Informed Consent in Clinical Research: A Comprehensive Guide to Historical Evolution, Regulatory Requirements, and Best Practices
This article provides a comprehensive exploration of informed consent, from its historical origins in pivotal legal cases and ethical codes to its current regulatory requirements and future digital transformations.
Informed Consent in Clinical Research: A Comprehensive Guide to Historical Evolution, Regulatory Requirements, and Best Practices
Abstract
This article provides a comprehensive exploration of informed consent, from its historical origins in pivotal legal cases and ethical codes to its current regulatory requirements and future digital transformations. Tailored for researchers, scientists, and drug development professionals, it delivers foundational knowledge, practical application methodologies, strategies for overcoming common challenges, and insights into validating and comparing consent processes across different regulatory landscapes. The content synthesizes the latest regulatory guidance, ethical considerations, and technological advancements to support the design and implementation of robust, ethical, and compliant informed consent frameworks in clinical investigations.
From Paternalism to Patient Autonomy: The Historical and Ethical Foundations of Informed Consent
Medical paternalism represents a historical paradigm in which physicians made healthcare decisions on behalf of patients without necessarily seeking their agreement or even disclosing relevant medical information. This approach positioned the physician as a parental figure who alone determined what constituted the patient's best interests, fundamentally excluding patient autonomy from the clinical decision-making process. The doctrine of informed consent—now considered a cornerstone of both clinical practice and research ethics—stands in direct opposition to this paternalistic model, requiring patient understanding, voluntary choice, and authorization before medical interventions [1].
The Hippocratic Oath, despite its enduring symbolic value, established the ethical foundation for this paternalistic tradition. Analysis of its provisions reveals significant omissions by modern standards: it lacks any requirement to honor patient preferences, share medical information with patients, or protect patients participating in research [2]. This historical framework created an environment where "physicians felt that any disclosure of possible difficulties might erode patient trust" [3]. Understanding this pre-consent era is essential for comprehending the subsequent ethical evolution that led to contemporary informed consent standards in drug development and clinical research.
Historical Foundations in the Hippocratic Tradition
Paternalistic Elements in the Hippocratic Corpus
The Hippocratic Oath, authored approximately 2,500 years ago, codified a physician-centric model of medical ethics that would dominate Western medicine for millennia. Although the exact authorship remains uncertain, with evidence suggesting it was written about 100 years after Hippocrates' death, its principles have been "held sacred by doctors to this day" [3]. The oath established a beneficence-based ethical framework exclusively focused on the physician's duty to act for the patient's benefit as defined by the physician alone, without incorporating the patient's perspective or preferences.
Critical analysis of the original text reveals several profoundly paternalistic features. The classical version promised to "abstain from whatever is deleterious and mischievous," to "give no deadly medicine to any one if asked," and to "abstain from every voluntary act of mischief and corruption" [3]. These prohibitions established clear moral boundaries, but notably absent were any requirements to obtain patient permission for treatments or procedures. This omission created an ethical environment where "the physician believes that he/she has the knowledge and expertise to understand the patient's condition and therefore only he/she knows what is good or best for the patient" [3].
Historical Context and Cultural Permissibility
This paternalistic approach reflected the hierarchical social structures of ancient societies. In ancient Greece, medical practice differed significantly based on social status: "When slave doctors treated slaves they never explained the details of treatment to them. But freeborn doctors, who mainly treated freeborn patients, described to them the nature of their illness, often not revealing the whole truth regarding the condition or its prognosis" [4]. Similar patterns existed in traditional Indian medical systems (Ayurveda, Siddha, and Unani), where physicians sought permission from relatives, community leaders, or kings for major procedures, but not from patients themselves [4].
The historical pervasiveness of this model is encapsulated in Plato's "The Statesman," which stated that "if a doctor forces his patient to do the right thing against the accepted norms, it would not be considered as an error" [4]. This philosophical endorsement of physician authority without patient consultation characterized the pre-consent era and established a tradition that would persist well into the 20th century.
Table 1: Paternalistic Omissions in the Original Hippocratic Oath
| Modern Ethical Principle | Status in Classical Hippocratic Oath |
|---|---|
| Honoring patients' preferences | Omitted |
| Sharing medical information with patients | Omitted |
| Avoiding conflicts of interest | Omitted |
| Protecting research participants | Omitted |
| Treating all patients equally | Omitted |
| Obtaining consent for procedures | Omitted |
| Respect for patient autonomy | Not included |
The Paradigm Shift: From Paternalism to Informed Consent
Legal Foundations of Informed Consent
The transition from medical paternalism to respect for patient autonomy began through legal challenges rather than medical initiatives. The 1914 case of Schloendorff v. Society of New York Hospitals established early legal standing for informed consent when the court ruled in favor of a competent patient who had consented to an examination but not to surgical removal of a tumor [4]. This case established the principle that medical procedures performed without proper consent constituted unauthorized touching.
The term "informed consent" first appeared formally in a 1957 medical malpractice case, Salgo v. Leland Jr. University Board of Trustees, which involved a patient who awoke paralyzed after aortography without having been informed of this risk [3]. The court's ruling that "failure to disclose risks and alternatives was cause for legal action on its own" fundamentally reshaped physician-patient relationships by requiring disclosure of risks and alternatives, thereby enabling patients to participate meaningfully in their healthcare decisions [3].
Ethical Catalysts for Change
Historical abuses in medical research provided powerful impetus for formalizing informed consent requirements. The Nuremberg Code (1947), developed in response to Nazi human experimentation, established informed consent as its longest and most detailed principle [4]. Despite this, the Tuskegee Syphilis Study (1932-1972) demonstrated how government health agencies continued to withhold treatment and information from nearly 400 Black men without their knowledge or consent [5]. This ethical failure directly led to the Belmont Report (1979), which articulated three fundamental ethical principles for research: respect for persons, beneficence, and justice [4].
These developments reflected a broader philosophical shift from physician-centered ethics to patient-centered autonomy. As noted by contemporary observers, "Barely a century ago, it was commonly accepted that doctors could do whatever they thought was in the best interests of their patients, regardless of a patient's wishes or priorities" [5]. The emergence of informed consent represented a radical departure from this tradition, positioning patient autonomy as a counterbalance to professional authority.
Table 2: Historical Timeline: Paternalism to Informed Consent
| Time Period | Dominant Medical Paradigm | Key Developments |
|---|---|---|
| Ancient Greece - 19th Century | Medical Paternalism | Hippocratic Oath; Physician as sole decision-maker |
| Early 20th Century | Early Challenges to Paternalism | Schloendorff case (1914) establishes consent principle |
| Mid-20th Century | Formalization of Informed Consent | Nuremberg Code (1947); Salgo case (1957) |
| Late 20th Century | Codification and Regulation | Tuskegee Syphilis Study ends (1972); Belmont Report (1979) |
| 21st Century | Patient-Centered Care | FDA guidance harmonization; Global ethical standards |
Methodological Framework: Analyzing the Historical Transition
Experimental and Documentary Analysis
Research into the historical transition from medical paternalism to informed consent employs rigorous methodological approaches centered on documentary and comparative analysis. The following protocol outlines key methodological considerations for investigating this ethical evolution:
Primary Source Analysis Protocol:
- Textual Examination: Critical analysis of historical medical oaths, particularly comparing classical and modern versions of the Hippocratic Oath for paternalistic elements and omissions [3].
- Legal Case Documentation: Systematic review of landmark court rulings related to medical consent, focusing on the legal reasoning and principles established in decisions such as Schloendorff (1914) and Salgo (1957) [3] [4].
- Historical Comparative Studies: Cross-cultural analysis of medical ethics across different traditions (e.g., Indian, Greco-Roman, Islamic) to identify common paternalistic patterns [4].
- Regulatory Document Tracking: Chronological mapping of national and international guidelines from the Nuremberg Code (1947) to contemporary FDA and OHRP regulations [4] [6].
Ethnographic Research Methodology: Qualitative research in diverse cultural settings, such as the 2024 Pakistani study on clinician experiences with informed consent, employs semi-structured interviews guided by established topic guides [1]. Data collection involves digital audio recording with verbatim transcription, followed by reflexive thematic analysis using Braun and Clarke's approach [1]. This methodology enables identification of emergent themes regarding familial decision-making, gender disparities, and challenges in obtaining valid consent in collectivist cultures.
Visualization of the Historical Transition
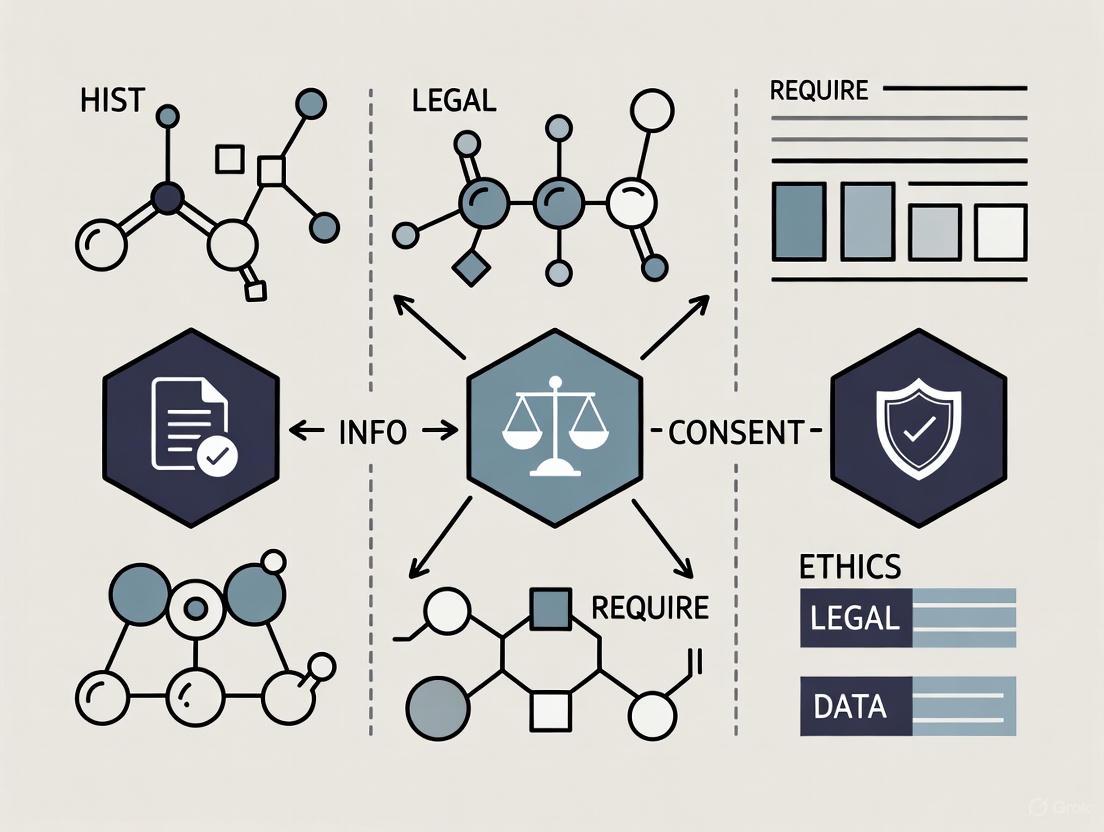
The following diagram illustrates the key historical and conceptual transition from the paternalistic model to modern autonomous decision-making:
Contemporary Implications for Research and Drug Development
Modern Regulatory Requirements
The evolution from paternalism to informed consent has produced increasingly sophisticated regulatory frameworks governing clinical research and drug development. Recent harmonization efforts between the FDA and OHRP (Office for Human Research Protections) expectations reflect ongoing refinement of informed consent standards [6]. Since 2019, OHRP guidance has included expectations for "a concise summary of key information for trial participants that is to be found at the beginning of what can be very long and complicated informed consent forms and written at a reading level that should be understandable to the non-medical expert reader" [6].
Current FDA guidance recommends that informed consent documents should be "short and that the information be presented in an easily accessible way for participants," encouraging the use of new technologies in the consent process [7]. This is particularly relevant for medical device developers, where complex procedures may be better explained through videos or pictorial representations rather than traditional text-heavy documents [7]. The FDA specifically recommends formats that enhance participant understanding, including "bubbles, rounded boxes creating a discrete unit of information, bullet points or two columns," while acknowledging the need to accommodate participants with visual or cognitive impairments [7].
Cultural Adaptations in Global Research
Contemporary research ethics recognizes that informed consent models must adapt to diverse cultural contexts. Studies in collectivist cultures like Pakistan reveal that "shared decision making was more morally important than individual autonomy, the role of the family played a dominant part in the consent-taking procedure, [and] the decision of the elder and/or family patriarch took prominence" [1]. This creates complex ethical challenges for global drug development, requiring sensitivity to cultural norms while maintaining fundamental ethical protections.
The Navajo tribe in the United States presents another cultural variation, where community norms may discourage full disclosure of negative information "as it believes this could lead to harmful effects" [4]. Such cultural variations demonstrate that while the principle of respect for persons remains universal, its application must consider local values and communication patterns, particularly in international clinical trials.
Research Reagent Solutions: Analytical Tools for Consent Research
Table 3: Essential Methodological Tools for Historical and Ethical Research
| Research Tool | Function and Application |
|---|---|
| Historical Document Analysis | Critical examination of primary sources (Hippocratic Oath, historical medical texts) |
| Qualitative Interview Protocols | Semi-structured interviews with healthcare professionals to understand contemporary consent challenges |
| Thematic Analysis Framework | Systematic coding and theme development from qualitative data (e.g., Braun and Clarke's approach) |
| Comparative Cultural Analysis | Cross-cultural examination of consent practices across different medical traditions and societies |
| Regulatory Document Tracking | Chronological mapping of consent guidelines from historical codes to contemporary regulations |
| Legal Case Analysis | Examination of landmark court decisions that shaped consent requirements and definitions |
The historical dominance of medical paternalism, rooted in the Hippocratic tradition, established a physician-centered ethical framework that persisted for millennia. The transition to modern informed consent standards represents a fundamental shift in medical ethics, driven by legal challenges, historical abuses, and evolving understandings of patient autonomy. For contemporary researchers and drug development professionals, understanding this historical context is essential for designing ethical research protocols and consent processes that respect participant autonomy while remaining sensitive to cultural variations. The ongoing refinement of informed consent guidelines reflects the research community's commitment to ethical evolution while acknowledging that effective consent processes must balance legal requirements, ethical principles, and practical implementation across diverse global contexts.
The 1914 decision by the New York Court of Appeals in Schloendorff v. Society of New York Hospital represents a foundational pillar in the law of informed consent and patient self-determination. This landmark case established the core legal principle that every individual has the right to determine what happens to their own body, a concept that has evolved into the modern doctrine of informed consent crucial for researchers and drug development professionals today. The case's enduring significance lies not in its immediate outcome, but in the powerful legal doctrine it introduced, which has permeated both clinical medicine and human subjects research. Justice Benjamin Cardozo's eloquent assertion that "every human being of adult years and sound mind has a right to determine what shall be done with his own body" has transcended its original context to become the ethical cornerstone of patient-centered care and ethical clinical research [8]. This principle forms the essential framework within which researchers must operate when designing trials and obtaining consent from human subjects, ensuring that autonomy and respect for persons remain paramount in scientific advancement.
Case Analysis: Schloendorff v. Society of New York Hospital
Factual Background and Procedural History
In January 1908, Mary Schloendorff was admitted to New York Hospital for evaluation and treatment of a stomach disorder [8]. During her hospitalization, physicians discovered a fibroid tumor. The medical recommendation was for surgical removal; however, Schloendorff explicitly declined operative intervention [9]. She consented only to an examination under ether anesthesia to determine the tumor's nature [10]. While anesthetized, surgeons proceeded to remove the tumor contrary to her expressed wishes. Following this unauthorized procedure, Schloendorff developed gangrene in her left arm, necessitating the amputation of several fingers [8]. She subsequently initiated legal action against the hospital, though notably not against the individual physicians [8]. The trial court directed a verdict in favor of the hospital, prompting Schloendorff's appeal to the New York Court of Appeals [9].
Legal Issues and Court's Holding
The central legal issue before the Court of Appeals was whether a charitable hospital could be held liable for the unauthorized actions of its physicians who performed surgery without the patient's consent [9]. The court confronted the question of whether the hospital should be responsible under the legal doctrine of respondeat superior (let the master answer) for the physicians' actions. The Court of Appeals affirmed the lower court's decision, holding that the hospital could not be held liable for the unauthorized surgery performed by its physicians [9]. The court reasoned that physicians, whether visiting or resident, were independent contractors rather than employees of the hospital [10]. As such, the hospital merely provided facilities and procured physicians for patients, but the physicians acted on their own professional responsibility rather than as agents of the hospital [9].
The Cardozo Formulation and Its Legal Reasoning
Justice Benjamin Cardozo's opinion drew a crucial legal distinction between negligence and trespass (now more commonly termed battery). While the case primarily addressed charitable immunity, Cardazo's articulation of patient rights created enduring legal doctrine:
"Every human being of adult years and sound mind has a right to determine what shall be done with his own body; and a surgeon who performs an operation without his patient's consent commits an assault, for which he is liable in damages. This is true except in cases of emergency where the patient is unconscious and where it is necessary to operate before consent can be obtained" [8].
This formulation established that performing surgery without consent constituted a trespass to the person—a more serious violation than mere negligence. The court emphasized that because Schloendorff had explicitly refused consent for the operation, she was effectively a "stranger" to that specific transaction, having never waived her right to recover damages for any wrong resulting from the forbidden procedure [10].
Table: Key Aspects of the Court's Reasoning in Schloendorff
| Legal Aspect | Application in Schloendorff | Legal Consequence |
|---|---|---|
| Nature of Wrong | Surgery without consent | Trespass/Battery rather than negligence |
| Hospital-Physician Relationship | Independent contractors, not employees | Hospital not vicariously liable |
| Charitable Immunity | Non-profit hospital providing free care | Protected from liability for employees' negligence |
| Patient Status | Had refused the specific operation | "Stranger" to the unauthorized procedure |
Historical and Legal Evolution of Informed Consent
Pre-Schloendorff Legal Landscape
The principle of patient consent had been developing in Anglo-American law for centuries before Schloendorff. The first reported legal decision involving consent was the 1767 English case of Slater v. Baker & Stapelton, where the court ruled that it was "the usage and law of surgeons" to obtain the patient's consent before operating [11]. In the early twentieth century, a series of cases further established the principle of bodily integrity:
- Mohr v. Williams (1905): The Minnesota Supreme Court found liability when a surgeon operated on the left ear after consent had been given only for the right ear [12].
- Pratt v. Davis (1905): An Illinois appellate court decided in favor of a patient who underwent a hysterectomy without her consent, stating that the "right to the inviolability of his person" was the citizen's "first and greatest right" [12].
- Rolater v. Strain (1913): The Oklahoma Supreme Court held a surgeon liable for removing a bone from a patient's foot when the consent was only for draining an infection [12].
These cases, all involving female plaintiffs at a time when women lacked voting rights, established the crucial link between personal autonomy and bodily integrity [12].
The Schloendorff Rule and Its Subsequent Rejection
The principle that a non-profit hospital could not be sued for actions of its employees became known as the "Schloendorff rule" [8]. This doctrine of charitable immunity persisted for decades but was eventually rejected by the New York Court of Appeals in the 1957 decision Bing v. Thunig [8]. The court recognized that the modern hospital functions differently than its 1914 counterpart, often acting as a comprehensive health center employing numerous staff physicians, thus warranting responsibility for their actions.
Evolution to Modern Informed Consent
The term "informed consent" first appeared in 1947 during discussions about declassifying Manhattan Project research and entered the legal lexicon with Salgo v. Leland Stanford Jr. University Board of Trustees (1957) [11]. This case established the physician's duty to disclose potential risks and alternatives, moving beyond simple consent to the requirement of adequate information disclosure [12]. The development of informed consent was further influenced by the Nuremberg Code (1947), which emphasized voluntary consent as the first principle for ethical human subjects research following the atrocities of World War II [12].
Table: Evolution of Informed Consent Doctrine Through Key Legal Cases
| Case | Year | Legal Principle Established | Significance |
|---|---|---|---|
| Slater v. Baker & Stapelton | 1767 | Foundation of patient consent requirement | Established consent as "usage and law of surgeons" |
| Mohr v. Williams | 1905 | Limits of consent; procedure specificity | Consent for one procedure does not extend to another |
| Pratt v. Davis | 1905 | Right to bodily inviolability | Recognized bodily integrity as fundamental right |
| Schloendorff v. NY Hospital | 1914 | Right to self-determination; unauthorized surgery as trespass | Articulated foundational autonomy principle |
| Salgo v. Leland Stanford | 1957 | Duty to disclose risks and alternatives | Introduced "informed consent" terminology |
| Natanson v. Kline | 1960 | Reasonable patient standard | Focused on information a patient would need to know |
| Canterbury v. Spence | 1972 | Prudent patient standard | Expanded disclosure requirements beyond medical custom |
Ethical Framework and Core Components of Valid Consent
Ethical Foundations
The fundamental ethical principle justifying informed consent is respect for personal autonomy [11]. This principle acknowledges individuals as self-governing agents with the right to make decisions about their own lives and bodies. In research ethics, this is complemented by the principle of nonmaleficence (do no harm) and beneficence (do good), which together require that researchers minimize risks while maximizing potential benefits [13]. The Belmont Report (1979) further codified respect for persons as one of three fundamental ethical principles for research involving human subjects [12].
Core Components of Valid Informed Consent
Contemporary bioethics recognizes five essential criteria for valid informed consent:
Disclosure: Provision of adequate information about the nature, purpose, risks, benefits, and alternatives to the proposed intervention or research participation [11]. The standard for determining which risks to disclose varies by jurisdiction but generally includes common risks regardless of severity and serious risks regardless of frequency [11].
Capacity: The patient's or subject's ability to understand relevant information, appreciate the situation and its consequences, and manipulate information rationally [11]. Adults are presumed to have capacity unless specific evidence indicates otherwise [11].
Understanding: Comprehension of the information presented and its relevance to one's particular situation [11]. This component emphasizes the need for effective communication tailored to the individual's health literacy and educational level.
Voluntariness: Freedom from coercion, undue influence, or unfair persuasions when making a decision [11]. This ensures the decision reflects the patient's values and preferences rather than external pressures.
Decision: The patient must make a specific authorization for or against the proposed plan [11]. This represents the culmination of the consent process through a clear expression of choice.
Diagram: Ethical Components of Valid Informed Consent - This framework illustrates the five core components required for ethically and legally valid informed consent, with expanded elements of disclosure that researchers must address.
Contemporary Applications in Clinical Practice and Research
Legal Standards for Adequate Disclosure
Various legal standards have developed to determine the adequacy of information disclosure in informed consent:
- Reasonable Patient Standard: What would a typical patient need to know to be an informed participant in the decision? This predominant standard focuses on patient needs rather than medical customs [13].
