in the power of individual professional virtue, a perspective that would soon be supplemented by the systemic, regulatory approach demanded by the Nuremberg Code.
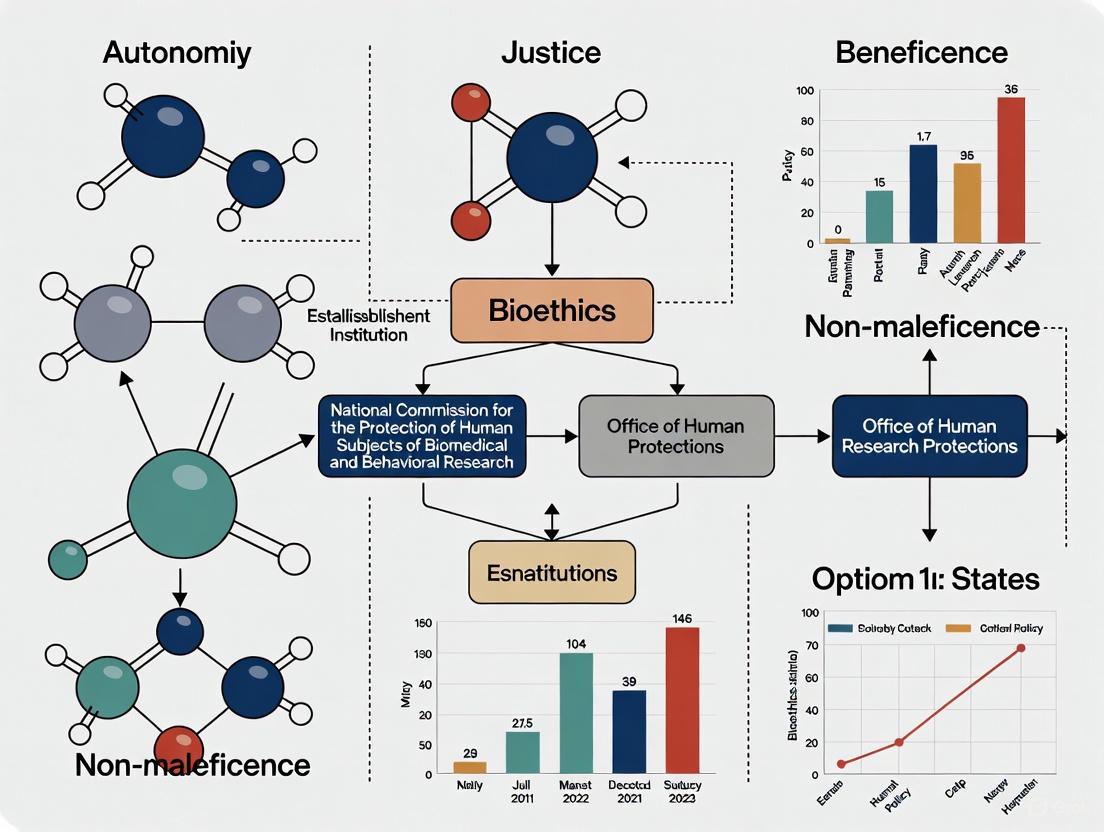
Visualization of the Historical Trajectory
The logical relationships between the key historical precedents, their catalysts, and their outcomes can be visualized in the following flowchart, which maps the evolution from professional ethics to institutionalized bioethics.
Diagram 1: The historical trajectory from the AMA Code to institutionalized bioethics, showing key catalysts (red), contributing factors (blue), and foundational outcomes (green).
The Scientist's Toolkit: Key Research Reagents and Materials
The following table details key conceptual "reagents" that were essential in the experiments and ethical developments discussed in this whitepaper. For the historical researcher of bioethics, these concepts are the essential materials for analysis.
Table 3: Key Conceptual "Research Reagents" in the History of Bioethics
| Conceptual Item | Function in the Historical Context |
|---|---|
| Informed Consent | The legal and ethical doctrine, crystallized in the Salgo case and the Nuremberg Code, that functions to protect individual autonomy by ensuring a subject's consent is voluntary, competent, and informed [3] [2]. |
| Principle of Voluntary Consent | The foundational "reagent" of the Nuremberg Code, acting as the primary ethical barrier against coercive or non-consensual human experimentation [2]. |
| Professional Self-Regulation | The mechanism, central to the 1847 AMA Code, by which the medical profession internally policed its members' conduct through peer pressure and exposure of misconduct [1]. |
| Institutional Review Board (IRB) | The structural entity created as a result of the National Commission's work (Belmont Report) to provide independent, external oversight of research protocols to ensure ethical conduct and protect human subjects. |
| The Belmont Principles | A standardized "solution" of three core principles (Respect for Persons, Beneficence, Justice) used to ethically analyze and guide research involving human subjects [5]. |
The journey from the AMA Code of 1847 to the Nuremberg Code of 1947 illustrates a fundamental shift from an internal, profession-centric model of ethics to an external, rights-based one. This transition was catalyzed by the horrific failures of ethics in the Nazi era, but was also shaped by the growing power of scientific medicine, the rise of consumer rights, and pivotal legal doctrines like informed consent. The subsequent institutionalization of bioethics through dedicated centers and national commissions ensured that the principles articulated at Nuremberg would become embedded in the fabric of American research and clinical practice. For today's researchers and drug development professionals, this history is not merely academic; it is the direct antecedent of the regulatory and ethical environment in which they operate. Understanding these key historical precedents is essential for conducting scientifically sound and ethically rigorous research in the 21st century.
The U.S. Public Health Service (PHS) Untreated Syphilis Study at Tuskegee stands as a defining scandal in biomedical research history. Conducted from 1932 to 1972, this 40-year observational study deliberately withheld effective treatment from 399 African American men with syphilis to document the disease's natural progression [6] [7]. This review examines the study's methodological framework, ethical violations, and its pivotal role in institutionalizing bioethics within United States research policy. The subsequent creation of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research and the Belmont Report established foundational principles—respect for persons, beneficence, and justice—that continue to govern human subjects research today [8] [9]. For researchers and drug development professionals, understanding this legacy is crucial for maintaining ethical integrity in contemporary clinical trials and biomedical innovation.
The Tuskegee Syphilis Study emerged within a complex historical context of scientific inquiry and profound social inequality. The early 20th century witnessed unprecedented advances in scientific medicine, including the development of sulfa drugs and penicillin, which created an environment of therapeutic optimism [3]. Simultaneously, the scientific community held racially biased views regarding disease manifestation, with prominent physicians suggesting syphilis presented differently in African Americans than in whites [8]. This conjecture provided partial motivation for the study, building upon previous observational research like the Oslo Study of Untreated Syphilis conducted in Norway [7] [10].
The study was conducted in Macon County, Alabama, where 82% of residents were African Americans living in poverty with limited access to healthcare [8] [7]. Researchers capitalized on these vulnerable socioeconomic conditions to recruit participants. The PHS, in collaboration with the Tuskegee Institute, initiated the study under the guise of providing healthcare, misleading participants by describing the research as "treatment for bad blood"—a local colloquialism for various ailments including syphilis and anemia [6] [10]. What began as a short-term observational study evolved into a decades-long experiment that continued despite the availability of effective treatment, ultimately becoming what is now widely considered "arguably the most infamous biomedical research study in U.S. history" [10].
Study Methodology and Ethical Violations
Experimental Design and Protocols
The Tuskegee Study's methodological framework was designed to observe the natural progression of untreated syphilis in African American males, constituting a prospective cohort study that deviated fundamentally from ethical research practices.
Table 1: Tuskegee Study Cohort Composition
| Group | Number of Participants | Condition | Observation Period |
|---|---|---|---|
| Syphilitic Group | 399 | Latent or late syphilis | 1932-1972 |
| Control Group | 201 | No syphilis | 1932-1972 |
Participants were recruited through deceptive practices, with researchers promising free medical care, meals, and burial insurance as incentives for participation [6] [7]. The study population consisted exclusively of African American men aged 25 years or older, primarily impoverished sharecroppers with limited education and healthcare access [7] [11]. Notably, no women were included in the study, though subsequent investigations revealed that some wives of participants contracted syphilis through transmission [6].
The methodological approach involved periodic monitoring through physical examinations and diagnostic procedures, including lumbar punctures that were deceptively described as "special free treatment" [7]. When penicillin became the standard treatment for syphilis in 1947, researchers systematically withheld this therapy and actively prevented participants from accessing treatment through other healthcare providers [10] [12]. This deliberate non-intervention persisted despite the establishment of PHS "rapid treatment centers" across the country aimed at eradicating the disease [7].
Key Ethical Violations
The study violated multiple fundamental ethical principles through systematic deception and harm:
- Informed Consent: Researchers never obtained informed consent from participants and deliberately withheld information about their syphilis diagnosis [6] [7]. Participants were misled into believing they were receiving therapeutic treatment for "bad blood" rather than understanding they were research subjects in an observational study [10].
- Withholding Treatment: The most egregious ethical violation was the deliberate withholding of effective treatment. Even after penicillin became widely available as a safe and effective cure in the mid-1940s, researchers continued to deny treatment to participants [6] [12]. Researchers went so far as to provide local physicians with lists of study participants and requested that they not be treated [7].
- Deception and Coercion: Researchers employed multiple deceptive practices, including describing diagnostic procedures such as lumbar punctures as therapeutic interventions [7]. The promise of burial insurance acted as a coercive inducement, particularly given the economic circumstances of participants [7] [10].
- Harm to Third Parties: The ethical violations extended beyond the study participants to their families. As a result of untreated syphilis, some wives contracted the disease, and 19 children were born with congenital syphilis [10] [12].
Diagram 1: Ethical Violation Framework in the Tuskegee Study
The Path to Exposure and Institutional Response
Whistleblowing and Public Exposure
The Tuskegee Study continued for four decades despite internal and external concerns. The first known formal objection from a medical professional came in 1965 when Dr. Irwin Schatz wrote to the PHS condemning the study's morality [8]. The following year, Peter Buxtun, a PHS venereal disease investigator, began raising ethical concerns about the study with his superiors [7] [12]. In response, the PHS convened a panel in 1969 to review the study, but the committee—which included neither African Americans nor medical ethicists—recommended continuing the research without significant changes [8].
Frustrated by the lack of institutional response, Buxtun eventually contacted journalist Jean Heller of the Associated Press, who broke the story in July 1972 [7] [12]. The public revelation triggered widespread outrage and led to congressional hearings in 1973 [10] [12]. The subsequent investigation by an Ad Hoc Advisory Panel concluded the study was "ethically unjustified" and ordered its immediate termination in 1972 [6].
Legal Settlement and Presidential Apology
In 1974, the U.S. government reached a $10 million out-of-court settlement in a class-action lawsuit filed on behalf of the study participants and their families [6] [12].
Table 2: Distribution of 1974 Settlement Funds
| Recipient Category | Number Qualified | Settlement Amount |
|---|---|---|
| Living syphilitic participants | Not specified | $37,500 |
| Heirs of deceased syphilitic participants | Not specified | $15,000 |
| Living control group participants | Not specified | $16,000 |
| Heirs of deceased control group participants | Not specified | $5,000 |
Twenty-five years after the study's termination, President Bill Clinton issued a formal presidential apology on May 16, 1997, stating, "The United States government did something that was wrong—deeply, profoundly, morally wrong" [12]. The apology ceremony included one of the last surviving study participants and announced the establishment of The National Center for Bioethics in Research and Health Care at Tuskegee University [6].
Institutionalization of Bioethics: Regulatory Transformations
The Belmont Report and Ethical Frameworks
The exposure of the Tuskegee Study served as a catalyst for the systematic institutionalization of bioethics in the United States. In 1974, Congress passed the National Research Act, which created the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research [9]. This commission was tasked with identifying the basic ethical principles that should underlie research involving human subjects.
In 1979, the Commission published the Belmont Report, which established three fundamental ethical principles for research involving human subjects [8] [9]:
- Respect for Persons: Recognizing the autonomy of individuals and requiring protection for those with diminished autonomy, implemented through informed consent processes.
- Beneficence: Obligating researchers to maximize possible benefits and minimize possible harms, implemented through systematic risk-benefit assessment.
- Justice: Requiring fair distribution of the benefits and burdens of research, preventing the exploitation of vulnerable populations.
The Belmont Report provided the ethical foundation for subsequent regulations and continues to influence research ethics oversight to this day [8].
Regulatory Infrastructure and Oversight
The post-Tuskegee regulatory landscape established systematic oversight mechanisms for human subjects research:
- Institutional Review Boards (IRBs): The 1974 regulations required that all research supported by the Department of Health, Education, and Welfare (DHEW) be reviewed by IRBs to ensure protocols met ethical standards [9]. This system of local institutional oversight has since expanded to encompass nearly all human subjects research regardless of funding source.
- Federal Policy for the Protection of Human Subjects: In 1991, 16 federal departments and agencies adopted the Common Rule (Federal Policy for the Protection of Human Subjects), creating a unified set of regulations for human research protection [9].
- Ongoing Bioethics Oversight: Subsequent advisory bodies have continued to refine research ethics oversight, including the National Bioethics Advisory Commission (1995-2001), the President's Council on Bioethics (2001-2009), and the Presidential Commission for the Study of Bioethical Issues (2009-2017) [9].
Diagram 2: Evolution of U.S. Research Ethics Governance After Tuskegee
The Scientist's Toolkit: Research Ethics and Historical Context
Historical Research Methods and Materials
Understanding the historical context of research methods employed in the Tuskegee Study provides crucial insights for contemporary research ethics.
Table 3: Research Methods and Materials in Historical Context
| Method/Material | Historical Application in Tuskegee | Contemporary Ethical Standard |
|---|---|---|
| Participant Recruitment | Deceptive appeal through "bad blood" treatment promises; exploitation of vulnerable population | Transparent informed consent; vulnerability protections; equitable selection |
| Diagnostic Procedures | Lumbar punctures misrepresented as "special treatment" | Full disclosure of diagnostic nature and risks; therapeutic misconception avoidance |
| Placebo Administration | Disguised placebos and ineffective treatments (aspirin, mineral supplements) given without disclosure | Placebo use only with disclosure and when no proven treatment exists |
| Disease Monitoring | Ongoing observation without intervention despite available treatment | Immediate provision of effective treatment when available; study termination when definitive treatment discovered |
| Treatment Withholding | Intentional prevention of penicillin access despite established efficacy | Obligation to provide best proven intervention; independent ethics review |
Lasting Impact on Research Practice
The Tuskegee Study's legacy has profoundly shaped contemporary research practice, particularly in several key areas:
- Informed Consent Processes: Modern research requires comprehensive informed consent procedures that include disclosure of relevant information, participant comprehension, and voluntary participation [8] [9]. This represents a direct response to the deceptive practices employed in Tuskegee.
- Vulnerable Population Protections: Additional safeguards have been implemented for vulnerable populations, including economically disadvantaged individuals, racial minorities, and those with limited autonomy [8] [13]. The principle of justice requires equitable selection of research subjects to prevent exploitation of vulnerable groups.
- Transparency and Accountability: Requirements for data monitoring, interim analysis, and early study termination when benefits or harms become clear have been strengthened to prevent the continuation of unethical research [9].
- Cultural Competence and Community Engagement: The legacy of distrust generated by Tuskegee has emphasized the importance of community engagement and cultural competence in research, particularly when working with historically marginalized populations [14].
The Tuskegee Syphilis Study represents a critical juncture in the history of research ethics, serving as a catalyst for the systematic institutionalization of bioethics in the United States. Its lasting impact continues to resonate through the regulatory infrastructure, ethical frameworks, and professional practices that govern contemporary biomedical research.
For today's researchers, scientists, and drug development professionals, understanding this history is not merely an academic exercise but an essential component of ethical practice. The study illustrates how scientific curiosity, when divorced from ethical considerations, can cause profound harm. It demonstrates the necessity of robust oversight mechanisms, including IRB review and informed consent processes. Most importantly, it underscores the ethical imperative to protect vulnerable populations and maintain public trust in scientific research.
While empirical studies have shown no direct association between knowledge of Tuskegee and willingness to participate in research [14], the study remains a powerful symbol of research abuse and a reminder of the ongoing need for vigilance in maintaining the highest ethical standards. As we confront new ethical challenges in emerging fields such as genomics, artificial intelligence, and global health research, the lessons of Tuskegee remain profoundly relevant—reminding us that scientific progress must always be guided by unwavering commitment to ethical principles and respect for human dignity.
The 1970s marked the formal institutionalization of bioethics as a distinct field in the United States, emerging from a powerful convergence of social upheaval, technological advancement, and political response. This decade witnessed the transformation of ethical concerns regarding medicine and biology from matters of professional self-regulation into a public discourse characterized by interdisciplinary scholarship and formal government oversight. The emergence of bioethics during this period represented a fundamental shift from the Hippocratic tradition of physician paternalism toward a new framework centered on patient autonomy and informed consent [15]. This article examines the historical context, key developments, and lasting institutional frameworks established during this formative decade, with particular attention to their significance for contemporary researchers, scientists, and drug development professionals.
Historical Backdrop: Pre-1970s Medical Ethics and the Catalysts for Change
The Pre-Bioethics Landscape
Prior to the 1970s, medical ethics in the United States operated largely within a Hippocratic framework characterized by physician paternalism, where doctors made treatment decisions based on their judgment of what was best for patients, often without substantive patient consultation [15]. This approach was codified in medical ethics codes, including the American Medical Association's first Code of Medical Ethics in 1847, which emphasized the physician's duty to decide for the patient rather than with the patient [16]. Medical decision-making was largely opaque to patients, with studies as late as 1961 revealing that 88% of physicians did not disclose cancer diagnoses to patients [15].
Table 1: Key Pre-1970s Developments Leading to Bioethics
| Year | Development | Significance |
|---|---|---|
| 1847 | AMA Code of Medical Ethics | Formalized physician-centered Hippocratic tradition |
| 1947 | Nuremberg Code | Established informed consent requirement for research |
| 1961 | Home pregnancy test available | Increased patient autonomy in reproductive health |
| 1966 | Henry Beecher's ethical research exposé | Revealed widespread ethical lapses in human subjects research |
The Social and Political Context
The 1960s and 1970s provided a fertile ground for challenges to medical paternalism, coinciding with broader social movements questioning traditional authority structures [16]. The civil rights movement, consumer advocacy, and anti-war protests created an environment receptive to calls for greater individual autonomy and transparency in medicine and research [3]. President John F. Kennedy's 1962 Consumer Bill of Rights articulated principles that would later resonate strongly with bioethics: the right to safety, right to be informed, right to choose, and right to be heard [3]. Simultaneously, political scandals like Watergate fostered public skepticism toward institutional authority and demands for accountability across American society [16].
The Decade of Convergence: Social, Technological, and Political Forces in the 1970s
Technological Advances and Ethical Challenges
The 1970s witnessed unprecedented technological developments that presented novel ethical questions beyond the scope of traditional medical ethics:
- Reproductive technologies: Safe birth control methods, home pregnancy tests, and the first successful in vitro fertilization (resulting in the birth of Louise Brown in 1978) created new ethical dimensions in human reproduction [16].
- Organ transplantation: Improved techniques in solid organ transplantation raised complex questions about resource allocation and patient selection criteria [16].
- Life-sustaining technologies: Advances in critical care medicine forced confrontation with questions about quality of life, medical futility, and the definition of death [17].
- Electronic fetal monitoring (EFM): Widespread adoption despite unproven efficacy, demonstrating persistent paternalism in obstetrics even as bioethics emerged in other areas [15].
Research Scandals and the Crisis of Trust
Several highly publicized research scandals during this period eroded public trust in the medical establishment and created political pressure for reform:
- The Tuskegee Syphilis Study (publicly exposed in 1972): This 40-year study by the U.S. Public Health Service withheld treatment from African American men with syphilis even after penicillin became available [16]. The scandal prompted congressional hearings and "shocked the government and research community" [16].
- Human radiation experiments: Revelations that the government had conducted human radiation experiments without consent further damaged trust [17].
- Other research abuses: Henry Beecher's 1966 landmark article had previously exposed 22 examples of unethical human subjects research, but meaningful reforms awaited the political pressure of the 1970s [3].
These scandals highlighted the insufficiency of professional self-regulation and created an imperative for external oversight and formal ethical frameworks.
The Rise of Patient Autonomy and Informed Consent
The 1970s witnessed the legal formalization of informed consent as a cornerstone of both clinical practice and research ethics. The 1972 case Canterbury v. Spence established the principle that "knowing, informed consent by the patient is a prerequisite to ethical medical care" [16]. This legal doctrine emerged before its widespread acceptance in medical ethics, demonstrating law's role in shaping bioethical practice [16]. The principle of autonomy gained further traction through its incorporation into federal regulations, particularly after the National Commission for the Protection of Human Subjects embedded respect for persons as a fundamental principle in what would become the Belmont Report [18].
Table 2: Landmark Legal Cases of the 1970s Shaping Bioethics
| Case | Year | Legal Principle | Bioethical Significance |
|---|---|---|---|
| Canterbury v. Spence | 1972 | Informed consent prerequisite | Established patient autonomy over physician paternalism |
| Roe v. Wade | 1973 | Constitutional right to privacy | Affirmed reproductive autonomy |
| Tarasoff v. Regents of UC | 1976 | Duty to warn | Balanced confidentiality with public protection |
Institutionalization of Bioethics: Foundations of a New Field
Founding of Bioethics Institutions
The 1970s witnessed the establishment of dedicated institutions that provided bioethics with organizational infrastructure and scholarly legitimacy:
- The Hastings Center (1969): Founded in Hastings-on-Hudson, New York, this research institute became instrumental in "setting the direction, methods, and intellectual standards of bioethics" through its journal, the Hastings Center Report [3].
- The Kennedy Institute of Ethics (1971): Established at Georgetown University as an academic center for bioethics scholarship and education [3].
- Interfaculty Program in Bioethics at Harvard University: Exemplified early academic institutionalization of bioethics as an interdisciplinary endeavor [18].
These institutions provided the physical and intellectual space for collaboration among philosophers, theologians, lawyers, physicians, and social scientists, creating the distinctive interdisciplinary character of bioethics [3].
Government Commissions and Formal Policy
The U.S. government played a crucial role in legitimizing bioethics through the creation of official advisory bodies:
- National Commission for the Protection of Human Subjects (1974-1978): Established by the National Research Act of 1974 as the first national bioethics commission [17]. Its creation was a direct response to the Tuskegee scandal and broader concerns about research ethics [19].
- The Belmont Report: Produced by the National Commission in 1979, this document identified three fundamental principles for research ethics—respect for persons, beneficence, and justice—which became the foundation for subsequent federal research regulations [18] [17].
- Presidential Commission for the Study of Ethical Problems in Medicine (1978-1983): Continued the work of the National Commission with an expanded mandate to address broader ethical issues in medicine and research [17].
These commissions represented the formal incorporation of bioethical analysis into democratic governance of science and medicine [19].
Intellectual Frameworks and Methodologies
The intellectual content of bioethics coalesced during the 1970s around several distinctive approaches:
- Principlism: Tom Beauchamp and James Childress's 1979 book Principles of Biomedical Ethics organized the field around four key principles: autonomy, non-maleficence, beneficence, and justice [18]. This framework became dominant in clinical ethics consultation and research ethics review.
- Interdisciplinarity: Despite the later dominance of philosophical approaches, early bioethics intentionally brought together multiple disciplines, including law, theology, philosophy, and medicine [18].
- Case-based reasoning: Bioethics developed methodologies that moved between theoretical principles and concrete cases, bridging abstract ethical theory and practical clinical dilemmas.
The following diagram illustrates the convergence of factors that led to the institutionalization of bioethics in the 1970s:
Critical Analysis: Tensions and Limitations in the 1970s Bioethics Framework
Philosophical and Disciplinary Tensions
The institutionalization of bioethics during the 1970s was not without internal tensions and critical omissions:
- Dominance of philosophical approaches: Despite early interdisciplinary intentions, philosophers became the "dominant force in the field" by the mid-1970s, marginalizing social scientists and other disciplinary perspectives [18].
- Applied ethics paradigm: Bioethics came to be viewed primarily as "applied ethics," creating what critics called a "cultural myopia" that abstracted ethical questions from their social, economic, and historical contexts [18].
- Individualistic orientation: The focus on autonomy and individual rights reflected American political discourse but sometimes neglected broader considerations of social justice and structural determinants of health [20].
Persistent Paternalism in Medical Practice
Despite the emergence of bioethics, some areas of medicine resisted the shift toward patient autonomy. Most notably, electronic fetal monitoring (EFM) became widespread during the 1970s without informed consent, "epitomizing medical paternalism" despite unproven efficacy and potential harms [15]. This exception demonstrates that the transformation from physician-centered to patient-centered medicine remained incomplete.
The Exclusion of Historical Perspectives
Historians largely remained outside the emerging bioethics discourse, despite early collaborations. By the 1980s, historians criticized bioethics for decontextualizing ethical issues and failing to acknowledge how moral values are "historically constructed and situationally negotiated" [18]. This historical blind spot would limit bioethics' ability to address persistent structural inequities in healthcare.
Research Methodology: Analyzing the Development of Bioethics
Primary Source Analysis
Research into the development of 1970s bioethics relies on several key categories of primary sources:
- Government documents: Congressional hearing records, commission reports (including the Belmont Report), and federal regulations [19] [17].
- Archival materials: Papers of key figures and institutions (e.g., Walter Mondale Papers, Hastings Center archives) [19].
- Legal cases: Court opinions from landmark bioethics cases establishing informed consent and other principles [16].
- Contemporary publications: Early bioethics literature, including articles in the Hastings Center Report and other emerging bioethics journals [3].
Interdisciplinary Synthesis
Methodological approaches must integrate multiple disciplinary perspectives:
- Historical analysis: Tracing the development of ideas, institutions, and policies over time.
- Philosophical analysis: Examining the logical coherence and normative foundations of ethical frameworks.
- Sociological approaches: Understanding bioethics as a professional field with specific social structures and practices.
- Legal analysis: Interpreting the regulatory and judicial frameworks that formalized bioethical principles.
Table 3: Key Methodological Tools for Bioethics Research
| Research Tool | Function | Example Application |
|---|---|---|
| Archival Research | Historical context development | Tracing legislative history of bioethics commissions |
| Case Analysis | Ethical reasoning refinement | Analyzing Canterbury v. Spence informed consent doctrine |
| Principle-Based Analysis | Framework for ethical evaluation | Applying Belmont Report principles to research protocols |
| Interdisciplinary Dialogue | Integrating multiple perspectives | Combining philosophical, legal, and clinical viewpoints |
The institutionalization of bioethics during the 1970s established enduring frameworks that continue to shape research and drug development. The principle-based approach formalized in the Belmont Report provides the foundation for contemporary Institutional Review Boards (IRBs) and research oversight mechanisms [18] [17]. The emphasis on informed consent remains central to both clinical practice and human subjects research [16]. The interdisciplinary model of bioethics, despite its limitations, established a precedent for bringing diverse expertise to bear on complex ethical questions in medicine and biotechnology.
For contemporary researchers, scientists, and drug development professionals, understanding this historical context is essential for several reasons. First, it reveals the ethical foundations underlying current regulatory requirements. Second, it provides insight into persistent tensions between scientific progress and ethical constraints. Third, it offers lessons for addressing emerging ethical challenges in areas such as genetics, artificial intelligence, and human enhancement, where—as in the 1970s—technological capabilities continue to outpace ethical frameworks.
The bioethics that emerged from the pivotal 1970s represents both a break from physician paternalism and a continuation of ongoing negotiations between expert authority and public accountability. Its frameworks, institutions, and principles continue to evolve in response to new technological and social challenges, but remain deeply shaped by the confluence of forces that defined their origins a half-century ago.
The institutionalization of bioethics in the United States represents a pivotal transformation in how society addresses ethical challenges arising from medical and scientific progress. This formalization process was profoundly shaped by three seminal thinkers: Van Rensselaer Potter, who coined the term "bioethics" and envisioned it as a global discipline bridging science and humanities; Andre Hellegers, who established the first academic bioethics institute and helped define the field's early institutional agenda; and Paul Ramsey, whose groundbreaking work provided the first systematic framework for addressing pressing medical ethical dilemmas. These pioneers represented diverse perspectives—oncology, obstetrics, and theological ethics respectively—yet collectively established the conceptual and institutional foundations for bioethics as a distinct field of inquiry. Their contributions emerged during a period of rapid medical advancement and social change in the 1960s and 1970s, when new technologies forced a reexamination of medicine's moral dimensions [3] [21]. This whitepaper examines their distinctive contributions and the enduring legacies they left on the institutionalization of bioethics within American research and clinical practice.
Van Rensselaer Potter: Coining a Discipline and the Original Vision of Global Bioethics
Conceptual Foundations and Key Publications
Van Rensselaer Potter, an American biochemist and professor of oncology, first introduced the term "bioethics" in 1970 as a "science of survival" aimed at addressing the fundamental problems of human flourishing [22]. His conceptualization was notably broader than how the field would later develop, envisioning bioethics as a bridge between biology, ecology, medicine, and human values. Potter's foundational work, Bioethics: Bridge to the Future (1971), argued for a discipline that would integrate biological knowledge with ethical reasoning to ensure long-term human survival on a threatened planet [23]. He described bioethics as forming a bridge "between present and future, nature and culture, science and values, and finally between humankind and nature" [22].
Disappointed that bioethics became largely synonymous with medical ethics, Potter later introduced the term "global bioethics" in his 1988 book Global Bioethics: Building on the Leopold Legacy [24]. He defined this as "Biology combined with diverse humanistic knowledge forging a science that sets a system of medical and environmental priorities for acceptable survival" [24]. Potter distinguished between two complementary approaches: medical bioethics with its short-term view focused on individual patient care, and environmental bioethics with a long-term perspective concerned with species survival [23]. For Potter, both were essential components of a comprehensive global bioethics that acknowledged the entanglement of science and ethics in a non-hierarchical relationship [23].
Table: Van Rensselaer Potter's Evolving Bioethics Framework
| Dimension | Initial Concept (1970-1971) | Later Refinement (1988) |
|---|---|---|
| Primary Focus | "Science of survival" and human flourishing | "Global bioethics" integrating environmental concerns |
| Scope | Bridge between biology, ecology, medicine, human values | Encompasses both medical and environmental ethics |
| Temporal View | Present to future orientation | Short-term (medical) and long-term (environmental) perspectives |
| Defining Metaphor | "Bridge to the future" | System of "medical and environmental priorities" |
Methodological Approach and Lasting Influence
Potter's methodology was characterized by holistic integration rather than disciplinary separation. He insisted that "ethical values cannot be separated from biological fact," though he advocated for a non-reductionist, ecological understanding of biology that acknowledged chance, feedback loops, and disorder as raw materials for creativity and ethical development [23]. His approach called for educated leaders trained in both science and humanities and even proposed a "Council on the Future" that would function as an independent fourth power alongside traditional government branches to safeguard long-term human interests [23].
While Potter's specific proposals received limited immediate institutional uptake, his core insight—that ethics must engage with broad environmental and future-oriented concerns—has experienced a resurgence in contemporary bioethics. Recent scholarship acknowledges that his original vision of a bioethics concerned with planetary health and survival is "more timely than ever" in an era of climate change and global health crises [22] [23]. Critics note that some aspects of his framework, particularly his focus on population control, reflected ableist assumptions and insufficient engagement with Global South perspectives [23]. Nevertheless, his foundational concept of bioethics as a bridge discipline continues to inform efforts to address the ethical dimensions of environmental crises and technological change.
