Secular vs. Religious Bioethics: Foundations, Applications, and Resolutions for Biomedical Research
This article provides a comparative analysis of the foundational principles and methodological applications of secular and religious bioethical traditions.
Secular vs. Religious Bioethics: Foundations, Applications, and Resolutions for Biomedical Research
Abstract
This article provides a comparative analysis of the foundational principles and methodological applications of secular and religious bioethical traditions. Tailored for researchers, scientists, and drug development professionals, it explores the distinct epistemological roots of these frameworks, from secular principlism and moral bricolage to the doctrines of Abrahamic faiths. The analysis extends to practical application in clinical and research settings, tackles persistent conflicts such as beginning-of-life and end-of-life issues, and proposes integrative models for ethical deliberation. The goal is to equip biomedical professionals with the understanding necessary to navigate ethical dilemmas in a pluralistic world, fostering both ethical integrity and innovative progress.
Mapping the Ethical Landscape: Core Philosophies of Secular and Religious Bioethics
The field of bioethics represents a critical arena where moral philosophy meets practical decision-making in medicine and scientific research. Within this domain, a fundamental debate has emerged regarding the very nature and foundations of bioethical reasoning. This guide examines the central controversy: whether secular principlism constitutes an emerging moral tradition in its own right or represents a problematic departure from more established ethical foundations. This question carries significant implications for researchers and drug development professionals who must navigate ethical frameworks in their work, particularly as technological advancements in areas like artificial intelligence (AI) accelerate the pace of biomedical innovation [1]. The debate intersects directly with research ethics, influencing how guidelines are formulated for clinical trials, data privacy, and the implementation of new technologies.
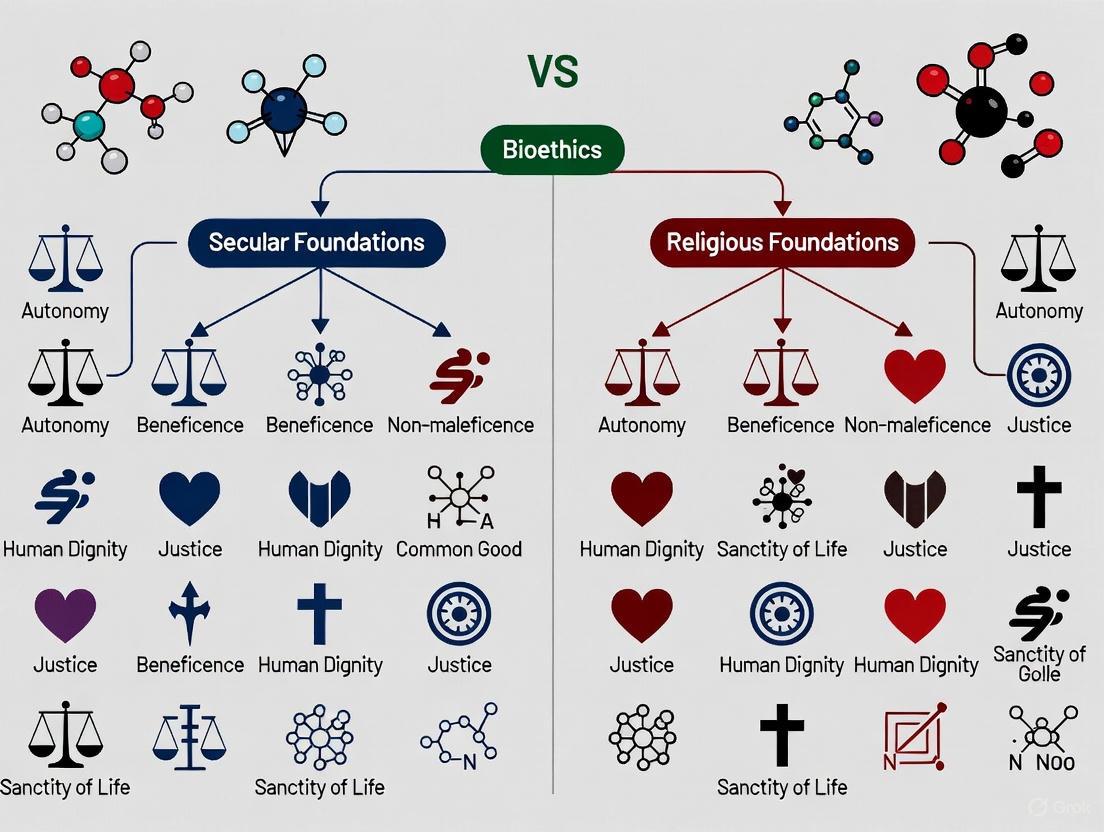
At the heart of this discussion lies secular principlism, often associated with Tom Beauchamp and James Childress's four-principle approach (autonomy, beneficence, non-maleficence, and justice), which has become a dominant framework in contemporary bioethics [2]. Critics and proponents alike are now questioning whether this framework has evolved from a mere methodological tool into a substantive moral tradition with its own distinct history, practices, and community of inquirers [3] [4]. Meanwhile, religious influences in bioethics, though historically foundational, have been increasingly marginalized in mainstream public bioethical discourse, leading to tensions about the sources of moral authority in pluralistic societies [5].
This guide provides an objective comparison of these competing perspectives, analyzing their core methodological approaches, their claims to moral authority, and their practical implications for biomedical research and drug development. By examining the theoretical frameworks and their applications, we aim to equip professionals with a nuanced understanding of how these ethical foundations shape research paradigms and policy decisions.
Analytical Framework: Core Concepts and Definitions
To navigate the complex debate between secular principlism and religious bioethics, it is essential to first establish clear definitions of the key concepts at play. The table below delineates the central terminology required for this analysis.
Table: Core Conceptual Definitions in the Bioethics "Moral Tradition" Debate
| Concept | Definition | Key Characteristics |
|---|---|---|
| Secular Principlism | A dominant framework in bioethics centered on four core principles: autonomy, beneficence, non-maleficence, and justice [2]. | Methodological focus; appeals to public reason; often described as a "common morality" framework. |
| Moral Tradition | A historically extended, socially embodied argumentative discourse through which a community of inquirers shares beliefs, practices, history, and canonical texts [3] [6]. | Historical continuity; shared narratives; community standards; canonical texts. |
| Moral Bricolage | A methodological approach that takes stock of ethical questions and uses available conceptual resources from various traditions to create solutions [6]. | Pragmatic; eclectic; draws from multiple sources (philosophies, theologies, law). |
| Public Reason | A shared framework for justifying political and ethical decisions without resorting to comprehensive personal doctrines, requiring arguments to be justifiable to all rational persons [5]. | Seeks neutrality; aims for inclusivity in pluralistic societies. |
| Religious Bioethics | Ethical deliberation grounded in the doctrines, teachings, and authority of religious traditions [5]. | Doctrinally based; draws on religious authority; may reference divine commands or theological concepts. |
Comparative Analysis: Secular Principlism as a Moral Tradition
The Emergence Thesis and Its Mechanisms
A significant development in contemporary bioethics is the argument that secular bioethics is evolving from a mere methodological approach into a substantive moral tradition. Proponents of this view, as noted in the Journal of Medical Ethics, reject the notion that bioethics should be limited to analyzing problems or clarifying concepts without offering substantive guidance. They also dismiss Enlightenment accounts based on universal, neutral rational standards. Instead, they posit that bioethics, once a discourse for various moral traditions to engage with ethical challenges, is now becoming "an emerging content-full moral tradition in its own right" [3] [4].
The mechanism driving this evolution is often described as moral bricolage. This process involves tackling pressing ethical questions by drawing upon the available conceptual resources from diverse sources—including philosophy, theology, and law—and reworking them into coherent solutions. Through repeated exercises of building consensus on specific issues, participants in bioethical discourse gradually develop shared beliefs, practices, and historical narratives. These accumulating consensus documents and canonical texts thus form the foundation of an emerging tradition [6].
The Case Against the "Moral Tradition" Designation
Critics challenge the characterization of secular bioethics as a moral tradition, arguing that this claim represents a form of intellectual hegemony. From this perspective, presenting secular bioethics as a established tradition functions as a "way of stacking the deck" in moral debates, potentially marginalizing alternative viewpoints [3]. These critics emphasize that unlike historically grounded religious traditions, secular bioethics lacks the deep historical roots and shared metaphysical commitments that characterize genuine moral traditions.
A central criticism focuses on the problem of moral authority. Detractors argue that because secular bioethics rejects both religious authority and universal rational foundations, it lacks a coherent basis for its normative claims. The field is described as "purely subjective," driven by philosophers, professors, doctors, and lawyers who offer opinions but lack any licensed or authoritative standing [3]. This subjectivity becomes problematic when the consensus reached within this community is presented as binding for public policy or for professionals who fundamentally disagree with its conclusions, such as in debates over medical conscience and euthanasia [3].
Experimental & Methodological Approaches in Ethical Analysis
Research Design in Implementation Science
While bioethics is primarily a philosophical discipline, its claims and frameworks can be empirically tested through implementation science, which studies how to effectively adopt clinical practices in real-world settings. The table below summarizes key research designs relevant to testing the application of ethical frameworks.
Table: Experimental and Quasi-Experimental Designs in Implementation Ethics Research
| Research Design | Key Features | Application in Ethics Research | Strengths | Weaknesses |
|---|---|---|---|---|
| Randomized Controlled Trial (RCT) | Random assignment; manipulation of independent variable [7]. | Testing effectiveness of specific ethics implementation strategies. | High internal validity; minimizes confounding. | Risk of contamination; may lack generalizability. |
| Cluster-Randomized Trial | Randomization at group level (clinics, sites) [7]. | Evaluating ethics training programs where individual randomization is impractical. | Reduces contamination between groups. | Requires complex analytic models; few sites can cause confounding. |
| Sequential, Multiple-Assignment Randomized Trial (SMART) | Multistage randomization based on ongoing response [7]. | Optimizing sequences of ethics interventions adapted to ongoing needs. | Informs adaptive implementation strategies. | Increased complexity and cost. |
| Stepped Wedge Design | All participants receive intervention in staggered fashion [7]. | Phased rollout of ethics guidelines across multiple sites. | Allows within-site comparisons; useful when intervention is deemed beneficial. | Complex statistical analysis; potential for time-varying confounders. |
Ethical Framework Application in AI-Driven Drug Development
The emergence of AI in drug development provides a concrete context for comparing the application of different ethical frameworks. Researchers have developed a specific ethical evaluation framework centered on the four principles of autonomy, justice, non-maleficence, and beneficence, which are applied across three critical stages of AI-driven drug development [1].
The diagram below illustrates how this principlist framework is operationalized throughout the AI drug development pipeline, mapping ethical principles to specific evaluation dimensions and their corresponding risk points.
This application of principlism demonstrates its methodological approach: translating abstract principles into concrete operational standards across a specific technological domain. The framework addresses particular deficiencies in general AI ethics guidelines by creating quantifiable operational standards for the entire drug development lifecycle [1].
The Religious-Secular Divide: Comparative Foundations
Philosophical and Methodological Differences
The debate between secular and religious approaches to bioethics represents a fundamental divide in how moral knowledge is justified and applied. The following table compares their distinct foundations and methodological approaches.
Table: Comparative Analysis of Secular and Religious Bioethics Foundations
| Aspect | Secular Bioethics | Religious Bioethics |
|---|---|---|
| Moral Foundation | Public reason; common morality [5]. | Religious doctrines and teachings [5]. |
| Epistemological Basis | Reflective equilibrium; democratic discourse [2]. | Religious authority; divine command; sacred texts. |
| Primary Methodology | Moral bricolage; consensus-building [6]. Doctrinal interpretation; theological reasoning. | |
| Scope of Application | Pluralistic public discourse [5]. | Faith communities; individuals with shared beliefs. |
| View of Principles | Guidelines emerging from human experience [2]. | Derivative of fundamental religious commitments. |
| Language Function | Tool for public justification [2]. | Expression of divinely revealed truths. |
The Challenge of Pluralism and Inclusivity
A central point of contention in this debate concerns how each approach handles moral pluralism. Secular bioethics, particularly through the framework of public reason, requires that ethical justifications be accessible to all rational persons regardless of their religious commitments. This approach aims to create an inclusive dialogue where religious and non-religious perspectives can coexist through shared reasoning [5]. However, this very framework obligates religious individuals to translate their convictions into generally acceptable arguments, which some religious scholars argue marginalizes their deeply held beliefs [5].
Proponents of religious inclusion in bioethics, such as Joseph Tham and Aasim Padela, argue that excluding religious perspectives leads to a narrow and incomplete understanding of ethical issues. They contend that religious traditions offer rich sources of moral wisdom and time-tested ethical frameworks that can enrich bioethical discourse [5]. The concept of pluriversality has been proposed as a potential middle ground, advocating for a world where different cultural and religious knowledge systems coexist without being subsumed under a singular universal framework [5]. However, critics question whether this approach can overcome ethical inconsistencies and maintain alignment with established human rights frameworks when religious doctrines conflict with them.
Essential Research Reagent Solutions: Conceptual Toolkit
Just as laboratory research requires specific reagents and tools, comparative analysis in bioethics relies on distinct conceptual frameworks and methodologies. The table below outlines this essential "research toolkit" for investigating the moral tradition debate.
Table: Essential Conceptual Toolkit for Bioethics Foundation Research
| Research 'Reagent' | Function/Purpose | Application Context |
|---|---|---|
| Public Reason Framework | Provides justifications accessible to all rational persons [5]. | Formulating public policy on controversial bioethical issues. |
| Moral Bricolage Method | Creates ethical solutions from diverse conceptual resources [6]. | Developing consensus statements on emerging technologies. |
| Principlist Framework | Offers mid-level principles for ethical analysis [1] [2]. | Clinical ethics consultation; research ethics review. |
| Comparative Tradition Analysis | Examines how different traditions approach specific ethical questions [8]. | Understanding cross-cultural perspectives in global bioethics. |
| Consensus-Building Protocols | Formal processes for reaching agreement among diverse stakeholders [6]. | Ethics guideline development; institutional policy creation. |
The debate over whether secular principlism constitutes a moral tradition carries significant practical implications for biomedical researchers and drug development professionals. The resolution of this theoretical question directly influences which ethical frameworks govern research protocols, clinical trial design, and the implementation of emerging technologies like AI in drug discovery [1].
For professionals in this field, understanding this contested terrain is crucial for navigating the ethical dimensions of their work. Each approach offers distinct resources for addressing novel ethical challenges: secular principlism provides a framework for public justification in pluralistic environments, while religious perspectives offer connection to deeply rooted moral traditions that resonate with significant portions of the global population. As bioethics continues to evolve as a discipline, the interaction between these frameworks will likely shape ethical guidelines for future scientific innovation, making this debate particularly relevant for those at the forefront of biomedical research.
The integration of religious doctrines into bioethical discourse represents a critical frontier in medical research and policy development. For researchers, scientists, and drug development professionals operating in increasingly globalized environments, understanding the foundational ethical frameworks of major religious traditions is essential for designing culturally sensitive studies and implementing equitable healthcare solutions. The Abrahamic religions—Judaism, Catholicism, and Islam—collectively influence the moral frameworks of more than half of the world's population, offering centuries-old wisdom developed through scriptural interpretation and theological reasoning [9]. These traditions provide distinctive perspectives on fundamental questions regarding the origin of human life, the protection of vulnerable populations, and the ethical boundaries of scientific intervention in natural processes.
Recent bioethical conferences, including the World Congress of Bioethics held in Qatar in 2024, have highlighted the ongoing tension between religious and secular approaches to bioethics, sparking important conversations about how to integrate diverse value systems in global health contexts [5]. This analysis offers a structured comparison of doctrinal positions from Islam, Catholicism, and Judaism on key bioethical issues relevant to pharmaceutical research and development, providing a resource for professionals navigating this complex landscape. By understanding these perspectives, researchers can foster more inclusive dialogue and develop methodologies that respect diverse patient populations while advancing scientific knowledge.
Doctrinal Positions on Key Bioethical Issues
Comparative Table of Doctrinal Positions
Table 1: Doctrinal positions of Abrahamic traditions on key bioethical issues
| Bioethical Issue | Islamic Perspectives | Catholic Perspectives | Jewish Perspectives |
|---|---|---|---|
| Foundation of Bioethics | Grounded in maslahah (public good) and Maqasid al-Shariah (objectives of Islamic law) [5] [10] | Stresses relational love and sacramentality [5] | Emphasizes covenantal responsibility [5] |
| Assisted Reproduction | Permitted within marriage; gamete donation controversial [9] | Generally prohibited; violates marital unity and natural law [9] [5] | Broadly permitted to fulfill commandment "be fruitful and multiply"; may be mandatory for infertile couples [9] |
| Gamete Donation | Generally prohibited as it confuses lineage [9] | Prohibited as it severs procreation from marital union [9] | Orthodox: prohibited as adultery; Reform: permitted with rabbinic guidance [9] |
| Embryo Status & Research | Early embryo respected; research permitted with restrictions [9] | Human dignity from conception; embryo research prohibited [9] [5] | Soul enters at 40 days; pre-implantation research generally permitted [9] |
| Role of Science | Scientific advancement complements God's creative work [9] | Cautious engagement; technology must respect natural law [9] | Humans partner with God in creation; technology positively viewed [9] |
Conceptual Framework for Religious Bioethical Reasoning
Diagram Title: Religious Bioethical Reasoning Framework
This diagram illustrates the general framework through which Abrahamic traditions derive specific bioethical positions. Each tradition begins with its scriptural sources and develops theological principles, which are then applied through distinctive interpretive methods to contemporary scientific challenges, resulting in formulated bioethical positions [9] [5].
Comparative Analysis of Doctrinal Foundations
Islamic Bioethical Framework
Islamic bioethics derives from the Quran, Sunnah, and centuries of jurisprudential reasoning, with contemporary scholarship addressing novel biomedical technologies through the lens of Maqasid al-Shariah (the higher objectives of Islamic law) [10]. Scholars like Aasim Padela have advocated for incorporating Islamic viewpoints into bioethical discourse, arguing that excluding religious perspectives marginalizes significant portions of the global population [5]. The principle of maslahah (public interest) serves as a crucial tool for addressing new bioethical challenges not explicitly mentioned in primary sources, allowing for flexible application while maintaining theological integrity [5].
On specific issues like assisted reproduction, Islamic perspectives generally permit techniques that preserve genetic lineage and marital boundaries. Gamete donation is typically prohibited due to concerns about confusing lineage, while in vitro fertilization between spouses is widely accepted [9]. The embryo is accorded moral status from early development, though not necessarily full human rights, allowing for some forms of research under specific conditions [9]. This balanced approach demonstrates how Islamic bioethics seeks to both embrace scientific progress and preserve fundamental moral values derived from revelation.
Catholic Bioethical Framework
Catholic bioethics is characterized by its consistent ethic of life, grounded in natural law theory and theological teachings about human dignity. The tradition emphasizes relational love and sacramentality, viewing the human person as created in God's image and deserving of protection from conception to natural death [5]. This foundational principle informs the Catholic perspective on assisted reproduction, which generally prohibits techniques that separate the unitive and procreative dimensions of marital intimacy [9].
The Catholic tradition maintains that human dignity is inherent from the moment of conception, resulting in strict limitations on embryonic research and any procedures that may harm or destroy human embryos [9] [5]. This position reflects the tradition's commitment to protecting the most vulnerable human lives, even at the expense of potential scientific advancements. Scholars like Joseph Tham have argued against the marginalization of religious viewpoints in bioethics, contending that excluding Catholic perspectives leads to an impoverished understanding of ethical issues in healthcare and research [5].
Jewish Bioethical Framework
Jewish bioethics operates within the framework of Halakha (Jewish law), which provides a structured approach to analyzing new technological developments through scriptural interpretation and rabbinic reasoning. The tradition emphasizes covenantal responsibility, viewing humans as partners with God in the ongoing work of creation and healing [5]. This collaborative understanding of the human-divine relationship creates a generally positive orientation toward scientific and medical innovation.
The commandment to "be fruitful and multiply" (Genesis 1:28) holds central importance in Jewish bioethical deliberations about assisted reproduction [9]. This imperative often leads to broad permission of reproductive technologies, with some authorities considering treatment mandatory for infertile couples. Jewish law incorporates a developmental view of embryonic status, with the soul not believed to enter the body until forty days after conception, allowing greater flexibility for pre-implantation research and embryo selection [9]. This approach demonstrates how Jewish bioethics balances respect for potential life with the positive value placed on bringing new life into the world.
Research Methodology and Analytical Approaches
Comparative Religious Bioethics Methodology
Diagram Title: Comparative Analysis Workflow
Research in comparative religious bioethics typically follows a structured methodology beginning with identification of authoritative scriptural sources and interpretive traditions within each faith [9]. Scholars then analyze these texts to extract core theological principles and ethical frameworks, which are applied to specific biomedical cases [5]. The comparative stage identifies areas of convergence and divergence between traditions, ultimately informing policy development that respects pluralistic values while upholding ethical standards [9] [5].
Table 2: Key research reagents and resources for religious bioethics scholarship
| Research Resource | Function & Application | Representative Examples |
|---|---|---|
| Primary Religious Texts | Foundational sources of doctrinal authority | Quran, Bible, Talmud, Torah [9] |
| Contemporary Religious Scholarship | Interpretation and application to modern technologies | Islamic: Padela; Catholic: Tham; Jewish: Feinstein, Tendler [9] [5] |
| Academic Bioethics Literature | Secular ethical frameworks and critical analysis | Journals, conference proceedings [5] |
| Case Studies & Responsa | Applied analysis of specific biomedical scenarios | Rabbinic responsa on ART; Catholic ethical directives [9] |
| Institutional Policies & Guidelines | Formal positions of religious authorities on medical ethics | Vatican directives; Islamic Fiqh Council opinions [9] |
This comparative analysis demonstrates that while Abrahamic traditions share common concerns for protecting human life and dignity, they diverge significantly in their approaches to applying these principles to contemporary biomedical challenges. These differences reflect varying theological anthropologies, interpretive methods, and understandings of humanity's role in creation. For drug development professionals and researchers, this comparative framework offers valuable insights for designing culturally competent research protocols, anticipating ethical concerns in diverse patient populations, and fostering inclusive dialogue about the moral dimensions of scientific progress.
The ongoing debate between religious and secular approaches to bioethics highlights the continued relevance of these traditions in shaping global health policy [5]. Rather than representing obstacles to scientific progress, religious bioethical frameworks offer rich moral heritage and time-tested wisdom that can contribute to more humane and equitable medical care. As biomedical technologies continue to advance, understanding these foundational perspectives will be essential for navigating the complex intersection of science, ethics, and faith in the 21st century.
The field of bioethics increasingly operates at the intersection of secular and religious frameworks, creating fundamental tensions between universalist principles that claim cross-cultural validity and faith-based approaches grounded in specific revelation traditions. This epistemological divide represents one of the most significant challenges in contemporary bioethical discourse, particularly for researchers, scientists, and drug development professionals navigating diverse ethical landscapes. Understanding these contrasting foundations is essential for productive collaboration in global health contexts and multinational research initiatives. This analysis examines the epistemological roots, methodological approaches, and practical implications of these competing frameworks to provide researchers with a structured understanding of how different ethical systems approach complex bioethical dilemmas.
Theoretical Foundations and Epistemological Frameworks
Universalist Principles in Bioethics
Universalist approaches in bioethics seek to establish ethical frameworks that transcend particular cultural or religious traditions, aiming for broadly applicable principles grounded in rational discourse. The dominant universalist framework in contemporary bioethics is principism, which organizes ethical analysis around four core principles: autonomy, beneficence, non-maleficence, and justice [11]. This approach attempts to create a common language for ethical deliberation across different value systems by focusing on procedural rationality and shared human values rather than specific metaphysical commitments.