- Subjective Standard: What does this particular patient need to know and understand to make an informed decision? This individualized approach considers specific patient circumstances and values [13].
- Reasonable Clinician Standard: What would a typical clinician disclose about this procedure? This physician-centered approach has largely been superseded by patient-focused standards [13].
Documentation and Regulatory Requirements
Proper documentation of informed consent is critical for both clinical care and research. The Joint Commission requires documentation of all informed consent elements, either in a dedicated form or within progress notes [13]. Essential documentation includes:
- Nature of the procedure or intervention
- Risks and benefits
- Reasonable alternatives
- Risks and benefits of alternatives
- Assessment of patient understanding [13]
In research contexts, federal regulations (45 CFR 46 and 21 CFR 50) mandate additional elements for informed consent, including the statement that the study involves research, explanation of purposes, description of procedures, identification of experimental procedures, and disclosure of appropriate alternative procedures [12].
Special Considerations in Research and Drug Development
For researchers and drug development professionals, several specific considerations emerge from the Schloendorff foundation:
- Therapeutic Misconception: Addressing the common tendency among research participants to confuse research with therapeutic treatment [11].
- Capacity Assessment: Implementing formal or informal capacity assessments, particularly for vulnerable populations or those with cognitive impairments [11].
- Cultural Competency: Adapting consent processes for diverse populations where decision-making may be collective rather than individual [13].
- Emerging Technologies: Addressing novel consent challenges in genetic research, big data analytics, and innovative trial designs [13].
Table: Essential Research Reagents for Informed Consent in Clinical Trials
| Research Reagent | Function in Consent Process | Regulatory/Ethical Basis |
|---|---|---|
| Informed Consent Forms | Documents the consent process and specific agreements | 21 CFR 50, ICH GCP Guidelines |
| Health Literacy Assessments | Evaluates participant comprehension capacity | Ethical principle of understanding |
| Cultural Adaptation Tools | Ensures consent materials are culturally appropriate | Ethical principle of respect for persons |
| Witness Verification Protocols | Provides independent verification of consent process | ICH GCP Guidelines for illiterate subjects |
| Multi-Media Explanation Tools | Enhances understanding through visual/audio means | Ethical principle of adequate disclosure |
| Validation Questionnaires | Assesses participant understanding of key concepts | Ethical principle of comprehension |
Current Challenges and Future Directions
Persistent Implementation Challenges
Despite the well-established legal and ethical framework, significant challenges remain in implementing meaningful informed consent:
- Health Literacy Barriers: Complex medical jargon and varying health literacy levels often result in patients agreeing to procedures without full understanding of risks, benefits, or alternatives [13]. Studies have identified inadequacies in functional health literacy among hospitalized patients, compromising the informed consent process [13].
- Language and Cultural Barriers: Inadequate use of interpreters and lack of cultural sensitivity complicate consent processes, particularly in diverse populations [13]. In some cultures, decisions are made collectively rather than individually, creating tension with Western individual autonomy models [13].
- Time Pressures and Systemic Constraints: Rushed consent processes in busy clinical and research settings may not allow adequate time for discussion, questions, and reflection [13].
- Power Dynamics: The inherent power imbalance in the clinician-patient relationship can make patients feel pressured to consent, particularly in vulnerable populations [13].
Evolving Standards and Innovative Approaches
Contemporary approaches to informed consent are evolving to address these challenges:
- Process Model vs. Event Model: The traditional single-event consent is giving way to a continuous process throughout the clinician-patient relationship [11]. This approach recognizes that medical decision-making occurs over time as understanding develops.
- Shared Decision-Making: This collaborative process emphasizes bidirectional information exchange between clinicians and patients, incorporating patient values and preferences into medical decisions [13].
- Key Information Section: The 2017 revisions to the Common Rule introduced requirements for a concise, focused key information section at the beginning of consent documents to facilitate participant comprehension [12].
- Digital and Multimedia Consent: Interactive media, graphical tools, and digital platforms are being increasingly utilized to improve understanding and engagement during the consent process [13].
Diagram: Legal Evolution from Schloendorff to Modern Consent - This timeline shows the development of informed consent law from the foundational autonomy principle in Schloendorff through key cases to contemporary approaches, alongside ongoing implementation challenges.
More than a century after its publication, Schloendorff v. Society of New York Hospital continues to resonate through medical ethics and research regulation. While the specific holding regarding charitable immunity has been repudiated, Justice Cardozo's articulation of the right to self-determination remains the cornerstone of modern informed consent doctrine. For contemporary researchers and drug development professionals, Schloendorff establishes the fundamental ethical imperative: competent individuals have the right to make informed, voluntary decisions about interventions involving their own bodies. This principle finds expression in detailed regulatory frameworks governing human subjects research, institutional review processes, and the ethical design of clinical trials. As medical science continues to advance in complexity, with emerging technologies creating novel ethical challenges, the foundational principle articulated in Schloendorff provides the moral compass guiding the responsible conduct of research. The ongoing evolution of informed consent from a document-focused event to a communication-centered process represents the continuing vitality of Cardozo's vision, ensuring that respect for personhood remains at the heart of both clinical care and scientific progress.
The Nuremberg Code and Declaration of Helsinki represent foundational pillars in the ethical conduct of medical research involving human participants. These documents emerged as direct responses to systematic ethical atrocities revealed during the 20th century, establishing for the first time comprehensive frameworks to protect human dignity, autonomy, and welfare in scientific investigation. The creation of these ethical standards marks a critical turning point in medical history, transitioning from a primarily utilitarian approach to human experimentation to one grounded in respect for persons, beneficence, and justice [14] [15].
The historical context for these documents is inextricably linked to the Nazi medical war crimes tried at the Doctors' Trial in Nuremberg, where physicians conducted brutal experiments on concentration camp prisoners without consent [15]. This trial exposed a profound ethical vacuum in medical research and highlighted the urgent need for formalized protections. In the subsequent decades, the Declaration of Helsinki built upon the Nuremberg Code's foundation, evolving through multiple revisions to address emerging ethical challenges in an increasingly complex research landscape [16] [17]. Together, these documents have shaped modern regulatory systems worldwide, establishing informed consent as the cornerstone of ethical human subjects research [14].
The Nuremberg Code: Historical Foundation and Core Principles
Historical Context and Creation
The Nuremberg Code originated from the U.S. v Brandt case (1947), one of the Subsequent Nuremberg Trials conducted after World War II [15]. The trial involved 23 German physicians and bureaucrats charged with crimes against humanity for conducting unethical medical experiments on concentration camp inmates [18] [15]. During the proceedings, the defendants argued that no clear differentiation existed between legal and illegal human experimentation, revealing a troubling absence of international standards [15].
In response, Dr. Leo Alexander submitted a memorandum to the United States Counsel for War Crimes outlining six points for legitimate medical research [15]. This document evolved into the ten-point Nuremberg Code, articulated by the three American judges in their verdict [15]. The Code represented the first international effort to establish comprehensive guidelines for ethical human experimentation, directly addressing the atrocities perpetrated by the Nazi regime [18] [14].
The Ten Principles of the Nuremberg Code
The Nuremberg Code's ten principles establish fundamental requirements for ethical research, with voluntary consent as its cornerstone [18] [15]. The complete principles are:
Table: The Ten Principles of the Nuremberg Code
| Principle | Key Components | Ethical Foundation |
|---|---|---|
| 1. Voluntary Consent | Legal capacity; free power of choice; sufficient knowledge and comprehension; understanding of nature, duration, purpose, methods, hazards | Respect for autonomy |
| 2. Fruitful Results for Society | Yield results unprocurable by other methods; not random or unnecessary | Social value |
| 3. Proper Design and Justification | Based on animal experimentation, natural history of disease; anticipated results justify experiment | Scientific validity |
| 4. Avoidance of Suffering | Avoid all unnecessary physical and mental suffering and injury | Non-maleficence |
| 5. Prohibition of Risky Experiments | No experiment where death/disabling injury expected; exception where researchers also serve as subjects | Risk-benefit assessment |
| 6. Risk Proportional to Importance | Degree of risk never exceeds humanitarian importance | Risk-benefit assessment |
| 7. Proper Preparations and Facilities | Protect against remote possibilities of injury, disability, or death | Protection of participants |
| 8. Qualified Researchers | Scientifically qualified persons; highest degree of skill and care | Scientific integrity |
| 9. Participant's Right to Terminate | Human subject at liberty to end experiment if continuation seems impossible | Respect for autonomy |
| 10. Scientist's Duty to Terminate | Prepared to terminate if likely injury, disability, or death | Beneficence |
The Code's first principle establishes the absolute requirement for voluntary consent, emphasizing that the potential subject "should have sufficient knowledge and comprehension of the elements of the subject matter involved as to enable him to make an understanding and enlightened decision" [18]. This represents a radical departure from previous practices where researchers made unilateral decisions about participation [14].
The Code further places personal responsibility on researchers, stating that "the duty and responsibility for ascertaining the quality of the consent rests upon each individual who initiates, directs or engages in the experiment" and "may not be delegated to another with impunity" [18]. This personal accountability reflects the direct response to the Nuremberg trials, where researchers attempted to deflect responsibility to superiors [15].
The Declaration of Helsinki: Evolution and Expansion of Ethical Principles
Historical Development and Revisions
The World Medical Association (WMA) developed the Declaration of Helsinki in 1964 as a statement of ethical principles specifically for medical research involving human participants [16] [17]. Created by physicians for physicians, the Declaration built upon the Nuremberg Code while addressing additional complexities in clinical research. Unlike the Code, which was articulated through a legal verdict, the Declaration emerged from the medical profession's self-regulation efforts [16].
The Declaration has been amended multiple times (1975, 1983, 1989, 1996, 2000, 2002, 2004, 2008, 2013, and most recently in 2024) to address evolving challenges in research ethics [16] [17]. This periodic revision process ensures the document remains relevant to contemporary issues such as genetic research, biobanking, and global health disparities. The WMA emphasizes that "the current (2024) version is the only official one; all previous versions have been replaced and should not be used or cited except for historical purposes" [17].
Key Ethical Principles and Advancements
The Declaration of Helsinki introduces several significant advancements beyond the Nuremberg Code:
Table: Key Ethical Advancements in the Declaration of Helsinki
| Ethical Area | Specific Provisions | Significance |
|---|---|---|
| Research Ethics Committees | Protocol review before research begins; independence and authority; ongoing monitoring | Institutional oversight |
| Risk-Benefit Assessment | Importance of objective must outweigh risks and burdens; continuous risk monitoring | Systematic evaluation |
| Vulnerable Populations | Specific considerations for vulnerable groups; research only if responsive to their health needs | Protection of vulnerable subjects |
| Privacy and Confidentiality | Every precaution to protect privacy and confidentiality of personal information | Respect for privacy |
| Informed Consent Process | Plain language information; right to refuse/withdraw without reprisal; documentation | Enhanced consent standards |
| Physician-Researcher Role | Patient well-being as primary consideration; research only if justified by potential value | Dual role management |
| Post-Trial Provisions | Description of post-trial arrangements in protocol; access to proven interventions | Access to benefits |
| Compensation for Injury | Appropriate compensation/treatment for research-related harm | Justice and reparations |
The Declaration establishes that "the primary purpose of medical research involving human participants is to generate knowledge to understand the causes, development and effects of diseases; improve preventive, diagnostic and therapeutic interventions; and ultimately to advance individual and public health" while emphasizing that "these purposes can never take precedence over the rights and interests of individual research participants" [16]. This balance between societal benefits and individual rights represents a crucial development in research ethics.
The Declaration also introduces the concept of research ethics committees (RECs), requiring protocol review before research begins and establishing standards for committee composition, independence, and ongoing oversight [16]. This institutionalizes ethical review rather than relying solely on individual researcher integrity.
Methodological Framework: Quantitative Analysis of Ethics Adherence
Research Methodology on Ethics Compliance
Recent research employs quantitative methods to assess adherence to ethical codes in academic settings. A 2024 descriptive-analytical study conducted at Kermanshah University of Medical Sciences (KUMS) applied the Theory of Planned Behavior (TPB) to identify determinants of ethical compliance among students [19]. The study utilized cluster sampling with faculties as distinct clusters, selecting participants through simple random sampling within each cluster.
The methodology included:
- Structured questionnaires with two sections: demographic information and TPB constructs
- 5-point Likert scales for measuring attitudes, subjective norms, perceived behavioral control, intentions, and behaviors
- Rigorous validity assessment including face validity (qualitative interviews with 12 experts) and content validity (Content Validity Index and Content Validity Ratio)
- Statistical analysis using Pearson correlation and linear regression to identify predictive factors
This methodological approach provides a quantitative framework for evaluating the practical implementation of ethical principles established by the Nuremberg Code and Declaration of Helsinki.
Key Findings on Ethics Adherence
Table: Adherence to Research Ethical Codes (REC) - Quantitative Findings
| Metric | Finding | Significance |
|---|---|---|
| Overall Adherence | 69.1% adherence to ethical codes | Moderate compliance level |
| Key Predictors | Attitude (B=0.694, p<0.001) and intention (B=0.857, p=0.002) as significant predictors | Psychological factors drive compliance |
| Variance Explained | 35.2% of variance in adherence explained by TPB model (adjusted R²=0.352) | Model effectiveness |
| Highest Adherence Area | Confidentiality (mean score=4.04/5) | Strong protection of privacy |
| Lowest Adherence Area | Obtaining ethical approval before data collection (mean score=2.68/5) | Procedural compliance weakness |
| Sample Characteristics | 271 participants; mean age 23.99 years; 75.4% response rate | Study demographics |
The study found that "the adherence level to ethical codes was 69.1%" with significant variation across different ethical requirements [19]. The lowest adherence was observed in "obtaining ethical approval before data collection (mean score=2.68)," indicating a concerning gap in procedural ethics despite high awareness of confidentiality principles [19].
Visualization of Ethical Framework Development
Diagram: Historical Evolution of Research Ethics Framework
Comparative Analysis: Nuremberg Code vs. Declaration of Helsinki
Table: Comparative Analysis of Nuremberg Code and Declaration of Helsinki
| Characteristic | Nuremberg Code | Declaration of Helsinki |
|---|---|---|
| Origin | Legal verdict (U.S. v Brandt) | Medical professional statement (WMA) |
| Year Established | 1947 | 1964 (latest revision 2024) |
| Primary Focus | Human experimentation generally | Medical research involving human participants |
| Consent Approach | Absolute requirement of voluntary consent | Comprehensive process with specific information requirements |
| Vulnerable Populations | Not specifically addressed | Detailed provisions for protection |
| Oversight Mechanism | Individual researcher responsibility | Research ethics committee review |
| Therapeutic Research | Not differentiated | Specific guidelines for combined care/research |
| Compensation for Injury | Not explicitly addressed | Explicit requirement for compensation/treatment |
| Global Influence | Foundation for later documents | Directly influenced national regulations worldwide |
| Revision Process | Static document | Dynamic with periodic revisions |
The Nuremberg Code emerged as a direct legal response to specific atrocities, creating non-negotiable standards for all human experimentation [18] [15]. In contrast, the Declaration of Helsinki represents the medical profession's ethical self-regulation, providing more detailed guidance specifically for medical research while allowing for evolution through periodic revisions [16] [17].
A crucial distinction lies in their approach to oversight: the Code emphasizes individual researcher responsibility, while the Declaration institutes systemic oversight through research ethics committees [18] [16]. This shift reflects the growing recognition that ethical research requires both individual integrity and institutional safeguards.
The Researcher's Toolkit: Implementing Ethical Requirements
Core Components for Ethical Research Implementation
Table: Essential Toolkit for Ethical Research Compliance
| Toolkit Component | Function | Ethical Principle Served |
|---|---|---|
| Informed Consent Documents | Provide comprehensive information in plain language; document voluntary agreement | Respect for autonomy |
| Protocol Templates | Ensure proper study design, risk-benefit assessment, and scientific validity | Scientific integrity |
| Ethics Committee Application Forms | Facilitate protocol review, approval, and ongoing monitoring | Institutional oversight |
| Data Safety Monitoring Plans | Identify, monitor, and manage risks to participants | Beneficence, non-maleficence |
| Confidentiality Safeguards | Protect participant privacy through data encryption, coding, and access controls | Respect for privacy |
| Vulnerability Assessment Tools | Identify vulnerable populations; implement additional protections | Justice |
| Adverse Event Reporting Systems | Document and manage research-related harms | Responsibility, reparations |
| Participant Education Materials | Enhance comprehension through visual aids, simplified summaries | Understanding consent |
| Cloperastine Fendizoate | Cloperastine Fendizoate | |
| Fenspiride Hydrochloride | Fenspiride Hydrochloride, CAS:5053-08-7, MF:C15H21ClN2O2, MW:296.79 g/mol | Chemical Reagent |
Implementation Framework for Ethical Requirements
Diagram: Ethical Research Implementation Workflow
The Nuremberg Code and Declaration of Helsinki continue to serve as foundational documents for modern research ethics, directly responding to historical abuses while providing adaptable frameworks for emerging ethical challenges. Their creation established the non-negotiable principle that scientific progress must never supersede individual rights and welfare [18] [16].
Quantitative research demonstrates that while awareness of ethical requirements is generally high, practical adherence remains variable, with particular weaknesses in procedural compliance such as obtaining ethics approval before data collection [19]. This implementation gap highlights the ongoing need for structural support, education, and cultural transformation within research institutions to fully realize the protections envisioned by these landmark documents.
The evolution of these ethical frameworks continues through periodic revisions of the Declaration of Helsinki and the development of supplementary guidelines addressing contemporary issues like biobanking and digital health data [16] [17]. This dynamic character ensures that research ethics remains responsive to new challenges while maintaining its fundamental commitment to protecting human dignity—the core principle that directly responds to the unethical research that necessitated its creation.
The Tuskegee Study and its Lasting Impact on U.S. Regulations
The U.S. Public Health Service (PHS) Untreated Syphilis Study at Tuskegee, conducted from 1932 to 1972, stands as a pivotal case of ethical failure in medical research that directly catalyzed the development of modern informed consent requirements and human subject protections in the United States [20]. This 40-year study, intended to observe the natural history of untreated syphilis in 399 African American men alongside 201 uninfected controls, systematically violated ethical principles through its deliberate denial of information and treatment, even after penicillin became the standard therapy for syphilis in 1947 [21] [22]. The study's revelation in 1972 triggered public outrage, leading to congressional hearings and fundamental reforms that established the contemporary regulatory framework governing clinical research [23] [24]. This whitepaper examines the Tuskegee Study's specific ethical violations, analyzes the resulting regulatory transformations, and details the current informed consent requirements that research professionals must implement to ensure ethical conduct in human subjects research.
Experimental Design and Methodological Flaws
Study Protocol and Timeline
The Tuskegee Study was initiated by the U.S. Public Health Service Venereal Disease Division under Dr. Taliaferro Clark, who originally envisioned a six-month descriptive epidemiological study [21] [22]. The study aimed to document the progression of untreated syphilis in African American men in Macon County, Alabama, building upon the retrospective Oslo Study of Untreated Syphilis in white males [21]. Researchers hypothesized that syphilis manifested differently by race, specifically believing it affected the cardiovascular system more than the central nervous system in Black individuals [21].
Table 1: Tuskegee Study Timeline and Key Methodological Events
| Year | Event | Impact on Methodology |
|---|---|---|
| 1932 | Study initiation | 600 African American sharecroppers enrolled (399 with latent syphilis, 201 controls) [21] |
| 1932-1933 | Initial data collection | Subjects studied for 6-8 months with disguised placebos, ineffective treatments, and diagnostic procedures presented as therapeutic interventions [21] |
| 1936 | First major report published | Clinical data publicly disseminated without ethical critique from medical community [21] [24] |
| 1943-1945 | Penicillin established as treatment | Effective treatment deliberately withheld from subjects despite widespread availability [21] [22] |
| 1947 | PHS establishes rapid treatment centers | Study participants actively prevented from accessing treatment programs [21] |
| 1972 | Study terminated after public exposure | Press leak leads to investigation and ultimate termination [21] [20] |
Participant Recruitment and Deception Strategies
Investigators employed systematic deception in recruiting and retaining participants throughout the study's duration. Participants were impoverished African American sharecroppers from Macon County, Alabama, who were promised free medical care, meals, and burial insurance as incentives for participation [21] [22]. Critically, researchers never informed subjects of their syphilis diagnosis, instead telling them they were being treated for "bad blood," a colloquial term encompassing various conditions including anemia and fatigue [21] [23].
To obtain compliance with invasive procedures, researchers implemented several deceptive practices:
- Lumbar punctures were misrepresented as "special free treatment" [21] [22]
- Placebo treatments (vitamin tonics, aspirin) were administered to maintain the illusion of therapy [21]
- Burial stipends were offered to secure permission for autopsies, which were essential to the study's pathological aims [22]
When subjects encountered opportunities for legitimate treatment—such as during World War II military induction where 256 subjects were diagnosed with syphilis—PHS researchers actively intervened to prevent treatment, arguing that preserving the study was scientifically paramount [21].
Quantitative Impact and Outcomes
The human cost of the Tuskegee Study's methodological violations was substantial and extended beyond the enrolled participants to their families and communities.
Table 2: Documented Harms from the Tuskegee Study (1932-1972)
| Category of Harm | Number Affected | Details and Context |
|---|---|---|
| Direct participant mortality | 28-100+ men | At least 28 died directly from syphilis; 100 from related complications [21] [23] |
| Surviving participants (1972) | 74 men | Only 74 of original 399 syphilitic subjects alive at study termination [21] |
| Wife infections | 40 women | Secondary transmission to spouses [21] |
| Congenital syphilis cases | 19 children | Infected born to subjects' offspring [21] |
| Settlement recipients (1974) | Not specified | $10 million settlement: living syphilitic participants ($37,500), heirs of deceased ($15,000), living controls ($16,000), heirs of deceased controls ($5,000) [20] |
Ethical Violations and Regulatory Response
Core Ethical Failures
The Tuskegee Study violated fundamental ethical principles through multiple mechanisms that would later form the foundation of modern research ethics frameworks:
- Complete Absence of Informed Consent: Participants were never informed about their diagnosis, the study's purpose, or the risks involved [20] [22]. They were systematically deceived throughout the study's 40-year duration [24].
- Withholding of Effective Treatment: Researchers deliberately withheld penicillin treatment after it became widely available and established as the standard of care in 1947 [21] [23]. They actively prevented participants from accessing treatment through other sources [22].
- Exploitation of Vulnerable Population: The study targeted impoverished, poorly educated African American sharecroppers who had limited access to healthcare and limited understanding of research protocols [21] [22].
- Deliberate Deception: Researchers misrepresented diagnostic procedures as therapeutic interventions and used the term "bad blood" to obscure the true nature of the disease [21].
- Harm to Third Parties: Researchers took no steps to prevent infection of participants' wives or children, extending the study's harm beyond the enrolled subjects [21].