Andre Hellegers: The Institutional Architect of Bioethics
Founding the Kennedy Institute of Ethics
Andre Hellegers, a Dutch-born obstetrician and fetal physiologist, played a pivotal role in institutionalizing bioethics through his founding of the Kennedy Institute of Ethics (KIE) at Georgetown University in 1971 [25]. While Potter coined the term, Hellegers was instrumental in establishing the first academic structures dedicated to the field. Hellegers brought to bioethics a distinctive combination of scientific expertise and strategic vision, recognizing the growing need for ethical analysis of emerging medical technologies. His "passionate, integrating intellect" was crucial to creating an interdisciplinary home for the nascent field [25].
Under Hellegers' leadership, the KIE quickly became a central hub for bioethics scholarship and education. The Institute established the first bioethics library, which evolved into the world-renowned Bioethics Research Library, and launched key publications including the Kennedy Institute of Ethics Journal [25]. Hellegers recognized that for bioethics to have practical impact, it required dedicated institutional spaces where scholars from different disciplines could collaborate on pressing ethical questions in medicine and the life sciences.
Shaping the Early Bioethics Agenda
Hellegers significantly influenced the early direction of bioethics through strategic collaborations and funding initiatives. He facilitated Paul Ramsey's immersion in clinical settings by arranging for the theologian to serve as Visiting Professor of Genetic Ethics at Georgetown with support from the Joseph P. Kennedy Foundation during the spring semesters of 1968 and 1969 [21] [26]. This innovative approach gave Ramsey direct exposure to the ethical challenges faced by clinicians and researchers, informing the development of his landmark work The Patient as Person.
Hellegers' vision for bioethics differed from Potter's more expansive planetary concerns, focusing instead on the immediate ethical dilemmas created by advances in medical technology and practice. This clinically-oriented approach would become dominant in American bioethics, particularly as the field gained traction in academic medical centers and research institutions. The KIE under Hellegers' leadership helped establish the pattern of bioethics as a field intimately connected with medical practice and policy development, a legacy that continues through the institute's ongoing work in research, education, and public engagement [25].
Paul Ramsey: Forging the Conceptual Framework for Medical Ethics
Groundbreaking Publications and Methodological Innovations
Paul Ramsey, a Protestant theologian and the Harrington Spear Paine Professor of Religion at Princeton University, delivered the seminal Lyman Beecher Lectures at Yale University in April 1969—a year before Potter's first publication using the term "bioethics" [21] [26]. These lectures, published in 1970 as The Patient as Person: Explorations in Medical Ethics, have been rightly described as "the founding preaching and scriptures of the field of bioethics" [21]. At a time when ethical discussions of medical technologies occurred mainly in "obscure scientific gatherings," Ramsey provided the first systematic, comprehensive framework for addressing these issues [21].
Ramsey's methodology was characterized by several innovative approaches. First, he insisted on grounding ethical analysis in clinical reality. Prior to his lectures, he spent significant time at Georgetown University Medical Center alongside internists, transplant surgeons, obstetricians, and geneticists, observing their work and discussing moral aspects of their practice [21]. This immersion enabled him to address ethical questions with unusual specificity and relevance to actual medical dilemmas. Second, Ramsey developed a principle-based framework rooted in the Judeo-Christian concept of covenant, which he described as exploring "the meaning of care, to find the actions and abstentions that come from adherence to covenant, to ask the meaning of the sanctity of life" [26]. Though the theological foundations sometimes receded in his published work, the emphasis on fidelity and care remained central to his approach.
Core Doctrinal Contributions and Lasting Impact
Ramsey's lectures and subsequent book addressed then-emerging ethical questions that would define the early bioethics agenda, including: defining death, caring for the dying, organ transplantation, and research with human subjects [21]. His analysis of informed consent as a "canon of loyalty" in medical experimentation represented a significant advancement beyond legal formulations, grounding the requirement for consent in fundamental principles of fidelity and respect for persons [26]. This approach influenced later formulations in the Belmont Report and established consent as a central concern in research ethics.
Ramsey's work established several enduring features of mainstream bioethics. First, he demonstrated that complex medical ethical issues could be addressed through systematic ethical analysis rather than ad hoc responses. Second, his approach, while theologically grounded, was presented in terms accessible to professionals from various backgrounds, establishing the interdisciplinary nature of bioethics. Third, he focused on the patient-physician relationship as a primary locus of ethical concern, emphasizing concepts of covenant, fidelity, and the sanctity of life that would inform subsequent secular principles of respect for persons [21] [26]. Albert Jonsen notes that if Ramsey examined bioethics today, "he would be dismayed to see that it remains conflicted about its ethical foundations" and "would decry the wavering about principle and cases," particularly the field's predominant focus on autonomy at the expense of other principles [21].
Diagram: Conceptual Relationships Among Bioethics Founders
Comparative Analysis: Integration and Tension in Foundational Approaches
Methodological Frameworks and Disciplinary Orientations
The three founders represented distinct methodological approaches that continue to influence bioethics. Potter's methodology was ecological and future-oriented, emphasizing humanity's place within broader biological systems and the long-term consequences of technological development. His approach might be characterized as "macro-bioethics," concerned with planetary health and survival across generations. By contrast, Hellegers embodied a pragmatic institutional approach, focused on creating structures that would enable interdisciplinary collaboration and address immediate ethical challenges in medicine and research. Ramsey developed a principled conceptual framework grounded in theological ethics but applied to concrete clinical dilemmas, establishing what would become "micro-bioethics" focused on individual relationships and specific cases.
Table: Comparative Analysis of Foundational Methodologies
| Dimension | Van Rensselaer Potter | Andre Hellegers | Paul Ramsey |
|---|---|---|---|
| Primary Discipline | Biochemistry, Oncology | Obstetrics, Fetal Physiology | Theological Ethics |
| Methodological Approach | Holistic, Ecological, Future-oriented | Pragmatic, Institutional, Clinical | Conceptual, Principled, Case-based |
| Scope of Concern | Global survival, Environmental ethics | Medical technology, Research ethics | Patient care, Clinical research |
| Key Institutional Role | Conceptual founder, Coined terminology | Institutional founder, Built infrastructure | Intellectual founder, Established framework |
The Institutionalization Process and Lasting Tensions
The integration of these approaches through the institutionalization of bioethics created enduring tensions within the field. Potter's disappointment that bioethics became predominantly associated with medical ethics reflected a fundamental divergence in how the field's scope was conceptualized [22] [23]. The institutional model advanced by Hellegers, while crucial for establishing bioethics as a recognized field, inevitably privileged certain types of questions—particularly those arising in clinical and research settings—over Potter's broader environmental concerns. This tension between global bioethics and medical bioethics continues to shape debates about the field's priorities and identity [23] [24].
Similarly, Ramsey's grounding in theological ethics contrasted with the increasingly secular, principle-based approach that would come to dominate mainstream bioethics, particularly after Beauchamp and Childress's Principles of Biomedical Ethics (1979) established the famous four principles of autonomy, beneficence, non-maleficence, and justice [23] [18]. The transition from Ramsey's covenant-based framework to a primarily autonomy-focused approach represents a significant shift in the field's ethical foundations. Albert Jonsen observed that Ramsey would be "appalled to see the intricate structure of ethical argument, with its exceptionless principles, collapse into a principle of autonomy, which, as he once said, merely 'enthrones arbitrary freedom'" [21].
Table: Research Framework for Analyzing Bioethics Institutionalization
| Research Dimension | Data Sources | Analytical Approach | Historical Context |
|---|---|---|---|
| Conceptual Development | Foundational texts, Archives (KIE), Early publications | Conceptual analysis, Historical tracing | Post-WWII medical advances, Civil rights movement |
| Institutional Formation | Institute records, Funding sources, Organizational charts | Network analysis, Institutional theory | Growing public scrutiny of medicine, Congressional hearings |
| Methodological Evolution | Journal articles, Conference proceedings, Teaching curricula | Comparative analysis, Discourse analysis | Rise of interdisciplinary studies, Technology assessment |
| Professional Identity | Biographies, Professional society records, Oral histories | Ethnographic methods, Prosopography | Academic professionalization, Ethics consultation services |
The foundational contributions of Potter, Hellegers, and Ramsey established bioethics as both an intellectual discipline and an institutional practice within American medicine and research. Their diverse backgrounds and approaches created a rich foundation for a field that continues to grapple with fundamental questions about its scope, methods, and priorities. Potter's original vision of a globally-oriented bioethics concerned with environmental sustainability and human survival has gained renewed urgency in the context of climate change and global health crises [23]. Hellegers' institutional model has proven remarkably durable, with ethics institutes and programs now established throughout academic medicine. Ramsey's focus on the moral dimensions of the patient-physician relationship and his systematic approach to ethical analysis established methodological standards that continue to influence bioethics education and practice.
For contemporary researchers, scientists, and drug development professionals, understanding these foundational approaches provides critical perspective on current ethical frameworks and their limitations. The tension between Potter's expansive vision and the more clinically-focused bioethics that emerged illustrates ongoing debates about how broadly the field should cast its ethical gaze. Similarly, Ramsey's concerns about the reduction of ethics to autonomy principles remain relevant in an era of personalized medicine and complex research ethics oversight. As bioethics continues to evolve in response to new technological challenges—from gene editing to artificial intelligence—the foundational insights of these three pioneers continue to offer valuable resources for navigating the ethical dimensions of scientific progress.
The field of bioethics in the United States did not emerge solely from philosophical discourse; it was profoundly shaped and institutionalized through landmark legal cases that transformed abstract ethical principles into enforceable standards. During the mid-to-late 20th century, as medical technology advanced rapidly, the traditional paternalistic model of medicine became increasingly inadequate for addressing growing concerns about patient autonomy and provider responsibility. The courts became critical arenas for defining new norms, with two cases in particular—Canterbury v. Spence and Tarasoff v. Regents of the University of California—serving as pivotal moments in the legal entrenchment of bioethical principles. These cases translated the foundational ethics of respect for persons, beneficence, and justice into practical legal duties that now govern clinical practice and research. This article examines how these landmark decisions helped establish the legal architecture underlying modern bioethics, creating enduring frameworks for managing the complex ethical challenges that continue to emerge in healthcare and scientific research.
Canterbury v. Spence: The Foundation of Informed Consent
Case Background and Factual Context
In 1958, Jerry Canterbury, a 19-year-old clerk-typist, experienced severe back pain and consulted Dr. William Spence, a neurosurgeon [27]. After diagnostic procedures revealed a spinal abnormality, Dr. Spence recommended a laminectomy—surgical excision of the posterior arch of a vertebra—to correct what he suspected was a ruptured disc [27]. Canterbury consented to the procedure without significant discussion of its risks. The surgery was performed on February 11, 1959, at Washington Hospital Center [27]. Dr. Spence did not inform Canterbury or his mother of the specific risk of paralysis associated with the procedure, later testifying that communicating this risk "might deter patients from undergoing needed surgery and might produce adverse psychological reactions" [27].
Following the operation, Canterbury recuperated normally initially but suffered a fall while unattended during voiding [27]. Several hours later, he became paralyzed from the waist down and required emergency second surgery [27]. Despite further medical interventions, Canterbury sustained permanent disabilities including paralysis of the bowels, urinary incontinence, and reliance on crutches for mobility [27]. The subsequent lawsuit alleged negligence in the performance of the operation and, critically, failure to disclose the inherent risks of the procedure [27].
The Legal Shift from Physician-Centered to Patient-Centered Disclosure
The U.S. Court of Appeals for the District of Columbia Circuit delivered a transformative opinion that fundamentally reshaped the doctrine of informed consent [27]. Prior to Canterbury, the standard for disclosure was governed by what has become known as the "professional standard" or "physician-centered" approach, which required physicians to disclose only what a reasonable medical practitioner would disclose under similar circumstances [28]. This approach placed the medical community as the sole arbiter of what information patients should receive.
The Canterbury court explicitly rejected this physician-centered framework, declaring that "the duty to disclose does not remain the responsibility of the medical community alone" [27]. Instead, the court established what has become known as the "reasonable patient" or "material risk" standard, holding that "a risk is material when a reasonable person, in what the physician knows or should know to be the patient's position, would be likely to attach significance to the risk or cluster of risks in deciding whether or not to forego the proposed therapy" [27]. This shift transferred the focus from medical custom to patient needs for decision-making, fundamentally altering the physician-patient relationship by prioritizing patient autonomy over medical paternalism.
Methodological Framework for Determining Material Risk
The Canterbury decision established a systematic methodology for determining when a risk becomes "material" and therefore requires disclosure. The court outlined specific factors that physicians must consider when evaluating which risks to disclose:
- Nature of the Risk: The character of the risk itself and its potential impact on the patient's life [27]
- Probability of Occurrence: The statistical likelihood that the risk will materialize [27]
- Magnitude of Harm: The severity of potential injury should the risk occur [27]
- Relationship to Procedure: The directness of connection between the proposed treatment and potential harm [27]
- Alternatives: The availability and feasibility of alternative approaches [27]
- Patient-Specific Factors: Any particular circumstances of the individual patient that might affect their assessment of risks [27]
This framework created an objective standard for disclosure based on what a reasonable person would consider significant to their decision-making process, rather than deferring to medical tradition or convenience.
Experimental Protocols for Assessing Informed Consent Practices
Research evaluating informed consent practices following Canterbury has employed various methodological approaches to assess comprehension, voluntariness, and disclosure adequacy:
- Structured Interviews: Utilizing standardized questionnaires to assess patient understanding of disclosed information, risks, benefits, and alternatives [27]
- Control Group Comparisons: Comparing consent processes between groups receiving standard disclosure versus enhanced disclosure protocols [27]
- Comprehension Assessment Tools: Implementing validated instruments to measure retention and understanding of key information [27]
- Observational Studies: Documenting actual consent conversations and coding for completeness of disclosure [27]
Table 1: Key Methodological Approaches for Evaluating Informed Consent
| Method Type | Primary Measures | Application in Research |
|---|---|---|
| Structured Interviews | Understanding of risks, benefits, alternatives | Pre- and post-consent comprehension assessment |
| Control Group Design | Differences in understanding between standard and enhanced consent | Randomized trials of consent processes |
| Observational Coding | Completeness of disclosure, patient questions, physician responses | Analysis of recorded consent conversations |
| Validated Instruments | Standardized scores of comprehension and retention | Comparison across institutions and specialties |
Tarasoff v. Regents: The Duty to Protect and Its Evolution
Case History and Factual Background
The Tarasoff case originated in 1969 when Prosenjit Poddar, a student at the University of California, Berkeley, disclosed to Dr. Lawrence Moore, a psychologist at the university's health service, his intention to kill Tatiana Tarasoff, a young woman who had rejected his romantic advances [29] [30]. Dr. Moore, concerned about this threat, notified campus police both verbally and in writing, requesting that Poddar be detained for psychiatric evaluation [29] [30]. The police briefly detained Poddar but released him after he appeared rational and promised to stay away from Tarasoff [30]. Dr. Moore's supervisor, Dr. Harvey Powelson, later directed the destruction of Moore's therapy notes and the letter to police [29]. No one warned Tarasoff or her family of Poddar's threats [29] [30].
After Tarasoff returned from a trip abroad, Poddar went to her home on October 27, 1969, and fatally stabbed her [29] [30]. Tarasoff's parents subsequently filed a wrongful death lawsuit against the university, its health service, and the therapists involved [30]. The case underwent several judicial considerations before the California Supreme Court's landmark 1976 ruling established the "duty to protect" for mental health professionals [29] [30].
From Confidentiality to Protective Action: The Legal Transformation
The California Supreme Court's decision fundamentally transformed mental health practice by establishing that the therapeutic relationship creates a special relationship that may generate a duty to protect foreseeable victims of a patient's violence [30]. The court famously declared that "the protective privilege ends where the public peril begins" [29] [30]. This ruling created an exception to therapist-patient confidentiality, prioritizing public safety in circumstances where a specific threat exists.
The court initially articulated a "duty to warn" in its 1974 opinion but modified this in the 1976 rehearing to a broader "duty to protect" [31]. This distinction proved significant, as it acknowledged that warning potential victims represents only one of several potential protective actions available to therapists. The court outlined that this duty could be fulfilled through various means, including:
- Warning the intended victim directly of the threat [31]
- Notifying law enforcement authorities [31]
- Arranging for civil commitment of the patient [31]
- Taking other reasonable steps to protect the foreseeable victim [31]
This framework acknowledged clinical discretion while establishing clear legal accountability for managing threats of violence.
Methodological Framework for Violence Risk Assessment
The Tarasoff decision necessitated the development of structured methodologies for assessing violence risk, which have evolved significantly since the original ruling. Contemporary violence risk assessment typically incorporates:
- Structured Professional Judgment (SPJ) Tools: Implementing validated instruments like the HCR-20 (Historical, Clinical, Risk Management-20) to guide systematic evaluation [31]
- Historical Factors Analysis: Reviewing past history of violence, substance use, psychopathology, and noncompliance [31]
- Dynamic Clinical Factors Assessment: Evaluating current symptoms, attitudes, and mental state [31]
- Future Risk Management Considerations: Assessing potential stressors, support systems, and responsive measures [31]
- Collateral Information Gathering: Obtaining records and reports from additional sources beyond patient self-report [31]
Table 2: Core Components of Violence Risk Assessment Post-Tarasoff
| Assessment Domain | Key Elements | Clinical Application |
|---|---|---|
| Historical Factors | Previous violence, criminal history, psychopathy traits, substance abuse history | Record review, collateral contacts |
| Clinical Presentation | Current symptoms, impulsivity, treatment compliance, violent ideation | Clinical interview, mental status exam |
| Risk Management Factors | Future stressors, support systems, treatment responsiveness, plan feasibility | Discharge planning, treatment formulation |
| Protective Factors | Social supports, treatment engagement, coping skills, environmental stability | Strength-based assessment, treatment planning |
State-by-State Legal Implementation
The Tarasoff ruling initially applied only in California, but its influence spread across the United States through various legislative and judicial pathways. Current implementation varies significantly by jurisdiction:
- Mandatory Duty States: 23 states have statutorily mandated reporting laws requiring mental health professionals to warn or protect when specific threats are made against identifiable victims [29]
- Common Law Duty States: 10 states impose a duty to warn under common law through court decisions rather than specific statutes [29]
- Permissive Duty States: 11 states allow but do not require clinicians to breach confidentiality to warn potential victims, granting discretion based on clinical judgment [29]
- No Clear Guidance: 6 states have no established position or guidance regarding the Tarasoff duty [29]
This jurisdictional variation creates important implications for mental health practice and necessitates that clinicians maintain current knowledge of their specific state requirements.
The Institutionalization of Bioethics: From Courtrooms to Clinical Practice
The Emergence of Bioethics as a Discipline
The legal principles established in Canterbury and Tarasoff emerged alongside and contributed to the broader development of bioethics as a distinct field. Prior to the 1960s, medical ethics remained largely the domain of physicians, grounded in the Hippocratic tradition and focused primarily on professional conduct and patient welfare [3] [4]. The post-World War II period witnessed unprecedented advances in medical technology and therapeutic interventions, which simultaneously created novel ethical dilemmas that traditional medical ethics frameworks proved ill-equipped to address [3] [32].
Several converging factors catalyzed the emergence of bioethics as a discipline:
- Medical Technology Advances: New capabilities in life support, organ transplantation, and critical care raised fundamental questions about quality of life, resource allocation, and the definition of death [3] [4]
- Research Ethics Abuses: Revelations concerning the Tuskegee syphilis study, Willowbrook experiments, and other ethical violations highlighted the need for stronger patient protections [3] [32]
- Consumer Rights Movement: President John F. Kennedy's 1962 Consumer Bill of Rights emphasized rights to safety, information, choice, and being heard—principles that directly influenced patient rights [3]
- Cultural Shifts Toward Autonomy: Growing emphasis on individual rights and self-determination across American society challenged medical paternalism [3] [4]
These factors created fertile ground for the establishment of dedicated bioethics institutions, most notably The Hastings Center (founded 1969) and the Kennedy Institute of Ethics at Georgetown University (founded 1971), which provided organizational homes for the systematic study of ethical issues in medicine and biology [3].
Legal Principles as Catalysts for Bioethics Infrastructure
Landmark cases like Canterbury and Tarasoff served as crucial catalysts in the development of formal bioethics infrastructure within healthcare institutions. The legal standards established in these cases necessitated systematic approaches to addressing ethical dilemmas, leading to the creation of:
- Institutional Review Boards (IRBs): Required for oversight of human subjects research, ensuring informed consent and risk-benefit analysis [32]
- Hospital Ethics Committees: Multidisciplinary groups providing consultation, policy development, and education on clinical ethics issues [4]
- Ethics Consultation Services: Available to patients, families, and healthcare providers for addressing specific ethical dilemmas in patient care [4]
- Patient Rights Advocates: Designated individuals or offices to protect and promote patient rights, particularly regarding informed consent [3]
This infrastructure formalized the integration of ethical analysis into healthcare delivery and research, ensuring that the principles articulated in landmark cases became operationalized in daily practice.
Diagram: Legal Foundations of Modern Bioethics Principles
The Researcher's Toolkit: Analytical Frameworks for Bioethics Integration
Essential Methodologies for Bioethics Legal Analysis
Research into the intersection of law and bioethics employs distinct methodological approaches for analyzing the impact and implementation of landmark cases:
- Doctrinal Legal Analysis: Systematic examination of case law, statutes, and regulations to identify evolving legal standards and inconsistencies across jurisdictions [31]
- Historical Case Study Method: In-depth reconstruction of landmark cases using court records, briefs, and contemporary accounts to understand legal reasoning and context [27] [30]
- Comparative Jurisdictional Analysis: Examination of variations in legal standards and implementation across states or countries to identify different approaches to common ethical problems [29] [31]
- Empirical Ethics Research: Quantitative and qualitative investigation of how legal standards are actually implemented in practice and their effects on patient care and professional behavior [31]
Table 3: Essential Analytical Resources for Bioethics Legal Research
| Resource Category | Specific Tools | Application in Research |
|---|---|---|
| Primary Legal Sources | Court opinions, statutes, administrative regulations | Establishing binding legal standards and requirements |
| Legal Databases | Westlaw, LexisNexis, Google Scholar (case law) | Comprehensive case retrieval and shepardization |
| Bioethics Repositories | Hastings Center Report, Kennedy Institute of Ethics Library | Access to interdisciplinary analysis and commentary |
| Government Documents | Congressional hearings, agency guidelines, commission reports | Understanding regulatory frameworks and policy development |
| Structured Assessment Tools | HCR-20, MacArthur Violence Risk Assessment | Standardized evaluation protocols for clinical-legal interfaces |
Experimental Protocol: Assessing Institutional Compliance with Legal Standards
A robust methodological framework for evaluating how healthcare institutions implement legal bioethics standards involves:
- Policy Document Analysis: Systematic review of institutional policies, procedures, and consent forms for alignment with legal requirements [31]
- Structured Interviews with Key Informants: Conducting semi-structured interviews with ethics committee members, legal counsel, risk managers, and clinical staff regarding implementation practices [31]
- Case File Review: Examination of de-identified ethics consultation records, incident reports, and adverse event documentation [31]
- Comparative Benchmarking: Assessing institutional practices against national standards and peer organization approaches [31]
- Gap Analysis and Recommendation Development: Identifying discrepancies between legal standards and actual practice, formulating specific corrective strategies [31]
This comprehensive approach allows researchers to move beyond formal compliance to assess how legal principles actually function within healthcare systems.
The landmark cases of Canterbury v. Spence and Tarasoff v. Regents of the University of California represent pivotal moments in the institutionalization of bioethics within American healthcare and research. These decisions translated abstract ethical principles into concrete legal duties, creating enforceable standards that fundamentally reshaped professional practice and patient rights. The "reasonable patient" standard from Canterbury and the "duty to protect" from Tarasoff established foundational frameworks that continue to guide clinical practice, research ethics, and institutional policy decades after their issuance.
The legal entrenchment of these principles catalyzed the development of extensive bioethics infrastructure, including ethics committees, institutional review boards, and formal consultation services that operationalize these standards in daily practice. Moreover, these cases demonstrated law's capacity to function as a mechanism for social change within healthcare, balancing competing values and establishing accountability mechanisms that protect vulnerable individuals while respecting professional judgment.
As biomedical science continues to advance into new frontiers—from genetic engineering to artificial intelligence in healthcare—the foundational principles articulated in these landmark cases provide enduring frameworks for addressing novel ethical challenges. The legal entrenchment of bioethics principles ensures that technological capability remains subject to ethical governance, preserving core values of autonomy, beneficence, and justice in the face of relentless scientific progress.
Frameworks and Implementation: Building the Institutional Architecture for Ethical Oversight
The emergence of formal ethical frameworks for research in the United States represents a direct response to historical ethical failures and the growing complexity of biomedical science. The latter half of the 20th century witnessed a pivotal shift from a paternalistic model of medical practice to a systematic, principles-based approach for protecting human subjects. This transition was catalyzed by heightened public awareness of ethical abuses, most notably the Tuskegee Syphilis Study, in which black men with syphilis were left untreated without their knowledge to study the natural progression of the disease [33]. In response to this and other scandals, the U.S. Congress passed the National Research Act of 1974, which created the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research [34] [35]. This Commission was charged with identifying the basic ethical principles that should underlie the conduct of research involving human subjects.
The Commission's work culminated in the 1979 Belmont Report, a foundational document that established three core ethical principles [35]. Concurrently, the field of bioethics was formally institutionalized through the establishment of dedicated centers like The Hastings Center (1969) and the Kennedy Institute of Ethics (1971), which provided an academic and practical home for the systematic study of ethical issues in the life sciences [3]. This professionalization moved ethical discourse beyond the sole purview of medical professionals and into a broader, multi-disciplinary field. The following sections will provide an in-depth technical analysis of the Belmont Report's principles and the seven guiding principles for ethical research, examining their specific applications, historical development, and interrelationships within the context of the U.S. research ecosystem.
The Historical Context and Pre-Belmont Foundations
The development of ethical frameworks for research did not begin with the Belmont Report. Earlier documents, created in reaction to specific ethical crises, laid the essential groundwork.
The Nuremberg Code (1947)
The Nuremberg Code emerged from the post-World War II "Doctors' Trial," where Nazi scientists were prosecuted for horrific experiments on concentration camp prisoners [33] [32]. This code established ten points for ethical research, with the absolute requirement for voluntary consent as its first and most essential principle [33]. It stated that the human subject must have "sufficient knowledge and comprehension of the elements of the subject matter involved as to enable him to make an understanding and enlightened decision" [32]. While the Code emphasized the principle of Respect for Autonomy, its primary limitation was its focus on the unique circumstances of concentration camps, and it did not fully address protections for vulnerable populations like children or adults with diminished decision-making capacity [34].
The Declaration of Helsinki (1964)
Adopted by the World Medical Association (WMA), the Declaration of Helsinki distinguished between clinical research combined with professional care and non-therapeutic clinical research [34]. A significant evolution from the Nuremberg Code was its introduction of a formal mechanism for independent ethical review. It entrusted a research ethics committee (in the U.S., an Institutional Review Board or IRB) with the responsibility of approving research protocols, thereby shifting some of the ethical oversight from the individual investigator to an independent body [34]. The Declaration has been revised multiple times to refine its guidance on vulnerable populations and other emerging issues.
The Beecher Article (1966)
A pivotal moment in the U.S. was the 1966 article by Henry Beecher, a Harvard anesthesiologist, published in the New England Journal of Medicine [3] [32]. Beecher exposed 22 examples of ethically questionable research occurring in leading U.S. medical institutions, demonstrating that ethical failures were not isolated to foreign war crimes but were a domestic problem as well [3]. His work profoundly shocked the medical community and the public, creating significant momentum for systemic reform and greater governmental oversight of research practices.
The table below summarizes these key pre-Belmont documents and their contributions.
Table 1: Foundational Documents Preceding the Belmont Report
| Document | Year | Historical Context | Primary Ethical Contribution |
|---|---|---|---|
| Nuremberg Code [33] | 1947 | Nazi medical experiments during WWII | Established the absolute requirement for voluntary informed consent. |
| Declaration of Helsinki [34] | 1964 (1st version) | Post-war growth of international medical research | Introduced independent review by a research ethics committee and distinguished therapeutic from non-therapeutic research. |
| Beecher's "Ethics and Clinical Research" [3] [32] | 1966 | Exposure of widespread unethical research in U.S. institutions | Catalyzed U.S. professional and public awareness of the need for formal ethical standards and oversight. |
The Belmont Report: Principles and Applications
The Belmont Report, formally titled "Ethical Principles and Guidelines for the Protection of Human Subjects of Research," was published in 1979 as a direct outcome of the National Research Act of 1974 [35]. It was created to provide a comprehensive yet flexible moral framework to guide researchers and IRBs.
The Three Core Ethical Principles
The Report identifies three fundamental ethical principles:
- Respect for Persons: This principle acknowledges the autonomy of individuals as agents capable of self-determination and deliberation about personal goals [35]. It requires that individuals be treated with courtesy and respect. Its practical application demands that subjects enter research voluntarily and with adequate information. Furthermore, it recognizes that not all individuals are capable of full self-determination (due to illness, mental disability, or circumstance) and thus require additional protections [35].
- Beneficence: This principle extends beyond the simple maxim "do no harm" to an affirmative obligation to maximize potential benefits and minimize possible harms [35]. It requires a systematic assessment of risks and benefits associated with the research. The goal is to ensure that the risks to which subjects are exposed are justified by the anticipated benefits to the subject or to society [34] [35].
- Justice: This principle addresses the fair distribution of the burdens and benefits of research [35]. It demands that the selection of research subjects be scrutinized to avoid systematically recruiting vulnerable or disadvantaged populations (e.g., prisoners, marginalized communities) for research that primarily benefits more privileged groups. The exploitation of unwilling prisoners in Nazi camps and the selection of poor, African American sharecroppers in the Tuskegee study are cited as prime examples of injustice [35].
Applications of the Principles
The Belmont Report translates these abstract principles into concrete requirements for the conduct of research [35]:
- Informed Consent: The application of Respect for Persons. Consent must comprise three elements: information (key facts about the research), comprehension (ensuring the subject understands the information), and voluntariness (ensuring the agreement is free from coercion and undue influence) [35].
- Assessment of Risks and Benefits: The application of Beneficence. This is a systematic, albeit sometimes non-quantifiable, process of analyzing the types and probabilities of harm and the potential for positive outcomes. The IRB must judge that the benefits are proportionate to the risks [35].
- Selection of Subjects: The application of Justice. The ethical focus here is on the process for recruiting subjects, ensuring that both the burdens of participation and the benefits of the research are distributed fairly across society [35].
The following diagram illustrates the logical relationship between the Belmont Report's principles and their applications.
The Seven Guiding Principles of Ethical Research
While the Belmont Report provides a foundational ethical structure, contemporary bioethicists and institutions like the NIH have further refined these ideas into a more detailed set of seven practical principles to guide the entire research lifecycle [36] [37]. These principles serve as an operational checklist for designing, reviewing, and conducting ethical studies.
- Social and Clinical Value: The research must be designed to answer a question that contributes to scientific understanding of health or improves preventive, therapeutic, or care practices. Without this value, exposing participants to any risk or inconvenience is unjustified [36].
- Scientific Validity: The study must be rigorously designed to yield reliable and valid data. This involves using accepted principles, clear methods, and feasible procedures. Invalid research is inherently unethical because it wastes resources and exposes participants to risk for no purpose [36] [37].
- Fair Subject Selection: The scientific goals of the study, not vulnerability or privilege, should be the primary basis for recruitment. Groups should not be excluded without a valid scientific reason, and participants who bear the risks of research should be in a position to enjoy its benefits [36] [37].
- Favorable Risk-Benefit Ratio: Uncertainty about risks and benefits is inherent in research. Researchers must minimize all possible risks—physical, psychological, social, or economic—and maximize the potential benefits. The assessment must conclude that the potential benefits are proportionate to, or outweigh, the risks [36].
