Lab Data Ethics: A Complete Guide to Responsible Management for Research Integrity
This comprehensive guide establishes essential ethical frameworks for managing laboratory data.
Lab Data Ethics: A Complete Guide to Responsible Management for Research Integrity
Abstract
This comprehensive guide establishes essential ethical frameworks for managing laboratory data. Tailored for researchers, scientists, and drug development professionals, it explores foundational principles like data integrity and FAIR principles, provides actionable methodologies for implementation, addresses common challenges in complex environments like AI integration, and offers validation strategies against global standards like ALCOA+. The goal is to ensure scientific reproducibility, compliance, and public trust in biomedical and clinical research.
Why Data Ethics Matter: Building Trust and Integrity in Scientific Research
Within the context of a broader thesis on ethical guidelines for data management in laboratory settings, this guide establishes a technical foundation. Modern research, particularly in drug development, generates complex, high-volume data. Ethical management transcends mere regulatory compliance; it is a core component of scientific integrity, ensuring data quality, reproducibility, and public trust. This document outlines core principles, provides implementable protocols, and defines the toolkit necessary for ethical data stewardship.
Core Ethical Principles for Laboratory Data Management
The following principles form the pillars of an ethical data management framework, addressing the entire data lifecycle from conception to archival.
| Principle | Technical & Operational Definition | Key Risk if Neglected |
|---|---|---|
| Integrity & Accuracy | Implementing systematic procedures for data capture, transformation, and analysis to prevent errors or loss. Includes version control, audit trails, and anti-tampering measures. | Irreproducible results, scientific retractions, flawed clinical decisions. |
| Security & Confidentiality | Applying technical controls (encryption, access controls) and administrative policies to protect sensitive data (e.g., PHI, proprietary compound structures) from unauthorized access or breach. | Data breaches, loss of intellectual property, violation of subject privacy (GDPR/HIPAA). |
| Stewardship & Provenance | Maintaining a complete, immutable record of data lineage: origin, custodians, processing steps, and transformations. Essential for auditability and reuse. | Inability to trace errors, compromised data utility for secondary research. |
| Transparency & Disclosure | Clear documentation of methodologies, algorithms, and any data manipulation. Full reporting of all results, including negative or contradictory data. | Publication bias, "cherry-picking" of results, hidden conflicts of interest. |
| Fairness & Non-Exploitation | Ensuring data collection and use does not unfairly target or disadvantage groups. Obtaining proper informed consent for human-derived data and respecting data sovereignty. | Ethical violations in human subjects research, biased AI/ML models, community harm. |
Quantitative Landscape: Data Volume and Compliance Incidents
A live search for current statistics reveals the scale and risks associated with laboratory data management.
Table 1: Recent Data on Research Data Volume and Security Incidents
| Metric | Estimated Figure (2023-2024) | Source / Context |
|---|---|---|
| Global Volume of Health & Biotech Data | ~2,314 Exabytes (EB) | Projection from industry reports on genomic, imaging, and clinical trial data. |
| Average Cost of a Healthcare Data Breach | $10.93 Million USD | IBM Cost of a Data Breach Report 2023, highest of any sector for 13th year. |
| Percentage of Labs Citing Data Management as a Major Challenge | >65% | Survey of biopharma R&D teams on digital transformation hurdles. |
| FDA Warning Letters Citing Data Integrity Issues (FY2023) | ~28% of all GxP letters | Analysis of FDA enforcement reports, highlighting persistent ALCOA+ failures. |
Experimental Protocol: Implementing a Data Integrity Audit
This detailed protocol provides a methodology for proactively assessing data integrity within a laboratory information management system (LIMS) or electronic lab notebook (ELN).
Title: Internal Audit for Data Integrity Compliance (ALCOA+ Framework) Objective: To verify that data generated within a specified experiment or process is Attributable, Legible, Contemporaneous, Original, Accurate, Complete, Consistent, Enduring, and Available (ALCOA+). Materials: See "Scientist's Toolkit" below. Procedure:
- Pre-Audit Planning:
- Define the scope (e.g., specific assay data from Q4).
- Assemble an audit team with relevant technical and process knowledge.
- Notify the data custodians of the audit window.
- Data Sampling:
- Use a risk-based approach to select a statistically relevant sample of final results.
- Trace each final result backward through all processing steps to its raw data source.
- Attributability & Contemporaneity Check:
- Verify every data entry and modification is linked to a unique user ID (no shared accounts).
- Confirm timestamps are logical and sequential, with no evidence of back-dating.
- Originality & Accuracy Check:
- Compare electronic records against any printed/hard copy annotations for discrepancies.
- Verify that data was recorded directly by the instrument or manually at the time of the activity.
- Check for evidence of unauthorized alterations or deletions.
- Completeness & Consistency Check:
- Ensure all protocol-defined data points are present.
- Confirm metadata (e.g., instrument calibration status, reagent lot numbers) is linked.
- Verify calculations and transformations are consistent and documented.
- Enduring & Available Check:
- Confirm data is backed up in a secure, unalterable format (e.g., WORM storage).
- Verify recovery procedures are in place and tested.
- Check that data retention policies comply with relevant regulations (e.g., 21 CFR Part 11, GDPR).
- Reporting:
- Document all findings, including non-conformances.
- Assign severity levels and root causes.
- Develop a corrective and preventive action plan (CAPA).
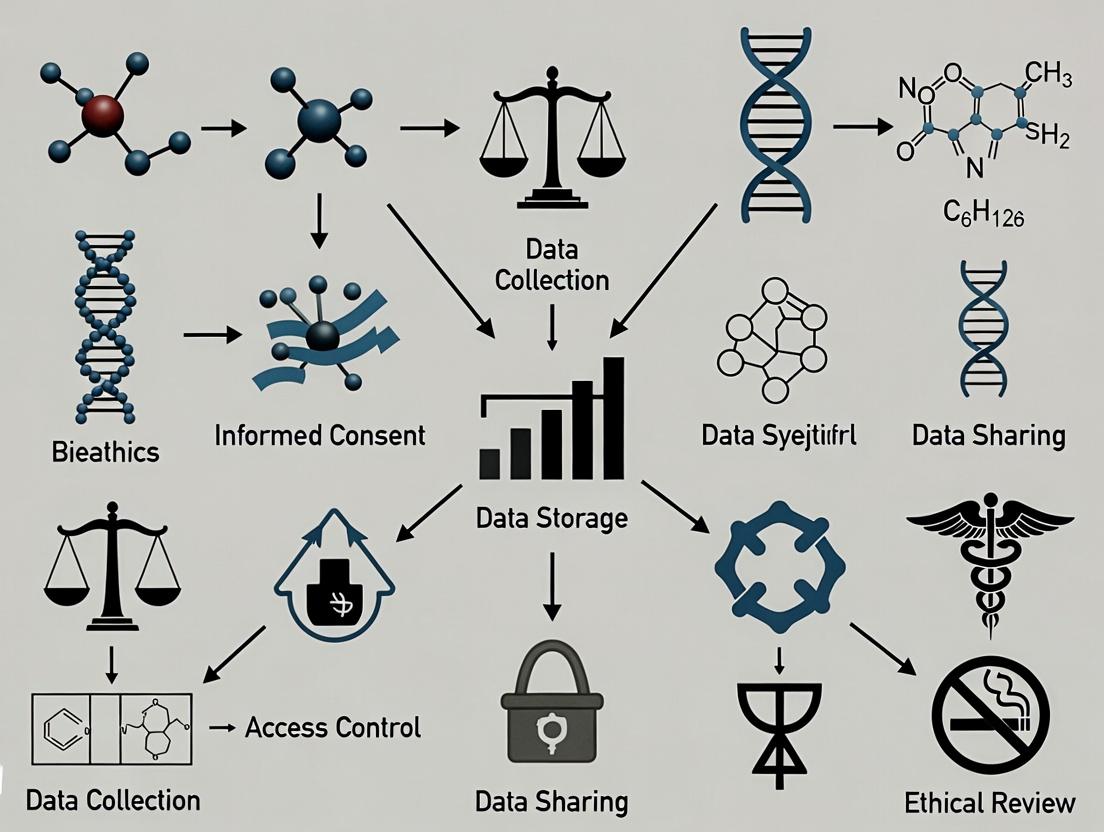
Diagram: Ethical Data Management Workflow
Title: Lifecycle of Ethically Managed Lab Data
The Scientist's Toolkit: Essential Reagents for Ethical Data Management
Table 2: Key Research Reagent Solutions for Data Integrity
| Item / Solution | Function in Ethical Data Management |
|---|---|
| Electronic Lab Notebook (ELN) | Primary system for recording experiments with user attribution, timestamps, and audit trails to ensure data originality and traceability. |
| Laboratory Information Management System (LIMS) | Tracks samples, associated data, and workflows, enforcing SOPs and maintaining complete data lineage (provenance). |
| 21 CFR Part 11 Compliant Software | Applications validated to meet FDA requirements for electronic records and signatures, ensuring legal acceptability. |
| Write-Once-Read-Many (WORM) Storage | Secures original data in an unalterable state, preserving integrity and meeting regulatory requirements for data endurance. |
| Data Encryption Tools (at-rest & in-transit) | Protects confidential data from unauthorized access, a core requirement for security and subject privacy. |
| Automated Data Backup & Recovery System | Ensures data availability and guards against loss due to system failure or catastrophe, a key stewardship duty. |
| Access Control & Identity Management | Manages user permissions based on role, enforcing the principle of least privilege and protecting data confidentiality. |
| Data Anonymization/Pseudonymization Tools | Enables the ethical reuse or sharing of human subject data by removing or masking personal identifiers. |
Defining and implementing these core principles is not a standalone IT exercise. Ethical data management must be integrated into the daily culture of the laboratory. It requires ongoing training, clear accountability, and leadership commitment. By adhering to these technical guidelines, researchers and drug development professionals uphold the highest standards of scientific integrity, accelerate discovery through reliable data, and fulfill their ethical obligation to research subjects, the scientific community, and society.
Within the broader thesis on ethical guidelines for data management in laboratory settings, this whitepaper examines the severe, tangible consequences of ethical lapses. For researchers, scientists, and drug development professionals, data integrity is not merely an abstract ideal but the bedrock of reproducible science, credible discovery, and sustained public trust. Failures in data ethics—spanning from poor record-keeping and p-hacking to outright fabrication—trigger a cascade of professional and institutional disasters, including manuscript retractions, loss of critical funding, and irreversible erosion of trust.
The following tables summarize recent, search-derived data on the consequences of poor data practices.
Table 1: Primary Causes of Research Article Retractions (2018-2023)
| Retraction Cause | Approximate Percentage | Key Characteristics |
|---|---|---|
| Data Fabrication/Falsification | 43% | Invented or manipulated results, image duplication/manipulation. |
| Plagiarism | 14% | Duplicate text without attribution, self-plagiarism. |
| Error (Non-malicious) | 12% | Honest mistakes in data, analysis, or reporting. |
| Ethical Issues (e.g., lack of IRB approval) | 10% | Patient/animal subject violations, consent problems. |
| Authorship Disputes/Fraud | 8% | Unauthorized inclusion, fake peer reviews. |
| Other/Unspecified | 13% | Miscellaneous issues including legal concerns. |
Table 2: Consequences of Data Ethics Violations: Case Studies
| Consequence Type | Example Incident (Post-2020) | Outcome |
|---|---|---|
| Funding Loss | A prominent Alzheimer's disease research lab at a major U.S. university. | Federal funding agencies (NIH) suspended and clawed back millions in grants following findings of image manipulation in key papers. |
| Retraction Cluster | A cardiology research group. | Over 100 papers retracted due to data integrity concerns, invalidating clinical trial conclusions. |
| Legal & Career | A pharmaceutical development scientist. | Criminal conviction for falsifying preclinical trial data, leading to imprisonment and permanent career termination. |
| Institutional Reputation | Multiple oncology research centers. | Loss of public and commercial partnership trust, requiring years and stringent oversight reforms to rebuild. |
Experimental Protocols: Methodologies for Ensuring Data Integrity
To mitigate these high-stakes risks, laboratories must implement rigorous, standardized protocols. The following are detailed methodologies for key experiments and processes cited in data ethics literature.
Protocol 1: Systematic Image Data Acquisition and Analysis (Microscopy)
- Objective: To prevent selective reporting and manipulation of image data.
- Materials: Confocal/fluorescence microscope, standardized cell lines, automated image capture software, raw data storage server.
- Procedure:
- Pre-Acquisition: Define all imaging parameters (exposure, gain, magnification) in the experimental plan. Use control samples to establish baseline settings.
- Blinded Acquisition: Where feasible, the technician acquiring images should be blinded to sample identity/group.
- Comprehensive Capture: Image entire wells/slides systematically using automated stage movement; avoid "cherry-picking" representative fields.
- Raw Data Preservation: Save all original, unprocessed image files (e.g., .lif, .nd2, .czi) immediately to a secure, immutable server with audit trails.
- Documented Processing: Any post-processing (background subtraction, thresholding) must be applied uniformly to all images within an experiment and detailed in the methods section.
Protocol 2: Principled Statistical Analysis and P-value Auditing
- Objective: To eliminate p-hacking and data dredging.
- Materials: Statistical software (R, Python, Prism), pre-registered analysis plan, version-controlled code repository.
- Procedure:
- Pre-registration: Before data collection, deposit the experimental hypothesis, design, sample size calculation, and planned statistical tests in a public repository (e.g., OSF, ClinicalTrials.gov).
- Data Lock: Once collection is complete, create a "locked" dataset version. All analyses must be performed on this version.
- Scripted Analysis: Perform all analyses using executable scripts, not GUI-based point-and-click software, to ensure an auditable trail.
- Audit Trail: Maintain code in a version control system (e.g., Git). All deviations from the pre-registered plan must be justified and documented in the manuscript.
Protocol 3: Robust Data Management and Electronic Lab Notebook (ELN) Use
- Objective: To ensure traceability, prevent loss, and facilitate replication.
- Materials: Institution-approved ELN platform, standardized naming conventions, FAIR (Findable, Accessible, Interoperable, Reusable) data repositories.
- Procedure:
- Daily Logging: Record all experimental procedures, observations, raw data file paths, and instrument outputs directly into the ELN on the day they are generated.
- Metadata Standardization: Adopt community-standard metadata schemas (e.g., MIAME for genomics, ARRIVE for animal research).
- Linking: Link entries to specific project identifiers, funding sources, and protocol versions.
- Regular Audits: Lab managers/PIs should conduct scheduled, random audits of ELN entries against physical lab books and raw data files.
- Public Archiving: Upon publication, deposit de-identified raw data and analysis code in a public repository like GEO, PRIDE, or Figshare.
Visualizing the Pathways to Consequence and Integrity
Diagram 1: Pathway from Data Ethics Failure to Systemic Consequences
Diagram 2: Data Integrity Workflow for Laboratory Research
The Scientist's Toolkit: Essential Research Reagent Solutions for Data Integrity
Table 3: Key Tools for Ethical Data Management
| Tool Category | Specific Item/Software | Function in Promoting Data Ethics |
|---|---|---|
| Electronic Lab Notebooks (ELN) | LabArchives, Benchling, RSpace | Provides timestamped, immutable records; links data files to protocols; enables easy audit and sharing. |
| Data Analysis & Statistics | R with knitr/rmarkdown, Jupyter Notebooks, SPSS | Scripted, reproducible analyses generate audit trails. Prevents post-hoc manipulation of analytical choices. |
| Image Acquisition & Analysis | MetaMorph, ImageJ/Fiji with macro recording, ZEN (Zeiss) | Automated image capture reduces bias. Macro recording ensures uniform processing. |
| Raw Data Storage | Institutional SAN/NAS with versioning, LabFolder Drive, OneDrive/Box (configured) | Secure, centralized, and backed-up storage for original instrument files, preventing loss or alteration. |
| Public Data Repositories | GEO (genomics), PRIDE (proteomics), Figshare (general), OSF (projects) | FAIR-compliant archiving fulfills funder mandates, enables replication, and builds public trust. |
| Pre-registration Platforms | Open Science Framework (OSF), ClinicalTrials.gov, AsPredicted | Time-stamps research plans, distinguishing confirmatory from exploratory work. |
| Reference & Collaboration | Zotero, Mendeley, Overleaf | Manages literature, ensures proper attribution, and prevents plagiarism in collaborative writing. |
In the domain of laboratory research and drug development, data is the fundamental currency. Its management directly impacts scientific validity, public trust, regulatory approval, and patient safety. This technical guide delineates four core ethical frameworks—Integrity, Transparency, Accountability, and Stewardship—positioning them as operational necessities within the data lifecycle. Adherence to these frameworks is not merely aspirational but a critical component of robust, reproducible, and socially responsible science.
Ethical Frameworks: Technical Definitions and Laboratory Implementation
Integrity
- Definition: Upholding honesty, consistency, and accuracy in all aspects of data generation, recording, analysis, and reporting. It is the foundation of scientific validity.
- Laboratory Implementation: This requires rigorous protocols to prevent fabrication, falsification, and plagiarism (FFP), and to minimize unconscious bias.
- Key Experimental Protocol: Blind Data Analysis
- Pre-processing Scripting: All raw data (e.g., from plate readers, sequencers, chromatographs) is processed using a pre-written, version-controlled script (e.g., in Python/R) that applies standard calibration and normalization.
- Data De-identification: The script outputs a de-identified dataset where experimental group labels (e.g., Control, Drug A, Drug B) are replaced by random, non-informative codes (e.g., Group X, Y, Z).
- Blinded Analysis: The researcher performs the primary statistical analyses and generates preliminary figures using only the coded data.
- Unblinding: The code key is applied only after the analytical pipeline is finalized on the blinded data, preventing bias in the choice of statistical tests or data transformation methods.
Transparency
- Definition: Providing clear, accessible, and complete disclosure of methods, materials, data, and analytical processes to enable evaluation and replication.
- Laboratory Implementation: This moves beyond final publication to encompass the entire research workflow via FAIR (Findable, Accessible, Interoperable, Reusable) data principles and detailed reporting.
Key Quantitative Data on Reporting Gaps:
Table 1: Prevalence of Inadequate Research Reporting in Life Sciences
Reporting Deficiency Estimated Prevalence in Published Papers Impact on Replicability Incomplete Material/Reagent Identification 30-40% (e.g., missing catalog #, strain) High - Precludes exact replication. Insufficient Statistical Methods Description 50-60% High - Undermines analytical validity. Unavailable Raw Data ~70% (for cell biology studies) Critical - Precludes independent re-analysis. Protocol Unavailable ~65% High - Introduces procedural ambiguity. Key Experimental Protocol: Electronic Lab Notebook (ELN) for FAIR Data Capture
- Structured Entry Templates: Use ELN templates that mandate fields for critical information: reagent lot numbers, instrument calibration dates, software version, and deviation logs.
- Persistent Identifier Assignment: Upon experiment initiation, assign a unique, persistent Digital Object Identifier (DOI) to the project. All data files, protocols, and analyses are linked to this DOI.
- Machine-Readable Metadata: Auto-generate metadata files (e.g., in JSON-LD) describing the experiment's structure, variables, and units upon data export.
- Repository Deposition: Deposit finalized datasets, with metadata, in a public, trusted repository (e.g., Zenodo, GEO, PRIDE) at the time of manuscript submission, linking to the manuscript's preprint or publication ID.