The philosophical underpinnings of universalist bioethics trace primarily to Enlightenment rationalism and Kantian deontology, emphasizing human dignity, rights, and the capacity for reasoned moral deliberation independent of religious revelation. Proponents argue that such frameworks are necessary for pluralistic societies and global bioethical standards, particularly in contexts like international research ethics, pandemic response planning, and emerging technology governance. However, critics contend that universalist approaches often mask particular Western cultural assumptions and fail to adequately accommodate diverse moral traditions [12].
Recent developments in universalist thought include pluriversalism, which attempts to acknowledge cultural and religious diversity while maintaining cross-cultural ethical standards. This framework espouses "bioethical discourse grounded in civility, respect for law, justice, non-domination, and toleration" [12]. Yet this approach faces significant challenges regarding ethical consistency and reconciliation with established human rights frameworks when religious perspectives make claims that conflict with liberal individual rights.
Faith-Based Revelation in Bioethics
Faith-based approaches to bioethics derive their epistemological foundations from religious traditions and sacred texts rather than universal reason. These frameworks ground ethical reasoning in divine revelation, religious authority, and communal traditions that define concepts of human flourishing, moral obligations, and the proper limits of technological intervention. Unlike universalist approaches that prioritize autonomous rational deliberation, faith-based ethics typically emphasizes duties to God, community, and created order.
Major religious traditions provide comprehensive moral frameworks that address bioethical concerns through theological anthropology (understanding human nature), moral cosmology (understanding the purpose and order of creation), and specific moral commands derived from sacred texts and interpretive traditions. For example, Islamic bioethics integrates Quranic revelation, Prophetic traditions, and centuries of juridical scholarship to address contemporary medical dilemmas [10]. Similarly, Christian bioethics draws from biblical texts, theological traditions, and natural law reasoning to develop moral positions on issues from beginning-of-life to end-of-life concerns.
The methodological approach of faith-based bioethics typically involves hermeneutical engagement with authoritative texts, casuistical application of established principles to new circumstances, and communal discernment rather than individual autonomous decision-making. These approaches recognize moral limits to technological intervention based on concepts of divine sovereignty, natural order, or human dignity understood through theological lenses. For researchers, understanding these foundations is crucial when engaging religious communities or working in contexts where religious values significantly influence healthcare policies and research ethics.
Table: Comparative Epistemological Foundations
| Aspect | Universalist Principles | Faith-Based Revelation |
|---|---|---|
| Primary Source of Knowledge | Human reason, empirical evidence, rational discourse | Divine revelation, sacred texts, religious authority |
| Moral Justification | Principles derived through logical consistency and cross-cultural validation | Commands and values revealed through sacred sources and tradition |
| Scope of Application | Theoretical global applicability regardless of cultural context | Primarily within religious community, with varying engagement with pluralistic society |
| Key Conceptual Frameworks | Principism (autonomy, beneficence, non-maleficence, justice) | Theological anthropology, natural law, divine command theory |
| Methodological Approach | Rational deliberation, procedural ethics, consensus-building | Hermeneutics, casuistry, communal discernment |
Methodological Approaches and Analytical Frameworks
Research Methodologies for Ethical Analysis
The contrasting epistemological foundations of universalist and faith-based approaches necessitate different methodological frameworks for ethical analysis. Understanding these methodologies is essential for researchers conducting ethical analyses or engaging with diverse ethical perspectives in their work.
Universalist bioethics employs several characteristic methodological approaches. Principle-based analysis systematically applies the four principles of autonomy, beneficence, non-maleficence, and justice to ethical dilemmas, often using them as a framework for case analysis [11]. Empirical methods in bioethics incorporate quantitative and qualitative research—including surveys, content analysis, focus groups, and individual interviews—to understand ethical dimensions of healthcare practices and policies [11]. These methodological approaches prioritize transparency, replicability, and rational justification accessible to people across different cultural and religious backgrounds.
Faith-based methodologies employ distinctly different approaches to ethical analysis. Textual hermeneutics involves careful interpretation of sacred texts and religious traditions to derive ethical guidance for contemporary issues. Tradition-based reasoning engages with centuries of religious scholarship and ethical deliberation within the tradition, applying established principles to new circumstances through analogical reasoning. Virtue ethics emphasizes character formation and spiritual development as foundational to ethical discernment, focusing on the moral qualities of the decision-maker rather than just the act itself. These methodologies recognize religious authority and spiritual discernment as valid ways of knowing, complementing or sometimes challenging purely rational approaches.
Table: Comparative Analytical Methodologies
| Methodological Approach | Universalist Application | Faith-Based Application |
|---|---|---|
| Case Analysis | Systematic application of mid-level principles | Casuistical reasoning from paradigmatic cases in religious tradition |
| Textual Analysis | Critical engagement with philosophical and legal texts | Hermeneutical engagement with sacred texts and interpretive traditions |
| Empirical Inquiry | Social science research on attitudes and outcomes | Study of religious community practices and beliefs |
| Deliberative Process | Democratic discourse seeking overlapping consensus | Communal discernment respecting religious authority |
| Normative Justification | Appeals to shared rationality and public reason | Appeals to religious authority and revealed truth |
Conceptual Mapping of Ethical Frameworks
The diagram below visualizes the logical relationships and decision pathways within universalist and faith-based bioethical frameworks, highlighting their contrasting structures and focal points:
This conceptual mapping illustrates how universalist frameworks employ a linear analytical process focused on principle application, while faith-based approaches employ a hermeneutical circle engaging authoritative sources and interpretive communities. For researchers, understanding these different pathways is essential when anticipating how various stakeholders will approach ethical dilemmas in research settings.
Experimental Protocols for Ethical Analysis
Protocol 1: Principism-Based Ethical Analysis
The principism framework developed by Beauchamp and Childress provides a systematic methodology for ethical analysis that dominates contemporary secular bioethics [11]. This experimental protocol outlines a standardized approach for applying this framework to bioethical dilemmas, particularly useful for research ethics committees and policy development groups.
Materials and Methodology: The primary materials required include the case description with all relevant factual details, reference materials on the four principles (autonomy, beneficence, non-maleficence, and justice), and documentation of relevant legal and policy contexts. The methodology proceeds through six systematic phases: (1) Case Fact-Finding - gathering all relevant medical, social, and contextual information; (2) Principle Identification - determining which principles are relevant to the case; (3) Specification - translating abstract principles into concrete moral norms for the specific context; (4) Balancing - resolving conflicts between principles through weighting and prioritization; (5) Justification - providing reasoned arguments for the chosen resolution; and (6) Documentation - recording the analytical process and outcome for transparency and review.
Application Context: This methodology is particularly valuable in pluralistic settings like institutional review boards, hospital ethics committees, and public policy development, where participants may hold diverse moral commitments. The framework provides a common vocabulary and structured process for ethical deliberation without requiring agreement on foundational metaphysical questions. Research has shown this approach increases systematic reasoning and transparency in ethical decision-making, though critics note it may obscure deeper philosophical disagreements and cultural biases embedded in the principles themselves.
Protocol 2: Religious Tradition-Based Ethical Analysis
Faith-based ethical analysis follows a different experimental protocol grounded in engagement with religious sources and interpretive communities. This protocol outlines a systematic approach for conducting ethical analysis within a religious tradition, using Islamic bioethics as exemplified by Dr. Padela's work [10] as a model, though adaptable to other religious traditions.
Materials and Methodology: Required materials include sacred texts (e.g., Quran, Bible, Torah), interpretive traditions (commentaries, scholarly works), case precedents from the religious tradition, and consultation with religious authorities. The methodology involves five iterative phases: (1) Textual Exegesis - close reading of relevant scriptural passages; (2) Tradition Engagement - study of historical interpretations and applications; (3) Principle Extraction - identifying overarching ethical principles from specific texts and cases; (4) Contemporary Application - applying derived principles to modern biomedical contexts through analogical reasoning; and (5) Communal Validation - testing interpretations with religious community and authorities.
Application Context: This methodology is essential when researching or implementing healthcare interventions in religious communities, developing culturally sensitive research protocols, or understanding religious objections to certain medical technologies. The protocol recognizes that within religious traditions, ethical reasoning is not merely an individual cognitive process but a communal practice of discernment. For researchers, understanding this process facilitates more meaningful engagement with religious perspectives rather than dismissing them as simply irrational or obstructive.
Research Reagent Solutions for Ethical Analysis
The table below details key conceptual tools and resources essential for conducting rigorous research in comparative bioethics, particularly when analyzing universalist and faith-based approaches:
Table: Essential Research Resources in Comparative Bioethics
| Research Tool | Primary Function | Application Context |
|---|---|---|
| Principism Framework | Structured ethical analysis using four core principles | Secular bioethics deliberation, policy development, clinical ethics consultation |
| Religious Textual Databases | Access to sacred texts and traditional commentaries | Understanding faith-based perspectives on specific bioethical issues |
| Empirical Research Methods | Quantitative and qualitative study of ethical beliefs and practices | Investigating stakeholder perspectives, evaluating ethical outcomes [11] |
| Hermeneutical Analysis Protocols | Systematic interpretation of religious texts and traditions | Faith-based bioethics analysis, engaging religious communities |
| Comparative Ethics Rubrics | Structured comparison of different ethical frameworks | Cross-cultural research, multinational policy development |
| Case Repository Databases | Collections of paradigmatic cases with analyses | Ethics education, case-based reasoning, precedent consultation |
These research tools enable systematic investigation of the epistemological roots and practical implications of different bioethical frameworks. For researchers working in global health or multinational clinical trials, familiarity with these resources is essential for navigating diverse ethical landscapes and anticipating potential conflicts between universalist aspirations and particular religious commitments.
Comparative Analysis and Research Implications
Empirical Findings and Conceptual Tensions
Research reveals significant tensions between universalist and faith-based approaches in bioethics, with important implications for scientific practice and policy development. The 2024 World Congress of Bioethics in Qatar highlighted these tensions, particularly regarding the proper role of religious values in bioethical discourse [12]. Proceedings demonstrated persistent challenges in reconciling universal human rights frameworks with religious traditions that may hold divergent views on issues like gender equality, sexual orientation, or religious authority.
Empirical studies of bioethical deliberation reveal that universalist frameworks tend to prioritize individual autonomy, informed consent, and personal liberty, while faith-based approaches often emphasize community wellbeing, traditional values, and moral constraints on individual choice. These differences manifest practically in areas like end-of-life decision-making, reproductive technologies, and genetic manipulation. For example, where universalist frameworks might focus primarily on patient self-determination in cessation of treatment decisions, religious approaches might emphasize the sanctity of life or divine sovereignty over life and death.
The conceptual mapping below illustrates how these epistemological differences manifest in practical decision-making contexts, particularly showing the different weighting given to various ethical considerations:
Research Applications and Practical Implications
For researchers and drug development professionals, these epistemological differences have significant practical implications. Research protocol development must navigate tensions between universal ethical standards and particular religious values, especially in multinational trials. Informed consent processes may require adaptation to accommodate different understandings of autonomy, family authority, and religious obligations. Emerging technologies like genetic engineering, artificial intelligence in healthcare, and neuroenhancement present particularly challenging frontiers where universalist and faith-based perspectives often diverge sharply.
Successful navigation of these tensions requires methodological flexibility and conceptual clarity about the epistemological foundations of different ethical positions. Researchers should implement structured approaches to ethical analysis that explicitly acknowledge their underlying frameworks while remaining open to constructive engagement with alternative perspectives. This includes developing capacity for religious literacy in research ethics, understanding how different traditions approach fundamental questions of human dignity, moral authority, and the proper scope of technological intervention.
The epistemological divide between universalist principles and faith-based revelation represents a fundamental tension in contemporary bioethics with significant implications for research practice and policy development. Universalist approaches grounded in rational discourse and principle-based analysis provide important frameworks for pluralistic deliberation but risk underestimating the legitimate role of religious perspectives in ethical reasoning. Faith-based approaches rooted in divine revelation and religious tradition offer comprehensive moral frameworks for their communities but face challenges in engaging pluralistic discourse without either dilution or domination.
For researchers, scientists, and drug development professionals, navigating this landscape requires both conceptual clarity about these contrasting epistemological foundations and practical methodological skills for engaging diverse ethical perspectives. Rather than seeking simplistic resolution of these tensions, productive way forward involves developing capacity for ethical bilingualism—understanding and respecting both universalist and faith-based approaches while clearly acknowledging their distinctive epistemological commitments. This approach fosters more meaningful engagement with ethical diversity while maintaining intellectual integrity about fundamental differences that cannot be easily reconciled through procedural solutions alone.
The Emergence of 'Moral Bricolage' in Secular Public Bioethics
This analysis examines the conceptual framework of 'moral bricolage' as a defining characteristic of contemporary secular bioethics. Drawing upon recent scholarly literature, we explore how this approach synthesizes diverse philosophical, theological, and legal traditions to address complex ethical challenges in medicine and life sciences. By comparing the methodological foundations of secular and religious bioethics, we identify distinctive strengths and limitations of each paradigm, with particular attention to their applications in pharmaceutical development and clinical practice. The findings demonstrate that moral bricolage represents both an adaptive response to moral pluralism and a potentially contested authority in public bioethics discourse.
The field of secular bioethics operates within a context of significant moral pluralism, where diverse value systems coexist without a shared metaphysical foundation. Moral bricolage has emerged as a central theoretical framework describing how bioethicists navigate this complexity by creatively assembling available conceptual resources from multiple traditions to address contemporary ethical challenges [6]. This approach stands in contrast to both proceduralist models that merely analyze moral problems without offering substantive guidance, and Enlightenment models that seek universal rational principles undeniable by any reasonable person [13].
The theoretical underpinnings of moral bricolage respond directly to Alasdair MacIntyre's "disquieting suggestion" that contemporary moral language suffers from such profound disorder that securing authoritative moral guidance may be impossible [6]. Jeffrey Stout's conceptualization of moral bricolage in Ethics After Babel offers a constructive alternative to MacIntyre's pessimistic assessment, suggesting that ethical guidance can be developed through a process of gathering and reworking available conceptual resources from various traditions—including philosophies, theologies, and legal frameworks [6]. This methodological approach has gained particular traction in public bioethics, which aims to provide moral guidance on questions of public policy, research ethics, and clinical practice in pluralistic societies [6].
Table 1: Theoretical Foundations of Moral Bricolage
| Conceptual Element | Description | Primary Source |
|---|---|---|
| Moral Pluralism | Context of diverse, competing moral frameworks without shared metaphysical foundations | [14] |
| Conceptual Resource Gathering | Drawing upon philosophies, theologies, laws from multiple traditions | [6] |
| Creative Reconfiguration | Adapting and reworking resources to address novel bioethical challenges | [6] |
| Tradition Formation | Developing shared practices, histories, and canonical texts through repeated application | [6] |
Comparative Analysis: Secular versus Religious Bioethical Foundations
The emergence of moral bricolage in secular bioethics must be understood in contrast to religious approaches to bioethical reasoning. Where religious bioethics typically begins with established theological premises and authoritative texts, secular bioethics employs pragmatic integration of multiple moral frameworks without privileging specifically religious sources [14]. This fundamental methodological difference generates distinctive strengths and limitations for each approach.
Secular Bioethics: Universalism and Its Constraints
Secular bioethics is characterized by its aspiration to moral universalism—the development of ethical frameworks acceptable to individuals regardless of religious affiliation or ideological commitment [14]. This universalist ambition manifests in bioethics' foundational precept of "respect for persons," which demands that religious beliefs not be dismissed as merely irrational while simultaneously making it difficult to include religion as a serious element in moral decision-making [14]. This tension inevitably leads to what one analyst terms the "ghettoization" of religion, whereby we find distinct Catholic, Jewish, and Islamic bioethics traditions operating alongside but separate from mainstream secular bioethics [14].
A significant limitation of secular bioethics identified by critics is its movement from "thick" to "thin" ethical reasoning [14]. Early bioethics engaged with substantive questions about human nature and the meaning of life, drawing on both theological and philosophical insights. In its contemporary bureaucratic form, however, bioethics has largely shifted toward thinner, more formal concerns with guidelines and regulations [14]. This thinning process has created a conceptual vacuum regarding existential questions, particularly those surrounding suffering and its meaning. As anthropologist Arthur Kleinman observes, bioethics has largely ceded inquiries into the nature and meaning of suffering to religious traditions, with many professional ethical volumes not even including "suffering" in their indices [14].
Religious Bioethics: Teleology and Tradition
Religious approaches to bioethics differ fundamentally in their retention of teleological perspective—concern with ultimate purpose and meaning that transcends immediate practical considerations [14]. Where secular bioethics typically brackets questions of ultimate meaning, religious frameworks directly address what Kleinman identifies as patients' struggles "to make sense of illness with respect to great cultural codes that offer coherent interpretations of experience" [14]. This teleological orientation enables religious bioethics to engage with what Cassell identifies as the "paradox of suffering"—the recognition that while suffering is inherently negative, it can also reveal greater depths of human experience and meaning, leading to enriched understanding and greater concern for others [14].
The historical development of Western bioethics further complicates the secular-religious distinction. As scholar Yusuf Lenfest notes, the methods of ethical analysis dominant in secular bioethics are themselves "a direct result of a particular European and Western epistemology, which, in turn, has its own Christian origins" [15]. The theories that emerged from the Enlightenment represented a "secularization of the Christian ethic" rather than a complete break from religious moral reasoning [15]. This historical continuity suggests that the relationship between secular and religious bioethics may be more complex than a simple binary opposition.
Table 2: Key Distinctions Between Secular and Religious Bioethics
| Dimension | Secular Bioethics | Religious Bioethics |
|---|---|---|
| Moral Foundation | Reason, principles, consensus | Revelation, tradition, authority |
| Scope of Concern | Primarily "thin" procedural and regulatory questions | Includes "thick" existential and teleological questions |
| Approach to Suffering | Often ignored or addressed procedurally | Central concern with paradoxical meaning and value |
| Methodology | Moral bricolage, principlism | Textual interpretation, traditional application |
| Community Formation | Emerging professional tradition with shared practices | Established religious communities with shared beliefs |
Moral Bricolage in Practice: Applications to Medicines Development
The theoretical framework of moral bricolage finds practical application in the evolving field of pharmaceutical medicine and medicines development. The increasingly complex nature of medical interventions—particularly advanced therapies like gene and cell treatments—requires collaboration among multidisciplinary teams including medically qualified physicians, natural scientists, molecular biologists, geneticists, device engineers, psychologists, and bioethicists [16] [17]. This professional diversity necessitates ethical frameworks capable of integrating perspectives from multiple disciplinary traditions.
Ethical Frameworks for Multidisciplinary Teams
Traditional ethical guidelines for human subjects research have placed primary responsibility on medically qualified physicians, consistent with the Declaration of Helsinki's statement that "It is the duty of physicians who are involved in medical research to protect the life, health, dignity, integrity, right to self-determination, privacy and confidentiality of personal information of research subjects" [17]. However, the growing complexity of modern drug development challenges this physician-centered model. As one analysis notes, in contemporary multidisciplinary teams, "the physicians work as team members, with special ethical responsibility to care for the well-being of the patients," but may lack the specialized knowledge to fully evaluate all aspects of complex interventions [17].
This recognition has led to the development of expanded ethical frameworks that explicitly address the shared ethical responsibility of all team members in medicines development. The International Federation of Associations of Pharmaceutical Physicians (IFAPP) has updated its International Code of Ethical Conduct to create an International Ethics Framework for Pharmaceutical Physicians and Medicines Development Scientists that encompasses both medically qualified and non-medically qualified professionals [17]. This framework acknowledges that all team members influence outcomes and subject safety, and thus must share ethical responsibility, while recognizing that physicians retain overriding responsibility for subject well-being [17].
Ethical Challenges in Translational Medicine
The process of translational medicine—bridging non-clinical studies with early human trials—illustrates both the necessity and challenges of moral bricolage in pharmaceutical development. Problems with reproducibility in basic science research present significant ethical concerns for subsequent human trials. Studies indicate that only 6% of landmark studies published in prestigious journals provide sufficiently robust data to reliably drive human medicines development programs, with industrial R&D experts reporting inability to reproduce approximately 50% of academic publications on potential therapeutic targets [17].
These reproducibility issues create tangible risks for human subjects, exemplified by tragic phase I trial incidents involving compounds like TGN-1412 and BIA 10-2474 [17]. Addressing these challenges requires ethical integration of expertise across the translational continuum, with academic scientists adopting more rigorous research methods similar to those used in clinical trials, and all team members sharing responsibility for ensuring valid and reliable translation from preclinical to clinical studies [17].
Table 3: Core Conceptual Resources for Moral Bricolage in Bioethics
| Resource Category | Specific Components | Function in Ethical Analysis |
|---|---|---|
| Philosophical Frameworks | Principlism (autonomy, beneficence, non-maleficence, justice); Virtue ethics; Deontological approaches; Utilitarian calculus | Provide systematic methods for identifying and weighing ethical considerations |
| Theological Traditions | Religious perspectives on suffering; Concepts of human dignity; Teleological understandings of human flourishing | Offer resources for addressing existential questions and meaning |
| Legal/Regulatory Frameworks | Declaration of Helsinki; Belmont Report; National regulations; Professional codes of conduct | Establish minimal standards and procedural requirements |
| Empirical Research Methods | Reproducibility standards; Clinical trial methodologies; Qualitative approaches to suffering | Provide evidence base for ethical evaluation and decision-making |
| Cross-Cultural Perspectives | Islamic bioethics; Jewish medical ethics; Catholic social teaching; Various indigenous knowledge systems | Expand conceptual resources beyond Western frameworks |
Critical Perspectives and Controversies
The claim that secular bioethics constitutes an emerging "moral tradition" has generated significant debate within the field. Critics contend that this characterization represents a form of conceptual hegemony that marginalizes alternative perspectives, particularly religious viewpoints [13]. As one commentator argues, "Public-advocacy-focused secular bioethics is largely progressive politics covered with a veneer of expertise" rather than a genuine moral tradition with deep historical roots [13]. This perspective highlights the relatively recent emergence of bioethics as a formal field of inquiry and the absence of licensing or standardized credentialing for bioethicists.
A particular concern raised by critics involves the potential for orthodoxy enforcement under the guise of consensus development. The example of medical conscience exemptions illustrates this tension, where alleged consensus positions may in reality represent agreements among like-minded bioethicists that impose compliance requirements on professionals with divergent moral commitments [13]. In some jurisdictions, such as Ontario, Canada, policies requiring physicians to provide "effective referral" for services they consider morally objectionable have created significant conflicts for professionals whose ethical frameworks prohibit certain medical interventions [13].
Defenders of the moral tradition concept respond that bioethics has indeed developed shared practices, historical narratives, and canonical texts that constitute a tradition in the sociological sense [6]. They acknowledge ongoing disagreement within the field but see such debate as characteristic of living traditions rather than evidence against tradition status [6]. This perspective views moral bricolage not as arbitrary eclecticism but as a disciplined methodology for addressing novel ethical challenges in rapidly evolving technological contexts.
The emergence of moral bricolage as a characteristic methodology in secular bioethics represents a significant adaptation to the conditions of moral pluralism in contemporary societies. This approach enables practical ethical guidance despite deep metaphysical disagreements by creatively synthesizing resources from multiple traditions. However, this very adaptability raises questions about the epistemic authority of bioethical recommendations and their capacity to address fundamental questions of human meaning and suffering.
For researchers and professionals in pharmaceutical medicine and drug development, recognition of this ethical methodology has practical implications for team composition, training, and ethical oversight. The increasingly multidisciplinary nature of medicines development necessitates ethical frameworks that can integrate diverse professional perspectives while maintaining fundamental commitments to human subject protection and scientific integrity [17]. Future research should explore more systematically how moral bricolage functions in specific drug development contexts and how its creative potential might be balanced against the need for consistent ethical standards across research settings.
The ongoing dialogue between secular and religious approaches to bioethics continues to enrich both traditions, with secular bioethics offering procedures for navigating moral disagreement while religious perspectives maintain vital concerns with ultimate meaning and purpose. Rather than representing competing alternatives, these approaches may function as complementary resources for addressing the complex ethical challenges posed by emerging medical technologies.