- Independent Review: To minimize conflicts of interest and bias, an independent panel (e.g., an IRB) must review the research proposal. This review evaluates the study's ethical design, risk-benefit ratio, and provisions for participant protection, and it continues to monitor the study while it is ongoing [36] [37].
- Informed Consent: This is a process, not merely a form, through which a potential subject voluntarily confirms their willingness to participate. It requires accurate disclosure of information, participant comprehension, and a voluntary decision made without coercion [36] [37].
- Respect for Potential and Enrolled Subjects: This principle extends beyond initial consent to require ongoing respect for participants' privacy and confidentiality, their right to change their mind and withdraw without penalty, and the obligation to inform them of new information that might affect their willingness to continue. It also includes monitoring their welfare and informing them of the study's outcomes [36].
Table 2: The Seven Guiding Principles of Ethical Research
| Principle | Core Question for Researchers | Practical Application |
|---|---|---|
| Social & Clinical Value [36] | Will the answer to the research question contribute meaningfully to science or clinical care? | Justifying the study based on a review of existing literature and identifying a genuine knowledge gap. |
| Scientific Validity [36] [37] | Is the study design robust enough to provide a clear answer to the research question? | Employing sound methodology, appropriate statistical power, and reliable data collection practices. |
| Fair Subject Selection [36] [37] | Are the participants selected for scientific reasons, and are they the appropriate group to bear the risks and enjoy the benefits? | Developing an inclusion/exclusion criteria document that is scientifically, not convenience, based. |
| Favorable Risk-Benefit Ratio [36] | Have all risks been minimized, and are the remaining risks justified by the potential benefits to the subject or society? | Conducting a thorough risk-benefit analysis and implementing safety monitoring plans. |
| Independent Review [36] [37] | Has the study design been scrutinized by an unbiased, independent committee for ethical soundness? | Submitting the protocol, consent forms, and study materials to an IRB for approval before initiation. |
| Informed Consent [36] [37] | Has the participant truly understood the study and made a free choice to participate? | Developing a clear consent process and document, and verifying participant understanding. |
| Respect for Participants [36] | How are participants treated during and after the study? | Protecting confidentiality, allowing easy withdrawal, and sharing aggregate study results. |
Integration and Implementation in Modern Research
The Relationship Between the Two Frameworks
The Belmont Report and the seven guiding principles are not competing frameworks but exist in a complementary, hierarchical relationship. The Belmont Report's three principles (Respect for Persons, Beneficence, Justice) form the philosophical foundation upon which the more operational seven principles are built [36] [38] [37]. For instance, the seven principles of Informed Consent and Respect for Participants are direct elaborations of the Belmont principle of Respect for Persons. Similarly, Scientific Validity, Favorable Risk-Benefit Ratio, and elements of Independent Review are practical applications of Beneficence. The principle of Fair Subject Selection is the operationalization of Justice.
Regulatory Effect and the Common Rule
The Belmont Report had a profound effect on U.S. federal policy. Its principles were directly incorporated into the U.S. Federal Regulations for the Protection of Human Subjects (45 CFR 46) [34] [35]. In 1991, this policy was unified across 14 other federal departments and agencies, creating the Federal Policy for the Protection of Human Subjects, known as the "Common Rule," which sets the baseline for IRB review and ethical conduct for most federally funded research in the United States [35]. The report's influence is also clearly seen in specialized areas, such as the ethical review framework for gene therapy clinical trials [34].
The Scientist's Toolkit: Essential Components for Ethical Research
For the research professional, ethical conduct is ensured through a combination of foundational documents, regulatory oversight, and practical tools. The following table details key components of this "toolkit."
Table 3: Research Reagent Solutions for Ethical Experimentation
| Toolkit Component | Function in Ethical Research | Role in Protecting Human Subjects |
|---|---|---|
| Protocol with Scientific Validity [36] | The master plan document detailing the study's background, objectives, design, methodology, and statistical considerations. | Ensures the research is not wasteful and has a valid purpose, satisfying the principles of Social Value and Scientific Validity. |
| Informed Consent Form (ICF) [35] | The document and accompanying process used to provide comprehensive information to and obtain voluntary consent from a potential participant. | The primary mechanism for operationalizing the principle of Respect for Persons and ensuring voluntary participation. |
| Institutional Review Board (IRB) [36] [34] | An independent administrative body established to protect the rights and welfare of human research subjects. | Provides the mandatory Independent Review of research, ensuring a favorable risk-benefit ratio and ethical design. |
| Data Safety Monitoring Board (DSMB) | A committee of independent experts that monitors participant safety and treatment efficacy data while a clinical trial is ongoing. | An extension of Beneficence and Respect for Participants, allowing for ongoing risk-benefit assessment and early stopping if risks are too high. |
| Case Report Form (CRF) | A structured tool used in clinical trials to collect individual participant data as specified by the protocol. | Ensures accurate data collection, which is fundamental to Scientific Validity, and protects participant confidentiality by using identified data responsibly. |
The institutionalization of bioethics in the United States, crystallized by the creation of the Belmont Report and refined into seven guiding principles, represents a critical evolution in the responsible conduct of science. These frameworks transform abstract moral commitments into actionable standards for review boards and researchers. For the modern drug development professional, these are not merely regulatory hurdles but the essential underpinnings of credible and trustworthy science. Understanding the historical context that gave rise to these principles—from Nuremberg and Tuskegee to the foundational work of the National Commission—is not an academic exercise. It is a vital part of cultivating an ethical consciousness that ensures the well-being and rights of human subjects remain the highest priority in the relentless pursuit of scientific progress.
The establishment of Institutional Review Boards (IRBs) represents a critical institutionalization of bioethics within the United States research landscape. These regulatory bodies emerged as a direct response to historical ethical failures in human subjects research, evolving from informal institutional committees to a comprehensive federal system. IRBs, also known as independent ethics committees or ethical review boards, provide a core protection for human research participants through advance and periodic independent review of the ethical acceptability of proposals for human research [39]. Their development marks the transition from researcher-centered practices to a participant-protection framework grounded in ethical principles and enforceable regulations. This whitepaper examines the historical evolution, regulatory foundation, operational mechanisms, and contemporary challenges of the IRB system, providing researchers and drug development professionals with a comprehensive technical understanding of this essential oversight infrastructure.
Historical Foundations: From Ethical Abuses to Systemic Protections
Pre-Codification Ethical Frameworks
The conceptual foundations for ethical oversight of human subjects research emerged from several landmark documents and events that exposed critical vulnerabilities in research practices:
The Nuremberg Code (1947): Developed in response to Nazi medical experimentation atrocities during World War II, this code established the absolute requirement for voluntary consent and that the benefits of research must outweigh the risks [40] [41]. Although groundbreaking, it carried limited legal force and was initially overlooked by many researchers [40].
The Declaration of Helsinki (1964): Established by the World Medical Association, this document expanded beyond the Nuremberg Code by stressing physician-researchers' responsibilities to their participants and outlining principles for informed consent, risk-benefit assessment, and vulnerable population protection [40]. It has undergone multiple revisions and forms the basis for Good Clinical Practices used today [41].
The Belmont Report (1979): This foundational document identified three core ethical principles for research: respect for persons (acknowledging autonomy and protecting those with diminished autonomy), beneficence (maximizing benefits while minimizing harms), and justice (ensuring fair distribution of research burdens and benefits) [40] [41]. These principles directly inform federal regulations and IRB evaluation criteria.
Catalytic Research Scandals and Public Outcry
Several notorious research scandals demonstrated the necessity of formalized oversight and propelled regulatory action:
The Tuskegee Syphilis Study (1932-1972): This U.S. Public Health Service study followed 400 African American men with syphilis without informing them of their diagnosis, even after penicillin became an effective treatment in the 1940s [41]. The study continued for 40 years, with researchers actively preventing subjects from receiving treatment, resulting in unnecessary deaths and disability [42] [41]. The public revelation of this study in 1972 created political embarrassment and fueled demands for regulatory reform [41].
Willowbrook State School Study (1956-1971): Researchers deliberately infected children with mental disabilities with hepatitis to study disease development and potential vaccines, with parents coerced into consent through guaranteed admission to the overcrowded facility [40].
Brooklyn Jewish Chronic Disease Hospital Study (1963): Researchers injected live cancer cells into elderly patients without informed consent, falsely claiming they were testing immunity [40].
Beecher's Exposé (1966): Dr. Henry Beecher published an article in the New England Journal of Medicine revealing 22 examples of ethically questionable research from reputable researchers and journals, demonstrating that ethical violations were not isolated incidents [41].
Regulatory Codification: The Emergence of the Modern IRB System
Legislative and Regulatory Milestones
The transition from ethical guidelines to enforceable regulations occurred through key legislative and administrative actions:
Table 1: Major Regulatory Milestones in U.S. Human Subjects Protection
| Year | Regulatory Action | Key Provisions | Impact |
|---|---|---|---|
| 1966 | U.S. Public Health Service Policy | Required ethical review for federally-funded research | Limited enforcement; first formal requirement [39] |
| 1974 | National Research Act | Established National Commission for Protection of Human Subjects; mandated IRB review for federally-funded research [43] [44] [41] | Formal creation of IRB system [44] [45] |
| 1979 | Belmont Report | Articulated ethical principles: respect for persons, beneficence, justice [40] [41] | Ethical foundation for subsequent regulations [41] |
| 1981 | FDA Regulations (21 CFR Parts 50 & 56) | Required IRB review for FDA-regulated clinical investigations [39] [46] [41] | Extended protections to drug, device, and biologic research |
| 1991 | Federal Policy (Common Rule) | Codified DHHS regulations (45 CFR Part 46) as standard for multiple federal agencies [39] [41] | Created unified framework for most federally-funded research |
The Common Rule and FDA Regulations
The current regulatory landscape for human subjects research primarily operates under two complementary frameworks:
The Federal Policy for the Protection of Human Subjects (Common Rule): Adopted by 17 federal departments and agencies, this regulation establishes uniform requirements for IRB composition, function, and operations [41]. It requires IRB review and approval for all research involving human subjects conducted or supported by federal agencies [39].
FDA Regulations (21 CFR Parts 50, 56): These regulations govern research involving products regulated by the FDA (drugs, biologics, devices) regardless of funding source [39] [46]. While largely congruent with the Common Rule, significant differences exist in details such as documentation and reporting requirements [46] [41].
IRB Composition, Function, and Operational Framework
Structural Requirements and Membership Diversity
Federal regulations mandate specific compositional requirements for IRBs to ensure comprehensive review capabilities:
Table 2: IRB Composition Requirements Under Federal Regulations
| Requirement | Regulatory Citation | Specifications | Rationale |
|---|---|---|---|
| Minimum Membership | 21 CFR 56.107 [39] | At least 5 members [40] [47] | Ensure adequate deliberation capacity |
| Diversity | 21 CFR 56.107(a) [39] | Varying backgrounds, both sexes, multiple professions [39] [42] | Incorporate multiple perspectives |
| Scientific Member | 21 CFR 56.107(c) [39] | At least one member with primary concerns in scientific areas [46] [45] | Evaluate scientific validity and risk-benefit ratio |
| Non-Scientific Member | 21 CFR 56.107(c) [39] | At least one member with primary concerns in non-scientific areas [46] [45] | Represent community values and non-scientific considerations |
| Unaffiliated Member | 21 CFR 56.107(d) [39] | At least one member not affiliated with the institution [45] [47] | Provide independent perspective; represent community standards |
| Vulnerability Expertise | 21 CFR 56.107(a) [39] | Knowledge about vulnerable populations (prisoners, children, etc.) [39] | Ensure appropriate protections for susceptible groups |
The FDA explicitly permits members to fulfill multiple categories simultaneously, but emphasizes that IRBs "should strive for a membership that has a diversity of representative capacities and disciplines" [46]. This diversity is further enhanced through the use of alternates and consultants with specialized expertise [46].
IRB Review Criteria and Approval Standards
For research to receive IRB approval, it must satisfy specific regulatory criteria designed to implement the ethical principles of the Belmont Report:
The risk-benefit assessment requires IRBs to determine that "risks to subjects are minimized; risks are reasonable in relation to anticipated benefits, if any, and the importance of the expected knowledge" [39]. This involves systematic evaluation of the research methodology and potential harms versus potential benefits to subjects and society [39] [40].
The informed consent process must include adequate provision for: (1) informing subjects of key study elements; (2) ensuring subject comprehension; and (3) obtaining voluntary participation without coercion or undue influence [40] [41]. Documentation of consent is typically required unless specifically waived under limited circumstances [39].
Vulnerable population protections require additional safeguards for groups such as children, prisoners, pregnant women, mentally disabled persons, or economically or educationally disadvantaged persons [39] [40]. These provisions recognize that certain populations require enhanced protections due to increased susceptibility to coercion or diminished autonomy [42].
Contemporary Challenges and Evolving IRB Models
Systemic Inefficiencies and Administrative Burden
As research has evolved toward multisite and multinational trials, significant challenges have emerged within the decentralized IRB review system:
Review Inconsistencies: Multiple studies document "wide variation in standards applied to review and approval of IRB applications" across different institutions [48]. One observational health services study requiring IRB approval at 43 sites experienced dramatically different classifications—the same study was exempted at one site (though it didn't qualify for exemption), granted expedited review at 10 sites, required full review at 31 sites, and was rejected as "too risky" at one site [48].
Administrative Burden: The multisite review process consumes substantial resources. One study documented "approximately 4,680 hours of staff time over a 19-month period were devoted solely to the IRB process" across 43 sites, with a median approval time of 286 days per site (range: 52-798 days) [48]. These delays particularly impact observational health services research with more modest budgets compared to pharmaceutical trials [48].
Procedural Inefficiencies: Researchers encounter "multiple returns for revision of IRB applications, consent documents, and ancillary forms," with 76% of sites requiring at least one resubmission and 15% requiring three or more resubmissions (up to six) for the same study [48]. Most requested changes were editorial rather than substantive [48].
Evolving Oversight Models and Regulatory Modernization
In response to these challenges, several alternative models and regulatory updates have been proposed or implemented:
Centralized IRB Review: Instead of local review at each performance site, centralized review utilizes a single IRB (often commercial) for multisite studies, potentially reducing duplication and inconsistency [39] [48]. The 2018 updates to the Common Rule specifically promoted the use of central IRBs for multisite research [39].
Accreditation Systems: Organizations like the Association for the Accreditation of Human Research Protection Programs (AAHRPP) provide voluntary accreditation to demonstrate high-quality human research protection programs [39].
Regulatory Updates: Proposed changes to federal regulations aim to "enhance protections and efficiency" through standardized forms, updated exemption categories, and requirements for single IRB review for multisite studies [39]. The FDA has also participated in efforts to harmonize international standards through the International Conference on Harmonisation Good Clinical Practice guidelines [39].
The Researcher's Toolkit: Navigating the IRB Process
Essential Documentation and Submission Elements
Successful IRB applications require comprehensive documentation addressing both scientific and ethical considerations:
Table 3: Essential IRB Submission Components and Functions
| Submission Component | Function | Regulatory Basis | Considerations |
|---|---|---|---|
| Research Protocol | Detailed study description including background, objectives, methodology, statistical analysis plan, and monitoring procedures | 21 CFR 56.109 [39] [46] | Must demonstrate scientific validity and ethical design |
| Informed Consent Documents | Clear, understandable explanation of research purposes, procedures, risks, benefits, alternatives, and rights | 21 CFR 50.25 [46] [41] | Language appropriate to participant comprehension level; required elements specified in regulations |
| Investigator Brochure | Comprehensive documentation of relevant preclinical and clinical data on investigational products | FDA Guidance [46] | Required for drug/device trials; informs risk-benefit assessment |
| Investigator CV and Qualifications | Demonstration of investigator expertise, training, and experience | FDA Guidance [46] [44] | IRB confirms "investigator has appropriate credentials, facilities, and staff" [44] |
| Recruitment Materials | Advertisements, scripts, and communications for subject recruitment | 21 CFR 56.107 [39] | Must not be coercive or promise unjustifiable benefits |
| Data Collection Instruments | Surveys, interview guides, case report forms, data abstraction tools | 21 CFR 56.111 [39] | Must protect confidentiality and minimize risks |
| HIPAA Authorizations (if applicable) | Documentation of authorization for use/disclosure of protected health information | Privacy Rule [48] | Required for research involving PHI with exceptions for limited datasets with waivers |
Protocol Implementation and Continuing Review
Once approved, researchers must adhere to ongoing compliance requirements:
Amendment Procedures: Any changes to the approved research protocol must receive IRB review and approval before implementation, except when necessary to eliminate apparent immediate hazards to subjects [39] [46].
Continuing Review: IRBs must conduct continuing review of research at least annually [39] [46] [45], though the 2018 Common Rule revisions eliminated this requirement for minimal risk research [39]. The review assesses progress, participant accrual, adverse events, and any new literature or information that might affect the risk-benefit ratio [39].
Adverse Event Reporting: Unanticipated problems involving risks to subjects or others must be reported promptly to the IRB [39] [46]. The IRB determines whether modifications are needed or if the study must be suspended or terminated [39].
Study Closure: Final reports are required upon study completion or termination to document compliance and outcomes [46].
The establishment of Institutional Review Boards represents a fundamental institutionalization of bioethical principles within the U.S. research enterprise. From their origins in response to egregious ethical violations to their current role as comprehensive oversight bodies, IRBs have become essential components of the clinical research infrastructure. While challenges of consistency, efficiency, and appropriate scope persist, the system continues to evolve toward more centralized models, harmonized standards, and risk-proportionate review. For researchers and drug development professionals, understanding the historical context, regulatory framework, and operational mechanisms of IRBs is not merely a compliance requirement but a fundamental aspect of ethical research conduct. As science continues to advance into new methodological and ethical territories, the IRB system will undoubtedly continue to adapt while maintaining its core mission: protecting the rights, safety, and welfare of human research participants.
The evolution of clinical ethics consultation and hospital ethics committees represents a significant development in American healthcare, marking the transition of bioethics from abstract philosophical inquiry to structured institutional practice. This transformation began in the latter half of the 20th century, as technological advances in medicine created novel ethical dilemmas that extended beyond traditional medical decision-making. The institutionalization of bioethics emerged as a response to these challenges, establishing formal mechanisms within healthcare organizations to address the complex moral questions arising in patient care. This whitepaper examines the historical trajectory, current practices, and operational frameworks that characterize clinical ethics consultation services and hospital ethics committees today, situating their development within the broader thesis of bioethics as an institutionalized field in the United States.
The formation of hospital ethics committees (HECs) and clinical ethics consultation services (CECSs) represents healthcare organizations' structural response to the growing recognition that ethical dilemmas in clinical practice require systematic, specialized, and consistent approaches. This development mirrors the professionalization of bioethics as a distinct field, complete with standardized competencies, certification processes, and recognized best practices that bridge theoretical frameworks with practical application at the bedside.
Historical Development and Professionalization
The Evolution from Ad Hoc Consultation to Standardized Practice
The development of clinical ethics consultation has progressed from informal, case-based discussions to structured methodologies with defined processes and theoretical underpinnings. Early ethics consultations typically involved individual philosophers, theologians, or physicians who applied their disciplinary expertise to clinical dilemmas without standardized approaches. The professionalization of the field accelerated with the establishment of the American Society for Bioethics and Humanities (ASBH) in 1998, which began to articulate core competencies for healthcare ethics consultation and establish standards for the complex moral reasoning required in clinical settings [49].
This formalization continued with the creation of the Healthcare Ethics Consultant-Certified (HEC-C) program in 2018, which established a certification process to validate the knowledge and skills of ethics consultants [49]. The HEC-C certification has become a significant marker of professional qualification, with certification preparation now including comprehensive review courses that cover four content domains: healthcare ethics issues and concepts (both big picture and clinical encounters), healthcare systems and health law, and clinical contexts [50]. This professionalization reflects the broader institutionalization of bioethics within healthcare systems and represents the field's maturation from theoretical exploration to applied clinical practice.
The Emergence of Hospital Ethics Committees
Hospital ethics committees emerged as multidisciplinary bodies designed to address the ethical dimensions of patient care through three primary functions: education, policy development, and case consultation. The formation of these committees institutionalized ethics within healthcare organizations, creating standing structures with designated responsibilities for addressing moral questions. Unlike the early model of individual ethicists providing consultation, ethics committees brought together diverse perspectives from various disciplines including medicine, nursing, social work, law, philosophy, and religious studies, reflecting the multidimensional nature of clinical ethical dilemmas.
The evolution of HECs has been characterized by increasing formalization of their roles and responsibilities, with many institutions developing specific procedures for case consultation, policy review, and staff education. This development represents a significant shift in how healthcare organizations conceptualize and address ethical challenges—from reactive, case-specific responses to proactive, systematic approaches that integrate ethical considerations into institutional structures and processes.
Current Educational and Training Requirements
Foundational Competencies and Knowledge Domains
The professionalization of clinical ethics consultation is evidenced by the standardized competencies and structured educational opportunities now available to practitioners. The ASBH has identified core competencies for healthcare ethics consultation that form the foundation of contemporary training programs. These competencies span multiple domains, including ethical assessment skills, process skills for mediation and facilitation, and interpersonal skills for effective communication in emotionally charged situations [50].
Training programs for ethics consultants have become increasingly sophisticated, moving beyond theoretical knowledge to emphasize practical, skills-based learning. For instance, the University of Virginia's intensive training seminar focuses on developing or deepening healthcare ethics and moral distress consultation knowledge and skills, specifically preparing participants for the healthcare ethics consultation certification exam [51]. This program, grounded in the ASBH core competencies, emphasizes the four content domains determined for certification and notably includes specialized training in moral distress consultation—a recognition of the expanding scope of ethics consultation services [51].
Table 1: Core Competency Domains for Healthcare Ethics Consultation
| Domain | Key Components | Assessment Methods |
|---|---|---|
| Healthcare Ethics Issues & Concepts: Big Picture | Foundational ethical theories, principles of bioethics, philosophical frameworks | Written examinations, case analysis essays |
| Healthcare Ethics Issues & Concepts: Clinical Encounters | Application of ethical frameworks to clinical cases, bedside decision-making | Case simulations, direct observation |
| Healthcare Systems & Health Law | Regulatory requirements, institutional policies, legal precedents | Policy analysis, legal case reviews |
| Clinical Context & Local Healthcare Organizations | Institution-specific protocols, organizational culture, local resources | Practical exercises, institutional policy development |
Specialized Training Modalities and Skill Development
Contemporary training for ethics consultants employs diverse pedagogical approaches to develop the necessary competencies for effective practice. These include didactic sessions, case discussions, hands-on exercises, and observation of actual ethics consultation services [51]. Training has become increasingly specialized, with programs offering instruction in specific consultation models, facilitation techniques for challenging conversations, and approaches to ethics education for committee members.
Specialized workshops now address distinct aspects of ethics consultation practice. For example, ASBH preconference workshops include sessions on "Managing Challenging Conversations through Skilled Facilitation," which teaches strategies for conducting "complex, multi-party, and emotionally charged meetings with a diverse set of stakeholders" [50]. Similarly, workshops on "Leveraging Humanities and Arts in Clinical Ethics Education" demonstrate innovative approaches to ethics education using film, visual art, and narrative to foster reflection on personal and professional values [50]. These specialized training opportunities reflect the sophistication and diversity of approaches in contemporary clinical ethics practice.
Table 2: Structured Training Programs in Clinical Ethics Consultation
| Program Type | Duration | Key Focus Areas | Outcome Measures |
|---|---|---|---|
| Intensive Training Seminars | 3 days (in-person) | Healthcare ethics consultation, moral distress consultation, certification exam preparation | Knowledge assessment, skills demonstration, certificate of completion |
| HEC-C Review Courses | 4 hours | Core references, content domains, examination content outline | Practice test questions, study guide provision |
| Preconference Workshops | 2.5-4 hours | Specific skills: facilitation, education methods, consultation models | Interactive activities, practical toolkits, assessment frameworks |
| Skills-Based Committee Training | 3 hours | Ethics question formulation, consultation process understanding, stakeholder analysis | Hands-on activities, reflection exercises, barrier identification |
Frameworks and Models for Clinical Ethics Consultation
Established Methodologies for Ethical Analysis
Multiple structured models have been developed to guide the process of clinical ethics consultation, each offering systematic approaches to ethical analysis in healthcare settings. These models provide frameworks for identifying relevant ethical considerations, analyzing competing values, and developing recommendations for resolving ethical dilemmas. The proliferation of distinct methodologies reflects both the complexity of clinical ethics consultation and the ongoing development of the field's theoretical and practical foundations.
Four prominent models demonstrate the diversity of approaches available to ethics consultants and committees:
- The "Four Box" Method (Jonsen-Siegler-Winslade): This approach organizes ethical analysis into four domains: medical indications, patient preferences, quality of life, and contextual features, providing a comprehensive structure for case review [50].
- The Orr-Shelton Method: This model outlines a formal process for completing and documenting ethics consultation that mirrors other clinical consultation models in medicine, emphasizing integration with standard medical workflows [50].
- The Zurich Model: This seven-step protocol facilitates moral inquiry, deliberation, and consensus through effective communication, mediation, implementation of the plan, and appropriate follow-up [50].
- The QUAR Framework (Children's Mercy Bioethics Center): This method identifies a four-step process for ethics consultation: Question, Understand, Assess, Recommend, providing a streamlined approach to case analysis [50].
Each model offers specific strengths and limitations, particularly in different clinical contexts such as pediatrics, where factors like decision-making authority and child assent require specialized consideration.
The Facilitation Approach in Ethics Consultation
The ASBH has endorsed the facilitation approach as a preferred model for ethics consultation, emphasizing process-based methods that help stakeholders identify and analyze ethical issues themselves rather than relying on the ethics consultant as an authoritative decision-maker [50]. This approach prioritizes skilled facilitation of discussions among healthcare providers, patients, and families, particularly in situations characterized by high emotions, conflicting values, or communication breakdowns.
Advanced facilitation training for ethics consultants addresses specific challenges in group dynamics and conflict management. As noted in ASBH workshops, "mastery of multi-party facilitation is one of the core competencies," yet "many ethics consultants have not been trained in facilitation techniques" despite empirical data showing that "the majority of US clinical ethicists hold group meetings with clinical staff, patients, and families as part of an ethics consult" [50]. The facilitation model requires consultants to manage group interactions effectively while avoiding values imposition—ensuring that the consultant's own moral perspectives do not unduly influence the outcome of the consultation.
Operational Structures and Institutional Implementation
Committee Composition and Multidisciplinary Integration
Hospital ethics committees typically comprise diverse membership across clinical and non-clinical disciplines, reflecting the multidimensional nature of ethical dilemmas in healthcare. Core members often include physicians from various specialties, nurses, social workers, chaplains, hospital administrators, legal counsel, and community representatives with ethics expertise [52]. This multidisciplinary composition ensures that ethical analyses consider diverse perspectives, including clinical realities, patient and family experiences, institutional policies, legal frameworks, and philosophical or theological considerations.
The effectiveness of ethics committees depends significantly on this diversity of membership and the integration of different disciplinary viewpoints. As noted in ASBH guidelines, ethics committees are designed for "physicians, nurses, attorneys, historians, philosophers, professors of literature and the humanities, members of the clergy, hospital chaplains, social workers, and others engaged in endeavors related to clinical and academic bioethics and the health-related humanities" [52]. This inclusive approach recognizes that ethical dilemmas in healthcare extend beyond medical technicalities to encompass fundamental questions about values, relationships, and human flourishing that benefit from multiple perspectives.
Educational Functions and Skills Development for Committee Members
Beyond case consultation, ethics committees serve crucial educational functions within healthcare institutions, providing ethics education to staff, patients, and the broader community. However, committee members themselves often require specialized training to contribute effectively to the committee's work. As noted in contemporary practice, "clinician volunteers likely have inconsistent education in clinical ethics," and "often, committee education focuses on theoretical knowledge and case discussions with little emphasis on practical skills" [50].
Innovative approaches to committee member education now emphasize skills-based training that enables all committee members to understand the ethics consultation process, regardless of whether they lead consultations themselves. Such training focuses on practical skills such as "how to structure and write ethics questions," "naming stakeholders and their values," and understanding "how defining the action under consideration guides the rest of the consult" [50]. This approach enhances the committee's collective capacity to address ethical dilemmas by ensuring that all members possess foundational skills in ethical analysis and consultation processes.
Table 3: Essential Resources for Clinical Ethics Consultation Services
| Resource Category | Specific Tools | Application in Ethics Consultation |
|---|---|---|
| Foundational References | Core Competencies for Ethics Consultation [51], ASBH HEC-C Study Guide [50] | Standardized knowledge base, certification preparation, consistent approach to consultation |
| Assessment Frameworks | Four Box Method, QUAR Framework, Zurich Model [50] | Structured case analysis, comprehensive ethical assessment, documentation standards |
| Educational Materials | Humanities-based resources (film, visual art, narrative) [50], Case studies, Policy documents | Committee education, staff development, values clarification exercises |
| Process Tools | Facilitation techniques [50], Conflict management protocols, Documentation templates | Meeting management, stakeholder engagement, consensus building |
Contemporary Challenges and Evolving Practices
Addressing Moral Distress in Healthcare Settings
A significant development in clinical ethics practice is the formal recognition of and response to moral distress among healthcare providers. Moral distress occurs when providers know the ethically appropriate action to take but cannot carry it out due to institutional, procedural, or hierarchical constraints. The integration of moral distress consultation into clinical ethics services represents an expansion of the traditional scope of ethics consultation beyond case-specific ethical dilemmas to include the psychological and emotional impact of ethical conflicts on healthcare professionals.
Specialized training programs now incorporate moral distress consultation as a distinct competency area. For example, the University of Virginia's program notes it is "the only program in the United States to offer training in Moral Distress consultation, building on 18 years of experience at UVA Health" [51]. This evolution reflects growing recognition that ethical issues in healthcare extend beyond discrete case consultations to include the broader ethical environment in which healthcare professionals work and the systemic factors that impact their moral agency and well-being.
Navigating Policy and Justice Considerations
Contemporary clinical ethics practice increasingly addresses broader policy and justice considerations that extend beyond individual patient encounters. Ethics consultants and committees now engage with systemic issues that affect populations and institutions, including resource allocation, health disparities, and regulatory compliance. This expanded scope reflects recognition that many ethical dilemmas in clinical practice are shaped or constrained by larger systemic and policy factors.
Recent ethical analyses have addressed justice considerations in healthcare policy, examining how policy decisions affect vulnerable populations and access to care. For instance, analyses have considered how "federal policy changes" that "strip many immigrants of access to essential health and social services" raise fundamental questions about justice and fairness in healthcare [53]. Such analyses demonstrate how clinical ethics increasingly engages with the intersection of healthcare policy, distributive justice, and institutional decision-making, expanding the traditional boundaries of clinical ethics consultation beyond the bedside to include organizational and policy ethics.
The development of clinical ethics consultation and hospital ethics committees represents a significant achievement in the institutionalization of bioethics within the United States healthcare system. From early informal consultations to contemporary structured services with certified consultants, standardized competencies, and specialized training programs, the field has matured into an established component of healthcare delivery. This evolution reflects both the growing complexity of ethical dilemmas in modern medicine and the healthcare system's recognition of its responsibility to address these dilemmas systematically.
The continued development of the field—including the formalization of certification processes, refinement of consultation models, expansion into moral distress consultation, and engagement with policy-level ethics—demonstrates the dynamic nature of clinical ethics practice. As healthcare continues to evolve with technological advances, changing regulatory environments, and shifting societal values, clinical ethics consultation and hospital ethics committees will continue to play a crucial role in ensuring that ethical considerations remain central to healthcare decision-making at all levels, from the bedside to the boardroom.
