Navigating the Ethical Landscape: A Comprehensive Guide to Randomized Controlled Trials in Community Settings
This article provides researchers, scientists, and drug development professionals with a comprehensive framework for addressing the distinct ethical challenges of conducting Randomized Controlled Trials (RCTs) in community settings.
Navigating the Ethical Landscape: A Comprehensive Guide to Randomized Controlled Trials in Community Settings
Abstract
This article provides researchers, scientists, and drug development professionals with a comprehensive framework for addressing the distinct ethical challenges of conducting Randomized Controlled Trials (RCTs) in community settings. Covering the spectrum from foundational principles to practical application, it explores the blurred research-practice distinction, adaptations to informed consent, and streamlined oversight for pragmatic and cluster designs. Drawing on recent literature and stakeholder interviews, the content offers actionable strategies for managing multi-site collaborations, engaging community stakeholders, and balancing scientific rigor with ethical obligations to participants in real-world environments. The article concludes by examining how innovations in trial methodology and evidence generation are shaping the future ethical landscape of community-based research.
Core Ethical Principles and the Distinct Nature of Community-Based RCTs
Randomized controlled trials (RCTs) remain the gold standard for generating evidence in health research, yet their design and implementation have evolved significantly to answer more complex questions in real-world settings. This evolution from traditional explanatory trials to pragmatic trials and cluster randomized designs has created a new ethical landscape that researchers must navigate. Explanatory trials are designed to assess intervention efficacy under ideal, tightly controlled conditions, while pragmatic trials assess whether research-proven interventions are effective in "real-world" settings without substantial research support [1]. Cluster randomized trials (CRTs), where intact social units rather than individuals are randomized to intervention or control conditions, have become an increasingly important methodological tool in health services research, public health, and quality improvement studies [2].
The ethical frameworks that guided traditional explanatory RCTs are insufficient for these more complex designs. Contemporary research ethics, largely structured around the protection of the autonomy and welfare interests of individual research subjects, faces serious challenges when applied to CRTs and pragmatic trials [2]. These challenges include identifying research subjects, obtaining informed consent, applying clinical equipoise, conducting benefit-harm analyses, protecting vulnerable populations, and determining the role and authority of gatekeepers [3]. This article explores these ethical challenges and provides practical guidance for researchers operating in community settings.
Key Ethical Distinctions Across Trial Designs
Comparative Analysis of RCT Typologies
Table 1: Fundamental Characteristics of RCT Design Types
| Attribute | Explanatory RCT | Pragmatic RCT | Quality Improvement Activities |
|---|---|---|---|
| Primary Purpose | Create generalizable knowledge; determine causes and effects of treatments under ideal conditions [4] | Create generalizable knowledge, improve care locally, and inform clinical and policy decisions [4] | Bring about immediate improvements in health care delivery in particular settings [4] |
| Research Question | Can this intervention work under ideal conditions? [4] | Does this intervention work under usual conditions? [4] | How do I best implement this intervention? [4] |
| Participant Enrollment | A cohort of patients with explicitly defined inclusion and exclusion criteria [4] | Diverse, representative populations; inclusion and exclusion criteria tend to be broader [4] | Patients in routine clinical care |
| Intervention Adherence | Strictly enforced [4] | Flexible (as it would be in usual care) [4] | Normal practice |
| Data Collection | Researchers; data collection occurs outside of routine clinical care [4] | Clinicians at the point of care in cooperation with researchers; EHRs and registries are used as sources of research data [4] | Clinicians at the point of care |
| Setting | Medical centers designated as research sites [4] | Multiple, heterogeneous settings [4] | Local clinic or hospital; may include multiple clinics or hospitals |
| Outcomes | May be surrogates or process measures [4] | "Directly relevant to participants, funders, communities, and healthcare practitioners" [4] | Directly relevant to local quality metrics |
Quantitative Comparison of Explanatory vs. Pragmatic Implementation
Table 2: Comparative Outcomes from Hyperlink Trials Illustrating Explanatory vs. Pragmatic Trade-offs [1]
| Design Element | Hyperlink 1 (Explanatory) | Hyperlink 3 (Pragmatic) |
|---|---|---|
| PRECIS-2 Score | More explanatory | More pragmatic |
| Patients Enrolled | 450 | 3071 |
| Recruitment Method | Study staff via mailings, telephone screening, research clinic determination | Clinic staff at routine encounters using automated EHR algorithms |
| Enrollment Rate | 2.9% of potentially eligible patients | 81% of eligible patients |
| Participant Demographics | Older, more likely to be male and White | Younger, less likely to be male and White; more likely to be female, Asian or Black, with lower socioeconomic indicators |
| Adherence to Initial Visit | 98% (study staff scheduled visits) | 27% (study staff did not assist with scheduling) |
| Baseline BP | Mean 148/85 mm Hg | Mean 158/92 mm Hg |
The comparison between Hyperlink 1 and Hyperlink 3 trials demonstrates the significant trade-offs between explanatory and pragmatic designs. The pragmatic design features of Hyperlink 3 substantially increased enrollment of study-eligible patients and those traditionally under-represented in clinical trials (women, minorities, and patients with less education and lower income) [1]. This demonstrates that identification and enrollment of a high proportion of study-eligible subjects could be done by usual primary care clinic staff. However, the trade-off was much lower adherence to the telehealth intervention than in Hyperlink 1, which is likely to reflect uptake under real-world conditions and substantially dilute intervention effect [1].
Ethical Challenges in Pragmatic and Cluster Randomized Trials
Conceptual Framework for Ethical Analysis
The ethical challenges in pragmatic and cluster RCTs can be understood through the lens of traditional research ethics principles—respect for persons, beneficence, and justice [2]—while recognizing their limitations when applied to these complex designs. A fourth principle, respect for communities, has been proposed to address the collective nature of these trials [2].
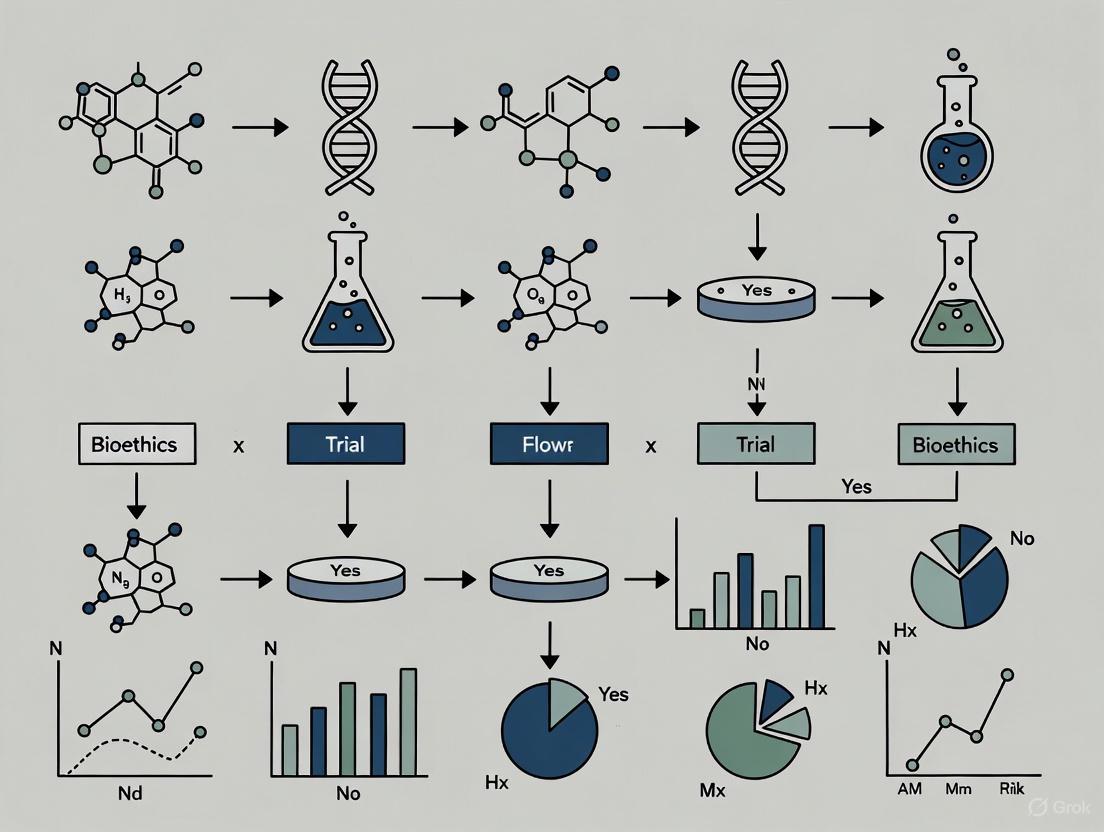
Diagram 1: Ethical Framework for Pragmatic and Cluster RCTs
Core Ethical Challenges in Cluster Randomized Trials
Cluster randomized trials pose at least six fundamental areas of ethical inquiry that must be addressed to establish a firm ethical foundation [3]:
Identification of Research Subjects: The question of who constitutes a research subject in CRTs is complex. Individuals may be subjects if their interests are compromised as a result of interventions in a research study, including those directly intervened upon, those intervened upon via manipulation of the environment, those with whom researchers interact for data collection, or those about whom researchers obtain identifiable private information [5].
Informed Consent Requirements: The ethical principle of respect for persons implies that researchers are generally obligated to obtain informed consent, but CRT designs present challenges to this requirement [5]. The appropriate approach to consent depends on whether interventions are administered at the individual or cluster level.
Application of Clinical Equipoise: The concept of clinical equipoise—that there must be genuine uncertainty in the expert medical community about the preferred treatment—may apply differently in CRTs, particularly those evaluating policy or health system interventions.
Benefit-Harm Analysis: Determining whether benefits outweigh risks requires consideration of both individual and cluster-level impacts, which may affect participants differently.
Protection of Vulnerable Groups: CRTs may involve vulnerable populations who require additional protections, particularly when entire communities or groups are enrolled.
Role and Authority of Gatekeepers: Gatekeepers—persons or bodies making decisions on behalf of clusters—play an important role in CRTs, but their appropriate authority and responsibilities require clarification [5].
Informed Consent Decision Framework
The requirement for informed consent represents one of the most challenging ethical issues in pragmatic and cluster RCTs. The level at which interventions are administered determines the appropriate approach to consent.
Diagram 2: Informed Consent Decision Framework for Cluster RCTs
For individual-level interventions, informed consent should generally be obtained from research subjects, as individuals can theoretically consent to the treatments offered within their cluster [5]. For cluster-level interventions, it may not be possible to obtain informed consent from individual cluster members, and a waiver of consent may be appropriate when the study intervention is delivered at the cluster level, making it difficult for cluster members to avoid the intervention if they don't wish to participate [5].
The Research-Practice Distinction Debate
A central ethical question in pragmatic RCTs is whether a meaningful distinction exists between research and clinical practice. Contemporary ethical frameworks distinguish research from practice to demarcate activities that ought to undergo ethical review for participant protection [6]. Most authors reject the need for a research-practice distinction in pragmatic RCTs, arguing that this distinction rests on the presumptions that research participation offers patients less benefit and greater risk than clinical practice—neither of which is necessarily true in pragmatic RCTs [6].
This debate has practical implications for regulatory oversight. There is consensus that oversight by research ethics committees is time-consuming, costly, and overly complex, making it an impediment to research [6]. Many authors believe existing oversight procedures should be streamlined for low-risk pragmatic RCTs, while a few argue for a wholly new system of oversight [6].
Practical Applications and Case Studies
Experimental Protocols for Ethical Cluster RCT Implementation
Protocol 1: Gatekeeper Engagement and Cluster Consent
Purpose: To establish legitimate authority for cluster participation when individual consent is not feasible.
Procedures:
- Identify appropriate gatekeepers with legitimate authority to represent the cluster's interests
- Assess the gatekeeper's understanding of the research and ability to represent cluster interests
- Provide comprehensive study information including intervention details, risks, benefits, and data collection procedures
- Document gatekeeper agreement through formal mechanisms
- Establish ongoing communication channels between researchers and gatekeepers throughout the study
Ethical Considerations: Gatekeepers should understand that their role is to represent cluster interests, not to compel individual participation. Researchers should clarify that gatekeeper permission does not replace individual consent when required for specific research procedures [5].
Protocol 2: Integrated Consent for Pragmatic RCTs
Purpose: To obtain meaningful consent while maintaining the real-world applicability of pragmatic RCTs.
Procedures:
- Disclose information about randomization and study participation during clinical encounters
- Utilize integrated consent materials that mirror clinical decision-making discussions
- Implement alternative consent methods such as electronic devices for information presentation, clinician-led verbal consent documented in electronic health records, or short-form consent documents [7]
- Focus disclosure on incremental risks of research participation compared to clinical practice
- Document consent processes in ways that integrate with clinical workflow
Ethical Considerations: Surveys indicate that patients generally prefer informed consent, highlighting the importance of ensuring participants are aware of potential side effects and can choose whether to participate [7]. The purpose of the study, risks and benefits, and voluntary participation should be disclosed, though there is disagreement as to whether randomization must be disclosed [6].
Protocol 3: Vulnerability Assessment in Community Settings
Purpose: To identify and protect vulnerable populations in cluster randomized trials.
Procedures:
- Conduct pre-trial assessment of potential vulnerabilities within clusters
- Implement additional protections for vulnerable participants, such as assessing decision-making capacity and screening for organ dysfunction while maintaining the trial's pragmatic nature [7]
- Establish monitoring mechanisms to detect disproportionate burdens on vulnerable subpopulations
- Create meaningful opt-out mechanisms for individuals within clusters when feasible
- Engage community representatives in ongoing oversight of participant welfare
Ethical Considerations: Pragmatic RCTs often include a broad range of patients, including older individuals with coexisting conditions, which increases applicability but also the risk of harm [7]. Additional protections should be implemented while maintaining the trial's pragmatic nature.
Table 3: Research Reagent Solutions for Ethical RCT Implementation
| Tool/Resource | Function | Application Context |
|---|---|---|
| PRECIS-2 Tool | Aids trialists in designing trials that are fit for purpose across nine domains on a continuum from explanatory to pragmatic [1] | Trial design phase; helps align design decisions with trial objectives |
| Electronic Health Record (EHR) Algorithms | Automated real-time identification of eligible patients during routine care encounters [1] | Patient recruitment in pragmatic trials; minimizes research-specific screening procedures |
| Gatekeeper Mechanism | Person or body charged with making decisions on behalf of an entire cluster when individual consent is not feasible [5] | Cluster randomized trials; provides ethical oversight for cluster-level interventions |
| Waiver of Consent Criteria | Regulatory provisions allowing research to proceed without consent when specific conditions are met (minimal risk, impracticability, research importance) [5] | Pragmatic trials where consent would render the study infeasible and risks are minimal |
| Community Advisory Board | Engages community representatives in research oversight and ensures community values are respected [2] | Community-based trials; promotes respect for communities and builds trust |
| Alternative Consent Methods | Electronic consent, integrated verbal consent, short-form documents that fit within clinical workflows [7] | Pragmatic trials in routine care settings where traditional consent is impractical |
The ethical landscape of randomized controlled trials has expanded significantly with the growth of pragmatic and cluster randomized designs. These methodologies offer powerful approaches to answering real-world questions about health interventions, but they challenge traditional ethical frameworks centered on individual autonomy and protection. Navigating this landscape requires a nuanced approach that balances scientific rigor with ethical responsibility, recognizing that different trial designs pose different ethical challenges.
The future of ethical RCTs in community settings lies in developing more sophisticated approaches to consent, recognizing legitimate community interests, creating proportionate oversight mechanisms, and maintaining transparency about the trade-offs inherent in different design choices. By adopting the protocols and frameworks outlined in this article, researchers can conduct methodologically sound and ethically robust trials that generate evidence relevant to real-world decision-making while respecting the rights and welfare of individuals and communities.
Challenging the Research-Practice Distinction in Real-World Settings
The traditional distinction between health-related research and clinical practice has become increasingly blurred, particularly with the rise of pragmatic randomized controlled trials (RCTs) in community and real-world settings. While conventional ethical frameworks were designed for explanatory RCTs that test efficacy under ideal conditions, pragmatic RCTs evaluate effectiveness in routine clinical practice, raising fundamental questions about the applicability of traditional ethical oversight mechanisms [8]. This paradigm shift challenges the long-accepted view that research participation inherently offers patients less benefit and greater risk than clinical practice—a presumption that no longer holds true in the context of many pragmatic trials investigating usual care interventions [8].
The growing international movement toward learning healthcare systems, where the provision of care is closely integrated with evidence generation, further complicates this distinction [9]. As health systems increasingly employ rigorous methodologies like pragmatic RCTs for quality improvement and program evaluation, the ethical foundation for differentiating between research and practice requires critical re-examination [8] [9]. This application note addresses the ethical and practical implications of this evolving landscape and provides frameworks for appropriate ethical appraisal of evidence-generating initiatives in community settings.
Core Ethical Framework and Analysis
Theoretical Foundations and Current Debate
The ethical justification for traditional RCTs typically rests on two conditions: (1) the existence of equipoise (genuine uncertainty within the expert medical community about the preferred treatment), and (2) that the trial must be scientifically promising [10]. In social and community settings, these conditions can create genuine moral conflicts, particularly when one intervention appears superior outside a controlled environment or when methodological rigor conflicts with real-world applicability [10].
Contemporary ethical discussion is predominantly framed by the assumption that the primary function of research oversight is to protect participants from risk. Since pragmatic RCTs commonly involve usual care interventions with minimal incremental risk, this has led many ethicists to question the need for traditional informed consent processes and intensive ethical review [8]. However, a more comprehensive understanding suggests that the function of oversight should be understood broadly as protecting both the liberty and welfare interests of participants while simultaneously promoting public trust in research activities [8].
Table 1: Key Ethical Considerations for Pragmatic RCTs in Real-World Settings
| Ethical Dimension | Explanatory RCT Perspective | Pragmatic RCT Perspective | Community Setting Implications |
|---|---|---|---|
| Research-Practice Distinction | Clear separation; different ethical standards apply | Blurred boundaries; similar ethical standards should apply | Activities traditionally considered "practice" may require ethical oversight |
| Informed Consent | Strict requirement for comprehensive written consent | May proceed with simplified consent or waiver when risks are low and consent is infeasible | Community engagement may supplement or replace individual consent in low-risk scenarios |
| Risk Assessment | Focus on incremental risks of experimental interventions | Focus on risks relative to usual clinical care | Must consider risks to communities and collectivities, not just individual participants |
| Oversight Mechanism | Mandatory research ethics committee review | Streamlined, proportionate review based on actual risk level | Requires flexible systems that can accommodate diverse community-based initiatives |
| Primary Ethical Concern | Protection from research-related risks | Protection of liberty and welfare interests while promoting trust | Balancing scientific rigor with community values and practical constraints |
Empirical Evidence and Current Trends
A comprehensive review of recent literature on pragmatic RCT ethics reveals that most authors reject the need for a sharp research-practice distinction [8]. This perspective is driven by several converging trends:
- Increased public funding for comparative effectiveness research and patient-oriented research initiatives [8]
- Advanced electronic data systems that facilitate data collection in routine care settings [8]
- Development of innovative trial designs (e.g., cluster crossover trials, stepped-wedge designs) that are embedded in healthcare systems [8]
- Growing recognition that many initiatives traditionally classified as "non-research" nonetheless impose risks that warrant ethical oversight [9]
This evolving landscape has created operational and ethical challenges, as existing regulatory frameworks were developed with pharmaceutical trials in mind rather than real-world evaluations of usual care interventions [8].
Data Presentation: Ethical Appraisal Frameworks
Risk Assessment Domains and Scoring
The Public Health Ontario (PHO) Risk Screening Tool offers a practical approach to ethical appraisal that transcends the research-practice distinction. This tool identifies potential project-associated risks across five key domains and generates a risk score (0-3) that determines the appropriate level of ethics review [9].
Table 2: Risk Domains and Assessment Criteria from the PHO Risk Screening Tool
| Risk Domain | Low Risk Indicators (Score 0-1) | High Risk Indicators (Score 2-3) | Community Setting Considerations |
|---|---|---|---|
| Sensitivity | Non-sensitive topics; anonymous data collection | Politically/culturally sensitive topics; stigmatizing information | Community perception of sensitivity may differ from institutional views |
| Participant Selection & Consent | Non-vulnerable populations; minimal intrusion | Vulnerable populations; potential for coercion | Existing power dynamics within communities may create vulnerability |
| Data Collection Methods | Routine non-intrusive methods; public data | Physically/psychologically intrusive methods; private data | Methods acceptable in clinical settings may be intrusive in community contexts |
| Identifiability & Privacy | Anonymous data; strong confidentiality protections | Direct identifiers collected; potential for re-identification | Community members may have heightened privacy concerns in close-knit groups |
| Commercial Interests | No commercial interests; public benefit primary | Significant commercial interests; potential conflicts | Exploitation concerns when research benefits external entities disproportionately |
The PHO tool employs a threshold approach to scoring, where the final risk level represents the highest level of risk identified in any single domain, ensuring comprehensive protection [9]. This approach acknowledges that a single high-risk element may warrant enhanced oversight regardless of low risks in other domains.
Implementation Framework for Ethical Review
The application of a risk-based approach to ethical appraisal requires a structured implementation framework that can be adapted to various community settings:
Ethical Review Pathway: This diagram illustrates the risk-proportionate approach to ethics review, where the level of scrutiny corresponds to the project's risk level.
Experimental Protocols for Ethical Pragmatic RCTs
Comprehensive Study Protocol Framework
Drawing from best practices in protocol development, an ethical framework for pragmatic RCTs in community settings should include the following essential components, adapted from laboratory research protocols [11] and reporting guidelines for life sciences [12]:
Protocol Title: [Specific Trial Name]: A Pragmatic RCT in [Community Setting]
1. Background and Rationale
- Scientific Basis: Current evidence gaps and clinical equipoise
- Community Relevance: Justification for conducting the study in real-world settings
- Stakeholder Engagement: Description of community involvement in study design
2. Study Objectives and Endpoints
- Primary Objective: Clearly stated main research question
- Secondary Objectives: Additional questions to be addressed
- Community Benefit: Explicit description of potential community-level benefits
3. Methodology
- Trial Design: Pragmatic randomized controlled trial design
- Setting: Description of real-world clinical or community settings
- Participant Selection: Inclusion/exclusion criteria reflecting usual care populations
- Randomization: Method and timing of randomization procedures
- Interventions: Description of experimental and control interventions
4. Ethical Considerations
- Risk Assessment: Systematic identification and categorization of risks
- Consent Procedures: Appropriate consent process for risk level
- Privacy Protections: Measures to protect participant confidentiality
- Vulnerable Populations: Special protections if applicable
- Community Protections: Measures to protect community interests
5. Data Collection and Management
- Data Sources: Description of data collection methods
- Quality Assurance: Procedures to ensure data integrity
- Privacy Safeguards: Technical and administrative protections
6. Oversight and Monitoring
- Ethics Review: Level and frequency of ethical oversight
- Safety Monitoring: Procedures for identifying and addressing adverse events
- Community Advisory: Role of community advisory boards
This protocol framework emphasizes the reproducibility of experimental procedures while incorporating essential ethical safeguards appropriate for real-world settings [12] [11].
Implementation Workflow for Community-Based Trials
The successful implementation of ethical pragmatic RCTs requires careful attention to operational details within community settings:
Community Trial Workflow: This workflow illustrates the sequential phases of implementing pragmatic RCTs in community settings, with integrated ethics considerations at each stage.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Methodological and Ethical Tools for Pragmatic RCTs in Community Settings
| Tool Category | Specific Tool/Resource | Function and Application | Ethical Considerations |
|---|---|---|---|
| Trial Design Tools | PRECIS-2 tool [8] | Helps design trials along pragmatic-explanatory continuum | Ensures alignment between research questions and design choices to minimize participant burden |
| Risk Assessment Tools | PHO Risk Screening Tool [9] | Systematic identification and rating of project-associated risks | Enables proportionate ethics review based on actual risk rather than project classification |
| Consent Frameworks | Integrated consent models [8] | Simplifies consent process for low-risk pragmatic trials | Balances informational needs with practical feasibility in real-world settings |
| Ethical Oversight Systems | Proportionate review mechanisms [8] | Matches level of ethics review to project risk level | Prevents both over-protection and under-protection of participants |
| Community Engagement Methods | Community advisory boards | Ensures community input throughout research process | Addresses power imbalances and promotes collaborative partnership |
| Data Privacy Protections | De-identification protocols [9] | Minimizes privacy risks while maintaining data utility | Protects participant confidentiality in contexts with enhanced identifiability concerns |
| Neticonazole Hydrochloride | Neticonazole Hydrochloride, CAS:130773-02-3, MF:C17H23ClN2OS, MW:338.9 g/mol | Chemical Reagent | Bench Chemicals |
| Eleutheroside B1 | Eleutheroside B1, CAS:16845-16-2, MF:C17H20O10, MW:384.3 g/mol | Chemical Reagent | Bench Chemicals |
Application in Drug Development Contexts
For drug development professionals implementing pragmatic RCTs, several specific considerations apply:
1. Post-Marketing Studies: Pragmatic designs are particularly valuable for assessing drug effectiveness in real-world populations after regulatory approval. The ethical framework suggests that when studying already-approved medications, simplified consent procedures may be appropriate when risks are minimal and full consent is impractical [8].
2. Comparative Effectiveness Research: When comparing approved therapeutic alternatives, the ethical justification for traditional RCTs with comprehensive consent is less compelling. A risk-proportionate approach to consent and oversight may be more appropriate when interventions reflect usual care options [8].
3. Cluster Randomized Trials: In studies where entire communities or practices are randomized, community-level consent procedures may need to supplement or replace individual consent, particularly when the research poses minimal incremental risk to individual participants [9].
4. Using Clinical Data for Research: When electronic health records or other clinical data are used for research purposes, the identifiability and sensitivity of the data should determine the level of review required, rather than whether the activity is classified as research or practice [9].
The movement toward a learning health system framework, where evidence generation is embedded in routine care, requires drug development professionals to adopt more flexible approaches to ethical considerations while maintaining rigorous protections for patients and communities [8] [9].
Randomized Controlled Trials (RCTs) represent the gold standard for evaluating medical interventions, but they create a fundamental ethical tension between the physician's duty to provide optimal patient care and the scientific requirement for unbiased comparison. This tension is particularly acute in community settings, where research and clinical practice intersect in complex ways. The concept of clinical equipoise—defined as "genuine uncertainty within the expert medical community... about the preferred treatment"—provides the essential ethical foundation for justifying RCTs [13]. First proposed by Benjamin Freedman in 1987, clinical equipoise resolves the ethical dilemma that arises when an individual investigator's beliefs conflict with collective medical uncertainty [13]. Unlike theoretical equipoise, which requires exactly balanced evidence and can be disturbed by minimal information, clinical equipoise focuses on genuine uncertainty within the expert community, creating a more practical and sustainable ethical framework for clinical research [13].
The application of clinical equipoise in community RCTs presents distinctive challenges, including maintaining ethical standards across diverse practice settings, ensuring valid informed consent, and managing the tension between clinical care and research objectives. Community-based research often involves heterogeneous populations and varied practice settings, making the assessment and maintenance of genuine community uncertainty particularly complex. This document revisits the principle of clinical equipoise, examining its theoretical foundations, practical applications, and implementation protocols specifically for community RCTs, providing researchers with ethical and methodological guidance for navigating these challenges.
Theoretical Foundations and Current Challenges
From Individual to Community Equipoise
The evolution from individual to community equipoise represents a critical development in research ethics. The "community equipoise" (CE) strategy suggests that the judgment that neither treatment is preferable should be assessed according to a community standard rather than an individual investigator's opinion [14]. Thus, even if a physician personally believes one treatment may be superior, randomization remains ethically permissible as long as genuine disagreement persists within the medical community [14]. This conceptual shift is supported by several rationales: medical knowledge fundamentally resides in the community rather than individuals; professional disagreements constitute evidence that should influence individual opinions; trial participants would not clearly be better outside the trial; and the primary purpose of trials is to resolve disputes within the medical community [14].
Despite its widespread acceptance, the community equipoise concept faces significant criticisms. Tensions exist between its underlying rationales, and important ambiguities persist in how the CE criterion should be operationalized [14]. Moreover, critics argue that even if justified, community equipoise alone cannot justify continuing RCTs long enough to generate reliable knowledge for evidence-based practice [14]. Some ethicists fundamentally challenge the premise, arguing that clinical equipoise conflates therapeutic and research ethics, creating a "therapeutic misconception" [13]. Franklin Miller and Howard Brody contend that "the ethics of research and of therapy are fundamentally different," suggesting that clinical equipoise should be abandoned in favor of a framework that more clearly distinguishes clinical care from research participation [13].
Contemporary Challenges to Equipoise in Community Settings
Table 1: Empirical Evidence on Equipoise Challenges in Clinical Research
| Challenge Category | Key Findings | Supporting Evidence |
|---|---|---|
| Systematic Violation of Equipoise | 100% of industry-sponsored rheumatology RCTs (45/45) favored sponsor's drug [15] | Predictable outcomes based solely on sponsorship (P < 0.0001) [15] |
| Physician Perspectives | 36% of clinicians found it appropriate to enter patients in trials despite viewing treatments as "unequal bet" prospectively [16] | 87% would enter more patients if informed consent not required [16] |
| Patient Understanding | Self-interest (>70% in 4 studies) more common than altruism as participation motive [16] | Many participants expect personal benefit despite equipoise requirement [16] |
| Informed Consent Gaps | 47% of doctors thought few patients understood they were in a controlled experiment [16] | Up to 20% of doctors entered competent patients without informed consent [16] |
Recent empirical evidence reveals significant challenges to maintaining equipoise in contemporary clinical research, particularly highlighting systematic deviations from ethical ideals. Design bias represents a particularly concerning challenge, occurring when extensive preliminary data is used to design studies with a high likelihood of producing positive results [15]. This pre-trial design process systematically violates equipoise by creating studies where outcomes can be predicted based solely on sponsorship [15]. From an industry perspective, the drug development process necessarily involves "designing for success," as pharmaceutical companies will not commit hundreds of millions of dollars to RCTs without considerable certainty of positive outcomes [15].
Additional challenges emerge in patient understanding and consent. Studies reveal that therapeutic misconception remains prevalent, with many participants failing to recognize the fundamental differences between research and clinical care [16]. Quantitative evidence indicates that a significant proportion of trial participants are motivated by self-interest rather than altruism, suggesting they may not understand the equipoise requirement that treatments are equally likely to benefit them [16]. Furthermore, audits of consent processes reveal substantial gaps, with nearly half of physicians doubting participants' understanding of their involvement in controlled experiments [16].
Application Notes: Implementing Clinical Equipoise in Community RCTs
Practical Framework for Assessing and Maintaining Equipoise
Pre-Trial Equipoise Assessment Protocol
Implementing clinical equipoise requires systematic assessment before trial initiation. The following protocol provides a structured approach:
Systematic Uncertainty Assessment: Conduct a formal survey of expert clinicians and community practitioners representing the target community for the RCT. Document the distribution of treatment preferences and the reasoning behind preferences. The criterion for equipoise is met when no single approach commands consensus (typically <70% agreement on preferred treatment).
