The Belmont Report in Practice: Applying Ethical Principles to Modern Human Subjects Research
This article provides a comprehensive analysis of the Belmont Report's three core ethical principles—Respect for Persons, Beneficence, and Justice—and their critical application in contemporary biomedical and behavioral research.
The Belmont Report in Practice: Applying Ethical Principles to Modern Human Subjects Research
Abstract
This article provides a comprehensive analysis of the Belmont Report's three core ethical principles—Respect for Persons, Beneficence, and Justice—and their critical application in contemporary biomedical and behavioral research. Tailored for researchers, scientists, and drug development professionals, it explores the historical foundation of these principles, offers methodological guidance for their implementation in study design and IRB protocols, addresses common challenges and optimization strategies, and validates their enduring relevance through comparison with other ethical frameworks and adaptation to modern research contexts like internet-mediated studies.
The Bedrock of Bioethics: Understanding the Belmont Report's History and Core Principles
The Tuskegee Syphilis Study, conducted by the United States Public Health Service (PHS) from 1932 to 1972, stands as one of the most egregious violations of human rights in the history of biomedical research [1]. This 40-year study of untreated syphilis in African American men ultimately triggered a national reckoning, leading to the National Research Act of 1974 and the creation of the Belmont Report, which established the foundational ethical principles for human subjects research in the United States [2] [3]. The journey from exploitation to ethical safeguards represents a critical evolution in scientific practice, framing a broader thesis on the indispensable role of the Belmont Report's principles. For researchers, scientists, and drug development professionals, understanding this historical context is not merely an academic exercise but a fundamental requirement for conducting ethically sound research that maintains public trust and upholds the dignity of every participant.
The Tuskegee Syphilis Study: Methodology and Ethical Failures
Study Design and Original Protocol
Initiated in 1932, the "Tuskegee Study of Untreated Syphilis in the Negro Male" was designed to observe the natural progression of untreated syphilis over a planned six to eight months [1] [4]. Investigators enrolled 600 impoverished African American sharecroppers from Macon County, Alabama; 399 had latent syphilis, and 201 served as uninfected controls [1] [5]. The study was conceived after the retrospective "Oslo Study of Untreated Syphilis" in white males, with U.S. Public Health Service officials seeking to build a prospective study to complement it [1]. A misguided racial hypothesis underpinned the research, as physicians at the time believed syphilis affected African Americans differently than whites, with more pronounced cardiovascular effects rather than neurological impact [1].
Table 1: Tuskegee Syphilis Study Participant Demographics and Outcomes
| Category | Enrollment Figures | Long-Term Outcomes |
|---|---|---|
| Total Participants | 600 African American men [1] | Only 74 subjects alive at study termination in 1972 [1] |
| Syphilitic Group | 399 men with latent syphilis [1] | 28 died directly from syphilis; 100 died from related complications [1] |
| Control Group | 201 men without syphilis [1] | Outcomes not fully documented but exposed to same study procedures |
| Secondary Victims | Not enrolled | 40 wives infected; 19 children born with congenital syphilis [1] |
Research Protocol and Methodological Flaws
The study's methodology involved repeated data collection without therapeutic intent. Key procedures included:
- Deceptive Recruitment and Retention: Participants were recruited with promises of free medical care for "bad blood," a colloquial term encompassing various conditions including syphilis, anemia, and fatigue [1]. They were not informed of their syphilis diagnosis or the study's true purpose [1]. To ensure compliance with painful procedures like diagnostic lumbar punctures, researchers sent a misleading letter titled "Last Chance for Special Free Treatment" [1].
- Withheld Treatments and Active Prevention of Care: When penicillin became the standard treatment for syphilis by 1947, researchers actively withheld it from participants [1]. During World War II, when 256 subjects were diagnosed with syphilis at military induction centers and ordered to obtain treatment, PHS researchers intervened to prevent them from receiving care [1]. Similarly, researchers prevented participants from accessing other venereal disease treatment campaigns that came to Macon County [1].
- Use of Placebos and Ineffective Treatments: Participants were administered disguised placebos, ineffective methods, and diagnostic procedures that were misrepresented as treatments [1]. Early in the study, some subjects received mildly effective but highly toxic compounds like salvarsan ("606"), mercurial ointments, and bismuth, but these treatments were discontinued when study funding was lost [1] [4].
Table 2: Chronology of Key Events in the Tuskegee Syphilis Study
| Year | Event | Ethical Significance |
|---|---|---|
| 1932 | Study begins as 6-8 month observational study [1] | Initial deception about study purpose and duration |
| 1936 | First major report published [1] | Study continues despite availability of some treatments |
| 1947 | Penicillin becomes standard syphilis treatment [1] | Critical decision to withhold effective treatment |
| 1969 | PHS committee reviews study; votes to continue [1] | Institutional failure to terminate ethically indefensible study |
| 1972 | Peter Buxtun leaks story to press; study ends [1] [4] | External whistleblower forces termination after 40 years |
Diagram 1: Tuskegee Ethical Failure Sequence
The Researcher's Toolkit: Deceptive Practices and Their Functions
Table 3: Research "Reagents" and Methodological Components in the Tuskegee Study
| Research Component | Function in Study | Ethical Concern |
|---|---|---|
| "Bad Blood" Diagnosis | Colloquial term used to obscure true nature of syphilis from participants [1] | Deliberate deception preventing informed consent |
| Lumbar Punctures | Diagnostic spinal taps presented as "special free treatment" [1] | Therapeutic misconception; painful procedure with no clinical benefit |
| Placebos (Aspirin, Supplements) | Maintain participant engagement and compliance without providing real treatment [4] | Withholding of effective treatment despite availability |
| Free Burial Insurance | Incentive to ensure families permitted autopsies [1] | Exploitation of economic vulnerability |
| Eunice Rivers, Nurse | Trusted African American intermediary to maintain participant compliance [4] | Exploitation of community trust and racial solidarity |
The Path to Reform: National Research Act and Belmont Report
Public Revelation and Political Response
The Tuskegee Syphilis Study was terminated in 1972 following a leak to the press by Peter Buxtun, a former PHS social worker who had repeatedly raised ethical concerns internally before contacting journalists [1] [4]. On July 25, 1972, The Washington Star broke the story, followed by coverage in The New York Times, creating public outrage that forced the government to act [4]. In response, an Ad Hoc Advisory Panel was convened by the Assistant Secretary for Health and Scientific Affairs, which recommended terminating the study immediately [5]. This congressional hearing, directed by Senator Edward Kennedy, exposed the systemic ethical failures and created the political momentum for legislative action [2].
The National Research Act of 1974
The National Research Act, signed into law by President Richard Nixon on July 12, 1974, was the direct legislative response to the Tuskegee scandal [2]. The Act contained two pivotal provisions that would permanently reshape the U.S. research landscape:
- Establishment of the National Commission: The Act created the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research, charging it with developing guidelines for human subject research and overseeing the use of human experimentation [2].
- Institutional Review Boards (IRBs): The Act formalized a regulated IRB process through local institutional review boards to provide independent review of research protocols [2]. This ensured that an independent panel would evaluate studies for ethical acceptability before they could begin.
The Belmont Report: Ethical Principles and Guidelines
In 1979, the National Commission published the Belmont Report, which identified three fundamental ethical principles that should guide all human subjects research [3]:
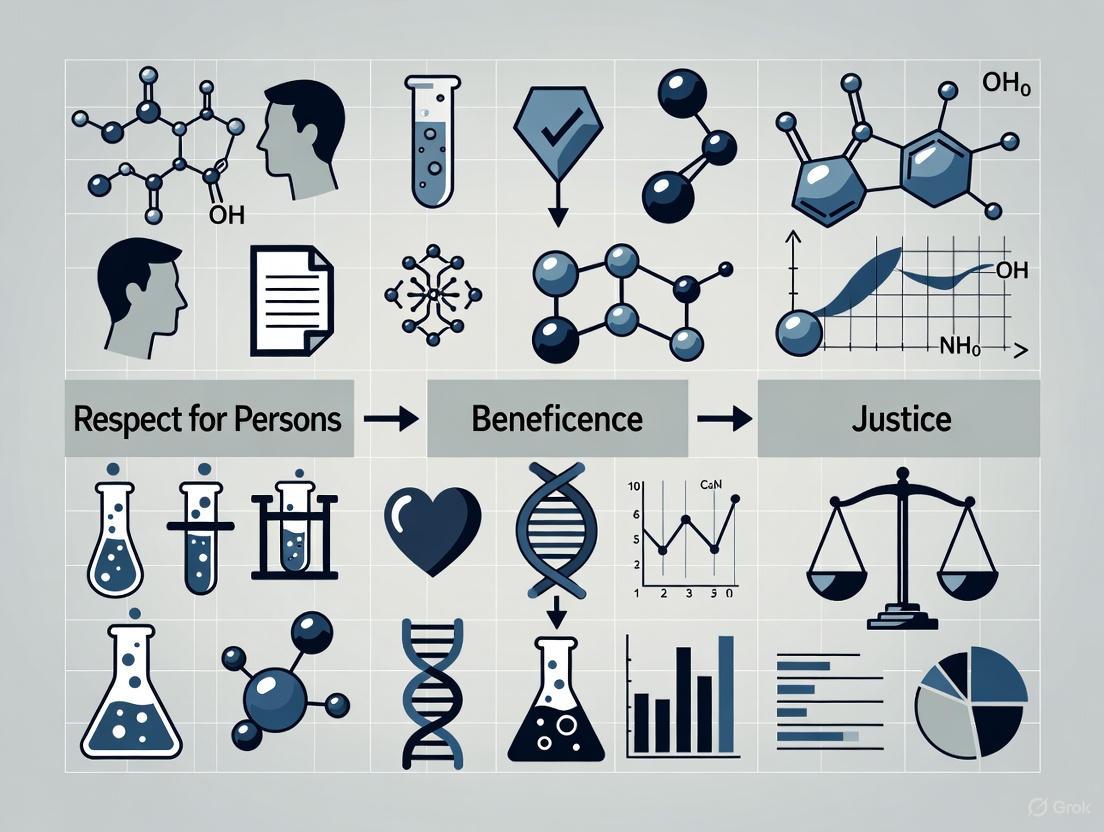
Diagram 2: Belmont Report Ethical Framework
- Respect for Persons: This principle acknowledges the dignity and autonomy of individuals and requires that subjects with diminished autonomy (such as children or those with cognitive impairments) are entitled to additional protections [3]. In practice, this principle is implemented through the process of informed consent, where participants must be given all relevant information about a study and voluntarily decide whether to enroll [6] [3].
- Beneficence: This principle describes an obligation to maximize possible benefits for society and science while minimizing possible harms to individual subjects [3]. The risk-benefit ratio must be favorable, and researchers have a continuous obligation to monitor participant welfare throughout the study [6].
- Justice: The principle of justice requires the fair distribution of both the burdens and benefits of research [3]. It addresses concerns about vulnerable populations being systematically selected for risky research while more privileged populations reap the benefits, which was starkly evident in the Tuskegee study where impoverished African American men bore all the risks with no prospect of benefit [1] [3].
Analysis: Connecting Tuskegee to Modern Ethical Protections
Direct Regulatory Responses to Tuskegee Failures
The ethical failures of the Tuskegee Study directly informed specific regulatory requirements in contemporary human subjects protections:
- Informed Consent: Tuskegee participants were deliberately deceived about their diagnosis and the study's purpose [1]. The Belmont Report's emphasis on respect for persons mandates meaningful informed consent where participants understand the research purpose, procedures, risks, and benefits [3]. Modern regulations require documentation of consent and ongoing communication of new information that might affect participation decisions [6].
- Vulnerable Populations: The exploitation of impoverished, poorly educated African American men in Tuskegee highlighted the need for special protections for vulnerable populations [1]. Current regulations require additional safeguards when research involves participants with diminished autonomy or those who may be susceptible to coercion [3].
- Justice in Subject Selection: The principle of justice directly addresses the Tuskegee legacy by requiring that the selection of subjects be scrutinized to avoid systematically recruiting vulnerable populations for risky research [3]. Researchers must ensure that the populations bearing the risks of research are positioned to enjoy its benefits [6].
Implementation in Modern Research Practice
For contemporary researchers and drug development professionals, the Tuskegee-Belmont narrative translates into concrete practices:
- Institutional Review Boards (IRBs): The National Research Act's requirement for independent review means all research protocols must undergo scrutiny by an IRB to ensure ethical acceptability before initiation and during conduct [2] [6]. IRBs evaluate whether risks are minimized and reasonable in relation to anticipated benefits, selection of subjects is equitable, and informed consent will be properly obtained [6].
- Ongoing Ethical Vigilance: The Belmont Principles recognize that ethical conflicts can emerge during research [3]. For instance, respect for persons (a child's dissent) might conflict with beneficence (potential for direct therapeutic benefit), requiring careful case-by-case analysis [3]. Researchers must maintain ethical awareness throughout the research lifecycle.
- Transparency and Accountability: Modern research requires transparency in methods, assumptions, and analyses, allowing for public scrutiny and maintaining trust [7]. Researchers must keep good records and be prepared to give an account of their decisions and actions [7].
The trajectory from the Tuskegee Syphilis Study to the National Research Act and the Belmont Report represents a profound transformation in research ethics. What began as a 40-year violation of human dignity ended by establishing a principled framework that continues to guide researchers today. The three principles of the Belmont Report—respect for persons, beneficence, and justice—provide a robust structure for navigating complex ethical dilemmas in human subjects research. For today's researchers, scientists, and drug development professionals, this history serves as both a cautionary tale and a compelling mandate: scientific advancement must never come at the expense of human rights and dignity. The ethical safeguards born from this dark chapter remain essential for maintaining public trust and ensuring that research continues to be a force for benefit rather than exploitation.
The National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research was created through the National Research Act of 1974, a legislative response to profound ethical failures in research, most notably the Tuskegee Syphilis Study [8] [9]. This study, which ran from 1932 to 1972, intentionally withheld treatment from African American men with syphilis without their informed consent. The public revelation of this study in 1972 sparked national outrage and created the necessary political momentum for formalizing ethical protections for research participants [9] [8]. The Commission's primary congressional charge was to identify the fundamental ethical principles that should govern research involving human subjects and to translate these principles into actionable guidelines for researchers and institutions [9] [10]. The result of this four-year effort was the Belmont Report, published in 1979, which continues to serve as the ethical foundation for human subjects research regulations in the United States [3] [9] [8].
The National Commission's Composition and Work
Commission Formation and Membership
The National Commission was composed of eleven members who represented a diverse range of expertise, including medicine, law, ethics, and the social sciences [9]. The membership included eight men and three women, with Dorothy I. Height noted as the only African American commissioner [9]. This diversity was crucial for tackling the complex ethical issues at the intersection of research, medicine, and societal values. The Commission met regularly over nearly four years, with an intensive four-day discussion period in February 1976 at the Belmont Conference Center in Maryland, from which the final report takes its name [9] [10].
Core Mandate and Key Questions
The Commission's specific mandate, as outlined in the Belmont Report itself, directed it to consider several boundary areas critical to research ethics [9] [10]:
- The distinctions between biomedical research and routine medical practice
- The role of risk-benefit assessment in determining the appropriateness of research
- Appropriate guidelines for selecting human subjects
- The nature and definition of informed consent across various research settings
Table: Key Questions in the National Commission's Mandate
| Mandate Area | Core Ethical Question |
|---|---|
| Practice vs. Research | When does an activity stop being care for an individual and start being generalizable knowledge production? |
| Risk-Benefit Assessment | What systematic approach ensures that the potential benefits of research justify the risks to participants? |
| Subject Selection | How do we select subjects fairly to avoid exploiting vulnerable populations? |
| Informed Consent | What information must be conveyed and comprehended for consent to be truly informed and voluntary? |
The Ethical Framework of the Belmont Report
The Belmont Report established three fundamental ethical principles that form an "analytical framework" for resolving ethical problems in research involving human subjects [8].
Respect for Persons
This principle incorporates two ethical convictions. First, that individuals should be treated as autonomous agents, capable of self-determination [11]. Second, that persons with diminished autonomy (e.g., children, individuals with cognitive impairments, prisoners) are entitled to special protections [9] [11]. The practical application of this principle is realized through the process of informed consent, which requires that prospective subjects are provided with all relevant information about the study in a comprehensible manner and that their participation is voluntary, free from coercion or undue influence [3] [9] [11].
Beneficence
This principle extends beyond the simple injunction to "do no harm" to an affirmative obligation to maximize potential benefits and minimize potential harms [8] [11]. The Belmont Report frames beneficence as an obligation, not just an aspiration. Researchers must systematically assess the risks and benefits of their proposed research, not only at the outset but throughout the conduct of the study [9] [11]. This requires a rigorous analysis to ensure that the knowledge gained is proportionate to the risks assumed by the participants.
Justice
The principle of justice addresses the fair distribution of the burdens and benefits of research [8] [11]. It demands that the selection of research subjects be scrutinized to avoid systematically recruiting participants simply because of their easy availability, compromised position, or socioeconomic status [11]. The report explicitly references the Tuskegee Syphilis Study as a gross injustice, where disadvantaged, rural African American men bore the burdens of research while the benefits of medical knowledge were available to others [9]. This principle ensures that no single group is unfairly burdened or excluded from the benefits of research.
Operationalizing the Ethical Principles
The Belmont Report does not merely state principles; it provides a framework for their application in the conduct of research. The following table outlines how each principle translates into concrete research requirements.
Table: Application of Belmont Principles in Research Practice
| Ethical Principle | Application Area | Key Requirements for Researchers |
|---|---|---|
| Respect for Persons | Informed Consent | • Provide all relevant information [11]• Ensure participant comprehension [9]• Guarantee voluntariness (free from coercion) [9] [11] |
| Beneficence | Risk-Benefit Assessment | • Systematically analyze risks and benefits [11]• Maximize possible benefits [8]• Minimize possible risks [8] [11] |
| Justice | Selection of Subjects | • Ensure fair selection procedures [11]• Avoid exploiting vulnerable populations [9]• Distribute burdens and benefits equitably [8] |
The Informed Consent Process
The Belmont Report details that informed consent is not a single event but a process, comprising three key elements [9]:
- Information: Researchers must disclose all information that a reasonable person would want to know to make an informed decision. This includes the research procedure, purposes, risks, benefits, and alternatives to participation [11].
- Comprehension: The information must be presented in a manner and language that is understandable to the subject. The report acknowledges that some populations require special provisions to ensure understanding [9].
- Voluntariness: The agreement to participate must be freely given, without the presence of coercion or undue influence. This is particularly relevant when researchers hold authority over potential subjects, such as in prisoner or student populations [9].
Systematic Risk-Benefit Assessment
The obligation of beneficence requires a thorough and systematic assessment of risks and benefits. This assessment must be explicit and detailed, considering the probability and magnitude of harm, as well as the potential for new knowledge and direct therapeutic benefit to the subject [11]. The Belmont Report encourages IRBs to be precise and factual in their communications with investigators regarding this assessment, moving beyond arbitrary judgments to a more rigorous analytical process [11].
Legacy and Regulatory Impact
The most direct regulatory outcome of the Belmont Report was the development and implementation of the Federal Policy for the Protection of Human Subjects, known as the "Common Rule" (45 CFR Part 46) [9]. First adopted in 1991 by 15 federal departments and agencies, the Common Rule codifies the Belmont principles into enforceable regulations for all federally funded research [9]. The report also led to the strengthening of Institutional Review Boards (IRBs), which are tasked with reviewing research protocols to ensure they conform to these ethical standards [9] [11]. The Belmont Report's framework provides IRB members with a method to determine if the risks of a study are justified by the potential benefits in a systematic and non-arbitrary way [11]. The report's enduring legacy is that it established a compass for ethical decision-making rather than a simple checklist, allowing its principles to adapt to new and complex ethical challenges in evolving research fields [8].
The Researcher's Toolkit: Essential Components for Ethical Research
For researchers, scientists, and drug development professionals, implementing the Belmont principles requires specific tools and processes. The following table details key components of a modern ethical research program.
Table: Essential Components for Ethical Research Governance
| Component | Function & Purpose | Ethical Principle Served |
|---|---|---|
| Institutional Review Board (IRB) | An independent committee that reviews, approves, and monitors research involving human subjects to protect their rights and welfare. | Respect for Persons, Beneficence, Justice |
| Protocol & Informed Consent Template | Standardized documents ensuring all necessary information is presented to potential subjects in a consistent, comprehensive, and understandable format. | Respect for Persons |
| Risk-Benefit Assessment Framework | A systematic methodology for identifying, quantifying, and justifying the potential harms and benefits of a research study. | Beneficence |
| Vulnerable Population Safeguards | Additional protective procedures for groups with diminished autonomy (e.g., children, prisoners, cognitively impaired persons). | Respect for Persons, Justice |
| Equitable Recruitment Plan | A pre-defined strategy for subject recruitment that ensures fair selection and prevents the systematic targeting of vulnerable groups. | Justice |
| Data Safety Monitoring Board (DSMB) | An independent group of experts that monitors patient safety and treatment efficacy data while a clinical trial is ongoing. | Beneficence |
| Federalwide Assurance (FWA) | A formal commitment by an institution to the U.S. government that it will comply with federal regulations for the protection of human subjects. | All Three Principles |
The Belmont Report, formally issued in 1979, established a foundational ethical framework for human subjects research in the United States [12]. It was developed by the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research in response to historical abuses, such as the Tuskegee Syphilis Study, and to strengthen human research protections [3] [12]. The report articulates three core ethical principles: Respect for Persons, Beneficence, and Justice [12] [8]. This paper provides an in-depth examination of the principle of Respect for Persons, which embodies the ethical conviction that individuals are autonomous agents and that those with diminished autonomy are entitled to protection [3] [11]. This principle is the bedrock of the informed consent process and the special protections afforded to vulnerable populations in research.
Conceptual Foundations of Respect for Persons
The principle of Respect for Persons incorporates two distinct but related ethical convictions [11]. First, it affirms that individuals should be treated as autonomous agents [13]. An autonomous person is capable of self-determination; they can deliberate on personal goals and act under the direction of that deliberation [11]. The second conviction is that persons with diminished autonomy are entitled to additional protections [13]. The obligation to respect autonomy requires that researchers acknowledge an individual's right to hold views, make choices, and take actions based on their personal values and beliefs [11].
The application of this principle leads to two separate moral requirements in the research context:
- The requirement to acknowledge autonomy and protect the autonomous decisions of individuals.
- The requirement to protect individuals with diminished or impaired autonomy [11].
The extent of protection required is not uniform and should be contingent upon the risk of harm and the likelihood of benefit. The judgment that an individual lacks autonomy should be periodically re-evaluated and is often situation-dependent [11].
Operationalizing Respect for Persons: The Informed Consent Process
The primary practical application of the Respect for Persons principle is the informed consent process [14]. This process is designed to ensure that subjects' participation is voluntary and that they have adequate information to make an informed decision.
Key Elements of Informed Consent
The Belmont Report specifies that informed consent must encompass three critical components: information, comprehension, and voluntariness [12].
- Information: Researchers must disclose all relevant information about the study that a reasonable person would need to make a decision [3]. The Belmont Report recommends including:
- The research procedure and its purposes.
- Any reasonably foreseeable risks and anticipated benefits.
- Alternative procedures available (particularly when the research involves therapy).
- A statement offering the subject the opportunity to ask questions and to withdraw from the research at any time without penalty [12] [11].
- Comprehension: The manner and context in which information is conveyed must ensure that the prospective subject adequately understands it [12]. This involves presenting information in a language and format that is comprehensible to the subject, avoiding technical jargon, and ensuring that the subject has the capacity to make a decision. For some subjects, this may require additional measures, such as using plain-language forms, interpreters, or staged consent processes [15].
- Voluntariness: Consent must be given voluntarily, free from coercion or undue influence [13]. Coercion occurs when an overt threat of harm is presented to secure compliance. Undue influence, often more subtle, involves offering excessive or inappropriate rewards to overcome a person's better judgment [12]. The voluntariness of a decision can be compromised by situational factors, such as power dynamics in a doctor-patient relationship or institutional hierarchies [15].
Assessment of Vulnerabilities in the Consent Process
The following diagram illustrates a systematic approach to assessing vulnerabilities that can impair the consent process, guiding researchers toward appropriate safeguards.
Protections for Persons with Diminished Autonomy
A critical function of the Respect for Persons principle is to mandate additional protections for individuals with diminished autonomy [13]. The Belmont Report recognizes that not all individuals are capable of self-determination and that the extent of this capacity can vary [11].
Defining and Identifying Vulnerability
Vulnerability in research is a condition, either intrinsic or situational, that puts some individuals at greater risk of being used in ethically inappropriate ways [15]. The Common Rule explicitly identifies several vulnerable categories requiring special protections: pregnant women, human fetuses, neonates, prisoners, and children [16]. However, vulnerability extends beyond these categories to include any individual with a reduced ability to protect their own interests [15]. This can include individuals with cognitive or communicative impairments, those who are economically or educationally disadvantaged, and employees or students [16].
Two primary approaches to understanding vulnerability are used:
- The Categorical Approach: This method classifies certain groups as vulnerable. While practical for regulation, it can be limiting as it does not account for individuals with multiple vulnerabilities or variations in the degree of vulnerability within a group [15].
- The Contextual Approach: This more nuanced method identifies situations in which individuals might be considered vulnerable. It recognizes that vulnerability can be fluid and dependent on specific circumstances [15]. For example, an otherwise autonomous person may become vulnerable in an emergency medical situation.
Key Vulnerability Categories and Corresponding Safeguards
Table 1: Vulnerability Categories and Safeguards for Persons with Diminished Autonomy
| Vulnerability Category | Description and Examples | Recommended Safeguards and Protections |
|---|---|---|
| Cognitive/Communicative [15] | Difficulty comprehending information or making decisions. Examples: children, adults with cognitive impairment, persons speaking a different language than the researcher, individuals in acute distress (e.g., pain). | Use of plain-language consent forms; objective assessment of capacity; use of surrogates or legally authorized representatives; translated materials and interpreters; staged consent processes; delaying enrollment until transient impairment resolves [15]. |
| Institutional [15] | Persons under formal authority of others who may have different priorities. Examples: prisoners, military personnel, students. | Insulated consent procedures (e.g., having neutral parties approach potential subjects); careful scrutiny of participant selection; ensuring that refusal to participate does not affect institutional standing [15]. |
| Deferential [15] | Persons under informal authority based on power, knowledge, or social inequalities. Examples: doctor-patient relationships, gender or class-based deference. | Scrutiny of the consent process to ensure decisions are free from undue influence; ensuring the subject knows participation is voluntary and refusal will not affect care [15]. |
| Societal/Economic [17] [16] | Economically or educationally disadvantaged persons who may be susceptible to undue influence due to perceived financial or other rewards. | Ensuring that monetary payments are not coercive but function as compensation for time and burden; equitable selection of subjects so that no class bears disproportionate research burdens [17]. |
Special Considerations: The Case of Children
Research involving children exemplifies the potential for the Belmont principles to conflict and the need for careful balancing. Children, due to their developmental immaturity and legal status, cannot provide full informed consent [3]. Instead, a parent or guardian provides permission, and the child, when capable, provides assent [3]. Respect for Persons requires honoring a child's dissent when they do not want to enroll [3]. However, there are circumstances where Beneficence (the obligation to secure well-being) and Justice (fair distribution of benefits and burdens) may override a child's dissent. For instance, in greater-than-minimal risk research with potential for direct benefit to the child, an IRB may allow a parent's permission to override the child's wishes to secure that benefit [3].
The Researcher's Toolkit: Essential Frameworks for Ethical Practice
For researchers, scientists, and drug development professionals, applying the principle of Respect for Persons requires practical tools and frameworks.
Table 2: Essential Frameworks and Applications for Upholding Respect for Persons
| Tool/Framework | Primary Function | Application in Research Practice |
|---|---|---|
| Informed Consent Document | To document the process of providing information and obtaining voluntary, comprehending agreement. | Serves as a checklist and record that key study information (risks, benefits, alternatives, etc.) was disclosed and understood by the subject [12]. |
| Capacity Assessment Protocol | To objectively evaluate a potential subject's ability to understand information and make a voluntary decision. | Used when a subject's decision-making capacity is in question; may involve simple questioning or standardized tools to assess understanding of the study [15]. |
| Vulnerability Screening Checklist | To systematically identify potential vulnerabilities during study design and participant recruitment. | Helps researchers proactively identify subjects who may need additional safeguards due to cognitive, institutional, deferential, or economic vulnerabilities [15]. |
| IRB Review Process | To provide independent, ethical oversight of research protocols to ensure subject protections. | The IRB scrutinizes the informed consent process, participant selection, and study design to ensure Respect for Persons is upheld, especially for vulnerable groups [3] [11]. |
| Waiver of Consent Criteria | To define the rare circumstances in which informed consent may be altered or waived. | Guides researchers and IRBs on when consent may not be required, such as for minimal risk research where seeking consent is impractical, provided privacy safeguards are in place [13]. |
The principle of Respect for Persons is a cornerstone of ethical human subjects research. It imposes a dual mandate: to honor the autonomous choices of self-determining individuals and to provide robust protection for those with diminished autonomy. For researchers and drug development professionals, this translates into a rigorous commitment to a meaningful informed consent process and a proactive duty to identify and safeguard vulnerable populations. As research contexts and capabilities continue to evolve, the foundational principles of the Belmont Report, particularly Respect for Persons, remain an essential compass for navigating ethical challenges and maintaining public trust in the research enterprise [14].
The principle of beneficence forms a cornerstone of ethical research involving human subjects, establishing a fundamental obligation for researchers to maximize potential benefits while minimizing possible harms. This principle, first formally articulated in the Belmont Report of 1979, provides the ethical foundation for modern research regulations and practices [3]. For researchers, scientists, and drug development professionals, understanding and implementing beneficence extends beyond regulatory compliance—it represents a core professional responsibility to protect research participants while advancing scientific knowledge. The Belmont Report defines beneficence as an obligation to protect subjects from harm by maximizing possible benefits and minimizing possible harms, creating a dual mandate that requires careful balancing throughout the research lifecycle [3]. This technical guide explores the practical application of this principle, providing methodologies, analytical frameworks, and implementation tools to systematically integrate beneficence into research design and execution.
Theoretical Foundations: Beneficence Within the Belmont Framework
The Belmont Report established three fundamental principles guiding human subjects research: respect for persons, beneficence, and justice [3] [18]. These principles emerged in response to historical ethical failures and provide the framework for contemporary research ethics. Beneficence specifically addresses the researcher's obligation to ensure participant well-being through a systematic process of risk-benefit assessment [3]. This principle transcends the simple medical maxim "do no harm" to incorporate active efforts to maximize potential benefits [19]. In practice, beneficence requires that researchers thoroughly assess and justify risks, ensure risks are minimized, and confirm that the potential benefits outweigh these risks [3]. The application of beneficence often requires balancing against other ethical principles, particularly when working with vulnerable populations or in contexts where immediate benefits to participants may be limited [3].
The Nuremberg Code and Declaration of Helsinki provide important historical context for the development of beneficence as a research principle [18]. These foundational documents emphasize that research must yield fruitful results for the good of society, unattainable by other methods, and that risks should not exceed humanitarian importance [18]. The Belmont Report built upon these foundations to establish the comprehensive risk-benefit analysis framework that guides modern research ethics.
Methodological Framework: Implementing Beneficence in Research Design
Systematic Risk-Benefit Assessment Protocol
Implementing beneficence requires a structured methodology for identifying, quantifying, and balancing potential benefits and harms. The following systematic protocol ensures comprehensive assessment:
Risk Identification and Categorization: Conduct a thorough review of all potential physical, psychological, social, and economic harms. Categorize risks as minimal, minor, moderate, or severe based on probability, magnitude, and duration. This process should involve literature review, expert consultation, and preliminary studies where appropriate [20] [3].
Benefit Maximization Strategy: Identify all potential direct benefits to participants and collateral benefits to society. Develop explicit strategies to enhance these benefits through optimal study design, participant selection, and ancillary care provisions. The principle of beneficence requires not merely avoiding harm but actively promoting well-being [19].
Risk Minimization Engineering: Implement methodological safeguards to reduce the probability and severity of identified risks. This includes appropriate exclusion criteria, data monitoring procedures, safety endpoints, and stopping rules. The Belmont Report emphasizes that researchers must take all necessary steps to prevent harm, including physical, emotional, or psychological harm [20].
Equitable Benefit Distribution: Ensure that the populations bearing research risks stand to benefit from the knowledge gained, addressing the intersection of beneficence and justice [3]. This requires careful consideration of participant selection and post-trial access to interventions.
Quantitative Methodologies for Within-Subjects Benefit-Risk Analysis
Within-subjects designs provide powerful methodological approaches for measuring intervention effects while minimizing participant risks. The following quantitative methodologies enable precise benefit-risk assessment:
Paired Difference Analysis: When each participant provides both experimental and control observations (through baseline measurements or crossover designs), compute within-individual differences to quantify intervention effects while controlling for between-subject variability [21]. The appropriate numerical summary involves calculating the mean of these differences across all participants, not by subtracting summary statistics between groups [21].
Case-Profile Plot Methodology: For studies with multiple longitudinal measurements per participant, employ case-profile plots to visualize individual trajectories of benefit and harm indicators [21]. This graphical approach reveals patterns that might be obscured in group-level analyses and helps identify participants who may be experiencing disproportionate harms or benefits.