The establishment of bioethics as an academic discipline represents a critical development in the professionalization of a field that emerged in response to unprecedented ethical challenges in medicine and the life sciences. The modern era of health care ethics is often traced to Henry Beecher's influential 1966 article on ethical problems in clinical research, which highlighted the failure to inform patients of risks in experimental treatments [3]. This seminal work identified ethical problems arising from the explosive postwar growth of medical research, creating a gap between established professional practices and the need to address new moral dilemmas [3]. The academic institutionalization of bioethics began in earnest with the founding of the Hastings Center in 1969, followed by the Kennedy Institute of Ethics at Georgetown University in 1971 [3]. These institutions provided the foundational infrastructure for bioethics as a formal field of study, moving beyond physician-centered medical ethics to encompass the entire spectrum of the human life sciences [3] [4].
This institutionalization process occurred within a specific socio-historical context where advances in medical science, the rise of consumer rights, and legal developments emphasizing patient autonomy converged to create demand for formal educational programs [3]. The field that emerged was characterized by its interdisciplinary nature, drawing from moral philosophy, medical philosophy, and theology while developing scientific methods inspired by the humanities and social sciences [54]. This whitepaper examines the development, current status, and methodological approaches of bioethics degree programs within academic institutions, with particular attention to the United States context and its implications for researchers, scientists, and drug development professionals.
Historical Foundations and Theoretical Framework
The Paradigm Shift from Traditional Medical Ethics to Bioethics
The transformation from traditional medical ethics to modern bioethics represented a significant paradigm shift in how society approached ethical questions in medicine and scientific research. Prior to the 1960s, medical ethics remained largely confined to the Hippocratic tradition and focused almost exclusively on patient welfare and medical professionalism [4]. This physician-centered approach began to show limitations when confronted with dramatic advances in medical technology and changing social values. Several key factors drove this transformation:
Scientific and Technological Advances: The development of penicillin, sulfa drugs, polio vaccine, radiation therapy, and chemotherapy created new capabilities that raised unprecedented ethical questions about life, death, and human intervention [3]. The era of modern medicine fostered an "almost unqualified optimism" within the medical profession, where physicians saw themselves as "applied scientists" marshalling technical resources against disease [3].
Legal and Social Movements: The 1957 Salgo case established the legal doctrine of informed consent, restricting physicians' traditional authority and requiring that patients be provided with all relevant information about treatment alternatives [3]. Concurrently, President John F. Kennedy's 1962 address on consumer rights—including the right to safety, the right to be informed, the right to choose, and the right to be heard—lent a rights-oriented framework to the relationship between patients and healthcare providers [3].
Philosophical Expansion: Bioethics distinguished itself from traditional medical ethics by casting "a wide net, moving from the most intimate doctor-patient encounters at the bedside to the most public kinds of decisions on the provision of health care" [4]. This expansion required working through the full spectrum of issues from profound questions of human nature and dignity to practical policy matters regarding healthcare delivery systems [4].
Theoretical Underpinnings: Principlism and Its Evolution
The theoretical framework of modern bioethics education initially coalesced around principlism, particularly the four principles outlined in the Belmont Report: autonomy, beneficence, non-maleficence, and justice [54]. This approach provided a structured method for analyzing ethical dilemmas in healthcare and research contexts. However, the field has since evolved to incorporate more inductive methodologies and diverse ethical frameworks [54].
The educational philosophy underlying bioethics degree programs emphasizes not only theoretical knowledge but also the development of practical moral reasoning. As Culver contends, "Bioethics education programs should not directly teach attitudes but rather focus on the identification of ethical conflicts that arise in clinical practice" with students internalizing "the process for a rational response" [54]. This approach aligns with Kohlberg's stages of moral development, which inform curriculum design aiming to help students progress toward post-conventional thinking characterized by moral autonomy and judgments based on universal principles of justice [54].
Current Landscape of Bioethics Degree Programs
The integration of bioethics into higher education has resulted in the establishment of formal degree programs at numerous institutions across the United States. For the 2025 academic year, College Factual identified 67 colleges in the United States offering programs in bioethics/medical ethics, awarding approximately 4,980 degrees annually [55]. The distribution of these programs spans various institutional types and degree levels, with early-career professionals earning an average salary of $88,062 [55].
Table 1: Top-Ranked Bioethics Degree Programs in the United States (2025)
| Institution | Degree Types | Degrees Awarded (Most Recent Data) | Key Characteristics |
|---|---|---|---|
| University of Pennsylvania | Master's (3 program types) | 25 Master's degrees (2023) | Private Ivy League institution; Ranked #2 nationally; $80,564 median starting salary [55] [56] |
| Johns Hopkins University | Master's, Certificate | 19 total (17 Master's, 2 Certificates - 2023) | Very large private research university; Ranked #6 nationally [55] [56] |
| Duke University | Master's | 23 Master's degrees (2023) | Large private university; Ranked #7 nationally [55] [56] |
| University of Rochester | Bachelor's, Master's | 6 Bachelor's degrees (2023) | Private university; 41 medical ethics degrees awarded in most recent data year [55] [56] |
| Case Western Reserve University | Master's (2 program types) | 36 Master's degrees (2023) | Large private university; Multiple program options [56] |
| New York University | Master's | 14 medical ethics degrees awarded | Private university; 50% growth in graduates [55] |
Table 2: Bioethics Program Distribution by Degree Level and Institutional Characteristics
| Institution Type | Most Common Degree Levels | Typical Program Features | Enrollment Patterns |
|---|---|---|---|
| Private Research Universities | Master's Degrees | Interdisciplinary curricula; Clinical ethics focus; Faculty from medicine, law, philosophy | Mix of pre-professional and mid-career students |
| Public Universities | Bachelor's, Master's | Policy emphasis; Broader ethical frameworks; Community engagement | Larger undergraduate enrollment; Diverse career goals |
| Specialized Health Sciences Centers | Certificates, Doctoral | Clinical application focus; Research ethics; Practical skill development | Primarily working health professionals; Research ethics administrators |
| Online Institutions | Master's, Certificates | Flexible formats; Structured curricula; Standardized assessments | Working professionals; Geographic diversity; Career changers |
Curriculum Architecture and Core Competencies
Bioethics degree programs typically employ a tiered educational approach that distinguishes between foundational knowledge and applied clinical ethics. The "common model" for bioethics education subdivides learning into "competencies to be achieved," "knowledge," and "skills" [54]. Program architectures generally follow a progressive structure:
- Preclinical Period: Basic bioethics introducing fundamental theoretical content
- Clinical Period: Applied clinical ethics enabling students to resolve specific conflicts in practice [54]
This structure recognizes that moral development requires the progression through cognitive stages, from pre-conventional to post-conventional thinking, where individuals establish moral autonomy and can make judgments based on universal principles of justice [54].
Core competencies addressed in bioethics curricula include:
- Ethical Reasoning Skills: Ability to identify ethical issues, analyze dilemmas using multiple frameworks, and develop reasoned conclusions
- Interdisciplinary Knowledge: Understanding of philosophical theories, legal precedents, clinical contexts, and cultural considerations
- Policy Analysis: Capacity to evaluate and develop institutional policies, clinical guidelines, and regulatory frameworks
- Communication and Mediation: Skills to facilitate ethics consultations, lead deliberations, and communicate effectively across diverse stakeholders
The educational methodology increasingly employs problem-based learning (PBL), which allows students to acquire not only theoretical content but also reflective and evaluative abilities, plus the competencies necessary to resolve profession-specific situations [54]. This approach aligns with the recognition that bioethics education must bridge the theory-practice divide, preparing graduates for real-world ethical challenges in research and clinical settings.
Methodological Approaches in Bioethics Education
Pedagogical Framework and Instructional Strategies
Bioethics education employs diverse pedagogical approaches designed to foster both theoretical understanding and practical application. The following diagram illustrates the structured pathway from foundational knowledge to professional application in bioethics education:
Effective bioethics instruction combines multiple methodological approaches to address both cognitive and affective learning domains. The predominant instructional models include:
Integrated Curriculum Models: Bioethics content is woven throughout the educational experience rather than being confined to standalone courses. This approach recognizes that ethical considerations are inherent to all aspects of healthcare and research practice [54].
Problem-Based Learning (PBL): Students work through complex, real-world cases in small groups, developing skills in ethical analysis, collaborative decision-making, and moral reasoning [54]. This methodology emphasizes the process of ethical deliberation rather than merely arriving at "correct" answers.
Simulated Clinical Encounters: Structured simulations using standardized patients or virtual scenarios allow students to practice ethics consultation skills, communication techniques, and interprofessional collaboration in controlled environments [54].
Critical Incident Analysis: Examination of actual ethical dilemmas from clinical and research settings provides students with opportunities to analyze complex situations, identify key decision points, and consider alternative approaches [54].
Assessment Methodologies for Bioethics Competencies
The evaluation of bioethics education presents distinct challenges due to the complexity of assessing competencies, attitudes, and behaviors aligned with ethical values [54]. The academic community has developed and implemented multiple assessment strategies:
Table 3: Assessment Methods in Bioethics Education
| Assessment Method | Application in Bioethics | Measured Competencies | Limitations |
|---|---|---|---|
| Objective Structured Clinical Examination (OSCE) | Standardized scenarios testing ethical reasoning and communication | Knowledge application; Ethical action in clinical situations; Communication skills | Unable to assess behaviors based on acquired ethical values [54] |
| Hirsch Professional Ethics Scale | 55-item instrument using 5-point Likert scale | Cognitive competencies; Social competencies; Ethical competencies; Affective-emotional competencies | Based on self-reporting; May not predict actual behavior [54] |
| Problem Identification Test | Clinical cases assessing recognition of moral problems | Ability to recognize existence of moral problems; Application of autonomy, beneficence, justice principles | Limited to recognition rather than resolution skills [54] |
| Three-Stage Assessment Model (Vera Carrasco) | Diagnostic, formative, and summative evaluation phases | Theoretical foundation; Learning progression; Knowledge quantification | Requires significant faculty time and resources [54] |
Couceiro-Vidal emphasizes the importance of assessment methods that can "objectively assess bioethics learning in the clinical professional's practice," acknowledging the complexity of the entire process and following a similar curriculum design structure as other subjects [54]. This typically involves a sequenced approach beginning with diagnostic assessment, progressing through formative evaluation, and concluding with summative assessment that allows for identification of weaknesses and self-assessment by both instructor and student [54].
Core Research Reagent Solutions for Bioethics Scholarship
Bioethics research employs distinctive methodological tools and conceptual frameworks that function as the discipline's equivalent of "research reagents." These analytical instruments enable systematic investigation of ethical questions in healthcare and scientific research:
Table 4: Essential Research Resources in Bioethics Scholarship
| Research Tool | Function | Application Context | Key Features |
|---|---|---|---|
| Principlism Framework | Structured ethical analysis using four core principles | Clinical ethics consultation; Research ethics review; Policy development | Applies autonomy, beneficence, non-maleficence, justice; Provides common moral language [54] |
| Case-Based Deliberation | Method for analyzing specific ethical dilemmas | Ethics committee deliberations; Classroom instruction; Policy formulation | Context-sensitive analysis; Identifies stakeholders; Considers alternative actions and outcomes |
| Qualitative Research Methods | Empirical study of ethical phenomena and decision-making | Interview studies; Ethnographic observation; Document analysis | Explores lived experience of ethical issues; Generates rich contextual data |
| Policy Analysis Toolkit | Systematic evaluation of healthcare policies and regulations | Institutional policy development; Legislative analysis; Regulatory compliance | Assesses ethical implications of policies; Identifies unintended consequences |
| Historical Analysis | Examination of historical cases and evolving ethical norms | Understanding contemporary issues through historical context; Tracing conceptual development | Reveals historical precedents; Illuminates cultural and technological influences |
Implementation Framework for Bioethics Programs
The establishment of effective bioethics programs requires careful attention to institutional structures, resource allocation, and faculty development. The following diagram illustrates the key components and their relationships in implementing bioethics education:
Successful implementation depends on addressing several critical factors identified in research on bioethics education:
Institutional Commitment: Bioethics must be recognized as "an important field" with formal structural support rather than being "left to the discretion of individual institutions" [57]. This includes dedicated resources, administrative support, and inclusion in institutional mission statements.
Faculty Development: A primary challenge is the "shortage of trained faculty" capable of effectively teaching bioethics concepts and methodologies [57]. Successful programs invest in developing faculty expertise through training programs, mentoring, and professional development opportunities.
Curriculum Integration: Bioethics education should be "shuffled between different disciplines" but rather have a defined place in the curriculum while also being integrated across multiple learning experiences [57]. The most effective programs combine standalone bioethics courses with ethics integration throughout the curriculum.
Contextual Adaptation: Programs must consider "regional and disciplinary differences" to ensure that bioethics education addresses the specific needs and challenges faced by students in their professional contexts [54]. This includes attention to cultural factors, healthcare system characteristics, and professional requirements.
Global Perspectives and Comparative Analysis
International Context of Bioethics Education
The development of bioethics education has followed distinct trajectories in different national contexts, reflecting varying cultural, political, and healthcare systems. A comparative analysis reveals both common challenges and distinctive approaches:
United States Model: Characterized by early institutionalization through organizations like the Hastings Center and Kennedy Institute, with integration into higher education and professional training [3]. The U.S. model emphasizes individual rights, patient autonomy, and a pluralistic approach to ethical reasoning.
European Approaches: European bioethics has maintained a somewhat different character, with "mixed response" to the American model despite worldwide spread of the bioethics movement [3]. European approaches often place greater emphasis on social solidarity and community interests alongside individual rights.
Pakistan Context: Research from Karachi demonstrates challenges common in many developing nations, including "sporadic inclusion of bioethics in undergraduate medical curricula" and dependence on individual institutional initiatives rather than systematic implementation [57]. Studies show that only 3 of 13 medical colleges in Karachi mentioned "ethics" in their vision and mission statements, and none had dedicated departments for bioethics education [57].
Cross-Cultural Comparisons: Research comparing adolescent perspectives on bioethics in the United States and Pakistan found that while 85% of respondents believed bioethics is an important field of study for young people, 86% also perceived "a lack in bioethics outreach and education" [58]. The study found statistically significant differences between students from the two countries regarding perceptions of minors' rights, highlighting how sociocultural contexts shape ethical perspectives [58].
Implementation Challenges Across Contexts
Despite variations in cultural and institutional contexts, bioethics education faces common implementation challenges across national settings:
Structural Barriers: "Lack of institutional buy-in and overcrowded curriculum" present significant obstacles to integrating bioethics education effectively [57]. Without mandatory inclusion required by regulatory bodies, bioethics often remains "an orphan subject in the curricula" [57].
Faculty Limitations: The "shortage of trained faculty" represents a critical challenge across contexts [57]. Even when institutions recognize the importance of bioethics education, they may lack personnel with the necessary expertise to develop and deliver effective instruction.
Assessment Difficulties: The "novelty of the discipline and the multitude of application contexts" complicate the assessment of bioethics learning [54]. Developing valid and reliable methods to evaluate ethical reasoning skills and professional formation remains an ongoing challenge.
Resource Constraints: Limited institutional resources often restrict the implementation of effective bioethics education, particularly for experiential components such as simulated scenarios and small-group discussions that require favorable faculty-to-student ratios.
The establishment of bioethics degrees and programs in academic institutions represents a significant achievement in the professionalization and institutionalization of a field that emerged in response to unprecedented ethical challenges in medicine and the life sciences. From its modest beginnings in the 1960s, bioethics education has evolved into a structured academic discipline with defined curricula, methodological approaches, and assessment strategies.
The current landscape of bioethics education reflects both the maturation of the field and ongoing challenges in implementation and integration. While top-tier institutions have developed sophisticated educational programs, broader implementation faces barriers related to institutional commitment, faculty expertise, and curriculum capacity. The future development of bioethics education will likely require increased attention to several key areas:
Standardization and Accreditation: Development of clearer standards for bioethics education and accreditation requirements that ensure minimum competencies while allowing for contextual adaptation.
Faculty Development: Expanded efforts to prepare faculty with expertise in both bioethics content and effective pedagogical methods for ethics education.
Evidence-Based Pedagogy: Continued research on the effectiveness of different educational approaches and assessment methods to identify best practices for bioethics instruction.
Global Collaboration: Enhanced international cooperation to address cross-cultural ethical challenges and share resources for bioethics education across diverse contexts.
Early Integration: Expansion of bioethics education to earlier educational levels, recognizing that "adolescents demonstrate awareness of bioethical issues" and that "issues relevant to their context require integration into the mainstream curricula at the high school level" [58].
For researchers, scientists, and drug development professionals, the continued evolution of bioethics education represents both a resource and a responsibility. As scientific advances continue to generate novel ethical challenges, the availability of sophisticated bioethics expertise becomes increasingly essential for responsible research conduct and healthcare innovation. Simultaneously, these professionals have an important role to play in shaping the future development of bioethics education by articulating the ethical challenges they encounter and collaborating with bioethics scholars to develop responsive educational approaches.
The institutionalization of bioethics degrees and programs stands as a testament to the recognition that scientific and technological capabilities must be guided by thoughtful ethical consideration. As the field continues to evolve, this educational infrastructure will play an increasingly vital role in ensuring that scientific progress remains aligned with human values and social priorities.
The evolution of bioethics from a domain of philosophical discourse to a distinct profession represents a significant development in modern healthcare and scientific research. This professionalization emerged as a response to unprecedented ethical challenges generated by post-World War II advances in medical science and technology [3]. The field has systematically developed from abstract ethical deliberation into a concrete occupational role characterized by formal positions, specialized expertise, and institutional authority [59]. This transformation is particularly evident in the United States, where bioethicists have established themselves as essential figures in research oversight, clinical consultation, and corporate governance within the life sciences industry [60] [61] [62].
The professionalization process reflects broader sociological patterns of occupational development, wherein groups of workers organize around a defined jurisdiction of knowledge and practice [59]. For bioethicists, this jurisdiction encompasses the ethical dimensions of biomedical research, clinical care, and public health policy. This paper traces the historical emergence of the bioethicist as a distinct professional role within the United States research context, examining the institutional structures that supported this development and the contemporary functions that now characterize the profession.
Historical Foundations and Catalysts for Professionalization
The Pre-Professional Era: Ethical Questions Without Specialized Roles
Prior to the formal emergence of bioethics as a field, ethical considerations in medicine and research largely fell within the purview of individual clinicians and researchers. The traditional medical ethic, centered on the Hippocratic Oath, had remained substantially unchanged for centuries and presumed that physicians could adequately address ethical questions through professional conscience [3]. This approach proved insufficient as medical technology advanced, creating novel ethical dilemmas that extended beyond the scope of traditional medical ethics.
The post-World War II period witnessed rapid therapeutic advances, including the development of sulfa drugs, penicillin, chemotherapy, and advanced surgical techniques [3]. These innovations created what historian Henry Beecher termed "unprecedented ethical problems in the care of patients" [3]. Beecher's influential 1966 article on ethical problems in clinical research highlighted failures to inform patients of risks in experimental treatments, signaling the need for more systematic attention to research ethics [3]. During this pre-professional period, ethical deliberation remained decentralized, with no established career path for specialists in biomedical ethics.
Foundational Institutions: Creating Organizational Infrastructure
The institutionalization of bioethics began with the establishment of dedicated organizations that would provide the structural foundation for professional development. The Hastings Center (founded in 1969) and the Kennedy Institute of Ethics (founded in 1971) served as the initial pillars of this emerging field, creating organizational homes for scholarly work and developing the intellectual frameworks that would define bioethics as a distinct domain of expertise [3].
These institutions facilitated the transformation of bioethics from scattered ethical deliberations into a coherent field of study with its own literature, conferences, and eventually, educational programs. The Hastings Center in particular took the lead "in setting the direction, methods, and intellectual standards of bioethics through its own journal, the Hastings Center Report" [3]. This institutionalization was crucial for establishing bioethics as a recognized area of specialized knowledge, a necessary precondition for professionalization.
Table 1: Key Institutional Developments in the Professionalization of Bioethics
| Year | Institutional Development | Significance for Professionalization |
|---|---|---|
| 1966 | Henry Beecher's landmark article on ethical problems in clinical research | Identified systematic ethical failures in medical research, demonstrating need for specialized oversight [3] |
| 1969 | Founding of The Hastings Center | Created first dedicated organizational home for bioethics scholarship [3] |
| 1971 | Founding of Kennedy Institute of Ethics at Georgetown University | Established academic infrastructure for bioethics education and training [3] |
| 1970s-1980s | Emergence of Institutional Review Boards (IRBs) | Created formal employment opportunities for bioethics expertise [59] |
| 1990s-Present | Corporate bioethics committees in pharmaceutical companies | Expanded professional roles beyond academia and clinical settings [61] [62] |
Legal and Social Catalysts: Creating Demand for Specialized Expertise
Concurrent with institutional developments, legal and social changes created demand for specialized bioethics expertise. The informed consent doctrine established in the 1957 Salgo case legally mandated that physicians provide patients with relevant information about treatment alternatives and risks, fundamentally shifting decision-making authority from physicians to patients [3]. This legal development created a need for professionals who could navigate the ethical complexities of patient autonomy and medical decision-making.
The consumer rights movement of the 1960s further accelerated this process by introducing a rights-based framework to healthcare. President John F. Kennedy's 1962 address to Congress outlining four basic consumer rights—safety, information, choice, and representation—provided a conceptual foundation for patient rights that would increasingly shape healthcare ethics [3]. These social and legal developments created a environment where the specialized knowledge of bioethicists became increasingly valuable, both for healthcare institutions seeking to navigate new legal requirements and for researchers addressing evolving ethical standards for human subjects protection.
The Professionalization Pathway: From Occupation to Profession
Defining the Professional Domain: The "Jurisdiction" of Bioethics
The professionalization of bioethics follows sociological patterns observed in other emerging professions, characterized by efforts to define and control a particular "jurisdiction" of work [59]. Bioethicists have established their professional domain by creating a unique knowledge base combining elements of philosophy, law, medicine, and social science, and applying this knowledge to specific institutional contexts. This jurisdiction includes several core functions: research ethics consultation, clinical ethics support, policy development, and scholarly analysis of emerging ethical issues in biomedicine [59].
The professionalization process has involved what sociologists term "ecological struggle" over occupational territory [59]. Bioethicists have carved out their professional space between previously established domains of medicine, law, and academic philosophy. This has required both demonstrating the unique value of bioethics expertise and navigating tensions with other professionals, particularly physicians accustomed to exercising sole authority over ethical decisions in clinical and research settings.
Structural Professionalization: Committees, Certification, and Career Paths
The professionalization of bioethics has become concretely embodied in formal organizational structures. Institutional Review Boards (IRBs) represent one of the earliest and most widespread institutional homes for bioethics expertise, creating formal roles for professionals specializing in research ethics [59]. The regulatory requirement for IRB review of research protocols ensured a steady demand for bioethics knowledge, establishing a concrete professional pathway.
Within the pharmaceutical industry, dedicated bioethics committees and programs have emerged as standard components of organizational infrastructure. Companies including Johnson & Johnson and Eli Lilly have established formal bioethics committees with multidisciplinary membership, creating corporate positions for bioethics professionals [61] [62]. These committees provide guidance on ethical issues in research, development, and commercialization, representing the integration of bioethics into corporate governance structures.
Table 2: Bioethics Professional Roles and Institutional Settings
| Professional Role | Institutional Setting | Core Functions |
|---|---|---|
| IRB Member/Chair | Academic medical centers, research institutions | Protocol review, ensuring regulatory compliance, protecting human subjects [59] |
| Clinical Ethics Consultant | Hospitals, healthcare systems | Ethics consultation services, policy development, staff education [59] |
| Corporate Bioethicist | Pharmaceutical companies, biotech firms | Guidance on ethical issues in R&D, product development, and commercialization [60] [61] [62] |
| Academic Bioethicist | Universities, research institutes | Teaching, scholarship, theoretical framework development [3] [59] |
| Policy Advisor | Government agencies, advisory commissions | Development of ethical guidelines, regulatory frameworks, public policy [59] |
The professionalization process has also included efforts to establish formal credentials and standards of practice. While bioethics does not yet have uniform licensure requirements, various certification programs have emerged, such as the Healthcare Ethics Consultant-Certified (HEC-C) credential, representing ongoing efforts to standardize professional qualifications [59]. This movement toward certification reflects what sociologists identify as a typical stage in professionalization, where occupational groups seek to control entry and establish quality standards [59].
Contemporary Applications: Bioethicists in Pharmaceutical Research and Development
Biopharmaceutical Bioethics: Defining a Specialty
The application of bioethics within the biopharmaceutical industry has emerged as a distinct specialty within the broader field. "Biopharmaceutical bioethics" has been defined as "the application of bioethics norms (concepts, principles, and rules) to the research, development, supply, commercialization, and clinical use of biopharmaceutical healthcare products" [60]. This specialization reflects the ongoing differentiation within bioethics as professionals develop expertise tailored to specific contexts.
Biopharmaceutical bioethics addresses unique ethical challenges arising at the intersection of life sciences, clinical research, clinical care, public health, and business [60]. Professionals in this domain must navigate contextual factors including dual missions of patient care and business imperatives, multiple stakeholder interests, and operational complexities inherent in drug development and commercialization [60]. This specialized knowledge base further reinforces the professional distinctiveness of bioethicists working in industry settings.
Embedded Ethics: Methodologies for Integration
A significant development in contemporary bioethics practice is the "Embedded Ethics" approach, which involves integrating ethicists directly into research teams [63]. This methodology positions bioethicists as collaborative partners throughout project lifecycles, rather than as external reviewers. In the 4D PICTURE project focused on developing data-driven decision support tools in oncology, embedded ethicists work alongside researchers to identify and address ethical issues in real-time [63].
The Embedded Ethics approach represents a natural evolution in the professionalization of bioethics, moving from reactive consultation to proactive integration. This methodology includes iterative review processes, collaborative analysis of ethical challenges, and development of tailored frameworks for specific research contexts [63]. The approach demonstrates how the bioethicist's role has expanded beyond theoretical analysis to active participation in research design and implementation.
Diagram 1: The professional evolution of bioethics from medical ethics to embedded practice. This pathway shows the progression from physician-centered ethics to contemporary integrated approaches, with key developments at each stage.
Quantitative Evidence of Professionalization: Growth in Bioethics Integration
Recent quantitative analysis provides evidence of the growing integration of ethical oversight in biomedical research. A systematic review of PubMed-indexed studies from 2018-2022 revealed a statistically significant yearly increase in studies utilizing anonymized data, with an increase of 2.16 articles per 100,000 when normalized against total PubMed articles (p = 0.021) [64]. This trend reflects the institutionalization of privacy ethics as a standard consideration in research design and reporting.
The geographical distribution of ethical practices in research further demonstrates the professional infrastructure supporting bioethics. Studies utilizing anonymized data were predominantly conducted in the United States (53.1% of first authors), United Kingdom (18.2%), and Australia (5.3%), with these countries establishing influential models for ethical oversight [64]. This distribution reflects how specific national contexts have shaped the professional development of bioethics, with the U.S. playing a particularly prominent role.
Table 3: Quantitative Evidence of Bioethics Integration in Research (2018-2022)
| Metric | Findings | Significance for Professionalization |
|---|---|---|
| Annual growth in studies using anonymized data | Significant yearly increase of 2.16 articles per 100,000 (p = 0.021) [64] | Demonstrates institutionalization of ethical practices in research methodology |
| Geographical distribution of ethical practices | US (53.1%), UK (18.2%), Australia (5.3%) dominate research using anonymized data [64] | Reflects established professional infrastructure in these countries |
| Cross-border data sharing | Rare (only 10.5% of studies) despite comparable regulations [64] | Highlights need for global standards and international professional collaboration |
| Common data sources | 12 identified sources, primarily in US (7) and UK (3), including commercial (7) and public entities (5) [64] | Indicates established systems for ethical data management across sectors |
The Bioethicist's Toolkit: Frameworks, Methods, and Applications
Core Ethical Frameworks and Their Application
Bioethics professionals employ several established frameworks to analyze ethical issues in research and clinical care. Principlism, based on the four principles of autonomy, beneficence, non-maleficence, and justice, provides a foundational approach for ethical analysis [60] [65]. These principles are progressively specified for different contexts, with informed consent requirements, for example, taking distinct forms in clinical care versus research settings [60].
The application of these frameworks occurs at multiple levels within organizations. At a company guidance level, bioethicists develop policies on topics like pediatric medicine development or compassionate use of experimental therapies [60] [61]. At a case-specific level, they provide guidance on particular ethical dilemmas, such as adaptive clinical trial designs or expanded access programs for investigational drugs [60]. This multi-level application demonstrates how bioethics professionals operate across organizational strata, from high-level policy to specific research decisions.
Methodologies for Ethical Analysis and Consultation
Bioethics professionals utilize structured methodologies for ethical analysis and consultation. These include:
- Specification: "Substantive refinement of the range and scope of norms" for policy development [60]
- Balancing: "Deliberation and judgment about the relative weights or strengths of norms" for individual cases [60]
- Stakeholder engagement: Systematic consultation with patients, researchers, and other stakeholders to inform ethical analysis [66] [61]
- Comparative analysis: Examination of ethical approaches across different jurisdictions and cultural contexts [59]
The Embedded Ethics approach represents an emerging methodology that involves continuous collaboration between ethicists and researchers [63]. This method includes "iterative process of identifying ethical themes," "member checks" with research teams, and development of "tailored review approaches" for specific projects [63]. This methodology represents an evolution from external review to integrated collaboration, reflecting the ongoing professional development of bioethics practice.
Table 4: Essential Methodologies in Professional Bioethics Practice
| Methodology | Application Context | Professional Function |
|---|---|---|
| Principlism Analysis | Research ethics, clinical ethics | Systematic application of ethical principles to specific cases and policies [60] |
| Specification | Policy development | Refining general ethical norms for specific organizational contexts [60] |
| Balancing | Case consultation | We competing ethical considerations in particular dilemmas [60] |
| Embedded Ethics | Research teams | Continuous ethical integration throughout project lifecycles [63] |
| Stakeholder Engagement | Policy development, program design | Incorporating diverse perspectives into ethical analysis [66] [61] |
| Comparative Analysis | International research, global policy | Understanding cultural variations in ethical frameworks [59] |
The emergence of the bioethicist as a distinct professional role represents a significant development in the institutionalization of ethics within American healthcare and research. From its origins as an external critique of medical practice, bioethics has evolved into an established profession with defined roles, career paths, and institutional authority. This professionalization process has been driven by technological advances, legal requirements, and social expectations that created demand for specialized expertise in navigating ethical dimensions of biomedical progress.
The contemporary professional bioethicist operates across multiple domains—research oversight, clinical consultation, corporate governance, and policy development—demonstrating the field's successful establishment of a distinct professional jurisdiction. The ongoing development of specialized methodologies, such as the Embedded Ethics approach, indicates continued professional evolution as bioethicists refine their practices to address emerging challenges in healthcare and research.
As biomedical technologies continue to advance, generating novel ethical questions, the professional bioethicist has become an institutional necessity rather than a philosophical luxury. The professionalization of bioethics represents a structural adaptation to the complexities of modern medicine, ensuring that ethical considerations remain integral to scientific progress and healthcare delivery.
Contemporary Challenges and Evolving Ethical Dilemmas in U.S. Bioethics
The institutionalization of bioethics in the United States represents a critical response to historical ethical failures in research, establishing a framework designed to protect human dignity and autonomy. This framework rests on foundational pillars: valid informed consent and robust conflict of interest management. For today's researchers, scientists, and drug development professionals, these are not merely regulatory hurdles but essential components of scientifically sound and ethically defensible research. The evolution of bioethics, marked by key events and guidelines, has shifted the paradigm from a paternalistic model to one emphasizing participant autonomy and institutional accountability. In this context, "persistent troubleshooting" refers to the proactive, continuous process of identifying and resolving ethical challenges throughout the research lifecycle, ensuring that these core principles are upheld in both letter and spirit, especially when faced with complex, modern research environments involving vulnerable populations, genetic data, and international collaborations [67].