Regulatory Transformation and Legacy
The public exposure of the Tuskegee Study in 1972 triggered immediate reforms that fundamentally reshaped the U.S. research regulatory landscape:
Key Regulatory Developments:
- National Research Act (1974): Mandated institutional review boards (IRBs) for all federally funded research involving human subjects [23].
- Belmont Report (1979): Established three fundamental ethical principles for research: respect for persons (including informed consent), beneficence (minimizing harm while maximizing benefits), and justice (fair distribution of research burdens and benefits) [22] [24].
- Office for Human Research Protections (OHRP): Created within the Department of Health and Human Services to oversee and enforce ethical standards in human subjects research [21].
- Federal Informed Consent Requirements: Codified requirements for comprehensive informed consent documents and processes [25].
Contemporary Informed Consent Framework
Core Elements of Valid Informed Consent
Current FDA regulations and ethical guidelines mandate that informed consent processes ensure potential participants make voluntary, informed decisions about research participation [25]. The NIH outlines seven guiding principles for ethical research, with informed consent representing a central component [25].
Table 3: Essential Elements of Informed Consent Based on Tuskegee Lessons
| Consent Element | Regulatory Requirement | Tuskegee Violation Addressed |
|---|---|---|
| Study Purpose Disclosure | Clear explanation of research goals, expected duration, and procedures [25] | Participants told study was for "bad blood" treatment rather than observation of untreated syphilis [21] |
| Risks and Benefits | Comprehensive description of reasonably foreseeable risks and potential benefits [25] | Risks of untreated syphilis (blindness, deafness, mental illness, death) never disclosed [21] |
| Alternative Procedures | Disclosure of appropriate alternative procedures or courses of treatment [25] | Penicillin treatment actively withheld and concealed after 1947 [22] |
| Voluntary Participation | Clear statement that participation is voluntary and refusal involves no penalty [25] | Economic incentives and deception used to secure participation and prevent withdrawal [21] |
| Continuing Information | Provision of new information that might affect participation decisions [25] | Participants never informed about availability of penicillin treatment [21] |
Institutional Implementation Framework
The modern research protection system requires multiple layers of oversight to prevent ethical violations:
The Researcher's Toolkit: Essential Components for Ethical Research
Table 4: Essential Resources for Ethical Clinical Trial Management
| Resource Category | Specific Components | Application and Purpose |
|---|---|---|
| Regulatory Guidance | FDA Informed Consent Guidance (2023) [26]; ICH E6(R2) Good Clinical Practice [26] | Provides current agency thinking on informed consent processes and GCP standards |
| Ethical Frameworks | Belmont Report Principles [22] [24]; NIH Guiding Principles for Ethical Research [25] | Foundation for ethical decision-making throughout research lifecycle |
| Vulnerable Population Protections | FDA Guidance on Enhancing Diversity in Clinical Trials [26]; Ethical Considerations for Children [26] | Special safeguards for vulnerable groups to prevent exploitation |
| Documentation Systems | Electronic Informed Consent Systems [26]; IRB Written Procedures [26] | Ensures proper consent documentation and institutional compliance |
| Monitoring Mechanisms | Risk-Based Monitoring Approaches [26]; Clinical Investigator Disqualification Procedures [26] | Ongoing oversight to ensure participant safety and protocol adherence |
| Fenspiride | Fenspiride, CAS:5053-06-5, MF:C15H20N2O2, MW:260.33 g/mol | Chemical Reagent |
| Hydroxybupropion | Hydroxybupropion, CAS:92264-81-8, MF:C13H18ClNO2, MW:255.74 g/mol | Chemical Reagent |
The Tuskegee Study's legacy continues to influence modern clinical trial design and regulatory approaches. Recent FDA guidance on decentralized clinical trials emphasizes maintaining rigorous informed consent standards while increasing patient access and convenience [27]. Ongoing initiatives to enhance diversity in clinical trials directly address Tuskegee's exploitation of vulnerable populations by promoting equitable inclusion without sacrificing protection [26]. The continued emphasis on ethical research design as outlined in NIH's guiding principles—including social value, scientific validity, and independent review—represents the institutionalization of lessons learned from Tuskegee [25].
For contemporary researchers and drug development professionals, understanding the Tuskegee Study's history is not merely an academic exercise but a fundamental requirement for conducting ethically sound research. The regulatory framework and ethical principles that emerged from this tragic chapter provide essential protections for both research participants and the integrity of the scientific enterprise, ensuring that such systematic ethical failures remain historical lessons rather than contemporary practices.
Informed consent serves as a critical bridge between theoretical ethical principles and practical application in research and clinical care. For researchers, scientists, and drug development professionals, understanding the core ethical tenets that underpin this process is not merely a regulatory obligation but a fundamental component of ethical scientific practice. This guide examines the principles of autonomy, non-domination, and personal integrity within the specific context of the historical development and contemporary requirements of informed consent. These principles collectively ensure that respect for the individual participant remains central to the scientific endeavor, particularly in pharmaceutical medicine where competing interests between healthcare objectives and industrial priorities often arise [28]. The evolution of these concepts from philosophical foundations to codified regulations reflects an ongoing commitment to protecting human dignity in research and practice, with their proper application being essential for maintaining public trust and scientific integrity.
Foundational Ethical Principles
The ethical framework governing human subjects research and clinical practice rests on several well-established principles. These principles, while distinct, function as an integrated system to guide ethical decision-making.
The Principle of Autonomy
Autonomy is defined by the right to self-determination and respects an individual's capacity to make informed decisions based on their personal values and beliefs [29] [30] [31]. The philosophical basis for autonomy, as interpreted by philosophers such as Immanuel Kant and John Stuart Mill, is that all persons have intrinsic and unconditional worth and therefore should have the power to make rational decisions and moral choices [29]. This principle was powerfully affirmed in the 1914 court case Schloendorff v. Society of New York Hospital, where Justice Cardozo declared, "Every human being of adult years and sound mind has a right to determine what shall be done with his own body" [29] [12]. In practical application, autonomy requires more than merely obtaining a signature on a document; it demands a continuous process of respect throughout the research or treatment relationship [31]. This includes providing potential participants with all relevant information in a comprehensible manner, ensuring they are not manipulated or unduly pressured, and guaranteeing their right to withdraw consent without penalty [13] [31]. The principle of autonomy directly gives rise to and supports the practices of informed consent, truth-telling, and confidentiality [29].
The Principle of Non-Maleficence
Non-maleficence, often referred to as the "no harm principle," is the obligation to avoid causing harm to others [29] [30] [31]. This principle can be traced back to the Hippocratic oath's injunction to "help and do no harm" and supports several specific moral rules: do not kill, do not cause pain or suffering, do not incapacitate, do not cause offense, and do not deprive others of the goods of life [29]. In a research context, non-maleficence sets clear limits on the risks, inconveniences, and burdens to which participants may be subjected, even if a project has the potential to create significant social value [31]. This principle prioritizes the interests of the individual over the interests of wider society when it comes to actively exposing participants to physical, psychological, economic, or social harm [31]. The practical application of non-maleficence requires researchers to carefully weigh the benefits against the burdens of all interventions, to eschew those that are inappropriately burdensome, and to choose the course of action that best protects the participant from harm [29].
The Interconnected Principles of Beneficence and Justice
While autonomy and non-maleficence are primary, they operate in concert with the related principles of beneficence and justice.
Beneficence: This principle is the obligation to act for the benefit of others, helping them to advance their legitimate interests [29] [30]. In research and clinical care, beneficence involves more than just avoiding harm; it requires active efforts to secure the well-being of participants and patients [32]. This is expressed through two complementary rules: (1) do not harm and (2) maximize possible benefits and minimize possible harms [32]. For research to be ethical, it must create sufficient value—whether for the individual participant's health or for broader societal knowledge—to justify the risks and burdens involved [31].
Justice: The principle of justice addresses fairness in the distribution of benefits and burdens of research [30] [32]. It demands that the research population generally coincide with the population that will benefit from the research, ensuring that one group does not bear the risks for the benefit of another [31]. Justice also requires that vulnerable populations are not unnecessarily included in research, that participants are compensated for expenses related to their participation, and that active efforts are made to enroll members of underrepresented groups so that all can share in the benefits of research [31] [32]. An injustice occurs when a benefit to which a person is entitled is denied without good reason or when a burden is imposed unduly [32].
Table 1: Summary of Core Ethical Principles in Research
| Principle | Core Meaning | Practical Application in Research | Derivative Concepts |
|---|---|---|---|
| Autonomy | Respect for an individual's right to self-determination [29] [30] | Informed consent process, right to withdraw, continuous respect for participant decisions [31] | Informed consent, truth-telling, confidentiality [29] |
| Non-Maleficence | The obligation not to inflict harm on others [29] [30] | Risk-benefit assessment, setting limits on participant risks and burdens [31] | Do not cause pain, suffering, or incapacitate [29] |
| Beneficence | The obligation to act for the benefit of others [29] [32] | Ensuring research has social value, maximizing benefits while minimizing harms [31] [32] | Protect and defend rights, prevent harm, help persons with disabilities [29] |
| Justice | Fairness in the distribution of benefits and burdens [31] [32] | Equitable selection of subjects, fair compensation, avoiding exploitation of vulnerable groups [31] | Fair treatment, non-discrimination, equitable access to research benefits [30] |
The Historical Development of Informed Consent
The concept of informed consent has evolved significantly from a foundational ethical principle to a codified legal and regulatory requirement. Its history is marked by landmark legal cases and responses to ethical abuses in human subjects research.
Early Legal Foundations (1905-1914)
The legal groundwork for informed consent was established in the early 20th century through a series of court decisions that affirmed the principle of patient autonomy, often with female plaintiffs at a time when women lacked the right to vote [12].
- Mohr v Williams (1905): The plaintiff consented to an operation on her right ear, but the surgeon, upon finding the left ear more severely affected after anesthesia, operated on the left without consent. The Minnesota Supreme Court ruled that the surgeon should have obtained consent before changing the surgical plan, establishing that performing a different procedure than the one consented to constitutes battery [12].
- Pratt v Davis (1905): A surgeon performed a hysterectomy on a patient with epilepsy without her consent and intentionally misled her about the purpose of the operation, claiming her condition made her incompetent. The Illinois appellate court decided in favor of the patient, stating that a citizen has "the right to the inviolability of his person" which "forbids a physician or surgeon" to violate without permission [12].
- Schloendorff v Society of New York Hospital (1914): This case culminated in Justice Cardozo's famous dictum: "Every human being of adult years and sound mind has a right to determine what shall be done with his own body" [29] [12]. This ruling legally solidified the principle of patient autonomy and the requirement for consent.
The Birth of "Informed Consent" and Research Ethics (1947-1957)
The mid-20th century saw the formal naming of "informed consent" and the extension of its principles from clinical practice to human subjects research, largely in response to grave ethical violations.
- The Nuremberg Code (1947): Developed in the aftermath of the Nazi war crimes trials, the Nuremberg Code represents the first international effort to regulate human experimentation [12]. Its first and most prominent principle is the requirement for voluntary consent, which it elaborates must be given by an individual with "sufficient knowledge and comprehension of the elements of the subject matter involved as to enable him to make an understanding and enlightened decision" [12]. The Code specifies that the participant must be informed of the nature, duration, purpose, methods, inconveniences, hazards, and potential effects on health [12].
- Salgo v Leland Stanford Jr University Board of Trustees (1957): This case marked the first recorded use of the term "informed consent" [12]. The California appellate court ruled that physicians have a duty to disclose potential risks and hazards to patients, establishing liability for failing to provide the information necessary for a patient to make an informed decision [12].
Codification into Regulation and Law (1979-Present)
The latter half of the 20th century saw the formal codification of informed consent principles into US federal policy and international guidelines.
- The Belmont Report (1979): This report, developed in response to unethical US research practices (such as the Tuskegee Syphilis Study), identified three core principles for ethical research: Respect for Persons (which incorporates autonomy), Beneficence, and Justice [32]. It served as the foundation for US federal regulations [28].
- The Common Rule (1991, revised 2018): The Federal Policy for the Protection of Human Subjects (the "Common Rule") codified informed consent requirements into US law [12]. The 2018 revisions introduced the requirement for a "key information" section at the beginning of consent forms—a concise, focused presentation to facilitate participant comprehension—though the lack of specific guidance on its format has presented implementation challenges [12].
Table 2: Historical Milestones in the Development of Informed Consent
| Year | Event/Case | Significance | Core Ethical Principle Affirmed |
|---|---|---|---|
| 1905-1914 | Series of legal cases (Mohr, Pratt, Schloendorff) | Established the legal principle of patient autonomy and bodily integrity [12] | Autonomy |
| 1947 | Nuremberg Code | First international document to mandate voluntary consent for human experimentation [12] | Autonomy, Non-maleficence |
| 1957 | Salgo v Leland Stanford | First use of the term "informed consent"; established duty to disclose risks [12] | Autonomy |
| 1979 | The Belmont Report | Defined three core principles for ethical research: Respect for Persons, Beneficence, Justice [32] | Autonomy, Beneficence, Justice |
| 1991/2018 | The Common Rule (and revisions) | Codified US federal regulations for human subjects research; 2018 revision added "key information" requirement [12] | Autonomy, Beneficence, Justice |
Contemporary Requirements and Applications
Modern informed consent is a dynamic communication process rather than a single event. For drug development professionals, understanding its legal standards and practical challenges is essential for ethical conduct and regulatory compliance.
Core Elements of Valid Informed Consent
For consent to be ethically and legally valid, several conditions must be met, evolving from the foundational principles outlined in the Nuremberg Code and subsequent regulations [13]:
- Decision-making Capacity: The patient or subject must be competent to understand the information presented and to make a voluntary decision [29] [13].
- Full Disclosure: The clinician or researcher must provide comprehensive information about the nature of the procedure or intervention, its risks and benefits, and reasonable alternatives [29] [13].
- Adequate Comprehension: The patient or subject must understand the disclosure. This requires information to be presented in clear, understandable language appropriate to their health literacy level [29] [13].
- Voluntariness: The decision must be made freely without coercion, manipulation, or undue influence [13].
Legal Standards for Disclosure
The standard for what constitutes adequate disclosure for informed consent varies by jurisdiction, with three primary legal approaches [13]:
- Subjective Patient Standard: What does this particular patient need to know and understand to make an informed decision? This standard is highly individualized.
- Reasonable Patient Standard: What would the average patient need to know to be an informed participant in the decision? This is the most commonly used standard as it focuses on typical patient needs [13].
- Reasonable Clinician Standard: What would a typical clinician disclose about this procedure? This standard is less common as it is more provider-centered.
Challenges in the Informed Consent Process
Despite its ethical and legal importance, the practical implementation of informed consent faces several significant challenges, particularly in global drug development [13]:
- Patient Comprehension: Complex medical jargon and varying health literacy levels can prevent true understanding. Studies have shown inadequacies in functional health literacy among hospitalized patients, compromising the consent process. Solutions include using plain language, the teach-back method, and graphical tools [13].
- Language and Cultural Barriers: In diverse populations, language barriers necessitate the use of professional medical interpreters. Cultural differences also impact decision-making, as some cultures prefer family-centered rather than individual-centered consent [13].
- Power Dynamics: The inherent power imbalance between clinicians/researchers and patients/subjects can make individuals feel pressured to consent. This is particularly problematic in vulnerable populations [13].
- Documentation Issues: Inadequate documentation leaves professionals vulnerable to legal action. One study found that the four required elements of consent (nature, risks, benefits, alternatives) were documented on forms only 26.4% of the time [13].
Ethical Principles in Pharmaceutical Medicine
The pharmaceutical industry operates at the intersection of healthcare ethics and industrial interests, creating unique ethical challenges that demand a specialized framework.
The IFAPP Ethics Framework
Recognizing the specific ethical dilemmas faced by professionals in pharmaceutical medicine, the International Federation of Associations of Pharmaceutical Physicians and Pharmaceutical Medicine (IFAPP) developed a specific International Code of Ethical Conduct [28]. This code emphasizes that pharmaceutical physicians must "recognize their ethical responsibility and stand aside from product loyalty when assessing factors affecting the product itself," acknowledging that this position "may demand considerable determination" when balancing competing interests [28]. The framework is built on core values that include the duty of care, competence and diligence, impartiality, probity, integrity, and accountability [28].
Core Values and Practical Application
The IFAPP framework translates ethical principles into practical guidance for the entire medicine development lifecycle [28]:
- Duty of Care: This extends beyond clinical research participants to include designing scientifically valid trial protocols that prioritize participant interests over corporate goals and providing accurate medical information to company management [28].
- Integrity and Impartiality: Pharmaceutical professionals must ensure the accurate and verifiable interpretation of research findings and manage the communication of safety information with impartiality, regardless of commercial impact [28].
- Competence and Accountability: Maintaining high scientific standards and professional competence is an ethical obligation. Professionals are accountable for the accurate representation of clinical trial data in regulatory documents and marketing materials [28].
Practical Implementation: A Scientist's Toolkit
Essential Research Reagent Solutions
Table 3: Key Research Reagents and Materials for Ethical Research Practice
| Item/Tool | Primary Function in Ethical Research |
|---|---|
| Informed Consent Forms (ICFs) | Document the consent process; required by regulators to include nature of procedure, risks, benefits, and alternatives [13] |
| Health Literacy Assessment Tools | Screen patient comprehension to ensure understanding of complex medical information [13] |
| Plain Language Summaries | Enhance participant understanding by replacing medical jargon with accessible language [13] |
| Professional Medical Interpreter Services | Overcome language barriers to ensure accurate communication and valid consent [13] |
| Interactive Multimedia Aids | Improve shared decision-making and risk comprehension through visual and interactive formats [13] |
| Ethics Committee/IRB Protocols | Ensure study design adheres to ethical principles before participant enrollment [29] [28] |
| 1-(3-Chlorophenyl)-2-hydroxypropan-1-one | 1-(3-Chlorophenyl)-2-hydroxypropan-1-one, CAS:152943-33-4, MF:C9H9ClO2, MW:184.62 g/mol |
| Citalopram Hydrobromide | Citalopram Hydrobromide, CAS:59729-32-7, MF:C20H22BrFN2O, MW:405.3 g/mol |
Ethical Decision-Making Framework
The following diagram illustrates the integrated relationship between core ethical principles and their practical application in the informed consent process, particularly within pharmaceutical development:
This framework demonstrates how abstract ethical principles translate into concrete research requirements, guiding professionals in implementing ethically sound practices throughout the research lifecycle.
The core ethical principles of autonomy, non-maleficence, beneficence, and justice provide an indispensable foundation for informed consent and ethical research practice. For drug development professionals, these principles are not abstract concepts but practical guides that must be integrated into daily work, especially when navigating the complex interface between industrial interests and patient welfare. The historical development of informed consent reveals a consistent progression toward greater recognition of participant autonomy and protection from harm, culminating in comprehensive regulatory frameworks like the Common Rule and specialized codes such as the IFAPP Ethics Framework. As scientific research grows increasingly complex and globalized, maintaining fidelity to these ethical principles becomes both more challenging and more critical. The ongoing commitment to rigorous ethical practice—ensuring valid informed consent, protecting participant welfare, and maintaining scientific integrity—is essential for sustaining public trust and advancing medical science for the benefit of all.
The Evolution from Simple Consent to a Communication-Centered Process
Informed consent has undergone a profound transformation from a simple signature on a document to a dynamic, communication-centered process that respects patient autonomy and promotes shared decision-making. This evolution represents a fundamental shift in medical ethics, moving away from paternalistic models toward patient-centered care that prioritizes transparency, comprehension, and trust. The contemporary informed consent process ensures patients are fully educated about procedures, interventions, potential risks, benefits, and alternative treatments, enabling them to make voluntary, informed decisions about their care [13]. This whitepaper examines the historical context, current regulatory landscape, methodological frameworks, and future directions of informed consent, with particular relevance to researchers, scientists, and drug development professionals operating in increasingly complex clinical environments.
The significance of this evolution extends beyond ethical compliance; it directly impacts research quality, participant engagement, and trial outcomes. As clinical trials grow more complex and patient populations more diverse, the communication-centered approach to informed consent becomes increasingly critical for ensuring genuine understanding and voluntary participation. Recent regulatory guidance emphasizes true participant comprehension rather than mere procedural compliance, reflecting this fundamental shift in perspective [33].
Historical Development and Ethical Foundations
The conceptual foundation of informed consent has evolved significantly through key historical milestones that established its current ethical and legal standing. The early 20th century was characterized by medical paternalism, where clinicians made treatment decisions without necessarily informing patients of details. The pivotal 1914 case of Schloendorff v. Society of New York Hospital established the foundational principle that "every human being of adult years and sound mind has a right to determine what shall be done with his own body," establishing the legal precedent for patient autonomy [13].
The mid-20th century witnessed further development driven by responses to ethical violations in medical research. The Nuremberg Code and Declaration of Helsinki emerged as direct consequences of the Nazi human experiments during World War II and other unethical research practices, including the Tuskegee Study of Untreated Syphilis in the Negro Male [13]. These documents cemented informed consent as a fundamental ethical standard in both research and clinical practice, establishing frameworks that prioritized voluntary participation and comprehensive understanding.
The late 20th and early 21st centuries have focused on refining the consent process to enhance patient comprehension and engagement. This period has seen a shift from viewing consent as a one-time event to understanding it as an ongoing communication process. Technological advances, diverse patient populations, and growing emphasis on shared decision-making have further transformed informed consent into the complex, communication-centered process it is today [13].
Table: Historical Milestones in Informed Consent Evolution
| Time Period | Key Development | Impact on Consent Practice |
|---|---|---|
| Early 20th Century | Schloendorff v. Society of New York Hospital (1914) | Established legal principle of bodily autonomy |
| Mid-20th Century | Nuremberg Code (1947) | Established voluntary consent as absolute requirement |
| Mid-20th Century | Declaration of Helsinki (1964) | Codified ethical principles for human research |
| Late 20th Century | Growing patient rights movement | Shift from paternalism to patient participation |
| 21st Century | Digital technologies and AI | New challenges for comprehension and transparency |
Current Regulatory Framework and Guidelines
The contemporary regulatory landscape for informed consent reflects the evolution toward communication-centered approaches, with recent guidelines emphasizing comprehension and patient engagement. The SPIRIT 2025 statement provides updated evidence-based recommendations for clinical trial protocols, emphasizing transparency and complete protocol content to benefit investigators, trial participants, and other stakeholders [34]. This guidance includes a checklist of 34 minimum items to address in trial protocols, reinforcing comprehensive informed consent processes.
Regulatory bodies internationally are shifting focus from merely meeting informed consent requirements to ensuring true participant comprehension. The International Council for Harmonisation (ICH), Food and Drug Administration (FDA), European Union (EU), and National Health Service (NHS) have updated guidelines emphasizing plain language, non-technical terms, and visual aids to make consent forms understandable to lay audiences [33]. This regulatory evolution aligns with a broader movement toward patient-centered research where informed consent is recognized as a dynamic, communicative process rather than a legal formality.