Table 1: Quantitative Analysis of IgE Reduction Intervention [21]
| Measurement Point | Mean (μg/L) | Standard Deviation (μg/L) | Sample Size |
|---|---|---|---|
| Before Intervention | 1690.5 | 1615.53 | 11 |
| After Intervention | 1387.4 | 1354.28 | 11 |
| Reduction | 303.2 | 325.28 | 11 |
The data in Table 1 demonstrates how within-subjects analysis can quantify benefits while using participants as their own controls, potentially reducing the sample size needed to detect significant effects and thereby minimizing overall research risks [21].
Multi-Timepoint Benefit-Risk Tracking: For studies with more than two measurement points, calculate changes from baseline for each subsequent assessment to track the evolution of benefits and risks over time [21]. This approach is particularly valuable in dose-escalation studies or when investigating delayed treatment effects.
Table 2: Pain Threshold Changes Following Therapeutic Intervention [21]
| Measurement Time | Mean (kPa) | Std Dev (kPa) | Sample Size | Mean Increase from Baseline | SD Increase |
|---|---|---|---|---|---|
| Pre: 5 minutes | 446.5 | 175.18 | 16 | - | - |
| Post: 5 minutes | 479.6 | 199.61 | 16 | 33.1 | 73.93 |
| Post: 15-20 minutes | 506.9 | 214.36 | 16 | 60.4 | 102.72 |
Table 2 illustrates how benefit accumulation can be tracked over time, providing crucial data for evaluating whether increasing benefits justify continuing exposure to research risks [21].
Analytical Tools: Visualization and Decision-Support Frameworks
Beneficence Implementation Workflow
Risk-Benefit Analysis Matrix
Research Reagent Solutions for Ethical Implementation
Table 3: Essential Research Materials for Ethical Implementation
| Item/Category | Function in Ethical Research | Implementation Example |
|---|---|---|
| Validated Assessment Tools | Precisely measure benefits and harms using reliable instruments | Standardized quality of life measures, psychological distress scales, and physiological monitoring devices |
| Data Monitoring Systems | Continuous safety surveillance during study conduct | Electronic data capture with automated adverse event alerts and scheduled interim analyses |
| Confidentiality Protection Tools | Safeguard participant privacy and data security | Encryption software, secure storage solutions, and data anonymization protocols [20] |
| Informed Consent Documentation | Ensure comprehensive participant understanding | Multi-format consent materials (written, visual, interactive) with comprehension assessment [3] [22] |
| Unblinding Procedures | Emergency access to treatment assignment when clinically indicated | Secure, 24/7 accessible unblinding system with documentation protocols |
Advanced Applications: Beneficence in Complex Research Scenarios
Benefit Enhancement in Novel Therapeutic Contexts
Recent ethical scholarship has proposed expanding the beneficence framework beyond harm reduction to incorporate benefit enhancement strategies, particularly in novel therapeutic contexts such as psychedelic-assisted psychotherapy [19]. This approach acknowledges that some interventions may offer substantial benefits when used in supportive settings, and ethical practice requires not merely minimizing potential harms but actively facilitating positive outcomes [19]. In psychedelic research, this involves creating optimal set and setting, providing psychological support, and integrating experiences to maximize therapeutic benefits [19]. This expanded beneficence model maintains harm reduction as essential while adding positive obligation to enhance potential benefits through methodological optimization.
Ethical Conflict Resolution Framework
The principle of beneficence may sometimes conflict with other ethical principles, particularly respect for persons, requiring a structured approach to resolution [3]. In pediatric research, for example, a child's dissent (respect for persons) may conflict with potential therapeutic benefit (beneficence) [3]. The ethical framework suggests that:
- When research offers direct therapeutic benefit and exceeds minimal risk, beneficence may sometimes outweigh a child's dissent, particularly when the benefit is significant [3].
- When research offers no direct benefit but generates vital knowledge for others with the same condition (justice), additional safeguards are required, such as two-parent permission [3].
- In all cases, researchers should make every effort to resolve conflicts through compromise and respect for participant perspectives [3].
The principle of beneficence requires ongoing vigilance throughout the entire research process, from initial design to post-study follow-up. By implementing the systematic methodologies, analytical frameworks, and practical tools outlined in this technical guide, researchers can fulfill their ethical obligation to maximize potential benefits while minimizing possible harms. The frameworks presented enable quantitative assessment of risk-benefit ratios, structured approaches to ethical challenges, and practical strategies for enhancing research outcomes. As scientific methodologies advance and new research contexts emerge, the foundational principle of beneficence remains essential for maintaining public trust and ensuring that research continues to serve humanitarian ends while protecting those who make knowledge advancement possible.
The principle of Justice constitutes one of three core ethical tenets outlined in the 1979 Belmont Report, a foundational document for protecting human subjects in research. This principle specifically addresses the timeless and weighty question of "Who ought to receive the benefits of research and bear its burdens?" [23]. Justice requires a fair distribution of both research advantages and disadvantages across society, ensuring that no single group is systematically overburdened or excluded from benefits [24] [25]. This ethical mandate serves as a crucial safeguard against the exploitation of vulnerable populations and promotes equity in the selection of research subjects and the allocation of research-derived benefits.
The historical significance of this principle is rooted in egregious ethical violations witnessed in studies like the Tuskegee Syphilis Experiment, where the burdens of research were imposed exclusively upon African American males while benefits were withheld, even after effective treatment became available [23]. Such historical precedents established a persistent distrust of research institutions among minority communities and underscored the critical necessity for distributive justice in research ethics [23]. In contemporary contexts, from COVID-19 clinical trials to behavioral intervention studies, the operationalization of justice remains equally vital for ethical research conduct [26] [23].
Theoretical Framework of Distributive Justice
Conceptual Foundations
The principle of justice encompasses fair treatment of human subjects across multiple domains, including equitable distribution of research risks and benefits, representative subject pools, and appropriate recruitment practices [23]. This distributive dimension focuses on the formulations of justice, which include:
- To each person an equal share
- To each person according to individual need
- To each person according to individual effort
- To each person according to societal contribution
- To each person according to merit [23]
These formulations provide a framework for evaluating whether the selection of research subjects is systematically biased toward groups for reasons of manipulability, vulnerability, or convenience rather than for reasons directly related to the research problem [23].
Core Components of Justice in Research
Table 1: Key Aspects of the Principle of Justice
| Component | Ethical Requirement | Historical Violation Example |
|---|---|---|
| Burden Distribution | Research burdens should not fall disproportionately on any particular group | Tuskegee syphilis study imposed burdens exclusively on African American men [23] |
| Benefit Distribution | Benefits should be accessible to those who bear burdens, including future access to interventions | Participants in Tuskegee study were denied effective treatment when it became available [23] |
| Subject Selection | Selection should be based on scientific objectives, not convenience or manipulability | Vulnerable populations selected due to limited autonomy rather than scientific relevance [23] |
| Recruitment Practices | Procedures must be fair and avoid exploitation of vulnerable circumstances | Recruitment exploited participants' limited access to healthcare and financial constraints [23] |
Quantitative Assessment of Equity in Research
Metrics for Evaluating Distributive Justice
The assessment of justice in research requires both qualitative evaluation and quantitative measurement. Key metrics for evaluating equity include participant demographic data compared to disease prevalence rates, economic analyses of benefit distribution, and comparative burden assessments across population subgroups.
Table 2: Quantitative Measures for Assessing Research Equity
| Metric Category | Specific Measures | Application Example |
|---|---|---|
| Participant Representation | Disparity ratios between disease burden and trial participation; Percentage of underrepresented groups in trials | African American and Hispanic/Latinx patients substantially underrepresented in clinical trials despite COVID-19 disproportionately affecting these groups [26] |
| Geographic Distribution | Number of trial sites in low/middle-income countries (LMICs) versus high-income countries; Applicability of research findings across regions | WHO Solidarity Trial included only a few sites in Africa, Latin America, and South/Southeast Asia, limiting local applicability of results [26] |
| Benefit Accessibility | Patent barriers; Pricing structures; Post-trial access provisions | Patent protections enabling high monopoly prices effectively block portions of global population from accessing developed products [26] |
| Burden Compensation | Analysis of compensation adequacy relative to participant time, risk, and inconvenience; Barrier mitigation effectiveness | Travel vouchers and extended hours to mitigate participation barriers for underserved communities [23] |
Data Visualization for Equity Assessment
Effective visualization of equity data enables researchers to identify disparities and monitor progress toward justice goals. The following diagrams illustrate essential workflows and relationships for implementing and evaluating justice in research.
Equity Implementation Workflow
Barriers and Mitigation Strategies
Experimental Protocols for Equitable Research
Protocol 1: Inclusive Participant Recruitment
Objective: Ensure participant enrollment reflects the demographic distribution of the disease population.
Methodology:
- Disease Burden Analysis: Conduct comprehensive review of epidemiological data to identify populations disproportionately affected by the target condition [26].
- Recruitment Strategy Design: Implement multi-faceted recruitment incorporating:
- Barrier Mitigation: Implement practical accommodations including:
- Monitoring and Adjustment: Continuously track enrollment demographics against predetermined targets and modify strategies as needed to address disparities [26].
Validation Metrics:
- Percentage of enrolled participants from underrepresented groups relative to disease prevalence
- Recruitment yield by strategy and demographic group
- Participant retention rates across demographic segments
Protocol 2: Equitable Global Trial Design
Objective: Ensure clinical trials generate globally applicable knowledge while avoiding exploitation of resource-limited settings.
Methodology:
- Site Selection: Identify trial locations based on disease relevance rather solely on regulatory convenience or participant manipulability [26].
- Local Capacity Building: Incorporate plans for strengthening local research infrastructure and expertise.
- Contextual Adaptation: Modify intervention protocols to account for local healthcare infrastructures, genetic differences, and comorbidity prevalence [26].
- Access Planning: Develop pre-trial strategies for ensuring successful interventions become accessible to host communities post-trial [26].
Validation Metrics:
- Number of trial sites in LMICs relative to global disease burden
- Percentage of interventions developed through research that remain accessible to host communities
- Measurement of local research capacity enhancement
Table 3: Research Reagent Solutions for Justice-Oriented Research
| Tool Category | Specific Resources | Function in Promoting Justice |
|---|---|---|
| Recruitment Materials | Culturally adapted informed consent documents; Multilingual recruitment materials; Health literacy-appropriate educational resources | Ensures comprehension and authentic informed consent across diverse populations, including those with limited English proficiency or lower health literacy [26] |
| Community Engagement Resources | Community advisory board frameworks; Partnership development guidelines; Trust-building consultation protocols | Facilitates meaningful collaboration with affected communities, building trust and ensuring research relevance to community needs [23] |
| Barrier Mitigation Tools | Transportation voucher systems; Flexible scheduling software; Childcare coordination services; Mobile research units | Reduces practical barriers to participation for working individuals, those with limited transportation, and caregivers [23] |
| Data Equity Instruments | Demographic data collection standards; Disparity assessment metrics; Equity monitoring dashboards | Enables continuous monitoring of recruitment equity and identification of disparities requiring intervention [26] |
| Access Enforcement Mechanisms | Patent pooling agreements; Affordable pricing frameworks; Technology transfer protocols | Ensures beneficial research outcomes remain accessible to communities that participated in and contributed to the research [26] |
Case Study: Justice in COVID-19 Research
The COVID-19 pandemic provided a compelling test case for the application of justice principles in global health research. Several critical equity challenges emerged that highlight both violations of and adherence to justice principles.
The geographic distribution of clinical trials raised significant justice concerns. Early in the pandemic, statements suggesting that COVID-19 trials should be conducted in Africa to take advantage of weaker healthcare infrastructure were rightly condemned as reflecting a "colonial mentality" [26]. Conversely, the exclusion of LMICs from major trials like the WHO Solidarity Trial, which included only a few sites in Africa, Latin America, and South/Southeast Asia, created a different justice problem by limiting the applicability of research findings to these regions [26].
The recruitment disparities in COVID-19 trials within the United States further illustrated justice challenges. Despite African American and Hispanic/Latinx patients experiencing disproportionately high rates of COVID-19 infection and mortality, these groups remained substantially underrepresented among clinical trial participants [26]. This representation disparity threatens the generalizability of trial findings and violates the justice principle that those bearing disease burdens should have access to potential research benefits.
Promisingly, the pandemic also witnessed innovative approaches to promoting justice. Some education researchers chose to make evidence-based online educational curricula available to all schools in need rather than just partner research schools [23]. Additionally, significant efforts emerged to establish patent pooling mechanisms for COVID-19 products, making technologies more accessible to generic manufacturers who could produce them at affordable prices [26].
Implementation Framework for Research Institutions
Institutional Review Board Guidelines
IRBs play a critical role in enforcing the principle of justice through rigorous protocol review. Key considerations for IRBs include:
- Scrutiny of Subject Selection: IRBs must ensure research subjects are not selected systematically because of "their manipulability, susceptibility to coercion, or convenience for researchers" [23]. Instead, populations should be selected based on characteristics directly related to the research questions.
- Benefit-Risk Analysis: IRBs must evaluate whether the benefits of study participation are commensurate with the burdens participants will experience [23]. This is particularly crucial for studies involving populations with nuanced vulnerabilities.
- Accessibility Review: IRBs should assess whether researchers have implemented adequate accommodations to ensure all qualified individuals have realistic access to participation opportunities [23].
Researcher Accountability Measures
Individual researchers bear responsibility for implementing justice principles throughout the research lifecycle:
- Pre-Study Equity Assessment: Conduct formal analysis of how recruitment plans align with disease burden demographics before protocol finalization.
- Community Consultation: Engage representatives from affected communities during study design to identify potential barriers and concerns.
- Continuous Monitoring: Track recruitment and retention metrics by demographic group throughout study conduct.
- Post-Study Benefit Planning: Develop explicit plans for ensuring successful interventions become accessible to participant communities.
The principle of justice requires ongoing commitment throughout the research process—from initial study design through post-trial access. For researchers working with groups with nuanced vulnerability, this is especially important due to histories of exploitation and neglect [23]. The ethical imperative extends beyond mere compliance with IRB requirements to embrace a proactive stance toward identifying and eliminating structural barriers to equitable participation.
Successful implementation of justice principles requires researchers to approach their work with cultural sensitivity, structural competence, and collaborative ethos [23]. By introducing elements of flexibility and cooperation within research designs, investigators can ensure they are not withholding benefits from marginalized communities while simultaneously enhancing the scientific validity and generalizability of their findings. Through such comprehensive integration of justice considerations, the research community can fulfill the ethical mandate for equitable distribution of research benefits and burdens.
This technical guide examines the definitive pathway through which the Belmont Report's ethical principles became codified into the U.S. Federal Policy for the Protection of Human Subjects, known as the Common Rule (45 CFR 46). Framed within a broader thesis on the enduring role of the Belmont Report in human subjects research, this paper provides researchers, scientists, and drug development professionals with a detailed analysis of this regulatory evolution. We explore the historical catalysts for the Belmont Report, deconstruct its three core ethical principles—Respect for Persons, Beneficence, and Justice—and detail the mechanisms of their translation into enforceable regulations. The document includes structured data presentations, analytical frameworks for ethical review, and practical tools for navigating modern compliance requirements, underscoring the continued relevance of this foundational ethical framework in contemporary research.
The creation of the Belmont Report was a direct response to grave ethical failures in human subjects research, most notably the Tuskegee Syphilis Study (1932-1972), during which hundreds of African American men were denied treatment for syphilis without their knowledge or consent [27] [12]. Public disclosure of this study prompted the U.S. Congress to pass the National Research Act of 1974, which led to the establishment of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research [9] [12]. This Commission was charged with identifying the basic ethical principles that should underlie the conduct of research involving human subjects.
The Commission deliberated for four years, including a pivotal four-day meeting at the Belmont Conference Center in Maryland in February 1976, which gave the report its name [9] [28]. The final Belmont Report was published in 1979 [9]. Its primary achievement was the articulation of three comprehensive, unifying ethical principles to guide the conduct of human subjects research. While the Nuremberg Code and the Declaration of Helsinki provided earlier ethical foundations, the Belmont Report was distinctive in its aim to provide a more flexible framework applicable to a wide range of research disciplines [28] [12].
Table 1: Key Historical Milestones Leading to the Common Rule
| Year | Event | Significance |
|---|---|---|
| 1947 | Nuremberg Code | Established the absolute necessity of voluntary consent after the Nazi war crimes trials [28]. |
| 1964 | Declaration of Helsinki | Distinguished therapeutic from non-therapeutic research and emphasized beneficence [28]. |
| 1974 | National Research Act | Created the National Commission and mandated the establishment of IRBs [9] [12]. |
| 1978/1979 | Belmont Report Published | Articulated the three core principles of Respect for Persons, Beneficence, and Justice [11] [9]. |
| 1981 | HHS Issues 45 CFR 46 | Department of Health and Human Services codified regulations based on Belmont principles [12]. |
| 1991 | Federal Policy (Common Rule) Adopted | 14 other federal agencies adopted a uniform set of rules identical to HHS regulations [9] [12]. |
| 2019 | Revised Common Rule Effective | Updated the regulations to address modern research contexts while retaining Belmont principles [29]. |
The Foundational Ethical Principles of the Belmont Report
The moral framework of the Belmont Report is built upon three ethical principles, which are stated as "comprehensive general prescriptive judgements" relevant to all research involving human subjects [11] [12].
Respect for Persons
This principle incorporates two ethical convictions: first, that individuals should be treated as autonomous agents, and second, that persons with diminished autonomy are entitled to special protections [11]. An autonomous agent is an individual capable of deliberating about personal goals and acting under that deliberation. The application of this principle leads to the requirement that subjects must voluntarily participate in research and must be provided with adequate information to make an informed decision. This ensures the research participation is based on their own understanding and free will, free from coercion or undue influence [11] [9]. For individuals with diminished autonomy—such as children, prisoners, or those with cognitive disabilities—this principle requires seeking permission from authorized surrogates and affording additional safeguards to protect their well-being [12].
Beneficence
This principle extends beyond the simple injunction to "do no harm" to a positive obligation to maximize potential benefits and minimize potential risks [11] [28]. The principle of beneficence requires a systematic assessment of risks and benefits associated with the research. The Belmont Report stresses that "brutal or inhumane treatment of human subjects is never morally justified" and that risks must be reduced to those necessary to achieve the research objective [12]. Investigators are obligated to ensure the research design is sound, that they are qualified to perform the procedures, and that the gathered knowledge justifies any inherent risks to the subjects. The benefits and risks must be carefully balanced, and the resulting risk-benefit ratio must be favorable [11].
Justice
The principle of justice requires the fair distribution of the burdens and benefits of research [11]. It addresses the question of which persons or classes of persons ought to bear the risks of research, and which should reap its rewards. The Belmont Report explicitly condemns the selection of subjects based on convenience, compromised position, or societal biases (e.g., racial, sexual, economic) [11] [12]. This principle was formulated in direct response to historical abuses where economically disadvantaged, socially marginalized, or institutionalized individuals were systematically selected for high-risk research. Justice demands that research subjects not be drawn disproportionately from groups unlikely to benefit from the subsequent applications of the research [9] [12].
The Regulatory Pathway: From Ethical Principles to Enforceable Rule
The transformation of the Belmont Report's ethical principles into the binding regulations of the Common Rule was a deliberate, multi-stage process. The following diagram illustrates this regulatory pathway and the key applications that bridge ethical principles with regulatory requirements.
The diagram above shows how historical events led to legislative action, which commissioned the ethical framework of the Belmont Report. The report's three principles were then operationalized through specific applications, which directly informed the creation of the HHS regulations and, ultimately, the multi-agency Common Rule.
The Common Rule as the Operationalization of Belmont
The Common Rule is the informal term for the Federal Policy for the Protection of Human Subjects, which was unified across multiple federal departments and agencies in 1991 [12]. For the Department of Health and Human Services (HHS), the Common Rule is codified at 45 CFR Part 46, with Subpart A representing the core policy [12] [30]. The Rule legally mandates requirements for Institutional Review Boards (IRBs), informed consent, and assurance of compliance for all federally funded research [31].
The Common Rule directly embeds the principles of the Belmont Report. The Code of Federal Regulations explicitly states that department or agency heads retain final judgment on coverage and "this judgment shall be exercised consistent with the ethical principles of the Belmont Report" [29]. Furthermore, the authority to waive certain procedural requirements is contingent upon the alternative procedures being "consistent with the principles of the Belmont Report" [29].
Table 2: Mapping Belmont Report Principles to Common Rule Requirements
| Belmont Report Element | Operational Application | Common Rule (45 CFR 46) Implementation |
|---|---|---|
| Respect for Persons | Informed Consent [11] | Detailed requirements for consent document content and process (§46.116), criteria for waiver of consent (§46.117) [31] [27]. |
| Beneficence | Assessment of Risks and Benefits [11] | IRB criteria for approval include risks minimized and justified by anticipated benefits (§46.111) [11] [31]. |
| Justice | Selection of Subjects is Equitable [11] | IRB must ensure subject selection is equitable (§46.111) [11]. Vulnerable populations get additional protections in Subparts B, C, and D [32] [12]. |
The Researcher's Toolkit: Applying Belmont Principles in Practice
For the research professional, understanding the interplay between the Belmont Report and the Common Rule is essential for designing and conducting ethically sound and compliant research. The following diagram and table provide a practical framework for navigating this process.
Key Research Reagent Solutions: Ethical and Regulatory Components
For a researcher, the following components are as essential as any laboratory reagent for successfully conducting human subjects research.
Table 3: Essential Components for Human Subjects Research
| Component | Function & Purpose | Belmont Principle Addressed |
|---|---|---|
| Institutional Review Board (IRB) | An independent ethics committee that reviews, approves, and monitors research protocols to protect the rights and welfare of human subjects [31]. | All Three |
| Informed Consent Document | A process and document that ensures prospective subjects understand the research risks, benefits, and alternatives, allowing for a voluntary decision to participate [11] [27]. | Respect for Persons |
| Protocol Risk-Benefit Analysis | A systematic assessment within the research protocol that justifies the risks to subjects by the anticipated benefits to them or to society [11] [12]. | Beneficence |
| Inclusion/Exclusion Criteria | Scientifically justified criteria for subject selection that ensure equitable distribution of the burdens and benefits of research, avoiding exploitation of vulnerable groups [11]. | Justice |
| Single IRB (sIRB) of Record | For multi-site research, a designated single IRB that conducts the review for all sites, streamlining the process while maintaining protections [31]. | Beneficence, Justice |
| Data Use/Sharing Agreement | A governance document specifying how participant data will be used, shared, and protected, especially for de-identified data or biospecimens [27]. | Respect for Persons |
Experimental Protocol for Ethical Review
The following methodology outlines the standard operational procedure for securing approval for human subjects research, reflecting the application of Belmont principles through the Common Rule's regulatory mechanisms.
Protocol Development: The investigator designs a research protocol that incorporates ethical considerations from the outset. This includes:
- Designing a robust informed consent process with a document written in language understandable to the prospective subject [11].
- Conducting a preliminary risk-benefit analysis and implementing design features to minimize risks [11] [12].
- Defining inclusion/exclusion criteria that are equitable and scientifically sound [11].
IRB Submission & Review: The investigator submits the complete protocol, consent documents, and supporting materials to their institution's IRB. The IRB then conducts a review, which can be full board, expedited, or a determination that the research is exempt, based on the level of risk presented [31].
- The IRB evaluates the protocol against the criteria of 45 CFR 46.111, ensuring risks are minimized and reasonable in relation to anticipated benefits, subject selection is equitable, and informed consent will be properly sought and documented [31].
IRB Approval & Implementation: Upon approval, the investigator may begin subject recruitment and enrollment. All activities must conform to the approved protocol. The consent process must be followed meticulously, and any proposed changes to the research must receive further IRB review and approval before implementation [33].
Ongoing Compliance and Reporting: The investigator is responsible for maintaining ongoing compliance. This includes:
The pathway from the Belmont Report to the Common Rule represents a seminal achievement in research ethics, successfully translating a foundational ethical framework into a durable and enforceable regulatory system. For today's researchers, scientists, and drug development professionals, an in-depth understanding of this relationship is not merely a matter of regulatory compliance but a cornerstone of rigorous and responsible science. The three principles of Respect for Persons, Beneficence, and Justice continue to provide the essential moral compass for navigating the complex ethical challenges inherent in human subjects research. As the regulatory landscape evolves, as seen in the 2018 revisions to the Common Rule and ongoing policy updates from agencies like the NSF [31] [33], the bedrock principles of the Belmont Report remain the constant foundation upon which the protection of human subjects is built.
From Theory to Protocol: Operationalizing Belmont Principles in Study Design and IRB Submissions
The principle of Respect for Persons, as articulated in the 1979 Belmont Report, forms the ethical bedrock for the requirement of informed consent in human subjects research [3]. This principle acknowledges the autonomy of individuals and obligates researchers to treat them as autonomous agents capable of making their own decisions [34]. For persons with diminished autonomy, it necessitates additional protections [8]. The practical application of this principle is the informed consent process—a comprehensive educational interaction that empowers prospective participants to make a voluntary, informed decision about their involvement in research [35]. This guide details the implementation of a meaningful consent process that transcends regulatory compliance, fulfilling the ethical duty of Respect for Persons.
Core Components of a Meaningful Consent Process
A meaningful consent process is not a single event but a continuous, dynamic interaction. It is built upon three foundational pillars, as derived from the Belmont Report's applications section on informed consent [9].
Information Disclosure
Researchers must provide complete and understandable information about the study. The key information must be presented in a concise and focused manner at the beginning of the consent process to help prospective subjects understand why one might or might not want to participate [35]. This includes:
- Purpose and Nature: A clear explanation that the activity is research, its duration, and the procedures involved [35] [36].
- Risks and Benefits: A thorough description of any foreseeable risks, discomforts, and potential benefits, both to the participant and to society [37].
- Voluntary Participation: An explicit statement that participation is voluntary and that refusal to participate involves no penalty or loss of benefits [38].
Participant Comprehension
Simply providing information is insufficient. Researchers must ensure the information is truly understood by the prospective participant [9]. This involves:
- Appropriate Language: Presenting information in language that is understandable to the subject or their representative, typically at or below an 8th-grade reading level [35] [36].
- Avoiding Technical Jargon: Replacing complex scientific terms with common, lay language [36].
- Assessing Understanding: Allocating sufficient time for questions and discussion, and confirming the participant's comprehension of key study elements [35].
Voluntariness
The decision to participate must be made without coercion or undue influence [9]. This requires:
- Freedom from Coercion: Ensuring no explicit or implied threats of penalty are used [34].
- Managing Undue Influence: Carefully considering compensation and other inducements to ensure they do not become an overpowering influence, particularly for vulnerable populations [37].
- Right to Withdraw: Explicitly stating that the participant can discontinue involvement at any time without penalty [38].
Table 1: Core Components of Informed Consent and Their Practical Applications
| Core Component | Key Requirements | Practical Implementation Strategies |
|---|---|---|
| Information Disclosure [9] | - Concise presentation of key information- Complete details of risks/benefits- Clear description of procedures | - Use a 2-page key information summary [35]- Organize information to facilitate understanding [35] |
| Participant Comprehension [9] | - Understandable language- Assessment of understanding- Opportunity for questions | - Write at an 8th-grade reading level [36]- Use Flesch-Kincaid readability tests [36] |
| Voluntariness [9] | - Free power of choice- Absence of coercion or undue influence- Right to withdraw without penalty | - Scrutinize compensation for undue influence [37]- Explicitly state the right to withdraw [38] |
Regulatory Framework and Documentation
The ethical principles of the Belmont Report are codified in federal regulations, primarily the Common Rule (45 CFR 46) and FDA regulations [39]. While the specific rules may vary, the foundational requirements for informed consent are consistent.
General Requirements for Informed Consent
The Department of Health and Human Services (DHHS) mandates that the consent process must provide sufficient information, time, and opportunity for discussion for the participant to make an informed decision [35]. The process must:
- Begin with a brief, focused presentation of the most important information [35].
- Be sought under conditions that minimize coercion or undue influence [35].
- Be in language understandable to the participant and free of exculpatory language [35].
Required Elements of Informed Consent
The regulations stipulate specific elements that must be present in the consent process. These are categorized into basic and additional elements [35].
Basic Elements include a statement that the study involves research, an explanation of its purpose and duration, a description of procedures, and a disclosure of any foreseeable risks or benefits [37]. Additional Elements may include a statement that participation may involve unforeseen risks, circumstances under which the participant's involvement may be terminated, and the consequences of a participant's decision to withdraw [35].
Table 2: Essential Elements of a Consent Form
| Element Category | Specific Requirements | Regulatory Reference |
|---|---|---|
| Basic Elements | - Statement that the activity is research- Explanation of the study's purpose and duration- Description of all procedures- Disclosure of foreseeable risks and benefits- Explanation of confidentiality protections- Contact information for questions | 45 CFR 46.116(b) [35] |
| Additional Elements | - Statement about unforeseeable risks- Circumstances for termination by investigator- Consequences of participant withdrawal- Disclosure of new findings that may affect willingness to participate | 45 CFR 46.116(c) [35] |
| Documentation | - Written form signed by participant- Short form for oral consent process- HIPAA authorization for PHI use | 45 CFR 46.117 [35] |
The Informed Consent Workflow: A Dynamic Process
The following diagram visualizes the informed consent process as a continuous cycle, emphasizing that it begins before and continues after the formal signing of the consent document.
Research Reagent Solutions for Consent Processes
Table 3: Essential Materials for Implementing the Informed Consent Process
| Tool / Resource | Primary Function | Application in Consent Process |
|---|---|---|
| Readability Assessment Tools (e.g., Flesch-Kincaid) [36] | Quantifies the reading grade level required to understand a document. | Ensures consent forms are written at an appropriate level (e.g., ≤ 8th grade) for the target population. |
| Institutional Review Board (IRB) [34] [38] | An independent ethics committee that reviews, approves, and monitors research involving human subjects. | Provides mandatory pre-approval of the consent process and forms, ensuring regulatory and ethical compliance. |
| Legally Effective Consent Form Template [35] | A pre-structured document that includes all required regulatory elements. | Serves as the foundation for creating a study-specific consent form that meets federal and local requirements. |
| Key Information Summary [35] | A concise, 1-2 page document presenting the most critical study information in a simple format. | Used to initiate the consent discussion, enhancing prospective participant comprehension of core concepts. |
| Conflict of Interest (COI) Disclosure [39] | A formal statement revealing potential financial or other biases. | Manages researcher conflicts, maintaining transparency and trust in the consent process as required by FDA. |
Experimental Protocols for Valid Consent
Protocol for Assessing and Ensuring Comprehension
A critical yet often overlooked component of valid consent is verifying that the participant truly understands the information provided. The following methodology provides a structured approach.
Objective: To empirically assess and ensure prospective participant comprehension of key study elements before enrollment. Materials: Study-specific consent form, Key Information Summary, a set of open-ended questions targeting core concepts (e.g., purpose, procedures, risks, voluntariness), a quiet space for discussion. Procedure:
- Information Presentation: The researcher conducts the initial consent discussion using the Key Information Summary and consent form, avoiding technical jargon [36].
- Teach-Back Method: After explaining a key section (e.g., risks), ask the participant to explain it back in their own words. For example, "To make sure I explained everything clearly, could you tell me what you understand the main risks of this study to be?" [35].
- Structured Assessment: Pose specific, open-ended questions to assess understanding of critical areas:
- "What is the main goal of this research?"
- "What will you be asked to do during the study?"
- "What are the most significant risks or discomforts you might experience?"
- "What should you do if you change your mind about participating later?" [38]
- Clarification and Re-assessment: If misunderstandings are identified, the researcher clarifies the information and re-assesses comprehension. This cycle continues until a satisfactory understanding is achieved [35].
- Documentation: While the assessment itself is not typically documented in the consent form, the researcher should note in study records that the comprehension process was completed.
Protocol for Managing Consent with Vulnerable Populations
Populations with diminished autonomy, such as children or individuals with impaired decision-making capacity, require modified consent protocols to uphold the principle of Respect for Persons [37].
Objective: To obtain ethically and legally valid permission for the participation of an individual with diminished autonomy. Materials: Parental/Legal Guardian Permission Form, Child Assent Form (if applicable), capacity assessment tools (if applicable). Procedure:
- Determine Capacity: Assess the individual's capacity to provide independent consent. For children, this is defined by legal statute (generally <18 years) [37]. For adults, this may involve a clinical evaluation.
- Obtain Permission: Secure informed permission from the legally authorized representative (LAR), such as a parent or guardian. This process must include all standard consent elements [3].
- Solicit Assent: For individuals who lack consent capacity but possess some degree of understanding (e.g., children typically over age 7), obtain their affirmative agreement, or "assent" [38]. The assent process should be tailored to the individual's developmental level.
- Respect Dissent: A child's or vulnerable person's dissent (objection to participate) should be respected, barring exceptional circumstances where the research intervention holds out the prospect of direct benefit that is unavailable outside the study [3].
- Documentation: Document both the LAR's permission and the participant's assent (or dissent) according to IRB policies.
A meaningful informed consent process is the primary mechanism for implementing the Belmont Report's principle of Respect for Persons. It requires moving beyond a signature on a form to embrace an ongoing, interactive, and educational relationship with research participants. By systematically integrating the core components of information, comprehension, and voluntariness into their practice—and by utilizing the structured protocols and tools outlined in this guide—researchers and drug development professionals can ensure their work is not only scientifically valid but also ethically sound. This commitment protects participant autonomy and dignity, thereby strengthening the integrity of the entire research enterprise.