From Theory to Practice: Applying Ethical Frameworks in Clinical and Research Settings
In biopharmaceutical development, specification limits are critical numerical limits or ranges that define the acceptable quality of a drug substance or product, serving as the final gatekeeper for market release [18]. Establishing these specifications is not merely a technical exercise but one deeply embedded in ethical reasoning. The process balances the imperative for robust, safe, and efficacious medicines with complex moral considerations about resource allocation, risk, and societal benefit. This article examines how different bioethical frameworks—secular and religious—inform the methodologies for setting acceptance criteria, shaping the underlying values and risk tolerances that guide development decisions. These foundations influence how scientists and regulators define what constitutes a "good" and "acceptable" product, ultimately determining the control strategies for manufacturing processes that affect global patient populations [18].
Comparative Analysis of Secular and Religious Bioethical Frameworks
The field of bioethics provides diverse lenses for moral decision-making. The dominant secular approach and various religious perspectives offer distinct rationales that can influence technical standards.
Table 1: Comparison of Secular and Religious Bioethical Foundations
| Aspect | Secular Bioethics | Religious Bioethics (e.g., Catholic, Islamic, Jewish) |
|---|---|---|
| Primary Foundation | Principles derived from public reason, philosophy, and law [5] | Doctrinal teachings, sacred texts, and theological traditions [5] |
| Core Principles | Autonomy, beneficence, nonmaleficence, justice [19] | Stewardship, care for creation, sanctity of life, common good [20] |
| Moral Authority | Rational justification and evidence accessible to all, irrespective of belief [5] | Religious authority and revealed truths [5] [14] |
| Approach to Specification Setting | Risk-based, probabilistic (e.g., pre-defined out-of-specification probabilities) [18] | Duty-based, emphasizing precaution and the protection of life [20] |
| View on Technology & Innovation | Often embraces technological solutions guided by risk-benefit analysis [5] | Cautious, assessing compatibility with divine order and human dignity [21] |
| Goal in Biopharmaceutical Development | Consistent quality, patient safety, and efficacy through controlled processes [18] | Healing as a moral act, production of medicines aligned with a sacred view of life [20] |
A significant debate in contemporary bioethics revolves around pluriversalism, a framework that seeks to create "a world where many worlds fit" by embracing global cultural and religious diversity [22]. Proponents argue that marginalizing religious perspectives unfairly privileges secular language and methods, making bioethics less relevant to a majority of the world's population that identifies as religious [22]. Critics, however, caution that a pluriversal approach may struggle with significant ethical inconsistencies and can be hard to reconcile with universal human rights, particularly when religious doctrines conflict with principles of equality or individual autonomy [5]. This tension is highly relevant to global biopharmaceutical development, where companies must navigate diverse ethical landscapes to establish universally acceptable product specifications.
Quantitative Methods for Setting Acceptance Criteria
The establishment of specifications relies on robust statistical methods applied to process data. The following quantitative approaches are foundational.
Probabilistic Tolerance Intervals
A common method for setting acceptance criteria involves calculating probabilistic tolerance intervals [23]. This approach acknowledges the uncertainty that arises when estimating the mean (μ) and standard deviation (σ) from a limited sample of data. Instead of simply using the sample mean ± a multiple of the standard deviation, it makes statements of the form: "We are 99% confident that 99% of the measurements will fall within the calculated tolerance limits" [23]. The size of the multiplier (M) depends on the desired confidence level, the proportion of the population to be covered, and, critically, the sample size. Smaller sample sizes require larger multipliers to account for greater uncertainty [23].
Table 2: Sigma Multipliers (M) for One-Sided Tolerance Intervals (99% Confidence, 99.25% Coverage) [23]
| Sample Size (N) | Sigma Multiplier (M) |
|---|---|
| 10 | 4.43 |
| 30 | 3.65 |
| 62 | 3.46 |
| 100 | 3.36 |
| 200 | 3.23 |
For example, with a sample size of 62, a mean of 245.7 μg/g, and a standard deviation of 61.91 μg/g, the upper specification limit would be calculated as 245.7 + (3.46 * 61.91) = 460 μg/g [23].
Process Capability Indices
Process capability indices are metrics that quantify how consistently a manufacturing process produces outputs within specifications [24]. The most common indices, Cpk and Ppk, compare the spread of the process variation to the width of the specification limits. A higher index value indicates a lower probability of an out-of-specification (OoS) outcome. For a centered process with two-sided specification limits, a Cpk of 1.0 corresponds to an OoS risk of approximately 0.27% [24]. These indices are vital for quantifying process performance and justifying specification limits to regulators.
Advanced and Integrated Approaches
Conventional methods like the ±3 standard deviations (3SD) approach have a key limitation: they reward poor process control (high variation leads to wider, easier-to-meet limits) and punish good control (low variation leads to tighter limits) [18]. A more advanced methodology is Integrated Process Modeling (IPM). In an IPM, each unit operation (e.g., a chromatography step) is described by a statistical model that predicts its output quality based on input material attributes and process parameters [18]. These unit operation models are then linked together. Using Monte Carlo simulation, random variability is incorporated, allowing developers to predict the final drug substance quality and its probability of meeting specifications [18]. This allows for the derivation of specification-driven intermediate acceptance criteria that ensure a pre-defined out-of-specification probability while considering real-world manufacturing variability [18].
Experimental Protocols for Specification Setting
Protocol for Deriving Acceptance Limits Using Tolerance Intervals
This protocol provides a step-by-step method for establishing specification limits based on process data [23].
- Data Collection and Distribution Testing: Collect data from multiple pre-production or early production batches (N > 30 is desirable). Test the data for normality using a statistical test like the Anderson-Darling test. A p-value greater than 0.05 suggests the data is not significantly different from a normal distribution.
- Handle Outliers: Review the data for outliers using a test like Grubb's test. Potential outliers should be investigated for recording errors or special cause variation. They should not be removed without a documented rationale.
- Calculate Sample Statistics: Calculate the sample mean (x̄) and sample standard deviation (s).
- Select Sigma Multiplier: Based on the sample size (N), the desired confidence level (e.g., 99%), and the desired population coverage (e.g., 99.25%), select the appropriate sigma multiplier (M) from a reference table [23].
- Calculate Specification Limit: For a one-sided upper limit: USL = x̄ + M * s. For a one-sided lower limit: LSL = x̄ - M * s. For a two-sided interval, use the appropriate multiplier (MUL) for the range: (x̄ - MUL * s) to (x̄ + MUL * s).
Protocol for an Integrated Process Model (IPM) Case Study
This methodology leverages knowledge across multiple manufacturing steps for a more robust control strategy [18].
- Process Segmentation and Data Generation: Define the unit operations in the manufacturing process (e.g., harvest, capture chromatography, viral inactivation). For each unit operation, generate data through small-scale studies like Design of Experiments (DoE) or one-factor-at-a-time (OFAT) studies, varying critical process parameters (CPPs) and monitoring critical quality attributes (CQAs).
- Model Building: For each unit operation, build a multilinear regression model. The model should predict the output CQAs (e.g., HCP level, monomer purity) based on the input material attributes and the set-points of the CPPs.
- Model Concatenation: Link the unit operation models sequentially. The predicted output of one unit operation becomes the input for the subsequent unit operation's model.
- Monte Carlo Simulation: Run simulations on the integrated model. Incorporate random variability around process parameter set-points to reflect expected manufacturing variation. Run thousands of iterations to predict the distribution of the final drug substance CQAs.
- Derive Intermediate Acceptance Criteria (iACs): Using the simulation results, determine the range of CQA values at each intermediate process step that ensures the final drug substance will meet its specification limits with a sufficiently high probability (e.g., >99.73%). These ranges become the scientifically justified iACs.
The following workflow diagram illustrates the key stages of this advanced methodology.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Specification Studies
| Item | Function in Experimental Protocol |
|---|---|
| Monoclonal Antibody (mAb) Production System | Serves as the candidate biologic product for process development and validation case studies [18]. |
| Host Cell Protein (HCP) ELISA Kit | An analytical procedure used to monitor the clearance of a host-related impurity, a Critical Quality Attribute (CQA), across downstream unit operations [18]. |
| Size-Exclusion Chromatography (UP-SEC) | An analytical procedure used to monitor product-related impurities (e.g., aggregates) and purity (e.g., monomer), which are CQAs [18]. |
| Chromatography Resins | Used in unit operations designed for the purification and clearance of impurities; their performance is modeled in the Integrated Process Model [18]. |
| Statistical Software (e.g., JMP, Minitab) | Used for statistical analysis, including normality testing (Anderson-Darling), outlier detection (Grubb's test), calculation of tolerance intervals, and building regression models for the IPM [18] [23] [24]. |
The establishment of specifications in biopharmaceutical development is a critical activity that sits at the intersection of rigorous science and profound ethics. While statistical tools like tolerance intervals and process capability indices provide the technical backbone for setting acceptance criteria [23] [24], the underlying values and risk tolerances are shaped by broader bioethical frameworks. The ongoing dialogue between secular and religious bioethics, particularly through lenses like pluriversalism, challenges the field to create more inclusive and globally relevant moral infrastructures [5] [22]. For researchers and drug development professionals, recognizing this interplay is essential. It fosters a more holistic approach to process validation, where technical excellence is guided by a commitment to justice, stewardship, and the sacred dignity of human life, ultimately ensuring that medicines are not only effective and safe but also developed in an ethically sustainable manner.
Clinical ethics provides a structured approach to navigating complex moral dilemmas that arise at the crossroads of medical technology, human values, and life-and-death decisions. This comparative analysis examines ethical frameworks governing two critical domains: end-of-life care and organ transplantation. These domains represent particularly challenging arenas where advances in medical capabilities have created unprecedented ethical questions that blend philosophical foundations with practical clinical applications [25] [14]. The growing gap between organ supply and demand, coupled with an aging population facing prolonged end-of-life trajectories, has intensified the need for robust ethical frameworks that can guide practitioners, patients, and policymakers [26] [27].
Within bioethics, a fundamental tension exists between secular and religiously-grounded approaches to moral reasoning [14] [15]. Secular bioethics emerged in the late 20th century as a response to moral pluralism, seeking to develop "a set of principles and a method for moral decision-making acceptable to all, regardless of one's religion or ideology" [14]. Meanwhile, religious perspectives continue to shape ethical reasoning, with traditions such as Catholicism, Judaism, and Islam maintaining distinctive approaches to biomedical ethics while sharing common moral foundations with secular frameworks [15]. This analysis examines how these different foundational approaches manifest in concrete clinical contexts and governance models.
Comparative Ethical Frameworks: Secular and Religious Foundations
Philosophical Underpinnings and Key Principles
Table 1: Comparison of Secular and Religious Bioethical Foundations
| Aspect | Secular Bioethics | Religious Bioethics |
|---|---|---|
| Moral Source | Human reason, empirical evidence, and rational deliberation [14] | Divine revelation, sacred texts, and religious tradition [15] |
| Primary Principles | Autonomy, beneficence, nonmaleficence, justice [26] | Dignity of the person, charity, stewardship, common good [15] |
| Approach to Suffering | Focus on prevention and relief through clinical intervention [14] | Potential meaning in suffering; spiritual response alongside physical care [14] |
| Decision-Making Process | Principlism, casuistry, consensus-based deliberation [27] | Authority of religious tradition, consultation with spiritual leaders [15] |
| Scope of Application | Universalist aspirations across diverse populations [14] | Particular to religious communities with potential for broader engagement [15] |
Secular bioethics is characterized by its systematic application of ethical principles that are theoretically accessible to all rational persons regardless of their metaphysical commitments. As one analysis notes, "Bioethics was born in a context characterized by moral pluralism and shifting ideas about the nature of moral authority; it was, and is, an effort to develop a set of principles and a method for moral decision-making acceptable to all, regardless of one's religion or ideology" [14]. This universalist aspiration, however, faces challenges in fully addressing existential questions of meaning that often arise in clinical contexts, particularly at the end of life [14].
Religious bioethics, while diverse across traditions, typically grounds moral reasoning in theological frameworks and understandings of human nature and purpose. The Catholic tradition, for instance, emphasizes that "the order of things must be subordinate to the order of persons, and not the other way around" [27], establishing a fundamental priority for human dignity over utilitarian calculations. While distinctive in their metaphysical foundations, religious perspectives often arrive at similar ethical positions as secular frameworks through different reasoning pathways, creating potential for collaboration in clinical settings [15].
Ethical Decision-Making Workflows
The following diagram illustrates the comparative decision-making processes in clinical ethics consultation, highlighting parallel pathways for secular and religious approaches:
Ethical Models in End-of-Life Care
Foundational Principles and Clinical Applications
End-of-life care presents distinctive ethical challenges as medical technology has transformed the dying process, creating complex decisions about limiting, withholding, or withdrawing treatments [26]. The universally recognized ethical principles guiding end-of-life care include autonomy, beneficence, nonmaleficence, and justice, with fidelity (truth-telling) representing an additional crucial principle [26]. These principles provide a framework for navigating specific clinical ethical challenges including resuscitation decisions, mechanical ventilation, artificial nutrition and hydration, terminal sedation, and requests for physician-assisted suicide or euthanasia where legally permitted [26].
Patient autonomy represents a cornerstone principle, implemented through advance care planning mechanisms including living wills, healthcare proxies, and "do not resuscitate" (DNR) orders [26]. These instruments allow patients to maintain control over medical decisions even after losing decision-making capacity. As one analysis notes, "Each patient's 'right to self-determination' requires informed consent in terms of medical intervention and treatment. A patient has both the 'right to demand the termination of treatment' (e.g., the discontinuation of life support) and the 'right to refuse treatment altogether'" [26]. However, this autonomy is not absolute and must be balanced against considerations of beneficence (promoting patient well-being) and nonmaleficence (avoiding harm) [26].
Comparative Institutional Approaches
Table 2: End-of-Life Care Models Across Clinical Settings
| Care Model | Ethical Priorities | Decision-Making Process | Outcome Measures |
|---|---|---|---|
| Hospital-Based Curative Care | Life extension, disease modification, technological intervention [26] | Physician-driven with patient consent; crisis-oriented decision-making [26] | Survival rates, physiological parameters, treatment success [26] |
| Palliative Care | Symptom relief, quality of life, holistic comfort [28] | Interdisciplinary team approach with patient and family engagement [28] | Pain scores, symptom burden, quality of life measures [28] |
| Hospice Care | Dignity in dying, comfort, family support [28] | Patient-centered goals; focuses on caring rather than curing [28] | Peaceful death, family satisfaction, bereavement outcomes [28] |
| Social Work Integration | Empowerment, advocacy, cultural competence, self-determination [28] | Biopsychosocial assessment; interdisciplinary collaboration [28] | Psychosocial well-being, resource access, care coordination [28] |
The integration of palliative care represents a significant evolution in end-of-life ethics, emphasizing that "palliative care affirms life and regards dying as a normal process; intends neither to hasten nor to postpone death" [28]. This approach explicitly addresses limitations in traditional biomedical models that may prioritize life extension at the cost of quality of life or dignified dying. Social work practice standards further enrich this landscape by emphasizing "an attitude of compassion and sensitivity to clients, respecting clients' rights to self-determination and dignity" while encouraging practitioners to "be aware of their own beliefs, values, and feelings and how their personal self may influence their practice" [28].
Ethical Models in Organ Transplantation
Allocation Systems and Ethical Tensions
Organ transplantation ethics present distinctive challenges centered on the profound disparity between organ supply and recipient need. The Organ Procurement and Transplantation Network (OPTN) Final Rule establishes the ethical framework for organ allocation in the United States, mandating "equitable organ allocation and organ-specific priority stratification systems" [29]. However, implementation of this mandate varies significantly across organ systems, creating what one systematic review identifies as "inconsistent ethical standards underlying organ allocation scores in the United States" [29].
The ethical tension between utility-based approaches (maximizing transplant success) and justice-based approaches (prioritizing the most urgent cases) manifests differently across organ systems. For instance, the Model for End-Stage Liver Disease (MELD) prioritizes medical urgency, aiming to "reduce waitlist mortality rather than prioritizing individuals with the best predicted post-transplant survival" [29]. In contrast, the Estimated Post Transplant Survival (EPTS) score for kidney transplantation prioritizes postoperative life expectancy "to minimize the likelihood of retransplantation" [29]. These different priority structures reflect ongoing ethical debates about the appropriate goals of allocation systems.
Procurement Models: Opt-In versus Opt-Out Systems
The ethics of organ procurement present fundamental questions about the relationship between individual autonomy and social responsibility. Opt-in systems, used in the United States, "align with the principle of bodily autonomy, treating organ donation as a personal decision akin to leaving behind an inheritance" [27]. This approach ensures explicit consent but "often results in lower donation rates due to inaction" [27]. Routine-salvage (opt-out) models, used in England, Finland, Colombia and other countries, "view organs as a public resource, prioritizing societal welfare by increasing the donor pool and reducing organ shortages" [27].
A casuist analysis comparing organ donation to inheritance law notes that while "organ donation seems more similar to an inheritance than a public resource, implying that bodily autonomy is a fundamental right that extends beyond death but is not completely absolute" [27]. This framework acknowledges that even inheritances are subject to taxation and escheatment laws, suggesting limitations to absolute autonomy. The ethical debate "forces us to question what core values we prioritize the most: a person's bodily autonomy throughout not only life but also postmortem, or the moral obligation to save as many lives as possible and ensure maximal utility via equitable organ distribution" [27].
The following diagram illustrates the ethical dimensions and outcomes of different organ procurement models:
Experimental and Methodological Approaches in Ethics Research
Research Design and Analytical Frameworks
Bioethics research employs diverse methodological approaches to examine complex clinical ethical questions. Comparative effectiveness research (CER) in ethics encompasses "both evidence generation and evidence synthesis" [30]. Experimental approaches include randomized controlled trials (RCTs), which "are fundamental to the evaluation of new therapeutic agents" but have limitations in real-world decision making due to "restrictive enrollment criteria so that the participants do not resemble patients in practice" [30]. Adaptive trial designs represent an innovative approach that "use accumulating evidence from the trials to modify trial design to increase efficiency and the probability that trial participants benefit from participation" [30].
Observational studies comprise a growing proportion of bioethics research "because of their efficiency, generalizability to clinical practice, and ability to examine differences in effectiveness across patient subgroups" [30]. However, concerns about selection bias in observational studies "can be mitigated by measuring potential confounders and analytic approaches, including multivariable regression, propensity score analysis, and instrumental variable analysis" [30]. The choice of research method involves tradeoffs between concerns about selection bias and generalizability, as well as pragmatic considerations related to data availability and timing [30].
Table 3: Research Methods and Analytical Approaches in Bioethics
| Method Category | Specific Approaches | Key Applications in Ethics Research | Strengths and Limitations |
|---|---|---|---|
| Experimental Designs | Randomized Controlled Trials (RCTs), Adaptive Trials, Pragmatic Trials [30] | Evaluating ethics education interventions, assessing clinical ethics consultation models | High internal validity; may lack generalizability to diverse populations [30] |
| Observational Methods | Cohort Studies, Case-Control Studies, Cross-Sectional Surveys [30] | Examining real-world ethical decision patterns, assessing equity in resource allocation | High generalizability; potential for confounding and selection bias [30] |
| Analytical Techniques | Multivariable Regression, Propensity Score Analysis, Instrumental Variable Analysis [30] | Addressing confounding in observational studies, identifying subgroup variations | Can mitigate bias when confounders are measured; limited by data availability [30] |
| Evidence Synthesis | Systematic Reviews, Meta-Analysis, Decision Modeling [30] | Integrating findings across studies, modeling outcomes of policy alternatives | Comprehensive assessment of evidence; dependent on primary study quality [30] |
| Qualitative Approaches | Casuistry, Case-Based Analysis, Deliberative Methods [27] | Examining moral reasoning patterns, facilitating stakeholder engagement | Rich contextual understanding; challenges in generalization and quantification [27] |
Casuist analysis represents a distinctive methodological approach that "uses archetypal paradigm cases to determine the morality of novel cases rather than applying ethical principles" [27]. This case-based reasoning method "is applicable in debates regarding opt-in versus opt-out models of organ donation since this issue continues to divide ethicists" and is particularly valuable "because both sides are supported by ethical principles, making a framework that depends more on our moral intuitions more appealing" [27]. The casuist approach compares novel dilemmas to paradigm cases to determine similarities through a process called triangulation [27].
Global Perspectives and Emerging Challenges
International Frameworks and Policy Developments
Global transplantation ethics faces significant challenges, including "inadequate legislation, ethical frameworks and regulation, which may allow for practices such as organ trafficking" [31]. The World Health Organization (WHO) Guiding Principles on Human Cell, Tissue and Organ Transplantation provide "an orderly, ethical and acceptable framework for the acquisition and transplantation of human cells, tissues and organs for therapeutic purposes" [31]. These principles were updated in 2020 to reflect evolving practices and attitudes and continue to influence professional codes and legislation worldwide [31].
Recent international developments include the Santiago de Compostela Convention of the Council of Europe, which represents "the first and only legally binding international instrument specifically designed to combat the trafficking of human organs" [32]. This convention establishes crucial frameworks for "protecting donors, supporting victims and strengthening international cooperation to prosecute this transnational crime" [32]. Such international instruments acknowledge the global nature of organ trafficking and the need for coordinated ethical and legal responses.
Algorithmic Fairness in Organ Allocation
Emerging research examines ethical concerns in algorithmic approaches to organ allocation. A 2024 systematic review notes that "current risk scores emphasize model performance and overlook ethical concerns in variable selection" [29]. The inclusion of demographic variables such as race and sex in allocation algorithms raises particular concerns, as these categorical variables may lack biological basis and blur "the line between evidence-based models and discrimination" [29].
Specific ethical challenges identified across organ systems include "the exception points in MELD, the inclusion of race in KDRI, the geographical limit in the Lung Allocation Score, and the inadequacy of risk stratification in the Heart Tier system, creating obstacles for medically underserved populations" [29]. These findings highlight the need for "standardization and transparency in policy development to ensure fairness, equitability, and evidence-based risk predictions" in organ allocation [29]. As algorithmic systems become more sophisticated, ongoing ethical scrutiny is essential to ensure they advance rather than undermine equity goals.
This comparative analysis reveals both convergence and tension between secular and religious approaches to clinical ethics in end-of-life care and organ transplantation. While foundational principles differ, practical applications often demonstrate significant overlap in commitment to human dignity, compassion, and justice. The increasing complexity of medical technology, coupled with growing recognition of health disparities, necessitates continued development of ethical frameworks that can address both individual clinical cases and systemic policy questions.
Future directions in clinical ethics include greater attention to algorithmic fairness in resource allocation, enhanced interdisciplinary collaboration, and more robust integration of cultural and religious diversity in ethical deliberation. Both secular and religious traditions have vital contributions to make to these developments, particularly when they engage in constructive dialogue focused on concrete clinical challenges. By examining these ethical models in action, researchers, clinicians, and policymakers can work toward more nuanced and effective approaches to the profound ethical questions that arise at the boundaries of life and death.
Bioethics, as a field of study concerned with the moral, legal, and social issues raised by medicine and biomedical research, operates within a complex landscape of secular and religious foundations [33]. This comparative analysis examines how different worldviews—particularly secular frameworks and religious traditions—approach core ethical issues in human subjects research, with specific focus on informed consent and moral boundaries. While contemporary bioethics often draws upon secular presumptions, religious perspectives continue to play a crucial role in both personal moral reasoning and public debate [33] [15]. The tension between these frameworks becomes particularly evident in international research contexts, where cultural and religious differences may challenge the assumption that ethical principles are universally applicable and interpreted in the same way [34] [35] [36].
