Legally Authorized Representative Informed Consent: A Comprehensive Guide for Ethical Research with Vulnerable Populations
This guide provides researchers, scientists, and drug development professionals with a comprehensive framework for the legally authorized representative (LAR) informed consent process.
Legally Authorized Representative Informed Consent: A Comprehensive Guide for Ethical Research with Vulnerable Populations
Abstract
This guide provides researchers, scientists, and drug development professionals with a comprehensive framework for the legally authorized representative (LAR) informed consent process. It covers the foundational ethical and legal principles derived from the Nuremberg Code and federal regulations, outlines practical methodological steps for implementation, addresses common challenges with vulnerable populations, and explores validation techniques to ensure comprehension and regulatory compliance. The article also discusses the implications of the 2025 FDAAA 801 Final Rule, which mandates the public posting of informed consent documents, emphasizing the growing importance of transparent, participant-centered consent processes.
The Bedrock of Ethical Research: Understanding LAR Consent and Its Legal Framework
In clinical research, the principle of informed consent is a cornerstone of ethical practice. However, a significant challenge arises when prospective adult participants lack the decision-making capacity to provide this consent due to cognitive impairment or other conditions. In these circumstances, the role of the legally authorized representative (LAR) becomes critical. An LAR is an individual or entity authorized under applicable law to consent on behalf of a prospective subject to their participation in research [1] [2]. This application note defines the LAR within the context of clinical research, delineating who qualifies for this role, the specific circumstances mandating their involvement, and the associated regulatory and ethical obligations for researchers. Establishing robust protocols for LAR consent is essential for the ethical inclusion of vulnerable populations in research, thereby advancing both scientific knowledge and patient care.
Defining the Legally Authorized Representative
Core Concept and Regulatory Basis
A Legally Authorized Representative (LAR) is an individual or judicial body empowered by law to provide informed consent for research participation on behalf of another adult who lacks the capacity to do so [1] [2]. This concept is distinct from a parent or guardian providing permission for a child to participate in research, as it pertains specifically to adults who have lost, either temporarily or permanently, the ability to make informed decisions [2].
The regulatory foundation for LARs is established in the Federal Regulations (45 CFR 46.102(c) and 21 CFR 50.3(l)), which define an LAR as an entity "authorized under applicable law to consent on behalf of a prospective subject" [1]. It is crucial to recognize that all adults are presumed competent to consent unless they have been legally adjudicated as incompetent [1]. Therefore, the use of an LAR is not based merely on a diagnosis but on a formal determination of impaired capacity.
Distinguishing LARs from Other Roles in the Consent Process
The consent process may involve several parties, and it is important to differentiate the LAR from other roles:
- LAR vs. Parent/Guardian for Minors: A parent or guardian provides permission for a child (a minor) to participate in research. An LAR, in contrast, provides consent for an adult who lacks capacity [2].
- LAR vs. Witness: A witness is an impartial observer of the consent process, often required when a participant cannot read or has a physical impediment to signing. The witness attests to the integrity of the consent process but does not make the decision for the participant [2].
- LAR vs. Healthcare Agent/Proxy: A healthcare agent, appointed through a healthcare proxy document, is a specific type of LAR. The proxy is a legally recognized document that allows a principal to designate an agent to make healthcare decisions, including research participation, upon the principal's loss of capacity [3]. Not all LARs are appointed via a proxy; many are designated by state statute based on their relationship to the patient.
Circumstances Requiring LAR Involvement
LARs are required in specific, legally-defined situations involving adults with compromised decision-making capacity. The table below summarizes the primary circumstances and the governing principles.
Table 1: Circumstances Requiring Legally Authorized Representative Consent
| Circumstance | Description | Governing Principle |
|---|---|---|
| Cognitive Impairment | Adults with conditions such as Alzheimer's disease, dementia, severe mental illness, or developmental disabilities that impair their ability to understand research and provide reasoned consent [1]. | Protection of a vulnerable population; the mental disability may compromise capacity for reasoned decision-making [1]. |
| Prospective Incapacity | For research involving subjects with progressive or fluctuating conditions (e.g., some organic brain diseases), where capacity may be lost during the study [1]. | Requires ongoing communication with the LAR and periodic re-assessment of the subject's capacity [1]. |
| Medical Emergency | In life-threatening situations where the subject is incapacitated, an LAR may be consulted for consent if it is impracticable to obtain consent from the subject and the research allows for such an exception [4]. | Justified when research has potential clinical relevance and obtaining direct consent is not feasible [4]. |
| Physical Incapacity | Rare cases where a subject has the mental capacity to consent but has a physical impediment that prevents them from documenting consent (e.g., complete paralysis). In such cases, a witness process is typically used, but an LAR may be involved if the physical condition is paired with cognitive issues [2]. | Focus on the ability to communicate a decision, not just the physical act of signing. |
It is important to note that LARs are generally not permitted to consent to certain high-sensitivity research categories. In Virginia, for example, an LAR cannot provide consent for non-therapeutic research that presents more than a minor increase over minimal risk, nor for procedures involving non-therapeutic sterilization, abortion, or psychosurgery [1]. Furthermore, any expressed objection from the prospective subject overrides the LAR's consent [1].
Qualification and Hierarchy of LARs
The qualifications for who may serve as an LAR are typically defined by state law, and the hierarchy can vary by jurisdiction. Researchers must be familiar with the laws of the state in which the research is conducted [1].
Table 2: Example Hierarchy of Legally Authorized Representatives for an Incapacitated Adult (Based on Virginia Law)
| Order of Priority | Legally Authorized Representative | Notes and Exceptions |
|---|---|---|
| 1 | Agent under an Advance Directive | The individual appointed by the subject in a healthcare proxy or advance directive, provided the document explicitly authorizes decisions regarding research participation [1] [3]. |
| 2 | Legal Guardian | A court-appointed guardian with authority to make healthcare decisions. |
| 3 | Spouse | Excludes cases where divorce proceedings have been filed and the decree is not yet final [1]. |
| 4 | Adult Child | |
| 5 | Parent | For an adult subject. |
| 6 | Adult Sibling | |
| 7 | Any other person/judicial body authorized by law | Serves as a catch-all for other specific situations defined by state statute [1]. |
Key considerations for LAR qualification:
- Conflict of Interest: Typically, the operator, administrator, or employee of a hospital may not act as an agent unless they are related to the principal. Similarly, a physician who is the subject's attending physician cannot also serve as their healthcare agent [3].
- Multiple LARs: If two or more persons with equal decision-making priority disagree about the subject's participation, the subject should not be enrolled in the research [1].
- Authority Commencement: The authority of a healthcare agent (a type of LAR) commences only after a physician or nurse practitioner makes a formal determination that the principal lacks decision-making capacity. This authority ceases if the principal regains capacity or revokes the proxy [3].
Protocols for LAR Consent and Subject Assent
Implementing a valid consent process involving an LAR requires a structured protocol to ensure ethical and regulatory compliance.
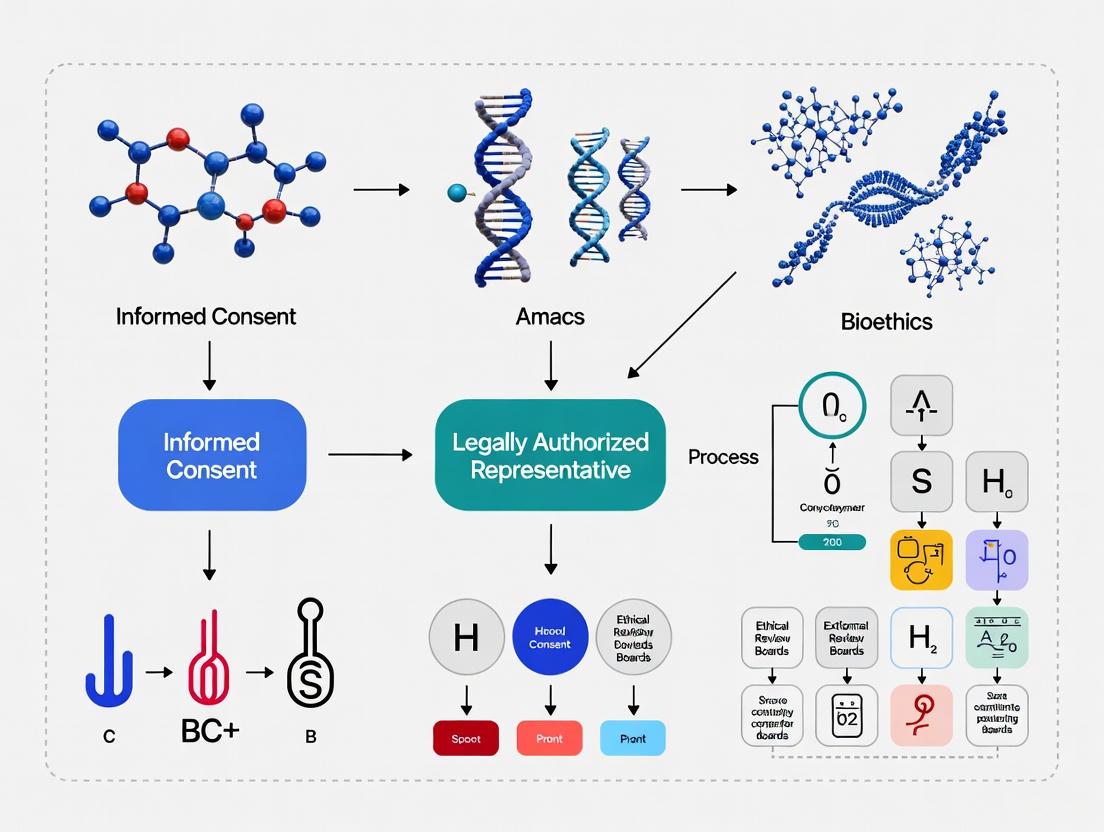
Protocol Workflow: LAR Identification and Consent Process
The following diagram visualizes the key stages of engaging a Legally Authorized Representative in the informed consent process.
Detailed Methodologies for Key Protocol Stages
1. Assessment of Decision-Making Capacity
- Purpose: To determine if a potential subject possesses the capacity to provide independent informed consent.
- Procedure: The Principal Investigator (or qualified designee) must conduct a direct assessment. The protocol submitted to the IRB must detail a specific plan for this assessment [1].
- Method: While no single standardized measure is mandated, the assessment should evaluate the subject's ability to:
- Understand the nature of the research and information relevant to participation.
- Appreciate the consequences of participation for their own situation.
- Understand the alternatives to participation.
- Reach a reasoned decision [1].
- Documentation: The assessment process and its outcome must be documented in the research record. The level of capacity required is proportional to the risks of the protocol.
2. Formal Determination of Incapacity
- Purpose: To legally trigger the authority of the LAR.
- Procedure: For a healthcare proxy to become active, a determination must be made by the subject's attending physician or attending nurse practitioner [3].
- Method: The determination must be in writing and include the clinician's opinion on the cause, nature, extent, and probable duration of the incapacity [3].
- Notification: Notice of this determination must be given to the subject (if able to understand) and to the identified LAR [3].
3. LAR Identification and Consent Discussion
- Purpose: To ensure the correct individual provides surrogate consent.
- Procedure: Consult the applicable state law hierarchy to identify the highest-ranking available LAR (see Table 2) [1].
- Method: The researcher must conduct a comprehensive informed consent discussion with the LAR, covering all elements required for the research study. The discussion must use language understandable to the LAR, and the LAR must be given sufficient time to ask questions.
- Documentation: The LAR's consent must be documented using a written consent form signed and dated by the LAR. Verbal consent from an LAR is not permissible if the study requires written consent [1]. The signature should be witnessed according to institutional policy.
4. Obtaining Subject Assent
- Purpose: To respect the autonomy of the subject, even when they lack full decision-making capacity.
- Procedure: The IRB will typically require that the assent of the subject be obtained whenever possible [1].
- Method: Actively solicit the subject's willingness to participate. Assent is defined as affirmative agreement; mere failure to object does not qualify as assent [1]. The process should be tailored to the subject's level of understanding.
- Handling Objections: If the subject objects to participation, whether to the determination of incapacity or to a decision made by the LAR, that objection prevails. The subject should not be enrolled, or if already enrolled, should be withdrawn, barring a court order to the contrary [1] [3].
The Scientist's Toolkit: Essential Materials for LAR Consent
Table 3: Research Reagent Solutions for LAR Consent Protocols
| Item | Function in the LAR Consent Process |
|---|---|
| Capacity Assessment Tool | A structured set of questions or a guide (e.g., based on the MacArthur Competence Assessment Tool for Clinical Research or similar) used by researchers to consistently evaluate a subject's understanding, appreciation, reasoning, and choice regarding the study. |
| State Statute Excerpt/Guide | A document summarizing or containing the full text of the relevant state law defining the hierarchy of who can serve as an LAR. This is crucial for proper LAR identification [1]. |
| IRB-Approved LAR Consent Form | The full-length informed consent document, identical in content to the subject version, but with a dedicated signature line for "Legally Authorized Representative," including a field to specify their legal relationship to the subject and the authority under which they are acting. |
| Subject Assent Script | A simplified, easy-to-understand explanation of the research study used to seek affirmative agreement from subjects with impaired capacity. Multiple scripts may be needed for varying levels of comprehension. |
| Documentation of Capacity Assessment & LAR Determination | A standardized form or note-to-file template for recording the outcome of the capacity assessment, the formal determination of incapacity (if applicable), and the rationale for the identified LAR. |
| Witness Protocol & Short Form Consent | A procedure and corresponding short-form consent document for use when an LAR is unable to read the primary consent form, requiring an impartial witness to the verbal consent process [2]. |
The integration of Legally Authorized Representatives into the informed consent framework is a critical safeguard for protecting the rights and welfare of potential research subjects who lack decision-making capacity. Adherence to a structured protocol—beginning with a rigorous capacity assessment, moving through the precise identification of an LAR as defined by state law, and culminating in a thorough consent process with the LAR coupled with seeking the subject's assent—is fundamental to ethical research practice. By meticulously implementing these application notes and protocols, researchers and drug development professionals can ensure the ethical enrollment of this vulnerable population, thereby upholding the highest standards of research integrity while expanding the scope of scientific inquiry.
The evolution of ethical frameworks governing human subjects research represents a critical foundation for modern clinical trial design and implementation. This application note delineates the historical trajectory from the Nuremberg Code to contemporary FDA and Common Rule regulations, providing researchers with essential context for understanding current informed consent requirements. Particular emphasis is placed on implications for research involving legally authorized representatives, a population of special significance for investigators working with vulnerable subjects or in emergency medicine contexts. The ethical principles codified over the past seven decades continue to inform protocol development, institutional review board (IRB) functions, and the legal underpinnings of human subject protections across the research continuum.
Historical Foundations: The Nuremberg Code
Origin and Context
The Nuremberg Code emerged in 1947 from the post-World War II Nuremberg Trials, specifically during the "Doctors' Trial" of 23 Nazi physicians accused of conducting brutal experiments on concentration camp prisoners [5]. The trial judges developed this 10-point statement to define ethical boundaries for medical experimentation on human beings, establishing foundational principles that would reverberate through subsequent research ethics frameworks [6] [5]. The Code was created, in part, because the Nazi doctors argued that no international laws clearly distinguished between legal and illegal human experimentation, exposing a critical regulatory gap [5].
Core Principles
The Nuremberg Code established ten foundational principles for ethical research, with voluntary consent as its cornerstone [5]. The first principle unequivocally states that "the voluntary consent of the human subject is absolutely essential," requiring that individuals have legal capacity to consent, exercise free power of choice, and possess sufficient knowledge to make an enlightened decision [6]. Additional principles emphasize that experiments should yield beneficial results for society unprocurable by other methods, should be based on animal experimentation and natural history knowledge, and should avoid unnecessary suffering [5]. The Code further establishes that risks should never exceed humanitarian importance, proper preparations must protect subjects, only qualified scientists should conduct research, subjects may terminate participation at any time, and scientists must be prepared to terminate experiments if risks materialize [5].
Table 1: Core Principles of the Nuremberg Code
| Principle Number | Key Focus | Research Implications |
|---|---|---|
| 1 | Voluntary consent | Absolute requirement for informed, voluntary participation |
| 2 | Societal benefit | Research must yield meaningful, unprocurable results |
| 3 | Animal research basis | Justification through preliminary data and animal studies |
| 4 | Avoid unnecessary suffering | Minimization of physical and mental harm |
| 5 | No expectation of death/disability | Prohibition of inherently fatal research designs |
| 6 | Risk proportional to benefit | Risk threshold determined by humanitarian importance |
| 7 | Proper preparations and facilities | Adequate infrastructure for subject protection |
| 8 | Qualified researchers | Scientific expertise requirement |
| 9 | Subject termination right | Unconditional right to withdraw without penalty |
| 10 | Investigator termination duty | Obligation to halt experiments when risks emerge |
Historical Connections and Limitations
Historical analysis reveals that the Nuremberg Code drew significantly from earlier ethical frameworks, particularly the 1931 German Guidelines for human experimentation [6]. A point-by-point comparison shows substantial similarities, with six of the ten Nuremberg principles deriving from the 1931 Guidelines [6]. This historical connection was obscured during the trials, where prosecutors appeared ignorant of these pre-existing guidelines [6]. Unlike modern ethical codes that undergo regular revision, the Nuremberg Code has remained static since its creation, limiting its direct applicability to contemporary research contexts [6].
Modern Regulatory Framework
The Common Rule
The Federal Policy for the Protection of Human Subjects, known as the Common Rule, establishes comprehensive requirements for IRB review and approval of human subjects research [7]. Recently revised with effective dates in 2018-2019, the Common Rule mandates specific consent form requirements, including that clinical trials post approved consent forms to publicly available federal websites within 60 days of the last study visit [7]. The Revised Common Rule introduces the concept of "broad consent" for storage and secondary research use of identifiable private information and biospecimens, though institutional implementation varies [7]. For multi-site research, the Common Rule generally requires use of a single IRB review to streamline oversight processes [7].
FDA Regulations
The U.S. Food and Drug Administration provides complementary regulations governing clinical research, particularly for drug and device development. Recent FDA draft guidance addresses requirements for informed consent to begin with key information and present information in a manner that facilitates understanding [8]. These provisions, which align with similar requirements in the Revised Common Rule, emphasize the importance of clear, accessible consent processes rather than merely regulatory-compliant documentation [8]. When finalized, these regulations will further harmonize FDA requirements with the Common Rule, pursuant to the 21st Century Cures Act [8].
International Harmonization
Contemporary research ethics increasingly reflect international harmonization efforts, notably through the International Council for Harmonisation (ICH) Good Clinical Practice (GCP) guidelines [9]. These international standards incorporate principles from the Nuremberg Code, Declaration of Helsinki, and other foundational documents while providing practical guidance for global research implementation [5]. The Canadian Institutes of Health Research have similarly developed a core set of 75 elements for participant consent documents, grouped into six categories to streamline consent forms while meeting regulatory requirements [9].
Comparative Analysis of Regulatory Evolution
Table 2: Evolution of Key Elements in Human Research Ethics Frameworks
| Ethical Element | Nuremberg Code (1947) | Common Rule (1991-2019) | FDA/ICH Guidelines (2024) |
|---|---|---|---|
| Consent Requirement | "Absolutely essential" voluntary consent | Written informed consent with specified elements | Beginning with key information; facilitating understanding |
| Vulnerable Populations | Not explicitly addressed | Additional protections for vulnerable subjects | Specific guidance for legally authorized representatives |
| Risk-Benefit Assessment | Risk must be justified by humanitarian importance | Minimization of risks; reasonable risk-benefit ratio | Systematic assessment of risks and benefits |
| Researcher Qualifications | "Qualified persons" requirement | IRB assessment of investigator qualifications | GCP training requirements and documentation |
| Withdrawal Rights | Unconditional right to terminate participation | Right to discontinue without penalty or loss of benefits | Clear procedures for withdrawal and data handling |
| Oversight Mechanism | Individual investigator responsibility | Institutional Review Board review and approval | IRB/IEC review plus regulatory agency oversight |
| Documentation | Implicit in consent requirement | Comprehensive documentation requirements | Written, signed, dated informed consent forms |
Legally Authorized Representatives in Research
Context and Applicability
Research involving legally authorized representatives (LARs) occurs when potential subjects lack capacity to provide independent informed consent due to cognitive impairment, developmental disability, psychiatric conditions, or medical emergencies [4]. The use of LARs represents a practical application of the ethical principle of respect for persons while enabling research participation for those who cannot consent for themselves. This approach acknowledges the relational nature of decision-making in vulnerable populations while maintaining ethical safeguards [9].
Regulatory Framework for LAR Consent
Modern regulations permit LAR consent under specific conditions. The Tri-Council Policy Statement in Canada and similar international guidelines recognize that certain research would be impossible without LAR involvement, particularly for conditions that directly impair decision-making capacity [9]. Emergency research represents a special case where consent may be obtained from LARs after initiation of study procedures, provided that strict criteria are met: the subject must have a life-threatening condition, available treatments are unproven or unsatisfactory, and obtaining prospective consent is not feasible [4]. The Common Rule specifies requirements for LAR-based consent, including that the representative have adequate authority under applicable law and that consent reflects the potential subject's presumed preferences or best interests [7].
Practical Implementation Protocol
Protocol Title: Consent Procedure Using Legally Authorized Representatives
Purpose: To establish standardized procedures for obtaining and documenting informed consent from legally authorized representatives for research subjects who lack decision-making capacity.
Materials:
- IRB-approved informed consent form designed for LAR use
- Capacity assessment tools (e.g., MacArthur Competence Assessment Tool for Clinical Research)
- Documentation of LAR authority (e.g., healthcare power of attorney, guardianship papers)
- Educational materials explaining study procedures in LAR-accessible language
Procedure:
Determine Need for LAR Involvement
- Assess potential subject's decision-making capacity using standardized tools
- Document assessment findings in research record
- Confirm absence of capacity for informed consent decision-making
Identify Appropriate LAR
- Establish hierarchy according to state law (typically: court-appointed guardian, healthcare agent, spouse, adult children, parents, adult siblings)
- Verify LAR identity and authority through documentation
- Document LAR relationship to potential subject
Consent Discussion with LAR
- Conduct consent discussion in private setting
- Present information in language appropriate to LAR's understanding
- Emphasize LAR's role as surrogate decision-maker
- Explain difference between research and clinical care
- Discuss potential risks, benefits, and alternatives
- Highlight right to withdraw subject without penalty
- Allow sufficient time for LAR questions and consideration
Documentation
- Obtain LAR signature and date on IRB-approved consent form
- Include signature of person obtaining consent
- Provide copy of signed consent form to LAR
- File original in research record
Ongoing Communication
- Provide ongoing information about study progress to LAR
- Re-consent for significant study changes or protocol modifications
- Inform LAR of new information that may affect continued participation
Special Considerations:
- When subjects regain capacity, seek direct consent for continued participation
- In emergency research, follow exception from informed consent requirements if applicable
- For pediatric populations, follow specific parental permission and child assent requirements
Research Reagent Solutions: Essential Materials for Consent Process Research
Table 3: Key Research Reagents and Materials for Informed Consent Process Studies
| Reagent/Material | Function/Application | Implementation Example |
|---|---|---|
| Validated Understanding Assessment Tools | Quantifies participant comprehension of consent information | Evaluation of key information presentation effectiveness in consent forms |
| Readability Analysis Software | Assesses reading level and complexity of consent documents | Ensuring consent forms meet recommended 6th-8th grade reading level |
| Consent Process Templates | Standardizes information disclosure across sites and studies | Implementing core consent elements identified by CIHR [9] |
| Digital Consent Platforms | Facilitates multimedia consent presentation and documentation | Testing impact of interactive content on understanding and retention |
| LAR Authority Verification Checklists | Ensures proper identification of legally authorized representatives | Standardizing documentation requirements for surrogate decision-makers |
| Vulnerable Population Assessment Tools | Identifies needs for additional consent process modifications | Adapting processes for cognitively impaired, pediatric, or non-English speaking populations |
Regulatory Evolution Pathway Visualization
Diagram Title: Evolution of Research Ethics Regulations
Legally Authorized Representative Decision Pathway
Diagram Title: LAR Consent Decision Pathway
The historical trajectory from the Nuremberg Code to contemporary FDA and Common Rule regulations demonstrates an evolving understanding of research ethics while maintaining foundational commitments to voluntary participation, comprehensive information disclosure, and subject protection. For researchers working with populations requiring legally authorized representatives, this historical context provides essential grounding for ethical protocol design and implementation. Modern frameworks have refined rather than replaced core Nuremberg principles, adapting them to complex contemporary research environments while preserving their fundamental ethical commitments. Continued attention to both historical foundations and emerging regulatory guidance remains essential for maintaining public trust and advancing ethical research practices across all participant populations.
Application Notes: Operationalizing Ethical Principles in Informed Consent
The informed consent process is a fundamental application of core ethical principles in human subjects research, serving as both a legal requirement and a continuous ethical dialogue. For research involving legally authorized representatives (LARs), who make decisions on behalf of potential participants who lack decision-making capacity, this process carries additional complexity and moral weight. The following application notes detail how the principles of respect for autonomy, beneficence, and non-domination can be operationalized when obtaining consent from LARs.
Respect for Autonomy Through the Legally Authorized Representative
Respect for autonomy recognizes the right of individuals to make informed, voluntary decisions about their own lives. When a potential research participant cannot exercise this right directly due to incapacity, the role transfers to a legally authorized representative who is entrusted to make decisions reflecting the participant's would-be wishes and best interests.
- Substituted Judgment Standard: Guide LARs to make decisions based on the participant's known values, beliefs, and prior expressed wishes, rather than the LAR's own preferences [10]. The consent process must facilitate this by helping the LAR understand what the participant would have chosen if capable.
- Voluntariness Assurance: The LAR's decision must be free from coercion, undue influence, or pressure. This is particularly crucial in emotionally stressful situations, such as when the participant is critically ill [11] [12]. Researchers must explicitly state that participation is voluntary and that declining will not affect the quality of clinical care.
- Ongoing Process: Consent is not a single event captured by a signature. It is a continuous process that should be reaffirmed throughout the study, especially if the participant's condition changes or new information emerges [13] [11]. This is vital for maintaining the autonomy of the participant through their representative.
Beneficence in Risk-Benefit Analysis and Communication
The principle of beneficence requires researchers to maximize potential benefits and minimize potential harms for the research participant. When working with LARs, this entails a rigorous and transparent risk-benefit analysis.
- Comprehensive Risk Disclosure: Clearly explain all foreseeable physical, psychological, social, and economic risks. For LARs of vulnerable individuals, this disclosure must be especially thorough and may require discussing risks specific to the participant's condition [10] [12].
- Honest Benefit Portrayal: Distinguish between direct therapeutic benefits for the participant and the broader, generalizable knowledge that may benefit future patients. Avoid the therapeutic misconception, where the LAR might mistakenly believe the primary purpose of the research is to provide direct treatment [12].
- Proportionality Assessment: The research protocol itself must be designed so that the risks are reasonable in relation to the potential benefits to the participant and the importance of the knowledge to be gained [12]. The researcher's role is to present this balance honestly to the LAR.
Non-Domination in Mitigating Power Imbalances
Non-domination, as a refinement of the justice principle, focuses on protecting individuals from arbitrary power and coercion. In the LAR consent process, this involves actively identifying and mitigating inherent power dynamics.
- Addressing Structural Vulnerabilities: LARs for individuals with cognitive impairments or rare diseases may feel particularly dependent on the healthcare system and hesitant to refuse a researcher's request [14] [10]. Researchers must be trained to create an environment where the LAR feels empowered to ask questions and decline participation.
- Combatting Therapeutic Misconception: Proactively correct the assumption that the research is solely for the participant's personal treatment. This misconception can dominate a LAR's decision-making, preventing a truly informed choice [12].
- Clarity on Legal Rights and Protections: Explicitly inform LARs of their rights, including the right to withdraw the participant from the study at any time without penalty, and the contact information for the Institutional Review Board (IRB) [11] [12]. This knowledge empowers the LAR against potential arbitrary use of power by the research institution.
Empirical data on the informed consent process helps identify areas for improvement, which is critical when the process is mediated by a LAR. The following tables summarize key findings from recent research.
Table 1: Research Staff Perspectives on the Informed Consent Process (Survey of 115 Staff) [15]
| Concern Area | Percentage of Staff Reporting | Implication for LAR Consent |
|---|---|---|
| Confidence in facilitating consent | 74.4% felt confident or very confident | Highlights need for specialized LAR training for remaining ~25% |
| Concerns about participant understanding | 56% were concerned about understanding of complex information | Suggests LAR comprehension may be similarly challenged, requiring enhanced communication |
| Perception of information materials | 63% felt information leaflets were too long and/or complicated | Underscores need for LAR-specific, plain-language summaries |
| Time constraints as a barrier | 40% felt time pressure was a barrier | LAR decisions often require more time; protocols must allocate adequate time |
Table 2: Participant Preferences in Digital Health Research Consent (Survey of 79 Participants) [16]
| Factor Influencing Preference | Impact on Preference for Modified (More Readable) Text | Application to LAR Communication |
|---|---|---|
| Character Length | Longer original text → less preference for original (P<.001) | Prioritize concise, essential information for LARs |
| Content Type | Text explaining risks significantly preferred in modified form (P=.03) | Use special care and clarity when communicating risks to LARs |
| Age | Older participants tended to prefer original text more than younger (P=.004) | Tailor communication format to the LAR's demographic; avoid assumptions |
Experimental Protocols for Ethical LAR Informed Consent
Protocol: A Multi-Method Consent Process Discussion
This protocol provides a structured methodology for the initial consent discussion between the researcher and the Legally Authorized Representative.