Evidence Synthesis and Gap Analysis: Perform a systematic review of existing evidence, focusing on methodological quality of prior studies, consistency of findings across studies, and directness of evidence to the specific patient population and outcomes relevant to the community setting. Equipoise exists when credible systematic reviews or meta-analyses indicate insufficient evidence for definitive conclusions.
Stakeholder Perspective Integration: Incorporate perspectives of patient representatives and community caregivers regarding treatment preferences, outcomes that matter, and risk-benefit tradeoffs. Equipoise should reflect uncertainty that acknowledges patient values and preferences, not merely clinical biomarkers.
Documentation and Transparency: Create a comprehensive equipoise statement for the trial protocol, explicitly documenting the sources of uncertainty, the methods used to assess equipoise, and the criteria that would disturb equipoise. This statement should be included in submissions to research ethics committees and institutional review boards.
Monitoring Equipoise During Trial Conduct
The ethical requirement for equipoise extends throughout the trial duration, necessitating ongoing monitoring:
Interim Analysis Planning: Establish a priori stopping guidelines that specify the statistical threshold at which interim results would definitively establish superiority of one intervention. These guidelines should be developed by an independent data monitoring committee (DMC) with clear protocols for maintaining trial blinding.
Community Sentiment Tracking: Periodically re-survey the expert community during trial conduct to detect shifts in opinion based on emerging external evidence (not trial results). The trial remains ethical as long as genuine disagreement persists within the broader community, regardless of any individual investigator's beliefs.
Practical Implementation: Utilize adaptive trial designs that allow for modifications based on accumulating evidence while preserving trial integrity. These may include response-adaptive randomization or pre-planned mid-trial adjustments that maintain ethical treatment of participants while pursuing scientific objectives.
Ethical Safeguards and Community Engagement
Enhanced Informed Consent Process
Traditional consent processes often fail to adequately convey the concept of equipoise and the nature of research participation. An enhanced consent framework for community RCTs should include:
Explicit Equipoise Education: Clearly explain the meaning of clinical equipoise using patient-friendly language: "Doctors and experts genuinely don't know which treatment is better, which is why we're doing this study." Avoid technical jargon while preserving the core concept of collective uncertainty.
Arms-length Consent Discussions: When possible, separate research consent from clinical care discussions, potentially using dedicated research coordinators not directly involved in the patient's clinical care. This helps mitigate the therapeutic misconception where patients conflate research with individualized therapeutic care.
Continuous Consent Processes: Implement ongoing consent discussions throughout trial participation, especially when new external evidence emerges that might affect the equipoise calculation. Participants should be informed of significant developments that might influence their willingness to continue.
Community Engagement and Stakeholder Involvement
Community RCTs require particularly robust engagement strategies to ensure ethical conduct:
Community Advisory Boards: Establish representative community advisory boards with meaningful involvement in trial design, implementation, and oversight. These boards should include patient representatives, community clinicians, and other stakeholders who can reflect community values and concerns.
Equipoise as a Shared Responsibility: Frame equipoise as a collective commitment rather than merely an individual investigator's determination. The broader community of clinicians and stakeholders shares responsibility for maintaining equipoise and ensuring the trial remains ethically justified throughout its duration.
Experimental Protocols
Protocol 1: Empirical Assessment of Community Equipoise
Objective
To quantitatively and qualitatively assess the state of clinical equipoise within the expert community regarding comparative interventions before initiating a community RCT.
Materials and Reagents
Table 2: Research Reagent Solutions for Equipoise Assessment
| Item Name | Function/Application | Specification Notes |
|---|---|---|
| Expert Practitioner Database | Identification and recruitment of content experts | Include academic and community-based practitioners; ensure geographic and practice diversity |
| Validated Survey Instrument | Quantitative assessment of treatment preferences | 7-point Likert scale from "strong preference A" to "strong preference B"; include uncertainty option |
| Semi-structured Interview Guide | Qualitative exploration of uncertainty rationale | Probe evidence basis for preferences, perceived evidence gaps, willingness to randomize patients |
| Evidence Synthesis Package | Standardized summary of existing evidence | Systematic review abstracts; evidence tables; methodological quality assessment |
| Delphi Process Framework | Structured group communication technique | Iterative rating with controlled feedback; statistical aggregation of group response |
Methodology
Stakeholder Mapping and Recruitment
- Identify all relevant stakeholder groups (specialists, primary care providers, methodological experts, patient representatives)
- Recruit a representative sample from each group (target n=30-50 per key stakeholder category)
- Obtain informed consent for participation in the equipoise assessment
Evidence Synthesis and Presentation
- Prepare standardized evidence summaries presenting methodological quality and findings of relevant studies
- Balance presentation to avoid bias toward either intervention
- Include evidence gaps and limitations in current knowledge
Data Collection
- Administer validated survey instrument to assess baseline preferences
- Conduct semi-structured interviews with a subset (n=15-20) to explore rationale
- Convene expert panel (n=10-15) for structured discussion of evidence
Data Analysis and Interpretation
- Quantitative: Calculate distribution of preferences; equipoise exists if no clear consensus (<70% preference for any single approach)
- Qualitative: Thematic analysis of interview transcripts to identify sources of uncertainty and perceived evidence gaps
- Integrated: Combine quantitative and qualitative findings to generate comprehensive equipoise assessment
Deliverable
A comprehensive equipoise assessment report documenting the degree and nature of uncertainty within the expert community, to be included in the RCT protocol submission to research ethics committees.
Protocol 2: Monitoring Equipoise During Trial Conduct
Objective
To establish an ongoing system for monitoring the state of clinical equipoise throughout the conduct of a community RCT, ensuring continuous ethical justification.
Methodology
Independent Data Monitoring Committee (DMC)
- Establish a DMC with relevant expertise and independence from investigators and sponsors
- Develop a priori statistical stopping guidelines based on pre-specified efficacy boundaries
- Schedule regular interim analyses with strict confidentiality protocols
External Evidence Surveillance System
- Implement systematic surveillance of newly published evidence relevant to the trial interventions
- Assess methodological quality and potential impact on equipoise of new studies
- Report significant developments to the DMC and research ethics committee
Community Sentiment Tracking
- Conduct abbreviated surveys of the expert community at predetermined intervals (e.g., annually)
- Monitor clinical practice guidelines and treatment recommendation changes
- Track enrollment patterns and clinician willingness to refer patients to the trial
Threshold Determination and Response Protocol
- Define clear thresholds for equipoise disturbance (e.g., consistent results from multiple high-quality trials)
- Establish protocol for response if equipoise is disturbed, including potential trial modification or termination
- Maintain transparent documentation of all monitoring activities and decisions
Deliverable
An ongoing monitoring system with regular reports to the trial steering committee and research ethics committee, documenting the continued ethical justification for the RCT based on preserved clinical equipoise.
Visualizing the Equipoise Assessment Workflow
Clinical Equipoise Assessment and Monitoring Pathway
Figure 1: Clinical Equipoise Assessment Pathway
Community Engagement Framework for Equipoise
Figure 2: Community Engagement Framework
Clinical equipoise remains an essential, though evolving, ethical requirement for randomized controlled trials in community settings. The concept has demonstrated remarkable resilience despite theoretical challenges and empirical evidence of systematic violations, particularly in industry-sponsored research [15]. The contemporary application of clinical equipoise requires robust assessment methodologies, transparent documentation, and ongoing monitoring to maintain ethical integrity throughout trial conduct.
For community RCTs specifically, the implementation of clinical equipoise must acknowledge the distinctive features of community-based research: diverse practice settings, heterogeneous populations, varying levels of research sophistication, and the central importance of trust relationships. The protocols and frameworks presented in this document provide practical approaches for addressing these challenges while maintaining the ethical rigor that underpins valid clinical research.
Future directions for strengthening the ethical foundation of community RCTs include developing more sophisticated metrics for assessing equipoise, enhancing community engagement models, and creating more adaptive trial designs that can respond to evolving evidence while preserving ethical treatment of participants. As clinical research continues to evolve, the principle of clinical equipoise must similarly develop, maintaining its central role in balancing scientific progress with ethical obligations to research participants.
Identifying Vulnerable Populations and Ensuring Additional Protections
Conducting randomized controlled trials (RCTs) in community settings introduces unique ethical imperatives, particularly concerning the engagement of vulnerable populations. Vulnerability in research is defined as a heightened likelihood of being wronged or incurring additional harm [17]. In community-based RCTs, which are often pragmatic in design and integrated into real-world settings, identifying and protecting these groups is a cornerstone of ethical research practice. The foundational ethical principles of respect for persons, beneficence, and justice demand that researchers move beyond a one-size-fits-all approach to ethics and instead implement tailored safeguards [6] [18]. This document outlines a structured framework for the identification of vulnerable groups and the implementation of additional, necessary protections to safeguard their welfare and rights within the context of community RCTs.
Defining and Categorizing Vulnerable Populations
A clear operational definition of vulnerability is critical for its consistent application in research practice. For the purpose of this protocol, a vulnerable population is any group whose members may have an increased likelihood of being wronged or of incurring additional harm due to their compromised capacity to protect their own interests [17]. This compromised capacity can stem from intrinsic factors (e.g., cognitive impairment) or contextual/situational factors (e.g., institutionalization or economic disadvantage).
The following table categorizes common vulnerable populations encountered in community-based research, their associated risk factors, and the primary ethical concerns their inclusion raises.
Table 1: Categorization of Vulnerable Populations and Associated Ethical Concerns
| Population Type | Specific Risk Factors | Primary Ethical Concerns |
|---|---|---|
| Individuals with Cognitive Impairment (e.g., Alzheimer's disease) | Lack of capacity to provide informed consent [17] | - Need for surrogate decision-making- Potential for coercion- Ensuring comprehension of research |
| Institutionalized Persons (e.g., nursing home residents) | Subordination within a hierarchy, limited autonomy [17] | - Coercion due to power dynamics- Privacy and confidentiality breaches- Undue influence from caregivers |
| Economically or Educationally Disadvantaged Persons | Economic instability, lower health literacy, limited resources [19] [18] | - Undue inducement by incentives- Lack of comprehension of research- Inequitable distribution of research burdens |
| Ethnic, Racial, or Linguistic Minorities | Historical marginalization, language barriers, cultural mistrust [18] | - Cultural insensitivity- Lack of equitable access to research benefits- Communication barriers during consent |
| Rural Populations in Low-Resource Settings | Less access to medical/social resources, poverty, collectivistic social structures [19] | - Complex community entry processes- Navigating patriarchal power structures- Ensuring individual consent within a collective |
It is essential to recognize that individuals may belong to multiple overlapping vulnerable groups, a situation that compounds risk and necessitates enhanced protections.
Ethical Framework and Regulatory Background
The ethical conduct of research with vulnerable populations is anchored in international guidelines which stipulate that special protections are required to ensure their participation is equitable and safe [17]. The traditional ethical framework for research was developed with explanatory RCTs in mind, but pragmatic RCTs in community settings challenge this model. A key debate revolves around the research-practice distinction [6]. Some argue that in pragmatic RCTs evaluating usual care, the risks are minimal and the distinction is less relevant, potentially justifying simplified consent or oversight. However, this view is insufficient when working with vulnerable communities, where the function of oversight must be understood broadly as protecting the liberty and welfare interests of participants and promoting public trust [6].
Furthermore, the principle of justice requires that the burdens and benefits of research are distributed fairly. Vulnerable populations should not be systematically selected for research due to their easy availability or manipulability, nor should they be excluded from the potential benefits of research participation. The ethical approach, therefore, is one of careful inclusion with robust protections, rather than blanket exclusion.
Experimental Protocols for Identification and Protection
Protocol 1: Community Entry and Participant Identification
Objective: To ethically gain entry into a community and identify potential research participants from vulnerable groups while respecting cultural norms and power structures.
Methodology:
- Engage Gatekeepers: The research team must first engage with formal community gatekeepers (e.g., chiefs, elders, council members) [19]. This is a non-negotiable first step in many rural African and other traditional contexts.
- Present Research: Present the study aims, significance, and expected duration to the gatekeepers, seeking their permission to operate within the community [19].
- Secure an Independent Mediator: Request the chief's assistance in identifying an independent mediator who is respected and eloquent, but who does not hold a position of power that could coerce community members. This individual will facilitate household introductions [19].
- Household Access: The research team, led by the independent mediator, approaches heads of households to introduce the study and seek permission to speak with household members [19].
- Individual Screening: Identify individuals who meet the study's scientific inclusion criteria. In the case of married women in patriarchal settings, it is often mandatory to also obtain permission from their husbands after the initial individual introduction [19].
Protocol 2: Culturally-Sensitive Capacity Assessment and Consent
Objective: To ensure informed consent is obtained in a manner that is comprehensible, culturally appropriate, and respects the decision-making capacity of potential participants.
Methodology:
- Assessment of Capacity: For studies involving populations where cognitive impairment may be present (e.g., Alzheimer's disease), a formal capacity assessment must be integrated into the screening process. This was identified as a frequent reporting deficiency in pragmatic RCTs, highlighting the need for explicit protocols [17].
- Tiered Consent Process:
- For participants with capacity: Proceed with standard informed consent.
- For participants lacking capacity: Secure consent from a legally authorized surrogate (e.g., family member) while also seeking the participant's assent (affirmative agreement) to the extent of their ability.
- Culturally-Tailored Consent Disclosure:
- Translation: All consent materials and discussions must be conducted in the participant's native language [19] [18].
- Simplification: Use clear, accessible language, avoiding complex jargon.
- Verbal Explanation & Written Documentation: The independent mediator or researcher should read the consent form aloud. For participants with low literacy, assist them in providing a thumbprint if they agree to participate [19].
- Time for Reflection: Ethically, selected individuals should be given adequate time (e.g., one week) to reflect on their decision and ask further questions before finalizing consent [19].
Protocol 3: Implementing Ongoing Safeguards and Monitoring
Objective: To create and maintain a "safe space" throughout the research process, protecting participants from harm and preserving their autonomy.
Methodology:
- Right to Withdraw: Emphasize explicitly and repeatedly that participants can withdraw from the study at any time without any negative consequences to the care or services they receive [18].
- Confidentiality and Data Protection: Implement rigorous data protection measures. This includes the anonymization of personally identifiable information and the use of secure storage solutions to prevent unauthorized access [18].
- Cultural Sensitivity and Training: Provide research team members with training on cultural norms, values, and practices of the community. Involve community members in the research design to align the study with community needs and values [18].
- Feedback Mechanisms: Establish avenues for participant feedback, such as post-study surveys or community meetings, to understand their experiences and improve future research practices [18].
Data Presentation and Analysis
The following table synthesizes the key protective strategies that correspond to the vulnerabilities identified in Table 1, providing a clear guide for ethical research design.
Table 2: Summary of Additional Protections for Vulnerable Populations
| Vulnerability | Additional Protective Strategies | Objective of Protection |
|---|---|---|
| All Vulnerable Groups | - Simplified, verbal consent processes- Secure data anonymization- Clear right to withdraw without penalty | To enhance autonomy, protect privacy, and prevent coercion. |
| Lack of Capacity | - Formal capacity assessment- Surrogate consent + participant assent | To respect the will of the individual while ensuring a legally valid consent process. |
| Institutionalization | - Oversight by an unaffiliated monitor- Ensuring private spaces for consent discussions | To mitigate power imbalances and protect against coercion from institutional caregivers. |
| Economic Disadvantage | - Careful calibration of incentives to avoid undue inducement- Provision of resources in non-cash form where appropriate | To ensure participation is voluntary and not driven by desperation. |
| Cultural/Linguistic Barriers | - Employing culturally-competent staff and translators- Community engagement in study design | To ensure true comprehension and cultural respect, building trust. |
Workflow Visualization
The following diagram illustrates the logical sequence and key decision points in the ethical engagement of vulnerable populations in a community-based RCT.
Ethical Participation Workflow for Vulnerable Populations
The Scientist's Toolkit: Essential Reagents and Materials
This section details key non-material "reagents" and resources essential for the ethical conduct of research with vulnerable populations in community settings.
Table 3: Essential Resources for Ethical Research in Vulnerable Communities
| Item / Resource | Function / Purpose | Application Notes |
|---|---|---|
| Culturally-Validated Capacity Assessment Tool | To objectively determine a potential participant's ability to understand and consent to the research study. | Essential for studies involving individuals with dementia or cognitive impairment. Must be validated in the local language and cultural context [17]. |
| Translated & Simplified Consent Forms | To ensure information is presented in a language and at a literacy level the participant can comprehend. | Forms should be translated by a professional and then reviewed by a community member for cultural and linguistic accuracy [19] [18]. |
| Independent Community Mediator | To act as a liaison between the research team and the community, facilitating trust and ensuring introductions are free from coercion. | Should be a trusted, eloquent community member who does not hold a powerful leadership position [19]. |
| Certificate of Confidentiality | To protect sensitive participant data from being disclosed to third parties (e.g., courts, other agencies). | Helps in building trust with participants, especially when collecting sensitive information, by providing a legal layer of privacy protection. |
| Ethics Committee Approval (REC/IRB) | To provide independent oversight and ensure the study design meets ethical standards for protecting participants. | Required for publication and is a cornerstone of credible research. Some pragmatic RCTs may argue for streamlined oversight, but this is risky with vulnerable groups [6] [17]. |
| Cultural Sensitivity Training Modules | To educate the research team on local customs, norms, and power structures to prevent cultural offenses and build rapport. | Training should be mandatory for all field staff and developed in consultation with community experts [18]. |
| Dhdps-IN-1 | Dhdps-IN-1|DHDPS Inhibitor|Research Use Only | |
| HPV18-IN-1 | HPV18-IN-1, MF:C14H10N4OS, MW:282.32 g/mol | Chemical Reagent |
Randomized controlled trials (RCTs) represent the gold standard for generating robust evidence on intervention effectiveness, yet their implementation in community settings raises complex ethical considerations that demand examination from multiple stakeholder perspectives [20] [21]. The fundamental ethical tension in RCTs stems from the reality that those who bear the risks and burdens of trial participation are not always the primary beneficiaries of the resulting knowledge [20]. This ethical challenge becomes particularly pronounced in community-based research, where interventions are implemented in real-world settings with diverse populations [22] [23].
The evolution of research ethics has been significantly influenced by historical documents developed in response to research misconduct, including the Nuremberg Code, the Declaration of Helsinki, and the Belmont Report [20]. These foundational frameworks establish core principles of respect for persons, beneficence, and justice that continue to guide contemporary research ethics [20] [21]. However, traditional ethical frameworks were primarily developed with explanatory RCTs in mind, creating potential misalignment with pragmatic and community-based trials that operate under different conditions and constraints [23] [6].
This application note examines the key ethical concerns in community-based RCTs from the perspectives of three central stakeholder groups: investigators, patients/participants, and regulators/ethics committees. By synthesizing recent empirical research and theoretical analyses, we provide methodological guidance for navigating these ethical challenges while maintaining scientific rigor in community-engaged research.
Stakeholder-Specific Ethical Concerns
Investigator Perspectives
Clinical investigators face the challenge of balancing scientific rigor with ethical practice when designing and implementing community-based RCTs. A primary concern involves maintaining clinical equipoise—the genuine uncertainty within the expert medical community about the comparative therapeutic merits of each arm in a clinical trial [21] [24]. The ethical justification for randomization rests on this principle of uncertainty, yet investigators must reconcile this with the therapeutic misconception that often leads participants to believe treatment assignments are based on individual therapeutic needs [20] [21].
Methodological challenges in community settings include contamination control in closely-knit communities and the practical feasibility of implementing rigorous RCT designs in real-world contexts [22]. Investigators conducting community-based participatory research (CBPR) randomized trials with American Indian communities noted significant methodological complexities, including geographic isolation, limited resources, and historical mistrust of researchers [25]. These challenges necessitate adaptive designs such as stepped-wedge cluster randomization, which allows all communities to eventually receive the intervention while maintaining scientific validity [25].
The design of control groups presents another significant ethical challenge for investigators. While placebo-controlled trials (PCTs) offer methodological advantages, they raise ethical concerns when proven effective interventions exist [21]. The Declaration of Helsinki states that new interventions should be tested against the best proven interventions, though it allows for placebo use under specific conditions, including when no proven intervention exists or when compelling methodological reasons justify its use and patients receiving placebo are not subjected to additional risks of serious harm [21].
Patient and Community Perspectives
Patients and community participants bring fundamentally different ethical concerns to RCTs, centered primarily on issues of autonomy, information, and relevance. The therapeutic misconception represents a crucial ethical challenge, where participants may incorrectly believe that research procedures are designed for their direct benefit rather than for generating generalizable knowledge [20]. This misunderstanding compromises the validity of informed consent, as participants may not fully appreciate the ways in which research participation differs from ordinary clinical care [20].
Community stakeholders often express concerns about control group allocation, particularly in cultures that value collectivism and equitable distribution of benefits [25]. In research with American Indian communities, for instance, control groups may be viewed as culturally inappropriate because they exclude some community members from potential benefits [25]. This has led to the development of alternative trial designs, such as wait-list control approaches where all participants eventually receive the intervention [25].
The informed consent process presents particular challenges in pragmatic RCTs that mimic usual care settings. Patients may not recognize they are participating in research when interventions are embedded in routine clinical practice, raising questions about when alterations to traditional consent procedures are appropriate [23] [6]. Empirical studies with patients and community members reveal strong preferences for transparent communication about randomization, even in low-risk studies [23] [6].
Community advisory boards in trials like the Emergency Medicine Palliative Care Access (EMPallA) study have demonstrated how patient and community stakeholders can identify ethically important considerations that researchers might overlook, including the need for culturally appropriate recruitment materials, inclusion of non-English speakers, and measurement of patient-centered outcomes like loneliness and caregiver burden [26].
Regulator and Ethics Committee Perspectives
Research ethics committees and regulators grapple with the application of existing ethical frameworks to community-based RCTs, which often differ significantly from the traditional explanatory trials for which these frameworks were developed [23] [6]. A central challenge involves categorizing activities as research versus practice, a distinction that determines which activities require ethics review [6]. Pragmatic RCTs that evaluate established interventions in routine care settings blur this boundary, creating regulatory uncertainty [23] [6].
The determination of minimal risk presents another challenge for regulators. While pragmatic RCTs often involve usual care interventions that may pose minimal incremental risk, ethics boards must consider potential harms that might not be immediately apparent to investigators [23]. This includes psychological distress related to randomization, privacy breaches in studies using administrative data, and group harms in cluster-randomized trials [23].
Regulators also face pressure to streamline oversight processes for low-risk pragmatic RCTs while maintaining appropriate protections [6]. Many authors view current regulatory oversight as burdensome and impractical, particularly for trials that closely mirror usual care [6]. This has led to calls for novel oversight systems specifically designed for pragmatic RCTs, though consensus on what these systems should entail remains elusive [6].
Table 1: Key Ethical Concerns by Stakeholder Group
| Stakeholder | Primary Ethical Concerns | Contextual Factors |
|---|---|---|
| Investigators | Clinical equipoise [21] [24]; Control group design [21]; Community contamination [22]; Balancing rigor with feasibility [22] | Trial design complexity; Resource constraints; Historical community relationships [25] |
| Patients/Community | Therapeutic misconception [20]; Informed consent quality [23] [6]; Control group exclusion [25]; Relevance of outcomes [26] | Cultural values [25]; Health literacy; Historical research exploitation [25] [27] |
| Regulators/Ethics Committees | Research-practice distinction [6]; Minimal risk determination [23]; Appropriate oversight level [6]; Balancing protection with facilitation [23] | Regulatory frameworks; Jurisdictional variations; Precedent concerns [23] |
Methodological Protocols for Addressing Ethical Challenges
Community-Engaged Research Protocol
The implementation of community-based participatory research (CBPR) principles provides a structured approach for addressing ethical concerns throughout the RCT process. The following protocol outlines key steps for integrating community engagement:
Pre-trial Community Partnership Development
Collaborative Study Design Phase
Implementation with Ongoing Community Input
Dissemination and Translation
The Anishinaabek Cervical Cancer Screening Study (ACCSS) exemplifies this approach, establishing research agreements with 11 First Nations communities and forming a Community Steering Committee that guided all aspects of the community-randomized controlled trial [27]. This partnership enabled the research team to integrate cultural considerations into trial design while maintaining scientific rigor.
Informed Consent Protocol for Community Settings
Traditional informed consent processes may require adaptation for community-based RCTs. The following protocol provides guidance for ethical consent in community settings:
Consent Format Determination
Information Disclosure Framework
Comprehension Enhancement Strategies
Voluntariness Assurance
In the EMPallA trial, the Study Advisory Committee recommended expanding recruitment to include Spanish-speaking patients and creating patient-friendly materials to enhance comprehension, demonstrating how community input can strengthen consent processes [26].
Table 2: Research Reagent Solutions for Ethical Community-Based RCTs
| Research 'Reagent' | Function | Application Example |
|---|---|---|
| Community Advisory Boards | Provide ongoing input on cultural appropriateness, study design, and implementation challenges [26] [27] | EMPallA trial's SAC provided 41 recommendations, with 63% implemented as IRB modifications [26] |
| Stepped-Wedge Cluster Design | Enables all participants to receive intervention eventually while maintaining methodological rigor [25] | Used in Nen ŨnkUmbi/EdaHiYedo sexual health intervention with Fort Peck Tribes [25] |
| Wait-List Control Design | Addresses ethical concerns about denial of beneficial interventions by delaying rather than withholding treatment [25] | Implemented in Báa nnilah chronic illness self-management study with Apsáalooke community [25] |
| Research Democracy Framework | Ensures all stakeholders have voice and vote in research decisions through structured participatory processes [28] | Nueva Vida Intervention used voting and open communication to engage Latina survivors and caregivers [28] |
| Cultural Mentoring Components | Integrates traditional knowledge and practices into intervention design and implementation [25] | Fort Peck SRH intervention connected youth with elders to discuss traditional beliefs about sexual health [25] |
Visualization of Stakeholder Engagement Framework
The following diagram illustrates the integrated stakeholder engagement process for addressing ethical concerns in community-based randomized controlled trials, synthesizing elements from multiple research approaches:
Stakeholder Engagement in Community RCTs
This framework visualization illustrates the integration of multiple stakeholder perspectives across three research phases, highlighting how investigator, community, and regulator concerns must be balanced throughout the RCT process.
Ethical RCT conduct in community settings requires thoughtful engagement with diverse stakeholder perspectives and adaptation of traditional research approaches to align with community contexts and values. By implementing structured community engagement protocols, adapting informed consent processes, and utilizing innovative trial designs that balance scientific rigor with ethical practice, researchers can address the legitimate concerns of investigators, patients, and regulators while generating valuable evidence to improve community health.
The examples and protocols provided in this application note demonstrate that ethical challenges in community-based RCTs are not insurmountable barriers but rather considerations that, when properly addressed, can strengthen both the scientific validity and community relevance of clinical research. Future methodological development should continue to refine approaches for balancing these complementary priorities across diverse community contexts and research questions.
Implementing Ethically Sound Community RCTs: Designs, Consent, and Oversight
Pragmatic Randomized Controlled Trials (RCTs) are designed to inform real-world clinical and policy decisions by evaluating interventions under usual practice conditions rather than in highly controlled settings [29] [30]. The PRECIS-2 (Pragmatic-Explanatory Continuum Indicator Summary 2) tool provides a framework for designing trials that are "fit for purpose" across nine key domains, helping trialists align design decisions with the intended goal of generating real-world evidence [31] [32]. However, as pragmatic trials operate within routine care settings, they introduce complex ethical challenges that extend beyond those encountered in traditional explanatory trials [29] [30] [23].
This application note explores the integration of ethical considerations into the nine PRECIS-2 domains to support researchers, ethics committees, and drug development professionals in designing ethically sound pragmatic trials within community settings. The ethical framework presented here addresses pressing issues including the blurring of research-practice boundaries, consent modifications in real-world contexts, and the protection of broader participant populations affected by cluster randomization [30] [23].
PRECIS-2 Domains and Corresponding Ethical Considerations
Table 1: Ethical Considerations Mapped to PRECIS-2 Domains
| PRECIS-2 Domain | Ethical Considerations | Recommended Mitigation Strategies |
|---|---|---|
| Eligibility | - Fair participant selection- Avoiding exclusion of vulnerable groups- Competing trials recruiting same population | - Broad inclusion criteria reflecting real-world patients- Transparency about competing studies [29] |
| Recruitment | - Perceptions of clinical care versus research- Potential for coercion in clinical settings- Privacy concerns during identification | - Clear differentiation between research and routine care- Protected time for decision-making [23] |
| Setting | - Variable standards of care across sites- Resource implications for host institutions- Contextual vulnerabilities | - Assessment of site-specific capacity and burdens- Engagement with local gatekeepers [29] [23] |
| Organization | - Expertise and training of personnel- High workload impacts on consent process- Resource constraints in developing countries | - Adequate training for healthcare providers acting as researchers- Monitoring workload and consent quality [29] |
| Flexibility: Delivery | - Variation in intervention fidelity- Differential provider expertise affecting safety- Documentation of modifications | - Clear parameters for acceptable flexibility- Monitoring systems for safety across variations [23] |
| Flexibility: Adherence | - Balancing real-world adherence with safety monitoring- Determining appropriate level of adherence support | - Clear thresholds for intervention in cases of non-adherence- Transparent reporting of adherence support [31] |
| Follow-up | - Privacy concerns with data collection methods- Use of electronic health records without explicit consent- Burden of data collection | - Ethical framework for using routinely collected data- Transparency about data access and use [29] [30] |
| Primary Outcome | - Relevance to patients and communities- Potential conflicts with clinician or payer interests- Use of patient-centered outcomes | - Community engagement in outcome selection- Alignment with patient values and preferences [30] [23] |
| Primary Analysis | - Implications of intention-to-treat analysis- Handling of missing data- Transparency of analytical decisions | - Pre-specified analysis plan- Clear communication of analytical approach including limitations [32] |
Ethical Analysis Framework for Pragmatic Trial Design
Distinguishing Research from Practice
A fundamental ethical challenge in pragmatic trials is the blurred boundary between clinical research and routine practice. As these trials embed research interventions within usual care settings, participants may not recognize they are involved in research, potentially undermining informed decision-making [30] [23]. This ambiguity is particularly pronounced when evaluating usual care interventions or when using exclusively routinely collected data for outcome assessment.
The case study of the Timasamalirana HIV trial in Malawi illustrates this challenge, where research activities were seamlessly integrated into standard antenatal and HIV care pathways [29]. Similar issues arose in the RTS,S/AS01 Malaria Vaccine Implementation, where controversy emerged regarding whether the initiative constituted a pragmatic trial or routine program implementation, raising questions about which activities required ethical review [29].
Protocol Recommendation: Implement a transparent disclosure process that clearly distinguishes research interventions from clinical care, even when they are closely aligned. This should include explicit communication about randomisation, data collection for research purposes, and any deviations from usual care.