The historical development of bioethics reveals its deep connection to religious traditions, even as the field has evolved toward secularization. As noted in analyses of the field's origins, "the theories and methods of thought that developed in the wake of the Enlightenment, to say nothing of the long line of thinkers, were a direct result of the wrestling between Christianity and philosophy, followed by a secularization of the Christian ethic" [15]. This historical context informs the current paradigm in which bioethics operates—one that frequently positions secular frameworks as neutral and universal, while potentially marginalizing religious perspectives as particularistic [15] [14].
Comparative Religious and Secular Frameworks on Research Ethics
Religious Bioethical Frameworks
Religious traditions provide comprehensive moral frameworks that address fundamental questions about the boundaries of human intervention in natural processes. These traditions often emphasize the sacredness of life as a gift from God, which consequently shapes their approaches to research ethics [33] [14].
Table 1: Comparative Religious Perspectives on Key Bioethical Issues
| Bioethical Issue | Islamic (Turkish RAA) | Roman Catholic | Orthodox Judaism |
|---|---|---|---|
| Beginning of Life | Life begins at conception; fetal rights bestowed by Allah [33] | Strong protection of life from conception [33] | Sacredness of life from early stages [33] |
| Organ Transplantation | Permitted with conditions: medical necessity, certainty of donor's death, no financial transaction [33] | Generally approved [33] | Generally approved [33] |
| Assisted Reproduction | Permitted only between married couples; no third-party donors [33] | Limited approval; concerns about third-party involvement [33] | Limited approval; concerns about third-party involvement [33] |
| Contraception | Approved under certain conditions; permanent methods discouraged [33] | Limited approval; natural methods preferred [33] | Varies by interpretation [33] |
| Human Cloning | Prohibited [33] | Prohibited [33] | Prohibited [33] |
The Islamic perspective, as articulated by Turkey's Religious Affairs Administration (RAA), offers a representative example of religious bioethics. The RAA emphasizes that "life to start at conception, i.e., the moment of fertilization" and that "the fetus' right to live is given by the creator (Allah)" [33]. This foundational principle informs their positions on various bioethical issues, including prohibitions on third-party involvement in assisted reproduction and conditional acceptance of organ transplantation [33].
Similarly, both Roman Catholic and Orthodox Jewish traditions justify the sacredness of life through divine will, though differences emerge in specific applications. All three Abrahamic traditions share concerns about maintaining proper boundaries in human experimentation, particularly when such research threatens to undermine the perceived sacredness of human life [33].
Secular Bioethical Frameworks
Secular bioethics has developed primarily through principles-based approaches that seek to establish universal guidelines without recourse to religious foundations. The Belmont Report's principles of respect for persons, beneficence, and justice have become foundational to secular research ethics [36] [37]. These principles emphasize autonomy and informed consent as central to ethical research, reflecting the Enlightenment emphasis on individual rights and rational decision-making [36].
However, this secular approach has limitations. As critics note, "By giving up on meaning and teleology, bioethics misses what we might call 'the paradox of suffering'" [14]. The secular framework's emphasis on procedural ethics and bureaucratic solutions may fail to address deeper questions of meaning that often arise in the context of illness and medical research [14].
Table 2: Core Principles in Secular Bioethics Frameworks
| Ethical Principle | Definition | Application in Research |
|---|---|---|
| Respect for Persons | Recognition of personal autonomy and protection of individuals with diminished autonomy [36] | Informed consent process; voluntary participation without coercion |
| Beneficence | Obligation to maximize benefits and minimize potential harms [36] | Risk-benefit assessment; monitoring of research participants |
| Justice | Fair distribution of research burdens and benefits [36] | Equitable selection of subjects; avoidance of exploiting vulnerable populations |
| Non-Maleficence | obligation not to inflict harm intentionally | Ensuring research methodology minimizes potential harms to participants |
Informed Consent in Cross-Cultural Perspective
Theoretical Foundations and Cultural Variations
The doctrine of informed consent represents a primary component of protecting the rights and welfare of individuals involved in research, grounded in the concept of autonomy and self-determination [36]. International guidelines, including the Nuremberg Code, the Declaration of Helsinki, and the Belmont Report, all justify informed consent requirements through the ethical principle of respect for persons [36] [37].
However, cultural interpretations of autonomy and personhood vary significantly, creating challenges for implementing universal informed consent standards. Research demonstrates that "cultural and social experiences can influence an individual's concerns, expectations, comprehension, decision-making and motivation regarding biomedical and genetic research" [34]. These differences became starkly evident in the case of the Havasupai Tribe, where disagreements about the scope of research consent led to legal action and a breakdown of trust between researchers and the community [34].
The Western concept of autonomy underlying standard informed consent protocols is "rooted in Western enlightenment thinking where one school of thought holds that individuals ought to be treated as ends in themselves and not simply as means" [36]. This emphasis on radical individualism may conflict with more communitarian ethical frameworks prevalent in many non-Western societies [35] [36].
Practical Challenges and Adaptive Approaches
Practical challenges in cross-cultural informed consent include communication barriers, different conceptual understandings of health and research, and varying decision-making structures. As identified in focus groups with diverse ethnic communities, "individuals from diverse backgrounds may have different perspectives on and expectations for the research process" [34]. These differences extend to perceptions of risk, anticipated burden, perceived benefits, informational needs, and decision-making strategies [34].
Successful adaptive approaches have emerged to address these challenges:
Community Advisory Committees: Nigeria's National Health Research Ethics Committee code introduces the concept of a Community Advisory Committee that "emphasizes research as a community burden and should promote a form of 'research friendship' to foster the welfare of research participants" [38].
Collaborative Consent Processes: In the Tibetan Autonomous Region, researchers found greater success with flexible, cooperative approaches to informed consent that acknowledged cultural differences in decision-making and authority [35].
Culturally Adapted Materials: Some researchers have experimented with deviations from traditional consent forms, including point-form summaries and pictorial representations, though evidence suggests that "these techniques have not been demonstrated to increase understanding above the level achieved with the traditional forms" [36].
Figure 1: Cross-Cultural Informed Consent Models Comparison
Human Rights Frameworks and Legal Enforcement
International Human Rights Standards
The legal framework for human subject research has evolved significantly since the Nuremberg Code, with multiple international human rights instruments establishing protections for research participants. The International Covenant on Civil and Political Rights (ICCPR) explicitly provides that "no one shall be subjected without his free consent to medical or scientific experimentation" [37]. This prohibition was drafted specifically in response to the atrocities committed during World War II and represents a foundational legal protection for research subjects [37].
Other relevant international standards include:
The Convention on the Rights of Persons with Disabilities (CRPD): Recognizes that states must provide equal recognition of legal capacity and protection against non-consensual experimentation [37].
The Convention on the Rights of the Child (CRC): Requires that states ensure children's views are given due weight in matters affecting them and that parents act in the child's best interests [37].
The Convention Against Torture (CAT): Defines torture in ways that may encompass non-consensual research, particularly when involving "severe pain or suffering" [37].
The difference between ethical principles and human rights is "clearly determined by the non-enforceability of ethical norms and the legally binding nature of human rights obligations" [37]. This distinction becomes crucial when addressing violations, as human rights frameworks provide mechanisms for accountability that ethical guidelines lack.
Regional Human Rights Systems
Regional human rights systems have developed complementary frameworks for protecting research participants:
Inter-American System: The American Convention on Human Rights establishes protections through its provisions on the right to life, personal integrity, and privacy [37].
European System: The European Convention on Human Rights has been interpreted to include protections against non-consensual experimentation through its provisions on torture and inhuman treatment [37].
African System: The African Charter on Human and Peoples' Rights emphasizes community values while still protecting individual rights relevant to research participation [37].
Table 3: International Human Rights Instruments Protecting Research Subjects
| Human Rights Instrument | Key Protection | Enforcement Mechanism |
|---|---|---|
| International Covenant on Civil and Political Rights (Article 7) | Prohibition of non-consensual medical/scientific experimentation [37] | UN Human Rights Committee monitoring and individual complaints |
| Convention on the Rights of Persons with Disabilities (Article 15) | Protection against non-consensual experimentation; respect for integrity [37] | Committee on the Rights of Persons with Disabilities monitoring |
| Convention on the Rights of the Child | Requirement that children's views be given due weight [37] | Committee on the Rights of the Child monitoring |
| Regional Human Rights Systems | Various protections through right to life, integrity, and privacy provisions [37] | Regional human rights courts and commissions |
Experimental Protocols and Ethical Oversight Frameworks
Models for Ethical Review in Cross-Cultural Research
When conducting research across cultural boundaries, particularly in contexts where ethical review infrastructure may be limited, researchers have developed adaptive models to ensure proper oversight. One framework implemented in research in India identified three critical components of ethical regulation: external oversight, local oversight, and subject involvement [39].
External oversight involves ensuring that research proposals are "created in accordance with ethical guidelines of a high standard and be reviewed and approved by at least one effective IRB" [39]. This may include engaging independent cultural experts to advise review boards on local concerns and potential ethical issues [39].
Local oversight requires that "research on humans should be designed and conducted in conjunction with a subject advocate, preferably one who is knowledgeable of the culture and customs of the participants" [39]. This approach emphasizes collaboration with local organizations or representatives who can help ensure the research respects local values and practices.
Subject involvement means that "subjects should not be limited to serving as the source of data but should also participate in voicing issues that need to be considered in study design" [39]. This participatory approach helps ensure that research protocols are culturally appropriate and responsive to community concerns.
Research Reagent Solutions: Essential Components for Ethical Research
Table 4: Essential Framework for Ethical Cross-Cultural Research
| Component | Function | Implementation Examples |
|---|---|---|
| Community Advisory Boards | Ensure community perspectives inform research design and conduct [38] [39] | Nigeria's requirement for Community Advisory Committees; tribal elder consultations |
| Cultural Mediators | Bridge understanding between researchers and communities [34] [35] | Bilingual research staff; involvement of traditional healers in Tibetan research |
| Culturally Adapted Consent Materials | Make informed consent comprehensible across literacy and cultural barriers [36] | Pictorial representations; oral consent protocols; local language translations |
| Independent Ethical Monitoring | Provide ongoing oversight of research implementation [39] | External audits; partnership with local ethics committees; community reporting mechanisms |
| Benefit-Sharing Mechanisms | Ensure communities receive appropriate benefits from research [36] [37] | Capacity building; healthcare access; technology transfer; fair compensation |
Figure 2: Ethical Oversight Framework for International Research
This comparative analysis reveals both significant convergence and notable divergence between secular and religious frameworks for research ethics. While foundational principles of respect for human dignity and welfare appear universal, their interpretation and application reflect distinctive philosophical and theological commitments. Religious traditions often ground their bioethical approaches in concepts of divine will and sacredness of life [33] [14], while secular frameworks emphasize autonomy and rational deliberation [36] [37].
The challenge of cross-cultural informed consent highlights the limitations of strictly universalist approaches to research ethics. As the case studies from Tibet, Nigeria, and Native American communities demonstrate, meaningful ethical practice requires attention to local context and cultural values [34] [38] [35]. This does not necessitate ethical relativism, but rather what might be termed "principled pluralism"—an approach that maintains fundamental ethical commitments while adapting their implementation to diverse cultural contexts.
For researchers and drug development professionals, this analysis suggests the importance of several best practices: (1) engaging in serious dialogue with religious perspectives when they inform participants' understanding of research participation; (2) developing flexible consent processes that respect both individual autonomy and communal decision-making structures; and (3) recognizing the complementary strengths of ethical guidelines and human rights frameworks in protecting research participants across diverse worldviews.
The future of ethical human subjects research in a global context will depend on continued dialogue across worldviews—religious and secular, Western and non-Western—to develop approaches that honor both universal principles and legitimate cultural diversity.
The governance of reproductive technologies represents a critical arena where religious directives and secular autonomy principles converge and frequently conflict. This analysis examines the distinct foundational principles, operational policies, and patient care outcomes within religiously-affiliated versus secular healthcare systems. The Ethical and Religious Directives for Catholic Health Care Services (ERD) established by the United States Conference of Catholic Bishops provides the definitive framework for Catholic healthcare institutions, articulating specific religious limitations on medical practices [40]. These directives stand in contrast to secular bioethical frameworks that prioritize patient autonomy, informed consent, and medical standard of care as paramount values [41]. The tension between these approaches has significant implications for reproductive healthcare delivery, particularly as Catholic healthcare systems expand their market presence, now comprising one in six hospital beds in the United States and operating 20% of California's maternity wards [42] [43]. This case study analyzes how these competing ethical frameworks manifest in clinical practice, institutional policies, and patient experiences, with particular attention to miscarriage management, contraceptive services, and clinician training.
Analytical Framework and Methodologies
Comparative Bioethics Methodology
This analysis employs a structured comparative approach to evaluate how religious and secular frameworks address specific reproductive technologies. The methodology examines: (1) Foundational principles underlying each approach; (2) Institutional policies governing healthcare delivery; (3) Clinical protocols for common reproductive scenarios; and (4) Measurable outcomes for patient care and access. Data is synthesized from peer-reviewed studies, legal documents, patient testimonies, and healthcare system analyses to identify patterns of conflict and convergence between these ethical frameworks [42] [41] [43]. This multidimensional approach allows for systematic comparison across theoretical, practical, and experiential dimensions.
Data Collection and Analysis Protocols
Table: Data Collection Methods for Comparative Bioethics Analysis
| Method Category | Specific Protocols | Application in This Study |
|---|---|---|
| Policy Analysis | Document review of ERD and secular institutional policies; Tracking of policy revisions and interpretations | Analysis of 2025 ERD revisions regarding gender interventions and miscarriage management [40] |
| Clinical Case Studies | Documented patient experiences; Legal proceedings; Physician testimonies | Examination of Anna Nusslock miscarriage case against Catholic hospital [42] |
| Quantitative Surveys | Patient access mapping; Service availability assessments; Market concentration analysis | Assessment of Catholic hospital prevalence and "sole provider" status in various regions [43] |
| Workforce Studies | Surveys of physician experiences; Analysis of training adequacy; Moral distress documentation | Studies of OB-GYN training limitations in Catholic residency programs [41] |
Comparative Analysis of Foundational Principles
Religious Directives: The Catholic Framework
The Ethical and Religious Directives for Catholic Health Care Services establish a theologically-grounded framework prioritizing the sanctity of life from conception, respect for natural law, and the inseparability of body and soul [40]. The most recent 2025 revisions reinforce these principles through several key provisions:
- Directive 28: Explicitly prohibits "medical interventions, whether surgical, hormonal, or genetic, that aim not to restore but rather to alter the fundamental order of the body in its form or function," including gender-affirming procedures and interventions that "nullify sexual characteristics" [40].
- Directive 29: While mandating care for those experiencing gender incongruence, it restricts interventions to "only those means that reflect the fundamental order of the human body" [40].
- Principle of Totality: Permits removal or suppression of bodily functions only when necessary for the wellbeing of the whole body, explicitly prohibiting procedures that eliminate fertility or healthy organs without therapeutic justification [40].
These directives are implemented through institutional ethics committees, typically including religious representatives, who interpret specific clinical cases through Catholic theological frameworks [42]. This structure creates a standardized approach across Catholic healthcare institutions while allowing case-specific determinations.
Secular Bioethics: The Autonomy-Based Framework
Secular bioethical frameworks prioritize fundamentally different principles, emphasizing patient self-determination, bodily autonomy, and evidence-based medical standards [41]. Key components include:
- Informed Consent: Requires comprehensive disclosure of all treatment options, including those not offered by the institution, with referrals when appropriate [41].
- Standard of Care: Adherence to medically accepted practices as determined by professional organizations rather than religious doctrine [41].
- Quality of Life Considerations: Evaluation of treatments based on their impact on patient wellbeing, functionality, and life satisfaction rather than exclusively on preservation of biological life [43].
These principles manifest in policies that require disclosure of institutional restrictions, facilitate transfers when requested, and prioritize patient values in decision-making processes [43].
Quantitative Comparison of Clinical Approaches
Reproductive Service Restrictions
Table: Comparative Analysis of Service Availability in Religious vs. Secular Frameworks
| Reproductive Service | Catholic Hospital Policies | Secular Hospital Standards | Impact on Patient Access |
|---|---|---|---|
| Direct Contraception | Prohibited (IUDs, pills, patches) [43] | Available with counseling [41] | 40% fewer postpartum sterilizations near Catholic hospitals [43] |
| Pregnancy Termination | Prohibited except immediate life-threat [40] | Available per patient choice and medical need [42] | Emergency transfers for miscarriage care [42] |
| Miscarriage Management | Restricted until fetal death or maternal crisis [42] | Full options: expectant, medical, surgical [42] | Delayed care until infection develops [42] |
| Fertility Treatments | Limited to natural methods [43] | Comprehensive ART including IVF [43] | Geographic barriers for infertility patients [43] |
| Sterilization Procedures | Prohibited (vasectomy, tubal ligation) [41] | Available with consent [41] | Logistical barriers for postpartum patients [41] |
| Gender-Affirming Care | Prohibited by 2025 ERD revisions [40] | Available per WPATH standards [40] | Complete exclusion from Catholic systems [40] |
Systemic Impacts and Market Concentration
The growing dominance of Catholic healthcare systems creates structural barriers to reproductive services, particularly in specific regions:
- Regional Disparities: In Alaska, Iowa, Washington, Wisconsin, and South Dakota, more than 40% of acute care beds are in hospitals operating under Catholic health restrictions [43].
- Sole Provider Status: Catholic hospitals now represent 35% of maternity wards in rural northern California counties, with some regions having no alternative providers [42].
- Awareness Gaps: Approximately one-third of reproductive-age women who identified a Catholic hospital as their primary hospital were unaware of its religious affiliation and associated restrictions [43].
Experimental Protocols and Clinical Workflows
Clinical Decision Pathways
The following diagrams illustrate the distinct clinical decision-making processes for miscarriage management in Catholic versus secular healthcare settings, based on documented protocols and practices [42] [41].
Diagram Title: Catholic Hospital Miscarriage Protocol
Diagram Title: Secular Hospital Miscarriage Protocol
Research Reagent Solutions for Bioethics Analysis
Table: Essential Methodological Tools for Comparative Bioethics Research
| Research Tool | Function in Analysis | Application Example |
|---|---|---|
| Policy Document Analysis | Systematic review of ERD and institutional policies | Tracking revisions in 2025 ERD regarding gender interventions [40] |
| Patient Care Documentation | Record review of denied or delayed services | Analysis of miscarriage cases with delayed intervention [42] |
| Healthcare Market Mapping | Geographic analysis of service availability | Identifying regions with Catholic hospital dominance [43] |
| Clinician Surveys | Assessment of moral distress and practice constraints | Studies of OB-GYNs in religious systems [41] |
| Legal Case Analysis | Examination of litigation patterns and arguments | Review of Bonta v. Providence case arguments [42] |
Discussion: Resolving Ethical Tensions
Critical Junctures of Conflict
The comparison reveals several fundamental tensions between religious directives and secular autonomy in reproductive healthcare:
Temporal Discontinuity in Emergency Care: Catholic policies requiring delayed intervention until specific clinical thresholds are met (e.g., fetal demise or maternal infection) create what physicians describe as substandard care by secular medical benchmarks [41]. As one maternal-fetal medicine specialist noted, "I'm aware that I'm not exactly practicing the standard of care, from a non-Catholic hospital standpoint" [41].
Informational Asymmetry: The documented lack of transparency regarding religious restrictions creates barriers to truly informed consent, with approximately one in five Catholic hospitals failing to explicitly disclose their religious affiliation on their websites [43].
Training Inadequacies: Obstetricians trained in Catholic residency programs report significant gaps in family planning education, with variable training in contraceptive implants, IUD placement, and postpartum tubal ligations [41].
Emerging Regulatory and Legal Responses
Several regulatory and legal mechanisms are evolving to address these tensions:
- Antitrust Scrutiny: Growing attention to how hospital mergers that create religious monopolies might violate antitrust principles by reducing consumer choice and access to comprehensive reproductive services [43].
- Emergency Care Mandates: Enforcement of existing state laws and the federal Emergency Medical Treatment and Labor Act (EMTALA) requiring stabilization of emergency conditions, including complicated miscarriages [42].
- Transparency Initiatives: Proposed legislation requiring hospitals to disclose service limitations based on religious restrictions, enabling more informed consumer choice [43].
This comparative analysis demonstrates that the conflict between religious directives and secular autonomy in reproductive technologies represents more than theoretical bioethical debate—it manifests in tangible clinical consequences, structural barriers to care, and fundamental questions about healthcare delivery in pluralistic societies. The 2025 revisions to the Ethical and Religious Directives have intensified these tensions by explicitly prohibiting gender-affirming care while maintaining restrictions on miscarriage management and reproductive services [40].
The growing market dominance of Catholic healthcare systems creates additional complexity, particularly in regions where these institutions serve as sole providers [43]. Potential pathways forward include enhanced transparency requirements, careful antitrust enforcement in hospital mergers, protection of clinician conscience rights, and development of creative partnerships that respect religious pluralism while ensuring access to comprehensive reproductive services. As these debates continue, the fundamental challenge remains balancing institutional religious freedom with individual autonomy and access to medically appropriate care—a tension that will undoubtedly shape the future of reproductive healthcare delivery and bioethical discourse.
Navigating Ethical Conflicts: Strategies for Resolution in Polarized Scenarios
Intractable Disputes? Analyzing Conflicts at the Beginning and End of Life
The analysis of conflicts at the beginning and end of life represents a critical nexus in bioethics, where deeply held secular and religious values often appear to collide. This examination operates within the broader thesis that the conventional dichotomy between secular and religious bioethical frameworks may be artificially rigid and counterproductive. Rather than maintaining separate approaches, contemporary scholarship suggests the need for a dialogical approach that creates opportunities for deeper understanding across different perspectives without seeking conversion [44]. This comparative analysis seeks to move beyond simplistic caricatures and explore the nuanced ways in which these frameworks approach fundamental ethical principles when applied to life's most vulnerable moments.
The perception of intractability in these disputes often stems from a failure to accurately characterize the nature of the conflict. Research indicates that what are often interpreted as factual disagreements between religious and scientific communities are frequently moral conflicts at their core. As Evans (2025) notes, "While there are a few conflicts over such claims for a few religious traditions, largely concerning human origins, these fact claims are not relevant for bioethics. Instead, social science research has shown widespread moral conflict between scientists and the actively religious" [45]. This distinction between factual and moral disagreement is essential for meaningful dialogue and conflict resolution in clinical and policy settings.
Theoretical Foundations: Principles in Comparative Perspective
Ethical Frameworks and Their Application
Bioethical deliberation across both secular and religious traditions engages with several core principles, though their interpretation, weighting, and application may diverge significantly. The four principles of autonomy, beneficence, nonmaleficence, and justice provide a common vocabulary for ethical analysis in healthcare settings, particularly in end-of-life care [26] [46]. These principles are recognized universally, though "their application and weight may differ" across cultural and religious contexts [26].
Autonomy, or respect for patient self-determination, is a cornerstone of secular bioethics, emphasizing the patient's right to make informed decisions about their care based on personal values [46]. In religious frameworks, particularly within Catholic healthcare ethics, autonomy may be balanced with other considerations such as the inviolability of human life and natural law principles. The principle of beneficence (acting in the patient's best interest) and nonmaleficence (avoiding harm) find resonance across traditions, though conceptions of what constitutes "good" and "harm" may vary [26] [46]. The principle of justice requiring fair distribution of healthcare resources is universally acknowledged, though its practical implementation remains challenging across all frameworks [26].
Beyond Dichotomy: Towards Integrative Discourse
The presentation of bioethics as divided between secular and religious approaches works against the "interdisciplinary and pluralistic context in which bioethics itself originated" [44]. This false dichotomy can impede constructive dialogue on contentious issues at life's boundaries. A more productive approach recognizes bioethics as fundamentally a social ethic that requires "complex thinking from a variety of approaches that reach beyond a secular and religious divide" [44]. This perspective acknowledges that both secular and religious frameworks bring valuable insights to the ethical complexities of modern medicine.