Objective: To ensure the LAR fully comprehends the study's purpose, procedures, risks, benefits, and alternatives, thereby enabling a decision that respects the participant's autonomy and is free from domination.
Materials:
- IRB-approved consent form and LAR information sheet.
- Visual aids (e.g., flowcharts, simplified diagrams).
- Teach-back method checklist.
- Documentation form (for noting the discussion, questions asked, and confirmation of understanding).
Workflow:
- Pre-Discussion Preparation: Provide the LAR with the consent form and a short, plain-language summary in advance of the meeting.
- Environment Setup: Conduct the discussion in a private, quiet setting with minimal interruptions. Allocate a minimum of 30-60 minutes for the discussion.
- Verbal Explanation & Dialogue:
- Introduce the study's purpose and clarify that it is research, not standard therapy.
- Systematically review all key elements of the consent form using the second person ("You have the right to...") [12].
- Use visual aids to explain complex concepts like randomization or data handling.
- Pause frequently to check for understanding and invite questions.
- Teach-Back Assessment: Ask the LAR to explain in their own words their understanding of a key aspect of the study, such as the main procedures or the primary risk [10]. This assesses comprehension more effectively than simply asking "Do you understand?"
- Documentation: After the discussion and before signature, document the key points covered, the questions raised by the LAR, and the use of the teach-back method in the participant's file or a research note [14].
Diagram 1: LAR Consent Discussion Workflow
Protocol: Evaluating and Improving Consent Form Readability
This protocol outlines a method for developing and refining consent forms to ensure they are accessible to Legally Authorized Representatives of diverse educational backgrounds.
Objective: To create consent materials that meet the recommended 6th to 8th-grade reading level and are responsive to user feedback, thereby promoting true understanding and autonomous decision-making.
Materials:
- Draft consent form.
- Readability analysis software (e.g., online readability calculators).
- Access to a panel of potential user reviewers (e.g., from a community advisory board).
Workflow:
- Initial Drafting: Compose the consent form using plain language principles: short sentences, common words, and active voice.
- Readability Analysis: Input the consent form text into readability software to obtain metrics like Flesch-Kincaid Grade Level and Reading Ease [11]. The target is ≤ 8th-grade level.
- Text Modification: Rewrite sections that exceed the target reading level. Strategies include:
- Replacing complex jargon with simpler terms.
- Breaking long sentences into shorter ones.
- Using bullet points for lists.
- User-Centered Feedback (Prototyping): Present pairs of text snippets (original vs. modified) to a small group of individuals representing the LAR demographic. Ask them to indicate their preference and explain why [16]. This identifies which versions are perceived as clearer.
- Finalization and IRB Approval: Integrate the feedback to create the final consent form and submit it, along with the readability metrics, for IRB review and approval.
The Scientist's Toolkit: Essential Reagents for Ethical Consent Research
Table 3: Key Resources for Implementing and Studying the LAR Informed Consent Process
| Tool / Resource | Function in Consent Research | Example / Application |
|---|---|---|
| Teach-Back Method | A validated health literacy tool to confirm understanding by asking individuals to explain information in their own words [10]. | After explaining study withdrawal procedures, the researcher asks the LAR, "Can you tell me in your own words what you would do if you wanted to stop the participant's involvement in the study?" |
| Readability Software | Quantitatively assesses the reading grade level and ease of written materials, such as consent forms and information sheets [16] [11]. | Using tools like the Flesch-Kincaid Grade Level test in Microsoft Word or online calculators to ensure forms meet the ≤ 8th-grade reading level target. |
| Informed Consent Checklist | A standardized list of required elements (e.g., risks, benefits, voluntariness) to ensure all are thoroughly discussed and documented [17] [12]. | Used by researchers to self-monitor the consent discussion and by IRBs to verify protocol completeness during review. |
| Verbal Consent Script | A structured script for obtaining consent verbally, often used in minimal-risk research or when written consent is impractical [14]. | Provides a standardized dialogue for phone-based consent with an LAR, ensuring consistency and completeness across participants. |
| Experimental Subject's Bill of Rights | A legally mandated document in some jurisdictions that outlines the rights of every research participant, which must be provided to the LAR [17]. | Serves as a foundational document to reinforce the principle of non-domination by explicitly stating the LAR's and participant's rights at the outset. |
Within clinical research, the ethical enrollment of participants hinges on a robust informed consent process. This process becomes complex when potential participants belong to vulnerable populations, defined as groups at an increased risk for health problems and health disparities due to a range of social, economic, and environmental factors [18]. For researchers investigating the legally authorized representative (LAR) informed consent process, a precise and systematic identification of these vulnerabilities is paramount. An LAR is an individual who provides consent on behalf of an adult who lacks the mental capacity to make decisions for themselves [2]. This protocol provides detailed application notes to aid researchers in identifying participants who may require LAR consent due to vulnerabilities impacting their decision-making capacity, thereby ensuring ethical rigor and regulatory compliance in studies focused on LAR-led informed consent.
Vulnerability in clinical research is multidimensional. It is shaped by factors such as age, education, health status, and socioeconomic conditions, which can be exacerbated by life events like abuse or neglect [18]. For the purpose of operationalizing assessments in LAR-informed consent research, vulnerabilities can be categorized into three core domains: physical, psychological, and social. Individuals often experience overlapping vulnerabilities across these domains, which compounds their risk and complicates the consent process [19]. The following tables summarize the key characteristics and prevalence data for each domain.
Table 1: Physical and Psychological Vulnerabilities
| Vulnerability Domain | Key Characteristics | Example Populations | Quantitative Insights |
|---|---|---|---|
| Physical Vulnerabilities [19] [20] | Presence of chronic illness, disability, or communication barriers that impede the ability to provide independent informed consent. | High-risk mothers & infants, the chronically ill (e.g., respiratory disease, diabetes, cancer), disabled persons, elderly, persons with HIV/AIDS [19]. | - ≈87% of those ≥65 years have ≥1 chronic condition; 67% have ≥2 [19].- Chronic conditions affect ~133M Americans (2005), projected to rise to 171M by 2030 [19]. |
| Psychological Vulnerabilities [19] [20] | Conditions affecting cognitive function, judgment, or emotional state, impairing understanding of research risks/benefits. | Persons with chronic mental conditions (schizophrenia, bipolar, major depression), alcohol/substance dependency, dementia, developmental disorders [19]. | - 17.4M (32.9%) adults with disabilities experience frequent mental distress [20].- >50% of incarcerated individuals have a mental health disorder [20]. |
Table 2: Social Vulnerabilities and Enabling Factors
| Vulnerability Domain | Key Characteristics | Example Populations | Quantitative Insights |
|---|---|---|---|
| Social Vulnerabilities [19] [20] | Social, economic, and environmental disadvantages that create barriers to healthcare and research participation. | Homeless, incarcerated, racial/ethnic minorities, LGBTQ+, immigrants/refugees, victims of human trafficking, rural residents [19] [20]. | - Nonwhite, unemployed, uninsured women (45-64) with lower income/education report poorest health [19].- Incarceration rate: 810 per 100,000 U.S. adults [20]. |
| Enabling Factors of Vulnerability [19] | Systemic and economic factors that directly limit access to care and the capacity to engage in research. | Economically disadvantaged, uninsured, those lacking a regular source of care. | - The uninsured are 7x less likely to get needed care and 4.5x more likely to not fill prescriptions [19].- 1 in 5 U.S. adults has multiple risk factors for unmet health needs [19]. |
Experimental Protocols for Assessing Vulnerability and Capacity
A standardized protocol is essential for consistently identifying vulnerabilities that may necessitate LAR consent. The following workflow provides a methodological approach for researchers specializing in the LAR informed consent process.
Diagram 1: Experimental workflow for assessing participant vulnerability and determining the need for LAR consent. LAR: Legally authorized representative.
Protocol 1: Initial Vulnerability Screening
Objective: To systematically identify participants who may have physical, psychological, or social vulnerabilities that could impair their capacity to provide independent informed consent. Materials: Study participant records, pre-screening questionnaire, vulnerability assessment checklist (derived from Tables 1 & 2). Methodology:
- Pre-Screening Questionnaire: Prior to the formal consent process, administer a questionnaire designed to identify potential vulnerabilities. This should include questions about:
- Checklist Application: Use a standardized checklist based on the vulnerability domains (Tables 1 and 2) to flag participants who meet one or more criteria. The presence of a vulnerability does not automatically preclude self-consent but triggers a formal capacity assessment. Data Analysis: Categorize identified vulnerabilities by domain (physical, psychological, social). Document the rationale for proceeding to a capacity assessment.
Protocol 2: Structured Decision-Making Capacity Assessment
Objective: To evaluate a participant's understanding, appreciation, reasoning, and ability to communicate a choice regarding research participation. Materials: MacArthur Competence Assessment Tool for Clinical Research (MacCAT-CR) or similar validated instrument, audio recorder (with consent), documentation form. Methodology:
- Structured Interview: Conduct a semi-structured interview using a validated tool like the MacCAT-CR. This assesses four key abilities:
- Understanding: Ability to comprehend the study's purpose, procedures, risks, and benefits.
- Appreciation: Ability to recognize how the research applies to one's own situation.
- Reasoning: Ability to logically weigh the options of participation versus non-participation.
- Expression of a Choice: Ability to communicate a stable decision clearly.
- Scenario-Based Questions: Present the participant with a simplified summary of the research and ask them to explain it back in their own words, state the potential downsides and benefits for themselves, and explain why they would or would not choose to participate. Data Analysis: Score the assessment based on the tool's guidelines. A finding of impaired capacity in one or more domains should trigger the initiation of the LAR consent process, in accordance with applicable state or institutional law [2] [21].
Protocol 3: LAR Identification and Consent Execution
Objective: To identify the correct Legally Authorized Representative and execute the informed consent process in accordance with regulatory and state-specific laws. Materials: Institutional policy documents, state statute guidelines (e.g., Missouri Revised Statutes 431.064 [21]), LAR consent form. Methodology:
- Hierarchy Verification: Consult applicable law to determine the order of priority for LAR designation. For example, the state of Missouri specifies the following order: spouse, adult child, parent, sibling, then relative by blood or marriage [21]. This priority order must be followed without deviation barring specific, documented circumstances (e.g., spouse is physically incapable or whereabouts unknown).
- LAR Informed Consent Process: The researcher must conduct the full informed consent discussion with the LAR. This process must include all basic elements of informed consent as per 45 CFR 46.116(a), such as a statement that the study involves research, an explanation of purposes and procedures, a description of foreseeable risks and benefits, and a statement that participation is voluntary [22].
- Documentation: The LAR must sign the IRB-approved consent document. The researcher should also document in the study records the specific rationale for using an LAR and the verification of the LAR's authority to consent [2] [21].
The Scientist's Toolkit: Research Reagent Solutions
For researchers conducting studies on the LAR informed consent process, specific tools and materials are essential for ensuring methodological rigor and ethical compliance.
Table 3: Essential Materials for LAR Informed Consent Research
| Item/Tool | Function/Benefit | Application Notes |
|---|---|---|
| Validated Capacity Assessment Tool (e.g., MacCAT-CR) | Provides a standardized, psychometrically valid method for assessing a participant's decision-making capacity. | Critical for producing objective, reproducible data on capacity impairment; strengthens research validity and defends LAR activation decisions. |
| Vulnerability Screening Checklist | Operationalizes the identification of at-risk participants based on physical, psychological, and social domains. | Ensures systematic screening across all participants; can be customized based on specific study population (e.g., geriatrics, psychiatry). |
| IRB-Approved LAR Consent Form Template | Ensures regulatory compliance by including all required elements of informed consent and signature lines for the LAR and witness if needed. | Prevents protocol deviations; templates often available via institutional IRB resource centers [2]. Must not contain exculpatory language [22]. |
| State Statute Guide on LAR Hierarchy | Provides the legally mandated order of authority for identifying a participant's LAR. | Essential for research legality; prevents consent invalidation. Researchers must use the most current version of their local statutes [21]. |
| Documentation & Audit Trail Protocol | Creates a detailed record of the screening, capacity assessment, and LAR consent process. | Serves as primary data for research on LAR processes; vital for regulatory audits and addressing IRB queries. |
Within clinical research, obtaining valid informed consent is a foundational ethical and legal requirement. This process becomes complex when potential participants have impairments affecting their decision-making abilities. A core challenge is determining when an individual lacks the capacity to provide autonomous consent, necessitating the involvement of a Legally Authorized Representative (LAR). This document provides application notes and detailed protocols for researchers on assessing patient capacity and implementing LAR-informed consent processes, framed within broader research on enhancing the ethical rigor of LAR consent.
Foundational Concepts and Definitions
A clear understanding of the distinction between key terms is essential for proper application.
Table 1: Key Definitions in Consent and Capacity
| Term | Definition | Determining Authority |
|---|---|---|
| Capacity | A functional, clinical assessment that an individual is or is not capable of making a specific medical or research decision at a given time [23]. | Qualified healthcare professional (e.g., physician, physician assistant, NP) [23]. |
| Competency | A legal status declaring an individual's ability to participate in legal proceedings; broadly referred to as "legal capacity" in modern healthcare contexts [24] [23]. | A court or judge [24] [23]. |
| Informed Consent | The systematic process of patient/participant education and decision-making regarding a treatment or research procedure, involving discussion of nature, risks, benefits, and alternatives [23]. | Researcher or clinician, following a comprehensive discussion with a capable individual or their LAR. |
| Legally Authorized Representative (LAR) | An individual or entity authorized by law to consent on behalf of a prospective participant who lacks capacity [2]. | Defined by state law; often a guardian, spouse, or family member. |
Critically, capacity is decision-specific. A patient with some cognitive impairment may retain the capacity to consent to a simple blood draw but lack the capacity to understand a complex clinical trial [24]. Capacity can also be intermittent or fluctuating, influenced by factors like medication, fatigue, or acute illness [24] [23].
Quantitative Data on Capacity and Consent Triggers
Research and clinical guidelines have identified specific triggers that should prompt a formal capacity assessment. The following table synthesizes this data for easy reference.
Table 2: Quantitative Clinical Triggers for Capacity Assessment
| Trigger Category | Specific Indicators | Rationale & Context |
|---|---|---|
| Decision-Making Patterns | - Blanket acceptance or refusal of care without rationale [23]. - Inability to voice a consistent decision [23]. - Providing excessive or inconsistent reasons for refusing care [23]. | Suggests a lack of appreciation or understanding of the situation and consequences. |
| Behavioral & Emotional State | - Hyperactivity, disruptive behavior, or agitation [23]. - Labile emotions or affect [23]. - Presence of hallucinations [23]. - Clinical intoxication [23]. | Acute behavioral health or neurological issues can temporarily impair reasoning and appreciation. |
| Cognitive & Functional Status | - New inability to perform activities of daily living [23]. - Absence of questions about complex treatment [23]. - Sensory deficits that impair understanding [24]. | Indicates a potential decline in the cognitive abilities required to process information and communicate a choice. |
Protocol for Assessing Decision-Making Capacity
This protocol provides a step-by-step methodology for conducting a clinically sound capacity assessment, based on established ethical principles and legal standards.
Experimental Protocol: Clinical Capacity Assessment
Objective: To determine if a potential research participant possesses the mental capacity to provide independent informed consent for a specific clinical trial.
Principles Governing Proportionality: The level of capacity required is proportional to the risk and complexity of the research. As the seriousness of the consequences increases, so too must the level of capacity required for a finding of competence [25]. This is often explained as balancing patient autonomy with their wellbeing, or as leaving a greater margin for error when the stakes are high [25].
Materials:
- Patient/participant medical records.
- Informed consent document for the proposed research.
- Capacity assessment checklist (e.g., based on Table 3 domains).
Procedure:
- Preparation: Review the patient's medical history, including any cognitive or psychiatric diagnoses, medications, and baseline functional status. Familiarize yourself with the key elements of the research protocol, especially risks, benefits, and alternatives.
- Environment Setup: Conduct the assessment in a quiet, private environment to minimize distractions. Ensure the participant has any necessary sensory aids (e.g., glasses, hearing aid).
- Capacity Domain Assessment: Engage the participant in a structured interview. The following table outlines the core functional domains to assess and the corresponding lines of questioning.
Table 3: Assessing the Functional Domains of Capacity
| Domain | Assessment Question | Sample Investigator Prompts |
|---|---|---|
| Understanding | Can the participant grasp the fundamental information about the research? | "Please tell me in your own words what this study involves." "What are the major risks or benefits you are expecting?" |
| Appreciation | Can the participant apply the information to their own personal situation? | "Why do you think this research is being offered to you?" "What do you believe will happen if you decide not to participate?" |
| Reasoning | Can the participant logically compare alternatives and consequences? | "Can you talk me through how you reached your decision?" "What makes this option better for you than the alternative treatments?" |
| Expression of Choice | Can the participant communicate a clear and stable decision? | "Having discussed everything, what is your decision about participating?" Re-assess consistency over a short period (e.g., after a break). |
- Documentation: Thoroughly document the assessment in the participant's record. Include the date, time, specific questions asked, the participant's responses, and the clinical justification for the final determination of capacity or lack thereof [23].
- Determination & Next Steps:
- If Capacity is Intact: The participant may proceed with the standard informed consent process.
- If Capacity is Impaired: The researcher must not proceed with enrollment based on the participant's consent. The process for seeking consent from an LAR must be initiated (see Section 5.0). If the impairment may be temporary (e.g., delirium, intoxication), the assessment should be repeated at a later time [24].
The following workflow diagram summarizes the clinical and legal pathways for determining the appropriate consent process.
Protocol for LAR-Informed Consent Process
When a participant lacks clinical capacity, the LAR becomes the decision-maker. This protocol outlines the steps for engaging an LAR.
Experimental Protocol: LAR Consent
Objective: To obtain valid informed consent for research participation from a Legally Authorized Representative on behalf of an incapacitated adult.
Materials:
- IRB-approved informed consent document.
- Signature lines for the LAR and an impartial witness (if required) [2].
- Documentation of the participant's lack of capacity.
Procedure:
- Verify LAR Authority: Confirm the individual's legal authority to serve as an LAR per state law. This may be a court-appointed guardian, a person designated in a durable power of attorney for healthcare, or a family member according to a statutory hierarchy [24].
- Conduct Consent Discussion: The individual conducting the informed consent discussion (e.g., principal investigator) must engage the LAR in a comprehensive conversation. This discussion must cover all elements of the informed consent form, including the purpose, procedures, risks, benefits, alternatives, and the voluntary nature of participation.
- Assess LAR Understanding: Employ the same principles of assessing understanding, appreciation, and reasoning as with a participant (Table 3) to ensure the LAR can fulfill their surrogate role.
- Document Consent: The LAR must sign and date the IRB-approved consent form. The individual who obtained the consent must also sign.
- Witness Involvement (if applicable): An impartial witness (e.g., a nurse not on the study team) is required in specific circumstances, such as when using a "short form" consent process for a participant who cannot read the form due to low literacy, visual impairment, or need for an unexpected translation [2]. The witness attests that the information was accurately explained and that consent was voluntary.
- Honor Participant Assent: Even when lacking capacity, the participant's wishes and feelings should be respected. If the participant objects, this objection should be honored unless the research intervention holds out the prospect of direct benefit and is unavailable outside the study [24].
The Scientist's Toolkit: Research Reagent Solutions
This table details key materials and conceptual tools essential for conducting ethical research with participants of impaired capacity.
Table 4: Essential Reagents and Tools for Capacity and Consent Research
| Item | Function & Application in Research |
|---|---|
| Structured Capacity Assessment Tools | Validated instruments (e.g., MacArthur Competence Assessment Tool for Clinical Research) provide a standardized framework for evaluating the four capacity domains, improving reliability and objectivity. |
| IRB-Approved LAR Consent Forms | Consent documents must include specific signature lines for the LAR, ensuring the legality and regulatory compliance of the surrogate consent process [2]. |
| Supported Decision-Making (SDM) Agreements | An emerging alternative to guardianship, SDM allows individuals with disabilities to retain decision-making rights with the help of trusted advisors, promoting autonomy as a less restrictive alternative [24]. |
| Impartial Witness | An individual independent of the research study who observes the consent process with an LAR or participant in specific scenarios (e.g., short-form consent) to attest to the integrity of the process [2]. |
Within the framework of legally authorized representative (LAR) informed consent process research, understanding the nuanced legal standards for evaluating consent validity is paramount. These standards establish the criteria by which courts and regulatory bodies assess whether consent was properly obtained, particularly when LARs make decisions on behalf of individuals who lack capacity. The three predominant standards—Subjective, Reasonable Patient, and Reasonable Clinician—provide distinct analytical frameworks for evaluating whether adequate information was provided and properly understood during the consent process [26] [22].
For researchers investigating LAR decision-making processes, these standards represent critical methodological frameworks for designing studies, assessing consent quality, and analyzing how surrogate decision-makers comprehend and balance risks, benefits, and alternatives when authorizing participation in research or treatment. The choice of standard significantly influences how we evaluate the effectiveness of consent processes and the adequacy of information disclosure in both clinical and research settings involving vulnerable populations.
Theoretical Foundations
The Subjective Standard
The Subjective Standard focuses exclusively on what the specific patient or LAR actually understood and considered important when providing consent. This standard requires evaluating whether the disclosure enabled that particular individual to make an informed decision based on their unique values, preferences, and circumstances [26]. Under this framework, the adequacy of information disclosure is measured against the individual's personal informational needs, regardless of whether a reasonable person would have found the disclosure sufficient.
In LAR consent research, this standard presents methodological challenges as it requires investigators to ascertain the specific decision-making factors and comprehension levels of each representative. The subjective standard aligns most closely with the philosophical foundations of informed consent that emphasize individual autonomy and respect for personal values [26]. However, its application in research is complicated by the need to document the specific understanding and priorities of each LAR, which may vary significantly across different representatives.
The Reasonable Patient Standard
The Reasonable Patient Standard establishes an objective benchmark based on the information a hypothetical "reasonable patient" would require to make an informed decision. This standard does not focus on the specific individual but rather on what information would be material to a typical patient in similar circumstances [26]. The materiality threshold encompasses any information that would significantly affect the decision-making process of a reasonable person.
This standard has gained prominence in judicial reasoning, particularly since the landmark case of Canterbury v. Spence (1972), which shifted focus from physician-centered disclosure to patient-centered information needs. For LAR consent research, this standard provides a more consistent and measurable framework for evaluating consent processes, as it establishes objective criteria for necessary disclosure elements rather than attempting to ascertain individual subjective priorities.
The Reasonable Clinician Standard
The Reasonable Clinician Standard (also known as the professional standard) evaluates consent based on what a reasonable medical professional would typically disclose under similar circumstances. This traditional approach defers to medical judgment in determining the appropriate scope and depth of information disclosure [26]. The standard reflects a more paternalistic approach to medical decision-making, where physicians retain significant discretion regarding what information to share.
In contemporary practice, this standard has been largely superseded by patient-centered approaches, though it remains influential in certain jurisdictions and specialized medical contexts. For LAR consent researchers, this standard raises important questions about the tension between professional discretion and patient autonomy, particularly when surrogates make decisions for vulnerable individuals who cannot express their own preferences.
Comparative Analysis of Legal Standards
Table 1: Comparative Analysis of Consent Legal Standards
| Evaluation Dimension | Subjective Standard | Reasonable Patient Standard | Reasonable Clinician Standard |
|---|---|---|---|
| Primary Focus | Actual understanding of specific patient/LAR | Information needs of hypothetical reasonable patient | Customary disclosure practices of medical profession |
| Measurement Approach | Individual-specific assessment | Objective, patient-centered materiality | Professional norms and customs |
| Research Methodologies | Qualitative interviews, comprehension assessment | Surveys of patient preferences, outcome studies | Practice guidelines analysis, expert consensus |
| Strengths | Maximizes individual autonomy, respects personal values | Consistent application, prevents under-disclosure | Respects clinical judgment, accounts for medical complexity |
| Limitations | Difficult to administer consistently, variable standards | May not address individual variations in preferences | Potentially paternalistic, may limit patient autonomy |
| Application in LAR Context | Assesses actual LAR understanding and decision factors | Establishes baseline disclosure requirements for surrogates | Guides professionals in LAR communication practices |
Experimental Protocols for Consent Standard Evaluation
Protocol 1: Assessing Information Comprehension Under Different Standards
Purpose: To evaluate how effectively LARs comprehend and retain essential consent information when disclosures are structured according to different legal standards.
Methodology:
- Participant Recruitment: Recruit three distinct cohorts of legally authorized representatives (n=45 each) including family members, court-appointed guardians, and healthcare agents.
- Stimulus Development: Create three parallel consent documentation sets—(1) Subjective-standard tailored communications, (2) Reasonable-patient standardized materials, and (3) Clinician-standard professional disclosures.
- Implementation: Administer pre-intervention baseline knowledge assessment, deliver standardized educational session, provide consent materials according to assigned protocol, and conduct post-intervention comprehension testing at 24 hours and 1 week.
- Metrics: Measure knowledge retention accuracy, risk-benefit understanding, alternative treatment awareness, and decision uncertainty.
Data Analysis: Employ mixed-effects modeling to account for within-subject changes over time and between-group differences in comprehension trajectories, controlling for representative characteristics and prior medical decision-making experience.
Protocol 2: Decision Quality Assessment Across Standards
Purpose: To evaluate how different consent standards influence the quality of decisions made by LARs, measured by alignment with patient values and clinical outcomes.
Methodology:
- Simulated Decision Scenarios: Develop eight complex medical decision scenarios involving common surrogate decision contexts (dementia progression, terminal illness, severe disability, etc.).
- Participant Groups: Recruit 240 LARs stratified by relationship type (spouse, adult child, parent, unrelated guardian).
- Intervention Arms: Randomize participants to receive consent information structured according to one of the three legal standards.
- Outcome Measures: Assess decision congruence with documented patient values (when available), decision confidence, regret scales, and consultation-seeking behaviors.
- Longitudinal Follow-up: Administer decision regret scale at 1-month and 3-month intervals to evaluate persistence of decision quality.
Analysis Plan: Conduct multinomial logistic regression to identify factors associated with high-quality decisions under each standard, including interaction effects between standard type and representative characteristics.
Research Reagent Solutions for Consent Studies
Table 2: Essential Research Materials for Consent Standard Investigation
| Research Tool | Specifications | Application in Consent Research |
|---|---|---|
| Decisional Conflict Scale (DSC) | 16-item validated instrument measuring personal uncertainty in healthcare decision making | Quantifies LAR decision difficulty under different consent standards |
| Modified MacArthur Competence Assessment Tool | Semi-structured interview evaluating understanding, appreciation, reasoning, and choice | Assesses LAR decision-making capacity and comprehension quality |
| LAR Information Preference Inventory | 24-item questionnaire measuring information priorities across clinical domains | Identifies disclosure elements most valued by surrogates across standards |
| Decision Regret Scale | 5-item post-decision evaluation tool measuring distress and remorse | Tracks longitudinal outcomes of consent processes under different standards |
| Standardized Patient Scenarios | Validated clinical vignettes with embedded decision conflicts | Provides consistent experimental stimuli for comparing consent standards |
| Video-Recorded Consent Encounter Protocol | Structured documentation of consent conversations with communication analysis | Enables micro-analysis of information exchange under different standards |
Integration with Legally Authorized Representative Research
The application of these three legal standards to LAR consent processes raises distinctive considerations beyond routine clinical consent. When representatives make decisions for others, the Subjective Standard must account for both the representative's understanding and their accurate representation of the patient's values and preferences [2]. This dual consideration creates complex methodological challenges for researchers evaluating consent quality in surrogate decision-making.
The Reasonable Patient Standard in LAR contexts must be adapted to consider what a reasonable surrogate would find material when making decisions for another person, accounting for the unique responsibilities and perspectives of representation [26]. This may include information about quality of life considerations, caregiving implications, and long-term prognosis that might be weighted differently when making decisions for oneself versus for another.
The Reasonable Clinician Standard applied to LAR interactions emphasizes the professional's duty to ensure representatives adequately understand the implications of decisions they are making on behalf of others [22]. This includes assessing representative comprehension and ensuring they can articulate the potential benefits, risks, and alternatives in a manner consistent with the patient's best interests and previously expressed values.