Informed Consent Modifications
Traditional informed consent processes may be impractical or inappropriate in some pragmatic trial contexts, potentially compromising the trial's real-world applicability by introducing significant selection bias [30] [23]. Stakeholder interviews with pragmatic trial investigators reveal ongoing ethical debates about when alterations to consent are appropriate, particularly for minimal-risk interventions or when obtaining consent is logistically prohibitive [23].
Table 2: Consent Approaches for Pragmatic Trial Contexts
| Consent Approach | Appropriate Context | Ethical Safeguards |
|---|---|---|
| Traditional Written Consent | Higher-risk interventionsSubstantial deviation from usual careVulnerable populations | - Comprehensive information disclosure- Documented consent- Adequate time for decision-making |
| Verbal Consent | Minimal risk interventionsIntegrated within clinical workflowLow literacy populations | - Scripted information disclosure- Witness to consent process- Documentation in medical record |
| Waiver/Alteration of Consent | Cluster randomizationUse of routinely collected dataMinimal risk research where consent would make trial infeasible | - Research Ethics Committee approval- Community consultation- Post-trial disclosure |
Gatekeeper Engagement and Community Protections
Pragmatic trials frequently employ cluster randomization, where groups rather than individuals are randomized to different interventions. This design raises ethical questions about who constitutes a research participant and what protections are owed to various stakeholders [30] [23]. The Malawi Timasamalirana case study demonstrated the critical role of district research committees in complementing traditional research ethics committees, particularly for trials embedded within healthcare systems [29].
Protocol Recommendation: Engage gatekeepers representing community interests throughout the trial lifecycle, from design through implementation to results dissemination. Gatekeepers should include patient representatives, community leaders, and healthcare system administrators who can advocate for participant and community interests.
Integrated Workflow for Ethical Pragmatic Trial Design
The following diagram illustrates a systematic workflow for integrating ethical considerations into pragmatic trial design using the PRECIS-2 framework:
Diagram 1: Ethics Integration Workflow for PRECIS-2
Table 3: Research Reagent Solutions for Ethical Pragmatic Trial Design
| Tool/Resource | Function | Application Context |
|---|---|---|
| PRECIS-2 Tool | Designs trials along pragmatic-explanatory continuum across 9 domains | Initial trial design and protocol development; communication with stakeholders [31] [32] |
| Ottawa Statement Guidelines | Guidance for ethical design and conduct of cluster randomized trials | Cluster randomized pragmatic trials where groups are randomized [30] |
| CONSORT-PRO Extension | Reporting guidelines for patient-reported outcomes trials | Ensuring transparent reporting of patient-centered outcomes [32] |
| Electronic Health Record Systems | Source of real-world data for outcome assessment | Efficient data collection with minimal participant burden [29] [30] |
| Stakeholder Engagement Framework | Structured approach to involving patients, providers, health systems | Ensuring trial relevance and addressing ethical concerns of all parties [29] [23] |
| Minimal Risk Assessment Tool | Determines level of research risk compared to usual care | Decisions about appropriate consent modifications and oversight level [23] |
Case Study Application: Timasamalirana HIV Trial in Malawi
The Timasamalirana study in Malawi provides a compelling case study of ethical challenges in pragmatic trials within resource-limited settings. This couple-based intervention for HIV-positive women evaluated the impact of partner engagement on viral suppression [29]. The trial demonstrated high pragmatism across multiple PRECIS-2 domains, including broad eligibility criteria, recruitment from routine clinical care, and follow-up aligned with standard antiretroviral therapy visits [29].
Ethical Challenges and Solutions
The implementation encountered several ethical challenges relevant to pragmatic designs:
- Infrastructure and Workload: High patient volumes and inadequate infrastructure created tensions between research and clinical responsibilities, potentially compromising the consent process [29].
- Competing Trials: Multiple pragmatic trials recruiting similar populations at the same facility raised concerns about fair participant selection and informed consent [29].
- Electronic Medical Records: Difficulties accessing EMR systems for research purposes highlighted tensions between efficient data collection and privacy protections [29].
The trial addressed these challenges through continuous monitoring by gatekeepers and active engagement of district research committees to complement the work of research ethics committees [29].
Integrating ethical considerations into PRECIS-2 domains provides a systematic approach to addressing the distinct challenges posed by pragmatic trial designs. By anticipating ethical issues across all trial domains—from eligibility through primary analysis—researchers can maintain the real-world applicability of pragmatic trials while ensuring adequate protection for participants and communities. The frameworks and protocols presented here offer practical guidance for designing ethically sound pragmatic trials that generate evidence relevant to clinical and policy decision-making in community settings.
Future work should continue to develop tailored ethical guidance specific to pragmatic designs, particularly for trials conducted in resource-limited settings and those employing novel methodologies like stepped-wedge cluster randomization or randomized registry trials. Such guidance should emerge from multidisciplinary collaboration including ethicists, trialists, methodologists, and community stakeholders.
Cluster Randomized Trials (CRTs) represent a critical methodological approach in community settings research, where intact groups—rather than individual participants—are randomized to different intervention arms. Also known as cluster-randomized trials, these designs are essential when interventions are naturally applied at a group level, such as in healthcare systems, community health initiatives, or educational programs [33] [34]. The fundamental characteristic of CRTs is that the unit of randomization is a cluster, which could be a geographic community, a hospital, a school, or any other collective entity [35].
The ethical framework for CRTs extends beyond conventional randomized controlled trial ethics due to their unique design characteristics. When clusters rather than individuals are randomized, it introduces complex ethical considerations regarding consent processes, risk-benefit assessments, and protection mechanisms for participants [35]. These challenges are particularly pronounced in community-based research where interventions may affect entire populations, and obtaining individual consent may be logistically challenging or methodologically problematic [23]. Furthermore, the distinction between research and usual care becomes blurred in pragmatic CRTs, necessitating careful ethical scrutiny to ensure participant rights and welfare are protected while generating scientifically valid evidence for community health improvement [23].
Core Methodological Principles and Unit of Intervention
Defining the Unit of Intervention and Inference
In CRTs, the unit of intervention refers to the level at which the study intervention is delivered, while the unit of inference refers to the level at which the study conclusions are directed [35]. These units may operate at different levels, creating methodological and ethical complexities that researchers must carefully navigate.
The table below outlines common relationships between randomization units, intervention units, and inference units in CRTs:
| Randomization Unit | Intervention Unit | Inference Unit | Example |
|---|---|---|---|
| Community | Community policy | Individual | Community-wide health education campaign assessing individual health outcomes [35] |
| Hospital | Healthcare providers | Provider behavior | Educational intervention for staff to reduce test ordering, measuring physician-level outcomes [35] |
| Primary care practice | Individual patients | Individual | Clinic randomization for cancer screening intervention delivered to individual patients [36] |
| Family | Family | Family | Safety advice provided to families, measuring family-level outcomes [35] |
| School | School environment | Individual | School-based nutrition program assessing individual student health metrics [33] |
A crucial consideration in CRT design is determining whether the primary research question targets individual-level effects or cluster-level effects [35]. When inferences are directed at individuals, but randomization occurs at the cluster level, the correlation between individuals within clusters (intra-cluster correlation) must be accounted for in both sample size calculations and analytical approaches [35]. Failure to appropriately identify the unit of inference can lead to invalid conclusions and ethical concerns about potentially misleading research findings [35].
Justifications for Cluster Randomization
Cluster randomization should be employed judiciously, as it introduces methodological complexities and typically requires larger sample sizes than individually randomized trials [36]. The primary justifications for adopting a CRT design include:
- Intervention Nature: When the intervention is inherently delivered at the cluster level (e.g., changes to healthcare policies, environmental modifications, or community-wide health campaigns) [33] [34]
- Contamination Risk: When there is a significant risk that intervention effects could spread from treatment to control participants in individually randomized designs, potentially diluting the observed treatment effect [36] [34]
- Practical Implementation: When logistical considerations make individual randomization infeasible, such as implementing different nursing shift patterns across hospital wards [34]
- Total Effect Assessment: When evaluating both direct and indirect effects of an intervention, particularly relevant in vaccine trials where herd immunity represents an important component of overall effectiveness [36]
The following diagram illustrates the key decision process for determining when cluster randomization is methodologically appropriate:
Ethical Framework and Consent Protocols
Consent Paradigms in Cluster Randomization
The ethical framework for obtaining consent in CRTs is necessarily more complex than in individually randomized trials, requiring consideration of multiple levels of permission and potential waivers [35]. The appropriate consent approach depends on the nature of the intervention, the cluster structure, and the risks involved.
The table below summarizes consent approaches and their applications in different CRT scenarios:
| Consent Type | Definition | When Appropriate | Ethical Safeguards |
|---|---|---|---|
| Individual informed consent | Standard consent obtained from each participant before participation | When individuals are subjected to research interventions that exceed minimal risk [37] | Capacity assessment, comprehensive information disclosure, voluntary participation [37] |
| Cluster-level permission | Consent from cluster representatives or leaders | When interventions are applied at cluster level and individual consent is impracticable [35] | Representation legitimacy, community engagement, individual opt-out options [35] |
| Waiver or alteration of consent | Modification or elimination of standard consent requirements | When research couldn't practicably be conducted without waiver, and risks are minimal [23] | Ethics committee approval, post-enrollment information, public disclosure [23] |
| Integrated consent | Consent process integrated into clinical care pathways | In pragmatic trials where research procedures closely align with usual care [23] | Transparency about research nature, distinction between research and care [23] |
| Proximal consent | Consent obtained from appropriate proxies | When potential participants lack decision-making capacity [37] | Adherence to legal frameworks, assessment of participant assent where possible [37] |
Assessing Capacity and Utilizing Proxies in Vulnerable Populations
Research involving populations with potential cognitive impairment, such as elderly residents in long-term care facilities, requires special ethical considerations [37]. A systematic review of CRTs in residential facilities for older people found that only 8 of 73 trials clearly reported processes for assessing residents' capacity to consent [37].
The following protocol outlines a comprehensive approach to capacity assessment and proxy utilization:
Protocol 1: Capacity Assessment and Proxy Consent Framework
Direct Capacity Assessment
- Implement standardized cognitive assessment instruments (e.g., Mini-Mental State Examination) as initial screening
- Conduct decision-specific capacity assessment by trained staff, evaluating understanding of research participation, risks, benefits, and alternatives
- Document assessment process and findings for each potential participant
Proxy Decision-Making
- Identify appropriate proxy decision-makers according to legal hierarchy (court-appointed guardian, healthcare power of attorney, family members)
- Provide proxies with complete study information equivalent to what competent participants would receive
- Document proxy's relationship to participant and authority to consent
Assent from Participants Lacking Capacity
- Seek affirmative agreement from participants even when they lack capacity for full informed consent
- Monitor for dissent through verbal or behavioral indicators and respect refusal
- Re-evaluate capacity at appropriate intervals, particularly for longitudinal studies
Vulnerable Population Safeguards
- Ensure research ethics committee includes expertise in the specific vulnerabilities of the study population
- Implement additional monitoring procedures for participants who lack capacity
- Consider whether the research question could be addressed in populations able to provide independent consent [37]
Rapid Ethical Assessment for Low-Resource Settings
In low-resource and low-literacy settings, standard consent processes may be inadequate to ensure genuine comprehension. A cluster randomized trial evaluating Rapid Ethical Assessment (REA) demonstrated significant improvements in comprehension scores (73.1% vs. 45.2%) and consent quality (89.1% vs. 78.5%) when REA was implemented [38].
Protocol 2: Rapid Ethical Assessment Implementation
Assessment Planning
- Allocate approximately 6 weeks for REA completion
- Identify key stakeholders: potential participants, community leaders, healthcare providers
- Develop interview and focus group guides addressing ethical concerns specific to the research context
Data Collection
- Conduct semi-structured interviews with stakeholders
- Facilitate focused group discussions to identify community-specific ethical concerns
- Observe community dynamics and decision-making processes
Consent Process Modification
- Revise consent forms based on REA findings: incorporate local terminology, concrete examples, contextual cues
- Modify consent procedures: adjust information delivery methods, timing, and setting
- Train consent administrators in culturally appropriate communication approaches
Evaluation
- Assess comprehension using validated tools (e.g., Modular Informed Consent Comprehension Assessment - MICCA)
- Evaluate quality of consent process (e.g., Quality of Informed Consent - QuIC tool)
- Monitor recruitment and retention rates as indicators of ethical process success [38]
Protection Mechanisms for Research Participants
Balancing Methodological and Ethical Requirements
Protecting participants in CRTs requires special considerations due to the unique design features that distinguish them from individually randomized trials. The following protection mechanisms address common ethical challenges in cluster randomization:
Protocol 3: Comprehensive Protection Framework for CRT Participants
Gatekeeper Engagement
- Identify appropriate "gatekeepers" at cluster level who control access to potential participants
- Clarify gatekeeper role: facilitating access rather than providing proxy consent for individuals
- Document gatekeeper engagement process and any permissions obtained
Dual-Level Risk Assessment
- Evaluate risks at both individual and cluster levels
- Consider potential group harms, including stigma, discrimination, or disruption of social structures
- Implement monitoring plans for both individual and collective risks
Equipoise Evaluation
- Ensure clinical equipoise exists at appropriate level (community, provider, or patient)
- Document genuine uncertainty within expert community regarding comparative benefits of interventions
- Re-evaluate equipoise as evidence accumulates during trial progression
Fair Distribution of Burdens and Benefits
Monitoring and Data Safety Considerations
Effective participant protection in CRTs requires ongoing monitoring throughout the trial lifecycle. The following table outlines key monitoring considerations specific to cluster randomized designs:
| Monitoring Area | CRT-Specific Considerations | Protection Mechanisms |
|---|---|---|
| Data Safety Monitoring | Correlation of outcomes within clusters affects stopping rules | Establish cluster-level monitoring boundaries; consider dependence of observations |
| Interim Analysis | Potential for cluster-level effects to emerge before individual-level effects | Plan interim analyses with appropriate statistical corrections for multiple comparisons |
| Protocol Implementation | Variation in intervention implementation across clusters | Monitor fidelity of intervention delivery at cluster level; assess contextual factors |
| Ancillary Care | Identification of healthcare needs unrelated to research | Establish referral pathways for participants in all clusters, considering varying local resources |
| Compensation for Research-Related Injury | Differential access to healthcare across clusters | Ensure equitable compensation mechanisms regardless of cluster location or resources |
Implementing ethically sound CRTs requires specific methodological tools to address their unique design and analytical challenges. The following table outlines essential resources for researchers:
| Tool/Resource | Function | Application in CRTs |
|---|---|---|
| Intraclass Correlation Coefficient (ICC) | Measures similarity of responses within clusters | Informs sample size calculations; quantifies design effect [35] |
| CONSORT Extension for CRTs | Reporting guidelines for cluster randomized trials | Ensures transparent reporting of cluster-specific methodology [36] |
| PRECIS-2 Tool | Assesses pragmatic versus explanatory design elements | Guides appropriate trial design based on intended application [23] |
| Restricted Randomization | Constrains randomization to achieve balance on key covariates | Improves statistical efficiency when few clusters are available [33] [36] |
| Mixed Effects Models | Statistical approach accounting for hierarchical data structure | Appropriate analysis method for correlated observations within clusters [35] |
| Rapid Ethical Assessment | Brief qualitative assessment of ethical terrain | Improves consent comprehension and process in low-resource settings [38] |
The following diagram illustrates the ethical review workflow for cluster randomized trials, incorporating the unique considerations previously discussed:
Cluster randomized trials present unique ethical challenges that require researchers to carefully balance methodological rigor with robust participant protections. The fundamental consideration is ensuring that the unit of intervention aligns with the scientific question while implementing appropriate consent processes that respect participant autonomy and welfare. This requires moving beyond formulaic applications of informed consent toward context-sensitive approaches that may include cluster-level permissions, waivers, or alterations when scientifically and ethically justified.
The protection of groups and individuals in CRTs demands ongoing vigilance throughout the research lifecycle—from initial design through implementation to dissemination of results. By adopting the frameworks and protocols outlined in this document, researchers can navigate the complex ethical terrain of cluster randomization while generating scientifically valid evidence to improve community health outcomes. As the use of CRTs continues to grow in response to demands for real-world evidence, maintaining this integration of ethical and methodological excellence remains paramount for responsible research conduct.
Within the ethical framework of randomized controlled trials (RCTs) conducted in community settings, the process of obtaining informed consent presents unique challenges. Traditional consent procedures can sometimes hinder otherwise valuable research, particularly in minimal-risk studies or those where full disclosure would compromise the scientific validity [10]. This document provides detailed application notes and protocols for researchers seeking to implement ethically sound waivers or alterations of informed consent, in accordance with federal regulations and institutional policy.
Regulatory Foundations and Criteria
The Common Rule and FDA regulations provide a structured pathway for IRBs to approve changes to the standard informed consent process. These are distinct from a simple waiver of signed documentation and require rigorous justification [39] [40] [41].
The following table summarizes the core regulatory criteria that must be met for an IRB to approve a waiver or alteration of informed consent.
Table 1: Regulatory Criteria for Waivers and Alterations of Informed Consent
| Criterion | Explanation for Researchers | Common Justification Strategies |
|---|---|---|
| Minimal Risk | The probability and magnitude of harm or discomfort anticipated in the research are not greater than those encountered in daily life or during routine physical or psychological examinations [41]. | Detail the specific procedures and argue why each poses no more than minimal risk, often by comparing them to everyday risks or standard clinical care. |
| Impracticability | The research could not practicably be carried out without the waiver or alteration [39] [40]. | Demonstrate that obtaining full consent is logistically prohibitive (e.g., large dataset analysis) or scientifically invalidating (e.g., in deception research). |
| Rights & Welfare | The waiver or alteration will not adversely affect the rights and welfare of the subjects [41]. | Explain how participant anonymity will be protected, how data will be kept confidential, and why the research procedures themselves do not infringe on participant autonomy. |
| Identifiable Information | If using private information or biospecimens, the research could not practicably be carried out without using them in an identifiable format [39]. | Justify why de-identified data is insufficient; for example, a need to link records or return results. |
| Post-Participation Debriefing | Whenever appropriate, subjects will be provided with additional pertinent information after participation [39] [40]. | Provide a debriefing script or plan for informing participants about the true nature of the study after their involvement is complete, especially in deception research. |
Application Notes and Experimental Protocols
Protocol: Implementing a Waiver of Consent for Secondary Data Analysis
This protocol is designed for research involving the analysis of pre-existing, non-public datasets where re-contacting individuals is not feasible.
- Objective: To analyze medical records for trends in diagnostic pathways without obtaining individual consent from patients.
- Materials:
- Data Use Agreement (DUA): A formal agreement with the data holder outlining permitted uses, confidentiality, and security requirements. Function: Ensures regulatory and contractual compliance [39].
- Secure Data Server: A password-protected, encrypted server with access controls for storing the dataset. Function: Protects data confidentiality and integrity.
- Statistical Analysis Software (e.g., R, SAS, Stata): Tools for cleaning, managing, and analyzing the dataset. Function: Enables the execution of the research plan on the quantitative data.
- Methodology:
- IRB Application: In the protocol, explicitly request a waiver of informed consent under 45 CFR 46.116(f) [39].
- Justification: Address each of the five criteria in Table 1. Argue that the research is minimal risk (data is abstract and procedures are non-invasive), impracticable (re-contacting thousands of patients is not feasible), and that rights are protected through robust de-identification and data security measures.
- Data Handling: All direct identifiers (name, address, medical record number) must be removed. A random, reversible code may be retained only if necessary and kept securely separate from the data.
- Analysis: Proceed with the planned analysis on the de-identified dataset.
Protocol: Implementing an Alteration of Consent for Deception Research
This protocol applies to studies where incomplete disclosure or deception is methodologically necessary, such as in certain behavioral RCTs in social psychology or economics [39].
- Objective: To evaluate decision-making biases by providing participants with incomplete information during the initial task.
- Materials:
- Baseline Consent Form: A document that obtains consent for participation while withholding the specific research hypothesis. Function: Maintains ethical standards by obtaining agreement for a known level of risk without biasing the results.
- Experimental Task Materials: The tools or software used for the deceptive intervention.
- Standardized Debriefing Script: A detailed, plain-language explanation of the study's true purpose, the nature of the deception, and the scientific reason for its use. Function: Fulfills the ethical obligation to provide post-participation information and allows for verbal consent to use collected data [40].
- Methodology:
- IRB Application: Request an alteration of the informed consent process, specifically to omit the true hypothesis from the initial consent form [39].
- Justification: Argue that the study is minimal risk (the deception is about a trivial task), that the research is impracticable without the alteration (full disclosure would create expectation bias), and that rights are protected by the comprehensive debriefing procedure.
- Initial Consent: Obtain consent for a described "decision-making study" without revealing the bias being tested.
- Post-Study Debriefing: Immediately after data collection, provide the debriefing script. Explain the deception, apologize for it, and provide the opportunity for participants to withdraw their data from the study.
Workflow Visualization
The following diagram illustrates the logical decision process for determining the appropriate informed consent pathway for a research study, as guided by IRB principles.
Research Reagent Solutions: Essential Materials for Ethical Consent Processes
The following table details key materials and documents essential for implementing robust informed consent processes, including waivers and alterations.
Table 2: Essential Materials for Ethical Consent Processes
| Item | Function in Research | Application Context |
|---|---|---|
| IRB Approval Protocol | Formal document submitted for ethics review detailing study design, risks, benefits, and the proposed consent process. | Required for all non-exempt human subjects research; must explicitly justify any waiver/alteration requests [42]. |
| Altered Consent Form Template | A version of the consent document from which specific elements (e.g., study purpose) have been omitted for scientific reasons. | Used in research approved for an alteration of consent, such as studies involving deception [39] [40]. |
| Debriefing Script & Protocol | A standardized explanation and procedure for informing participants about the true nature of the research after their involvement, especially if deception was used. | Critical for fulfilling ethical obligations in studies with an altered consent process; allows participants to withdraw their data post-study [40]. |
| Letter of Information | A document containing all required consent elements but used when a waiver of documentation (signature) has been granted. | Used in minimal-risk research where the signed form is the only link to the participant, thus waiving signature protects confidentiality [40]. |
| Data Use Agreement (DUA) | A contractual agreement outlining the terms, limitations, and security requirements for using a specific dataset. | Essential for justifying a waiver of consent in secondary data analysis, as it demonstrates formal, controlled access to data [39]. |
Determining Minimal Risk in the Context of Usual Care Interventions
The concept of minimal risk is fundamental to the ethical review of human subjects research, serving as a threshold that determines the level of oversight and the appropriateness of waived or expedited consent procedures. Regulatory guidelines define minimal risk as the state where "the probability and magnitude of harm or discomfort anticipated in the research are not greater in and of themselves than those ordinarily encountered in daily life or during the performance of routine physical or psychological examinations or tests" [43]. This definition becomes particularly complex when applied to pragmatic randomized controlled trials (RCTs) that evaluate usual care interventions—treatments or procedures already accepted by medical experts as appropriate and commonly used by healthcare professionals [6] [44].
In community settings, where research integrates with routine clinical practice, determining minimal risk requires careful consideration of the incremental risks imposed by research activities beyond those inherent in standard care. This assessment is complicated by the blurred distinction between research and practice in pragmatic trials, where study interventions often consist of treatments used routinely in practice, provided by health providers in ordinary clinical settings, with data collected from electronic health records [6]. This application note provides structured guidance for researchers and ethics committees navigating these determinations, with specific protocols for implementing minimal risk assessments in community-based RCTs.
Conceptual Framework and Regulatory Background
The Minimal Risk Standard in Research Ethics
The minimal risk threshold serves as a critical gatekeeper for several ethical safeguards in human subjects research. According to prominent research ethicists, ethical research must fulfill seven requirements, including offering a favorable risk-benefit ratio and undergoing independent review [45]. When research involves minimal risk, it may qualify for expedited review or be deemed exempt from certain regulatory requirements, depending on the jurisdiction and specific nature of the research [45].
A persistent conceptual challenge in applying the minimal risk standard has been determining whose "daily life" serves as the appropriate comparator. Early interpretations varied between a general population standard (based on the daily life of an average healthy person) and a population-specific standard (based on the daily lives of the research subjects themselves) [43]. A consensus has developed that the population-specific approach should be rejected because it can result in an unjust distribution of risks, permitting individuals to be exposed to higher levels of risk simply because their daily lives are filled with greater risk than healthy individuals or those living in safe environments [43].
Usual Care Interventions in Pragmatic Trials
Pragmatic RCTs are designed to evaluate the effectiveness of interventions in real-world clinical conditions, contrasting with explanatory trials that seek to establish efficacy in ideal, controlled circumstances [6]. These trials frequently employ usual care control groups, which aim to reflect typical, normative non-study care [44]. The terminology varies across studies, with designations including Treatment as Usual (TAU), Usual Care (UC), Standard Care (SC), or Routine Care (RC) [44].
Table 1: Types of Existing Practice Control Groups in Behavioral Trials
| Condition | Description | Stringency | Uniformity |
|---|---|---|---|
| Naturalistic Inadequate Care (IC) | Inaccessible or poor quality non-study care | Low | Trial-dependent |
| Treatment As Usual (TAU) | Typical, normative non-study care | Moderate | Trial-dependent |
| Standard of Care (SOC) | State-of-the-art, guideline-adherent non-study care | High | Low to High |
| Enhanced Usual Care (EUC) | Usual care systematically improved by research protocol | Moderate to High | Trial-dependent |
Variants on usual care include Enhanced Usual Care (EUC), where usual care is systematically improved by the research protocol to overcome ethical or methodological problems, and Constrained Usual Care (CUC), where specific aspects of usual non-study care are withheld or discouraged during the trial [44]. The degree of enhancement can range from minimal to extensive, with more extensive enhancement making the intervention less representative of routine care and more resembling an experimental intervention in its own right [44].
Risk Assessment Framework for Usual Care Interventions
Incremental Risk Assessment Methodology
When evaluating minimal risk in usual care interventions, the focus must be on incremental risks—those risks that research participation adds beyond the risks of usual clinical care and daily life [6]. The assessment requires systematic evaluation of both the probability and magnitude of potential harms across multiple domains.
Table 2: Domains of Risk in Usual Care Intervention Research
| Risk Domain | Incremental Risk Considerations | Assessment Methodology |
|---|---|---|
| Physical Risks | Risks beyond those of the usual care intervention itself; includes device-related risks for wearable sensors [45] | Comparison to risks of daily life; expert review of device biocompatibility |
| Psychological Risks | Stigma, labeling, emotional distress from study participation | Evaluation of interview protocols, survey instruments, and assessment procedures |
| Social Risks | Breach of confidentiality, privacy violations, community stigmatization | Data protection plan review, community consultation |
| Economic Risks | Financial costs of participation, insurance implications, opportunity costs | Analysis of participant compensation, time requirements, and cost disclosures |
For research involving wearable health devices and other minimal-risk technologies, even seemingly harmless sensors require careful assessment. For example, wet adhesives used in on-skin sensors involve chemicals that can irritate the skin or cause allergic reactions, necessitating review of their material safety [45]. The assessment must consider not only immediate physical risks but also potential psychological, social, and economic risks [45].
Protocol for Determining Minimal Risk in Community Settings
Objective: To provide a standardized methodology for determining whether research involving usual care interventions meets the minimal risk threshold in community settings.
Materials:
- Research protocol document
- Description of usual care interventions
- Data collection instruments
- Community engagement framework
- Risk classification matrix
Procedure:
Characterize the Usual Care Intervention
- Document the standard clinical procedures that constitute usual care for the condition
- Identify the known risks and discomforts associated with these procedures
- Establish the frequency and severity of adverse events in routine practice
Identify Research Procedures
- List all procedures, assessments, and data collection activities that are purely research-related
- Determine which activities are part of both clinical care and research
- Document the timing, frequency, and intensity of each research procedure
Assess Incremental Risks
- For each research procedure, evaluate the probability and magnitude of harm
- Compare these risks to those "ordinarily encountered in daily life" using the general population standard
- Consider both the absolute level of risk and the incremental increase over standard care
Evaluate Risk Distribution
- Assess whether risks are distributed fairly across participant groups
- Identify any vulnerable subpopulations that may experience different risk levels
- Ensure the research does not unjustly expose participants to higher risks based on pre-existing conditions or environmental factors
Document the Determination
- Create a detailed rationale for the minimal risk classification
- Specify any procedures that require additional safeguards despite overall minimal risk designation
- Submit to Research Ethics Committee for review and confirmation
Workflow for Minimal Risk Determination
Ethical Considerations and Community Applications
Consent Requirements in Minimal Risk Usual Care Research
The majority of ethics scholars question whether traditional informed consent is always needed in pragmatic RCTs involving minimal risk interventions [6]. According to international guidelines, a research ethics committee may grant a waiver of consent when risks to study participants are minimal, the research has important social value, and requiring consent would render the study infeasible [6]. These conditions commonly apply to pragmatic RCTs evaluating usual care interventions [6].
When consent is required, most authors agree that detailed information about the trial need only be disclosed when research participation involves incremental risks compared to clinical practice [6]. There is disagreement among ethicists about whether randomization must always be disclosed in minimal risk usual care research, with some arguing that disclosure is essential to respect autonomy, while others contend that it may be omitted when the risks are minimal and disclosure would compromise study validity [6].
In community-based research, additional consent considerations emerge. For research testing interventions affecting entire communities, consent may be waived when: (I) research participants are at minimal risk; (II) obtaining individual consent would not be practicable; and (III) the ethics committee has determined that waiving consent does not increase the risk of harm to participants [46]. In such cases, community engagement through meetings, awareness campaigns, and open communication channels with researchers becomes essential to ethical conduct [46].
Community Engagement Protocol for Minimal Risk Research
Objective: To establish procedures for meaningful community engagement in minimal risk usual care research, particularly when individual consent may be waived.
Materials:
- Community profile and leadership directory
- Engagement meeting materials
- Communication plan template
- Feedback mechanism framework
Procedure:
Community Mapping
- Identify formal and informal community leaders
- Map existing community structures and advisory groups
- Determine appropriate communication channels
Stakeholder Consultation
- Present research objectives, methods, and potential benefits
- Explain the minimal risk determination and rationale for waived consent (if applicable)
- Solicit feedback on research design and implementation plans
Ongoing Communication
- Establish regular updates to the community throughout the research process
- Provide accessible mechanisms for questions and concerns
- Maintain transparency about study progress and findings
Results Dissemination
- Share research findings with the community in accessible formats
- Acknowledge community contributions to the research
- Discuss implications for ongoing practice and policy
Regulatory Oversight and Implementation Tools
Research Ethics Committee Review Procedures
There is consensus that oversight by Research Ethics Committees (RECs) or Institutional Review Boards (IRBs) is often time-consuming, costly, and complex, potentially impeding valuable research [6]. Many authors argue that existing oversight procedures should be streamlined for minimal risk pragmatic RCTs, with some advocating for a wholly new system of oversight [6].