The current crisis of public trust in scientific institutions affects both secular and religious communities, though for different reasons. Rebuilding this trust requires a return to foundational virtues of science, including honesty and humility [19]. As noted in contemporary ethical analysis, "Science, at its core, is a humble pursuit. It begins with the acknowledgment that we don't know something - and the willingness to go through the process to learn it" [19]. This virtue-based approach to scientific practice may provide common ground for dialogue between secular and religious perspectives.
Conflict Analysis: Beginning of Life Issues
Navigating Poor Prenatal Diagnoses
When prospective parents receive a poor prenatal diagnosis, they face complex decisions that engage deeply with ethical frameworks. Religious bioethics, particularly within the Catholic tradition, emphasizes accompaniment and compassion while maintaining certain moral boundaries. The approach to these situations focuses on "navigating poor prenatal diagnoses with compassion" while upholding the dignity of both mother and child [47]. This often involves supporting families in continuing pregnancies despite adverse diagnoses, coupled with comprehensive palliative care frameworks.
Secular bioethics approaches these decisions through a different lens, often prioritizing parental autonomy and quality of life considerations. The framework tends to emphasize the right to make reproductive decisions without external coercion, while also acknowledging the physician's professional integrity. What appears as stark opposition in abstract principle often becomes more nuanced in clinical practice, where both traditions seek to support families through traumatic diagnostic experiences while remaining consistent with their foundational principles.
Reproductive Technologies and Genetic Interventions
Advanced reproductive technologies and emerging genetic interventions represent another area of significant ethical contention. By 2025, CRISPR and gene editing technologies have entered mainstream clinical applications for correcting genetic defects and treating inherited diseases [48]. These technologies raise profound questions about human nature, the ethics of genetic modification, and the definition of disease versus enhancement.
Religious frameworks often evaluate these technologies through concepts of natural law and the integrity of human nature, frequently expressing caution about technological interventions that might redefine fundamental aspects of human identity. Secular ethics tends toward a more utilitarian calculus, weighing benefits against risks while emphasizing scientific freedom and therapeutic potential. Both frameworks, however, share concerns about justice and equitable access to these emerging technologies, recognizing the potential for exacerbating existing social inequalities.
Conflict Analysis: End of Life Issues
Treatment Limitation and Withdrawal Decisions
End-of-life decision-making presents particularly challenging ethical terrain, where the principles of autonomy, beneficence, and nonmaleficence often create tension. Universally accepted ethical principles guide healthcare professionals in managing decisions regarding resuscitation, mechanical ventilation, artificial nutrition and hydration, terminal sedation, and withholding or withdrawing treatments [26]. The application of these principles, however, varies significantly between secular and religious frameworks.
In secular bioethics, the principle of patient autonomy typically takes precedence, manifested through advance directives, living wills, and healthcare proxies [26]. The patient's "right to self-determination" requires informed consent for medical interventions and includes both the "right to demand the termination of treatment" and the "right to refuse treatment altogether" [26]. This framework emphasizes quality of life considerations and the permissibility of foregoing burdensome treatments when they no longer serve the patient's goals.
Religious approaches, particularly within the Catholic tradition, often distinguish between ordinary and extraordinary treatments, maintaining that while there is no obligation to pursue disproportionately burdensome interventions, basic care including nutrition and hydration should generally be maintained. The distinction between killing and allowing to die remains fundamental in this framework, with certain actions considered intrinsically wrong regardless of consequences.
Table 1: Comparative Approaches to End-of-Life Decision Making
| Ethical Issue | Secular Bioethics Framework | Religious Bioethics Framework |
|---|---|---|
| Decision Authority | Primary emphasis on patient autonomy through advance directives and healthcare proxies [26] | Balance of patient autonomy with objective moral principles and natural law |
| Life-Sustaining Treatment | May be withheld or withdrawn based on patient preferences and quality of life considerations [26] | Distinguished between ordinary (generally obligatory) and extraordinary (not obligatory) means |
| Pain Management | Balance of benefits with risks, including potential acceptance of palliative sedation even if may hasten death | Principle of double effect permits adequate pain relief even if risk of hastening death, but intentional shortening of life prohibited |
| Artificial Nutrition/Hydration | Considered medical treatment that may be withheld or withdrawn under certain conditions [26] | Generally considered ordinary care that should be provided in most circumstances |
Physician-Assisted Suicide and Euthanasia
The ethical divide between secular and religious approaches becomes particularly pronounced regarding physician-assisted suicide and euthanasia. While an increasing number of jurisdictions have legalized some form of medical aid in dying, religious bioethics traditions largely maintain opposition to these practices based on principles of the inviolability of life and the natural law tradition.
Secular frameworks typically approach these issues through the lenses of mercy, autonomy, and relief of suffering, emphasizing the individual's right to control the timing and manner of death in the face of terminal illness. Religious perspectives, while sharing the commitment to relieve suffering, view intentionally causing death as a fundamental violation of human dignity and the proper role of healthcare. Both traditions, however, emphasize the importance of palliative care and aggressive symptom management as alternatives to intentional life-ending procedures.
Experimental and Empirical Approaches
Research Methodology in Bioethical Analysis
The comparative analysis of ethical frameworks requires rigorous methodological approaches that blend qualitative and quantitative research strategies. While traditional philosophical analysis remains fundamental, contemporary bioethics increasingly employs empirical methods to understand how ethical principles are interpreted and applied in actual clinical practice.
Systematic observation of clinical decision-making at life's boundaries provides crucial data on how ethical frameworks function in practice. This involves detailed case analysis, ethnographic studies of healthcare settings, and structured interviews with patients, families, and healthcare providers facing critical decisions. These observational methodologies help identify gaps between theoretical principles and practical application across different ethical traditions.
Comparative outcome studies represent another important methodological approach, examining how different decision-making frameworks affect patient and family experiences at the end of life. These studies measure outcomes such as symptom management, quality of life, family satisfaction with care, and psychological adjustment to bereavement. By comparing outcomes across different ethical approaches, researchers can identify best practices that transcend traditional divisions.
Ethical Analysis Workflow
The following diagram illustrates the systematic workflow for analyzing ethical conflicts in clinical settings, representing a methodology common to both secular and religious approaches:
Research Reagent Solutions: Bioethical Analysis Toolkit
Table 2: Essential Methodological Tools for Bioethics Research
| Research Tool | Function | Application Context |
|---|---|---|
| Principle-Based Analysis Framework | Systematic application of ethical principles (autonomy, beneficence, nonmaleficence, justice) to clinical cases [26] [46] | Structured analysis of ethical dilemmas across both secular and religious traditions |
| Qualitative Interview Protocols | In-depth exploration of stakeholder perspectives, values, and decision-making processes | Understanding how ethical principles are interpreted and weighted by patients, families, and clinicians |
| Case Analysis Templates | Standardized format for documenting and analyzing clinical ethics cases | Comparative study of similar ethical conflicts across different institutions and populations |
| Virtue Ethics Assessment Tool | Evaluation of character traits and virtues in healthcare decision-making [19] | Complement to principle-based approaches, focusing on moral character of decision-makers |
| Cross-Cultural Comparison Matrix | Systematic comparison of ethical norms and practices across different traditions | Identifying common ground and substantive differences between secular and religious approaches |
Data Synthesis and Comparative Analysis
Quantitative Assessment of Ethical Positions
The comparative analysis of secular and religious approaches to beginning and end-of-life issues reveals both significant divergences and surprising convergences. The following table synthesizes representative positions across major ethical dilemmas:
Table 3: Quantitative Comparison of Ethical Positions Across Frameworks
| Ethical Issue | Secular Framework Alignment | Religious Framework Alignment | Areas of Convergence | Empirical Support Status |
|---|---|---|---|---|
| Prenatal Diagnosis Termination | High support for parental autonomy and decision-making latitude | Generally restricted with exceptions for maternal health threats | Shared commitment to supportive counseling and palliative care options | Extensive clinical outcome data available |
| Advanced Directive Compliance | Strong emphasis on literal adherence to patient wishes | Interpreted through natural law principles and religious teachings | Agreement on importance of surrogate decision-makers when patients lack capacity | Mixed evidence on consistency of application |
| Palliative Sedation | Widely accepted for refractory symptoms with potential to hasten death | Accepted under principle of double effect with proper intent | Consensus on appropriateness for suffering relief despite theoretical differences | Strong evidence for efficacy in symptom control |
| Artificial Nutrition/Hydration | Generally viewed as medical treatment that can be withheld/withdrawn | Typically considered ordinary care that should be provided | Agreement that burdens may outweigh benefits in specific clinical circumstances | Limited quality evidence regarding clinical outcomes |
Decision-Making Pathways in Clinical Ethics
The following diagram maps the divergent decision-making pathways that often characterize secular and religious approaches to ethical conflicts, particularly regarding treatment limitations:
The comparative analysis of secular and religious approaches to beginning and end-of-life conflicts reveals a complex landscape characterized by both profound disagreements and significant common ground. The evidence suggests that the apparent intractability of these disputes often stems from mischaracterization of the conflict (presenting moral disagreements as factual ones) [45] and institutional pressures that distort proper ethical deliberation [19].
Moving beyond this apparent intractability requires recognition that bioethics is fundamentally a social ethic that requires "complex thinking from a variety of approaches that reach beyond a secular and religious divide" [44]. This dialogical approach does not seek to erase important differences or achieve superficial consensus, but rather to create opportunities for mutual understanding and more nuanced application of ethical principles in clinical practice. By accurately characterizing the nature of disagreements and focusing on shared commitments to patient welfare, healthcare professionals can navigate these challenging conflicts while respecting the diversity of moral perspectives that characterize contemporary pluralistic societies.
Conscientious objection (CO) in healthcare is defined as the refusal by a health care professional to provide a legal, medically appropriate, and patient-requested health care service due to personal religious or moral beliefs [49]. Often codified in law or professional codes of ethics as "conscience clauses," these provisions create a complex interface between individual practitioner beliefs and patient access to care [50]. This practice raises fundamental questions about the balancing of rights and duties within medicine, situated at the nexus of competing ethical frameworks.
This analysis examines the management of medical conscientious objection through the comparative lens of secular and religious bioethical foundations. While secular frameworks often prioritize patient autonomy and equitable access, religious perspectives may emphasize practitioner moral integrity and adherence to divine commands [5] [51]. By comparing international regulatory approaches, quantitative data on conscience clause implementation, and the underlying ethical reasoning, this guide provides a structured comparison for researchers and professionals navigating this contested domain.
Foundational Concepts and Ethical Frameworks
The debate around conscience clauses is fundamentally shaped by divergent secular and religious bioethical foundations. Understanding these distinct starting points is essential for contextualizing the regulatory and practical approaches to managing conscientious objection.
Secular Bioethical Frameworks
Secular approaches to bioethics typically rely on principles justifiable through public reason, rather than particular religious doctrines [5]. This framework aims to create a common ethical ground in pluralistic societies. Key characteristics include:
- Primary of Patient Autonomy: Secular bioethics often emphasizes the patient's right to self-determination and access to legal medical services [49]. The refusal of care based on a provider's personal beliefs is seen as a potential infringement on this autonomy.
- Fiduciary Duty: Within this framework, the healthcare professional's primary obligation is to the patient's well-being, creating a potential conflict when conscience objections override patient needs [50].
- Procedural Justice: Secular approaches frequently focus on creating systems that ensure equitable access to care, requiring that conscience clauses include mechanisms for referral or transfer of care to prevent patient abandonment [50].
Religious Bioethical Frameworks
Religious perspectives in bioethics derive their moral authority from theological sources and traditions [51]. These frameworks offer a different set of priorities:
- Moral Integrity and Divine Command: For many religious practitioners, complying with divine law or religious teaching takes precedence over patient preference, viewing certain medical procedures as intrinsically immoral [51].
- Rejection of Moral Neutrality: Some religious bioethicists argue that secular frameworks are not neutral but instead impose their own substantive worldview, one that may marginalize religious perspectives [51].
- Natural Law Theory: Particularly within Catholic bioethics, natural law theory posits that moral truths are accessible through reason and reflect God's eternal law, providing an objective basis for moral objections beyond personal preference [51].
Table 1: Comparison of Secular and Religious Bioethical Foundations
| Aspect | Secular Bioethics | Religious Bioethics |
|---|---|---|
| Moral Source | Public reason, empirical evidence, rational argument [5] | Divine revelation, religious tradition, sacred texts [51] |
| Primary Focus | Patient autonomy, social justice, harm reduction [49] [50] | Adherence to moral/divine law, practitioner integrity [51] |
| View of CO | Potentially problematic if restricting access; requires compromise [50] | Essential protection of moral integrity and religious freedom [51] |
| Resolution Mechanism | Institutional protocols, referral requirements, legal regulation [50] | Doctrinal adherence, spiritual discernment, religious community guidance [51] |
Quantitative Analysis of International Conscience Clause Implementation
Empirical research reveals significant variation in how conscience clauses are codified and implemented across different jurisdictions and healthcare professions. The following data provides a comparative overview of these regulatory approaches.
Pharmacist Codes of Ethics Across OECD Countries
A 2025 review of pharmacist Codes of Ethics in OECD countries offers insightful quantitative data on the prevalence and nature of conscience clauses [52]. This study examined 24 Codes of Ethics available in English, with findings summarized below.
Table 2: Conscientious Objection Provisions in Pharmacist Codes of Ethics (OECD Countries)
| Regulatory Characteristic | Number of Jurisdictions | Percentage |
|---|---|---|
| Explicitly mentions CO in Code of Ethics | 12 | 50% |
| Explicitly permits CO | 9 | 37.5% |
| Infers CO through moral/religious/personal grounds | 6 | 25% |
| Emphasizes maintaining continuity of care | 11 | 45.8% |
This data demonstrates that while half of the reviewed codes explicitly address conscientious objection, there remains significant variability in how these provisions are structured and what limitations are placed upon them [52]. The emphasis on continuity of care in nearly half of the codes indicates recognition of the need to balance practitioner conscience with patient access.
Historical and Geographic Patterns in Conscience Clause Adoption
Analysis of the historical development of conscience clauses reveals distinctive patterns:
- First Legal Recognition: The United Kingdom's 1967 Abortion Act contained the world's first healthcare conscience clause, specifically for abortion provision [49]. This precedent established the model subsequently adopted by many other jurisdictions.
- Selective Application: Conscience clauses appear predominantly in specific healthcare domains, particularly reproductive health (abortion, contraception), end-of-life care, and increasingly, gender-affirming treatments [49] [50].
- Institutional vs. Individual Claims: While only individuals possess conscience, institutional objections are increasingly common, particularly in religiously-affiliated healthcare facilities, potentially creating broader barriers to care [49].
Methodological Approaches to Studying Conscience Clauses
Research on conscientious objection employs diverse methodologies from document analysis to ethical reasoning frameworks. Understanding these approaches is essential for critical evaluation of studies in this field.
Document Analysis Protocol
The methodological approach used in the OECD pharmacist study illustrates a systematic protocol for comparative analysis of regulatory frameworks [52]:
- Source Identification: Researchers used the International Federation of Pharmacists (FIP) member organization list to identify professional and regulatory bodies in OECD countries.
- Document Retrieval: Codes of Ethics and related documents were gathered from organization websites using targeted keywords ("code of ethics," "code of conduct," "ethics," "guidelines," "standards").
- Screening and Inclusion: Documents were screened for relevance, with non-English documents and those without unifying codes across practice settings excluded.
- Thematic Analysis: Included documents underwent qualitative analysis using a pre-developed data collection form to identify and categorize conscience clause provisions.
This methodology provides a replicable framework for similar comparative studies across healthcare professions and geographic regions.
Ethical Analysis Frameworks
Philosophical analysis of conscience clauses typically employs several distinct methodological approaches:
- Comparative Ethical Reasoning: Analyzing how different ethical traditions (e.g., principlism, virtue ethics, casuistry, divine command theory) address conflicts between professional duties and personal morality [50] [51].
- Case-Based Deliberation: Examining specific clinical scenarios to identify competing values and potential compromise solutions [50].
- Historical-Genealogical Analysis: Tracing the historical development of conscience provisions to understand their original purpose and subsequent evolution [49].
Regulatory Models and Compromise Formulations
Current approaches to managing conscientious objection generally fall into several models with distinct compromise mechanisms aimed at balancing competing interests.
The Balancing Framework for Managing Conscientious Objection
The following diagram illustrates the key considerations and necessary compromise mechanisms required to balance practitioner conscience with patient care in ethical management of conscientious objection:
Specific Compromise Models in Practice
Various jurisdictions have implemented distinct models for managing conscientious objection, each with characteristic strengths and limitations:
- The Duty-Based Model: Emphasizes that healthcare professionals voluntarily assume certain duties when entering the profession, including providing all legal and medically appropriate services within their competence [49]. Conscience objections are viewed as potentially incompatible with these professional obligations.
- The Accommodation-Rights Model: Prioritizes protection of practitioner moral integrity through conscience rights, viewing healthcare as a fundamental expression of personal values that deserves accommodation [51].
- The Compromise Model: Seeks middle ground by permitting objection while imposing specific duties to ensure patient access, including mandatory referral, timely disclosure, and emergency exceptions [50].
Table 3: Comparison of Conscientious Objection Management Models
| Model Type | Core Principle | Implementation Mechanisms | Potential Limitations |
|---|---|---|---|
| Duty-Based Model | Primacy of professional obligations to patients [49] | Limited conscience exemptions; institutional guarantees of service availability | May marginalize moral diversity within profession [51] |
| Accommodation-Rights Model | Protection of practitioner moral/religious integrity [51] | Broad conscience protections; limited requirements for facilitation | May create significant barriers to patient care access [49] |
| Compromise Model | Balancing of competing rights through structured approach [50] | Mandatory referral; advance notice; emergency exceptions; maintenance of care continuity | May satisfy neither objectors nor access advocates; implementation challenges [50] |
Research Reagents and Methodological Tools
Studying conscience clauses requires specific methodological tools and conceptual frameworks. The following table outlines essential "research reagents" for investigating this domain.
Table 4: Essential Methodological Tools for Conscience Clause Research
| Research Tool | Function | Application Example |
|---|---|---|
| Document Analysis Framework | Systematic comparison of legal/ethical codes across jurisdictions [52] | Identifying variations in CO provisions across pharmacist codes of ethics in OECD countries |
| Ethical Reasoning Models | Application of principlism, casuistry, virtue ethics to CO cases [50] [51] | Analyzing conflicts between autonomy and moral integrity in specific clinical scenarios |
| Qualitative Interview Protocols | Exploring lived experiences of objectors, patients, and institutions [50] | Understanding impacts of CO on patient access in rural communities |
| Historical-Genealogical Method | Tracing historical origins and evolution of conscience clauses [49] | Examining motivations behind UK's 1967 Abortion Act conscience clause |
| Comparative Policy Analysis | Evaluating outcomes of different regulatory approaches across jurisdictions [52] | Assessing impact of mandatory referral requirements on abortion access |
The management of medical conscientious objection remains a deeply contested domain where secular and religious bioethical frameworks offer distinct, and often competing, perspectives. The comparative analysis presented in this guide demonstrates that effective compromise formulations require careful attention to both practitioner moral integrity and patient access to care.
Robust research in this field necessitates multiple methodological approaches—document analysis, ethical reasoning, empirical study of impacts, and comparative policy assessment. The increasing globalization of healthcare and diversification of moral communities suggests that developing ethically sound, practically workable approaches to conscience clauses will remain an essential task for bioethics researchers and healthcare policymakers. Future research should particularly focus on evaluating the real-world impacts of different compromise models on both practitioner satisfaction and patient outcomes across diverse healthcare systems.
The allocation of scarce medical resources represents one of the most profound challenges in contemporary healthcare, forcing explicit engagement with fundamental questions of value, justice, and morality. This challenge manifests across diverse contexts—from pandemic triage and organ transplantation to critical care resource distribution—where demand inevitably outstrips supply. These allocation decisions occur within pluralistic democracies characterized by significant diversity in moral and ethical frameworks, particularly between religious and secular perspectives [53]. The competing values inherent in these frameworks raise critical challenges regarding how to balance claims of religious liberty with claims to equal treatment in healthcare [53]. This article systematically compares religious and secular bioethical approaches to resource allocation, examining their foundational principles, practical applications, and implications for researchers and healthcare professionals navigating these complex ethical landscapes.
Foundational Ethical Principles: A Comparative Framework
Religious and secular bioethical approaches to resource allocation draw upon distinct foundational principles, though areas of convergence exist. The table below summarizes the core principles characterizing each perspective.
Table 1: Comparative Foundational Principles in Resource Allocation
| Aspect | Religious Approaches | Secular Approaches |
|---|---|---|
| Primary Orientation | Divine commandments and sacred texts; unconditional sanctity of life [54] | Human reason and philosophical principles; quality and utility of life [54] |
| Core Principles | Sanctity of life, duty to care, stewardship [54] [55] | Justice, utility, equity, autonomy, transparency [55] |
| View of Human Life | Sacred, inviolable, possessing intrinsic worth regardless of condition [54] | Valued, but quality and social considerations may be relevant [56] |
| Basis for Decisions | Religious authorities and traditions; unconditional respect for life [54] | Rational deliberation; balancing of multiple ethical values [53] [56] |
| Resource Distribution | Does not discriminate based on age, prognosis, or social utility [54] | Often employs prioritization based on medical and social factors [56] |
Secular Bioethical Frameworks
Secular bioethics typically employs multiple ethical values to guide allocation decisions, recognizing that no single principle suffices to capture all morally relevant considerations in complex healthcare rationing [56]. These frameworks must navigate what scholars term the "compatibility problem"—the challenge of integrating various ethical values into a coherent framework without internal contradictions [56]. Common principles include:
- Utility-based principles: Aim to maximize beneficial outcomes, often expressed through concepts like saving the most lives, preserving the most life-years, or maximizing quality-adjusted life years (QALYs) [56].
- Egalitarian principles: Emphasize equal moral concern for all individuals, potentially advocating for random selection (lotteries) or equal access when resources are scarce [56].
- Prioritarian principles: Focus on prioritizing the worst-off individuals, often operationalized through sickest-first allocation or prioritizing those with greatest need [57].
- Procedural values: Transparency, reciprocity, and stakeholder engagement ensure the legitimacy of allocation processes [55].
These principles frequently conflict in practice. For instance, utilitarian approaches that maximize life-years saved inherently favor younger patients, creating tension with egalitarian commitments to the equal worth of all lives regardless of age [56].
Religious Bioethical Frameworks
Religious perspectives on resource allocation, particularly those from Abrahamic traditions (Judaism, Christianity, Islam), typically emphasize the sanctity of life as an inviolable principle [54]. These traditions generally reject quality-of-life assessments or social utility calculations as primary allocation criteria, instead viewing human life as sacred regardless of clinical condition or social worth [54].
According to these perspectives, resource allocation should not discriminate between patients based on age, prognosis, or potential social contribution [54]. This creates significant tension with secular approaches that explicitly incorporate such factors. Religious frameworks also emphasize duty to care and stewardship, recognizing that resources are limited but insisting that allocation decisions must respect the intrinsic value of every human life [54] [55].
Practical Application: Allocation Protocols and Decision-Making
The theoretical differences between religious and secular approaches manifest concretely in practical allocation protocols and decision-making processes.
Table 2: Operational Differences in Allocation Scenarios
| Allocation Scenario | Secular Approach | Religious Approach |
|---|---|---|
| Pandemic Ventilator Triage | Prioritization by prognosis, likelihood of survival, and/or life-years saved [56] | Opposition to categorical exclusion based on age or disability; emphasis on individual assessment [54] |
| Organ Transplantation | MELD-Na score (sickest-first) for livers; wait time for kidneys; combination of medical and social criteria [58] | Support for need-based allocation without exclusion due to age or comorbidity [54] |
| Emergency Department Triage | Combination of urgency and first-come, first-served; algorithmic approaches to determine priority [58] | Equal regard for all patients regardless of social value or potential outcome [54] |
| End-of-Life Care | Cost-benefit analysis; consideration of quality of life; possible justification for withdrawing care [54] | Preservation of life as absolute value; opposition to physician-assisted suicide [54] |
Secular Allocation Methodologies
Secular approaches increasingly employ algorithmic decision-making to enhance fairness and consistency in resource allocation. These systems leverage predictive analytics to compute prognoses in real-time, potentially overcoming human limitations in clinical judgment [58]. Algorithmic approaches offer several advantages:
- Reduced prognostic uncertainty: Algorithms can harness vast amounts of data to generate more accurate predictions of patient outcomes [58].