Data Synthesis and Analytical Framework
The investigation of legal standards within LAR consent research requires sophisticated analytical approaches that account for both quantitative metrics of understanding and qualitative dimensions of decision-making quality. Future research should develop integrated assessment frameworks that combine comprehension scores, value congruence measures, and longitudinal decision regret to provide comprehensive evaluation of how different standards perform in actual practice.
Research in this domain must also consider contextual factors including the type of medical decision, urgency, relationship between representative and patient, and previous experience with healthcare decision-making. These variables likely interact with consent standards to produce different outcomes across the spectrum of surrogate decision-making contexts encountered in clinical practice and research settings.
From Theory to Practice: A Step-by-Step Guide to the LAR Consent Process
Within the framework of research involving cognitively impaired populations, the process of obtaining informed consent via a Legally Authorized Representative (LAR) is a critical ethical and legal safeguard. This protocol details the systematic preparation of documents and training of research staff, a foundational element for the integrity of the LAR-informed consent process. Proper pre-consent preparation ensures compliance with federal regulations and institutional policies, protects the rights and welfare of vulnerable subjects, and enhances the reliability of research data [2] [1]. This application note provides a standardized, actionable framework for researchers and drug development professionals engaged in studies where potential subjects may lack decision-making capacity.
Foundational Concepts and Definitions
A Legally Authorized Representative (LAR) is "an individual, or judicial or other body authorized under applicable law to consent on behalf of a prospective subject to the subject’s participation in the procedure(s) involved in the research" [1]. An LAR is distinct from a parent or guardian consenting for a child, as their role is specifically for adults who lack the mental capacity to provide informed consent themselves [2].
Decision-making capacity refers to a prospective subject's ability to understand the nature of the research, the consequences of participation, and the alternatives, and to make a reasoned choice. This capacity is not a global trait but is assessed in the context of the specific research protocol, with greater capacity required for higher-risk studies [1]. The pre-consent preparation phase encompasses all activities prior to the consent discussion with an LAR, including document assembly, staff training, and planning for capacity assessment.
Document Assembly and Checklist
A comprehensive document package must be assembled before approaching an LAR. The following checklist and table summarize the core and conditional elements.
Table 1: Essential Document Checklist for LAR Informed Consent
| Document Category | Specific Elements & Requirements | Applicable Regulation/Guidance |
|---|---|---|
| Core Consent Form | - Concise Key Information summary at the beginning.- Statement that the study is research, its purpose, and expected duration.- Description of procedures and experimental components.- Reasonably foreseeable risks and discomforts.- Reasonably expected benefits to the subject or others.- Disclosure of alternative procedures.- Confidentiality statement regarding records.- Compensation and treatment information for research-related injuries.- Contact information for questions and research-related injuries.- Voluntary participation statement. | Revised Common Rule [27] |
| Supporting Documents | - IRB-approved protocol for staff reference.- Capacity assessment tool or guide, if applicable.- LAR identity and authority verification form.- Study information sheets or visual aids for the LAR/subject. | FDA Regulations [28] |
| Conditional Elements | - Statement on unforeseeable risks to a subject or embryo/fetus.- Circumstances for termination of participation.- Details of any payment to the subject.- Additional costs to the subject.- Consequences of withdrawal from research.- Statement on provision of significant new findings.- Approximate number of subjects in the study.- Statements on commercial profit from biospecimens and disclosure of research results. | IU HRPP Guidance [27] |
Additional conditional elements are required for specific types of research. For genetic studies, the consent must include statements about the potential for commercial profit from biospecimens and whether the subject will share in those profits, as well as information about whole genome sequencing [27]. For NIH-funded research generating large-scale genomic data, specific language regarding data sharing, de-identification, and potential risks of re-identification must be incorporated [27].
Staff Training Protocols and Competencies
Research staff involved in the LAR consent process must undergo standardized training beyond standard human subjects protection education. The training should be documented for each staff member.
Table 2: Essential Staff Training Modules and Competencies
| Training Module | Key Content | Method of Assessment |
|---|---|---|
| LAR Regulations & Hierarchy | - Definition of LAR versus guardian for a minor.- Understanding the state-specific hierarchy of LAR authority (e.g., agent under advance directive, legal guardian, spouse, adult child, parent).- Conditions limiting LAR use in your jurisdiction. | Written quiz or certification based on state law and institutional policy [1]. |
| Capacity Assessment | - Protocols for assessing a subject's decision-making capacity.- Evaluating understanding of research, consequences, and alternatives.- Differentiating between capacity for low-risk and high-risk protocols. | Observed structured clinical evaluation (OSCE) or role-playing scenarios [1]. |
| Effective Communication & The Consent Discussion | - Using lay language (8th-grade reading level or lower).- Employing the "teach-back" method to confirm LAR understanding.- Discussing procedure-specific risks and benefits realistically.- Managing the consent discussion with diverse populations (non-English speakers, those with low health literacy). | Direct observation of mock consent sessions with standardized LARs; evaluation of drafted consent documents for readability [29] [27]. |
| Documentation & Compliance | - Procedures for obtaining and witnessing signatures.- Handling version control of consent forms.- Processes for secure storage and retention of consent documents (typically at least 7 years).- Correcting errors in documentation. | Audit of simulated study files for compliance with documentation standards [2] [30]. |
Training must emphasize effective communication strategies. Staff should be proficient in using simple, non-technical language and avoiding complex medical jargon. The "teach-back" method, where the LAR is asked to explain the key information in their own words, is a critical technique for verifying comprehension [29]. Furthermore, staff must be trained to conduct these discussions in a manner that minimizes the possibility of coercion or undue influence, ensuring the LAR's decision is truly voluntary [4] [27].
Experimental Protocol for Pre-Consent Workflow
The following detailed protocol outlines the steps from initial planning to the final readiness for the LAR consent interview.
Protocol: Pre-Consent Preparation for LAR Process
Objective: To ensure all documents are compliant and all research staff are trained and competent before initiating the informed consent process with a Legally Authorized Representative.
Materials: Institutional Review Board (IRB)-approved study protocol, IRB-approved informed consent form(s), LAR hierarchy guide per state law, capacity assessment tool, staff training manuals, signature logs, and secure document storage system.
Procedure:
- Document Finalization (Lead: Principal Investigator):
- Confirm that the most recent IRB-approved version of the consent form is available.
- Verify the consent form begins with a "concise and focused presentation" of key information as required by the Revised Common Rule for federally-funded research [27].
- Assemble the complete document package as outlined in Table 1.
Staff Identification and Training (Lead: Study Coordinator):
- Identify all research staff (e.g., investigators, study coordinators, clinical nurses) who will be involved in assessing capacity, approaching potential LARs, or conducting the consent discussion.
- Enroll identified staff in the training modules described in Table 2.
- Document completion and successful assessment for each staff member. Only staff who have completed training should engage in the consent process.
Verification and Quality Control (Lead: QA Manager or PI):
- Conduct a pre-initiation audit to ensure:
- Consent form versions match the IRB-approved version.
- Staff training records are complete.
- The process for verifying LAR identity and authority is clear.
- Resolve any discrepancies before the enrollment of any potential subject requiring an LAR.
- Conduct a pre-initiation audit to ensure:
Troubleshooting:
- Problem: An LAR is not available or cannot be identified from the hierarchy.
- Solution: Halt the enrollment process for that subject. Consult the IRB and legal counsel for guidance before proceeding.
- Problem: A potential subject objects to participation, despite LAR willingness.
- Solution: Per federal regulations and Virginia state law, the subject must not be enrolled. The objection of the prospective subject must be respected [1].
- Problem: Two LARs with equal priority (e.g., two adult children) disagree on participation.
- Solution: Do not enroll the subject. The disagreement prohibits enrollment [1].
Workflow Visualization
The following diagram illustrates the logical sequence and decision points in the pre-consent preparation phase.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for LAR Consent Process Implementation
| Item | Function in Pre-Consent Preparation |
|---|---|
| IRB-Approved Informed Consent Template | Provides a regulatory-compliant structure for creating the study-specific consent form, ensuring all required elements are included [27]. |
| State Statute on LAR Hierarchy | Legally defines the order of individuals authorized to provide surrogate consent, preventing improper delegation of consent authority [1]. |
| Readability Analysis Tool | Assesses the reading grade level of the consent form to ensure it is written in lay language (e.g., 8th-grade level) for better comprehension [27]. |
| Capacity Assessment Guide | A standardized tool or set of questions to help staff consistently evaluate a potential subject's decision-making capacity [1]. |
| Secure Document Management Platform | A HIPAA-compliant system for storing and managing versions of consent forms, training records, and signed consent documents [30] [31]. |
| "Teach-Back" Method Guide | A communication aid that trains staff to confirm LAR understanding by having them explain the information back in their own words [29]. |
Rigorous pre-consent preparation is a non-negotiable prerequisite for ethically and legally sound research involving Legally Authorized Representatives. By systematically assembling compliant documents, training staff to a high level of competency, and implementing a verified workflow, research teams can uphold the principle of respect for persons and ensure the validity of the informed consent process for vulnerable populations. This protocol provides a replicable framework to achieve these critical objectives.
Within the critical framework of legally authorized representative (LAR) informed consent process research, the consent form itself serves as the foundational document ensuring ethical and regulatory compliance. For researchers, scientists, and drug development professionals, crafting a consent form that is both legally robust and accessible is paramount, particularly when the consent process involves surrogate decision-makers for vulnerable populations. This document transitions from a mere regulatory requirement to a vital tool for autonomy protection and transparent communication. This application note delineates the essential elements of a compliant consent form, emphasizing the specific disclosures required when an LAR is involved and mandating the use of plain language to ensure genuine understanding by all parties, including the LAR and the participant for whom they are deciding.
Regulatory Framework & Core Components
The informed consent process is governed by a multi-faceted regulatory landscape, including FDA regulations [32] and the Common Rule. The foundational principle is that informed consent is a continuous process, not a single signature event, starting with recruitment and continuing through the study's conclusion [32]. This is especially critical in LAR-based consent, where the representative must be kept apprised of any significant new findings that might affect the participant's continued involvement [32].
The table below summarizes the mandatory basic and additional elements of informed consent as per current FDA guidance, which builds upon longstanding regulatory requirements [32].
Table 1: Essential Elements of a Compliant Informed Consent Form
| Element Category | Element Description | Key Considerations for LAR Consent |
|---|---|---|
| Basic Elements | Explanation of the research purpose, procedures, and duration [32] | The LAR must understand the procedures to which the participant will be subjected. |
| Description of reasonably foreseeable risks and discomforts [32] | Must include risks of unintended private information disclosure [32]. | |
| Description of any benefits to the subject or others [32] | For comparative studies, benefits of standard care can be described generally in the form and in detail during the discussion [32]. | |
| Disclosure of appropriate alternative procedures [32] | The final FDA guidance recommends disclosing alternatives during the consent discussion rather than necessarily within the form itself [32]. | |
| Statement on confidentiality [32] | Must explain measures to protect privacy and their limitations; Certificates of Confidentiality are pertinent [32]. | |
| Explanation of compensation, medical treatment, and contacts for injuries [32] | Must be clearly stated. | |
| Information on financial conflicts of interest [32] | The IRB determines if financial interests of involved parties must be disclosed [32]. | |
| Additional Elements | Statement on unforeseeable risks [32] | May include discussion of birth control measures and pregnancy notification [32]. |
| Anticipated circumstances for termination without subject's consent | Clearly outline conditions under which the investigator may terminate participation. | |
| Additional costs to the subject [32] | Must detail protocol requirements and time commitment so the LAR can appreciate associated costs [32]. | |
| Consequences of a subject's decision to withdraw [32] | Counsel LARs that they should not enroll the participant if they do not foresee completing the study [32]. | |
| Statement that significant new findings will be provided [32] | This includes interim analyses, new efficacy data, or new alternative treatments [32]. |
The Legally Authorized Representative (LAR) in Practice
Definition and Distinctions
A Legally Authorized Representative (LAR) is an individual or entity authorized under applicable law to consent on behalf of a prospective adult participant who lacks the mental capacity to provide informed consent themselves [2] [1]. It is crucial to distinguish an LAR from a parent or guardian consenting for a child, which involves a different regulatory and ethical paradigm [2]. The use of an LAR, or surrogate consent, is reserved for adults with cognitive impairments—such as those caused by Alzheimer's disease, dementia, or mental illness—that compromise their capacity for reasoned decision-making [1].
Determination of Capacity and LAR Hierarchy
A protocol involving potential LAR consent must include a specific, IRB-approved plan for assessing the decision-making capacity of the prospective subject [1]. This assessment, conducted by the investigator, evaluates the individual's ability to understand the nature of the research, the consequences of participation, and the alternatives [1]. The following diagram illustrates the logical workflow for determining the need for and obtaining LAR consent.
The hierarchy of who can serve as an LAR is defined by state law. For example, Virginia law specifies the following order of priority: 1) an agent under an advance directive, 2) a legal guardian, 3) a spouse, 4) an adult child, 5) a parent, 6) an adult sibling, or 7) any other person or body authorized by law [1]. It is critical that researchers understand the specific LAR laws in the jurisdiction where the research is conducted [1].
Assent and Ongoing Communication
Even when an LAR provides formal consent, the research team must invite the participant's involvement in the consent discussion. For subjects with fluctuating or limited capacity, investigators should seek their affirmative assent—defined as a positive agreement, not merely the absence of objection [1]. Furthermore, investigators should establish and maintain ongoing communication with the LAR and involved caregivers throughout the study, consistent with the subject's autonomy and medical confidentiality [1].
Experimental Protocol: Implementing a Compliant LAR Consent Process
Protocol: Assessment of Decision-Making Capacity and LAR Consent
Objective: To systematically assess the decision-making capacity of prospective adult research subjects with cognitive impairments and, where appropriate, obtain valid informed consent from a legally authorized representative while respecting the autonomy of the subject.
Table 2: Research Reagent Solutions for LAR Consent Research
| Item/Tool | Function/Explanation |
|---|---|
| Capacity Assessment Plan | An IRB-approved, protocol-specific set of questions and criteria to evaluate a subject's understanding of the research and its consequences [1]. |
| State Statute Reference | The official state law defining the hierarchy of who can serve as an LAR; essential for determining the correct representative [1]. |
| LAR-Specific Consent Form | The full-length IRB-approved consent document containing all required elements, with signature lines for the LAR and a witness if required [2]. |
| Assent Script | A simplified, age- and capacity-appropriate explanation of the research used to seek affirmative agreement from the subject [1]. |
| Short Form Consent Document | Used when an unexpected translation need or literacy barrier arises with an LAR, requiring an impartial witness to the verbal consent process [2]. |
Methodology:
- Pre-Screening and Identification: Within the study protocol, pre-define the population for which LAR consent is a possibility (e.g., patients diagnosed with moderate to severe dementia). During recruitment, flag potential subjects who meet these criteria.
- Capacity Assessment: For any subject identified as potentially impaired, the Principal Investigator (or qualified, trained designee) will conduct a formal capacity assessment. The assessment will evaluate the subject's ability to:
- Understand the nature of the research and the information relevant to their participation.
- Appreciate the consequences of participation for their own situation.
- Understand the consequences of the alternatives to participation [1].
- Note: The required level of understanding may be proportionate to the risks of the protocol [1].
- LAR Identification and Verification: If a subject is determined to lack capacity, the research team will identify the individual with the highest priority to act as LAR according to the applicable state law [1]. The team will document the basis for this determination and the LAR's relationship to the subject.
- The LAR Consent Discussion: Conduct the informed consent process with the LAR. This must be a full, interactive discussion using the IRB-approved consent form. The discussion should cover all basic and additional elements of consent, with special emphasis on:
- Subject Assent: The subject must be invited to participate in the consent discussion to the greatest extent possible. The investigator must seek the subject's affirmative assent. A subject's objection to participation is binding, regardless of LAR consent [1].
- Documentation: The LAR must sign and date the current IRB-approved consent form. The signature must be witnessed according to IRB policy and state law. For subjects providing assent, their verbal agreement or signature (if capable) should be documented in a note to file or on an assent form. If a subject lacks capacity but is physically able to sign, they may be invited to provide a signature as a mark of assent alongside the LAR's signature [1].
- Ongoing Communication: Throughout the study, the investigator must maintain communication with the LAR, providing any new information that may impact the subject's willingness to continue [32]. The subject's capacity should be re-assessed for longer-term studies, as appropriate.
Plain Language and Accessible Presentation
Regulatory guidance emphasizes that the consent form is only one part of the broader consent process, which is designed to provide information to aid a subject's decision [32]. Using plain language is a legal and ethical imperative.
Best Practices for Plain Language Implementation:
- Simplify Language: Use words familiar to a layperson. Replace "myocardial infarction" with "heart attack," and "contraindication" with "reason not to take." Aim for an 8th-grade reading level [33].
- Structure for Readability: Use short sentences and paragraphs. Employ bulleted lists and clear subheadings (like those in this document) to break up dense text. A structured summary can greatly enhance comprehension [34].
- Offer Multilingual Options: With over 65 million Americans speaking a language other than English at home, providing consent forms in multiple languages is critical. Use certified medical translators for accuracy [33].
- Utilize Visual Aids: The FDA final guidance notes that pictures, diagrams, and other visual aids can be used to improve understanding of complex research procedures during the consent discussion [32].
- Digital Consent Platforms: Digital management systems can streamline the process, ensure all required elements are included, and incorporate multimedia (e.g., videos, interactive quizzes) to enhance understanding and document comprehension [33].
The creation of a compliant consent form for use in a legally authorized representative context demands a meticulous, multi-disciplinary approach. It requires a deep understanding of the regulatory requirements for both content and process, a commitment to ethical principles of respect for persons and justice, and the skillful application of plain language and accessible presentation techniques. For researchers and drug development professionals, mastering this process is not merely about satisfying IRB review; it is about upholding the highest standards of ethical research and ensuring the trust and safety of some of the most vulnerable participants in clinical science. By adhering to the structured protocols and best practices outlined in this application note, research teams can ensure their work is built upon a foundation of truly informed and ethically sound consent.
Within the framework of research on informed consent processes, the interview with a Legally Authorized Representative (LAR) presents unique challenges and ethical imperatives. An LAR, tasked with providing consent on behalf of a potential subject who lacks capacity to do so independently, operates under conditions of significant emotional and decisional burden. The primary objective of the consent interview is therefore not merely the transactional completion of a form, but the establishment of a supportive environment that facilitates genuine understanding and autonomous decision-making. This document outlines application notes and detailed protocols for conducting these critical interactions, providing researchers with structured methodologies to ensure ethical rigor and participant protection.
Data Presentation: Interview Typologies and Considerations
The approach to a consent interview is contingent on its formality, setting, and the specific information collected. The following tables summarize key structural and ethical considerations.
Table 1: Comparison of Consent Interview Modalities
| Feature | Casual Interview | Formal Interview | Group Interview / Focus Group |
|---|---|---|---|
| Setting | Public area, informal [35] | Private setting [35] | Group setting [35] |
| Structure | Short, conversational [35] | Detailed, appointment-based [35] | Guided group discussion [35] |
| Identifiable Information | Generally not collected [35] | Likely collected [35] | Collected, but confidentiality cannot be guaranteed [35] |
| Consent Process | Oral consent/disclosure [35] | Formal written or oral consent [35] | Formal consent required [35] |
| Recording | Not appropriate (written notes only) [35] | Acceptable with permission (audio, video) [35] | Acceptable with permission [35] |
| Primary Risk Consideration | Minimally risky topics [35] | Potential for more than minimal risk; plan for sensitive topics [35] | Lack of privacy and confidentiality [35] |
Table 2: Digital Interview Platform Security Considerations
| Security Feature | Implementation Best Practice |
|---|---|
| Platform Selection | Use institution-approved platforms (e.g., Zoom, Google Meet) [35]. |
| Access Control | Utilize waiting rooms and require passwords to prevent unauthorized entry [35]. |
| Data Encryption | Ensure in-transit and at-rest encryption for data protection [35]. |
| Researcher Training | Become familiar with the platform's security features before the interview [35]. |
Experimental Protocols
Protocol for a Formal LAR Consent Interview
This protocol provides a step-by-step methodology for conducting a formal consent interview with an LAR.
I. Pre-Interview Preparation (Researcher Responsibilities)
- Protocol Review: Ensure the study protocol and consent form have been approved by the relevant Institutional Review Board (IRB) or ethics committee.
- Scheduling and Setting: Schedule the interview at a time convenient for the LAR. Book a private, quiet location free from interruptions to ensure confidentiality and comfort [35].
- Materials Preparation: Prepare the IRB-approved consent document, any supplemental information sheets, and a copy of the study summary. If applicable, test audio or video recording equipment.
II. Interview Execution
- Initial Rapport Building:
- Greet the LAR warmly and introduce yourself and your role.
- Engage in brief, neutral small talk to alleviate anxiety.
- Reiterate that the purpose of the meeting is to ensure they fully understand the study before making any decision.
- Comprehensive Consent Process:
- Provide the LAR with the consent document.
- Systematically review each section of the form (purpose, procedures, risks, benefits, alternatives, confidentiality, compensation).
- Use layperson's language and avoid jargon. For example, instead of "randomization," say "like a flip of a coin."
- Pause frequently to check for understanding (e.g., "Would you like me to go over the different visits again?" or "What questions do you have about the potential side effects?").
- Emphasize the voluntary nature of participation and their right to withdraw the subject at any time without penalty.
- Assessment of Understanding:
- Do not rely on a simple "Do you understand?" Instead, use open-ended questions to assess comprehension (e.g., "Could you describe in your own words what the main goal of this study is?" or "What would you do if you wanted to stop participation?").
- Clarify any misconceptions immediately.
- Documentation of Consent:
- After all questions have been answered, ask if the LAR is ready to provide consent.
- If yes, proceed with the signature process according to IRB requirements (e.g., signing and dating the form).
- Provide the LAR with a copy of the signed document.
III. Post-Interview Procedures
- Data Handling: De-identify the interview data as described in the protocol to protect the LAR's and subject's privacy [35].
- Documentation: File the original signed consent form as per institutional policy.
- Ongoing Support: Reiterate your contact information and availability for any future questions.
Protocol for Handling Sensitive Situations
A key methodological consideration is managing unexpected disclosures during the interview.
- Redirection and Termination: If an LAR begins to discuss illegal behaviors not covered by the protocol, the researcher must either attempt to redirect the conversation or stop the interview entirely [35]. This is particularly critical if the research does not hold a Certificate of Confidentiality.
- De-escalation: If the LAR becomes visibly distressed or uncomfortable, pause the interview. Acknowledge their feelings and ask if they would like to take a break or discontinue. Have a plan for this scenario detailed in the research protocol [35].
Mandatory Visualization
The following diagram illustrates the logical workflow and decision points for a consent interview, from preparation to completion.
The Scientist's Toolkit: Research Reagent Solutions
This table details essential materials and tools for implementing the described consent interview protocols.
Table 3: Essential Materials for Consent Interview Research
| Item | Function & Application in Protocol |
|---|---|
| IRB-Approved Consent Document | The legally and ethically mandated document detailing study information. Serves as the primary tool for the structured review during the formal interview [35]. |
| Digital Recording Equipment | For audio or video recording of the consent interview to ensure accurate data collection, used only with the explicit, documented permission of the LAR [35]. |
| Secure Data Storage Solution | Encrypted digital storage (e.g., secure servers) or physical storage (e.g., locked cabinets) for storing signed consent forms and recorded media, protecting participant confidentiality [35]. |
| Interview Protocol Script | A guide for researchers to ensure consistent and comprehensive coverage of all consent elements, reducing variability between interviewers. |
| Contact Information Sheet | A document provided to the LAR with names and phone numbers of key research personnel for follow-up questions, reinforcing ongoing support. |
| Certificate of Confidentiality | A federal certificate that may protect research data from forced disclosure (e.g., by a court subpoena). Its presence or absence directly impacts the protocol for handling disclosures of sensitive illegal behaviors [35]. |
Within the context of legally authorized representative (LAR) informed consent process research, applying health literacy principles is an ethical and methodological necessity. LARs, often making critical decisions under stress, require materials they can understand to fulfill their fiduciary duties. This document provides detailed application notes and experimental protocols for implementing the 8th-grade readability standard and plain language principles in informed consent forms (ICFs) and processes, with a specific focus on studies involving LARs.
Quantitative Foundation: Establishing the Readability Standard
Extensive research supports targeting an 8th-grade reading level for consumer-facing materials, including informed consent documents. The quantitative justifications for this standard are summarized in the table below.
Table 1: Quantitative Evidence for the 8th-Grade Readability Target
| Evidence Source | Key Metric | Recommended Target | Rationale and Supporting Data |
|---|---|---|---|
| General Population Readability [36] [37] [38] | Flesch-Kincaid Grade Level | Grade 8 | The average American reads at a 7th to 8th-grade level. A Grade 8 target ensures accessibility for the majority of adults, including LARs. |
| Health & Research Communication [37] | Flesch-Kincaid Grade Level | Grade 8 (General); Grade 10-12 (Technical) | Balances scientific accuracy with comprehension. The 8th-grade level is recommended for general content, with a higher level acceptable for technical appendices. |
| Readability Score Conversion [38] | Flesch Reading Ease | Score of 60-70 | A Flesch Reading Ease score of 60-70 corresponds to an 8th-grade reading level, where a higher score indicates easier reading. |
| Institutional Guidelines [36] [39] | Readability Tools | Flesch-Kincaid, Gunning Fog, SMOG | Major institutions (Intuit, ClearCompany, RSNA) advocate for an 8th-grade level checked by multiple validated tools. |
| Comprehension & Inclusivity [36] | - | Grade 5-8 | This range supports neurodivergent individuals, non-native speakers, and those who are distracted or in a hurry, critical for LARs in high-stakes situations. |
Experimental Protocol: Assessing and Revising Informed Consent Materials
This protocol provides a step-by-step methodology for evaluating and improving the health literacy demand of informed consent documents intended for participants and their LARs.
Protocol: Readability and Suitability Assessment of Informed Consent Documents (ICDs)
Objective: To quantitatively and qualitatively evaluate the health literacy demands of ICDs and ensure they adhere to plain language principles suitable for LARs.
Materials:
- Informed Consent Documents (ICDs) in editable digital format.
- Readability analysis software (e.g., Hemingway Editor, Readable, Microsoft Word’s built-in tool).
- Suitability Assessment of Materials (SAM) instrument or SAM+CAM instrument [40].
- Access to representatives from the target population or LAR community for usability testing.
Procedure:
Step 1: Preliminary Legal and Regulatory Review
- Action: Identify all legally required elements for informed consent as per relevant regulations (e.g., the Revised Common Rule in the US, which mandates a "concise and focused presentation of key information") [41].
- Output: A checklist of mandatory content to ensure compliance is not compromised during simplification.
Step 2: Quantitative Readability Analysis
- Action: Analyze the entire ICD and its "Key Information" section separately using readability software.
- Measurements:
- Flesch-Kincaid Grade Level
- Flesch Reading Ease Score
- Gunning Fog Index
- SMOG Index [40]
- Success Criterion: The document achieves an average grade level of ≤ 8.0 across multiple metrics [36] [37].
Step 3: Qualitative Suitability Assessment
- Action: Two independent reviewers score the ICD using the SAM or SAM+CAM tool. This tool evaluates [40]:
- Content (purpose, behavioral objectives)
- Literacy Demand (vocabulary, structure, active voice)
- Graphics (efficacy of tables/charts)
- Layout & Typography
- Scoring: Materials are rated as "Superior," "Adequate," or "Not Suitable."
- Output: A scored SAM sheet highlighting specific areas for improvement.
Step 4: Usability Testing with the LAR Population
- Action: Conduct cognitive interviews or usability tests with individuals representative of LARs.
- Method: Participants are given the revised ICD and asked to "teach-back" key concepts, such as the study's purpose, procedures, risks, and alternatives [41].
- Data Collection: Record comprehension errors, points of confusion, and participant feedback.
Step 5: Iterative Revision
- Action: Integrate feedback from Steps 2-4 to revise the ICD.
- Focus: Apply plain language principles (outlined in Section 4) to address identified issues.
- Validation: Repeat readability and suitability assessments (Steps 2-3) on the revised document to confirm improvement.
The following workflow diagram illustrates this iterative protocol.
The Scientist's Toolkit: Plain Language Reagent Solutions
Implementing health literacy principles requires a set of standardized "reagents" — reliable word and sentence structures — to construct clear consent materials.