Protocols for minimal risk research may undergo different levels of review depending on specific aspects of the study's design and risk profile. In the United States, for example, there are three main designations: exempt research, expedited review, and full committee review [45]. Research that involves minimal risk and includes only behavioral research may be deemed exempt from federal regulations, while research involving minimal risk that doesn't meet exemption requirements may qualify for expedited review [45]. Importantly, researchers themselves do not determine the appropriate level of review; this assessment is made by the committee after protocol submission [45].
Table 3: Essential Documentation for Minimal Risk Determination
| Documentation Element | Purpose | REC Review Focus |
|---|---|---|
| Detailed Risk Assessment Matrix | Systematically compares research risks to daily life risks | Completeness of risk identification; appropriateness of comparators |
| Justification for Waived or Altered Consent | Explains why traditional consent is not required or practicable | Alignment with regulatory criteria; adequacy of alternative protections |
| Community Engagement Plan | Demonstrates efforts to involve affected communities | Appropriateness of engagement methods; inclusiveness of stakeholders |
| Data Safety Monitoring Plan | Outlines procedures for identifying unanticipated risks | Feasibility of monitoring approach; threshold for stopping rules |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Implementing Minimal Risk Usual Care Research
| Tool Category | Specific Instruments | Function in Minimal Risk Research |
|---|---|---|
| Risk Assessment Tools | PRECIS-2 tool, Risk Classification Matrix | Helps characterize the pragmatic nature of trials and systematically evaluate potential harms |
| Community Engagement Frameworks | Community Advisory Boards, Stakeholder Meeting Guides | Facilitates appropriate community involvement, particularly when individual consent may be waived |
| Data Collection Instruments | Wearable Sensors, Electronic Health Record Interfaces, Patient-Reported Outcome Measures | Enables efficient data collection with minimal participant burden in usual care settings |
| Regulatory Documentation Templates | SPIRIT 2025 Checklist, Protocol Templates, REC Submission Packages | Ensures complete protocol reporting and facilitates efficient ethics review [47] |
| DC-CPin7 | DC-CPin7|CBP Bromodomain Inhibitor|For Research Use | DC-CPin7 is a potent CBP bromodomain inhibitor (IC50 = 2.5 µM). For Research Use Only. Not for human or veterinary diagnosis or therapeutics. |
| YG1702 | YG1702|ALDH18A1 Inhibitor|For Research | YG1702 is a potent, specific ALDH18A1 inhibitor for cancer research. It attenuates growth in MYCN-amplified neuroblastoma models. For Research Use Only. Not for human use. |
Determining minimal risk in the context of usual care interventions requires a sophisticated understanding of both regulatory standards and clinical reality. The framework presented in this application note emphasizes incremental risk assessment focused on the additional risks imposed by research activities beyond those inherent in standard care and daily life. As pragmatic clinical trials continue to grow in importance for evaluating real-world clinical effectiveness, appropriate minimal risk determinations will be essential for balancing the ethical imperative to protect research participants with the social value of generating evidence to improve healthcare delivery and outcomes.
The protocols and tools provided here offer a structured approach for researchers and ethics committees navigating these complex determinations, with particular attention to community settings where research and practice increasingly intersect. Proper implementation of these guidelines will support the ethical conduct of socially valuable research while maintaining appropriate protections for individuals and communities participating in usual care intervention studies.
Streamlining Research Ethics Committee Oversight for Low-Risk Pragmatic Trials
Application Note: Rationale and Framework for Streamlined Oversight
The Ethical Challenge in Pragmatic Trial Oversight
Pragmatic Randomized Controlled Trials (RCTs) are designed to evaluate the effectiveness of interventions in real-world clinical conditions, contrasting with explanatory trials that test efficacy under ideal, controlled circumstances [6]. The fundamental ethical challenge stems from applying oversight frameworks developed for explanatory RCTs to pragmatic designs, creating significant operational burdens. Research Ethics Committees (RECs) frequently perceive existing ethical and regulatory frameworks as substantial obstacles to the design, review, and conduct of pragmatic RCTs [6]. This misalignment creates inefficiencies that can delay socially valuable research aimed at improving routine care.
Traditional research oversight requires REC review to ensure fair participant selection, favorable risk-benefit balance, and informed consent. However, pragmatic RCTs often involve treatments used routinely in practice, delivered by typical health providers in ordinary clinical settings, with data collected from electronic health records [6]. These fundamental differences have prompted ethical debates about whether novel ethical frameworks are required and whether REC review and informed consent are necessary for all pragmatic trials [6].
Quantitative Evidence of Oversight Challenges
Table 1: Key Findings on Ethical Challenges in Pragmatic RCTs from Literature Review (2012-2017)
| Ethical Theme | Percentage of Publications Addressing Theme | Key Findings from Content Analysis |
|---|---|---|
| Research-Practice Distinction | 86% (31/36 articles) | Majority rejected relevance of traditional distinction for pragmatic RCTs [6] |
| Consent Requirements | 81% (29/36 articles) | Most questioned need for traditional consent when risks are low and consent impractical [6] |
| Consent Disclosure Elements | 64% (23/36 articles) | Agreement that only incremental risks versus clinical practice need disclosure [6] |
| REC Oversight Burden | 100% (36/36 articles) | Consensus that oversight is time-consuming, costly, and impedes research [6] |
Source: Adapted from BMC Medical Ethics review of 36 articles on ethical issues in pragmatic RCTs [6]
The multifaceted oversight process is particularly challenging for multisite research where each site independently completes all required local reviews [48]. The lack of inter-institutional standardization frequently results in different review outcomes for the same protocol, delaying study operations from initiation through completion [48]. Data from empirical studies demonstrate that variability in REC decision-making and interpretation of regulations across institutions contributes significantly to problems reviewing multisite research [48].
Protocol for Streamlined Ethics Review of Low-Risk Pragmatic Trials
Centralized Ethics Review Implementation
Protocol Objective: Establish a standardized framework for using central institutional review boards (IRBs) for multisite pragmatic RCTs classified as low-risk.
Background and Rationale: While the use of a central IRB for multisite research has been proposed as a remedy to oversight inefficiencies, this approach alone does not address the larger problem of completing non-IRB institutional reviews in addition to IRB review—and coordinating the interdependence of these reviews [48]. A comprehensive streamlining approach must address both procedural and organizational issues while maintaining protection of human subjects as the paramount concern [48].
Eligibility Criteria for Streamlined Review:
- Interventions involve routine clinical treatments with established safety profiles
- Study procedures pose minimal incremental risk beyond usual clinical care
- Protocol employs broad eligibility criteria mirroring real-world patient populations
- Primary data collection utilizes routinely collected clinical data or electronic health records
- Waiver or alteration of informed consent is scientifically and ethically justified
Table 2: Oversight Streamlining Protocol for Multisite Pragmatic RCTs
| Review Component | Traditional Approach | Streamlined Approach | Implementation Guidelines |
|---|---|---|---|
| Ethics Review Mechanism | Local IRB review at each site | Single central IRB of record | Use mandated central IRB for federally-funded trials; voluntary adoption for others [48] |
| Informed Consent Process | Comprehensive written consent for all trials | Targeted consent approaches based on risk | Implement waiver/alteration of consent when risks are minimal and consent impractical [6] |
| Institutional Reviews | Sequential, uncoordinated IRB and institutional reviews | Harmonized institutional review requirements | Develop reciprocity agreements for institutional approvals; standardized facility questionnaires |
| Oversight Coordination | Separate review of interdependent elements | Integrated review of protocol and institutional feasibility | Pre-review feasibility assessment; coordinated reliance agreements between institutions |
Risk Assessment and Tiered Oversight Framework
A critical component of streamlined oversight involves implementing risk-proportionate review processes. The following workflow diagram outlines a decision pathway for determining the appropriate level of REC oversight for pragmatic trial protocols:
Risk Assessment Criteria:
- Minimal Risk: Interventions and procedures that do not exceed risks encountered in routine clinical management for the condition being studied
- Incremental Risk: Any research procedures that exceed usual care and present more than minimal risk to participants
- Consent Assessment: Determination of whether traditional informed consent, simplified consent, or waiver of consent is appropriate based on risk level and practical constraints
Stakeholder Engagement and Embedded Ethics Approach
Empirical research with stakeholders reveals that effective ethical oversight requires understanding participant experiences and concerns throughout the trial lifecycle [49]. The implementation of embedded, real-time research ethics approaches can support participants and research teams by addressing challenges as they arise during trial conduct [49].
Key Considerations for Stakeholder Engagement:
- Participant Concerns: Common issues include anxieties, mistrust of researchers, rumors, fears of exploitation, and misconceptions about research purposes [49]
- Support Mechanisms: Establish anonymous reporting channels for participant concerns and responsive communication strategies
- Continuous Consent: Implement processes for ongoing participant understanding and voluntary participation throughout the trial
Research Reagent Solutions for Ethical Oversight
Table 3: Essential Methodological Tools for Ethical Pragmatic Trial Design
| Research Reagent | Primary Function | Application in Pragmatic Trials |
|---|---|---|
| PRECIS-2 Tool | Trial design matching to purpose | Helps align trial design decisions along pragmatic-explanatory continuum across 9 domains [50] |
| Central IRB Agreements | Standardized ethics review | Reduces duplication and inconsistencies in multisite research oversight [48] |
| Electronic Health Record Systems | Routine clinical data collection | Enables efficient outcome assessment with minimal research-specific procedures [6] |
| Risk-Proportionate Consent Frameworks | Participant informed consent | Guides appropriate consent approaches (traditional, simplified, or waiver) based on risk level [6] |
| Embedded Ethics Assessment | Real-time ethical monitoring | Identifies and addresses participant concerns during trial conduct [49] |
Implementation Workflow for Streamlined Oversight
The following diagram illustrates the integrated workflow for implementing streamlined REC oversight from protocol development through ongoing review:
This structured approach to streamlining research ethics oversight for low-risk pragmatic trials maintains rigorous human subjects protections while reducing unnecessary administrative burdens. By implementing risk-proportionate review, centralized ethics review processes, and embedded ethics monitoring, researchers and RECs can facilitate the efficient conduct of socially valuable pragmatic research that generates evidence to improve routine clinical care.
Integrating rigorous research, such as randomized controlled trials (RCTs), into the dynamic environments of community pharmacies and clinics presents unique project management and ethical challenges. A defining feature of research in these settings is the complex network of stakeholders, each with the power to significantly facilitate or hinder a project's success [51]. Effective stakeholder engagement is not merely an ethical imperative to ensure community-centric research; it is a critical strategic function that can determine the ultimate feasibility, relevance, and impact of a study [52] [53]. This article provides practical application notes and protocols for managing projects and engaging stakeholders within the specific ethical context of community-based RCTs, offering researchers a structured approach to navigating this complex landscape.
Core Principles and Ethical Foundations
The ethical foundation of RCTs in community settings often hinges on the concept of equipoise—a genuine uncertainty within the expert medical community about the preferred treatment or intervention [10]. This uncertainty helps to justify randomizing participants to different study arms. However, in social and clinical settings, this principle can conflict with a researcher's or clinician's duty of care, creating genuine moral conflicts [10]. For instance, a community pharmacist might feel a professional obligation to provide what they believe is the best available service to all patients, making it difficult to withhold a potentially beneficial intervention from a control group.
Stakeholder engagement serves as a critical mechanism for navigating this ethical tension. By involving patients, providers, and community leaders from the outset, researchers can:
- Enhance Social Value: Ensure that the research question addresses the real-world needs and priorities of the community, thereby justifying the research endeavor [52].
- Validate Equipoise: Community input can help confirm whether genuine uncertainty about the best approach exists in the practice setting [10].
- Mitigate Ethical Pitfalls: Proactive engagement can help identify and plan for potential ethical issues, such as perceived coercion within tight-knit community groups or threats to participant privacy [54].
Stakeholder Identification and Analysis: The COSMOS Framework
The first practical step is a systematic stakeholder analysis. We recommend adapting the Contextual and Organizational Support Mapping of Stakeholders (COSMOS) model, a visualization tool developed for healthcare implementations [51].
Application Protocol: Conducting a COSMOS Analysis
Objective: To identify all relevant stakeholders, understand their relationships, and assess their support level and criticality to the project's success.
Materials: Whiteboard, digital drawing software, or presentation tools.
Steps:
- List Stakeholders: Brainstorm all individuals, groups, and organizations that can affect or are affected by the research project. For a community pharmacy trial, this typically includes:
- Patients/Service Users: The end-users of the intervention.
- Provider Community: Community pharmacists, pharmacy owners/managers, general practitioners, nurses, and specialist physicians [55] [56].
- Leadership & Government: Senior Medicaid/agency leadership, the Governor's office, State legislatures, and Centers for Medicare & Medicaid Services (CMS) for publicly funded programs [55].
- Regulators & Payers: Entities that control medicine distribution and reimbursement [57].
- Advocacy Groups: Patient advocacy organizations and professional bodies (e.g., Royal Pharmaceutical Society) [56].
- Research Team & IT Support: Key for studies involving electronic health record modifications [51].
Map Organizational Relationships: Create an organizational chart displaying the formal and informal reporting relationships between these stakeholders.
Assess Support and Criticality: For each stakeholder on the map, indicate:
- Level of Support: Use a color code (e.g., Green = Supporter, Yellow = Neutral, Red = Opponent).
- Criticality: Use border thickness to denote how essential the stakeholder is to project success (e.g., Thick border = Critical, Thin border = Non-critical).
Table 1: COSMOS Color and Border Conventions
| Visual Element | Meaning | Application Example |
|---|---|---|
| Green Fill | Supportive Stakeholder | A pharmacy owner who champions the study. |
| Red Fill | Opposing Stakeholder | A physician concerned about workflow disruption. |
| Thick Border | Critical to Success | The Head of Pharmacy commissioning services. |
| Thin Border | Lower Criticality | A third-party software vendor. |
Visualization: COSMOS Diagram for a Pharmacy-Based RCT
The following diagram illustrates a hypothetical COSMOS map for an RCT implementing a new screening service in community pharmacies.
Diagram 1: COSMOS for a pharmacy RCT. Node color indicates support (Green=Supportive, Yellow=Neutral, Red=Opposed). Border thickness indicates criticality (Thick=High, Thin=Low).
Engagement Strategies and Co-Design Protocols
After mapping stakeholders, the next step is active engagement. The goal is a bidirectional process where stakeholders are not merely informed but collaborate in decision-making [52].
Identifying and Utilizing Champions
Application Note: Program "champions" are stakeholders who are actively involved and influential among their peers and are invaluable for building sustainability and managing expectations [55].
Protocol:
- Identification: Find champions through meetings with providers interested in the program or via existing advisory groups (e.g., a Physician Advisory Group) [55].
- Engagement: Provide champions with preliminary evaluation results and solicit their feedback on program refinement. In one example, Wyoming piloted an electronic health record with providers identified as champions to gather feedback on usability and billing [55].
- Empowerment: Allow champions to act as ambassadors to their peers and to other stakeholder groups, leveraging their credibility to build broader support.
The Co-Design Protocol for Intervention Development
A powerful method for ensuring an intervention is relevant and feasible is to co-design it with stakeholders. The following protocol is adapted from a study that developed a community pharmacy service for atrial fibrillation screening [58].
Objective: To collaboratively design a research intervention or service model that is acceptable, feasible, and addresses the real needs of end-users.
Workflow Overview:
Diagram 2: Three-phase co-design protocol.
Detailed Methodology:
Step 1: Exploring the Views of Potential Service Users
- Method: Conduct a focus group and/or semi-structured interviews with potential end-users (e.g., patients over 65 with hypertension for an AF screening trial) [58].
- Goals:
- Explore their knowledge, concerns, and needs regarding the health condition.
- Understand their experiences with existing health services and monitoring.
- Gauge their opinions about the community pharmacist's role and a hypothetical new service.
- Outcome: A qualitative thematic analysis of user needs that directly informs the preliminary model for the next step.
Step 2: Delineating a Preliminary Model of the Service
- Method: Conduct a 4.5-hour focus group with a mixed group of 8-10 stakeholders, including a service user from Step 1, community pharmacists, physicians, specialist nurses, and representatives from relevant health foundations [58].
- Goals: Sequentially discuss and define:
- The target population for the service.
- The service components (e.g., patient education, self-monitoring, referral pathways, follow-up).
- The circumstances that could enable or hinder implementation.
- Outcome: A collaboratively generated, preliminary model of the service or intervention.
Step 3: Initial Assessment of Feasibility and Appropriateness
- Method: Conduct a 2-hour focus group with community pharmacy owners and managers [58].
- Goal: Present the co-designed model from Step 2 and explore its feasibility, appropriateness, and professional/economic implications from a business perspective.
- Outcome: A refined service model that has been vetted for practical implementation within the constraints of the community pharmacy setting.
The Scientist's Toolkit: Key Research Reagents for Stakeholder Engagement
Beyond conceptual frameworks, successful engagement requires practical "reagents" or tools. The following table details essential materials for designing and executing a robust stakeholder engagement strategy.
Table 2: Essential Reagents for Effective Stakeholder Engagement
| Research Reagent | Function & Application | Specific Examples from Literature |
|---|---|---|
| Stakeholder Register | A document capturing relevant information about identified stakeholders, including their interests, expectations, and level of influence. | Key output from the "Identify Stakeholders" process in PMI guidelines [52]. |
| Stakeholder Focus Group Guide | A semi-structured script used by a facilitator to elicit detailed opinions and experiences from a group of stakeholders. | Used to explore patient needs in AF study and provider input in Washington state [58] [55]. |
| Communication Plan | A strategy for regular, two-way communication with different stakeholder groups, defining messages, channels, and frequency. | North Carolina maintained support via websites, annual reports, and a two-page "At-A-Glance" document [55]. |
| Advisory Group Structure | A formalized group (e.g., Physician Advisory Group, Clinical Advisory Committee) that provides ongoing input on policy, design, and evaluation. | Iowa's standing clinical advisory committee and North Carolina's Physician Advisory Group [55]. |
| Qualitative Data Analysis Software | Software used to manage, code, and thematically analyze qualitative data from interviews and focus groups. | The atrial fibrillation study used NVivo for inductive thematic analysis [58]. |
| Pfkfb3-IN-2 | PFKFB3-IN-2|PFKFB3 Inhibitor | |
| HDAC1-IN-7 | HDAC1-IN-7|HDAC Inhibitor | HDAC1-IN-7 is a Chidamide impurity for cancer research. This product is for Research Use Only and not for human or diagnostic use. |
Managing Expectations and Communication
Continuous communication is vital to secure and maintain stakeholder support, particularly when sharing outcomes that may impact perceptions of the RCT's success or ethical standing.
Application Notes:
- Tailor the Message: Different stakeholder groups value different outcomes. Providers and consumer groups may be interested in standardized clinical measures, while the legislature is likely focused on cost savings [55]. Share early outcomes that each group would define as a "success."
- Communicate Early and Often: Regular updates, even in the absence of final results, help manage expectations and build long-term support. Program staff can serve as the key contact to ensure stakeholders receive consistent and correct information [55].
- Be Transparent: Share both program successes and failures. This builds credibility and allows for collective problem-solving, which is essential for maintaining trust throughout a trial, especially when ethical challenges arise [54].
The successful management of research in community pharmacies and clinics hinges on a paradigm that views stakeholder engagement not as an administrative hurdle, but as the core of the project's methodology and ethical justification. By systematically identifying stakeholders through tools like COSMOS, actively involving them in co-design processes, and maintaining transparent communication, researchers can navigate the complex ethical terrain of RCTs in these settings. This approach enhances the scientific promise of the research by ensuring it is grounded in real-world needs and increases the likelihood that successful interventions will be sustainable and effectively integrated into practice long after the trial has concluded.
Solving Common Ethical Dilemmas in Community Trial Implementation
The placebo-controlled, double-blind, randomized clinical trial (RCT) remains the historical gold standard for pharmaceutical medical research, serving as the foundation for evidence-based medicine and regulatory approval of new interventions [59]. This design enables researchers to isolate the specific physiological effects of an investigational treatment from non-specific healing factors, including the psychological placebo effect, natural history of the disease, and regression to the mean [60] [61].
The fundamental ethical tension arises when the scientific requirement for methodological rigor conflicts with physician-investigators' ethical duty to provide optimal patient care, particularly in serious or critical medical conditions. This creates what bioethicists term "therapeutic misconception" - a false belief among participants that the primary purpose of clinical research is therapeutic rather than generating knowledge for future patients [21]. This application note examines this ethical dilemma and provides frameworks for the ethical implementation of placebo controls in community-based research settings.
Ethical Frameworks and Justifications
Core Ethical Considerations
The ethics of placebo use in clinical trials involves balancing multiple competing principles. The following table summarizes the primary ethical considerations and their implications for trial design:
Table 1: Ethical Framework for Placebo-Controlled Trials
| Ethical Principle | Definition | Application to Placebo Controls |
|---|---|---|
| Social Value | Research must produce socially valuable knowledge to justify resources and risks [62]. | Placebo arms must yield scientifically necessary data to address significant health burdens. |
| Clinical Equipoise | Genuine uncertainty in the expert medical community about comparative therapeutic merits of trial arms [21] [62]. | Placebo use requires genuine uncertainty whether the experimental treatment is superior to no specific treatment. |
| Favorable Risk-Benefit Ratio | Potential benefits must justify risks to participants [62]. | Risks of receiving placebo rather than active treatment must be reasonable and adequately managed. |
| Informed Consent | Participants must understand research nature, risks, benefits, and alternatives [59]. | Clear explanation of randomization, placebo use, and available alternatives outside the trial. |
| Standard of Care | Medical care consistent with prevailing professional standards in the participant's context [62]. | Placebo may be justified when it reflects actual local standard care, even if superior treatment exists elsewhere. |
Regulatory Guidelines and Positions
International guidelines provide specific conditions under which placebo controls are ethically acceptable, even when effective treatments exist:
The Declaration of Helsinki states placebo use is acceptable "where for compelling and scientifically sound methodological reasons the use of any intervention less effective than the best proven one, the use of placebo, or no intervention is necessary to determine the efficacy or safety of an intervention and the patients who receive any intervention less effective than the best proven one, placebo, or no intervention will not be subjected to additional risks of serious or irreversible harm as a result of not receiving the best proven intervention" [21].
The Council for International Organizations of Medical Sciences (CIOMS) guidelines permit placebo when: no effective intervention exists; withholding established intervention exposes subjects to temporary discomfort only; using established intervention as comparator wouldn't yield reliable results without adding serious harm risk [21].
Experimental Design and Methodology
Placebo-Controlled Trial Designs
Several methodological approaches can help balance scientific and ethical requirements in placebo-controlled trials:
Table 2: Placebo-Controlled Trial Designs and Applications
| Trial Design | Description | Ethical Advantages | Methodological Considerations |
|---|---|---|---|
| Add-on Design | Placebo versus experimental treatment added to standard background care [59]. | All participants receive established effective therapy. | Tests specific incremental benefit of new intervention. |
| Three-Arm Design | Investigational drug, active comparator, and placebo [59]. | Provides direct comparison to both placebo and standard treatment. | Requires larger sample size; complex statistical analysis. |
| Randomized Withdrawal | Participants receive active treatment then randomized to continue or switch to placebo. | Limits placebo exposure duration; identifies treatment maintenance effect. | Only applicable to certain chronic conditions. |
| Early Escape | Protocol allows switching from placebo to active treatment if predefined criteria met. | Prevents prolonged exposure to ineffective treatment. | May complicate assessment of primary endpoints. |
Figure 1: Placebo-Controlled Trial Workflow with Ethical Safeguards
Enhanced Informed Consent Protocol
The informed consent process is crucial for ethical placebo implementation. Research indicates approximately 50% of participants in RCTs have incomplete understanding of one or more consent components [59]. The following enhanced consent methodology has demonstrated improved participant comprehension:
Protocol: Enhanced Informed Consent for Placebo-Controlled Trials
- Objective: Ensure participants understand key study elements, particularly randomization, placebo use, and therapeutic alternatives
- Materials: Study information document, consent form, visual aids, comprehension assessment tool
Procedure:
- Pre-Consent Preparation: Provide study information at least 24 hours before consent discussion
- Structured Discussion: Cover study purpose, procedures, random assignment, placebo explanation, risks/benefits, alternatives to participation, right to withdraw
- Quantitative Benefit Disclosure: Clearly state potential outcomes for each study arm (e.g., "40% improvement with placebo control vs. 65% with individualized care") [59]
- Placebo Explanation: Define placebo beyond "sugar pill"; explain purpose and placebo/nocebo effects [59]
- Comprehension Assessment: Use teach-back method or structured questionnaire to verify understanding
- Documentation: Obtain written consent with witness present
Quality Control: Monitor consent process; assess therapeutic misconception; document consent discussions
Case Studies in Placebo Implementation
Metformin Aneurysm Trial (MAT)
The MAT trial provides a contemporary example of ethically justified placebo use in a serious medical condition:
Background: Abdominal aortic aneurysm (AAA) is a life-threatening condition with no established drug therapy to prevent progression or rupture. Observational studies suggested metformin might reduce AAA growth [63].
Ethical Justification:
- No proven effective pharmacological intervention exists
- Clinical equipoise regarding metformin's efficacy for AAA
- Surgical repair remains available for all participants if thresholds met
- Placebo group reflects current standard care (monitoring until surgical threshold)
Methodological Safeguards:
- 6-week active run-in phase to identify and exclude metformin-intolerant participants before randomization
- Careful monitoring with predefined criteria for surgical intervention
- Large international sample to ensure adequate power [63]
IMPROV Primaquine Antirelapse Trial
This malaria trial illustrates ethical placebo use in infectious diseases in resource-limited settings:
Background: Plasmodium vivax malaria requires radical cure of both blood stages and dormant liver stages (hypnozoites). Primaquine is the only available hypnozoitocidal drug but has uncertain efficacy and significant toxicity risks [62].
Ethical Justification:
- Placebo necessary to distinguish relapse from reinfection in endemic areas
- Actual standard of care in many participating regions does not include primaquine
- Clinical equipoise exists between primaquine regimens and placebo in specific contexts
- Social value significant due to substantial malaria burden [62]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Research Reagent Solutions for Placebo-Controlled Trials
| Reagent/Material | Function | Ethical Considerations |
|---|---|---|
| Matched Placebo | Physically identical inactive version of investigational product | Must be indistinguishable from active treatment while containing no active ingredients; requires careful manufacturing documentation |
| Active Comparator | Established effective treatment for active-control designs | Selection should reflect "best proven" therapy unless scientifically justified otherwise; requires evidence of comparable efficacy to standard |
| Blinding Materials | Opaque packaging, identical labeling systems | Maintains allocation concealment; prevents unintentional unblinding; essential for objective outcome assessment |
| Randomization System | Computer-generated allocation sequences with stratification | Must ensure unpredictable assignment; typically managed by independent third party to prevent selection bias |
| Unblinding Procedure | Emergency code-break system for clinical emergencies | Must be immediately accessible for clinical care while minimizing unnecessary unblinding; requires clear activation criteria |
| Data Monitoring Committee | Independent expert committee reviewing interim data | Protects participant safety and trial integrity; makes recommendations about continuation based on emerging benefit-risk profile |
| 2,5-Dimethylphenyl 10-undecenoate | 2,5-Dimethylphenyl 10-Undecenoate|High-Purity Research Chemical | 2,5-Dimethylphenyl 10-undecenoate is a high-purity chemical for research, such as synthesizing chiral selectors. This product is for laboratory research use only (RUO) and is not for human or veterinary use. |
Community-Based Research Considerations
Implementing placebo-controlled trials in community settings presents distinctive challenges and opportunities:
Protocol Adaptations for Community Settings
Enhanced Community Engagement:
- Involve community representatives in trial design and review
- Adapt consent processes for local literacy levels and cultural understandings of research
- Develop community advisory boards to provide ongoing input
Accessibility Considerations:
- Design participant materials with adequate color contrast for graphical elements (minimum 3:1 contrast ratio for essential graphical objects) [64] [65]
- Ensure trial information is accessible to participants with visual impairments or low literacy
- Provide information in appropriate languages and cultural contexts
Logistical Adaptations:
- Implement decentralized follow-up through community health workers where appropriate
- Use technology-assisted monitoring to reduce participant burden
- Establish clear referral pathways for participants requiring additional care
Ethical Analysis Framework for Community Settings
Figure 2: Ethical Decision Pathway for Placebo Controls
The ethical implementation of placebo controls in clinical research, particularly for critical conditions, requires careful balancing of scientific rigor with patient protection. Based on current evidence and ethical frameworks, the following recommendations are provided:
Placebo Justification: Clearly document why placebo is scientifically necessary and why an active-control design would not yield reliable results.
Risk Mitigation: Implement methodological safeguards such as active run-in periods, early escape criteria, and add-on designs to minimize risks to placebo recipients.
Enhanced Consent: Develop and validate comprehensive informed consent processes that specifically address therapeutic misconception and ensure participant understanding of placebo use.
Community Integration: Engage community stakeholders in trial design and implementation, particularly for community-based research settings.
Ongoing Monitoring: Establish independent data monitoring committees with clear stopping guidelines based on emerging benefit-risk profiles.
When these principles are applied, placebo-controlled trials can maintain scientific validity while respecting ethical obligations to research participants, even in the context of serious medical conditions. The continuing development of innovative trial designs and ethical safeguards promises to enhance this balance further, preserving the scientific value of placebo controls while strengthening participant protections.
Managing the Therapeutic Misconception in Community Participant Recruitment
Application Note: Understanding and Identifying Therapeutic Misconception
Definition and Ethical Significance
Therapeutic misconception (TM) is a persistent ethical challenge in clinical research, particularly within Randomized Controlled Trials (RCTs) conducted in community settings. It occurs when research participants fail to adequately distinguish between the goals of clinical research and those of ordinary therapeutic care [10] [66]. Within the ethical framework of RCTs, this represents a fundamental compromise of informed consent, as participants may enroll based on incorrect beliefs about the nature and purpose of the study [10].
Empirical studies of genomic research recruitment, such as the H3Africa Rheumatic Heart Disease (RHDGen) study in South Africa, found that a majority of patient "cases" decided to join the study because of therapeutic misconception [66]. This demonstrates the pervasive nature of this challenge, especially in settings where research interfaces with clinical care for underserved populations.
Key Differentiating Factors Between Research and Clinical Care
The table below outlines core distinctions between clinical research and therapeutic care that participants often misunderstand:
Table 1: Key Differences Between Clinical Research and Therapeutic Care
| Factor | Clinical Research (RCT Context) | Therapeutic Care |
|---|---|---|
| Primary Goal | To generate generalizable knowledge [10] | To provide optimal care for an individual patient |
| Methodology | Rigid protocols, randomization, use of placebos/blinding [67] | Individualized, flexible treatment plans |
| Benefit Focus | Societal benefit (future patients) [10] | Direct benefit to the individual patient |
| Clinical Equipoise | Treatment arms are considered equally preferable at trial inception [10] | Treatment is selected based on believed superior benefit |
Protocol for Mitigating Therapeutic Misconception in Recruitment and Consent
This protocol provides a structured, evidence-based approach to minimizing therapeutic misconception during participant recruitment for community-based RCTs.