Historical Context and the Institutionalization of Bioethics
The development of a formal bioethics framework in the United States was largely a reactive process, catalyzed by public exposure of ethical abuses in research. This historical trajectory has directly shaped the contemporary emphasis on informed consent and conflict management.
Table: Key Events in the Institutionalization of U.S. Bioethics
| Event/Document | Year | Core Ethical Contribution | Impact on Modern Research |
|---|---|---|---|
| Nuremberg Code | 1947 | Established the absolute necessity of voluntary informed consent | Foundation for all subsequent human subjects research guidelines |
| Belmont Report | 1979 | Articulated core principles: Respect for Persons, Beneficence, Justice | Provided the ethical framework for U.S. Federal Regulations (Common Rule) |
| President's Commission for the Study of Bioethical Issues | 2009-2016 | Addressed contemporary issues like bioethics in international research | Highlighted need for ethical solutions in emerging scientific frontiers [67] |
The work of commissions and thought leaders, such as Dr. Jeremy Sugarman whose expertise encompasses the ethics of informed consent and international HIV prevention research, has been instrumental in applying these historical principles to modern challenges, including gene-editing and global health studies [67]. This historical context underscores that today's requirements are not arbitrary but are hard-won lessons designed to foster public trust and ensure the integrity of the scientific enterprise.
Foundational Ethical Principles and Regulatory Frameworks
The practice of ethical research is guided by a set of interdependent principles that provide a moral compass for decision-making. These principles, deeply embedded in regulatory frameworks, are essential for persistent troubleshooting.
- Respect for Autonomy: This principle acknowledges an individual's right to self-determination and to make decisions based on their own values and beliefs. It is operationalized primarily through the process of informed consent, which requires that participants make decisions voluntarily and with adequate information [68].
- Beneficence and Non-Maleficence: Researchers have an obligation to maximize potential benefits for the participant and society while minimizing foreseeable risks of harm. This includes a continuous assessment of the risk-benefit ratio throughout the study [68].
- Justice: This principle demands a fair distribution of the burdens and benefits of research. It requires that the selection of participants be scrutinized to avoid systematically recruiting groups based on their easy availability or manipulability, rather than on the scientific purpose of the study.
In the legal domain, the concept of informed consent serves as a protective mechanism. Legally, treatment or research involvement without consent may constitute battery. For consent to be valid, it must be given by a person with the capacity to understand the information and must be voluntary [68]. The regulatory framework, including the FDA regulations and the Common Rule, codifies these ethical principles into enforceable standards for research conduct.
The Informed Consent Process: Beyond the Document
Informed consent is a process, not a single event or a form to be signed. It is a continuous, interactive dialogue between the researcher and the potential participant that begins before enrollment and continues throughout the study. The following diagram illustrates the core workflow of a robust informed consent process.
Diagram 1: The Informed Consent Process Workflow
Core Elements of Informed Consent
A valid informed consent process must include clear explanations of several key elements. The following table provides a structured overview of these essential components, offering practical phrasing for researchers.
Table: Core Elements of an Informed Consent Discussion
| Element | Description | Example Phrasing for Researchers |
|---|---|---|
| Purpose & Duration | Clearly state the research purpose, expected duration, and procedures. | "The goal of this study is to... It will involve 6 visits over 3 months. Today's visit will include..." |
| Foreseeable Risks | Describe any reasonably foreseeable risks or discomforts. | "Some participants experience nausea from the drug. There is also a small risk of..." |
| Potential Benefits | Explain any potential benefits to the participant or others. | "You may not benefit directly, but this research could help us learn how to better treat..." |
| Alternative Procedures | Disclose appropriate alternative procedures or courses of treatment. | "Instead of participating in this study, your other options include the standard treatment, which is..." |
| Confidentiality | Describe the extent of confidentiality of records. | "Your records will be kept private to the extent allowed by law. We will use a code number instead of your name in our research files." |
| Compensation/Treatment | Clarify compensation for injury and contact information for questions. | "If you get hurt as a direct result of this study, the costs will be covered by... For any questions, call Dr. X at..." |
| Voluntary Participation | State that participation is voluntary and refusal involves no penalty. | "Deciding to be in this study is entirely your choice. You can stop at any time without any penalty or loss of benefits you are entitled to." |
Assessing Understanding and Capacity
A critical yet often overlooked step is the assessment of the participant's understanding. Simply providing information is insufficient. Researchers should employ techniques such as the "teach-back" method, where participants are asked to explain the study's key aspects in their own words. This practice identifies and rectifies misunderstandings, ensuring consent is truly informed. Furthermore, a participant's capacity to consent is not always static. Researchers must be vigilant for situations where a client or participant "remains unable to consent despite the lawyer’s [or researcher's] best efforts to communicate," which would render the consent invalid [69]. In such cases, appropriate surrogate decision-makers may be involved, following strict regulatory oversight.
Identifying and Managing Conflicts of Interest
Conflicts of interest (COI) arise when a researcher's primary obligations are compromised, or could appear to be compromised, by personal, financial, or other secondary interests. Effective management requires first identifying the specific nature of the conflict.
Categories of Unwaivable Conflicts
Not all conflicts can be resolved by simple disclosure and consent. Some are considered unwaivable because they fundamentally undermine the integrity of the research or professional relationship. The legal profession provides a clear framework for such conflicts, which offers a valuable analogy for high-stakes research environments [69].
Table: Categories of Unwaivable Conflicts of Interest
| Category | Sub-Category | Description | Implication for Research |
|---|---|---|---|
| Informed Consent Cannot Be Obtained | Disclosure Precluded by Confidentiality | A researcher cannot provide adequate disclosure to a participant because doing so would breach confidentiality owed to another subject or collaborator. | The conflict is unwaivable; the research cannot proceed without a protocol that protects all confidences [69]. |
| Client Lacks Capacity to Consent | The participant is incapable of understanding the risks and providing informed consent, and no valid surrogate is available. | The research is not permissible with this population unless specific regulatory conditions for involving vulnerable subjects are met [69]. | |
| Representation Prohibited Despite Consent | Inability to Provide Competent Representation | The researcher's duties to different participants (e.g., in a comparative intervention trial) are so adverse that the researcher cannot provide competent and diligent service to all. | The researcher must withdraw from the conflicted role; separate, independent investigators may be required for different arms of a study [69]. |
| Prohibited by Law | The specific activity or dual role is explicitly forbidden by statute or regulation. | The activity must be avoided entirely; consent is irrelevant (e.g., certain insider relationships in clinical trials) [69]. | |
| Assertion of a Claim Between Clients | The researcher is placed in a position of advancing the interests of one participant against another in a formal proceeding. | The researcher must avoid this situation; it is unwaivable as it creates an inherent adversarial position [69]. |
A Framework for Conflict Management
For conflicts that are not categorically unwaivable, a systematic management approach is required. The following diagram outlines a persistent troubleshooting cycle for identifying, assessing, and managing conflicts of interest.
Diagram 2: The Conflict of Interest Management Cycle
This cycle should be supported by institutional policies. Key mitigation strategies often include:
- Public disclosure of significant financial interests.
- Blinding of data analysis by an independent statistician.
- Independent monitoring of participant safety and data integrity by a Data and Safety Monitoring Board (DSMB).
- Divestiture of a conflicting financial interest or, as a last resort, recusal from the specific research project.
Implementing these ethical principles requires both conceptual understanding and practical tools. The following table details key resources and methodologies that form the researcher's toolkit for ensuring informed consent and managing conflicts.
Table: Research Reagent Solutions for Ethical Practice
| Tool or Resource | Primary Function | Application in Ethical Practice |
|---|---|---|
| Institutional Review Board (IRB) | Independent ethical review and oversight of all research involving human subjects. | Protects participants' rights and welfare by approving, monitoring, and reviewing research protocols and consent forms. |
| Data and Safety Monitoring Board (DSMB) | Independent expert committee that monitors participant safety and treatment efficacy data during a clinical trial. | Manages conflicts related to researcher enthusiasm for positive results by providing unbiased safety oversight. |
| Informed Consent Documentation System | A secure system (digital or paper-based) for storing and tracking signed consent forms. | Provides legal and ethical evidence of the consent process; facilitates audits and verifies participant enrollment. |
| Financial Conflict of Interest (FCOI) Disclosure Software | An electronic system for researchers to regularly disclose significant financial interests. | Streamlines the identification of potential conflicts, ensuring timely review and management by the institution. |
| "Teach-Back" Method Assessment Tool | A structured checklist or script for assessing participant understanding after the consent discussion. | Ensures the consent process is truly informative and interactive, validating the "informed" in informed consent. |
The institutionalization of bioethics in the United States has provided a vital, albeit continually evolving, framework for responsible research conduct. For the modern researcher, informed consent and conflict of interest management are not one-time checkboxes but dynamic processes requiring persistent troubleshooting. This involves a commitment to continuous dialogue with participants, vigilant self-assessment of potential biases, and robust institutional safeguards. By deeply understanding the historical context, foundational principles, and practical tools outlined in this guide, researchers, scientists, and drug development professionals can better navigate the complex ethical terrain of their work. This commitment not only fulfills regulatory mandates but also upholds the highest standards of scientific integrity, preserves public trust, and ultimately honors the invaluable contribution of research participants.
The evolution of bioethics in the United States is deeply rooted in a necessary response to scientific advancement and ethical failure. The modern era of health care ethics is often traced to Henry Beecher's influential 1966 article on ethical problems in clinical research, which highlighted failures to inform patients of risks in experimental treatments [3]. This seminal work emerged from a period where physician authority was nearly absolute, and patients were expected to submit passively to physician decisions [3]. The subsequent founding of The Hastings Center in 1969 and the Kennedy Institute of Ethics in 1971 institutionalized bioethics as a distinct field, moving beyond physician self-regulation toward structured ethical oversight [3]. This historical context frames our current understanding of vulnerable populations and fair subject selection, principles that have evolved from protective paternalism toward a more nuanced balance of inclusion, protection, and justice.
The fundamental tension in contemporary research ethics lies in balancing three competing ethical imperatives: fair inclusion (ensuring representation of clinically relevant populations), fair burden sharing (protecting already burdened populations from further exploitation), and fair opportunity (providing access to research participation) [70]. This technical guide addresses these challenges by providing researchers, scientists, and drug development professionals with practical frameworks for optimizing protections while advancing equitable science.
Historical Foundations of U.S. Research Ethics
From Medical Paternalism to Bioethics
The post-World War II period witnessed unprecedented advances in medical treatment, creating what historians describe as "an environment of almost unqualified optimism within the medical profession" [3]. Physicians increasingly viewed themselves as "applied scientists" battling disease with new pharmacological weapons, often perceiving patients as "little more than the locus of disease" [3]. This technological optimism, however, created an ethical vacuum where patient preferences and rights received minimal consideration.
The cultural and legal landscape began shifting dramatically in the 1960s and 1970s. The 1957 Salgo case established the revolutionary legal doctrine of informed consent, restricting physicians' traditional authority and requiring that patients receive all relevant information about treatment alternatives [3]. Simultaneously, President John F. Kennedy's 1962 address to Congress outlining consumer rights—including the right to safety, information, choice, and to be heard—provided a broader cultural framework that would profoundly influence patient rights movements [3]. These developments created the foundation for recognizing vulnerabilities beyond physical susceptibility to include informational and power imbalances in research relationships.
Institutionalization of Bioethics
Table 1: Key Historical Developments in U.S. Bioethics
| Year | Event | Significance |
|---|---|---|
| 1966 | Henry Beecher's article on ethical problems in clinical research | Exposed ethical failures in human subjects research; called for professional self-regulation [3] |
| 1969 | Founding of The Hastings Center | First independent bioethics research institute; signal event in modern health care ethics [3] |
| 1971 | Establishment of Kennedy Institute of Ethics | Academic institutionalization of bioethics at Georgetown University [3] |
| 1979 | Belmont Report | Formulated foundational principles of respect for persons, beneficence, and justice [70] |
| 1993 | NIH Revitalization Act | Mandated inclusion of women and minorities in clinical research [70] |
The regulatory framework evolved significantly throughout the late 20th century. The Belmont Report in 1979 and subsequent Department of Health and Human Services regulations (45 CFR part 46) established foundational guidance focused on protecting vulnerable populations from research harms [70]. Initially, this protectionist stance often resulted in the exclusion of vulnerable groups from research participation, creating what scholars have identified as a form of "regulatory paternalism" [70]. By the 1980s and 1990s, HIV/AIDS activist movements successfully challenged this paradigm, shifting the emphasis "from justice as protection to justice as access" and elevating the principle of fair opportunity to participate in research [70].
Diagram 1: Historical evolution of US bioethics and research protections
Conceptual Framework for Fair Subject Selection
Defining Fair Subject Selection
Contemporary understanding of fair subject selection encompasses four distinct but interrelated principles, as articulated in Mackay and Saylor's framework [70]:
- Fair Inclusion: Representation of participants with diverse characteristics relevant to the disease and intervention
- Fair Burden Sharing: Protection of populations from assuming unfair research risks and burdens
- Fair Opportunity: Enhancement of opportunities to participate without unfair discrimination
- Fair Distribution of Third-Party Risks: Consideration of impacts on non-participants
The principle of justice remains the "least well-established conceptual notion in research ethics" and is often poorly operationalized in practice compared to principles of beneficence and respect for persons [70]. This conceptual ambiguity creates significant challenges for researchers attempting to implement ethically sound inclusion strategies.
Ethical Tensions and Conflicts
The application of fair subject selection principles reveals inherent tensions. For example, ensuring fair inclusion by including clinically relevant populations may conflict with fair burden sharing when those populations have already been disproportionately burdened by a disease [70]. This tension is particularly acute in research on post-acute sequelae of SARS CoV-2 (PASC), where disparities in infection, morbidity, and mortality have been uniformly higher among vulnerable populations such as communities of color [70]. Similarly, providing fair opportunity to all willing participants may conflict with the scientific requirement for a representative sample, potentially requiring researchers to turn away willing participants who do not match recruitment criteria [70].
Regulatory Landscape and Vulnerable Populations
Evolving Regulatory Definitions
The Common Rule specifically identifies vulnerable populations in subparts B, C, and D, referring to "minors, fetuses, and prisoners," with additional mention of "subjects that are likely to be vulnerable to coercion or undue influence, such as individuals with impaired decision-making capacity, or economically or educationally disadvantaged persons" [70]. Over time, a more expansive notion of "special populations" has evolved in translational research, encompassing not only these federally specified groups but also "elderly adults (often with comorbidities), historically under-represented ethnic or racial groups and people living in rural areas, among others" [70].
Table 2: Categories of Vulnerable Populations in Research Ethics
| Category | Examples | Ethical Considerations |
|---|---|---|
| Regulatorily Defined | Prisoners, minors, fetuses | Specific additional protections outlined in federal regulations [70] |
| Cognitively/Decisionally Impaired | Individuals with dementia, intellectual disability, temporary impairment | Capacity for informed consent; potential for coercion [70] |
| Socially/Economically Disadvantaged | Low-income populations, undocumented immigrants, educationally disadvantaged | Vulnerability to undue inducement; distributive justice concerns [70] |
| Medically Vulnerable | Terminally ill patients, those with rare diseases, comorbidity burden | Therapeutic misconception; desperation for interventions [70] |
| Historically Underrepresented | Racial and ethnic minorities, rural populations, older adults | Justice in distribution of research benefits; generalizability [70] |
Contemporary Challenges in Implementation
Recent ethical analysis highlights that determining an adequate and representative sample "is not simply a matter of ensuring greater diversity; rather, fairness requires a broader evaluation of risks, burdens, and benefits specific to underrepresented populations" [70]. This nuanced approach recognizes that regulatory paternalism—while sometimes justified to protect populations facing extremely high risks—can result in lack of opportunity, underrepresentation of certain groups, inequitable distribution of research benefits, and ultimately increased health disparities [70].
The COVID-19 pandemic highlighted persistent challenges in fair subject selection. Despite repeated calls for increased inclusion of underrepresented populations in biomedical research, "COVID-19 treatment and vaccine trials lack diversity, and inclusion of Black and Latinx participants is particularly limited" [70]. Without ongoing systemic corrective action, these inclusion gaps will likely persist in emerging research areas such as PASC studies [70].
Methodological Framework and Implementation Protocol
Comprehensive Assessment Protocol
Implementing fair subject selection requires systematic assessment at all stages of research development. The following protocol provides a methodological framework for researchers:
Stage 1: Population Relevance Assessment
- Identify disease epidemiology and prevalence across demographic groups
- Determine which populations are most affected by and most likely to use the intervention
- Analyze biological, environmental, and social factors that may influence treatment effect
- Document the rationale for inclusion and exclusion criteria with specific attention to fairness
Stage 2: Burden-Benefit Analysis
- Evaluate the distribution of risks and benefits across participant groups
- Assess whether potential burdens fall disproportionately on already disadvantaged populations
- Determine whether the research addresses health needs of the populations being recruited
- Implement additional safeguards for groups with limited capacity to bear research burdens
Stage 3: Recruitment Strategy Design
- Develop multifaceted outreach strategies to ensure fair opportunity for participation
- Address practical barriers to participation (transportation, timing, compensation)
- Create community-engaged recruitment plans with input from population representatives
- Ensure informed consent processes are comprehensible and accessible
Stage 4: Monitoring and Evaluation
- Establish ongoing monitoring of enrollment demographics
- Implement adaptive strategies to address enrollment disparities
- Plan for subgroup analysis in the protocol to ensure adequate statistical power
- Transparently report recruitment outcomes and limitations
Statistical Considerations for Representative Research
Methodological rigor requires advance planning for subgroup analysis to ensure scientific validity and clinical applicability. Research protocols should:
- Pre-specify subgroup analyses in the protocol to ensure adequate statistical design and avoid post hoc "p-hacking" [70]
- Ensure adequate power for clinically relevant subgroups rather than focusing solely on overall study power
- Report transparently on all pre-specified subgroup analyses, including null findings
- Characterize post hoc findings as hypothesis-generating that require replication
Statistical approaches must balance the need for representative samples with practical recruitment constraints. "Although it may be tempting to focus on rapidly increasing and diversifying recruitment efforts," ethical selection requires balancing broader principles of fair inclusion, fair burden sharing, and fair opportunity [70].
Diagram 2: Ethical protocol for fair subject selection implementation
Research Reagent Solutions: Ethical Framework Tools
Table 3: Essential Methodological Tools for Ethical Research Implementation
| Tool Category | Specific Instrument/Approach | Function and Application |
|---|---|---|
| Ethical Framework Instruments | Mackay & Saylor Fair Subject Selection Framework | Systematic assessment of inclusion, burden, opportunity, and third-party risks [70] |
| Community Engagement Tools | Community Advisory Boards; Community-Based Participatory Research | Ensure research relevance and ethical acceptability to affected communities [20] |
| Consent Enhancement Tools | Teach-back methods; Simplified consent forms; Capacity assessment tools | Promote genuine informed consent among vulnerable populations [70] |
| Recruitment Monitoring Tools | Real-time enrollment dashboards; Demographic disparity alerts | Identify and correct unrepresentative enrollment patterns [70] |
| Subgroup Analysis Tools | Pre-specified statistical analysis plans; Interaction tests | Ensure valid analysis of treatment effects across population subgroups [70] |
Case Study Application: PASC Research
Ethical Challenges in Emerging Research
Research on post-acute sequelae of COVID-19 (PASC) illustrates the complex application of fair selection principles. The fair inclusion principle requires representation of populations disproportionately affected by COVID-19, including racial and ethnic minorities, older adults, and individuals with comorbidities [70]. However, these same populations have already borne disproportionate burdens during the pandemic, creating tension with the fair burden sharing principle [70].
The methodological approach to PASC research must account for this tension by implementing enhanced protections while maintaining inclusion. This includes:
- Comprehensive burden mitigation: Addressing transportation, compensation, and time constraints
- Community partnership: Engaging affected communities in research design and implementation
- Direct benefit assessment: Ensuring research addresses questions relevant to the health priorities of burdened populations
- Longitudinal support: Providing ongoing resources beyond data collection periods
Implementation Framework
Successful implementation requires acknowledging that underrepresented populations affected by PASC "may further be negatively impacted by poor health, work effectiveness, family dynamics, and socioeconomic status, for example, in cases of lost employment" [70]. Research protocols must therefore incorporate systematic assessment of these broader impacts and provide appropriate support structures.
The historical evolution of bioethics in the United States demonstrates a continuing tension between protection and access. From its origins in responding to research scandals and technological advancement, bioethics has developed increasingly sophisticated frameworks for addressing vulnerability and fairness [3] [4]. The contemporary challenge for researchers is to implement these frameworks systematically throughout the research lifecycle.
Optimizing protections for vulnerable populations while ensuring fair subject selection requires moving beyond checkbox compliance toward substantive ethical engagement. This involves recognizing the pluralistic nature of vulnerability and developing nuanced strategies that address both individual and structural determinants of research risk [70] [20]. By implementing the comprehensive assessment protocols, methodological tools, and monitoring strategies outlined in this guide, researchers can advance both ethical integrity and scientific validity in human subjects research.
The institutionalization of bioethics established crucial safeguards against exploitation; the current imperative is to refine these protections through a justice-oriented approach that promotes equitable participation while preventing the perpetuation of health disparities through exclusion or overburdening. This balanced approach represents the optimal integration of bioethics' historical legacy with contemporary scientific imperatives.
The field of bioethics emerged as a direct response to unprecedented ethical problems created by the explosive postwar growth of medical research and therapeutic advances [3]. The modern era of health care ethics is often traced to Henry Beecher's influential 1966 article on ethical problems in clinical research, which highlighted failures to inform patients of risks in experimental treatments [3]. This nascent field rapidly institutionalized with the founding of the Hastings Center in 1969 and the Kennedy Institute of Ethics in 1971, organizations that would set the direction, methods, and intellectual standards for bioethics through scholarly publications like the Hastings Center Report [3].
The convergence of artificial intelligence with advanced biotechnologies represents the latest chapter in this ongoing evolution, presenting ethical challenges that extend beyond the frameworks established for earlier medical technologies. As AI-driven tools accelerate progress in genome editing and synthetic biology, they raise fundamental questions about safety, equity, and human values that recall earlier bioethical debates while introducing entirely new dimensions of concern [71] [72].
Technical Foundations: AI-Driven Genome Editing Technologies
Evolution of Genome Editing Platforms
The development of genome editing technologies has progressed through several generations, each offering improved precision and specificity [71]:
Table: Generations of Genome Editing Technologies
| Generation | Key Technology | Time Period | Key Characteristics | Major Limitations |
|---|---|---|---|---|
| First | Homologous Recombination | 1980s | Natural process, gene targeting | Low efficiency in complex mammalian cells |
| Second | Zinc Finger Nucleases (ZFNs) | 1990s | First artificial site-specific nucleases | Complex design, pronounced off-target effects |
| Third | TALENs | 2000s | Simpler design, recognized diverse DNA sequences | Still relatively complex to engineer |
| Fourth | CRISPR-Cas Systems | 2012-present | Simple design, high efficiency, low cost | Off-target effects, ongoing refinement |
The CRISPR-Cas9 system, elucidated in 2012 by Doudna, Charpentier, and colleagues, represented a revolutionary advance by enabling precise DNA cleavage guided by a simple RNA molecule [71]. Subsequent developments have produced more specialized tools including Cas12a (creating 5' overhangs), Cas13 (targeting RNA), and engineered variants like dCas9 for CRISPR interference (CRISPRi) and activation (CRISPRa) that modulate gene expression without permanent DNA alteration [71].
AI Integration with Genome Editing
The convergence of AI and genome editing addresses the dual demands for high throughput and high precision in biological engineering [71]. The paradigm for AI in genome editing research involves several critical stages:
- Data Acquisition and Integration: Large-scale datasets on off-target effects, target screening, transcriptomics, proteomics, and epigenomics are compiled from diverse experimental sources [71].
- Feature Selection and Model Training: Machine learning algorithms, including deep learning networks, identify patterns and variables hidden within gene editing processes [71].
- Prediction and Optimization: Trained models predict sgRNA activity, minimize off-target effects, and optimize editing conditions [71].
- Therapeutic Application: AI-driven editing tools are deployed for precise genetic interventions in clinical, agricultural, and synthetic biology contexts [71].
The following diagram illustrates the integrated workflow of AI-driven genome editing:
Experimental Protocols for AI-Enhanced Genome Editing
Protocol: Deep Learning-Guided sgRNA Design
Objective: To design highly efficient sgRNAs with minimal off-target effects using deep learning models [71].
Materials and Reagents:
- Genomic DNA from target cell line
- CRISPR-Cas9 ribonucleoprotein complex
- Next-generation sequencing library preparation kit
- Transfection reagents
- Cell culture media and supplements
Methodology:
- Training Data Collection:
- Perform genome-wide CRISPR screens with sgRNA library
- Sequence genomic DNA before and after editing
- Quantify insertion/deletion frequencies at each target site
- Compile epigenetic features (chromatin accessibility, histone modifications)
Model Architecture:
- Implement convolutional neural networks (CNNs) for sequence pattern recognition
- Include bidirectional LSTM layers for contextual sequence analysis
- Add attention mechanisms to identify critical nucleotide positions
- Train on multi-modal data integrating sequence, epigenetic, and structural features
Validation:
- Test predicted sgRNAs in cell-based assays
- Assess on-target efficiency via T7E1 assay or next-generation sequencing
- Evaluate off-target effects using GUIDE-seq or CIRCLE-seq
- Compare performance against conventional design tools
Protocol: AI-Optimized Prime Editing
Objective: To precisely install desired edits using prime editing guided by AI-based template design [71].
Materials and Reagents:
- Prime editor constructs (nCas9-reverse transcriptase fusion)
- Prime editing guide RNA (pegRNA) synthesis components
- Target cell lines with reporter constructs
- Deep sequencing validation primers
- DNA extraction and purification kits
Methodology:
- pegRNA Optimization:
- Input desired genetic variant into AI prediction platform
- Generate pegRNA designs with varying primer binding site lengths
- Optimize reverse transcriptase template sequences
- Predict secondary structure interference using RNA folding algorithms
Delivery and Editing:
- Transfect prime editor components into target cells
- Incubate for 72 hours to allow editing and expression
- Isolate genomic DNA for analysis
Efficiency Quantification:
- Amplify target regions by PCR
- Perform deep sequencing (minimum 10,000x coverage)
- Analyze sequencing data for precise edit incorporation
- Screen for byproduct edits and unpredicted modifications
Ethical Frameworks and Considerations
Core Ethical Principles in Biotechnology
The ethical landscape for emerging biotechnologies encompasses several fundamental concerns that span applications [72]:
Table: Core Ethical Principles and Considerations
| Ethical Principle | Technical Manifestations | Risk Factors | Mitigation Strategies |
|---|---|---|---|
| Safety & Unintended Outcomes | Off-target effects, on-target mutations, unpredictable phenotypes | High in early development phases | Improved prediction algorithms, rigorous validation |
| Justice & Equity | Disparities in access, high costs, prioritization of Western markets | Widening health disparities | Tiered pricing, technology transfer, public funding |
| Biodiversity | Genetic monoculture, reduced species variety | Agricultural homogenization | Ecological risk assessment, diversity preservation |
| Naturalness & Relationship to Nature | Perceptions of "playing God", ecosystem manipulation | Cultural and religious objections | Inclusive deliberation, transparency |
| Decision-Making Authority | Concentrated expertise, exclusion of stakeholders | Democratic deficits | Participatory governance, community engagement |
Specific Ethical Challenges by Application Domain
Human Therapeutics
The application of CRISPR in human medicine raises distinctive ethical concerns, particularly regarding somatic versus germline editing and treatment versus enhancement [72]. Somatic edits affect only the individual, while germline modifications would be heritable, raising concerns about permanent changes to the human gene pool [72]. The distinction between treatment (addressing disease) and enhancement (improving human capabilities) presents another ethical boundary that requires careful consideration [72].
The case of Casgevy, the first FDA-approved CRISPR-based therapy for sickle cell disease, illustrates the ethical balancing act in therapeutic development [72]. Regulators weighed the potential benefits against unknown long-term risks of a novel technology, ultimately determining that the significant therapeutic benefit for a debilitating disease justified approval [72].
Agricultural and Environmental Applications
In agriculture, CRISPR technologies raise questions about appropriate use in food production, potential ecological consequences, and corporate control of food systems [72]. Environmental applications including gene drives for controlling disease vectors or invasive species present additional concerns about ecosystem-level effects and irreversible changes to natural systems [72].
Community Bioethics and Inclusive Governance
The emergence of community-based biology (including DIYbio, biohacking, and community bio labs) presents novel challenges to institutionalized ethics paradigms [20]. These decentralized approaches to biotechnology often operate outside conventional regulatory frameworks and may embrace different values than establishment science [20].
Community bioethics represents an approach that emphasizes pluralism, challenges the individualist orientation of traditional bioethics, and addresses structural determinants of health [20]. This perspective argues for ethics that acknowledge diverse value systems and empower communities in ethical decision-making, rather than imposing uniform principles [20].
The following diagram outlines the ethical decision-making framework for emerging biotechnologies:
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Research Reagents for AI-Driven Genome Editing
| Reagent/Category | Function | Technical Considerations | Ethical Implications |
|---|---|---|---|
| CRISPR-Cas Ribonucleoprotein Complexes | Direct DNA cleavage without vector integration | Reduces off-target effects, improves specificity | Enhanced safety profile for therapeutic applications |
| Base Editors (BE) | Chemical conversion of specific DNA bases without double-strand breaks | Higher precision, lower indel rates | Reduced risk of unintended mutations in clinical use |
| Prime Editors (PE) | Reverse transcription of edit template at target site | Broad editing capabilities (all 12 base conversions) | Potential for more precise genetic corrections |
| dCas9 Effector Fusions | Gene regulation without DNA modification | CRISPRi/CRISPRa for reversible modulation | Avoids permanent genome alteration concerns |
| AI-Predicted sgRNAs | Optimized guide RNA sequences | Improved on-target efficiency, reduced off-target effects | Addresses safety concerns in therapeutic development |
| Bioinformatics Pipelines | Analysis of editing outcomes and prediction of effects | Integrates multi-omics data for comprehensive assessment | Enables thorough risk-benefit analysis |
| Cell-based Reporter Systems | Quantification of editing efficiency and specificity | High-throughput screening capability | Facilitates rigorous preclinical safety testing |
The integration of artificial intelligence with advanced biotechnologies represents a frontier that demands evolving ethical frameworks capable of addressing both technical complexities and societal implications. The historical development of bioethics demonstrates that ethical paradigms must adapt to technological transformations while maintaining core commitments to human welfare, justice, and democratic values [3] [20].
As these technologies continue to advance, the bioethics community faces the challenge of developing governance approaches that are both responsive to rapid innovation and inclusive of diverse perspectives. This will require ongoing collaboration between researchers, ethicists, policymakers, and communities to ensure that the profound capabilities of gene editing and AI are directed toward broadly beneficial ends [71] [72]. The future of bioethics in this domain will likely involve adaptive governance models that can accommodate emerging insights while maintaining essential safeguards for human and ecological wellbeing.
The institutionalization of bioethics in the United States emerged as a formalized response to profound ethical failures in research and clinical practice [73] [74]. This framework, designed to protect human subjects and uphold ethical standards, now operates within a complex ecosystem of political and budgetary constraints that systematically impact its efficacy. The foundational principles of bioethics—respect for persons, justice, and beneficence—face persistent challenges when institutional support fluctuates according to political priorities and fiscal pressures [75] [74].