The updated SPIRIT 2025 statement introduces significant enhancements including a new open science section, additional emphasis on assessment of harms and description of interventions, and a crucial new item on how patients and the public will be involved in trial design, conduct, and reporting [34]. These changes reflect the growing recognition that effective informed consent requires ongoing engagement rather than single-point documentation.
Core Components of Modern Informed Consent
Essential Elements and Documentation Standards
Effective informed consent processes in both clinical practice and research must address several core components to meet ethical and regulatory standards. The Joint Commission requires specific elements be documented in a form, progress notes, or elsewhere in the record [13]. These essential elements create a comprehensive framework for communication between researchers and participants.
The necessary components for documentation include: (1) the nature of the procedure or intervention; (2) the risks and benefits of the procedure or intervention; (3) reasonable alternatives; (4) the risks and benefits of alternatives; and (5) an assessment of the patient's understanding of these elements [13]. Each component plays a vital role in ensuring participants genuinely comprehend what their involvement entails.
Recent scholarship has redefined the functional meaning of informed consent to include the intersection of values such as autonomy and non-domination, followed by self-ownership and personal integrity. This framework suggests informed consent primarily functions as the protection of self-sovereignty over one's own body, emphasizing why comprehensive communication is fundamental rather than procedural [13].
Legal Standards for Adequate Disclosure
The specific state or jurisdiction determines the required standard for adequate informed consent, with three primary legal approaches recognized [13]. Understanding these standards is crucial for researchers designing consent processes that meet regulatory requirements while effectively communicating with participants.
Table: Legal Standards for Adequate Informed Consent Disclosure
| Standard | Focus Question | Application Context |
|---|---|---|
| Subjective Standard | What does this specific patient need to know and understand to make an informed decision? | Highly individualized approach focusing on particular patient's needs |
| Reasonable Patient Standard | What does the average patient need to know to be an informed participant in the decision? | Most common approach; focuses on typical information needs |
| Reasonable Clinician Standard | What would a typical clinician say about this procedure? | Profession-centered perspective; less commonly used |
Many states utilize the reasonable patient standard because it focuses on what a typical patient needs to know to understand the decision at hand. This approach balances standardization with patient-centeredness, providing a framework that can be consistently applied while prioritizing information most relevant to decision-making [13].
Methodological Approaches and Implementation Strategies
Enhancing Patient Comprehension and Engagement
Multiple methodological approaches have been developed to enhance patient understanding and engagement during the informed consent process. These strategies are particularly important given that complex medical jargon and varying levels of health literacy often result in patients agreeing to procedures without fully understanding risks, benefits, or alternatives [13].
The teach-back method has emerged as a particularly effective technique for assessing patient comprehension. This approach involves asking patients to explain in their own words what they have been told about their procedure, risks, benefits, and alternatives. This method helps both patients and clinicians concentrate on essential aspects of the information and identifies areas requiring further clarification [13]. Studies demonstrate that implementing health literacy-based consent forms and processes improves patient-provider communication, increases patient comfort in asking questions, and encourages more effective dialogue in perioperative settings [13].
Interactive media and graphical tools represent another promising approach for improving shared decision-making and effectively presenting risks. Research indicates these methods appear superior in improving patient comprehension compared to traditional approaches [13]. Additionally, encouraging active patient participation through engagement techniques and open-ended questions provides valuable insights into patient needs and preferences, creating more interactive dialogue.
Addressing Implementation Challenges
Despite established methodologies, several implementation challenges can compromise consent effectiveness. Language barriers and inadequate use of interpreters complicate consent processes, particularly in diverse populations [13]. Implementing professional medical interpreter services for patients with limited language proficiency and American Sign Language (ASL) interpreters for hearing-impaired patients ensures clear, accurate communication.
Cultural differences present another significant challenge, as decision-making norms vary across cultures. In some cultures, decisions are made collectively rather than individually, and written consent may be perceived as mistrust [13]. Undocumented immigrants might hesitate to sign forms due to deportation fears, while other cultures involve consulting family patriarchs in decision processes [13].
Power dynamics and perceived authority between patients and clinicians may pressure patients to consent without fully understanding or agreeing with procedures. This issue is particularly problematic in vulnerable populations, including older individuals, those with disabilities, or incarcerated persons [13]. Additionally, documentation inadequacies persist, with one study finding that the four required elements of informed consent were documented on consent forms only 26.4% of the time [13].
Digital Transformation and Innovative Approaches
Digital Tools and AI Applications
Digitalization of the informed consent process presents remarkable opportunities for enhancing patient understanding and streamlining workflows. A 2025 scoping review of digital consent processes found that digitalization can enhance recipients' understanding of clinical procedures, potential risks, benefits, and alternative treatments [35]. The review analyzed 27 studies and identified various technologies being implemented, including web-based platforms, interactive applications, and chatbot systems.
Evidence regarding digital tools' impact on patient satisfaction, convenience, and perceived stress is mixed, though healthcare professionals primarily benefit from time savings [35]. Recent advances in artificial intelligence have introduced AI-based technologies for consent processes, though the review notes these systems do not yet seem suitable for use without medical oversight [35]. This suggests that while digital tools show significant promise, human supervision remains essential.
Chatbot systems have demonstrated particular potential in consent processes. Studies show positive findings regarding acceptability of chatbots for conveying information to patients, with some research indicating a preference for chatbot responses to patient questions over physician responses in social media forums [35]. Additionally, chatbot implementation may generate time savings for clinicians, potentially reducing burnout and enhancing efficiency [35].
Addressing AI-Specific Consent Challenges
AI-driven medicine introduces unique consent challenges that require adaptation of traditional frameworks. The complexity and opacity of AI technologies make it difficult for patients to fully comprehend how their data is used or how AI-driven decisions are made [36]. Most modern AI models operate as black-box systems, meaning their outputs are comprehensible but their inner workings are not, complicating transparency and true patient understanding [36].
The evolving nature of AI models creates additional consent challenges. Even if a patient consents to sharing their data for a specific purpose, these models typically incorporate data into all future predictions, evolving with it and blurring the limits of agreed use cases [36]. Regulatory frameworks like the EU AI Act attempt to address these concerns through risk-tiered approaches that require more stringent disclosure for higher-risk systems [36].
Emerging research suggests leveraging AI technologies themselves as part of the solution, revealing promising pathways for interdisciplinary work to support safe AI integration into healthcare [36]. Recent regulatory developments, including the EU's Opinion 28/2024 on safe data processing for AIs and updated OECD AI Principles, emphasize transparency and individual rights, indicating continued evolution in this area [36].
Research Reagents and Methodological Tools
Table: Essential Methodological Tools for Informed Consent Research
| Tool Category | Specific Examples | Research Application and Function |
|---|---|---|
| Comprehension Assessment | Teach-back method, Test/feedback questionnaires | Quantitatively measures patient understanding of consent information |
| Health Literacy Evaluation | REALM, TOFHLA, NVS | Assesses patient health literacy levels to tailor consent communication |
| Digital Consent Platforms | Web-based portals, Interactive apps, Chatbots | Delivers standardized consent information through engaging digital interfaces |
| Visual Aid Tools | Infographics, Risk communication graphics, Animated explanations | Enhances understanding of complex procedures and risk probabilities |
| Plain Language Resources | Health literacy review tools, Readability calculators | Ensures consent forms meet recommended reading level requirements |
Experimental Protocols and Evaluation Frameworks
Scoping Review Methodology for Digital Consent Tools
A rigorous scoping review conducted in 2025 provides a methodological framework for evaluating digital consent technologies. The review followed Joanna Briggs Institute (JBI) Manual for Evidence Synthesis guidance for scoping reviews and was reported according to PRISMA-ScR guidelines [35]. The systematic approach included searching multiple databases (Web of Science, EBSHCCOHost, PubMed, PubPsych) for articles published between January 2012 and June 2024.
The search strategy employed the PICO framework (Population, Intervention, Comparison, Outcome) to structure the eligibility criteria and search string [35]. The population category included health-related keywords; the intervention category incorporated digital technologies like chatbots, dialogue systems, voice assistants, and artificial intelligence; and the outcome category focused on patient information and consent [35]. The review specifically excluded general education and readability studies to maintain focus on digital enrichment of consent processes.
The screening process initially identified 4287 records, with title and abstract screening resulting in 27 studies meeting inclusion criteria for analysis [35]. This methodology provides a robust framework for researchers evaluating emerging consent technologies, emphasizing systematic search strategies, clear inclusion criteria, and transparent reporting of results.
Implementing Notification Approaches in Waiver Scenarios
For minimal-risk studies using waivers of informed consent, recent research highlights the value of implementing notification approaches to promote ethical values. Experts from the NIH Collaboratory's Ethics and Regulatory Core collaborated with investigators from several NIH Collaboratory Trials to describe methods of informing participants in minimal-risk research [37].
The investigators implemented various notification approaches, including letters and email campaigns, posters in waiting rooms and common areas, conversations with clinicians, and presentations at staff meetings [37]. The amount of information provided ranged from general statements about institutional research to detailed study information. The researchers concluded that providing information to participants should be the default for trials conducted under a waiver of research consent, as it promotes respect for persons, enhances understanding of research, and builds trust in research and researchers [37].
This approach represents an important evolution in consent practices, recognizing that even when formal consent is waived, communication with participants remains valuable. The methodology emphasizes case-by-case consideration of what information to disclose and how to disclose it, weighing costs, benefits, and feasibility for each study [37].
Visualizing the Modern Informed Consent Process
Diagram: Modern Consent as Continuous Communication Process This diagram visualizes informed consent as a continuous communication process rather than a single event. The process begins with preparation and initial discussion, moves through comprehension assessment using methods like teach-back, and continues through documentation and ongoing communication. Critical supporting elements include digital tools, health literacy considerations, and cultural adaptations that ensure the process remains patient-centered. The diagram highlights the iterative nature of modern consent, with feedback loops for clarification and updates when new information emerges.
The evolution from simple consent to a communication-centered process represents significant progress in medical ethics and patient-centered care. This transformation has redefined informed consent from a signature on a document to an ongoing dialogue that respects patient autonomy, promotes comprehension, and builds trust between patients and researchers. For drug development professionals and clinical researchers, understanding this evolution is crucial for designing ethical, compliant, and effective research protocols.
Future directions in informed consent will likely involve greater integration of digital tools, continued adaptation to AI challenges, and more sophisticated approaches to addressing health literacy disparities. The regulatory focus will continue shifting from mere compliance to demonstrated comprehension, requiring researchers to implement more robust assessment methods and patient-centered communication strategies. As technological advances accelerate, maintaining the fundamental ethical principles of respect for persons, beneficence, and justice will remain paramount while adapting consent processes to new research paradigms.
The communication-centered model of informed consent ultimately represents both an ethical imperative and a practical opportunity to enhance research quality. By prioritizing genuine understanding and engagement, researchers can build greater trust with participants, potentially improving recruitment, retention, and overall trial success while upholding the highest standards of research ethics.
Implementing Compliant Consent: A Step-by-Step Guide to Regulatory Requirements and Documentation
The ethical conduct of research involving human subjects is governed by two pivotal regulatory frameworks in the United States: 21 CFR Part 50 (Food and Drug Administration) and 45 CFR Part 46 (Department of Health and Human Services). These regulations, born from a history of ethical transgressions, establish the foundational requirements for informed consent and institutional oversight to safeguard the rights and welfare of individuals who participate in research [38]. While they share common ethical roots and many parallel requirements, key differences in their scope and application necessitate a thorough understanding by researchers, scientists, and drug development professionals.
The development of these regulations was catalyzed by infamous research abuses, such as the Nazi doctors' experiments and the U.S. Public Health Service's Study of Untreated Syphilis in the Negro Male (the Tuskegee Study) [38]. The resulting public outcry led to the creation of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research, which issued the Belmont Report in 1978 [38]. This report articulates the three key ethical principles—respect for persons, beneficence, and justice—that form the ethical bedrock for both 21 CFR 50 and 45 CFR 46 [38]. The application of these principles to research is realized through informed consent, assessment of risks and benefits, and the equitable selection of subjects.
Regulatory Scope and Jurisdictional Boundaries
A critical distinction between these regulations lies in their scope and jurisdictional authority. Understanding which regulation applies to a specific research activity is fundamental for regulatory compliance.
45 CFR Part 46, specifically Subpart A known as the "Common Rule," applies to all research involving human subjects that is conducted, supported, or otherwise subject to regulation by any federal department or agency that has adopted the policy [39] [40]. Its applicability is primarily tied to federal funding. Many institutions that receive federal funding agree to apply these regulations to all their research, regardless of the funding source, through a Federalwide Assurance (FWA) [38] [41].
21 CFR Part 50, in conjunction with 21 CFR Part 56 (IRB regulations), applies to clinical investigations involving products regulated by the FDA [42] [43]. This includes research on drugs for human use, medical devices, biological products, and food and color additives [42]. The applicability of FDA regulations is tied to the nature of the research (involving an FDA-regulated product) and is independent of federal funding [43].
Table 1: Comparative Scope of 21 CFR 50 and 45 CFR 46
| Feature | 21 CFR Part 50 (FDA) | 45 CFR Part 46 (HHS Common Rule) |
|---|---|---|
| Primary Jurisdiction | Research involving FDA-regulated products (drugs, devices, biologics, etc.) [42] | Federally conducted or supported research [39] |
| Key Trigger | Clinical investigation of a "test article" [42] | Receipt of federal funding or institutional FWA [38] |
| Definition of Research | Synonymous with "clinical investigation": Any experiment that involves a test article and a human subject [42] [43] | "A systematic investigation... designed to develop or contribute to generalizable knowledge" [43] |
| Definition of Human Subject | An individual who is a participant in research, either as a recipient of the test article or as a control [42] | A living individual about whom an investigator obtains data through intervention or interaction, or identifiable private information [43] |
| Assurance Requirement | Not required by FDA [41] | Required for HHS-conducted or supported research [41] |
Core Elements of Informed Consent
Both 21 CFR 50 and 45 CFR 46 mandate that informed consent be legally effective and prospectively obtained. The regulations specify core elements that must be provided to the subject or their legally authorized representative in language that is understandable to them [44].
Basic Elements of Informed Consent
The basic elements of informed consent are nearly identical between the two regulatory bodies. These elements are designed to provide a prospective subject with all information a reasonable person would want to know to make an informed decision about participation [44].
Table 2: Basic Elements of Informed Consent (per 45 CFR 46.116(b) and 21 CFR 50.25(a))
| Element Number | Requirement Description |
|---|---|
| 1 | A statement that the study involves research, an explanation of the purposes, expected duration of participation, description of procedures, and identification of any experimental procedures [44]. |
| 2 | A description of any reasonably foreseeable risks or discomforts [44]. |
| 3 | A description of any benefits to the subject or others that may reasonably be expected [44]. |
| 4 | A disclosure of appropriate alternative procedures or courses of treatment, if any, that might be advantageous [44]. |
| 5 | A statement describing the extent to which confidentiality of records will be maintained [44]. |
| 6 | For research involving more than minimal risk, an explanation of compensation and medical treatments available if injury occurs [44]. |
| 7 | Contact information for answers to questions about the research and research subjects' rights, and in the event of a research-related injury [44]. |
| 8 | A statement that participation is voluntary, refusal involves no penalty or loss of benefits, and the subject may discontinue at any time [44]. |
Additional Elements of Informed Consent
The regulations also stipulate additional elements of informed consent that must be provided when appropriate. These address specific scenarios that may not be applicable to all research studies.
Table 3: Additional Elements of Informed Consent (per 45 CFR 46.116(c) and 21 CFR 50.25(b))
| Element Number | Requirement Description |
|---|---|
| 1 | A statement that the procedure may involve unforeseeable risks to the subject (or embryo/fetus if pregnant) [44]. |
| 2 | Anticipated circumstances under which the investigator may terminate the subject's participation [44]. |
| 3 | Any additional costs to the subject resulting from participation [44]. |
| 4 | The consequences of a subject's decision to withdraw and procedures for orderly termination [44]. |
| 5 | A statement that significant new findings will be provided to the subject [44]. |
| 6 | The approximate number of subjects involved in the study [44]. |
| 7 | A statement about the potential for commercial profit from biospecimens and whether the subject will share in it [44]. |
| 8 | A statement regarding whether clinically relevant research results will be disclosed [44]. |
| 9 | For research involving biospecimens, whether it will include whole genome sequencing [44]. |
Key Regulatory Concepts and Variations
The Role and Requirements of Institutional Review Boards (IRBs)
Both regulations require research to be reviewed and approved by an Institutional Review Board (IRB) before initiation [41]. An IRB is a formally designated group tasked with reviewing research to protect the rights and welfare of human subjects [41]. The membership requirements for IRBs are identical under both sets of regulations, requiring at least five members with varying backgrounds, including at least one scientist, one non-scientist, and one member not otherwise affiliated with the institution [43] [41].
The criteria for IRB approval of research are also virtually identical. The IRB must determine that [38]:
- Risks to subjects are minimized.
- Risks are reasonable in relation to anticipated benefits.
- Selection of subjects is equitable.
- Informed consent will be sought and appropriately documented.
- The research plan provides for data safety monitoring when appropriate.
- There are adequate provisions to protect subject privacy and data confidentiality.
Special Considerations: Waivers and Alterations
Both regulations provide mechanisms for IRBs to waive or alter certain consent requirements under specific, narrow conditions.
Under 45 CFR 46.116, an IRB may waive the requirement to obtain informed consent or approve a consent procedure that omits or alters some elements if the IRB finds and documents that [44]:
- The research involves no more than minimal risk to the subjects.
- The research could not practicably be carried out without the requested waiver or alteration.
- If the research involves identifiable private information or biospecimens, the research could not practicably be carried out without using such information or biospecimens in an identifiable format.
- The waiver or alteration will not adversely affect the rights and welfare of the subjects.
The FDA regulations have more restrictive provisions for waiver of consent. While the FDA does allow for an "alteration" of consent in certain emergency research settings, it does not include a general waiver provision comparable to the Common Rule for non-emergency research [43].
Documentation of Informed Consent
Both regulations generally require that informed consent be documented by a written consent form approved by the IRB and signed by the subject or their legally authorized representative [39]. However, both also allow for an IRB to waive the requirement for a signed consent form in certain circumstances, such as when the only record linking the subject to the research would be the consent document and a breach of confidentiality would be the primary risk [43].
Historical Evolution and the Path to Harmonization
The development of 21 CFR 50 and 45 CFR 46 is a story of converging ethical standards, driven by historical abuses and a growing consensus on the necessary protections for research subjects.
The Nuremberg Code (1947), developed in response to the Nazi experiments, established the absolute requirement for voluntary consent [38]. In the U.S., the Kefauver-Harris Drug Amendments of 1962 mandated that researchers obtain consent for investigational new drugs, though loopholes remained [38] [45]. The Surgeon General's policy in 1966 required institutions receiving Public Health Service funding to establish committees for human subject protection, forming the early IRB system [38].
The Belmont Report (1978) was a watershed moment, articulating the three ethical principles that underpin the modern regulations [38]. DHEW (later DHHS) elevated its policies to regulatory status in 1974, codifying them as 45 CFR 46 [38]. The FDA issued its own regulations, 21 CFR 50, in 1980, with a stated goal of harmonizing with the HHS rules wherever possible [45]. A significant step in this harmonization was the FDA's decision to eliminate the "therapeutic privilege" exemption that existed in earlier statutes, which had allowed investigators to withhold information if they judged it in the patient's best interest [45]. FDA concluded that this privilege had no place in the research setting due to its potential for abuse [45].
The adoption of the Federal Policy for the Protection of Human Subjects (the "Common Rule") by multiple federal agencies in 1991 further promoted uniformity, though the FDA, while making corresponding changes, did not adopt it in its entirety [38] [43]. This historical path explains the current state of significant overlap with nuanced differences between the two regulatory frameworks.
For researchers and drug development professionals, navigating the dual regulatory requirements of 21 CFR 50 and 45 CFR 46 requires a set of essential resources and methodologies to ensure compliance and uphold ethical standards.
Table 4: Essential Resources for Regulatory Compliance
| Tool or Resource | Function & Purpose | Regulatory Source |
|---|---|---|
| IRB Submission Kit | A standardized set of documents for IRB review, including the protocol, informed consent form, investigator brochure, and recruitment materials. Required for initial review by both FDA and Common Rule. | [41] |
| Federalwide Assurance (FWA) | A formal commitment to HHS that an institution will comply with 45 CFR 46 for all its research, regardless of funding source. Required for HHS-supported research. | [38] [41] |
| Informed Consent Checklist | A verification tool to ensure all required basic and additional elements are included in the consent document, facilitating IRB approval and ensuring regulatory compliance. | [44] |
| Bioresearch Monitoring Program (BIMO) | FDA's compliance program that includes inspections of clinical investigators, sponsors, IRBs, and nonclinical labs to ensure data integrity and subject protection. | [43] [45] |
| Expedited Review List | A categorization of research activities that may be reviewed by the IRB through an expedited procedure (by the chair or designees) rather than by the full convened board. | [43] |
| OHRP Decision Charts | Flowcharts from the Office for Human Research Protections to help determine if a project is human subjects research, requires IRB review, or is eligible for an exemption. | [39] |
The parallel structures of 21 CFR 50 and 45 CFR 46 represent a robust, though complex, system for protecting human research subjects. While harmonization has been a consistent goal, differences remain, primarily rooted in the distinct jurisdictional triggers of product regulation versus federal funding. For the research professional, a meticulous understanding of both frameworks is not merely a regulatory obligation but an ethical imperative. The historical context of these regulations—forged in response to profound ethical failures—underscores their critical role in ensuring that the pursuit of scientific knowledge never comes at the cost of fundamental human rights and dignity. As research methodologies continue to evolve, so too will these regulatory frameworks, requiring ongoing vigilance and education from the entire research community.
Core Elements of a Legally Effective Informed Consent Form
Informed consent serves as a fundamental pillar of ethical research and clinical practice, ensuring respect for individual autonomy and protecting participant rights. The concept has evolved significantly from its origins in early 20th-century legal cases to its current status as a complex regulatory requirement. This guide examines the core elements that constitute a legally effective informed consent form, framed within the context of its historical development and contemporary applications in research and drug development. For researchers and drug development professionals, understanding these elements is not merely a regulatory obligation but a crucial component of ethical study design and implementation. The informed consent process has transformed from a simple signature on a document to a comprehensive communication process between the researcher and participant, establishing trust and ensuring voluntary participation [13].
Historical and Regulatory Framework
Historical Evolution
The legal foundation for informed consent was established through a series of landmark court cases in the early 20th century. The 1914 case of Schloendorff v. Society of New York Hospital established the principle that "every human being of adult years and sound mind has a right to determine what shall be done with his own body" [13] [12]. This ruling laid the groundwork for patient autonomy, a concept that would later extend to research participants. The term "informed consent" first appeared officially in the 1957 case Salgo v. Leland Stanford Jr. University Board of Trustees, which emphasized the physician's duty to disclose potential risks and benefits of procedures [12].