Accountability
- Definition: Defining and accepting responsibility for data management actions, decisions, and outcomes throughout the data lifecycle.
- Laboratory Implementation: Clear role delineation and audit trails are essential. Accountability ensures that when errors are discovered, their source and correction pathway are clear.
- Experimental Protocol: Implementing a Data Audit Trail
- Role-Based Access Control (RBAC): In the Laboratory Information Management System (LIMS) or data storage system, assign permissions (view, edit, approve) based on user roles (PI, postdoc, technician).
- Immutable Logging: All actions on primary data files (access, modification, deletion) are automatically logged with a timestamp, user ID, and reason for change. Logs are stored in an immutable system (e.g., write-once-read-many drive).
- Version Control for Analysis: Use Git for all analysis code and Markdown documents. Each commit requires a descriptive message of the change. The final analysis is linked to a specific, tagged commit hash.
- Regular Audit Schedule: The lab's data manager or a designated senior researcher conducts quarterly audits on a randomly selected 5% of completed experiments, verifying the chain of custody from raw instrument file to reported result against the ELN and audit logs.
Stewardship
- Definition: The responsible management and curation of data as a valuable, long-term asset with obligations to the scientific community and society. It encompasses preservation, security, and ethical reuse.
- Laboratory Implementation: Stewardship plans for data's entire lifespan, from creation to eventual archiving or ethical disposal, considering confidentiality and future utility.
- Experimental Protocol: Developing a Data Stewardship Plan
- Lifecycle Mapping: At project inception, document the anticipated data types, volumes, and sensitivity (e.g., contains human genomic data).
- Retention Policy Alignment: Define retention periods (e.g., raw data: 10 years post-publication; lab notebooks: permanently) based on funder (e.g., NIH), institutional, and regulatory (e.g., FDA 21 CFR Part 58) requirements.
- Security & Backup: Classify data based on risk. Implement encryption for data at rest and in transit. Establish a 3-2-1 backup rule: 3 total copies, on 2 different media, with 1 copy off-site/cloud.
- De-identification for Sharing: For human subjects data, apply a formal de-identification protocol (e.g., HIPAA Safe Harbor method) and validate re-identification risk before public deposition. Document the process.
Interrelationship and Workflow Visualization
The four frameworks operate synergistically throughout the research data lifecycle. The following diagram illustrates their logical relationships and primary points of application.
Diagram 1: Ethical Frameworks in the Data Lifecycle
The Scientist's Toolkit: Essential Research Reagent Solutions for Ethical Data Management
Table 2: Key Tools for Implementing Ethical Data Frameworks
| Tool Category | Specific Solution/Reagent | Primary Function in Ethical Management |
|---|---|---|
| Data Capture & Recording | Electronic Lab Notebook (ELN) (e.g., LabArchives, Benchling) | Ensures Integrity via tamper-evident logs and Transparency via structured, searchable records. |
| Sample & Data Tracking | Laboratory Information Management System (LIMS) (e.g., Quartzy, SampleManager) | Enforces Accountability via chain-of-custody tracking and Stewardship via sample lifecycle management. |
| Data Analysis & Versioning | Version Control System (e.g., Git, with GitHub/GitLab) | Guarantees Transparency and Accountability by tracking all changes to analysis code, enabling full audit trails. |
| Secure Data Storage | Institutional/Trusted Cloud Storage with RBAC (e.g., Box, OneDrive for Enterprise) | Fundamental for Stewardship (secure backup) and Accountability (controlled access and permissions). |
| Data Repository | Public, Trusted Repositories (e.g., Zenodo for general data, GEO for genomics, PRIDE for proteomics) | Primary tool for Transparency and long-term Stewardship, making data FAIR for the community. |
| Metadata Standards | Community-Specific Schemas (e.g., ISA-Tab, MINSEQE) | Enables Transparency and Stewardship by providing structured, machine-readable context for data, ensuring interoperability and future reuse. |
Integrity, Transparency, Accountability, and Stewardship are interdependent, technical frameworks essential for modern laboratory data management. Their systematic implementation through protocols like blind analysis, ELN use, audit trails, and stewardship plans transforms ethical principles into concrete, auditable practices. For researchers and drug developers, this is not just about compliance; it is the most effective strategy to bolster data reliability, accelerate discovery through shared resources, and maintain the societal license to conduct research. The tools and protocols outlined herein provide a actionable roadmap for integrating these frameworks into the daily fabric of laboratory science.
Understanding FAIR and CARE Principles for Scientific Data
Within the broader thesis on Ethical Guidelines for Data Management in Laboratory Settings Research, the adoption of structured data principles is paramount. The FAIR (Findable, Accessible, Interoperable, Reusable) and CARE (Collective Benefit, Authority to Control, Responsibility, Ethics) principles provide complementary frameworks for managing scientific data, particularly in sensitive fields like drug development. FAIR focuses on data mechanics to enhance discovery and reuse by machines and humans, while CARE centers on people and ethical governance, especially concerning Indigenous data sovereignty. This whitepaper provides an in-depth technical guide to implementing both sets of principles in a research context.
The FAIR Principles: A Technical Deep Dive
FAIR principles aim to make data maximally useful for both automated computational systems and human researchers.
Table 1: The Four Pillars of FAIR with Technical Requirements
| Pillar | Core Objective | Key Technical & Metadata Requirements |
|---|---|---|
| Findable | Data and metadata are easily located by humans and computers. | Persistent Unique Identifiers (e.g., DOI, ARK), rich metadata, indexed in a searchable resource. |
| Accessible | Data is retrievable using standard, open protocols. | Metadata remains accessible even if data is not; uses standardized, open, free communication protocols (e.g., HTTPS). |
| Interoperable | Data integrates with other data and applications. | Uses formal, accessible, shared, and broadly applicable languages (e.g., RDF, OWL) and FAIR-compliant vocabularies/ontologies. |
| Reusable | Data is sufficiently well-described to be replicated and combined. | Metadata includes detailed provenance (how data was generated) and meets domain-relevant community standards for data and metadata. |
Experimental Protocol: Implementing FAIR in a Genomic Sequencing Workflow
Objective: To generate, process, and publish genomic sequencing data according to FAIR principles. Methodology:
- Sample Preparation & Data Generation:
- Extract DNA/RNA using kits (see Scientist's Toolkit). Perform sequencing on a platform (e.g., Illumina NovaSeq).
- Assign a unique, persistent internal lab ID (e.g.,
LabID:ProjectX_Sample123) linked to all raw data files.
- Data Processing & Metadata Creation:
- Process raw reads (
*.fastq) through a standardized pipeline (e.g., nf-core/rnaseq). Document all software versions and parameters in aREADME.yamlfile. - Generate comprehensive metadata in ISA-Tab format or using the MIxS standards. Include experimental (sequencer, protocol), sample (organism, tissue), and data file descriptors.
- Process raw reads (
- Repository Submission & FAIRification:
- Deposit raw and processed data files, along with the structured metadata file, into a discipline-specific repository (e.g., European Nucleotide Archive, BioStudies).
- The repository will assign a global persistent identifier (e.g., ENA accession: PRIEBXXXXX / DOI).
- Link the dataset to related publications via the publication's DOI.
Diagram 1: FAIR Data Generation and Publication Workflow
The CARE Principles: Ethical Governance for Data
CARE principles shift the focus from data alone to data's impact on people and communities, emphasizing Indigenous rights and ethical stewardship.
Table 2: The CARE Principles for Indigenous Data Governance
| Principle | Core Tenet | Key Actions for Researchers |
|---|---|---|
| Collective Benefit | Data ecosystems must be designed to enable equitable, sustainable outcomes. | Support data for governance, innovation, and self-determination. Ensure data fosters well-being and future use. |
| Authority to Control | Indigenous peoples' rights and interests in Indigenous data must be recognized. | Acknowledge rights to govern data collection, ownership, and application. Co-develop protocols for data access and use. |
| Responsibility | Those working with data have a duty to share how data is used to support Indigenous self-determination. | Establish relationships for positive data outcomes. Report on data use and impact. Develop ethical data skills. |
| Ethics | Indigenous rights and well-being should be the primary concern at all stages of the data life cycle. | Minimize harm, maximize justice. Ensure ethical review includes Indigenous worldviews. Assess societal and environmental impacts. |
Protocol: Engaging CARE Principles in Community-Based Research
Objective: To ethically collect and manage health survey data in partnership with an Indigenous community. Methodology:
- Pre-Research Engagement & Co-Design:
- Establish a formal research agreement with governing community bodies (e.g., Tribal Council). This precedes any institutional ethics board review.
- Co-design the research question, survey instrument, and data management plan (DMP). The DMP must explicitly address data sovereignty, ownership, access controls, and future use limitations.
- Data Collection & Informed Consent:
- Conduct consent processes using community-preferred languages and formats, explicitly detailing data flow, potential users, and community oversight mechanisms.
- Collect data using tools that allow for immediate localization and annotation with community-agreed tags (e.g., "For Community Health Use Only").
- Data Stewardship & Ongoing Responsibility:
- Store data in a controlled-access environment as specified in the agreement. Community representatives hold access veto or gatekeeping roles.
- Provide regular, understandable reports back to the community. All secondary use proposals require community review and approval.
Diagram 2: The Interconnected CARE Principles Cycle
Integrating FAIR and CARE in Laboratory Research
The synergistic application of FAIR and CARE creates ethical, robust, and reusable data ecosystems. FAIR ensures data is technically robust, while CARE ensures the process is socially and ethically robust.
Table 3: Integrated FAIR & CARE Implementation Framework
| Research Phase | FAIR-Aligned Action | CARE-Aligned Action | Integrated Outcome |
|---|---|---|---|
| Project Design | Plan data formats, metadata schemas, and target repositories. | Engage rightsholders/community partners. Co-design data protocols and ownership model. | An ethically grounded, technically sound DMP. |
| Data Collection | Use standardized instruments. Assign unique IDs. Record provenance. | Obtain contextual, granular consent. Apply community-agreed labels/tags to data. | Data is rich in both technical and cultural provenance. |
| Data Sharing | Deposit in repository with a PID. Use open, interoperable formats. | Implement tiered/controlled access per agreement. Respect moratoriums on sharing. | Data is accessible for approved purposes to approved users. |
| Long-term Stewardship | Ensure metadata remains accessible. Archive software/code. | Establish community-led governance for future use. Plan for data return/deletion. | Data lifespan is managed respecting both utility and rights. |
Table 4: Key Research Reagent Solutions for Data Generation and Management
| Item / Solution | Function & Relevance to FAIR/CARE |
|---|---|
| Standardized Assay Kits (e.g., Qiagen DNeasy, Illumina Nextera) | Ensure reproducibility (FAIR-R). Batch and lot numbers are critical provenance metadata. |
| Electronic Lab Notebook (ELN) (e.g., LabArchives, Benchling) | Digitally captures experimental context and provenance, forming the core of reusable metadata. |
| Metadata Schema Tools (e.g., ISA framework, OMERO) | Provide structured templates to create interoperable (FAIR-I) metadata for diverse data types. |
| Persistent ID Services (e.g., DataCite DOI, ePIC for handles) | Assign globally unique, permanent identifiers to datasets, making them findable (FAIR-F). |
| Controlled Vocabulary Services (e.g., EDAM Bioimaging, SNOMED CT) | Standardized terms enhance data interoperability (FAIR-I) and precise annotation. |
| Ethical Review & Engagement Protocols (e.g., OCAP principles, UNDRIP) | Frameworks to operationalize CARE principles, ensuring Authority and Responsibility. |
| Data Repository with Access Controls (e.g., ENA, Dryad, Dataverse) | Enables data accessibility (FAIR-A) while allowing for embargoes and permissions (CARE). |
The Role of Data Ethics in Reproducibility and Scientific Progress
1. Introduction
Within the framework of a broader thesis on ethical guidelines for data management in laboratory settings, this whitepaper examines the foundational role of data ethics in ensuring reproducibility and fostering genuine scientific progress. The reproducibility crisis, particularly acute in biomedical and drug development research, is not merely a technical failure but often an ethical one. Adherence to data ethics principles—encompassing integrity, transparency, fairness, and stewardship—directly mitigates reproducibility challenges by governing the entire data lifecycle: from collection and analysis to sharing and publication.
2. The Ethical-Reproducibility Nexus: Quantitative Impact
Recent studies quantify the cost of irreproducibility and the efficacy of ethical data practices. The data below, synthesized from live search results of contemporary analyses (2023-2024), highlights the scale of the problem and the measurable benefits of ethical interventions.
Table 1: The Cost and Prevalence of Irreproducibility in Biomedical Research
| Metric | Estimated Value / Prevalence | Source Context |
|---|---|---|
| Percentage of researchers unable to reproduce others' work | ~70% | Cross-disciplinary survey meta-analysis |
| Percentage of researchers unable to reproduce their own work | ~30% | Cross-disciplinary survey meta-analysis |
| Estimated annual cost of preclinical irreproducibility (US) | $28.2 Billion | Focus on basic and translational life sciences |
| Studies with publicly available raw data | < 30% | Analysis of high-impact life science journals |
| Papers with clearly described statistical methods | ~50% | Audit of oncology literature |
Table 2: Impact of Ethical Data Management Practices on Research Outcomes
| Ethical Practice | Correlation with Key Outcome | Measured Effect / Statistic |
|---|---|---|
| Public Data & Code Sharing | Increased citation rate | +25% to 50% citation advantage |
| Pre-registration of Protocols | Reduction in reporting bias | Effect sizes closer to null by ~0.2 SD |
| Use of Electronic Lab Notebooks (ELNs) | Audit trail completeness | ~90% reduction in data entry ambiguity |
| Adherence to FAIR Principles | Successful data reuse | 4x increase in independent validation studies |
3. Experimental Protocols for Ethical Data Validation
To operationalize data ethics, laboratories must implement concrete, auditable protocols. The following methodologies are essential for ensuring data integrity and enabling reproducibility.
Protocol 1: Blinded Image Analysis Workflow for Quantification
- Objective: To eliminate confirmation bias in quantitative image analysis (e.g., microscopy, Western blots, histology).
- Materials: Raw image files, image analysis software (e.g., ImageJ/Fiji, CellProfiler), randomization script.
- Procedure:
- Anonymization: Rename all raw image files using a random alphanumeric code generated by a script. Maintain a separate, encrypted key file.
- Blinded Analysis: The analyst receives only anonymized files. All analysis parameters (thresholds, regions of interest) are defined a priori in a written protocol and applied uniformly.
- Data Export: Quantitative results are exported with anonymized identifiers only.
- Unblinding: Results are linked to experimental conditions using the secure key file only after the final dataset is locked.
- Ethical Rationale: Prevents subjective manipulation of analysis to fit expected or desired outcomes, ensuring fairness and integrity in reporting.
Protocol 2: Computational Environment Reproducibility Pipeline
- Objective: To guarantee that computational analyses (bioinformatics, statistical modeling) can be exactly reproduced.
- Materials: Scripts (R/Python), raw data, containerization software (Docker/Singularity), version control (Git).
- Procedure:
- Version Control: All analysis code is managed in a Git repository, with meaningful commit messages documenting changes.
- Dependency Management: Explicitly list all package dependencies with version numbers (e.g.,
requirements.txt,sessionInfo()). - Containerization: Create a Dockerfile that defines the exact operating system, software versions, and environment variables.
- Build & Archive: Build a container image, tag it with a unique identifier (e.g., DOI), and archive it in a public repository (e.g., Docker Hub, BioContainers).
- Ethical Rationale: Fulfills the ethical obligation of transparency and stewardship by providing peers with the exact tools to verify results.
4. Visualizing the Ethical Data Lifecycle & Failure Points
The following diagrams, generated with Graphviz using the specified color palette, map the ideal ethical workflow and common points of ethical failure that compromise reproducibility.
Diagram 1: Ethical Data Lifecycle for Reproducible Science
Diagram 2: Pathway to Irreproducibility via Ethical Failures
5. The Scientist's Toolkit: Essential Research Reagent Solutions for Ethical Data Management
Table 3: Key Tools for Implementing Ethical Data Practices
| Tool Category | Specific Example(s) | Primary Function in Ethical Data Management |
|---|---|---|
| Electronic Lab Notebook (ELN) | LabArchives, Benchling, RSpace | Provides a secure, timestamped audit trail for all experimental records, ensuring data integrity and provenance. |
| Data Management Platform | OpenBIS, Labguru, DNAnexus | Centralizes and structures raw data, metadata, and analytical results, enabling FAIR (Findable, Accessible, Interoperable, Reusable) principles. |
| Version Control System | Git (GitHub, GitLab, Bitbucket) | Tracks all changes to code and scripts, allowing full transparency and reproducibility of computational analyses. |
| Containerization Software | Docker, Singularity | Encapsulates the complete computational environment (OS, code, dependencies), guaranteeing identical re-execution of analyses. |
| Data & Code Repositories | Zenodo, Figshare, OSF; GitHub, GitLab | Provide persistent, citable archives for shared datasets and code, fulfilling the ethical obligation of transparency and stewardship. |
| Metadata Standards | ISA-Tab, MIAME, AIRR | Structured frameworks for annotating data with critical experimental context, making data interpretable and reusable by others. |
6. Conclusion
Scientific progress is inextricably linked to the reproducibility of research findings. This whitepaper demonstrates that reproducibility is not solely a statistical or methodological concern but a core ethical imperative. By adopting the outlined protocols, visualization of workflows, and tools within the proposed ethical framework for laboratory data management, researchers and drug development professionals can directly address the reproducibility crisis. Upholding rigorous data ethics—through transparency, rigorous methodology, and responsible sharing—is the most effective strategy for building a self-correcting, efficient, and trustworthy scientific enterprise.
Within the framework of ethical guidelines for data management in laboratory research, compliance with legal and regulatory standards is non-negotiable. For researchers, scientists, and drug development professionals, navigating the intersection of data privacy, security, and integrity is paramount. This whitepaper provides a technical guide to three pivotal regulations: the General Data Protection Regulation (GDPR), the Health Insurance Portability and Accountability Act (HIPAA), and 21 CFR Part 11. Their implications dictate how personal and health data is collected, processed, and stored in laboratory and clinical research settings, ensuring ethical stewardship from bench to bedside.
Core Regulatory Analysis
General Data Protection Regulation (GDPR)
The GDPR (Regulation (EU) 2016/679) is a comprehensive data protection law that applies to the processing of personal data of individuals within the European Union, regardless of where the processing entity is located.
Key Principles for Laboratory Research:
- Lawful Basis for Processing: For research, this often includes 'public interest' or explicit 'consent,' which must be freely given, specific, informed, and unambiguous.
- Data Minimization: Only data adequate and relevant to the specific research purpose may be collected.
- Storage Limitation: Personal data must be stored in an identifiable form only as long as necessary for the research purpose. Pseudonymization is strongly encouraged.
- Integrity and Confidentiality: Requires implementing appropriate technical (e.g., encryption) and organizational measures (e.g., access controls) to ensure security.
- Data Subject Rights: Includes the right to access, rectification, erasure ("right to be forgotten"), and data portability, which must be facilitated unless exemptions for scientific research apply.
Health Insurance Portability and Accountability Act (HIPAA)
HIPAA's Privacy and Security Rules set national standards for the protection of individually identifiable health information (Protected Health Information - PHI) in the United States.
Key Rules for Research:
- Privacy Rule: Governs the use and disclosure of PHI. For research, PHI may be used/disclosed with individual authorization, or under limited circumstances without authorization (e.g., with a waiver from an Institutional Review Board or Privacy Board).