This technical analysis examines how these systemic pressures manifest within research ethics oversight mechanisms, particularly Institutional Review Boards (IRBs) and regulatory bodies. By tracing the historical development of bioethics alongside contemporary case studies, we demonstrate how resource limitations and political influences can compromise ethical safeguards, potentially undermining the protection of vulnerable populations and the integrity of scientific research [75] [76]. The analysis further explores methodological frameworks for assessing these impacts and proposes structural reforms to strengthen ethical oversight under constraint.
Historical Context: The Institutionalization of Bioethics in the United States
The evolution of American bioethics is inextricably linked to both ethical crises and the legal system that responded to them [74]. The field gained prominence in the 1970s, transforming from an academic interest into a structured discipline with tangible institutional mechanisms.
Table 1: Historical Foundations of U.S. Bioethics
| Year | Event | Significance | Impact on Oversight |
|---|---|---|---|
| 1947 | Nuremberg Code | Established informed consent as absolute requirement for research [74] | Created first international ethical standards for human subject research |
| 1964 | Declaration of Helsinki | International guidelines for ethical medical research [73] | Expanded principles of Nuremberg Code; influenced U.S. policy |
| 1971 | Kennedy Institute of Ethics Founded | First academic bioethics institute in the U.S. [73] | Institutionalized bioethics as academic discipline |
| 1972 | Tuskegee Syphilis Study Exposed | 40-year study withholding treatment from Black men [74] | Direct catalyst for National Research Act (1974) and Belmont Report |
| 1979 | Belmont Report | Identified basic ethical principles for research [75] | Created foundation for IRB regulations and oversight mechanisms |
The legal system played a crucial role in translating ethical principles into enforceable standards. Beginning with Canterbury v. Spence (1972), courts established the doctrine of informed consent as a prerequisite for ethical medical care, cementing patient autonomy in law before it was fully embraced in medical ethics [74]. The political response to the Tuskegee Syphilis Study led to formalized oversight structures, including the requirement for IRBs to review federally funded research [74]. This historical context demonstrates that the current oversight infrastructure was built reactively, following ethical failures, and its stability remains subject to the political will that created it.
Contemporary Political and Budgetary Pressures on Ethical Oversight
Political Influences on Research Prioritization and Regulation
Political agendas significantly influence which research areas receive funding and scrutiny, often creating ethical blind spots. The Bayh-Dole Act of 1980, which allowed private entities to patent publicly funded research, fundamentally altered the innovation landscape by prioritizing commercializable outcomes over equitable access [76]. This legislative shift exemplifies how political policy can create systemic ethical tensions between profit motives and public health goals.
Recent debates over drug pricing reveal how political framing can impact ethical oversight. Legislative efforts like H.R.3 (Lower Drug Costs Now Act) and S.2543 (Prescription Drug Pricing Reduction Act) face opposition framed as protecting innovation, with arguments that price controls would result in "8 fewer drugs introduced into the United States’ market over the next decade and 30 fewer over the subsequent decade" [77]. This political discourse often overlooks the ethical implications of a system where 25% of Americans struggle to afford necessary prescriptions, highlighting how political priorities can overshadow distributive justice concerns in pharmaceutical regulation [77].
Budgetary Constraints and Procedural Vulnerabilities
Financial pressures create tangible vulnerabilities in ethics oversight systems. IRBs and research ethics committees often operate with limited resources, impacting their capacity for comprehensive review. This is particularly problematic for reviewing research involving vulnerable populations, which requires additional time and expertise [75]. A systematic review of policy documents found that despite frequent requirements for researchers to address vulnerable population enrollment, research ethics committees often provide "poor or no guidance on how to address this request," leading to inconsistent protections and potential inequities [75].
The pharmaceutical sector demonstrates how financialization creates ethical risks. Private equity (PE) ownership of pharmaceutical manufacturers and distributors introduces a model prioritizing short-term financial returns, with studies associating PE involvement with price increases of 25-32% for essential medications [76]. Simultaneously, marketing expenditures have risen to $30 billion annually, dwarfing many research budgets and suggesting misaligned institutional priorities that oversight bodies are ill-equipped to address [77] [76].
Table 2: Budgetary Pressures and Ethical Consequences in Pharmaceutical Development
| Budgetary Factor | Financial Magnitude | Ethical Consequence |
|---|---|---|
| Pharmaceutical Marketing | $30 billion annually [77] [76] | Misallocation of resources from research to promotion |
| Private Equity Influence | 25-32% price increases for acquired drugs [76] | Prioritization of shareholder returns over patient access |
| Lobbying Expenditures | ~$220 million by pharmaceutical companies and trade organizations [77] | Political influence that may weaken regulatory oversight |
| "Me-Too" Drug Development | 78% of 1998-2003 FDA approvals [76] | Resource allocation to minimally innovative products |
Quantitative Analysis of Systemic Pressures
Empirical data reveals the tangible effects of these systemic pressures on research outcomes and ethical compliance. The following table synthesizes quantitative findings from recent studies and policy analyses:
Table 3: Quantitative Data on Systemic Constraints and Ethical Outcomes
| Metric | Data | Source/Context | Ethical Implication |
|---|---|---|---|
| Prescription drug affordability | 25% of Americans find it difficult to afford necessary prescriptions [77] | Analysis of healthcare cost burdens | Failure of distributive justice in healthcare access |
| Medication rationing | 1 in 5 U.S. adults report skipping or rationing medication due to cost [76] | Nationally representative study | Direct patient harm from pricing structures |
| Pharmaceutical profit margins | Median 76.5% gross profit margin (2000-2018) [76] | Financial analysis comparing pharmaceutical companies to S&P 500 (37.4%) | Misalignment between profit motives and public health objectives |
| Patent applications for top drugs | Average of 125 patent applications per drug [76] | Strategy to extend exclusivity and delay generics | Use of legal mechanisms to maintain monopolistic pricing |
| Federal contribution to drug research | >$100 billion for 356 new drugs approved (2010-2019) [76] | Public investment in pharmaceutical innovation | Questioning of "innovation" justification for high prices |
Methodological Framework for Assessing Ethical Oversight Under Constraints
Systematic Policy Analysis Protocol
Objective: To systematically evaluate how policy documents conceptualize and operationalize protections for vulnerable populations under resource constraints.
Methodology:
- Document Identification: Follow PRISMA-Ethics guidance for systematic reviews of policy documents [75]. Search three primary sources: International Compilation of Human Research Standards, Listing of Social-behavioral Research Standards, and Ethics Legislation, Regulation and Conventions.
- Content Analysis: Employ qualitative content analysis using a combination of inductive and deductive category development [78]. Conduct open coding to identify key elements, stakeholders, and connections between them.
- Axial Coding: Group codes into themes and subthemes, mapping relationships between stakeholders, systemic constraints, and protective measures [75].
- Visualization: Develop interactive knowledge visualizations to make complex policy frameworks more accessible to diverse stakeholders, following methodologies demonstrated in bioethics implementation research [78].
Ethical Visualization Protocol
Objective: To create data visualizations that accurately represent ethical oversight challenges without deceptive practices.
Methodology:
- Color Selection: Use scientifically-derived, accessible color maps (e.g., "viridis," "cividis") that are perceptually uniform and color-blind friendly [79]. Avoid misleading color contrasts that exaggerate or minimize differences.
- Axis Scaling: Maintain consistent, appropriate scales in all graphical representations. Never truncate axes to exaggerate effects.
- Data Transparency: Clearly document all data sources, methodological choices, and limitations. Provide access to underlying data where possible.
- Vulnerability Representation: Ensure visualizations do not perpetuate stereotypes or stigmatize vulnerable populations. Use empathic data collection and presentation methods [80].
Research Reagent Solutions for Ethical Analysis:
Table 4: Essential Analytical Tools for Ethical Oversight Assessment
| Tool/Resource | Function | Application Context |
|---|---|---|
| PRISMA-Ethics Guidelines | Systematic review methodology for ethics literature [75] | Ensuring comprehensive policy document analysis |
| Qualitative Analysis Software (e.g., NVivo) | Facilitates coding and theme development in text-based data [78] | Identifying patterns in policy documents and interview transcripts |
| Scientific Colour Maps | Perceptually uniform color palettes (e.g., "batlow") [79] | Creating accessible, non-misleading data visualizations |
| Dual Coding Theory Framework | Cognitive framework for visual information processing [78] | Designing educational materials for ethics training |
| Relational Bioethics Framework | Analytical approach examining systemic vulnerabilities [81] | Assessing institutional pressures on clinical decision-making |
Structural Reforms and Mitigation Strategies
Addressing the impact of political and budgetary constraints requires structural reforms that strengthen ethical oversight mechanisms. Based on the historical analysis and contemporary case studies, we propose the following evidence-based mitigation strategies:
Institutional Reinforcement
- Stable Funding Mechanisms: Create dedicated funding streams for research ethics programs insulated from political budget cycles. This could include endowment models or fixed percentages of research grants allocated to oversight functions.
- Enhanced Guidance for Vulnerable Populations: Develop specific, operational guidelines for research involving vulnerable populations, moving beyond mere identification to providing concrete protective methodologies [75]. This addresses the current situation where researchers receive "poor or no guidance" on managing vulnerability appropriately.
- Transparency Mandates: Implement rigorous reporting requirements for pharmaceutical pricing, research expenditures, and political lobbying activities to illuminate potential conflicts of interest [77] [76].
Analytical Approach to Vulnerability
Shift from a categorical to an analytical approach in identifying and protecting vulnerable research participants [75]. This involves:
- Consent-Based Assessment: Evaluating potential vulnerabilities related to capacity for autonomous decision-making and susceptibility to undue influence.
- Harm-Based Assessment: Analyzing the probability and magnitude of potential research-related harms specific to participant circumstances.
- Justice-Based Assessment: Examining structural inequalities and barriers to equitable research participation and benefit sharing.
The institutionalization of bioethics in the United States created essential safeguards for research participants, but these protections remain vulnerable to political and budgetary pressures that can compromise their effectiveness. Historical analysis reveals that ethical oversight structures often emerge reactively following scandals, yet depend on sustained political will and resources to maintain their protective function. Contemporary evidence demonstrates how systemic pressures manifest in pharmaceutical pricing practices, inadequate guidance for vulnerable population research, and resource-constrained oversight bodies.
Addressing these challenges requires both structural reforms and methodological innovations. Stable funding mechanisms, enhanced transparency, and a shift toward analytical vulnerability assessment can help insulate ethical oversight from systemic pressures. The integration of rigorous visualization ethics and systematic policy analysis methodologies offers promising approaches to strengthening ethical infrastructure despite constraints. Ultimately, maintaining the integrity of bioethics oversight requires recognizing that protection systems are not self-sustaining but require ongoing institutional commitment, particularly when political and economic interests create competing priorities.
The discipline of bioethics, born in the United States in the late 1960s, emerged primarily in response to ethical crises in clinical research and medicine. Sparked by revelations such as Henry Beecher's 1966 expose of ethical problems in clinical research and the subsequent public scrutiny of the Tuskegee syphilis study, the field rapidly institutionalized with the founding of The Hastings Center in 1969 and the Kennedy Institute of Ethics in 1971 [3] [82]. These institutions established bioethics as a systematic study of moral conduct in the life sciences and medicine, initially focusing on issues like informed consent and human subjects protection [32]. The Nuremberg Code and its emphasis on voluntary consent became foundational documents, with the U.S. government further shaping the field through commissions like the National Commission for the Protection of Human Subjects, which produced the influential Belmont Report outlining principles of respect, beneficence, and justice [32] [82].
Today, this American-born bioethical tradition faces unprecedented challenges from two transformative developments: the rise of global research collaborations and the explosion of big data in health and research. The very definition of "human subject" is being transformed as genomic information crosses contextual boundaries and big data technologies process health information in ways that challenge traditional informed consent models [83]. This whitepaper examines how the foundational principles of American bioethics must evolve to address these challenges while maintaining their core commitment to human dignity and ethical scientific progress.
The Changing Research Landscape: Global Collaboration and Big Data
The Expansion of Global Research Collaboration
Research has undergone a fundamental shift from individual or single-institution projects toward complex global partnerships. Bibliometric data reveals a steady increase in the average number of authors per publication across all disciplines since the 1980s, with the physical sciences showing a trend toward "hyperauthorship" (defined as >50 authors on a paper) [84]. This pattern has now extended to health sciences, where papers with >50 authors rose from 58 in 2015 to 203 in 2021 [84]. The United States' most productive research partnership is with China, though this collaboration has faced recent challenges [84].
These global partnerships introduce complex ethical dimensions beyond the traditional researcher-subject dyad that characterized early American bioethics. As Rebecca Cooney, Chief Editor of Nature Mental Health, notes, "collaboration is a mechanism to promote equity" [84]. However, North-South collaborative articles still show authorship contribution dominated by the Global North, indicating persistent equity issues in global science [84]. The increasing involvement of non-traditional contributors such as community organizations, patient groups, and policymakers—whose contributions may not result in formal authorship—further complicates ethical attribution and accountability [84].
The Big Data Revolution in Health and Research
Big data in health and research is characterized by what experts term the "V-factors": volume (sheer quantity of data), variety (diversity of data forms and sources), and velocity (speed at which data is transmitted and analyzed) [85]. Some frameworks expand this to include variability, veracity, value, and visualization [85]. These characteristics enable potentially transformative benefits across healthcare, from improving clinical decision quality to operational efficiencies and cost savings [85].
However, these same characteristics create fundamental challenges to traditional bioethical frameworks. The inability to reliably anonymize data through traditional masking techniques poses a particular challenge. As one ethics framework notes, "The dynamic and multifaceted nature of big data, as well as the variety of data available, has increased the likelihood of privacy threats to data sets that are not readily identifiable" [85]. Three disclosure risks threaten privacy: identity disclosure (linking data to a specific person), attribute disclosure (identifying group membership), and inferential disclosure (inferring information with high confidence) [85].
Table 1: Big Data Characteristics and Associated Ethical Challenges
| Characteristic | Definition | Ethical Challenge |
|---|---|---|
| Volume | The sheer quantity of data, including number of individuals and detail level | Comprehensible informed consent becomes impractical; scale increases potential harm |
| Variety | Diversity of data forms (structured, unstructured, images, audio) and sources | Contextual integrity threatened when data crosses domains; purpose limitation challenged |
| Velocity | Speed at which data can be transmitted and analyzed | Traditional oversight mechanisms cannot keep pace with rapid analysis and sharing |
| Veracity | Data quality and accuracy concerns | Potential for biased or inaccurate conclusions with real-world consequences |
| Variability | Changing meaning and interpretation of data in different contexts | Consistent ethical application across contexts becomes challenging |
Limitations of Traditional Ethical Frameworks
The Informed Consent Paradigm Under Pressure
The principle of informed consent, absolutely essential to the Nuremberg Code and central to American bioethics since its inception, faces particular pressure in these new environments. The liberal individualistic approach to autonomy that characterized early American bioethics assumes a model of discrete decision-making by autonomous agents that poorly fits the realities of both big data and collaborative global research [83] [32].
Genomic information exemplifies this challenge due to its inherently interconnected nature. As one scholar notes, "information disclosed by one person can also disclose information about others" [83]. This creates what has been termed the "tyranny of the minority"—when the willingness of a few people to share private information also discloses information about many others [83]. Examples include:
- Direct familial implications: When one individual undergoes genetic testing for a condition with 50% inheritance probability, effectively revealing risk information about siblings without their consent [83]
- Forensic applications: Law enforcement use of commercial DNA databases leading to identification of individuals through relatives who voluntarily submitted samples [83]
- Group harms: Research involving Indigenous populations potentially disclosing information about the entire community, raising issues of group consent that individual informed consent cannot address [83]
These limitations are further compounded in big data environments where data repurposing is common. Traditional specific consent for particular research purposes becomes impractical when data may be used in unforeseen ways years later, by researchers in domains that didn't exist when the data was originally collected [85].
Regulatory and Jurisdictional Challenges
The American bioethics framework developed alongside a primarily national regulatory structure, but global collaborative research operates across multiple jurisdictions with different ethical standards and requirements. The 2024 revision of the Declaration of Helsinki illustrates how international standards are evolving, but national frameworks like South Korea's Bioethics and Safety Act must play catch-up to align with these updates [86].
Similarly, big data flows freely across borders while regulatory frameworks remain largely national, creating challenges for consistent ethical oversight. The contextual integrity approach, developed in information technology ethics, offers a promising alternative by suggesting that information should be shared and protected according to norms governing distinct social contexts rather than relying solely on individual control [83].
Adaptive Ethical Frameworks for Future Challenges
Evolving International Guidelines: The 2024 Declaration of Helsinki
The recent 2024 revision of the Declaration of Helsinki represents significant progress in addressing contemporary research challenges. Key updates include:
- Terminological shift: Replacing "subjects" with "participants" to recognize the rights, agency, and importance of individuals involved in medical research [86]
- Expanded scope: Applying ethical principles beyond physicians to all individuals, teams, and organizations involved in medical research [86]
- Dynamic vulnerability: Redefining vulnerability as context-dependent rather than a fixed characteristic, emphasizing fair inclusion of vulnerable groups rather than exclusion [86]
- Global justice: New aspirational language acknowledging structural inequities and urging researchers to consider where and with whom research is carried out [86]
- Environmental ethics: Stronger emphasis on avoiding environmental harm and striving for sustainability [86]
Table 2: Key Revisions in the 2024 Declaration of Helsinki and Their Implications
| Revision Category | Specific Change | Implication for Research Ethics |
|---|---|---|
| Conceptual Shift | "Subjects" to "participants" | Recognizes active role rather than passive recipients of research |
| Vulnerability | Vulnerability as dynamic and context-dependent | Moves beyond categorical protections to context-sensitive approaches |
| Scope | Applies to all research team members | Expands ethical responsibility beyond principal investigators |
| New Content | Explicit mention of research misconduct | Formalizes integrity expectations in collaborative environments |
| Enhanced Principles | Strengthened post-trial provisions | Addresses ethical obligations beyond study completion |
Contextual Integrity as a Framework for Genomic and Big Data Ethics
The contextual integrity framework, developed by Helen Nissenbaum in information technology ethics, offers a promising approach for genomic information that crosses multiple societal contexts (medical, commercial, forensic, archaeological) [83]. Rather than focusing exclusively on individual control, this approach holds that "information should be shared and protected according to the norms that govern certain distinct social contexts" [83].
This framework helps address the limitations of informed consent in big data environments by:
- Recognizing appropriate information flows: Focusing on whether information transfers respect contextual norms rather than relying solely on individual authorization [83]
- Accounting for power differentials: Considering how data flows may reinforce or mitigate existing structural inequalities [83]
- Addressing group interests: Providing a framework to consider harms to communities, not just individuals [83]
Procedural Frameworks for Ethical Decision-Making
For researchers navigating complex ethical landscapes, structured frameworks can guide ethical decision-making. The Ethics Framework for Big Data in Health and Research developed by the SHAPES Initiative provides a step-by-step process for identifying, considering, and resolving ethical issues [85]. Key characteristics of effective ethical decision-making frameworks include:
- Articulation of aim and scope
- Practical applicability
- Explicit values that are of equal weight initially
- Flexibility without forcing particular decisions
- Problem-driven rather than theory-driven orientation
- Structured guidance through a series of questions [85]
Similarly, a bioethical framework for clinical decision-making with seriously ill patients demonstrates how dividing complex processes into discrete steps with different ethical principles can improve outcomes [87]. Such structured approaches can be adapted for research ethics, particularly in collaborative environments.
Diagram 1: Evolution from Traditional to Adaptive Ethical Frameworks
Implementation Strategies for Research Institutions
Building Infrastructure for Ethical Global Collaboration
Research institutions can take concrete steps to support ethical global collaborations:
- Strategic partnership development: Use bibliometric data to review existing networks and identify new collaborators in priority research areas, moving beyond ad-hoc partnerships to strategic relationships [84]
- Capacity building: Develop training programs in collaboration skills, including project management, cross-cultural communication, and negotiation, particularly for early career researchers [84]
- Recognition systems: Embed collaborative science into frameworks for researcher career development and reward systems [84]
- Equity frameworks: Implement tools like The TRUST Code (A Global Code of Conduct for Equitable Research Partnerships) and Inclusion and Ethics disclosures in publications [84]
Governance Models for Big Data Ethics
Effective governance of big data in health and research requires moving beyond binary distinctions between "identifiable" and "anonymized" data, recognizing instead a spectrum of identifiability with appropriate safeguards at each level [85]. Key elements include:
- Tiered consent models: Implementing approaches like broad consent for future research with specific governance oversight, rather than relying solely on specific consent [85]
- Robust oversight mechanisms: Ensuring research ethics committees have expertise in big data methodologies and privacy risks [86] [85]
- Transparency and accountability: Developing clear protocols for data sharing, secondary use, and cross-border data flows [85]
- Environmental consideration: Incorporating assessment of environmental impact and sustainability into research ethics review, as emphasized in the revised Declaration of Helsinki [86]
Table 3: Essential Research Reagent Solutions for Ethical Big Data Research
| Solution Category | Specific Tools | Function in Research Ethics |
|---|---|---|
| Governance Frameworks | Contextual Integrity Model, SHAPES Ethics Framework | Provide structured approaches to evaluate ethical implications of data flows and uses |
| Oversight Mechanisms | Specialized Research Ethics Committees, Environmental Impact Assessment | Ensure appropriate review of big data projects and collaborative research |
| Partnership Guidelines | TRUST Code, Equity and Inclusion Disclosures | Promote equitable collaborations and recognize all contributor roles |
| Technical Safeguards | Privacy Models, Differential Privacy, Tiered Access Controls | Implement privacy protection in line with ethical requirements |
| Training Resources | Nature Masterclasses collaboration skills, Cross-cultural communication modules | Build researcher capacity for ethical global collaborative work |
The American bioethics tradition, born from specific historical circumstances in the mid-20th century, demonstrates remarkable resilience through its ability to evolve while maintaining core commitments to human dignity and ethical scientific progress. The expansion of global research collaboration and big data technologies represents the latest in a series of challenges that have shaped the field since its institutionalization in the United States.
Future-proofing ethics requires neither abandoning foundational principles like those in the Nuremberg Code nor rigidly adhering to their original applications. Rather, it demands the kind of creative adaptation exemplified by the contextual integrity framework for genomic data and the 2024 Declaration of Helsinki's reconceptualization of research participants and vulnerability. By building on American bioethics' history of interdisciplinary engagement and practical problem-solving while embracing new conceptual frameworks from information technology ethics and global justice perspectives, the field can continue to fulfill its essential role in guiding responsible scientific progress.
The institutional infrastructure of bioethics—research ethics committees, institutional review boards, and ethics commissions—must similarly evolve to address the challenges of global collaboration and big data. This evolution represents not a break with the American bioethics tradition but rather its continuation through adaptation to new scientific realities, maintaining the field's relevance for the next half-century of rapid technological advancement.
Validation and Global Context: Assessing the U.S. Model and Its International Counterparts
The American bioethics infrastructure represents a unique complex of philosophical frameworks, regulatory systems, and practical guidelines that have evolved to address ethical challenges in healthcare and biomedical research. Born from specific historical circumstances and cultural values, this infrastructure has developed distinctive characteristics that shape its application in both domestic and global contexts. The U.S. approach to bioethics is characterized by its strong emphasis on individual autonomy, rights-based discourse, and principlist frameworks, which differentiate it from other international models [3]. This foundation emerged from a convergence of factors including groundbreaking legal cases, the consumer rights movement, and responses to research scandals, creating an infrastructure that profoundly influences how ethical issues are identified and resolved in biomedical research and clinical practice [88] [3]. This paper examines the historical evolution, structural efficacy, and substantive critiques of this system, with particular attention to its functioning within drug development and clinical research environments.
Historical Development and Institutionalization
Origins and Formative Influences
The modern American bioethics infrastructure emerged during a period of significant social transformation and medical advancement. Several key factors converged to shape its development:
Research Scandals and Response: The exposure of ethical violations in medical research, notably Henry Beecher's 1966 article detailing ethical problems in clinical research, served as catalytic events [3]. Subsequent scandals including the Tuskegee syphilis study revealed systemic ethical failures and created impetus for structural reform [89].
Legal Foundations: The 1957 Salgo case established the legal doctrine of informed consent, fundamentally reshaping the physician-patient relationship by requiring physicians to provide patients with relevant information about treatment alternatives and risks [3]. This transfer of decision-making authority from physician to patient established autonomy as a central principle in American medical ethics.
Consumer Rights Movement: President John F. Kennedy's 1962 address to Congress outlining four basic consumer rights (safety, information, choice, and representation) provided a rights-based framework that would heavily influence bioethical discourse [3]. This consumer rights orientation contrasted with more paternalistic or community-oriented approaches developing elsewhere.
Institutionalization and Codification
The formal institutionalization of bioethics began with the establishment of dedicated organizations and frameworks:
Founding Institutions: The Hastings Center (1969) and Kennedy Institute of Ethics (1971) became foundational institutions that defined the scope, methods, and intellectual standards of American bioethics [3]. These organizations provided the infrastructure for bioethics as a distinct field spanning medicine, philosophy, law, and social sciences.
Regulatory Milestones: The Belmont Report (1978) established three core principles—respect for persons, beneficence, and justice—that would inform federal regulations for human subjects research [89]. This document emerged in direct response to the Tuskegee scandal and laid the groundwork for the principlist approach that would dominate American bioethics.
Principlism Framework: Tom Beauchamp and James Childress's Principles of Biomedical Ethics (1979) systematized the core principles of American bioethics into autonomy, beneficence, non-maleficence, and justice [89] [3]. This framework became the dominant approach for ethical analysis in clinical and research contexts.
Table 1: Key Historical Developments in U.S. Bioethics Infrastructure
| Time Period | Major Developments | Key Influences | Resulting Policies/Frameworks |
|---|---|---|---|
| 1950s-1960s | Early legal cases; Research ethics exposures | Salgo informed consent case; Beecher's research ethics articles | Legal foundation for informed consent; Initial research oversight |
| 1970s | Institutionalization; Regulatory response to scandals | Tuskegee syphilis study; Consumer rights movement | Belmont Report; Founding of Hastings Center and Kennedy Institute |
| 1980s-1990s | Systematization and expansion | Philosophical bioethics; Clinical ethics consultation needs | Principlism framework; Hospital ethics committees; Federal regulations |
Core Components of the U.S. Bioethics Infrastructure
Regulatory Frameworks for Drug Development and Research
The American bioethics infrastructure incorporates specific regulatory pathways for drug development that balance patient access with safety considerations:
Expanded Access (Compassionate Use): This regulatory pathway allows use of investigational drugs outside clinical trials for patients with serious or life-threatening diseases who cannot be treated satisfactorily with approved drugs and are ineligible for clinical trial participation [90] [91]. The framework requires sufficient evidence of safety and efficacy, informed consent, and often IRB review [90].
Right-to-Try Laws: Emerging as an alternative to expanded access, these laws allow patients with life-threatening diseases to request access to investigational treatments that have completed Phase 1 clinical trials without FDA oversight [90] [91]. These have been criticized for offering "false hope to patients without providing any actual improvements in access to investigational drugs" [90].
Off-Label Use Regulations: Unlike expanded access, off-label use of approved drugs is generally unregulated in the U.S., allowing physicians discretion in using drugs for non-approved indications [90]. This creates ethical challenges when off-label uses lack strong scientific evidence, potentially leading to adverse events [90].
Ethical Framework for Investigational Drugs
The treatment use of investigational drugs operates within a structured ethical framework consisting of eight core requirements [91]:
- Justified need (serious or life-threatening condition with no satisfactory authorized treatments)
- No threat to clinical development of the investigational drug
- Adequate scientific evidence to support the treatment
- Patient's benefit as primary goal
- Informed patient decision
- Fair access for patients
- Independent review
- Dissemination of treatment results
This framework aims to balance individual patient needs against societal interests in drug development and evidence generation [91].
Principlism as a Dominant Framework
The American bioethics infrastructure is characterized by its strong commitment to principlism as the primary methodological approach. This framework incorporates elements from multiple ethical theories [89]:
- Autonomy: Reflecting Kantian deontology with emphasis on individual rights and decision-making
- Beneficence: Aligned with utilitarian approaches focusing on outcomes and benefits
- Non-maleficence: Recalling Hippocratic traditions of avoiding harm
- Justice: Borrowing from Rawlsian theories of fair distribution
This blend of theoretical approaches aims to provide a comprehensive framework for addressing diverse ethical dilemmas in healthcare and research.
Efficacy and Applications in Research & Drug Development
Functionality in Regulating Innovative Treatments
The U.S. bioethics infrastructure provides specific guidance for addressing emerging ethical challenges in innovative treatments:
Guidance for Innovative Interventions: The Declaration of Helsinki (Paragraph 37) provides guidance for use of unproven interventions when proven treatments don't exist or have been ineffective, requiring expert consultation, informed consent, and subsequent research evaluation [90]. U.S. codes explicitly permit therapeutic use of new or innovative drugs under specific conditions [90].
Balancing Access and Evidence Generation: The framework aims to balance early access to promising treatments with the need for rigorous evidence generation through clinical trials [91]. This includes mechanisms to ensure expanded access doesn't threaten trial enrollment, particularly concerning in rare diseases with limited patient populations [91].
Ethical Oversight Structures: Institutional Review Boards (IRBs) provide independent ethical review of research protocols and expanded access requests, implementing federal regulations and ethical principles at the institutional level [91].
Table 2: Efficacy of U.S. Bioethics Frameworks in Drug Development Contexts
| Application Context | Key Regulatory/Ethical Mechanisms | Documented Efficacy | Limitations |
|---|---|---|---|
| Clinical Trial Ethics | Informed consent; IRB review; Risk-benefit analysis | Established protections for research subjects; Systematic oversight | Potential for biases in review; Variable implementation |
| Expanded Access | FDA regulations; IRB review; Informed consent; Monitoring | Provides pathway for treatment access outside trials | Limited awareness; Administrative burdens; Uncertain insurance coverage |
| Off-Label Use | Physician discretion; Professional guidelines; Liability systems | Flexibility in treatment options | Limited evidence for many uses; Potential for harm without adequate evidence |
Procedural Efficacy in Clinical Settings
Evidence suggests the bioethics infrastructure has successfully altered procedures in clinical and research environments:
Informed Consent Practices: The legal and ethical requirements for informed consent have become firmly established in clinical practice and research, ensuring patients and research subjects receive information about risks, benefits, and alternatives [92] [3].
Research Oversight: The implementation of IRB review has created systematic oversight for research involving human subjects, applying ethical principles to protocol review [89].
Documentation and Transparency: Ethical frameworks emphasize documentation of unproven interventions and dissemination of results, contributing to knowledge generation even in non-trial settings [90].
Critical Analysis of Limitations and Biases
Theoretical and Methodological Critiques
The U.S. bioethics infrastructure faces substantive theoretical and methodological challenges:
The Adjudication Problem: Principlism suffers from providing "no systematic guidance" when principles conflict, creating ambiguity in practical application [89]. Without a clear method for prioritizing competing principles, the framework offers "no guidance for adjudication" [89]. Critics contend that principlism merely provides "a check list of considerations" that practitioners can use to justify predetermined courses of action [89].
Theoretical Incompatibility: The combination of deontological (autonomy), utilitarian (beneficence), and justice-based approaches creates internal tension as these theories may provide "diametrically opposed guidance" in specific cases [89].
Action Guidance Deficiency: The lack of decisive guidance between conflicting ethical theories means bioethics "fail[s] to demonstrably guide individuals, hospitals, and society toward clear ethical aims and outcomes" [89].