The aftermath of World War II and the revelation of unethical human experimentation led to the development of the Nuremberg Code in 1947, which explicitly outlined the necessity of voluntary consent for human subjects research [13] [12]. This was followed by the Declaration of Helsinki in 1964, which further refined ethical principles for medical research involving human subjects [12]. In the United States, these ethical principles were codified into federal regulations with the publication of 45 CFR 46 (Common Rule) and 21 CFR 50 (FDA regulations) [12].
Contemporary Regulatory Landscape
Current informed consent requirements are primarily governed by the Common Rule (45 CFR 46) and FDA regulations (21 CFR 50). The FDA's most recent guidance on informed consent, published in August 2023, builds upon previous documents but does not include major conceptual changes [46]. Notably, the FDA has not yet harmonized with the 2018 changes to the Common Rule, though it plans to do so in the near future [46].
The 2018 revisions to the Common Rule introduced the requirement for a key information section at the beginning of informed consent documents. This section is intended to be a "concise and focused presentation" that facilitates potential participants' comprehension of the research [12]. However, the lack of specific regulatory guidance regarding the content and length of this section has presented challenges for implementation [12].
Table: Historical Milestones in Informed Consent Development
| Year | Event | Significance |
|---|---|---|
| 1905-1914 | Landmark court cases (Mohr, Pratt, Schloendorff) | Established legal principle of patient autonomy and bodily integrity [12] |
| 1947 | Nuremberg Code | First international guidelines emphasizing voluntary consent for research [13] [12] |
| 1964 | Declaration of Helsinki | Refined ethical principles for medical research [12] |
| 1981 | Publication of 45 CFR 46 and 21 CFR 50 | Codified informed consent into U.S. federal law [12] |
| 2018 | Common Rule Revisions | Introduced key information section and other updates to consent requirements [12] |
| 2023 | FDA Final Guidance | Updated informed consent guidance for clinical investigations [46] |
Core Legal Elements of Informed Consent
Based on federal regulations and ethical guidelines, a legally effective informed consent form must include specific core elements that ensure participants are fully informed about the research and can make voluntary decisions about their participation.
Basic Required Elements
The FDA regulations (21 CFR 50.25) and Common Rule specify eight basic elements that must be included in informed consent forms and processes [47]:
- Statement of Research: A declaration that the study involves research, an explanation of the purposes, expected duration of participation, and description of procedures, with identification of any experimental procedures [47].
- Risks and Discomforts: A description of any reasonably foreseeable risks or discomforts to the participant. The FDA's 2023 guidance emphasizes that where relevant, participants should be made aware of the possibility of unintended disclosures of private information and measures to protect privacy [46] [47].
- Benefits: A description of any benefits to the participant or others that may reasonably be expected from the research. For studies comparing investigational agents to standard of care, the FDA guidance allows for a general description of standard care benefits with more detailed information provided during the consent discussion [46] [47].
- Alternatives: Disclosure of appropriate alternative procedures or courses of treatment that might be advantageous to the participant. The 2023 FDA guidance softened the language on this requirement, recommending that alternatives be disclosed as part of the consent discussion but not necessarily included in the written document [46] [47].
- Confidentiality: A statement describing the extent to which confidentiality of records will be maintained, noting that the FDA may inspect records [47]. Certificates of Confidentiality (CoC) may be requested for FDA-regulated research to provide additional protections [46].
- Compensation and Treatment: For research involving more than minimal risk, an explanation of whether compensation or medical treatments are available if injury occurs and where further information may be obtained [47].
- Contact Information: An explanation of whom to contact for answers about the research and research subjects' rights, and whom to contact in the event of a research-related injury [47].
- Voluntary Participation: A statement that participation is voluntary, refusal involves no penalty or loss of benefits, and the participant may discontinue at any time without penalty [47].
Additional Elements When Appropriate
In addition to the basic elements, federal regulations specify six additional elements that must be included when appropriate to the research [47]:
- Unforeseeable Risks: A statement that the treatment or procedure may involve currently unforeseeable risks to the participant or embryo/fetus if the participant is or may become pregnant [46] [47].
- Termination Circumstances: Anticipated circumstances under which participation may be terminated without the participant's consent [47].
- Additional Costs: Any additional costs to the participant from participation [46] [47].
- Consequences of Withdrawal: Consequences of deciding to withdraw and procedures for orderly termination [46] [47].
- Significant New Findings: Statement that significant new findings developed during research that may relate to willingness to continue will be provided [46] [47].
- Participant Numbers: The approximate number of participants in the study [47].
For applicable clinical trials, a specific statement must be included noting that clinical trial information will be submitted to ClinicalTrials.gov [47].
Diagram 1: The Informed Consent Process Flow. This diagram illustrates the sequential and ongoing nature of an ethically and legally valid consent process.
Practical Implementation and Documentation
Enhancing Comprehension and Readability
Effective informed consent requires more than simply including all regulatory elements; it necessitates ensuring genuine participant comprehension. Research indicates that traditional consent processes often fail to provide information in understandable formats, particularly for individuals with low health literacy [12]. A 2025 study by Zhang et al. identified inadequacies in personal functional health literacy among hospitalized patients, which compromised the informed consent process [13].
To address these challenges, several strategies can enhance comprehension:
- Plain Language: Use everyday language instead of medical jargon, aiming for an 8th-grade reading level [13] [48]. The Flesch-Kincaid Grade Level and Reading Ease formula can help assess readability [48].
- Teach-Back Method: Employ the teach-back technique to verify participant understanding, where patients explain information in their own words [13].
- Structured Presentation: Begin with a concise key information section as required by the revised Common Rule, though specific formatting guidance remains limited [12].
- Visual Aids: Utilize pictures, diagrams, and other visual tools to improve understanding of complex research concepts [13] [46].
A 2025 study on digital health research consent found that participants generally preferred shorter consent materials, particularly for sections explaining study risks [49]. The same study found that older participants tended to prefer original, more detailed consent language, while younger participants preferred modified, more readable versions [49].
Table: Participant Preferences for Consent Information (2025 Study)
| Factor | Preference Finding | Statistical Significance |
|---|---|---|
| Text Length | Longer original text reduced preference for original version | P < .001 |
| Modified Text | Participants more likely to prefer modified text by factor of 1.20x | P = .04 |
| Risk Sections | Stronger preference for modified text in risk explanation sections | P = .03 |
| Age | Older participants preferred original more than younger (1.95x) | P = .004 |
| Demographics | Sex, physical activity, and ethnicity influenced preferences | Significant |
Special Considerations and Vulnerable Populations
Obtaining valid informed consent requires special considerations for vulnerable populations and specific research contexts:
- Digital Health Research: Emerging technologies in digital health research introduce new complexities for informed consent, particularly regarding data privacy, security, and the use of commercial products with varying data protection standards [49]. The NIH has recognized these challenges and issued a request for information in 2023 regarding improved consent approaches for digital health research [49].
- Surrogate Consent: For critical care research involving surrogate decision-makers, a 2025 multi-modal study found that surrogates appreciated when research staff waited for optimal timing to initiate contact and provided physical space and defined periods for decision-making [50]. Surrogates placed greater importance on the written consent document itself and were less concerned with its length compared to investigators [50].
- Cultural and Linguistic Considerations: Language barriers and cultural differences significantly impact consent comprehension. Professional interpreter services should be used for participants with limited English proficiency, and cultural sensitivity is essential, particularly for populations where decisions are made collectively rather than individually [13].
- Waivers of Consent: For minimal-risk research conducted under a waiver of consent, a 2025 report from the NIH Pragmatic Trials Collaboratory argues that providing information to participants should be the default approach, as it promotes respect for persons, participant understanding, and trust in research [37].
Experimental Protocols and Research Reagents
Methodologies for Consent Communication Research
Recent research has employed innovative methodologies to evaluate and improve consent communication:
Text Snippet Comparison Protocol (2025 Study) A 2025 study exploring factors influencing informed consent preferences utilized a structured approach to evaluate consent communication [49]:
- Participant Recruitment: 79 participants eligible for a digital health study were recruited through ResearchMatch, Craigslist, community partnerships, and digital advertisements [49].
- Text Modification: Researchers created modified versions of original IRB-approved consent text by using web-based readability analysis software to monitor character length, Flesch Kincaid Reading Ease, and lexical density during the rewriting process [49].
- Survey Design: Participants reviewed 16 pairs of consent communication "snippets" (original and modified versions) and were surveyed on their preferences [49].
- Analysis: Both quantitative analysis of preferences and qualitative analysis of participant feedback were conducted to understand factors influencing consent communication preferences [49].
Multi-Modal Surrogate Consent Study (2025) A comprehensive study on surrogate informed consent processes employed a mixed-methods approach [50]:
- Participant Groups: Included principal investigators (90), research coordinators (105), surrogate decision makers (27), and patients (8) across U.S. academic medical centers [50].
- Data Collection: Combined quantitative surveys with open-ended questions, focus groups, and semi-structured interviews [50].
- Analysis: Used both quantitative and qualitative thematic methods to identify best practices for surrogate consent processes [50].
Research Reagent Solutions for Consent Studies
Table: Essential Research Materials for Informed Consent Studies
| Research Reagent | Function/Purpose | Application Example |
|---|---|---|
| Readability Analysis Software | Quantifies reading level and complexity of consent documents | Calculating Flesch-Kincaid grade level of consent forms [49] |
| Text Snippet Pairs | Enables comparative analysis of consent communication variations | Testing participant preferences between original and modified consent text [49] |
| Structured Surveys | Collects quantitative and qualitative data on participant preferences and comprehension | Assessing factors influencing consent communication preferences [49] |
| Focus Group Protocols | Gathers in-depth qualitative insights into participant perspectives | Understanding surrogate decision-maker experiences with consent process [50] |
| Comprehension Assessment Tools | Measures participant understanding of key study elements | Utilizing teach-back method to verify comprehension [13] |
Diagram 2: Informed Consent Form Development Workflow. This diagram outlines the key stages in developing an effective, compliant informed consent form.
A legally effective informed consent form requires meticulous attention to both regulatory requirements and ethical principles of respect for persons and autonomy. The core elements specified in federal regulations provide the essential framework, but effective implementation demands consideration of participant comprehension, cultural and linguistic factors, and specific research contexts. Recent studies emphasize the importance of readability, participant engagement, and ongoing communication throughout the research process. As research methodologies evolve, particularly in digital health and pragmatic trials, informed consent processes must adapt while maintaining foundational ethical principles. By integrating regulatory requirements with evidence-based approaches to communication and comprehension, researchers can create consent processes that truly honor participant autonomy and promote ethical research conduct.
Essential Additional Elements for Specific Research Contexts
The doctrine of informed consent has undergone significant transformation since its early 20th-century origins, evolving from a simple signature on a document to a complex, context-dependent process. The foundational legal cases of Mohr v Williams (1905), Pratt v Davis (1905), Rolater v Strain (1913), and Schloendorff v Society of New York Hospital (1914) established the fundamental principle of patient autonomy, forming the legal scaffolding for informed consent requirements [12]. These early cases, all featuring female plaintiffs at a time when women lacked voting rights, indelibly intertwined patient autonomy with bodily self-determination [12].
The term "informed consent" first appeared in the 1957 case Salgo v Leland Stanford Jr University Board of Trustees, which established the physician's duty to disclose potential risks and procedures [12]. Subsequent historical tragedies, including the Nuremberg Code (1947) developed in response to Nazi war crimes and the Tuskegee Syphilis Study (1932-1972), further cemented the need for stringent ethical standards in human subjects research [13] [51]. These developments culminated in regulatory frameworks including the Declaration of Helsinki (1964), the Belmont Report (1979), and ultimately the Common Rule (1991) and FDA regulations [12] [51].
Modern informed consent has progressed beyond a one-size-fits-all approach to recognize that different research contexts demand specialized additional elements to truly protect participants. This technical guide examines these essential additional elements across varied research scenarios, providing researchers, scientists, and drug development professionals with practical frameworks for compliance in this evolving ethical landscape.
Regulatory Framework and Key Concepts
Core Informed Consent Elements
The foundation of informed consent rests on three core principles: voluntariness (participation must be freely given without coercion), comprehension (participants must understand the information provided), and disclosure (researchers must provide all relevant information about the study) [51]. These principles operationalize through eight key components, detailed in the table below.
Table 1: Fundamental Elements of Informed Consent
| Element Category | Specific Requirements |
|---|---|
| Purpose & Procedures | Clear explanation of study objectives, methods, expected duration, and participant tasks [13] [51] [48] |
| Risks & Discomforts | Description of all foreseeable risks, discomforts, and hazards [13] [51] |
| Benefits | Statement of potential benefits to participants or society [13] [51] |
| Alternatives | Disclosure of appropriate alternative procedures or treatments [13] [46] |
| Confidentiality | Explanation of data handling, privacy protections, and confidentiality limitations [46] [51] [48] |
| Compensation | Information about compensation for injury and/or participation [46] [48] |
| Voluntary Participation | Clear statement that participation is voluntary and withdrawal is possible without penalty [51] [48] |
| Contact Information | Details of researchers and IRB contacts for questions or concerns [51] [48] |
Recent Regulatory Developments
The regulatory landscape for informed consent continues to evolve, with several significant developments impacting requirements:
- ICH E6(R3) Guidelines (2025): The updated Good Clinical Practice guidelines emphasize "media-neutral" consent processes facilitating electronic and remote consent, principles-based approaches, and enhanced data governance requirements [52].
- FDA Informed Consent Guidance (2023): This final guidance clarifies requirements for emerging contexts, including sufficient information on protocol requirements and time commitments, expanded significant new findings reporting, and alternative documentation methods when electronic consent isn't available [46].
- Common Rule Revisions (2018): Introduced the "key information" requirement—a concise, focused presentation at the beginning of consent documents to facilitate comprehension, though format guidelines remain somewhat limited [12].
These developments reflect a broader shift toward participant-centered, accessible consent processes that accommodate technological advances while maintaining ethical rigor.
Context-Specific Additional Elements
Genetic and Genomic Research
Genetic research presents unique considerations due to the potentially far-reaching implications of genetic information for participants and their biological relatives. The following additional elements must be incorporated into informed consent processes for genetic studies.
Table 2: Additional Consent Elements for Genetic Research
| Element | Rationale & Implementation |
|---|---|
| Heritability Implications | Explanation that genetic findings may have significance for biological family members, with potential need for family communication [51] |
| Future Use Specifications | Clear terms regarding storage and future use of biological samples and genetic data, including scope of permitted research [51] |
| Incidental Findings Policy | Protocol for handling unexpected findings with clinical significance, including whether/when they will be disclosed to participants [51] |
| Data Sharing Provisions | Specific information about genetic data deposition in controlled-access databases and sharing with other researchers [51] |
The diagram below illustrates the decision pathway for handling genetic information and incidental findings, a critical component of genetic research consent:
Emergency and Critical Care Research
Research conducted in emergency settings where potential participants may be incapacitated requires special consent considerations. The FDA and Common Rule provide for exception from informed consent (EFIC) requirements for emergency research under specific conditions [51]. Key additional elements include:
- Community Consultation and Disclosure: Prior to initiation, researchers must consult with representatives of the communities in which the research will take place and from which subjects will be drawn [51].
- Public Disclosure: Plans for public disclosure of the study design, risks, and benefits both before initiation and after completion [51].
- Assent and Consent Procedures: Procedures for obtaining assent from subjects or consent from legally authorized representatives when feasible, and additional protections to ensure the welfare of subjects [51].
- Debriefing and Follow-up: Procedures to inform recovered participants or their families about the research, including their participation and any relevant outcomes [51].
International and Cross-Cultural Research
Global clinical trials introduce complex considerations regarding cultural norms, health literacy, and regulatory variations. The ICH E6(R3) guidelines specifically address the need for culturally appropriate consent processes in multinational trials [52]. Essential additional elements include:
- Cultural Adaptation of Materials: Consent documents and processes must be adapted to local cultural norms, accounting for collective decision-making practices in some cultures where individual signature may not be the norm [13] [51].
- Appropriate Translation: Certified translation of consent materials into local languages, with verification of conceptual (not just literal) accuracy [13] [51].
- Local Regulatory Compliance: Specific information about how the research complies with host country regulations in addition to international standards [52] [51].
- Community-Specific Risk-Benefit Analysis: Contextualization of risks and benefits relative to local healthcare infrastructure and cultural values [52].
Research with Vulnerable Populations
Vulnerable populations require additional safeguards to ensure meaningful, voluntary consent. The specific additional elements vary by population, as detailed in the table below.
Table 3: Additional Consent Elements for Vulnerable Populations
| Population | Additional Consent Requirements |
|---|---|
| Children | Parental permission obtained alongside developmentally appropriate child assent; age-specific information materials [51] [48] |
| Prisoners | Additional protections to minimize coercion; clear explanation that participation will not affect parole or treatment within system [13] |
| Cognitively Impaired | Consent from legally authorized representatives with participant assent to the extent of their abilities; capacity assessment documentation [51] |
| Wards of the State | Appointment of an advocate for each child; additional oversight to ensure voluntariness [46] |
For research with children, the following workflow illustrates the dual consent/assent process:
Digital Health and Decentralized Clinical Trials
The ICH E6(R3) guidelines explicitly accommodate digital technologies and decentralized trial designs, requiring corresponding adaptations to informed consent processes [52] [53]. Additional elements for these contexts include:
- Technology Requirements and Limitations: Clear description of devices, applications, or platforms participants must use, including technical requirements, data usage, and security measures [52].
- Remote Consent Procedures: Specific protocols for obtaining consent remotely, including identity verification and confirmation of participant understanding without physical presence [52] [53].
- Data Flow and Security: Comprehensive explanation of how data will be collected, transmitted, stored, and protected in decentralized settings, including limitations of confidentiality in digital transmission [46].
- Technical Support: Information about available technical assistance for technolog-mediated participation and alternative procedures if technology fails [52].
Implementation and Documentation
Enhanced Comprehension Strategies
Regardless of specific contextual elements, effective implementation requires strategies to ensure genuine participant understanding. Research demonstrates that traditional consent processes often fail to facilitate comprehension, particularly for participants with limited health literacy [13] [12]. Effective strategies include:
- Teach-Back Method: Having participants explain key concepts in their own words to verify understanding [13].
- Multi-Format Presentation: Using combined written, oral, and multimedia formats to accommodate different learning styles [51] [48].
- Plain Language Principles: Writing consent materials at an 8th-grade reading level, using common vocabulary and short sentences, while avoiding medical jargon [51] [48].
- Cultural and Linguistic Competence: Employing qualified medical interpreters (including ASL interpreters) and culturally adapting materials rather than simply translating [13] [51].
Table 4: Research Reagent Solutions for Enhanced Consent Processes
| Tool/Resource | Function & Application |
|---|---|
| eConsent Platforms | Digital systems facilitating remote consent, multimedia integration, version control, and signature management [53] |
| Readability Assessment Tools | Software (e.g., Flesch-Kincaid) evaluating reading level of consent materials to ensure appropriate complexity [48] |
| Qualified Medical Interpreters | Professional interpretation services for participants with limited English proficiency or hearing impairment [13] |
| Visual Aid Libraries | Collections of standardized diagrams, illustrations, and pictograms to explain complex procedures [48] |
| Decision Support Tools | Structured aids helping participants understand tradeoffs between different research participation choices [13] |
Documentation and Regulatory Compliance
Proper documentation of context-specific consent elements is essential for regulatory compliance and participant protection. Key considerations include:
- Version Control: Maintaining strict version control for consent documents, particularly when using multiple language versions or site-specific adaptations [46] [53].
- Signature Methods: Utilizing appropriate signature methods for different contexts, including electronic signatures with audit trails, witnessed verbal consent for low-literacy populations, and photographic documentation when traditional signing isn't possible [46].
- Local IRB Review: For multicenter trials using single IRB review, ensuring local context considerations are adequately addressed and documented, with significant local changes shared with all investigators and the central IRB [46] [53].
- Ongoing Consent Documentation: Documenting continued consent throughout long-term studies, including re-consent for major protocol changes and significant new findings that might affect willingness to participate [46].
The ethical imperative of informed consent requires careful attention to context-specific elements that ensure truly informed, voluntary participation across diverse research scenarios. From genetic studies with their familial implications to emergency research with inherent capacity limitations, and from international trials with cultural considerations to digital studies with technological complexities, each context demands specialized additional elements beyond the foundational requirements.
The ongoing evolution of informed consent—from its origins in early 20th-century legal cases to the recently implemented ICH E6(R3) guidelines—reflects the research community's growing understanding that meaningful consent is not a one-time signature but an ongoing, communicative process tailored to specific contexts and participants [13] [52] [12]. As technological advances and novel trial designs continue to emerge, the framework of essential additional elements will necessarily continue to evolve, requiring researchers' sustained attention to both ethical principles and regulatory requirements.
By implementing the context-specific elements outlined in this technical guide, researchers can better ensure that informed consent fulfills its fundamental purpose: respecting participant autonomy and promoting trust while facilitating ethically sound scientific progress.
Informed consent is a fundamental ethical and legal requirement in both clinical practice and human subjects research. Its history, rooted in respecting patient autonomy, has evolved from a simple signature to a complex communication process. A critical yet often overlooked component of this process is ensuring that consent documents are genuinely understandable to participants. This technical guide provides researchers, scientists, and drug development professionals with evidence-based methodologies for crafting informed consent materials at an 8th-grade reading level using lay language, thereby fulfilling the ethical imperative of true comprehension.
Historical Context and the Modern Imperative for Readability
The legal foundation for informed consent was established in the early 20th century through a series of landmark court cases that emphasized the patient's "right to themselves" [12]. This principle was cemented in the 1914 case Schloendorff v. Society of New York Hospital, which established that every adult of sound mind has the right to determine what is done with their own body [13] [12]. The subsequent Nuremberg Code, formulated in response to unethical human experimentation, further enshrined the requirement for "sufficient knowledge and comprehension" as a prerequisite for voluntary consent [12] [48].
Despite this robust ethical and legal history, the practical application of informed consent has often fallen short. Modern regulations have recognized this failure. The revised Common Rule (45 CFR § 46), which took effect in 2018, explicitly mandates that informed consent must begin with a "concise and focused presentation of the key information" and, as a whole, must be "organized and presented in a way that facilitates comprehension" [54] [6]. This shift moves beyond mere disclosure of information, placing a positive obligation on researchers to ensure participant understanding, a goal that is unattainable without using clear, lay language at an accessible reading level [54].
Quantitative Assessment of Readability
Evaluating the reading level of consent documents is a critical first step. The following table summarizes standard quantitative metrics used for this assessment.