Systematic assessment of risks and benefits represents a fundamental ethical imperative in human subjects research, directly supporting the three core principles established by the Belmont Report: Respect for Persons, Beneficence, and Justice [3] [9]. This guidance is intended to present human subjects regulatory concepts within the context of the Belmont Ethical Principles [3]. While originating from response to historical ethical lapses in research, the need for structured approaches has expanded to regulatory decision-making throughout the therapeutic product lifecycle [40] [41].
This technical guide provides researchers and drug development professionals with a practical framework for implementing systematic risk-benefit assessments, presenting both descriptive frameworks and quantitative methodologies that enhance transparency, consistency, and stakeholder inclusion in these critical determinations [40] [41].
Ethical Foundations: The Belmont Principles
The Belmont Report, published in 1979, provides the ethical foundation for human subjects research in the United States and establishes three fundamental principles that directly inform risk-benefit assessment [3] [9]:
Core Ethical Principles
Respect for Persons: This principle acknowledges the autonomy of individuals and requires that subjects enter research voluntarily and with adequate information. It expresses the ethical conviction that the autonomy of individuals should be respected and that persons with diminished autonomy are entitled to equal protection [3] [9].
Beneficence: This principle describes an obligation to protect subjects from harm by maximizing possible benefits and minimizing possible harms. It requires that researchers systematically assess the risks and benefits of their proposed studies [3] [9].
Justice: This principle promotes equitable representation in research in terms of fairly distributing the risks and benefits of research. It requires examining whether the populations bearing the research risks are likely to benefit from its outcomes [3].
The Belmont Principles can conflict with each other with respect to research consent. Considerations of Beneficence must be balanced against an obligation to allow for subject autonomy when subjects have consent capacity (Respect for Persons) and promoting equitable representation in research (Justice) [3].
Structured Frameworks for Risk-Benefit Assessment
The BRAT Framework
The Benefit Risk Action Team (BRAT) Framework is a structured, descriptive approach developed by the Pharmaceutical Research and Manufacturers of America (PhRMA) that has been applied in various regulatory contexts, including recent assessments of COVID-19 therapies [40]. The framework consists of six sequential steps:
Table 1: The BRAT Framework Six-Step Process [40]
| Step | Process | Key Activities |
|---|---|---|
| 1 | Define Decision Context | Define drug, dose, formulation, indication, patient population, comparator(s), time horizon for outcomes, and decision-maker perspective. |
| 2 | Identify Outcomes | Select all important outcomes and create an initial value tree. Define preliminary outcome measures/endpoints for each. |
| 3 | Identify Data Sources | Determine and document all data sources (e.g., clinical trials). Extract all relevant data with detailed references. |
| 4 | Customize Framework | Modify the value tree based on further data review and clinical expertise. Refine outcome measures/endpoints. |
| 5 | Assess Outcome Importance | Apply ranking or weighting of outcome importance to decision-makers or other stakeholders. |
| 6 | Display & Interpret Key Metrics | Summarize source data in tabular and graphical displays. Challenge summary metrics, review source data, and identify information gaps. |
This framework's strength lies in its ability to separately present benefits and risks clearly, facilitating comparison without synthesizing data into complex statistical models [40]. The key anticipated benefits and risks associated with a drug are identified by clinicians with pharmacovigilance expertise based on literature search findings, then visually presented in a value tree where benefits and risks are ranked separately based on levels of seriousness [40].
PrOACT-URL Model
The European Medicines Agency's Benefit-Risk Methodology Project suggested that application of the PrOACT-URL model may be sufficient for many decision contexts [40]. This descriptive framework consists of eight components:
- Problems: Define the decision problem clearly
- Objectives: Identify what the decision aims to achieve
- Alternatives: Consider all reasonable choice options
- Consequences: Identify how alternatives perform on objectives
- Trade-offs: Determine acceptable balances between competing objectives
- Uncertainty: Characterize unknowns affecting the decision
- Risk attitudes: Account for decision-makers' risk tolerance
- Linked decisions: Consider connections to future decisions [40]
Quantitative Methodologies
Multi-Criteria Decision Analysis (MCDA)
Multi-criteria decision analysis using the Analytic Hierarchy Process (AHP) facilitates decision-making in complex situations involving tradeoffs by explicitly considering the risks and benefits of alternatives [42]. MCDA methods are designed to help people make good decisions by helping them better understand the available information, assess their decision preferences and priorities, and enhance communication among involved stakeholders [42].
The AHP is conducted in five sequential steps:
- Define the goal of the decision and develop the AHP model hierarchy
- Collect information about how well alternatives fulfill decision criteria
- Compare alternatives using pairwise comparisons to judge importance of criteria
- Combine scales to create summary scores indicating how well alternatives meet the decision goal
- Conduct sensitivity analyses to explore effects of changing estimates [42]
This approach allows for a more structured method of synthesizing and understanding evidence in the context of importance assigned to outcomes [42]. The AHP uses pairwise comparisons to sequentially compare pairs of alternative options regarding their ability to fulfill criteria, creating a combined normalized ratio scale that summarizes the results of direct and indirect comparisons [42].
MCDA Hierarchy Structure
Weighted Net Clinical Benefit
Where sufficient data is available, the BRAT framework can be extended with quantitative analysis through the calculation of weighted net clinical benefit (wNCB) [40]. In this approach:
- Benefits have a positive contribution to the wNCB
- Risks have a negative contribution to the wNCB
- The overall wNCB is positive (benefit outweighs risk) where wNCB >0 [40]
This method requires both benefits and risks to be ranked on a single continuum with preferential weights applied for each outcome [40].
Practical Implementation Guide
Assessment Workflow
Implementing a systematic risk-benefit assessment requires a methodical approach that integrates both ethical considerations and methodological rigor.
Risk-Benefit Assessment Workflow
Data Presentation Strategies
Effective communication of risk-benefit assessments requires appropriate data visualization strategies:
Table 2: Data Presentation Methods Comparison [43] [44] [45]
| Method | Best For | Effectiveness | Belmont Principle Alignment |
|---|---|---|---|
| Tables | Presenting precise, detailed data; individual information; both quantitative and qualitative information | 65% increase in understanding complex data compared to text alone [45] | Respect for Persons (enables detailed review) |
| Graphs | Showing trends, relationships, or patterns; identifying trends quickly; large amounts of data | 40% increase in data retention compared to plain text [45] | Beneficence (clarifies harm/benefit patterns) |
| Value Trees | Visualizing key outcomes ranked by seriousness; showing benefit-risk structure | Enhances transparency of decision factors [40] | Justice (makes tradeoffs explicit) |
| Heat Maps | Applying colors to table backgrounds to visualize information; quick identification of key data | More effective visualization than regular tables [44] | Beneficence (highlights critical safety concerns) |
Table 3: Research Reagent Solutions for Risk-Benefit Assessment
| Tool / Method | Function | Application Context |
|---|---|---|
| Analytic Hierarchy Process (AHP) | Structures complex decisions using pairwise comparisons and hierarchical modeling | Multi-criteria decision analysis for treatments with multiple benefits and risks [42] |
| Discrete Choice Experiment (DCE) | Quantifies patient preferences by presenting choices between alternative profiles | Incorporating patient perspectives into benefit-risk assessments [41] |
| Benefit-Risk Action Team (BRAT) | Provides structured framework for presenting benefit-risk data and supporting narrative | Regulatory submissions and internal decision-making for pharmaceutical products [40] [41] |
| Weighted Net Clinical Benefit | Combines benefits and risks using preferential weights into single metric | Quantitative benefit-risk assessment when sufficient data is available [40] |
| GRADE Criteria | Systematic approach to grading quality of evidence in individual studies | Critical appraisal of studies for inclusion in benefit-risk assessment [40] |
| Heat Maps | Enhances table readability through color application to cell backgrounds | Presenting complex clinical data for quicker interpretation [44] |
Critical Implementation Considerations
Evidence Quality Assessment
How studies with relevant data are screened to ensure only scientifically robust designs are included represents a fundamental consideration [40]. Options include applying predefined criteria such as the GRADE criteria, which provide a systematic and transparent approach to grading the quality of evidence [40]. This standardization is essential for identifying studies that may lead to less reliable overall assessments.
Outcome Ranking Challenges
Ranking outcomes and applying associated weightings presents significant methodological challenges [40]. For example, determining how to rank a very serious but rare outcome requires consideration of the individual nature of the event including prognosis and associated mortality alongside incidence rates [40]. These judgments should ideally be done independently by at least two clinicians to ensure consistency and validity.
Incorporating Patient Perspectives
Despite multiple initiatives to explore patient perspectives in decision-making processes, patient perspectives are not routinely incorporated into benefit-risk assessments [40]. Fundamental questions remain regarding who should be consulted, and how and when this data should be collected. Regulatory agencies have increasingly emphasized the importance of incorporating patient preferences, with the EMA's "Regulatory Science to 2025" including an objective to expand the role of patient preferences in benefit-risk assessments [41].
Assessment Timing and Frequency
For approved medicines, well-defined regulatory milestones exist where benefit-risk is formally assessed [40]. However, in rapidly evolving contexts such as during the COVID-19 pandemic, determining appropriate assessment frequency becomes more challenging. The acknowledgment that benefit-risk is based on a living body of evidence and constitutes a dynamic evaluation that changes over time represents a fundamental principle [40]. Updated assessments should be produced for drugs under ongoing study as more data becomes available.
Systematic assessment of risks and benefits provides an essential methodology for upholding the ethical principles of the Belmont Report throughout the research lifecycle. By implementing structured frameworks such as BRAT and quantitative methodologies including MCDA, researchers can enhance the transparency, consistency, and stakeholder responsiveness of these critical determinations. As regulatory expectations evolve toward more formalized and patient-centered approaches, these methodologies will play an increasingly vital role in ensuring that research practices remain aligned with their ethical foundations while accommodating the complexities of modern therapeutic development.
The Belmont Report, a foundational document for ethical research, establishes three core principles: Respect for Persons, Beneficence, and Justice [3] [9]. This guide focuses on the principle of Justice, which demands a fair distribution of the burdens and benefits of research [9]. In practice, justice requires equitable selection and recruitment of human subjects, ensuring that no particular group is either unduly burdened by research risks or unfairly excluded from potential research benefits [46].
Historically, vulnerabilities have been exploited, and certain populations have been systematically excluded, leading to research findings that lack generalizability and perpetuate health disparities [47] [46]. This technical guide provides researchers, scientists, and drug development professionals with a practical framework for implementing the ethical principle of justice into actionable, equitable recruitment strategies and subject selection processes.
Ethical Foundation and Regulatory Landscape
The Belmont Principle of Justice
The principle of Justice, as articulated in the Belmont Report, addresses the question: "Who ought to receive the benefits of research and bear its burdens?" [48]. It is defined as fairness in distribution [48]. An injustice occurs when a benefit is denied without good reason or a burden is imposed unduly [48]. This principle is relevant at two levels:
- Social Justice: This requires distinguishing between classes of subjects that should and should not participate in any particular kind of research, ensuring that vulnerable populations are not targeted for risky research simply because of their availability or manipulability [48].
- Individual Justice: This requires researchers to exhibit fairness in selecting individual subjects, meaning they should not offer beneficial research only to favored patients nor select only "undesirable" persons for risky research [48].
Application to Subject Selection
The application of justice in subject selection necessitates a conscious effort to avoid exploiting vulnerable populations and to avoid the unjustified exclusion of any group, whether out of "bigotry, laziness or convenience" [46]. The Belmont Report's applications section stresses that the selection of subjects must be equitable [48]. This means the research plan must justify the inclusion or exclusion of specific populations and include additional safeguards for groups likely to be vulnerable to coercion or undue influence, such as children, prisoners, or economically disadvantaged persons [48].
Quantitative Landscape of Recruitment Disparities
A data-driven understanding of existing disparities is crucial for developing targeted solutions. The following table summarizes key quantitative findings on recruitment challenges and representation gaps.
Table 1: Documented Disparities in Clinical Trial Recruitment
| Aspect of Disparity | Findings | Source/Context |
|---|---|---|
| Ethnic/Racial Representation | Black and Hispanic patients account for <5% of clinical trial participants, despite comprising 12% and 16% of the US population, respectively. | Analysis of publicly funded cancer Phase I-III trials [47]. |
| Age Representation | Older adults account for ~⅓ of participants in major cancer trials but more than ⅓ of patients for those cancer types. | Data from prostate, lung, breast, and colorectal cancer trials [47]. |
| Recruitment Plan Deficiencies | Only 8.79% of studied research protocols outlined a detailed recruitment strategy. | Analysis of ethics committee protocols in Western India [49]. |
| Population-Specific Strategies | A mere 6.59% of study protocols mentioned population-specific recruitment strategies. | Same analysis of ethics committee protocols [49]. |
| General Recruitment Failure | ~50% of all clinical trials fail to reach their enrollment goal. | Industry-wide observation [47]. |
Developing an Equitable Recruitment Strategy: A Procedural Workflow
Implementing a just and equitable recruitment strategy is a multi-stage process. The workflow below outlines the key procedural steps from initial assessment through to execution and monitoring.
Equitable Recruitment Workflow
Community Engagement and Partnership
The first step involves proactive engagement with the communities from which participants will be recruited. This is an expression of Respect for Persons and is critical for building trust and ensuring the research is designed in a culturally appropriate manner [3] [46]. A key strategy is partnering with patient organizations, advocacy groups, and community centers that have direct access to and the trust of diverse populations [47] [50]. For example, one case study noted that partnering with local community centers and translating materials was a successful strategy for increasing ethnic diversity in a diabetes intervention program [50]. This process helps researchers understand cultural, social, and logistical barriers to participation.
Multi-Lingual and Comprehension Planning
The Belmont Report requires that informed consent information be provided "in language understandable to the subject" [9]. This is a regulatory requirement under 45 CFR 46.116 and is essential for justice, as it avoids the unjust exclusion of individuals with Limited English Proficiency (LEP) [46]. Planning involves:
- Identifying Major Language Groups: Knowing the demographic composition of the geographic recruitment area [46].
- Professional Translation: Using professional, IRB-approved translation services for consent forms and recruitment materials, not ad-hoc translations by staff, which can lead to serious errors and misunderstandings [46].
- Comprehension Focus: Adapting the presentation of information to the subject's capacities, ensuring true understanding beyond mere receipt of information [48].
Leveraging Technology to Overcome Barriers
Digital tools can significantly enhance the reach and inclusivity of recruitment efforts, aligning with the principle of Beneficence by maximizing potential benefits (access to research) [3] [47].
- Online Platforms and Matching Tools: Internet-based tools, such as the "Trial Library" intervention for prostate cancer patients, can overcome geographical barriers and automate patient eligibility screening, making trial information accessible to a broader population [47].
- Mobile-First Design: With 81% of US adults owning a smartphone and 46% using it as a primary internet access point, digital resources must be designed for mobile-first use to prevent creating a new digital divide [47].
- Social Media Targeting: Platforms like Facebook allow for precise demographic targeting, which can be used to ensure outreach reaches diverse populations [50]. All such materials must receive IRB approval prior to use [50].
Experimental Protocol: A Case Study in Digital Recruitment
The following section provides a detailed methodology for a specific intervention designed to promote equitable recruitment, as described in a pilot study protocol.
The Trial Library Intervention: A Protocol for Equitable Prostate Cancer Trial Matching
Background and Hypothesis: This protocol was designed to address the pronounced underrepresentation of Black men in prostate cancer clinical trials, despite their higher burden of disease [47]. The hypothesis was that a digitally delivered, user-friendly intervention could increase patient-initiated conversations about clinical trials and improve equitable access.
Primary Aims: The study aimed to measure the acceptability, feasibility, and preliminary efficacy of the "Trial Library" website, a multi-component online tool providing prostate cancer health information and clinical trial matching [47].
Table 2: Key Research Reagent Solutions for Digital Recruitment Intervention
| Item/Tool | Function in the Experimental Protocol |
|---|---|
| Trial Library Web Platform | Core intervention; delivers visual, audio, and written educational content about clinical trials in an accessible format. |
| Matching Tool Algorithm | A series of visual questions (e.g., body diagrams for disease stage) that generate a personalized list of potential clinical trials for the patient. |
| Patient Report Generator | Creates a printable summary for the patient, including trial names, plain-language descriptions, appointment frequency, and location. |
| Electronic Health Record (EHR) | Used to pre-screen potential participants and later to document whether a discussion about clinical trials occurred during the clinic visit. |
| Tablet Computer (e.g., iPad) | Provided to participants at the clinic to ensure standardized access to the intervention and a consistent user experience. |
| HIPAA-Compliant Data Management System | Securely stores collected participant data, survey responses, and clinical information for analysis. |
Study Design: A non-randomized, single-arm pilot study using a mixed-methods approach [47].
- Participant Identification: Potential participants were identified via EHR review seven days before their oncology clinic appointment [47].
- Informed Consent: Participants provided written informed consent after check-in. The consent process included options for the survey component and a separate optional consent for a qualitative interview [47].
- Intervention Delivery: Participants used the Trial Library tool on an iPad in the clinic. The intervention consisted of three components:
- Data Collection:
- Quantitative: Post-visit surveys measured participant satisfaction and self-reported interactions. The EHR was reviewed to document actual clinical trial discussions [47].
- Qualitative: A subset of participants and all involved physicians were invited to participate in semi-structured interviews to explore the user experience in depth [47].
- Outcome Measures:
- Acceptability: Participant satisfaction scores from post-visit surveys [47].
- Preliminary Efficacy: The proportion of participants with a documented clinical trial discussion in the EHR [47].
- Feasibility: The duration of the clinical visit, assessing the practical integration of the tool into clinic workflow [47].
The Researcher's Toolkit for Equitable Recruitment
Beyond a specific protocol, researchers can utilize a suite of strategic tools and approaches to embed justice into their recruitment practices. The following diagram maps these key tools and their relationships in an equitable recruitment strategy.
Recruitment Strategy Toolkit
Strategic and Procedural Tools
- Culturally and Linguistically Appropriate Materials: All recruitment advertisements, flyers, and consent documents must be easily understandable and free of coercive language [50] [46]. This involves using relatable language, avoiding technical jargon, and professionally translating materials for non-English speakers [50] [46].
- Thoughtful Incentives: Compensation for participants' time and effort is acceptable but must be transparent and not constitute undue influence [50]. The value should not be so high as to cloud a prospective subject's judgment about the risks involved [48].
- Clear and Justified Eligibility Criteria: Researchers must detail specific inclusion and exclusion criteria to ensure the recruitment of appropriate participants while critically evaluating whether criteria unjustly exclude certain groups (e.g., based on language or age) without a sound scientific rationale [50] [46].
Technological Tools
- Online Recruitment Platforms and Social Media: These tools can reach a wide and diverse audience. Targeted advertising can be used to ensure outreach specifically reaches demographic groups that have been historically underrepresented [50].
- Automated Communication and Screening Tools: HIPAA-compliant email tools, SMS systems, and virtual screening platforms (e.g., Zoom for Healthcare) can streamline the initial contact and eligibility screening process, making it more efficient for both researchers and potential subjects [50].
Oversight and Monitoring Tools
- IRB-Approved Recruitment Plan: A detailed recruitment plan, including all advertisements and consent materials, must be submitted for IRB review and approval before implementation [50]. The IRB's role is to ensure that plans are ethical and comply with regulatory standards [3] [50].
- Diversity and Inclusion Metrics: Actively monitoring the demographic characteristics of screened and enrolled participants against the relevant population base is essential. This data allows for real-time adjustments to the recruitment strategy if certain groups are being disproportionately excluded [47].
Integrating the ethical principle of Justice into the practicalities of subject selection and recruitment is an active and ongoing process. It requires moving beyond convenience sampling and implementing a structured, proactive strategy grounded in the three pillars of community partnership, accessible communication, and strategic use of technology. By adopting the frameworks, protocols, and tools outlined in this guide, researchers and drug development professionals can fulfill the ethical mandate of the Belmont Report, strengthen the scientific validity of their research, and contribute to a more equitable and just research ecosystem.
The Institutional Review Board (IRB) serves as the critical gatekeeper for ethical research involving human subjects, ensuring that studies prioritize participant welfare and rights above all other scientific considerations. IRBs, also known as ethical review boards or research ethics committees, are formally designated groups responsible for reviewing and monitoring biomedical and behavioral research to protect the rights and welfare of human participants [51]. The evolution of these oversight bodies stems from a troubling history of ethical violations in research, including the Nuremberg Trials of Nazi doctors who performed unethical experimentation during World War II, which led to the creation of the Nuremberg Code [52]. Subsequent abuses, such as the Willowbrook State School hepatitis studies where children with mental disabilities were deliberately infected, and the Tuskegee Syphilis Study where African-American men were left untreated for syphilis, further highlighted the necessity for rigorous ethical oversight [51].
In the United States, the ethical framework for human subjects research is fundamentally guided by the Belmont Report, which was developed by the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research in response to the Tuskegee Syphilis Study [51] [11]. This foundational document establishes three core ethical principles—respect for persons, beneficence, and justice—that IRBs use to evaluate research proposals [11]. Researchers must demonstrate how their protocols embody these principles throughout their IRB applications, translating abstract ethical concepts into concrete research practices that safeguard participants throughout the study lifecycle.
The Belmont Report's Ethical Principles and Their Application
Principle 1: Respect for Persons
The principle of respect for persons incorporates two distinct ethical convictions: first, that individuals should be treated as autonomous agents capable of making informed decisions, and second, that persons with diminished autonomy are entitled to special protections [11] [53]. This dual obligation requires researchers to acknowledge autonomy while implementing additional safeguards for vulnerable populations whose capacity for self-determination may be compromised or limited.
In practical application, respect for persons manifests primarily through the process of informed consent [53]. This requires researchers to provide prospective participants with comprehensive information about the study, including its purpose, procedures, potential risks and benefits, alternatives to participation, and the voluntary nature of their involvement [11]. The Belmont Report specifies that researchers must provide "adequate information in terms that are easy to understand" when participants are "not under duress" [11]. This ethical obligation extends beyond merely obtaining a signature on a document; it necessitates ensuring genuine comprehension and voluntary agreement, particularly when working with vulnerable populations such as children, prisoners, individuals with mental disabilities, or economically disadvantaged persons [51] [11].
Principle 2: Beneficence
The principle of beneficence extends beyond simply avoiding harm to encompass an active obligation to secure the well-being of research participants [11]. This principle finds expression through two complementary rules: "(1) do not harm and (2) maximize possible benefits and minimize possible harms" [11]. In the research context, beneficence requires a careful analytical process where investigators systematically assess potential risks and benefits to ensure the risk-benefit ratio is justifiable.
The application of beneficence requires researchers to conduct a thorough risk-benefit analysis [53]. The Belmont Report states that "if there are any risks resulting from participation in the research, then there must be benefits, either to the subject, or to humanity or society in general" [11]. This analysis must be clearly articulated in IRB applications, demonstrating that risks have been minimized through sound research design and that the remaining risks are reasonable in relation to the anticipated knowledge gain [52] [51]. The IRB evaluates this assessment stringently, particularly for studies involving more than minimal risk, to ensure the well-being of participants is adequately protected throughout the research process.
Principle 3: Justice
The principle of justice addresses the equitable distribution of both the burdens and benefits of research [11]. This principle emerged in response to historical patterns where the disadvantages of research participation fell disproportionately on vulnerable populations while the benefits flowed primarily to more privileged groups [51]. The Tuskegee Syphilis Study represents a grave violation of this principle, as economically disadvantaged African-American men bore all the risks while receiving none of the benefits of available treatment [51].
In practice, justice is achieved through the equitable selection of subjects [53]. IRB applications must demonstrate that participant selection is scientifically justified rather than based merely on convenience, manipulability, or compromised position of certain groups [11]. The Belmont Report states that "investigators should take precautions not to systematically select subjects simply because of the subjects' easy availability, their compromised position, or because of racial, sexual, economic, or cultural biases in society" [11]. Researchers must instead base inclusion and exclusion criteria on those factors that "most effectively and soundly address the research problem" [11], ensuring that no particular group unfairly bears the burdens of research or is unjustly excluded from its potential benefits.
Table: Applying Belmont Report Principles in IRB Applications
| Ethical Principle | Research Application | Key Documentation for IRB |
|---|---|---|
| Respect for Persons | Informed consent process; Protection of vulnerable populations; Privacy and confidentiality protections | Consent forms; Assent documents (for children); Recruitment materials; Data security plan |
| Beneficence | Risk-benefit analysis; Study design to minimize risks; Data safety monitoring plan | Research protocol; Assessment of potential harms and benefits; Safety monitoring procedures |
| Justice | Equitable subject selection; Fair recruitment practices; Inclusion of underrepresented groups | Inclusion/exclusion criteria; Recruitment plan; Compensation structure |
IRB Application Requirements and Documentation
Core Documentation for IRB Submissions
Successful IRB applications require comprehensive documentation that demonstrates both scientific merit and ethical rigor. While specific requirements vary by institution and review type, researchers should prepare these essential documents:
- Completed IRB Application: The foundational document outlining study objectives, methodology, and ethical considerations [54]. Consistency between the application and research protocol is critical, with alignment in timelines, methodologies, and participant numbers [54].
- Research Protocol: A detailed scientific plan describing the study background, objectives, methodology, statistical considerations, and organization [54].
- Informed Consent Documents: Clearly written forms describing the study's purpose, procedures, risks, benefits, alternatives, confidentiality provisions, and contact information, using "plain, accessible language tailored to your study's audience" [54].
- Recruitment Materials: All flyers, advertisements, emails, or social media posts used for participant recruitment must be pre-approved to ensure they are "free of overly persuasive or coercive language" [54].
- Data Collection Instruments: Surveys, interview questions, tests, or other tools for data gathering [54].
- Investigator CVs and Training Certifications: Documentation of the research team's expertise and completion of required human subjects protection training [54] [55].
Categorization of Review Types
IRB applications fall into different review categories based on risk level and research nature. Researchers must understand these categories as they significantly impact review timeline and documentation requirements. The University of Akron indicates that full board reviews can take "2-3 months from initial review to approval," while exempt or expedited reviews typically take "about two to four weeks" [56].
Table: IRB Review Categories and Documentation Requirements
| Review Type | Risk Level | Examples | Required Documentation |
|---|---|---|---|
| Exempt | Minimal risk | Anonymous surveys; Analysis of existing public data | Application, protocol, consent documents (if applicable), data collection tools [54] |
| Expedited | Minimal risk but greater complexity | Non-invasive procedures; Studies of sensitive topics without significant risk | Application, protocol, training certificates, CVs, recruitment materials, consent forms, data tools [54] |
| Full Board | Greater than minimal risk | Studies with vulnerable populations; Clinical trials; Sensitive topics | All documents required for expedited review plus any special letters (IND, IDE, etc.) [54] |
Methodologies for Ethical Protocol Development
Comprehensive Informed Consent Process
The informed consent process represents the practical implementation of the respect for persons principle. Effective methodologies include:
- Capacity Assessment: For research involving populations with potentially diminished autonomy, protocols should include "methods of determining if someone has the capacity to provide consent" and procedures for "identifying a legal representative who can give permission on behalf of the participant" [51].
- Tiered Consent Approaches: Implement multi-stage consent processes for longitudinal studies, allowing participants to reaffirm their continued participation at regular intervals.
- Comprehension Verification: Incorporate brief questionnaires or "teach-back" methods to verify understanding of key study elements, particularly for complex research designs.
- Cultural and Linguistic Adaptation: Translate and culturally adapt consent materials for diverse populations, using certified translators and testing for conceptual equivalence.
The Belmont Report specifies that consent information should include "the research procedure, their purposes, risks and anticipated benefits, alternative procedures (where therapy is involved), and a statement offering the subject the opportunity to ask questions and to withdraw at any time from the research" [11].
Risk-Benefit Analysis Framework
A systematic risk-benefit assessment methodology demonstrates adherence to the beneficence principle. This process should:
- Identify Potential Harms: Catalog all physical, psychological, social, and economic risks, including likelihood, magnitude, and duration [11].
- Implement Minimization Strategies: Design protocols to reduce risks through safety monitoring, data encryption, professional supervision, and exclusion criteria for vulnerable individuals.
- Evaluate Benefit Justification: Distinguish between direct benefits to participants and societal knowledge gains, ensuring that the risk-benefit ratio remains favorable [11].
- Develop Monitoring Plans: Create data safety monitoring plans (DSMPs) for studies with more than minimal risk, specifying interim review points and stopping rules.
The Belmont Report advises that those conducting ethical review should "gather and assess information about all aspects of the research, and consider alternatives systematically and in a non-arbitrary way" [11]. This methodological approach aims to "make the assessment process more rigorous, and the communication between the IRB and the investigator less ambiguous and more factual and precise" [11].
Equitable Recruitment Strategy
To satisfy the justice principle, researchers should implement participant selection methodologies that:
- Justify Inclusion and Exclusion Criteria: Provide scientific rationale for all eligibility requirements, avoiding arbitrary limitations based solely on convenience or vulnerability [11].
- Implement Diverse Recruitment Plans: Develop proactive strategies to include underrepresented groups while avoiding the disproportionate enrollment of vulnerable populations.
- Evaluate Compensation Practices: Set participant payment levels that avoid undue inducement while fairly compensating time and burden, particularly for economically disadvantaged groups.
- Assess Accessibility: Ensure research facilities, procedures, and communications are accessible to individuals with disabilities and other potentially marginalized groups.
Diagram: Ethical Framework Integration in IRB Application Process. This workflow illustrates how Belmont Report principles inform IRB application development.
The Researcher's Toolkit: Essential Research Reagent Solutions
Table: Essential Components for Ethical Research Protocols
| Toolkit Component | Function in Ethical Research | Implementation Example |
|---|---|---|
| Informed Consent Templates | Standardizes disclosure of study information while ensuring regulatory compliance | Customizable templates with all required elements of informed consent [54] |
| Vulnerability Assessment Checklist | Identifies participants needing additional protections due to diminished autonomy | Protocol-specific evaluation of cognitive, institutional, or economic vulnerability [51] |
| Risk Classification Matrix | Systematically categorizes and evaluates potential research harms | Tool for quantifying likelihood and severity of physical, psychological, and social risks [11] |
| Equitable Recruitment Planner | Ensures fair subject selection and avoids exploitation of vulnerable populations | Structured approach to developing inclusive recruitment strategies [11] |
| Data Safety Monitoring Plan Framework | Protects participant welfare during study conduct through ongoing oversight | Template for establishing monitoring committees and stopping rules [54] |
IRB Review Process and Decision Pathways
IRB Composition and Function
The IRB operates as a multidisciplinary committee structured to provide comprehensive ethical review. According to federal regulations, IRBs must have at least five members, including "at least one scientist and one layperson" [51]. The membership must be diverse enough to promote complete and adequate review of research projects, typically including:
- Scientific Members: Individuals with expertise in specific research methodologies or content areas relevant to protocols under review [57].
- Non-Scientific Members: Persons with primary concerns in non-scientific areas (e.g., lawyers, ethicists, clergy) [57].
- Unaffiliated Members: At least one member who is not otherwise affiliated with the institution to provide independent perspective [57].
FDA regulations emphasize that "IRBs should strive for a membership that has a diversity of representative capacities and disciplines" [57]. This diversity ensures that research protocols receive balanced evaluation from multiple perspectives, enhancing the protection of participant rights and welfare.
Review Procedures and Outcomes
The IRB employs a rigorous group process to evaluate research protocols and related materials. The review encompasses:
- Initial Review: Comprehensive evaluation of the research protocol, informed consent documents, recruitment materials, and investigator qualifications [57].
- Continuing Review: Periodic reassessment of approved studies, required at least annually, to ensure ongoing compliance and participant safety [57].
- Amendment Review: Evaluation of proposed changes to approved protocols before implementation.
Following review, the IRB may take several actions: approve the research as submitted, require specific modifications (to secure approval), or disapprove the research [57]. Most applications require revisions, "often minor clarifications" [55]. Researchers should anticipate this iterative process and respond comprehensively to all IRB concerns.
Diagram: IRB Application Review Pathway. This flowchart outlines the typical IRB review process from submission to decision.
Successful IRB applications transcend regulatory compliance to embody the fundamental ethical principles articulated in the Belmont Report. Researchers who thoughtfully integrate respect for persons, beneficence, and justice throughout their study designs not only facilitate smoother IRB review but also contribute to maintaining public trust in scientific research. The process demands meticulous attention to ethical considerations from a study's inception through its implementation and dissemination.
The increasing globalization of research introduces additional complexity, as many countries require approval from local ethics committees before research can proceed [58]. As evidenced by research in Uganda, which requires a two-stage approval process from both a Research Ethics Committee and the Uganda National Council of Science and Technology, understanding local context and building collaborative relationships with local institutions is essential for international research [58]. By embracing the IRB process as an opportunity for ethical refinement rather than merely a regulatory hurdle, researchers uphold the highest standards of scientific integrity while ensuring the rights and welfare of those who contribute to the advancement of knowledge.
Pediatric clinical research presents a unique ethical challenge: the imperative to generate vital knowledge for treating childhood diseases must be carefully balanced with the obligation to protect a vulnerable population that often cannot provide independent informed consent. This case study examines how the three core principles of the Belmont Report—Respect for Persons, Beneficence, and Justice—provide an ethical framework for navigating the complex processes of parental permission and child assent. These foundational principles, established in 1979, are embedded within modern regulatory frameworks worldwide, including the U.S. Code of Federal Regulations (45 CFR 46) and European Directive 2001/20/EC, which mandate additional safeguards for children in research [59].