Table 2: Research Reagent Solutions for Plain Language Protocol
| Reagent Solution | Function | Example Application in ICDs |
|---|---|---|
| Active Voice | Clarifies the agent of action, reducing ambiguity and strengthening sentences. | Instead of: "The study drug will be administered by the clinician."Use: "The clinician will give you the study drug." [39] |
| Everyday Vocabulary | Replaces jargon and complex terms with words common in everyday conversation. | Instead of: "Utilize," "Commence," "Terminate," "Remuneration."Use: "Use," "Start," "End," "Payment." [36] [39] |
| Short Sentences (<20 words) | Reduces cognitive load by presenting one idea at a time, improving processing speed. | Instead of: "In the event that you choose to withdraw from the study, which you may do at any time without penalty, all of the data collected up to that point will still be utilized."Use: "You may leave the study at any time. If you leave, we will keep and use the information we already have." [36] [39] |
| Logical Organization with Headings | Creates a predictable structure that helps users find information quickly and aids navigation. | Begin with a "Key Information" section. Use descriptive headings like "What happens in the study?" and "What are the risks?" [41] |
| Second-Person Pronouns ("You") | Directly addresses the reader (participant or LAR), making the document more personal and engaging. | Instead of: "The subject must report any adverse events."Use: "You must tell us about any side effects you have." [39] |
| Simple Verb Tenses | Uses past, present, and future tenses instead of complex perfect or continuous tenses for easier translation and comprehension. | Instead of: "You will be undergoing..."Use: "You will have..." [36] |
| Chunking & White Space | Groups related information into short paragraphs and uses white space to avoid overwhelming the reader visually. | Break long text blocks into sections with headings. Use bulleted lists for risks or procedures. [39] |
Data Presentation Protocol: Quantitative Data Summaries for Evaluation
When presenting quantitative data in study results or the consent form itself, clarity is paramount. The following protocol ensures data is accessible to LARs and participants.
Protocol: Summarizing and Presenting Quantitative Data in ICDs
Objective: To translate complex study data (e.g., outcome rates, risk probabilities) into clear, understandable formats.
Procedure:
Step 1: Data Preparation
- Action: Clean the dataset by removing blanks, duplicates, and obvious errors. Ensure variables are in the correct format (e.g., numbers, percentages) [42].
Step 2: Calculate Descriptive Statistics
- Action: Choose the most appropriate statistics to describe the data [42]:
- Frequencies/Percentages: For categorical data (e.g., side effects).
- Mean/Average: For normally distributed data (e.g., average age of participants).
- Median: For skewed data (e.g., participant income).
- Range or Standard Deviation: To describe the variation or spread of the data.
Step 3: Construct Summary Tables
- Action: Present data in clearly structured tables. The table below provides a template for presenting risk data clearly.
Table 3: Example Template for Presenting Risk Data in an ICD
| Potential Side Effect | Frequency in Study Participants (n=150) | What this means |
|---|---|---|
| Headache | 75 participants (50%) | About half of the people in the study got a headache. |
| Nausea | 30 participants (20%) | About 1 in 5 people in the study felt sick to their stomach. |
| Serious Rash | 3 participants (2%) | A very small number of people in the study got a serious rash. |
Step 4: Visualize Data Appropriately
- Action: Select simple charts for data that requires comparison.
- Guidance: Use bar charts to compare frequencies between groups. Avoid complex charts like 3D pie charts [42].
- Inclusion: Always report the sample base (e.g., n=150) with any percentage to provide context [42].
The logical process for selecting the right data presentation format is shown below.
Informed consent is a foundational ethical and regulatory requirement in human subjects research, serving as a critical mechanism for upholding the principle of autonomy. This process requires researchers to provide prospective participants with adequate information about the study in language that is understandable, allowing them to make a voluntary decision about whether to participate [43] [44]. Proper documentation of this process is not merely administrative—it provides tangible evidence that a meaningful consent interaction occurred between the researcher and participant before any research procedures commenced.
For studies involving participants who lack decision-making capacity, the informed consent process must be adapted while maintaining the same ethical rigor. Federal regulations and institutional policies provide specific frameworks for obtaining consent through Legally Authorized Representatives (LARs), who are empowered to make research decisions on behalf of potential participants who cannot provide consent for themselves [1]. This application note details the signature requirements and documentation standards that researchers must follow when working with LARs throughout the consent process, ensuring both regulatory compliance and ethical integrity.
Regulatory Framework and Signature Requirements
General Regulatory Requirements for Informed Consent
Informed consent for human subjects research is governed by multiple regulatory frameworks, each with specific requirements for documentation. The Common Rule (45 CFR 46) establishes the foundational requirements for studies funded by the Department of Health and Human Services (HHS) and other federal agencies [45] [43]. The Food and Drug Administration (FDA) regulations (21 CFR 50) provide additional standards for clinical investigations involving drugs, biological products, and medical devices [45] [43]. These regulations establish six general requirements for informed consent:
- Consent Required: Investigators must obtain consent from participants or their LARs unless a specific waiver is justified and approved [43].
- Voluntary Participation: Participants must have sufficient time to consider participation without coercion or undue influence [43].
- Understandable Language: Consent information must be presented in language accessible to the participant or LAR [43] [46].
- No Waiver of Rights: Consent language cannot include exculpatory clauses through which participants waive legal rights [43].
- Key Information Presentation: Consent must begin with a concise presentation of key information to facilitate understanding of reasons for or against participation [43].
- Organized for Understanding: The consent document as a whole must be organized to facilitate comprehension rather than presenting isolated facts [43].
Signature Requirements and Documentation Standards
Documentation of informed consent typically requires a written consent form signed by the participant or their LAR, containing all required elements and approved by the Institutional Review Board (IRB) before use [43]. The signature requirements follow specific standards:
- The participant or LAR must sign and date the consent form before any research procedures begin [43] [44].
- The individual obtaining consent must also sign and date the form, confirming the process was properly conducted [43] [44].
- A copy of the signed consent form must be provided to the person signing it [46].
- The original signed consent form must be maintained in the research records [44].
For research involving LARs, the consent process should still include the prospective participant to the greatest extent possible, and their assent (affirmative agreement) should be obtained when feasible, even when the LAR provides the formal consent [1].
Table 1: Signature Requirements for Informed Consent Documentation
| Role | Signature Requirement | Purpose | Timing |
|---|---|---|---|
| Legally Authorized Representative | Required | Provides legally effective permission for participation | Before any research procedures |
| Participant | Recommended (assent) when capable | Documents agreement to participate | Concurrent with LAR signature |
| Consent Designee | Required | Verifies proper consent process was conducted | At time of consent conversation |
| Impartial Witness | Required when LAR/participant cannot read | Attests that information was accurately presented and understood | During consent process |
Circumstances Requiring an Impartial Witness
Special provisions apply when LARs or participants cannot read the consent form. In these situations, an impartial witness must be present during the entire consent process [44]. After the consent information is presented and explained, the witness must attest that the information was accurately presented and that consent was freely given, by signing and dating the consent document [44].
An impartial witness must be independent of the research team and cannot be unduly influenced by people involved with the trial [44]. This individual serves to safeguard the rights and welfare of the participant by ensuring the consent process is conducted properly and that the LAR fully understands what they are consenting to on behalf of the participant.
Legally Authorized Representatives: Definition and Authorization
Determining Decision-Making Capacity
A fundamental prerequisite for using an LAR is determining that the prospective participant lacks decision-making capacity to provide informed consent. Adults are presumed competent to consent unless legally judged to be incompetent [1]. For individuals with cognitive impairments, the research protocol must detail a specific assessment plan for evaluating decision-making capacity [1]. This assessment typically evaluates the individual's ability to:
- Understand the nature of the research and information relevant to participation
- Comprehend the consequences of participation for their own situation and health condition
- Understand the consequences of alternatives to participation [1]
The extent of required capacity depends on the research risks—greater capacity is required for higher-risk protocols [1]. This assessment should be documented in the research record and is typically conducted by the principal investigator or qualified designee.
Hierarchy of Legally Authorized Representatives
State laws determine who may serve as an LAR and the priority order for surrogate decision-makers. The following hierarchy represents a typical structure, though researchers must consult applicable state regulations where the research is conducted.
Figure 1: Decision hierarchy for identifying a Legally Authorized Representative. Researchers must progress through this hierarchy sequentially, obtaining consent from the highest-ranking available LAR.
For research conducted in Virginia, the following priority order applies [1]:
- Advance directive agent appointed by the prospective subject with authorization for research decisions
- Legal guardian of the prospective subject
- Spouse of the prospective subject (unless divorce proceedings are pending)
- Adult child of the prospective subject
- Parent of the prospective subject when the subject is an adult
- Adult brother or sister of the prospective subject
- Any person or judicial body authorized by law to consent on behalf of the prospective subject
If a higher-ranking LAR is identified after consent has been obtained from a lower-ranking representative, the researcher must contact the higher-ranking LAR, provide them with study information and the signed consent form, and document these communications [1].
State-Specific Variations and Considerations
LAR regulations vary by state, creating important considerations for multi-site research [1]. Researchers must understand the implications of state laws for all locations where research will be conducted. Key variations between states may include:
- Definitions of children and minors, including emancipated minors
- Individuals qualified to give permission for research participation
- Priority order of who may serve as an LAR
- Specific limitations on LAR authority for certain research categories
For research outside Virginia, investigators must cite or provide excerpts of the relevant law regarding LAR designation and describe how differing state requirements will be met [1]. The IRB may consult with legal counsel to determine the appropriateness of LAR eligibility for such research.
Special Circumstances and Limitations on LAR Authority
Restrictions on LAR Consent
While LARs generally have authority to provide consent for research participation, specific limitations protect vulnerable individuals from inappropriate enrollment. In Virginia, an LAR may not consent [1]:
- For non-therapeutic research unless the IRB determines it presents no more than a "minor increase over minimal risk" to the participant
- To participation in research that is contrary to the known religious beliefs or basic values of the prospective participant
- To participation in research involving non-therapeutic sterilization, abortion, or psychosurgery
- To admission for research purposes to a facility defined in Virginia Code §37.1-1
- If the prospective participant protests participation in the research
When two or more persons with equal decision-making priority disagree about research participation, the prospective subject cannot be enrolled in the study [1]. These limitations emphasize that LAR authority is not absolute and must be exercised with consideration for the participant's known preferences and values.
Documentation of LAR Authority
Researchers must document the LAR's authority to consent for the participant. This documentation typically includes [44] [1]:
- Verification of the LAR's relationship to the participant according to the established hierarchy
- Assessment of decision-making capacity of the prospective participant
- LAR's government-issued identification for identity verification
- Contact information for the LAR
- Documentation of any capacity assessment performed
This documentation should be maintained with the signed consent form in the research record. For participants with fluctuating capacity, researchers should establish and maintain ongoing communication with caregivers and document assessments of capacity at different time points throughout the study [1].
Electronic Consent and Digital Documentation
Electronic Signature Platforms
Modern research environments increasingly utilize electronic systems for consent documentation. Several validated platforms can facilitate the consent process while maintaining regulatory compliance:
Table 2: Electronic Signature Technology Options for Informed Consent Documentation
| Platform | Validation Status | Signature Mechanism | Best Use Context |
|---|---|---|---|
| REDCap | Not validated | Unique link/login | Non-FDA regulated studies |
| MyChart | Yes* | Portal username and password | Studies involving established patient portal users |
| Epic eConsents | Yes* | Typed name signature line | FDA and non-FDA regulated in-person studies |
| TrialX | Yes | Typed name, signature line | FDA and non-FDA regulated virtual and in-person studies |
| DocuSign | Yes | Unique link/username and password | FDA-regulated studies requiring regulatory applications |
*While the EMR is not validated to 21 CFR Part 11 standards, signing credentials meet Onc certification standards and can be used in accordance with Part 11 [47].
Remote Consent Procedures
Remote consent processes allow for participant enrollment without in-person interactions, which can be particularly valuable when LARs are not physically present with the participant. The Penn IRB supports remote consent when appropriate, provided that [46]:
- Risks to subjects continue to be minimized
- Data integrity can be maintained
- The remote method is outlined for IRB review
- The process ensures participant privacy
For remote consent with LARs, researchers should utilize video conferencing platforms that allow for identity verification and include the opportunity for the LAR to ask questions in real-time. The process should still include all elements of a traditional consent discussion, with documentation of the date, time, participants, and method of consent [46].
Comprehensive Workflow for LAR Consent Documentation
The following workflow provides a detailed methodology for researchers obtaining informed consent through Legally Authorized Representatives.
Figure 2: Comprehensive workflow for obtaining and documenting informed consent from a Legally Authorized Representative.
Protocol for Assessment of Decision-Making Capacity
Purpose: To standardize the evaluation of potential participants' capacity to provide informed consent for research participation.
Materials Needed:
- Protocol-specific capacity assessment tool
- Documentation forms
- Time and private space for assessment
Procedure:
- Screen for potential impairments: Identify potential participants with conditions that may affect decision-making capacity (e.g., dementia, severe mental illness, developmental disabilities, acute medical conditions affecting cognition) [1].
- Conduct capacity assessment: Engage the potential participant in a discussion about the research study, evaluating their ability to:
- Understand the nature of the research and procedures involved
- Appreciate the consequences of participation for their own situation
- Reason about the alternatives to participation
- Express a clear and consistent choice [1]
- Document assessment findings: Record the specific assessment conducted, the participant's responses, and the determination regarding capacity.
- Determine need for LAR: If capacity is impaired, proceed with identifying an LAR according to the state-specific hierarchy.
Interpretation: The level of capacity required should be commensurate with the research risk. For higher-risk studies, greater demonstration of understanding is required. When in doubt, researchers should consult with colleagues specializing in bioethics or neuropsychology.
Protocol for LAR Identity Verification and Authority Documentation
Purpose: To verify the identity of the LAR and document their authority to provide consent on behalf of the research participant.
Materials Needed:
- Government-issued photo identification
- Documentation of relationship to participant
- IRB-approved consent form
- Research record documentation forms
Procedure:
- Request identification: Ask the LAR to provide government-issued photo identification (e.g., driver's license, passport) [44].
- Verify relationship: Document the LAR's relationship to the participant according to the established hierarchy [1].
- Confirm authority: For guardians or individuals with power of attorney, request and make copies of relevant legal documents establishing authority.
- Record verification: Document the verification process in the research record, including:
- Type of identification reviewed
- Relationship of LAR to participant
- Date of verification
- Name of researcher conducting verification
- Note special circumstances: Document any relevant information about the participant's values, beliefs, or previously expressed preferences that might influence the LAR's decision [1].
Interpretation: If the LAR cannot provide sufficient documentation of their relationship and authority, researchers should progress to the next individual in the state-specific hierarchy. Legal consultation may be necessary for complex cases.
The Scientist's Toolkit: Essential Materials for LAR Consent Documentation
Table 3: Research Reagent Solutions for LAR Consent Documentation
| Item | Function | Application Notes |
|---|---|---|
| IRB-Approved Consent Forms | Provides regulatory-compliant documentation of consent | Must contain all Common Rule and FDA required elements; institution-specific language; approved by IRB before use [48] [43] |
| Capacity Assessment Tools | Standardizes evaluation of decision-making capacity | May include standardized instruments or protocol-specific questions; should be appropriate to research risk level [1] |
| Identity Verification Documents | Confirms LAR identity and authority | Government-issued photo ID; legal documents establishing authority (guardianship papers, advance directives) [44] [1] |
| Electronic Signature Systems | Enables digital documentation of consent | Platforms like DocuSign, REDCap, or Epic eConsents; selection depends on study type and validation requirements [47] |
| Audio-Visual Recording Equipment | Creates record of consent process | Required for certain vulnerable populations in specific regulatory contexts; must maintain confidentiality [44] |
| Witness Documentation Forms | Records impartial witness participation | Required when LAR/participant cannot read; documents witness presence during entire consent process [44] |
Proper documentation of the informed consent process when working with Legally Authorized Representatives requires meticulous attention to regulatory requirements and ethical principles. Researchers must follow state-specific hierarchies for LAR identification, thoroughly document the consent process, and understand the limitations on LAR authority. By implementing the protocols and utilizing the tools outlined in this application note, researchers can ensure that participants who lack decision-making capacity are enrolled in research studies with appropriate safeguards, maintaining the ethical integrity of the research process while generating legally effective documentation.
Within the framework of legally authorized representative (LAR) informed consent process research, the post-initial-consent phase demands rigorous scientific and ethical management. Ongoing communication and systematic re-consent are critical for maintaining the integrity of clinical research and protecting participants, particularly when the initial consent was provided by an LAR. Regulatory authorities and ethical guidelines mandate that consent is a continuous process, not a single event [49] [50]. This is especially vital in long-term studies involving vulnerable populations reliant on LARs, where a participant's capacity to provide direct consent may change over time, or where new safety information may alter the study's risk-benefit profile.
The foundation for re-consent is embedded in major regulatory frameworks like the ICH-GCP E6 guidelines and 21 CFR Part 50 [50]. These guidelines impose a duty on research teams to maintain consent integrity throughout the trial lifecycle. For research involving an LAR, this process carries additional complexity. Changes in the participant's clinical status, cognitive ability, or legal standing may trigger a need to re-evaluate who is the appropriate decision-maker. Furthermore, the communication strategies employed to convey new information to LARs must be tailored to ensure clarity and comprehension, ensuring that ongoing consent remains fully informed and ethically sound [51] [50].
Quantitative Data on Re-consent Triggers and Processes
A summary of the primary circumstances necessitating re-consent, derived from regulatory guidance and institutional playbooks, is provided in Table 1. These triggers are universally applicable but require particular vigilance in studies involving LARs.
Table 1: Circumstances Requiring Re-consent of Participants or Legally Authorized Representatives
| Trigger Category | Specific Circumstance | Key Actions & Considerations |
|---|---|---|
| Protocol Modifications | Significant changes to study procedures, objectives, risks, or benefits [49]. | Revise ICF; explain changes and implications clearly; obtain signature on updated IRB-approved form [49]. |
| Emerging Safety Information | New risk information becomes available [49]. | Inform participant/LAR of new risks; provide opportunity to ask questions; document the process [49] [50]. |
| Temporal Changes | Study duration extends beyond originally agreed period [49]. | Re-consent should be sought for the continued participation. |
| Administrative Changes | Significant changes to study personnel or location impacting data/samples [49]. | Re-consent may be required depending on the nature of the change. |
| Participant Status Evolution | A child participant reaches the age of majority [49]. | Critical for LAR context: The now-adult participant must provide direct consent. |
| A participant's cognitive abilities improve or decline [49]. | Re-assess the need for LAR involvement; Re-consent must involve the LAR if the participant lacks capacity. |
The execution of the re-consent process must follow a structured protocol to ensure regulatory compliance and ethical validity. The steps outlined in Table 2 provide a methodology for conducting re-consent, with special attention to the role of the Clinical Research Coordinator (CRC) and the context of LARs.
Table 2: Experimental Protocol for Executing Re-consent
| Protocol Step | Detailed Methodology | LAR-Specific Considerations |
|---|---|---|
| Step 1: Identify Need | Implement version tracking of ICFs and monitor for protocol amendments or new safety data [50]. | Proactively monitor for changes in participant status (e.g., age, cognitive capacity) that would alter LAR authority. |
| Step 2: Revise ICF | Clearly state changes and their implications in the revised ICF; Highlight new risks, benefits, or procedures [49]. | Ensure language is accessible for the LAR, who may not have a medical background. |
| Step 3: Obtain Approval | Submit the revised ICF for review and approval by the Institutional Review Board (IRB) before use [49]. | Maintain documentation of all approved versions. |
| Step 4: Contact Participant/LAR | Provide a clear explanation of the new information; Allow ample opportunity for questions [49] [50]. | The communication should be directed to the LAR, but involve the participant to the greatest extent possible. |
| Step 5: Document Re-consent | Participants/LARs who agree to continue must sign the updated ICF [49]. If verbal consent is IRB-approved, document in study records [49]. | Clearly document the identity and authority of the LAR in the source records. |
| Step 6: Manage Withdrawal | Participants/LARs who do not agree to the changes must be allowed to withdraw without penalty [49]. | Document the reason for withdrawal and ensure a safe termination of study procedures. |
Workflow Visualization of Re-consent Triggers and Actions
The logical relationship between key triggers, decision points, and subsequent actions in the re-consent process, particularly from an LAR perspective, can be visualized in the following workflow. This diagram outlines the critical pathway from trigger identification to process resolution.
Diagram 1: Re-consent Trigger and LAR Decision Workflow. This chart visualizes the process from identifying a re-consent trigger through the critical decision point regarding LAR authority, culminating in documentation.
The Scientist's Toolkit: Essential Materials for Re-consent Research
For researchers designing and implementing studies on LAR-informed consent processes, specific tools and reagents are essential for ensuring compliance, data integrity, and ethical rigor. The following toolkit details key resources.
Table 3: Research Reagent Solutions for Informed Consent Process Research
| Tool or Material | Function/Description | Application in LAR Research |
|---|---|---|
| IRB-Approved Informed Consent Form (ICF) | The legally and ethically approved document detailing study procedures, risks, benefits, and participant rights [49]. | The foundational document for the initial consent and all subsequent re-consent events. |
| eConsent Platform | A 21 CFR Part 11 compliant digital system for delivering consent forms, capturing electronic signatures, and managing versions [50]. | Provides audit trails for LAR interactions, ensures version control, and facilitates remote consent with LARs who may not be on-site. |
| Consent Version Tracker | A log (digital or paper-based) that records the IRB approval date and version number of every ICF used in the study [50]. | Critical for ensuring that the correct, updated form is used during re-consent discussions with the LAR, preventing protocol deviations. |
| Teach-Back Scripts & Comprehension Tools | Structured questions and plain-language explanations used to verify a participant's or LAR's understanding of the study [50]. | Essential for assessing and documenting the LAR's comprehension during the re-consent process, ensuring consent is truly informed. |
| Source Documentation Template | Standardized forms within the study records for documenting the specifics of each consent and re-consent interaction [50]. | Used to meticulously record the date, time, individuals present (LAR, witness, CRC), and key points discussed during the re-consent process. |
Within the specialized domain of LAR-informed consent research, the protocols for ongoing communication and re-consent are fundamental to upholding ethical principles. The triggers and methodologies detailed in this application note provide a structured, evidence-based framework for investigators. Adherence to these protocols—supported by robust version control, clear communication tailored to LARs, and meticulous documentation—ensures regulatory compliance and, more importantly, honors the ethical commitment to participants and their representatives throughout the research lifecycle. As regulatory landscapes evolve, a proactive and rigorous approach to post-consent continuation remains a critical component of responsible clinical research.
Navigating Complex Scenarios: Troubleshooting Common LAR Consent Challenges
Within the specific context of research on the legally authorized representative (LAR) informed consent process, overcoming communication barriers is not merely an operational detail but a fundamental ethical and legal imperative. LARs, who make decisions on behalf of potential participants who lack capacity, often face complex medical information under stressful conditions. When compounded by language and cultural differences, the risk of misunderstanding escalates, potentially compromising the validity of consent and the ethical integrity of the research. The use of qualified interpreters and cultural mediators is therefore essential to ensure that LARs fully comprehend the research protocol, including its purpose, procedures, risks, potential benefits, and alternatives. This document provides detailed application notes and protocols for researchers, scientists, and drug development professionals to effectively integrate these professionals into the LAR consent process, thereby upholding the principles of respect for persons, beneficence, and justice.
Application Notes: Foundational Principles and Quantitative Evidence
Regulatory and Ethical Mandates
Recent regulatory updates have solidified the requirements for language services. As of June 2025, new federal regulations under Section 1557 of the Affordable Care Act have strengthened protections for patients with Limited English Proficiency (LEP), which directly extends to research participants and their LARs [52]. Key mandates include:
- Qualified Interpreters Only: Healthcare providers and researchers must use interpreters who meet strict qualifications in language proficiency, ethics, and confidentiality. Bilingual staff or family members alone are not sufficient to meet these standards [52] [53].
- Free Language Assistance: LARs cannot be asked to bring or pay for their own interpreters; these services must be provided free of charge [52].
- Privacy and HIPAA Compliance: Interpreters accessing Protected Health Information (PHI) must adhere to updated HIPAA security rules, including multi-factor authentication and faster breach reporting (within 30 days) [52].
Comparative Effectiveness of Communication Strategies
A systematic review of strategies for mitigating language barriers provides critical evidence for policy and practice. The findings demonstrate clear hierarchies in effectiveness, which should guide resource allocation in research settings, especially during the sensitive LAR consent process.
Table 1: Effectiveness of Different Communication Strategies for Mitigating Language Barriers in Healthcare [53]
| Strategy | Relative Effectiveness | Key Findings and Appropriate Use Cases |
|---|---|---|
| Shared Language (e.g., provider speaks patient's language) | Most positive outcomes | Ideal, but often not feasible; maximizes comprehension and trust. |
| Professional Interpreters | Superior outcomes, second only to shared language | In-person or video interpreters outperform telephone interpreters. The gold standard for formal consent discussions. |
| Video Remote Interpreting (VRI) | Effective, better than telephone | Good alternative when in-person interpreters are unavailable; preserves some non-verbal cues. |
| Telephone Interpreters | Less effective than in-person/VRI | Can be used for simpler, follow-up communications but less suitable for complex consent processes. |
| Digital Translation Tools | Sufficient only for simple, pre-translated messages | Not recommended for nuanced consent discussions due to lack of cultural sensitivity and accuracy. |
| Informal Interpreters (e.g., family, staff) | Lowest quality for consent; similar outcomes only for simple post-op checks | Not recommended for LAR consent due to risks of omission, errors, and breaches of confidentiality. |
Public Willingness to Share Data and the Importance of Trust
Understanding participant attitudes is crucial for designing inclusive research. A recent meta-analysis revealed that a pooled estimate of 77% (95% CI: 71–82%) of the public in predominantly high-income countries is willing to share their health data for secondary purposes, such as research [54]. However, this willingness is highly conditional. Participants expressed significant concerns about privacy, consent, and transparency [54]. For LARs, who are making a profound decision on behalf of another, establishing trust through transparent communication facilitated by a qualified professional is paramount to their willingness to engage in the research process.
Experimental Protocols for LAR Informed Consent
Protocol 1: Integrating Qualified Interpreters in the LAR Consent Process
Objective: To ensure that a LAR with LEP fully understands the research study to provide truly informed consent on behalf of a potential participant.
Materials:
- IRB-approved informed consent documents (ICF) and Patient Information Sheets (PIS) in the LAR's preferred language.
- A certified medical interpreter (in-person or via a secure video platform).
- A quiet, private room or virtual meeting space to ensure confidentiality.
Methodology:
- Pre-Session Briefing (10-15 minutes): The principal investigator (PI) or designated consent official meets with the interpreter before the LAR arrives. The PI reviews the study's purpose, key procedures, major risks/burdens, and potential benefits. The interpreter is given a copy of the translated consent form to preview.
- Introduction and Setting Roles (5 minutes): At the session's start, the PI introduces the interpreter to the LAR, explains the interpreter's role as a neutral conduit of information, and emphasizes that everything said will be confidential.
- Explanation and Interpretation (60-90 minutes): The PI explains the research study to the LAR, speaking in short, clear segments. The interpreter consecutively interprets everything for the LAR. The PI uses plain language, avoids jargon, and pauses frequently to check for understanding.
- Assessment of Comprehension (15-20 minutes): The PI employs the "teach-back" method. The LAR is asked to explain in their own words their understanding of key elements (e.g., "Can you tell me what you believe the main purpose of this study is?" and "What are the main risks or discomforts you understand to be involved?"). The interpreter facilitates this dialogue exactly.
- Documentation: Upon confirmation of comprehension, the LAR is invited to sign the consent form. The interpreter signs as a witness to the consent process, attesting that the interpretation was accurate and complete. Notes from the session, including the comprehension assessment, are filed in the study records.
Protocol 2: Utilizing Cultural Mediators for Community-Engaged Consent
Objective: To employ a cultural mediator to navigate not only language but also cultural norms, beliefs, and trust barriers that may impact the LAR's decision-making process, particularly in underserved ethnic minority communities.
Materials:
- Co-created informational resources (e.g., storyboards, multilingual videos) [55].
- A trained cultural mediator with trusted ties to the community.
- Scripts or talking points reviewed and approved by the IRB and community partners.
Methodology:
- Community Partnership and Resource Development: Prior to recruitment, engage with community leaders and organizations representing the target population. Collaboratively develop and refine consent materials, such as simplified scripts and visual aids, to ensure they are culturally appropriate and accurate [55].
- Mediator-Facilitated Discussion: The cultural mediator leads the consent discussion alongside the researcher. Their role expands beyond that of a pure interpreter (conduit) to include:
- Clarifier: Explaining concepts that may not have direct cultural equivalents.
- Cultural Broker: Contextualizing the research within the LAR's cultural framework (e.g., beliefs about illness, authority, or medical research).
- Advocate: Ensuring the LAR feels empowered to ask questions and voice concerns [56].
- Trust-Building and Dialogue: The session is structured as a dialogue rather than a one-way explanation. The cultural mediator uses their position of trust to foster an environment where the LAR feels comfortable discussing fears or misconceptions.
- Iterative Understanding Check: The mediator and researcher work together to assess understanding, paying close attention to non-verbal cues and asking open-ended questions about the LAR's perspective on the study's value and impact.
- Post-Consent Support: The cultural mediator remains a point of contact for the LAR for any follow-up questions that may arise after the formal consent process, facilitating ongoing communication.
Visualization of Workflows
The following diagram illustrates the critical decision pathway for selecting and deploying language services during the informed consent process with a Legally Authorized Representative (LAR).