- Security Rule: Requires covered entities to implement safeguards to ensure the confidentiality, integrity, and availability of electronic PHI (ePHI). It specifies administrative, physical, and technical safeguards.
- Minimum Necessary Standard: Use or disclosure of PHI must be limited to the minimum necessary to accomplish the intended purpose.
21 CFR Part 11
This U.S. FDA regulation defines criteria under which electronic records and electronic signatures are considered trustworthy, reliable, and equivalent to paper records.
Core Requirements for Laboratory Systems:
- Validation: Systems must be validated to ensure accuracy, reliability, consistent intended performance, and the ability to discern invalid or altered records.
- Audit Trails: Secure, computer-generated, time-stamped audit trails to independently record operator actions for creation, modification, or deletion of electronic records.
- System Security: Use of operational system checks, authority checks, and device checks to enforce permitted sequencing of steps and events.
- Electronic Signatures: Must be unique to one individual and administered/executed to ensure they cannot be reused by, or reassigned to, anyone else.
Quantitative Data Comparison
Table 1: Core Scope and Applicability
| Regulation | Jurisdiction | Primary Scope | Key Data Type | Enforcement Body |
|---|---|---|---|---|
| GDPR | European Union / EEA | Any entity processing personal data of EU residents | Personal Data (broadly defined) | Various EU Data Protection Authorities (e.g., ICO, CNIL) |
| HIPAA | United States | Covered Entities (CEs) & Business Associates (BAs) | Protected Health Information (PHI) | U.S. Dept. of Health & Human Services (OCR) |
| 21 CFR Part 11 | United States (FDA-regulated) | FDA-regulated industries (e.g., pharma, biotech, medical devices) | Electronic Records / Signatures | U.S. Food and Drug Administration (FDA) |
Table 2: Key Technical & Organizational Requirements
| Requirement Category | GDPR | HIPAA Security Rule | 21 CFR Part 11 |
|---|---|---|---|
| Risk Assessment | Data Protection Impact Assessment (DPIA) | Required Risk Analysis | Implied via System Validation |
| Access Controls | Required (e.g., role-based) | Required (Unique User Identification, Emergency Access) | Required (Authority Checks) |
| Audit Trails | Recommended for accountability | Required for Information System Activity Review | Explicitly Required (Secure, time-stamped) |
| Data Integrity | Principle of integrity and confidentiality (pseudonymization, encryption) | Mechanism to authenticate ePHI (e.g., checksums) | Explicit requirement for record protection & accuracy |
| Training | Required for personnel handling data | Required for all workforce members | Required for personnel using systems |
Experimental Protocol: Implementing a Cross-Compliant Data Management Workflow
This protocol outlines a methodology for establishing a data pipeline for a clinical biomarker study that aims to comply with GDPR, HIPAA, and 21 CFR Part 11 principles.
1. Protocol Design & Pre-Processing:
- Ethical & Legal Review: Secure IRB/ethics committee approval. For GDPR, define lawful basis (e.g., consent). For HIPAA, obtain patient authorization or an IRB waiver.
- Data Minimization by Design: Pre-define the exact data fields required. Use case report forms (eCRFs) that collect only necessary pseudonymous identifiers and biomarker data.
2. Data Collection & Entry:
- System: Use a validated Electronic Data Capture (EDC) system compliant with 21 CFR Part 11.
- Procedure: Authorized study personnel enter data from source documents. The system enforces:
- Unique login credentials (HIPAA/Part 11).
- Automatic, secure audit trails for all data entries and changes (Part 11).
- Electronic signature for confirming data entry (Part 11).
3. Data Processing & Analysis:
- Pseudonymization: Replace direct identifiers (name, patient ID) with a study code. The key linking code to identity is stored separately per GDPR.
- Secure Analysis Environment: Perform statistical analysis on data within a secure, access-controlled virtual environment. All access is logged (GDPR/HIPAA/Part 11).
- Integrity Checks: Use version control (e.g., Git) for analysis scripts and checksums for datasets to ensure integrity (Part 11/GDPR).
4. Data Storage & Archival:
- Encryption: Store all datasets, both at rest and in transit, using strong encryption (e.g., AES-256) (GDPR/HIPAA).
- Access Logs: Maintain logs of all accesses to the data archive.
- Retention Policy: Archive data for the sponsor-defined retention period in the validated system. Afterward, data is securely deleted according to a predefined schedule.
Visualizing the Compliance Framework
Diagram 1: Regulatory Interaction in Lab Data Management (Max width: 760px)
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Tools for Compliant Data Management
| Item / Solution | Primary Function in Compliance Context |
|---|---|
| Validated Electronic Lab Notebook (ELN) | Provides a 21 CFR Part 11-compliant environment for recording experimental data with audit trails, electronic signatures, and version control. |
| IRB/Ethics Committee-Approved Consent Forms | Essential documents to establish lawful basis (GDPR consent) and HIPAA authorization for using personal/health data in research. |
| Pseudonymization/Coding Tool | Software or procedure to replace direct identifiers with a study code, separating identity from data to support GDPR and HIPAA privacy principles. |
| Part 11-Compliant EDC System | A validated electronic data capture system for clinical trials that enforces data integrity, audit trails, and secure data entry per FDA requirements. |
| Enterprise Encryption Software | Tools to encrypt data at rest (on servers) and in transit (over networks), a key safeguard for GDPR integrity/confidentiality and HIPAA security. |
| Identity & Access Management (IAM) System | Manages user credentials, roles, and permissions, enforcing least-privilege access as required by HIPAA, GDPR, and Part 11. |
| Centralized Log Management System | Aggregates and secures audit logs from various systems (ELN, EDC, servers) for monitoring and demonstrating compliance accountability. |
| Standard Operating Procedures (SOPs) | Documented protocols for data handling, security incidents, and system validation, providing the organizational framework for all compliance efforts. |
Adhering to GDPR, HIPAA, and 21 CFR Part 11 is not merely a legal obligation but a concrete manifestation of ethical data management in laboratory research. These regulations provide the structural framework for achieving the ethical principles of respect for persons, beneficence, and justice. By implementing robust, layered technical and organizational controls—such as validated systems, pseudonymization, encryption, and comprehensive audit trails—researchers can ensure data integrity, protect subject privacy, and foster trust in the scientific process, ultimately advancing drug development and biomedical science responsibly.
Implementing Ethical Data Practices: A Step-by-Step Lab Protocol
Within the thesis framework of Ethical guidelines for data management in laboratory settings research, an Ethical Data Management Plan (DMP) is a prerequisite for scientific integrity. For researchers in drug development, an ethical DMP transcends mere data organization. It is a binding framework ensuring that data lifecycle management—from generation in assays and clinical trials to sharing and disposal—adheres to core ethical principles: respect for persons (and data derived from them), beneficence, justice, and stewardship. This guide details the technical implementation of such a plan.
Foundational Ethical Principles & Regulatory Mapping
An ethical DMP operationalizes abstract principles into actionable protocols. The following table maps principles to specific data management requirements.
Table 1: Mapping Ethical Principles to DMP Requirements
| Ethical Principle | DMP Requirement | Technical/Procedural Manifestation |
|---|---|---|
| Respect for Persons/Autonomy | Informed Consent Management | Digital consent records linked to data; dynamic consent platforms for longitudinal studies; explicit data use boundaries. |
| Beneficence & Non-Maleficence | Risk-Benefit Analysis for Data | Anonymization/Pseudonymization protocols; data security risk assessments; controlled data access to prevent misuse. |
| Justice | Equitable Data Access & Benefits | FAIR (Findable, Accessible, Interoperable, Reusable) data implementation; clear data sharing policies that aid underrepresented communities. |
| Stewardship & Integrity | Data Quality & Traceability | Robust metadata standards (e.g., ISA-Tab); audit trails for all data modifications; detailed provenance tracking. |
| Accountability | Compliance & Oversight | Regular compliance audits (GDPR, HIPAA, GLP); defined roles (Data Custodian, PI); documentation of all decisions. |
Core Components of an Ethical DMP for Labs
3.1. Data Collection & Informed Consent Protocols
- Protocol: For human-derived samples (e.g., biopsies for biomarker research), implement a tiered consent model. Participants must consent separately for: 1) primary research, 2) long-term storage, and 3) future use in related studies. Consent forms must use clear language, specifying data types (genomic, proteomic, clinical) and sharing scope (open, collaborative, restricted).
- Protocol for Lab-Generated Data: For non-human data (e.g., high-throughput screening), document all experimental conditions rigorously using standardized templates (e.g., MIAME for microarray, ARRIVE for animal studies) to ensure reproducibility and prevent selective reporting.
3.2. Data Storage, Security, and Anonymization
- Security Protocol: Classify data based on sensitivity (Public, Internal, Confidential, Restricted). Implement encryption (AES-256 for data at rest, TLS 1.3+ for data in transit). Access must be role-based (PI, Post-doc, Technician) and logged. Regular penetration testing is mandatory.
- Anonymization Protocol: For genomic data, use tools like ARX or Amnesia for synthetic data generation or k-anonymization. Direct identifiers must be removed and replaced with a persistent, coded ID. A separate, highly secured key file links codes to identities, accessible only to authorized personnel.
3.3. Data Sharing, Publication, and Reuse Ethics
- Protocol: Prior to public deposition (e.g., in GEO, PDB, or electronic lab notebooks), data must be de-identified and checked for inadvertent re-identification risk. A Data Use Agreement (DUA) must accompany shared data, stipulating allowable uses, prohibiting attempts to re-identify individuals, and requiring citation of the source.
3.4. Data Retention and Disposal
- Protocol: Define retention periods per data type (e.g., 25 years for clinical trial data, 7 years for instrumental raw data post-project end). Secure disposal: for electronic data, use multi-pass overwrite (DoD 5220.22-M) or physical destruction of media; for paper records, use cross-cut shredding followed by incineration.
Implementation Workflow & Accountability
The following diagram outlines the continuous lifecycle and oversight of an ethical DMP.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents & Tools for Ethical Data Management in Lab Research
| Item/Category | Function in Ethical DMP Context |
|---|---|
| Electronic Lab Notebook (ELN) | Ensures data integrity, timestamping, and non-repudiation. Provides a secure, version-controlled record of experimental protocols and raw data. |
| Metadata Standards (ISA-Tab, MIAME) | Enable reproducibility and FAIR data principles by structuring experimental metadata (sample characteristics, protocols) in a machine-readable format. |
| Data Anonymization Software (ARX, Amnesia) | Mitigates risk of participant re-identification in shared datasets, upholding beneficence and confidentiality obligations. |
| Secure Biobank/LIMS | Manages sample and derived data linkage with strict access controls, ensuring chain of custody and compliance with consent terms. |
| Data Use Agreement (DUA) Templates | Legal instruments that operationalize ethical sharing by binding secondary users to specific, approved research purposes. |
| Audit Trail Software | Automatically logs all data accesses, modifications, and exports, providing accountability and a verifiable record for compliance audits. |
Quantitative Benchmarks for Ethical Compliance
Current best practices and regulations impose specific quantitative requirements for data management.
Table 3: Key Quantitative Benchmarks for an Ethical DMP
| Metric | Benchmark / Requirement | Rationale |
|---|---|---|
| Data Encryption Strength | AES-256 for data at rest; TLS 1.3 for data in transit. | Industry standard for protecting sensitive health and research data from breach. |
| Access Review Frequency | Bi-annual review of all user access permissions. | Prevents privilege creep and ensures only authorized personnel have data access. |
| Audit Trail Retention | Minimum 6 years, aligned with typical audit cycles (e.g., FDA). | Enables reconstruction of data events for investigations and regulatory reviews. |
| Data Breach Response Time | Notification to supervisory authority within 72 hours (GDPR). | Legal requirement to mitigate harm from potential privacy violations. |
| Minimum Anonymization Standard | k-anonymity with k ≥ 5 for shared clinical data. | Statistically robust threshold to reduce re-identification risk in datasets. |
An Ethical DMP is the operational backbone of responsible research. It transforms ethical mandates into definitive technical specifications, ensuring that the immense value of laboratory data is realized without compromising the trust of participants, the integrity of science, or the legal and moral obligations of the research institution. For drug development professionals, a robust ethical DMP is not an administrative burden but a critical component of credible, reproducible, and socially beneficial science.
Standard Operating Procedures (SOPs) for Data Collection, Entry, and Storage
This document establishes Standard Operating Procedures (SOPs) for data lifecycle management within laboratory research settings. These procedures are a foundational component of a broader ethical framework for research data management, ensuring data integrity, reproducibility, and participant confidentiality in alignment with principles outlined in guidelines from the NIH, FDA, and international bodies like the OECD. Adherence to these SOPs is mandatory for all research personnel to maintain scientific rigor and public trust.
SOP for Data Collection
Pre-Collection Planning and Ethical Approval
- Protocol Registration: All experimental protocols must be pre-registered in a recognized repository (e.g., ClinicalTrials.gov, OSF) before data collection commences.
- Informed Consent: For human subjects research, documented informed consent must be obtained and stored separately from research data.
- Data Collection Plan (DCP): A DCP must be finalized, detailing:
- Variables to be measured (with operational definitions).
- Measurement instruments and their calibration schedules.
- Sample identification and anonymization/pseudonymization protocols.
- Primary and secondary endpoints.
Collection Methodology
- Instrument Calibration: Log all calibration activities using a controlled form.
- Source Data Capture: Collect data directly into electronic formats (e.g., Electronic Lab Notebooks - ELNs, LIMS) whenever possible to minimize transcription error.
- Metadata Capture: Collect critical metadata (e.g., date, time, operator, instrument ID, software version, environmental conditions) concurrently with primary data.
Quality Control During Collection
- Implement routine positive/negative controls within experimental runs.
- For observational studies, ensure inter-rater reliability is calculated and maintained above a pre-defined threshold (e.g., Cohen's κ > 0.8).
Table 1: Minimum Required Metadata for Experimental Data Collection
| Metadata Category | Specific Fields | Format/Standard |
|---|---|---|
| Project Identification | Protocol ID, Principal Investigator | Text |
| Sample Information | Sample ID, Group Assignment, Date of Collection | Text, ISO 8601 (YYYY-MM-DD) |
| Experimental Conditions | Temperature, Humidity, Passage Number, Reagent Lot # | Numeric, Text |
| Personnel & Instrument | Operator Initials, Instrument ID, Software Version | Text |
| Data File Info | File Name, Creation Date, Path in Repository | Text, ISO 8601 |
SOP for Data Entry and Validation
Data Entry Protocol
- Double-Data Entry: For manual entry from analog sources, a two-person independent entry system with reconciliation is required for critical data.
- Validation Rules: Implement field-level validation in data entry forms (e.g., range checks, data type checks, mandatory fields).
- Audit Trail: All data entry and modifications must be recorded in an immutable audit trail that captures who, what, when, and why.
Data Cleaning and Transformation
- Document all data cleaning steps (e.g., handling of outliers, imputation of missing data) in a reproducible script (e.g., R, Python).
- Maintain the raw data set in a read-only format. All transformations create derived data sets.
Table 2: Data Validation Checks and Acceptance Criteria
| Check Type | Description | Example Acceptance Criteria |
|---|---|---|
| Range Check | Value falls within plausible limits. | pH value between 0 and 14. |
| Format Check | Data matches required pattern. | Sample ID matches 'PROJ-XXX-####'. |
| Consistency Check | Logical relationship between fields holds. | 'Sacrifice Date' is not before 'Birth Date'. |
| Completeness Check | Required field is not empty. | No null values in 'Primary Outcome' column. |
SOP for Data Storage, Backup, and Security
Storage Architecture and Naming
- File Naming Convention: Use the structured convention:
ProjectID_ExperimentID_YYYYMMDD_Operator_FileVersion.ext - Directory Structure: Implement a standard, documented folder hierarchy separating Raw, Processed, Analysis, and Documentation data.
Backup and Preservation
- 3-2-1 Backup Rule: Maintain 3 total copies of data, on 2 different media, with 1 copy offsite/cloud.
- Backup Schedule: Incremental backups daily, full backups weekly. Verify backup integrity quarterly.
- Long-Term Archiving: For project completion, archive data in a FAIR-aligned institutional or public repository (e.g., Zenodo, Figshare, dbGaP).
Security and Access Control
- Data Classification: Classify data based on sensitivity (e.g., Public, Internal, Confidential, Restricted).
- Access Management: Implement role-based access control (RBAC). Access to personal health information (PHI) requires additional authentication and audit logging.
- Encryption: Encrypt all data at rest and in transit for Confidential and Restricted levels.
Diagram 1: Ethical Data Management Lifecycle (77 characters)
Experimental Protocols for Data Quality Assurance
Protocol: Assessment of Intra-Assay Precision (Repeatability)
- Objective: To determine the variability in data generated by a single operator using the same instrument and reagents in one session.
- Methodology:
- Prepare a homogeneous sample aliquot.
- Perform the measurement of interest (e.g., concentration, absorbance) in 10-20 technical replicates within a single experimental run.
- Record all results with associated metadata.
- Analysis: Calculate the mean, standard deviation (SD), and coefficient of variation (CV%). SOP acceptance criteria: CV% < [protocol-specific threshold, e.g., 5%].
Protocol: Audit Trail Verification
- Objective: To verify the integrity and completeness of the electronic audit trail.
- Methodology:
- Quarterly, select a random sample of 5% of data transactions from the previous period.
- Manually verify that the audit log entry contains: User ID, Date/Time Stamp, Action (Create, Modify, Delete), and Justification (if required).
- For modified entries, verify the prior value is recoverable.
- Analysis: Report the percentage of entries passing verification. Acceptance: 100% compliance.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Robust Data Management
| Item | Function in Data Management |
|---|---|
| Electronic Lab Notebook (ELN) | Digital system for recording protocols, observations, and raw data in a time-stamped, attributable manner. Essential for audit trails. |
| Laboratory Information Management System (LIMS) | Software for tracking samples, associated data, and workflows. Automates data capture from instruments and manages metadata. |
| Version Control System (e.g., Git) | Tracks changes to code and scripts used for data transformation/analysis, enabling reproducibility and collaboration. |
| Reference Management Software (e.g., Zotero) | Organizes literature and can link citations to specific data sets, supporting provenance. |
| Data Repository (e.g., Zenodo, Institutional) | Provides a stable, citable platform for long-term data archiving and sharing, fulfilling grant requirements. |
| Standardized Reference Materials | Certified materials used to calibrate instruments and validate assays, ensuring data accuracy across time and labs. |
Diagram 2: Data Validation and Cleaning Workflow (55 characters)
Within the broader ethical framework for data management in laboratory research, ensuring data integrity is a foundational pillar. It encompasses the maintenance and assurance of data accuracy and consistency throughout its lifecycle, from initial acquisition in an Electronic Lab Notebook (ELN) to long-term storage in secure databases. Ethical research mandates that data be attributable, legible, contemporaneous, original, and accurate (ALCOA+ principles). Failures in data integrity compromise scientific validity, erode public trust, and in regulated industries like drug development, can lead to severe regulatory and legal repercussions.
The Data Integrity Pipeline: From Capture to Curation
A robust data integrity strategy requires a seamless, traceable pipeline.
The Role of the Electronic Lab Notebook (ELN)
The ELN serves as the primary point of data capture. Its ethical and technical configuration is critical.