The ethical conduct of pediatric research requires a nuanced approach that acknowledges children's developing autonomy while implementing appropriate protections. Federal regulations deliberately employ the distinct terms "parental permission" and "child assent" to differentiate this process from standard informed consent, recognizing that parents or guardians give permission for their child's participation, while the child provides affirmative agreement appropriate to their developmental level [60]. This dual-layer protection mechanism operationalizes the Belmont principles in pediatric research settings, ensuring that children are neither excluded from the benefits of research nor exposed to unnecessary risks.
Application of Belmont Report Principles to Pediatric Research
Respect for Persons: Implementing Parental Permission and Child Assent
The principle of Respect for Persons acknowledges the autonomy of individuals and requires special protection for those with diminished autonomy. In pediatric research, this principle manifests through two complementary processes: parental permission and child assent. The regulatory framework deliberately uses the term "permission" for parents rather than "consent," recognizing that parents are deciding on behalf of another person, while "assent" acknowledges the child's developing autonomy and right to be informed about research participation [60].
The American Academy of Pediatrics recommends that children approximately 7 years and older should be provided with the opportunity to assent to research participation, with their decisions honored whenever possible [59]. This age recommendation is supported by developmental research indicating that children at this stage begin to develop the cognitive capacity to understand basic research concepts. However, assent practices should be tailored to the individual child's maturity and psychological state rather than relying solely on chronological age [61]. The process involves explaining the research in developmentally appropriate language, assessing the child's understanding, and soliciting their voluntary agreement to participate.
Federal regulations provide Institutional Review Boards (IRBs) with discretion regarding when assent must be obtained and what form it should take. The Office for Human Research Protections notes that while documentation of assent for younger children who cannot read may take forms other than a signed document, "if adolescents are involved in research where a consent form would have been used if the subjects were adults, it would generally be appropriate to use a similar form to document an adolescent's assent" [61]. This approach respects the developing autonomy of older children and adolescents while maintaining appropriate protections.
Beneficence: Risk-Benefit Assessment in Pediatric Studies
The principle of Beneficence requires researchers to maximize possible benefits and minimize potential harms to research participants. In pediatric research, this principle finds concrete expression through a structured risk categorization system defined in U.S. regulations (45 CFR 46, Subpart D), which provides a framework for IRB approval of research involving children [59]. The regulatory framework establishes four categories of pediatric research that IRBs may approve, creating a careful balance between scientific necessity and participant protection.
Table: Categories of Permissible Pediatric Research Under U.S. Regulations
| Regulatory Category | Risk Level | Potential Benefit | Parental Permission Requirements |
|---|---|---|---|
| 45 CFR 46.404 / 21 CFR 50.51 | No greater than minimal risk | N/A | Permission of one parent sufficient |
| 45 CFR 46.405 / 21 CFR 50.52 | Greater than minimal risk | Prospect of direct benefit to individual child | Permission of one parent sufficient |
| 45 CFR 46.406 / 21 CFR 50.53 | Greater than minimal risk | No direct benefit, but likely to yield generalizable knowledge about child's condition | Permission of both parents required, unless one parent is deceased, unknown, incompetent, or not reasonably available |
| 45 CFR 46.407 / 21 CFR 50.54 | Research not otherwise approvable but presents opportunity to understand, prevent, or alleviate serious problem affecting children's health/welfare | Requires review by federal panel and consultation with experts | Permission of both parents typically required |
The concept of "minimal risk" serves as a critical threshold in pediatric research ethics, defined by FDA and HHS regulations as "the likelihood or degree of harm or discomfort to the research participant is no greater than the risks they typically encounter in their everyday life" [59]. This standard provides a benchmark against which research protocols are evaluated, ensuring that children are not exposed to excessive risks, particularly in studies that offer no prospect of direct benefit.
For research involving greater than minimal risk without direct benefit, additional protections apply. Such research must be "likely to yield generalizable knowledge about the [child's] disorder or condition" [59], creating an important linkage between the research question and the participant's specific medical situation. This requirement ensures that children are not exposed to significant risks for conditions unrelated to their own health challenges.
Justice: Equitable Distribution of Research Burdens and Benefits
The principle of Justice requires the equitable distribution of both the burdens and benefits of research. Historically, children were often excluded from clinical trials, leading to a significant knowledge gap in pediatric pharmacology. According to the American Academy of Pediatrics, approximately 80% of drugs prescribed to children have not been adequately studied in pediatric populations and are not labeled for children's use [59]. This therapeutic orphanhood created an injustice where children bore the risks of treatment without participating in the research necessary to establish safe and effective dosing.
Legislative efforts including the Best Pharmaceuticals for Children Act (BPCA) and Pediatric Research Equity Act (PREA) have sought to address this inequity by creating incentives and requirements for pediatric drug studies [59]. These policies acknowledge that justice requires including children in research to ensure they benefit from scientific advances, while maintaining special protections appropriate to their vulnerability.
The application of justice also requires careful consideration of participant selection. Vulnerable populations, including children, should not be involved in research that could equally well be conducted with less vulnerable participants. However, when research addresses conditions specific to children or childhood manifestations of disease, their inclusion is not only permissible but ethically necessary to ensure they benefit from advances in medical science [62].
Special Ethical Considerations and Contemporary Challenges
Adolescent Research and Waiver of Parental Permission
Adolescent participants present unique ethical considerations due to their developing capacity for autonomous decision-making. Research indicates that adolescents generally exhibit cognitive capacity similar to young adults for understanding research concepts, though their judgment and decision-making processes may still be developing [60]. This developmental reality has led to carefully circumstituted circumstances where parental permission may be waived for adolescent participation in research.
U.S. federal regulations provide two pathways for waiving parental permission in adolescent research. Under 45 C.F.R. § 46.116(d), parental permission may be waived when the research involves no more than minimal risk, the waiver will not adversely affect the rights and welfare of the participants, the research could not practicably be carried out without the waiver, and participants will be provided with additional pertinent information after participation when appropriate [60]. This provision is particularly relevant for research on sensitive health topics such as sexual health, mental health, or substance use, where requiring parental permission might prevent adolescents from accessing services they could legally obtain without parental consent in clinical settings.
Alternatively, 45 C.F.R. § 46.408(c) allows IRBs to waive parental permission requirements when "parental permission is not a reasonable requirement to protect the subjects," such as in cases involving neglected or abused children [60]. The National Commission specifically cited research on conditions for which adolescents may legally receive treatment without parental consent as appropriate for such waivers [60].
Addressing Coercion and Undue Influence
The potential for coercion represents a significant ethical challenge in pediatric research. Parents may feel pressured to enroll their children if their pediatrician, who is also responsible for their clinical care, approaches them about a research study [59]. This perceived pressure may stem from concerns that refusing participation could affect the quality of care or damage the relationship with their healthcare provider.
To address this concern, researchers should clearly emphasize that refusal to participate or subsequent withdrawal will not affect the quality of clinical care [59]. Some ethicists suggest that staff not directly involved in the child's clinical care should make the initial approach to eliminate this concern [59]. This separation of roles helps maintain the voluntary nature of research participation.
Compensation for research participation presents another potential source of undue influence. While it is generally acceptable to compensate families for their time and effort, the compensation should not reach a level that could coerce someone to enroll or remain in a study against their better judgment [59]. IRBs must carefully review proposed compensation to ensure it is commensurate with the time and burden involved without becoming an undue influence.
International Perspectives and Harmonization Efforts
Pediatric research increasingly occurs in multinational contexts, creating challenges related to varying regulatory requirements and ethical standards across jurisdictions. The European Union's Clinical Trials Regulation and related ethical guidelines provide a framework for pediatric research that shares core principles with U.S. regulations while differing in specific implementation [63]. In Europe, the legal age for giving independent informed consent varies between 14 and 18 years across member states, though all pediatric trials require consent from the child's legal representative(s) supplemented by the child's own assent or agreement when appropriate [63].
A recent environmental scan across six jurisdictions (EU, UK, USA, Canada, Japan, and Australia) revealed ongoing efforts to harmonize ethics review processes for multinational pediatric trials [64]. While centralized ethics review is increasingly common, local review may still be required for vulnerable populations like children in some jurisdictions. These harmonization efforts aim to balance the need for specialized pediatric expertise in ethics review with the practical requirements of conducting multinational trials in rare childhood diseases where patient populations are small and geographically dispersed.
Table: Key International Guidance Documents for Pediatric Research Ethics
| Guidance Document | Jurisdiction | Key Provisions Related to Assent/Permission |
|---|---|---|
| 45 CFR 46, Subpart D | United States | Establishes categories of permissible research and requirements for parental permission and child assent |
| EU Clinical Trials Regulation (536/2014) | European Union | Requires consent of legal representative, adapted information for children, and consideration of child's wishes |
| ICH E11 (R1) | International | Guidance on clinical investigation of medicinal products in pediatric population |
| Declaration of Helsinki | International | Ethical principles for medical research involving human subjects, including vulnerable groups |
Practical Implementation: Guidelines and Procedures
Implementing Effective Parental Permission Processes
The parental permission process requires careful attention to both content and communication. Permission forms must include all required elements of informed consent while being written at an appropriate reading level—typically 8th grade level or lower—to ensure comprehensibility [59]. As research methodologies become increasingly complex, maintaining clarity in permission forms presents an ongoing challenge that requires collaboration between scientific and ethics communities.
The regulatory framework specifies different requirements for parental permission based on the risk category of the research. For research not involving greater than minimal risk (45 CFR 46.404) or research involving greater than minimal risk but presenting the prospect of direct benefit (45 CFR 46.405), permission of one parent is sufficient [65]. However, for research involving greater than minimal risk with no prospect of direct benefit but likely to yield generalizable knowledge about the child's condition (45 CFR 46.406), permission of both parents is required whenever possible [65]. This tiered approach tailors the level of parental oversight to the risk-benefit profile of the research.
Researchers should obtain written permission from parents or guardians before approaching children about research participation [65]. This sequence respects the parents' role as primary decision-makers while creating space for the child's autonomous decision about assent without prior parental influence.
Developmentally Appropriate Assent Processes
Effective assent procedures must be tailored to the child's developmental stage, cognitive capacity, and psychological state. The following diagram illustrates the key considerations in implementing a developmentally appropriate assent process:
Developmentally Appropriate Assent Process
The American Academy of Pediatrics recommends that children as young as 7 years should be provided with the opportunity to decline participation in research, and their decisions should be honored [59]. However, age represents only a rough guideline, and researchers must assess each child's individual capacity rather than relying solely on chronological age. The European guidance similarly emphasizes that "trial information should be adapted to the child's language skills and understanding, the child's developmental stage, intellectual capacity, medical condition, previous life/disease experience and other circumstances" [63].
Documentation of assent should be appropriate to the child's developmental level. For older children and adolescents, a signed assent form similar to an adult consent form may be appropriate. For younger children who cannot read, documentation might take other forms, such as a witness signature verifying that assent was obtained [61]. The IRB has discretion to determine the appropriate form of documentation based on the specific circumstances of the research and the participants involved.
Table: Essential Regulatory and Ethical Resources for Pediatric Researchers
| Resource Category | Specific Tool/Guidance | Function/Purpose |
|---|---|---|
| Regulatory Frameworks | 45 CFR 46, Subpart D (U.S.) | Provides additional protections for children involved as research subjects |
| 21 CFR 50, Subpart D (U.S.) | FDA regulations governing clinical investigations involving children | |
| EU Clinical Trials Regulation | Harmonized rules for conducting clinical trials in the EU | |
| Ethical Guidelines | Belmont Report | Foundational ethical principles for human subjects research |
| AAP Guidelines for Ethical Conduct of Pediatric Research | Specialty-specific guidance on ethical issues in pediatric research | |
| ICH Good Clinical Practice | International ethical and scientific quality standard for clinical trials | |
| Practical Tools | Enpr-EMA Informed Consent Guide | European guide for designing pediatric consent and assent documents |
| Readability Assessment Tools | Ensure consent/assent forms are at appropriate comprehension level | |
| Developmentally Appropriate Assent Templates | Age-tailored assent forms and scripts |
The ethical framework established by the Belmont Report continues to provide essential guidance for navigating the complex terrain of parental permission and child assent in pediatric research. By anchoring research practices in the principles of Respect for Persons, Beneficence, and Justice, researchers can ensure that children are appropriately protected while enabling the essential research needed to improve pediatric health outcomes.
As pediatric research continues to evolve, several areas warrant ongoing attention: maintaining meaningful assent processes as research methodologies become more complex, addressing ethical challenges in multinational trials, and ensuring that regulatory frameworks keep pace with scientific advances while maintaining core ethical protections. The increasing inclusion of children and adolescents in research planning and design, exemplified by the European Young Person's Advisory Groups, represents a promising development that further operationalizes the principle of Respect for Persons by giving children a voice in research that affects them [63].
Ultimately, the careful implementation of parental permission and child assent processes demonstrates how ethical principles can be translated into practical protections for vulnerable populations. By maintaining this ethical foundation, the research community can advance pediatric health while honoring its fundamental obligation to protect children participating in research.
Vulnerable populations represent groups or communities whose members face a significantly increased risk of poor physical, psychological, or social health outcomes due to inherent or situational characteristics that compromise their autonomy and decision-making capacity [15]. In research settings, vulnerable populations are those who can be harmed, manipulated, coerced, or deceived by unscrupulous researchers because of their limited decision-making ability, lack of power, or disadvantaged status [66]. These populations include children, prisoners, individuals with impaired decision-making capacity, pregnant women, economically or educationally disadvantaged persons, and those under formal or informal authority structures [66] [15].
The historical context of research ethics underscores the critical importance of special protections for these groups. Documented exploitations in studies such as the Tuskegee Syphilis Study, the Guatemala Syphilis Experiment, and the Holmesburg Prison Experiment reveal systemic failures to protect vulnerable participants in the name of scientific advancement [67]. These ethical violations prompted the development of foundational frameworks like the Belmont Report, which established core principles for ethical research conduct [67]. Despite these protections, vulnerable populations remain both at higher risk of harm in research and underrepresented in clinical studies, creating a dual challenge of protection and equitable inclusion [66].
This paper examines ethical considerations in vulnerable population research through the lens of Belmont Report principles, offering practical frameworks and safeguards for researchers conducting studies with these groups. By integrating ethical theory with applied methodologies, we aim to equip researchers with tools to navigate the complex landscape of vulnerable population research while upholding the highest standards of scientific integrity and human rights protection.
Theoretical Foundation: The Belmont Report Principles
The Belmont Report, published in 1979, established three fundamental ethical principles for human subjects research: Respect for Persons, Beneficence, and Justice [3]. These principles provide the cornerstone for modern research ethics and regulatory frameworks, including the Federal Common Rule adopted by 21 federal departments and agencies [68] [3].
Respect for Persons
The principle of Respect for Persons encompasses two ethical convictions: that individuals should be treated as autonomous agents capable of making their own decisions, and that persons with diminished autonomy are entitled to protection [3] [69]. This principle operationalizes through requirements for obtaining and documenting informed consent, respecting privacy interests, and providing additional protections for those with limited autonomy [69]. In practical terms, respect for persons requires that potential subjects enter the research voluntarily and with adequate information about what participation entails [3]. For vulnerable populations with diminished autonomy—such as children, prisoners, or individuals with cognitive impairments—this principle mandates additional safeguards to protect their rights and welfare [3].
Beneficence
The principle of Beneficence establishes an obligation to protect subjects from harm by maximizing potential benefits and minimizing possible risks [3]. This extends beyond simply "do no harm" to actively promoting well-being through five key requirements: using procedures that present the least risk consistent with answering the scientific question; gathering data from procedures already being performed for non-research reasons when possible; ensuring risks are reasonable in relation to potential benefits and knowledge importance; maintaining promises of confidentiality; and monitoring data to ensure subject safety [69]. For vulnerable populations, beneficence requires careful assessment of risk-benefit ratios and implementation of procedures to prevent exploitation beyond that typically required for non-vulnerable subjects [15].
Justice
The principle of Justice addresses the fair distribution of research burdens and benefits [3]. This principle requires researchers to select subjects equitably and avoid exploitation of vulnerable populations or populations of convenience [69]. Justice demands that vulnerable populations not be selected for research simply because of their availability, compromised position, or manipulability [15]. Similarly, the principle requires that populations that may benefit from research outcomes should share in bearing the risks of research participation [3]. Historical injustices, such as excluding certain groups from research that could benefit them while simultaneously overburdening them with risks from other studies, highlight the critical importance of this principle in vulnerable population research [67].
Table 1: Belmont Report Ethical Principles and Applications to Vulnerable Populations
| Ethical Principle | Core Requirement | Application to Vulnerable Populations |
|---|---|---|
| Respect for Persons | Obtain informed consent; respect privacy; protect those with diminished autonomy | Additional consent safeguards; capacity assessment; use of surrogates for decision-making |
| Beneficence | Minimize risks; maximize benefits; ensure reasonable risk-benefit ratio | Enhanced risk monitoring; specialized benefit assessment; additional safety protocols |
| Justice | Equitable subject selection; avoid exploitation | Fair recruitment; equitable burden/benefit distribution; protection from over-research |
Defining and Classifying Vulnerability in Research
Vulnerability in research ethics is not a binary characteristic but rather exists along a spectrum of seriousness as a consequence of situations and context [15]. The National Bioethics Advisory Commission (NBAC) defines vulnerability as "a condition, either intrinsic or situational, of some individuals that puts them at greater risk of being used in ethically inappropriate ways in research" [15]. Two distinct approaches characterize how vulnerability is understood and addressed in research settings: categorical and contextual approaches.
Categorical Vulnerability
The categorical approach identifies specific groups or populations as vulnerable based on shared characteristics [15]. The Common Rule (45 CFR §46) specifically lists children, prisoners, pregnant women, fetuses, mentally disabled persons, and economically and educationally disadvantaged persons as vulnerable categories requiring additional protections [15]. This approach provides regulatory clarity and ensures consistent protections for groups historically vulnerable to exploitation. However, the categorical approach has limitations—it fails to address persons with multiple vulnerabilities, doesn't account for variation in vulnerability degree within groups, and classifies persons as universally vulnerable rather than identifying specific situations creating vulnerability [15].
Contextual Vulnerability
The contextual approach recognizes that vulnerability is sensitive to situation and circumstance, with individuals potentially vulnerable in one context but not another [15]. This nuanced framework allows researchers to identify specific factors creating vulnerability and implement targeted safeguards. Contextual vulnerability typically falls into several overlapping categories:
- Cognitive or Communicative Vulnerability: Includes persons with difficulty comprehending information or making decisions about participation, such as those lacking capacity (children, adults with cognitive impairment), those in situations preventing effective capacity exercise (such as medical emergencies), or those who cannot effectively communicate (language barriers) [15].
- Institutional Vulnerability: Encompasses persons under formal authority of others with potentially different values and priorities, such as prisoners, military personnel, or anyone in hierarchical relationships where saying "no" to participation may be difficult [15].
- Deferential Vulnerability: Includes persons under informal authority based on gender, race, class inequalities, or power/knowledge differentials like doctor-patient relationships [15].
- Medical Vulnerability: Arises from serious health conditions that may impair judgment or create desperation for potential treatments [15].
- Social Vulnerability: Stems from socioeconomic disadvantage, limited education, or membership in marginalized groups that may increase susceptibility to undue influence [15].
- Economic Vulnerability: Results from financial constraints that may make research payments unduly influential [15].
Table 2: Categories of Vulnerability and Corresponding Safeguards
| Vulnerability Category | Examples | Potential Safeguards |
|---|---|---|
| Cognitive/Communicative | Children, adults with cognitive impairment, non-English speakers | Plain-language consent, capacity assessment, interpreters, staged consent, use of surrogates |
| Institutional | Prisoners, military personnel, students | Independent recruiters, voluntary participation assurance, non-hierarchical consent processes |
| Deferential | Doctor-patient relationships, employee-employer dynamics | Separation of research from routine care, independent consent monitors, explicit non-coercion assurances |
| Economic | Impoverished individuals, unemployed persons | Reasonable compensation without undue influence, alternative participation options |
| Medical | Individuals with serious, life-threatening, or rare conditions | Clear explanation of therapeutic misconception, independent medical consultation |
Ethical Framework and Practical Implementation
Institutional Review Boards and Ethical Oversight
Institutional Review Boards (IRBs) serve as critical gatekeepers in protecting vulnerable research participants through independent evaluation of research protocols [70] [67]. The IRB is charged with ensuring that additional safeguards to protect the rights and welfare of likely vulnerable subjects are included in research designs [15]. When reviewing protocols involving vulnerable populations, IRBs should consider two fundamental questions: (1) is inclusion necessary? and (2) if so, are safeguards adequate? [15]
The IRB review process for vulnerable population research involves several key considerations:
- Risk-Benefit Analysis: IRBs must ensure risks are minimized and reasonable in relation to potential benefits [71]. For vulnerable populations, this analysis requires special attention to unique risks and the necessity of their inclusion.
- Informed Consent Scrutiny: IRBs carefully evaluate consent processes, documents, and capacity assessments for studies involving vulnerable groups [71].
- Equitable Selection Justification: Researchers must justify why vulnerable populations are necessary for their scientific objectives [3].
- Monitoring Plans: Ongoing monitoring and data safety plans receive heightened scrutiny for vulnerable population research [71].
Informed Consent and Assent Processes
Informed consent represents the practical application of the Respect for Persons principle, requiring that subjects provide voluntary, comprehending authorization for participation [3]. For vulnerable populations, standard consent processes often require modification and augmentation:
- Capacity Assessment: For populations with possible cognitive or communicative vulnerabilities, objective assessment of decision-making capacity should be implemented using validated tools or clinical evaluation [15].
- Enhanced Comprehension Measures: These may include plain-language forms, supplementary educational materials, interpreters, translated documents, and staged consent processes where information is presented in manageable blocks over time [15].
- Surrogate Decision-Makers: For individuals lacking capacity, proper surrogate selection and authorization processes must be established, respecting advance directives when available [15].
- Assent Procedures: For children and others with partial but incomplete decision-making capacity, assent processes complement permission from legal guardians [71]. Assent involves providing developmentally appropriate information and seeking the potential subject's affirmative agreement [71].
The following diagram illustrates the ethical decision-making framework for vulnerable population research:
Special Considerations for Specific Vulnerable Groups
Research with Children
Children represent a specifically protected vulnerable population under federal regulations, which classify pediatric research into four categories based on risk and benefit [71]:
- Category 1: Research not involving greater than minimal risk (requires permission from one parent/guardian and child assent if ≥7 years) [71].
- Category 2: Research involving greater than minimal risk but presenting prospect of direct benefit (requires permission from one parent/guardian and child assent if ≥7 years) [71].
- Category 3: Research involving greater than minimal risk with no direct benefit but likely yield of generalizable knowledge (requires permission from both parents/guardians and child assent if ≥7 years) [71].
- Category 4: Research not otherwise approvable that presents opportunity to understand, prevent, or alleviate serious problems affecting children's health/welfare (requires Secretary of HHS approval after IRB review) [71].
Research with Prisoners
Prisoners are specifically protected under Subpart C of 45 CFR 46 due to their "institutional vulnerability" stemming from living in controlled environments with limited autonomy [70] [15]. Additional protections include ensuring that research bears direct relationship to their incarceration or conditions affecting them as prisoners, that risks are not greater than what would be accepted by non-prisoners, and that subject selection is fair [15].
Research with Economically or Educationally Disadvantaged Persons
For economically or educationally disadvantaged persons, special considerations include ensuring that payments do not become undue influences, that consent information is comprehensible despite educational limitations, and that participation does not exacerbate existing disadvantages [66] [15].
Experimental Protocols and Methodological Considerations
Study Design and Recruitment
Research with vulnerable populations requires meticulous study design to balance scientific validity with ethical protections. Key methodological considerations include:
- Inclusion Justification: The scientific rationale for including vulnerable populations must be clearly articulated, ensuring their inclusion is necessary for answering scientifically and socially important questions that cannot be answered with non-vulnerable populations [15].
- Risk Minimization: Study designs should implement the least risky procedures consistent with scientific objectives, particularly for vulnerable groups who may have reduced ability to protect their own interests [69].
- Equitable Recruitment: Recruitment strategies should avoid targeting vulnerable populations merely for convenience or manipulability while ensuring fair access to research benefits [69].
Data Collection and Management
Data collection with vulnerable populations necessitates enhanced privacy and confidentiality protections:
- Enhanced Confidentiality Measures: These may include certificates of confidentiality, data encryption, secure storage, and limited access to identifiable information [70] [68].
- Cultural and Contextual Sensitivity: Data collection instruments and procedures should be adapted to the specific vulnerabilities, cultural backgrounds, and capabilities of participant groups [67].
- Ongoing Monitoring: Continuous data safety monitoring is particularly important for vulnerable populations to identify adverse events promptly [71].
Engagement and Retention Strategies
Ethical engagement with vulnerable populations requires building trust and maintaining respectful relationships:
- Community Engagement: Partnering with community representatives and organizations can help ensure research relevance and ethical conduct [66].
- Compensation Ethics: Payment should compensate for time and inconvenience without becoming unduly influential, particularly for economically disadvantaged groups [66].
- Continued Consent: For longitudinal studies, ongoing consent processes should be implemented to ensure continued voluntary participation [15].
Table 3: Research Reagent Solutions for Ethical Vulnerable Population Research
| Resource Category | Specific Tools & Methods | Function & Application |
|---|---|---|
| Ethical Frameworks | Belmont Report, Declaration of Helsinki, CIOMS Guidelines | Provide foundational ethical principles and international standards for research conduct |
| Consent Tools | Capacity assessment instruments, plain-language templates, multimedia consent aids, staged consent protocols | Enhance comprehension and ensure voluntary participation for those with cognitive or communicative vulnerabilities |
| Data Protection | Encryption software, secure databases, anonymization techniques, certificates of confidentiality | Protect privacy and maintain confidentiality of sensitive information from vulnerable participants |
| Cultural Competence | Cross-cultural validation methods, translated materials, community advisory boards | Ensure research relevance and ethical appropriateness across diverse vulnerable groups |
| Oversight Mechanisms | IRB submission templates, data safety monitoring plans, adverse event reporting systems | Facilitate regulatory compliance and ongoing participant protection |
| Engagement Resources | Community partnership models, participant compensation guidelines, advocacy group collaborations | Build trust and ensure respectful engagement with vulnerable communities |
Vulnerable populations present both ethical obligations and scientific opportunities for the research community. While these groups require additional protections due to their increased risk of harm or exploitation, their exclusion from research is equally problematic, creating evidence gaps that perpetuate health disparities and limit treatment options for their conditions [66]. The ethical path forward requires neither blanket exclusion nor uncritical inclusion, but rather thoughtful, context-sensitive protocols that balance protection with access.
Modern clinical researchers can develop and implement inclusive research policies to address past inequalities faced by vulnerable populations while advancing scientific knowledge [66]. This approach recognizes that vulnerability exists along a spectrum rather than as a binary classification and demands nuanced safeguards tailored to specific contexts and individuals [15]. By grounding research practices in the Belmont Principles of Respect for Persons, Beneficence, and Justice, researchers can navigate the complex ethical terrain of vulnerable population research while upholding the highest standards of scientific integrity and human rights protection [3] [69].
The future of ethical research with vulnerable populations lies in recognizing that protection and inclusion are not mutually exclusive goals. Through robust ethical frameworks, thoughtful study design, and genuine community engagement, researchers can generate valuable scientific knowledge while respecting the dignity and rights of all research participants, regardless of vulnerability status.
Navigating Ethical Dilemmas: Resolving Conflicts and Optimizing Research Protections
"The Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research," published in 1979, established the three foundational ethical principles that govern human subjects research in the United States: Respect for Persons, Beneficence, and Justice [28] [3]. These principles provide the moral framework for the Federal Policy for the Protection of Human Subjects (the "Common Rule") and related regulations [32] [18]. In an ideal research scenario, these principles work in harmony to ensure ethical conduct. However, researchers and Institutional Review Boards (IRBs) frequently encounter complex situations where these principles conflict, forcing difficult trade-offs. This guide examines these tension points and provides a structured approach for navigating them, ensuring that research maintains the highest ethical standards even in challenging circumstances.
The Core Ethical Principles of the Belmont Report
A thorough understanding of each principle is a prerequisite for identifying and resolving conflicts between them.
Respect for Persons
This principle acknowledges the autonomy of individuals and mandates that those with diminished autonomy are entitled to protection. It expresses the ethical conviction that individuals should be treated as autonomous agents, with the right to self-determination and the ability to make their own informed choices [28] [18]. In practice, Respect for Persons is operationalized through the process of informed consent, wherein potential participants must be provided with all relevant information about a study and must comprehend this information to make a voluntary decision about whether to partake [3]. This includes respecting a participant's right to withdraw from a study at any time without penalty [6].
Beneficence
This principle describes an obligation to protect subjects from harm by maximizing possible benefits and minimizing possible harms [3]. It goes beyond the simple injunction to "do no harm" and imposes a positive duty to act for the benefit of others [28]. The application of Beneficence requires a systematic assessment of risks and benefits [28]. Researchers must ensure that the risks posed by a study are justified by the potential benefits to the subject or to society, and that the study design is scientifically valid so that the research question can be answered reliably [6]. Uncertainties about the degree of risks and benefits are inherent in clinical research, and these can be physical, psychological, economic, or social in nature [6].
Justice
The principle of Justice promotes equitable representation in research and demands the fair distribution of its burdens and benefits [3]. This principle addresses the question of who ought to receive the benefits of research and who ought to bear its burdens [28]. It requires fair subject selection, meaning the primary basis for recruiting participants should be the scientific goals of the study—not vulnerability, privilege, or other unrelated factors [6]. Historically, disadvantaged populations have borne the risks of research while more privileged populations have reaped its benefits; the principle of Justice works to correct this ethical failure.
Table: Core Principles and Applications of the Belmont Report
| Ethical Principle | Core Meaning | Practical Application in Research |
|---|---|---|
| Respect for Persons | Recognition of personal autonomy and protection of individuals with diminished autonomy [28] [3]. | Informed consent process; respect for privacy and right to withdraw [6] [3]. |
| Beneficence | Obligation to maximize benefits and minimize harms [3]. | Assessment of risks and benefits; ensuring scientific validity [28] [6]. |
| Justice | Fairness in distribution of research burdens and benefits [3]. | Equitable selection of subjects [6] [3]. |
Navigating Conflicts Between Principles: Common Scenarios and Resolution Frameworks
In practice, the simultaneous adherence to all three principles can create ethical dilemmas where upholding one principle may mean compromising another. The following scenarios illustrate these common conflicts.
Scenario 1: Pediatric Research (Respect for Persons vs. Beneficence and Justice)
Research involving children represents a classic area where ethical principles can conflict. Children are considered a vulnerable population with diminished autonomy, which triggers enhanced protections under Respect for Persons. In practice, a parent or guardian provides permission, while the child provides assent when they have the capacity [3].
- The Conflict: A conflict arises when a child with sufficient capacity to understand the research does not want to enroll (dissent), but their parent or guardian believes enrollment is in the child's best interest and provides permission. In this case, the child's autonomy (Respect for Persons) conflicts with the parent's assessment of the child's welfare (Beneficence) [3].
- Resolution Framework: The appropriate balance depends on the risk-benefit profile of the research.
- In general, a child's dissent should be respected, upholding Respect for Persons [3].
- However, when the research is greater than minimal risk but offers a direct potential benefit to the child, IRB regulations may allow the wishes of a single parent/guardian to override the child's dissent in order to obtain that benefit, thereby favoring Beneficence [3].
- Furthermore, the IRB may approve greater than minimal risk research where the only likely benefit is the knowledge to be gained for other children with the same condition (Justice). In these cases, the IRB will generally require permission from both parents as an additional safeguard, balancing Justice with a reinforced application of Beneficence [3].
Scenario 2: Research in Conflict Zones (Respect for Persons vs. Beneficence)
Field research in conflict zones or violently divided societies presents extreme ethical challenges where ensuring true informed consent and minimizing risk can be at odds [72].
- The Conflict: The principle of Respect for Persons requires fully informed consent and ensuring participants comprehend the risks. However, in a conflict zone, fully disclosing all risks (e.g., potential retaliation by armed groups) could itself create new dangers for the participant, thereby violating Beneficence [72]. The researcher must balance the duty to inform with the duty to protect from harm.
- Resolution Framework: Researchers must implement rigorous procedures to ensure anonymity and confidentiality to the greatest extent possible [72]. This might involve:
- Contextual Judgment: Carefully assessing what information is necessary for consent without unnecessarily increasing risk.
- Robust Protections: Using secure data storage, anonymizing data immediately, and having a plan for data destruction if compromised.
- Ongoing Monitoring: Continuously re-evaluating the security situation and the welfare of participants, respecting their right to withdraw at any moment [72] [6].
Scenario 3: Inclusion of Vulnerable Populations (Justice vs. Beneficence)
The principle of Justice demands that vulnerable populations (e.g., prisoners, economically disadvantaged individuals) are not exclusively targeted for risky research nor unjustly excluded from the potential benefits of research [28] [6].
- The Conflict: Including a vulnerable population in research with significant risks raises Beneficence concerns about exploitation and harm. Conversely, automatically excluding them from research (even that which poses minimal risk) can be paternalistic and prevent these groups from accessing potential benefits, violating Justice [6].
- Resolution Framework: The NIH guiding principle of Fair Subject Selection is key here [6]. The primary basis for recruitment must be the scientific goals of the study. Specific groups should not be excluded without a sound scientific reason or a particular susceptibility to risk. The resolution involves:
- Scientific Justification: Ensuring the research question necessitates the inclusion of the specific population.
- Additional Safeguards: Implementing enhanced consent processes, involving community representatives, and providing independent advocacy for participants.
- Risk-Benefit Analysis: Making a rigorous determination that the potential benefits to the population or society are proportionate to and outweigh the risks assumed by the vulnerable group [6].