Pre-Recruitment Community Engagement
Utilizing Community-Based Participatory Research (CBPR) principles before formal recruitment begins is a critical preventive strategy [68].
Detailed Methodology:
- Objective: To build trust, understand community perceptions, and tailor consent materials to be culturally and linguistically appropriate.
- Procedure: Conduct focus groups and interviews with community members who represent the target recruitment population [68]. These sessions should explore perceptions of research, genomics (if applicable), and specific concerns about participation.
- Outcome Integration: Use qualitative data from these engagements to refine informed consent documents and recruitment scripts. For example, the Heart Healthy Lenoir study used focus group findings to reduce misconceptions and foster trust, which contributed to high enrollment rates among both African-American and White participants [68].
The Consent Process Script: A Structured Approach
The following workflow formalizes a multi-step consent conversation designed to explicitly address and correct TM. The diagram below illustrates the integrated protocol for recruitment and consent.
Protocol Steps with Scripting Examples:
Explicitly Distinguish Roles: The recruiter begins by clearly stating their role as a researcher and differentiating it from a treating clinician.
- Script Example: "My name is [Name], and I am a researcher on this study. It is important to know that I am not your doctor. The decisions we discuss today are about participating in a research study, which is different from the medical care you receive from your primary physician."
State the Primary Research Purpose: Emphasize that the goal is to gain knowledge to help future patients, not to provide superior, personalized care to the participant [10].
- Script Example: "The main goal of this study is not to provide you with the best possible treatment for your condition, but to learn which of several approaches is better for people in general. This knowledge may not help you directly, but it could benefit others in the future."
Explain Randomization and its Rationale (Equipoise): Clearly describe the randomization process and justify it using the principle of clinical equipoise [10].
- Script Example: "In this study, you will be assigned by chance, like flipping a coin, to one of two groups. This is done because expert doctors genuinely do not know which of the two approaches is better. If one were known to be superior, we would not be doing the study this way."
Clarify Protocol Rigidity: Explain that certain aspects of the study, like the number of visits or tests, are fixed by the protocol and cannot be altered based on individual patient needs.
- Script Example: "The schedule of visits and tests in this study is set and cannot be changed, even if it becomes inconvenient for you. This is different from regular healthcare, where your doctor can adjust your treatment plan as needed."
Discuss Key Uncertainties: Explicitly address the unproven nature of the intervention, the potential for unforeseeable risks, and the possibility of receiving no direct benefit [66].
- Script Example: "Because this is a new intervention, there may be risks we do not know about. Also, you may not get any personal benefit from being in the study. We will closely monitor your health, but some aspects are unknown."
Assess Understanding: Use open-ended questions to verify the participant's comprehension of key concepts, particularly the differences between research and care.
- Script Example: "To make sure I have explained everything clearly, could you please tell me in your own words what you believe the main purpose of this study is?" and "Can you describe what will be different for you compared to seeing your regular doctor for treatment?"
Reagent and Resource Toolkit for Ethical Recruitment
The following table details essential "research reagents" – the non-material tools and resources required to implement this protocol effectively.
Table 2: Research Reagent Solutions for Ethical Recruitment
| Reagent / Resource | Function & Purpose | Implementation Notes |
|---|---|---|
| Culturally-Tailored Consent Scripts | To communicate complex concepts (e.g., randomization, equipoise) in plain, accessible, and culturally resonant language. | Developed and refined through preliminary community engagement (CBPR) [68]. Must be translated and back-translated for non-native speakers. |
| Visual Aids & Decision Support Tools | To illustrate key study design elements (e.g., randomization, blinding, follow-up) and correct common misconceptions visually. | Diagrams should be simple, use culturally appropriate imagery, and be tested with the community for clarity. |
| Open-Ended Assessment Questions | To actively probe and verify participant understanding of the research-care distinction and the voluntary nature of participation. | A predefined set of questions (e.g., "What is the main purpose of this study?") should be part of the consent checklist. Responses should be documented. |
| Trained Community Liaisons | To bridge cultural and linguistic gaps, build trust, and vouch for the legitimacy of the research process within the community [68]. | Individuals respected within the target community who are trained in the research protocol and ethical principles. |
| Documentation Template (for Consent Process) | To systematically record the consent discussion, including specific questions asked and participant responses, ensuring procedural rigor. | Goes beyond a signature; provides an audit trail demonstrating how key concepts were explained and understood. |
The table below synthesizes empirical findings on the prevalence and characteristics of therapeutic and diagnostic misconception, providing a quantitative basis for understanding the problem's scope.
Table 3: Empirical Evidence on Misconception in Research Recruitment
| Study Context | Participant Group | Key Finding Related to Misconception | Enrollment Impact |
|---|---|---|---|
| RHDGen Genomic Study (South Africa) [66] | Healthy Controls (n=Not Specified) | Most joined in order to be screened for rheumatic heart disease (Diagnostic Misconception). | Not Specified |
| RHDGen Genomic Study (South Africa) [66] | Patient Cases (n=Not Specified) | Majority joined the study because of Therapeutic Misconception. | Not Specified |
| Heart Healthy Lenoir (HHL) Genomics [68] | African-American & White Adults (Total n=35 in formative FGs) | Qualitative themes (privacy, impact of knowing) informed consent process redesign to foster trust and understanding. | Post-CBPR interventions: 80.3% of eligible African-American and 86.9% of eligible White participants enrolled. Overall enrollment was 57.8% African-American. |
Application Notes: Consent Modalities for Community-Based RCTs
In community-based randomized controlled trials (RCTs), the research context presents unique challenges for obtaining valid informed consent, including diverse participant populations, varying literacy levels, and non-traditional research settings. Optimizing consent processes through electronic, verbal, and short-form approaches is essential for maintaining ethical standards while ensuring practical implementability.
Electronic Informed Consent (e-Consent)
Electronic informed consent utilizes digital platforms to present consent information and document participant agreement. This approach enhances participant comprehension through interactive multimedia elements while streamlining data management for researchers [69].
Key Advantages:
- Improved Comprehension: Incorporates audio-visual explanations and interactive quizzes to verify understanding [69].
- Enhanced Accessibility: Allows participants to review materials at their own pace and convenience [69].
- Streamlined Documentation: Facilitates efficient storage and management of consent records [69].
Implementation Challenges:
- Must address the digital divide to ensure equitable access across diverse populations [69].
- Requires robust data security measures to protect participant information [69].
- Needs maintenance of personal interaction despite digital interface [69].
Verbal Informed Consent
Verbal consent involves explaining research information orally and obtaining verbal agreement, typically using a script based on the written consent form. This approach is particularly valuable in specific research contexts where written consent is impractical or could compromise participant anonymity [69].
Primary Applications:
- Minimal risk studies where signed documentation could threaten confidentiality [69].
- Research with participants of limited literacy [69].
- Cultural contexts where signing formal documents is not the norm [69].
- Anonymous studies with minimal risk [69].
Documentation Requirements: Verbal consent processes require careful documentation, which may include audio recording, detailed written documentation by the researcher, or witnessed documentation of the consent process [69].
Short-Form Consent
Short-form consent is a specialized process used when researchers unexpectedly encounter potential participants who do not speak English. It involves verbally translating the IRB-approved informed consent document into a language the subject understands [70].
Key Limitations:
- Typically limited to enrolling up to five subjects per study; beyond this, a fully translated IRB-approved consent document must be used [70].
- For studies longer than 60 days, researchers must provide a fully translated consent document within 30 days of enrollment [70].
Process Requirements: The short-form process requires both a translator to verbally present consent information and a witness fluent in both English and the subject's language to observe and attest to the validity of the consent process [70].
Experimental Protocols
Protocol for Electronic Consent Implementation
Materials Required:
- Secure digital platform with accessibility features
- Multimedia consent presentation (video/audio explanations)
- Interactive comprehension assessment
- Electronic signature system with authentication
- Secure data storage system
Procedure:
- Platform Preparation: Configure secure e-consent platform with all necessary accessibility features and multimedia content.
- Participant Access: Provide participant with secure access to e-consent materials through personalized portal.
- Interactive Presentation: Participant engages with multimedia consent information including study purpose, procedures, risks, benefits, and alternatives.
- Comprehension Assessment: Administer interactive quiz to verify understanding of key consent elements.
- Question Resolution: Facilitate real-time communication with research team for any participant questions.
- Documentation: Obtain electronic signature after all questions resolved and comprehension verified.
- Copy Provision: Automatically provide participant with copy of signed consent document.
- Secure Storage: Store consent documentation in encrypted research database.
Protocol for Verbal Consent with Documentation
Materials Required:
- IRB-approved verbal consent script
- Audio recording equipment (if approved)
- Witness (if required by IRB)
- Documentation form for recording consent process
Procedure:
- Script Preparation: Prepare comprehensive script covering all required consent elements based on IRB-approved written consent.
- Verbal Presentation: Orally present all consent information to potential participant using clear, understandable language.
- Question Opportunity: Provide ample opportunity for participant to ask questions and receive answers.
- Comprehension Assessment: Ask participant to explain key aspects of study to verify understanding.
- Verbal Agreement: Obtain explicit verbal agreement to participate.
- Documentation: Complete detailed documentation of entire consent process including date, time, participants, and confirmation of verbal agreement.
- Witness Attestation: If required, have witness attest to observing consent process and participant understanding.
- Copy Provision: Provide participant with written summary of consent information (if appropriate).
Protocol for Short-Form Consent Process
Materials Required:
- Short-form consent document in participant's language
- IRB-approved English version of full consent document
- Qualified translator fluent in English and participant's language
- Witness fluent in both languages
- Documentation materials
Procedure:
- Form Preparation: Complete identifying information on short-form document (subject name, study ID, PI information) [70].
- Verbal Translation: Translator verbally presents full IRB-approved English consent content to participant in understandable language [70].
- Question Facilitation: Translator facilitates two-way communication for any participant questions [70].
- Participant Signature: Participant signs short-form document indicating consent was presented understandably and they agree to participate [70].
- Research Team Signature: Research team member signs English consent document as "Person Who Obtained Consent" [70].
- Witness Signature: Witness signs both short-form and English documents attesting to observing consent process and accurate translation [70].
- Translator Signature: Translator signs short-form affirming accurate presentation of information [70].
- Copy Provision: Provide participant with copies of both short-form and English consent documents [70].
Quantitative Data Comparison
Table 1: Comparative Analysis of Consent Modalities
| Parameter | Electronic Consent | Verbal Consent | Short-Form Consent |
|---|---|---|---|
| Comprehension Verification | Interactive quizzes and tracking of review time [69] | Researcher assessment of verbal understanding [69] | Dependent on translator accuracy and witness confirmation [70] |
| Documentation Method | Electronic signature with authentication [69] | Audio recording or detailed written documentation [69] | Signed short-form document + English consent + process documentation [70] |
| Personnel Requirements | Technical support team | Single researcher (plus witness if required) | Translator + witness (must be different individuals unless translator can also serve as witness) [70] |
| Participant Literacy Requirement | Moderate digital literacy | Minimal literacy | Minimal literacy in native language |
| Implementation Timeline | Initial setup extensive, subsequent consent efficient | Efficient for individual participants | Time-intensive due to translation needs |
| Best Application Context | Online studies, tech-savvy populations, large-scale trials [69] | Minimal risk studies, low-literacy populations, anonymous research [69] | Unexpected enrollment of non-English speakers, limited non-English enrollment [70] |
| Regulatory Oversight | FDA regulations on electronic signatures and records [69] | IRB approval of verbal script and documentation method [69] | IRB policy on short-form processes, translator credentials [70] |
Table 2: Ethical Considerations in Community-Based RCTs
| Ethical Principle | Electronic Consent | Verbal Consent | Short-Form Consent |
|---|---|---|---|
| Respect for Autonomy | Enhanced through self-paced review and interactive verification [69] | Maintained through verbal understanding assessment [69] | Upheld via accurate translation and cultural appropriateness [70] |
| Beneficence/Nonmaleficence | Comprehensive risk/benefit presentation with pause/reflect capability | Direct researcher interaction for immediate question resolution | Dependent on translator's ability to convey complex risk/benefit information |
| Justice | Potential exclusion of those with limited technology access [69] | Increased accessibility for vulnerable populations [69] | Addresses language barriers for non-English speakers [70] |
| Regulatory Compliance | Must comply with FDA e-signature regulations and data security requirements [69] | Must meet IRB requirements for documentation and process [69] | Must follow specific institutional short-form policies and limitations [70] |
Workflow Visualization
Consent Modality Selection Workflow: This decision tree guides researchers in selecting the appropriate consent process based on participant characteristics and study context, ensuring ethical optimization for community-based RCTs.
Short-Form Consent Process: This workflow details the sequential steps for implementing short-form consent when unexpectedly encountering non-English speaking participants in community-based RCTs.
Research Reagent Solutions
Table 3: Essential Materials for Optimized Consent Processes
| Item | Function | Implementation Notes |
|---|---|---|
| Secure e-Consent Platform | Digital framework for presenting consent information and obtaining electronic signatures [69] | Must comply with FDA 21 CFR Part 11 for electronic records and signatures; should include accessibility features |
| Multimedia Consent Presentation | Audio-visual explanations of complex study concepts to enhance understanding [69] | Should be developed at appropriate literacy level (typically 8th grade); available in multiple languages |
| Interactive Comprehension Assessment | Quiz functionality to verify participant understanding of key consent elements [69] | Questions should cover risks, benefits, alternatives, and voluntary participation; allows progression only after demonstration of understanding |
| Digital Signature Authentication | System to verify identity and document consent agreement [69] | Should include audit trail documenting date, time, and process of consent |
| Verbal Consent Script | IRB-approved standardized text for oral consent presentation [69] | Must contain all required consent elements; adapted for cultural appropriateness and literacy level |
| Audio Recording Equipment | Device to document verbal consent process (when approved) [69] | Requires specific IRB approval; must include secure storage protocols for recordings |
| Short-Form Consent Templates | Pre-translated brief consent documents in multiple languages [70] | Available from institutional IRB offices; summary documents without study-specific information |
| Translator Credential Documentation | Verification of translator qualifications and language proficiency [70] | Required for short-form process; includes qualifications, experience, and language proficiency verification |
| Bilingual Witness Documentation | Forms for witness attestation of consent process validity [70] | Witness must be fluent in both languages and not a research team member; documents observation of process and accurate translation |
Engaging Community Partners and Patient Advocates from Protocol Development to Dissemination
Application Notes: Rationale and Key Principles
Engaging community partners and patient advocates throughout the research process is a critical methodology for enhancing the ethical integrity, relevance, and impact of randomized controlled trials (RCTs) conducted in community settings. This approach, often termed Patient and Public Involvement (PPI), is defined as research carried out ‘with’ or ‘by’ members of the public rather than ‘to’, ‘about’ or ‘for’ them [71]. The "public" includes patients, carers, and people from organizations that represent service users [71].
The primary rationale for this engagement is to ensure that research addresses questions and outcomes that are meaningful to the patients and communities it is intended to serve, thereby improving the relevance and quality of research [71]. This is particularly crucial in pragmatic RCTs, which are designed to evaluate interventions in real-world clinical conditions and often raise unique ethical considerations regarding participant risk, consent, and the distinction between research and clinical practice [23] [6]. Effective engagement can facilitate participant recruitment and retention, build trust, and ensure that research solutions are respectful of cultural traditions and community needs [72].
The following table summarizes the core objectives and principles of successful engagement.
Table 1: Core Principles for Partner and Advocate Engagement
| Principle | Description | Ethical Justification |
|---|---|---|
| Meaningful Partnership | Moving from tokenistic consultation to active collaboration where lived experience influences key decisions [71]. | Embodies respect for persons and promotes shared governance of research [71]. |
| Integrated Process | Embedding engagement from the earliest stages of trial design through to dissemination of results [71]. | Enhances the social value of research and its alignment with community priorities, a key tenet of justice [23]. |
| Clear Purpose & Structure | Defining the objective and methodology for involvement from the outset [71]. | Ensures transparency and manages expectations, building trust essential for ethical community-based research. |
| Reciprocity & Capacity Building | Providing training, support, and fair compensation to empower partners and advocates [72]. | Fosters equitable partnerships and ensures that the burdens and benefits of research are justly distributed. |
Experimental Protocols: A Phased Workflow for Engagement
This protocol outlines a structured, phased approach for engaging community partners and patient advocates throughout the RCT lifecycle, drawing from established models like the LYSA trial and resources from the NIH HEAL Initiative [71] [72]. The entire workflow is designed to be iterative, with continuous feedback.
Figure 1: A phased workflow for integrating community and patient engagement throughout the RCT lifecycle.
Phase 1: Protocol Development and Trial Design
Objective: To integrate lived experience into the foundational elements of the trial, ensuring the research question, design, and materials are relevant, acceptable, and feasible for the target community.
Methodology:
- Identifying and Prioritizing Research Questions: Convene a diverse group of patient advocates and community organization representatives to identify and refine the trial's primary and secondary outcomes. Their input ensures the research focuses on issues of genuine importance to patients, such as symptom management or quality of life [71].
- Grant Application and Protocol Development: Involve partners in reviewing and contributing to the grant application and study protocol. This collaboration typically results in a more patient-focused study design, including the review of participant eligibility criteria to enhance inclusivity and the development of a patient-friendly study acronym [71].
- Ethical Framework Co-Development: Discuss and refine ethical approaches with the engagement panel, particularly for pragmatic RCTs where traditional consent models may be a barrier. This includes planning for waivers of consent or simplified consent procedures where risks are minimal and the research has high social value, ensuring these approaches are ethically sound and acceptable to the community [23] [6].
Phase 2: Trial Conduct and Monitoring
Objective: To maintain collaboration during trial execution, optimizing participant-facing materials and strategies to improve recruitment, retention, and intervention delivery.
Methodology:
- Review and Co-design of Study Materials: Establish a formal process for partners to review all participant-facing materials, including surveys, questionnaires, and consent forms. Feedback often leads to amendments in language to improve clarity and accessibility [71]. Furthermore, partners should co-design interventions or symptom management resources in partnership with the project team [71].
- Participant Recruitment and Retention Strategies: Leverage the insights of community partners to develop culturally and linguistically appropriate recruitment materials and strategies. Their trusted status within communities can help build trust and encourage participation [72].
- Ongoing Monitoring and Feedback: Maintain regular contact with the engagement panel through virtual meetings, emails, and structured feedback forms. Record all interactions, including the date, format, feedback provided, and direct changes made to the study as a result, using a standardized worksheet [71].
Phase 3: Analysis, Interpretation, and Dissemination
Objective: To ensure trial results are accurately interpreted, disseminated in accessible formats, and leveraged to advocate for further research or policy change.
Methodology:
- Interpretation of Findings: Involve patient advocates in interpreting the study results, providing context on the clinical and human significance of the data beyond mere statistical analysis [71].
- Development of Plain Language Summaries: Co-create plain language summaries (PLS) of the research findings with patient contributors. These summaries should be free of technical jargon and communicate the results in a way that is meaningful to the lay public [73].
- Broad Dissemination of Results: Engage partners in disseminating findings through diverse channels. This includes co-authoring manuscripts for academic journals, presenting at community forums and scientific conferences, and leveraging social media and patient advocacy networks to share results [71] [72]. This ensures the research reaches both academic and public audiences.
Successful engagement requires specific tools and resources to plan, conduct, and evaluate the process. The following table details key solutions.
Table 2: Essential Reagents and Resources for Community and Patient Engagement
| Tool/Resource | Function/Description | Application in RCTs |
|---|---|---|
| GRIPP2 Reporting Checklist [71] | A standardized checklist (Long Form and Short Form) to strengthen the quality and transparency of PPI reporting in research publications. | Ensures comprehensive documentation and reporting of PPI activities, methods, and impacts in trial manuscripts. |
| PPI Ignite Network [71] | Provides resources and support to researchers to foster advancements in health and social care research through PPI. | Offers practical guidance and infrastructure for building PPI into research projects from their inception. |
| NIH HEAL Initiative Tip Sheets [72] | Practical tip sheets and worksheets on planning, conducting, and disseminating findings with patient and community partners. | Equips research teams with structured approaches for effective partnership at each stage of the trial. |
| Partnership Trust Tool Survey [72] | A survey instrument designed to measure and build trust between research institutions and community partners. | Monitors the health of the collaborative relationship, allowing for proactive intervention to maintain strong partnerships. |
| CONSORT Statement [74] [75] | An evidence-based guideline comprising a checklist and flow diagram to improve the reporting of randomized controlled trials. | Serves as a foundational standard for transparent trial reporting, which can be enhanced by integrating PPI reporting via GRIPP2. |
Anticipated Outcomes and Ethical Considerations
Quantitative and Qualitative Impact
Systematic engagement yields tangible outcomes. For example, in the LYSA trial, PPI directly led to amendments in survey language, co-design of symptom management resources, and initiation of further research in metastatic breast cancer [71]. A PPI contributor also became a co-author on the resultant publication [71]. Beyond specific changes, engagement improves the participant experience and strengthens the ethical foundation of the research by aligning it with patient needs and promoting transparency.
Navigating Ethical and Logistical Challenges
Despite its benefits, implementation faces barriers. These include significant resource and time constraints, and varying levels of stakeholder engagement, which can challenge effective integration [71]. Ethically, while pragmatic RCTs in community settings may prompt discussions about altering traditional informed consent to better reflect usual care, these approaches must be carefully evaluated with community input to protect participant autonomy and welfare [23] [6]. The function of research oversight should be understood broadly as protecting participants and promoting public trust, not merely as a bureaucratic hurdle [6].
Negotiating Legal Agreements and Service Specifications with Community Sites
Engaging community sites as research partners in randomized controlled trials (RCTs) introduces unique ethical and operational challenges that extend beyond conventional clinical research settings. Community pharmacies, clinics, and other decentralized settings are increasingly vital for conducting pragmatic RCTs that evaluate interventions under real-world conditions, thereby enhancing the external validity and applicability of trial results [76] [23]. The very nature of community-engaged research blurs the traditional boundary between research and clinical practice, creating a complex landscape for negotiation and collaboration [6]. This application note establishes that successful negotiation of legal agreements and service specifications with community sites is not merely a procedural prerequisite but a fundamental ethical commitment to fostering equitable partnerships, ensuring research integrity, and respecting the operational realities of community settings.
The ethical framework for this process is anchored in the core principles of respect for persons, beneficence, and justice, which must guide interactions from initial contact through trial closure [20]. These principles manifest practically through negotiations that protect the interests of all stakeholders—participants, community sites, researchers, and funders—while facilitating the collection of robust, generalizable knowledge. As community sites often function with different resources, workflows, and priorities than academic medical centers, the agreements governing their participation must be meticulously crafted to minimize burden, clarify responsibilities, and allocate risk appropriately, thereby safeguarding both the scientific validity and ethical soundness of the research [76].
Key Ethical Considerations in Community Site Agreements
The Research-Practice Distinction and Oversight
Pragmatic RCTs conducted in community settings often challenge the traditional distinction between research and clinical practice. Most ethicists argue that this distinction, which historically justified stringent regulatory oversight, rests on presumptions that research participation offers patients less benefit and greater risk than clinical care—presumptions that often do not hold true in pragmatic RCTs evaluating usual care interventions [6]. This blurred boundary necessitates careful consideration during agreement negotiations regarding which activities will be governed by research protocols versus existing clinical operational guidelines.
The oversight mechanisms themselves become a point of ethical and practical negotiation. Stakeholders consistently report that regulatory oversight is often perceived as burdensome and a practical impediment to the conduct of pragmatic RCTs [6] [23]. When negotiating with community sites, researchers should discuss the possibility of streamlined oversight procedures for trials posing minimal incremental risk, including centralized IRB review or adapted monitoring plans that align with the risk level of the intervention. This approach demonstrates respect for the site's operational constraints while maintaining ethical rigor.
Informed Consent Adaptations
The informed consent process represents a critical ethical consideration that requires negotiation with community sites. For some low-risk pragmatic RCTs conducted in community settings, researchers and ethicists have questioned whether traditional, comprehensive informed consent is always necessary or appropriate [6]. International guidelines permit research ethics committees to grant a waiver or alteration of consent when risks are minimal, the research has significant social value, and obtaining individual consent would render the study infeasible [6].
When negotiating agreements with community sites, researchers should discuss and document the appropriate consent approach for the specific trial context. Alternatives may include:
- Simplified consent forms that focus on information material to participation decisions
- Verbal consent processes more suited to clinical workflows
- Notification models with opt-out options rather than formal consent
- Integrated consent processes that fold research authorization into clinical care discussions
The chosen approach must be explicitly detailed in the service specifications and approved by the research ethics committee, ensuring community site staff understand their roles and responsibilities in the consent process [23].
Risk Determination and Management
A fundamental ethical requirement in community-based RCTs is the appropriate identification and management of research-related risks. Negotiations must address how risks will be identified, monitored, and managed within the community setting. The determination of what constitutes minimal risk is particularly nuanced in pragmatic trials, as it requires consideration of the incremental risks of research participation above those inherent in usual clinical care [23].
Service agreements should clearly delineate procedures for adverse event reporting, monitoring responsibilities, and emergency unblinding if applicable. The allocation of liability for different categories of risk must be explicitly negotiated, with careful attention to limitations of liability that protect both the institution and the community site while ensuring participant safety remains paramount.
Quantitative Analysis of Community Site Negotiation Timelines
Data from retrospective analysis of RCTs conducted in community pharmacies reveal significant timelines required for key negotiation and startup activities. The following table summarizes duration metrics for essential processes across the trial lifecycle, drawn from actual community-based trials [76].
Table 1: Negotiation and Startup Timelines for Community-Based RCTs
| Activity | Phase | Median Duration (Days) | Key Dependencies |
|---|---|---|---|
| Pharmacy contract negotiation | Planning | 92 | Ethical approval, funding confirmation |
| Patient Group Direction development | Planning | 112 | Final protocol, regulatory review |
| Site recruitment | Execution | 78 | Contract execution, staff training |
| Ethics approval | Initiation | 65 | Finalized protocol, insurance |
| Participant recruitment | Execution | Varies by site | Site readiness, marketing materials |
The protracted timelines for legal agreement negotiation, particularly with pharmacy contracting bodies and corporate entities, highlight the critical importance of early engagement with potential community sites. Developing documentation for trial drug supply, including Patient Group Directions (PGDs) in jurisdictions where they are required, represents the most time-consuming preparatory activity, requiring median durations of over 100 days [76]. These quantitative benchmarks underscore the necessity of incorporating sufficient lead time—often 4-6 months—into trial planning specifically for agreement negotiation and regulatory processes.
Stakeholder Mapping and Engagement Protocol
Successful negotiation with community sites requires systematic identification and engagement of all relevant stakeholders. The following protocol provides a methodological framework for stakeholder analysis and engagement throughout the agreement negotiation process.
Stakeholder Identification and Mapping
Initial stakeholder mapping should identify eight primary groups involved in or affected by community-based RCTs [76]:
- Public Services/Agencies (health departments, regulatory bodies)
- Community Sites (pharmacies, clinics, their management and staff)
- Communications Intermediaries (professional associations, networks)
- Funders/Sponsors (research funders, industry sponsors)
- Academic/Research Institutions (investigators, trial management units)
- Healthcare Providers (physicians, specialists, allied health)
- Suppliers (medication, equipment, technology vendors)
- Regulators (ethics committees, regulatory authorities)
Table 2: Stakeholder Engagement Strategies and Responsibilities
| Stakeholder Group | Primary Interests | Engagement Strategies | Agreement Negotiation Role |
|---|---|---|---|
| Community Site Owners/Corporate | Business continuity, liability protection, reputation | Early consultation, risk-benefit analysis, financial compensation | Contract signatory, resource allocation approval |
| Site Staff (Pharmacists, Nurses) | Workflow integration, clarity of responsibilities, training | Co-design of procedures, hands-on training, ongoing support | Protocol adherence, service specification input |
| Patients/Participants | Access to care, safety, convenience | Patient advisory groups, plain language summaries, feedback mechanisms | Indirect influence through preferences and engagement |
| Research Ethics Committee | Participant safety, ethical conduct, regulatory compliance | Pre-submission meetings, detailed protocols, regular reporting | Approval of consent processes and risk management |
| Trial Management Team | Timeline adherence, data quality, budget management | Regular coordination meetings, progress tracking, problem-solving | Primary negotiator, relationship manager |
Engagement Methodology
The stakeholder engagement process should follow a structured approach:
Initiation Phase (Months 1-2):
- Identify key decision-makers and influencers at each community site
- Conduct initial exploratory meetings to understand site-specific constraints and requirements
- Develop draft service specifications collaboratively with site representatives
Negotiation Phase (Months 2-4):
- Circulate draft agreements to all stakeholders for review
- Conduct structured negotiation sessions focusing on high-priority terms (liability, payment, IP)
- Document all requested modifications and rationales
- Iterate agreement language until consensus reached
Finalization Phase (Month 4-5):
- Obtain necessary institutional signatures according to authority delegations
- Execute final agreements with community sites
- Develop simplified summary documents for site staff implementation
This protocol emphasizes tailored engagement strategies for different stakeholder groups, recognizing that corporate entity negotiations will focus on liability and compensation, while front-line staff engagement must address workflow integration and training needs [76].
Negotiation Framework for Key Contractual Provisions
Legal agreements with community sites require careful attention to specific provisions that allocate risk, define responsibilities, and protect all parties' interests. The following framework addresses the most critically negotiated terms in service agreements for community-based research.
Scope of Services and Specifications
The service specification annex represents the operational heart of the agreement, translating research protocols into actionable tasks for community sites. Effective service specifications should [77]:
- Clearly define the services the site will provide and any specific deliverables
- Establish objective metrics and key performance indicators rather than assuming parties will determine these as the relationship progresses
- Specify interim and final timelines for service delivery
- Detail what the research organization must provide to enable service performance
- Explicitly state that the community site is not responsible for delays caused by research organization failures to provide necessary inputs
During negotiations, researchers should advocate for balanced performance standards that ensure scientific integrity without imposing unrealistic demands on community operations. Including examples of acceptable documentation formats, data collection methods, and reporting mechanisms aligned with existing site workflows increases practicality and compliance.
Intellectual Property and Ownership Rights
The allocation of rights in intellectual property (IP) generated during the research represents one of the most challenging aspects of agreement negotiation [77] [78]. Community sites may contribute valuable operational insights, service delivery innovations, or data management solutions that generate intellectual property.
Negotiations should address:
- Pre-existing IP: Each party should retain ownership of their background IP, with clear identification of what constitutes pre-existing materials [77]
- New IP ownership: Establish protocols for determining ownership of newly developed IP, with preference for project-specific IP residing with the research institution while operational improvements remain with the community site
- Residual knowledge: Protect the right of both parties to utilize knowledge, techniques, and expertise gained during the collaboration in future projects [77]
- Publication rights: Balance the community site's interest in acknowledging contributions with the research institution's need to disseminate findings
A principled approach to IP negotiation recognizes and values the intellectual contributions of community partners while maintaining the research organization's ability to fulfill dissemination requirements.