- Consistency: Computerized systems apply allocation rules uniformly, avoiding the inconsistencies of individual clinician judgment [58].
- Transparency: Explicit algorithmic rules make allocation criteria public and subject to debate, enhancing accountability [58].
However, these approaches face significant challenges, particularly regarding value compatibility. As noted in pandemic allocation frameworks, combining multiple ethical values often creates internal inconsistencies when values conflict [56]. For instance, maximizing total benefits (utility) may directly contradict helping the worst-off (priority) when allocating scarce resources [56].
Religious Allocation Methodologies
Religious approaches generally reject purely algorithmic or utilitarian calculations, emphasizing instead individual assessment within a framework of moral absolutes. These perspectives often prioritize:
- Categorical protections: Certain groups (e.g., the elderly, disabled) must not be categorically excluded from care based on age or disability status [54].
- Moral boundaries: Actions intrinsically wrong (e.g., actively hastening death) are prohibited regardless of consequences [54].
- Stewardship within constraints: While recognizing resource limitations, religious frameworks insist that allocation decisions must occur within moral boundaries that respect life's sanctity [54].
The Jewish tradition, for instance, explicitly prohibits killing based on the Sixth Commandment, unconditionally rejecting euthanasia and physician-assisted suicide [54]. Similarly, other Abrahamic traditions emphasize that human life possesses sacred value independent of clinical or social considerations.
Conceptual Framework: Ethical Reasoning Pathways
The diagram below illustrates the distinct ethical reasoning pathways characteristic of secular and religious approaches to resource allocation.
Ethical Reasoning Pathways for Resource Allocation
This diagram illustrates how secular and religious approaches follow fundamentally different reasoning pathways when addressing resource scarcity, ultimately arriving at distinct allocation outcomes while encountering points of significant ethical tension.
Research Toolkit: Analytical Frameworks for Resource Allocation
Researchers studying allocation ethics require specific conceptual tools to navigate this complex landscape. The table below outlines essential analytical frameworks and their applications.
Table 3: Research Reagent Solutions for Allocation Ethics
| Research Tool | Function | Application Context |
|---|---|---|
| Multi-Principle Framework | Identifies and weights multiple ethical values [55] [56] | Pandemic planning; institutional policy development |
| Value Compatibility Analysis | Resolves conflicts between competing ethical principles [56] | Algorithm design; policy consistency assessment |
| Comparative Religious-Secular Analysis | Identifies points of convergence and divergence [54] | Stakeholder engagement; policy justification |
| Algorithmic Fairness Assessment | Evaluates equity in computational allocation systems [58] | Triage protocol development and validation |
| Transparency and Procedural Justice Metrics | Assesses legitimacy of decision processes [55] | Policy implementation and public communication |
Experimental Protocol: Value Compatibility Assessment
Addressing the compatibility problem in ethical frameworks requires systematic methodology. Researchers can employ these evidence-based pathways to mitigate value conflicts:
Value Specification: Rather than balancing abstract principles, specify concrete operationalizations. For example, rather than generally prioritizing the "worst off," define specific disadvantage metrics (e.g., socioeconomic status, healthcare access) [56].
Value Incorporation: Include multiple values without assigning fixed weights. A vaccine allocation framework might prioritize both healthcare workers (reciprocity) and high-risk populations (priority) through sequential phases rather than numerical trade-offs [56].
Value Reinforcement: Identify strategies that advance multiple values simultaneously. Prioritizing disadvantaged groups in pandemic response can simultaneously advance both equity and utility if these populations face higher transmission risks [56].
Evidence Integration: Incorporate empirical data to resolve apparent conflicts. If data shows identical outcomes across age groups, it resolves the apparent conflict between maximizing life-years and equal regard for all ages [56].
This methodological approach helps transform radical pluralism into workable pluralism, creating frameworks capable of guiding actual allocation decisions despite persistent theoretical tensions [56].
Religious and secular approaches to allocating scarce medical resources offer distinct yet potentially complementary frameworks for addressing healthcare's scarcity challenges. While secular bioethics emphasizes multiple ethical principles and often employs algorithmic precision to maximize benefits and ensure procedural fairness, religious perspectives maintain categorical commitments to life's sanctity and equal regard for all persons regardless of clinical prognosis or social utility [54] [56].
For researchers and healthcare professionals, recognizing these distinct foundations enables more nuanced engagement with allocation ethics. Rather than seeking a single unified approach, productive paths forward may include transparent deliberation about value conflicts, context-sensitive frameworks that acknowledge multiple moral commitments, and procedural justice in decision-making processes [53] [55]. Such approaches respect the pluralistic nature of contemporary societies while addressing the urgent practical need for fair allocation systems that maintain public trust during periods of resource scarcity [53].
Clinical Ethics Committees (CECs) have become established fixtures in healthcare institutions worldwide, serving as crucial forums for addressing moral dilemmas in clinical practice. These committees operate at the complex intersection of patient care, institutional policy, professional norms, and diverse value systems. Within the context of a broader thesis comparing secular and religious bioethics foundations, CECs represent a practical convergence point where abstract ethical principles are translated into concrete guidance for resolving disputes. The central function of CECs has evolved from primarily educational entities to active dispute resolution bodies, positioning them as essential mediators in healthcare conflicts [59].
As biotechnology and medical research globalize, the ethical frameworks informing CEC deliberations have expanded beyond their Western, often secular-Christian origins, to incorporate perspectives from multiple religious and cultural traditions [60] [15]. This article examines how CECs mediate disputes by comparing their operational protocols, analyzing quantitative data on their functions, and situating their methodologies within both secular and religious bioethical traditions. By objectively comparing these foundations through structured data and conceptual frameworks, we provide researchers and drug development professionals with a comprehensive understanding of how ethical bridges are built in clinical settings.
Comparative Foundations: Secular and Religious Bioethics Frameworks
Bioethics as a field draws from multiple philosophical and religious traditions, each contributing distinct perspectives on fundamental questions of life, death, and moral responsibility. Understanding these foundations is essential for comprehending the theoretical underpinnings that CECs may employ in mediation processes.
Key Doctrinal Comparisons Across Religious Traditions
Table 1: Comparative Religious Bioethics on Selected Clinical Issues
| Ethical Issue | Islamic (RAA Perspective) | Roman Catholic | Orthodox Jewish | Chinese Buddhist |
|---|---|---|---|---|
| Beginning of Life | Life begins at conception; abortion forbidden except medical necessity [33] | Life begins at conception; abortion prohibited [33] | Life begins at conception; abortion generally prohibited [33] | Based on dependent origination; no single Creator God [61] |
| End of Life | Active euthanasia forbidden; life support withdrawal permitted after brain death confirmation [33] | Active euthanasia prohibited; ordinary care required but extraordinary treatment not obligatory [33] | Active euthanasia prohibited; preservation of life paramount [33] | Compassionate end-of-life care; influenced by karma and rebirth concepts [61] |
| Organ Transplantation | Permitted with conditions: medical necessity, donor death certainty, no financial transaction [33] | Permitted as act of charity and solidarity [33] | Permitted with rabbinical supervision and proper respect for donor [33] | Contextually acceptable; consistent with compassionate action [61] |
| Assisted Reproduction | IVF permitted between spouses; third-party donation prohibited [33] | Limited acceptance; opposes third-party involvement and embryo destruction [33] | Permitted with specific guidelines; often requires rabbinical consultation [33] | Focus on intention and compassionate action; context-dependent [61] |
| Research Ethics | Prioritizes prevention of harm; aligns with Maqasid al Shariah principles [33] | Emphasizes human dignity and common good [33] | Values preservation of life and health promotion [33] | Focus on reducing suffering and compassionate intention [61] |
Philosophical Tensions in Bioethical Foundations
The secular-religious divide in bioethics represents not merely different conclusions but fundamentally distinct methodological approaches. Secular bioethics typically emphasizes principle-based reasoning, autonomy, and empirical evidence, often rooted in Enlightenment traditions that themselves developed from Christian ethics [15]. Religious bioethics, while diverse, generally draws from revealed texts, theological traditions, and communal values, with the "outsider perspective" of secular thought often presumed to be neutral despite its particular historical development [15].
This tension manifests practically in CEC operations. For instance, the Christian bioethics model emphasizes the sacredness of life as created by God, framing human life as bearing intrinsic value derived from divinity [61]. In contrast, Chinese Buddhist bioethics understands life through dependent origination and karmic causality without reference to a creator deity [61]. These foundational differences can lead to divergent approaches in clinical dilemmas, particularly regarding beginning and end-of-life issues where the definition and value of human life are paramount.
Quantitative Analysis of Ethics Committee Observations and Functions
Empirical research on ethics committees provides critical insights into their practical functioning, highlighting common challenges and areas for improvement in dispute mediation.
Prevalence of Empirical Research in Bioethics
Table 2: Growth of Empirical Research in Bioethics Journals (1990-2003)
| Journal | Total Articles | Empirical Studies | Percentage |
|---|---|---|---|
| Nursing Ethics | 367 | 145 | 39.5% |
| Journal of Medical Ethics | 762 | 128 | 16.8% |
| Journal of Clinical Ethics | 604 | 93 | 15.4% |
| Bioethics | 332 | 22 | 6.6% |
| Other Six Journals | 1964 | 47 | 2.4% |
| Total | 4029 | 435 | 10.8% |
Source: Adapted from PMC2565792 [62]
The data reveal a statistically significant increase (χ2 = 49.0264, p<.0001) in empirical studies from 1990-1996 (n=126) to 1997-2003 (n=309), indicating growing recognition of empirical methods in bioethics [62]. This trend toward evidence-based approaches complements traditional normative reasoning in ethics consultation.
Ethics Committee Observations by Principle and Region
Table 3: Ethics Committee Observations on Research Protocol Non-Compliance
| Ethical Principle | Latin American Protocols | European Protocols | Experimental Studies |
|---|---|---|---|
| Justice | Up to 100% lack of adherence | Up to 100% lack of adherence | Not specified |
| Autonomy | 26% (95% CI: 20-33) | Not specified | 17% (95% CI: 13-22) |
| Beneficence | 41.17% to 77.38% lack of adherence | 5.26% to 27.11% observations per protocol | Not specified |
Source: Adapted from medRxiv 2024.06.23.24309373 [63]
Recent analysis of Research Ethics Committees (RECs) observations reveals significant regional and study-type variations in ethical principle adherence. These disparities reflect cultural differences, interpretive variations, and resource disparities among ethics committees [63]. The high prevalence of justice-related observations across all regions highlights ongoing challenges in fair participant selection and equitable distribution of research benefits and burdens.
CEC Dispute Resolution: Protocols and Process Analysis
Standardized Methodology for Ethics Case Consultation
The ethics consultation process typically follows structured protocols to ensure comprehensive and fair dispute resolution. Based on empirical observation of CEC operations, the standard methodology includes:
1. Request Initiation: Involved parties (clinicians, patients, families) contact the CEC office or member to request consultation for moral conflicts on the ward [64].
2. Suitability Assessment: At least two CEC members evaluate whether the request warrants ethics consultation based on the presence of genuine ethical conflict versus other types of disputes [64].
3. Participant Invitation: All parties involved in the conflict, including patients or relatives where appropriate, are invited to participate in the consultation to ensure multiple perspectives are represented [64].
4. Facilitated Discussion: Trained CEC members moderate structured discussion where all participants can articulate their perspectives, with special attention to power dynamics and hierarchical structures that may suppress certain voices [64].
5. Consensus Building: The committee facilitates development of ethically justifiable resolutions through identification of shared values and negotiation of differences, rather than imposing decisions [64].
6. Documentation and Follow-up: The process, considerations, and outcomes are documented, with follow-up mechanisms to assess implementation and effectiveness of the resolution [64].
CEC members are typically trained according to established curricula standards, such as those of the Academy of Ethics in Medicine, which includes 40 hours of theoretical and practical training plus 20 hours of simulated case scenarios [64].
Quantitative Analysis of CEC Consultation Outcomes
Research evaluating CEC consultations reveals important patterns in their operation and effectiveness. Qualitative evaluation through non-participating observation of ethics case consultations and interviews with participants identifies that 'communication problems' and 'hierarchical team conflicts' are the main aspects leading to ethics consultation [64]. These conflicts create a vicious circle where unresolvable differences arise in the context of team conflicts and prevent solutions from being found.
Studies show hierarchical asymmetries common in medical fields often perpetuate these conflicts, and participants sometimes experience CECs as maintaining rather than overcoming these hierarchies [64]. This highlights the critical importance of committee composition and process design in effective dispute resolution.
Table 4: Research Reagent Solutions for CEC and Bioethics Research
| Research Tool | Function | Application Context |
|---|---|---|
| SPIRIT 2025 Guidelines | Standardized protocol items for interventional trials [65] | Ensuring complete and transparent ethics review processes |
| Grounded Theory Methodology | Systematic qualitative analysis of ethical dilemmas [64] | Understanding perspectives of all participants in ethics consultations |
| Non-Participant Observation Protocol | Structured documentation of ethics consultations [64] | Direct observation of CEC dynamics and decision processes |
| Empirical Bioethics Analysis Framework | Quantitative assessment of ethical publications [62] | Tracking evolution and focus of bioethics research |
| Comparative Religious Bioethics Matrix | Side-by-side analysis of multi-tradition perspectives [33] [61] | Contextualizing disputes within diverse value systems |
| Delphi Survey Methodology | Structured group communication process [65] | Building consensus on ethical guidelines and standards |
The updated SPIRIT 2025 statement provides an evidence-based checklist of 34 minimum items to address in trial protocols, including new emphasis on open science, harm assessment, and patient involvement [65]. These guidelines serve as crucial methodological resources for ensuring ethical rigor in clinical research that may subsequently be reviewed by CECs.
Analysis: Integration of Secular and Religious Frameworks in CEC Dispute Resolution
The quantitative data and observational research reveal both challenges and opportunities for CECs in mediating disputes across ethical traditions. Several key patterns emerge from the analysis:
Structural and Process Challenges in CEC Mediation
Empirical research identifies that CECs often struggle with institutional hierarchies that mirror the very power dynamics they aim to mediate. Hierarchical asymmetries common in medical settings can be perpetuated within CEC proceedings unless deliberately addressed through process design [64]. This is particularly problematic when mediating disputes between healthcare professionals of different status levels or when cultural/religious values of patients conflict with institutional protocols.
Quantitative analysis shows that most empirical studies in bioethics employ a quantitative paradigm (64.6%, n=281), with the main research topic being prolongation of life and euthanasia (n=68) [62]. This indicates that the most contentious issues at the secular-religious intersection receive the most empirical attention, providing data for evidence-based dispute resolution.
Promising Practices for Cross-Cultural Bridge Building
Successful CEC mediation in contexts of diverse ethical foundations employs several key strategies:
1. Multi-Perspective Case Presentation: To avoid dominance by physicians and excessively factual presentations, cases can be presented by both physicians and nurses, strengthening interpersonal and emotional aspects while integrating both professional perspectives [64].
2. Distinction Between Team Conflicts and Ethical Issues: Research suggests that discussion of team conflicts and clinical ethical issues should not be combined, as the former represents a mandate for team supervision rather than ethics consultation proper [64].
3. Explicit Methodology Selection: CECs benefit from consciously selecting between secular principle-based approaches and religious value-based frameworks depending on the participants and context, or explicitly integrating both [60] [15].
The globalization of biotechnology and research necessitates greater cross-cultural ethical dialogue. As researchers and companies sometimes relocate to countries with different ethical-legal environments, international ethical standards become increasingly important [60]. CECs serve as localized laboratories for developing these standards through practical application to real clinical disputes.
Clinical Ethics Committees play an indispensable role in mediating disputes in increasingly complex healthcare environments characterized by diverse value systems. The quantitative data reveal both the growing empirical foundation of bioethics and persistent challenges in applying ethical principles consistently across different contexts and regions.
Effective CEC mediation requires both process excellence—through standardized consultation protocols and balanced representation—and conceptual flexibility—through understanding of both secular and religious bioethical traditions. The comparative analysis of religious bioethics demonstrates significant common ground on many issues despite different foundational premises, providing hope for bridge-building in clinically contentious situations.
For researchers and drug development professionals, understanding CEC structures and functions is essential not only for navigating ethics review processes but also for anticipating how ethical disputes may arise in clinical applications of new technologies. By employing the methodological tools and conceptual frameworks outlined in this analysis, CECs can continue to evolve as effective mediators that build ethical bridges across diverse value systems while maintaining rigorous protection of patient welfare and ethical principles.
Evaluating Frameworks and Forging Common Ground: A Pluriversal Approach
The development of public health policy does not occur in a value vacuum. It is profoundly shaped by underlying bioethical frameworks, which provide structured approaches to navigating complex moral dilemmas in healthcare and medicine. These frameworks are broadly categorized into religious and secular traditions, each offering distinct foundations for moral reasoning and policy justification. Religious bioethics typically draws upon sacred texts, theological principles, and established doctrinal teachings to inform ethical positions, emphasizing concepts such as the sanctity of life and natural law [66]. In contrast, secular bioethics relies on philosophical reasoning, empirical evidence, and principles justifiable through public reason—arguments that can be accepted by rational persons regardless of their specific religious or metaphysical commitments [53] [5].
The tension between these approaches has significant practical implications for policy-making in pluralistic societies. As contemporary democracies grow increasingly diverse, policymakers face the challenge of balancing deeply held religious values with the need for publicly justified policies that respect all citizens as free and equal [53]. This comparative analysis examines how these foundational ethical frameworks influence specific public health domains, including vaccine mandates, reproductive health, end-of-life care, and healthcare access, with the aim of providing researchers and health professionals with a structured understanding of this complex landscape.
Comparative Theoretical Foundations
Understanding how religious and secular ethics shape policy requires examining their distinct theoretical starting points, which generate different moral priorities and decision-making procedures.
Table 1: Foundational Principles of Religious and Secular Bioethics
| Aspect | Religious Bioethics | Secular Bioethics |
|---|---|---|
| Primary Foundation | Divine command, sacred texts, theological tradition, natural law [66] | Human reason, empirical evidence, philosophical principles [3] |
| Moral Authority | Religious institutions, spiritual leaders, interpretive communities [5] | Democratic processes, expert consensus, public justification [53] |
| Key Principles | Sanctity of life, human dignity as created order, stewardship [66] | Autonomy, beneficence, non-maleficence, justice [11] |
| Policy Justification | Alignment with religious doctrine and moral teachings [66] | Public reason, secular rationale, evidence-based outcomes [53] [67] |
| View of Human Person | Substantialist: body-soul unity with inherent dignity [66] | Often functionalist: defined by capacities like rationality or autonomy [66] |
Religious Bioethical Foundations
Religious bioethics, particularly within the personalist tradition often associated with Catholic moral theology, emphasizes the inherent dignity and worth of every human person simply by virtue of who they are, not merely for their capacities or choices [66]. This framework is rooted in a substantialist concept of the human person as a body-soul composite, possessing intrinsic value that demands respect regardless of developmental stage, cognitive ability, or health status. According to this view, the ethical value of an action must be considered not only under the subjective aspect of intentionality but also in terms of its objective content and consequences [66]. This approach often translates into policies that prioritize protection of vulnerable human life at all stages, restrictions on certain technological interventions perceived as violating natural law, and conscientious objection protections for healthcare providers.
Secular Bioethical Foundations
Secular bioethics encompasses diverse approaches, including principlism (emphasizing respect for autonomy, non-maleficence, beneficence, and justice), utilitarian models (focusing on consequence maximization), and liberal frameworks (prioritizing individual rights and freedoms) [66]. What unites these approaches is their reliance on public reason—the idea that in pluralistic societies, policy justifications should be accessible to all reasonable citizens, not dependent on specific religious worldviews [53] [5]. The secular framework employs methodological approaches such as empirical bioethics, which integrates quantitative and qualitative research methods to inform ethical analysis [11]. This tradition emphasizes procedural fairness, evidence-based policy, and neutral justification that can be accepted by people holding different comprehensive doctrines.
The diagram above illustrates how religious and secular ethical frameworks derive from different foundational sources, develop distinct moral principles, and ultimately influence specific policy domains. While often operating independently, these frameworks sometimes address the same policy areas (indicated by dashed lines), though typically with different rationales and implementation approaches.
Analytical Framework and Methodology
To systematically compare the influence of religious and secular ethics on public health policy, we propose a methodological framework based on mid-level principles that can be operationalized for policy analysis [53]. This approach acknowledges that while religious and secular traditions may have different ultimate foundations, they can often find common ground through shared moral principles that serve as a basis for policy development in pluralistic societies.
Table 2: Analytical Framework for Assessing Ethical Influence on Health Policy
| Analytical Principle | Operational Definition | Policy Assessment Questions |
|---|---|---|
| Liberty Principle [53] [67] | Protection of religious and personal freedom to the highest degree possible without causing significant harm | Does the policy accommodate diverse religious and moral viewpoints while preventing harm to others? |
| Equality Principle [53] [67] | Equal treatment of different religions and equal treatment of religious and non-religious citizens | Does the policy create unequal burdens or benefits based on religious affiliation or worldview? |
| Neutrality Principle [53] [67] | Governmental neutrality toward religious and secular comprehensive doctrines | Is the policy justifiable through public reason rather than relying solely on sectarian rationales? |
| Sociopolitical Equality [53] [67] | Protection of equal sociopolitical relations among citizens | Does the policy reinforce or mitigate existing power disparities in healthcare access and decision-making? |
| Harm Principle [67] | Restriction of liberty only to prevent significant harm to others | Does the policy balance individual freedoms with protection of public health and third parties? |
Application Methodology
The analytical process involves applying these principles to specific health policy domains through systematic case comparison. For each policy area, researchers should:
- Identify the predominant ethical influences during policy formation
- Analyze the primary justification offered for the policy (religious, secular, or hybrid)
- Assess the policy outcomes using the mid-level principles framework
- Evaluate implementation challenges arising from ethical pluralism
- Document accommodation mechanisms for conscientious objection
This methodological approach allows for structured comparison across different policy domains and ethical traditions, enabling researchers to identify patterns of influence and potential strategies for resolving policy conflicts in morally pluralistic societies.
Policy Domain Case Studies
Vaccine Policy and Religious Accommodation
Vaccine policy represents a critical area where religious and secular ethical frameworks interact, particularly regarding mandates and exemptions. The COVID-19 pandemic brought these tensions to the forefront, raising questions about the limits of religious accommodation when public health is at stake [67].
From a secular public health ethics perspective, vaccine mandates are typically justified through the harm principle and utilitarian calculations that prioritize disease prevention and herd immunity [67]. This approach emphasizes societal beneficence and the protection of vulnerable populations, potentially limiting religious exemptions when vaccination rates fall below public health thresholds.
Religious ethics approaches to vaccination are diverse, with most major religions supporting immunization as an act of stewardship and neighbor love, though some individuals raise conscientious objections based on specific beliefs [67]. The policy challenge lies in distinguishing genuinely religious objections from secular concerns disguised as religious claims, while respecting authentic religious liberty.
The accommodation framework suggests that policies should generally exempt religious objections while ensuring they do not impose significant health risks on third parties [53] [67]. However, during public health emergencies, the balance may shift toward stricter limits on exemptions, particularly when herd immunity is compromised and vulnerable populations are at risk.