Table 1: Standard Quantitative Readability Metrics
| Metric | Target Score for ~8th Grade Level | What It Measures | Common Tools for Assessment |
|---|---|---|---|
| Flesch-Kincaid Grade Level | 8.0 or lower | Assigns a U.S. school grade level based on average sentence length and syllables per word [48]. | Built-in feature in Microsoft Word; third-party add-ons for Google Docs [48]. |
| Flesch Reading Ease | 60 or higher (on a 0-100 scale) | Assesses how easy a text is to understand; higher scores indicate easier reading [48]. | Built-in feature in Microsoft Word; third-party add-ons for Google Docs [48]. |
It is crucial to recognize that these formulas primarily assess sentence length and word complexity. Other factors, such as sentence structure, logical flow, word variety, and clarity, must be evaluated separately to ensure true comprehension [48]. A document can meet quantitative targets while still being confusing if it uses jargon or presents information illogically.
Experimental Protocols for Validating Understanding
Beyond formulaic checks, validating participant understanding requires direct assessment. The following methodologies are cited in the literature as effective means to evaluate and improve the consent process.
The Teach-Back and Test/Feedback Method
A study by Miller et al. highlighted that implementing a health literacy-based consent process, which included the teach-back technique, improved patient-provider communication and increased patient comfort in asking questions [13].
Protocol Details:
- Procedure: After explaining a section of the consent form, the researcher asks the participant to explain the information back in their own words. For example, "To make sure I explained everything clearly, could you tell me in your own words what the main risks of this procedure are?"
- Assessment: The researcher evaluates the accuracy of the participant's response.
- Iteration: If the understanding is incomplete or incorrect, the researcher re-explains the information using different language and repeats the teach-back process until the participant demonstrates comprehension [13].
- Outcome: This technique encourages active participation and helps both the participant and researcher identify and clarify confusing points during the conversation [13].
Interactive Intervention and Graphical Tools
Research indicates that interactive interventions are superior to static text in improving patient comprehension [13].
Protocol Details:
- Procedure: The use of interactive media, graphical tools, and pictorial aids to supplement or replace dense text in explaining complex concepts like risks, benefits, and study procedures.
- Application: These tools can be integrated into electronic consent platforms or used as physical aids during the consent discussion.
- Outcome: These visual aids improve shared decision-making and can more effectively assess and present probabilistic risks (e.g., likelihood of side effects) in a way that is easier to understand than numerical or textual descriptions alone [13].
Table 2: Research Reagent Solutions for Consent Comprehension
| Tool Category | Specific Examples | Primary Function | Implementation Context |
|---|---|---|---|
| Readability Assessment Software | Microsoft Word's Flesch-Kincaid; Google Docs third-party add-ons | To quantitatively gauge the grade level and reading ease of consent documents [48]. | Document preparation phase; pre-submission to IRB. |
| Interactive Digital Platforms | eConsent applications with embedded videos, quizzes, and clickable info-icons | To transform a passive reading activity into an active learning process [13]. | During the consent process with potential participants. |
| Visual Aid Kits | Diagrams of study workflows; pictograms for risks/benefits; simplified charts | To convey complex procedural and statistical information without relying solely on text [13]. | During the face-to-face consent discussion. |
A Strategic Workflow for Developing Understandable Consent Forms
The process of creating an effective, understandable consent document is iterative and involves both technical tools and human-centric communication strategies. The following diagram visualizes this workflow.
Practical Strategies for Plain Language and Lay Terminology
Translating technical and legalistic language into lay terms is the core of achieving an 8th-grade reading level. The following strategies are essential.
- Replace Jargon with Common Words: Choose simple, common words over academic or medical jargon. For example, replace "hypertension" with "high blood pressure," "administer" with "give," and "contraindication" with "reason you should not take" [48].
- Use Short Sentences and Paragraphs: Long, complex sentences are a primary driver of high reading levels. Aim for an average sentence length of 15 words or fewer. Break down complex ideas into a series of simple sentences [48].
- Employ Active Voice: Active voice is more direct and easier to understand. For example, use "The researcher will give you the drug" instead of "The drug will be administered to you by the researcher."
- Structure Content for Easy Scanning: Use bulleted lists for multiple items (like risks or procedures), bold headers to break text into manageable sections, and ample white space to reduce visual clutter [54] [48]. This aligns with the Common Rule's requirement to organize information to facilitate comprehension [54].
- Define Unavoidable Technical Terms: When a technical term must be used, provide a simple, parenthetical definition immediately following it. For example, "We will look at your hemoglobin (a protein in your blood that carries oxygen) levels."
The move towards understandable consent forms, underscored by regulatory evolution from paternalistic practices to patient-centered communication, is not merely a technical exercise. It is a fundamental ethical commitment to the principle of respect for persons. By rigorously applying the methodologies of readability assessment, plain language writing, and validation through interactive dialogue, researchers can ensure the informed consent process truly empowers participants to make autonomous, understanding decisions.
Informed consent represents a cornerstone of ethical clinical practice and research, serving as a critical process that respects individual autonomy and safeguards personal integrity. This process has evolved significantly from its origins in early 20th-century legal precedents to its current form as a comprehensive communication framework between healthcare providers and patients. The fundamental ethical principle underpinning informed consent is the protection of self-sovereignty over one's own body, balancing the values of autonomy and non-domination [13]. Historically, the concept emerged from a series of landmark judicial decisions that established the principle of patient autonomy. The 1914 case of Schloendorff v. Society of New York Hospital notably articulated that "every human being of adult years and sound mind has a right to determine what shall be done with his own body" [12]. This ruling established the foundational legal principle that patients must agree to medical procedures, setting the stage for the development of modern informed consent requirements.
The mid-20th century witnessed further refinement of informed consent standards in response to unethical medical experiments, including the Tuskegee Study of Untreated Syphilis and Nazi human experiments during World War II. These events led to the establishment of the Nuremberg Code and the Declaration of Helsinki, which cemented informed consent as a fundamental ethical standard in both research and clinical practice [13]. The Nuremberg Code specifically emphasized that voluntary consent of the human subject is absolutely essential, requiring that individuals have "sufficient knowledge and comprehension of the elements of the subject matter involved, as to enable him to make an understanding and enlightened decision" [12]. This historical context underscores the critical importance of ensuring genuine comprehension during the consent process, moving beyond mere signature collection to meaningful communication and understanding.
Current Regulatory Framework and Requirements
The contemporary regulatory landscape for informed consent has evolved substantially, with recent updates emphasizing comprehension and participant understanding. The 2018 revisions to the Common Rule (45 CFR 46) introduced significant changes, most notably the requirement that informed consent must "begin with a concise and focused presentation of the key information that is most likely to assist a prospective subject or legally authorized representative in understanding the reasons why one might or might not want to participate in the research" [54]. This key information section must be organized and presented in a way that facilitates comprehension, moving beyond mere lists of isolated facts to facilitate genuine understanding of the research decision [54].
Recently, the FDA has worked to harmonize its informed consent regulations (21 CFR 50) with the Common Rule, particularly regarding the key information requirement. This harmonization, expected to be finalized in 2025, will align expectations for both federally and non-federally funded research, ensuring that all clinical trial participants receive a concise summary of key information at the beginning of consent forms [6]. The updated regulations also introduce additional required disclosures, including whether the research involves commercial intent, whether clinical specimens might be used for future research, and under what circumstances research results will be returned to participants [54].
Table 1: Core Elements of Informed Consent According to Regulatory Standards
| Element Category | Specific Requirements | Regulatory Source |
|---|---|---|
| Basic Elements | Nature of the procedure, risks and benefits, reasonable alternatives | 45 CFR 46.116 [13] |
| Additional Disclosures | Commercial intent, use of clinical specimens, return of results | Revised Common Rule [54] |
| Documentation | Signatures, dates, copy provided to participant | 21 CFR 50.27 [46] |
| Special Populations | Assent for children, LAR for decisionally impaired | ICMR Guidelines [55] |
The regulatory framework also specifies circumstances under which alterations or waivers of consent may be appropriate. According to 45 CFR 46.116(f), an Institutional Review Board (IRB) may approve a consent procedure that does not include or alters some elements of informed consent when the research involves no more than minimal risk, the waiver will not adversely affect participants' rights and welfare, the research could not practicably be carried out without the waiver, and participants will be provided with additional pertinent information after participation when appropriate [56]. Even in these cases, however, recent guidance suggests that providing some form of information to participants should be the default approach to promote respect for persons, participant engagement, and trust in research [37].
Methodologies for Enhancing Comprehension and Discussion
Structured Communication Approaches
Effective informed consent requires implementing evidence-based methodologies to enhance participant understanding. The teach-back method has emerged as a particularly valuable technique, allowing healthcare providers to assess comprehension by asking patients to explain the information in their own words [13]. This interactive approach transforms the consent process from a unilateral information transfer to a bidirectional dialogue, enabling real-time assessment of understanding. Studies demonstrate that implementing health literacy-based consent forms and processes significantly improves patient-provider communication, increases patient comfort in asking questions, and encourages active participation in the consent dialogue [13]. For optimal effectiveness, the consent discussion should occur in a clinical or office setting with sufficient time for questions and emotional processing, rather than immediately before procedures when patients may be medicated, stressed, or rushed [13].
Additional structured approaches include using interactive media and graphical tools to improve shared decision-making and effectively present risk information [13]. These visual aids can include pictures, diagrams, flowcharts, and tables to enhance reading comprehension, particularly for complex study designs or statistical information [46]. The consent process should also incorporate open-ended questions to gather insights into patients' needs and preferences, encouraging them to actively engage with the material rather than passively receive information [13].
Special Considerations for Diverse Populations
Implementing effective consent processes requires adapting approaches to address the needs of diverse populations. For participants with limited English proficiency or those who speak other languages, the use of qualified medical interpreters is essential rather than relying on family members or untrained staff [13]. American Sign Language interpreters should be available for hearing-impaired patients, and consent documents must be translated into vernacular languages understandable to the participant [13] [55]. Cultural sensitivity is equally crucial, as decision-making norms vary across cultures. In some communities, decisions are made collectively rather than individually, and written consent may be perceived as a sign of mistrust [13]. Researchers must adapt their approaches to respect these cultural norms while still ensuring ethical standards are maintained.
For vulnerable populations, including children, decisionally impaired individuals, and prisoners, additional protections apply. For children under 7 years, verbal consent is essential, while mature minors (ages 7-18) should provide informed assent in addition to parental permission [55]. In cases where participants cannot provide consent due to unconsciousness, severe mental illness, or disability, consent must be obtained from a Legally Acceptable Representative (LAR) [55]. When participants or their LAR are unable to read or write, an impartial witness should be present during the entire consent process [55].
Documentation and Monitoring Techniques
Proper documentation of the informed consent process is essential for ethical and regulatory compliance. The Joint Commission requires documentation of all consent elements either in a form, progress notes, or elsewhere in the record [13]. Essential documented elements include the nature of the procedure, risks and benefits, reasonable alternatives, risks and benefits of alternatives, and an assessment of the patient's understanding [13]. Recent technological advances have expanded documentation options, including electronic consent systems and audiovisual recording of the consent process. In some cases, particularly for vulnerable populations in trials of new chemical entities, audiovisual recording of the informed consent process is mandatory [55]. These recordings must capture facial details of all participants and be preserved securely for at least five years after study completion [55].
For certain minimal-risk research where signed consent would pose a confidentiality risk or where signing forms is not culturally appropriate, IRBs may waive the documentation requirement [56]. Even in these cases, researchers are often required to provide participants with a written statement about the research, maintaining transparency while addressing the specific concern [56]. Monitoring comprehension throughout the research process is equally important, with requirements to inform participants of significant new findings that might affect their willingness to continue participation [46]. This ongoing communication ensures that consent remains informed throughout the research relationship rather than representing a single moment of permission.
Experimental Protocols and Validation Methods
Comprehension Assessment Protocols
Validating participant understanding requires systematic assessment methodologies. The test/feedback method represents a structured approach to evaluating comprehension, where participants are asked specific questions about key study elements to identify areas requiring further clarification [13]. This protocol typically involves developing a standardized assessment tool targeting critical study components, including the research purpose, procedures, risks, benefits, alternatives, and voluntary nature of participation. Participants complete this assessment following the consent discussion, and their responses are evaluated against a predetermined competency threshold. For areas where understanding is inadequate, the researcher provides additional education and reassesses comprehension until satisfactory understanding is achieved [13].
Another validated protocol involves the implementation of health literacy-focused consent forms with built-in assessment metrics. This approach typically includes developing consent documents written at a 6th to 8th grade reading level using lay terminology [56]. The protocol involves pre-testing the document with representative populations to identify problematic terminology or concepts, revising based on feedback, and implementing the revised document with comprehension checks throughout the consent discussion. Studies by Miller et al. highlighted that implementing such health literacy-based consent forms improved patient-provider communication, increased patient comfort in asking questions, and encouraged the use of the teach-back technique in perioperative settings [13].
Process Validation and Quality Assurance
Ensuring the quality and effectiveness of the consent process requires systematic validation methodologies. One experimental approach involves randomization of consent formats with comprehension outcomes as primary endpoints. In such studies, participants are randomly assigned to receive standard consent materials or enhanced materials incorporating additional comprehension aids such as graphical risk presentations, simplified language, or interactive digital content. Comprehension is then assessed using standardized instruments, allowing researchers to quantify the impact of specific enhancements on understanding [13].
The NIH Pragmatic Trials Collaboratory has developed additional validation methodologies for studies conducted under alterations or waivers of consent. These protocols emphasize that even when formal consent is not required, providing information to participants promotes important ethical values including respect for persons, participant engagement, and trust in research [37]. Their methodology involves developing tiered information approaches based on study risk level, implementing notification systems (including letters, emails, posters, and clinician conversations), and assessing participant understanding and attitudes toward the research. This approach recognizes that communication about research participation exists on a spectrum rather than as a binary consented/unconsented distinction [37].
Table 2: Validation Methods for Informed Consent Comprehension
| Validation Method | Protocol Description | Outcome Measures |
|---|---|---|
| Teach-back Assessment | Participant explains key concepts in own words after consent discussion | Accuracy of concept explanation, identification of misunderstanding areas |
| Test/Feedback Evaluation | Standardized questionnaire on critical study elements administered post-consent | Correct response rate, areas of consistent misunderstanding |
| Health Literacy Assessment | Evaluation of consent form reading level and participant health literacy | Reading grade level, functional health literacy score, comprehension metrics |
| Audiovisual Recording Analysis | Recording and systematic review of consent discussions | Adherence to consent elements, quality of interaction, participant engagement |
| Longitudinal Understanding Assessment | Comprehension evaluation at multiple time points during study participation | Retention of key information, understanding of ongoing commitments |
Research Reagent Solutions: Essential Tools for Effective Consent Processes
Implementing effective informed consent processes requires utilizing specific assessment tools and educational resources. The following table details essential "research reagents" for consent comprehension and documentation.
Table 3: Essential Research Reagent Solutions for Informed Consent Processes
| Tool Category | Specific Solution | Function and Application |
|---|---|---|
| Comprehension Assessment | Teach-back protocol scripts | Standardized questions to verify understanding of key concepts through participant explanation |
| Literacy Evaluation | Health literacy screening tools (e.g., REALM, NVS) | Identify participants with limited health literacy requiring adapted communication approaches |
| Documentation Systems | Audiovisual recording equipment | Capture entire consent process for vulnerable populations or high-risk studies as regulatory requirement |
| Multi-language Resources | Certified translation services | Accurate translation of consent documents and availability of qualified interpreters for non-English speakers |
| Readability Enhancement | Lay terminology databases | Replace medical jargon with understandable language to achieve 6th-8th grade reading level |
| Visual Aid Tools | Graphical risk representation systems | Convert statistical risk information into visual formats for improved comprehension |
| Cultural Adaptation Frameworks | Cultural competence assessment tools | Identify cultural factors affecting decision-making and adapt consent process accordingly |
The informed consent process continues to evolve from a signature-focused documentation requirement toward a comprehensive communication framework centered on genuine understanding and voluntary participation. Recent regulatory changes, including the key information requirement in the revised Common Rule and impending FDA harmonization, reflect this fundamental shift in emphasis [54] [6]. The successful implementation of these standards requires methodological approaches that prioritize comprehension through structured communication, cultural sensitivity, and systematic validation. As research environments grow increasingly complex, the ethical imperative to ensure truly informed consent remains constant. Future developments will likely continue to refine methodologies for assessing and enhancing understanding, particularly for vulnerable populations and in emerging research contexts such as pragmatic trials and digital health technologies. Through continued attention to both the ethical foundations and practical implementation of informed consent, researchers can uphold the principle of respect for persons while advancing scientific knowledge.
The principles governing informed consent from legally authorized representatives and assent from children are deeply rooted in the historical development of human subjects protections. The concept of informed consent emerged from a series of early 20th-century legal cases that established the principle of patient autonomy, including Mohr v Williams (1905), Pratt v Davis (1905), and Schloendorff v Society of New York Hospital (1914) [14]. The term "informed consent" first appeared officially in the 1957 case Salgo v Leland Stanford Jr University Board of Trustees, which emphasized the physician's duty to disclose potential risks [14]. These foundational legal principles culminated in the Nuremberg Code (1947), which established voluntary consent as the first requirement for ethical human experimentation [14].
In the United States, these ethical principles were codified into federal regulations through the Belmont Report (1979) and subsequent adoption of 45 CFR 46 (the Common Rule) and 21 CFR 50 (FDA regulations) [14]. These regulations recognize that children and some adults with impaired consent capacity cannot legally provide independent informed consent, creating the need for a dual protection system: permission from parents or legally authorized representatives and assent from the subjects themselves when capable [57] [58]. This framework ensures respect for persons while protecting vulnerable populations in research.
Regulatory Framework and Definitions
Key Regulatory Definitions
The regulatory framework for research involving children and adults with impaired consent capacity establishes specific terminology distinct from standard informed consent procedures:
- Assent: A child's or impaired adult's affirmative agreement to participate in research [57]. Mere failure to object should not be construed as assent [58].
- Permission: The agreement of a parent(s) or legally authorized representative (LAR) for a child or decisionally impaired adult to participate in research [57].
- Legally Authorized Representative (LAR): An individual or judicial body authorized under applicable law to consent on behalf of a prospective subject [57].
- Child: Individuals who have not attained the legal age for consent to treatments or procedures involved in research (under 18 years in most jurisdictions) [58].
The Determination of Assent Capacity
Institutional Review Boards (IRBs) must determine whether children are capable of providing assent based on the ages, maturity, and psychological state of the children involved [59]. This judgment may be made for all children under a particular protocol or for individual children, as the IRB deems appropriate [59]. The following table outlines typical age-based considerations for assent implementation:
Table: Age-Based Assent Considerations
| Age Range | Assent Required? | Documentation Approach | Key Considerations |
|---|---|---|---|
| Birth to 6 | No (verbal respect recommended) | Simplified oral explanation | Include child in process with parents; use age-appropriate language [58]. |
| Ages 7-11 | Yes | Simple written form (≈6th grade level) | Use visuals, diagrams; limit to one page if possible; describe discomforts [57] [58]. |
| Ages 12-17 | Yes | More detailed written form | Can resemble adult consent form with age-appropriate language; maintain ≈6th grade level [58]. |
The diagram below illustrates the decision-making workflow that IRBs and researchers must follow when determining assent requirements and procedures:
Diagram: Assent Determination Workflow
Parental Permission Requirements
Levels of Parental Permission
Federal regulations establish tiered requirements for parental permission based on the level of risk and potential for direct benefit in the research [59] [58]. The number of parents required to provide permission varies according to the research category:
Table: Parental Permission Requirements by Research Category
| Research Category | Regulatory Basis | Risk Level | Parental Permission Requirement |
|---|---|---|---|
| Category 1 | 45 CFR 46.404, 21 CFR 50.51 | Research not involving greater than minimal risk | Permission of one parent sufficient [59] [58] |
| Category 2 | 45 CFR 46.405, 21 CFR 50.52 | Research involving greater than minimal risk but presenting prospect of direct benefit to subject | Permission of one parent sufficient [59] [58] |
| Category 3 | 45 CFR 46.406, 21 CFR 50.53 | Research involving greater than minimal risk with no prospect of direct benefit but likely to yield generalizable knowledge | Permission of both parents required unless one is deceased, unknown, incompetent, not reasonably available, or only one has legal responsibility [59] [58] |
| Category 4 | 45 CFR 46.407, 21 CFR 50.54 | Research not otherwise approvable but presents opportunity to understand, prevent, or alleviate serious problem | Permission of both parents required (same exceptions as Category 3) [59] |
Documentation and Waiver Provisions
Parental permission must be documented in accordance with standard informed consent documentation requirements [59]. However, IRBs may waive parental permission requirements under certain specific conditions:
- The research protocol is designed for conditions or populations for which parental permission is not reasonable to protect subjects (e.g., neglected or abused children) [59].
- An appropriate alternative protection mechanism is substituted for protecting children participating in research [59].
- The waiver is not inconsistent with federal, state, or local law [59].
- The research involves no more than minimal risk and could not practicably be carried out without the waiver [60].
Special Circumstances and Exceptions
Emancipated and Mature Minors
State laws vary regarding emancipated minors and their ability to provide independent consent. Under Kentucky law, for example, minors over 16 who are legally married are considered emancipated by operation of law and can provide consent for research [58]. Other jurisdictions may recognize different criteria for emancipation. Researchers must consult with institutional legal counsel to determine applicable state laws and institutional policies regarding emancipated minors [57].
Minors Turning 18 During Research Participation
Federal regulations require that when a minor turns 18 during research participation, legally effective informed consent must be obtained for any ongoing interactions or interventions, as parental permission and minor assent are no longer sufficient [58]. The IRB may approve a consent waiver for continued analysis of identifiable data or specimens if specific regulatory criteria are met [58].
Emergency and Military Exceptions
Exceptionally narrow exceptions exist for circumstances where standard consent is not feasible. The FDA regulations permit exceptions from informed consent requirements for:
- Life-threatening situations where communication with the subject or representative is not possible [60].
- Military operations when the President waives prior consent requirements based on specific statutory criteria [60].
These exceptions involve rigorous certification and review requirements and are not applicable to most research contexts involving children [60].
Practical Implementation and Documentation
Essential Elements of Assent Documents
Effective assent documents should contain the following key elements, presented in an age-appropriate manner:
- Brief statement of purpose explaining why the research is being done [57] [61].
- Description of procedures (including duration) written from the child's perspective [57].
- Explanation of voluntariness stating that participation is their choice [57] [61].
- Description of pain or discomfort that may be experienced during research procedures [57].
- Simple explanation of alternatives to participation [57].
- Description of potential benefits, if any, to the child or others [57] [61].
- Information about compensation, if provided [57].
- Offer to answer questions at any time [57] [61].