Liability, Indemnification, and Risk Management
The allocation of liability and risk represents a central focus of legal negotiations. Service providers (community sites) naturally seek to limit their liability, while research organizations must ensure adequate protection for participants and the institution [77] [78].
Successful risk allocation strategies include:
- Mutual indemnification for negligence, misconduct, or protocol violations
- Liability caps tied to the contract value or a reasonable multiple thereof
- Insurance requirements specifying types, amounts, and evidence of coverage
- Exclusions for consequential damages with carve-outs for data breaches or participant injury
- Clear protocols for addressing participant injuries, including coverage for non-negligent harm
When negotiating with community sites, particularly smaller organizations, researchers should consider proportional liability approaches that reflect the actual risk exposure and resources of each party. Requiring insurance coverage levels that would cripple a community site's operations undermines the collaborative spirit and may preclude participation of diverse sites.
Payment Terms and Compensation Structure
Financial arrangements must balance the research organization's need for cost control with the community site's requirement for adequate compensation. Payment terms should [77]:
- Clearly specify invoicing procedures, payment timelines, and billing periods
- Consider initial deposits to support site startup costs and establish commitment
- Establish milestone-based payments tied to specific deliverables (e.g., site initiation, participant enrollment targets, data submission)
- Include payment enforcement mechanisms for delayed payments, while recognizing community sites' limited capacity to absorb cash flow disruptions
- Detail reimbursement procedures for pre-approved study-related expenses
Negotiations should acknowledge that community sites often lack the administrative infrastructure of large research institutions, necessitating simplified payment processes and reasonable documentation requirements.
Essential Research Reagent Solutions for Community Trial Management
The following toolkit outlines critical resources and methodologies required for successful implementation of negotiated agreements in community-based RCTs.
Table 3: Research Reagent Solutions for Community Trial Management
| Tool/Resource | Primary Function | Application in Community Agreements |
|---|---|---|
| Project Management Framework | Structured timeline, task, and resource management | Aligns site activities with research milestones; referenced in service specifications [76] |
| Stakeholder Engagement Platform | Facilitates communication and document sharing | Supports negotiation transparency; maintains relationship records [23] |
| Centralized Ethics Submission Portal | Streamlines regulatory approval processes | Expedites multisite ethics review; documented in agreements as primary pathway [6] |
| Standardized Service Specification Templates | Pre-approved language for common site activities | Accelerates negotiation; ensures consistency across sites [77] |
| Risk Assessment Matrix | Evaluates and categorizes protocol-specific risks | Informs liability negotiations; basis for insurance determinations [23] |
| Data Transfer and Security Protocols | Governs collection, sharing, and protection of research data | Annexed to agreements; specifies technical and administrative safeguards [76] |
| Participant Recruitment Materials | Site-specific advertising, screening, and consent documents | Detailed in service specifications; requires site input during development [23] |
Workflow Visualization: Community Site Negotiation Pathway
The following diagram illustrates the complete negotiation workflow from initial site identification through agreement execution and implementation, integrating ethical considerations and stakeholder engagement checkpoints.
Community Site Negotiation and Activation Workflow
This workflow emphasizes the iterative nature of community site negotiations, with multiple feedback loops and concurrent processes. The ethical foundation informs all phases of negotiation, ensuring that practical considerations never override core principles of research ethics. The visualization highlights how stakeholder engagement begins early and continues throughout the process, reinforcing that successful agreements depend on relationships as much as legal provisions.
Negotiating legal agreements and service specifications with community sites for RCTs requires a balanced approach that respects both ethical imperatives and operational realities. By applying the frameworks, protocols, and visualizations presented in this application note, researchers can establish partnerships that advance scientific knowledge while honoring the trust participants place in both community providers and research institutions. The measurable timelines and structured processes provided enable realistic planning and resource allocation, increasing the likelihood of successful community-engaged research that generates meaningful evidence for improving health outcomes.
Addressing Resource Constraints and Infrastructure Limitations in Community Settings
Conducting randomized controlled trials (RCTs) in community settings presents a unique convergence of ethical obligations and practical challenges. While RCTs represent the gold standard for generating clinical evidence, their implementation in community contexts—such as community pharmacies, rural health clinics, and public health centers—requires careful navigation of inherent resource constraints and infrastructure limitations [76] [21]. The ethical framework for such research must extend beyond traditional considerations of informed consent and risk minimization to address distributive justice and the avoidance of exploitation, ensuring that research burdens do not disproportionately affect resource-limited communities and that benefits are equitably shared [79].
This application note establishes that addressing infrastructure limitations is not merely an operational concern but a fundamental ethical requirement. When communities participate in research without adequate support to overcome their constraints, investigators risk perpetuating the same power imbalances and inequities that often characterize traditional research paradigms [80] [79]. We present practical protocols and solutions framed within this ethical context, ensuring that research conducted in community settings maintains scientific rigor while respecting the limitations and autonomy of community partners.
Understanding the Challenges: A Quantitative Assessment
Resource constraints in community settings manifest across multiple dimensions, including financial limitations, staffing shortages, technological barriers, and regulatory complexities. A retrospective analysis of two multicentre RCTs conducted in community pharmacies quantified the extensive operational requirements, identifying 94 distinct high-level tasks across project phases [76].
Table 1: Project Management Tasks in Community-Based RCTs
| Project Phase | Number of High-Level Tasks | Key Challenges | Typical Duration |
|---|---|---|---|
| Initiation | 7 | Stakeholder identification, ethical approvals | 1-3 months |
| Planning | 30 | Legal agreements, documentation development | 3-6 months |
| Execution/Monitoring | 43 | Pharmacy recruitment, data collection | 6-18 months |
| Closure | 14 | Data analysis, results dissemination | 2-4 months |
Recruitment of pharmacy sites and development of key documents for trial drug administration (such as patient group directions) were identified as the most time-consuming early-phase activities [76]. These operational challenges exist within a broader ethical context where the principle of justice requires that research burdens be fairly distributed and that communities receive a fair share of research benefits [79].
Ethical Framework for Addressing Resource Limitations
Avoiding Exploitation in Resource-Constrained Settings
Environmental health researcher David B. Resnik emphasizes that investigators have ethical obligations to avoid exploitation even when no physician-patient relationship exists [79]. This obligation implies duties to protect subjects' rights and welfare while ensuring they receive fair benefits from research participation. Exploitation can occur when resource-constrained communities contribute to research without receiving adequate benefits in return, such as when studies extract data without building local capacity or addressing community-identified priorities [80] [79].
The community data justice model proposes reimagining data governance through the lenses of data ethics, justice, and community-engaged research [80]. This approach emphasizes formal agreements about power sharing, building trust through sustained relationships, and ensuring communities have control over research agendas and dissemination. When implemented effectively, this model allows communities to shape research narratives, pilot community-generated initiatives, and sustain research capacity beyond individual projects [80].
Ethical Justifications for Control Groups in Community Trials
The use of control groups in community-based RCTs raises distinctive ethical considerations, particularly when one group receives fewer resources or interventions. Placebo-controlled trials are ethically justified when: (1) no proven intervention exists; (2) the intervention under investigation is for a minor condition and withholding it does not pose risks of serious harm; or (3) compelling methodological reasons require use of a placebo and patients won't be subjected to additional risks [21] [79].
In community intervention trials, control groups typically receive education and counseling rather than placebos, while experimental groups receive additional interventions [79]. The ethical justification for such designs depends on the state of clinical equipoise—a genuine uncertainty in the expert community about the comparative therapeutic merits of each arm [21]. Additionally, researchers must ensure that control group participants still receive a fair share of benefits, such as educational resources or access to the intervention after trial completion [79].
Protocols for Community-Engaged Research Infrastructure
Stakeholder Engagement and Partnership Protocol
Objective: To establish equitable partnerships between researchers and community stakeholders that address power imbalances and resource constraints through formalized agreements and capacity building.
Table 2: Stakeholder Engagement Protocol
| Phase | Key Activities | Ethical Considerations | Resource-Saving Strategies |
|---|---|---|---|
| Pre-Engagement | Community asset mapping; Identification of community priorities | Historical acknowledgment of extractive research practices | Utilize existing community networks rather than building new ones |
| Partnership Formation | Memorandum of Understanding (MOU) negotiation; Joint agenda setting | Power-sharing in research question development and design | Formalize roles to prevent mission creep and redundant efforts |
| Capacity Building | Training community researchers; Data stewardship development | Investing in sustainable community infrastructure | Build skills transfer into research protocol to maximize local benefits |
| Ongoing Governance | Regular partnership meetings; Transparent decision-making | Continuous consent and community oversight | Efficient communication channels to minimize meeting burdens |
This protocol emphasizes that trust-building is a fundamental aspect of community-based engagement, though it requires substantial time investment [80]. The Ferguson Commission, Native Lands Advocacy Project, and Greensboro Health Disparities Collaborative represent case examples where communities have exerted greater control over research and data governance [80].
Data Collection Infrastructure Protocol
Community-engaged data collection requires methodologies that are both scientifically rigorous and feasible within resource constraints. Three established methods include:
Concept Mapping: A structured conceptualization process that engages community members in defining research priorities and strategies [81]. The process involves:
- Preparation: Identifying focal questions and participant criteria
- Generation: Brainstorming sessions to generate items
- Structuring: Sorting and rating items by perceived similarity and importance
- Representation: Statistical analysis creating visual concept maps
- Interpretation: Community review and discussion of maps
- Utilization: Applying findings to research implementation
In implementation research on HPV vaccination, concept mapping engaged clinic members and community advocates in prioritizing evidence-based strategies, resulting in eight key strategy clusters rated by importance and feasibility [81]. This method efficiently leverages community expertise while generating quantifiable data for implementation planning.
Rapid Ethnographic Assessment: This method combines structured observation with community engagement to efficiently understand local contexts and implementation barriers [81]. The protocol includes:
- Community member training in data collection techniques
- Structured environmental observations using standardized tools
- Key informant interviews conducted by community researchers
- Triangulation of multiple data sources to enhance validity
- Collaborative analysis sessions with academic and community partners
Photovoice: A participatory method that empowers community members to document and discuss their realities through photography [81]. Implementation steps include:
- Training participants in photography ethics and techniques
- Guided photo documentation of community strengths and challenges
- Structured discussion sessions using the SHOWED framework (What do you See here? What's really Happening? How does this relate to Our lives? Why does this situation Exist? What can we Do about it?)
- Collaborative thematic analysis of images and narratives
- Community exhibitions to disseminate findings to policymakers
Research Reagent Solutions for Community Settings
Table 3: Essential Research Infrastructure Solutions
| Solution Category | Specific Tools/Resources | Function | Ethical Considerations |
|---|---|---|---|
| Data Collection Tools | Qualitative Data Sharing (QuaDS) software; Digital recorders; Tablet computers | Enable efficient data capture while maintaining confidentiality | Ensure tools are accessible and don't create technological barriers |
| Data Governance Infrastructure | Memorandum of Understanding templates; Data ownership agreements; IRB documentation | Formalize data sharing, ownership, and use parameters | Protect community interests while satisfying institutional requirements |
| Analysis Support Tools | Concept mapping software (Groupwisdom); Qualitative analysis packages; Data visualization tools | Facilitate collaborative data interpretation | Balance analytical sophistication with community accessibility |
| Capacity Building Resources | Community researcher training curricula; Data stewardship guidelines; Implementation science frameworks | Build sustainable local research infrastructure | Address power differentials in knowledge valuation and control |
The Qualitative Data Sharing (QuaDS) software represents a particularly valuable tool, as it automatically flags HIPAA safe harbor identifiers and potentially identifying variables in qualitative data, facilitating responsible data sharing while protecting participant confidentiality [82]. This tool helps address the ethical imperative to share research data for verification and secondary analysis while managing the unique sensitivities of qualitative community data.
Integrated Workflow for Resource-Constrained Community Trials
The following workflow integrates ethical considerations with practical implementation strategies for conducting RCTs in community settings with limited resources:
This workflow emphasizes continuous community engagement throughout the research process, with explicit checkpoints for addressing resource constraints at each phase. The protocol adaptation phase specifically focuses on modifying traditional research approaches to be feasible within community infrastructure limitations while maintaining scientific integrity.
Addressing resource constraints and infrastructure limitations in community settings requires both methodological innovation and a fundamental commitment to ethical partnership. The protocols and solutions presented here emphasize that building equitable research infrastructure is not merely an operational concern but a core ethical requirement for community-engaged research. By implementing these approaches, researchers can generate rigorous evidence while ensuring that community partners receive fair benefits and that research contributes to sustainable capacity building rather than extraction.
The growing emphasis on community data governance and participatory models reflects an important shift in research ethics, recognizing that addressing power imbalances and resource constraints is essential to conducting truly ethical research in community settings [80]. As regulatory agencies increasingly require data sharing and community engagement, these protocols provide a roadmap for implementing these ethical mandates in practical, feasible ways that respect the limitations and strengths of community partners.
Assessing Ethical Frameworks and Emerging Alternatives to Traditional RCTs
Randomized Controlled Trials (RCTs) and Real-World Evidence (RWE) studies represent two pivotal approaches in clinical and health services research. While RCTs are considered the gold standard for establishing causal efficacy under controlled conditions, RWE studies generate evidence from data collected during routine healthcare delivery [83] [84]. The ethical frameworks governing these methodologies differ significantly due to their distinct designs, data sources, and potential impacts on participants and patients. This analysis examines their ethical dimensions, with particular attention to research conducted in community settings, to provide researchers, scientists, and drug development professionals with practical guidance for navigating these considerations.
RWE is derived from real-world data (RWD), which encompasses information relating to patient health status and/or healthcare delivery routinely collected from sources including electronic health records, medical claims data, disease registries, and patient-generated data from digital health technologies [83]. The fundamental ethical tension lies in balancing the scientific imperative to generate robust evidence with the protection of patient rights, privacy, and autonomy across these different research paradigms.
Comparative Ethical Frameworks
Table 1: Core Ethical Principles and Their Application to RCTs and RWE Studies
| Ethical Principle | Application in RCTs | Application in RWE Studies |
|---|---|---|
| Informed Consent | Well-established process with detailed participant information and explicit written consent [23]. | Often relies on broad consent, opt-out models, or waived consent for de-identified data; significant transparency challenges [85] [86] [23]. |
| Privacy & Confidentiality | Protected through research-specific data collection with controlled access [86]. | Heightened risk due to use of pre-existing, often detailed, patient data; potential for re-identification even after anonymization [85] [86]. |
| Risk Minimization | Focuses on physical and psychological risks from interventions and trial procedures [23]. | Primarily centers on privacy breaches, data security, and potential group harms from research findings [85] [86]. |
| Equity & Justice | Concerns about participant selection, fair inclusion, and relevance of research questions [87]. | Risks from biased datasets that underrepresent certain populations, potentially perpetuating health disparities [85] [86]. |
| Distinction from Practice | Clear boundary between research and clinical care, with formal research protocols [23]. | Blurred lines, especially in pragmatic trials and quality improvement initiatives embedded in care [23]. |
Table 2: Ethical Oversight and Stakeholder Considerations
| Consideration | RCTs | RWE Studies |
|---|---|---|
| Primary Regulatory Focus | Participant safety, protocol adherence, data integrity [87]. | Data provenance, privacy safeguards, and appropriateness of consent model [86] [83]. |
| Typical Consent Model | Explicit, study-specific informed consent [23]. | Varied models: broad consent, tiered consent, dynamic consent, or waiver of consent [85] [86]. |
| Key Stakeholders | Investigators, participants, sponsors, research ethics committees [76]. | Patients, healthcare providers, data custodians, insurers/payers, community representatives [23] [83]. |
| Community Engagement | Often focused on participant recruitment and retention [76]. | Essential for building trust, ensuring data use is socially acceptable, and interpreting findings [23]. |
Ethical Protocols and Application Notes
Protocol for Ethical RWE Study Design
Objective: To establish a methodology for designing RWE studies that uphold ethical principles while generating scientifically valid evidence.
Background: The use of RWE is evolving, with growing recognition by regulators, payers, and health technology assessment bodies to answer specific research questions throughout the medical product lifecycle [83]. Ethical design is paramount to maintain public trust.
Procedure:
- Data Fitness Assessment: Scientifically evaluate the suitability of the RWD source for the research question. Assess data quality, completeness, and representativeness of the target population. Identify potential biases and underrepresentation of specific subgroups [83].
- Privacy-by-Design Implementation: Incorporate data protection measures at the study design phase. This includes determining the appropriate level of data de-identification (anonymization or pseudonymization), planning for secure data storage and transfer protocols (e.g., encryption, access controls), and defining data retention periods [85] [86].
- Consent Model Selection: Determine the appropriate consent framework based on the study design, data sources, and regulatory context.
- Broad Consent: Obtain patient consent for future use of their data in a range of research projects, with oversight by an ethics committee [85].
- Dynamic Consent: Use digital platforms to allow patients ongoing choice about how their data is used [86].
- Waiver of Consent: For research using exclusively de-identified data, a research ethics committee may grant a waiver of informed consent where the research would not be practicable otherwise and poses minimal risk [23].
- Transparency and Patient Communication: Develop public-facing materials explaining the study's purpose, data sources, and safeguards. Provide mechanisms for patients to opt-out where feasible and accessible [86].
Protocol for Ethical Pragmatic RCTs in Community Settings
Objective: To provide a framework for addressing ethical challenges in pragmatic RCTs conducted within routine community practice settings.
Background: Pragmatic RCTs are intended to inform clinical or health policy decisions by mimicking real-world conditions [23]. This blurring of research and clinical care creates distinct ethical challenges.
Procedure:
- Risk Assessment in Real-World Context:
- Evaluate both the risks of the intervention and the risks of the research procedures themselves.
- Determine if the study qualifies as "minimal risk" because the interventions and procedures are commensurate with those encountered in routine clinical care for the condition [23].
- Alternate Consent Models:
- Assess whether traditional, written informed consent is necessary or if an alternate model (e.g., verbal consent, implied consent, notification with opt-out) is appropriate and ethically justifiable.
- Justification may include that the risk is minimal, the intervention is embedded in usual care, and obtaining individual consent is impracticable [23].
- Stakeholder Identification and Engagement:
- Map all stakeholders, including clinical investigators, patient partners, healthcare providers, health system administrators, and payers [23] [76].
- Engage patient partners and community representatives early in the design process to ensure the research question and outcomes are relevant and the conduct of the trial is acceptable [23].
- Clarity on "Usual Care" and Reporting:
- Clearly define and document what constitutes "usual care" for the control arm. This ensures transparency and avoids therapeutic misconception [23].
- Community Pharmacy and Setting Management: When trials are conducted in accessible community settings like pharmacies:
- Engage with pharmacy contracting bodies and chains early to secure agreements, which can be time-consuming [76].
- Streamline trial processes to minimize burden on pharmacy staff who have primary clinical responsibilities [76].
- Implement tailored training and support for site staff who may be less familiar with research protocols [76].
Visualizing Ethical Assessment Workflows
The following diagram illustrates a decision pathway for selecting and implementing an appropriate consent model in RWE studies and pragmatic RCTs.
Table 3: Key Methodological and Ethical Resources for Clinical Research
| Tool / Resource | Category | Function / Purpose |
|---|---|---|
| PRECIS-2 Tool [23] | Methodological Framework | Helps trialists design trials that are more pragmatic (real-world) or explanatory (controlled), clarifying the ethical context. |
| STaRT-RWE Template [83] | Reporting Standard | A structured template for planning and reporting on the implementation of RWE studies, promoting transparency and reproducibility. |
| HARPER Protocol [83] | Protocol Development | Facilitates harmonized study protocol development to enhance reproducibility of RWE studies. |
| Cairo Consensus Statements [87] | Integrity Guidelines | Discipline-specific research integrity guidelines for the entire RCT lifecycle, promoting responsible conduct. |
| Dynamic Consent Platforms [86] | Consent Technology | Digital tools enabling ongoing participant engagement and choice in how their data is used for research. |
| Federated Data Systems [83] | Data Architecture | An organized network of distinct RWD sources analyzed separately using the same protocol, enabling research while potentially retaining data locally to enhance privacy. |
| Community Engagement Policy [88] | Governance Framework | An internal organizational framework outlining principles and goals for meaningful community interaction, building trust for community-based research. |
Pragmatic Clinical Trials (PCTs) represent a fundamental shift in clinical research, moving from highly controlled explanatory trials to studies designed to inform real-world clinical and policy decisions by assessing interventions in routine practice conditions [89]. Unlike traditional randomized controlled trials (RCTs) that prioritize internal validity through strict protocols and homogeneous populations, PCTs emphasize external validity and generalizability by incorporating broader patient populations, typical clinical settings, and outcomes relevant to daily practice [89]. This paradigm shift challenges the foundational ethical frameworks that govern human subjects research, creating significant tension between traditional oversight mechanisms and the practical realities of pragmatic research.
The research-practice distinction, a cornerstone of contemporary research ethics, becomes blurred in PCTs where interventions often consist of usual care treatments and data collection occurs through electronic health records within routine clinical workflows [6]. This blurring raises critical questions about whether current Research Ethics Committee (REC) and Institutional Review Board (IRB processes—designed primarily for explanatory trials—remain adequate for evaluating studies that deliberately integrate research with clinical care [23] [6]. As PCTs grow in popularity to meet evidence needs for learning healthcare systems, examining the fitness of ethical oversight processes becomes increasingly urgent for researchers, regulators, and drug development professionals working in community settings [89].
Ethical Challenges Unique to Pragmatic Trial Designs
Core Ethical Tensions in Pragmatic Trials
PCTs generate distinctive ethical challenges that existing oversight frameworks struggle to address adequately. Through interviews with key stakeholders in PCT design and conduct, researchers have identified several predominant areas of ethical tension that complicate traditional ethical review [23]:
- Identification and assessment of research risks: Determining what constitutes "minimal risk" proves challenging when study interventions are embedded in usual care, complicating regulatory determinations and participant protections [23] [90].
- Informed consent approaches: The practicality and necessity of traditional written informed consent is frequently questioned when interventions pose minimal incremental risk and study designs mimic clinical practice [23] [6].
- Distinction between research and quality improvement: The blurred boundaries between clinical practice, quality improvement, and research activities create confusion about what activities require ethical review [23].
- Protections for broader affected populations: PCTs may impact not only direct participants but also clinicians, healthcare organizations, and even entire communities, raising questions about what protections these groups might be owed [23] [91].
- Stakeholder roles and responsibilities: The broader range of stakeholders involved in PCTs—including health systems, payors, and community partners—creates ambiguity regarding their respective roles and responsibilities [23].
- Determination of "usual care": Defining what constitutes appropriate usual care and understanding the implications for trial reporting presents both methodological and ethical challenges [23].
Empirical Analysis of Ethical Concerns
A comprehensive scoping review of empirical ethics research related to PCTs analyzed 82 published studies and identified 22 distinct ethical themes, with the five most prevalent being consent and disclosure, risk assessment, trust and transparency, operational burdens and implementation barriers, and the role of engagement [90]. This research highlights that engagement practices in PCTs have been "limited and inconsistent," revealing what the authors term "a persistent gap between the ideal of inclusive, sustained collaboration and the realities of constrained resources, power dynamics, and unclear stakeholder roles" [90].
Table 1: Most Prevalent Ethical Themes in Pragmatic Clinical Trials
| Ethical Theme | Prevalence | Core Challenge |
|---|---|---|
| Consent & Disclosure | High | Traditional written informed consent often impractical; alternatives needed |
| Risk Assessment | High | Defining "minimal risk" complicated for usual care interventions |
| Trust & Transparency | High | Necessary for participant confidence but challenging with consent alterations |
| Operational Burdens | High | Logistical challenges when integrating interventions into routine care |
| Engagement | High | Gap between ideal collaboration and practical implementation |
Limitations of Current Ethical Oversight Frameworks
Regulatory Misalignment with Pragmatic Design
Current ethical oversight frameworks demonstrate significant misalignment with the design and implementation of PCTs. The conventional distinction between research and practice—which underpins most research regulations—rests on presumptions that research participation offers patients less benefit and greater risk than clinical practice, assumptions that frequently do not hold true in the context of PCTs [6]. This misalignment leads to inappropriate application of regulations designed for early-phase drug trials to studies comparing established interventions in routine care settings.
Oversight by RECs/IRBs is widely viewed as "burdensome and a practical impediment" to the conduct of PCTs, with many arguing that oversight procedures ought to be streamlined when risks to participants are low [6]. This burden manifests particularly in consent requirements that may be impractical for large-scale trials embedded in clinical care and which potentially compromise the external validity of the research by creating selection bias [6] [89]. The fundamental tension lies in balancing the protection of participant autonomy and welfare with facilitating socially valuable research that can improve healthcare delivery and outcomes.
Geographic and Methodological Limitations in Ethics Research
The empirical basis for ethical oversight of PCTs suffers from significant limitations. Most empirical ethics research has been concentrated in the United States and other Western countries and relies heavily on surveys and hypothetical scenarios rather than real-world contexts [90]. This limits the generalizability and applicability of current findings, particularly for PCTs conducted in low-resource settings or diverse cultural contexts. This geographic and methodological narrowness constrains the development of nuanced, context-sensitive oversight approaches that can adapt to varying healthcare systems and cultural norms.
Proposed Models for Adapted Ethical Oversight
Innovative Approaches to Consent and Oversight
Several innovative models have been proposed to address the ethical challenges unique to PCTs while maintaining appropriate participant protections:
- Integrated Consent Model: This approach, proposed by Kim and Miller, suggests that formal consent may not be needed under certain circumstances for many pragmatic trials, particularly those comparing validated usual care interventions with minimal incremental risk [89].
- Prescribed versus Invited Trials: Largent and Joffe advocate separating trials into "prescribed" and "invited" categories. Prescribed clinical trials compare interventions viewed as optimal medical care and involve minor net risk, allowing for a less formal consent process. Invited medical trials have greater uncertainty about benefits and involve more than minor net risk, thus requiring conventional consent and oversight [89].
- Waivers and Alterations of Consent: For lower-risk PCTs where traditional consent would be impractical or would compromise study validity, RECs/IRBs can grant waivers or alterations of consent, such as opt-out mechanisms or general notification approaches [90] [6].
- Contextual Risk Assessment: Rather than applying uniform standards, this approach tailors oversight to the specific risks and characteristics of each PCT, focusing particularly on incremental risks beyond those of usual clinical care [6].
Enhanced Stakeholder Engagement Framework
Addressing the identified gaps in engagement practices requires a more structured approach to stakeholder involvement throughout the PCT lifecycle. Community-Based Participatory Research (CBPR) principles, while challenging to implement within RCT frameworks, offer valuable insights for meaningful engagement [92]. Successful models emphasize genuine collaboration between researchers and community members to identify research goals, questions, methods, and dissemination strategies, with explicit focus on utilizing the research process to improve lives and promote social justice [92].
The Refugee Well-being Project provides an illustrative case study of sustained community engagement, featuring a Community Advisory Council (CAC) of refugees, former students, and service providers that has been involved in all aspects of the study for nearly a decade, including interview protocol design, participant recruitment, intervention implementation, data analysis, and dissemination [92]. This long-term partnership model demonstrates how academic-community collaborations can navigate the tensions between research rigor and community relevance while maintaining ethical integrity.
Implementation Tools and Protocols for Ethical PCT Oversight
Research Reagent Solutions: Ethical Oversight Toolkit
Table 2: Essential Methodological Tools for Ethical PCT Design and Oversight
| Tool/Method | Primary Function | Application in PCTs |
|---|---|---|
| PRECIS-2 Tool | Trial design assessment | Qualitatively ranks studies across design characteristics to visualize pragmatic/explanatory balance [89] |
| Integrated Consent Model | Consent process framework | Guides appropriate consent level based on risk and intervention characteristics [89] |
| Stakeholder Engagement Mapping | Identifying relevant parties | Identifies all groups affected by PCT and determines appropriate protections [23] [91] |
| Incremental Risk Assessment | Risk evaluation | Focuses review on risks beyond those of usual clinical care [6] |
| Aggregate Results Sharing Protocol | Post-trial ethics | Guides appropriate sharing of lay-friendly summaries with participants and stakeholders [91] |
| Community Advisory Councils | Stakeholder engagement | Provides structured mechanism for community input throughout research process [92] |
Experimental Protocol for Ethical Risk Assessment in PCTs
Protocol Title: Structured Approach to Determining Minimal Risk and Appropriate Consent Modifications in Pragmatic Clinical Trials
Background: Traditional risk assessment frameworks struggle with PCTs where interventions often constitute usual care and incremental research risks may be minimal. This protocol provides a systematic method for RECs/IRBs to evaluate risks and determine appropriate consent approaches.
Methodology:
Characterize Intervention Components:
Assess Incremental Risks:
- Identify potential harms beyond those encountered in usual clinical care
- Evaluate the probability and magnitude of incremental harms
- Consider whether risks exceed those "ordinarily encountered in daily life" [89]
Evaluate Consent Requirements:
- Determine if waiver or alteration of consent is justified using recognized criteria:
- Research involves no more than minimal risk
- Waiver or alteration will not adversely affect rights and welfare
- Research could not practicably be carried out without waiver or alteration
- Whenever appropriate, subjects will be provided with additional pertinent information [6]
- Determine if waiver or alteration of consent is justified using recognized criteria:
Design Appropriate Notification Processes:
Implement Ongoing Monitoring:
- Establish data safety monitoring board commensurate with study risks
- Develop plan for monitoring stakeholder concerns throughout trial
- Create protocol for addressing participant or clinician questions [23]
Expected Outcomes: Application of this protocol should yield appropriate, risk-proportionate oversight that protects participants while facilitating valuable pragmatic research.
Discussion and Future Directions
The ethical oversight landscape for PCTs requires reconceptualization rather than minor adjustments. Current REC/IRB processes, while fit for purpose in many traditional research contexts, demonstrate significant limitations when applied to pragmatic trials that deliberately blur the boundaries between research and practice [23] [6]. Moving forward, several critical areas require attention and development.
First, the empirical basis for ethical oversight must be strengthened through nested methodological studies within ongoing PCTs, particularly in underrepresented geographic regions [90]. Second, trust-building practices such as transparent communication and appropriate sharing of aggregate results must become standard components of PCT design rather than afterthoughts [90] [91]. Third, engagement frameworks need structural support and resources to bridge the gap between theoretical ideals and practical implementation [92] [90].
The ultimate goal is developing an oversight system that protects the liberty and welfare interests of participants while promoting public trust in research and enabling the conduct of socially valuable studies that can improve healthcare delivery and outcomes [6]. This requires recognizing that the function of ethical oversight should be understood broadly—not merely as protection from physical risk, but as safeguarding autonomy, promoting justice, and maintaining public trust in the research enterprise [6] [89].
As PCTs continue to evolve and expand, ethical oversight mechanisms must similarly adapt through ongoing critical evaluation, stakeholder engagement, and evidence-based refinement. Only through this dynamic process can we ensure that ethical oversight remains fit for purpose in the era of pragmatic research.