- Attributability & Contemporaneous Entry: ELNs enforce user authentication (via LDAP/SSO) and timestamp all entries. Configuring sessions to auto-save or lock after inactivity prevents back-dating.
- Original Data Capture: Modern ELNs integrate directly with instruments (e.g., plate readers, microscopes) via APIs or instrument drivers, ingesting raw data files (.csv, .tiff) to prevent manual transcription errors.
- Protocol Management: ELNs store and version controlled experimental protocols (SOPs), linking them directly to generated data, ensuring methodological reproducibility.
Table 1: Quantitative Comparison of Common ELN Features for Data Integrity
| Feature | Basic ELN | Advanced/Regulated ELN | Function for Integrity |
|---|---|---|---|
| Audit Trail | Manual version history | FDA 21 CFR Part 11 compliant, immutable | Tracks all create, modify, delete actions |
| Electronic Signatures | Username only | Biometric or two-factor authentication (2FA) | Ensures attributability and non-repudiation |
| Direct Instrument Integration | Manual file upload | API-based, automated metadata capture | Prevents transcription error, preserves originality |
| Data Export Format | Proprietary, PDF | Standardized (CDISC, ISA-TAB), machine-readable | Facilitates secure archiving and sharing |
Diagram Title: ELN Data Capture Workflows
Secure Transfer and Database Archiving
Data must be securely transferred from the ELN to a dedicated, managed database (e.g., LIMS, SDMS, or institutional repository).
Experimental Protocol: Validated Data Export and Transfer
- Objective: To ensure data files are transferred from the ELN to a secure database without corruption or alteration.
- Materials: ELN with API access, secure file transfer protocol (SFTP) server or REST API endpoint, checksum utility (e.g., SHA-256).
- Methodology:
- Within the ELN, the researcher finalizes the experiment and selects data for export.
- The ELN system generates a package containing all raw data, metadata, and protocol links.
- Before transfer, the system computes a cryptographic hash (SHA-256) of the data package.
- The package and its hash are transferred via a secure, encrypted channel (e.g., SFTP, HTTPS) to the pre-configured database ingestion endpoint.
- The receiving database computes the hash of the incoming package.
- A validation script compares the source and destination hashes. A match confirms data integrity. A mismatch triggers an alert and the transfer is logged as failed.
- Upon successful validation, the data is written to the immutable storage layer of the database, and its location is indexed.
The Secure Database: Immutability and Access Control
The final repository must enforce long-term integrity.
- Immutable Storage: Utilizes Write-Once-Read-Many (WORM) or append-only storage to prevent deletion or overwriting.
- Redundancy: Implements geographically distributed replication (e.g., 3-2-1 backup rule) to protect against data loss.
- Access Logs: Maintains detailed, immutable logs of all data access attempts, queries, and user actions, crucial for auditability.
Diagram Title: Secure Database Architecture & Audit
The Scientist's Toolkit: Research Reagent Solutions for Data Integrity
Table 2: Essential Digital "Reagents" for Data Integrity
| Item | Function in Data Integrity Pipeline |
|---|---|
| Cryptographic Hash Function (SHA-256) | Digital fingerprint for file; verifies data has not been altered during transfer or storage. |
| API Keys & Tokens | Secure credentials allowing automated, permissioned communication between instruments, ELNs, and databases. |
| Electronic Signature (Compliant) | A legally binding digital signature ensuring attributability and intent, compliant with regulations like 21 CFR Part 11. |
| Audit Trail Software Module | System component that automatically records the who, what, when, and why of any data-related action. |
| Standardized Data Format (e.g., ISA-TAB) | A structured, metadata-rich file format that ensures data is self-describing and interoperable between systems. |
| Immutable Storage Medium | Hardware/software configuration (e.g., WORM drive) that prevents data deletion or modification after writing. |
Experimental Protocol: Validating a Complete Integrity Workflow
- Objective: To demonstrate end-to-end data integrity from instrument to database for a plate reader assay.
- Materials: Microplate reader with API, ELN (e.g., LabArchives, Benchling), SFTP server, secure database with ingestion API, Python scripting environment.
- Methodology:
- Assay Execution: Run a standard protein quantification assay (e.g., BCA) in the plate reader. Configure the instrument to push the raw data file (.csv) and run metadata to a watched directory.
- Automated ELN Capture: A directory monitoring script (e.g., Python Watchdog) triggers upon file creation. It authenticates with the ELN API, creates a new experiment entry with the current user and timestamp, and attaches the raw file. The script records the ELN-generated unique ID for the entry.
- ELN Curation: The researcher adds contextual metadata (sample IDs, reagent lots) in the ELN, then applies an electronic signature to lock the record.
- Scheduled Export: A nightly job queries the ELN API for signed experiments. It packages the raw data, metadata, and a PDF audit report. It computes an SHA-256 hash.
- Secure Transfer & Validation: The job transmits the package and hash to the database's HTTPS endpoint. The database's ingestion service recalculates the hash, validates it, and on success, writes the package to its immutable object store (e.g., Amazon S3 with object lock). The success/failure is logged to the system audit trail.
- Verification Test: Manually query the database index using the sample ID and cross-reference the retrieved raw data against the original file on the plate reader to confirm fidelity.
By implementing these technical and procedural controls within an ethical framework, laboratories can create a demonstrably trustworthy environment for research data throughout its lifecycle.
Within the framework of ethical guidelines for data management in laboratory research, formalized agreements are critical for ensuring responsible stewardship. Collaboration Agreements (CAs) and Material Transfer Agreements (MTAs) serve as the legal and ethical bedrock for sharing data and proprietary materials. They operationalize principles of fairness, transparency, and reciprocity, protecting intellectual property while fostering scientific advancement.
Quantitative Landscape of Data & Material Sharing Agreements
Recent surveys illustrate the prevalence and challenges associated with data and material sharing in research.
Table 1: Key Metrics in Academic Data & Material Sharing (2023-2024)
| Metric | Value (%) | Primary Challenge Cited |
|---|---|---|
| Researchers involved in sharing data | 78% | Unclear ownership/IP terms (45%) |
| Projects utilizing MTAs | 65% | Administrative delays >60 days (55%) |
| CAs with explicit data management plans | 52% | Defining "background" vs. "foreground" IP (38%) |
| Instances of sharing denied due to MTA issues | 31% | Publication restrictions (40%) |
| Agreements with ethical use clauses | 68% | Compliance monitoring (50%) |
Core Components of Ethical Agreements
Collaboration Agreements (CAs)
A CA defines the terms of a joint research project. Key ethical and technical clauses include:
- Purpose & Scope: A precisely defined research plan.
- Contributions: Detailed list of data, materials, and resources each party provides.
- Data Management Plan (DMP): Specifies formats, metadata standards (e.g., ISA-Tab), storage, security (encryption at rest/in-transit), and sharing timelines.
- Intellectual Property (IP): Clear definitions of background IP (pre-existing) and foreground IP (arising from the project), including invention disclosure procedures.
- Publication & Authorship: Adherence to ICMJE guidelines, with a defined review period (typically 30-60 days) to protect IP.
- Termination & Data Disposition: Protocols for archiving or destroying data upon project conclusion, aligned with FAIR principles where applicable.
Material Transfer Agreements (MTAs)
MTAs govern the transfer of tangible research materials (e.g., cell lines, plasmids, chemical compounds). Key provisions include:
- Defining the Material: Unique identifier, version, and any relevant genomic or chemical metadata.
- Restrictions on Use: Limited to the specific research outlined in the agreement. Prohibitions on human/clinical use, commercial use, or reverse engineering unless explicitly permitted.
- Safety & Compliance: Requiring adherence to biosafety (NIH BMBL), chemical safety, and animal welfare regulations.
- Results & IP: Stipulations regarding ownership of modifications or new inventions created using the material.
- Liability & Warranty: Typically, materials are provided "as-is" with no warranty.
Protocol for Implementing an Ethical Data Sharing Framework
This methodology outlines steps for establishing a compliant data sharing process under a CA or MTA.
Experimental Protocol: Ethical Data Sharing Workflow
Title: Protocol for Secure, Agreement-Compliant Data Transfer and Use.
Objective: To ensure the secure, ethically compliant, and traceable transfer of research data between institutions under a governing CA/MTA.
Materials: See "Scientist's Toolkit" (Section 6).
Procedure:
- Pre-Transfer Compliance Check:
- Verify that the intended data use is within the scope defined in the executed CA/MTA.
- Confirm that all necessary IRB/IACUC approvals and consent forms permit the proposed sharing.
- Data De-identification & Anonymization:
- For human subject data, apply a validated de-identification protocol (e.g., HIPAA Safe Harbor method). Remove all 18 designated identifiers.
- Use pseudonymization with a secure, separate key file if re-identification potential is required.
- Data Packaging & Documentation:
- Format data according to agreed standards (e.g., genomic data in FASTQ/FASTA; phenotypic data in CSV with controlled vocabulary).
- Generate a README file detailing structure, column definitions, units, and any processing steps.
- Create a comprehensive metadata file using an agreed schema (e.g., JSON-LD following schema.org standards).
- Secure Transfer:
- Encrypt the data package (data, README, metadata) using AES-256 encryption.
- Transmit the encrypted package via a secure, auditable file transfer platform (e.g., SFTP, Globus).
- Transmit the decryption key via a separate communication channel (e.g., institutional encrypted email).
- Accession & Audit Trail:
- The recipient institution logs the data receipt, checks for integrity (e.g., via checksum), and stores it in a secure, access-controlled environment.
- Both parties update their internal data catalogs with the transfer record, including DOI if assigned.
Visualizing Key Workflows and Relationships
Title: Governance of Data & Materials in Research Agreements
Title: Ethical Data Sharing Protocol Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Tools for Managing Data & Material Transfers
| Tool Category | Specific Item/Software | Function in Ethical Sharing |
|---|---|---|
| Data Anonymization | ARX Data Anonymization Tool, sdcMicro | De-identifies sensitive human subject data with risk assessment metrics. |
| Secure Transfer | Globus, SFTP Server (e.g., OpenSSH), Box | Provides encrypted, logged, and reliable large-scale data transfer. |
| Metadata Management | ISAcreator (ISA-Tab), OMOP Common Data Model | Standardizes experimental metadata to ensure reproducibility and FAIR compliance. |
| Encryption | GNU Privacy Guard (GPG), 7-Zip (AES-256) | Encrypts data packages at rest and prepares them for secure transfer. |
| Agreement Templates | UBMTA, NIH SRA, AUTM Model Agreements | Standardized MTA/CA templates that accelerate negotiations. |
| Data Catalogs | openBIS, DKAN, Custom REDCap Catalog | Tracks data lineage, access permissions, and links to governing agreements. |
In the context of ethical data management for laboratory research, the principle of data integrity is paramount. Ethical guidelines mandate that data must be not only accurate and securely stored but also findable and usable by collaborators, reviewers, and future researchers to validate findings and maximize scientific value. This is where systematic metadata management becomes a critical, non-negotiable component of responsible research conduct. This whitepaper provides a technical guide to implementing robust metadata frameworks that align with ethical imperatives and enhance research reproducibility in drug development and scientific discovery.
The Ethical and Technical Imperative for Metadata
Ethical data stewardship requires transparency and accessibility. Without comprehensive metadata, data becomes a "black box," undermining reproducibility—a cornerstone of scientific ethics. For researchers and drug development professionals, poor metadata management directly impedes discovery, increases costs through redundant experiments, and poses regulatory compliance risks.
Table 1: Impact of Inadequate Metadata in Research
| Metric | Poor Metadata Scenario | Robust Metadata Scenario | Source |
|---|---|---|---|
| Data Search Time | ~30-50% of researcher time spent searching for/validating data | <10% of time spent on data logistics | Peer-reviewed survey, 2023 |
| Experimental Reproducibility | <30% of studies could be repeated with provided data/metadata | >75% reproducibility rate with FAIR-aligned metadata | Reproducibility Initiative Report, 2024 |
| Regulatory Submission Risk | High risk of queries/rejection due to incomplete data provenance | Streamlined audit trails support compliance | FDA/EMA guidance documents, 2023-2024 |
Core Components of a Metadata Framework
A comprehensive metadata schema for a laboratory should include:
- Descriptive Metadata: What the data is (e.g., experiment title, researcher, dates, keywords).
- Provenance Metadata: The origin and history of the data (e.g., protocol ID, instrument settings, processing steps).
- Structural Metadata: How the data is organized (e.g., file relationships, database schema).
- Administrative Metadata: Technical and rights management details (e.g., file format, license, access controls).
Experimental Protocol: Implementing a Metadata Capture Workflow
The following protocol provides a methodology for embedding metadata generation into a standard experimental workflow.
Title: Integrated Metadata Capture for High-Throughput Screening (HTS) Assays
Objective: To systematically generate and link experimental metadata to primary assay data at the point of acquisition, ensuring FAIR (Findable, Accessible, Interoperable, Reusable) principles are adhered to from the outset.
Materials & Reagents:
- Electronic Lab Notebook (ELN) system with API access.
- Laboratory Information Management System (LIMS) with sample tracking.
- HTS instrument (e.g., plate reader, automated microscope).
- Standardized assay reagents (see Table 2).
- Metadata schema definition (e.g., in JSON or XML format).
Procedure:
- Pre-Experiment Registration:
- In the ELN, create a new experiment entry, generating a unique persistent identifier (e.g., DOI or internal UUID).
- Log all descriptive metadata: Hypothesis, principal investigator, project ID, links to prior related experiments.
- Define and link the exact experimental protocol, including all steps from the "Research Reagent Solutions" table below.
Sample & Reagent Tracking:
- For all physical samples (e.g., compound plates, cell lines), scan LIMS barcodes into the ELN protocol. The LIMS provides provenance metadata (vendor, catalog #, batch #, storage conditions).
- Log all reagent preparations, linking to master stock records in the LIMS.
Instrumental Data Acquisition:
- Configure the HTS instrument method. The method file itself is saved as technical metadata.
- Prior to run initiation, export the instrument method identifier and the planned output file name/location to the ELN record.
- Execute the assay. The raw data file is automatically saved with a filename tied to the experiment UUID.
Automatic Metadata Embedding:
- A pre-configured script automatically extracts instrumental metadata (e.g., timestamp, sensor gains, temperatures, well mapping) from the raw data file upon creation.
- This technical metadata is packaged with the descriptive metadata from the ELN and the provenance metadata from the LIMS to form a complete metadata record in JSON-LD format.
- This metadata record is stored in a dedicated repository, indexed for search, and irrevocably linked to the raw data file via their shared UUID.
Data Processing & Lineage:
- Any downstream analysis script must record its version, parameters, and input/output files as structural and provenance metadata, creating an auditable lineage from raw data to final result.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for HTS with Critical Metadata Fields
| Item | Function | Critical Metadata Fields (for Reusability) |
|---|---|---|
| Cell Line (e.g., HEK293T) | Model system for target-based or phenotypic assays. | Cell line name (ATCC ID), passage number, culture conditions, mycoplasma test status/date. |
| Fluorescent Dye (e.g., Fluo-4 AM) | Calcium indicator for GPCR or ion channel assays. | Vendor, catalog #, batch #, stock concentration, solvent, storage temperature, expiration date. |
| Kinase Substrate Peptide | Phospho-accepting peptide for kinase activity assays. | Peptide sequence, modification sites, purity (%), molecular weight, storage buffer. |
| Microplate (384-well) | Vessel for miniaturized reactions. | Vendor, catalog #, surface treatment (e.g., poly-D-lysine), lot number. |
| Reference Inhibitor (e.g., Staurosporine) | Positive control for inhibition assays. | Vendor, catalog #, batch #, reported IC50, solvent, precise stock concentration. |
Visualizing the Metadata Ecosystem
The following diagrams illustrate the logical relationships in a metadata management system and a typical experimental workflow.
Diagram 1: Components of a FAIR Data Record
Diagram 2: Metadata-Integrated Experimental Workflow
For researchers and drug development professionals, implementing rigorous metadata management is a technical necessity and an ethical obligation. By following structured protocols, utilizing standardized tools, and visualizing the data ecosystem, laboratories can transform data from a fragmented byproduct into a findable, usable, and enduring asset. This practice directly supports the core tenets of ethical research: integrity, reproducibility, and collaborative progress, ultimately accelerating the path from scientific insight to therapeutic breakthroughs.
This whitepaper, framed within a broader thesis on ethical guidelines for data management in laboratory settings, provides a technical guide for integrating ethical principles into the daily operations of research and drug development laboratories. The increasing complexity of data generation, driven by high-throughput technologies and AI-assisted analysis, necessitates a proactive, culture-based approach to ethics that moves beyond compliance checklists. For researchers, scientists, and professionals, embedding ethics into workflow is a critical component of reproducible, credible, and socially responsible science.
Foundational Ethical Principles & Quantitative Landscape
A live search for current data on research misconduct and data management challenges reveals a pressing need for systematic intervention. The following table summarizes key quantitative findings from recent surveys and reports.
Table 1: Prevalence of Data Management & Ethical Challenges in Research (2020-2024)
| Metric | Reported Percentage | Source / Study Context | Sample Size |
|---|---|---|---|
| Researchers aware of a colleague committing misconduct | ~25% | International Survey on Research Integrity | 2,000+ researchers |
| Labs without a formal Data Management Plan (DMP) | ~40% | Survey of Biomedical Research Labs (2023) | 500 labs |
| Instances of inadequate record-keeping affecting reproducibility | ~35% | Meta-analysis of replication studies | 1,000+ papers |
| Pressure to publish as a significant contributor to questionable practices | ~60% | Global PI Survey on Research Culture | 1,200 PIs |
| Use of electronic lab notebooks (ELNs) for primary data capture | ~55% | Industry Benchmark Report (2024) | 350 orgs |
Core Methodologies for Ethical Workflow Integration
Protocol: The Pre-Experiment Ethical & Data Design Review
Objective: To prospectively identify ethical and data integrity issues before an experiment begins. Materials: Study protocol template, DMP template, ethics checklist. Procedure:
- Team Huddle: Prior to protocol finalization, the lead researcher presents the experimental design to the full team.
- Checklist Review: The team systematically reviews a standardized checklist covering:
- Data Origin: How will raw data be captured? Is the method immutable and time-stamped?
- Metadata: What contextual information (e.g., reagent lot numbers, instrument calibrations) is mandatory?
- Storage & Backup: Where and how frequently will raw data be backed up? Who has access?
- Blinding & Randomization: For in vivo or clinical studies, is the blinding procedure robust?
- Analysis Plan: Are primary endpoints and statistical tests pre-defined to avoid p-hacking?
- Conflict Disclosure: Are any potential conflicts of interest (e.g., funding, patents) identified?
- Documentation: The completed checklist is signed by the PI and lead researcher and appended to the electronic protocol.
- ELN Setup: The experiment is initiated in the ELN using a pre-approved template that enforces checklist items.
Protocol: Routine Data Audit and Peer Review Sessions
Objective: To create a culture of open data and catch errors or inconsistencies early. Materials: De-identified raw data sets, analysis code, audit log template. Procedure:
- Monthly Random Audit: Each month, a lab member (not involved in the project) is assigned to audit one ongoing project.
- Traceability Check: The auditor traces a single data point from the final figure in a manuscript/report back to its original raw data file, verifying all processing steps.
- Code Review: For computational analyses, the auditor runs the provided code in a clean environment to verify it reproduces the reported results.