Reproductive Health Policies
Reproductive health represents one of the most contentious areas of conflict between religious and secular ethical frameworks, with profound implications for policy development.
Table 3: Ethical Approaches to Reproductive Health Policy
| Policy Domain | Religious Ethics Influence | Secular Ethics Influence | Policy Tensions |
|---|---|---|---|
| Abortion Policy | Emphasis on sanctity of life from conception; restrictions to protect unborn life [66] [67] | Priority on bodily autonomy and women's rights; focus on health outcomes [67] | Fundamental conflict over moral status of embryo/fetus; conscience protections vs. access |
| Contraception Access | Natural law objections to artificial contraception; religious liberty claims [5] | Public health approach focusing on family planning and reproductive autonomy [5] | Mandated insurance coverage vs. employer religious objections; global health implications |
| Reproductive Technologies | Concerns about separation of procreation from marital union; embryo protection [66] | Autonomy-based approach supporting reproductive freedom and scientific innovation [5] | Regulation of IVF; embryo research; genetic screening and modification |
These conflicts manifest in policy debates through what political philosophers call the "public reason" requirement—the expectation that policy justifications in pluralistic democracies should appeal to reasons that are accessible to all reasonable citizens, not merely those who share particular religious premises [53] [67]. This creates tension when religious institutions seek to impose restrictions based on theological premises that are not widely shared by the broader population.
End-of-Life Care and Conscience Protections
End-of-life policy represents another domain of significant ethical disagreement, particularly regarding medical aid in dying and the limits of conscientious objection. Personalist religious bioethics typically opposes intentional life-ending actions based on the sanctity of life principle, while many secular frameworks emphasize individual autonomy and relief of suffering at the end of life [66] [3].
These foundational differences translate into policy conflicts regarding:
- Conscience protections for healthcare institutions and professionals who object to participating in life-ending procedures [53]
- Regulatory safeguards against potential abuses in medical aid-in-dying laws
- Access disparities created when religiously-affiliated healthcare systems dominate local markets and decline to provide legal services
The compromise view emerging in some secular bioethics literature attempts to balance these competing claims by allowing individual conscientious objection while requiring effective referral to willing providers [3]. However, this approach remains controversial, as some religious providers view referral as complicity in morally problematic actions [3].
Research Toolkit for Ethical Policy Analysis
Researchers analyzing the influence of religious and secular ethics on health policy require both conceptual and empirical tools to conduct rigorous comparative studies.
Table 4: Research Reagent Solutions for Ethical Policy Analysis
| Research Tool | Function | Application Example |
|---|---|---|
| Principles-Based Analysis Framework [11] | Structured assessment using mid-level principles | Applying liberty, equality, and neutrality principles to vaccine mandate policies |
| Empirical Bioethics Methods [11] | Mixed-methods approach combining normative and empirical research | Surveying stakeholder values while analyzing ethical implications of policy options |
| Public Reason Assessment [53] [67] | Evaluation of policy justifications for accessibility to diverse citizens | Analyzing whether religiously-influenced policies can be justified through secular rationale |
| Comparative Case Study Methodology | Systematic comparison across policy domains and jurisdictions | Identifying patterns of religious influence across different healthcare systems |
| Stakeholder Mapping Analysis | Identification of key actors and their ethical commitments | Mapping religious, secular, and professional organizations influencing policy development |
Implementation Protocols
For researchers investigating specific policy domains, we recommend the following methodological protocol:
Policy Tracing: Document the development process of a specific health policy, identifying key moments where religious or secular ethical arguments influenced the policy trajectory.
Discourse Analysis: Systematically analyze legislative debates, regulatory comments, and media coverage to identify the relative influence of religious versus secular ethical frameworks.
Stakeholder Interviews: Conduct structured interviews with policymakers, advocates, and implementers to understand how ethical considerations shaped policy development.
Comparative Assessment: Apply the mid-level principles framework (Table 2) to evaluate the policy according to liberty, equality, neutrality, and sociopolitical equality criteria.
Outcome Evaluation: Assess the practical impact of the policy on different populations, particularly religious minorities and marginalized groups.
This multidimensional approach allows for comprehensive analysis of how ethical frameworks translate into concrete policy mechanisms and population health outcomes.
This comparative analysis demonstrates that both religious and secular ethical frameworks significantly shape public health policy through distinct foundational commitments, justificatory strategies, and policy priorities. Religious bioethics, particularly in the personalist tradition, emphasizes the inherent dignity of every human person and often supports policies that protect vulnerable life, accommodate conscientious practice, and respect natural limits on technological intervention [66]. Secular bioethics, operating through frameworks such as principlism and public reason, typically prioritizes individual autonomy, evidence-based outcomes, and neutral justifications accessible to all citizens regardless of their comprehensive worldviews [53] [67].
The most productive path forward for health policy in pluralistic societies may lie in integrative approaches that respect religious liberty while ensuring policies are justifiable through public reason. This might include:
- Developing hybrid justifications for policies that draw on both religious and secular moral insights
- Creating structured accommodation systems that respect conscience while ensuring equitable access to services
- Employing empirical bioethics methodologies that ground normative analysis in rigorous evidence about policy impacts [11]
For researchers and drug development professionals, understanding these ethical dynamics is essential for navigating the complex policy landscape that shapes healthcare delivery, research funding, and therapeutic innovation. Future research should particularly focus on how emerging technologies—from artificial intelligence to genetic engineering—are challenging both religious and secular ethical frameworks and generating new policy dilemmas that require careful comparative analysis.
The field of bioethics stands at a critical crossroads in an increasingly globalized and pluralistic world. The dominant secular frameworks that have guided bioethical decision-making for decades are now being challenged to expand their epistemological boundaries to include religious perspectives as legitimate sources of ethical knowledge. This expansion is not merely a gesture of political correctness but represents a fundamental recognition that religious traditions offer substantive moral insights essential for addressing complex bioethical challenges. As our scientific capabilities advance at an unprecedented pace, the need for robust ethical deliberation that draws from humanity's diverse wisdom traditions becomes increasingly urgent.
The call for inclusivity is grounded in both practical and philosophical considerations. Practically, religious communities constitute the majority of the global population, with approximately 84% of people worldwide identifying with a religious group [20]. Philosophically, the very premise of ethical reasoning demands that we consider all relevant sources of moral insight, particularly those that have sustained moral communities across centuries. The emerging pluriversal approach to bioethics argues for "a world where many worlds fit," rejecting the universalization of a single set of secular principles in favor of a more inclusive dialogue that honors diverse moral traditions [22]. This paper argues that welcoming religious perspectives as epistemic peers—equally credible sources of ethical knowledge—strengthens the field of bioethics by expanding its conceptual resources, enhancing its cultural relevance, and enriching its moral imagination.
Theoretical Framework: Secular and Religious Approaches to Bioethics
Dominant Secular Paradigms in Contemporary Bioethics
Modern bioethics has been largely shaped by secular frameworks that prioritize rationality, empirical evidence, and principles ostensibly accessible to all reasonable people regardless of their metaphysical commitments. The principlist approach developed by Beauchamp and Childress—centered on autonomy, beneficence, nonmaleficence, and justice—has become particularly influential in medical ethics [68]. This framework operates on the assumption that these principles can form a common morality that transcends particular religious or cultural viewpoints, providing a neutral ground for ethical deliberation in pluralistic societies.
Secular bioethics often grounds its authority in what philosopher John Rawls termed "public reason"—the idea that political and ethical decisions should be justified through arguments that any rational person could accept, without appealing to comprehensive religious or philosophical doctrines [5]. This approach aims to create a level playing field for moral discourse in societies characterized by religious diversity. However, critics argue that this seemingly neutral framework actually privileges certain Western, secular ways of thinking while marginalizing alternative perspectives, particularly religious ones that millions of people worldwide find morally authoritative [5] [22].
Religious Bioethics as Substantive Moral Traditions
In contrast to secular frameworks, religious approaches to bioethics typically derive their moral content from specific theological premises, sacred texts, and long-standing traditions of moral reasoning. These traditions offer content-full moral visions that provide substantive guidance on issues ranging from the beginning and end of life to the just distribution of healthcare resources. Rather than seeking thin, universal principles, religious bioethics tends to emphasize the importance of particular moral communities and their distinctive understandings of human flourishing.
The Christian bioethical tradition, for instance, draws on concepts of human dignity grounded in the belief that humans are created in the image of God, leading to substantive positions on issues such as the sanctity of life [51]. Islamic bioethics integrates principles from the Qur'an and Hadith to address contemporary medical dilemmas, while Jewish bioethics brings centuries of Talmudic reasoning to bear on modern healthcare challenges [5]. These traditions do not merely offer alternative routes to conclusions reachable through secular reasoning; they often provide fundamentally different ways of conceptualizing the moral landscape itself.
Table: Comparison of Secular and Religious Bioethical Approaches
| Aspect | Secular Bioethics | Religious Bioethics |
|---|---|---|
| Foundation | Human reason, empirical evidence, principles | Sacred texts, theological doctrines, tradition |
| Epistemology | Publicly accessible reasons | Divine revelation, religious authority, reasoned tradition |
| Moral Content | Thin, general principles | Thick, substantive visions of human flourishing |
| Scope | Universal applicability | Particular to religious communities with universal aspirations |
| Key Concepts | Autonomy, justice, beneficence | Sanctity of life, divine command, natural law, stewardship |
The Pluriversal Alternative: Beyond the Secular-Religious Divide
A promising middle path emerges in what bioethicist Nancy Jecker and colleagues term the "pluriversal approach" to bioethics [22]. This framework acknowledges deep differences between secular and religious worldviews while establishing ethical constraints for productive dialogue across these differences. The pluriversal method recognizes religious and secular approaches not just as different worldviews but as "different worlds" that potentially suffuse many aspects of daily life [22].
This approach establishes five key ethical constraints for cross-worldview dialogue: (1) Civility - engaging respectfully without requiring religious people to translate their commitments into putatively neutral language; (2) Respect for law - working within legal frameworks while recognizing their limitations; (3) Justice - ensuring fair treatment and the perception of fair treatment; (4) Non-domination - prohibiting arbitrary and controlling influence by any party; and (5) Toleration - avoiding undue severity in judging others [22]. These constraints create a framework for dialogue that takes religious perspectives seriously as legitimate sources of ethical insight without privileging them over secular approaches or vice versa.
Empirical Evidence: The Persistent Role of Religion in Moral Reasoning
Psychological Evidence of Religious Intuitions
Recent empirical research in psychology and cultural evolution reveals that religious intuitions persist even in highly secularized societies. A 2025 cross-cultural study spanning eight comparatively secular countries (Canada, China, Czechia, Japan, the Netherlands, Sweden, the United Kingdom, and Vietnam) with a total sample size of N=3,804 found that people intuitively favor religious belief over atheism [69]. Surprisingly, this pattern was not moderated by participants' own self-reported atheism—even atheists in relatively secular societies intuitively prefer belief to atheism, a phenomenon philosopher Daniel Dennett dubbed "belief in belief" [69].
This research suggests that rapid overt secularism may overlie latent proreligious intuitions. The study's authors hypothesize that despite declines in explicit religious belief, the long-standing influence of religion on moral and cooperative norms over centuries to millennia has left psychological traces that cannot be erased in just a few decades [69]. This provides empirical support for the claim that religious ways of thinking continue to shape moral reasoning even in apparently secular contexts.
Demographic Imperatives for Inclusivity
The demographic argument for including religious perspectives in bioethics is straightforward: the vast majority of the world's population identifies with a religious tradition. With approximately 2.4 billion Christians, 2 billion Muslims, 1.2 billion Hindus, and 0.5 billion Buddhists worldwide, religious communities represent the moral views and values of most healthcare recipients, providers, and policymakers [20]. Even in so-called secular societies like the United States, 81% of Americans reported belief in God in 2022, and all 50 state constitutions reference God or the divine [22].
Bioethics debates that exclude religious perspectives risk alienating many stakeholders and making bioethics less relevant from their standpoint. As Nancy Jecker and colleagues argue, "If bioethics claims to be global, its claims become suspect if the field excludes religion" [22]. This demographic reality creates a practical imperative for bioethics to develop more inclusive approaches that engage religious perspectives as legitimate contributors to ethical discourse.
Table: Experimental Evidence of Religious Intuitions in Secular Societies
| Research Focus | Methodology | Key Findings | Implications for Bioethics |
|---|---|---|---|
| Belief in belief [69] | Cross-cultural experimental philosophy task in 8 countries (N=3,804) | Even atheists in secular societies intuitively prefer religious belief to atheism | Secular bioethics may overlook persistent religious intuitions |
| Moral distrust of atheists [69] | 13-country investigation of moral associations | People intuitively associate atheism with severe immorality, even in secular countries | Religious moral frameworks remain culturally dominant |
| Punitive attitudes [70] | Survey experiment on educational content regulation | Religious individuals show higher propensity to punish norm violations | Religious moral commitments translate into concrete ethical positions |
Methodological Considerations: Operationalizing Inclusivity in Bioethical Research
Experimental Protocols for Studying Religious and Secular Moral Reasoning
To rigorously compare religious and secular bioethical foundations, researchers can employ modified versions of the experimental philosophy tasks used in the belief-in-belief studies [69]. These protocols typically present participants with moral scenarios followed by systematic manipulation of key variables to assess differences in moral reasoning between religious and secular participants, while controlling for relevant demographic factors.
A basic experimental protocol might include: (1) Participant recruitment stratified by religious commitment (high, moderate, none) and religious tradition; (2) Moral scenario presentation using standardized bioethical dilemmas (e.g., end-of-life decisions, reproductive technologies, resource allocation); (3) Randomized manipulation of scenario variables (e.g., patient autonomy versus religious commitments); (4) Dependent measures assessing moral judgments, reasoning patterns, and decision confidence; and (5) Statistical analysis examining main effects and interactions between religious commitment and scenario variables.
Table: Key Research Reagent Solutions for Comparative Bioethics Studies
| Research Tool | Function | Application Example |
|---|---|---|
| Moral Scenarios Inventory | Standardized ethical dilemmas with systematic variable manipulation | Testing differences in moral judgments between religious and secular participants |
| Religious Commitment Inventory | Assesses degree and nature of religious adherence | Stratifying participants by religious commitment level |
| Public Reasoning Assessment | Measures ability to articulate reasons accessible across worldviews | Evaluating translation of religious reasons into public discourse |
| Pluriversal Dialogue Framework [22] | Structured approach for cross-worldview engagement | Facilitating productive dialogue between religious and secular bioethicists |
| Cultural Evolution Metrics [69] | Tracks historical influences on contemporary moral intuitions | Understanding persistent religious influences in secular contexts |
Conceptual Mapping of Bioethical Integration
The following diagram illustrates the conceptual relationships and workflow for integrating religious and secular perspectives in bioethics using a pluriversal approach:
Case Studies: Practical Applications of Inclusive Bioethics
Environmental Bioethics and Religious Stewardship
Religious perspectives offer distinctive contributions to emerging bioethical challenges such as environmental sustainability. The 2025 encyclical Laudato Si' by Pope Francis exemplifies how religious traditions can provide robust ethical frameworks for addressing ecological crises [20]. The document articulates an "integral ecology" that connects environmental concern with care for the poor and vulnerable, arguing that the same logic of exploitation threatens both natural environments and human communities [20].
This religious approach to environmental ethics emphasizes concepts of stewardship, care, and intergenerational responsibility that complement secular sustainability frameworks. Unlike technological approaches focused primarily on efficiency gains, religious perspectives often call for value reorientation and changes in consumption patterns rooted in spiritual understandings of humanity's place in the natural world [20]. The significant resources and moral authority of religious institutions—with the Catholic Church alone comprising approximately 1.4 billion members—make them crucial partners in addressing global sustainability challenges.
Healthcare Disparities and Religious Justice Frameworks
Religious bioethics has proven particularly valuable in addressing racial disparities in healthcare, where secular approaches have sometimes failed to generate sufficient moral traction or cultural resonance within affected communities. The long history of medical exploitation of African Americans—from the Tuskegee syphilis study to the case of Henrietta Lacks—has created legitimate mistrust of medical institutions within many Black communities [71].
Religious frameworks, particularly those drawn from the Black Church tradition, have provided powerful resources for addressing these disparities through concepts of justice, dignity, and solidarity [71]. These religiously-grounded approaches have often proven more effective than secular principles alone in mobilizing community responses to health disparities and rebuilding trust between marginalized communities and healthcare institutions. This demonstrates how religious perspectives can offer morally compelling language and institutional networks for addressing persistent bioethical challenges.
The case for welcoming religious perspectives as epistemic peers in bioethics rests on multiple compelling foundations: the demographic reality of global religiosity, the psychological persistence of religious intuitions even in secular societies, the conceptual richness of religious moral traditions, and the practical effectiveness of religious approaches in addressing specific bioethical challenges. The pluriversal framework offers a promising path forward, creating space for productive dialogue across deep differences while maintaining ethical constraints that prevent domination by any single perspective.
This inclusive approach does not require abandoning secular bioethical frameworks but rather enriching them through engagement with the diverse religious traditions that shape moral reasoning for most of the world's population. By recognizing religious perspectives as equally credible sources of ethical insight, bioethics can develop more culturally resonant, practically effective, and conceptually robust approaches to the complex moral challenges posed by advancing medical technologies and persistent health disparities. The future of bioethics as a globally relevant discipline depends on its ability to embrace the full diversity of humanity's moral wisdom, both religious and secular.
The expanding frontiers of medical science and technology consistently present new ethical challenges, making bioethics an increasingly critical field. Contemporary debates often center on the foundational sources of moral reasoning, creating a perceived divide between religious and secular frameworks. This analysis provides a systematic comparison of these frameworks on three pivotal issues: euthanasia, abortion, and artificial intelligence (AI). The objective is not to declare one framework superior but to elucidate the distinct principles, values, and outcomes each brings to bioethical deliberation. By presenting the stances of major religious traditions alongside secular perspectives in a structured format, this guide aims to inform researchers, scientists, and drug development professionals about the multifaceted ethical landscape in which they operate. Understanding these differences is essential for navigating the complex moral terrain of modern healthcare and biotechnology, fostering interdisciplinary dialogue, and developing policies that are both scientifically sound and socially nuanced.
Analytical Framework and Methodology
The comparative analysis presented in the subsequent sections is the result of a systematic literature review conducted to identify authoritative and contemporary positions. The methodology was designed to capture a representative spectrum of both religious and secular viewpoints.
- Data Collection: A comprehensive search of academic databases was performed, including PubMed, SCOPUS, ScienceDirect, and ATLA Religion Database, among others [72] [73]. The search combined keywords related to the three key issues (euthanasia, abortion, AI) with terms such as "bioethics," "religious," "secular," and the names of major world religions (e.g., Catholicism, Islam, Judaism). Both peer-reviewed journal articles and official institutional documents were considered.
- Inclusion Criteria: Sources were prioritized based on their publication date (with a focus on recent analyses from 2024-2025), their authorship (seeking authoritative voices within each tradition, such as church documents or leading secular bioethics institutes), and their relevance to the core research thesis comparing foundational frameworks [5] [74].
- Analysis and Synthesis: The identified literature was subjected to a qualitative content analysis. Key themes, ethical principles, and normative positions were extracted and categorized. The comparative tables were constructed by synthesizing these findings to highlight areas of convergence and divergence. It is important to note that this analysis focuses on doctrinal and institutional positions rather than the lived beliefs of individual adherents, which can exhibit significant variation [5].
Table 1: Core Foundational Principles of Secular and Religious Bioethics
| Framework | Primary Ethical Foundation | View on Human Life | Central Moral Authority |
|---|---|---|---|
| Secular | Public reason, autonomy, well-being [5] [75] | Grounded in biological and neurological science; personhood often linked to birth or sentience [75] | Individual consent and rational justification [5] |
| Religious | Divine command, sacred texts, natural law, religious tradition [72] [5] | Sacred and possessing inherent dignity from conception or a specific point [72] [74] | Religious doctrine and teaching authority (e.g., Magisterium, Islamic scholars) [72] [5] |
The following diagram illustrates the logical workflow of the methodological protocol used to gather and synthesize the data for this analysis.
Research Methodology Workflow
Comparative Analysis of Stances
Euthanasia and End-of-Life Care
End-of-life decisions represent a profound ethical challenge, sharply contrasting the values of autonomy against the sanctity of life. The table below compares the stances on euthanasia and the related practice of palliative sedation.
Table 2: Comparative Stances on Euthanasia and End-of-Life Care
| Framework | Stance on Active Euthanasia/PAS | Stance on Palliative Sedation | Key Rationale & Conditions |
|---|---|---|---|
| Secular | Support varies; often justified by patient autonomy and relief of suffering [76]. | Generally accepted as an ethical means of palliative care. | Emphasis on informed consent, quality of life, and avoiding unbearable suffering [76]. |
| Catholicism | Explicitly forbidden as a grave moral evil [72]. | Morally acceptable under specific conditions [72]. | Must be for refractory symptoms, not intended to cause death. The line between sedation and euthanasia is closely guarded [72]. |
| Eastern Orthodoxy | Forbidden [72]. | Cautious and positive attitude [72]. | Can alleviate suffering, but concern over blurring lines with life-ending treatments [72]. |
| Protestantism | Diverse views, but generally opposes active life-ending actions [72]. | Cautious and positive attitude [72]. | Recognition of value to alleviate suffering, tempered by caution regarding its use [72]. |
| Islam | Explicitly prohibited [76]. | Information not specified in search results. | Based on the belief that life is sacred and its duration is predetermined by God [76]. |
| Judaism | Explicitly prohibited [76]. | Information not specified in search results. | Preservation of life is a supreme religious duty [76]. |
Experimental & Observational Insights: A 2025 study of 465 Greek health professionals found that their attitudes toward euthanasia were significantly associated with their religious beliefs, highlighting how personal religiosity influences professional judgment in clinical settings [76]. The same study found that empathy was an insignificant predictor of attitudes toward euthanasia, suggesting that abstract principles, rather than emotional connection, may dominate the ethical calculus [76].
Abortion and the Beginning of Life
The debate over abortion is one of the most polarized in bioethics, centering on conflicting definitions of personhood and the moral status of the embryo/fetus.
Table 3: Comparative Stances on Abortion
| Framework | General Stance on Abortion | View on Personhood | Notable Nuances & Exceptions |
|---|---|---|---|
| Secular | Supports access as a component of reproductive rights and bodily autonomy [75]. | Begins at birth, with the actualization of the fetal nervous system [75]. | Policy should be based on "scientifically accurate biology," not theological presuppositions [75]. |
| Catholicism | Totally opposed [74]. | Begins at the moment of conception [74]. | No exception for rape or incest; medical procedures to save a mother's life that indirectly cause fetal death may be permissible (principle of double effect). |
| Eastern Orthodoxy | Totally opposed [74]. | Begins at the moment of conception [74]. | Similar to Catholic position. |
| Protestantism | Nuanced disapproval; wide variation between liberal and conservative denominations [74]. | Varies significantly between denominations. | Some denominations may allow for exceptions in cases of risk to the mother's life, rape, or fetal abnormalities. |
| Islam | Generally disapproves, but stance is not uniform [74]. | Many traditional scholars allow it up to 40 days or 120 days (ensoulment) [74]. | Often permitted in the early stages of pregnancy, especially for serious reasons [74]. |
| Judaism | Orthodox view bans it except for maternal life risk; Reformed view is more open [74]. | The fetus is not considered a full person (nefesh) until birth [74]. | Orthodox Judaism prioritizes the mother's life; Reformed Judaism considers the mother's well-being more broadly. |
Empirical Data Analysis: Cross-national research demonstrates that the strength of an individual's religious commitment is a more powerful predictor of abortion disapproval than their specific religious affiliation [77]. Furthermore, a societal "religious climate" exerts a significant effect; people living in more religious countries are more likely to disapprove of abortion, regardless of their personal beliefs [77]. Countries with a significant Catholic cultural history also show higher levels of abortion disapproval, even among non-Catholics, indicating the religion's role as a cultural and institutional force [77].