The Evidence Crisis? RCTs at the Intersection of Innovation for Cell, Gene, and Precision Therapies
Application Note: Navigating the RCT Evidence Gap for Advanced Therapies
The development of cell, gene, and precision therapies represents a paradigm shift in therapeutic intervention, moving medicine from broad population-based treatments toward highly individualized approaches. These advanced therapies offer potentially transformative health gains for serious conditions, with some achieving long-term remission or cure after a single administration [94]. However, this revolution creates a fundamental tension with traditional randomized controlled trial (RCT) methodologies, generating what has been termed an "evidence crisis" at the intersection of rapid therapeutic innovation and rigorous evidence generation.
This application note examines the specific challenges that cell, gene, and precision therapies pose to conventional RCT frameworks and explores innovative trial designs and methodologies that can bridge this evidence gap while maintaining ethical rigor. The content is framed within the broader context of RCT ethics in community settings research, emphasizing protections for vulnerable populations and appropriate integration of stakeholder perspectives [95] [23].
The Core Challenges in Evidence Generation
Methodological-Ethical Tensions
Advanced therapies create several fundamental tensions with traditional RCT methodologies:
Clinical Trial Design Conflicts: Cell and gene therapies often target rare diseases with small patient populations, making large-scale traditional RCTs statistically and practically challenging [94]. The potentially curative nature of these therapies raises ethical concerns about withholding them from control groups, while the use of single-arm trials creates challenges for establishing comparative effectiveness [94]. Additionally, the need for long-term follow-up to establish durability of effect conflicts with pressures for rapid regulatory approval and patient access.
Manufacturing and Standardization Complexities: The manufacturing processes for cell and gene therapies are notably complex and can introduce variability in the final therapeutic product [96]. For cell-based therapies like Mesenchymal Stem Cells (MSCs) and CAR-T cells, challenges include maintaining cell potency, viability, and preventing contamination throughout expansion and delivery processes [96]. Viral vectors for gene therapy, such as Adeno-Associated Viruses (AAVs) and Lentiviral Vectors (LVs), face difficulties with separating empty from full capsids and optimizing transfection conditions [96]. This manufacturing complexity creates unique challenges for ensuring product consistency across clinical trial sites and throughout extended trial durations.
Table 1: Key Manufacturing Challenges for Advanced Therapies
| Therapy Type | Manufacturing Challenge | Impact on Trial Design |
|---|---|---|
| MSC-based Cell Therapies | Donor variability, maintenance of potency during expansion, use of xenogeneic serum [96] | Requires rigorous potency assays and may limit trial scale-up |
| Viral Vector Gene Therapies (AAV, LV) | Separation of empty from full capsids, residual impurities, optimization of transfection [96] | Necessitates extensive product characterization and quality control across trial sites |
| CAR-T Cell Therapies | Quality of leukapheresis material, complex multi-step procedures, impurities [96] | Demands coordinated logistics and potentially limits trial to specialized centers |
Evidence Needs for Health Technology Assessment (HTA): HTA bodies face particular challenges in evaluating cell and gene therapies, as they must consider evidence that often deviates from traditional standards [94]. Single-arm trials without matched controls, unvalidated surrogate endpoints, and short-term follow-up data for potentially curative treatments present significant hurdles for comprehensive assessment. Additionally, economic evaluations must grapple with substantial uncertainty when extrapolating long-term outcomes from limited trial data [94].
Innovative RCT Designs and Methodological Approaches
Precision Medicine Trial Designs
Phase III biomarker-driven RCTs integrate treatment assessment with biomarker validation to identify responsive patient subpopulations [97]. Several designs have emerged to address different evidence scenarios:
Enrichment Designs: These designs restrict trial participation to biomarker-positive patients predicted to respond to treatment. This approach is statistically efficient when compelling evidence suggests treatment benefit is limited to a specific subgroup [97]. For example, the BRIM3 trial for vemurafenib in BRAF-mutated melanoma screened 2,107 patients to enroll 675 biomarker-positive participants [97].
Biomarker-Stratified Designs: These designs randomize patients within biomarker-defined subgroups, enabling simultaneous evaluation of treatment effects across different subpopulations [97]. Common strategies include:
- Subgroup-specific strategy: Tests treatment effects separately in biomarker-positive and biomarker-negative groups
- Biomarker-positive and overall strategy: Tests effects in biomarker-positive subgroup and overall population
- Sequential testing strategy: Allocates significance levels between subgroups to optimize statistical power
Adaptive Trial Designs: Platforms like I-SPY 2 for breast cancer use adaptive designs to evaluate multiple targeted therapies simultaneously within biomarker-defined subsets [98]. These trials use prospective interim analyses to modify the trial course, potentially dropping ineffective arms or reassigning randomization probabilities based on accumulating data [98].
Table 2: Biomarker-Driven Phase III RCT Designs for Precision Medicine
| Trial Design | Key Features | Indication | Evidence Requirements |
|---|---|---|---|
| Enrichment Design | Eligibility limited to biomarker-positive patients; maximizes efficiency for strong biomarker credentials [97] | BRAF-mutated melanoma (BRIM3 trial) [97] | Strong prior evidence that treatment only works in biomarker-positive subgroup |
| Biomarker-Stratified Design | Randomization within biomarker subgroups; assesses treatment effects across subpopulations [97] | KRAS wild-type colorectal cancer (PRIME trial) [97] | Strong evidence that treatment more likely to work in biomarker-positive, but potential benefit in negative subgroup |
| Adaptive Design | Interim analyses modify trial course; can drop arms or adjust randomization [98] | Neoadjuvant breast cancer (I-SPY 2) [98] | Multiple candidate therapies; need for efficient screening of promising approaches |
Pragmatic and Cluster RCT Approaches
Pragmatic RCTs conducted in real-world settings can provide complementary evidence to traditional explanatory trials, particularly for understanding effectiveness in routine practice [95] [99]. These trials face unique ethical considerations, including appropriate approaches to informed consent and protection of vulnerable participants [95] [23].
Cluster randomization, where groups rather than individuals are randomized, can be valuable for evaluating system-level interventions or when individual randomization is impractical [95]. However, this approach raises distinct ethical questions, particularly regarding the justification for cluster randomization and consent requirements, which are determined by the unit of intervention rather than the unit of randomization [95].
Ethical Framework and Community Engagement
Core Ethical Considerations
The ethical challenges in advanced therapy trials extend beyond traditional RCT considerations [23]. Interview studies with key stakeholders identify several issues of particular importance in pragmatic and community-based RCTs, including identification of relevant risks, determination of when alterations to traditional informed consent are appropriate, and clarification of what constitutes "usual care" in trial reporting [23].
The distinction between research, quality improvement, and clinical practice becomes increasingly blurred in pragmatic trials, necessitating careful consideration of what protections participants are owed [23]. Additionally, the broader range of stakeholders in these trials requires clear delineation of roles and responsibilities [23].
Patient and Community Involvement
Meaningful engagement of patients and community members throughout the research process is essential for ethical trial conduct [95] [23]. Effective patient and public involvement initiatives engage community members from the beginning in formulating research questions and can aid in patient recruitment and retention [95]. These approaches are particularly important for building trust with marginalized and underserved communities, ensuring that research addresses questions relevant to these populations, and enhancing the ethical conduct of trials in community settings [95].
Experimental Protocols
Protocol 1: Biomarker-Stratified RCT for Precision Therapies
Objective
To evaluate the efficacy of a targeted therapy in biomarker-defined patient subgroups while controlling for multiple comparisons and maintaining statistical power.
Methodology
Pre-Randomization Phase:
- Biomarker Assessment: Collect appropriate biospecimens (tissue, blood, etc.) from all potential participants prior to randomization.
- Centralized Testing: Process samples in a CLIA-certified laboratory using validated assay methods.
- Stratification: Categorize patients into predefined biomarker subgroups based on established cutpoints.
Randomization and Masking:
- Stratified Randomization: Randomize patients within each biomarker subgroup (1:1) to experimental therapy or control.
- Allocation Concealment: Utilize central web-based randomization system with dynamic balancing to maintain allocation concealment.
- Blinding: Implement double-blinding where feasible; if not possible, utilize blinded endpoint adjudication committee.
Intervention Phase:
- Treatment Administration: Administer investigational product according to predefined schedule with standardized supportive care.
- Dose Modifications: Implement protocol-defined dose modification guidelines for management of adverse events.
- Concomitant Therapies: Document all concomitant medications and therapies throughout trial participation.
Endpoint Assessment:
- Primary Endpoint: Assess primary endpoint (e.g., progression-free survival, overall survival) at protocol-defined intervals.
- Secondary Endpoints: Evaluate secondary endpoints (response rate, quality of life, biomarker dynamics) according to schedule.
- Biomarker Validation: Collect additional biospecimens at progression for correlative studies.
Statistical Analysis:
- Multiple Testing Control: Implement hierarchical testing procedure to control overall type I error.
- Subgroup Analysis: Pre-specify analysis plan for biomarker subgroups with appropriate power considerations.
- Interim Analyses: Plan prospective interim analyses with independent data monitoring committee oversight.
Ethical Considerations
- Ensure adequate informed consent process explaining biomarker testing and potential randomization outcomes
- Establish data safety monitoring board with predetermined stopping rules
- Plan for post-trial access to effective therapies, particularly for patients in control arm
- Address potential disparities in access to biomarker testing and trial participation
Protocol 2: Pragmatic Cluster RCT for Community Implementation
Objective
To evaluate the effectiveness of a community-delivered intervention (e.g., social participation program) in real-world settings using cluster randomization.
Methodology
Cluster Identification and Recruitment:
- Site Selection: Identify community organizations (clinics, community centers, etc.) that represent diverse practice settings.
- Stratification: Stratify clusters by relevant characteristics (size, patient demographics, geographic location).
- Baseline Assessment: Conduct baseline assessment of cluster characteristics and patient outcomes.
Randomization:
- Unit of Randomization: Randomize at the cluster level (organization or practice) rather than individual level.
- Balancing: Use constrained randomization to balance important prognostic factors across study arms.
- Timing: Implement randomization after baseline data collection and participant identification.
Intervention Delivery:
- Training: Provide standardized training to intervention providers with flexibility for local adaptation.
- Fidelity Monitoring: Implement systems to monitor intervention fidelity while allowing real-world adaptation.
- Usual Care Definition: Clearly define and document "usual care" in control clusters.
Data Collection:
- Routine Outcomes: Utilize routine clinical data and administrative databases where possible to enhance pragmatism.
- Patient-Reported Outcomes: Implement efficient systems for collecting patient-reported outcomes.
- Process Measures: Document implementation process, barriers, and facilitators.
Analysis:
- Cluster Adjustment: Account for intracluster correlation in sample size calculations and statistical analyses.
- Mixed Methods: Combine quantitative effectiveness measures with qualitative implementation data.
- Handling Missing Data: Pre-specify approaches for handling missing data common in pragmatic settings.
Ethical Considerations
- Justify use of cluster design based on scientific rationale and potential for intervention contamination
- Determine appropriate consent approach based on risk level and intervention characteristics
- Ensure protection of vulnerable participants within cluster settings
- Address potential conflicts between research and clinical roles in community settings
Visualization of Methodological Approaches
Biomarker-Stratified RCT Design Workflow
Diagram 1: Biomarker-Stratified RCT with Subgroup Analysis
Advanced Therapy Manufacturing and Evaluation Pathway
Diagram 2: Advanced Therapy Manufacturing and Evaluation Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for Advanced Therapy Development
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Fetal Bovine Serum (FBS) | Supplement for cell culture media providing growth factors and nutrients [96] | High batch-to-batch variability; raises safety concerns about immunological reactions; efforts to develop serum-free alternatives [96] |
| Viral Vectors (AAV, LV) | Delivery of genetic material to target cells for gene therapy approaches [96] | AAV offers low immunogenicity, high delivery efficiency; LV enables long-term transgene expression in non-dividing cells [96] |
| Plasmids (Cis/Trans-Acting) | Encoding therapeutic genes and proteins necessary for viral vector replication and capsid formation [96] | Critical for AAV manufacturing; typically requires three plasmid types for transfection into producer cell lines [96] |
| Producer Cell Lines (HEK293/HEK293T) | Generation of viral vectors through transfection with plasmid constructs [96] | HEK293T provides high titer production but raises safety concerns due to SV40 T-antigen; development of alternative lines underway [96] |
| Cell Separation Media | Isolation of specific cell populations from heterogeneous mixtures (e.g., leukapheresis material) [96] | Critical first step in CAR-T manufacturing; quality of starting material significantly impacts final product efficacy [96] |
| Biomarker Assay Kits | Detection and quantification of molecular biomarkers for patient stratification [97] | Require rigorous validation; choice of platform depends on biomarker type (genomic, proteomic, etc.) and sensitivity requirements [97] |
| Cryopreservation Media | Long-term storage of cell-based products while maintaining viability and function [96] | Essential for maintaining chain of identity and managing logistics in multicenter trials; formulation affects post-thaw recovery [96] |
The "evidence crisis" at the intersection of RCT methodology and advanced therapy innovation requires multifaceted approaches that balance scientific rigor with ethical considerations and practical realities. No single trial design or methodological approach will adequately address all challenges presented by cell, gene, and precision therapies. Rather, a toolkit of complementary approaches—including biomarker-stratified designs, adaptive platforms, and pragmatic trials—combined with innovative manufacturing solutions and comprehensive ethical frameworks, will be necessary to generate meaningful evidence for these transformative therapies.
Successful navigation of this landscape will require ongoing collaboration among researchers, clinicians, regulators, HTAs, patients, and communities to develop methodologies that are both scientifically valid and ethically sound, ultimately ensuring that promising advanced therapies can be efficiently evaluated and made available to patients who need them.
The randomized controlled trial (RCT) has long been considered the scientific gold standard for evaluating new medical interventions, prized for its ability to minimize bias and establish causal inference [21]. However, in community settings and pragmatic research contexts, traditional RCT designs often face substantial practical and ethical challenges that can limit their feasibility, efficiency, and relevance to real-world populations [100]. These challenges have stimulated the development and adoption of alternative trial designs that can better accommodate the complexities of implementation science while maintaining scientific rigor.
The ethical framework for clinical research rests on foundational principles including respect for persons, beneficence, and justice [21]. Within community-based research, these principles translate to specific requirements: ensuring genuine informed consent, minimizing harms while maximizing benefits, and fair distribution of research burdens and advantages [100]. Alternative trial designs each present distinct approaches to balancing these ethical demands against methodological requirements. Stepped-wedge cluster randomized trials, historical control trials, and adaptive designs each reconfigure the research approach to address specific ethical concerns while generating reliable evidence about interventions in real-world settings.
This article examines the ethical merits and practical applications of these three alternative designs, with particular attention to their use in community-based research. We analyze the specific ethical challenges each design presents, provide structured protocols for their implementation, and offer evidence-based recommendations for maximizing their ethical integrity while maintaining scientific validity.
Stepped-Wedge Cluster Randomized Trials
The stepped-wedge cluster randomized trial (SW-CRT) is a distinctive research design characterized by the sequential rollout of an intervention to clusters over multiple time periods [101]. In this design, all clusters begin in the control condition, and at regularly spaced intervals, a cross-sectional group of clusters transitions to the intervention condition according to a randomized schedule. This process continues until all clusters have implemented the intervention [102]. The design is particularly suited for evaluating interventions that are presumed to be beneficial and where logistical constraints prevent simultaneous implementation across all settings [101].
From an ethical perspective, the SW-CRT offers several significant advantages. First, it addresses concerns about withholding potentially beneficial interventions by ensuring that all participating clusters eventually receive the experimental intervention [103]. This feature is particularly valuable in community settings where resource constraints might otherwise prevent widespread implementation. Second, the design acknowledges practical realities of phased implementation when interventions require significant organizational change or staff training [102]. Third, by allowing simultaneous evaluation and implementation, SW-CRTs can accelerate the translation of research findings into practice, potentially benefiting communities more rapidly than traditional parallel designs [101].
Table 1: Key Ethical Considerations in Stepped-Wedge Cluster Randomized Trials
| Ethical Consideration | Ethical Challenge | Design-Based Mitigation |
|---|---|---|
| Delayed Intervention Access | Clusters randomized to later sequences experience prolonged control conditions | All clusters eventually receive intervention; careful justification of rollout sequence |
| Informed Consent | Complexities in explaining cluster-level randomization and stepped implementation | Tailored consent processes; waivers where appropriate with ethical oversight |
| Equipoise | Perception that intervention is known to be effective before trial completion | Clear evidence that genuine uncertainty exists about net intervention benefit |
| Risk-Benefit Balance | Potential harms from unproven intervention during rollout | Ongoing safety monitoring; escape mechanisms for adverse effects |
Methodological Protocol and Implementation
The successful implementation of a SW-CRT requires meticulous planning across multiple dimensions. The following protocol outlines key considerations for designing and conducting an ethically and methodologically sound stepped-wedge trial.
Cluster and Sequence Definition: Identify clearly defined clusters (e.g., schools, communities, healthcare centers) that constitute the unit of randomization. Determine the number of steps (transition points) and sequences (groups of clusters that transition together) based on both statistical requirements and practical implementation constraints [102]. Research indicates that 3-5 steps often balance statistical power with logistical feasibility in community settings.
Randomization Procedure: Develop a randomization scheme that assigns clusters to sequences using restricted or stratified randomization if needed to balance important prognostic factors. The randomization schedule should be generated by an independent statistician to prevent selection bias and implemented through a concealed allocation mechanism [101].
Timeline Development: Create a detailed timeline specifying the duration of each step, including any run-in periods for baseline measurement and wash-in phases for intervention implementation. In school-based studies, for instance, timelines must account for academic calendars and seasonal variations in outcomes [102].
Ethical Review and Consent: Seek research ethics committee review early in the design process, specifically addressing the justification for the stepped-wedge design and the approach to participant consent [103]. For individual-level participants, determine whether full consent, altered consent, or waiver of consent is appropriate based on the study risks and the practicality of obtaining individual consent [104] [101].
Data Collection Plan: Establish a data collection schedule that accounts for both outcome assessment and process evaluation measures. Consider whether an open cohort (mix of new and repeated participants), closed cohort (same participants throughout), or cross-sectional (different participants at each time point) approach best addresses the research question while minimizing participant burden [102].
Figure 1: Stepped-Wedge Cluster Randomized Trial Workflow. This diagram illustrates the sequential transition of clusters from control to intervention conditions according to a randomized schedule.
Ethical Analysis and Current Evidence
Recent systematic reviews of SW-CRTs reveal important patterns in how ethical considerations are addressed in practice. An analysis of 160 SW-CRTs published between 2016-2022 found that only 40% provided explicit justification for both cluster randomization and the stepped-wedge design [104]. This justification gap represents a significant ethical concern, as the rationale for using a complex design that delays intervention access should be clearly articulated.
The same review revealed that while 94% of trials reported research ethics committee approval, informed consent practices varied substantially. Among trials reporting on consent from patient participants, 41% did not obtain consent, with 76% of these providing justifications for this approach [104]. Common justifications included minimal risk research, impracticality of obtaining consent, and the use of routinely collected data.
The ethical defensibility of SW-CRTs often hinges on the justification for delayed rollout. In low-resource settings, where SW-CRTs are increasingly common, the design may be justified when logistical constraints prevent simultaneous implementation or when preliminary evidence suggests but does not conclusively establish intervention benefit [103]. However, researchers must carefully balance the desire to provide all participants with eventual access to the intervention against the ethical concerns of delaying access for some clusters.
Historical Control Trials
Historical control trials (HCTs) utilize previously collected data from external control groups rather than concurrently randomized controls [105]. This approach can reduce the number of participants needed for trials, accelerate research timelines, and in some cases, address ethical concerns about randomizing patients to control conditions when effective treatments exist or when diseases are serious and rare [106]. HCTs are particularly valuable in rare disease research where recruiting sufficient participants for concurrent controls may be impractical or impossible [105].
The primary ethical advantage of HCTs lies in their potential to reduce the burden on research participants by decreasing the number assigned to control groups, which may involve placebo or less effective standard care [106]. This is especially relevant in pediatric rare diseases, progressive neurological conditions, and oncology research where patient populations are small and the willingness to participate in trials with potential placebo assignment may be limited. Additionally, HCTs can make drug development for rare diseases more feasible and cost-effective, potentially encouraging investment in underserved therapeutic areas [105].
Table 2: Data Sources for Historical Controls with Applications and Limitations
| Data Source | Best Application Context | Key Limitations | Ethical Considerations |
|---|---|---|---|
| Patient Registries | Chronic diseases requiring long-term follow-up; rare conditions | Variable data quality; missing data elements | Data privacy; secondary use permissions |
| Electronic Health Records | Real-world treatment effectiveness; pragmatic studies | Unstructured data; documentation variability | Informed consent waivers; data security |
| Natural History Studies | Progressive diseases; biomarker validation | May include patients on standard care | Justification for non-intervention observation |
| Previous Clinical Trials | Drug development programs; dose optimization | Strict inclusion criteria limit generalizability | Cross-study comparability; publication bias |
Methodological Protocol and Implementation
Implementing a robust historical control trial requires rigorous methodology to ensure the validity of comparisons between current intervention groups and historical controls. The following protocol outlines key steps in this process.
Historical Control Selection: Identify potential sources of historical control data through systematic literature review, registry data, or previous clinical trials. Prioritize data sources with comparable patient populations, similar standard of care, and equivalent outcome measures collected using similar methods [105]. Assess data quality, completeness, and potential biases in the historical data.
Similarity Assessment: Document similarities and differences between the historical control population and the current trial population across key demographic, clinical, and methodological dimensions. Important factors include disease definition and staging, diagnostic criteria, background treatments, healthcare settings, and temporal trends in standard care [105]. Use standardized tools to quantify the degree of similarity between populations.
Statistical Analysis Planning: Pre-specify statistical methods that will account for potential confounding and bias in the historical comparison. These may include propensity score matching, Bayesian dynamic borrowing, or meta-analytic approaches that account between-trial heterogeneity [105] [106]. Plan sensitivity analyses to assess the robustness of findings to different methodological assumptions.
Regulatory Engagement: Engage regulatory agencies early when considering a historical control design for pivotal trials, particularly for non-randomized phase III studies [105]. Document the rationale for using historical controls rather than concurrent randomization, noting both ethical and practical justifications.
Bias Mitigation Strategy: Develop a comprehensive plan to address potential biases, including temporal trends in diagnosis or treatment, stage migration due to improved diagnostic techniques, and differences in supportive care [105]. Consider using concurrent randomization for a subset of participants to validate the historical control comparison.
Figure 2: Historical Control Trial Implementation Workflow. This diagram outlines the process for designing and conducting a trial using historical controls, emphasizing systematic assessment of data suitability.
Ethical Analysis and Current Evidence
The ethical justification for using historical controls rests on the principle of beneficence – by reducing the number of participants exposed to potentially inferior control conditions – and the principle of justice – by facilitating research in rare diseases that might otherwise not be studied [106]. However, this approach introduces distinct ethical challenges that require careful management.
A fundamental concern is the potential for bias in treatment effect estimation due to unmeasured differences between historical and concurrent populations [106]. This bias can lead to false conclusions about intervention efficacy, potentially exposing future patients to ineffective or harmful treatments. The ethical implication is clear: methodological limitations that compromise scientific validity ultimately undermine the social value of research and waste scarce resources [105].
Historical control designs are most ethically justifiable when: (1) the disease is serious and rare with high unmet medical need; (2) randomization is not practical due to patient or physician preferences; (3) the historical data are of high quality and comparable to the prospective study; and (4) the expected treatment effect is large enough to overcome residual concerns about bias [105]. In such circumstances, the use of historical controls can accelerate development of promising therapies while reducing the research burden on vulnerable populations.
Regulatory acceptance of historical control designs has been most prominent in oncology and rare diseases. For example, the drug carglumic acid (Carbaglu) for N-acetylglutamate synthase deficiency was approved based on a medical chart case series derived from fewer than 20 patients compared to historical controls, appropriate given the extremely rare nature of this condition [105].
Adaptive Trial Designs
Adaptive trial designs incorporate preplanned modifications to study parameters based on accumulating interim data without undermining the trial's validity and integrity [107]. These designs include a spectrum of adaptations, from relatively simple sample size re-estimation to complex multi-arm, multi-stage (MAMS) platforms that evaluate multiple interventions simultaneously against a shared control group.
The ethical advantages of adaptive designs primarily stem from their increased efficiency and flexibility. By allowing modification of the trial based on emerging evidence, adaptive designs can more rapidly identify effective interventions and discard ineffective ones, potentially exposing fewer participants to inferior treatments [107]. This responsive approach aligns well with the ethical principle of beneficence by maximizing the potential benefits and minimizing the harms for research participants.
MAMS designs offer particular ethical advantages when evaluating multiple potential interventions for the same condition. Rather than conducting separate trials for each intervention – each with its own control group – MAMS designs share a common control group across multiple intervention comparisons, reducing the total number of participants needed [107]. This approach accelerates the identification of promising treatments while conserving scarce research resources.
Methodological Protocol and Implementation
Implementing a robust adaptive trial requires careful planning to preserve trial integrity while building in flexibility. The following protocol outlines key considerations.
Adaptation Plan Development: Pre-specify the potential adaptations, the decision criteria for implementing them, and the timing of interim analyses. Common adaptations include: sample size re-estimation, treatment arm dropping, population enrichment, and endpoint modification [107]. Ensure that adaptation rules are sufficiently strict to maintain trial integrity.
Trial Simulation: Conduct comprehensive simulation studies to evaluate the operating characteristics of the adaptive design under various scenarios. Assess type I error control, statistical power, sample size distribution, and bias in treatment effect estimation [107]. Simulations are particularly valuable for complex adaptive designs with multiple potential decision pathways.
Independent Decision Committee: Establish an independent data monitoring committee (DMC) with authority to review interim results and implement pre-specified adaptations. Shield the investigative team from interim results to protect trial integrity and prevent operational bias [107].
Statistical Analysis Planning: Develop a detailed statistical analysis plan that accounts for the adaptive nature of the design. Pre-specify alpha spending functions for interim analyses and methods for bias correction in treatment effect estimates when appropriate [107]. For Bayesian adaptive designs, clearly specify prior distributions and decision criteria.
Operational Infrastructure: Implement robust data management systems capable of rapid data processing and quality verification. Since adaptive decisions rely on current data, efficient data capture and cleaning processes are essential for valid interim decision-making [107].
Ethical Analysis and Current Evidence
Adaptive designs present a distinctive ethical profile, offering significant potential benefits while introducing novel ethical challenges. The primary ethical advantage is the potential to maximize research efficiency, answering scientific questions more quickly with fewer participants [107]. This efficiency is particularly valuable in serious conditions with high unmet medical need, where accelerated development of effective treatments can have significant public health impact.
The use of a shared control group in MAMS designs raises specific ethical considerations. While this approach reduces the total number of participants assigned to control conditions, it also means that control participants may be compared against multiple experimental interventions [107]. The ethical justification rests on the social value of efficiently evaluating multiple interventions, provided that the control condition remains appropriate throughout the trial duration.
A key ethical challenge in adaptive designs is maintaining the validity of informed consent when the trial may change fundamentally based on interim results. Participants should be informed about the adaptive nature of the trial, including the possibility that treatment arms may be dropped or that their own assignment may change based on accumulating data [107]. This requires clear communication about complex methodological concepts, presenting challenges for the consent process.
Comparative Analysis and Research Toolkit
Direct Comparison of Alternative Designs
Table 3: Comparative Analysis of Alternative Trial Designs
| Design Feature | Stepped-Wedge CRT | Historical Control Trial | Adaptive Design |
|---|---|---|---|
| Primary Ethical Justification | All participants eventually receive intervention | Reduces participants in concurrent control groups | More efficient identification of effective treatments |
| Informed Consent Challenges | Explaining cluster randomization; delayed intervention | Understanding use of existing data; non-concurrent control | Understanding potential trial modifications during participation |
| Key Methodological Concerns | Time trends; cross-cluster contamination | Between-group comparability; temporal biases | Type I error inflation; operational bias |
| Ideal Application Context | Implementation research; health systems interventions | Rare diseases; conditions with stable natural history | Life-threatening diseases with multiple candidate interventions |
| Regulatory Considerations | Justification for delayed rollout; consent approach | Quality and relevance of historical data; bias assessment | Control of type I error; pre-specification of adaptation rules |
Statistical Software for Design: Specialized software is essential for designing alternative trials. For SW-CRTs, the Shiny CRT Calculator helps determine sample size and power accounting for both within-cluster and across-time correlations [101]. For adaptive designs, nQuery provides frameworks for simulating complex adaptive designs and evaluating their operating characteristics [107].
Ethical Framework Documentation: The Ottawa Statement on the Ethical Design and Conduct of Cluster Randomized Trials provides specific guidance for SW-CRTs, addressing justification, consent, and protection of vulnerable participants [103] [104]. For historical control trials, the DIA-ADSWG Roadmap offers practical guidance on appropriate use and bias mitigation [105].
Data Standardization Tools: When using historical controls, CDISC standards facilitate harmonization of data from different sources. For registry data, the Clinical Trials Transformation Initiative (CTTI) recommendations provide guidance on evaluating registry quality and suitability for research use [105].
Alternative trial designs represent important methodological innovations that can address persistent ethical challenges in community-based research. When appropriately selected and rigorously implemented, stepped-wedge, historical control, and adaptive designs each offer distinct pathways to balancing scientific rigor with ethical requirements in specific research contexts. The key to their ethical implementation lies in matching the design to the research question and context, providing clear justification for the approach, and implementing robust methodological safeguards against bias.
Future developments in this field will likely include refined ethical guidance specific to alternative designs, particularly as evidence accumulates about their real-world performance. The planned update to the Ottawa Statement, informed by systematic reviews of SW-CRT practice, represents an important step in this direction [104]. Additionally, methodological advances in statistical approaches for handling complex designs and integrating real-world evidence will continue to expand the ethical application of these designs.
As alternative trial designs become increasingly common in community settings, researchers must maintain focus on their ultimate ethical purpose: generating reliable evidence to improve health and healthcare while respecting the rights and welfare of research participants. By thoughtfully applying these innovative designs with attention to both methodological and ethical considerations, researchers can advance both scientific knowledge and ethical practice in community-based research.
Randomized Controlled Trials (RCTs) represent the gold standard for generating clinical evidence, but their ethical assessment has traditionally focused on pre-trial regulatory approvals and safety monitoring during conduct [108] [109]. A comprehensive ethical framework must extend beyond these conventional boundaries to encompass the entire trial lifecycle, particularly for research conducted in community settings where engagement and real-world applicability are paramount. This document establishes protocols for measuring ethical outcomes that reflect a trial's broader societal impact, community engagement, and contribution to equitable healthcare. The growing emphasis on patient and public involvement in research, as reflected in the updated SPIRIT 2025 statement, underscores the importance of integrating these considerations directly into trial design and reporting [47]. This approach aligns with evolving ethical paradigms that recognize successful research not only by its scientific findings but also by its respectful engagement with communities and contribution to sustainable healthcare improvements.