Decision Workflow for Interpreter-Assisted LAR Consent
The Scientist's Toolkit: Research Reagent Solutions
This table details the essential "research reagents" – the human resources and materials – required to execute the protocols for overcoming communication barriers in LAR consent research.
Table 2: Essential Reagents for Research on Communication in LAR Consent Processes
| Research Reagent | Function / Rationale | Certification / Quality Control |
|---|---|---|
| Certified Medical Interpreter | Serves as the core reagent for accurate linguistic translation during consent dialogues, ensuring fidelity of information. | Certification from CCHI or NBCMI; adherence to a code of ethics (confidentiality, accuracy, impartiality) [57] [58]. |
| Trained Cultural Mediator | Functions as a specialized reagent to address cultural translation, build trust, and navigate culturally-specific health beliefs that impact decision-making. | Training in cultural brokerage and advocacy roles; established trust and recognition within the target community [56]. |
| Co-Created Consent Resources | Act as standardized stimuli to improve comprehension and engagement. Include multilingual videos, storyboards, and simplified scripts. | Developed and validated through participatory methods (e.g., PPIE, public deliberation) with the target community [55] [59]. |
| Readability Analysis Software | A quality control tool to ensure translated and original consent materials meet recommended reading levels (e.g., 6th-8th grade) [16]. | Software calculating Flesch-Kincaid Grade Level, Gunning-Fog Index, and Flesch Reading Ease Score. |
| Secure Teleconferencing Platform | The delivery vehicle for remote interpreter services (VRI), enabling access to specialists regardless of geography. | HIPAA-compliant platform with end-to-end encryption to maintain patient privacy and data security [52]. |
Health literacy is critically defined as the degree to which individuals have the ability to find, understand, and use information and services to inform health-related decisions and actions for themselves and others [60]. This concept extends to organizational health literacy, which is the degree to which organizations equitably enable individuals to perform these same actions [60]. Within the specific context of legally authorized representative informed consent processes, these representatives are often required to process complex medical information under stressful circumstances, making effective communication strategies paramount. The teach-back method emerges as a vital evidence-based technique to confirm understanding by asking individuals to explain in their own words what they have just been told, thereby ensuring true comprehension rather than mere acknowledgment.
Research from the National Institutes of Health emphasizes that we must not blame the individual for not understanding information that has not been made clear, and that everyone, no matter how educated, is at risk for misunderstanding health information if the topic is emotionally charged or complex [60]. This is particularly relevant for legally authorized representatives who may be making critical healthcare decisions under conditions of significant stress and emotion. Studies show that between 40-80% of medical information patients receive is forgotten immediately after a provider-patient encounter, and nearly half of the recalled information is incorrect [61]. The teach-back method directly addresses these challenges by transforming passive information reception into active, confirmable understanding.
Experimental Evidence and Quantitative Outcomes
Recent research provides substantial quantitative evidence supporting the implementation of teach-back methods in healthcare communication. A 2023 study evaluated pharmacist-provided teach-back medication counseling at hospital discharge, demonstrating significant improvements in patient understanding and confidence [62].
Table 1: Quantitative Outcomes from Teach-Back Implementation Study
| Metric | Result | Significance |
|---|---|---|
| Patients Surveyed | 32 patients | 100% response rate |
| Mean Patient Age | 57 years (range: 19-91) | Applicable across age groups |
| Medications Counselled | Mean 2.94 medications/patient | Effective for multiple medications |
| Counselling Time | Mean 23.6 minutes/patient | Resource requirement identified |
| Patient Confidence | 93.7% had increased confidence | Majority benefit in knowledge |
| Patient Satisfaction | 93.7% satisfied with counselling | High acceptability |
| Pharmacist Feasibility | 100% agreed feasible to apply | Clinical practicality confirmed |
This study demonstrated that teach-back medication counselling at hospital discharge increases patients' satisfaction and confidence regarding medication knowledge [62]. The research also highlighted that providing written information about medications alongside verbal teach-back counselling is important for patients and acts as a useful reference point after the clinical encounter [62]. These findings have direct relevance to informed consent processes with legally authorized representatives, where understanding retention and reference materials are equally crucial.
Additional studies have demonstrated even more profound outcomes. One investigation of 189 coronary artery bypass surgery patients who received teach-back patient education found readmissions were 25% in the pre-intervention group compared with 12% in the post-intervention group—effectively cutting admissions in half for the group who received teach-back [61]. This substantial reduction in healthcare utilization indicates the profound impact that improved understanding can have on health outcomes and resource allocation.
Teach-Back Protocol for Research Implementation
Core Methodology
The teach-back method involves asking recipients to explain in their own words the key information they have just received. This process is not a test of the individual but rather a verification of how well the information was communicated by the provider [61]. The protocol requires the following key elements:
- Open-Ended Questions: Use questions that cannot be answered by "yes" or "no" but require explanation in the individual's own words [61].
- Non-Judgmental Approach: Phrase requests in a manner that assumes responsibility for clear communication, using phrases such as "I want to be sure I explained this clearly. Can you please explain it back to me so I can be sure I did?" [61].
- Focus on Critical Content: Identify and prioritize the 2-3 most essential concepts that must be understood, particularly for complex situations [61].
- Multiple Cycles: Be prepared to re-explain concepts using different approaches if the initial explanation proves insufficient, followed by another teach-back cycle.
Structured Workflow Implementation
The following diagram illustrates the standardized teach-back procedure for implementation in research settings involving legally authorized representatives:
Training Protocol for Research Staff
Implementing teach-back effectively requires systematic training of research staff. Based on successful protocols from clinical studies, the following training methodology should be employed:
- Online Education Module: Utilize evidence-based interactive learning modules that demonstrate correct integration of teach-back into practice, including descriptions of teach-back and demonstrations of its effectiveness [62].
- Video Demonstrations: Create or source videos simulating teach-back scenarios specific to the research context, such as obtaining informed consent from legally authorized representatives [62].
- Competency Elements: Provide staff with documented elements of competence for using teach-back effectively, including techniques for asking open-ended questions and responding non-defensively to incorrect explanations [62].
- Practice Sessions: Implement supervised practice sessions with standardized scenarios to build proficiency before implementation with study participants.
A 2023 study found that all pharmacist survey respondents (n=8) agreed they were given adequate training and that teach-back was feasible to apply in practice when this comprehensive training approach was utilized [62].
Application to Legally Authorized Representative Informed Consent
Adaptation Framework
The teach-back method requires specific adaptations when working with legally authorized representatives in research contexts. The emotional burden and potential stress of decision-making for another person create unique communication challenges that must be addressed:
- Representative's Emotional State: Acknowledge that stress and emotion can significantly impact comprehension and recall, regardless of education level [61].
- Complex Medical Information: Prioritize information hierarchy to ensure understanding of critical elements first, using the same principles applied to patients with complex health conditions [61].
- Documentation Protocol: Develop standardized documentation of the teach-back process that can demonstrate the representative's understanding at the time of consent.
Health Literacy Considerations
When implementing teach-back with legally authorized representatives, it is essential to recognize that health literacy is complex and not correlated with general education or intelligence. Research confirms that "one cannot assume that people understand health communications based on dress, education, and how they present themselves. It's entirely possible to have a high level of overall literacy but low health literacy" [61]. The National Assessment of Adult Literacy found that only 12% of Americans are proficient in health literacy, highlighting the necessity of universal precautions rather than targeted interventions [61].
Table 2: Research Reagent Solutions for Teach-Back Implementation
| Tool Category | Specific Resource | Function in Research Context |
|---|---|---|
| Training Tools | AHRQ Health Literacy Universal Precautions Toolkit [61] | Provides foundational training materials and implementation guides |
| Assessment Tools | Teach-Back Self Evaluation and Tracking Log [61] | Allows researchers to monitor fidelity to protocol and quality of delivery |
| Educational Aids | Demonstration Videos (e.g., medication changes) [61] | Standardizes training and provides concrete examples of technique |
| Support Materials | Patient-Friendly Medication Lists [62] | Provides reference material for representatives to reinforce verbal communication |
| Evaluation Tools | Post-Process Satisfaction Surveys [62] | Measures representative experience and identifies areas for improvement |
Measurement and Evaluation Framework
Process Metrics
Successful implementation of teach-back requires systematic measurement of both process and outcome metrics. The following evaluation framework should be incorporated into research protocols:
- Fidelity Measures: Document adherence to teach-back protocol through checklists or audio recording reviews.
- Time Requirements: Track the duration of consent processes to inform resource allocation, recognizing that effective teach-back requires approximately 20-30 minutes per session based on research findings [62].
- Representative Experience: Assess satisfaction and perceived clarity using standardized instruments.
Outcome Metrics
The effectiveness of teach-back in improving understanding should be evaluated through both immediate and longitudinal measures:
- Knowledge Retention: Assess understanding of key concepts immediately after consent and at predetermined follow-up intervals.
- Decision Consistency: Evaluate whether decisions remain stable over time when understanding is verified through teach-back.
- Process Outcomes: Document completion rates, withdrawal rates, and protocol adherence comparisons between standard consent and teach-back enhanced processes.
The following diagram illustrates the relationship between health literacy, communication methods, and outcomes in the informed consent process:
The integration of the teach-back method into protocols for obtaining informed consent from legally authorized representatives represents an evidence-based approach to addressing the critical challenges of health literacy and comprehension in research contexts. The standardized procedures, training protocols, and evaluation frameworks outlined in these application notes provide researchers with practical tools for implementation. As healthcare and research continue to emphasize patient-centered and representative-centered approaches, methods like teach-back that prioritize true understanding over procedural compliance will become increasingly essential to ethical research practice and valid informed consent.
Application Note
This document provides researchers and drug development professionals with evidence-based protocols to mitigate the effects of time pressure and coercion in the informed consent process, with a specific focus on contexts involving Legally Authorized Representatives (LARs). Ensuring that consent is truly voluntary and informed is a critical ethical and regulatory requirement, particularly when consent is provided on behalf of another individual.
Recent research highlights that coercion is a multi-faceted problem, ranging from formal measures to subtle informal pressures. A nationwide study on staff attitudes found that the use of coercion is often justified by healthcare professionals as necessary for security, though it is widely acknowledged that it can harm the therapeutic relationship and could be reduced with more time and personal contact [63]. Furthermore, a scoping review indicates that digitalization of the consent process shows significant potential for enhancing understanding among participants and their representatives by providing information in a more accessible and comprehensible manner [64]. Critically, coercion often begins long before any formal admission or consent process is initiated, through mechanisms such as psychological pressure, threats, or manipulation by clinicians, family, or others [65]. These findings underscore the necessity of proactive, structured strategies to manage time constraints and prevent coercive influences throughout the consent workflow.
Quantitative Data on Coercion and Time Constraints
The following tables summarize key empirical findings related to coercion and the impact of time in clinical settings.
Table 1: Pre-Admission Coercion Experienced by Patients (Survey of 318 Psychiatric Inpatients) [65]
| Type of Coercion | Sub-Type | Percentage Reporting | Key Demographic Variances |
|---|---|---|---|
| Any Pre-Admission Coercion | --- | 53% | --- |
| Informal Coercion | --- | 45% | Women reported higher rates. |
| Psychological Pressure, Threats, Deception | (Reported in detail) | ||
| Formal Coercion | --- | 8% | Men were more likely to report. |
| Police Intervention, Forced Transport | (Reported in detail) | Individuals with stigmatized diagnoses (e.g., schizophrenia) experienced higher rates. |
Table 2: Staff Attitudes Towards Coercion (Survey of 1702 German Psychiatric Staff) [63]
| Attitude Statement | Mean Agreement (1-5 scale) | Significant Influencing Factors |
|---|---|---|
| Coercion could be reduced with more time and personal contact. | 4.20 | Specialization and professional affiliation. |
| Coercion sometimes needs to be used for security reasons. | 4.10 | Forensic staff showed more positive attitudes than adult or child/adolescent psychiatry staff. |
| Coercion can harm the therapeutic relationship. | 4.08 |
Experimental Protocols for Mitigating Coercion
Protocol for a Digital Augmented Consent Process
This protocol outlines a methodology for implementing and evaluating a digital consent aid to reduce time pressure and improve understanding for LARs.
I. Objective: To determine if a digital consent tool improves LARs' comprehension, perceived voluntariness, and satisfaction compared to a standard paper-based process.
II. Materials & Reagents:
- Digital Consent Platform: A tablet or computer-based application housing the consent information.
- Multi-Media Content: Interactive diagrams, video explanations of the procedure, and a click-through interface with built-in comprehension checks.
- Validated Questionnaires: Pre- and post-test surveys measuring comprehension, the Decision-Making Involvement Scale (for perceived coercion), and a satisfaction survey.
- Control Materials: Standard paper consent forms.
III. Procedure:
- Recruitment & Randomization: Recruit LARs for a specific clinical trial. Randomize them into an Intervention group (digital consent) and a Control group (standard consent).
- Intervention Group Workflow: a. The LAR uses the digital platform, which presents information in segmented modules. b. The system incorporates mandatory pauses and interactive quizzes to verify understanding of key concepts like risks, benefits, and alternatives. c. The LAR can bookmark areas of confusion or questions for the investigator.
- Control Group Workflow: The LAR engages in the standard, paper-based consent discussion with the investigator.
- Consolidated Discussion: In both groups, a final discussion with the investigator is held to address any remaining questions before signing.
- Outcome Measurement: Administer the outcome questionnaires to both groups immediately after the consent process and at a 24-hour follow-up to assess knowledge retention.
IV. Analysis: Compare mean comprehension scores, coercion scores, and satisfaction ratings between the Intervention and Control groups using t-tests or non-parametric equivalents. Analyze qualitative feedback from LARs and investigators [64].
Protocol for Assessing Environmental and Interpersonal Coercion
This protocol provides a framework for systematically observing and auditing the consent environment for coercive pressures.
I. Objective: To identify and quantify environmental and interpersonal factors that may contribute to a LAR's sense of being rushed or pressured during the consent process.
II. Materials & Reagents:
- Structured Observation Checklist: A tool for recording timing, location, and behaviors.
- Audio-Recording Equipment: To record consent conversations for later analysis (with permission).
- Time-Tracking Software: A simple application to log the duration of each consent phase.
III. Procedure:
- Pre-Consent Assessment: a. Environment Audit: Document the physical setting (e.g., private room vs. busy hallway, presence of windows, comfort). b. Scheduling Audit: Review how the consent meeting is scheduled—avoid clustering multiple complex consents back-to-back for a single investigator.
- Process Observation: a. An independent observer (or audio recorder) documents the interaction using the checklist. b. Metrics: Record the total time of the interaction; time dedicated to the LAR's questions; number of interruptions; use of jargon; investigator's verbal and non-verbal cues (e.g., rushing speech, checking the clock).
- Post-Consent Debrief: The LAR completes a short, anonymous survey about their perceived time pressure and freedom to decide.
IV. Analysis: Correlate observed environmental and interpersonal factors (e.g., total time, number of interruptions) with LARs' self-reported measures of time pressure and coercion. The results can inform institutional guidelines on minimum consent durations and environmental standards [63] [65].
Workflow Visualization
The following diagram illustrates a recommended LAR consent workflow designed to systematically mitigate time pressure and coercion at critical points.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Coercion-Mitigation Research
| Item Name | Function/Benefit | Example Application |
|---|---|---|
| Validated Coercion Assessment Scale | Quantifies subjective feelings of pressure and influence. | Measuring the outcome of a new consent protocol on LARs' perceived voluntariness. |
| Digital Consent Platform with Analytics | Provides objective data on interaction time and content engagement; allows for standardized, self-paced information delivery. | Tracking time spent on each module and identifying areas where LARs consistently re-read information. |
| Structured Environment & Behavior Checklist | Standardizes the observation of potential coercive factors in the consent setting. | Auditing consent practices across multiple research sites to ensure protocol adherence. |
| Interactive Comprehension Assessment | Ensures understanding before proceeding, reducing the risk of uninformed consent. | Replacing simple "Do you have any questions?" with multiple-choice questions on key risks and procedures. |
| Decision-Support Tools for LARs | Provides a structured framework (e.g., pro/con grids) to help LARs deliberate according to the patient's known values. | Aiding LARs in weighing potential benefits against burdens in a non-rushed manner. |
Within the critical framework of informed consent for clinical research, the utilization of a Legally Authorized Representative (LAR) is a fundamental safeguard for adult prospective subjects who lack the mental capacity to make such decisions independently [2]. An LAR is an individual or judicial body authorized by applicable law to provide surrogate consent on behalf of the prospective subject [1]. The process, however, is not immune to conflict. Disagreements can arise in two primary scenarios: between the expressed wishes of the patient and the decision of the LAR, or among multiple individuals who qualify as LARs for a single prospective subject. Such conflicts pose significant ethical and operational challenges, potentially halting research enrollment and undermining the principles of patient autonomy and welfare. This document provides detailed application notes and protocols for researchers and drug development professionals to proactively manage and resolve these disputes, ensuring compliance with regulatory standards and upholding the highest ethical commitments.
Legal and Ethical Foundations of LAR Authority
Definition and Role of an LAR
A Legally Authorized Representative (LAR) is formally defined as "an individual, or judicial or other body authorized under applicable law to consent on behalf of a prospective subject to the subject’s participation in the procedure(s) involved in the research" [1]. It is crucial to distinguish an LAR from a parent or guardian consenting for a child; the LAR functions specifically for adults whose cognitive impairments, such as those caused by Alzheimer's disease, dementia, mental illness, or developmental disabilities, compromise their capacity to provide reasoned consent [2] [1]. The assessment of decision-making capacity is a primary consideration, and the research protocol must detail a specific plan for this assessment, evaluating the subject's ability to understand the nature of the research, its consequences, and the alternatives [1].
Hierarchical Priority of LARs
Virginia law, for example, provides a clear, descending order of priority for who may serve as an LAR for an incapable adult, which is critical for resolving initial disputes about authority [1]:
- Agent under an Advance Directive: Provided the advance directive authorizes the agent to make decisions regarding research participation.
- Legal Guardian.
- Spouse (except where divorce proceedings are pending).
- Adult Child.
- Parent.
- Adult Sibling.
- Any person or judicial body authorized by law or regulation.
It is important to note that different states and foreign countries may vary in their definitions of LARs and their order of priority. The Principal Investigator (PI) must understand and describe how differing state or international requirements will be met for the research [1].
The Critical Role of Assent
Even when surrogate consent is obtained from an LAR, the informed consent process is not complete. The IRB will typically require that the assent of the subject be obtained [1]. Assent is defined as an "affirmative agreement to participate in research," and it is explicitly noted that "failure to object does not qualify as assent" [1]. This process respects the residual autonomy of the individual and serves as a primary mechanism for identifying potential disagreements between the patient and their LAR.
Protocol for Handling Disagreements Between an LAR and Patient Wishes
Assessment and Continuous Monitoring
The cornerstone of managing disagreements is a proactive and ongoing assessment of the subject's wishes and capacity.
- Initial Capacity Assessment: Prior to obtaining LAR consent, the investigator must conduct a formal assessment of the prospective subject's decision-making capacity, as approved by the IRB [1].
- Ongoing Communication: For subjects with fluctuating or limited decision-making capacity, the PI should establish and maintain ongoing communication with both the subject and their caregivers [1]. This allows for the continuous monitoring of the subject's views and potential changes in capacity.
Operational Protocol for Patient-LAR Disagreement
The following workflow should be followed when a subject's actions or expressions conflict with the LAR's decision to enroll or continue participation in the research.
Diagram 1: Protocol for resolving disagreements between an LAR and a patient.
Identification and Immediate Action: If a prospective subject, through verbal objection or behavioral resistance (e.g., pulling away, expressing distress), indicates disagreement with participation, the research procedures must halt immediately [1]. The protocol states unequivocally that "if participation in the research is protested by the prospective subject," the LAR may not consent [1].
Formal Re-assessment of Capacity: The investigator must formally re-evaluate the subject's decision-making capacity. This assessment should determine if the subject has regained the capacity to provide their own informed consent or if the objection stems from a retained lack of capacity.
Resolution Pathways:
- If Capacity is Regained: The subject's own decision is paramount. The LAR's authority is superseded, and the subject must provide or withhold their own informed consent [1].
- If Capacity is Not Regained: The subject's protest, even without full capacity, must be respected. The LAR's consent is invalidated by the protest, and the subject cannot be enrolled or must be withdrawn from the study [1]. The only exception noted is for certain experimental treatments for progressive organic brain diseases, where implementation does not constitute the use of force despite objection [1].
Protocol for Handling Disagreements Among Multiple LARs
Establishing and Identifying the Authorized LAR
The first step in preventing conflict is to diligently identify the LAR with the highest priority according to the applicable law [1]. If a higher-ranking LAR is identified after consent has been obtained from a lower-ranking one, the researcher must contact the higher-ranking LAR, provide them with study information, and obtain their consent. All communications must be documented in a note to file [1].
Operational Protocol for Inter-LAR Disagreement
When two or more individuals with equal decision-making priority (e.g., two adult children) disagree on the subject's participation, a strict protocol must be followed.
Diagram 2: Protocol for resolving disagreements among multiple LARs.
Immediate Halt: The regulation is explicit: "If two or more persons who qualify as legally authorized representatives and have equal decision-making priority... inform the principal investigator... that they disagree as to participation... the subject shall not be enrolled in the human research" [1]. This is a non-negotiable requirement.
Facilitated Discussion: The researcher's role is to facilitate a structured discussion among the disagreeing LARs. This involves:
- Re-explaining the Research: Ensure all parties have a complete and identical understanding of the protocol, risks, and benefits.
- Referencing Subject Values: Guide the LARs to consider the prospective subject's own religious beliefs, basic values, and previously expressed wishes [1]. An LAR cannot consent to research that is "contrary to the religious beliefs or basic values of the prospective subject" [1].
- Employing Conflict Resolution Techniques: Utilize strategies such as active listening (paying complete attention and acknowledging emotions) and seeking common ground to de-escalate tension and foster a collaborative environment [66] [67].
Resolution and Documentation:
- If Consensus is Reached: Consent may be obtained from the agreeing LAR(s) and the enrollment process may proceed.
- If Consensus Fails: The subject must not be enrolled, or if the disagreement arises after enrollment, the subject should be withdrawn. The decision to withdraw must factor in any clinical risks associated with withdrawal, and the LARs should be fully informed of these risks [1].
Data and Conflict Management Strategies
Table 1: Legally Authorized Representative (LAR) hierarchy and regulatory constraints based on Virginia law [1].
| LAR Priority Level | Defining Relationship to Subject | Key Regulatory Constraints on LAR Authority |
|---|---|---|
| 1 | Agent under Advance Directive | Must be authorized for research decisions; highest priority. |
| 2 | Legal Guardian | Legal appointment required. |
| 3 | Spouse | Excludes cases where divorce is pending. |
| 4 | Adult Child | Any adult child can serve. |
| 5 | Parent | For adult subjects. |
| 6 | Adult Sibling | Any adult sibling can serve. |
| 7 | Other Authorized Body | As defined by specific law or regulation. |
| N/A | Multiple Equal-Priority LARs | Disagreement outcome: Subject cannot be enrolled. |
| N/A | Subject Protest | Disagreement outcome: LAR consent is invalidated. |
Conflict Resolution Strategies for Research Teams
Managing interpersonal conflict is a critical skill in these situations. Evidence-based strategies from healthcare settings can be directly applied [68] [67].
Table 2: Conflict management styles and their application in LAR disagreements [68] [67].
| Conflict Management Style | Description | Application in LAR Disputes |
|---|---|---|
| Collaborating | Working with all parties to find a mutually beneficial solution. | Ideal for facilitating discussions among multiple LARs to reach a consensus based on the subject's values. |
| Accommodating | Allowing the other party to address their concerns. | May be used by the researcher to yield to the LAR's deep knowledge of the subject's values. |
| Compromising | Seeking a middle ground that partially satisfies all. | Of limited use, as consent is binary; however, can be used to agree on a process for decision-making. |
| Avoiding | Neglecting or postponing the conflict. | Contraindicated. Delaying resolution violates ethical duties and regulatory timelines. |
| Controlling | Using authority to impose a solution. | Not applicable to the consent decision itself, but may be used by the PI to enforce procedural rules. |
Table 3: Research reagents and essential materials for implementing LAR consent protocols.
| Item/Reagent | Function/Explanation | Protocol Application |
|---|---|---|
| IRB-Approved Capacity Assessment Tool | A structured set of questions and observations to evaluate a subject's understanding of the research. | Used to formally determine the need for an LAR and to re-assess capacity in case of patient objection [1]. |
| LAR Hierarchy Reference Chart | A site-specific guide based on state or local law outlining the order of LAR priority. | Prevents procedural errors by ensuring the correct LAR is identified and consulted first [1]. |
| Witness (Impartial) | An individual not involved in the research (e.g., a nurse from another unit) who observes the consent process. | Required for specific consent processes (e.g., short-form consent); adds a layer of verification to the LAR consent process [2]. |
| Advance Directive / Durable Power of Attorney Document | Legal document in which a subject may have previously designated a healthcare agent. | The first resource to check; if present and it authorizes research decisions, it identifies the primary LAR [1]. |
| Documentation Kit (Note to File Template) | Pre-formatted templates for documenting unusual circumstances, LAR disagreements, and consent process details. | Critical for creating an auditable trail. Used to document the identification of a higher-ranking LAR, patient protests, or inter-LAR disagreements [2] [1]. |
Navigating disagreements between LARs and patients, or among multiple LARs, is a complex but manageable aspect of clinical research with vulnerable populations. The protocols outlined herein—prioritizing the cessation of procedures upon patient protest, adhering strictly to the legal hierarchy of LARs, and employing structured conflict resolution techniques—provide a robust framework for action. Meticulous documentation and proactive communication with the IRB are not merely best practices but ethical imperatives. By integrating these application notes and protocols, researchers can uphold the dual mandates of advancing scientific knowledge and steadfastly protecting the rights and welfare of all research subjects.
The process of informed consent is a cornerstone of ethical clinical research. However, within the specific context of studies involving Legally Authorized Representatives (LARs), researchers may encounter scenarios where obtaining even LAR consent is impracticable or would undermine the scientific validity of a study that offers significant clinical relevance. A LAR is an individual or judicial body authorized under applicable law to consent on behalf of a prospective participant who lacks the mental capacity to make such a decision [2]. Research involving adults with impaired decision-making capacity relies on LARs to protect the participants' rights and welfare.
This application note provides detailed protocols for navigating the strict regulatory conditions under which an Institutional Review Board (IRB) may grant a waiver or alteration of informed consent, including when the consent process would need to be conducted through a LAR. Framed within broader research on LAR-informed consent processes, this document aligns with the increasing focus on pragmatic clinical research and learning health systems, where traditional consent models can introduce selection bias and hinder the generation of generalizable evidence [69]. The guidelines herein are designed for researchers, scientists, and drug development professionals operating under stringent regulatory frameworks like the U.S. FDA's regulations and the Common Rule.
Regulatory Foundations and International Guidelines
The waiver of consent is not a discretionary shortcut but a formally regulated exception. Understanding the harmonized yet distinct international standards is crucial for designing ethical and compliant research protocols, especially for multi-site or global trials.
The U.S. FDA and Common Rule Framework
In the United States, the FDA established a final rule effective January 22, 2024, which harmonizes with the revised Common Rule (45 CFR 46.116(f)(3)) [70]. This rule allows an IRB to waive or alter the requirement for informed consent for minimal risk clinical investigations that include appropriate safeguards. The core criteria, as per FDA's § 50.22, are detailed in the experimental protocols section below [70].
International Perspectives on Waiver of Consent
A 2025 systematic review of guidelines identified broad international consensus on the principles for waiving consent in low-risk research [69]. The following table summarizes key international and national guidelines, demonstrating the global acceptance of these exceptions under specific conditions.
Table 1: International and National Guidelines on Waiver of Consent for Non-Emergency Clinical Research
| Governing Organisation (Region/Country) | Guideline Name | Year | Key Scope of Waiver Guideline |
|---|---|---|---|
| Council for International Organisations of Medical Sciences (CIOMS) (International) | International Ethical Guidelines for Health-related Research Involving Humans | 2016 | Applies to all health-related research, including studies with identifiable data/biospecimens, and research involving participants incapable of consenting [69]. |
| US Department of Health & Human Services (USA) | Code of Federal Regulations (The Common Rule) | 2019 (revised) | Applies to all "clinical investigations" and outlines specific criteria for IRB approval of a waiver [69]. |
| Canadian Institutes of Health Research (Canada) | Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans | 2018 | Articles 3.7A and 3.7B apply to all clinical research, with reference to use of data/biological materials and public health research [69]. |
| National Health and Medical Research Council (Australia) | National Statement on Ethical Conduct in Human Research | 2018 | Chapter 2.3.10 applies to all clinical research using personal or personal health information [69]. |
| European Parliament and Council (European Union) | Regulation No 536/2014 On Clinical Trials on Medicinal Products for Human Use | 2014 | Includes provisions for cluster randomised trials where groups rather than individuals are allocated to interventions [69]. |
This global alignment confirms that the waiver of consent is a recognized ethical tool for facilitating valuable, low-risk research that would otherwise be impracticable.