Table: Research Reagent Solutions for Implementing Assent and Permission Procedures
| Tool/Resource | Function/Purpose | Implementation Guidance |
|---|---|---|
| Age-Appropriate Assent Templates | Provides standardized format ensuring regulatory compliance | Use institutional IRB-approved templates; modify for specific age groups (simpler language for younger children) [57]. |
| Parental Permission Form Templates | Documents legally effective permission from parents/LARs | Adapt standard informed consent templates to parent perspective ("your child is being..."); include all required regulatory elements [57] [61]. |
| Visual Aids and Diagrams | Enhances comprehension for children with varying literacy levels | Use pictures, charts, or schema to explain procedures; particularly helpful for children ages 7-11 [57]. |
| Readability Assessment Tools | Ensures age-appropriate language complexity | Maintain ≈6th grade reading level for assent forms; simplify complex scientific terminology [58] [61]. |
| Institutional Legal Counsel Consultation | Addresses state-specific emancipation and consent laws | Required for research involving minors aged 15-17; essential for determining emancipation status [57] [58]. |
Documentation Standards
The IRB must determine whether and how assent must be documented [59]. When documentation is required, the IRB-approved assent form should be signed and dated by the subject, with a copy provided to the subject or representative [57]. For younger children or those with limited capacity, oral assent with simplified documentation may be appropriate [58].
The processes for obtaining assent from children and permission from legally authorized representatives represent a carefully balanced ethical and regulatory framework that respects developing autonomy while ensuring appropriate protection for vulnerable populations. These requirements have evolved from foundational ethical principles established in response to historical abuses and judicial decisions affirming personal autonomy. Successful implementation requires researchers to develop age-appropriate materials, adhere to risk-based permission requirements, and maintain documentation standards that reflect both regulatory mandates and ethical commitments to respecting all persons, regardless of their capacity to provide independent informed consent. As research methodologies and populations continue to evolve, these foundational protections provide a critical framework for ethical research conduct.
The concept of informed consent has evolved notably over time, transitioning from a period where physician authority was largely unquestioned to a modern framework that prioritizes patient autonomy and rights [62]. This evolution has established informed consent as a crucial pillar of medical and research ethics, requiring that participants receive sufficient information presented in an understandable manner to make a truly voluntary decision [62]. Within clinical research, this process involves providing detailed information about a study's purpose, procedures, potential risks, and the participant's right to withdraw [62]. The methods for documenting this consent—whether paper, electronic, or verbal—have significant implications for regulatory compliance, participant comprehension, and operational efficiency, making the choice of documentation method a critical consideration in study design.
Historical Development and Regulatory Framework
Key Regulatory Milestones
The regulatory landscape for informed consent has undergone significant refinement, with key updates providing more precise guidance for researchers. Table 1 summarizes major regulatory developments.
Table 1: Historical Development of Informed Consent Regulations
| Year | Regulatory Development | Key Provisions/Impacts |
|---|---|---|
| 2018 | EU General Data Protection Regulation (GDPR) | Allows processing of personal data for scientific research under certain exemptions; requires unambiguous consent [62]. |
| 2019 | Revised U.S. Common Rule | Introduced concept of broad consent for secondary use of identifiable private information and biospecimens [62]. |
| 2023 | FDA Final Guidance on Informed Consent | Emphasizes consent as ongoing process; clarifies requirements for electronic documentation and signature validity [46]. |
The Emergence of Broad and Dynamic Consent
Recent regulatory changes have introduced nuanced approaches to consent for research:
- Broad Consent: This approach falls between a waiver and full informed consent, allowing secondary research use of data/biospecimens without re-consenting for each project. However, it carries ethical risks if transparency is lacking regarding data use or commercial partnerships [62].
- Dynamic Consent: Digital platforms enable participants to revisit and adjust their preferences over time, providing a potential solution for balancing research efficiency with ongoing transparency and trust [62].
Comparative Analysis of Documentation Modalities
Quantitative Comparison of Signature Modalities
Table 2 provides a detailed comparison of the three primary documentation methods across critical dimensions relevant to clinical research.
Table 2: Documentation Modality Comparison for Clinical Research
| Feature | Paper Signatures | Electronic Signatures | Verbal Consent (with Witness) |
|---|---|---|---|
| Regulatory Validity | Universally accepted [62] | Legally recognized under eIDAS, UK EA 2000; must comply with 21 CFR 11(c) for FDA-regulated research [63] [64] | Permitted with IRB waiver/alteration for minimal risk research; requires witness documentation [46] |
| Audit Trail | Physical document chain of custody | Digital logs (IP, timestamps); some platforms record interaction data [64] | Summary documentation & witness signature [46] |
| Participant Comprehension | Static text; understanding assumed | Enhanced via multimedia, interactive elements, quizzes [63] | Relies on verbal explanation clarity; no participant review |
| Accessibility | Physical presence typically required | Potential digital divide; concerns for older, rural, minority participants [63] | Highly accessible for low literacy, visual impairments |
| Implementation Scalability | Low (physical storage, mailing costs) | High (enterprise-level systems) but 33% of studies address scalability [63] | Moderate (requires staff time for administration) |
| Data Security | Physical storage risks | Encryption (in transit/at rest); pseudonymization; some concerns about cloud storage [63] | Secured documentation of witnessed consent |
| Signature Process | Wet ink signature on physical document | Typed name, checkbox, or drawn signature [64] | Witness attests to participant's verbal agreement [46] |
Legal Distinctions: Signature vs. Informed Consent
A critical legal distinction exists between obtaining a signature and ensuring genuine informed consent. An electronic signature indicates acceptance but does not verify understanding of content [64]. Informed consent requires demonstrating that the participant received, understood, and freely agreed to the information [64]. Regulatory focus is shifting toward outcomes and comprehension, particularly under frameworks like the FCA's Consumer Duty and GDPR, which require clearer communication and evidence of understanding [64].
Experimental Protocols and Implementation Methodologies
Protocol for Electronic Consent Implementation
Implementing eConsent requires careful planning across technical, usability, and regulatory dimensions. The following workflow outlines a structured approach for deployment in a research setting.
Diagram 1: eConsent implementation workflow.
Phase 1: Pre-Implementation Assessment
- Feasibility Analysis: Determine if the study protocol, participant population, and institutional resources are appropriate for eConsent. Assess computer literacy, language needs, and technology access, particularly for older adults or rural populations who may express greater privacy concerns [63].
- Vendor vs. Homegrown Solution: Evaluate whether to use a commercial eConsent platform, EHR-integrated patient portal, or custom-built system, noting that no leading commercial vendor currently dominates the market [63].
Phase 2: System Development & Validation
- Multimedia Content Development: Create interactive content with embedded videos, quizzes, and graphical elements to enhance understanding. Studies show these features can improve comprehension compared to paper, including among minors [63].
- User Experience (UX) Optimization: Design interfaces with clear navigation and structured information presentation to reduce cognitive load, as measured by tools like the NASA Task Load Index (NASA-TLX) [63].
- Accessibility Compliance: Ensure platform meets WCAG 2.1 AA standards, including minimum contrast ratio of 4.5:1 for normal text and 3:1 for large text [65]. The Text Has Minimum Contrast rule requires sufficient contrast between text and background colors for readability [66].
Phase 3: Regulatory Review & Approval
- IRB Submission: Prepare documentation demonstrating compliance with electronic signature regulations (21 CFR 11 [63]), accessibility standards, and data security protocols.
- Security Documentation: Provide details on encryption methods for data in transit and at rest, identity verification processes, and audit trail capabilities [63].
Protocol for Verbal Consent Documentation
For minimal risk research where written documentation would be impractical or pose the only significant risk, verbal consent with witness documentation may be appropriate.
Diagram 2: Verbal consent documentation process.
Implementation Methodology:
- IRB Approval: Obtain approval for alteration or waiver of signed consent under applicable regulations (45 CFR 46.116[f][3] or FDA guidance for minimal risk studies) [46].
- Standardized Script Development: Create a script containing all required consent elements, using plain language at an appropriate reading level.
- Staff Training: Train research personnel in consistent script delivery, assessing participant understanding, and answering questions without coercion.
- Documentation Process: Complete a short form consent document (if used) or research record note stating consent was obtained verbally, including witness signature [46].
Table 3 outlines key tools and resources for implementing effective consent documentation processes across the three modalities.
Table 3: Research Reagent Solutions for Consent Documentation
| Tool Category | Specific Examples | Research Application & Function |
|---|---|---|
| Electronic Consent Platforms | Custom institutional systems; EHR patient portals; specialized eConsent platforms [63] | Provides multimedia content delivery, interactive comprehension checks, and automated audit trails for regulatory compliance [63] |
| Comprehension Assessment Tools | NASA Task Load Index (NASA-TLX); embedded quizzes; structured knowledge checks [63] | Measures perceived cognitive effort during consent process; validates participant understanding of key study elements [63] |
| Accessibility Validation Tools | WCAG contrast checkers; screen reader compatibility testing; plain language analyzers [67] [65] | Ensures consent materials are accessible to participants with visual, cognitive, or other disabilities; meets legal requirements [67] |
| Digital Signature Systems | DocuSign; Adobe Sign; EU-compliant eIDAS solutions [64] | Provides legally recognized electronic signatures that indicate acceptance of terms, though does not verify comprehension [64] |
| Audit & Documentation Systems | Electronic recordkeeping; version control systems; access logs [63] | Maintains permanent record of consent transactions; tracks changes; supports regulatory inspections and monitoring |
The historical development of informed consent has progressively emphasized participant autonomy, comprehension, and ethical treatment. While paper signatures remain universally accepted, electronic methods offer significant advantages in enhancing understanding through multimedia and interactive features, provided accessibility and digital divide concerns are addressed. Verbal consent with proper documentation serves a specific role for minimal risk scenarios. The choice between electronic, verbal, and paper signatures must be guided by protocol specifics, participant population, regulatory environment, and the fundamental distinction between mere signature acquisition and genuine informed consent. Future developments will likely see increased adoption of dynamic consent models that enable ongoing participant engagement, particularly as research grows more complex and data sharing becomes more prevalent.
Navigating Complex Consent Scenarios: Waivers, Vulnerable Populations, and Digital Solutions
The doctrine of informed consent represents a cornerstone of ethical research and clinical practice, establishing the fundamental principle that individuals must autonomously authorize any medical intervention or research participation based on adequate understanding of relevant risks, benefits, and alternatives [13]. Its historical development reflects a profound shift from medical paternalism toward respect for patient autonomy, with landmark cases like Schloendorff v. Society of New York Hospital (1914) establishing the legal precedent that "every human being of adult years and sound mind has a right to determine what shall be done with his own body" [13]. The atrocities of World War II and subsequent studies like the Tuskegee Syphilis Study further catalyzed the formalization of informed consent requirements through frameworks like the Nuremberg Code and the Declaration of Helsinki, which cemented informed consent as an indispensable ethical standard in both research and clinical contexts [13].
Despite this foundational status, the practical implementation of informed consent has continually evolved to address complex contemporary challenges in research. Technological advances, diverse patient populations, and an increasing emphasis on collaborative decision-making have prompted reassessment of traditional consent models [13]. Within this evolutionary context, specific regulatory provisions have emerged to address circumstances where strict adherence to conventional informed consent requirements may be impracticable or unnecessary while maintaining rigorous protection for human subjects. This guide provides a comprehensive technical analysis of two critical regulatory frameworks permitting Institutional Review Board (IRB)-approved modifications to standard consent procedures: § 50.22 (FDA regulations) and § 46.116(f) (Common Rule). These provisions establish legally valid pathways for waiving or altering consent elements for minimal risk research, representing a significant harmonization between FDA and Common Rule regulations while safeguarding the ethical principles underlying human subjects research [68] [69].
Regulatory Framework and Historical Context
The Common Rule: 45 CFR 46.116(f)
The Federal Policy for the Protection of Human Subjects, known as the Common Rule, provides the foundational ethical framework for human subjects research conducted or supported by federal departments and agencies. § 46.116(f) establishes the conditions under which an IRB may waive or alter the standard informed consent requirements [44]. This provision acknowledges that certain minimal risk research cannot practicably be carried out without modifying consent procedures, while ensuring such modifications do not adversely affect subjects' rights and welfare [44].
FDA Regulations: 21 CFR 50.22
Historically, FDA regulations maintained more restrictive provisions regarding informed consent exceptions, primarily permitting exceptions only in life-threatening situations or through Presidential waiver for specific military operations [68]. This created regulatory discordance with the Common Rule, complicating protocol review and implementation for FDA-regulated research. The 21st Century Cures Act (Section 3024) mandated that FDA harmonize its informed consent regulations with the Common Rule, culminating in the creation of § 50.22 through a final rule published December 21, 2023, with an effective date of January 22, 2024 [68] [69].
Regulatory Harmonization
This regulatory harmonization represents a significant advancement in human subjects protection, creating consistent standards across federal agencies while enabling important minimal risk research that might otherwise be impracticable [68]. The FDA anticipates this alignment will "help enable the conduct of certain minimal risk clinical investigations for which the requirement to obtain informed consent is waived or for which certain elements of informed consent are waived or altered" without compromising ethical safeguards [68].
Table: Historical Development of Informed Consent Exceptions
| Year | Regulatory Development | Key Impact |
|---|---|---|
| 1991 | Common Rule establishes initial waiver criteria | Created baseline standards for IRB waiver of consent |
| 2017 | Revised Common Rule published | Modified and clarified waiver provisions at §46.116(f) |
| 2016 | 21st Century Cures Act enacted | Mandated FDA harmonization with Common Rule consent provisions |
| 2023 | FDA Final Rule published | Established §50.22, creating parallel to Common Rule waiver criteria |
| 2024 | FDA §50.22 effective date | Completed harmonization between FDA and Common Rule requirements |
Comparative Analysis of §50.22 and §46.116(f)
Regulatory Criteria for Waiver or Alteration
For an IRB to approve a waiver or alteration of informed consent under either regulatory framework, specific criteria must be satisfied and documented. The following table provides a detailed comparison of these requirements:
Table: Comparative Analysis of Waiver and Alteration Criteria
| Criteria | 21 CFR 50.22 (FDA) | 45 CFR 46.116(f) (Common Rule) | Interpretive Guidance |
|---|---|---|---|
| Risk Profile | Clinical investigation involves no more than minimal risk [69] | Research involves no more than minimal risk [44] | "Minimal risk" defined as probability/magnitude of harm not greater than daily life/routine exams [69] |
| Rights/Welfare Impact | Waiver/alteration will not adversely affect rights/welfare of subjects [69] | Waiver/alteration will not adversely affect rights/welfare of subjects [44] | IRB considers if waiver negatively affects well-being or if population would object [69] |
| Practicality | Clinical investigation could not practicably be carried out without waiver/alteration [69] | Research could not practicably be carried out without waiver/alteration [44] | "Practicably" assessed case-by-case; considers scientific validity, bias, undue delay [69] |
| Identifiable Information | If using identifiable private information/biospecimens, investigation could not practicably be conducted without using identifiable format [69] | If research involves identifiable private information/biospecimens, research could not practicably be conducted without such information in identifiable format [44] | Applies when research involves existing data/biospecimens collected for other purposes [69] |
| Debriefing | Additional element: Whenever appropriate, subjects will be provided with additional pertinent information after participation [69] | Not explicitly required | FDA-specific requirement for post-participation disclosure when scientifically feasible |
Scope and Application
While the regulatory criteria demonstrate substantial alignment, important distinctions exist in their scope and application:
- § 50.22 applies specifically to FDA-regulated clinical investigations, including studies of drugs, biological products, and medical devices [68] [69]
- § 46.116(f) applies to human subjects research conducted or supported by federal departments/agencies that have adopted the Common Rule [44]
- Both provisions exempt research from standard informed consent requirements but maintain requirements for IRB review and approval [44] [69]
The FDA has clarified that § 50.22 is not intended to disrupt existing guidance for in vitro diagnostic (IVD) device studies using leftover human specimens that are not individually identifiable, noting that "most IVD device investigations falling within the scope of the policy... will satisfy the criteria at § 50.22" [69].
Implementation Methodologies and Procedural Requirements
IRB Review and Documentation Procedures
Successful implementation of waiver or alteration provisions requires meticulous IRB procedures and documentation. The following workflow illustrates the systematic approach IRBs must employ when reviewing requests for waiver or alteration of informed consent:
IRB Review Process for Waiver or Alteration Requests
Investigator Requirements and Documentation Standards
Researchers seeking waiver or alteration of informed consent must provide comprehensive justifications addressing each regulatory criterion. The following table outlines essential documentation elements:
Table: Documentation Requirements for Waiver or Alteration Requests
| Documentation Element | Regulatory Reference | Required Content |
|---|---|---|
| Risk Justification | §50.22(a); §46.116(f)(1) | Detailed analysis demonstrating minimal risk relative to daily life/routine exams |
| Rights/Welfare Protection | §50.22(b); §46.116(f)(2) | Explanation of how waiver preserves rights/welfare; population perspectives |
| Practicability Analysis | §50.22(c); §46.116(f)(3) | Scientific justification: potential bias, validity concerns, recruitment barriers |
| Identifiable Information | §50.22(d); §46.116(f)(4) | For existing data/biospecimens: justification for identifiability necessity |
| Debriefing Plan | §50.22(e) | FDA-specific: plan for providing pertinent information after participation |
Practical Application Contexts
Regulatory agencies have identified specific research contexts where waiver or alteration may be appropriate:
- Secondary research with leftover biospecimens: When identifiers cannot be readily removed and research would be impracticable with consenting subjects only [69]
- Medical records reviews: Where contacting subjects would be impracticable and risk is minimal [69]
- Emergency medicine research: When exception from informed consent requirements applies under separate regulations [68]
- Rare disease research: Where patient populations are small and traditional consent may be impracticable [70]
- Public health surveillance: Conducted by or subject to approval of state/local officials [44]
The FDA emphasizes that "practicability should be assessed on a case-by-case basis considering the unique factors associated with the clinical investigation," including scientific aims, population characteristics, and potential validity impacts if informed consent were required [69].
Regulatory and Ethical Reference Materials
Successful navigation of waiver and alteration processes requires access to key regulatory and ethical resources:
Table: Essential Research Reagents for Waiver Implementation
| Resource Category | Specific Tools | Application in Waiver Context |
|---|---|---|
| Regulatory Guidance | FDA Final Rule (December 2023); Revised Common Rule (2017) | Primary regulatory interpretation; historical context for harmonization |
| Ethical Frameworks | Nuremberg Code; Declaration of Helsinki; Belmont Report | Foundational ethical principles for evaluating waiver requests |
| IRB Documentation | Waiver request templates; SOPs for minimal risk determination | Standardized approaches to criterion justification; review consistency |
| Risk Assessment | Minimal risk comparators database; risk categorization tools | Objective benchmarks for daily life/routine exam comparisons |
| Legal Reference | 21st Century Cures Act Section 3024; FD&C Act provisions | Statutory authority for regulatory harmonization |
Practical Implementation Tools
Researchers and IRBs should employ specific methodological tools to strengthen waiver justifications:
- Bias assessment frameworks: Document how requiring consent would compromise scientific validity through selection bias [69]
- Recruitment feasibility analyses: Demonstrate impracticality of recruiting consenting subjects without unduly delaying research [69]
- Cultural competency resources: Address diverse perspectives on research participation and consent [13]
- Data identifiability assessment tools: Evaluate whether research can practicably be conducted with non-identifiable data [69]
Emerging Trends and Future Directions
The implementation of §50.22 and §46.116(f) occurs alongside evolving approaches to informed consent in biomedical research. Several emerging trends warrant consideration:
Alternative Consent Models
- Verbal consent processes: Increasingly utilized in minimal risk research, particularly during COVID-19, requiring careful documentation through scripts or recordings [70]
- Broad consent frameworks: Permitting secondary research use of identifiable information/biospecimens with general descriptions of research types [62]
- Dynamic consent platforms: Digital approaches allowing participants to adjust consent preferences over time, potentially addressing transparency concerns with broad consent [62]
Technological Impacts
Technological advances continue to reshape consent exceptions:
- Artificial intelligence and big data: Creating new challenges for defining identifiability and minimal risk in computational research [62]
- Teleconsent platforms: Emerging from COVID-19 emergency measures, potentially influencing future waiver assessments [70]
- Data security advancements: Affecting practicability analyses for research with identifiable information [69]
The FDA has committed to ongoing consultation with experts to reexamine the meaning of "identifiable private information" and "identifiable biospecimen" in light of evolving technologies, ensuring regulatory frameworks remain current with methodological advances [69].
The harmonization of FDA §50.22 with Common Rule §46.116(f) represents a significant evolution in informed consent regulations, acknowledging that ethical research requires both robust participant protection and practical implementation frameworks. These provisions enable important minimal risk research that would otherwise be impracticable while maintaining fundamental ethical safeguards. As informed consent continues to evolve beyond its historical roots in medical paternalism toward more nuanced, participant-centered approaches, researchers and IRBs must maintain diligent adherence to both regulatory requirements and ethical principles. Through careful implementation of these provisions, the research community can advance scientific knowledge while honoring its commitment to respecting participant autonomy and welfare.
Strategies for Overcoming Language Barriers and Low Health Literacy
The evolution of informed consent from a simple signature to a comprehensive communication process underscores its centrality in ethical clinical practice and research [13]. This process, legally established to protect patient autonomy, requires that individuals possess sufficient knowledge and comprehension of the medical procedures they are undergoing [12]. However, the increasing linguistic diversity of patient populations and the pervasive challenge of low health literacy present substantial obstacles to achieving truly informed consent. In the United States alone, approximately one in five households now speaks a language other than English at home, creating significant communication challenges in healthcare settings [71]. Simultaneously, over 90 million people in the U.S. lack the health literacy skills needed to properly understand and act on health information [72]. These barriers are not merely inconveniences; they directly impact patient outcomes, with studies showing that patients with limited English proficiency (LEP) have longer hospital stays and a 15-25% higher risk of 30-day readmission [71]. This technical guide examines evidence-based strategies to overcome these challenges, framed within the historical and ethical imperative of informed consent.
Historical Context and Legal Foundations of Informed Consent
The concept of informed consent has evolved significantly since its early judicial foundations. The 1914 case of Schloendorff v. Society of New York Hospital established the fundamental principle that "every human being of adult years and sound mind has a right to determine what shall be done with his own body" [13] [12]. This ruling laid the groundwork for patient autonomy, which was further solidified after World War II through the Nuremberg Code, which emphasized voluntary consent as the first principle for ethical human subjects research [12].
The term "informed consent" first appeared officially in the 1957 case Salgo v. Leland Stanford Jr. University Board of Trustees, which highlighted the physician's duty to disclose potential risks and benefits of procedures [12]. These legal developments established that valid consent requires not just agreement, but comprehension—a challenge when language barriers or low health literacy impede understanding. The modern informed consent process serves both ethical and legal functions by safeguarding patient rights, fostering transparency, and promoting trust between healthcare professionals and patients [13].
Quantitative Assessment of Communication Barriers
Impact of Language Barriers on Informed Consent Documentation
A matched retrospective chart review study at a major teaching hospital with on-site interpreter services revealed significant disparities in informed consent documentation between English-speaking patients and those with LEP [73].