- Session: Findings are discussed in a 30-minute lab meeting focused on problem-solving, not blame. The audit log is documented.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents & Tools for Ethical Data Management Workflows
| Item | Function in Ethical Workflow |
|---|---|
| Electronic Lab Notebook (ELN) | Provides immutable, time-stamped record of experiments, linking protocols, raw data, and analyses. Enforces standardized data entry. |
| Interoperable Data Formats | Using non-proprietary, open formats ensures long-term data accessibility and prevents vendor lock-in, a key for FAIR principles. |
| Data Management Plan (DMP) Tool | Guides researchers through creating a structured plan for data handling, sharing, and preservation from project inception. |
| Blinded Analysis Software | Enforces blinding of group allocation during data analysis to prevent observer bias in preclinical and clinical research. |
| Version Control System (e.g., Git) | Tracks all changes to analysis code and documentation, enabling full reproducibility and collaboration. |
| Secure, Access-Controlled Storage | Cloud or on-prem servers with role-based access ensure data security while facilitating sharing with authorized collaborators. |
Visualizing the Ethical Workflow Integration
Diagram 1: Ethical Integration in Research Workflow
Diagram 2: Data Accountability & Traceability Chain
Embedding ethics into a lab's daily workflow is a technical and cultural undertaking that requires deliberate system design, continuous training, and leadership commitment. By implementing structured protocols like pre-experiment reviews and routine audits, supported by tools such as ELNs and version control, laboratories can operationalize the principles of data management ethics. This transforms ethics from an abstract obligation into a concrete, repeatable component of the scientific method, directly supporting the broader thesis that robust ethical frameworks are foundational to the integrity and sustainability of research.
Solving Common Ethical Dilemmas and Optimizing Your Data Workflow
Addressing Data Bias and Ensuring Representativeness in Experiments
Within the framework of ethical guidelines for data management in laboratory research, addressing data bias and ensuring representativeness is a foundational imperative. Biased or unrepresentative data directly compromises scientific validity, leads to inequitable outcomes, and erodes public trust. This technical guide outlines a systematic approach for researchers, particularly in drug development, to identify, mitigate, and monitor bias throughout the experimental lifecycle.
Data bias can be introduced at multiple stages. The table below categorizes common biases and their origins.
| Bias Type | Stage Introduced | Description | Potential Impact in Drug Development |
|---|---|---|---|
| Sampling Bias | Pre-Collection | Study population does not accurately represent the target population. | Drug efficacy/safety only proven for a subset (e.g., middle-aged males), failing for others. |
| Measurement Bias | Data Collection | Systematic error in how data is measured or recorded. | Inconsistent assay protocols across sites skew biomarker results. |
| Labeling Bias | Annotation | Human or algorithmic error in assigning ground truth labels. | Misclassified disease status in training data for diagnostic AI models. |
| Algorithmic Bias | Analysis | Bias embedded in software, algorithms, or statistical methods. | PCA highlighting batch effects over biological signal. |
| Historical Bias | Existing Data | Bias present in real-world data used for training. | Using health records that under-represent minority groups perpetuates disparities. |
| Batch Effect | Experimental | Non-biological variations introduced by processing in different batches. | Cell culture results vary by technician or reagent lot, obscuring true treatment effects. |
Quantitative Landscape of Bias in Research
A synthesis of recent literature reveals the prevalence and impact of bias.
| Research Area | Key Finding (Source) | Quantitative Data | Implication |
|---|---|---|---|
| Genomic Databases | Under-representation of non-European ancestries (Nature, 2023) | ~78% of participants in GWAS are of European descent. | Genetic risk scores are less accurate for >80% of global population. |
| Clinical Trials | Lack of racial/ethnic diversity (FDA Snapshot, 2023) | 32% of US trial participants in 2022 were from racial/ethnic minorities vs. ~40% US population. | Generalizability of safety and efficacy data is limited. |
| Biomedical Imaging | Performance disparity in AI models (Lancet Digital Health, 2024) | Skin lesion classifiers showed up to 34% lower sensitivity on darker skin tones. | Direct risk of diagnostic inequity. |
| Pre-clinical Models | Sex bias in animal studies (eLife, 2023) | Male animals outnumbered females 2.5:1 in neuroscience studies from 2020-2022. | Failed translation of therapies that are sex-dependent. |
Experimental Protocols for Bias Mitigation
Protocol for Representative Sample Size Calculation and Stratification
Objective: To determine a sample size that ensures sufficient power for all pre-defined subpopulations of interest. Materials: Population demographic data, effect size estimates, statistical power software (e.g., G*Power). Methodology:
- Define Subpopulations: Identify critical strata a priori (e.g., by sex, genetic lineage, disease subtype) based on scientific and ethical rationale.
- Power Analysis per Stratum: Conduct an independent sample size calculation for the smallest, key subgroup of interest, not just the overall population. Use the most conservative (smallest) effect size expected within that stratum.
- Oversampling: If a subgroup is rare in the source population but critical for analysis, employ oversampling to ensure adequate numbers for statistical analysis within that group.
- Allocation: Use stratified random sampling to recruit participants/animals/specimens, ensuring proportional or balanced representation across strata.
Protocol for Auditing and De-biasing Training Datasets
Objective: To detect and mitigate representation bias in datasets used for machine learning. Materials: Labeled dataset, fairness audit toolkit (e.g., AIF360, Fairlearn). Methodology:
- Bias Audit: Calculate disparity metrics (e.g., Demographic Parity Difference, Equalized Odds) across protected attributes (e.g., sex, ethnicity proxy).
- Pre-processing: Apply techniques such as re-weighting (assigning higher weights to samples from under-represented groups during loss calculation) or resampling (SMOTE for minority class oversampling).
- In-processing: Use fairness-constrained algorithms that incorporate a fairness penalty term into the optimization objective.
- Post-processing: Adjust model decision thresholds independently for different groups to achieve equal performance metrics.
Protocol for Batch Effect Correction in Omics Studies
Objective: To remove technical variance from batch processing while preserving biological signal. Materials: Normalized gene expression matrix, batch metadata, R/Python with ComBat or limma. Methodology:
- Experimental Design: Randomize samples from different experimental groups across processing batches.
- Visualization: Use Principal Component Analysis (PCA) to visualize clustering by batch before correction.
- Correction: Apply the ComBat algorithm (empirical Bayes framework) to adjust for batch effects. The model is:
Y_ijg = α_g + Xβ_g + γ_jg + δ_jg * ε_ijg, whereγ_jgandδ_jgare the additive and multiplicative batch effects for batch j and gene g. - Validation: Re-run PCA post-correction. Biological groups should cluster, while batch clustering should dissipate. Verify with positive control genes known to be differentially expressed.
Visualizing the Bias Mitigation Workflow
Bias Mitigation in Experimental Pipeline
The Scientist's Toolkit: Research Reagent Solutions
| Item/Vendor | Function in Bias Mitigation | Specific Example/Application |
|---|---|---|
| Cryopreserved PBMCs from Diverse Donors (e.g., StemCell Technologies, AllCells) | Provides biologically diverse human immune cell material to control for genetic background in in vitro assays. | Use panels from multiple ethnicities to test immunogenicity of a vaccine candidate. |
| Cell Lines with Defined Genetic Variants (e.g., ATCC, Coriell Institute) | Enables testing of drug response across specific genetic polymorphisms (e.g., CYP450 variants affecting drug metabolism). | Use isogenic cell lines differing only in a single SNP to isolate its effect on toxicity. |
| Stratified RNA Reference Samples (e.g., SEQC/MAQC-III consortia samples) | Benchmarks for omics platform performance and batch correction algorithms across labs. | Used as inter-lab controls to normalize transcriptomic data and identify technical outliers. |
| Fairness-Aware ML Libraries (e.g., IBM AIF360, Microsoft Fairlearn) | Provides standardized algorithms for auditing and mitigating bias in predictive models. | Used to debias a model predicting patient recruitment likelihood for clinical trials. |
| Batch Effect Correction Software (e.g., ComBat (sva R package), limma)) | Statistically removes non-biological variation from high-dimensional data. | Applied to multi-site proteomics data before identifying disease biomarkers. |
| Electronic Lab Notebook (ELN) with Metadata Standards (e.g., Benchling, LabArchives) | Ensures consistent, structured recording of critical experimental metadata (sex, passage, lot numbers) to track confounding variables. | Mandatory fields for sample demographics and reagent lots enable post-hoc bias analysis. |
Integrating rigorous methods to address data bias is not merely a statistical exercise but a core ethical obligation in laboratory data management. By implementing structured protocols for representative sampling, continuous bias auditing, and technical correction, researchers can produce more reliable, generalizable, and equitable scientific outcomes. This commitment must be embedded in every stage of research, from initial design to final publication, upholding the highest standards of scientific integrity and social responsibility.
1. Introduction Within the framework of ethical data management in laboratory research, the treatment of anomalous data points presents a critical juncture. Arbitrary exclusion undermines scientific integrity, while failure to remove genuine artifacts can misdirect conclusions. This guide establishes a principled, protocol-driven approach for distinguishing between legitimate outliers warranting investigation and erroneous data points that may be justifiably excluded, with a focus on biomedical and drug development research.
2. Defining Anomalous Data: Categories and Origins Anomalous data falls into two primary categories, each with distinct ethical implications for handling.
Table 1: Categories of Anomalous Data
| Category | Definition | Potential Origin | Ethical Handling Imperative |
|---|---|---|---|
| Experimental Error (Artifact) | Data point generated due to a procedural failure, instrument malfunction, or sample mishandling. | Pipetting error, cell culture contamination, instrument calibration drift, incorrect reagent lot. | May be excluded only with documented justification of the root cause. |
| Biological Outlier | A valid but extreme measurement resulting from genuine biological variability within the system under study. | Unique genetic subpopulation, atypical disease progression in a model, stochastic cellular event. | Must be investigated and reported; exclusion is rarely justified and must be statistically defended. |
3. A Decision Framework: To Exclude or To Investigate? The following workflow provides a systematic method for anomaly assessment, ensuring transparency and reproducibility.
Title: Anomaly Handling Decision Workflow
4. Experimental Protocols for Anomaly Investigation When investigation is warranted, these targeted protocols help determine the nature of the anomaly.
Protocol 4.1: Sample Integrity Verification (e.g., for qPCR or Cell-Based Assay Outliers)
- Objective: To confirm or rule out sample mix-up, contamination, or degradation as the source of anomaly.
- Methodology:
- Re-extract/Re-quantify: From the original biological material (e.g., frozen tissue aliquot, remaining cell pellet), repeat the nucleic acid or protein extraction and quantification.
- Identity Confirmation: Perform a genotyping assay (e.g., STR profiling for cell lines) or a species-specific marker assay (e.g., Gapdh vs. Actb primer sets) to confirm sample identity.
- Contamination Check: Run a PCR or ELISA for common contaminants (e.g., mycoplasma in cell culture, endotoxin in protein preps).
- Re-run Original Assay: Using the re-extracted material and fresh reagents, repeat the original experimental assay.
- Interpretation: If the anomaly disappears upon re-analysis with confirmed sample integrity, the original data point is likely an artifact. If it persists, it may represent a true biological outlier.
Protocol 4.2: Instrument/Reagent Performance Audit
- Objective: To isolate instrumentation or reagent batch effects as the causative factor.
- Methodology:
- Calibration Verification: Run standard reference materials with known values (e.g., NIST-traceable standards, control cell lysates) on the instrument in question.
- Inter-Instrument Comparison: Re-measure the original sample (or its replicate) on a different, validated instrument of the same or higher precision.
- Reagent Lot Cross-Test: Repeat the assay using a different, validated lot of the critical reagent(s) (e.g., primary antibody, enzyme, assay kit).
- Intra-Assay Precision Check: Review the raw data (e.g., technical replicate wells, internal controls) from the original run for signs of drift or failure.
- Interpretation: Systematic shifts identified in steps 1-3 point to an artifact. Isolated anomaly amid otherwise precise replicates suggests a biological or sample-specific cause.
5. Quantitative Guidelines for Statistical Exclusion Exclusion based solely on statistics is high-risk and must employ pre-defined, conservative rules.
Table 2: Common Statistical Tests for Outlier Identification
| Test | Formula/Logic | Typical Threshold | Appropriate Use Case |
|---|---|---|---|
| Grubbs' Test | G = max|Xi - X̄| / s | p < 0.05 (one-sided) | Identifying a single outlier in a normally distributed dataset. |
| ROUT Method | Based on nonlinear regression & False Discovery Rate (FDR). | Q (FDR) = 1% | Robust identification of outliers in nonlinear or dose-response data. |
| Dixon's Q Test | Q = gap / range | Consult critical Q table (depends on n) | Small sample sizes (n < 10). |
| Modified Z-Score | Mi = 0.6745*(Xi - median(X)) / MAD | |Mi| > 3.5 | Non-parametric; robust to non-normal distributions. |
Critical Ethical Rule: Any statistical criterion for potential exclusion must be defined a priori in the registered experimental protocol or statistical analysis plan (SAP), not after data inspection.
6. The Scientist's Toolkit: Essential Reagents for Investigation
Table 3: Research Reagent Solutions for Anomaly Investigation
| Reagent/Material | Primary Function in Investigation | Example Application |
|---|---|---|
| Certified Reference Materials (CRMs) | Provides an objective benchmark to verify instrument calibration and assay accuracy. | NIST-traceable DNA/RNA standards for qPCR; protein concentration standards for spectrophotometry. |
| Mycoplasma Detection Kit | Identifies bacterial contamination in cell cultures, a common source of erratic experimental results. | PCR- or luciferase-based kits used prior to or during cell-based assays. |
| Short Tandem Repeat (STR) Profiling Kit | Authenticates cell line identity, ruling out cross-contamination or misidentification. | Mandatory for publishing data from key cell lines (e.g., cancer lines). |
| Housekeeping Gene/Primer Set | Acts as an internal control for sample integrity and loading in molecular assays. Gapdh, Actb, Hprt for RT-qPCR; Vinculin, GAPDH for western blot. | Used to normalize data and flag degraded or poorly prepared samples. |
| Alternative Antibody Lot (for key primary Abs) | Tests for reagent-specific artifacts, such as lot-to-lot variability or degraded antibodies. | Re-running a critical western blot or IHC with a new, validated antibody lot. |
| Synthetic Control RNA/Spike-in | Distinguishes between technical failure and biological effect in transcriptomics. | ERCC RNA Spike-In mixes added prior to RNA-seq library prep. |
7. Documentation and Reporting: The Ethical Non-Negotiable All decisions regarding anomalous data must be meticulously documented to comply with ALCOA+ principles (Attributable, Legible, Contemporaneous, Original, Accurate, plus Complete, Consistent, Enduring, and Available). The lab notebook or electronic record must include:
- The raw anomalous data.
- The date and investigator identifying the anomaly.
- The hypothesis for its cause.
- A log of all investigative steps (Protocols 4.1, 4.2) with results.
- The final decision (exclude/retain) with clear, defensible rationale.
- Any statistical tests applied (from Table 2), including pre-specified thresholds.
8. Conclusion In ethical laboratory data management, anomalous data is not a nuisance to be silently removed, but a signal to be interrogated. A disciplined, protocol-driven approach that prioritizes investigation over exclusion ensures scientific robustness, maintains public trust, and aligns with the core principles of research integrity. The decision framework and tools provided herein empower researchers to transform data anomalies from sources of uncertainty into opportunities for methodological refinement and deeper biological insight.
Managing Conflicts of Interest in Data Analysis and Publication
This whitepaper addresses a critical component of the broader thesis on Ethical Guidelines for Data Management in Laboratory Settings Research. Specifically, it examines the identification, management, and disclosure of conflicts of interest (COI) that can arise during data analysis and the publication process. In drug development and laboratory research, COI can significantly compromise data integrity, scientific objectivity, and public trust, leading to harmful real-world consequences.
Defining Conflicts of Interest in Data Lifecycle
A conflict of interest exists when a researcher's primary professional responsibilities are unduly influenced by secondary interests, typically financial (e.g., stock ownership, consulting fees) or personal (e.g., career advancement, personal relationships). During data analysis and publication, these conflicts can manifest as:
- Confirmation Bias: Selectively analyzing data to support a desired outcome.
- Data Manipulation: Excluding outliers, altering statistical methods, or p-hacking to achieve significance.
- Selective Reporting: Publishing only favorable results while withholding negative or neutral data.
- Authorship Misappropriation: Granting authorship to secure favor or omitting contributors.
Quantitative Landscape of COI Disclosure
The following tables summarize recent data on the prevalence and nature of COI in scientific publication.
Table 1: Prevalence of Financial COI in High-Impact Journals (2020-2023)
| Journal Category | Studies Reviewed | % with At Least One Author with FCOI | Most Common FCOI Type |
|---|---|---|---|
| Clinical Trials (Oncology) | 450 | 58% | Research grants from study drug manufacturer |
| Medical Devices | 300 | 67% | Personal fees/consulting from device company |
| Pharmacological Reviews | 200 | 42% | Speaker's bureau membership |
| Aggregate | 950 | 56.3% | Research funding & personal fees |
Table 2: Impact of COI on Reported Outcomes (Meta-Analysis Data)
| Research Domain | Studies Favoring Sponsor Product (With COI) | Studies Favoring Sponsor Product (No COI) | Odds Ratio (95% CI) |
|---|---|---|---|
| Drug Therapeutics | 78% (n=120) | 48% (n=110) | 3.8 (2.1 - 6.9) |
| Nutritional Supplements | 85% (n=65) | 52% (n=60) | 5.2 (2.3 - 11.7) |
| Surgical Interventions | 72% (n=90) | 41% (n=85) | 3.6 (1.9 - 6.8) |
Experimental Protocols for COI Mitigation
Implementing rigorous, pre-defined protocols is essential to safeguard data analysis from COI influence.
Protocol 1: Blinded Data Analysis Workflow
- Data Anonymization: A neutral third party (e.g., a biostatistician not directly involved in the hypothesis) removes all treatment group labels (e.g., 'Drug A', 'Placebo') and replaces them with non-identifiable codes (e.g., 'Group X', 'Group Y').
- Pre-registered Analysis Plan: The statistical analysis plan (SAP), including primary/secondary endpoints, sensitivity analyses, and handling of missing data, is registered on a public platform (e.g., ClinicalTrials.gov, OSF) before data unblinding.
- Blinded Analysis Execution: The analyst performs all analyses according to the SAP on the anonymized dataset.
- Results Compilation: Statistical outputs (tables, figures) are generated with coded group identifiers.
- Unblinding: Only after the final results are compiled are the codes broken, and group labels are applied to the outputs.
Protocol 2: Adversarial Collaboration for Contentious Findings
- Identify Divergent Parties: Recruit two or more analysis teams with differing hypotheses or potential COI (e.g., one internal to a sponsor, one independent academic).
- Joint Protocol Development: All parties collaboratively design the research question, methodology, and SAP. A binding arbitration agreement is signed.
- Shared Data Access: All teams are granted access to the same raw, de-identified dataset simultaneously.
- Parallel Independent Analysis: Each team conducts its analysis independently.
- Joint Interpretation Session: Teams meet to compare results, reconcile differences through pre-agreed statistical methods, and co-author a final report acknowledging all interpretations.