Core Conditions for a Waiver of Consent
The regulations stipulate a set of mandatory, interconnected conditions that must all be satisfied for an IRB to approve a waiver or alteration of consent. The following diagram illustrates the logical relationship and decision pathway for these core conditions.
Detailed Analysis of Condition Criteria
The Clinical Investigation Involves No More Than Minimal Risk to the Subjects: The FDA defines "minimal risk" in § 50.3(k) as the state where "the probability and magnitude of harm or discomfort anticipated in the research are not greater in and of themselves than those ordinarily encountered in daily life or during the performance of routine physical or psychological examinations or tests" [70]. This is a foundational threshold assessment.
The Waiver or Alteration Will Not Adversely Affect the Rights and Welfare of the Subjects: This criterion requires the IRB to consider whether the waiver itself could negatively affect the subjects' well-being. The FDA has clarified that it is not necessary to find that obtaining consent would be harmful, but rather that the waiver itself is not adverse to the subjects' rights and welfare. The IRB may also consider if the subject population would likely object to the waiver [70].
The Clinical Investigation Could Not Practicably Be Carried Out Without the Waiver or Alteration: This is the "impracticability" requirement. The FDA emphasizes that "practicably" does not mean "impossible" but rather that carrying out the investigation as designed without the waiver is impracticable [70]. Key considerations include:
- Scientific Validity: Would requiring consent introduce significant selection bias, rendering the study scientifically invalid? This is often the case in large-scale comparative effectiveness research or health system studies where a consenting population would not be representative [69].
- Undue Delay: Would restricting the research to consenting subjects unduly delay the investigation? For example, in research using archived, identifiable biospecimens, tracking down all donors for consent may be impracticable without compromising the timeline or feasibility of the research [70].
- Ethical Integrity: The Secretary's Advisory Committee on Human Research Protections (SACHRP) notes that ethical concerns can be raised if consent were required, supporting the argument for impracticability [70].
Additional Criterion for Identifiable Information/Biospecimens: Whenever the research involves using identifiable private information or identifiable biospecimens, a fourth criterion must be met: the investigation could not practicably be carried out without using such information or biospecimens in an identifiable format [70]. This addresses privacy concerns and ensures that identifiers are not used unnecessarily.
Distinguishing Between Types of Waivers
A critical operational distinction exists between a full Waiver of Consent and a Waiver of Written Documentation of Consent. Confusing these can lead to serious regulatory non-compliance.
Table 2: Comparison of Waiver of Consent vs. Waiver of Written Consent
| Aspect | Waiver of Consent | Waiver of Written Consent |
|---|---|---|
| Definition | IRB fully waives the requirement to obtain informed consent from participants or LARs [71]. | IRB waives the requirement to obtain a signed consent form. The full consent process must still occur [71]. |
| When Granted | Rare; for minimal risk research where consent is impracticable and the other regulatory criteria are met. Often for research on non-identifiable data or specific public health programs [71]. | More common; when the signed document itself is the only risk to the participant (e.g., research on sensitive topics), or in virtual/decentralized trials where verbal/electronic consent is obtained without a signature [71]. |
| Consent Process | No consent process is undertaken. Participants are not informed of the research, typically because the research would be invalidated by the act of consenting [69]. | The entire consent discussion, including all required elements of informed consent, must be delivered and understood by the participant or LAR. The only element waived is the signature [71]. |
| Typical Use Cases | Retrospective chart reviews, analysis of leftover anonymized biospecimens, large-scale health system quality improvement studies [69]. | Telephone-based consent, online surveys, decentralized clinical trials where consent is confirmed via a digital "click-to-agree" instead of a wet signature [71]. |
Experimental Protocol for IRB Application and Implementation
This section provides a detailed, step-by-step protocol for researchers to follow when seeking a waiver of consent, particularly for studies where LAR consent would typically be required.
Protocol: Application for Waiver of Consent for Minimal Risk Research
Aim: To provide a standardized methodology for preparing and submitting an IRB application for a waiver or alteration of informed consent under FDA 21 CFR 50.22 and the Common Rule 45 CFR 46.116(f).
Background: This protocol is designed for research involving adults who lack capacity, where seeking LAR consent may be impracticable, and the study poses no more than minimal risk. An example is a retrospective data analysis to compare the outcomes of two standard-of-care therapies for dementia patients.
Materials/Reagent Solutions: Table 3: Research Reagent Solutions for Consent Waiver Applications
| Item/Tool | Function in Protocol |
|---|---|
| IRB Submission Forms | Official documents required by the reviewing IRB to initiate the waiver request. |
| Study Protocol Document | The master document detailing the study's background, objectives, methodology, and statistical analysis plan. |
| Waiver Justification Template | A structured document (internal or from the IRB) to systematically address each of the four regulatory criteria. |
| Data Security Plan | A detailed description of the administrative, technical, and physical safeguards to protect participant data, crucial for satisfying the "no adverse effect" criterion. |
| HIPAA Authorization Waiver Application | If applicable, a separate application for waiver of HIPAA authorization for use of Protected Health Information (PHI). |
Methodology:
Pre-Submission Assessment:
- Confirm Minimal Risk: Justify in the protocol why the probability and magnitude of harm are no greater than those encountered in daily life. For a records review, the primary risk is often a privacy breach, not a physical risk.
- Define the Population: Clearly describe the participant population (e.g., "adults aged 65+ with a diagnosis of Alzheimer's disease and at least one hospitalization in 2024"). Justify why these individuals lack capacity and why the research cannot be conducted with a population that can consent.
Drafting the Waiver Justification:
- Criterion 1 - Minimal Risk: State the minimal risk designation and provide the rationale. Reference the study procedures (e.g., "review of existing medical records") to support the claim.
- Criterion 2 - No Adverse Effect on Rights/Welfare: Argue that the waiver itself will not harm participants. Emphasize robust data protection measures (e.g., de-identification, secure data storage, limited access). State that participants will not be deprived of any rights or beneficial treatments as a result of the waiver.
- Criterion 3 - Impracticability: This is the most critical justification. Provide a detailed, evidence-based argument for why the study could not practicably be carried out without the waiver. For research involving those who lack capacity, arguments may include:
- Infeasibility of LAR Identification: For large datasets, identifying and contacting a current LAR for hundreds or thousands of potential participants may be logistically impossible.
- Selection Bias: If the study aims to be representative of all patients with a condition, requiring LAR consent would systematically exclude those without an engaged LAR, introducing significant bias and compromising the scientific validity [69].
- Undue Burden: The resource and time burden of obtaining LAR consent for a minimal risk study may be disproportionate and could unduly delay the research, which has significant clinical relevance for improving care for this vulnerable population.
- Criterion 4 (if applicable) - Use of Identifiers: Justify why the research requires identifiable information. For example, a chart review may require identifiers to link data from different hospital systems for a complete clinical picture. Argue that the research could not be practicably carried out in an anonymized format.
IRB Submission and Review:
- Submit the complete application package, including the filled IRB forms, study protocol, and the detailed waiver justification.
- Be prepared to answer IRB questions and provide additional clarification, particularly on the impracticability argument.
Post-Approval Workflow: The following diagram outlines the operational workflow following IRB approval of a waiver of consent.
Expected Outcomes: Upon successful justification, the IRB will issue a formal approval of the waiver or alteration. The research may then proceed without obtaining consent from participants or their LARs, in strict adherence to the approved protocol and the described data safety measures.
The waiver of informed consent, including in the context of research involving individuals who require a LAR, is a carefully circumscribed regulatory exception. It is not an absence of ethical consideration but a different pathway grounded in the principles of minimal risk, impracticability, and the protection of rights and welfare. For researchers working with populations lacking capacity, understanding these strict conditions is paramount. By applying the structured protocols and justifications outlined in this document, researchers can ethically and lawfully advance clinically relevant studies that would otherwise be impossible, thereby contributing to the evidence base for treating some of the most vulnerable patient populations.
Special Considerations for Emergency Research and Cluster Randomized Trials
Cluster Randomized Trials (CRTs) represent a critical methodological approach in clinical research, particularly in fields like emergency medicine where individual randomization is often impractical or unethical. In CRTs, groups of individuals (clusters)—such as hospital emergency departments, ambulances, or geographic regions—are randomly assigned to different intervention arms rather than randomizing individuals themselves. This design is especially relevant for researching legally authorized representative informed consent processes, as consent procedures often need to be implemented at an institutional or system level rather than determined individually. The complexity of emergency settings introduces unique methodological challenges that require special consideration beyond standard individually randomized trials, particularly regarding statistical power, ethical implementation, and analytical approaches that account for the clustered nature of the data [72] [73].
The application of CRTs to emergency research involving legally authorized representatives necessitates careful planning to address both the inherent clustering effects and the specific ethical dimensions of obtaining consent under time-sensitive, stressful conditions. This article outlines the specialized frameworks, methodologies, and analytical considerations required to conduct rigorous CRTs in this domain, with particular emphasis on recent methodological advances and their practical application.
Core Methodological Considerations for CRTs
Defining Appropriate Estimands
The ICH E9(R1) addendum on estimands, while foundational for clinical trials, requires specific extensions when applied to CRTs in emergency settings. An estimand—a precise description of the treatment effect to be quantified—must account for the clustered data structure and unique aspects of emergency research. A recent scoping review identified eight additional items that require consideration when defining estimands for CRTs beyond the standard five attributes in ICH E9(R1) [74]:
- Population of clusters: Clearly defining the clusters being randomized (e.g., emergency departments, ambulance services)
- Population of individuals under selection bias: Accounting for potential biases in patient selection within clusters
- Exposure time of individuals/clusters on treatment: Considering variable exposure durations in emergency settings
- How individuals and clusters are weighted: Distinguishing between individual-average versus cluster-average effects
- Whether summary measures are marginal or cluster-specific: Determining the appropriate level of analysis
- Strategies for cluster-level intercurrent events: Handling events that affect entire clusters
- How interference/spillover is handled: Managing cross-contamination between clusters
- Handling individuals who leave or change clusters: Addressing patient transfer between emergency facilities
For legally authorized representative consent research, the estimand must specifically address whether the primary interest lies in the average effect across all individuals (regardless of cluster size) or the average effect across clusters (where each cluster contributes equally regardless of size). This distinction is crucial as these estimands can differ in both magnitude and interpretation, potentially leading to different conclusions about intervention effectiveness [74] [73].
Statistical Analysis Plans for CRTs
Statistical Analysis Plans (SAPs) for CRTs require substantial adaptation from standard templates developed for individually randomized trials. Current reporting quality for CRT SAPs shows significant gaps, with fewer than 25% of SAPs reporting how a small number of clusters would be accommodated, and only 6% describing how the intracluster correlation would be estimated [75]. A proposed extension to SAP guidelines for CRTs addresses these deficiencies through specific modifications:
Table 1: Essential SAP Components for Cluster Randomized Trials
| SAP Component | Standard Trial Focus | CRT-Specific Adaptation |
|---|---|---|
| Terminology | Participant recruitment | Careful use of "identification of participants" where direct recruitment doesn't occur [73] |
| Baseline Characteristics | Individual-level characteristics | Presentation of both cluster-level and individual-level characteristics without statistical testing of cluster-level characteristics [73] |
| Estimands | Treatment effect at individual level | Clarification of target estimand(s) for each outcome; specifying whether interest lies in average effect across clusters or individuals [73] |
| Clustering Adjustment | Independence of observations | Specification of methods to accommodate clustering (cluster-level analysis, GLMM, GEE) and reporting of intra-cluster correlation [73] |
| Small Sample Corrections | Large sample approximations | Use of small sample corrections when number of clusters is small (<40) [73] |
For emergency research on consent processes, the SAP must additionally pre-specify how potential imbalances in cluster characteristics—which may arise from post-randomization identification of participants—will be handled analytically, typically through covariate adjustment or propensity score methods [73].
Advanced Design Considerations for Emergency Settings
Adaptive Designs with Limited Clusters
Emergency research often involves a limited number of available clusters due to practical constraints, making traditional fixed designs statistically challenging. Adaptive designs offer a promising approach for optimizing implementation strategies while maintaining statistical rigor. Simulation studies have demonstrated that adaptive designs with features such as early stopping for futility and arm dropping can provide modest power gains without increasing type I error rates, even with few clusters [72].
However, the feasibility of adaptive designs diminishes when the intra-cluster correlation (ICC) is high, as this increases the risk of incorrect interim decisions. For a four-arm CRT evaluating different consent process interventions, Bayesian hierarchical models have shown promise for interim decision-making, though they require careful specification of design parameters [72]:
- Number and timing of interim analyses
- Stopping rules for futility
- Arm dropping criteria based on accumulating data
- Sample size re-estimation procedures
For legally authorized representative research in emergency settings, where clusters may be limited and ICC potentially high, preliminary simulations are recommended to assess whether adaptive designs offer sufficient benefits to justify their added complexity.
Network Structure and Contamination Effects
The structure of relationships within and between clusters can significantly impact trial power, particularly for studies involving infectious processes or information transfer—both relevant to consent procedure implementation. Traditional power calculations based solely on the intra-cluster correlation coefficient (ICC) assume uniform correlation within clusters, but this often fails to capture complex network structures that affect intervention spread [76].
Simulation studies incorporating network models demonstrate that:
- Between-cluster mixing (cross-contamination) can severely reduce power, particularly when approximately half of contacts occur between clusters
- Within-cluster network structure affects power for certain types of interventions, with scale-free (Barabási-Albert) networks showing reduced power under "degree infectivity" conditions
- Standard power calculations tend to be conservative with no between-cluster mixing but can severely overestimate power with moderate to high mixing [76]
For consent process research, these findings highlight the importance of mapping communication networks within and between emergency departments to properly assess and account for potential contamination effects in trial design.
Implementation Protocols for Consent Process Research
Equity-Focused Implementation Mapping
Research on legally authorized representative consent processes must prioritize equitable implementation across diverse emergency care settings. The Implementation Mapping (IM) approach, guided by the Consolidated Framework for Implementation Research integrated with Health Equity (CFIR/HE), provides a structured framework for developing and evaluating consent interventions [77]. This approach involves five key tasks:
- Conducting a needs assessment to identify barriers and facilitators across different implementation stages
- Developing implementation outcomes and specifying performance objectives
- Selecting evidence-based implementation strategies
- Producing implementation protocols and materials
- Evaluating implementation outcomes and generating continuous feedback
For consent process research, this approach emphasizes the identification and addressing of structural, cultural, and systematic factors that may create disparities in how legally authorized representatives engage with consent processes across different patient populations [77].
Hybrid Stepped-Wedge Cluster Randomized Design
The FOCUS (Facilitating the Implementation of Population-wide Genomic Screening) study protocol offers a relevant template for implementing complex interventions across multiple emergency settings. This hybrid stepped-wedge CRT design combines implementation and effectiveness evaluation while systematically rolling out interventions across clusters [77]. Key features include:
- Staged implementation across clusters over multiple time periods
- Collection of both process and outcome measures throughout implementation
- Explicit focus on equity metrics across diverse populations and settings
- Practical packaging of implementation strategies into freely available toolkits
For consent process research, this design enables sequential implementation across emergency departments while collecting systematic data on both the consent process outcomes (e.g., timing, comprehension, satisfaction) and implementation facilitators and barriers.
Table 2: Data Collection Framework for Consent Process CRTs
| Domain | Implementation Stage | Key Metrics | Equity Considerations |
|---|---|---|---|
| Reach | Exploration & Emerging | Proportion of eligible patients/LARs engaged | Demographic comparability between engaged and non-engaged populations |
| Effectiveness | Implementation | Consent comprehension scores; decision conflict measures | Differential effectiveness across patient subpopulations |
| Adoption | Planning & Implementation | Proportion of clinicians using standardized consent protocols | Variation in adoption across different types of emergency settings |
| Implementation | Implementation | Fidelity to consent protocol; time to consent completion | Resource requirements across different settings |
| Maintenance | Sustainment | Continued use of consent protocols over time | Long-term sustainability across diverse resource environments |
Visualization of CRT Workflow for Emergency Consent Research
The following diagram illustrates the key decision points and workflow for designing and implementing CRTs in emergency research on legally authorized representative consent processes:
CRT Design Workflow for Emergency Consent Research
This workflow emphasizes the sequential phases of CRT design, highlighting critical decision points specific to emergency consent research, from initial estimand definition through implementation planning to analytical considerations.
The Researcher's Toolkit: Essential Methodological Components
Successful implementation of CRTs in emergency consent research requires specific methodological tools and approaches. The following table summarizes key components and their applications:
Table 3: Methodological Toolkit for Emergency Consent CRTs
| Toolkit Component | Function | Application in Consent Research |
|---|---|---|
| Implementation Mapping | Structured framework for developing and evaluating implementation strategies | Systematically addressing barriers to equitable consent process implementation [77] |
| Bayesian Hierarchical Models | Analytical approach for complex data structures with limited clusters | Enabling adaptive designs and providing robust effect estimation with few clusters [72] |
| Small Sample Corrections | Statistical adjustments for limited number of clusters | Preventing biased standard errors when few emergency departments participate [75] [73] |
| Network Analysis | Assessment of within-cluster and between-cluster structures | Mapping communication pathways that affect consent process implementation [76] |
| Equity Frameworks | Structured assessment of implementation equity | Ensuring consent processes work effectively across diverse patient populations [77] |
| Hybrid Effectiveness-Implementation Designs | Simultaneous evaluation of intervention and implementation | Assessing both consent process outcomes and implementation facilitators/barriers [77] |
Cluster randomized trials present powerful methodological approaches for researching legally authorized representative informed consent processes in emergency settings, where individual randomization is often impractical. The special considerations outlined in this article—including appropriate estimand definition, accounting for cluster effects in analysis, utilizing adaptive designs with limited clusters, and addressing network structures and contamination effects—provide a framework for conducting methodologically rigorous research in this critical area. By applying these specialized methods and protocols, researchers can generate robust evidence to improve consent processes while respecting the unique ethical and practical constraints of emergency care environments.
Ensuring Excellence: Validating Comprehension and Comparing International Standards
Table of Contents
- Introduction
- Quantitative Comparison of Validation Techniques
- Experimental Protocols
- Process Workflows
- Research Reagent Solutions
- Conclusion
Within the critical context of obtaining informed consent from legally authorized representatives (LARs), ensuring true comprehension of complex clinical research information is a fundamental ethical and legal requirement. LARs, often making decisions under significant stress, may face challenges in processing and retaining detailed procedural, risk, and benefit information. This document provides detailed application notes and protocols for three evidence-based techniques—Teach-Back, Quiz/Feedback, and Interactive Media—to validate the understanding of LARs in the informed consent process. The systematic implementation of these techniques safeguards participant rights, enhances the quality of consent, and strengthens the integrity of clinical research data.
Quantitative Comparison of Validation Techniques
The following tables summarize key performance metrics and operational characteristics of the three validation techniques, aiding researchers in selecting and implementing the most appropriate method for their specific consent context.
Table 1: Efficacy and Outcome Measures of Understanding Validation Techniques
| Technique | Key Efficacy Findings | Impact on Knowledge/Understanding | Impact on Process/Behavioral Outcomes |
|---|---|---|---|
| Teach-Back | Reinforces patient education; improves knowledge retention [78]. Significantly higher scores on diagnosis knowledge and follow-up instructions [78]. | Improved patient understanding and adherence; up to 80% of medical information is forgotten immediately without it [79]. | Decreased call backs and cancelled appointments; improved patient satisfaction and outcomes [79]. Statistically significant improvement in 30-day readmission rates for certain conditions (e.g., from 25% to 12%) [78]. |
| Quiz/Feedback | Authentic quizzes assessing application, not just recall, provide deeper insights into understanding [80]. | Effectively measures learner success and reinforces key concepts; short response questions can assess higher-order thinking [80]. | Data from quizzes can identify patterns of misunderstanding, skills gaps, and prove training ROI for organizations [80]. |
| Interactive Media | An interactive media development process was categorized as 84% valid by experts [81]. | Improves shared decision-making and effectively assesses and presents risks [10]. Particularly useful for improving specific literacy (e.g., financial) [81]. | The ADDIE model (Analysis, Design, Development, Implementation, Evaluation) provides a structured framework for creating effective media [81]. |
Table 2: Operational Characteristics and Implementation Context
| Technique | Primary Implementation Setting | Method of Delivery | Time & Resource Investment |
|---|---|---|---|
| Teach-Back | Clinical settings: during discharge instructions, medication education, and explaining a new diagnosis [82] [79]. | A conversational loop: explain a concept, ask the patient/LAR to explain it back in their own words, re-clarify if needed [82]. | Takes longer initially but can save time later by preventing misunderstandings; requires staff training [82]. |
| Quiz/Feedback | Educational and assessment settings; can be integrated throughout a learning journey [80]. | Can be delivered via digital platforms; formats include permanent question sets or pools for unique assessments [80]. | Low-cost delivery and automatic grading; manual feedback is more resource-dependent [80]. |
| Interactive Media | Used to supplement explanations, especially for complex concepts or varying health literacy levels [10]. | Digital platforms (e.g., tablets, computers) presenting information in an engaging, multi-modal format [81]. | Requires significant upfront development effort (e.g., following the ADDIE model) but is scalable [81]. |
Experimental Protocols
Protocol 1: Implementing the Teach-Back Method for LAR Understanding
Objective: To confirm a legally authorized representative's comprehension of informed consent information by having them restate key concepts in their own words.
Materials: Informed consent document, plain language summary (optional).
Methodology:
- Explanation: Provide information to the LAR in small, manageable chunks. Use plain, simple, and clear language, avoiding medical jargon [79]. For example, explain the primary purpose of the research study.
- Soliciting Teach-Back: Ask the LAR to explain the information back to you in their own words. Use open-ended, non-threatening questions such as, "I want to be sure I explained everything clearly. Can you please tell me back in your own words what you understand this study involves?" [82] Avoid closed-ended questions like "Do you understand?" [82].
- Assessment and Re-clarification: Listen carefully to the LAR's response.
- If the explanation is correct and complete, acknowledge their understanding and proceed to the next segment of information [78].
- If any information is incorrect, incomplete, or misunderstood, gently correct the misunderstanding using an alternative explanation or different words. Avoid blaming the LAR (e.g., "I realize I didn't explain that well enough. Let me try again...") [79].
- Iteration: Repeat this process—explain, solicit teach-back, and clarify—for all critical elements of the informed consent, including procedures, risks, benefits, alternatives, and the voluntary nature of participation [10].
- Documentation: Document the use of the teach-back method and the LAR's demonstrated understanding in the research record or progress notes [10].
Protocol 2: Designing and Administering a Comprehension Quiz with Feedback
Objective: To quantitatively and qualitatively assess a LAR's retention and understanding of key informed consent elements and provide targeted feedback to correct misconceptions.
Materials: Validated quiz instrument (digital or paper-based).
Methodology:
- Quiz Design:
- Focus on Application: Construct questions that mirror real-world decisions the LAR might face, assessing application and higher-order thinking rather than rote memorization [80]. For example, present a scenario and ask what action they should take based on the protocol.
- Question Format: Utilize a mix of multiple-choice questions for breadth and short-response questions for depth, allowing LARs to articulate understanding in their own words [80].
- Pilot Testing: Pre-validate the quiz tool with a small sample to reveal unclear or leading questions, ensuring it accurately captures understanding [83].
- Administration: Administer the quiz after the initial consent discussion but before the LAR provides formal, signed consent.
- Analysis and Feedback:
- Scoring: Score the quiz to identify specific areas of misunderstanding.
- Targeted Feedback: Provide immediate, targeted feedback. For incorrect answers, explain why the chosen answer is incorrect and clarify the correct information. This feedback resolves misconceptions and delivers insights into areas for improvement [80]. This step is crucial for rectifying knowledge gaps before consent is finalized.
- Documentation and Action: Document the quiz results and any corrective feedback provided. If significant misunderstandings are identified, schedule a follow-up discussion with the principal investigator to revisit and clarify the information before proceeding.
Protocol 3: Developing and Deploying Interactive Media for Consent Education
Objective: To create and implement an interactive media tool that improves LAR engagement and comprehension of complex research information.
Materials: Multimedia development tools (e.g., graphic design software, video editing, e-learning authoring tools).
Methodology (Based on the ADDIE Model) [81]:
- Analysis: Analyze the needs and constraints. Identify the specific complex concepts from the informed consent that require clarification (e.g., randomization, placebo). Assess the target audience (LARs) and their potential literacy and technological barriers.
- Design: Storyboard the interactive experience. Define the learning objectives for each segment. Plan the user interface, interactions (e.g., clickable information points, embedded quizzes), and media elements (graphics, animations, voice-overs).
- Development: Produce the interactive media asset according to the design. Use simple language and clear visuals. Incorporate self-assessment questions or interactive prompts to reinforce learning.
- Implementation: Deploy the media with LARs during the consent process. This can be used as a preparatory tool before meeting the investigator or as a supplementary aid during the discussion. Ensure the technology is accessible and user-friendly.
- Evaluation: Conduct a validity test via expert review (e.g., media and material experts) to ensure accuracy and usability [81]. Gather feedback from LARs on the tool's helpfulness and clarity to inform future iterations.
Process Workflows
Teach-Back Validation Workflow
Interactive Media Development Process
Research Reagent Solutions
Table 3: Essential Materials and Tools for Validating Understanding
| Item/Category | Function in Validation Protocol | Example Application in LAR Consent |
|---|---|---|
| Plain Language Summary | A simplified version of the informed consent document, written at an accessible reading level. | Serves as the primary text for the Teach-Back protocol, ensuring information is initially conveyed in an understandable manner [10]. |
| Validated Quiz Instrument | A structured set of questions designed to assess comprehension of key consent elements. | Used in the Quiz/Feedback protocol to quantitatively measure the LAR's understanding of risks, procedures, and rights [80]. |
| Interactive Media (e.g., App, Video) | A digital tool that uses multimedia (animation, video, interactive Q&A) to explain complex concepts. | Deployed in the Interactive Media protocol to visually explain concepts like randomization or the mechanism of action of the investigational product [81]. |
| Health Literacy Screening Tool (e.g., NVS, REALM) | A brief tool to identify individuals with limited health literacy. | Used during the initial consent meeting to tailor the communication strategy (e.g., more visuals, slower pace) to the LAR's needs [10]. |
| Professional Medical Interpreter | A qualified linguist for communicating with LARs with limited English proficiency. | Essential for ensuring all three validation techniques are implemented accurately and without language barriers [10] [82]. |
| Standardized Documentation Form | A checklist or template for recording the validation process. | Used across all protocols to consistently document the use of Teach-Back, quiz results, or the use of interactive media, creating an audit trail [10]. |
The integration of structured validation techniques—Teach-Back, Quiz/Feedback, and Interactive Media—into the process of obtaining consent from legally authorized representatives represents a significant advancement in ethical clinical research practice. These methods move beyond mere signature acquisition to actively verify and promote comprehension. By adopting the detailed application notes and protocols provided, researchers and drug development professionals can ensure that consent is truly informed, thereby upholding the highest standards of participant autonomy, regulatory compliance, and research integrity. The choice of technique can be tailored to the complexity of the study and the specific needs of the LAR, and these methods are often most effective when used in combination.
For clinical investigations involving legally authorized representatives (LARs), who provide consent on behalf of prospective subjects who lack capacity, auditing and monitoring the consent process is a critical ethical and regulatory safeguard. The informed consent process is not a single event but a continuum that begins with recruitment and continues throughout the study, requiring ongoing verification to ensure LARs can provide truly informed permission [32]. Effective oversight relies on Key Performance Indicators (KPIs) to quantitatively measure compliance, process quality, and ethical rigor. This document provides detailed application notes and experimental protocols for establishing a robust monitoring framework.
Regulatory guidance from the FDA emphasizes that Institutional Review Boards (IRBs) have the authority to observe the consent process as part of their quality assurance activities, which can be delegated to a qualified monitor [84] [32]. The 2025 updates to the FDAAA 801 Final Rule further underscore the importance of transparency, now requiring the public posting of redacted informed consent documents for Applicable Clinical Trials (ACTs) [85]. This elevates the need for meticulous pre-submission auditing of these documents.
Key Performance Indicators (KPIs) for Consent Compliance
Tracking the right KPIs is essential for demonstrating that a compliance program is not only well-designed but also functioning effectively in practice [86]. The following quantitative metrics are categorized to evaluate different facets of the consent process involving LARs.