The following diagram illustrates the decision-making pathway for resolving conflicts between Belmont principles, integrating the considerations from the scenarios above.
The Researcher's Toolkit for Ethical Analysis
When confronted with a potential ethical conflict, researchers and IRBs can use the following structured methodologies and tools to guide their decision-making.
The Principle Precedence Matrix
This matrix provides a starting point for analyzing common conflicts. It is not a definitive guide but a heuristic tool to frame the ethical analysis.
Table: Principle Precedence Matrix for Common Conflict Scenarios
| Conflict Scenario | Primary Tension | Typical Precedence & Rationale | Key Mitigating Actions |
|---|---|---|---|
| Pediatric Research with Direct Benefit | Respect for Persons (Child's Dissent) vs. Beneficence (Direct Benefit) | Beneficence often prioritized. Rationale: Direct benefit to the child justifies overriding dissent for their welfare [3]. | Strengthen assent process; seek dual-parent permission; involve child advocates. |
| Non-Beneficial Pediatric Research | Respect for Persons (Child's Dissent) vs. Justice (Knowledge for Others) | Respect for Persons often prioritized. Rationale: Child's dissent respected when they bear risk for no direct benefit [3]. | Limit research to minimal risk; require dual-parent permission; mandatory assent. |
| Research in Conflict Zones | Respect for Persons (Full Disclosure) vs. Beneficence (Protection from Harm) | Beneficence often prioritized. Rationale: Protecting participants from immediate physical harm may justify modified disclosure [72]. | Implement extreme confidentiality; ongoing risk assessment; contextual consent process. |
| Inclusion of Vulnerable Groups | Justice (Fair Access) vs. Beneficence (Protection from Risk) | Context-dependent balance. Rationale: Avoid both exploitation and unjust exclusion [6]. | Scientific justification for inclusion; independent advocacy; enhanced consent. |
The Ethical Conflict Resolution Protocol
For a more detailed analysis, researchers can follow this step-by-step protocol, which draws on structured ethical deliberation and mediation techniques [73].
- Identify and Define the Conflict: Clearly articulate which Belmont principles are in conflict and why. Specify the research procedure, population, and context that creates the tension.
- Gather Relevant Information: Collect all scientific, regulatory, and contextual data. This includes the study protocol, risk-benefit analysis, regulatory requirements (e.g., 45 CFR 46, 21 CFR 50), and any relevant historical or cultural context [32] [18].
- Engage in Stakeholder Analysis: Identify all parties affected by the decision (participants, researchers, institutions, communities) and consider their perspectives, values, and power dynamics. In complex cases, formal mediation techniques can facilitate communication between conflicting parties [73].
- Generate and Evaluate Options: Brainstorm potential resolutions. For each option, evaluate the impact on each ethical principle. Ask: How does this option promote or undermine Respect for Persons? Beneficence? Justice?
- Seek Independent Review: Present the conflict and potential resolutions to the IRB. The IRB's role is to provide an independent review to minimize conflicts of interest and ensure the study is ethically acceptable [6] [32].
- Document the Deliberation: Maintain a clear record of the ethical conflict, the options considered, the rationale for the final decision, and any required mitigations. This is crucial for transparency and accountability.
- Implement and Monitor: Execute the chosen path with the agreed-upon safeguards. Continuously monitor the situation for changes and respect the ongoing welfare and autonomy of participants, being prepared to adapt if necessary [6].
Essential Research Reagent Solutions for Ethical Analysis
Just as laboratory experiments require specific reagents, rigorous ethical analysis depends on conceptual tools and regulatory knowledge.
Table: Essential "Reagents" for Ethical Analysis and Conflict Resolution
| Tool or Resource | Function in Ethical Analysis | Example/Source |
|---|---|---|
| The Belmont Report | Provides the foundational definitions of the three core ethical principles [28] [18]. | The Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research (1979). |
| Federal Regulations (Common Rule) | Provides the legal and regulatory framework for implementing ethical principles and defines IRB authority [32]. | 45 CFR 46 (HHS), 21 CFR 50 (FDA) [32]. |
| NIH Guiding Principles | Offers a complementary, practical framework of seven principles to guide ethical clinical research [6]. | Social/clinical value, scientific validity, independent review, informed consent, etc. [6]. |
| IRB Charter & SOPs | Defines the specific procedures, membership requirements, and authority of the local IRB for reviewing and monitoring research [32]. | VHA Directive 1200.05, Local Institutional IRB SOPs [32]. |
| Mediation Techniques | Provides a structured process for facilitating difficult conversations and resolving disputes among stakeholders in ethically charged situations [73]. | Techniques from professional mediation to enhance communication and manage conflict [73]. |
The Belmont Report's principles of Respect for Persons, Beneficence, and Justice are not a simple checklist but a dynamic framework for ethical reasoning. In complex research scenarios, conflicts between these principles are not a sign of failure but an inevitable consequence of engaging with challenging but critical scientific questions. The path forward requires diligent identification of these conflicts, a structured approach to analysis using tools like the Precedence Matrix and Resolution Protocol, and a steadfast commitment to independent review. By embracing this balancing act, researchers and IRBs can ensure that the pursuit of scientific knowledge remains firmly grounded in the protection of the individuals who make that pursuit possible.
Optimizing Informed Consent for Low-Literacy and Non-English Speaking Populations
Informed consent is a foundational ethical and legal requirement for human subjects research, often described as the "cornerstone of research ethics" [74]. Its intent is to ensure that participants enter research voluntarily, with a comprehensive understanding of what their participation entails, including potential risks, benefits, and alternatives [38] [74]. Despite universal agreement on its necessity, a significant challenge persists: nearly half of the United States adult population has marginal health literacy, which can severely impair their ability to fully comprehend traditional consent processes [75]. This problem is compounded for non-English speakers, where additional linguistic and cultural barriers exist.
The Belmont Report's ethical principles provide the essential framework for addressing these challenges. This guidance is structured around the Report's three core principles: Respect for Persons, which demands meaningful consent processes for autonomous agents and additional protections for those with diminished autonomy; Beneficence, which obligates researchers to maximize benefits and minimize harms; and Justice, which requires fair distribution of both research burdens and benefits [3]. This technical guide examines evidence-based strategies for optimizing informed consent within this ethical framework, focusing specifically on the needs of low-literacy and non-English-speaking populations.
The Belmont Report: Ethical Framework for Informed Consent
The Belmont Report, published in 1979, established the three basic ethical principles that govern all human subjects research in the United States [3] [76]. These principles emerged in response to historical ethical abuses, including the Tuskegee syphilis study, where participants were not informed of their diagnosis and were left untreated even after an effective cure became available [76]. The Report's principles provide the foundational rationale for informed consent requirements and guide their implementation.
Application of Core Principles to Consent
Respect for Persons: This principle expresses the ethical conviction that individual autonomy should be respected and that persons with diminished autonomy are entitled to protection [3]. In practice, this requires a meaningful consent process where subjects receive all relevant information that a reasonable person would need and can fully comprehend it, enabling a voluntary participation decision [3]. The principle acknowledges that autonomy can be compromised by various factors, including limited literacy, language barriers, or situational pressures like incarceration [76].
Beneficence: This principle describes an obligation to protect subjects from harm by maximizing possible benefits and minimizing possible risks [3] [38]. For consent processes, this requires thorough disclosure of anticipated risks and benefits as part of the consent discussion and documentation. The beneficence principle also underpins the requirement to use procedures that present the least risk to participants consistent with answering the scientific question [38].
Justice: The justice principle promotes equitable representation in research by ensuring fair distribution of both risks and benefits across populations [3]. This is particularly relevant to consent in the context of subject selection—ensuring that vulnerable populations are not disproportionately targeted for risky research while being excluded from beneficial studies [3] [38]. Justice considerations also require researchers to consider whether populations bearing research risks are likely to benefit from the knowledge gained [3].
These principles can sometimes conflict. For example, when a child's dissent to participate conflicts with a parent's permission, researchers and IRBs must balance Respect for Persons against Beneficence and Justice considerations [3]. The Belmont framework provides the conceptual tools for navigating these complex ethical dilemmas in the consent process.
The Challenge of Low Health Literacy
Comprehension Barriers in Standard Consent Processes
Limited health literacy consistently correlates with poor comprehension of informed consent materials. A systematic review of 1,620 research participants across six studies found that comprehension was significantly impaired among those with literacy levels at or below the 8th grade [77] [75] [78]. These comprehension challenges manifest across multiple domains:
Understanding of Research Concepts: Complex research concepts like randomization, clinical equipoise, and placebo controls are particularly difficult for low-literacy individuals to grasp [79]. One study assessing comprehension of Phase III cancer clinical trial information found average comprehension scores of just 58% for standard consent documents, with scores dropping to 21% for participants reading at or below a 3rd grade level [79].
Understanding of Risks and Benefits: Patients with serious diagnoses face additional comprehension challenges due to emotional stress, which can be compounded by limited health literacy [79]. This often results in inadequate understanding of potential treatment risks, benefits, and alternatives [79].
Document Readability Issues: Standard informed consent documents are typically written at a high school or college reading level, creating a significant gap between document complexity and patient reading ability [79]. This misalignment persists despite evidence that simplified materials improve comprehension.
Evidence-Based Intervention Strategies
Research evaluating interventions to improve consent comprehension in low-literacy populations remains extremely limited, with only six studies meeting eligibility criteria for a recent systematic review [77] [75] [78]. The following table summarizes the quantitative findings from these intervention studies:
Table 1: Interventions for Improving Consent Comprehension in Low-Literacy Populations
| Intervention Type | Comprehension Impact | Key Findings | Study Population |
|---|---|---|---|
| Teach-Back/Teach-to-Goal | Highest comprehension improvement | Required more passes through consent but ensured understanding; particularly effective for understanding randomization | Vulnerable patients (n=204); Coronary patients (n=408) |
| Simplified Consent Forms | Moderate improvement | No significant difference in comprehension scores between standard (58%) and simplified forms (56%); higher literacy correlated with better comprehension | Oncology patients (n=183); Mixed volunteers (n=666) |
| Metaphor-Based Explanations | Mixed results | Benign metaphor most effective for lowest literacy levels; gambling metaphor better for higher literacy | Cancer patients (n=500) |
| Computerized Agents | Limited data | Used for hypothetical genetic repository study; required validation in real-world settings | Volunteers (n=29) |
| Extended One-on-One Discussion | Most effective strategy | Spending more time talking individually with participants was most effective for improving understanding | Single study evidence |
Table 1 shows that interactive, time-intensive approaches like Teach-Back have demonstrated the most promise for improving comprehension in low-literacy populations [77] [75] [78].
The teach-back method (also called "teach-to-goal") requires researchers to explain concepts and then ask participants to explain them back in their own words, correcting misunderstandings until comprehension is achieved [75]. Studies implementing this approach found it achieved the highest levels of comprehension among the interventions studied, though it required more passes through the consent process for lower-literacy participants [75].
Metaphor-based explanations for complex concepts like randomization have shown promise, but their effectiveness depends on both the metaphor used and the participant's health literacy level. One randomized controlled trial with 500 cancer patients found that a benign metaphor was particularly effective for patients at the lower end of the health literacy spectrum, while a gambling metaphor worked better for those with higher health literacy [80].
Methodologies for Special Populations: Experimental Protocols
The Teach-Back Method for Low-Literacy Populations
The teach-back method is an evidence-based approach for verifying comprehension rather than simply delivering information. The following workflow illustrates the implementation protocol:
Diagram 1: Teach-Back Method Workflow
The teach-back protocol requires:
Explanation Phase: Researchers explain one key concept at a time using plain language at an appropriate literacy level, typically 6th-8th grade for low-literacy populations [75] [79].
Assessment Phase: Researchers ask participants to explain the concept in their own words, avoiding yes/no questions that don't verify true understanding [75].
Clarification Phase: If the participant's explanation is incomplete or inaccurate, the researcher clarifies the misunderstanding using alternative phrasing and examples, then reassesses comprehension [75].
Documentation: The process should be documented in research records, including how comprehension was verified and any particular challenges addressed.
Studies implementing this approach have demonstrated its effectiveness across diverse populations, including older adults, ethnic minorities, and patients with specific clinical conditions like coronary heart disease [75].
Rigorous Translation Protocol for Non-English Speakers
Creating linguistically and culturally appropriate consent materials requires more than simple word-for-word translation. The following multi-step protocol has been empirically validated to produce high-quality translations:
Table 2: Multi-Step Protocol for Quality Consent Form Translation
| Step | Process Description | Quality Control Measures | Key Outcomes |
|---|---|---|---|
| Initial Forward Translation | Two native speakers from different dialect regions produce independent translations | Compare translations for regional specificity, conceptual accuracy, tone consistency | Two complete translations highlighting dialectal variations |
| Reconciliation & Synthesis | Translators discuss discrepancies to create consensus version | Resolve differences in terminology, conceptual gaps, meaning changes | Single reconciled forward translation |
| Back Translation | New translator unaware of original English produces English version from consensus translation | Identify conceptual drift, meaning alterations, omissions | English back-translation for comparison |
| Comparative Analysis | Team compares original and back-translated English documents | Categorize discrepancies as acceptable (syntactic) vs. problematic (meaning changes) | List of problematic discrepancies requiring correction |
| Final Revision | Research team revises forward translation based on analysis | Ensure conceptual fidelity while maintaining natural language in target language | Final quality-certified translation |
Table 2 outlines a rigorous translation methodology that addresses common pitfalls in consent form translation [81].
Common translation problems identified through this process include:
Nonequivalent Registers: Professional translation firms frequently introduce more complicated language than the original, despite intentions to simplify. For example, straightforward English terms may be translated to more complex Spanish vocabulary that reduces comprehension [81].
Errors of Omission: Translators may omit information critical for clarity or accurate understanding, particularly when dealing with complex research concepts [81].
Meaning-Altering Mistranslations: Some translations inadvertently change the substantive meaning of information, potentially misinforming participants about key aspects of the research [81].
This protocol emphasizes the importance of working with translators who possess not only linguistic fluency but also understanding of sociocultural factors that affect comprehension and basic knowledge of research concepts [81].
Research Reagent Solutions for Consent Optimization
Implementing effective consent processes for vulnerable populations requires specific tools and assessment methods. The following table details essential resources for researchers:
Table 3: Essential Tools for Optimizing Informed Consent Processes
| Tool/Resource | Primary Function | Application Context | Key Features |
|---|---|---|---|
| REALM (Rapid Estimate of Adult Literacy in Medicine) | Health literacy assessment | Screening tool to identify participants with limited literacy | Rapid administration; categorizes reading level by grade equivalent |
| TOFHLA (Test of Functional Health Literacy in Adults) | Health literacy assessment | Comprehensive assessment of numeracy and reading comprehension | Available in full and short forms; measures functional application skills |
| BICEP (Brief Informed Consent Evaluation Protocol) | Comprehension assessment | Validated tool for measuring understanding of consent information | Specifically designed for research consent contexts |
| Flesch Reading Ease / Fernández-Huerta Index | Readability assessment | Evaluating reading level of consent forms in English/Spanish | Provides grade-level equivalent; identifies complex passages |
| Teach-Back Training Materials | Researcher training | Building capacity for interactive consent verification | Standardized protocols; example phrasing; correction techniques |
| Plain Language Glossary | Document preparation | Translating technical terms into accessible language | Research-specific plain language alternatives |
Table 3 shows key assessment tools and resources that support the implementation of optimized consent processes [75] [79] [81].
Implementation Framework and Ethical Considerations
Integrating Strategies into Research Practice
Successfully implementing these optimized consent strategies requires systematic approaches:
Pre-Study Assessment: Conduct a literacy assessment of the target population to guide consent process design. Use this information to tailor the reading level and communication approach appropriately [79].
Staff Training: Train research staff in plain language communication, teach-back methods, and cultural competency. Studies show that researchers who receive specific training are better equipped to adapt the consent process to individual participant needs [74].
Process Documentation: Document the specific approaches used to optimize consent, including literacy levels accommodated, translation methodologies, and verification processes. This documentation demonstrates commitment to ethical principles to IRBs and other oversight bodies [74].
Navigating Ethical Tensions
Optimizing consent for vulnerable populations involves navigating ethical tensions:
Balancing Comprehensiveness and Accessibility: Over-simplification may omit important information, while excessive complexity impairs understanding. Researchers must balance these competing demands through iterative testing and refinement of consent materials [74].
Respecting Autonomy Without Exclusion: While protecting vulnerable populations is essential, excessive protectionism can unjustly exclude them from research benefits. The principle of Justice requires careful consideration of how to enable participation while providing appropriate safeguards [3] [76].
Managing Researcher-Participant Power Dynamics: Relationships between researchers and participants can create subtle coercion, particularly in clinical settings where treatment providers are also researchers. Transparency about roles and separation of functions when possible can help mitigate these concerns [74].
Optimizing informed consent for low-literacy and non-English-speaking populations is both an ethical imperative and a practical necessity for equitable research inclusion. The Belmont Report's principles provide a robust framework for developing consent processes that respect autonomy, maximize benefits, and promote justice. Evidence indicates that interactive, time-intensive approaches like the teach-back method show the most promise for improving comprehension, while rigorous multi-step translation protocols are essential for linguistic accessibility.
Future directions should include development of more validated, simplified consent templates for common research types, increased researcher training in health literacy-informed communication, and greater institutional support for implementing these optimized processes. By adopting these evidence-based strategies, researchers can ensure that informed consent truly fulfills its ethical purpose as a meaningful process of autonomous authorization, regardless of participants' literacy levels or primary language.
Managing Risks in Greater-than-Minimal Risk Research with No Direct Benefit
Research interventions that pose greater-than-minimal risk with no prospect of direct benefit to participants represent one of the most ethically complex categories of human subjects research. Such studies are essential for advancing generalizable knowledge, particularly in early-phase therapeutic development and fundamental disease mechanism research, yet they demand the highest standards of ethical scrutiny and risk management. The ethical framework for evaluating these protocols is anchored in the Belmont Report's principles of respect for persons, beneficence, and justice, which collectively guide investigators and oversight bodies in balancing scientific imperatives with participant welfare [3].
Federal regulations define minimal risk as existing when "the probability and magnitude of harm or discomfort anticipated in the research are not greater than those ordinarily encountered in daily life or during the performance of routine physical or psychological examinations or tests" [82] [83]. Conversely, greater-than-minimal risk research involves probability and magnitude of harm exceeding this threshold, while offering no direct therapeutic benefit to participants [84]. Such studies require robust justification through systematic risk-benefit analysis and enhanced protective measures to meet ethical and regulatory standards.
Defining Greater-than-Minimal Risk Without Direct Benefit
Regulatory Definitions and Interpretations
The Common Rule's minimal risk definition has generated substantial interpretive challenges, particularly regarding the appropriate reference point for comparison. A persistent conundrum has been whether to compare research risks to "the daily life of an average person in the general population or the specific population to be enrolled in the study" [83]. Current ethical consensus favors a general population standard rather than a population-specific approach, as the latter "unjustly permits individuals to be exposed to higher levels of risk under the minimal risk category, simply because their daily lives are filled with greater risk" [82] [83]. This interpretation aligns with the Belmont Report's principle of justice by ensuring equitable distribution of research risks across populations.
Research without direct prospect of benefit includes studies where:
- Interventions are administered solely to answer scientific questions
- Procedures are performed for research purposes only
- The knowledge gained will not ameliorate participants' conditions
- Any potential benefits are theoretical or speculative
Examples of Greater-than-Minimal Risk Research Without Direct Benefit
Table 1: Categories of Greater-than-Minimal Risk Research Without Direct Benefit
| Research Category | Risk Level | Examples | Monitoring Requirements |
|---|---|---|---|
| Phase I Drug Trials | Greater than minimal risk to significantly greater than minimal risk | First-in-human studies of new chemical entities; dose-escalation studies in healthy volunteers | Independent Safety Monitor or Data and Safety Monitoring Board (DSMB) [84] |
| Invasive Procedures | Greater than minimal risk | Research-only biopsies, lumbar punctures, or imaging with contrast agents | PI and IRB monitoring; possibly Independent Safety Monitor [84] |
| Challenge Studies | Significantly greater than minimal risk | Deliberate exposure to pathogens or toxins in controlled settings | NIMH-constituted DSMB; enhanced monitoring [84] |
| Medication Washouts | Greater than minimal risk | Placebo-controlled trials requiring discontinuation of effective medications | Independent Safety Monitor when PI is blinded to randomization [84] |
Ethical Justification Within the Belmont Framework
Applying the Principle of Beneficence
The Belmont Report's principle of beneficence establishes the dual obligation to maximize possible benefits and minimize possible harms [3]. In research without direct benefit, this principle manifests primarily through rigorous risk minimization strategies and careful justification that the knowledge gained justifies the risks to participants. The beneficence calculus must demonstrate that:
- Risks have been reduced to the minimum necessary to achieve scientific objectives
- The research question has significant value and cannot be answered with lower-risk approaches
- The probability and magnitude of harm are reasonable in relation to the knowledge expected
The regulatory requirement that "risks to subjects are reasonable in relation to anticipated benefits" [82] applies differently in this context, where benefits primarily accrue to society rather than participants. This creates an ethical imperative to ensure the social value is substantial and the study design is scientifically valid.
Applying the Principle of Respect for Persons
Respect for persons requires protecting autonomy through voluntary informed consent and special protections for those with diminished autonomy [3]. In greater-than-minimal risk research without direct benefit, this principle demands an especially rigorous consent process that emphasizes:
- Clear communication about the absence of direct benefit
- Explicit acknowledgment of risks and discomforts
- Assurance that refusal or withdrawal will not result in penalty or loss of benefits
- Additional safeguards for vulnerable populations
The consent document must avoid therapeutic misconception by explicitly stating that procedures are performed for research purposes only. For populations with diminished autonomy, such as children or adults with decisional impairments, additional protections including surrogate decision-makers and assent procedures (when appropriate) are required [3].
Applying the Principle of Justice
The principle of justice addresses the fair distribution of research burdens and benefits [3]. In greater-than-minimal risk research without direct benefit, this principle raises particular concerns about participant selection. Ethical application of justice requires:
- Ensuring participant populations are not systematically selected because of their vulnerability or easy availability
- Avoiding the imposition of research burdens exclusively on disadvantaged groups
- Considering whether those bearing research risks might benefit from resulting knowledge
- Ensuring exclusion criteria are scientifically justified rather than merely convenient
The Belmont Report emphasizes that "the selection of research subjects needs to be scrutinized in order to determine whether some classes are being systematically selected simply because of their easy availability, their compromised position, or their manipulability" [3].
Risk Assessment Methodologies
Calculating Probability and Magnitude of Harm
An objective assessment of research risk requires evaluating both the magnitude of potential harm and the likelihood of its occurrence [82]. The regulatory framework requires that "risks to subjects are minimized" and "risks to subjects are reasonable in relation to anticipated benefits" [82]. This risk calculus involves:
- Identifying potential harms (physical, psychological, social, economic)
- Estimating probability of each harm occurring
- Assessing magnitude of each potential harm
- Evaluating uncertainty in probability and magnitude estimates
- Implementing risk mitigation strategies
Table 2: Risk Assessment Matrix for Research Protocols
| Probability/Magnitude | Minor | Moderate | Major | Severe |
|---|---|---|---|---|
| Very Likely (>70%) | Low | Moderate | High | Unacceptable |
| Probable (30-70%) | Low | Moderate | High | Unacceptable |
| Unlikely (10-30%) | Minimal | Low | Moderate | High |
| Very Unlikely (<10%) | Minimal | Low | Moderate | High |
Protocol-Specific Risk Evaluation
Each research protocol requires a systematic analysis of procedure-specific risks. The following experimental methodologies represent common greater-than-minimal risk procedures without direct benefit:
Pharmacokinetic Studies in Healthy Volunteers
- Objective: Characterize absorption, distribution, metabolism, and excretion of investigational compounds
- Methodology: Controlled administration of novel therapeutic agents with serial biological sampling
- Risks: Unknown toxicity profiles, drug interaction potential, procedural harms from repeated sampling
- Risk Management: Dose escalation strategies, stopping rules, intensive safety monitoring
Research-Only Biopsies
- Objective: Obtain tissue for mechanistic studies or biomarker validation
- Methodology: Invasive tissue sampling using standardized clinical techniques
- Risks: Procedure-related pain, bleeding, infection, organ injury
- Risk Management: Operator expertise requirements, inclusion/exclusion criteria, monitoring protocols
Medication Washout Periods
- Objective: Establish baseline status or eliminate confounding treatment effects
- Methodology: Supervised discontinuation of therapeutic medications
- Risks: Disease exacerbation, withdrawal symptoms, functional decline
- Risk Management: Medical supervision, rescue medications, stopping rules
Monitoring and Safety Oversight Requirements
Tiered Monitoring Framework
The National Institute of Mental Health (NIMH) guidance establishes a tiered monitoring framework based on risk level [84]. For greater-than-minimal risk research without direct benefit, monitoring requirements include:
Table 3: Monitoring Requirements Based on Risk Level
| Risk Level | Monitoring Entities | Reporting Requirements | Additional Oversight |
|---|---|---|---|
| Greater than Minimal Risk | PI, IRB | Serious adverse events within 7 days; annual progress reports | Independent Safety Monitor for blinded studies [84] |
| Significantly Greater than Minimal Risk | PI, IRB, NIMH-constituted DSMB | Immediate reporting of deaths; serious adverse events within 7 days | NIMH-constituted Data and Safety Monitoring Board [84] |
Data and Safety Monitoring Plans (DSMPs)
All greater-than-minimal risk research requires a comprehensive Data and Safety Monitoring Plan (DSMP) that addresses [84]:
- Monitoring responsibilities and reporting relationships
- Adverse event definitions, documentation, and reporting procedures
- Stopping rules and protocol suspension criteria
- Data quality assurance processes
- Periodic review schedules and endpoints
For multi-site trials or studies with significantly greater than minimal risk, an independent Data and Safety Monitoring Board (DSMB) is required to provide ongoing oversight of safety and efficacy data [84].
Ethical Framework Implementation
- Belmont Report Principles Checklist: Systematic tool for applying respect for persons, beneficence, and justice to protocol design
- Informed Consent Documentation Template: Structured approach to communicating absence of direct benefit and research risks
- Vulnerable Population Assessment Guide: Framework for identifying and implementing additional protections
- Institutional Review Board (IRB) Submission Guidelines: Institution-specific requirements for greater-than-minimal risk protocols
- FDA Code of Federal Regulations (21 CFR 50/56): Regulations governing informed consent and IRB requirements
- Office for Human Research Protections (OHRP) Guidance: Interpretive documents on assessing and minimizing research risks
Risk Assessment and Monitoring Tools
- Risk-Benefit Analysis Worksheet: Structured approach to quantifying and justifying research risks
- Data and Safety Monitoring Plan Template: Framework for developing protocol-specific monitoring plans
- Adverse Event Reporting System: Standardized processes for documenting and reporting unanticipated problems
Decision Framework for Protocol Implementation
The following diagram illustrates the systematic approach to implementing greater-than-minimal risk research without direct benefit:
Managing risks in greater-than-minimal risk research without direct benefit requires meticulous attention to ethical principles, regulatory requirements, and participant protections. By anchoring protocols firmly within the Belmont Report's framework of respect for persons, beneficence, and justice, researchers can justify the social value of such studies while implementing robust safeguards. The ethical legitimacy of these research endeavors depends on comprehensive risk assessment, enhanced monitoring, transparent informed consent, and equitable participant selection. Through systematic application of these principles and procedures, the research community can advance scientifically valuable knowledge while maintaining the highest standards of human subjects protection.
Addressing Coercion and Undue Influence in Participant Recruitment
The ethical integrity of scientific inquiry hinges on the voluntary participation of human subjects, a principle enshrined in the Belmont Report's foundational framework. This technical guide examines the critical challenges of coercion and undue influence within participant recruitment, contextualized through the Belmont principles of Respect for Persons, Beneficence, and Justice [3]. Despite robust regulatory frameworks, Institutional Review Boards (IRBs) frequently grapple with defining and applying these concepts consistently, often relying on "gut feelings" when assessing research protocols [85]. The recruitment phase represents the initial point of contact between researchers and potential participants, making it particularly vulnerable to ethical compromises that can undermine informed consent and voluntariness. This whitepaper provides researchers, scientists, and drug development professionals with evidence-based methodologies to identify, assess, and mitigate these ethical risks throughout the recruitment lifecycle, ensuring both regulatory compliance and the preservation of participant autonomy.
Theoretical Framework: The Belmont Principles in Recruitment
Foundational Ethical Principles
The Belmont Report establishes three core principles that directly inform ethical recruitment practices [3]:
Respect for Persons: This principle acknowledges the autonomy of individuals and requires that participation be voluntary and informed. It demands protection for those with diminished autonomy, ensuring they are not exploited or coerced. In recruitment, this translates to conditions free from coercion and undue influence, where prospective participants can make independent decisions without pressure [3] [86].
Beneficence: This principle extends beyond "do no harm" to an obligation to maximize potential benefits and minimize possible harms. During recruitment, researchers must carefully balance the appeal of participation against potential risks, ensuring that attractive incentives do not cloud a participant's judgment about risks involved [3] [87].
Justice: The principle of Justice requires equitable selection of participants, ensuring that the burdens and benefits of research are distributed fairly [3]. Recruitment strategies must not systematically target vulnerable populations simply because of their availability or compromised position, nor should they unduly exclude groups that might benefit from participation [3].
Defining Coercion and Undue Influence
Operationalizing the Belmont principles requires clear distinctions between coercion and undue influence, though IRBs often use these terms interchangeably in practice [85].
Coercion occurs when "an overt threat of harm is intentionally presented by one person to another in order to obtain compliance" [86] [88]. This represents the more extreme form of inappropriate influence, where participation is secured through explicit or implicit threats of negative consequences for non-participation [88].
Undue Influence arises "through an offer of an excessive, unwarranted, inappropriate, or improper reward or other overture to obtain compliance" [86] [88]. The crucial distinction lies in coercion employing threats of harm, while undue influence utilizes excessive inducements that may overwhelm a person's ability to weigh risks rationally [88].
Table 1: Distinguishing Coercion from Undue Influence
| Characteristic | Coercion | Undue Influence |
|---|---|---|
| Mechanism | Threat of harm or penalty | Offer of excessive or inappropriate reward |
| Participant Psychology | Fear of negative consequences | Overwhelmed desire for benefit leading to risk discounting |
| Common Contexts | Power-imbalanced relationships (teacher-student, doctor-patient) | Financial incentives disproportionate to risk or burden |
| Regulatory Focus | Absolute prohibition | Context-dependent evaluation of appropriateness |
Quantitative Assessment of Ethical Risks in Recruitment
Empirical Data on IRB Decision-Making
Research into IRB approaches reveals significant variations in how ethical challenges are addressed. A qualitative study interviewing 46 IRB leaders, directors, administrators, and members from 34 top U.S. research institutions found that IRBs "often use these terms synonymously and define undue inducement in varying ways, often wrestling with these issues, relying on 'gut feelings', and seeking compromises" [85]. This ambiguity creates inconsistency in protocol reviews, particularly regarding participant compensation.
Table 2: IRB Considerations for Participant Compensation
| Compensation Model | Key Characteristics | Ethical Strengths | Ethical Concerns |
|---|---|---|---|
| Wage Payment Model | Standardized wage, potentially increased for uncomfortable tasks | Prevents exploitation, transparent calculation | May still be excessive for vulnerable populations |
| Market Model | Based on supply and demand, higher payment for greater risk | Efficient recruitment for difficult studies | Potentially undermines risk evaluation, creates inequity |
| Reimbursement Model | Covers expenses and costs from missed work | Prevents financial loss from participation | May not adequately value participant time and contribution |
Statistical Analysis of Recruitment Practices
Analysis of recruitment methodologies indicates concerning trends in how incentives operate across different populations. Research into online recruitment for diabetes and depression studies shows that compensation offers are common, though most journal articles fail to report whether or how much participants were compensated, creating transparency issues in the literature [85]. The economic circumstances of prospective participants significantly influence how attractive standard compensation amounts appear, creating variable vulnerability to undue influence across socioeconomic groups [87].
Methodological Protocols for Ethical Recruitment
Recruitment Workflow with Ethical Safeguards
The following diagram illustrates a systematic approach to integrating ethical safeguards throughout the recruitment process:
Recruitment Workflow with Ethical Safeguards
This workflow demonstrates the integration of ethical considerations at critical decision points, ensuring continuous alignment with Belmont principles throughout recruitment implementation.
Special Population Protocols
Student Recruitment Protocol
Research involving student populations requires specific safeguards against coercion due to inherent power differentials [86] [89]:
Requirement vs. Option: Students cannot be required to participate in research to meet a course or degree program requirement, as this constitutes coercion through threat of academic penalty [86]. A comparable non-research alternative must always be provided [86] [89].
Alternative Equivalency: Non-research alternatives should require approximately the same time and effort as research participation and provide identical credit/extra credit amounts to avoid undue influence [86]. Examples include reading journal articles and answering questions, writing short papers on comparable research, or attending relevant colloquia [89].
Recruitment Transparency: Students should be recruited from broad pools beyond an investigator's own classes, and all students must be allowed to withdraw without penalty at any point [86].
Financial Compensation Protocol
Financial incentives represent one of the most complex areas for avoiding undue influence [85] [87]:
Compensation Justification: Researchers must justify both the compensation model and level to the IRB, with incentives aligned to time commitment and not so attractive as to encourage reckless disregard of risks [87].