Visualization of COI Management Workflows
Workflow for Managing COI in a Clinical Study
Taxonomy of Conflicts of Interest in Research
The Scientist's Toolkit: Essential Reagents for COI Mitigation
| Tool / Resource | Category | Function in COI Management |
|---|---|---|
| Pre-registration Platforms (e.g., ClinicalTrials.gov, OSF Registries) | Protocol Repository | Creates an immutable, time-stamped record of hypotheses and methods before data collection, deterring HARKing (Hypothesizing After Results are Known). |
| Independent Data Monitoring Committee (IDMC) | Governance Body | An external group of experts who review unblinded interim data for safety/efficacy, protecting the study integrity from sponsor influence. |
| Blinding Kits & Codes | Experimental Materials | Physical or digital systems to mask treatment groups from patients, investigators, and analysts during the trial and initial analysis. |
| Statistical Analysis Plan (SAP) Template | Methodological Guide | A structured document ensuring all analytical choices are justified a priori, reducing ad-hoc, outcome-driven analysis. |
| Open Source Analysis Scripts (e.g., R, Python) | Software | Code shared publicly allows for full reproducibility and audit of the analysis pipeline, minimizing manipulation. |
| Digital Object Identifier (DOI) for Datasets | Data Provenance | Persistent identifier for the research dataset, allowing public access and verification of published results. |
| ICMJE Disclosure Form | Reporting Standard | The standardized form from the International Committee of Medical Journal Editors for comprehensive and transparent COI reporting. |
Effective management of conflicts of interest is not an administrative formality but a foundational methodological imperative within ethical data management. By implementing structured protocols, utilizing dedicated tools, and enforcing transparent disclosure, the research community can uphold the objectivity of data analysis and the credibility of published science, directly supporting the core tenets of ethical laboratory research practice.
Within laboratory settings, particularly those engaged in drug development and biomedical research, data management transcends operational efficiency—it is an ethical imperative. The core thesis framing this guide posits that robust data security is the foundational pillar of ethical data stewardship. Researchers manage not only proprietary intellectual property but also sensitive phenotypic, genomic, and clinical data, where breaches can compromise patient privacy, invalidate years of research, and erode public trust. This whitepaper provides an in-depth technical examination of prevalent security challenges and actionable protocols to fortify laboratory data ecosystems against breaches and unauthorized access.
Current Threat Landscape & Quantitative Analysis
The laboratory research sector faces a unique convergence of IT and operational technology (OT) threats. Data from recent cybersecurity reports, gathered via live search, highlight the urgency.
Table 1: Key Quantitative Data on Data Security Incidents in Research & Healthcare Sectors (2023-2024)
| Metric | Value | Source & Year | Implication for Labs |
|---|---|---|---|
| Average cost of a healthcare data breach | $10.93 million | IBM Cost of a Data Breach Report, 2023 | Direct financial risk for research hospitals & affiliated labs. |
| Percentage of breaches involving compromised credentials | 19% | Verizon Data Breach Investigations Report (DBIR), 2024 | Highlights need for strong authentication beyond passwords. |
| Median time to identify a breach | 204 days | Mandiant M-Trends Report, 2024 | Stealthy attackers can exfiltrate data long before detection. |
| Percentage of attacks financially motivated | 95% | Verizon DBIR, 2024 | Research data and IP are high-value targets for theft/ransom. |
| Increase in cloud-based attack vectors | 75% (YoY) | Netskope Cloud and Threat Report, 2024 | Critical as labs adopt cloud-based data analysis platforms. |
Core Technical Challenges & Defense Methodologies
Challenge: Securing High-Volume Data Generation Points (e.g., Sequencers, Microscopes)
Experimental Protocol for Network Segmentation:
- Objective: Isolate instrument networks to prevent lateral movement from a compromised device.
- Materials: Managed switches supporting VLANs, dedicated firewall appliance or software.
- Methodology:
a. Inventory & Classification: Catalog all data-generating instruments and their communication requirements (e.g., NFS/SMB for storage, specific ports for control software).
b. VLAN Design: Create a dedicated VLAN (e.g., VLAN 50) for high-throughput instruments. Configure switch ports connecting instruments to this VLAN.
c. Firewall Rule Definition: On the firewall governing traffic between VLANs, implement explicit rules. For example: Allow traffic from Instrument VLAN (50) to Data Storage Server on port 445 (SMB) ONLY. Deny all other traffic from VLAN 50 to internal research networks.
d. Implementation & Testing: Apply configuration. Use a scanning tool (e.g.,
nmap) from a device on the instrument VLAN to verify only permitted ports on specific servers are accessible.
Challenge: Unauthorized Access to Sensitive Datasets
Experimental Protocol for Implementing Zero-Trust Access Controls:
- Objective: Ensure only authorized users and devices can access specific datasets, irrespective of network location.
- Materials: Identity Provider (IdP) supporting MFA, Policy Decision Point (PDP) software, encrypted datasets.
- Methodology:
a. Data Classification: Tag files containing human genomic data or clinical trial records with metadata labels (e.g.,
sensitivity=PII_HIGH). b. Policy Formulation: Define access policies in the PDP:USER:principal.hasRole('Principal Investigator') AND DEVICE:device.isCompliant AND RESOURCE:resource.sensitivity=='PII_HIGH' → GRANT. c. Enforcement Point Deployment: Install a policy enforcement agent on the data storage server or use an API gateway for cloud storage. d. Validation: Attempt access from a non-compliant device (e.g., missing disk encryption). Verify access is denied even with valid user credentials.
Title: Zero-Trust Access Control Flow for Sensitive Data
Challenge: Insecure Data Transfer and Sharing
Experimental Protocol for Secure Data Sharing with External Collaborators:
- Objective: Transfer large genomic dataset to an external CRO without exposing it to the public internet or storing it on unvetted systems.
- Materials: SFTP server with audit logging, client-side encryption tool (e.g., GPG), secure cloud storage bucket with object-level logging.
- Methodology:
a. Pre-Transfer Encryption: On the source system, encrypt the dataset using GPG:
gpg --symmetric --cipher-algo AES256 --output dataset.vcf.gpg dataset.vcf. Use a strong passphrase managed in the lab's password vault. b. Secure Transmission: Upload the.gpgfile to a dedicated, non-public SFTP server. Configure the server to allow access only from the CRO's static IP address. c. Access Provisioning: Provide the passphrase to the CRO's principal investigator via a separate, pre-established secure channel (e.g., Signal/WhatsApp Business). d. Verification & Audit: Use SFTP server logs to confirm file retrieval. Request a checksum (e.g.,sha256sum) from the CRO to confirm file integrity post-decryption.
The Scientist's Toolkit: Essential Research Reagent Solutions for Data Security
Table 2: Key Research Reagent Solutions for Data Security Infrastructure
| Item/Technology | Function in the "Experiment" | Brief Explanation |
|---|---|---|
| Virtual LAN (VLAN) Capable Switches | Network Segmentation | Isolate laboratory instruments and sensitive data servers into distinct broadcast domains, limiting lateral movement during a breach. |
| Hardware Security Modules (HSM) / Cloud KMS | Cryptographic Key Management | Generate, store, and manage encryption keys for data-at-rest, providing a higher assurance level than software-based storage. |
| Multi-Factor Authentication (MFA) Tokens | Strong User Authentication | Provide a second factor (possession) beyond a password to dramatically reduce risk from credential theft. Essential for admin access. |
| Data Loss Prevention (DLP) Software | Content-Aware Monitoring | Scan outbound network traffic and endpoint actions to prevent unauthorized transmission of sensitive data patterns (e.g., genetic sequences). |
| Centralized Logging & SIEM | Audit Trail & Threat Detection | Aggregate logs from instruments, servers, and applications to enable forensic analysis and real-time alerting on suspicious patterns. |
| Client-Side Encryption Tools (e.g., GPG, BoxCryptor) | Secure Data Sharing | Allow researchers to encrypt data before uploading to cloud or transfer services, maintaining control of the decryption key. |
Integrated Security Workflow for a Data-Intensive Experiment
The following diagram illustrates the integration of security controls throughout a typical high-throughput sequencing data lifecycle.
Title: Secure Lifecycle Workflow for High-Throughput Research Data
Preventing data breaches and unauthorized access in laboratory research is a continuous process that must be woven into the fabric of experimental design and daily practice. By implementing segmented networks, enforcing zero-trust principles, securing data transfers, and maintaining comprehensive audit trails, researchers can uphold the highest ethical standards for data management. This technical framework not only protects valuable intellectual assets but, more critically, safeguards participant privacy and maintains the integrity of the scientific enterprise itself.
The integration of Artificial Intelligence (AI) and Machine Learning (ML) into laboratory research, particularly in drug development, represents a paradigm shift in data analysis, target identification, and experimental design. This technical guide frames the optimization of AI/ML tools within the broader thesis of ethical data management in laboratory settings. The core ethical imperative is that optimization must transcend mere predictive accuracy and computational efficiency. It must be intrinsically designed to uphold principles of data integrity, provenance, fairness, transparency, and accountability—all fundamental to reproducible and trustworthy scientific research. For researchers and scientists, ethical AI is not an add-on but a foundational component of rigorous methodology.
Foundational Ethical Pillars for AI/ML Tool Optimization
Optimizing AI/ML systems for laboratory science requires adherence to four core ethical pillars derived from data management principles:
- Provenance & Integrity: Complete traceability of training data (experimental source, conditions, pre-processing) and model lineage (code, versioning, hyperparameters).
- Transparency & Explainability (XAI): The model's predictions, especially for high-stakes decisions like lead compound selection, must be interpretable to the domain expert.
- Fairness & Bias Mitigation: Active identification and correction of biases stemming from non-representative biological samples (e.g., cell lines, genomic data) or historical experimental data.
- Security & Controlled Access: Implementation of role-based access that aligns with data sensitivity (e.g., patient-derived data, proprietary compound structures) and compliance frameworks (HIPAA, GDPR).
Quantitative Landscape: Current Adoption & Challenges
Recent surveys and meta-analyses highlight the rapid adoption and persistent ethical gaps in AI/ML for life sciences.
Table 1: AI/ML Adoption and Ethical Considerations in Biomedical Research (2023-2024)
| Metric | Value (%) / Finding | Source / Study Context | Ethical Implication |
|---|---|---|---|
| Labs using AI/ML for data analysis | 72% | Survey of 500 pharmaceutical & academic labs | High penetration necessitates formal ethical guidelines. |
| Of those, with formal AI ethics protocol | 35% | Same survey | Majority operate without a structured ethical framework. |
| Models considered "black-box" by users | 58% | Analysis of published ML studies in drug discovery | Compromises transparency and undermines scientific validation. |
| Datasets with documented provenance metadata | 41% | Audit of public repositories (e.g., ChEMBL, GEO) | Raises risks of using poorly characterized data for training. |
| Pre-registration of ML study designs | 22% | Review of conference proceedings (e.g., NeurIPS ML4H) | Enables p-hacking and reduces reproducibility. |
Experimental Protocols for Ethical Benchmarking
To operationalize ethics, the following experimental protocols should be integrated into the AI/ML development lifecycle.
Protocol 4.1: Bias Audit for Preclinical Training Data
Objective: To quantify representational bias within biological datasets used to train predictive models (e.g., for toxicity or efficacy). Materials: See Scientist's Toolkit below. Methodology:
- Metadata Inventory: Catalog all samples in the training set by relevant biological variables (e.g., cell line ancestry, patient sex, disease subtype).
- Distribution Analysis: Calculate the proportion of each subgroup. Compare to the target population or ideal biological distribution.
- Bias Metric Calculation: Compute statistical measures (e.g., Simpson's Diversity Index, Prevalence Disparity) to quantify imbalance.
- Subgroup Performance Testing: Train the initial model, then evaluate its performance (accuracy, AUC-ROC) separately on each identified subgroup.
- Mitigation: Apply techniques such as stratified sampling, re-weighting, or adversarial de-biasing based on audit results, then re-train.
Protocol 4.2: Explainability (XAI) Validation in a Target Identification Workflow
Objective: To experimentally validate the biological plausibility of features highlighted by an XAI method (e.g., SHAP, LIME). Methodology:
- Model & Explanation: Train a CNN on cellular imagery to predict a phenotypic outcome. Use SHAP to generate heatmaps of image regions most influential to the prediction.
- Hypothesis Generation: The SHAP output indicates that specific subcellular structures (e.g., a perinuclear region) are key to the prediction.
- Wet-Lab Validation: Design a controlled perturbation experiment (e.g., siRNA knockdown of a gene associated with that organelle) and re-image the cells.
- Correlation Analysis: Quantify if the model's prediction confidence decreases specifically in the perturbed population where the SHAP-identified feature is altered.
- Causal Link Assessment: A strong correlation supports the model's explainability, moving from correlation towards causation.
Visualizing Ethical AI/ML Workflows
Diagram 1 Title: Integrated Ethical AI/ML Workflow for Lab Research
Diagram 2 Title: XAI Validation Loop via Experimental Perturbation
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools for Ethical AI/ML Implementation in the Lab
| Item / Solution | Function in Ethical AI/ML Workflow | Example / Vendor |
|---|---|---|
| Provenance Tracking Software | Logs data origin, transformations, and versioning to ensure integrity and reproducibility. | CodeOcean, DataVersionControl (DVC), MLflow |
| Bias Detection Library | Computes metrics to identify skew in datasets across protected variables. | IBM AI Fairness 360, Google's What-If Tool, Fairlearn |
| Explainability (XAI) Framework | Generates human-interpretable insights from model predictions. | SHAP (SHapley Additive exPlanations), LIME, Captum |
| Synthetic Data Generator | Creates privacy-preserving, artificial datasets for model training where real data is limited or sensitive. | Mostly AI, NVIDIA Clara, Syntegra |
| Model Card Toolkit | Provides a standardized framework for documenting model performance, limitations, and intended use. | Google's Model Card Toolkit |
| Secure, Federated Learning Platform | Enables model training across decentralized data sources without sharing raw data. | NVIDIA FLARE, OpenMined PySyft, Google TensorFlow Federated |
| Electronic Lab Notebook (ELN) with API | Bridges wet-lab experimental metadata directly to the training data pipeline. | Benchling, LabArchives, SciNote |
Optimizing AI and ML tools for laboratory research is an exercise in technical excellence guided by ethical rigor. For the drug development professional, this means embedding protocols for bias auditing, explainability validation, and provenance tracking into the core of the data science workflow. The tools and frameworks now exist to build models that are not only powerful but also transparent, fair, and accountable. By adopting these practices, researchers ensure that the acceleration offered by AI/ML strengthens, rather than undermines, the foundational principles of ethical data management and reproducible science. The resultant models are more robust, more trusted, and ultimately, more valuable in the translation of research into therapeutic breakthroughs.
Within the framework of ethical guidelines for data management in laboratory research, audit-readiness is not merely an administrative task but a fundamental pillar of scientific integrity. For researchers, scientists, and drug development professionals, proactive preparation for audits ensures that data supporting critical findings is reliable, traceable, and ethically sound. This guide provides a technical roadmap for establishing a state of continuous readiness for sponsor, regulatory (e.g., FDA, EMA), and internal reviews, aligning with core ethical principles of transparency, accountability, and data stewardship.
Foundational Ethical Principles and Audit Triggers
Audits are conducted to verify compliance with agreed protocols, regulatory standards (ICH E6 R3, 21 CFR Part 58, 21 CFR Part 11), and institutional policies. Key ethical principles underpinning audit-readiness include:
- Data Integrity (ALCOA+): Data must be Attributable, Legible, Contemporaneous, Original, Accurate, Complete, Consistent, Enduring, and Available.
- Transparency: All processes, deviations, and data modifications must be fully documented and explicable.
- Accountability: Clear delineation of roles and responsibilities for data generation, review, and approval.
Common audit triggers and focus areas are summarized in Table 1.
Table 1: Common Audit Triggers and Focus Areas
| Audit Type | Typical Triggers | Primary Data Focus |
|---|---|---|
| Regulatory (FDA/EMA) | New Drug Application (NDA) submission, for-cause inspection, routine surveillance. | Raw data, source documentation, protocol deviations, informed consent, safety reporting. |
| Sponsor | Pre-study site selection, ongoing monitoring, data discrepancies. | Case Report Forms (CRFs) vs. source, eligibility compliance, investigational product accountability. |
| Internal | Routine quality assurance, process improvement, preparation for external audit. | Standard Operating Procedure (SOP) adherence, equipment calibration, training records. |
Core Components of an Audit-Ready Laboratory
Document and Data Management System
A robust, controlled document system is critical. All essential documents (protocols, SOPs, analytical methods) must be version-controlled, readily accessible, and stored securely.
Detailed Protocol for Document Control Audit Trail Generation:
- Objective: To demonstrate a controlled, traceable document lifecycle.
- Materials: Electronic Document Management System (EDMS) or controlled paper system with logbooks.
- Methodology:
- Authoring: All documents are created using approved templates with unique identifiers.
- Review & Approval: A pre-defined list of approvers (e.g., Principal Investigator, QA) reviews electronically or on paper. All comments, responses, and approvals are recorded.
- Issuance: The finalized version is published and made available to authorized personnel only. The EDMS automatically archives previous versions.
- Periodic Review: The system flags documents for scheduled review (e.g., every 2 years). The review process is re-initiated.
- Retrieval: During an audit, present the full audit trail for requested documents, showing author, approvers, dates, and changes between versions.
Raw Data Integrity and Traceability
The ethical principle of data integrity is paramount. All data, electronic or paper-based, must adhere to ALCOA+.
Detailed Protocol for Raw Data Verification:
- Objective: To ensure the accuracy and completeness of transcribed data.
- Materials: Source documents (lab notebooks, instrument printouts), derived datasets, a second trained scientist.
- Methodology:
- Source Identification: Identify the original, first-capture record (e.g., a signed notebook page, a direct instrument output file).
- Independent Verification: A second individual, not involved in the original data entry, compares 100% of the data points in the derived dataset (e.g., Excel spreadsheet, LIMS entry) against the source.
- Discrepancy Management: Any discrepancy is highlighted, investigated, and resolved. A dated, signed note explaining the correction (without obscuring the original entry) is added.
- Documentation: The verification is documented via a signature in the notebook or an electronic audit trail entry in the LIMS.
Deviation and Corrective Action Prevention (CAPA) Management
Ethical research requires transparent handling of unexpected events.
Detailed Protocol for Deviation Management:
- Objective: To systematically document, assess, and address protocol or procedure deviations.
- Methodology:
- Documentation: The discoverer documents the deviation immediately in a dedicated log or system, noting the date, test/article ID, and nature of the issue.
- Impact Assessment: The PI and QA assess the impact on data integrity and subject safety/study outcomes. It is classified as minor, major, or critical.
- Root Cause Analysis: For major/critical deviations, a formal investigation (e.g., using 5 Whys or Fishbone diagram) is conducted to identify the root cause.
- CAPA Plan: A Corrective and Preventive Action plan is developed to address the root cause and prevent recurrence.
- Closure: The deviation is closed only after CAPA effectiveness is verified. The entire record is retained for audit.