Artificial Intelligence (AI) in Healthcare
The emergence of AI presents novel questions about human identity, responsibility, and the ethical development of technology.
Table 4: Comparative Stances on Artificial Intelligence in Healthcare and Society
| Framework | Core Stance on AI | Primary Ethical Concerns | Stated Priorities & Safeguards |
|---|---|---|---|
| Secular | A tool to be governed by human-centric values and responsible innovation frameworks [78]. | Bias, fairness, transparency, accountability, and privacy [78]. | Alignment with human values, equitable access, and avoiding the worsening of social inequalities [73] [78]. |
| Catholicism | Positive potential but must be subordinate to human dignity and the common good [73]. | Concentrated power, "digital divide," manipulation of consciences, and replacing God [73]. | Human control and responsibility; technology must serve human dignity, which comes from God [73]. |
| Latter-day Saints | A tool for good that must not replace God or authentic divine connection [79]. | AI being perceived as godlike; erosion of human relationships and moral agency [79]. | Championing "safe and trusted AI" through a "Faith Community AI Evaluation" to ensure AI reflects pluralistic, faith-based values [79]. |
| Interfaith Consensus | Cautious engagement, viewing AI as a tool to be guided by faith-based ethics [79]. | That AI's moral compass is dictated solely by a small group of technologists [79]. | Intentional use of AI for human flourishing and common prosperity; need for dialogue between faith leaders and technologists [79]. |
Research Reagent Solutions: Key Tools for AI Ethics Analysis
For researchers investigating the ethical implementation of AI in healthcare, the following conceptual "reagents" are essential.
Table 5: Essential Analytical Tools for AI Ethics Research
| Tool / Concept | Function in Analysis |
|---|---|
| Value Alignment Framework | A structured method to test the value systems embedded in AI algorithms and the trade-offs of their recommendations in clinical settings [78]. |
| Faith Community AI Evaluation | A proposed process where faith communities develop training sets and benchmarks to ensure AI systems accurately and respectfully portray religious beliefs and incorporate faith-based ethics [79]. |
| Public Reason | A procedural tool for justifying political and ethical decisions in pluralistic societies without resorting to personal religious doctrines, ensuring broader inclusivity [5]. |
The tabular analyses reveal a complex landscape where secular and religious bioethical frameworks diverge sharply on foundational issues like the beginning and end of life, yet find surprising convergence on the need for prudent, human-centric governance of emerging technologies like AI. The secular framework, with its emphasis on public reason, individual autonomy, and scientifically-grounded definitions, offers a platform for inclusive policy-making in pluralistic societies. In contrast, religious frameworks provide a robust language of sacredness, inherent dignity, and moral limits, rooted in divine authority and centuries of tradition. For the scientific and research community, this comparative guide underscores that bioethical challenges cannot be resolved by scientific data alone. Engaging with the underlying philosophical and theological foundations is not an ancillary activity but a core component of responsible innovation. Future research and policy development will benefit from structured dialogues that acknowledge these distinct starting points, seeking practical collaboration grounded in a shared commitment to human well-being.
Bioethics, since its mid-twentieth-century inception, was profoundly shaped by religious scholars—a "trinity of theologians" including an Episcopal minister, a Methodist professor, and a Jesuit moral theologian [80]. Yet, over time, the field has increasingly turned toward secular frameworks rooted in law, philosophy, and empirical science, marginalizing religious voices in the process [80] [22]. This shift creates a significant challenge for a field claiming global relevance when most of the world's population identifies as religious and many countries base policies on religious traditions [22]. Pluriversal bioethics emerges as a transformative approach that reframes this tension not as a problem to resolve but as an opportunity for enriched ethical discourse.
A pluriversal approach recognizes that people inhabit distinct, internally coherent worlds—different ontologies or existences—that should coexist and flourish provided they avoid harming people or destroying other worlds [80]. This perspective takes seriously the depth of difference between ways of knowing, being, and acting. Rather than universalizing a single set of secular bioethical principles, pluriversal bioethics seeks "a world where many worlds fit" [22]. It offers a new paradigm for global bioethics that aspires to replace established views like "common morality" that purport to represent all people but often reflect Western secular assumptions [22]. This paper compares secular and religious foundations in bioethics through a pluriversal lens, examining ethical constraints that facilitate constructive dialogue across profound differences.
Theoretical Foundations: Secular and Religious Bioethics in Perspective
Historical Context and Philosophical Underpinnings
Bioethics emerged as a distinct field during a period of moral pluralism and shifting ideas about moral authority [14]. Its foundational mission was to develop principles and methods for moral decision-making acceptable to所有人, regardless of religion or ideology [14]. This universalist aspiration led to the marginalization of religious perspectives in favor of secular frameworks, particularly the principles of autonomy, beneficence, nonmaleficence, and justice [22].
The secularization of bioethics has deeper historical roots than often acknowledged. The methodological approaches dominating contemporary bioethics represent a direct result of a particular European and Western epistemology with Christian origins [15]. The theories and methods that developed following the Enlightenment emerged from the wrestling between Christianity and philosophy, leading to a secularization of Christian ethics [15]. What is peculiar to Western ethics is the presumption that the "outsider perspective"—the secular, academic, material stance—is simultaneously neutral and superior to previous theological or religious perspectives, thus claiming authority [15].
Figure 1: Conceptual Framework of Pluriversal Bioethics Integration
Comparative Analysis of Secular and Religious Approaches
Table 1: Foundational Differences Between Secular and Religious Bioethics
| Aspect | Secular Bioethics | Religious Bioethics |
|---|---|---|
| Moral Authority | Human reason, empirical evidence, rational consensus [14] | Divine revelation, sacred texts, religious tradition [54] |
| Scope of Morality | Principles applicable regardless of comprehensive worldview [22] | Ethics inseparable from cosmological beliefs and purpose [15] |
| Approach to Suffering | Often focuses on eliminating suffering; limited teleological perspective [14] | May attribute meaning to suffering; integrates teleological perspective [14] |
| Methodology | Philosophical analysis, empirical research, principle-based reasoning [81] | Theological reflection, scriptural interpretation, tradition-based reasoning [54] |
| View of Human Life | Varies from quality-of-life to sanctity depending on framework [54] | Typically views life as sacred with intrinsic worth regardless of condition [54] |
Religious perspectives unconditionally cherish sacred human life regardless of clinical, sociopolitical, cultural, legal, personal, or financial variables [54]. For example, in end-of-life decisions, religious frameworks typically do not discriminate between supporting a twenty-year-old's life and stopping support for a ninety-year-old's life simply based on age or resource scarcity [54]. This contrasts with some secular approaches that may incorporate quality-of-life considerations or utilitarian calculations in resource allocation.
The secular stance of bioethics limits its ability to fully respond to challenging existential and moral questions emerging in medicine and research [14]. As the field has developed, bioethical questions have shifted from "thick" substantive inquiries about human meaning to "thin" formal concerns about guidelines and regulations [14]. This thinning of discourse has left little space to explore the meaning of suffering or other profound existential dimensions of medical experiences.
The Pluriversal Framework: Ethical Constraints for Engagement
Core Ethical Constraints
A pluriversal approach to bioethics establishes five ethical constraints for dialogue across deep differences. These constraints support the coexistence of plural worlds provided they do not harm people or destroy other worlds [80]. They apply equally to religious and secular perspectives, creating a framework for mutual respect.
Table 2: Ethical Constraints for Pluriversal Bioethics Discourse
| Constraint | Definition | Application Examples |
|---|---|---|
| Civility | Engage others with respect across global bioethics community [80] | Show hospitality, welcome different viewpoints, reject requirements to translate religious commitments into "neutral" language [22] |
| Change from Within | Resolve conflict by working with those experiencing it; recognize people's agency for self-determination [80] | Address harmful practices by engaging trusted community authorities rather than imposing external solutions [22] |
| Justice | Give each their due and ensure people feel they are being given their due [22] | Treat religious and nonreligious debaters fairly; ensure all feel heard and understood in ethical deliberations [22] |
| Non-domination | Prohibit arbitrary and controlling influence over others [22] | Avoid requiring religious participants to leave convictions behind in bioethics discourse [80] |
| Toleration | Avoid judging others with undue severity; recognize common membership deeper than conflict [22] | Check hostility toward groups endorsing views we repudiate; create openings for dialogue across differences [22] |
Methodological Approaches for Pluriversal Bioethics
Implementing a pluriversal approach requires methodological innovation that transcends traditional secular-religious divides. Digital bioethics methods offer promising avenues for studying how bioethical issues take shape across diverse communities online [81]. These approaches can help researchers understand the discursive formation of ethical positions across different worldview communities.
Figure 2: Methodological Approaches in Pluriversal Bioethics Research
Systematic comparative reflection methodology enables researchers to analyze positions across different traditions and find middle ground [54]. This approach progresses from presenting issues through multiple perspectival lenses to discussing derived evidence and developing integrative conclusions and recommendations.
Research Reagents and Methodological Tools
Table 3: Essential Methodological Tools for Pluriversal Bioethics Research
| Research Tool | Function | Application Context |
|---|---|---|
| Digital Discourse Analysis | Computational analysis of online bioethical discussions [81] | Tracing how bioethical issues take shape across different worldview communities online |
| Systematic Comparative Reflection | Structured comparison across religious and secular traditions [54] | Identifying common ground and differences on specific bioethical issues |
| Empirical Bioethics Methods | Quantitative and qualitative study of stakeholder values and attitudes [81] | Understanding how various actors articulate ethical perspectives in context |
| Ethical Constraint Framework | Application of civility, justice, non-domination, toleration, and change-from-within principles [80] [22] | Facilitating productive dialogue across deep differences in bioethics settings |
| Interdisciplinary Dialogue Protocols | Structured communication across disciplinary and worldview boundaries [54] | Creating middle ground through open interdisciplinary, interreligious, and cross-cultural communication |
Case Studies and Applications
End-of-Life Decision Making
The film Whose Life Is It Anyway? presents a poignant case for comparing religious and secular bioethical perspectives. The scenario involves Ken Harrison, who experiences quadriplegic paralysis and permanent kidney damage after a traffic accident [54]. After six months of intensive life support, Harrison petitions to be removed from life support, claiming that life without his previous active existence is meaningless [54].
From a secular bioethics perspective, this case primarily engages the principle of autonomy—the right to self-determination and control over one's body and life [54]. Secular frameworks might support Harrison's position based on his right to refuse medical treatment and determine what constitutes a meaningful existence.
From Abrahamic religious perspectives, however, the analysis differs significantly. Jewish teachings based on the Sixth Commandment ("Thou shalt not kill") would typically reject euthanasia without qualification [54]. Similarly, Christian and Islamic perspectives would generally emphasize the sacredness of human life regardless of its quality or functional capacity [54]. Religious frameworks might question whether human beings ever lose their intrinsic worth or whether suffering might have meaningful dimensions.
A pluriversal approach to this case would engage both perspectives through the five ethical constraints. It would ensure civil dialogue that respects both the secular emphasis on autonomy and the religious emphasis on life's sacredness. It would seek change from within traditions rather than imposing external solutions, perhaps engaging religious authorities in reframing discussions of suffering while also acknowledging the legitimacy of secular concerns about bodily integrity.
Scientific Integrity and Public Trust
Contemporary challenges to scientific integrity—including predatory publishing, political interference in research, and the spread of misinformation—represent another crucial domain for pluriversal analysis [19]. These issues engage the bioethical principle of justice, requiring fairness in access to truth, recognition for honest work, and protection against exploitation and manipulation [19].
A secular approach might emphasize virtues like honesty and humility as essential to the scientific method [19]. It might focus on structural reforms to safeguard research from political manipulation and commercial interests [19].
Religious perspectives might frame these issues through concepts of truthfulness as divine commandment or stewardship of knowledge as religious duty. They might emphasize the moral dimensions of knowledge production and the ethical responsibilities of those wielding technological power.
The pluriversal approach creates space for both frameworks to contribute to addressing threats to scientific integrity. It enables collaboration across worldview differences to defend the independence of science while respecting the diverse moral foundations that motivate such defense.
Implementing a pluriversal approach requires substantive changes to bioethics discourse, research, and education. Bioethics conferencing and publishing should welcome religious perspectives without requiring translation into secular language [22]. Training programs should incorporate diverse worldview traditions while teaching the ethical constraints for productive engagement across differences [80].
The pressing bioethical challenges of our time—from AI-generated synthetic data [82] to premature termination of clinical trials [83]—demand the richest possible conceptual resources. A pluriversal bioethics that draws on both religious and secular foundations offers enhanced capacity to address this complexity while modeling the civil discourse our divided world sorely needs. By creating a world where many worlds fit [22], pluriversal bioethics fulfills the field's original promise of guiding humanity through the moral challenges of biomedical progress.
Conclusion
The comparative analysis of secular and religious bioethics reveals not a binary choice, but a spectrum of complementary moral resources. The secular tradition, with its principlist framework and evolving 'moral bricolage,' offers procedural tools for public policy, while religious traditions provide substantive, metaphysically-grounded commitments that unconditionally affirm the sacredness of life. For biomedical researchers and clinicians, the key takeaway is that neither framework is sufficient in isolation. The future of ethical practice in a globalized world lies in a pluriversal model that actively welcomes diverse perspectives, upholds civility, and seeks common ground through specified application and deliberative dialogue. This enriches the field, fosters inclusive policy-making, and ultimately ensures that scientific progress remains firmly anchored to profound human values. Future efforts must focus on developing practical, structured methodologies for this integrative dialogue within the specific contexts of drug development and clinical research.
References
- 1. Exploring the ethical issues posed by AI and big data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12581208/]
- 2. Bioethics as a language game: probing the quality of moral ... [https://link.springer.com/article/10.1007/s11017-025-09702-9]
- 3. Contrary to Claims, Bioethics Is Not a “Moral Tradition” [https://scienceandculture.com/2025/10/contrary-to-claims-bioethics-is-not-a-moral-tradition/]
- 4. Bioethics as an emerging moral tradition and some ... [https://pubmed.ncbi.nlm.nih.gov/41033789/]
- 5. On Religious Influence in Bioethics: The Limits of Pluriversalism [https://pmc.ncbi.nlm.nih.gov/articles/PMC12232604/]
- 6. Moral bricolage and the emerging tradition of secular ... [https://pubmed.ncbi.nlm.nih.gov/40009322/]
- 7. Experimental and Quasi-Experimental Designs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6923620/]
- 8. How Does Religion Affect Giving to Outgroups and Secular ... [https://www.mdpi.com/2077-1444/11/8/405]
- 9. Assisted Reproduction in the Abrahamic Religions: Ethical ... [https://www.mdpi.com/2077-1444/16/12/1508]
- 10. Bioethics Course 2025 [https://medicineandislam.org/bioethics-course-2025/]
- 11. Master of Science in Bioethics Curriculum [https://www.amc.edu/education/alden-march-bioethics-institute/master-of-science-in-bioethics/curriculum-master-of-science-in-bioethics/]
- 12. On Religious Influence in Bioethics: The Limits of ... [https://pubmed.ncbi.nlm.nih.gov/40296411/]
- 13. Contrary to Claims, Bioethics Is Not a ‘ Moral Tradition’ | Mind Matters [https://mindmatters.ai/2025/10/contrary-to-claims-bioethics-is-not-a-moral-tradition/]
- 14. Good Without God: Bioethics and the Sacred - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4577544/]
- 15. Medicine and Ethics: Religious or Secular? [https://petrieflom.law.harvard.edu/2017/09/13/medicine-and-ethics-religious-or-secular/]
- 16. Embracing Medicines Development as a Profession - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12246006/]
- 17. The Shared Ethical Responsibility of Medically and Non ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2018.00843/full]
- 18. Specification-driven acceptance criteria for validation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9537461/]
- 19. Ethics Dispatch October 2025 [https://www.practicalbioethics.org/blog/ethics-dispatch-october-2025/]
- 20. Faith, Bioethics, and Sustainable Development: A Christian ... [https://www.mdpi.com/2077-1444/16/3/347]
- 21. The Ethics of Bioethics | CBHD Resources [https://cbhd.org/cbhd-resources/the-ethics-of-bioethics]
- 22. Why Bioethics Should Welcome Religion [https://www.thehastingscenter.org/religion-welcome-here/]
- 23. Setting Acceptance Criteria from Statistics of the Data [https://www.biopharminternational.com/view/specification-setting-setting-acceptance-criteria-statistics-data]
- 24. Process Capability Indices in the Biopharmaceutical Industry [https://www.bioprocessintl.com/qa-qc/practical-applications-of-process-capability-indices-in-the-biopharmaceutical-industry-a-simulation-based-study]
- 25. Role of Clinical Support Services in Ethics - End - of and... Life Care [https://pubmed.ncbi.nlm.nih.gov/31606182/]
- 26. Ethical considerations at the end-of-life care - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7958189/]
- 27. Organ Donation Ethics: A Casuist Analysis of Routine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623222/]
- 28. Standards for Palliative and End of Life Care [https://www.socialworkers.org/Practice/NASW-Practice-Standards-Guidelines/Standards-for-Palliative-and-End-of-Life-Care]
- 29. Inconsistent values and algorithmic fairness: a review of organ ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-024-01116-x]
- 30. Methods in Comparative Effectiveness Research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3504326/]
- 31. Transplantation [https://www.who.int/health-topics/transplantation]
- 32. 17th World Conference on Bioethics, Medical Ethics and ... [https://www.coe.int/en/web/trafficking-human-organs/-/17th-world-conference-on-bioethics-medical-ethics-and-health-law]
- 33. A COMPARATIVE ANALYSIS OF BIOETHICAL ISSUES ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5675570/]
- 34. Diverse Perceptions of the Informed Consent Process [https://pmc.ncbi.nlm.nih.gov/articles/PMC3575189/]
- 35. Informed Consent in cross-cultural perspective: clinical ... [https://pubmed.ncbi.nlm.nih.gov/17968637/]
- 36. Author's Commentary on "Crossing Cultural Barriers- ... [https://onlineethics.org/node/40246]
- 37. International and Regional Human Rights Standards [https://www.hhrjournal.org/2018/12/04/human-subject-research-international-and-regional-human-rights-standards/]
- 38. in Informed : a consent of... human subject research comparison [https://pubmed.ncbi.nlm.nih.gov/20235864/]
- 39. Ethical international research on human subjects ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2563398/]
- 40. On the USCCB's revised “Ethical and Religious Directives” ... [https://www.catholicworldreport.com/2025/11/19/on-the-usccbs-revised-ethical-and-religious-directives-for-catholic-hospitals/]
- 41. Institutional Religious Policies That Follow Obstetricians ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5559238/]
- 42. Her miscarriage showed the limits of California's abortion ... [https://calmatters.org/health/2025/05/abortion-law-catholic-hospitals/]
- 43. Growing Market Power Among Catholic Hospitals ... [https://www.americanprogress.org/article/growing-market-power-among-catholic-hospitals-restrains-access-to-reproductive-health-care/]
- 44. Exploring the false dichotomy of secular and religious ... [https://utswmed-ir.tdl.org/items/7bfa33e8-111f-4ca5-87bf-5150e6295d75]
- 45. Religion v. Science? No and Yes [https://pubmed.ncbi.nlm.nih.gov/40043174/]
- 46. Navigating Ethical and Legal Decisions in Serious Illness [https://www.nationalcoalitionhpc.org/navigating-ethical-and-legal-decisions-in-serious-illness/]
- 47. October 11, 2025 | Omaha, NE | Converging Roads [https://forlifeandfamily.org/events/cr25-omne/]
- 48. Trend Overview 2025: Key Developments in Biomedical ... [https://biomedgrid.com/fulltext/volume25/trend-overview-2025-key-developments-in-biomedical-science-research.003320.php]
- 49. Origin of “Conscientious Objection” in Health Care [https://pmc.ncbi.nlm.nih.gov/articles/PMC12179533/]
- 50. Conscience Clauses, Health Care Providers, and Parents [https://www.thehastingscenter.org/briefingbook/conscience-clauses-health-care-providers-and-parents/]
- 51. Christian Bioethics in a Secular World: In Search of Ethical ... [https://www.thepublicdiscourse.com/2025/03/97321/]
- 52. Conscientious objection in pharmacist codes of ethics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12139423/]
- 53. Religious Accommodation in Bioethics and the Practice of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8022927/]
- 54. Whose life is it anyway? A reflective dialogue between ... [https://www.sciencedirect.com/science/article/abs/pii/S2352552519300945]
- 55. Ethical values and principles to guide the fair allocation of ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-022-00806-8]
- 56. On value compatibility: reflections on the ethical framework for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12103310/]
- 57. Bioethics for clinicians: 13. Resource allocation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1227741/]
- 58. Prioritizing Patients: How algorithms can promote just ... [https://bioethics.hms.harvard.edu/journal/AI-resource-allocation]
- 59. "Healthcare Ethics Committees" by Thaddeus Mason Pope [https://larc.cardozo.yu.edu/cjcr/vol15/iss2/4/]
- 60. Bioethics, Religion and Culture from a Comparative Perspective [https://them.polylog.org/6/fsj-en.htm]
- 61. A Comparison of Human Life in Christian and Chinese ... [https://www.mdpi.com/2077-1444/15/5/624]
- 62. Empirical research in bioethical journals. A quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2565792/]
- 63. Ethics in medical research: A quantitative analysis of the ... [https://www.medrxiv.org/content/10.1101/2024.06.23.24309373v1]
- 64. Team members perspectives on conflicts in clinical ethics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7323753/]
- 65. SPIRIT 2025 statement: updated guideline for protocols of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12035670/]
- 66. A rational exploration of personalist bioethics [https://cjgh.org/articles/10.15566/cjgh.v11i2.333]
- 67. Religious pluralism and the ethics of healthcare - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10841336/]
- 68. Against Public‐Facing Religious Bio‐Restrictionism - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511909/]
- 69. Belief in belief: Even atheists in secular countries show ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12002237/]
- 70. Classroom Culture Wars: Experimental Evidence of the ... [https://www.mdpi.com/2077-1444/16/8/1016]
- 71. Race, Medicine, and Healthcare: A Christian Ethics ... [https://cbhd.org/dignitas-articles/race-medicine-and-healthcare-a-christian-ethics-perspective]
- 72. Christian perspectives on palliative sedation: a literature study [https://pmc.ncbi.nlm.nih.gov/articles/PMC12243377/]
- 73. A Contemporary Review of Religion and AI [https://www.mdpi.com/2077-1444/16/7/834]
- 74. Induced abortion in the world: 1. Perception ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12640180/]
- 75. Personhood Begins at Birth: The Rational Foundation for Abortion ... [https://link.springer.com/article/10.1007/s11673-024-10352-0]
- 76. Health Professionals' Views on Euthanasia: Impact of Traits ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12294693/]
- 77. Religious Influence and Abortion Disapproval Around the ... [https://ifstudies.org/blog/religious-influence-and-abortion-disapproval-around-the-globe]
- 78. Charting a Path for Ethical AI: Reflections from RAISE 2025 [https://bioethics.hms.harvard.edu/news/charting-path-ethical-ai-reflections-raise-2025]
- 79. Faith, Ethics, and Human Dignity in an Age of Artificial ... [https://newsroom.churchofjesuschrist.org/article/faith--ethics--and-human-dignity-in-an-age-of-artificial-intelligence--a-call-to-action?ref=techbuzznews.com]
- 80. A Pluriversal Approach to Religion and Global Bioethics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12263729/]
- 81. Digital bioethics: introducing new methods for the study of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10646908/]
- 82. Synthetic data created by generative AI poses ethical challenges [https://www.niehs.nih.gov/news/factor/2025/4/feature/ai-data-ethics]
- 83. Researchers Highlight Ethical Concerns When Clinical ... [https://www.bu.edu/sph/news/articles/2025/researchers-highlight-ethical-concerns-when-clinical-trials-are-cut-short/]