Table 1: Execution and Process KPIs for Consent Monitoring
| KPI Category | Specific Metric | Target/Standard | Data Collection Method |
|---|---|---|---|
| Process Adherence | Percentage of consent sessions where all required elements are verbally disclosed [32] | >98% | Consent Monitor Checklist [84] |
| Percentage of consent forms that are 100% complete and correctly executed | 100% | Document Audit | |
| Timeliness | Average time from LAR identification to completed consent process | Site-defined benchmark | Study tracking log |
| Percentage of consent forms updated within protocol-defined timeframe for new information [32] | >95% | Protocol and Document Audit | |
| Documentation Quality | Rate of documentation errors per consent form (e.g., unsigned corrections, missing dates) | <2% | Quality Control Sample Audit |
| Percentage of redacted consent forms posted to ClinicalTrials.gov per FDAAA 801 [85] | 100% | Regulatory Submission Audit |
Table 2: Outcome and Effectiveness KPIs for Consent Monitoring
| KPI Category | Specific Metric | Target/Standard | Data Collection Method |
|---|---|---|---|
| LAR Understanding | Percentage of LARs who successfully answer all key comprehension questions post-consent discussion [84] | >90% | Structured Quiz or Teach-Back Assessment |
| Participant & LAR Experience | LAR satisfaction score with the consent process (e.g., % rating clarity and respect as "high") [87] | >4.0 on 5-point scale | Post-Consent Survey |
| Protocol Compliance | Percentage of enrolled subjects/LARs with no audit findings related to consent | >95% | Internal Quality Assurance Review |
| Rate of consent-related protocol deviations or violations | <5% | Deviation Tracking System |
Experimental Protocols for Consent Auditing
Protocol 1: Direct Observation of the LAR Consent Process
This protocol outlines the methodology for a consent monitor to directly observe the dynamic interaction between the investigator and the LAR.
3.1.1 Methodology
- Objective: To verify that the investigator provides all required information in a manner that is understandable and free from coercion, and that the LAR has an adequate opportunity to ask questions.
- Materials: IRB-approved consent form, consent monitor checklist, quiet/private room for observation.
- Procedure:
- Pre-Session Briefing: The consent monitor meets with the investigator to confirm the version of the consent form to be used.
- Observation: The monitor silently observes the entire consent discussion, documenting against a standardized checklist [84].
- Assessment of Understanding: The monitor listens to the LAR's questions and the investigator's answers. The monitor may also directly facilitate comprehension by asking the LAR open-ended questions that require thoughtful responses, such as "Can you describe what you believe the main risks of this study are?" [84].
- Documentation: The monitor documents the interaction, including the duration, all questions asked, the adequacy of answers, and the overall dynamic.
- Post-Session Debrief: Immediately after the session, the monitor reviews observations with the investigator, providing additional training if needed [84]. A summary report is submitted to the IRB.
Protocol 2: Audit of Informed Consent Documentation
This protocol describes a systematic review of completed consent forms to ensure accuracy, completeness, and regulatory compliance.
3.2.1 Methodology
- Objective: To ensure every informed consent form in the study records is executed according to FDA regulations, IRB policies, and protocol specifications.
- Materials: Source documents, IRB-approved consent form templates, regulatory binder, audit checklist.
- Procedure:
- Sample Selection: Determine audit sample size (e.g., 100% of initial consents, plus a random sample of re-consents).
- Verification of Elements: For each form, verify the presence of all required elements as per 21 CFR 50.25, including a statement that the study involves research, a description of foreseeable risks, and a clear explanation of the LAR's role and authority [32].
- Execution Check: Confirm the form is signed and dated by the LAR and the investigator before any study procedures are initiated. Ensure any corrections are initialed and dated.
- Version Control: Confirm the correct IRB approval date and version number of the form is used.
- Findings and Remediation: Document any findings. Classify errors by severity and require immediate corrective and preventive action (CAPA) for critical findings.
Protocol 3: LAR Understanding Assessment using the Teach-Back Method
This protocol assesses the effectiveness of the consent communication by evaluating the LAR's comprehension.
3.3.1 Methodology
- Objective: To quantitatively and qualitatively measure the LAR's understanding of key study elements after the consent discussion.
- Materials: Scripted, open-ended questionnaire (e.g., covering purpose, procedures, risks, benefits, alternatives, rights).
- Procedure:
- Administration: After the consent discussion but before the LAR signs the form, a neutral party (e.g., the consent monitor) administers the questionnaire.
- Questioning Technique: Use the teach-back method: "To make sure I did a good job explaining, could you tell me in your own words what you believe will happen if you decide to withdraw from the study?"
- Scoring: Score responses using a pre-defined rubric (e.g., 2=full understanding, 1=partial understanding, 0=misunderstanding or no understanding).
- Action: If understanding is inadequate, the monitor informs the investigator, who must re-explain the misunderstood concepts. The process is repeated until understanding is satisfactory. This data is aggregated to calculate the KPI for LAR understanding.
Visualization of Consent Monitoring Workflows
The following diagram illustrates the logical workflow and decision points for monitoring the LAR consent process, from preparation through to reporting and potential remediation.
The Scientist's Toolkit: Essential Materials for Consent Auditing
Implementing a rigorous consent auditing program requires specific tools and documents to ensure consistency, compliance, and thorough documentation.
Table 3: Research Reagent Solutions for Consent Process Auditing
| Tool / Material | Function & Application | Critical Attributes |
|---|---|---|
| Consent Monitor Checklist | Standardized form to ensure all regulatory and protocol-required elements are consistently discussed during the consent process with the LAR [84]. | IRB-approved, protocol-specific, includes space for qualitative notes. |
| Electronic Consent (eConsent) System | Digital platform for presenting consent information, capturing e-signatures, and potentially embedding multimedia or comprehension checks. | 21 CFR Part 11 compliance, audit trail functionality, accessibility features. |
| LAR Understanding Assessment Tool | A structured questionnaire, typically using open-ended questions or the Teach-Back method, to quantitatively assess the LAR's comprehension post-discussion [84]. | Validated for clarity and objectivity, covers key concepts (risks, benefits, alternatives, rights). |
| Informed Consent Form (ICF) Template | The master document, approved by the IRB, used for obtaining consent from LARs. | Contains all elements per 21 CFR 50.25, uses lay-friendly language at an appropriate reading level, includes LAR-specific designation sections. |
| FDA Final Guidance on Informed Consent | The foundational regulatory document (August 2023) outlining current FDA expectations for the entire consent process, from recruitment through study conduct [32]. | Reference for defining audit criteria and interpreting regulatory requirements for LAR situations. |
| Quality Management System (QMS) Software | A centralized system (e.g., Hyperproof, AuditBoard) for storing audit evidence, tracking findings, managing CAPA, and monitoring KPI dashboards [88] [89]. | Automated evidence collection, issue tracking, real-time reporting capabilities. |
The globalization of clinical research requires robust frameworks to ensure ethical conduct and data reliability across regions. For professionals conducting multi-regional clinical trials (MRCTs), navigating the harmonized yet distinct requirements of the International Council for Harmonisation (ICH), U.S. Food and Drug Administration (FDA), and European Medicines Agency (EMA) is critical [90]. The informed consent process, particularly when involving Legally Authorized Representatives (LARs) for decisionally impaired or vulnerable participants, sits at the intersection of ethics and regulation. This application note provides a detailed comparison of these regulatory frameworks, with a specific focus on LAR consent processes, and offers actionable protocols for compliance.
Regulatory Framework Comparison
The following table summarizes the core regulatory frameworks governing clinical trials, highlighting their status, foundational principles, and specific stances on LAR consent.
Table 1: Key Regulatory Frameworks for Clinical Trials
| Framework | Status & Jurisdiction | Core Principles & Focus | LAR Consent Stipulations |
|---|---|---|---|
| ICH E6(R3) Good Clinical Practice | Final Guideline (Step 4); Adopted internationally (e.g., EU from July 2025; U.S. FDA Sept 2025) [91] [92] [93]. | Principles-based, risk-proportionate approach [91]. Embraces digital technologies (eConsent, DCTs) and robust data governance [91] [92]. | Refers to "legally acceptable representative" throughout, aligning with Declaration of Helsinki on participant autonomy [92]. |
| U.S. FDA Regulations | Legally binding U.S. law under 21 CFR Parts 50, 56, 312 [92] [94]. | Focus on data integrity and patient safety for FDA-regulated investigational products [94] [95]. ICH E6(R3) is adopted as guidance, but specific CFRs are binding [92]. | 21 CFR 50.20 allows consent from LAR if patient cannot consent. 21 CFR 50.25 defines basic & additional consent elements but does not detail LAR process [96]. |
| EU Clinical Trials Regulation (CTR) | Legally binding in EU/EEA; ICH E6(R3) compliance required from 23-Jul-2025 [97] [92]. | Single submission portal (CTIS) for member states [97]. Protects participant rights, safety, well-being, and data credibility [97]. Equivalent ethical standards required for non-EU trials [97]. | National laws of EU Member States implement CTR and define who qualifies as an LAR and the specific consent procedures. |
The landscape is evolving, with ICH E6(R3) representing a significant modernization. Its structure now comprises a high-level Principles document, Annex 1 for interventional trials, and a planned Annex 2 for non-traditional trials [91]. A key conceptual shift in R3 is the move from a "one-size-fits-all" approach to a risk-proportionate system for oversight activities like continuing review, which ethics committees should calibrate to real participant risk [92].
Application Note: LAR Informed Consent in Multi-Regional Trials
Key Challenges and Regulatory Alignment
Obtaining informed consent via an LAR in MRCTs presents distinct challenges. Regulations agree on the ethical imperative but differ in implementation details, creating operational complexity.
- LAR Definition and Hierarchy: The legal definition of who can serve as an LAR (e.g., court-appointed guardian, family member hierarchy) is determined by national or local law, not ICH-GCP [94]. A central protocol may define a standard, but sites must always defer to their applicable local legislation.
- Documentation Practices: ICH E6(R2) guidelines required that the LAR receive a copy of the signed consent form [94]. While FDA regulations require the participant or LAR to receive a copy, it does not explicitly mandate it be the signed version [94]. ICH E6(R3) reinforces the principle of transparent information sharing.
- Cultural and Operational Hurdles: Cultural perceptions of legal authority and familial decision-making vary. Operationalizing LAR consent in Decentralized Clinical Trial (DCT) settings, endorsed by R3, requires secure, validated digital platforms for remote consent processes [91] [92].
Quantitative Data and Comparison
The following table compares specific consent elements across regulations, illustrating areas of harmony and divergence critical for LAR processes.
Table 2: Detailed Comparison of Informed Consent and LAR Provisions
| Regulatory Aspect | ICH E6(R3) & ICH GCP | U.S. FDA Regulations | EMA / EU CTR |
|---|---|---|---|
| Informed Consent Foundation | Protects participant rights, safety, well-being; essential prior to participation [91]. | Must comply with 21 CFR 50.20/27; legally effective consent is a prerequisite [94] [96]. | Mandated by Clinical Trials Regulation; details implemented via Member State law [97]. |
| LAR Consent Provision | Explicitly provided for when a participant is incapable of giving independent consent [91]. | Explicitly allowed under 21 CFR 50.20 [94]. | Required by CTR; specific LAR qualifications and processes defined by national law. |
| Consent Form Signature | Should be signed and dated by participant/LAR and person conducting consent discussion [94]. | Requires signature of participant/LAR only (21 CFR 50.27(a)) [94]. | Follows national member state law implementation of the CTR. |
| Copy of Consent Form | Subject/LAR should receive a signed and dated copy [94]. | Subject/LAR must receive a copy, but it need not be signed [94]. | Follows national member state law. |
| Additional Transparency | Requires informing participants about data fate upon withdrawal, storage duration, and results communication [92]. | 21 CFR 50.25(b) includes additional elements, e.g., consequences of withdrawal, as appropriate [96]. | The EU CTR emphasizes transparency, with specifics guided by national law and ICH E6(R3). |
Experimental Protocol: LAR Informed Consent Process
This protocol provides a standardized methodology for obtaining and documenting informed consent from an LAR in an MRCT setting, aligning with FDA, EMA, and ICH E6(R3) standards.
Materials and Reagents
Table 3: Research Reagent Solutions for Consent Documentation
| Item | Function/Application | Specifications/Standards |
|---|---|---|
| IRB/EC Approved Consent Form | Legally required document detailing study info, risks, benefits, rights. | Must be in language understandable to LAR/participant; version-controlled and IRB/EC-stamped [98]. |
| Electronic Consent (eConsent) Platform | Digital system for presenting consent info, capturing signatures. | Must be 21 CFR Part 11 compliant; validated for integrity, authenticity, confidentiality [95]. |
| Signature Log Form | Documents identity and legal authority of LAR. | Captures LAR's name, relationship, legal basis for authority, contact info. |
| Audio-Visual Recording Equipment | (Optional) Records consent conversation for verification. | Requires explicit permission from LAR; data storage must meet privacy laws (e.g., GDPR, HIPAA). |
| Legally Authorized Representative | Individual legally empowered to provide consent on behalf of prospective participant. | Authority must be verified per local site law (e.g., court order, healthcare proxy). |
Step-by-Step Procedure
Pre-Consent Verification of LAR Status (Site Responsibility)
- Action: Prior to the consent discussion, the site investigator or designee must verify the individual's legal authority to act as an LAR for the prospective participant.
- Documentation: This verification must be documented in the participant's source records (e.g., via a signature log or note to file). Acceptable documentation includes a certified copy of a court order for guardianship, a healthcare power of attorney document, or reference to a specific local statute granting automatic authority to a family member.
Consent Discussion and Process
- Action: The investigator or a designated, qualified sub-investigator must conduct the consent discussion with the LAR. The discussion must cover all elements required by 21 CFR 50.25 and the IRB/EC-approved consent form, using language that is understandable to the LAR [96].
- Timing: The discussion must occur in a setting and timeframe that allows the LAR to ask questions and consider participation freely, without coercion.
- Witness: A witness should be present if required by local law or IRB/EC policy.
Consent Documentation and Copy Provision
- Action: Obtain the signature of the LAR and the date on the IRB/EC-approved consent form.
- ICH E6(R3) Aligned Practice: Also have the person who conducted the informed consent discussion sign and date the form [94].
- Copy Provision: Immediately provide a copy of the fully executed consent form to the LAR. ICH GCP recommends this copy be signed and dated; FDA regulations require a copy but do not specify it must be signed [94]. Best practice is to provide a complete, signed copy.
Ongoing Communication (Post-Consent)
- Action: Inform the LAR that they will receive any significant new findings that may affect their willingness to continue the participant's involvement, as per 21 CFR 50.25(b)(5) [96].
- Data Transparency: Per ICH E6(R3), the consent form should also describe what happens to the participant's data if they withdraw from the study [92].
Workflow Visualization
The following diagram illustrates the logical workflow and decision points for the LAR consent process.
Successfully navigating the FDA, ICH-GCP, and EMA landscapes for LAR consent requires a meticulous, process-oriented approach. The modernization brought by ICH E6(R3), with its principles-based and risk-proportionate framework, supports the ethical and operational flexibility needed for complex MRCTs [91] [92]. The core regulatory requirement remains constant: LAR consent must be legally effective, thoroughly documented, and obtained with the same rigor as participant consent. By implementing the detailed protocols and comparisons provided, researchers can ensure robust compliance, strengthen participant protections, and facilitate the successful global acceptance of their clinical trial data.
The Food and Drug Administration Amendments Act of 2007 (FDAAA) Section 801 established mandatory registration and results reporting for certain clinical trials on the ClinicalTrials.gov database [85]. The 2025 Final Rule amendments introduce significant modifications that substantially reshape compliance requirements for clinical trial sponsors, investigators, and institutions [85]. These changes specifically enhance transparency through mandatory posting of informed consent documents and strengthen enforcement mechanisms with elevated penalties for non-compliance [85]. Within the context of research on legally authorized representative informed consent processes, these regulatory changes necessitate revised protocols and procedures to ensure compliance while maintaining ethical standards for participants who lack decision-making capacity [99]. The updated rule reflects regulatory alignment with global transparency initiatives while addressing technological advancements in clinical trial design and data management [100].
Key Regulatory Changes and Quantitative Specifications
The 2025 amendments introduce several critical modifications affecting how clinical trials are registered, monitored, and reported [85]. These changes impact various aspects of trial conduct from initiation through results dissemination.
Mandatory Posting of Informed Consent Documents: All Applicable Clinical Trials (ACTs) must now submit redacted versions of approved informed consent forms used to enroll participants [85]. These documents will be made publicly available on ClinicalTrials.gov or other designated federal websites, increasing transparency about what information participants receive [99].
Enhanced Penalty Structure: The FDA has strengthened enforcement mechanisms with increased civil monetary penalties that can now reach $15,000 per day for ongoing violations, a significant elevation from previous amounts [85]. This reflects a more aggressive stance on compliance enforcement.
Shortened Results Submission Timeline: The deadline for submitting summary results has been reduced from 12 months to 9 months after the primary completion date, except when a certificate of delay is formally granted [85]. This accelerates public access to trial outcomes.
Expanded Definition of Applicable Clinical Trials: The scope of trials subject to FDAAA requirements has been broadened to include more early-phase investigations and device trials that were previously exempt [85].
Real-Time Public Notification of Noncompliance: ClinicalTrials.gov will now publicly flag sponsors who miss registration or results submission deadlines, creating reputational incentives for compliance [85].
Quantitative Compliance Data and Historical Context
Table 1: Clinical Trial Results Reporting Compliance Before and After Regulatory Implementation
| Time Period | Reporting Within 12 Months | Reporting Within 36 Months | Key Regulatory Context |
|---|---|---|---|
| 2010-2014 | 8.3% | 40.8% | Pre-Final Rule implementation |
| 2017-2021 | 23.2% | 49.2% | Post-Final Rule implementation |
| Change | +14.9% | +8.5% | FDAAA Final Rule in effect |
Source: Mughal et al. (2025) analysis of ClinicalTrials.gov data [101]
Table 2: Penalty Structure for FDAAA 801 Non-Compliance
| Violation Type | Maximum Penalty | Enforcement Mechanism |
|---|---|---|
| Failure to register applicable clinical trial | Up to $15,000 per day | Civil monetary penalties |
| Failure to submit required results information | Up to $15,000 per day | Civil monetary penalties |
| Knowingly submitting false or misleading information | Up to $15,000 per day | Civil monetary penalties + potential criminal prosecution |
| Non-compliance after Notice | Additional penalties accrue daily after 30-day correction period | FDA enforcement actions [102] |
Source: 2025 FDAAA 801 Final Rule provisions [85]
Experimental Protocols for Compliance Implementation
Protocol 1: Informed Consent Document Redaction and Posting Workflow
Purpose: To establish a standardized methodology for preparing, redacting, and submitting informed consent documents in compliance with 2025 FDAAA 801 requirements while protecting participant privacy and confidential commercial information.
Materials and Reagents:
- Final IRB-approved informed consent document(s)
- Digital redaction software (e.g., Adobe Acrobat Pro)
- ClinicalTrials.gov PRS login credentials
- Document tracking spreadsheet
Procedure:
Document Identification: Identify the final version of the IRB-approved informed consent document actually used to enroll participants [99].
Redaction Preparation: Create a copy of the original consent document for redaction purposes, preserving the original approved version.
Systematic Redaction: Remove the following elements from the consent document copy:
- Participant identifying information (names, addresses, contact details)
- Investigator and site personnel signatures
- Confidential commercial information (proprietary manufacturing processes)
- Any other information that could compromise participant privacy or trade secrets [99]
Quality Verification: Implement a two-person verification process to ensure all required redactions are complete and no protected information remains.
Documentation: Maintain comprehensive records of:
- Original consent document
- Redacted version
- Redaction log with justification for each modification
- Verification documentation
Submission: Upload the redacted consent form to ClinicalTrials.gov via the Protocol Registration and Results System (PRS) within 60 days after the study is closed to recruitment, but no later than 60 days after the last study visit by any participant, as specified in the 2018 Common Rule [99].
Archiving: Store all documentation in the trial's master file with appropriate version control.
Protocol 2: Legally Authorized Representative Consent Process Documentation
Purpose: To establish specialized procedures for documenting informed consent processes involving legally authorized representatives (LARs) that meet both ethical standards and enhanced FDAAA 801 transparency requirements.
Materials and Reagents:
- LAR-specific consent form templates
- Capacity assessment documentation tools
- Electronic data capture system
- Audit trail functionality
Procedure:
Participant Capacity Assessment: Document the formal assessment of participant decision-making capacity using institutional standards, including:
- Specific cognitive assessment tools employed
- Clinical findings supporting determination
- Identification of the specific condition impairing decision-making capacity
LAR Qualification Verification: Establish and record the legal authority of the representative through:
- Documentation of relationship to participant
- Verification of legal authority to provide consent (e.g., court appointment documents, healthcare power of attorney)
- Confirmation of understanding of their role as decision-maker
LAR-Specific Consent Process: Implement a modified consent discussion that includes:
- Explanation of the participant's condition and inability to provide personal consent
- Discussion of the LAR's role and responsibilities
- Deliberation of the participant's previously expressed values and preferences (if known)
- Assessment of LAR understanding through teach-back methods
Dual Documentation: Create comprehensive records capturing:
- Standard consent form with LAR signature
- Supplemental documentation of the capacity assessment and LAR authorization
- Description of any participant assent obtained when possible
Regulatory Alignment: Ensure the redacted version for public posting maintains privacy while transparently demonstrating ethical LAR consent processes through appropriate redaction techniques that preserve process integrity without exposing protected health information.
Compliance Implementation Toolkit
Regulatory Compliance Workflow and Deadline Management
Purpose: To visualize the integrated compliance timeline and relationship between different regulatory requirements under the 2025 FDAAA 801 Rule.
Essential Research Reagents and Compliance Solutions
Table 3: Research Reagent Solutions for FDAAA 801 Compliance Implementation
| Tool Category | Specific Solution | Function in Compliance Process |
|---|---|---|
| Electronic Trial Master File | Veeva Vault Clinical, MasterControl | Centralized repository for consent documents, redaction logs, and submission confirmations |
| Clinical Trial Registry Software | TrialAssure Transparency Suite, Citeline | Automated tracking of registration and results submission deadlines |
| Redaction Technology | Adobe Acrobat Pro, Litera | Secure removal of protected health information from consent forms prior to posting |
| Regulatory Intelligence | FDAMap, ProRelix Research | Current regulatory interpretation and compliance strategy development |
| Document Management | SharePoint, Box | Version control and audit trails for consent form revisions and redactions |
| Submission Portal | ClinicalTrials.gov PRS | Official system for registration, results, and consent form submission |
Discussion and Strategic Implications
The 2025 FDAAA 801 Final Rule amendments represent a substantial shift toward greater transparency and accountability in clinical research [85]. The mandatory posting of informed consent documents creates both opportunities and challenges for research involving participants who require legally authorized representatives. While this requirement enhances public understanding of consent processes, it necessitates careful balancing between transparency and protection of vulnerable participants' privacy [99].
The enhanced penalty structure, with maximum fines of $15,000 per day, significantly raises the financial risk of non-compliance [85]. Recent FDA enforcement actions demonstrate increased regulatory attention to reporting violations [103] [102]. These penalties, combined with public notification of noncompliance, create powerful financial and reputational incentives for timely and accurate reporting.
For researchers focused on LAR consent processes, these regulatory changes necessitate protocol modifications that:
- Systematically document capacity assessments and LAR authorization
- Develop specialized redaction protocols for LAR consent forms
- Implement robust tracking systems for multiple regulatory deadlines
- Integrate compliance activities throughout the trial lifecycle
The shortened results submission timeline (9 months versus previous 12 months) accelerates the timeline for data analysis and presentation, requiring more efficient close-out processes [85]. This compression particularly impacts complex trials involving vulnerable populations with LARs, where data interpretation may require additional contextual analysis.
The 2025 FDAAA 801 Rule amendments substantially reshape the clinical trial regulatory landscape by increasing transparency through consent form posting and strengthening enforcement through enhanced penalties. For researchers studying legally authorized representative consent processes, these changes require implementation of robust compliance protocols that address both ethical and regulatory requirements. The experimental protocols and workflows presented in this document provide a framework for meeting these new requirements while maintaining scientific integrity and protecting participant rights. As regulatory enforcement intensifies [103], proactive compliance planning becomes essential for successful clinical trial management under these updated standards.
Application Notes: Context and Significance
Within the broader thesis on Legally Authorized Representative (LAR) informed consent process research, this document provides a detailed comparative analysis of LAR application in clinical (biomedical) versus behavioral research contexts. The responsible inclusion of adults with impaired decision-making capacity is a cornerstone of ethical research, yet practical approaches diverge significantly across disciplines. These differences arise from distinct risk profiles, regulatory interpretations, and the nature of participant interactions. This analysis provides researchers, scientists, and drug development professionals with structured data, standardized protocols, and practical tools to navigate these complexities and implement ethically sound, legally compliant LAR consent processes across research domains.
Quantitative Data Analysis
Table 1: Comparative Analysis of LAR Consent in Clinical vs. Behavioral Research
| Analysis Parameter | Clinical/Biomedical Research Context | Social-Behavioral Research Context |
|---|---|---|
| Primary Regulatory Focus | FDA regulations [21 CFR 50, 56]; Health Canada exceptions for clinical trials [14] [28] | Common Rule (45 CFR 46); Disability rights principles (presumption of competence, relational autonomy) [104] |
| Typical Risk Profile | Often greater than minimal risk (e.g., drug trials, invasive procedures) [2] | Often minimal risk (e.g., interviews, surveys) [104] |
| Core Ethical Principle | Protection from harm; waiver of LAR consent possible in emergency/COVID-19 settings [14] | Responsible inclusion; right to participate and make one's own decisions [104] |
| Documentation Standards | Formalized LAR signature on IRB-approved consent form; detailed documentation of capacity assessment [2] | Flexible documentation; emphasis on process (assent, ongoing consent) over form [104] |
| LAR Role Specification | Clearly defined in regulation; LAR provides full informed consent [2] | Often involves supported decision-making; LAR may act as a facilitator alongside participant [104] |
| Reported Prevalence of LAR Use | More commonly reported and structured [2] | Frequently excluded; lack of agreed-upon guidelines leads to widespread exclusion [104] |
Table 2: Key Research Reagent Solutions for LAR Consent Process Research
| Reagent/Material | Primary Function in LAR Consent Research |
|---|---|
| Informed Consent Capacity Assessment Tools | Quantitative or semi-structured tools to evaluate a potential participant's understanding, appreciation, and reasoning regarding research participation [104]. |
| IRB-Approved Consent Forms (LAR Version) | Consent documents with dedicated signature lines for the LAR, ensuring regulatory compliance and proper documentation [2]. |
| Supported Decision-Making Aids | Tools (e.g., simplified documents, pictorial aids, video explanations) to enhance participant understanding and involvement in the consent process [104]. |
| Verbal Consent Scripts | REB-reviewed scripts for obtaining and documenting consent verbally from an LAR, crucial for remote or low-literacy contexts [14]. |
| Documentation Template (for Capacity Assessment) | Standardized "Note to File" templates to consistently record observations and outcomes of decision-making capacity assessments. |
Experimental Protocols
Protocol: Assessing and Implementing LAR Consent in Clinical Research
Aim: To establish a standardized methodology for obtaining valid, well-documented informed consent from a Legally Authorized Representative (LAR) for an adult with impaired decision-making capacity in a clinical trial.
Background: In clinical research, an LAR is an individual who provides consent on behalf of an adult who lacks the mental capacity to make decisions for themselves [2]. This protocol is designed for studies regulated by health authorities like the FDA or Health Canada.
Methodology:
- Step 1: Determination of Need. The research team must first determine that the potential participant lacks capacity to provide independent informed consent. This assessment should be conducted by a qualified professional (e.g., physician, clinical psychologist) using a validated capacity assessment tool appropriate for the research context. The outcome and justification must be documented.
- Step 2: LAR Identification and Eligibility. Identify the individual authorized to act as the LAR, as defined by state or provincial law. This is typically a court-appointed guardian, a healthcare proxy, or a family member in a specified order of succession. Verify their identity and authority.
- Step 3: The Consent Discussion. The investigator or designated qualified individual must conduct the consent discussion with the LAR. The process must include:
- A complete presentation of the IRB-approved informed consent document.
- An explanation of the study's purpose, duration, procedures, and foreseeable risks/discomforts.
- A description of any benefits to the participant or others.
- Disclosure of appropriate alternative procedures.
- A statement regarding confidentiality and the possibility of regulatory review of records.
- For research involving more than minimal risk, an explanation of compensation and medical treatments available for injury [28] [2].
- Step 4: Documentation. The LAR must sign and date the current IRB-approved consent form. The person obtaining consent must also sign the form. The participant's medical record and the study documentation must clearly note that consent was provided by an LAR, with the LAR's name and relationship documented [2].
- Step 5: Ongoing Communication. Throughout the study, the research team must provide the LAR and the participant (to the extent they are able) with significant new findings and reaffirm continued participation.
Protocol: Implementing Supported Decision-Making in Behavioral Research
Aim: To employ a supported decision-making framework for the responsible inclusion of adults with intellectual disability in minimal-risk social-behavioral research, aligning with disability rights principles.
Background: For social-behavioral research, which is often minimal risk, emphasis is on enhancing comprehension and providing decision-making supports rather than surrogate consent [104]. This approach presumes competence and focuses on facilitating the individual's own decision.