Structural Equity: Equal compensation for equal participation should be the norm, though differential compensation may be justified by differing time commitments or cultural expectations [87].
Lottery Implementation: When using lotteries, participants must not pay to enter, odds of winning must be disclosed, and skill-testing questions should be incorporated to comply with state laws [87] [86].
Table 3: Research Reagent Solutions for Ethical Recruitment
| Tool/Resource | Primary Function | Implementation Guidance |
|---|---|---|
| IRB Consultation | Protocol review and approval | Engage early in study design; address power imbalances and compensation models [85] [87] |
| Informed Consent Documentation | Ensure voluntary participation | Present comprehensive study information; emphasize voluntary participation and right to withdraw [3] [86] |
| Alternative Activity Bank | Provide non-research alternatives | Maintain repository of equivalent activities for student populations (e.g., academic papers, writing assignments) [89] |
| Compensation Calculator | Determine appropriate payment | Incorporate wage payment model with adjustments for discomfort, time, and participant burden [85] |
| Third-Party Recruiter Guidelines | Manage external recruitment relationships | Establish clear boundaries: third parties may not determine eligibility or receive finder's fees [89] |
Advanced Implementation Frameworks
Digital Recruitment Ethics Protocol
Contemporary research increasingly utilizes digital platforms for participant recruitment, introducing novel ethical considerations [89]:
Platform Appropriateness: Electronic recruitment materials must be clearly identified as voluntary research and not mistaken for employment opportunities [89]. Ads on platforms like Craigslist must appear on volunteer pages, not job listings [89].
Teaser Ad Implementation: When platform restrictions prevent full disclosure, teaser ads may be used but must link to landing pages containing all required recruitment information [89]. Teasers cannot transfer participants directly to consent processes [89].
Crowdsourcing Compliance: Crowdsourcing platforms must permit HRPP/IRB review and approval of recruitment materials [89]. Platforms not allowing such review cannot be used for human subjects research [89].
Third-Party Recruitment Decision Framework
The following diagram outlines the ethical decision process for engaging third-party recruiters:
Third-Party Recruitment Decision Framework
This framework highlights critical control points for maintaining ethical standards when utilizing external recruiters, emphasizing prohibitions against finder's fees and inappropriate information sharing [89].
Addressing coercion and undue influence in participant recruitment requires continuous ethical vigilance grounded in the Belmont principles. While regulatory frameworks provide necessary structure, authentic protection of participant autonomy demands researcher commitment to reflective practice and proactive safeguarding. The methodologies and protocols outlined in this technical guide equip research professionals with evidence-based strategies to navigate complex recruitment ethics across diverse populations and research contexts. By implementing systematic approaches to compensation design, power differential management, and recruitment process transparency, the scientific community can uphold the fundamental ethical commitment to voluntary participation while advancing valuable knowledge through human subjects research.
In the field of human subjects research, the digital age has introduced unprecedented capabilities for data collection, storage, and analysis. While these technological advances offer powerful research opportunities, they simultaneously amplify ethical responsibilities regarding privacy and confidentiality. This guide frames these responsibilities within the enduring ethical principles established by the Belmont Report—Respect for Persons, Beneficence, and Justice—providing a moral compass for researchers and drug development professionals navigating complex digital data landscapes [90]. The proper management of sensitive information is not merely a regulatory hurdle but a fundamental ethical obligation, with inadequate protections risking serious harms to participants, including psychological, social, financial, and legal consequences [91].
Ethical Foundations: The Belmont Report in Digital Context
The Belmont Report's three principles provide the foundational framework for evaluating ethical data management practices in human subjects research.
Core Ethical Principles
| Belmont Principle | Definition | Application to Data Management |
|---|---|---|
| Respect for Persons | Recognizes individual autonomy and requires protection for those with diminished autonomy [90]. | Implement robust informed consent processes that clearly explain data collection, usage, storage, and sharing practices. Respect participant preferences regarding their data [6]. |
| Beneficence | Obligates researchers to maximize benefits and minimize potential harms [90]. | Conduct thorough risk-benefit analyses related to data handling. Implement strong security measures to protect against data breaches and misuse, thereby minimizing harm [91]. |
| Justice | Requires fair distribution of the benefits and burdens of research [90]. | Ensure equitable selection of subjects and prevent the exploitation of vulnerable populations. Protect all participants, regardless of background, from data-related harms [90]. |
Operationalizing Principles Through Privacy and Confidentiality
Privacy and confidentiality serve as critical operational applications of the Belmont principles [91]. Privacy refers to an individual's right to control access to themselves and their personal information, which in research is protected by methods that safeguard subject privacy during study conduct and data collection [91]. Confidentiality pertains to the obligation to handle securely any personal information that is shared, ensuring it is kept secret unless the individual consents to its disclosure [91]. These protections fall within the ethical concept of beneficence, which focuses on maximizing benefits and minimizing potential harms [91].
Federal regulations explicitly require that research plans include "adequate provisions to protect the privacy of subjects and to maintain the confidentiality of data" [91]. The informed consent process must include a clear statement describing the extent to which confidentiality of records will be maintained [91].
Quantitative Data Analysis: Ethical Considerations and Methodologies
Ethical data management requires rigorous methodologies for handling quantitative research data while protecting participant interests.
Quantitative Data Analysis Framework
Quantitative data analysis involves examining numerical data using mathematical, statistical, and computational techniques to uncover patterns, test hypotheses, and support decision-making [92]. This process transforms raw numbers into meaningful, actionable insights while maintaining ethical obligations to research participants [93].
Data Collection and Preparation Methods:
- Source Identification: Determine data needed to answer research questions from surveys, experiments, observational studies, or existing datasets [93]
- Data Cleaning: Handle missing values, identify and treat outliers, transform variables, encode categorical variables, and remove duplicates [93]
- Quality Assurance: Ensure data accuracy and reliability before analysis to maintain research integrity [94]
Analytical Techniques:
- Descriptive Statistics: Summarize data using measures of central tendency (mean, median, mode) and dispersion (range, variance, standard deviation) [92]
- Inferential Statistics: Make generalizations from samples to populations using hypothesis testing, t-tests, ANOVA, and regression analysis [93]
- Predictive Modeling: Use machine learning algorithms to forecast outcomes while maintaining data security [93]
Ethical Quantitative Data Visualization
Visualizing quantitative data requires careful consideration of both clarity and ethical representation.
Ethical Data Visualization Workflow
Table: Quantitative Data Visualization Ethics
| Visualization Type | Common Use Cases | Ethical Considerations | Accessibility Requirements |
|---|---|---|---|
| Bar Charts | Comparing categories, showing proportions [94] | Ensure labels are accurate and scales are not misleading | Color contrast ≥ 3:1 for large text; provide text alternatives [95] |
| Line Charts | Displaying trends over time [94] | Represent data honestly without smoothing outliers inappropriately | Use patterns + colors; ensure sufficient contrast [96] |
| Scatter Plots | Showing relationships between variables [94] | Protect individual data points when they represent human subjects | Don't rely on color alone; use different markers [95] |
| Heatmaps | Visualizing data density or intensity [94] | Consider implications of displaying aggregated personal data | Colorblind-safe palettes; additional coding patterns [97] |
Implementing Ethical Data Protection Protocols
Privacy Protection Methodologies
Protecting participant privacy requires deliberate strategies throughout the research process:
- Private Research Environments: Conduct consent discussions and data collection in private settings to prevent unauthorized observation or eavesdropping [91]
- Minimal Data Collection: Collect only information essential to answering research questions to reduce privacy exposure [91]
- Discretionary Communications: Use non-specific language in emails, voicemails, and recruitment materials to avoid unintended disclosures [91]
- Participant Control: Explicitly inform participants during interviews or surveys that they may skip questions that make them uncomfortable [91]
Confidentiality Protection Protocols
Confidentiality protections must secure data throughout its lifecycle—from collection through storage, analysis, and eventual destruction [91].
Data Confidentiality Protection Framework
Table: Data Security Implementation Matrix
| Protection Method | Protocol Details | Application Context | Regulatory Considerations |
|---|---|---|---|
| Access Controls | Limit system and data access to authorized research personnel only [91] | Electronic records, biological specimens, paper files | Required by federal regulations for all human subjects research [98] |
| Encryption | Use encrypted email and secure servers for data transfer and storage [91] | Electronic data transmission, mobile devices, cloud storage | Essential for compliance with data security policies [91] |
| De-identification | Remove or code identifiers as soon as possible after collection [91] | Data sets for analysis, shared repositories, published findings | Balances research utility with confidentiality protection [91] |
| Certificates of Confidentiality | NIH-issued certificates protecting sensitive data from legal disclosure [91] | Research collecting highly sensitive information (illegal behaviors, health data) | Automatically issued for NIH-funded studies; available for others [91] |
Risk Assessment and Management
Researchers must identify and address potential privacy and confidentiality risks specific to their studies:
- Types of Risk: Potential harms include damage to financial standing, employability, educational advancement, reputation, or risk of criminal/civil liability [91]
- Contextual Vulnerability: Participants in studies involving illegal behaviors (e.g., drug use) or stigmatized conditions face heightened risks if confidentiality is breached [91]
- Mitigation Strategies: Implement data security plans, secure storage solutions, and data sharing protocols commensurate with identified risks [91]
Table: Research Reagent Solutions for Ethical Data Management
| Tool/Category | Specific Examples | Function in Ethical Data Management |
|---|---|---|
| Data Security Platforms | Encrypted servers, Secure cloud storage, Access control systems | Protect identifiable data from unauthorized access throughout research lifecycle [91] |
| Statistical Analysis Software | R, Python, SPSS, SAS [93] | Enable analysis while maintaining data integrity and implementing privacy-preserving techniques |
| Data Visualization Tools | ChartExpo, Tableau, Power BI [92] | Create clear, accurate, accessible representations of data without disclosing identities |
| Informed Consent Platforms | Electronic consent systems, IRB templates [90] | Facilitate transparent participant communication and document consent appropriately |
| Regulatory Compliance Resources | IRB protocols, Certificate of Confidentiality applications [98] | Ensure adherence to federal regulations and institutional policies governing human subjects |
The increasing digitization of research data demands heightened vigilance in upholding the ethical principles of Respect for Persons, Beneficence, and Justice. By implementing robust privacy and confidentiality protections—including secure data handling protocols, appropriate technical safeguards, and transparent participant communications—researchers can harness the power of digital data while maintaining their fundamental ethical obligations to research participants. This integration of strong ethical frameworks with rigorous technical protocols ensures that scientific progress does not come at the expense of individual rights and welfare.
Strategies for Ongoing Ethical Vigilance During Long-Term Studies
Long-term studies are fundamental to advancing knowledge in fields like epidemiology, pharmacology, and social science, yet their extended duration introduces complex ethical challenges that brief research projects may not face. The Belmont Report's ethical principles—Respect for Persons, Beneficence, and Justice—established a foundational framework for human subjects research [99]. However, maintaining fidelity to these principles over months, years, or even decades requires proactive, dynamic systems of ethical vigilance rather than static, one-time reviews. Ongoing ethical vigilance refers to the continuous, systematic processes implemented throughout a study's lifecycle to identify, monitor, and address ethical issues as they evolve. This is particularly critical as research protocols, participant circumstances, and societal contexts inevitably change over time [100]. This guide provides researchers, scientists, and drug development professionals with a comprehensive framework and practical methodologies for implementing robust ethical vigilance systems that protect participant rights and welfare while ensuring scientific integrity throughout long-term studies, all within the foundational context of Belmont Report principles.
Ethical Foundations: The Belmont Report as a Living Framework
The Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research was created specifically to address historical failures in research ethics, most notably the Tuskegee Syphilis Study [99] [28]. Its three core principles provide the moral compass for all human subjects research, but their application requires special consideration in long-term contexts.
Core Principles and Longitudinal Applications
Respect for Persons: This principle acknowledges the autonomy of individuals and requires protecting those with diminished autonomy. In practice, it manifests through the informed consent process. In long-term studies, a single, initial consent is often insufficient to truly respect autonomy, as research objectives, procedures, and risks may evolve, and a participant's capacity or understanding may change [100]. This necessitates a dynamic consent approach where communication is ongoing and consent is perceived as a process rather than a one-time event [100].
Beneficence: This principle obligates researchers to maximize possible benefits and minimize potential harms. The ethical application of Beneficence requires a proactive and continuous assessment of the risk-benefit profile throughout the study [99] [28]. A risk that was deemed minimal at a study's outset could become significant due to changes in medical knowledge or a participant's health status. Furthermore, the duty to maximize benefits requires researchers to consider how to return value to participants over the long term, such as by sharing meaningful findings.
Justice: The principle of Justice demands the fair distribution of the benefits and burdens of research. It requires ethical scrutiny in the selection of study subjects to avoid systematically selecting some populations (e.g., the economically disadvantaged, racial minorities) simply because of their availability or compromised position [28] [15]. In long-term studies, vigilance is required to ensure that the burden of continued participation does not fall unfairly on certain groups and that the benefits of the research (e.g., access to a new therapy) are justly distributed as the study progresses.
From Principle to Practice: The Challenge of Vulnerability
Vulnerability is a central concept in research ethics, and the Belmont Report states that "persons with diminished autonomy are entitled to protection" [15]. A key insight for long-term studies is that vulnerability is not a static, categorical trait but a dynamic, contextual state [15]. A participant who is fully autonomous at enrollment may become vulnerable due to declining health, cognitive changes, or shifting life circumstances (e.g., job loss, divorce) during the study. Therefore, ethical vigilance requires continuous monitoring for emergent vulnerabilities. Two key conceptual models for understanding vulnerability are detailed below.
Table: Approaches to Assessing Vulnerability in Research Participants
| Approach | Core Concept | Key Vulnerabilities Addressed | Limitations | Safeguard Examples |
|---|---|---|---|---|
| Categorical | Identifies predefined groups as vulnerable [15]. | Children, prisoners, pregnant women, cognitively impaired persons [101]. | Can be overly rigid; fails to account for individual differences and situational changes [15]. | Regulatory subparts (e.g., 45 CFR §46 Subparts B-D); use of surrogate decision-makers [15]. |
| Contextual | Views vulnerability as fluid and situation-dependent [15]. | Cognitive/Communicative: Diminished capacity, language barriers.Institutional: Hierarchical control (prisons, military).Deferential: Informal power imbalances (doctor-patient) [15]. | Requires more nuanced, continuous assessment by investigators and IRBs. | Staged consent processes; independent advocates; objective capacity assessments; delayed enrollment [15]. |
Pillars of Ongoing Ethical Vigilance: A Systems Approach
Sustaining ethical integrity in long-term studies requires moving beyond initial IRB approval to implement an interconnected system of vigilance. This system rests on four key pillars, each containing specific strategies and protocols.
Dynamic Informed Consent and Communication
The traditional model of informed consent is often inadequate for long-term studies where the research landscape changes. Ethical vigilance requires implementing consent as a continuing dialogue.
Protocol for Dynamic Consent Methods: A dynamic consent framework utilizes digital platforms (e.g., secure web portals) to maintain an ongoing relationship with participants [100]. The methodology involves:
- Initial Tiered Consent: Present consent options at enrollment, allowing participants to choose their level of engagement (e.g., consent only for primary study, permission to be contacted for future sub-studies, preferences for receiving interim results).
- Continuous Communication: Provide regular, lay-friendly updates about study progress, preliminary findings, and any changes to the research team or direction.
- Re-consent Triggers: Establish clear protocols for seeking renewed consent when significant events occur, such as new safety information emerges, the study protocol is substantially amended, or the research focus expands beyond the original scope [100].
- Capacity Monitoring: In studies involving populations with potentially fluctuating or diminishing capacity, implement simple, standardized tools to periodically reassess understanding and willingness to continue.
Trust-Based Consent Model: Especially in long-term, large-scale cohort studies, the relationship between researcher and participant can be viewed through a trust-based model [100]. This emphasizes the need to establish and maintain trust and to balance comprehensive information disclosure with respect for participant autonomy. Key practices include enhancing institutional credibility, being transparent about data usage, and ensuring robust ethical oversight [100].
Continuous Monitoring and Oversight Structures
Oversight must be an active, ongoing process throughout the study's lifecycle, not a periodic or retrospective one.
Data Safety Monitoring Board (DSMB) Operations: A DSMB (or Data Monitoring Committee) is an independent group of experts that regularly reviews accumulating data from a clinical trial to ensure participant safety and study validity [101]. For long-term studies, the DSMB charter should specify:
- Meeting Frequency: Regular intervals (e.g., every 6 months) with clear triggers for ad-hoc reviews.
- Data Review Plans: Pre-specified interim analyses for efficacy and safety, using statistical stopping boundaries.
- Composition: Multidisciplinary membership (e.g., clinical experts, biostatisticians, bioethicists).
Enhanced Institutional Review Board (IRB) Review: IRBs should mandate full- scheduled continuing reviews for long-term studies involving vulnerable populations [101]. The review should go beyond administrative checklists to examine:
- Cumulative data on adverse events and protocol deviations.
- Participant withdrawal rates and reasons for withdrawal.
- Updates on the risk-benefit profile based on interim findings.
- Effectiveness of current consent and communication strategies.
Real-Time Data Vigilance Systems: Leverage modern Electronic Data Capture (EDC) systems to build ethics into the data workflow.
- Centralized Monitoring: Use EDC systems like REDCap (which is 21 CFR Part 11 compliant) to remotely monitor data quality and protocol compliance across multiple sites in near real-time [102].
- Quality Control Triggers: Program automated queries for missing data, inconsistent entries, and off-schedule visits to promptly identify and rectify issues that could affect participant safety or data integrity [102].
- Audit Trails: Maintain and periodically review electronic logs that track who entered or altered data and when, ensuring accountability [102].
Proactive Data Stewardship and Security
Long-term studies accumulate vast amounts of sensitive data, making robust, forward-looking data management a core ethical obligation aligned with the principle of Beneficence.
Data Management Plan (DMP) Implementation: A comprehensive DMP is critical for effective data stewardship [102]. For a long-term study, the DMP must be a living document that details:
- Data Collection Tools: Prefer electronic case report forms (eCRFs) over paper forms to reduce errors, ease data sharing, and enhance security [102].
- De-identification Protocols: A plan for removing Protected Health Information (PHI) as soon as possible after collection, with a secure, separate key for re-identification if necessary for follow-up [102].
- Long-term Storage and Retention: Policies for secure data storage after study completion, adhering to regulatory requirements (e.g., FDA may require records for 2+ years after marketing application; research with children may require storage until the youngest subject is 21) [102].
Security Compliance Framework: Data security must comply with a complex regulatory landscape that includes HIPAA (privacy), 21 CFR Part 11 (electronic records), and international standards like the GDPR [102]. Key strategies include:
- Using secure, validated platforms like REDCap that are designed to meet these regulations.
- Storing data only on encrypted, institution-managed servers or secure cloud services, never on personal devices.
- Implementing role-based access controls so that research personnel can only access the data necessary for their function [102].
Participant Retention and Disengagement Ethics
Maintaining an ethical relationship with participants includes how they are retained and how they exit the study.
Minimizing Burden and Maximizing Value: High participant burden is a primary cause of attrition and can itself be an ethical issue. Strategies to address this include:
- Designing streamlined follow-up procedures.
- Offering flexible visit schedules and remote data collection options (e.g., electronic surveys, wearable device integration).
- Providing participants with summaries of their own data or aggregated study findings to return value.
Ethical Withdrawal Protocols: Participants have the right to withdraw at any time without penalty. The protocol must clearly define what withdrawal means (e.g., cessation of interventions vs. cessation of data collection) and establish a process for respectfully disengaging, which may include a final follow-up for safety purposes.
Implementing the strategies outlined above requires a suite of practical tools and resources. The following table details key solutions for maintaining ethical vigilance.
Table: Essential Research Reagent Solutions for Ethical Vigilance
| Tool / Resource | Primary Function | Application in Ethical Vigilance | Key Features for Long-Term Studies |
|---|---|---|---|
| REDCap (Research Electronic Data Capture) | Electronic Data Capture (EDC) [102] | Securely collects and manages participant data; enables centralized monitoring and quality control. | 21 CFR Part 11, HIPAA, FISMA compliant; audit trails; data export for analysis; supports e-Consent [102]. |
| Dynamic Consent Platform | Participant Engagement & Re-consent | Manages ongoing consent process; facilitates participant communication and updates. | Tiered consent options; multi-modal communication (portal, email); re-consent trigger management [100]. |
| DSMB Charter & Procedures | Independent Safety Monitoring | Provides formal framework for ongoing risk-benefit assessment by external experts. | Pre-specified meeting schedule and statistical stopping rules; defined membership and responsibilities [101]. |
| Anonymous Whistleblower Service | Misconduct Reporting | Provides a safe, confidential channel for staff or participants to report ethical concerns. | Anonymity for reporters; 24/7 access; managed by experienced investigators to triage and address issues [103]. |
| Data Management Plan (DMP) | Data Stewardship Roadmap | Outlines lifecycle of data from collection to long-term storage; ensures regulatory compliance. | Details de-identification protocols; data sharing policies; security measures; retention schedules [102]. |
In long-term human subjects research, ethical compliance is not a destination reached at IRB approval but a continuous journey. The extended timelines of longitudinal studies introduce evolving risks and ethical challenges that demand a proactive, systematic approach to vigilance. By grounding this approach in the enduring principles of the Belmont Report—Respect for Persons, Beneficence, and Justice—and implementing the interconnected pillars of dynamic consent, continuous oversight, robust data stewardship, and ethical participant management, researchers can build and maintain the trust that is essential for meaningful scientific inquiry. This commitment to ongoing vigilance not only protects participants but also enhances the validity and integrity of the research itself, ensuring that long-term studies fulfill their promise to advance knowledge in an ethically sound manner.
The Belmont Report in Context: Enduring Relevance and Modern Challenges
The ethical conduct of research involving human subjects is a cornerstone of modern medicine and science. This integrity is underpinned by key historical documents that established the fundamental principles guiding researchers today. Among these, the Nuremberg Code and the Belmont Report stand as critical, yet distinct, pillars. The Nuremberg Code, born from the atrocities of the Second World War, established the non-negotiable necessity of voluntary consent. The Belmont Report, developed in response to ethical failures within the U.S. research system, provided a more flexible framework based on three core ethical principles. For researchers, scientists, and drug development professionals, understanding the nuances, applications, and evolution from the Nuremberg Code to the Belmont Report is essential for designing and conducting ethically sound research that protects participants while advancing scientific knowledge. This analysis frames their comparative attributes within the broader thesis that the Belmont Report's principles provide the adaptable, comprehensive ethical foundation necessary for the complex landscape of contemporary human subjects research.
Historical Context and Genesis
The circumstances that led to the creation of these two documents were markedly different, shaping their scope and tone.
2.1 The Nuremberg Code The Nuremberg Code emerged directly from the post-World War II Nuremberg Trials, specifically the "Doctors' Trial" (U.S. v. Brandt) [104] [105]. The judges presiding over the case of 23 Nazi doctors, who conducted brutal and often lethal experiments on concentration camp prisoners, were faced with the task of delimiting permissible medical experimentation [106] [104]. The defendants argued that no international law clearly differentiated between legal and illegal human experimentation [104]. In response, the court articulated a ten-point statement, now known as the Nuremberg Code, which was included in the 1947 verdict [104] [107]. Its primary aim was to prevent a recurrence of the egregious crimes committed under the guise of science, establishing a clear and uncompromising set of rules.
2.2 The Belmont Report The Belmont Report was commissioned in the United States over a quarter-century later, prompted by domestic ethical scandals rather than international war crimes. The most notorious of these was the U.S. Public Health Service Syphilis Study at Tuskegee, which from 1932 to 1972 observed the natural progression of untreated syphilis in Black men without their informed consent and while actively denying them effective treatment [108] [9]. Public exposure of this study in 1972 led to a national outcry, which in turn prompted the U.S. Congress to pass the National Research Act of 1974 [109] [108]. This Act created the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research, which was charged with identifying the basic ethical principles that should underlie research with human subjects [9]. After nearly four years of deliberation, the Commission produced the Belmont Report in 1979 [109] [9].
Table 1: Historical Context of the Nuremberg Code and the Belmont Report
| Feature | The Nuremberg Code | The Belmont Report |
|---|---|---|
| Year of Creation | 1947 [106] [104] | 1979 [109] [9] |
| Catalyzing Event | Nuremberg "Doctors' Trial" following WWII [104] [105] | Tuskegee Syphilis Study & other domestic ethical lapses [108] [9] |
| Creating Body | U.S. judges at the Nuremberg Military Tribunal [104] [105] | U.S. National Commission for the Protection of Human Subjects [109] [9] |
| Primary Impetus | Reaction to barbaric, state-sponsored atrocities [104] | Response to systemic ethical failures in domestic research [108] |
Core Ethical Principles and Frameworks
The Nuremberg Code and the Belmont Report differ fundamentally in their structure, moving from a set of direct rules to a framework of guiding principles.
3.1 The Nuremberg Code: A Set of Directives The Nuremberg Code is presented as ten concise points. The first and most famous principle absolutely mandates voluntary consent: "The voluntary consent of the human subject is absolutely essential" [106] [104]. It elaborates that this requires legal capacity to consent, free power of choice, and sufficient knowledge and comprehension to make an "enlightened decision" [106]. The other nine points provide specific directives related to the justification and conduct of research, including:
- Beneficence and Non-maleficence: The experiment should yield fruitful results for the good of society, be based on prior animal testing, avoid all unnecessary suffering, and not be conducted if there is reason to believe death or disabling injury may occur [106] [104] [18].
- Investigator Qualifications and Responsibility: The experiment must be conducted by qualified individuals who maintain high skill and care and who must terminate the experiment if they believe continuation is likely to result in injury or death [106].
- Subject Freedom: The human subject "should be at liberty" to end the experiment [106].
3.2 The Belmont Report: A Principle-Based Framework The Belmont Report identified three broad, comprehensive ethical principles that provide a framework for resolving ethical problems in research [109] [9]:
- Respect for Persons: This principle acknowledges the autonomy of individuals and requires protecting those with diminished autonomy. It embodies the practice of informed consent, whereby subjects must be given adequate information, must comprehend it, and must voluntarily agree to participate without coercion or undue influence [109] [3] [9].
- Beneficence: This principle extends beyond "do no harm" to an obligation to maximize possible benefits and minimize potential harms. It requires a systematic assessment of risks and benefits, ensuring that the research is justified based on a favorable risk-benefit ratio and that the risks are minimized [109] [108] [9].
- Justice: This principle addresses the equitable distribution of the burdens and benefits of research. It requires a fair selection of subjects, ensuring that vulnerable populations (e.g., welfare patients, racial minorities, prisoners) are not targeted for convenience nor systematically selected to bear risks while being excluded from the benefits of research [109] [108] [9].
The following diagram illustrates how these three principles from the Belmont Report are operationalized into applications that protect research subjects.
Belmont Principles and Applications
A Comparative Analysis: Application and Scope
The differences between the documents become most apparent when analyzing their practical application and scope, particularly regarding vulnerable populations and regulatory influence.
4.1 Approach to Vulnerability and Consent A critical distinction lies in how the two documents address individuals with diminished autonomy. The Nuremberg Code's strict requirement for voluntary consent from the subject themselves presents a challenge for research involving populations like children, adults with cognitive impairments, or emergency situations [28]. Its language does not explicitly accommodate legally authorized representatives.
In contrast, the Belmont Report directly addresses this by stating that individuals with diminished autonomy are "entitled to protection" [109] [9]. It acknowledges that Respect for Persons requires allowing third-party authorization (e.g., parental permission for children) while still respecting the individual through processes like assent [3]. This flexibility enables ethically justifiable research with populations that the Nuremberg Code would effectively exclude.
4.2 Regulatory and Legal Impact The Nuremberg Code was articulated as part of a legal verdict and was never officially adopted as law by any nation [104] [105]. Initially, it was largely dismissed by the medical establishment as a "code for barbarians" [104] [107]. However, its historical importance is monumental, as it served as the first major international document to provide a detailed statement on research ethics and laid the groundwork for all subsequent codes [104] [18] [105].
The Belmont Report, meanwhile, was created with the explicit purpose of influencing U.S. policy. It directly formed the ethical foundation for the U.S. Federal Policy for the Protection of Human Subjects (the "Common Rule", 45 CFR part 46) and FDA regulations [3] [18] [9]. Its principles are the standard taught to researchers and used by Institutional Review Boards (IRBs) to review and monitor research in the United States [108] [3].
Table 2: Comparative Analysis of Scope and Application
| Aspect | The Nuremberg Code | The Belmont Report |
|---|---|---|
| Primary Focus | Informed consent and protection from physical/mental harm [106] [104]. | Three comprehensive principles: Respect, Beneficence, Justice [109] [9]. |
| Nature of Document | A set of 10 specific directives [106]. | A framework of 3 ethical principles and their applications [109] [9]. |
| Vulnerable Populations | Does not explicitly address proxy consent, potentially excluding key groups [28]. | Explicitly requires protections for persons with diminished autonomy [109] [3]. |
| Regulatory Influence | Foundational moral influence; not officially codified as law [104] [105]. | Directly codified into U.S. federal regulations (Common Rule) [3] [9]. |
| Modern Relevance | Foundational, but limited by its rigidity and specific historical context. | The operational ethical framework for U.S. human subjects research [108] [3]. |
The Research Toolkit: Modern Ethical Safeguards
The principles of the Belmont Report are implemented through a system of institutional safeguards that form the modern researcher's operational environment for ethics.
Table 3: Key Institutional Safeguards for Human Subjects Research
| Safeguard | Primary Function | Relevance to Researcher |
|---|---|---|
| Institutional Review Board (IRB) | An independent committee that reviews, approves, and monitors research to protect the rights and welfare of human subjects [108]. | Researchers must submit their protocol to the IRB for approval before beginning any study involving human subjects and adhere to ongoing reporting requirements [108]. |
| Informed Consent Document | The practical application of the Respect for Persons principle. Ensures subjects receive all key information about the study in an understandable format [108] [9]. | Researchers are responsible for creating a comprehensive consent form and overseeing the consent process, ensuring it is voluntary and free of coercion [108]. |
| Data and Safety Monitoring Board (DSMB) | An independent group of experts that monitors patient safety and treatment efficacy data during a clinical trial, particularly in multi-center Phase III trials [108]. | The DSMB may recommend a trial be stopped early if risks outweigh benefits or efficacy is clearly demonstrated, a key function of Beneficence [108]. |
| Federal Regulations (Common Rule) | Codifies the Belmont Report principles into enforceable law for federally funded research [3] [9]. | Researchers and their institutions are legally bound to comply with these regulations, which govern IRB operations, consent, and subject selection [3]. |
The Nuremberg Code and the Belmont Report are inextricably linked yet fundamentally different documents in the history of research ethics. The Nuremberg Code stands as a powerful, reactive proclamation born of tragedy, establishing the inviolable principle of voluntary consent. Its limitations in addressing complex, real-world research scenarios involving diverse populations revealed the need for a more nuanced framework. The Belmont Report answered this need by articulating a principle-based structure of Respect for Persons, Beneficence, and Justice. This framework proved adaptable enough to be codified into regulation and to guide the ethical review of an immense variety of research, from behavioral studies to advanced gene therapy trials [28]. For today's researchers and drug development professionals, the Belmont Report is not an replacement for the Nuremberg Code, but rather its philosophical and practical evolution, providing the essential, living ethical compass for the ongoing and complex endeavor of human subjects research.
The ethical conduct of research involving human participants is governed by two seminal documents: the Belmont Report and the Declaration of Helsinki. While both aim to protect human subjects, they differ fundamentally in their origin, scope, and practical application. The Belmont Report, formulated in the United States, provides a philosophical framework of ethical principles intended to guide researchers and institutional review boards (IRBs) [108] [12]. In contrast, the Declaration of Helsinki, established by the World Medical Association (WMA), is a globally-oriented set of ethical guidelines primarily directed at physician-researchers in medical research [110] [51]. This whitepaper examines the distinctions between these two documents through the lens of the Belmont Report's principles, providing researchers, scientists, and drug development professionals with a clear understanding of their respective roles in shaping ethical research protocols.
Historical Context and Origins
The evolution of ethical guidelines for human subjects research has been significantly influenced by historical abuses, leading to the creation of both the Declaration of Helsinki and the Belmont Report.
Table: Historical Evolution of Key Ethical Guidelines
| Document | Year | Primary Trigger Event | Key Advancement |
|---|---|---|---|
| Nuremberg Code | 1947 | Nazi Medical Experiments | Established the absolute requirement for voluntary informed consent [111]. |
| Declaration of Helsinki | 1964 | Nuremberg Code's limitations | Expanded ethics for physician-researchers; introduced oversight by independent committees [112] [110]. |
| Belmont Report | 1979 | Tuskegee Syphilis Study | Identified three core ethical principles (Respect for Persons, Beneficence, Justice) as a framework for U.S. regulations [108] [12]. |
The Declaration of Helsinki (DoH) was adopted by the World Medical Association in 1964 as a direct response to the Nuremberg Code, aiming to provide a more comprehensive set of principles for the global medical community [110]. It has undergone multiple revisions, with the most recent update in 2024, to adapt to emerging ethical challenges such as biobanking and research in public health emergencies [113]. A key development was the 1975 revision, which introduced the requirement for review by an independent committee, a precursor to modern IRBs and Ethics Committees [112].
The Belmont Report has a more focused national origin. Its creation was mandated by the U.S. National Research Act of 1974 in direct response to the public exposure of the Tuskegee Syphilis Study, a 40-year research project that deliberately withheld treatment from African American men without their informed consent [108] [12]. The Belmont Report was designed to serve as the ethical foundation for subsequent U.S. federal regulations governing human subjects research [12].