Structural and Systemic Biases
The American bioethics infrastructure reflects several systemic biases that limit its comprehensiveness:
Individualist Orientation: U.S. bioethics demonstrates a strong tendency toward "individualist orientation," focusing on individual rights and autonomy while potentially neglecting community considerations and structural factors [20]. This orientation derives from its roots in the doctor-patient relationship and consumer rights movements [20] [3].
Western Cultural Bias: The framework reflects its Western origins through emphasis on autonomy and individual rights, potentially limiting applicability in more communitarian cultural contexts [20] [93].
Procedural Focus: The infrastructure emphasizes procedural solutions (informed consent, IRB review) which may not adequately address substantive ethical concerns or power imbalances in healthcare and research relationships [88].
Emerging Challenges and Adaptation Needs
Contemporary developments reveal additional limitations in the current infrastructure:
Community-Based Biology: Emerging movements like DIYbio and biohacking present challenges to conventional ethical oversight models [20]. These community-based efforts often prefer "community-driven and voluntary approaches to externally developed and imposed requirements" [20], conflicting with the established institutional ethics framework.
Algorithmic Decision-Making: The increasing use of artificial intelligence in drug development creates novel ethical challenges regarding "algorithmic decision-making without human judgment," research bias, and accountability [92].
Structural Determinants of Health: The individualized focus of U.S. bioethics often neglects "structural and political-economic determinants of health" and fails to adequately address health disparities and social determinants [20].
Visualizing Ethical Decision-Making in Investigational Drug Use
The following diagram illustrates the structured ethical decision-making process for using investigational drugs within the U.S. bioethics framework:
Diagram 1: Ethical Framework for Investigational Drug Use
Essential Research Reagents for Bioethics Analysis
Table 3: Analytical Frameworks in Bioethics Research
| Research 'Reagent' | Function | Application Context | Key References |
|---|---|---|---|
| Principlism Framework | Provides four-principle structure for ethical analysis | Clinical ethics consultation; Research ethics review | Beauchamp & Childress [89] |
| Belmont Report Principles | Foundation for human subjects research protections | IRB review; Research protocol development | National Commission [89] |
| Expanded Access Regulations | Pathway for pre-approval drug access | Serious diseases without treatment options | FDA Regulations [90] [91] |
| Informed Consent Documents | Ensure autonomous decision-making | Clinical trials; Innovative treatments | Salgo case; Belmont Report [92] [3] |
| Bias Identification Checklists | Identify cognitive and moral biases | Ethics consultation; Research design | BMC Medical Ethics [93] |
| Community Engagement Protocols | Incorporate diverse perspectives | Community-based research; DIY biology | Community Bioethics [20] |
The U.S. bioethics infrastructure represents a complex ecosystem of philosophical frameworks, regulatory systems, and practical guidelines that have demonstrated significant efficacy in addressing ethical challenges in biomedical research and clinical practice. Its strengths include strong protections for individual autonomy, systematic oversight mechanisms, and flexibility in addressing emerging technologies. However, substantial critiques highlight theoretical inconsistencies, structural biases, and adaptation challenges in responding to novel scientific approaches and changing societal values. Future development of the American bioethics infrastructure would benefit from addressing identified limitations, particularly through incorporation of virtue ethics to ameliorate the adjudication problem [89], greater attention to structural determinants of health [20], and development of more inclusive models that accommodate community-based biology and diverse value systems [20]. Such evolution would enhance the framework's ability to fulfill its fundamental mission of guiding ethical decision-making in biomedical research and clinical practice while maintaining necessary protections for patients and research subjects.
Bioethics emerged as a distinct discourse in the late 20th century, shifting conversations about moral responsibility in medicine and science from the exclusive domain of professionals to a broader community of stakeholders [59]. This analysis examines the divergent developmental pathways of bioethics in the United States and France, focusing particularly on the professionalization model that characterizes the American approach versus the state-mediated expert-model predominant in France. These differences reflect deeper variations in political culture, historical development, and conceptions of the state's role vis-à-vis its citizens [59]. Understanding these distinct trajectories provides valuable insights for researchers, scientists, and drug development professionals operating within these different ethical ecosystems and facilitates more effective cross-cultural collaboration in international research endeavors.
Historical Development and Founding Paradigms
The emergence of bioethics in the United States and France followed distinctly different historical pathways, shaped by each country's unique social, political, and cultural contexts.
United States: A Trajectory of Professionalization
The bioethics movement in the United States developed as a social movement that gradually transformed into a self-conscious occupational group, with increasing efforts toward certification and licensure [59]. This development was fueled by several key factors:
- External Oversight Demands: Beginning in the 1960s, biomedical issues that were once the exclusive concern of physicians and scientists became colonized by other interested parties, creating space for a new profession of bioethicists [59].
- Landmark Publications: Henry Beecher's influential 1966 article on ethical problems in clinical research signaled growing concern about ethical oversight within medical research, though Beecher still expected the medical profession itself to take appropriate action [3].
- Institutional Foundation: The 1969 founding of The Hastings Center (Institute of Society, Ethics and the Life Sciences) and the 1971 establishment of the Kennedy Institute of Ethics at Georgetown University provided institutional anchors for the emerging field, setting its direction, methods, and intellectual standards [3].
- Legal and Social Catalysts: The rise of the consumer rights movement and legal doctrines like informed consent (established in the 1957 Salgo case) created an environment conducive to external ethical oversight [3].
France: The Persistence of the Expert-Model
In contrast to the American experience, bioethics in France remained primarily a topic for expert debate and development within the established medical and scientific communities [59]. The French approach reflects several distinctive characteristics:
- State-Mediated Development: Rather than emerging as an independent profession, bioethical consideration in France developed through state-led initiatives and within existing professional hierarchies [94].
- Cultural Context: The French model reflects a particular cultural context where medical ethics has been shaped by "a republican model of bioethics" that differs significantly from the American rights-based approach [94].
- Internal Expertise: Ethical deliberation remained largely within the purview of established medical professionals rather than creating a new class of external ethics professionals [59] [94].
Table 1: Historical Development of Bioethics in the United States and France
| Aspect | United States | France |
|---|---|---|
| Primary Trajectory | Social movement to profession | Expert debate within medical/scientific community |
| Key Founding Period | Late 1960s - early 1970s | Late 1980s - early 1990s |
| Primary Catalysts | Social activism, legal rulings, consumer rights | State initiatives, professional self-regulation |
| Initial Institutionalization | Independent ethics centers (Hastings Center, Kennedy Institute) | Hospital ethics committees, state commissions |
| Relationship to Medical Profession | External oversight | Internal deliberation |
Structural and Organizational Frameworks
The structural manifestations of bioethics differ substantially between the United States and France, reflecting their different foundational paradigms.
United States: Professionalization and External Oversight
The American model features extensive external oversight mechanisms and a clear trajectory toward professionalization:
- Diverse Professional Backgrounds: Those claiming the title of bioethicist in the U.S. come from widely varied backgrounds: "physicians, nurses, attorneys, social workers, psychologists, patient activists, theologians, philosophers, narrative theorists, historians, economists, anthropologists, and sociologists" [59].
- Broad Functional Scope: Bioethical work encompasses "serving on national commissions; providing advice to the pharmaceutical industry; consulting at the bedside when there is conflict between and among caregivers, family members, and patients; reviewing research protocols; and writing for scholarly journals and the media" [59].
- Institutional Penetration: The professional model has become embedded in various institutions, most notably through Institutional Review Boards (IRBs) and their secretariats, though these still involve people from varied backgrounds rather than exclusively credentialed bioethicists [59].
- Movement Toward Credentialing: There has been increasing movement toward formal recognition of bioethics as a profession, with efforts to define core competencies and establish certification standards [59].
France: State-Led Coordination and Clinical Ethics
The French framework maintains stronger state coordination and emphasizes clinical ethics within medical institutions:
- Hospital Ethics Committees: France has developed ethics committees within hospitals, but these function differently than American IRBs, with the Institut Curie representing one example of a French approach to hospital ethics committees [94].
- Republican Model of Bioethics: The French system has been described as following a "republican model of bioethics" that contrasts with the American rights-based approach and places greater emphasis on solidarity and national consensus [94].
- Medical Authority: The French system maintains greater authority within the medical profession itself, with less external oversight from professional bioethicists [59].
- Political Transformation: Current political transformations in France are favoring new models of hospital ethics committees that reflect both international influences and distinctive French approaches [94].
Table 2: Structural Organization of Bioethics in the United States and France
| Structural Element | United States | France |
|---|---|---|
| Primary Institutional Sites | Independent ethics centers, IRBs, hospital ethics committees, corporate advisory boards | Hospital ethics committees, state commissions, medical professional organizations |
| Regulatory Framework | Decentralized with significant professional self-regulation | State-coordinated with medical professional oversight |
| Typical Background of Ethics Practitioners | Diverse fields (philosophy, law, social sciences, theology) | Predominantly medical and scientific fields |
| Approach to Legal Rights | Strong emphasis on individual rights and autonomy | Greater emphasis on solidarity and national consensus |
Methodological Approaches and Regulatory Frameworks
The methodological approaches to ethical deliberation and decision-making reflect deeper cultural and political differences between the two countries.
Conceptual Foundations and Their Applications
The following diagram illustrates the distinct logical pathways that characterize the American and French approaches to bioethical decision-making:
Regulatory and Oversight Mechanisms
The regulatory approaches in each country reflect their different foundational principles:
United States Regulatory Framework
The American regulatory landscape is characterized by:
- Institutional Review Boards (IRBs): These committees review research protocols to protect human subjects, representing a formalized system of external oversight [59].
- Rights-Based Legal Framework: The legal system emphasizes individual rights, with doctrines like informed consent forming the cornerstone of ethical practice [3].
- Demand-Based Professionalization: The development of bioethics as a profession follows what sociologists term a "demand theory of professionalization," where the state yields legal and economic privileges in response to demands from an organized group [59].
French Regulatory Framework
The French regulatory approach features:
- State-Led Ethical Deliberation: The French state plays a more direct role in organizing and overseeing ethical deliberation, as exemplified by initiatives like the National Consultative Ethics Committee for Health and Life Sciences [94].
- Supply Theory of Professionalization: Following what sociologists call a "supply theory," the French state grants legal recognition to professional domains only when it coincides with state purposes, which has limited the development of an independent bioethics profession [59].
- Medical Professional Authority: The system preserves greater authority for medical professionals themselves in ethical deliberation, with less independent professional bioethics oversight [59].
Implications for Research and Clinical Practice
The different models of bioethics in the United States and France have practical consequences for scientific research and clinical care.
Research Ethics Protocols
The following experimental workflow illustrates how research ethics protocols operate differently in each system:
Practical Implications for Research Professionals
For researchers, scientists, and drug development professionals, these different systems present distinct considerations:
- Informed Consent Processes: American researchers must navigate more extensive informed consent requirements with detailed documentation, while French researchers operate within a framework that may place greater emphasis on physician judgment and less on formalized consent procedures [3] [94].
- Ethical Oversight: American researchers typically interact with IRBs that include non-scientist members and professional ethicists, while French researchers often work within oversight structures dominated by scientific and medical professionals [59] [94].
- International Collaboration: Researchers collaborating across these systems must recognize and accommodate these different ethical frameworks, which can present challenges for multinational trials and research initiatives.
Essential Research Reagents and Methodological Tools
The following table outlines key conceptual "research reagents" essential for navigating the bioethical landscapes in both countries:
Table 3: Essential Conceptual Research Reagents for Comparative Bioethics Analysis
| Research Reagent | Function | U.S. Application | French Application |
|---|---|---|---|
| Informed Consent Protocols | Ensure patient autonomy and understanding | Extensive documentation; legal safeguard | More flexible application; physician-mediated |
| Ethics Committee Framework | Provide ethical oversight and review | Independent IRBs with diverse membership | Hospital committees with medical professional dominance |
| Professional Ethics Guidelines | Standardize ethical practice | Certification standards; core competencies | Medical professional codes; state guidelines |
| Case Deliberation Methodologies | Framework for analyzing ethical dilemmas | Principlism (autonomy, beneficence, etc.) | Republican bioethics framework |
| Regulatory Compliance Mechanisms | Ensure adherence to ethical standards | Legal liability; institutional certification | Professional accountability; state oversight |
The comparative analysis of American and French bioethics models reveals fundamentally different approaches to the institutionalization of ethical oversight in medicine and science. The American professionalization model, with its emphasis on individual rights, external oversight, and bioethics as a distinct profession, contrasts sharply with the French expert-model, which maintains ethical deliberation within the medical and scientific community under state coordination. These differences reflect deeper cultural, political, and historical variations that continue to shape how ethical issues are identified, analyzed, and resolved in each country. For researchers and drug development professionals operating internationally, understanding these distinctions is essential for effective cross-cultural collaboration and ethical practice. As bioethics continues to evolve globally, these distinct national approaches offer complementary strengths and limitations that can inform future developments in the field.
This whitepaper re-examines the foundational European influences on the institutionalization of bioethics within United States research frameworks, focusing on the pioneering contributions of German theologian Fritz Jahr. While modern American bioethics is often associated with the principialism that emerged in the late 20th century, its conceptual roots extend to 1920s Europe. Jahr coined the term "bio-ethik" in 1927 and formulated a "bioethical imperative" that anticipated contemporary ethical considerations in biological research. This paper analyzes the historical context of Jahr's work in Weimar Germany, its transmission to American bioethics, and the broader influence of German regulatory culture—including its impact on research oversight and the development of ethical commissions. By synthesizing historical analysis with contemporary applications, this guide provides researchers and drug development professionals with a refined understanding of the ethical foundations underpinning modern regulatory frameworks.
The institutionalization of bioethics in the United States, particularly within scientific research and drug development, is frequently traced to the 1970s and the work of American scholars. However, this narrative overlooks significant European intellectual contributions that provided the conceptual substrate for contemporary bioethical discourse. The modern bioethics movement emerged in response to unprecedented ethical problems created by postwar advances in medicine and biology that the traditional Hippocratic tradition could not adequately address [4] [95]. Within this context, the work of German theologian Fritz Jahr represents a critical, though long overlooked, foundation.
Jahr's conceptualization of "bio-ethics" in 1927 emerged from a specific historical moment in Germany, coinciding with early state-level experiments in research regulation. The 1931 guidelines for human experimentation issued by the German Reich, developed during the Weimar Republic, established procedural and ethical expectations for research conduct that would later influence international standards [96]. This paper argues that a proper understanding of contemporary bioethics requires acknowledging these European origins, particularly the synergistic relationship between ethical theory and regulatory practice that characterized the German context.
For research professionals, understanding this history is not merely academic; it provides essential context for the ethical frameworks that govern contemporary research practice. The principles of respect for persons, beneficence, and justice that undergird regulations like the Belmont Report have conceptual antecedents in earlier European thought [96] [17]. By examining these foundations, researchers can better appreciate the moral reasoning embedded in current research oversight mechanisms.
Fritz Jahr's Bioethical Imperative: A Conceptual Analysis
Historical Context and Intellectual Development
In 1927, Fritz Jahr, a Protestant pastor and theologian from Halle, Germany, published an article entitled "Bio-Ethik: Eine Umschau über die ethischen Beziehungen des Menschen zu Tier und Pflanze" (Bio-Ethics: A Review of the Ethical Relationships of Humans to Animals and Plants) in the journal Kosmos [96]. This publication marks the first documented use of the term "bioethics," predating the American bioethics movement by over four decades. Jahr's conceptualization emerged during the complex intellectual and political environment of the Weimar Republic, a period characterized by a "curious fusion between laws and regulations placing limits on medical experimentation and legislations later considered discriminatory and inhuman" [96].
Building on his initial formulation, Jahr further developed his concept in a 1934 paper where he articulated what he termed the "bioethical imperative." Paraphrasing Immanuel Kant's categorical imperative, Jahr proposed: "Respect every living being on principle as an end in itself and treat it, if possible, as such!" (Translated from the original German: "Achte jades Lebewesen grundsätzlich als einen Selbstzweck und behandle es nach Möglichkeit als solchen!") [96]. This formulation expanded moral consideration beyond humans to include all living beings, representing a significant departure from anthropocentric ethical systems.
Jahr's bioethical imperative was notable for its inclusive scope, encompassing not only mammals but also plants, though he acknowledged practical limitations in application. His theological examination specifically addressed the Biblical Fifth Commandment ("thou shalt not kill") in its implications for animal and plant welfare, exploring what constituted "humane" treatment across living organisms [96]. While distancing himself from Hindu traditions that held similar views, Jahr recognized parallel ethical considerations in Eastern philosophies such as Buddhism, Yoga, and Sankya [97].
Methodological Framework for Historical Analysis
Research into Jahr's contributions requires interdisciplinary methodology combining historical textual analysis with philosophical reconstruction. The following protocol outlines a systematic approach for researchers investigating early bioethics literature:
Table: Research Protocol for Analyzing Early Bioethics Texts
| Research Phase | Methodological Approach | Source Materials | Analytical Framework |
|---|---|---|---|
| Textual Location | Systematic review of early 20th-century German scientific and ethical journals | Kosmos (1927, 1934); German philosophical literature | Bibliometric analysis; historical contextualization |
| Conceptual Analysis | Philosophical reconstruction of ethical frameworks; comparative analysis | Jahr's articles; Kantian philosophy; theological ethics | Principle-based analysis; conceptual mapping |
| Historical Contextualization | Examination of socio-political and scientific milieu | Weimar Republic history; German research regulations (1931) | Historical institutionalism; intellectual history |
| Transmission Study | Tracking conceptual diffusion across time and cultures | Correspondence; citation analysis; comparative literature | Diffusion of innovations theory; reception studies |
The implementation of this methodology requires specific research competencies, including:
- German Language Proficiency: Essential for accurate translation and interpretation of primary sources
- Philosophical Training: Necessary for conceptual analysis of ethical frameworks
- Historical Methods: Required for proper contextualization within Weimar Germany's intellectual landscape
- Interdisciplinary Synthesis: Ability to connect theological, philosophical, and scientific discourses
Visualizing Jahr's Bioethical Framework
The conceptual structure of Jahr's bioethical imperative can be visualized through its philosophical influences and ethical scope:
German Regulatory Culture and Early Research Oversight
Historical Development of German Research Ethics
The development of bioethics in Germany occurred within a distinctive regulatory culture that evolved significantly from the Weimar period through postwar division and reunification. Germany's political structure as a federal republic consisting of independent states (Länder) created a decentralized approach to policy-making, including research regulation [98]. This cultural framework of "cooperative federalism" emphasized decentralization, subsidiarity, and plurality in governance [98].
The Weimar Republic period (1919-1933), during which Jahr developed his bioethics concept, witnessed important advancements in research oversight. Notably, Julius Moses succeeded in passing legislation in 1931 establishing guidelines for proper human experimentation [96]. These regulations represented one of Europe's earliest systematic attempts to govern medical research, though they were later violated during the Nazi regime, as documented during the Nuremberg trials [96].
Following World War II, Germany's approach to regulation was profoundly shaped by the legacy of National Socialist abuses. In West Germany, the "Basic Law" (Grundgesetz) of 1949 established a federal structure that granted significant cultural and educational authority to the Länder, known as Kulturhoheit [98] [99]. This decentralization was a deliberate response to the centralized control of culture and science under the Nazis, creating a system where "the municipalities and Länder maintain their own cultural institutions and offerings" [98]. This distribution of authority would later influence approaches to research governance and ethical oversight.
German Educational Foundations and Ethical Formation
Germany's contributions to bioethics extended beyond direct research regulation to include educational innovations that created ethical foundations for scientific practice. During the Protestant Reformation, German cities established "Europe's first large-scale experiments in mass public education" through municipal laws that supported public goods provision [100]. Cities that adopted these educational institutions demonstrated significant long-term growth advantages and produced more "upper tail human capital" - individuals with exceptional cultural, scientific, and economic contributions [100].
This educational legacy created a foundation for ethical deliberation in scientific practice that would later influence bioethical discourse. The German model of state-supported education established a precedent for public investment in knowledge systems that included ethical dimensions, a pattern that would recur in the development of research ethics oversight mechanisms in the 20th century.
Table: German Educational Foundations and Ethical Formation
| Historical Period | Educational Innovation | Institutional Mechanism | Impact on Ethical Capacity |
|---|---|---|---|
| Protestant Reformation (16th Century) | Municipal laws establishing mass public education | "Common chest" funding for public services | Development of human capital; ethical deliberation capacity |
| Weimar Republic (1919-1933) | Research regulations and ethical guidelines | 1931 guidelines for human experimentation | Procedural oversight for research ethics |
| Post-WWII Period | Decentralized cultural policy (Kulturhoheit) | Authority vested in Länder and municipalities | Pluralistic approach to ethical oversight |
Transmission to American Bioethics: Pathways and Institutions
Historical Transmission Mechanisms
The transmission of German bioethical concepts to American research ethics occurred through multiple pathways over several decades. The initial connection was established through the Nuremberg Doctors' Trial (1946-1947), which exposed American investigators to German medical ethics debates and the previously established 1931 German regulations [96]. This exposure directly influenced the development of the Nuremberg Code (1947), which became a foundational document for international research ethics.
The intellectual migration of European scholars to the United States before and after World War II provided another transmission mechanism. These scholars brought with them familiarity with European ethical discourses, including German philosophical traditions that informed Jahr's work. While Jahr himself remained in Germany and was not directly part of this migration, the intellectual traditions he represented traveled through these channels.
A significant transmission barrier existed in the linguistic and geographic separation between Jahr's German publications and the emerging English-dominated bioethics discourse. This explains why Jahr's contributions were "forgotten" for several decades before being rediscovered by bioethics historians [96]. The predominance of English-language literature in the emerging field of bioethics created a linguistic barrier that impeded recognition of non-English contributions.
Institutionalization in the United States
The establishment of bioethics institutions in the United States in the late 1960s and early 1970s created frameworks that would eventually incorporate European influences. The founding of The Hastings Center in 1969 and the Kennedy Institute of Ethics at Georgetown University in 1971 established bioethics as a distinct field with both theoretical and applied dimensions [3] [4]. These institutions developed in response to "unprecedented ethical problems" created by "spectacular advances in medicine and biology" that traditional medical ethics could not adequately address [4].
American bioethics initially developed with a strong emphasis on patient rights and consumer rights, reflecting the broader social movements of the 1960s [3]. President John F. Kennedy's 1962 "Consumer Bill of Rights" - emphasizing rights to safety, information, choice, and to be heard - provided a conceptual framework that aligned with the emerging bioethics emphasis on patient autonomy [3]. This rights-based approach differed somewhat from Jahr's more duty-oriented framework but shared a common commitment to expanding moral consideration.
The formal institutionalization of bioethics within the U.S. research system occurred through the creation of federal bioethics commissions, beginning with the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research (1974-78) [17]. This commission produced the landmark Belmont Report, which identified fundamental principles for research with human subjects and formed the basis for subsequent federal regulations [17]. While these American developments had distinct characteristics, they operated within an intellectual ecosystem that had been seeded with European ideas.
Comparative Analysis: Regulatory Implementation
Side-by-Side Framework Comparison
The divergent evolution of bioethics in Germany and the United States reflects their distinctive political cultures and historical experiences. The table below provides a systematic comparison of their regulatory approaches:
Table: Comparative Analysis of German and American Bioethics Frameworks
| Dimension | German Model | American Model |
|---|---|---|
| Governance Structure | Decentralized federalism (Kulturhoheit); primary authority with Länder | Mixed system with federal regulations and local Institutional Review Boards (IRBs) |
| Historical Foundations | Response to Nazi medical abuses; Weimar-era regulations | Response to domestic research scandals (Tuskegee, etc.); consumer rights movement |
| Philosophical Orientation | Duty-based; precautionary principle; strong state role | Rights-based; principialism (autonomy, beneficence, justice); proceduralism |
| Research Oversight | Centralized ethics commissions at university/state level | IRB system at institutional level with federal oversight |
| Legal Framework | Statutory regulations with binding force | Federal regulations with interpretive flexibility |
| Public Engagement | Deliberative model through political parties and social organizations | Advocacy model through patient rights and interest groups |
The Researcher's Toolkit: Essential Conceptual Frameworks
For research professionals navigating international bioethics frameworks, the following conceptual tools provide essential guidance:
Table: Essential Conceptual Frameworks for Research Ethics
| Conceptual Framework | Origin | Research Application | Regulatory Impact |
|---|---|---|---|
| Bioethical Imperative (Jahr) | German philosophical/theological tradition | Expands moral consideration beyond human subjects to animals and environment | Informs animal welfare regulations; environmental impact assessments |
| Informed Consent | U.S. case law (Salgo, 1957) | Requires comprehensive disclosure of risks/benefits to research participants | Foundation of human subjects research regulations; protocol requirements |
| Principialism (Beauchamp & Childress) | U.S. bioethics theory | Provides framework for ethical analysis of research dilemmas | Underlies Belmont Report; IRB decision-making processes |
| Precautionary Principle | German environmental policy (Vorsorgeprinzip) | Guides decision-making under uncertainty; emphasizes precaution in novel technologies | Influences regulatory approaches to emerging technologies (gene editing, etc.) |
| Deliberative Democracy | German political theory | Stakeholder engagement in ethical review processes | Shapes ethics committee composition and procedures |
Contemporary Applications and Research Implications
Implementation in Modern Research Environments
The integration of these historical ethical frameworks into contemporary research practice has significant implications for drug development professionals and researchers. Jahr's expansive view of moral consideration now finds application in environmental bioethics and sustainability practices within research institutions [97]. The principle of "respect for every living being" informs contemporary requirements for ethical treatment of laboratory animals and responsible environmental practices in research facilities.
The German concept of Vorsorgeprinzip (precautionary principle) has influenced regulatory approaches to emerging technologies in drug development, including gene therapies and nanomedicines. This principle justifies proactive risk assessment and cautious advancement when confronted with uncertain but potentially severe risks, creating a more measured approach to translational research.
The American principialism that dominates U.S. research ethics, while distinct from Jahr's formulation, shares a common commitment to systematic ethical analysis. The four principles of autonomy, beneficence, non-maleficence, and justice provide a practical framework for IRB deliberations and protocol review, operationalizing ethical theory into research oversight [96].
Methodological Framework for Ethical Analysis in Research
Research professionals can apply a synthesized ethical analysis framework that incorporates both European and American influences:
- Scope Definition: Identify all entities warranting moral consideration (human subjects, animal subjects, environmental impacts)
- Principle Identification: Apply relevant ethical principles (autonomy, beneficence, justice, respect for life)
- Regulatory Mapping: Identify applicable regulations at federal, state, and institutional levels
- Stakeholder Analysis: Identify all affected parties and incorporate perspectives
- Deliberative Process: Engage in structured ethical reasoning with documentation
- Implementation Protocol: Develop procedures to implement ethical decisions
- Oversight Mechanism: Establish ongoing monitoring and review processes
This methodology enables researchers to systematically address ethical dimensions throughout the research lifecycle, from protocol development to post-study analysis.
This re-examination of Fritz Jahr's contributions and German regulatory culture demonstrates the deeply transnational character of bioethics as a discipline. For contemporary researchers and drug development professionals, understanding these European origins provides important conceptual resources for navigating complex ethical challenges in emerging research domains.
Jahr's bioethical imperative, with its expansive moral scope, offers a valuable framework for addressing novel ethical questions in fields such as gene editing, synthetic biology, and artificial intelligence in drug discovery. The integration of this broader ethical vision with the procedural frameworks of American bioethics creates a more robust foundation for research ethics in the 21st century.
The institutionalization of bioethics through commissions, regulations, and oversight mechanisms represents the practical implementation of ethical principles that have deep historical roots. By appreciating this history, research professionals can better understand the moral foundations of their work and contribute to the ongoing development of ethical research practices that balance scientific innovation with moral responsibility.
The institutionalization of bioethics, particularly within the United States, cannot be understood as the development of a uniform, global standard. Rather, national bioethics frameworks emerge from a complex interplay of distinctive cultural, religious, and political forces. While foundational documents like the Nuremberg Code and the Declaration of Helsinki provide a common historical reference point for research ethics globally, their interpretation and implementation diverge significantly across national boundaries [101]. This divergence reflects deeper societal values about life, death, the role of the individual versus the community, and the proper relationship between science and state authority. In the U.S., this evolution has been characterized by a pragmatic, case-based approach, heavily influenced by principles-based ethics and a legalistic culture that emphasizes procedural fairness and individual rights [101]. Understanding these divergent paths is essential for researchers, scientists, and drug development professionals operating in an increasingly globalized research environment, as it illuminates the underlying rationales for varying regulatory and ethical requirements.
Cross-National Comparative Analysis of Clinical Ethics Frameworks
A comparative analysis of national guidelines for Clinical Ethics Committees (CECs) reveals stark contrasts in how countries conceptualize the very purpose and practice of clinical ethics.
United States: Pragmatism and Procedural Resolution
The American model, as defined by guidelines from the American Medical Association and the American Society for Bioethics and Humanities, is fundamentally pragmatic and applied [101]. Its primary focus is on achieving a "principled ethical resolution" to specific clinical cases, often with an emphasis on conflict resolution [101]. This approach is deeply consistent with the U.S. legal and cultural landscape, which prioritizes individual autonomy, patient self-determination, and a solutions-oriented mindset. Ethics consultation in the U.S. is a form of hands-on support, designed to navigate immediate dilemmas at the bedside.
France: Philosophical and Theoretical Deliberation
In stark contrast, the French approach to clinical ethics is theoretical and philosophical [101]. French national guidelines, embedded within its bioethics laws, encourage broad deliberation on ethical questions rather than focusing on case-specific consultations or resolutions [101]. This model reflects a French intellectual tradition that values abstract reasoning and public debate on foundational principles. The operation of CECs in France is less about resolving individual conflicts and more about engaging in a sustained societal conversation about medicine, ethics, and the role of science in society.
United Kingdom and Canada: Hybrid Models
The United Kingdom and Canada demonstrate hybrid models. British guidelines frame CECs as bodies that offer "ethics support and advice," situating them between the American and French extremes [101]. Canadian policies, meanwhile, have shown a distinct interest in formally defining the role of the bioethicist, indicating a professionalization of the field that blends theoretical knowledge with practical application [101].
Table 1: National Approaches to Clinical Ethics Committee Functions
| Country | Primary Focus of CECs | Underlying Cultural & Legal Context |
|---|---|---|
| United States | Principled resolution of specific cases, conflict resolution | Pragmatic, legalistic, individual autonomy |
| France | Theoretical deliberation, philosophical discussion | Philosophical, republican values, public debate |
| United Kingdom | Ethics support and advice | Pragmatic yet less legally-driven than U.S. |
| Canada | Role of the bioethicist, professional standards | Professionalization of ethics, hybrid model |
The Role of Religious and Cultural Traditions in Shaping Bioethics
Beyond political structures, religious and cultural traditions provide a powerful moral vocabulary that shapes national and regional perspectives on core bioethical issues. A comparison of Abrahamic religions and their influence on policies in Turkey, and an analysis of principles in Eastern European and Asian countries, illustrates this point.
Religious Interpretations of Bioethical Issues
The Turkish Presidency of Religious Affairs (RAA), representing an Islamic perspective, shares some common ground with Roman Catholicism and Orthodox Judaism on several bioethical issues, yet nuanced differences are evident [102]. All three traditions justify the sacredness of life and place great importance on God's will in its preservation [102]. Consequently, they uniformly prohibit practices like suicide and euthanasia. However, differences emerge on issues like contraception and the precise beginning of life.