Methodology:
- Step 1: Presumption of Capacity and Assessment. Begin with the presumption that the individual can consent with appropriate supports. Engage in a dialogue to assess their understanding of the research and tailor support needs dynamically, rather than via a single pass/fail test [104].
- Step 2: Environmental and Communicative Support. Implement reasonable modifications to facilitate understanding. This includes:
- Simplified Consent Materials: Using easy-to-read language, large print, or pictorial aids.
- Iterative Explanation: Breaking down information into small chunks and using teach-back methods to check understanding.
- Support Person: Allowing a trusted person of the participant's choice to be present to assist with understanding and expressing decisions [104].
- Step 3: Expression of Decision. Provide multiple means for the individual to express their consent or assent. This could be verbal agreement, a gesture, or another non-written form of communication. If the individual demonstrates understanding and provides voluntary agreement, they provide consent directly [104].
- Step 4: Documentation of Process. Document the process of supported decision-making, including the supports provided and how the participant expressed their decision. This is often more flexible than a signed form and may involve a consent log, detailed notes, or an audio recording of the consent conversation [14] [104].
- Step 5: Ongoing Consent (Process Consent). Treat consent as an ongoing process, not a one-time event. Regularly check in with the participant throughout the research to ensure they continue to understand and agree to participate [104].
Workflow Visualization
LAR Consent Implementation Workflow
Consent Framework Comparison
Utilizing IRB Feedback and Mock Audits for Continuous Process Improvement
Within clinical research, the process of obtaining informed consent from a Legally Authorized Representative (LAR) for vulnerable subjects presents unique challenges. Ensuring this process is consistently executed with the highest ethical and regulatory rigor is paramount. This document details how to systematically leverage Institutional Review Board (IRB) feedback and mock audits not merely as compliance checkpoints, but as powerful drivers for continuous process improvement. This approach transforms regulatory oversight from a reactive exercise into a proactive strategy for enhancing subject protection, data integrity, and operational efficiency within the specific context of LAR consent process research.
The Foundation: IRB Feedback as a Critical Input
The IRB's primary role is to protect the rights and welfare of human subjects [28]. Their feedback on LAR consent processes is a rich, expert source of data for identifying improvement opportunities.
Categorizing and Analyzing IRB Feedback
Systematic analysis of IRB feedback is the first step toward meaningful improvement. Feedback should be logged and categorized to identify trends and root causes.
Table: Categorization and Analysis of IRB Feedback on LAR Consent Processes
| Feedback Category | Description & Examples | Common Root Causes | Potential Improvement Initiatives |
|---|---|---|---|
| Regulatory & Ethical Deficiencies | Issues pertaining to federal regulations (21 CFR 50, 45 CFR 46) and ethical standards. • Example: Inadequate description of procedures involving greater than minimal risk. • Example: Missing elements per 21 CFR 50.25(a), such as confidentiality statements. | • Unclear protocol or investigator's brochure. • Use of outdated consent form templates. • Insufficient training on regulatory requirements for LAR scenarios. | • Develop and validate LAR-specific consent form templates. • Implement enhanced, scenario-based staff training on LAR regulations. |
| Process & Workflow Inefficiencies | Feedback highlighting cumbersome, unclear, or inconsistent consent processes. • Example: Confusing sequence for assessing LAR authority and understanding. • Example: Inconsistent documentation of the LAR's decision-making process. | • Lack of standardized operating procedures (SOPs). • Complex, multi-page consent forms. • Inadequate tools or checklists for coordinators. | • Streamline and map the LAR consent workflow. • Create a LAR consent process checklist. • Utilize ancillary documents for site-specific details [105]. |
| Participant/LAR Comprehension | Concerns regarding the readability, clarity, and overall understandability of the consent form and process. • Example: Use of highly technical scientific jargon. • Example: Reading level exceeding the 8th grade, making it difficult for LARs to understand. | • Consent forms not written for a lay audience. • Lack of plain language summaries or visual aids. • No formal assessment of LAR understanding. | • Incorporate plain language principles and readability testing. • Develop "teach-back" method protocols to verify LAR understanding. |
Protocol for Implementing a Systematic IRB Feedback Loop
A structured protocol ensures IRB feedback is consistently captured, analyzed, and acted upon.
- Capture and Log: Designate a quality or compliance lead to maintain a centralized log of all IRB correspondence, stipulations, and required modifications related to the LAR consent process. This can be managed within a specialized eReg/eISF system [106].
- Categorize: Upon receipt, classify each piece of feedback into the categories listed in the table above (e.g., Regulatory, Process, Comprehension).
- Root Cause Analysis: For recurring or critical issues, conduct a formal root cause analysis. The "5 Whys" technique is highly effective [107] [108]. For example:
- Problem: The IRB notes the wrong version of the LAR consent form was used.
- Why? The site staff printed forms before final IRB approval was received.
- Why? There is no clear system for alerting staff to final approved documents.
- Why? Document distribution relies on manual email and lacks version control.
- Why? There is no centralized, electronic document management system.
- Root Cause: Reliance on inefficient, error-prone manual processes for version control.
- Develop Corrective and Preventive Actions (CAPA): Based on the root cause, develop a targeted CAPA. In the example above, the CAPA might involve implementing an eReg system with automatic version control and access permissions [109] [106].
- Close the Loop: Communicate the implemented changes back to the study team and, if appropriate, to the IRB, demonstrating a responsive and robust quality system.
The Validation Engine: Conducting Mock Audits
Mock audits are simulated regulatory inspections that serve as a proactive tool to identify gaps before a real FDA inspection or sponsor audit [110] [106]. For LAR consent processes, they are indispensable.
Key Areas of Focus for LAR Consent Mock Audits
Mock audits should evaluate the entire LAR consent lifecycle against a predefined checklist.
Table: Mock Audit Checklist for LAR Informed Consent Processes
| Audit Area | Key Questions for Mock Auditors | Documentation/Evidence to Review |
|---|---|---|
| LAR Determination & Qualification | • Is the process for identifying and verifying a LAR's legal authority clearly defined and documented?• How is the LAR's relationship to the subject and legal capacity (e.g., court appointment) verified and recorded? | • Source documents (medical records, court documents).• Delegation of Authority Log entries.• Site SOPs for LAR determination. |
| Consent Process Execution | • Was the consent discussion conducted in a language and manner understandable to the LAR?• Was adequate time provided for the LAR to ask questions?• Were all key study elements (risks, benefits, alternatives) discussed as per the IRB-approved form? | • Signed and dated ICF (correct version).• Notes-to-file documenting the consent process.• Study coordinator training records. |
| Documentation & Version Control | • Does the signed ICF use the IRB-approved version and include all required signatures and dates?• Is there a system to prevent the use of obsolete consent forms?• How are re-consents (e.g., for new protocol information) handled and documented? | • IRB approval letters for all ICF versions.• eReg/eISF system audit trails [106].• Documentation of any re-consent processes. |
| Staff Training & Delegation | • Are all staff members involved in the LAR consent process appropriately trained and listed on the delegation log?• Is training specific to the complexities of LAR consent? | • Delegation of Authority Log.• Curriculum and attendance records for LAR consent training. |
Experimental Protocol for a Mock Audit
A detailed, repeatable protocol ensures mock audits are consistent and effective.
Planning (Plan):
- Define Scope & Team: Appoint an independent, qualified auditor or team. Define the scope (e.g., LAR consent processes for a specific study or across all studies).
- Develop Agenda & Tools: Create an audit agenda and assemble the checklist (as above). Prepare request forms for documents and interviews.
- Schedule & Notify: Inform the site staff of the audit dates to ensure availability, but maintain the element of surprise regarding specific details to be examined.
Execution (Do):
- Opening Meeting: Brief the site team on the audit's purpose and process.
- Document Review: Systematically review regulatory binders (physical or electronic), delegation logs, training records, and a sample of subject records involving LAR consent.
- Staff Interviews: Interview key personnel (Principal Investigator, study coordinators) to assess their understanding of the LAR consent process and protocol requirements. Train staff to answer questions clearly and concisely [106].
- Facility & Process Observation: Observe the environment where consent discussions typically occur and, if possible, simulate the process.
Analysis & Reporting (Check):
- Debriefing: Hold a closing meeting to present preliminary findings.
- Formal Report: Issue a formal mock audit report that clearly differentiates between observations (potential weaknesses), deficiencies (deviations from protocol/GCP), and findings (major issues impacting subject safety/data integrity). The report should link deficiencies to process failures [109].
Corrective Action & Follow-up (Act):
- CAPA Development: The site team develops a CAPA plan addressing each finding. The plan should focus on process-level solutions, not just one-time fixes [109].
- Implementation & Verification: Implement the CAPA and schedule a follow-up audit to verify the effectiveness of the corrective actions.
Integrating Data for Continuous Improvement
The true power of this approach is realized when data from IRB feedback and mock audits are integrated into a unified continuous improvement model.
The Continuous Improvement Cycle for LAR Consent
The following workflow visualizes how IRB feedback and mock audits feed into a perpetual improvement cycle, grounded in the Plan-Do-Check-Act (PDCA) model [108] [111].
Quantitative Tracking and Measurement
To close the loop and demonstrate improvement, sites must track key performance indicators (KPIs). The table below outlines essential metrics for the LAR consent process.
Table: Key Performance Indicators for LAR Consent Process Improvement
| Metric Category | Specific Metric | Data Collection Method | Target / Benchmark |
|---|---|---|---|
| Process Efficiency | • Mean time from subject identification to completed LAR consent.• Rate of protocol deviations related to the consent process. | • Electronic clinical trial management system (CTMS).• Deviation tracking log. | • Reduce mean time by 15% per quarter.• Zero critical deviations. |
| Quality & Compliance | • Percentage of consent forms with zero documentation errors (version, signatures, dates).• Number of IRB stipulations per protocol related to consent. | • Internal quality control checks.• IRB communication log. | • >95% error-free forms.• Reduce stipulations by 50% year-over-year. |
| LAR & Staff Experience | • LAR comprehension scores (via post-consent questionnaire).• Staff confidence scores in administering LAR consent (via survey). | • Short, validated understanding assessment.• Anonymous staff surveys. | • >90% comprehension score.• >4.0/5.0 confidence score. |
Successful implementation of this framework requires specific tools and resources.
Table: Research Reagent Solutions for Process Improvement
| Tool / Resource | Function / Purpose | Application in LAR Consent Research |
|---|---|---|
| Electronic Regulatory Binder (eReg/eISF) | A centralized, secure digital repository for all regulatory documents [106]. | Ensures version control of ICFs, provides audit trails, and streamlines document retrieval for audits and IRB submissions. |
| eSource Systems | Captures clinical data directly at the point of care, eliminating transcription from paper sources [106]. | Reduces errors in documenting the consent process and timestamps key actions, enhancing data integrity for LAR consent events. |
| Business Process Management (BPM) Software | Platforms for designing, mapping, and analyzing workflows [107] [112]. | Used to visually map the "as-is" LAR consent process, identify bottlenecks, and model the "to-be" improved process. |
| Root Cause Analysis Templates (5 Whys, Fishbone) | Structured templates to guide the investigation of the underlying causes of problems [107]. | Provides a consistent methodology for analyzing IRB feedback and mock audit findings to ensure CAPA addresses the true root cause. |
| Performance Dashboards & Analytics | Tools for visualizing KPIs and tracking trends over time [113] [112]. | Allows research administrators to monitor the metrics defined in Section 4.2, providing data-driven evidence of improvement. |
Integrating IRB feedback and mock audits into a continuous improvement cycle, as outlined in this protocol, transforms regulatory compliance from a static goal into a dynamic, value-added activity. By systematically collecting data, analyzing root causes, implementing targeted corrections, and measuring outcomes, research organizations can significantly enhance the ethical rigor, quality, and reliability of the legally authorized representative informed consent process. This proactive, process-oriented approach not only ensures inspection readiness but, more importantly, fosters a culture of quality that prioritizes and protects the most vulnerable research subjects and their representatives.
Conclusion
The process of obtaining informed consent from a legally authorized representative is a critical safeguard for both vulnerable research participants and the integrity of clinical research. A robust LAR consent process, built on a solid ethical foundation, executed with methodological precision, and continuously validated for comprehension and compliance, is non-negotiable. The evolving regulatory landscape, including the 2025 FDAAA 801 mandate for public consent form posting, underscores a permanent shift towards greater transparency and participant-centricity. Future success in biomedical research will depend on the industry's ability to adapt to these changes, leveraging digital tools and health literacy principles to build trust, ensure ethical rigor, and accelerate the development of new therapies for all populations.
References
- 1. Surrogate Consent /Use of a Legally Authorized ... [https://hrpp.research.virginia.edu/teams/irb-hsr/researcher-guide-irb-hsr/surrogate-consent-use-legally-authorized-representative-lar]
- 2. What Is the Role of a Legally Authorized Representative in ... [https://www.wcgclinical.com/insights/what-is-the-role-of-a-legally-authorized-representative-in-informed-consent/]
- 3. Healthcare Proxies: Appointing People with the Power to ... [https://www.albanylaw.edu/government-law-center/healthcare-proxies-appointing-people-the-power-make-healthcare-decisions]
- 4. How to obtain informed consent for research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5980471/]
- 5. Nuremberg Code | History, Date, & 10 Points [https://www.britannica.com/topic/Nuremberg-Code]
- 6. The Nuremberg Code–A critique - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3121268/]
- 7. The Common Rule - IRB - UC Davis [https://irb.ucdavis.edu/project-guidance/federal-funding/]
- 8. Key Information and Facilitating Understanding in ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/key-information-and-facilitating-understanding-informed-consent-guidance-sponsors-investigators-and]
- 9. Core elements of consent documentation for clinical research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12448764/]
- 10. Informed Consent - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK430827/]
- 11. The Requirements for Informed Consent (Series #1) [https://www.tc.columbia.edu/institutional-review-board/irb-blog/2025/informed-consent-the-requirements-for-informed-consent-series-1/]
- 12. Research Ethics and Informed Consent [https://researchbasics.education.uconn.edu/ethics-and-informed-consent/]
- 13. Informed consent guidance and templates for psychologists [https://www.apaservices.org/practice/business/management/informed-consent]
- 14. Verbal consent in biomedical research: moving toward a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11906376/]
- 15. An evaluation of the process of informed consent - Trials [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-021-05493-1]
- 16. Factors Influencing Informed Consent Preferences in ... [https://www.jmir.org/2025/1/e63349/]
- 17. 2025 Guidelines | State of California - Department of Justice [https://oag.ca.gov/research/guide]
- 18. Vulnerable populations | Research Starters [https://www.ebsco.com/research-starters/political-science/vulnerable-populations]
- 19. Vulnerable Populations: Who Are They? [https://www.ajmc.com/view/nov06-2390ps348-s352]
- 20. VULNERABLE POPULATIONS - Nursing - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK616981/]
- 21. Use of Legally Authorized Representatives | Research | WashU [https://research.washu.edu/legally-authorized-representatives/]
- 22. Informed Consent: The Elements of ... [https://www.tc.columbia.edu/institutional-review-board/irb-blog/2025/informed-consent-the-elements-of-informed-consent-documents-series-2/]
- 23. Competency and Capacity - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK532862/]
- 24. Capacity (Competence) and Incapacity - Special Subjects - Merck Manual Professional Edition [https://www.merckmanuals.com/professional/special-subjects/medicolegal-issues/capacity-competence-and-incapacity]
- 25. Mental capacity, legal competence and consent to treatment - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1079581/]
- 26. 知情同意临床实践的伦理隐忧及其消解 [https://yizhe.dmu.edu.cn/article/doi/10.12014/j.issn.1002-0772.2024.20.03?viewType=HTML]
- 27. Informed consent: Guidance - IU Research - Indiana University [https://research.iu.edu/compliance/human-subjects/guidance/informed-consent.html]
- 28. Institutional Review Boards Frequently Asked Questions [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/institutional-review-boards-frequently-asked-questions]
- 29. Informed Consent in Aesthetic Surgery: Best Practices [https://www.prospyrmed.com/blog/post/informed-consent-in-aesthetic-surgery-best-practices]
- 30. Clinical Documentation Best Practices: Ensuring Accuracy ... [https://www.indwes.edu/articles/2025/10/clinical-documentation-best-practices-ensuring-accuracy-compliance]
- 31. 2025 Medical Record Review: Best Practices for Attorneys ... [https://superinsight.ai/blog/medical-record-review-best-practices-2025.html]
- 32. What You Should Know About FDA Final Informed Consent ... [https://www.wcgclinical.com/insights/what-you-should-know-about-fda-final-informed-consent-guidance/]
- 33. HIPAA-Compliant Patient Consent Forms: What You Need ... [https://scribejoy.com/guides/hipaa-compliant-patient-consent-forms-what-you-need-to-know/?srsltid=AfmBOopwdrDFnM7W95bmGvxeBuyQpeUI8kBEDEqR7cVOlM0oFE7pK8EC]
- 34. SPIRIT 2025 statement: Updated guideline for protocols of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037212/]
- 35. Interviews - Human Research Protection Program (HRPP) [https://hrpp.research.virginia.edu/teams/irb-sbs/researcher-guide-irb-sbs/interviews]
- 36. – Intuit Content Design Readability [https://contentdesign.intuit.com/accessibility-and-inclusion/readability/]
- 37. Writing level and plain | RSNA language [https://www.rsna.org/style-guide/writing-level-and-plain-language]
- 38. Flesch Reading Ease and the Flesch Kincaid Grade Level – Readable [https://readable.com/readability/flesch-reading-ease-flesch-kincaid-grade-level/]
- 39. Instructions and examples for writing clear, accessible content... [https://gist.github.com/mpaiva-cc/7efb75232c291098170fc45c365a8e3a]
- 40. Health Literacy and Informed Consent Materials [https://pmc.ncbi.nlm.nih.gov/articles/PMC6155979/]
- 41. Consent Guide - Health Literacy in Clinical Research [https://mrctcenter.org/health-literacy/tools/overview/consent-guide/]
- 42. Analysing quantitative data for evaluation [https://www.ncvo.org.uk/help-and-guidance/strategy-and-impact/impact-evaluation/evaluation-and-impact-reporting/how-to-analyse-quantitative-data-for-evaluation/]
- 43. Informed Consent Guidance [https://www.hopkinsmedicine.org/institutional-review-board/guidelines-policies/guidelines/informed-consent-i]
- 44. Informed Consent Process: Foundation of the Researcher ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5527718/]
- 45. Learn More: Informed Consent Process [https://clinicalresearch.unc.edu/playbooks/my-study-lifecycle/study-start-up/institutional-review-board-irb-approval/informed-consent-process/]
- 46. Informed Consent - Penn IRB - University of Pennsylvania [https://irb.upenn.edu/homepage/biomedical-homepage/guidance/recruitment-and-consent/informed-consent/]
- 47. Informed Consent Development | Penn Medicine Clinical ... [https://www.med.upenn.edu/clinicalresearch/informed-consent-development.html]
- 48. IRB Protocol and Consent Form Resources | Columbia [https://research.columbia.edu/irb-protocol-and-consent-form-resources]
- 49. Ongoing Consent & Re-Consent - One UNC Clinical Research [https://clinicalresearch.unc.edu/playbooks/my-study-lifecycle/study-conduct/ongoing-consent-and-re-consent/]
- 50. Informed Consent for CRCs – Best Practices, Tools, and ... [https://ccrps.org/clinical-research-blog/informed-consent-essentials-crcs-guide-to-best-practices]
- 51. Strategies for Meaningful, Effective and Compliant Medical ... [https://lifesciences.enago.com/blogs/strategies-for-meaningful-effective-and-compliant-medical-communication-in-2025]
- 52. New Federal Regulations for Medical Interpreters in 2025 [https://www.linkedin.com/posts/reviverglobal_medicalinterpreting-360smartlingo-hipaa2025-activity-7371875229825925121-hEfh]
- 53. Effectiveness of interpreters and other strategies for ... [https://www.sciencedirect.com/science/article/pii/S073839912500134X]
- 54. Worldwide willingness to share health data high but privacy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12375002/]
- 55. March 2025 - Center for Informed Consent Integrity [https://ge2p2global-centerforinformedconsentintegrity.org/2025/03/]
- 56. Semi-professional language mediators in patient-provider ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12063309/]
- 57. Understanding the Role of Language Services in Clinical ... [https://globalinterpreting.com/blog/understanding-the-role-of-language-services-in-clinical-trials/]
- 58. What is Medical Interpreter? Impressive 2025 [https://globalarena.com/what-is-a-medical-interpreter/]
- 59. Improving Consent Processes for Clinical Research Using ... [https://www.pcori.org/research-results/2019/improving-consent-processes-clinical-research-using-public-deliberation-methods]
- 60. Health Literacy | National Institutes of Health (NIH) [https://www.nih.gov/institutes-nih/nih-office-director/office-communications-public-liaison/clear-communication/health-literacy]
- 61. The teach-back method: Communicating more effectively ... [https://webmdignite.com/blog/teach-back-method-communicating-more-effectively-patients-improve-health-outcomes]
- 62. Development and evaluation of pharmacist-provided teach ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10124684/]
- 63. Attitudes of psychiatric staff toward coercion [https://pmc.ncbi.nlm.nih.gov/articles/PMC12451713/]
- 64. Digitalizing informed consent in healthcare: a scoping review [https://pmc.ncbi.nlm.nih.gov/articles/PMC12225439/]
- 65. Before Involuntary Commitment: Coercion in the Shadows [https://www.madinamerica.com/2025/07/hidden-coercion-how-pressure-mounts-before-psychiatric-admission/]
- 66. 11 Effective Conflict Resolution Techniques in Healthcare [https://futuramo.com/blog/11-effective-conflict-resolution-techniques-in-healthcare-settings/]
- 67. Strategies for Resolving Conflict to Enhance Patient Care ... [https://www.capphysicians.com/articles/strategies-resolving-conflict-enhance-patient-care-and-fostering-positive-work-environment]
- 68. Conflict Management in Nursing: Analyzing Styles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11676306/]
- 69. Waiver of informed consent in clinical research [https://pmc.ncbi.nlm.nih.gov/articles/PMC11927427/]
- 70. FDA Final Rule - Waiver or Alteration of Informed Consent ... [https://thehrpconsultinggroup.com/fda-final-rule-waiver-or-alteration-of-informed-consent-for-minimal-risk-clinical-investigations/]
- 71. Waiver of Consent vs Waiver of Written Consent - Castor EDC [https://www.castoredc.com/blog/waiver-of-consent-vs-waiver-of-written-consent/]
- 72. Properties of adaptive, cluster-randomised controlled trials ... [https://implementationscience.biomedcentral.com/articles/10.1186/s13012-025-01443-6]
- 73. protocol for an extension to cluster randomized trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC11866560/]
- 74. A scoping review identified additional considerations for ... [https://pubmed.ncbi.nlm.nih.gov/41077325/]
- 75. Review of the quality of reporting of statistical analysis ... [https://www.sciencedirect.com/science/article/pii/S0895435625000599]
- 76. Incorporating Contact Network Structure in Cluster ... [https://www.nature.com/articles/srep17581]
- 77. Implementation Mapping to Identify Best Practices for ... [https://www.researchprotocols.org/2025/1/e73718]
- 78. Use and Effectiveness of the Teach-Back Method in Patient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6590951/]
- 79. How To Improve Your Patients' Understanding Of Their Care [https://www.louisianahealthconnect.com/newsroom/teach-back--how-to-improve-your-patients-understanding-of-their-.html]
- 80. Strategies for Creating Authentic Quizzes and Assessments [https://www.guroolearning.com/blog/strategies-for-creating-authentic-quizzes-and-assessments]
- 81. Development of Interactive Media to Improve Early ... [https://eudl.eu/doi/10.4108/eai.31-8-2021.2313809]
- 82. Tool: Teach-Back | Agency for Healthcare Research and ... [https://www.ahrq.gov/teamstepps-program/curriculum/communication/tools/teachback.html]
- 83. Five Methods to Validate Customer Feedback for Quality ... [https://syncly.app/blog/validate-customer-feedback]
- 84. Consent Monitoring [https://ohrpp.research.ucla.edu/consent-monitoring/]
- 85. 2025 FDAAA 801 Final Rule Changes Impacting Clinical ... [https://prorelixresearch.com/2025-fdaaa-801-clinical-trial-rule-impact/]
- 86. Compliance Program Performance Metrics [https://www.onetrust.com/blog/compliance-program-performance-metrics/]
- 87. Top 10 KPIs for Modern Audit Teams - Empowered Systems [https://empoweredsystems.com/blog/top-10-kpis-for-modern-audit-teams/]
- 88. The Future of Auditing: What to Look for in 2025 [https://hyperproof.io/resource/the-future-of-auditing-2025/]
- 89. KPI Audit Checklist: Top Metrics to Track [https://auditboard.com/blog/top-metrics-to-track-in-your-audits-checklist]
- 90. FDA Draft Guidance on Multiregional Clinical Development ... [https://www.wcgclinical.com/insights/fda-draft-guidance-on-multiregional-clinical-development-programs-for-oncology/]
- 91. ICH E6(R3) Explained: A Guide to the 2025 GCP Update [https://intuitionlabs.ai/articles/ich-e6-r3-gcp-guidelines-2025]
- 92. The Impact of ICH E6(R3) on U.S. and Canadian IRBs [https://www.advarra.com/blog/the-impact-of-ich-e6r3-on-u-s-and-canadian-irbs/]
- 93. Regulatory Updates, September 2025 [https://www.caidya.com/resources/regulatory-updates-sept-2025/]
- 94. Application of Good Clinical Practice at UW-Madison - Research [https://research.wisc.edu/application-of-good-clinical-practice-at-uw-madison/]
- 95. Clinical Trials Guidance Documents [https://www.fda.gov/science-research/clinical-trials-and-human-subject-protection/clinical-trials-guidance-documents]
- 96. 21 CFR 50.25 -- Elements of informed consent. [https://www.ecfr.gov/current/title-21/chapter-I/subchapter-A/part-50/subpart-B/section-50.25]
- 97. Clinical trials in human medicines [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/clinical-trials-human-medicines]
- 98. Posting of Consent Forms for Federally-Funded Clinical ... [https://www.hopkinsmedicine.org/institutional-review-board/guidelines-policies/guidelines/posting-cf-federally-funded-clinical-trials]
- 99. Clinical Trials Registration and Informed Consent Posting ... [https://research.washu.edu/clinical-trials-registration-guideline/]
- 100. Navigating FDA Clinical Trial Regulations - FDAMap [https://www.fdamap.com/valuable-insights/navigating-fda-regulations-on-clinical-trials-insights-from-a-seasoned-expert.html]
- 101. Compliance with Results Reporting at ClinicalTrials.gov ... [https://publichealth.realclearjournals.org/research-articles/2025/01/compliance-with-results-reporting-at-clinicaltrials-gov-before-and-after-the-2017-fdaaa-final-rule-a-comparative-analysis/]
- 102. Notices of Noncompliance and Civil Money Penalty Actions [https://www.fda.gov/science-research/fdas-role-clinicaltrialsgov-information/clinicaltrialsgov-notices-noncompliance-and-civil-money-penalty-actions]
- 103. Clinicaltrials.gov: Recent Action May Signal Increased ... [https://www.morganlewis.com/blogs/asprescribed/2025/01/clinicaltrialsgov-recent-action-may-signal-increased-attention-from-fda-on-trial-data-reporting-compliance]
- 104. Responsible inclusion: A systematic review of consent to ... [https://www.sciencedirect.com/science/article/abs/pii/S1936657424001080]
- 105. Ways to Streamline Informed Consent Process in Clinical ... [https://www.advarra.com/blog/ways-to-streamline-informed-consent-process-in-clinical-trial-startup/]
- 106. How to Prepare for an FDA Audit: A Comprehensive Guide ... [https://realtime-eclinical.com/2025/06/18/preparing-for-an-fda-audit-a-comprehensive-guide-for-clinical-research-sites/]
- 107. 7 Types of Process Improvement Methodologies [2025] [https://asana.com/resources/process-improvement-methodologies]
- 108. The continuous improvement process: key steps, ... [https://www.atlassian.com/agile/project-management/continuous-improvement]
- 109. Clinical Investigator Site Audits: A Guide and Checklist ... [https://www.thefdagroup.com/blog/clinical-trial-investigator-site-audits]
- 110. Clinical Trial Compliance: Preparing for FDA Inspection ... [https://www.srainternational.org/blogs/srai-news/2025/10/09/clinical-trial-compliance-fda-inspection-readiness]
- 111. Continuous Improvement Model [https://asq.org/quality-resources/continuous-improvement?srsltid=AfmBOoqz2MxXUJGNMS-tb4dkPlpfmWQr3iFSd4Wb844E0zuEQSO1qEOX]
- 112. Continuous Process Improvement (CPI): A Guide for ... [https://www.6sigma.us/process-improvement/continuous-process-improvement-cpi/]
- 113. The 9 Principles of Continuous Process Improvement [https://www.blueprintsys.com/blog/the-9-principles-of-continuous-process-improvement]