The Scientist's Toolkit: Key Research Reagent Solutions for Audit-Ready Assays
Table 2: Essential Materials for Audit-Ready Experimental Workflows
| Item | Function in Audit-Readiness |
|---|---|
| Certified Reference Standards | Provides traceable and accurate calibration of instruments, ensuring data accuracy. Lot-specific certificates of analysis must be retained. |
| Controlled, Versioned Reagent Lots | Use of reagents tracked by lot number. Changes in lot require documentation and potential re-qualification to ensure assay consistency. |
| Electronic Lab Notebook (ELN) | Secures data with audit trails, ensures attribution and contemporaneous recording, and facilitates data retrieval. |
| Laboratory Information Management System (LIMS) | Manages sample lifecycle, links data to specific samples/protocols, automates data capture, and controls user access. |
| Calibrated and Maintained Equipment | Equipment with up-to-date calibration (traceable to national standards) and maintenance logs provides assurance of measurement validity. |
| Secure, Backed-Up Data Storage | Prevents data loss. Must include regular, tested backups and an archive policy for long-term retention of raw data. |
Visualizing the Audit-Ready Data Lifecycle
Diagram 1: Audit-Ready Data & Quality Management Lifecycle
Preparing for the Audit Event
Pre-Audit:
- Notification & Agenda: Review the audit announcement and proposed agenda. Designate a primary point of contact and logistics coordinator.
- Document Room: Prepare a clean, organized space for auditors. Pre-assemble frequently requested documents (SOP index, training records, master schedules, deviation log).
- Staff Briefing: Conduct a brief team meeting to review audit etiquette: be polite, factual, and answer only the question asked. Direct auditors to the point of contact for document requests.
During the Audit:
- Escort: Provide an escort for all auditors at all times.
- Document Production: Provide copies, not originals, when possible. Log all document requests.
- Response Strategy: For findings or questions, acknowledge and note them. Avoid defensive arguments. Commit to providing a follow-up written response if immediate answers aren't available.
Post-Audit:
- Debrief: Conduct an internal debrief to discuss observations.
- Audit Report: Carefully review the draft audit report.
- Response & CAPA: Develop a formal, timely written response to all findings. For each observation, provide a root cause analysis and a detailed, actionable CAPA plan with realistic timelines.
Achieving and maintaining audit-readiness is a continuous process embedded in the daily practice of ethical data management. By institutionalizing the principles of data integrity, transparency, and proactive quality management, laboratories not only ensure successful audits but, more importantly, uphold the scientific and ethical standards that are the foundation of trustworthy research and drug development.
Benchmarking Success: Validating Practices Against Global Standards
In the pursuit of scientific truth within laboratory research and drug development, the ethical management of data is foundational. It transcends regulatory compliance, forming the bedrock of research integrity, patient safety, and public trust. The ALCOA+ framework, endorsed by the FDA, EMA, and other global regulatory bodies, provides the definitive criteria for data quality. This whitepaper posits that adherence to ALCOA+ is not merely a procedural task but a core ethical obligation for researchers, ensuring that data supporting scientific claims and therapeutic approvals is demonstrably reliable and traceable.
Deconstructing ALCOA+: Principles and Technical Implementation
ALCOA+ defines the essential attributes of data quality. "Plus" commonly extends to include Complete, Consistent, Enduring, and Available.
Core Principles & Operational Definitions
- Attributable: Data must be linked to the individual who generated it and the source system.
- Legible: Data must be permanently readable and understandable by humans.
- Contemporaneous: Data must be recorded at the time of the activity.
- Original: The first recorded capture of data, or a certified copy.
- Accurate: Data must be correct, truthful, and free from errors.
- Complete: All data is present, including repeat or reanalysis results.
- Consistent: Data is chronologically sequenced and follows protocol.
- Enduring: Recorded on durable media and preserved for the required lifetime.
- Available: Accessible for review and inspection over its lifetime.
Quantitative Impact of Poor Data Governance
Data integrity failures carry significant consequences, as evidenced by regulatory actions.
Table 1: Common Data Integrity Findings and Their Impacts (FDA Warning Letters 2020-2023)
| ALCOA+ Principle Violated | Frequency (%) in Cited Observations | Typical Regulatory Action |
|---|---|---|
| Attributable & Contemporaneous | 42% | Clinical hold, study rejection |
| Accurate & Complete | 31% | Product approval delay |
| Original | 18% | Mandated third-party audit |
| Enduring & Available | 9% | Consent decree, monetary fine |
Technical Validation Methodologies for ALCOA+ Compliance
Implementing ALCOA+ requires deliberate technical and procedural controls. Below are key experimental protocols and validation steps.
Protocol 1: Validating Attributability and Contemporaneity in Electronic Lab Notebooks (ELNs)
- Objective: To verify that all entries in an ELN are securely linked to a unique user identity and timestamped by the system.
- Methodology:
- Create a standardized test procedure (e.g., "pH Measurement of Buffer XYZ").
- Have five distinct users execute the procedure and record results in the ELN.
- Export the audit trail for all entries.
- Validation Criteria: For each record, the audit trail must show: (a) User ID, (b) Action (create, modify, delete), (c) System-generated timestamp, and (d) No evidence of back-dating or credential sharing.
Diagram Title: ELN Attributability & Contemporaneity Validation Pathway
Protocol 2: Ensuring Originality and Accuracy of Instrument Raw Data
- Objective: To confirm that primary (raw) data from an analytical balance is preserved in its original state and accurately linked to a sample ID.
- Methodology:
- Configure balance to auto-save weighings to a network folder with read-only permissions upon completion.
- Weigh five reference standards. Each file name includes SampleID, InstrumentID, and DateTime.
- Manually transcribe values into a LIMS. Use automated script to compare LIMS entry against the original file data.
- Validation Criteria: 100% match between raw data file content and transcribed data. Zero evidence of file overwriting or manual alteration of raw files.
Diagram Title: Original Data Capture and Accuracy Verification Workflow
The Scientist's Toolkit: Essential Reagents and Solutions for Data Integrity
Table 2: Key Research Reagent Solutions for ALCOA+-Compliant Experiments
| Item / Solution | Function in Supporting ALCOA+ | Example Product / Standard |
|---|---|---|
| Controlled, Traceable Reagents | Ensures Accuracy & Attributability. Lot-specific QC data links result to material source. | NIST-traceable reference standards, ACS-grade solvents with Certificate of Analysis. |
| Stable Isotope-Labeled Internal Standards | Ensures Accuracy & Consistency in bioanalytics by correcting for sample preparation variability. | Deuterated or 13C-labeled analogs of analytes for LC-MS/MS. |
| Electronic Lab Notebook (ELN) | Enforces Attributable, Legible, Contemporaneous recording with audit trails. | Platforms like LabArchives, Benchling, or IDBS E-WorkBook. |
| Laboratory Information Management System (LIMS) | Maintains data Completeness, Consistency, and Availability by managing sample lifecycle. | STARLIMS, LabWare, or SampleManager. |
| System Suitability Test (SST) Kits | Provides evidence of Accuracy and system performance at the time of analysis (Contemporaneous). | Pre-mixed HPLC column test solutions, qPCR efficiency standards. |
| Secure, Audit-Enabled Storage | Ensures data is Enduring and Available in its Original form. | WORM (Write-Once-Read-Many) drives, validated cloud archives. |
| Digital Signatures & Time Servers | Cryptographically enforces Attributability and Contemporaneity for electronic records. | PKI-based digital IDs, NTP-synchronized network time. |
Validating processes against ALCOA+ criteria is the technical manifestation of an ethical commitment to scientific rigor. In laboratory research for drug development, where data decisions impact human health, there is no ethical data management without ALCOA+. By embedding these principles into experimental design, instrument validation, and daily practice, researchers uphold the highest standards of integrity, ensuring that every data point is not just a number, but a trustworthy piece of evidence in the mission to advance public health.
The management of research data in laboratory settings is governed by ethical imperatives that ensure integrity, reproducibility, and societal trust. While the core principles of data ethics are universal, their interpretation, formalization, and enforcement diverge significantly between academic and industrial research environments. This analysis, situated within a broader thesis on ethical data management frameworks, dissects these differences in requirements, drivers, and implementation. The focus is on life sciences and drug development, where data serves as the fundamental currency for discovery and regulatory approval.
Foundational Ethical Principles and Their Differential Weighting
Both sectors adhere to a common core of principles, but with varying emphasis.
| Ethical Principle | Academic Laboratory Emphasis | Industry Laboratory Emphasis |
|---|---|---|
| Integrity & Honesty | Fundamental to scholarly reputation. Focus on preventing fabrication, falsification, plagiarism (FFP). | Paramount; directly tied to regulatory compliance, product safety, and legal liability. |
| Transparency & Openness | High ideal; encouraged via open data, open source, and pre-registration to advance public knowledge. | Severely restricted by proprietary and competitive concerns. Transparency is inward (within company) and toward regulators. |
| Privacy & Confidentiality | Governed by IRB/Human Subject protocols (e.g., HIPAA, GDPR for human data). | Extremely high priority due to stringent regulatory oversight (FDA, EMA), clinical trial subject protection, and competitive secrecy. |
| Stewardship & Preservation | Often resource-constrained. Reliant on institutional repositories and funder mandates (e.g., NIH). | Systematic, resourced, and mandated by ALCOA+ principles for data integrity. Long-term archiving is standard. |
| Accountability | Primarily rests with the Principal Investigator (PI) and individual researchers. | Clearly defined, hierarchical chains of command. Roles like Data Integrity Officer are common. |
Quantitative Comparison of Governance Drivers & Outcomes
A summary of key quantitative differences in governance structures and reported issues.
Table 1: Governance Drivers and Data Issue Reporting
| Metric | Academic Labs (Typical) | Industry Labs (Pharma/Biotech Typical) |
|---|---|---|
| Primary Regulatory Driver | Funding Agency Policies (NIH, NSF), Journal Requirements | FDA 21 CFR Part 11/58/312, EMA GxP, ICH E6(R3) |
| Data Audit Frequency | Ad-hoc (for cause, or by funder) | Scheduled, routine, and for-cause (by Quality Assurance) |
| Standard for Data Integrity | FAIR Principles (aspirational) | ALCOA+ (Attributable, Legible, Contemporaneous, Original, Accurate + Complete, Consistent, Enduring, Available) - Mandatory |
| Reported Falsification/Fabrication Rate (Estimated) | ~2% in surveys (meta-analyses) | <0.1% in GxP audits; failure leads to severe action (Warning Letters, trial halt) |
| Formal Data Management Plan Requirement | ~80% for major grants (e.g., NIH, ERC) | 100% (embedded in Standard Operating Procedures - SOPs) |
| Primary Consequence for Breach | Retraction, grant revocation, career damage | Regulatory rejection, multi-million dollar fines, product approval delays, criminal liability |
Experimental Protocol Analysis: A Case Study in Data Handling
Protocol: Multi-Omics Biomarker Discovery in Oncology This protocol highlights divergent data handling steps.
4.1. Methodology Common to Both:
- Sample Acquisition: Patient-derived xenografts (PDX) or clinical biospecimens with informed consent.
- Multi-Omics Profiling: Parallel Next-Generation Sequencing (NGS) for genomics, LC-MS/MS for proteomics, and LC-MS for metabolomics.
- Primary Data Generation: Instruments output raw data files (e.g., .bcl, .raw, .d).
4.2. Divergent Data Management Pathways:
Academic Protocol (Open Science Aim):
- Step A1 (Processing): Raw data processed through open-source pipelines (e.g., nf-core) on institutional HPC. Version-controlled code on public GitHub.
- Step A2 (Annotation & Storage: Annotated with public ontologies. Processed data deposited in public repository (e.g., GEO, PRIDE) post-acceptance, per journal/funder mandate.
- Step A3 (Analysis & Sharing: Statistical analysis in R/Python. Manuscript includes detailed methods. Pre-print server use encouraged.
Industry Protocol (GxP-Compliant Aim):
- Step I1 (Processing): Raw data processed using validated software (IQ/OQ/PQ documented). All processing steps recorded in Electronic Lab Notebook (ELN) with audit trail.
- Step I2 (Annotation & Storage: Data annotated with internal controlled vocabularies. Raw and processed data stored in validated, secure, 21 CFR Part 11-compliant databases with strict access controls. No public deposition.
- Step I3 (Analysis & Reporting: Analysis performed per pre-specified Statistical Analysis Plan (SAP). Full data package compiled for internal decision-making and eventual regulatory submission (e.g., to FDA as part of IND/NDA).
The Scientist's Toolkit: Essential Reagent Solutions for Data Integrity
Table 2: Key Tools for Ethical Data Management
| Tool Category | Example Solutions | Primary Function in Data Ethics |
|---|---|---|
| Electronic Lab Notebook (ELN) | Benchling, LabArchives, IDBS E-WorkBook | Ensures data is Attributable, Legible, Contemporaneous, and Original (ALCOA). Provides audit trails. |
| Laboratory Information Management System (LIMS) | LabVantage, STARLIMS, LabWare | Manages sample lifecycle, links samples to data, enforces SOPs, ensuring process consistency and data lineage. |
| Scientific Data Management System (SDMS) | Titian Mosaic, LABTrack | Automatically captures, indexes, and archives raw instrument data, preventing loss and ensuring availability. |
| Quality Management System (QMS) Software | Veeva Vault, MasterControl | Manages deviations, corrective actions (CAPA), and change controls, addressing data integrity issues systematically. |
| 21 CFR Part 11 Compliant Cloud Storage | AWS GovCloud, Azure for Life Sciences | Provides secure, scalable, and validated infrastructure for storing regulated data with full access control. |
The comparative analysis reveals a fundamental dichotomy: academic labs are primarily governed by norms of transparency and scholarly contribution, while industry labs are governed by regulations enforcing rigor, traceability, and proprietary control. The academic pathway is optimized for knowledge dissemination, though often under-resourced for long-term stewardship. The industry pathway is a controlled, audited system designed to withstand regulatory scrutiny and mitigate risk. Both are essential to the research ecosystem, and understanding their respective ethical requirements is crucial for professionals navigating either sector or collaborating across them. The convergence point for both remains the non-negotiable ethical bedrock of data integrity and honesty, without which neither scientific progress nor patient safety can be assured.
Within the broader thesis on ethical guidelines for data management in laboratory research, this whitepaper provides a technical framework for assessing and advancing a lab's maturity in implementing these principles. For researchers and drug development professionals, moving from ad-hoc, reactive practices to a systematic, optimized culture is critical for scientific integrity, reproducibility, and regulatory compliance. This guide outlines a maturity model, provides actionable assessment protocols, and details essential resources for progression.
The Ethical Data Management Maturity Model
The maturity model is structured across five sequential levels, each defined by specific capabilities in data handling, documentation, and governance.
Table 1: Ethical Data Management Maturity Model Levels
| Maturity Level | Data Capture & Integrity | Metadata & Provenance | Access Control & Security | Audit & Compliance | Culture & Training |
|---|---|---|---|---|---|
| 1. Ad Hoc | Manual, paper-based notes; inconsistent formats; high error risk. | Minimal or non-standardized; provenance tracking is manual. | Ad-hoc sharing (e.g., USB, email); no formal access policies. | Reactive to issues; no regular audits. | Individual responsibility; no formal ethics training. |
| 2. Defined | Digital templates (e.g., ELN); basic version control. | Standardized basic metadata fields (date, author). | Role-based access on shared drives. | Scheduled internal checklists for data backup. | Annual mandatory data management training. |
| 3. Managed | Structured ELN with audit trails; automated instrument data capture. | Use of controlled vocabularies; digital provenance chains. | Granular, project-based permissions; data encryption at rest. | Proactive internal audits against SOPs; discrepancy logging. | Regular ethics case-study discussions; designated data steward. |
| 4. Quantitatively Managed | Integrated lab informatics platform (LIMS/ELN); data quality metrics monitored. | Machine-actionable metadata (e.g., following FAIR principles). | Dynamic access controls; automated de-identification for sharing. | Key performance indicators (KPIs) for data quality; external audits. | Continuous improvement culture; training integrated with workflows. |
| 5. Optimized | Predictive data quality checks; AI-assisted anomaly detection. | Full FAIR compliance; automated metadata generation. | Blockchain-based provenance for critical data; risk-adaptive security. | Real-time compliance dashboards; industry benchmark leadership. | Ethics by design; pervasive training integrated into all processes. |
Assessment Protocol: Measuring Your Lab's Current State
To objectively determine your lab's maturity level, conduct the following systematic assessment.
Experimental Protocol 1: Maturity Assessment Audit
- Objective: To quantitatively score a laboratory's current operational practices against the Ethical Data Management Maturity Model.
- Materials: Assessment team (2-3 members), interview guides, system access for verification, scoring spreadsheet (based on Table 1).
- Methodology:
- Pre-assessment: Define the scope (e.g., specific project, departmental lab).
- Document Review: Examine existing SOPs, data management plans, training records, and audit reports.
- Researcher Interviews & Observation: Conduct structured interviews with PIs, post-docs, and technicians. Observe actual data entry, sharing, and storage practices.
- System Analysis: Evaluate the configuration and use of ELN, LIMS, servers, and backup systems.
- Scoring: For each of the five categories in Table 1, assign a score (1-5) corresponding to the level whose description best matches the observed evidence. The overall maturity level is the lowest category score (the "weakest link" principle).
- Gap Analysis Report: Document scores, provide evidence, and list critical gaps preventing advancement to the next level.
Progression Pathway: From Defined to Managed
A critical jump is from Level 2 (Defined) to Level 3 (Managed), which establishes systematic control. The following workflow is essential.
Diagram Title: Key Steps to Advance from Defined to Managed Maturity
The Scientist's Toolkit: Essential Research Reagent Solutions
Implementing ethical data management requires both policy and technology. The following tools are critical for labs operating at Level 3 (Managed) and above.
Table 2: Essential Toolkit for Ethical Data Management
| Item Name | Category | Function in Ethical Data Management |
|---|---|---|
| Electronic Lab Notebook (ELN) | Software | Replaces paper notebooks; ensures data integrity via audit trails, timestamps, and non-editable records. Enforces standardized templates. |
| Laboratory Information Management System (LIMS) | Software | Manages sample metadata, workflows, and results. Maintains chain of custody and links derived data to source materials. |
| Institutional Repositories & Data Lakes | Infrastructure | Provides secure, centralized, and backup-enabled storage for raw and processed data with managed access controls. |
| Controlled Vocabularies & Ontologies | Standard | Standardizes terminology (e.g., Cell Ontology, CHEBI) to ensure metadata is unambiguous and machine-readable (FAIR). |
| Data Management Plan (DMP) Tool | Software/Policy | Guides researchers in creating comprehensive plans for data collection, documentation, sharing, and preservation at project inception. |
| Automated Data Integrity Checks | Software Scripts | Scripts (e.g., in Python/R) that validate data formats, ranges, and completeness upon ingestion, flagging potential errors or fraud. |
| De-identification & Anonymization Software | Software | Tools for removing or encrypting personally identifiable information (PII) from human subject data prior to sharing or publication. |
Protocol for Implementing Automated Data Integrity Checks
A hallmark of Level 4 maturity is the quantitative management of data quality.
Experimental Protocol 2: Automated Ingest Validation Script
- Objective: To programmatically validate incoming experimental data files against predefined quality rules before acceptance into the primary repository.
- Materials: Python 3.8+ environment with
pandas,numpy,jsonschemalibraries; validation rule specification file (YAML/JSON); designated quarantine storage area. Methodology:
Rule Definition: Document validation rules in a YAML file (e.g.,
assay_rules.yaml). Example for a plate reader assay:Script Development: Write a Python script (
validate_ingest.py) that:- Watches a designated "inbox" folder for new files.
- Loads the file and the appropriate rule set.
- Validates file structure, column presence, data types, value ranges, and adherence to patterns.