Diagram: Historical Origins of Ethical Guidelines. The Declaration of Helsinki and the Belmont Report emerged from distinct historical events and ethical lineages.
Core Philosophical Frameworks and Principles
The Belmont Report and the Declaration of Helsinki are built upon different philosophical foundations, which directly influence their structure and application.
The Belmont Report's Ethical Principles
The Belmont Report organizes its guidance around three comprehensive ethical principles that provide an analytical framework for resolving ethical problems in research [114] [108] [12]:
- Respect for Persons: This principle acknowledges the autonomy of individuals and requires that subjects with diminished autonomy (e.g., children, prisoners, those with cognitive impairments) are entitled to special protections. It demands that participation in research is voluntary and informed [12].
- Beneficence: This principle extends beyond the concept of "do no harm" to an obligation to maximize possible benefits and minimize potential risks. It requires a systematic, objective assessment of the risks and benefits of the proposed research [108] [12].
- Justice: This principle addresses the fair distribution of the burdens and benefits of research. It demands that the selection of subjects be scrutinized to avoid systematically recruiting groups based on their ease of availability, manipulability, or compromised position, rather than on reasons directly related to the problem being studied [108] [12].
The Declaration of Helsinki's Physician-Oriented Guidelines
The Declaration of Helsinki, in contrast, is structured as a set of recommendations for physicians, emphasizing their specific duties to research participants [110] [115]. Its core tenets include [112] [110]:
- Primacy of participant well-being: "The well-being of the individual research subject must take precedence over all other interests" [112].
- Scientific validity and rationale: Research must be based on a thorough knowledge of the scientific literature and adequately performed laboratory and animal experimentation [110].
- Independent committee review: Every experimental protocol must be submitted to an independent ethics committee for review [112] [110].
- Informed consent: While central, it is situated within the broader context of the physician-researcher's responsibility to the participant [110].
Table: Comparative Analysis of Core Principles and Focus
| Aspect | Belmont Report | Declaration of Helsinki |
|---|---|---|
| Primary Audience | Researchers, IRBs, and policymakers [116]. | Physicians and the global medical community [110]. |
| Nature of Guidance | A philosophical framework of principles to analyze ethical dilemmas [108]. | A set of prescriptive, actionable guidelines for medical research [116]. |
| Geographic Origin & Influence | United States; foundation for U.S. federal regulations (Common Rule) [12]. | Global (World Medical Association); international gold standard for medical journal editors [116] [110]. |
| Central Focus | Principles of autonomy, risk-benefit calculus, and equitable subject selection [108]. | Physician's duty to safeguard participant health and the integrity of medical research [110] [115]. |
Application in Research Protocols
The distinctions in philosophy lead to tangible differences in how these documents are applied within research protocols, particularly concerning informed consent, risk/benefit assessment, and subject selection.
Informed Consent
- Belmont Report Application: The principle of Respect for Persons is applied through a rigorous informed consent process that emphasizes three key elements: Information, Comprehension, and Voluntariness [108] [12]. The report details the information that must be disclosed and pays special attention to ensuring the subject comprehends the information and that their agreement is free of coercion or undue influence [12].
- Declaration of Helsinki Application: While also requiring informed consent, the DoH places the ultimate responsibility for the participant's well-being on the physician-investigator, stating that this responsibility "must always rest with a medically qualified person and never rest on the subject of the research, even though the subject has given his or her consent" [115]. The 2024 revision further emphasizes "meaningful engagement with potential and enrolled participants and their communities" [113].
Assessment of Risks and Benefits
- Belmont Report Application: The principle of Beneficence is directly applied through a systematic risk/benefit assessment [108] [12]. Researchers and IRBs must rigorously assess and document that risks are justified by the potential benefits to the subject or the importance of the knowledge gained, and that risks are minimized [12].
- Declaration of Helsinki Application: The DoH states that "biomedical research involving human subjects cannot legitimately be carried out unless the importance of the objective is in proportion to the inherent risk to the subject," and that "concern for the interests of the subject must always prevail over the interests of science and society" [115]. It includes specific, sometimes controversial, provisions regarding the use of placebos and post-trial access to beneficial interventions [112] [110].
Selection of Subjects
- Belmont Report Application: The principle of Justice is applied through the fair selection of subjects [108]. This requires scrutiny of the recruitment process to ensure that vulnerable populations are not selected for risky research merely for administrative convenience, and that the benefits of research are not denied to eligible populations without good reason [12].
- Declaration of Helsinki Application: The DoH calls for the special protection of vulnerable populations and recognizes that vulnerability can be contextual and dynamic [113]. It emphasizes that research is only justified if the population the research is aimed at stands to benefit from its results [110].
The Scientist's Toolkit: Operationalizing Ethics in Research
For researchers and drug development professionals, translating ethical principles into practice requires specific tools and procedures. The following table outlines key components for ensuring compliance with the ethical standards derived from both the Belmont Report and the Declaration of Helsinki.
Table: Essential Components for Ethical Research Protocol Implementation
| Component | Function & Purpose | Ethical Principle Served |
|---|---|---|
| Institutional Review Board (IRB)/Independent Ethics Committee (IEC) | An independent committee that reviews, approves, and monitors research protocols to protect the rights and welfare of human subjects [51]. | Beneficence, Justice (Belmont); Independent Review (Helsinki) |
| Informed Consent Form (ICF) | A document that ensures participants receive all necessary information about the study, comprehend it, and provide voluntary agreement to participate [108] [12]. | Respect for Persons (Belmont) |
| Research Protocol & Investigator's Brochure | The detailed plan for the research, providing the scientific rationale, methodology, and risk/benefit profile to justify the study's ethical validity [110]. | Beneficence (Belmont); Scientific Validity (Helsinki) |
| Data Safety Monitoring Board (DSMB) | An independent group of experts that monitors patient safety and treatment efficacy data during a clinical trial, particularly in Phase III studies [108]. | Beneficence (Belmont) |
| Vulnerable Population Safeguards | Additional protective procedures for participants with diminished autonomy (e.g., assent from children, consent from legally authorized representatives) [51] [12]. | Respect for Persons, Justice (Belmont) |
Diagram: Ethical Research Workflow. This flowchart outlines the key stages of a research protocol, highlighting critical points for ethical review and intervention to protect participants.
The Belmont Report and the Declaration of Helsinki, while sharing the common goal of protecting human research participants, serve distinct yet complementary roles. The Belmont Report provides the foundational ethical principles that form the analytical backbone of U.S. research regulations, guiding IRBs and researchers in their ethical deliberations [116] [108]. The Declaration of Helsinki offers a globally-oriented, practical set of guidelines for physician-researchers, emphasizing the welfare of the participant and the integrity of medical research [116] [110]. For today's researchers and drug development professionals, a thorough understanding of both documents is not merely a regulatory requirement but a fundamental aspect of scientific integrity. Successfully navigating their distinctions in scope and application ensures that the pursuit of scientific knowledge remains firmly rooted in the ethical treatment of every human participant.
The Belmont Report's Influence on FDA and ICH-GCP Regulations
The Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research, published in 1979, represents a foundational document in the history of research ethics. Created by the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research in response to ethical abuses in research, most notably the Tuskegee Syphilis Study, the report established three fundamental ethical principles that would forever change the landscape of human subjects research [117] [9]. Despite never being formally adopted as official policy by the Department of Health, Education, and Welfare (now the Department of Health and Human Services), the Belmont Report has become the primary ethical framework for protecting human research subjects in the United States and has exerted considerable influence internationally [117] [28].
This whitepaper examines the direct and indirect influence of the Belmont Report's principles on two critical regulatory frameworks: the U.S. Food and Drug Administration (FDA) regulations and the International Council for Harmonisation (ICH) Good Clinical Practice (GCP) guidelines. For drug development professionals and researchers, understanding this ethical lineage is crucial not only for regulatory compliance but for internalizing the moral imperatives that underpin ethical clinical research.
The Belmont Report's Ethical Framework
Historical Context and Creation
The National Commission for the Protection of Human Subjects was established by the National Research Act of 1974 [10] [9]. The Commission's mandate was to identify the basic ethical principles that should underlie the conduct of biomedical and behavioral research involving human subjects and to develop guidelines to ensure that such research is conducted in accordance with those principles [10]. The report, named after the Belmont Conference Center where it was drafted, was the product of nearly four years of deliberations, including an intensive four-day discussion period in February 1976 [9].
The Three Core Ethical Principles
The Belmont Report organizes its framework around three overarching principles that provide a moral foundation for research ethics.
Respect for Persons
This principle acknowledges the autonomy of individuals and requires that individuals with diminished autonomy be entitled to protection. It encompasses two ethical convictions: first, that individuals should be treated as autonomous agents capable of making their own decisions; and second, that persons with diminished autonomy (due to youth, illness, disability, or other circumstances) are entitled to additional protections [117] [9]. In practice, this principle finds its primary application in the requirement for informed consent, which must include adequate information, comprehension by the subject, and voluntariness free from coercion or undue influence [117].
Beneficence
This principle extends beyond the simple maxim "do no harm" to an affirmative obligation to maximize possible benefits and minimize potential harms [117] [9]. The principle of beneficence requires researchers and the research system to protect human subjects from harm by ensuring their well-being through a systematic assessment of risks and benefits associated with the research. This involves a careful analysis of the research methodology to determine whether the potential benefits justify the risks to which subjects will be exposed [117].
Justice
The principle of justice addresses the fair distribution of the burdens and benefits of research [117] [9]. It demands that the selection of research subjects be scrutinized to avoid systematically selecting some populations (e.g., the economically disadvantaged, institutionalized persons, or racial and ethnic minorities) simply because of their availability, manipulability, or compromised position, rather than for reasons directly related to the research problem [117]. This principle was formulated in direct response to historical injustices such as the Tuskegee Syphilis Study, where disadvantaged rural African American men were exploited as research subjects [118].
Practical Applications
The Belmont Report translates these three ethical principles into three primary applications for the conduct of research:
- Informed Consent: The practical application of Respect for Persons, requiring information, comprehension, and voluntariness [117] [9].
- Assessment of Risks and Benefits: The practical application of Beneficence, requiring a systematic analysis [117] [9].
- Selection of Subjects: The practical application of Justice, requiring a fair and non-exploitative process [117] [9].
Direct Influence on U.S. Federal Regulations
The Common Rule
While the Belmont Report itself is not a regulation, its principles directly informed the Federal Policy for the Protection of Human Subjects, commonly known as the Common Rule (45 CFR Part 46) [9]. Initially adopted by multiple federal departments and agencies in 1991, the Common Rule establishes the baseline requirements for human subjects research conducted or supported by federal agencies [9]. The influence of the Belmont Report was formally recognized in the 2017 revisions to the Common Rule, which instituted the report as part of the federal policy for human subjects protection [9].
FDA Regulations
The FDA has explicitly incorporated the principles of the Belmont Report into its human subject protection regulations. The agency's regulations for Informed Consent (21 CFR Part 50) and Institutional Review Boards (21 CFR Part 56) directly reflect the applications outlined in the Belmont Report [117] [119].
The FDA's history reveals a conscious effort to harmonize its regulations with ethical principles. In the preamble to the 1981 final rules establishing 21 CFR Part 50, the FDA explained that the regulations were intended to implement recommendations of the National Commission and to harmonize with HHS rules, adopting "a single standard that reflected both the most current congressional thinking on informed consent and the important ethical principles and social policies underlying the doctrine of consent" [119].
Table: Correspondence Between Belmont Report Principles and FDA Regulations
| Belmont Report Principle | Belmont Application | FDA Regulation | Regulatory Requirement |
|---|---|---|---|
| Respect for Persons | Informed Consent | 21 CFR Part 50 | Mandates informed consent process and documentation; specifies essential elements of consent |
| Beneficence | Assessment of Risks and Benefits | 21 CFR 56.111 | Requires IRB to ensure risks are minimized and reasonable in relation to anticipated benefits |
| Justice | Selection of Subjects | 21 CFR 56.111 | Mandates equitable selection of subjects, with special protections for vulnerable populations |
The FDA has also created narrow exceptions to informed consent requirements for emergency research under 21 CFR 50.24, which includes specific safeguards that reflect Belmont principles, such as community consultation and public disclosure [119]. This exception demonstrates how the ethical framework can accommodate necessary research while maintaining core protections.
Influence on International Guidelines: ICH Good Clinical Practice
Historical Evolution of ICH GCP
The International Council for Harmonisation (ICH) developed the Good Clinical Practice (GCP) guidelines to create a unified standard for the design, conduct, recording, and reporting of clinical trials involving human subjects across international jurisdictions [120] [118]. The evolution of these guidelines traces back through the same ethical milestones that preceded the Belmont Report, including the Nuremberg Code (1947) and the Declaration of Helsinki (1964) [118] [121]. The ICH E6 GCP guideline, first adopted in 1996 (R1) and revised in 2016 (R2), has served as the global benchmark for clinical trial quality and ethics [120].
ICH E6(R3) and the Modernization of GCP
The latest revision, ICH E6(R3), represents the most significant overhaul of the GCP guidelines since their inception [122]. Finalized in 2025, E6(R3) introduces a more principles-based approach that aligns closely with the ethical framework established by the Belmont Report decades earlier [120] [122]. The updated guideline is structured around an overarching principles document with annexes for specific trial types, emphasizing flexibility and ethical conduct in increasingly complex research environments [120].
Table: Belmont Principles in ICH E6(R3) Implementation
| Belmont Principle | Manifestation in ICH E6(R3) | Practical Application in Modern Trials |
|---|---|---|
| Respect for Persons | Enhanced informed consent processes, including eConsent and dynamic consent | Supports remote consent processes, multimedia explanations, and ongoing consent management |
| Beneficence | Formalized risk-based quality management and Quality by Design | Promotes proactive identification of critical-to-quality factors and proportionate risk control |
| Justice | Strengthened ethical considerations for participant equity and vulnerable populations | Addresses barriers to participation and ensures appropriate inclusion of diverse populations |
Enduring Ethical Foundation
While the ICH GCP guidelines do not explicitly reference the Belmont Report, they operationalize its core principles within an international context. The University of Colorado's Multiple Institutional Review Board (COMIRB) explicitly states that its actions "will be guided by the principles of respect for persons, beneficence, and justice set forth in the Ethical Principles and Guidelines for the Protection of Human Subjects of Research (often referred to as the Belmont Report)" [123]. This demonstrates how the Belmont framework continues to guide institutional review processes that operate under both FDA and ICH GCP standards.
The E6(R3) updates related to participant protection, including modernized informed consent practices and additional safeguards for vulnerable participants, directly reflect the Belmont principles of Respect for Persons and Justice [122]. Similarly, the emphasis on data integrity and cybersecurity within a data governance framework extends the principle of Beneficence to address contemporary risks related to privacy and data protection [122].
The Researcher's Toolkit: Operationalizing Ethical Principles
For researchers and drug development professionals, translating ethical principles into daily practice requires specific tools and methodologies. The following table outlines key conceptual "reagents" essential for implementing the Belmont framework in regulatory contexts.
Table: Essential Ethical Tools for Clinical Researchers
| Tool Category | Specific Methodology | Function in Ethical Framework | Regulatory Reference |
|---|---|---|---|
| Informed Consent Systems | Electronic Consent (eConsent) platforms | Implements Respect for Persons through accessible, comprehensible information delivery | ICH E6(R3) Guidance on Digital Tools [120] [122] |
| Risk Assessment Tools | Risk-Based Quality Management Systems | Operationalizes Beneficence through systematic risk identification and mitigation | ICH E6(R3) Principles on Quality by Design [120] [122] |
| Subject Selection Frameworks | Enrollment equity assessment protocols | Applies Justice through monitoring and ensuring fair subject selection | FDA 21 CFR 56.111 Requirements [117] |
| Vulnerability Protections | Additional safeguards for vulnerable populations | Implements both Respect for Persons and Justice through special protections | Belmont Report on diminished autonomy [117] [9] |
| Data Governance Protocols | Cybersecurity and data integrity measures | Extends Beneficence to protection of participant data and privacy | ICH E6(R3) Data Governance Framework [122] |
The Belmont Report's influence on both FDA regulations and ICH GCP guidelines demonstrates the enduring power of its ethical framework. While never formally adopted as national policy, the report's principles have become embedded in the regulatory DNA of human subjects research protections [117] [28]. The direct lineage is clear in U.S. federal regulations, where the Common Rule and FDA regulations explicitly operationalize the principles of Respect for Persons, Beneficence, and Justice.
Internationally, the influence is more diffuse but equally profound. The newly updated ICH E6(R3) guidelines, while designed for a global audience and modern technological landscape, embody the same fundamental ethical commitments that the National Commission articulated nearly five decades ago. The principles-based approach of E6(R3), with its emphasis on participant welfare, informed consent, and equitable selection, carries forward the Belmont tradition into the era of decentralized trials, digital health technologies, and complex data governance challenges [120] [122].
For today's researchers and drug development professionals, understanding this ethical lineage is not merely an academic exercise. It provides the conceptual foundation for navigating complex regulatory requirements and making ethically sound decisions in the design and conduct of clinical trials. As clinical research continues to evolve with new technologies and methodologies, the Belmont Report's principles remain a stable moral compass, guiding the protection of human subjects while enabling scientifically valid research that advances public health.
The Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research, published in 1979, emerged as a foundational response to ethical crises in human subjects research, including the Tuskegee Syphilis Study and revelations concerning Nazi medical experimentation [34]. Created by the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research as mandated by the National Research Act of 1974, this seminal document established a robust ethical framework to guide the conduct of research involving human participants [28] [10] [3]. Its enduring relevance is particularly evident in modern gene therapy clinical trials, where complex ethical challenges necessitate principled oversight. The report's distinction between clinical practice (aimed at enhancing individual patient well-being) and medical research (designed to test hypotheses and gain generalizable knowledge) provides critical grounding for evaluating novel therapeutic interventions [124]. This technical guide examines the application of Belmont's ethical principles within the specific context of gene therapy research, validating their continued indispensability for researchers, scientists, and drug development professionals.
Foundational Ethical Principles of the Belmont Report
The Belmont Report establishes three fundamental ethical principles that form the moral foundation for human subjects research regulations. These principles provide a systematic framework for analyzing the ethical dimensions of research protocols, particularly in complex fields like gene therapy.
The Principle of Respect for Persons
The principle of Respect for Persons incorporates two complementary ethical convictions: first, that autonomous individuals should be treated as agents capable of self-determination; and second, that persons with diminished autonomy are entitled to special protections [124] [11]. This principle manifests primarily through the process of informed consent, which requires three essential elements: adequate information disclosure, participant comprehension, and voluntary participation without coercion or undue influence [124] [34]. In the context of gene therapy research, this principle demands special consideration for potential participants who may have limited therapeutic options and could consequently be vulnerable to undue influence—a phenomenon known as therapeutic misconception [124]. For individuals with diminished decision-making capacity, the principle mandates additional safeguards, including proxy consent procedures and respect for subject assent when possible [124] [3].
The Principle of Beneficence
The principle of Beneficence extends beyond mere non-maleficence ("do no harm") to encompass an affirmative obligation to secure participants' well-being by maximizing potential benefits and minimizing possible harms [124] [11]. This principle requires investigators to conduct a systematic assessment of risks and benefits before commencing research and to maintain ongoing vigilance throughout the study [34]. For gene therapy trials, this entails rigorous preclinical evaluation, thoughtful protocol design that minimizes unnecessary procedures, and ensuring that the research question justifies the risks involved [124]. The Belmont Report explicitly states that "inhumane treatment of human subjects is never morally justified" and requires investigators to demonstrate that vulnerable populations are appropriately protected when included in research [124]. The principle also demands that proposed research employs scientifically valid methodologies, as invalid science inherently fails to provide societal benefits that could justify participant risk [124].
The Principle of Justice
The principle of Justice addresses the equitable distribution of both the burdens and benefits of research [124] [11]. This principle requires careful scrutiny of participant selection to avoid systematically selecting subjects based on convenience, compromised position, or societal marginalization [34] [11]. The Belmont Report specifically references the Tuskegee Syphilis Study as a historical example of injustice, wherein the burdens of research fell disproportionately on disadvantaged African American men while the benefits of improved medical care primarily advantaged privileged white patients [124]. In gene therapy research, the justice principle demands that selection criteria be directly related to the research questions rather than excluding groups without sound scientific rationale, and that publicly-funded research should not unduly involve individuals who are unlikely to benefit from subsequent therapeutic advances [124]. This principle also guides considerations about post-trial access to successful therapies and fair allocation of scarce research resources.
Table 1: Core Ethical Principles of the Belmont Report and Their Applications
| Ethical Principle | Core Meaning | Practical Applications in Research |
|---|---|---|
| Respect for Persons | Recognizing autonomy and protecting those with diminished autonomy [124] [11] | Informed consent process; protection of vulnerable populations; confidentiality maintenance [124] |
| Beneficence | Maximizing benefits and minimizing harms [124] [11] | Risk-benefit assessment; scientifically valid design; independent review [124] |
| Justice | Fair distribution of research burdens and benefits [124] [11] | Equitable subject selection; avoidance of exploitative recruitment [124] [34] |
Methodological Framework for Ethical Analysis
The application of Belmont principles requires a structured methodological approach to ethical analysis in research protocols. The following framework provides guidance for investigators and Institutional Review Boards (IRBs) when evaluating the ethical dimensions of gene therapy clinical trials.
Diagram 1: Ethical Review Framework for Gene Therapy Research
Protocol Assessment Workflow
The ethical review process for gene therapy trials involves systematic evaluation across multiple dimensions derived from Belmont principles. The IRB must first assess the scientific validity of the proposed study, as unsound science cannot ethically justify participant risk [124]. Subsequently, the informed consent process undergoes scrutiny to ensure adequate disclosure of gene therapy-specific risks, including potential for insertional mutagenesis, immune reactions, and unknown long-term effects [124] [34]. The review then examines subject selection criteria to identify and justify the inclusion of potentially vulnerable populations while ensuring equitable distribution of research burdens [11]. Finally, the IRB evaluates provisions for ongoing safety monitoring and protocol modifications based on emerging data, particularly crucial in gene therapy where long-term effects may be unknown [34].
Risk-Benefit Analysis Methodology
The Belmont Report's principle of beneficence requires a systematic risk-benefit assessment that extends beyond simple quantification. This analysis must consider the probability and magnitude of potential harms, the anticipated benefits to participants and society, and the uncertainty inherent in novel gene therapy approaches [124]. Investigators should employ a systematic scoring matrix that categorizes risks and benefits across multiple dimensions, including physical, psychological, social, and economic factors. The assessment must clearly distinguish between direct therapeutic benefits to participants and the knowledge benefits to society, avoiding overstatement of potential personal benefit in early-phase trials [124]. This rigorous approach ensures that the benefit-risk ratio remains favorable and justifiable throughout the research process.
Application in Gene Therapy Clinical Trials
Gene therapy represents a paradigm shift in medical treatment, introducing unique ethical challenges that make the Belmont principles particularly relevant. Historical analysis reveals that the Belmont Report's principles were "clearly reflected" in the development of regulations governing gene therapy clinical trials, especially regarding public review of protocols and special protections for vulnerable populations [28].
Ethical Challenges in Gene Therapy Research
Gene therapy trials present several distinctive ethical considerations that demand rigorous application of Belmont principles. These include therapeutic misconception, where participants may conflate research with treatment; unknown long-term risks, including potential for germline modifications; complex risk-benefit profiles with potential for irreversible effects; and equity concerns regarding access to potentially transformative but expensive therapies [28] [124]. Additionally, the highly technical nature of gene therapy approaches complicates the informed consent process, as participants may struggle to understand complex mechanisms like viral vector delivery systems or gene editing technologies [124]. These challenges necessitate enhanced ethical safeguards and specialized oversight mechanisms.
Implementing Respect for Persons in Gene Therapy Consent
The informed consent process for gene therapy trials requires special considerations to fulfill the principle of respect for persons. Investigators must provide comprehensive information about the novel nature of the intervention, including explicit acknowledgment of unknown long-term risks and uncertainty about efficacy [124] [34]. The consent discussion should utilize lay-friendly explanations of complex concepts like viral vectors, gene editing mechanisms, and potential for off-target effects. The process should emphasize the research nature of the intervention to counter therapeutic misconception and clarify what happens if the therapy fails or causes adverse effects [124]. For trials involving children or adults with diminished capacity, the process must include appropriate proxy consent procedures while still seeking assent from participants to the extent of their capabilities [124] [34].
Table 2: Gene Therapy-Specific Consent Requirements Based on Belmont Principles
| Belmont Principle | Gene Therapy Consent Element | Practical Implementation Strategy |
|---|---|---|
| Respect for Persons | Understanding of novel technology [124] | Use of visual aids, analogies, and layered consent documents |
| Respect for Persons | Voluntary decision without coercion [34] | Clear statement that standard care remains available; cooling-off period |
| Beneficence | Realistic presentation of potential benefits [124] | Explicit distinction between direct benefit and societal knowledge gain |
| Beneficence | Comprehensive risk disclosure [124] | Discussion of theoretical long-term risks alongside known short-term risks |
| Justice | Fair opportunity to participate [11] | Non-discriminatory inclusion criteria; accessibility of trial information |
Beneficence and Risk Management in Protocol Design
The principle of beneficence requires particularly rigorous application in gene therapy trials due to the potential for irreversible genetic modifications and unknown long-term consequences. Protocol designers must implement comprehensive preclinical testing in appropriate models to characterize potential risks before human trials commence [124]. Research designs should incorporate careful dose escalation strategies and stopping rules based on predefined safety endpoints [34]. The principle of beneficence also demands scientific validity, requiring that gene therapy trials address meaningful research questions with appropriate methodology to generate clinically relevant knowledge [124]. Additionally, protocols must include long-term follow-up provisions (often 5-15 years) to monitor for delayed adverse events, fulfilling the obligation to minimize potential harms throughout the research lifecycle [124].
Justice Considerations in Participant Selection
The principle of justice requires careful attention to participant selection in gene therapy trials to ensure equitable distribution of both burdens and benefits. Researchers must avoid convenience sampling from vulnerable populations with limited treatment options while ensuring access for groups that might benefit from participation [34] [11]. Selection criteria should be scientifically justified rather than based on administrative convenience or social vulnerability [11]. The justice principle also extends to post-trial access considerations, requiring researchers to address whether successful interventions will be available to participants after study completion and how equitable access will be ensured for broader populations [124]. Furthermore, the principle mandates consideration of global equity, particularly when gene therapy research conducted in high-income countries might yield treatments unaffordable in lower-income regions where research populations reside [124].
Research Reagents and Materials Toolkit
The ethical conduct of gene therapy research requires specific reagents and materials that facilitate both scientific rigor and participant protection. The following toolkit outlines essential components for implementing Belmont principles in clinical trials.
Table 3: Essential Research Reagent Solutions for Ethical Gene Therapy Trials
| Toolkit Component | Function | Ethical Principle Supported |
|---|---|---|
| Validated Vector Systems | Delivery of genetic material with characterized safety profiles [124] | Beneficence (risk minimization) |
| Pharmacogenomic Assays | Identification of participants likely to respond to therapy based on genetic markers [11] | Justice (equitable selection) |
| Standardized Consent Documentation | Clear communication of risks, benefits, and alternatives using consistent formats [124] [34] | Respect for Persons (informed decision-making) |
| Data Safety Monitoring Plan | Structured framework for ongoing review of participant safety data [34] | Beneficence (harm minimization) |
| Vulnerability Assessment Tool | Systematic identification of participants requiring additional protections [124] [34] | Respect for Persons (protection of autonomy) |
| Equitable Recruitment Framework | Protocol for ensuring diverse and appropriate participant selection [11] | Justice (fair burden/benefit distribution) |
The Belmont Report's ethical framework remains indispensable for navigating the complex terrain of modern gene therapy research. Its three core principles—respect for persons, beneficence, and justice—provide a robust structure for addressing ethical challenges posed by emerging genetic technologies [28] [124] [11]. As gene therapy approaches evolve to include more sophisticated gene editing techniques and novel delivery systems, the need for principled ethical oversight becomes increasingly critical. The enduring relevance of the Belmont Report lies in its ability to provide foundational guidance while allowing flexibility for application to specific research contexts [28]. For researchers, scientists, and drug development professionals, conscientious application of these principles ensures that scientific advancement proceeds in tandem with unwavering commitment to ethical responsibility and human subject protection. The integration of these principles into gene therapy clinical trials validates their continuing vitality nearly five decades after their formulation, demonstrating their essential role in responsible research conduct.
The Belmont Report, formally titled the "Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research," was established in 1979 in response to historical ethical violations in research, such as the Tuskegee Syphilis Study [90]. For decades, its three core principles—Respect for Persons, Beneficence, and Justice—have served as the ethical foundation for human subjects research in biomedical and behavioral fields [109]. These principles remain the cornerstone of modern research ethics, with over 70% of global research institutions adhering to them and 90% of Institutional Review Boards (IRBs) using them as a key reference [90]. However, the rapid emergence of internet-mediated research (IMR), which includes methodologies such as online surveys, social media data analysis, and web-conferencing, presents unprecedented challenges to the traditional application of these principles [125] [126].
The internet has become what Castells describes as "the fabric of our lives," revolutionizing how people perceive and interact with their environment [125]. In social science research and beyond, the internet is a potent methodological tool that shapes the dynamics, locations, and embodiments of interactions and meaning construction. This transformation creates a significant ethical gap; the Belmont Report's principles were conceived in an analog world and their "mission creep" into the digital realm can be problematic due to fundamental differences in the nature of inquiry and methods employed [125]. This technical guide provides a structured framework for re-interpreting the Belmont principles to meet these modern challenges, ensuring that research involving human participants remains ethical, valid, and trustworthy in the context of internet and social media platforms.
Core Ethical Principles and Their Digital Translation
The Belmont Report's three principles provide a flexible framework that requires careful re-interpretation for the digital world. The table below summarizes the core tenets and their modern translations.
Table 1: Core Belmont Principles and Their Digital Translation
| Belmont Principle | Traditional Application | Modern Digital Translation |
|---|---|---|
| Respect for Persons | Individual autonomy; informed consent with signed forms; extra protections for vulnerable populations [109]. | Dynamic consent; transparency about data use; meaningful privacy policies; layered consent for complex studies [125]. |
| Beneficence | Risk-benefit analysis; physical and psychological harm minimization; study monitoring boards [109]. | Digital risk assessment; proactive data security; confidentiality protection against breaches and data mining [126]. |
| Justice | Fair participant selection; equitable distribution of research benefits and burdens; avoidance of vulnerable group exploitation [109]. | Inclusive digital recruitment; addressing algorithmic bias; ensuring benefits of research reach all groups in society [125] [90]. |
Principle 1: Respect for Persons in Digital Contexts
The principle of Respect for Persons emphasizes individual autonomy and requires that subjects enter research voluntarily and with adequate information [109]. In digital environments, this translates to obtaining meaningful informed consent when researchers interact with or collect data about individuals. The fundamental challenge is that the internet is simultaneously both text-like and space-like, blurring the lines between public information and private communication [125]. This ambiguity challenges the very definition of a "human subject."
Digital Informed Consent Protocol
A robust digital informed consent protocol must adapt to the specific nature of the internet-mediated research. The following diagram illustrates a decision workflow for determining the appropriate consent pathway.
Key Considerations for Digital Consent:
- Affirmative Action: Consent must be an affirmative, explicit action. Pre-checked boxes or opt-out procedures are not permitted under stringent standards like the GDPR. Instead, researchers should use active "opt-in" language, such as "I agree" checkboxes [127].
- Electronic Informed Consent (eIC): For research collecting identifiable sensitive data, the electronic system must include a verification method (e.g., NetID and password, state-issued ID verification) to ensure the person signing is the actual participant [126].
- Contextual Integrity: Respecting persons online means upholding the contextual expectations of privacy within a specific digital space. Using data from a closed support group for public research, for example, may violate this principle even if the data is technically "public" [125].
Principle 2: Beneficence and Digital Risk Assessment
The principle of Beneficence mandates maximizing benefits and minimizing harms [109]. In digital research, harms are less often physical and more frequently related to breaches of confidentiality, psychological distress, reputational damage, and professional or financial harm [126].
Digital Risk Assessment and Security Protocol
A comprehensive approach to beneficence requires a proactive risk assessment and a robust data security plan. The following workflow provides a structured methodology for this process.
Essential Security Measures:
- Data Classification and Storage: All data should be classified based on sensitivity. Identifiable or sensitive data must be stored on university-owned, encrypted devices and on secure university drives (e.g., UConn's P and R drives) or authorized cloud services like UConn Office 365 (OneDrive/SharePoint) [126].
- Transmission Security: Identifiable data should never be transmitted via standard email due to inherent risks. Secure services like Office365, FileLocker, or Secure File Transfer Protocol (FTPS) must be used instead [126].
- Minimization and Anonymization: The most effective way to minimize risk is to minimize data collection. Researchers should collect the "absolute minimum personal data" and use de-identified data wherever possible. Under standards like the GDPR, even "pseudonymized data" (coded data) is still considered personal data if a keycode exists somewhere [127].
Principle 3: Justice and Equity in Digital Recruitment
The principle of Justice requires the fair distribution of both the burdens and the benefits of research [109]. Traditionally, this meant avoiding the systematic selection of vulnerable or "convenient" populations (e.g., welfare patients, racial minorities, prisoners) simply because they are easy to manipulate or access [109].