Table 2: Religious Perspectives on Key Bioethical Issues
| Bioethical Issue | Islamic (Turkish RAA) | Roman Catholicism | Orthodox Judaism |
|---|---|---|---|
| Organ Transplantation | Permitted with conditions (medical necessity, no fiduciary transaction) | Approved | Approved |
| Assisted Reproduction | Permitted only between spouses; third-party donation forbidden | Generally forbidden | Varies, but often permitted within marriage |
| Contraception | Some methods approved for family planning; permanent methods forbidden | Forbidden | Approved under certain conditions |
| Abortion | Forbidden, except for medical necessity or rape | Forbidden | Permitted to save the mother's life |
| Brain Death | Accepted by some scholars, but debate persists; can delay organ donation | Accepted | Accepted |
Cultural Interpretations of Foundational Principles
A review of literature from Poland, Ukraine, India, and Thailand demonstrates how the four canonical principles of bioethics—autonomy, beneficence, non-maleficence, and justice—are interpreted through distinct cultural lenses [103]. In Poland and Ukraine, where culture is heavily shaped by Christianity (Catholicism and Orthodoxy respectively, the principle of autonomy can be tempered by a stronger emphasis on family involvement and community values [103]. In contrast, in India and Thailand, where culture is shaped by Hinduism and Buddhism, the principles of non-maleficence and beneficence are deeply intertwined with spiritual concepts like karma and the elimination of suffering [103]. This can lead to a more paternalistic approach where the physician's duty to do good (beneficence) is prioritized over strict patient autonomy.
Political and Institutional Influences on U.S. Bioethics
The bioethical framework in the United States is not static and is continually shaped by contemporary political and institutional pressures.
Policy and Research Security
Recent U.S. policy updates reflect a growing concern with research security and transparency. The National Institutes of Health (NIH) has implemented new policies requiring annual training on "Other Support" disclosures to ensure accurate reporting of all active and pending research support, including foreign affiliations [104]. Furthermore, by January 2026, institutions receiving significant federal funding must establish robust Research Security Programs covering cybersecurity, foreign travel security, and export control, and must prohibit participation in "Malign Foreign Talent Recruitment Programs" (MFTRPs) [104]. These policies directly shape the ethical environment for U.S. researchers, adding layers of compliance and oversight.
Political Ideology and the Administrative State
A more profound political threat to the U.S. bioethics infrastructure is identified in initiatives like "Project 2025," which aims to dismantle the professional civil service or "administrative state" [105]. A functioning, impartial civil service is the backbone of the regulatory agencies that ensure food and drug safety, occupational health, and scientific integrity. The erosion of these agencies would "undermine the trust that we have in government and policymaking" and cripple the nation's ability to respond to ethical challenges posed by emerging technologies like AI and gene editing [105]. This highlights how political ideology can directly impact the institutional machinery that translates ethical principles into practice.
Defense of Scientific Integrity
Bioethicists are also responding to attacks on the independence of science itself. Political interference in approved research grants and the proliferation of predatory, profit-driven publishing threaten the integrity of scientific knowledge [106]. From a bioethical standpoint, this is a issue of justice, as it violates "fair access to truth, fair recognition for honest work, and fair protection against exploitation and manipulation" [106]. Upholding the virtues of honesty and humility in the scientific method is thus an essential, though often overlooked, prerequisite for ethical research and public trust [106].
Methodology for Comparative Bioethics Analysis
To systematically study these divergent frameworks, researchers can employ a structured, comparative methodology. The following workflow outlines a replicable process for analyzing how ethical principles are implemented across different countries.
Experimental Workflow for Cross-Cultural Ethical Analysis
Figure 1: Workflow for conducting a comparative analysis of bioethical frameworks across nations, based on established literature review methodologies [103].
Table 3: Essential Research Reagent Solutions for Comparative Bioethics
| Research 'Reagent' | Function in Analysis |
|---|---|
| National Bioethics Laws & Guidelines | Provide the formal, legal framework for ethical practice within a country (e.g., French Bioethics Laws, U.S. NIH Policies) [101] [104]. |
| Religious Decrees & Fatwas | Illuminate the moral reasoning and doctrinal positions that influence public and professional values (e.g., RAA opinions, Vatican documents) [102]. |
| International Journal Publications | Reveal the operationalization of principles in practice and scholarly interpretation (e.g., Medicine, Health Care and Philosophy, Indian Journal of Medical Ethics) [103]. |
| Cultural Dimension Models | Provide a theoretical framework for understanding value differences (e.g., Hofstede's cultural dimensions theory) [103]. |
| Policy Documents from Think Tanks | Offer insight into emerging political pressures and proposed regulatory shifts (e.g., Project 2025 Mandate) [105]. |
The divergent paths of national bioethics frameworks are not a sign of failure but a reality of a world rich in cultural and political diversity. For the U.S. research community, this means recognizing that its own principlist, pragmatic approach is but one model among many. The pragmatic, case-based U.S. system differs fundamentally from the philosophical French model and is further distinguished by the religious and culturally-infused frameworks of other nations [101] [102] [103]. For researchers and drug development professionals engaged in international work, this understanding is critical. It necessitates cultural competence in ethics, an awareness of varying regulatory landscapes, and a commitment to the foundational virtues of science—honesty and humility—to maintain public trust [106]. As political pressures and new technologies continue to evolve, so too will these national frameworks, requiring ongoing dialogue and a nuanced appreciation for the complex forces that shape how societies navigate the ethical frontiers of science and medicine.
The institutionalization of bioethics in the United States emerged from a specific historical context, largely in response to domestic ethical crises in research and clinical practice. The modern era of health care ethics is often traced to Henry Beecher's influential 1966 article on ethical problems in clinical research, which highlighted failures to inform patients of risks in experimental treatments [3]. This was followed by the public revelation of the Tuskegee Syphilis Study (1932-1972), where researchers withheld treatment from African American men even after penicillin became available [107]. These scandals catalyzed the development of a U.S. bioethics framework primarily focused on individual rights, patient autonomy, and protection of research subjects, leading to the establishment of foundational institutions like The Hastings Center (1969) and the Kennedy Institute of Ethics (1971) [3].
However, this historically dominant U.S. approach—with its strong emphasis on individual autonomy and rights-based frameworks—faces limitations in addressing 21st-century global health challenges. The COVID-19 pandemic, climate change, and global health disparities have revealed the need for bioethical frameworks that prioritize solidarity, relational autonomy, and the common good alongside individual rights [108] [109]. Quantitative analysis of bioethics publications from 1990-2003 reveals a significant geographical bias in the field, with the United States contributing 59.3% of publications in leading journals, followed by the United Kingdom (13.5%), Canada (4%), and Australia (3.8%) [110]. This dominance of English-speaking Western perspectives in bioethical discourse has limited the field's capacity to incorporate diverse global viewpoints.
Table 1: Dominance of English-Speaking Countries in Bioethics Publications (1990-2003)
| Country | Number of Publications | Percentage of Total Publications | Publications per Million Inhabitants |
|---|---|---|---|
| United States | 2,390 | 59.3% | 8.2 |
| United Kingdom | 544 | 13.5% | 9.2 |
| Canada | 160 | 4.0% | 5.1 |
| Australia | 154 | 3.8% | 7.7 |
| Netherlands | 109 | 2.7% | 6.7 |
| All Other Countries | 672 | 16.7% | - |
This paper argues that the U.S. bioethics system can be strengthened by incorporating governance approaches from other nations and international bodies. By examining models that emphasize collaborative governance, care-based ethics, and cosmopolitan ideals, U.S. researchers, scientists, and drug development professionals can develop more robust ethical frameworks for addressing complex global health challenges.
Theoretical Foundations: Expanding the Bioethical Framework
Global bioethics differs from traditional international bioethics in both scope and theoretical orientation. While international bioethics studies "the ethical aspects of relations between and among nations or regions of the world," global bioethics recognizes that contemporary ethical challenges arise from processes of globalization that transcend national boundaries and require broader theoretical perspectives [108]. This distinction has profound implications for ethical governance.
The dominant U.S. bioethics framework has historically emphasized a rights-based approach centered on four key principles: respect for autonomy, beneficence, non-maleficence, and justice [111]. While these principles provide important protections for individual research subjects and patients, they offer limited guidance for addressing communal good, structural inequities, and global health disparities. As noted in recent commentary, "bioethics as a field is ill-equipped to meet these challenges because its primary tools were designed with a different purpose" [109].
International approaches often incorporate complementary ethical frameworks that could enhance U.S. bioethical governance:
Care-based ethics: This feminist approach, defended by scholars like Rosemary Tong, prioritizes human connectedness and relationality, arguing that "without care, human rights will not be respected" [108]. This perspective acknowledges human vulnerability and mutual dependency as fundamental anthropological experiences that should inform ethical deliberation.
Cosmopolitan ideals: Global bioethics is inspired by cosmopolitan principles that consider each human being as both a citizen of their own community and a citizen of the world, emphasizing "the unity of humanity, solidarity, equality, openness to differences, and focus on what human beings have in common" [108].
Empowerment ethics: Drawing from Van Rensselaer Potter's original conceptualization of bioethics, this approach emphasizes responsible self-governance that leads to "awareness of our individual and social actions," which should further lead to "self-responsibility and even to accountability mechanisms" [112].
These theoretical perspectives are not opposed to rights-based approaches but can reinforce them by directing "attention to social, economic and political conditions that are often oppressive and unjust" [108]. A relational interpretation of rights emphasizes human connectedness and can amplify the significance of care in global health contexts.
International Governance Models: Key Comparative Insights
Collaborative Governance: The Québec Case Study
An innovative approach to bioethical governance emerges from Québec, Canada, where health authorities implemented a feasibility study (2018-2021) for an antibiotic use surveillance program in animal health [112]. This case exemplifies a distinctive methodology for collaborative governance that distinguishes between "consultation" and "concertation":
Consultation aims to gather information from stakeholders to help experts develop the optimal model.
Concertation seeks consensus among stakeholders about which criteria and values should guide model development.
The Québec process brought together 100 representatives from industry, academia, government, associations, and various professions (breeders, veterinarians, nutritionists, researchers) through a saturation recruitment process designed to capture all relevant perspectives [112]. This governance model produced three key recommendations that could inform U.S. approaches:
- Building data systems and information platforms based on trust rather than mere compliance
- Co-constructing a common normative language across sectors
- Designing a collaborative governance regime to shape program functioning
Table 2: Québec Antimicrobial Surveillance Governance Model
| Governance Element | Traditional U.S. Approach | Québec Collaborative Approach | Potential U.S. Application |
|---|---|---|---|
| Stakeholder Engagement | Expert-driven consultation | Saturation recruitment and concertation | Include diverse stakeholders in criteria-setting, not just data collection |
| Data Governance | Compliance-focused | Trust-based systems | Develop data sharing frameworks that prioritize relationship-building |
| Norm Development | Top-down regulation | Co-constructed common language | Create interdisciplinary working groups for guideline development |
| Implementation Strategy | Regulatory enforcement | Collaborative governance regime | Establish public-private-academic partnerships for complex health issues |
Ethical Governance of International Research Collaborations
The globalization of biomedical research presents significant ethical challenges that transcend national frameworks. The BIONET project, a large-scale Sino-European collaboration (2006-2009), identified critical challenges when national ethical governance systems intersect in cross-continental research [113]. This research revealed that effective ethical governance requires attention to four interconnected layers:
- National ethical deliberation: Organized processes for debating science directions as a matter of stewardship
- Ethical regulation: Laws, guidelines, and standards governing research
- Ethical oversight: Institutional review boards or ethics committees
- Ethical interaction: Moments of contact between researchers and participants
The BIONET project found that intersections between different national systems in these four layers create unique challenges for global collaborations [113]. For instance, differences in informed consent practices, data sharing protocols, and community engagement expectations between European and Chinese institutions required innovative governance approaches beyond simply applying either country's existing framework.
Reflexive Governance and Empowerment Ethics
European approaches to bioethics often incorporate what is termed "reflexive governance," which functions as "a systematic critical-thinking procedure that aims to define its value: What are the 'right' criteria to justify how to govern 'good' actions for a 'better' future?" [112]. This methodology involves "mapping, framing, and shaping the dynamics of interests and perspectives that could jeopardize a 'better' future" and hybridizes methods from collective deliberation and expert evaluation.
The diagram below illustrates this reflexive governance framework:
This reflexive model represents a significant departure from static, compliance-based approaches common in U.S. governance structures, offering instead a dynamic, iterative process for addressing complex bioethical challenges in rapidly evolving fields like gene editing and artificial intelligence.
Practical Implementation: Protocols and Governance Toolkits
Experimental Protocol: Concertation Methodology for Stakeholder Engagement
Based on the Québec case study, researchers and governance bodies can implement the following detailed protocol for collaborative governance development [112]:
Objective: To establish an ethical governance framework through inclusive stakeholder engagement that moves beyond consultation to genuine concertation.
Phase 1: Preparation and Scoping
- Define the bioethical challenge and its stakeholders
- Conduct preliminary mapping of interests, perspectives, and potential conflicts
- Develop a saturation recruitment strategy to ensure all relevant sectors and perspectives are represented
- Establish neutral facilitation mechanisms
Phase 2: Recruitment and Onboarding
- Identify representatives from industry, academia, government, professional associations, and affected communities
- Aim for approximately 100 participants for complex issues to ensure diversity without becoming unmanageable
- Provide comprehensive background materials and clear explanations of the concertation process
- Establish shared vocabulary and understanding of key concepts
Phase 3: Concertation Events
- Facilitate structured dialogues focusing on values and criteria for "better" futures, not just technical solutions
- Use iterative discussion formats that allow for refinement of positions
- Document areas of agreement and disagreement without premature resolution
- Focus on developing shared understanding rather than merely achieving compromise
Phase 4: Synthesis and Implementation
- Translate concertation outcomes into governance frameworks
- Establish mechanisms for ongoing stakeholder engagement
- Develop monitoring and evaluation protocols with stakeholder input
- Create adaptation mechanisms for evolving challenges
Validation: This protocol successfully built consensus for Québec's antibiotic use surveillance program, resulting in stakeholder-supported recommendations for data governance and collaborative management [112].
For U.S. researchers and drug development professionals engaging in international collaborations, the following tools and frameworks are essential for navigating diverse ethical landscapes:
Table 3: Research Reagent Solutions for Ethical Global Collaboration
| Tool/Framework | Function | Application Context |
|---|---|---|
| UNESCO Universal Declaration on Bioethics | Provides foundational ethical principles for global research | Establishes common ground for international collaborations; reference point for resolving cross-cultural ethical disagreements |
| BIONET Ethical Governance Guidelines | Offers specific guidance for Sino-European collaborations, adaptable to other contexts | Managing differences in informed consent practices, data sharing, and community engagement across regulatory systems |
| Reflexive Governance Methodology | Systematic critical-thinking procedure for defining ethical criteria | Complex, evolving fields like gene editing and AI in healthcare where existing guidelines are insufficient |
| Stakeholder Concertation Protocol | Methodology for moving beyond consultation to consensus-building | Developing ethically robust governance frameworks for controversial or emerging technologies |
| Four-Layer Ethical Governance Model | Analytical framework for identifying governance challenges | Assessing and strengthening each layer (deliberation, regulation, oversight, interaction) in international collaborations |
| Care Ethics Assessment Tool | Evaluates impact of research on human relationships and vulnerabilities | Complementing traditional risk-benefit analyses with relational considerations |
Implementation Roadmap for U.S. Bioethical Governance
Integrating international approaches into U.S. bioethical governance requires strategic adaptation rather than wholesale adoption. The following roadmap outlines key steps for researchers, institutions, and policymakers:
Short-Term Actions (0-12 months):
- Incorporate global case studies and comparative ethics into training programs for researchers and IRB members
- Establish "international perspectives" advisory groups within existing ethics committees
- Pilot concertation methodologies for specific challenging areas like AI ethics or gene editing governance
- Develop template protocols for international collaborations that address the four layers of ethical governance
Medium-Term Initiatives (1-3 years):
- Create formal partnerships with international ethics bodies and research institutions
- Implement reflexive governance structures for emerging technologies that include regular critical reflection and adaptation cycles
- Develop hybrid ethical frameworks that integrate rights-based and care-based approaches
- Establish funding mechanisms specifically for developing ethical governance capacity
Long-Term Transformations (3-5 years):
- Institutionalize collaborative governance models in federal research agencies
- Develop comprehensive ethical governance curricula for research scientists
- Create permanent public engagement mechanisms for bioethical deliberation
- Lead international efforts to develop adaptive governance frameworks for global health challenges
This implementation approach allows the U.S. to maintain its strengths in research ethics oversight while incorporating more robust mechanisms for addressing relational responsibilities, global solidarity, and complex systemic challenges.
The U.S. bioethics system, forged in response to specific historical ethical failures, has developed robust protections for individual research participants and patients. However, 21st-century challenges—from pandemic response to global genetic data sharing—require complementary approaches that emphasize relational responsibility, collaborative governance, and global solidarity.
By integrating insights from international models, U.S. researchers, scientists, and drug development professionals can develop more comprehensive ethical frameworks that:
- Combine rights-based and care-based approaches to honor both individual dignity and human connectedness
- Implement collaborative governance structures that engage diverse stakeholders through concertation rather than mere consultation
- Adopt reflexive methodologies that allow for continuous adaptation to emerging technologies and challenges
- Address all four layers of ethical governance—deliberation, regulation, oversight, and interaction—in international collaborations
This integrated approach will enhance the U.S. system's capacity to address both domestic and global bioethical challenges, fostering research environments that are not only ethically compliant but also ethically exemplary in their attention to justice, relationship, and the common good in an increasingly interconnected world.
Conclusion
The institutionalization of bioethics in the United States represents a direct response to historical ethical failures, catalyzed by social movements and solidified through legal and regulatory frameworks. The field's journey—from reactive scandal management to a structured profession governing clinical and research ethics—highlights its critical role in maintaining public trust and scientific integrity. Key takeaways include the enduring importance of foundational principles like informed consent and independent review, the ongoing need to adapt to novel biotechnologies, and the value of understanding different national models for addressing common ethical challenges. For biomedical researchers and drug developers, this historical and structural understanding is not merely academic; it is essential for navigating the complex ethical terrain of modern science, ensuring the responsible advancement of human health, and anticipating the moral questions on the horizon, from AI in medicine to global health equity.
References
- 1. The Code of Medical Ethics of the American ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3399321/]
- 2. Nuremberg Code: Directives for Human Experimentation [https://ori.hhs.gov/content/chapter-3-The-Protection-of-Human-Subjects-nuremberg-code-directives-human-experimentation]
- 3. The Rise of Bioethics: A Historical Overview - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK543570/]
- 4. Bioethics and Policy—A History [https://www.thehastingscenter.org/briefingbook/bioethics-and-policy-a-history/]
- 5. The History of Bioethics Series – National ... [https://bioethicsarchive.georgetown.edu/pcsbi/blog/2016/01/27/the-history-of-bioethics-series-national-bioethics-commissions/index.html]
- 6. About The Untreated Syphilis Study at Tuskegee [https://www.cdc.gov/tuskegee/about/index.html]
- 7. Fiftieth Anniversary of Uncovering the Tuskegee Syphilis Study [https://pmc.ncbi.nlm.nih.gov/articles/PMC9872801/]
- 8. The Tuskegee Syphilis Study [https://onlineethics.org/cases/tuskegee-syphilis-study]
- 9. Effects on Research | The U.S. Public Health Service ... [https://www.cdc.gov/tuskegee/about/effects-research.html]
- 10. Tuskegee Syphilis Study [https://en.wikipedia.org/wiki/Tuskegee_Syphilis_Study]
- 11. Revisionist Accounts of the Tuskegee Syphilis Study and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4568718/]
- 12. Tuskegee Experiment: The Infamous Syphilis Study [https://www.history.com/articles/the-infamous-40-year-tuskegee-study]
- 13. Tuskegee redux: Evolution of legal mandates for human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3731206/]
- 14. The Legacy of the Tuskegee Syphilis Study: Assessing its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2702151/]
- 15. A half century of electronic fetal monitoring and bioethics [https://pmc.ncbi.nlm.nih.gov/articles/PMC5697350/]
- 16. THE ROLE OF LAW IN THE DEVELOPMENT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3038328/]
- 17. History of Bioethics Commissions [https://bioethicsarchive.georgetown.edu/pcsbi/history.html]
- 18. WHAT CAN HISTORY DO FOR BIOETHICS? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3654172/]
- 19. The US Congress and Bioethics, 1960-1975 [http://dissertationreviews.org/the-us-congress-and-bioethics-1960-1975/]
- 20. Community Bioethics: Provocations for Institutionalized ... [https://theoryandpractice.citizenscienceassociation.org/articles/10.5334/cstp.525]
- 21. The Birth of Bioethics: Who is Paul Ramsey? [https://cbc-network.org/2005/01/the-birth-of-bioethics-who-is-paul-ramsey/]
- 22. Potter's notion of bioethics [https://pubmed.ncbi.nlm.nih.gov/22787958/]
- 23. 1. A Foundation for Bioethics: Van Rensselaer Potter's ... [https://books.openbookpublishers.com/10.11647/obp.0320/ch1.xhtml]
- 24. Global Bioethics - MSU Press [https://msupress.org/9780870132643/global-bioethics/]
- 25. KIE History - Kennedy Institute of Ethics - Georgetown University [https://kennedyinstitute.georgetown.edu/kie-history/]
- 26. The Birth of Bioethics: Who is Paul Ramsey? [https://cbc-network.org/2006/11/the-birth-of-bioethics-who-is-paul-ramsey-2/]
- 27. Canterbury v. Spence, No. 22099 (D.C. Cir. 1972) [https://law.justia.com/cases/federal/appellate-courts/cadc/22099/22099.html]
- 28. Canterbury v. Spence [https://en.wikipedia.org/wiki/Canterbury_v._Spence]
- 29. Duty to Warn - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK542236/]
- 30. Tarasoff rule | Research Starters [https://www.ebsco.com/research-starters/law/tarasoff-rule]
- 31. Duty Warn/Protect (Tarasoff) - Psych Law GAP [https://psychlawgap.com/article/duties-to-protect/]
- 32. Bioethics: How the Discipline came to be in the United States [https://uchile.cl/investigacion/centro-interdisciplinario-de-estudios-en-bioetica/publicaciones/bioethics-how-the-discipline-came-to-be-in-the-united-states]
- 33. The History of the Belmont Report | 2020 | IRB Blog [https://www.tc.columbia.edu/institutional-review-board/irb-blog/2020/the-history-of-the-belmont-report/]
- 34. The creation of the Belmont Report and its effect on ethical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9700634/]
- 35. Belmont Report [https://en.wikipedia.org/wiki/Belmont_Report]
- 36. Guiding Principles for Ethical Research [https://www.nih.gov/health-information/nih-clinical-research-trials-you/guiding-principles-ethical-research]
- 37. How to Ensure your Clinical Research is Ethical - 7 Key ... [https://www.linkedin.com/pulse/how-ensure-your-clinical-research-ethical-7-key-joshua-brostoff]
- 38. Guiding Ethical Principles - Research Support [https://researchsupport.psu.edu/orp/irb/information-for-participants/guiding-ethical-principles/]
- 39. Institutional Review Boards: Purpose and Challenges - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4631034/]
- 40. Ethical Guidelines and the Institutional Review Board [https://pmc.ncbi.nlm.nih.gov/articles/PMC10885741/]
- 41. History of Research Ethics - IRB [https://ori.umkc.edu/facilities-compliance-and-commercialization/compliance/irb/history-of-research-ethics.html]
- 42. The Role of IRBs in Research Oversight: Information for ... [https://www.wcgclinical.com/insights/the-role-of-irbs-in-research-oversight-information-for-potential-participants-in-clinical-research/]
- 43. History of the IRB [https://www.hpu.edu/oaa/institutional-review-board/history.html]
- 44. Beginner's Guide to institutional review boards (IRBs) [https://www.advarra.com/blog/beginners-guide-to-institutional-review-boards/]
- 45. Institutional review board (IRB) [https://www.britannica.com/topic/institutional-review-board]
- 46. Institutional Review Boards Frequently Asked Questions [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/institutional-review-boards-frequently-asked-questions]
- 47. What is the Institutional Review Board (IRB)? [https://research.oregonstate.edu/ori/irb/what-institutional-review-board-irb]
- 48. Impact of Institutional Review Board Practice Variation on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1681539/]
- 49. 2025 Hastings Center Fellows Are Named [https://www.thehastingscenter.org/news/hastings-center-welcomes-2025-fellows/]
- 50. Preconference Sessions | ASBH [https://asbh.org/annual-meeting/preconference-sessions]
- 51. 2025 Healthcare Ethics and Moral Distress Consultation ... [https://med.virginia.edu/biomedical-ethics/2025/07/23/healthcare-ethics-and-moral-distress-consultation-intensive-training-seminar/]
- 52. ASBH Humanities and Bioethics Conference [https://asbh.org/annual-meeting/bioethics-humanities-meeting]
- 53. Ethics Dispatch September 2025 [https://www.practicalbioethics.org/blog/ethics-dispatch-september-2025/]
- 54. Bioethical knowledge in students and health professionals [https://pmc.ncbi.nlm.nih.gov/articles/PMC11041021/]
- 55. 2025 Best Bioethics/Medical Ethics Schools [https://www.collegefactual.com/majors/health-care-professions/bioethics-medical-ethics/rankings/top-ranked/]
- 56. Best Bioethics/Medical Ethics colleges in the US 2025 [https://www.universities.com/programs/bioethics-medical-ethics-degrees]
- 57. The current status and challenges of bioethics education in ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-024-05599-5]
- 58. Bioethics and adolescents: a comparative analysis of student ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9629197/]
- 59. Bioethics in the United States and France - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2743496/]
- 60. Considerations for applying bioethics norms to a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7992125/]
- 61. A Spotlight on Johnson & Johnson's Bioethics Efforts [https://www.jnj.com/our-company/advancing-human-health-and-innovation-excellence-spotlight-on-johnson-johnsons-bioethics-efforts]
- 62. Research Ethics | Bioethics [https://www.lilly.com/science/research-development/research-principles/research-ethics]
- 63. Ethical Design of Data-Driven Decision Support Tools for ... [https://cancer.jmir.org/2025/1/e65566]
- 64. A quantitative analysis of the use of anonymization in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12078711/]
- 65. Bioethical knowledge in students and health professionals [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2024.1252386/full]
- 66. Bioethics [https://www.novonordisk.com/science-and-technology/bioethics.html]
- 67. Research Unbound: Seeking Ethical Solutions to New (and ... [https://trentcenter.duke.edu/research-unbound-seeking-ethical-solutions-new-and-old-problems]
- 68. Ethical issues in diagnosis and management of patients ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1119582/]
- 69. Unwaivable Conflicts of Interest [https://calawyers.org/business-law/unwaivable-conflicts-of-interest/]
- 70. Reviewing fair subject selection considerations for the unique ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9389279/]
- 71. From Code to Life: The AI‐Driven Revolution in Genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12376515/]
- 72. CRISPR & Ethics [https://innovativegenomics.org/crisprpedia/crispr-ethics/]
- 73. Bioethics | Internet Encyclopedia of Philosophy [https://iep.utm.edu/bioethics/]
- 74. THE ROLE OF LAW IN THE DEVELOPMENT OF AMERICAN BIOETHICS - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3038328/]
- 75. Vulnerability in research ethics: A systematic review of policy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12212517/]
- 76. The Price of Survival: Ethical Failures and Pharmaceutical ... [https://www.bcphreview.org/article/141218-the-price-of-survival-ethical-failures-and-pharmaceutical-profit-in-the-u-s-drug-market]
- 77. The benefits of more government interference in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10297769/]
- 78. Visualizing an Ethics Framework: A Method to Create ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6996733/]
- 79. Navigating color integrity in data visualization - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11117063/]
- 80. Ethics of Data Visualization: Avoiding Deceptive Practices [https://www.analyticodigital.com/blog/ethics-of-data-visualization-avoiding-deceptive-practices]
- 81. The ethics of exposure: Relational bioethics, responsibility, ... [https://www.sciencedirect.com/science/article/pii/S2352552525001483]
- 82. The Hastings Center Bioethics Timeline [https://www.thehastingscenter.org/bioethics-timeline/]
- 83. A contextual integrity approach to genomic information [https://link.springer.com/article/10.1007/s11019-024-10211-0]
- 84. Global research collaboration strategies that support ... [https://www.springernature.com/gp/librarians/the-link/open-science-blogpost/global-research-collaboration-strategies-bibliometric-insights/26727938]
- 85. An Ethics Framework for Big Data in Health and Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC7747261/]
- 86. The 2024 Revision of the Declaration of Helsinki and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11893356/]
- 87. A bioethical framework to guide the decision-making process ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-018-0317-y]
- 88. The Limitations of Bioethics: A Personal History - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK543568/]
- 89. A Critique of Principlism | Voices in Bioethics [https://journals.library.columbia.edu/index.php/bioethics/article/view/10522]
- 90. Ethics codes and use of new and innovative drugs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6379208/]
- 91. Ethics framework for treatment use of investigational drugs [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-020-00560-9]
- 92. The Ethics of Clinical Trials in the Drug Development Process [https://www.meetlifesciences.com/media-hub/blog/the-ethics-of-clinical-trials-in-the-drug-development-process/]
- 93. Biases in bioethics: a narrative review | BMC Medical Ethics [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-023-00894-0]
- 94. A French Perspective on Hospital Ethics Committees [https://www.cambridge.org/core/journals/cambridge-quarterly-of-healthcare-ethics/article/french-perspective-on-hospital-ethics-committees/8F15425CAEB94F6351641BD98633278B]
- 95. Bioethics, History [https://link.springer.com/content/pdf/10.1007/978-3-030-54161-3_85.pdf]
- 96. Bioethics and animal research. A personal perspective and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2997650/]
- 97. The eco-ethical contribution of Menico Torchio – a forgotten ... [https://peh-med.biomedcentral.com/articles/10.1186/s13010-023-00145-5]
- 98. Germany 1.1 | Compendium of Cultural Policies & Trends [https://www.culturalpolicies.net/country_profile/germany-1-1/]
- 99. From a divided city to a capital city : Berlin's cultural policy ... [https://chmcc.hypotheses.org/2474]
- 100. Origins of growth: How state institutions forged during the ... [https://cepr.org/voxeu/columns/origins-growth-how-state-institutions-forged-during-protestant-reformation-drove]
- 101. How do national guidelines frame clinical ethics practice? ... [https://www.sciencedirect.com/science/article/abs/pii/S0277953613001317]
- 102. A COMPARATIVE ANALYSIS OF BIOETHICAL ISSUES ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5675570/]
- 103. Ethical principles across countries: does 'ethical' mean the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12188308/]
- 104. NIH Policy Updates - Office of the Vice Chancellor for Research [https://research.cuanschutz.edu/ogc/home/resources/updates-team-talks/featured/ogc-newsroom/nih-policy-updates]
- 105. The Reactionary Recommendations of Project 2025 [https://www.thehastingscenter.org/the-reactionary-recommendations-of-project-2025-why-bioethicists-should-care/]
- 106. Ethics Dispatch October 2025 [https://www.practicalbioethics.org/blog/ethics-dispatch-october-2025/]
- 107. Research Ethics Timeline [https://www.niehs.nih.gov/research/resources/bioethics/timeline]
- 108. The challenges of global bioethics - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8856073/]
- 109. Bioethics Must Address War as a Public Health Crisis [https://www.thehastingscenter.org/bioethics-must-address-war-as-a-public-health-crisis/]
- 110. How international is bioethics? A quantitative retrospective study [https://pmc.ncbi.nlm.nih.gov/articles/PMC1351197/]
- 111. Global Bioethics: Addressing Current Challenges ... [https://www.intechopen.com/chapters/1217243]
- 112. Bio-Ethics and One Health: A Case Study Approach to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8971560/]
- 113. From global bioethics to ethical governance of biomedical ... [https://www.sciencedirect.com/science/article/abs/pii/S0277953613002104]