- Logs all discrepancies with severity levels (WARN, ERROR).
- Quarantine Logic: Files passing all checks are moved to the approved repository and registered in the LIMS. Files with ERRORs are moved to a quarantine folder, triggering an alert to the data steward. Files with only WARNs may be moved but flagged for review.
- KPI Monitoring: The script logs all validation outcomes. Monthly reports track the pass/fail rate by assay and user, providing KPIs for data quality trends.
Optimizing ethical practices in lab data management is a continuous journey, not a destination. By using the maturity model for assessment, implementing the provided protocols to address gaps, and leveraging the essential toolkit, research teams can build a robust, compliant, and efficient data ecosystem. This systematic approach directly supports the core thesis of ethical research by making integrity, traceability, and fairness measurable and managed components of the scientific process.
Within the context of ethical guidelines for data management in laboratory settings, data integrity is the non-negotiable foundation. It ensures that data are complete, consistent, accurate, and trustworthy throughout their lifecycle. This whitepaper examines high-profile case studies of success and failure, extracting technical lessons and methodological frameworks. The ethical duty to maintain data integrity extends beyond regulatory compliance; it is fundamental to scientific validity, patient safety, and public trust in research.
Part 1: High-Profile Failures and Their Technical Root Causes
Case Study A: The Duke University Cancer Trial Scandal (2010) A researcher was found guilty of fabricating and falsifying data in grant applications for lung cancer research, leading to the retraction of numerous papers and the dismissal of clinical trials.
Experimental Protocol Flaw: The researcher used publically available genomic datasets, claiming they were derived from his experiments. The fraud was uncovered through statistical analysis by a biostatistician who found the data were biologically impossible.
Case Study B: The Amgen & Bayer "Reproducibility" Crisis (2011-2012) Landmark studies revealed that a significant majority of published preclinical cancer research from academia could not be reproduced by industry scientists, pointing to systemic data integrity issues.
Experimental Protocol Flaw: Common culprits included: lack of blinding during analysis, inappropriate statistical methods (e.g., p-hacking), use of poorly characterized reagents, and selective reporting of positive results.
Summary of Quantitative Data from Failures
| Case / Study | Scale of Impact | Primary Technical Cause | Key Ethical Breach |
|---|---|---|---|
| Duke University Scandal | 60+ papers retracted; $112M in grants implicated | Data fabrication & falsification; no source data traceability | Fraud, deception, waste of public funds |
| Amgen/Bayer Reproducibility Review | ~89% (47 of 53) of landmark studies not reproducible | Poor experimental design & unblinded analysis | Lack of scientific rigor, misleading the scientific community |
| General FDA 483 Observations (2020-2023) | Hundreds of citations annually | Inadequate control of electronic data; lack of audit trails; data deletion without justification | Failure to ensure data ALCOA+ principles |
Part 2: Success Stories and Robust Methodologies
Case Study C: The Framingham Heart Study (Ongoing since 1948) A paradigm of longitudinal observational study integrity, generating thousands of validated data points on cardiovascular health across generations.
Detailed Methodology for Data Integrity:
- Standardized Data Collection: Protocols for blood pressure measurement, BMI calculation, and lab tests are rigorously defined and unchanged across decades.
- Blinded Analysis: Epidemiological analyses are conducted with blinding to participant identity and outcome status to reduce bias.
- Independent Verification: All major findings are subject to internal and external replication before publication. Original data forms are archived permanently.
- Transparent Data Sharing: De-identified datasets are made available to qualified researchers under a governance model, enabling external validation.
Case Study D: The mRNA Vaccine Development (Pfizer/BioNTech & Moderna) The rapid, successful development of COVID-19 vaccines demonstrated data integrity under immense pressure, leading to robust regulatory approval.
Detailed Methodology for Clinical Trial Data Integrity:
- Pre-registered Protocols & SAP: Trial designs and Statistical Analysis Plans were publicly filed before data unblinding.
- Electronic Data Capture (EDC) with Audit Trails: All case report form data were entered into validated EDC systems with immutable, timestamped audit trails.
- Centralized Blinding & Randomization: Interactive Response Technology (IRT) ensured proper blinding and randomization across global sites.
- Independent Data Monitoring Committee (DMC): An unblinded, external DMC performed interim analyses on safety and efficacy, protecting trial integrity.
The Scientist's Toolkit: Research Reagent Solutions for Data Integrity
| Reagent / Material | Function | Role in Ensuring Data Integrity |
|---|---|---|
| Cell Line Authentication Kit (e.g., STR Profiling) | Genetically identifies cell lines. | Prevents misidentification and contamination, a major source of irreproducible data. |
| Validated, Lot-Controlled Antibodies | Specific binding to target proteins. | Ensures experimental specificity and reproducibility across experiments and labs. |
| Standard Reference Materials (e.g., NIST) | Certified materials with known properties. | Provides a benchmark for calibrating instruments and validating assay performance. |
| Electronic Lab Notebook (ELN) | Digital record of experiments and results. | Creates immutable, timestamped records with audit trails, replacing error-prone paper notebooks. |
| Sample Tracking LIMS | Manages sample lifecycle and metadata. | Maintains chain of custody, prevents sample mix-ups, and links data to its biological source. |
Part 3: Implementing Foundational Protocols
Core Experimental Protocol: Procedure for a Blinded, Controlled In-Vivo Study
- Pre-Experimental Registration: Document hypothesis, primary endpoint, statistical power calculation, and analysis plan in an ELN or registry.
- Randomization: Use a computer-generated randomization schedule (e.g., in R or a dedicated tool) to assign subjects to treatment/control groups. Conceal schedule from personnel performing interventions.
- Blinding (Masking):
- Preparation: A third party codes treatment vials (A, B, C). The key is secured separately.
- Administration: Technicians administer codes without knowledge of group assignment.
- Assessment: Researchers evaluating outcomes (e.g., tumor size, behavioral score) are blinded to the code.
- Data Recording: Record raw data directly into the ELN or a pre-formatted spreadsheet. All entries must be attributable, legible, contemporaneous, original, and accurate (ALCOA).
- Unblinding & Analysis: Only after all data collection and quality checks are complete is the randomization code broken. Analyze according to the pre-specified SAP.
Visualizations of Key Concepts
Title: Data Integrity Lifecycle (PDCA Cycle)
Title: Clinical Trial Blinding & Data Flow
The case studies demonstrate that data integrity failures are often rooted in poor process, not just individual malfeasance. Success is built on a technical foundation of pre-registration, blinding, robust controls, transparent methodologies, and technology-enforced audit trails. Ethically, this translates to a culture where the complete, accurate record of research is valued as highly as the result itself. For researchers and drug developers, implementing the protocols and tools outlined here is not merely a regulatory step—it is the embodiment of responsible scientific conduct and the surest path to valid, reliable outcomes.
Within the critical framework of ethical data management in laboratory research, self-assessment tools are not merely administrative exercises. They are fundamental to ensuring data integrity, reproducibility, and compliance with ethical standards. This technical guide details the implementation of structured checklists and systematic audit protocols as mechanisms for continuous improvement in drug development and basic research settings.
The Ethical Imperative for Structured Self-Assessment
Ethical data management extends beyond privacy; it encompasses the entire data lifecycle—from generation and recording to analysis, reporting, and archiving. Failures at any stage can lead to scientific misconduct, irreproducible results, and compromised patient safety in clinical development. Checklists and audits provide a tangible, proactive defense against such ethical lapses by embedding rigor and accountability into daily practice.
Core Self-Assessment Tools: Design and Implementation
Pre-Experiment Data Management Checklist
This checklist ensures ethical and methodological rigor is established before data generation begins.
Table 1: Pre-Experiment Data Management Checklist Criteria
| Checklist Item | Ethical & Technical Rationale | Compliance Verification |
|---|---|---|
| Protocol pre-registration in internal system | Mitigates bias, ensures transparency | Link to registered protocol documented |
| Data Capture Sheet (electronic/lab notebook) validated | Prevents data loss, ensures ALCOA+ principles (Attributable, Legible, Contemporaneous, Original, Accurate) | Format locked, audit trail enabled |
| Statistical analysis plan finalized | Prevents p-hacking and data dredging | Signed plan attached to protocol |
| Equipment calibration and QC logged | Ensures data accuracy and reliability | Calibration certificate referenced |
| Ethical approval (IACUC/IRB) confirmed for all samples | Mandatory for ethical research conduct | Approval number and date recorded |
In-Process Data Integrity Audit
A spot-check tool for ongoing monitoring of data handling practices.
Experimental Protocol for a Data Integrity Spot Audit
- Objective: To assess contemporaneous, accurate, and attributable recording of primary data.
- Materials: Randomly selected experiment from active lab portfolio, associated protocol, raw data source (instrument output, lab notebook), and derived data files.
- Methodology:
- Random Sampling: Using a random number generator, select 10% of data points or 20 data points (whichever is larger) from the experiment's dataset.
- Traceability Verification: For each selected point, trace from the derived/analyzed data back to the original raw data record (e.g., from a publication figure back to the instrument printout).
- Attributability Check: Confirm the identity of the individual who recorded each data point is clearly noted (via handwritten initials or electronic login).
- Contemporaneity Assessment: Verify the date of data recording matches or is logically consistent with the experimental timeline in the protocol.
- Anomaly Logging: Document any breaks in the chain of custody, missing metadata, or unexplained alterations.
- Output: A quantitative score (e.g., 95% traceability) and a corrective action report.
Diagram 1: In-Process Data Integrity Audit Workflow (79 chars)
Post-Study Data Archiving and Sharing Audit
Ensures long-term ethical responsibility for data preservation and accessibility.
Table 2: Post-Study Archiving Audit Metrics (Based on Current Best Practices)
| Audit Dimension | Recommended Standard (from FAIR/peer guidelines) | Common Deficiency Rate* |
|---|---|---|
| Data Format | Non-proprietary, open format (e.g., .csv, .txt) used | ~40% of datasets |
| Metadata Completeness | Minimum Information Guidelines (e.g., MIAME for genomics) fulfilled | ~65% of repositories |
| Repository Suitability | Data deposited in discipline-specific trusted repository (e.g., GEO, PDB) | ~70% compliance in funded studies |
| License & Access | Clear usage license (e.g., CCO, MIT) attached; access instructions precise | ~50% of shared datasets |
| Embargo Adherence | Public release aligns with publication or agreed embargo period | >90% adherence |
*Note: Rates are approximate syntheses of recent journal compliance studies and repository surveys.
Signaling Pathway for Ethical Data Management Culture
A robust ethical data culture requires interconnected components, from top-level leadership to individual researcher practice.
Diagram 2: Pathway to an Ethical Data Management Culture (65 chars)
The Scientist's Toolkit: Research Reagent Solutions for Data Integrity
Table 3: Essential Materials for Implementing Data Self-Assessments
| Item | Function in Self-Assessment |
|---|---|
| Electronic Lab Notebook (ELN) with audit trail | Provides immutable, timestamped record of all entries, ensuring data attributability and preventing retroactive alteration. |
| Version Control System (e.g., Git) | Manages changes to code and analytical scripts, creating a transparent history of analyses critical for reproducibility audits. |
| Trusted Digital Repository Credentials | Access to institutional or public repositories (e.g., Figshare, institutional SQL DB) is necessary for verifying archiving compliance. |
| Standard Operating Procedure (SOP) Database | Centralized, version-controlled SOPs are the benchmark against which checklist compliance is measured. |
| Random Number Generator Tool | Essential for performing unbiased sampling during spot audits, ensuring audit integrity. |
| Metadata Schema Template | Pre-formatted templates (e.g., based on ISA-Tab standards) guide researchers in creating complete metadata, facilitating sharing audits. |
In the context of ethical data management, checklists and audits transform abstract principles into actionable, measurable behaviors. They are the engineered safeguards that systematically close the gap between ethical aspiration and daily practice. For researchers and drug developers, their consistent application is not a burden but a cornerstone of scientific integrity, directly contributing to the reliability of research outcomes and the acceleration of trustworthy science.
The integration of high-throughput omics (genomics, proteomics, metabolomics) with clinical trial data presents an unprecedented opportunity for precision medicine. However, this convergence amplifies ethical imperatives: ensuring data integrity, patient privacy, and reproducible science. Ethical data management is no longer ancillary; it is the prerequisite for future-proofing research. This guide provides a technical roadmap for aligning experimental and data workflows with emerging global standards, ensuring that research is both cutting-edge and ethically sound.
Adherence to evolving standards is non-negotiable for data interoperability, reusability, and auditability. The following table summarizes core standards and their applications.
Table 1: Key Emerging Standards for Clinical and Omics Data Integration
| Standard/Framework | Governing Body/Project | Primary Scope | Relevance to Omics-Clinical Integration |
|---|---|---|---|
| CDISC SEND | CDISC | Standardized non-clinical data (toxicology, pathology) | Essential for preclinical omics data structuring for regulatory submission. |
| CDISC ADaM | CDISC | Analysis-ready clinical trial datasets | Framework for creating derived analysis variables from integrated clinical and biomarker/omics data. |
| FHIR Genomics | HL7 International | Clinical genomics data exchange via EHRs | Enables linking clinical trial phenotypes with genomic observations in a modern web-based format. |
| ISA-Tab | ISA Commons | Multi-omics experimental metadata | Provides a flexible, spreadsheet-based format to describe the experimental workflow from sample to data file. |
| MIAME/MINSEQE | FGED | Microarray & high-throughput sequencing experiments | Defines minimum information required for omics data reproducibility and submission to repositories like GEO. |
| FAIR Principles | GO FAIR | Data management and stewardship (Findable, Accessible, Interoperable, Reusable) | Overarching guiding principles for designing all data management workflows. |
| GA4GH Phenopackets | Global Alliance for Genomics & Health | Standardized phenotyping data exchange | Facilitates sharing rich phenotypic descriptions alongside genomic data for rare disease and cancer studies. |
Experimental Protocol: An Integrated Multi-Omics Workflow for Clinical Trial Biomarker Discovery
This protocol outlines a methodology for generating FAIR-compliant data from patient-derived samples within a clinical trial.
Title: Integrated Serum Proteomics and Clinical Endpoint Analysis for Predictive Biomarker Discovery.
Objective: To identify serum proteomic signatures predictive of clinical response (e.g., PFS - Progression-Free Survival) in a Phase II oncology trial.
Materials & Workflow:
Diagram Title: Integrated Omics-Clinical Trial Workflow
Detailed Protocol:
3.1 Ethical Pre-Collection Phase:
- Obtain IRB-approved informed consent specifically covering genomic/proteomic profiling and future data sharing in controlled-access repositories.
- Sample Collection: Collect baseline serum using standardized SOPs. Use barcoded tubes scanned directly into a Laboratory Information Management System (LIMS) to ensure chain of custody. Annotate immediately with critical metadata (visit date, time, patient trial ID).
3.2 Sample Processing & Proteomics Analysis:
- High-Abundance Protein Depletion: Use a commercial immunoaffinity column (e.g., MARS-14) to remove top abundant proteins, increasing dynamic range for biomarker discovery.
- Trypsin Digestion: Perform reduction, alkylation, and overnight tryptic digestion using a standardized kit (e.g., FASP filter-aided sample preparation).
- LC-MS/MS Data Acquisition: Analyze peptides on a high-resolution tandem mass spectrometer coupled to nano-UHPLC. Utilize Data-Independent Acquisition (DIA) mode for comprehensive, reproducible quantification of all detectable peptides.
- Data Processing: Process raw DIA files using DIA-NN software. Search spectra against a species-specific spectral library. Output: a quantified protein intensity matrix.
3.3 Data Curation & Integration (The Critical Step):
- Clinical Data: Map curated clinical data (demographics, efficacy endpoints, adverse events) to CDISC SDTM/ADaM models.
- Omics Data: Format the protein matrix according to ISA-Tab specifications. Annotate each protein with stable identifiers (UniProt ID). Link the sample list in the ISA-Tab to the trial specimen IDs.
- Database Creation: Create a secure, relational database (e.g., PostgreSQL). Use a dedicated bridge table to link the three core entities: Patient (CDISC ID) <-> Biological Sample (LIMS ID) <-> Omics Dataset (ISA-Tab Reference).
3.4 Analysis & Reporting:
- Perform supervised multivariate analysis (e.g., partial least squares-discriminant analysis) to identify proteins associated with clinical response.
- Report results following the FAIR Principles. Ensure all analysis code (e.g., R/Python scripts) is version-controlled and shared on platforms like GitLab.
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 2: Key Reagents and Tools for Integrated Omics-Clinical Studies
| Item/Category | Example Product/Standard | Function in Workflow |
|---|---|---|
| Standardized Sample Collection Kit | Pre-barcoded serum separator tubes (SST) | Ensures consistent sample quality and enables automatic tracking via LIMS integration, critical for audit trails. |
| High-Abundance Protein Depletion Kit | Agilent Human MARS-14 Column, ProteoPrep Immunoaffinity Kit (Sigma) | Removes high-abundance proteins (e.g., albumin) from serum/plasma to enhance detection of lower-abundance potential biomarkers. |
| Universal Proteomics Standard | Pierce HeLa Protein Digest Standard (Thermo) | Spiked into samples as a process control to monitor technical variability across sample preparation and MS runs. |
| Data-Independent Acquisition (DIA) Kit | Biognosys’s HRM Kit (Hyper Reaction Monitoring) | Provides optimized chromatographic libraries and protocols for robust, large-scale DIA-MS studies. |
| Spectral Library Search Engine | DIA-NN, Spectronaut (Biognosys) | Specialized software for identifying and quantifying peptides/proteins from complex DIA-MS data. |
| Metadata Annotation Tool | ISAcreator (ISA-Tools Suite) | Desktop software to create and manage ISA-Tab formatted metadata, enforcing minimum reporting standards. |
| Controlled Vocabulary | NCI Thesaurus, EDAM Ontology, SNOMED CT | Standardized terms for diseases, interventions, and omics processes ensure semantic interoperability between datasets. |
| Secure Data Repository | EGA (European Genome-phenome Archive), dbGaP | Controlled-access repositories for sharing sensitive clinical-omics data in a standards-compliant, ethical manner. |
Visualization: The FAIR Data Lifecycle from Collection to Submission
The ethical management of data requires a defined lifecycle that embeds standards at every stage.
Diagram Title: FAIR Data Lifecycle with Embedded Standards
Future-proofing clinical trial research in the omics era is a technical and ethical mandate. It requires the deliberate integration of emerging data standards (CDISC, FHIR, ISA) into experimental design itself. By adopting the protocols, tools, and lifecycle model outlined here, researchers can build a robust foundation for data integrity, interoperability, and ethical stewardship. This alignment not only satisfies regulatory expectations but also maximizes the long-term scientific value of every patient's contribution, turning data into enduring, reusable knowledge for the benefit of future patients.
Conclusion
Ethical data management is the non-negotiable backbone of credible laboratory science, directly impacting drug development timelines, regulatory approval, and public health. By integrating foundational principles into methodological protocols, proactively troubleshooting biases and security risks, and continuously validating against evolving standards, research teams can safeguard integrity and accelerate discovery. The future of biomedical research demands not just sophisticated data generation but an unwavering commitment to its ethical stewardship. Embracing these guidelines will be paramount for navigating complex data landscapes, fostering collaborative innovation, and ultimately, ensuring that scientific progress translates into trustworthy and equitable health outcomes.