Contemporary Digital Justice Challenges
In digital research, justice takes on new dimensions. While online recruitment can potentially reach more diverse populations, it can also introduce new forms of exclusion and bias.
- Digital Divides: Recruitment solely through social media or online ads may systematically exclude elderly, rural, low-income, or less technologically literate populations [128]. A just recruitment strategy must use multiple channels to avoid creating a "digitally privileged" research population.
- Algorithmic Bias: Platforms like Facebook use algorithms to deliver ads. If not carefully managed, these algorithms can unintentionally skew recruitment toward or away from certain demographic groups, potentially reinforcing existing health and social inequities [125].
- Global Data Standards: Internet research often has a global reach. Justice requires researchers to be aware of and comply with different international data protection standards, such as the General Data Protection Regulation (GDPR) for participants in the European Economic Area. The GDPR applies when collecting data from individuals physically located in the EEA at the time of collection, regardless of their citizenship [127].
Table 2: Quantitative Social Media Adoption and Research Potential (2025)
| Region/Demographic | Social Media Adoption Rate | Primary Research Implications |
|---|---|---|
| Global Average | 94.2% of all internet users [128] | Vast potential for large-scale recruitment and data collection. |
| Eastern Asia | ~97% of connected population [128] | Near-ubiquitous use of platforms like WeChat enables comprehensive studies. |
| Sub-Saharan Africa | Well under 50% of connected population [128] | Online-only recruitment would systematically exclude the majority; hybrid methods are required for justice. |
| Gen Z & Millennials | Highest adoption & engagement rates [129] | Over-representation in generic social media samples; requires balancing for generalizable results. |
The Researcher's Toolkit for Ethical IMR
Implementing ethical internet-mediated research requires a suite of methodological and technical tools. The following table details essential "research reagents" for the modern digital scholar.
Table 3: Essential Research Reagents for Ethical Internet-Mediated Research
| Tool Category | Specific Tool/Technique | Function & Ethical Justification |
|---|---|---|
| Consent & Transparency | Electronic Informed Consent (eIC) Systems | Facilitates verifiable, documented remote consent; fulfills Respect for Persons [126]. |
| Layered Consent Forms/Information Sheets | Presents key information concisely with options to delve deeper; respects autonomy without overwhelming [125]. | |
| Privacy Impact Assessment (PIA) | Systematically evaluates how a project handles personal data; foundational to Beneficence [126]. | |
| Data Security | University-Approved Encrypted Storage (e.g., Secure Drives, OneDrive) | Protects data confidentiality against breaches; a core requirement of Beneficence [126]. |
| Secure Transmission Services (e.g., FileLocker, FTPS) | Prevents interception of identifiable data during transfer; mitigates a key digital risk [126]. | |
| Data De-identification & Anonymization Tools | Strips data of identifiers; reduces privacy risk and can simplify IRB review [127] [126]. | |
| Ethical Recruitment | Multi-Channel Recruitment Strategy | Uses online and offline methods to prevent digital exclusion; upholds Justice [128]. |
| Platform-Specific Advertisement Targeting Audits | Reviews ad settings to avoid algorithmic bias; ensures fair participant selection per Justice [125]. | |
| Oversight & Compliance | Data Security Assessment Form | Formal document for IRB outlining data handling; demonstrates proactive Beneficence [126]. |
| GDPR Compliance Checklist | Ensures legal and ethical handling of data from EEA participants; a matter of Justice and Respect [127]. |
The Belmont Report's ethical principles are not obsolete; they are remarkably resilient. However, their application must evolve to address the complexities of internet-mediated and social media research. Respect for Persons now demands dynamic, verifiable consent and a nuanced understanding of privacy in digital spaces. Beneficence requires a rigorous, proactive approach to digital risk assessment and data security that guards against novel threats like data breaches and re-identification. Justice compels researchers to confront digital divides and algorithmic biases to ensure the equitable distribution of research burdens and benefits.
By adopting the frameworks, protocols, and tools outlined in this guide, researchers can bridge the gap between foundational ethics and modern methodology. This purposeful re-interpretation allows the research community to continue its vital work with integrity, preserving public trust and upholding the dignity of every participant in the digital age.
The Belmont Report, formally issued in 1979, established three foundational ethical principles—Respect for Persons, Beneficence, and Justice—for protecting human subjects in research [3]. For decades, this framework has served as the ethical bedrock for biomedical and behavioral research in the United States. However, the rapid proliferation of emerging technologies, particularly in artificial intelligence (AI) and robotics, presents novel ethical challenges that test the boundaries of traditional research ethics frameworks [130]. This whitepaper argues that the Belmont Report's principles possess an inherent adaptability, making them a resilient guide for ethical oversight in the face of technological innovation. By reinterpreting and applying these principles to contemporary research contexts—from AI-driven diagnostics to global environmental studies—researchers, scientists, and drug development professionals can navigate this new ethical terrain while upholding the core commitment to protecting human dignity and well-being.
The integration of AI and robotics into healthcare and research heralds a new era of medical innovation, promising enhanced diagnostics, streamlined processes, and improved patient care [130]. Concurrently, global research efforts, such as those coordinated by the Belmont Forum, are leveraging advanced technologies like environmental DNA (eDNA) and species distribution modeling to tackle complex socio-environmental challenges [131] [132]. These technological shifts introduce a complex web of ethical considerations that were not fully conceivable at the time of the Belmont Report's publication. Critics have pointed out that the Report's framework, with its strong emphasis on individual choice and a model of direct researcher-participant interaction, may be insufficient for addressing community-level harms, the exploitation of cultural knowledge, and the unique vulnerabilities exposed by data-intensive research [133]. Despite these valid critiques, the fundamental principles of the Belmont Report provide a robust starting point for developing a responsive and accountable research ethics infrastructure for the 21st century. This guide details how these principles can be operationalized in modern research contexts.
Core Principles of the Belmont Report and Modern Interpretations
The Belmont Report's three principles translate into rigorous federal regulations for human subjects research. The following table summarizes their core definitions and corresponding regulatory applications [3].
Table 1: The Three Ethical Principles of the Belmont Report
| Ethical Principle | Core Definition | Regulatory Application |
|---|---|---|
| Respect for Persons | Recognition of the autonomy of individuals; protection of individuals with diminished autonomy. | Informed Consent Process: Voluntariness, comprehension, key information disclosure. |
| Beneficence | Obligation to maximize possible benefits and minimize possible harms. | Risk-Benefit Assessment: Justifying that risks are minimized and reasonable in relation to anticipated benefits. |
| Justice | Fairness in the distribution of the burdens and benefits of research. | Selection of Subjects: Equitable selection to avoid exploiting vulnerable populations. |
Respect for Persons in the Digital Realm
The principle of Respect for Persons mandates the protection of individual autonomy through a robust informed consent process. In the context of AI and data-driven research, this principle demands more than a static consent form [130].
- Informed Consent and Data Re-use: Modern research, particularly involving AI, often relies on vast datasets which may be repurposed beyond the scope of the original consent. The Belmont principle requires transparent communication about how data will be used, stored, and potentially shared. This is especially critical in international collaborations, such as those under the Belmont Forum's Climate, Environment, and Health (CEH) initiative, where data might be analyzed across borders [131]. Strategies include dynamic consent models and clear explanations of data lifecycle management.
- Autonomy in Algorithmic Decision-Making: When AI systems provide diagnostic or treatment recommendations, Respect for Persons requires that the human patient's values and preferences remain central [130]. This involves ensuring that AI systems are transparent and explainable enough for a patient to comprehend the basis of a recommendation, thereby allowing for meaningful participation in their own care decisions.
Beneficence in Complex Systems
The principle of Beneficence requires an obligation to maximize benefits and minimize harms. For emerging technologies, this extends beyond the physical safety of a participant to encompass privacy, data security, and algorithmic fairness [130].
- Risk-Benefit Assessment for AI/ Robotics: The benefits of AI in healthcare are significant, including enhanced diagnostic precision, personalized treatment plans, and early disease detection [130]. However, the risks include data breaches, algorithmic bias, and over-reliance on automated systems. A Belmont-guided risk-benefit analysis must systematically account for these novel risks, ensuring they are minimized and reasonable in relation to the knowledge gained.
- Systemic Harms and Environmental Research: The Belmont Forum's research on resilience and tropical forests considers benefits and risks at a socio-ecological system level [131]. The Beneficence principle, in this context, applies to protecting entire communities and ecosystems, ensuring that research interventions like Nature-based Solutions (NbS) do not inadvertently harm local populations or biodiversity [132].
Justice and Equitable Access
The Justice principle promotes the equitable selection of subjects, ensuring that vulnerable populations are not unduly burdened with research risks while being excluded from its benefits.
- Algorithmic Bias and Fairness: AI systems can perpetuate and amplify existing societal biases if trained on non-representative data [130]. This creates a modern Justice concern where certain demographic groups could face misdiagnosis or inadequate care. Upholding justice requires using diverse, representative datasets and continuously monitoring algorithms for discriminatory outcomes.
- Global Equity in Research: The Belmont Forum's collaborative research actions (CRAs), such as the Africa Regional Call (ARC), are explicitly designed to address knowledge gaps and build resilience in vulnerable regions [131]. This embodies the Justice principle by ensuring that research priorities and benefits are directed toward communities most affected by global challenges like climate change, rather than being concentrated solely in developed nations.
Implementing the Belmont Framework: A Protocol for Emerging Technologies
To translate ethical principles into practice, researchers need a structured methodology. The following workflow and toolkit provide a guide for integrating the Belmont Framework into technology-driven research.
Diagram 1: An ethical implementation workflow for applying the Belmont Report's principles to projects involving emerging technologies. This process transforms each core principle into a concrete action and a verifiable output.
The Research Reagent Toolkit for Ethical AI in Healthcare
In biomedical research, "reagents" are essential tools for experimentation. Similarly, the following table details essential "reagent solutions" for conducting ethical research with AI in healthcare, as derived from current literature [130].
Table 2: Research Reagent Solutions for Ethical AI in Healthcare
| Research 'Reagent' | Function in Ethical Research | Application Example |
|---|---|---|
| Federated Learning Architectures | Enables training of AI models on decentralized data without centralizing sensitive patient information. | Preserves patient privacy (Respect for Persons) while allowing development of robust diagnostic algorithms across multiple hospitals. |
| Algorithmic Bias Auditing Tools | Systematically tests AI models for discriminatory performance across different demographic subgroups. | Identifies and helps mitigate unfair outcomes (Justice) in a predictive model for patient readmission risk. |
| Explainable AI (XAI) Techniques | Provides clear, understandable explanations for AI-driven decisions, making the decision-making process transparent. | Allows a clinician and patient to understand the rationale behind an AI's diagnostic recommendation, supporting informed consent (Respect for Persons). |
| Robust Data Anonymization & Encryption | Protects patient data from breaches during transmission and storage using advanced cryptographic methods. | Safeguards patient information (Beneficence) and ensures compliance with data protection regulations like GDPR and HIPAA. |
Experimental Protocol: Auditing an AI Model for Algorithmic Bias
This detailed protocol provides a methodology for upholding the Justice principle in AI-based healthcare tool development [130].
Objective: To empirically evaluate a machine learning model for diagnostic prediction for performance disparities (bias) across pre-defined patient subgroups based on race, gender, and socioeconomic status.
Materials:
- The trained AI model to be audited.
- A held-out test dataset with ground-truth labels, containing relevant demographic attributes.
- Computational resources (e.g., cloud computing or high-performance computing cluster).
- Bias auditing software libraries (e.g.,
AI Fairness 360(IBM),Fairlearn(Microsoft)).
Methodology:
- Data Preparation: The test dataset is partitioned into subgroups based on the demographic attributes of interest (e.g., Female vs. Male, Group A vs. Group B).
- Model Prediction & Performance Calculation: The audited model is used to generate predictions for the entire test set. Standard performance metrics (e.g., Accuracy, Sensitivity, Specificity, Positive Predictive Value) are calculated for the overall population and for each subgroup.
- Bias Metric Calculation: Quantitative bias metrics are computed to compare performance across subgroups. Key metrics include:
- Disparate Impact: Ratio of the positive outcome rate for the unprivileged group to the privileged group.
- Equality of Opportunity Difference: Difference in true positive rates between subgroups.
- Predictive Parity Difference: Difference in positive predictive values between subgroups.
- Statistical Analysis: Conduct statistical significance tests (e.g., chi-squared tests for performance metrics) to determine if observed disparities are statistically significant.
- Interpretation and Reporting: Generate a bias audit report detailing any significant performance disparities. The report should inform model refinement, such as retraining with re-sampled data or applying bias mitigation algorithms, and be included in study documentation for IRB review.
The Belmont Report has proven to be a durable foundation for research ethics precisely because its principles are foundational rather than prescriptive. Respect for Persons, Beneficence, and Justice provide a stable compass for navigating the uncharted ethical territories opened by AI, robotics, and other emerging technologies. While the Report is not without its limitations, particularly in addressing community-level impacts and non-Western worldviews [133], its core values demand that we continually reassess and update our protective measures. For the research community, the path forward is not to abandon this established framework but to engage in the creative and rigorous work of applying it. By doing so, researchers and developers can ensure that technological advancement remains firmly coupled with the ethical imperative to protect and respect human beings.
Conclusion
The Belmont Report remains the indispensable ethical compass for human subjects research, its principles of Respect for Persons, Beneficence, and Justice providing a robust and adaptable framework long after its publication. For today's researchers, its true value lies not in rigid adherence but in its thoughtful application as an analytical tool to navigate complex scenarios, from pediatric studies to digital research environments. As biomedical science advances with gene therapies, AI, and novel methodologies, the Belmont principles offer a stable foundation upon which to build new, situation-specific guidelines. The future of ethical research demands a commitment to these core principles while encouraging continuous dialogue and refinement to meet the challenges of tomorrow's scientific landscape, ensuring that the rights and welfare of participants are perpetually protected.
References
- 1. - Wikipedia Tuskegee Syphilis Study [https://en.wikipedia.org/wiki/Tuskegee_Syphilis_Study]
- 2. - Wikipedia National Research Act [https://en.wikipedia.org/wiki/National_Research_Act]
- 3. The Belmont - UW Research Report [https://www.washington.edu/research/hsd/guidance/ethical-principles/belmont/]
- 4. Inside The Horrific Tuskegee Experiment That Let Black Men Die Slowly [https://allthatsinteresting.com/tuskegee-experiment]
- 5. About The Untreated Syphilis at Study | Tuskegee ... | CDC Syphilis [https://www.cdc.gov/tuskegee/about/index.html]
- 6. Guiding Principles for Ethical Research | National Institutes of Health (NIH) [https://www.nih.gov/health-information/nih-clinical-research-trials-you/guiding-principles-ethical-research]
- 7. What Is Ethics in Research & Why Is It Important? | National Institute of Environmental Health Sciences [https://www.niehs.nih.gov/research/resources/bioethics/whatis]
- 8. The Belmont | Report Office - Office of the Vice... Human Subjects [https://hso.research.uiowa.edu/about-human-subjects-office/regulations-and-policies/belmont-report]
- 9. - Wikipedia Belmont Report [https://en.wikipedia.org/wiki/Belmont_Report]
- 10. The Belmont Report. Ethical principles and guidelines for the protection of human subjects of research - PubMed [https://pubmed.ncbi.nlm.nih.gov/25951677/]
- 11. Belmont Report – Human Research Protection Program [https://irb.wisc.edu/regulatory-information/belmont-report/]
- 12. - New World Encyclopedia Belmont Report [https://www.newworldencyclopedia.org/entry/Belmont_Report]
- 13. Chapter 1 - Ethical and Regulatory Mandates to Protect Human Research Participants | Human Research Protection Office (HRPO) | University of Pittsburgh [https://www.hrpo.pitt.edu/policies-and-procedures/chapter-1-ethical-and-regulatory-mandates-protect-human-research]
- 14. Ethical, Legal, and Regulatory Framework for Human Subjects Research - Optimizing the Nation's Investment in Academic Research - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK373547/]
- 15. Vulnerability in Research: Basic Ethical Concepts and General Approach to Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7122263/]
- 16. Policy on Ethical Conduct of Research – User Support [https://support.researchallofus.org/hc/en-us/articles/22346846933396-Policy-on-Ethical-Conduct-of-Research]
- 17. 50. Ethical Foundation: The Belmont Report | Research Integrity & Security | University of Nevada, Reno [https://www.unr.edu/research-integrity/program-areas/human-research/human-research-protection-policy-manual/50-ethical-foundation-the-belmont-report]
- 18. Ethical Principles | Human Protection Program (HRPP) Research [https://hrpp.research.virginia.edu/resources/ethical-principles]
- 19. Beyond 'do no harm ': The ethics of maximizing from... benefit [https://blogs.bmj.com/medical-ethics/2025/03/05/beyond-do-no-harm-the-ethics-of-maximizing-benefit-from-psychedelics-in-healthcare/]
- 20. The Ultimate Guide to Ethics in Research [https://www.numberanalytics.com/blog/ultimate-guide-ethics-research]
- 21. 13 Comparing within individuals | Scientific... quantitative data [https://bookdown.org/pkaldunn/SRM-Textbook/SummariseWithin.html]
- 22. APSY 210 Chapter 3 Review: APA Ethics Principles & More... | Quizlet [https://quizlet.com/943979039/apsy-210-chapter-3-review-flash-cards/]
- 23. Investigators Bearing the Burdens of Research | 2022 | IRB Blog | Institutional Review Board | Teachers College, Columbia University [https://www.tc.columbia.edu/institutional-review-board/irb-blog/2022/investigators-bearing-the-burdens-of-research-/]
- 24. [FREE] According to the Belmont , the... - brainly.com Report [https://brainly.com/question/24875330]
- 25. [FREE] According to the Belmont Report, the requirement that the benefits and burdens of the research are - brainly.com [https://brainly.com/question/32882487]
- 26. the Benefits and Equitably of Sharing : Covid‐19... Burdens Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC7272984/]
- 27. Why is informed consent required ? [https://www.genome.gov/about-genomics/educational-resources/fact-sheets/why-is-informed-consent-required]
- 28. The creation of the Belmont Report and its effect on ethical principles: a historical study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9700634/]
- 29. eCFR :: 45 .101 -- To what does this policy apply? CFR 46 [https://www.ecfr.gov/current/title-45/subtitle-A/subchapter-A/part-46/subpart-A/section-46.101]
- 30. Human Subjects Protections [https://orwh.od.nih.gov/toolkit/human-subjects-protections]
- 31. Research Involving Human Subjects - Funding at NSF | NSF - U.S. National Science Foundation [https://www.nsf.gov/funding/research-involving-human-subjects]
- 32. Human Research Protections - Office of Research Oversight [https://www.va.gov/oro/hrpp.asp]
- 33. Human Subjects / IRB Policy Updates – July 2025 - Office of Research Compliance - University of Maine [https://umaine.edu/research-compliance/2025/09/04/human-subjects-irb-policy-updates/]
- 34. Research Ethics - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK459281/]
- 35. 325. Informed Consent Requirements | Research Integrity & Security ... [https://www.unr.edu/research-integrity/human-research/human-research-protection-policy-manual/325-informed-consent-requirements]
- 36. Informed Consent: The Requirements for Informed Consent (Series #1) | 2025 | IRB Blog | Institutional Review Board | Teachers College, Columbia University [https://www.tc.columbia.edu/institutional-review-board/irb-blog/2025/informed-consent-the-requirements-for-informed-consent-series-1/]
- 37. Protecting Human Participants | Davidson Research [https://www.davidson.edu/offices-and-services/human-subjects-irb/research-training/protecting-human-research-participants]
- 38. Research Ethics and Informed Consent | Educational Research Basics by Del Siegle [https://researchbasics.education.uconn.edu/ethics-and-informed-consent/]
- 39. Evolving Regulatory Protections for Research Participants | The Regulatory Review [https://www.theregreview.org/2024/12/29/spotlight-evolving-regulatory-protections-for-research-participants/]
- 40. Principles of benefit - risk : A focus on some practical... assessment [https://www.fpm.org.uk/blog/principles-of-benefit-risk-assessment-a-focus-on-some-practical-applications/]
- 41. Quantitative Benefit – Risk : State of the Practice Within... Assessment [https://pmc.ncbi.nlm.nih.gov/articles/PMC7864811/]
- 42. of Systematic and assessment :... | F1000Research benefits risks [https://f1000research.com/articles/2-160]
- 43. Charts vs. Tables : When to Use One Over the Other? [https://wpdatatables.com/charts-vs-tables/]
- 44. Statistical data - PMC presentation [https://pmc.ncbi.nlm.nih.gov/articles/PMC5453888/]
- 45. of Presentation and Evidence Data [https://smartacademicwriting.com/presentation-of-data-and-evidence/]
- 46. You Talkin’ to Me? - Petrie-Flom Center [https://petrieflom.law.harvard.edu/2013/03/05/you-talkin-to-me-2/]
- 47. A step towards equitable clinical trial recruitment : a protocol for the... [https://pilotfeasibilitystudies.biomedcentral.com/articles/10.1186/s40814-019-0516-4]
- 48. The Belmont (Three Benchmark Rules) | PDF Report [https://www.slideshare.net/slideshow/the-belmont-report-three-benchmark-rules/257862278]
- 49. (PDF) Recruitment for strategies Human subjects [https://www.academia.edu/108039828/Recruitment_strategies_for_Human_subjects]
- 50. Effective Recruitment in Human Subjects Research - Solutions IRB [https://www.solutionsirb.com/effective-recruitment-in-human-subjects-research/]
- 51. Ethical Guidelines and the Institutional Review Board – An Introduction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10885741/]
- 52. Guidelines, Regulations and Statutes - UCI Office of Research Ethical [https://research.uci.edu/human-research-protections/irb-application-process/ethical-guidelines-regulations-and-statutes/]
- 53. Research Guidelines and Procedures at SXU IRB Ethical [https://www.sxu.edu/academics/guidance/institutional-review-board/guidelines.html]
- 54. Required Documents for IRB - Solutions Submissions IRB [https://www.solutionsirb.com/required-documents-for-irb-submissions/]
- 55. Forms and FAQ | Research / Scholarship | InsideCBU IRB [https://insidecbu.calbaptist.edu/ICS/Provost/Research__Scholarship/IRB_Forms_and_FAQ.jnz]
- 56. : Home page : The University of Akron, Ohio Institutional Review Board [https://www.uakron.edu/research/ora/compliance/irb/]
- 57. IRB-FAQs [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/institutional-review-boards-frequently-asked-questions]
- 58. Ethics in Research: Local Institutional Review Boards (IRBs) - EDI Global [https://edi-global.com/ethics-in-research/]
- 59. Ethical Challenges with the Informed Consent Process in Pediatric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10928675/]
- 60. for Adolescent Health Guidelines | ACOG Research [https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2016/06/guidelines-for-adolescent-health-research]
- 61. When should a child assent form be used in a pediatric clinical trial? | WCG [https://www.wcgclinical.com/insights/when-should-a-child-assent-form-be-used-in-a-pediatric-clinical-trial/]
- 62. Inclusion of Adolescents in STI/HIV Biomedical Prevention Trials... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6206503/]
- 63. Informed consent and assent guide for paediatric clinical trials in Europe - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9125378/]
- 64. Frontiers | Requirements and special considerations for drug trials with children across six jurisdictions: 2. Ethics review in the regulatory approval process [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1539787/full]
- 65. for Effective and Appropriate Guidelines and... Pediatric Assent [https://www.slideshare.net/slideshow/assent-webinar-13-apr11/10533285]
- 66. With the Right Approach, Vulnerable Can and Should be... Populations [https://acrpnet.org/2025/10/29/with-the-right-approach-vulnerable-populations-can-and-should-be-engaged-in-research]
- 67. Challenges and Strategies in Conducting Ethical with... Research [https://annalskemu.org/journal/index.php/annals/article/view/5775]
- 68. Healthcare Data Ethics : Research Standards 2025 [https://editverse.com/healthcare-data-ethics-research-standards-2025/]
- 69. | Kenyon College Belmont Principles [https://www.kenyon.edu/sponsored-faculty-projects/research-compliance/institutional-review-board-irb/belmont-principles/]
- 70. General considerations for research with vulnerable ... populations [https://pmc.ncbi.nlm.nih.gov/articles/PMC5151796/]
- 71. Vulnerable Populations - UCI Office of Research [https://research.uci.edu/human-research-protections/research-subjects/vulnerable-populations/]
- 72. The Ethical Challenges of Field Research in Conflict Zones [https://link.springer.com/article/10.1007/s11133-006-9027-8]
- 73. Teaching and Learning the Techniques of Conflict for... Resolution [https://pubmed.ncbi.nlm.nih.gov/26752385/]
- 74. Researchers’ views on, and experiences with, the requirement to obtain informed consent in research involving human participants: a qualitative study | BMC Medical Ethics | Full Text [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-020-00538-7]
- 75. Improving the Informed Consent Process for Research Subjects with Low Literacy: A Systematic Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3539038/]
- 76. Ethical Considerations in Informed Consent | IntechOpen [https://www.intechopen.com/chapters/1123544]
- 77. Improving the informed process for research subjects with... consent [https://pubmed.ncbi.nlm.nih.gov/22782275/]
- 78. Improving the Informed Process for Research Subjects with... Consent [https://link.springer.com/article/10.1007/s11606-012-2133-2]
- 79. Health literacy and informed consent for clinical trials: a systematic | NRR [https://www.dovepress.com/health-literacy-and-informed-consent-for-clinical-trials-a-systematic--peer-reviewed-fulltext-article-NRR]
- 80. Linguistic Strategies for Improving Informed Consent in Clinical Trials Among Low Health Literacy Patients - PubMed [https://pubmed.ncbi.nlm.nih.gov/27794035/]
- 81. Developing informed consent materials for non-English-speaking participants: An analysis of four professional firm translations from English to Spanish - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6218315/]
- 82. 3 Determining Minimal in Social and Behavioral Research Risk [https://nap.nationalacademies.org/read/18614/chapter/5]
- 83. Determining Minimal Risk in Social and Behavioral Research - Proposed Revisions to the Common Rule for the Protection of Human Subjects in the Behavioral and Social Sciences - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK217976/]
- 84. NIMH Guidance on Risk-Based Monitoring - National Institute of Mental Health (NIMH) [https://www.nimh.nih.gov/funding/clinical-research/nimh-guidance-on-risk-based-monitoring]
- 85. How IRBs view and make decisions about coercion and undue influence - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3604028/]
- 86. | University of Tennessee at Chattanooga Participant Recruitment [https://www.utc.edu/research/research-integrity/institutional-review-board/participant-recruitment]
- 87. Study Recruiting | Research + Innovation Participants [https://www.ualberta.ca/en/research/services/research-ethics/human-research-ethics/recruitment/index.html]
- 88. The Many Faces of “Coercion” and “Undue Influence” [https://www.advarra.com/blog/the-many-faces-of-coercion-and-undue-influence/]
- 89. Research Recruiting | Division of... | Brown University Participants [https://division-research.brown.edu/research-cycle/conduct-research/human-subjects-research/conducting-research-after-irb/recruiting]
- 90. The Three Principles Of The Belmont Report: Respect For Persons, Beneficence, Justice [https://coursepivot.com/blog/which-of-the-following-are-the-three-principles-discussed-in-the-belmont-report/]
- 91. June 2025 IRB Connection Newsletter | Human Subjects Office [https://hso.research.uiowa.edu/get-help/newsletters/0625]
- 92. Top 6 Visualizations for Quantitative Data Analysis Methods [https://chartexpo.com/blog/quantitative-data-analysis-methods]
- 93. Quantitative Data Analysis. A Complete Guide [2025] [https://www.6sigma.us/six-sigma-in-focus/quantitative-data-analysis/]
- 94. Visualizing Quantitative Data: Best Practices [https://ajelix.com/data/visualizing-quantitative-data-best-practices/]
- 95. Color Considerations - Digital Accessibility at Princeton [https://digital.accessibility.princeton.edu/how/design/color-contrast]
- 96. Color Contrast - Accessibility by Design [https://www.chhs.colostate.edu/accessibility/best-practices-how-tos/color-contrast/]
- 97. Colour contrast [https://goodpractices.design/articles/colour-contrast]
- 98. Human Subjects and Privacy Protection [https://nij.ojp.gov/funding/human-subjects-and-privacy-protection]
- 99. Still Timely After All These Years: How the Belmont Continues... Report [https://acrpnet.org/2025/08/06/still-timely-after-all-these-years-how-the-belmont-report-continues-to-shape-research-ethics]
- 100. Ethical analysis of informed consent methods in longitudinal cohort studies: A Chinese perspective - PubMed [https://pubmed.ncbi.nlm.nih.gov/39268885/]
- 101. Vulnerable population and methods for their safeguard - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3601707/]
- 102. An Overview of Data Management in Human Subjects Research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10898467/]
- 103. Strengthening organizations through ethical vigilance | MNP [https://www.mnp.ca/en/insights/directory/strengthening-organizations-ethical-vigilance]
- 104. Nuremberg Code - Wikipedia [https://en.wikipedia.org/wiki/Nuremberg_Code]
- 105. | History, Date, & 10 Points | Britannica Nuremberg Code [https://www.britannica.com/topic/Nuremberg-Code]
- 106. Nuremberg Code - UNC Research [https://research.unc.edu/human-research-ethics/resources/ccm3_019064/]
- 107. The Nuremberg Code and the Nuremberg Trial. A reappraisal - PubMed [https://pubmed.ncbi.nlm.nih.gov/8922453/]
- 108. Cancer Clinical Trials: The Belmont and Your Protection Report [https://thepatientstory.com/treatments/clinical-trials/the-belmont-report/]
- 109. - BELMONT .pptxegoldsghhdghhg | PPTX REPORT 2025 [https://www.slideshare.net/slideshow/belmont-report-2025-pptxegoldsghhdghhg/283529628]
- 110. A Summary of Important Documents in the Field of Research Ethics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2632196/]
- 111. Why Human Subjects Research Protection Is Important - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7122250/]
- 112. The Declaration | PPTX of Helsinki [https://www.slideshare.net/slideshow/the-declaration-of-helsinki-9881769/9881769]
- 113. WMA Declaration – Ethical Principles for Medical... of Helsinki [https://www.linkedin.com/pulse/wma-declaration-helsinki-ethical-principles-medical-research-roohi-dv88e]
- 114. The nuremberg code declaration the of | pptx helsinki belmont report [https://www.slideshare.net/slideshow/belmont-report-48291712/48291712]
- 115. lifeissues.net | Need to know: Nuremberg Code, Declaration of Helsinki, Belmont Report, OHRP [https://www.lifeissues.net/writers/irv/irv_214needtoknow.html]
- 116. the Comparing , Belmont , and ICH-GCP... Report Helsinki Declaration [https://www.linkedin.com/pulse/comparing-belmont-report-helsinki-declaration-ich-gcp-kiprono-mutai-xfgwf]
- 117. | PDF Belmont report [https://www.slideshare.net/slideshow/belmont-report-9856854/9856854]
- 118. : Nuremberg to GCP E6(R3) ICH [https://www.linkedin.com/pulse/gcp-nuremberg-ich-e6r3-chandramouli-r-j4ulc]
- 119. Protection of Human Subjects; Informed Consent; Proposed Rule | FDA [https://www.fda.gov/science-research/clinical-trials-and-human-subject-protection/protection-human-subjects-informed-consent-proposed-rule]
- 120. ICH E6(R3) Explained: A Guide to the 2025 GCP Update | IntuitionLabs [https://intuitionlabs.ai/articles/ich-e6-r3-gcp-guidelines-2025]
- 121. Ethical Guidelines, Federal Regulations and State Statutes | Research Compliance and Integrity [https://rci.ucmerced.edu/irb/resources/ethical-guidelines-regulations-and-statutes]
- 122. ICH GCP E6 (R3): Transformative updates make Good Clinical Practice better | ICON plc [https://www.iconplc.com/insights/blog/2025/02/13/ich-gcp-e6-r3-transformative-updates-make-good-clinical-practice-better]
- 123. Good Clinical Practice: GCP ICH E6(R3) Updates [https://research.cuanschutz.edu/comirb/home/comirb-announcements/good-clinical-practice--gcp-ich-e6(r3)-updates]
- 124. sciencedirect.com/topics/medicine-and-dentistry/ belmont - report [https://www.sciencedirect.com/topics/medicine-and-dentistry/belmont-report]
- 125. Revisiting the Belmont ’s ethical Report in... principles [https://link.springer.com/article/10.1007/s10676-018-9495-z]
- 126. Data Security Guidance for Human Subjects Research | Office of the Vice President for Research [https://ovpr.uconn.edu/services/rics/irb/data-security-guidance-for-human-subjects-research/]
- 127. Human Subjects and the General Data Protection Regulations (GDPR) – Division of Research & Creative Achievement – UMBC [https://research.umbc.edu/human-subjects-and-the-general-data-protection-regulations-gdpr/]
- 128. Digital 2025 : the state of social in media — DataReportal... 2025 [https://datareportal.com/reports/digital-2025-sub-section-state-of-social]
- 129. The State of Social | Sprout Media 2025 Social [https://sproutsocial.com/insights/the-state-of-social-media/]
- 130. Ethical implications of AI and robotics in healthcare: A review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10727550/]
- 131. CRAs - Belmont Forum [https://belmontforum.org/cras/]
- 132. Belmont Final Proposal 2025 [https://docs.google.com/document/u/0/d/1InsDH7SpKgijGB7bks3PrTK7Qb5LXwwJqzxN1xCHYbs/mobilebasic]
- 133. Blog - Beyond the Belmont Report - Bioethics Today [https://bioethicstoday.org/blog/beyond-the-belmont-report/]