Core Ethical Outcome Domains and Measurement Framework
Defining Ethical Success in Community-Engaged Research
Ethical outcomes in community-based RCTs extend beyond traditional metrics of scientific validity and safety monitoring. The following domains represent core components of ethical success that should be measured throughout the trial lifecycle:
- Community Engagement & Partnership: Assessing the depth and quality of community involvement in trial design, conduct, and dissemination
- Participant & Community Burden: Evaluating the practical impact of trial participation on individuals and community resources
- Accessibility & Equity: Measuring how trial design and implementation affect participation across diverse populations
- Capacity Building: Documenting development of local research infrastructure and community expertise
- Translational Impact: Tracking how research findings are translated into accessible community benefits
Quantitative Metrics for Ethical Assessment
Table 1: Core Metrics for Evaluating Ethical Outcomes in Community-Based RCTs
| Domain | Quantitative Metrics | Measurement Methods | Target Values |
|---|---|---|---|
| Community Engagement | - Percentage of community stakeholders in governance roles- Number of community consultation sessions pre-trial- Budget allocation for community engagement | - Document review- Stakeholder surveys- Budget analysis | - >30% community representation |
| Participant Burden | - Time commitment for participants- Out-of-pocket expenses incurred- Drop-out rates due to logistical barriers | - Time-motion studies- Cost diaries- Retention analysis | - <2 hours/month beyond clinical care- Full reimbursement model |
| Accessibility & Equity | - Demographic representativeness compared to disease prevalence- Accessibility accommodations provided- Participation across socioeconomic strata | - Demographic analysis- Accommodation documentation- Socioeconomic indexing | - Within 10% of population prevalence |
| Capacity Building | - Local research staff trained- Community co-authorship on publications- Infrastructure improvements sustained post-trial | - Training records- Publication audit- Resource inventory | ->50% local staff |
| Translational Impact | - Community dissemination events conducted- Policy changes influenced- Clinical practice adaptations in community settings | - Event documentation- Policy tracking- Practice surveys | ->1 dissemination event per 100 participants- Documented policy input |
Experimental Protocols for Ethical Outcome Assessment
Protocol 1: Community Engagement and Partnership Assessment
Objective: To quantitatively and qualitatively evaluate the depth and effectiveness of community engagement throughout the RCT lifecycle.
Materials:
- Community stakeholder identification matrix
- Engagement tracking database
- Validated community partnership assessment tool
- Audio recording equipment for focus groups
- Qualitative analysis software
Methodology:
- Pre-Trial Phase:
- Convene a Community Advisory Board (CAB) with representation reflecting the trial's target population
- Conduct structured focus groups to review trial design, informed consent processes, and outcome measures
- Co-develop recruitment materials and strategies with CAB input
- Establish formal agreements regarding community intellectual property and data governance
Trial Conduct Phase:
- Document CAB meeting frequency, attendance, and decision-making authority
- Track incorporation of community feedback into trial modifications
- Implement systematic assessment of community satisfaction with engagement processes
- Maintain log of community-identified issues and institutional responses
Post-Trial Phase:
- Conduct paired interviews (investigators and community partners) to assess partnership quality
- Document community involvement in results interpretation, dissemination, and authorship
- Assess plans for sustaining community benefits post-trial
- Evaluate mechanisms for sharing trial results with participants in accessible formats
Analysis: Quantitative data should be analyzed using descriptive statistics and trends over time. Qualitative data from interviews and focus groups should undergo thematic analysis using a constant comparative approach. Results should be benchmarked against predefined targets for community engagement.
Protocol 2: Participant Burden and Equity Assessment
Objective: To systematically measure and minimize participant burden and ensure equitable participation across diverse groups.
Materials:
- Time-tracking applications or diaries
- Cost documentation tools
- Demographic and socioeconomic assessment questionnaires
- Accessibility audit checklist
- Geographic information system (GIS) mapping tools
Methodology:
- Burden Assessment:
- Implement time-motion studies for a subset of participants to document time commitment
- Create cost diaries for participants to record out-of-pocket expenses
- Monitor dropout reasons through structured exit interviews
- Assess opportunity costs through qualitative interviews
Equity Evaluation:
- Collect detailed demographic data and compare with community disease prevalence data
- Conduct accessibility audits of trial sites using standardized checklists
- Map participant residences relative to trial sites using GIS
- Analyze participation rates across socioeconomic strata using area-based indices
Barrier Mitigation:
- Implement and document accommodations for transportation, childcare, and missed work
- Track flexible scheduling options and after-hours availability
- Document language translation and health literacy adaptation efforts
- Monitor implementation of financial toxicity mitigation strategies
Analysis: Use regression analyses to identify predictors of high burden and participation barriers. Calculate burden scores and equity indices for regular reporting. Compare actual participation proportions with population-based expected proportions using chi-square tests.
Visualization of Ethical Framework and Implementation
Ethical Outcomes Assessment Framework
Ethical Outcomes Measurement Workflow
Table 2: Research Reagent Solutions for Ethical Outcome Assessment
| Tool/Resource | Function | Application in Ethical Assessment |
|---|---|---|
| Community Partnership Assessment Tool | Validated instrument measuring quality of community-academic partnerships | Quantifies engagement quality across multiple dimensions including communication, governance, and benefit sharing |
| Participant Burden Metric | Composite score incorporating time, cost, and inconvenience | Provides objective measure of participant burden for comparison across trials and identification of inequities |
| Equity Inclusion Index | Multi-item assessment of demographic representativeness | Evaluates how well trial participants reflect target population demographics and disease burden |
| Ethical Outcomes Dashboard | Real-time visualization of key ethical metrics | Enables continuous monitoring and prompt intervention when metrics deviate from targets |
| Stakeholder Engagement Platform | Digital platform for facilitating community input | Supports inclusive participation in trial governance through accessible communication channels |
| Cost Documentation Toolkit | Standardized tools for capturing participant expenses | Enables accurate assessment of financial burden and development of appropriate reimbursement models |
| Capacity Building Assessment | Framework for documenting research capacity development | Tracks transfer of skills, resources, and infrastructure to community partners |
Implementation Guidelines and Reporting Standards
Integrating Ethical Assessment into Existing Trial Frameworks
The ethical outcome measures outlined in this document should be integrated into standard trial protocols and reporting frameworks. Specifically:
- SPIRIT 2025 Integration: The updated SPIRIT statement includes a new item on patient and public involvement, providing a natural placement for ethical outcome measures within trial protocols [47]. Ethical outcome assessment plans should be detailed in Item 5 (Interventions) and Item 13 (Participant Flow).
- CONSORT 2025 Reporting: The CONSORT statement provides a framework for complete reporting of randomized trials [74]. Ethical outcomes should be reported in conjunction with participant flow diagrams (Item 13) and discussion of generalizability (Item 21).
- Registry Integration: Ethical outcome metrics should be specified in trial registrations to enhance transparency and accountability.
Adapting Protocols for Diverse Community Settings
The protocols presented should be adapted to specific community contexts while maintaining methodological rigor. Adaptation considerations include:
- Cultural Appropriateness: All assessment tools should be validated in specific cultural contexts and translated appropriately
- Resource Constraints: Implement tiered approaches that maintain core elements while allowing flexibility in implementation methods
- Capacity Building: Prioritize tools that simultaneously assess outcomes and build local research capacity
- Sustainability: Design assessment strategies that can be maintained with available local resources beyond the trial period
Large simple RCTs demonstrate that efficient trial designs can maintain rigor while reducing barriers to participation [110]. Similarly, ethical assessment protocols should balance comprehensiveness with practical implementability in diverse community settings.
Randomized controlled trials (RCTs) conducted within community settings represent the benchmark of original evidence in the medical field, forming the bedrock for translating hypothesized improvements in care into standard clinical practice [76]. Community-based interventions are increasingly conducted across diverse settings including pharmacies, community centers, and social service organizations, targeting complex health issues from hepatitis C virus (HPV) among people who use drugs to depression and suicidal behavior through multilevel approaches [76] [111]. The European Alliance Against Depression's 4-level intervention, for instance, simultaneously targets primary care health professionals, the general public, community facilitators, and patients with depressive symptoms through a coordinated community approach [111].
The ethical framework for such interventions extends beyond conventional research ethics, embracing guiding principles that include: "do no harm," respect people as ends rather than means, respect participants' ability to determine what they need, respect everyone's human, civil, and legal rights, and actively strive to improve situations of participants and the community [112]. As community interventions evolve to incorporate novel modalities—including digital health tools, multi-stakeholder implementations, and integrated care models—researchers face emerging ethical challenges that demand proactive, future-proofed approaches to research ethics and protocol design.
Application Notes: Ethical Framework Implementation
Core Ethical Principles for Community Intervention Trials
Community-based intervention trials operate within a complex ethical landscape that balances scientific rigor with community welfare. The following table summarizes core ethical principles and their practical application in novel community intervention contexts:
Table 1: Ethical Principles and Applications for Community-Based Trials
| Ethical Principle | Application in Novel Modalities | Stakeholder Considerations |
|---|---|---|
| Do No Harm [112] | Carefully assess whether non-intervention may be preferable; consider unintended consequences of digital tools and community disruption [112] | Community members, intervention participants, healthcare providers |
| Respect People as Ends [112] | Avoid treating participants as means to political, social, or clinical calculations; ensure genuine community benefit [112] | Participants, community organizations, vulnerable populations |
| Respect Participant Autonomy [112] | Respect participants' ability to help determine what they need; avoid presuming professional knowledge always knows best [112] | Patients, community representatives, client groups |
| Confidentiality Management [112] | Implement robust data protection for digital tools; establish clear information-sharing protocols between community partners [112] | Participants, healthcare providers, community facilitators |
| Cultural Sensitivity [112] | Adapt interventions to local cultural contexts; employ community-based participatory research methods [112] | Diverse communities, cultural groups, indigenous populations |
Data Presentation and Visualization Ethics
Ethical data presentation in community-based research requires careful consideration of audience needs and appropriate visualization techniques. The table below outlines selection criteria for data presentation methods aligned with ethical communication standards:
Table 2: Ethical Data Presentation Selection Criteria
| Presentation Method | Best Use Cases | Ethical Considerations |
|---|---|---|
| Tables [113] | When precise values are crucial; for scientific audiences requiring detailed examination; presenting multidimensional information [113] | Ensure accessibility; provide appropriate context; avoid misrepresentation through selective presentation |
| Charts/Graphs [113] | Identifying patterns and trends; presenting to general audiences; showing relationships between variables [113] | Avoid misleading scales; ensure accurate labeling; prevent oversimplification of complex issues |
| Text Summaries [114] | Explaining results and trends; providing contextual information; emphasizing key findings [114] | Maintain balance between accuracy and accessibility; avoid subjective language |
| Network Diagrams [115] | Showing interconnections between entities; mapping relationships in community partnerships [115] | Protect sensitive relational data; ensure appropriate abstraction of individual identities |
Experimental Protocols
Protocol: Ethical Stakeholder Engagement for Community RCTs
Purpose: To systematically identify and engage stakeholders in community-based randomized controlled trials, ensuring ethical implementation and sustainable partnerships.
Background: Community trials involve multiple stakeholder groups with varying interests and influences. The execution of RCTs in community settings such as pharmacies identified eight key stakeholder groups: public services/agencies; community pharmacies; communications actors; funders/sponsors; universities/research institutes; healthcare providers; suppliers; and regulators [76].
Table 3: Research Reagent Solutions: Stakeholder Engagement Toolkit
| Tool/Resource | Function | Application Context |
|---|---|---|
| Stakeholder Mapping Matrix | Identifies key stakeholders and their influence level | Initiation phase of community trials [76] |
| Community Advisory Board | Provides ongoing community perspective and oversight | All project phases; particularly important for vulnerable populations |
| Participant Burden Assessment | Evaluates and minimizes participation burden | Intervention design and protocol refinement [76] |
| Cultural Adaptation Framework | Ensures intervention appropriateness for local context | Implementation in diverse communities [111] |
| Data Sharing Agreement Templates | Establishes clear parameters for data confidentiality and use | Multi-partner collaborations involving sensitive data [112] |
Methodology:
Stakeholder Identification: Conduct systematic stakeholder analysis using collaborative mapping software (e.g., MindView) during project initiation phase [76]. Identify all potential stakeholders using the eight-category framework demonstrated in community pharmacy RCTs.
Engagement Planning: Develop tailored engagement strategies for each stakeholder group, recognizing that community pharmacies, healthcare providers, and regulatory bodies require different approaches and communication methods [76].
Ethical Safeguards Implementation:
- Establish clear confidentiality protocols specifying what information will be shared with which stakeholders, particularly when working with vulnerable populations [112].
- Implement participatory design sessions for intervention development, respecting participants' ability to help determine what they need [112].
- Create transparent communication channels for ongoing stakeholder input throughout the project lifecycle.
Evaluation and Adaptation: Continuously monitor stakeholder engagement effectiveness using process evaluation metrics and adapt strategies based on feedback, maintaining flexibility to address emerging ethical concerns.
Protocol: Ethical Digital Tool Implementation in Community Interventions
Purpose: To guide the ethical integration of digital tools (such as the iFightDepression tool for mental health) within community-based interventions, ensuring safety, efficacy, and appropriate implementation.
Background: Digital tools are increasingly incorporated into community interventions, such as the iFightDepression tool implemented as part of the European Alliance Against Depression's 4-level intervention [111]. This web-based tool, based on cognitive behavioral therapy principles, supports self-management of people with mild-to-moderate depression when guided by healthcare professionals.
Methodology:
Tool Selection and Validation:
Implementation Framework:
- Ensure adequate training for community facilitators and healthcare professionals who will guide participants in using digital tools [111].
- Integrate digital tools within broader intervention frameworks rather than as standalone solutions, creating synergistic effects across multiple intervention levels [111].
Ethical Monitoring:
- Establish clear protocols for identifying when digital tools are insufficient and higher levels of care are required.
- Implement ongoing safety monitoring, particularly for tools used with vulnerable populations.
- Maintain appropriate professional oversight while promoting self-management.
Evaluation Metrics: Track both process measures (tool usage, adherence rates) and outcome measures (clinical outcomes, participant satisfaction) to comprehensively assess tool effectiveness and ethical implementation.
Ethical Framework Visualization
The ethical implementation of community-based interventions requires navigating complex relationships between principles, stakeholders, and practical constraints. The following diagram illustrates this integrated ethical framework:
Future-proofing ethics for novel community-based intervention modalities requires proactive approaches that address emerging challenges while maintaining fidelity to core ethical principles. The integration of structured ethical protocols, systematic stakeholder engagement, appropriate data presentation methods, and flexible implementation frameworks creates a foundation for ethically sound community research. As community intervention modalities continue to evolve—incorporating digital tools, multi-level approaches, and novel settings—researchers must maintain commitment to ethical priorities that protect participants while generating valuable evidence for improving community health outcomes.
Conclusion
Conducting ethically robust RCTs in community settings requires a fundamental re-examination of traditional ethical frameworks originally designed for explanatory trials. Key takeaways include the necessity of context-sensitive approaches to consent, where simplified procedures or waivers may be justified in low-risk pragmatic trials, and the importance of redefining oversight to avoid impeding socially valuable research without compromising participant protection. Furthermore, successful implementation hinges on early and meaningful engagement with a broad range of stakeholders, including community providers and patient partners. The future of ethical community trials will be shaped by the continued evolution of pragmatic and cluster designs, the integration of real-world evidence, and the development of tailored oversight mechanisms that can efficiently review these complex studies while upholding the core principles of respect for persons, beneficence, and justice.
References
- 1. Comparison of explanatory and pragmatic design choices in... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9387034/]
- 2. Ethical and policy issues in cluster randomized trials: rationale and design of a mixed methods research study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2725043/]
- 3. Ethical issues posed by cluster randomized trials in health research | Trials | Full Text [https://trialsjournal.biomedcentral.com/articles/10.1186/1745-6215-12-100]
- 4. Differentiating Between RCTs , PCTs, and... - Rethinking Clinical Trials [https://rethinkingclinicaltrials.org/archived-what-is-a-pragmatic-clinical-trial/rcts-pcts-and-qia/]
- 5. When is informed consent required in cluster randomized trials in health research? | Trials | Full Text [https://trialsjournal.biomedcentral.com/articles/10.1186/1745-6215-12-202]
- 6. issues in Ethical randomized controlled trials: a review of... pragmatic [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-018-0253-x]
- 7. Challenges With Ethical and Pragmatic Cluster RCTs [https://healthmanagement.org/c/icu/news/ethical-challenges-with-pragmatic-and-cluster-rcts]
- 8. Ethical issues in pragmatic randomized controlled trials: a review of the... [https://link.springer.com/article/10.1186/s12910-018-0253-x]
- 9. A risk screening tool for ethical appraisal of evidence-generating... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4494793/]
- 10. ERIC - EJ1049359 - The Ethics of Randomized in... Controlled Trials [https://eric.ed.gov/?id=EJ1049359]
- 11. Chapter 15 Experimental protocols | Lab Handbook [https://ccmorey.github.io/labHandbook/experimental-protocols.html]
- 12. A guideline for reporting experimental protocols in life sciences - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5978404/]
- 13. - Wikipedia Clinical equipoise [https://en.wikipedia.org/wiki/Clinical_equipoise]
- 14. - Community and the ethics of randomized equipoise trials clinical [https://pubmed.ncbi.nlm.nih.gov/11653056/]
- 15. Equipoise, design bias, and randomized controlled trials: the elusive ethics of new drug development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC416446/]
- 16. The ethics of randomised controlled trials from the perspectives of patients, the public, and healthcare professionals - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1114158/]
- 17. within pragmatic Ethical ... considerations randomized controlled [https://pmc.ncbi.nlm.nih.gov/articles/PMC9060321/]
- 18. Safe Spaces in Research: Ethical for... - PSYFORU Considerations [https://psyforu.com/safe-spaces-in-research-ethical-considerations-for-working-with-vulnerable-populations/]
- 19. -based participatory research in rural African contexts... Community [https://publichealthreviews.biomedcentral.com/articles/10.1186/s40985-020-00145-2]
- 20. The ethics of clinical trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3894239/]
- 21. Randomized Controlled Trials: Ethical and Scientific Issues in the Choice of Placebo or Active Control - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5579903/]
- 22. Challenges and Innovations in a Community - Based Participatory... [https://pubmed.ncbi.nlm.nih.gov/27179291/]
- 23. The ethical challenges raised in the design and conduct of pragmatic... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-019-3899-x]
- 24. The ethical problem of randomization | Internal and Emergency Medicine [https://link.springer.com/article/10.1007/s11739-014-1118-z]
- 25. Using Community - Based Participatory Research to Design, Conduct... [https://www.cdc.gov/pcd/issues/2020/20_0099.htm]
- 26. Advancing patient-centered research practices in a pragmatic... [https://researchinvolvement.biomedcentral.com/articles/10.1186/s40900-023-00539-x]
- 27. Frontiers | Using Community Engagement to Inform and Implement... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2014.00027/full]
- 28. Research Democracy in a Randomized : Engaging... Controlled Trial [https://link.springer.com/chapter/10.1007/978-3-030-29286-7_16]
- 29. and regulatory complexities posed by a Ethics clinical pragmatic ... trial [https://pmc.ncbi.nlm.nih.gov/articles/PMC9641616/]
- 30. Developing a framework for the ethical design and conduct of pragmatic trials in healthcare: a mixed methods research protocol - PMC [https://ncbi.nlm.nih.gov/pmc/articles/PMC6161426/]
- 31. Framing the conversation: use of PRECIS-2 ratings to advance understanding of pragmatic trial design domains | Trials | Full Text [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-017-2267-y]
- 32. Informing real-world practice with real-world evidence: the value of... [https://biomedcentral.eu/articles/10.1186/s12916-018-1071-1]
- 33. The Method of Randomization for Cluster - Randomized Trials... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4963011/]
- 34. Cluster Randomized Trials - Rethinking Clinical Trials [https://rethinkingclinicaltrials.org/chapters/design/experimental-designs-and-randomization-schemes/cluster-randomized-trials/]
- 35. Pitfalls of and Controversies in Cluster Randomization Trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1448267/]
- 36. Key considerations for designing, conducting and analysing a cluster randomized trial - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10555937/]
- 37. in Consent - processes trials in residential... cluster randomised [https://pmc.ncbi.nlm.nih.gov/articles/PMC3710983/]
- 38. trial assessing the effects of rapid ethical... Cluster randomized [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-016-0127-z]
- 39. & Waivers of Alterations – Human Research... Informed Consent [https://irb.wisc.edu/manual/investigator-manual/conducting-human-participant-research/consent-processes-and-documentation/waivers-and-alterations-of-informed-consent/]
- 40. | Office of Research Institutional Review Board | USU Informed Consent [https://research.usu.edu/irb/informed-consent]
- 41. Changes to, or Waiver of, the DHHS or FDA... | Johns Hopkins Medicine [https://www.hopkinsmedicine.org/institutional-review-board/guidelines-policies/guidelines/waiver-alteration-consent]
- 42. Recommended format for a 'research protocol' [https://www.who.int/groups/research-ethics-review-committee/recommended-format-for-a-research-protocol/]
- 43. 3 Determining Minimal in Social and Behavioral Risk Research [https://nap.nationalacademies.org/read/18614/chapter/5]
- 44. and Unusual Usual : Existing Practice Care Groups In... Control [https://pmc.ncbi.nlm.nih.gov/articles/PMC3091006/]
- 45. considerations for Ethical developing and testing... researchers [https://pmc.ncbi.nlm.nih.gov/articles/PMC10122640/]
- 46. treatment of participants in public health Ethical research [https://jphe.amegroups.org/article/view/4312/5144]
- 47. SPIRIT 2025 statement: Updated guideline for protocols of randomised trials - PubMed [https://pubmed.ncbi.nlm.nih.gov/40294521/]
- 48. Harmonization and streamlining of research for oversight ... pragmatic [https://pubmed.ncbi.nlm.nih.gov/26374678/]
- 49. Examining study participants’ decision-making and ethics -related... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-021-00729-w]
- 50. Stakeholder views regarding ethical issues in the design and conduct... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-018-0332-z]
- 51. Visualizing implementation: contextual and organizational support mapping of stakeholders (COSMOS) | Implementation Science Communications | Full Text [https://implementationsciencecomms.biomedcentral.com/articles/10.1186/s43058-020-00030-8]
- 52. Project Stakeholder Management in the Clinical Research Environment: How to Do it Right - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4434843/]
- 53. Frontiers | Stakeholders’ engagement for improved health outcomes: a research brief to design a tool for better communication and participation [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1536753/full]
- 54. challenges in a Ethical of peer education... randomized controlled trial [https://pubmed.ncbi.nlm.nih.gov/21133786/]
- 55. Section 2: Engaging Stakeholders in a Care Management Program | Agency for Healthcare Research and Quality [https://www.ahrq.gov/patient-safety/settings/long-term-care/resource/hcbs/medicaidmgmt/mm2.html]
- 56. ’ Views about the Stakeholders of Stable Chronic... Management [https://pmc.ncbi.nlm.nih.gov/articles/PMC9231151/]
- 57. How can Stakeholder provide “Value†to Pharma? Engagement [https://www.linkedin.com/pulse/how-can-stakeholder-engagement-provide-value-pharma-salanitri-md]
- 58. A stakeholder co-design approach for developing a community ... [https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-018-2947-7]
- 59. considerations in Ethical - placebo clinical... controlled randomised [https://pmc.ncbi.nlm.nih.gov/articles/PMC5000495/]
- 60. 1.4.4 - Control and Placebo | STAT 200 Groups [https://online.stat.psu.edu/stat200/lesson/1/1.4/1.4.4]
- 61. - Placebo study - Wikipedia controlled [https://en.wikipedia.org/wiki/Placebo-controlled_study]
- 62. The ethics of using placebo in randomised : a case... controlled trials [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-018-0259-4]
- 63. for the Metformin Aneurysm Protocol ... Trial [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-021-05915-0]
- 64. Informational Graphic Contrast (Minimum) - Low Vision Accessibility Task Force [https://www.w3.org/WAI/GL/low-vision-a11y-tf/wiki/Informational_Graphic_Contrast_(Minimum)]
- 65. Colour contrast for graphical objects - ADG [https://www.accessibility-developer-guide.com/knowledge/colours-and-contrast/graphical-objects/]
- 66. “I passed the test!†Evidence of diagnostic misconception in the... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-017-0175-z]
- 67. Randomized Controlled Trial - Study Design 101 - Research Guides at George Washington University [https://guides.himmelfarb.gwu.edu/studydesign101/randomized-controlled-trial]
- 68. Using Community -Based Participatory Research Principles to Develop... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4418607/]
- 69. Types of Informed in Research Consent [https://www.infonetica.net/articles/types-of-informed-consent]
- 70. Document and Process | Human Subjects Office... Short Form Consent [https://hso.research.uiowa.edu/get-help/educational-tools/short-form-consent-document-and-process]
- 71. and public involvement in Patient design... randomised controlled trial [https://researchinvolvement.biomedcentral.com/articles/10.1186/s40900-025-00746-8]
- 72. Patient and Community Engagement Resources | NIH HEAL Initiative [https://heal.nih.gov/resources/engagement]
- 73. Patient Advocacy & Engagement: Putting Patients First | Pfizer [https://www.pfizer.com/about/responsibility/patient-advocacy-engagement-putting-patients-first]
- 74. CONSORT 2025 Statement: updated guideline ... | EQUATOR Network [https://www.equator-network.org/reporting-guidelines/consort/]
- 75. CONSORT: when and how to use it - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4520133/]
- 76. Lessons learned from two multicentre randomised ... controlled trials [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-025-09196-9]
- 77. | DLA Piper Negotiating service agreements [https://www.dlapiper.com/en/insights/publications/2020/08/negotiating-service-agreements]
- 78. Get details on negotiating | Thomson Reuters service agreements [https://legal.thomsonreuters.com/en/insights/articles/negotiating-service-agreements]
- 79. Randomized Controlled Trials in Environmental Health Research: Ethical Issues - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2653276/]
- 80. Supporting a community -led data infrastructure to build... | Brookings [https://www.brookings.edu/articles/supporting-a-community-led-data-infrastructure-to-build-local-and-equitable-governance-that-advances-policy/]
- 81. Methods for community-engaged data collection and analysis in implementation research | Implementation Science Communications | Full Text [https://implementationsciencecomms.biomedcentral.com/articles/10.1186/s43058-025-00722-z]
- 82. Exchanging words: Engaging the challenges of sharing qualitative research data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10614603/]
- 83. Realâ€World Data and Realâ€World Evidence in Regulatory Decision Making: Report Summary From the Council for International Organizations of Medical Sciences (CIOMS) Working Group XIII - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11897686/]
- 84. Randomized Controlled Trials Versus Real World Evidence: Neither... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8246742/]
- 85. Day 70: Ethics of RWE [https://www.linkedin.com/pulse/day-70-ethics-rwe-jm-biologics-z2nbe]
- 86. Considerations in Ethical RWE [https://orbitalglobalresearch.com/blog/ethical-considerations-in-rwe-balancing-privacy-security-and-advancements-in-healthcare]
- 87. Editorial: The integrity of randomized clinical trials: consensus statements from Hong Kong to Cairo - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12185446/]
- 88. engagement | Community RWE [https://www.rwe.com/en/responsibility-and-sustainability/social-affairs-and-society/community-engagement/]
- 89. Pragmatic Clinical Trials: The Ethics of Conducting Research in the Real World - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11831573/]
- 90. October 16, 2025 : New Article Surveys... - Rethinking Clinical Trials [https://rethinkingclinicaltrials.org/news/october-16-2025-new-article-surveys-landscape-of-empirical-ethics-research-related-to-pragmatic-clinical-trials/]
- 91. Considerations for Sharing Aggregate Results from Ethical ... Pragmatic [https://pmc.ncbi.nlm.nih.gov/articles/PMC11991889/]
- 92. CHALLENGES AND INNOVATIONS IN A COMMUNITY-BASED PARTICIPATORY RANDOMIZED CONTROLLED TRIAL - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5107362/]
- 93. Physicians’ perspectives regarding pragmatic clinical trials - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4975022/]
- 94. How are health technology assessment bodies responding to the... [https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-023-09494-5]
- 95. With Pragmatic and Cluster Ethical Challenges RCTs [https://healthmanagement.org/c/icu/News/ethical-challenges-with-pragmatic-and-cluster-rcts]
- 96. Manufacturing Cell and Gene : Therapies in Clinical... Challenges [https://pmc.ncbi.nlm.nih.gov/articles/PMC10961620/]
- 97. Phase III Precision Medicine Clinical Trial Designs That Integrate Treatment and Biomarker Evaluation - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7446320/]
- 98. Precision Medicine Clinical Trials: Defining New Treatment Strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4280791/]
- 99. Strengths, challenges , and strategies for implementing pragmatic... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-024-08248-w]
- 100. of alternative Ethics and methods in low-resource settings trial designs [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-019-3841-2]
- 101. - Stepped Designs - Rethinking Clinical Wedge Trials [https://rethinkingclinicaltrials.org/chapters/design/experimental-designs-and-randomization-schemes/stepped-wedge-designs/]
- 102. Designing stepped to evaluate physical activity... wedge trials [https://ijbnpa.biomedcentral.com/articles/10.1186/s12966-025-01720-z]
- 103. issues in the design and conduct of Ethical - stepped cluster... wedge [https://pubmed.ncbi.nlm.nih.gov/31852547/]
- 104. Identifying ethical issues in stepped - wedge cluster randomized trials ... [https://pubmed.ncbi.nlm.nih.gov/41241086/]
- 105. A roadmap to using historical controls in clinical trials – by Drug Information Association Adaptive Design Scientific Working Group (DIA-ADSWG) | Orphanet Journal of Rare Diseases | Full Text [https://ojrd.biomedcentral.com/articles/10.1186/s13023-020-1332-x]
- 106. Historical Controls in Randomized Clinical Trials: Opportunities and Challenges - PubMed [https://pubmed.ncbi.nlm.nih.gov/32602555/]
- 107. Flexible Clinical Trial Design [https://www.statsols.com/guides/survival-stepped-wedge-and-mams-designs]
- 108. The CONSORT statement - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6398298/]
- 109. Understanding Randomized : Design, Controlled , and... Trials Ethics [https://www.bioaccessla.com/blog/understanding-randomized-controlled-trials-design-ethics-and-impact]
- 110. Large simple randomized controlled trials—from drugs to medical devices: lessons from recent experience | Trials | Full Text [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-025-08724-x]
- 111. JMIR Research Protocols - Community - Based 4-Level Intervention ... [https://www.researchprotocols.org/2025/1/e64218]
- 112. Chapter 19., Section 5. Ethical Issues in Community ... Interventions [https://ctb.ku.edu/en/table-of-contents/analyze/choose-and-adapt-community-interventions/ethical-issues/main]
- 113. Charts vs. Tables : When to Use One Over the Other? [https://wpdatatables.com/charts-vs-tables/]
- 114. METHODS - 1.pptx DATA PRESENTATION [https://www.slideshare.net/slideshow/data-presentation-methods-1pptx/254304984]
- 115. Network diagram – from Data to Viz [https://www.data-to-viz.com/graph/network.html]