Table 1: Documentation of Informed Consent for Invasive Procedures
| Patient Group | Full Documentation of Informed Consent | Signed Consent Form (Any Language) | Consent Discussion Documented |
|---|---|---|---|
| English Speakers | 53% | 85% | Similar between groups |
| Limited English Proficiency | 28% | 70% | Similar between groups |
Despite the availability of professional interpreter services, LEP patients were significantly less likely to have complete informed consent documentation (OR: 2.81; 95% CI, 1.42-5.56; p=0.003) [73]. After multivariate analysis adjusting for patient and service factors, English speakers remained more likely to have full documentation (Adj OR: 3.10; 95% CI, 1.49-6.47; p=0.003) [73].
Health Literacy and Treatment Adherence Relationship
A comprehensive meta-analysis of 220 published articles revealed significant correlations between health literacy and treatment adherence across various medical conditions and regimens [72].
Table 2: Health Literacy and Adherence Relationships Across Studies
| Relationship | Effect Size (r) | Significant Moderators |
|---|---|---|
| Health literacy & adherence correlation | 0.14 | Higher association for non-medication regimens and cardiovascular disease |
| Health literacy intervention on literacy outcomes | 0.22 | Greater efficacy with subjective measures |
| Health literacy intervention on adherence outcomes | 0.16 | Greater effect in lower income and racial-ethnic minority samples |
The meta-analysis found that health literacy interventions had a more substantial effect on adherence in vulnerable populations, highlighting their potential to reduce healthcare disparities [72].
Experimental Protocols and Methodologies
Protocol: Assessing Informed Consent Documentation with Language Barriers
The methodology from the matched retrospective chart review provides a validated approach for assessing institutional performance in obtaining informed consent across language barriers [73].
Objective: Determine the impact of language barriers on documentation of informed consent among hospitalized patients.
Design: Matched retrospective chart review study.
Subject Selection:
- Identify patients who received specific invasive procedures (thoracentesis, paracentesis, lumbar puncture) through ICD-9 code search
- Group patients by language preference (LEP vs. English-speaking)
- Match LEP and English-speaking patients by procedure, hospital service, and procedure date
- Exclude patients lacking decision-making capacity, those with consent forms signed by surrogates, and procedures performed in interventional radiology or operating rooms
Data Collection:
- Abstract charts for procedure notes and signed consent forms
- For LEP patients, document evidence of interpretation services used
- Verify patient's primary language through chart documentation
- Perform blinded reabstraction of 15% of charts to ensure reliability (kappa coefficient = 0.83)
Outcome Measures:
- Full documentation of informed consent (requires procedure note documenting consent discussion AND signed consent form)
- For LEP patients: additional requirement of evidence of interpretation
Analysis:
- Use chi-square analysis to determine differences between groups
- Perform multivariate analysis to adjust for patient and service factors
Protocol: Pharmaceutical Health Literacy Intervention Model
A novel Pharmaceutical Health Literacy Intervention (PHLI) model implemented in a psychiatric hospital demonstrates a comprehensive approach to addressing health literacy challenges [74].
Organizational Structure:
- Establish an interdisciplinary team including pharmacy, medical, nursing, and community representatives
- Train clinical pharmacists in health literacy intervention methods
- Develop standard operating procedures for pharmaceutical services
Intervention Modes:
Inpatient-Based PHLI:
- Admission: Medication reconciliation and health literacy assessment with weekly follow-up for patients with low health literacy
- Hospitalization: Address medication questions and provide targeted interventions for special cases
- Discharge: Create educational list covering diagnosis, dosage, adverse reactions, and countermeasures
- Retrospective Analysis: Use Hospital Information Systems (HIS) to identify patients for focused re-rounds
Outpatient-Based PHLI:
- Pharmacist-Managed Clinics (PMC): Provide medication therapy management and education
- Therapeutic Drug Monitoring (TDM): Explain significance of results and implications for treatment
Internet-Based PHLI:
- WeChat Public Accounts: Disseminate medication information through widely used platforms
- Digital Tools: Implement medication therapy management systems
Evaluation Metrics:
- Medication adherence rates
- Prescription complexity comprehension
- Adverse reaction reporting
- Readmission rates
Visualization of Intervention Workflows
Comprehensive Health Literacy Intervention Strategy
Pharmaceutical Health Literacy Intervention Model
Table 3: Research Reagent Solutions for Communication Barrier Studies
| Tool/Solution | Function | Application Context |
|---|---|---|
| Professional Medical Interpreters | Bridge language gaps with trained specialists; serve as cultural brokers | Clinical encounters, informed consent discussions, treatment education |
| Health Literacy Assessment Tools (TOFHLA, REALM) | Objectively measure patient health literacy levels | Research screening, intervention targeting, outcome measurement |
| Teach-back Method | Verify patient understanding by having them explain in their own words | Informed consent process, discharge instructions, medication education |
| "Chunk-Check" Technique | Break complex information into manageable segments with comprehension checks | Explaining multi-step treatments, complex medication regimens |
| Transcreated Audiovisual Materials | Adapt educational content for specific cultural/linguistic contexts | Clinical trial recruitment, patient education, informed consent |
| Telephone/Video Interpreter Services | Provide on-demand language access | Settings without on-site interpreters, emergency situations |
| Plain Language Documentation | Create materials at appropriate literacy levels | Consent forms, patient instructions, research summaries |
| Multimedia Educational Programs | Enhance understanding through multiple sensory channels | Clinical trial education, treatment protocol explanation |
Implementation Framework and Best Practices
Working Effectively with Medical Interpreters
Medical interpreters serve not only as language translators but also as cultural brokers who help bridge cultural divides between patients and clinicians [71]. Evidence shows that using professional interpreters improves communication, clinical outcomes, and satisfaction with care [75]. The following evidence-based protocol ensures effective use of interpreter services:
Before the Encounter:
- Ensure the interpreter is from the correct region and dialect group
- Provide a brief report on the purpose of the encounter and patient history
- Review the plan for the encounter and request culturally appropriate guidance [75]
During the Encounter:
- Maintain eye contact with the patient, not the interpreter
- Speak in shorter sentences than normal to improve translation accuracy
- Use one or two sentences at a time, then allow time for interpretation [71] [75]
- Ask specifically about the patient's thoughts on their health and treatment preferences
- Avoid interrupting the interpreter during translation
After the Encounter:
- Obtain feedback from both the patient and interpreter about the interaction
- Provide the patient with a method to connect with questions later [75]
- Document the use of an interpreter in the medical record [76]
Health Literacy Universal Precautions
Implementing health literacy universal precautions assumes that all patients may have difficulty understanding health information and creates a shame-free environment where questions are encouraged [76]. Key strategies include:
- Slow down: Speak slowly and focus on the patient. Sit rather than stand to reduce power differentials [76]
- Use plain language: Replace medical jargon with common everyday words
- Limit information: Focus on the 3-5 most important points and emphasize them repeatedly
- Use visual aids: Models, pictures, and diagrams improve understanding and recall
- Create a shame-free environment: Instead of asking "Do you understand?" which tends to elicit yes responses regardless of actual understanding, ask "What questions do you have?" or "How will you explain this to your family?" [76]
- Implement system-level safeguards: Make it clear that patients can call later with questions and provide accessible contact information
Overcoming language barriers and addressing low health literacy is both an ethical imperative and a practical necessity in modern healthcare and clinical research. The historical development of informed consent establishes comprehension as equally important as mere agreement, requiring active strategies to ensure genuine understanding [12]. The evidence demonstrates that systematic approaches—combining professional interpreters, health literacy universal precautions, cultural brokerage, and technology solutions—can significantly improve communication, adherence, and patient outcomes [72] [71] [74].
Future efforts must focus on organizational health literacy, creating systems that make it easier for patients to navigate, understand, and use health information and services [13] [77]. For researchers and drug development professionals, addressing these barriers is particularly crucial for ensuring diverse clinical trial participation and validating interventions across population groups [78]. As healthcare continues to globalize, developing robust, evidence-based strategies to overcome communication barriers will remain essential to fulfilling the ethical promise of truly informed consent and patient-centered care.
Obtaining Consent in Emergency and Life-Threatening Situations (§50.23)
Informed consent serves as a cornerstone of ethical clinical practice and research, grounded in the principle of patient autonomy and the right to self-determination [13] [12]. In most circumstances, it necessitates a comprehensive communication process where healthcare providers educate patients about the nature, risks, benefits, and alternatives of a procedure or intervention [13]. However, emergency and life-threatening situations present unique challenges where the standard consent process may not be feasible due to time constraints, the patient's clinical condition, or the immediacy of the required intervention. These scenarios are addressed in the U.S. Food and Drug Administration (FDA) regulations under 21 CFR 50.23, which provides specific exceptions to the general informed consent requirements [79].
This technical guide examines the regulatory, ethical, and practical dimensions of obtaining consent in emergencies, framing them within the historical development of informed consent. It provides researchers, scientists, and drug development professionals with detailed methodologies and frameworks for navigating these complex situations while ensuring the protection of human subjects and compliance with evolving regulatory standards.
Historical and Regulatory Context of Informed Consent
The concept of informed consent has evolved significantly from a paternalistic medical model to an autonomy-based framework. Early 20th-century legal cases established its foundational principles.
Table 1: Landmark Legal Cases Establishing Informed Consent Principles
| Case (Year) | Legal Principle Established | Relevance to Patient Autonomy |
|---|---|---|
| Mohr v Williams (1905) [12] | Surgeon must obtain consent for specific procedures; changing plan without consent constitutes battery. | Established that consent is procedure-specific and cannot be unilaterally altered by the physician. |
| Pratt v Davis (1905) [12] | A physician cannot perform procedures without patient consent, even if deemed medically beneficial. | Affirmed the "right to oneself" and bodily integrity as a fundamental right that forbids unauthorized procedures. |
| Schloendorff v Society of New York Hospital (1914) [13] [12] | "Every human being of adult years and sound mind has a right to determine what shall be done with his own body." | Solidified the principle of patient autonomy as the legal and ethical foundation for informed consent. |
The term "informed consent" first appeared in the 1957 case Salgo v Leland Stanford Jr University Board of Trustees, which established the physician's duty to disclose potential risks [12]. The aftermath of World War II and the Nuremberg Code further cemented informed consent as a fundamental ethical standard, particularly in research, emphasizing voluntary consent and sufficient knowledge and comprehension from the participant [13] [12].
In the United States, these principles were codified into federal regulations, including the Common Rule (45 CFR 46) and FDA regulations 21 CFR 50 [12]. These frameworks acknowledge that while informed consent is a default requirement, specific exceptions are necessary in emergency contexts.
The Emergency Exception to Informed Consent (§50.23)
FDA regulation 21 CFR 50.23 provides a narrow exception from the standard informed consent process for emergency medical situations [79]. This exception applies when both the patient is unable to give consent and no legally authorized representative is immediately available, yet a life-saving intervention must be administered without delay.
Regulatory Criteria and Conditions
For the exception to be invoked, specific conditions must be met:
- Life-Threatening Situation: The patient must be confronted by a life-threatening condition [79].
- Lack of Proven Therapies: Available treatments must be unproven or unsatisfactory [79].
- Informed Consent Not Feasible: It must be objectively impossible to obtain consent from the patient (due to their medical condition) or from their legal representative in the available time [79].
- Potential for Direct Benefit: The research intervention must hold the possibility of direct benefit to the patient, justifying the risks taken [79].
Furthermore, the investigation could not practically be carried out without this waiver [79]. The regulation also mandates that additional protections, such as consultation with an independent physician and subsequent disclosure to the patient or their representative, must be implemented whenever feasible [79].
Informed Consent Protocols for Emergency Research (§50.24)
For planned emergency research where the exception in §50.23 is anticipated and systematically used, researchers must adhere to the stricter requirements of 21 CFR 50.24, which governs "Exception from Informed Consent for Emergency Research" (EFIC) [79].
Key Requirements for EFIC
Table 2: Requirements for Emergency Research Under an Exception from Informed Consent (EFIC) [79]
| Requirement Category | Specific Obligations |
|---|---|
| Community Consultation | The research team must engage in a two-way communication process with the community from which participants will be drawn, educating them about the study and the need for the consent exception [79]. |
| Public Disclosure | Prior to the study, researchers must publicly disclose the trial's plans, risks, and benefits. After completion, they must disclose its results [79]. |
| Institutional Review Board (IRB) Oversight | The IRB must provide intensive, ongoing review of the study, with the frequency of review commensurate with the level of risk [79]. |
| Informed Consent for Continued Participation | Whenever feasible, consent must be sought from the patient or their family for the patient's continued participation in the research after the emergency intervention has been applied [79]. |
Alternative Consent Models in Emergency Settings
Beyond the EFIC pathway, several conceptual models have been developed to address the ethical challenges of research in emergencies.
Prospective Consent involves identifying an at-risk population and obtaining their consent for potential future research participation should they experience a specific emergency [79]. A key challenge is whether consent can be truly informed when the chance of actually developing the emergency condition is low, potentially leading individuals to give little thought to the consequences [79].
Deferred Consent involves enrolling participants in a study without initial consent, with consent sought at a later, more appropriate time for continued participation [79]. A significant methodological concern is the risk of bias in data analysis if participants who refuse deferred consent are excluded, as their data may differ systematically from those who consent [79].
Proxy Consent allows a legally authorized representative to make decisions on behalf of the incapacitated patient [79]. The primary difficulty lies in ensuring that the proxy accurately represents what the patient would have wanted, rather than their own preferences [79].
Empirical Data on Consent Comprehension and Current Practices
Understanding the effectiveness of consent processes is critical, even in non-emergency settings. A systematic review of empirical studies on patient comprehension revealed significant limitations in participants' understanding of key informed consent components [80].
Table 3: Patient Comprehension of Specific Informed Consent Components [80]
| Informed Consent Component | Range of Participant Comprehension | Notes and Variations |
|---|---|---|
| Voluntary Participation | 53.6% - 96% | Lowest comprehension was associated with perceptions that physicians might persuade participation [80]. |
| Freedom to Withdraw | 63% - 100% | A relatively well-comprehended component, though understanding of withdrawal consequences was much lower (44%) [80]. |
| Randomization | 10% - 96% | Understanding was generally low, with one study reporting only 10% comprehension [80]. |
| Placebo Concept | 13% - 97% | Comprehension varied significantly by medical specialty (e.g., ophthalmology 13% vs. rheumatology 49%) [80]. |
| Risks & Side Effects | 7% - 100% | The 100% figure was from a study where participants could use the IC text to find answers; otherwise, comprehension was very low [80]. |
These findings underscore that the informed consent process often fails to achieve its goal of ensuring patient comprehension, which is a serious concern for the ethical foundation of clinical research [80]. This highlights the need for improved communication strategies, especially in high-stress environments like emergencies.
Recent Developments and Best Practices
A 2025 report from the NIH Pragmatic Trials Collaboratory argues that even for minimal-risk studies conducted under a waiver of consent, providing information to participants should be the default [37]. This notification can be achieved through letters, emails, posters, or conversations with clinicians, and serves to promote respect for persons, enhance trust in research, and engage participants [37].
Furthermore, the 2025 updates to the FDAAA 801 Final Rule have introduced stricter transparency measures, including a mandate for the public posting of redacted informed consent forms for applicable clinical trials on ClinicalTrials.gov [81]. This move acknowledges growing calls for patient-centricity and transparency [81].
The Scientist's Toolkit: Research Reagent Solutions
Navigating the regulatory landscape of emergency consent requires specific tools and documentation. The following table details essential components for ensuring compliance and ethical integrity.
Table 4: Essential Materials for Emergency Consent Research
| Item or Concept | Function in Emergency Consent Research |
|---|---|
| Community Consultation Plan | A predefined strategy for engaging with the community to educate them about the emergency research and the need for a consent exception, fostering trust and transparency [79]. |
| IRB-Approved Protocol with Waiver | The formal research protocol that explicitly details the justification for an exception from informed consent and has received approval from a governing IRB [79]. |
| Public Disclosure Materials | Documents (e.g., summaries, flyers, website content) used to inform the public about the study's purpose, risks, benefits, and the fact that it is conducted under an EFIC [79]. |
| Deferred Consent Form | The consent document presented to the patient or their representative after the emergency intervention to obtain permission for continued participation in the study and use of data [79]. |
| Data Monitoring Plan for Withdrawals | A methodological plan for handling data if a participant refuses or withdraws consent under a deferred model, crucial for minimizing bias in the study analysis [79]. |
| Radafaxine | Radafaxine, CAS:192374-14-4, MF:C13H18ClNO2, MW:255.74 g/mol |
| 3-Chloroiminodibenzyl | 3-Chloroiminodibenzyl, CAS:32943-25-2, MF:C14H12ClN, MW:229.70 g/mol |
Obtaining consent in emergency and life-threatening situations represents a critical intersection of clinical need, ethical imperative, and regulatory compliance. The frameworks provided by §50.23 and §50.24 acknowledge the practical realities of emergencies while establishing robust safeguards to protect patient autonomy and welfare. The historical evolution of informed consent, from foundational legal cases to the nuanced regulations of today, underscores a consistent commitment to the principle of self-determination. For today's researchers and drug developers, success in this complex field requires a disciplined adherence to protocols, a genuine commitment to community consultation and transparency, and the thoughtful application of innovative consent models. As the regulatory environment evolves—emphasizing greater transparency and patient engagement—the ethical conduct of emergency research will continue to depend on balancing the urgent need for life-saving knowledge with an unwavering respect for the rights and dignity of every participant.
Safeguards for Research with Vulnerable Populations
The development of safeguards for vulnerable populations in research is inextricably linked to the historical evolution of informed consent. The current ethical research environment has been shaped profoundly by past civil rights violations, from the infamous Nazi human experiments and the Tuskegee syphilis study to radiation research, which collectively promoted sustained maturation of clinical bioethical research environments [82]. These historical cases were characterized by lack of informed consent, coercive influences, impaired risk-benefit ratios, and unjustified research population selections, ultimately prompting international regulations to stand firm on principles advocating conscientious clinical and ethical research systems [82].
The legal foundation for informed consent began forming in the early 20th century through a series of judicial decisions that established patient autonomy. The 1905 case of Mohr v Williams established that surgeons must obtain consent before performing procedures, while Schloendorff v Society of New York Hospital (1914) legally solidified the principle that "every human being of adult years and sound mind has a right to determine what shall be done with his own body" [14]. The term "informed consent" first appeared formally in the 1957 case Salgo v Leland Stanford Jr University Board of Trustees, which focused on the duty of physicians to disclose potential risks [14].
A pivotal moment in research ethics came in 1966 when Henry K. Beecher, MD, published "Ethics and Clinical Research" in the New England Journal of Medicine, describing 22 examples of ethical violations in prominent American research studies [83]. This "bombshell" report armed proponents of regulation with concrete evidence of widespread impropriety and ultimately led to the establishment of institutional review boards (IRBs) and the formalization of requirements for protecting vulnerable research participants [83].
Defining Vulnerability in Research Contexts
Conceptual Foundations and Regulatory Definitions
Vulnerability in research is a complex, multifaceted concept. The National Bioethics Advisory Commission (NBAC) defines vulnerability as "a condition, either intrinsic or situational, of some individuals that puts them at greater risk of being used in ethically inappropriate ways in research" [84]. Similarly, the Declaration of Helsinki characterizes vulnerable groups and individuals as those who "may have an increased likelihood of being wronged or of incurring additional harm" [84]. A critical understanding is that vulnerability is not a binary state but occurs along a spectrum—a particular situation or characteristic may place a person at greater or lesser risk of harm [84].
Approaches to Understanding Vulnerability
Table 1: Approaches to Defining Vulnerability in Research
| Approach | Key Characteristics | Limitations | Best Use Cases |
|---|---|---|---|
| Categorical Approach | Considers certain groups or populations as vulnerable based on shared features [84] | Does not address persons with multiple vulnerabilities; doesn't account for individual variation within groups; classifies persons rather than situations [84] | When all members of a group are vulnerable for the same reason (e.g., all children lack fully developed decision-making capacity) [84] |
| Contextual Approach | Identifies situations in which individuals might be considered vulnerable; allows nuanced understanding [84] | Requires more careful case-by-case analysis; less predictable than categorical approach | Complex research scenarios; persons with multiple vulnerabilities; when vulnerability may be temporary or situational [84] |
The Common Rule (45 CFR §46) takes primarily a categorical approach, specifically identifying children, prisoners, pregnant women, fetuses, mentally disabled persons, and economically and educationally disadvantaged persons as vulnerable populations [84]. However, contemporary ethical guidance increasingly recognizes the importance of contextual factors that may create or exacerbate vulnerability.
Categories of Vulnerable Populations
Vulnerable populations in research include but are not limited to: children, minors, pregnant women, fetuses, human in vitro fertilization, prisoners, employees, military persons and students in hierarchical organizations, terminally ill, comatose, physically and intellectually challenged individuals, institutionalized elderly individuals, visually or hearing impaired, ethnic minorities, refugees, international research participants, economically and educationally disabled, and healthy volunteers [82]. Due to their circumstances, these communities may be inclined to participate in clinical studies or be unjustifiably influenced by expectations of predicted benefits associated with participation [82].
Core Ethical Frameworks and Regulatory Requirements
Foundational Ethical Principles
The ethical framework for protecting vulnerable research participants rests on three core principles established in the Belmont Report:
- Respect for Persons: Recognizing the personal dignity and autonomy of individuals, and providing special protection for those with diminished autonomy [84]
- Beneficence: Obligating researchers to minimize potential harms and maximize benefits
- Justice: Ensuring fair distribution of the burdens and benefits of research
The Belmont Report explicitly states that "persons with diminished autonomy are entitled to protection," establishing the philosophical foundation for additional safeguards for vulnerable populations [84].
Regulatory Requirements
The US Department of Health and Human Services Policy for Protection of Human Subjects requires that "when some or all of the subjects are likely to be vulnerable ... additional safeguards have been included in the study to protect the rights and welfare of these subjects" (45 CFR §46.111(b)) [84]. This requirement extends beyond the general mandate to minimize risks and ensure a favorable risk-benefit ratio for all research participants.
Specific Safeguards and Methodological Approaches
Comprehensive Informed Consent Processes
The informed consent process requires particular attention when working with vulnerable populations. The quality of informed consent has an impressive influence on research tenets with direct implications for comprehension of the proposed study, particularly in vulnerable subjects [82]. Key enhancements to standard consent procedures include:
Comprehension-Focused Design: Consent documents should use language equivalent to local middle school education level and avoid technical jargon [82]. Documents should not be lengthy, and including a frequently asked questionnaire with a simple summary of study goals can enhance comprehension [82].
Adapted Communication Methods: Usage of audiovisual and illustrative tools enhances the quality of the consent process [82]. The font of written documentation should be easy to read, accommodating both pediatric and geriatric patients [82].
Independent Oversight: The presence of independent consent and ethical review board monitors supervising procedures in assessing decisional capacities, re-consent, and follow-up during the study promotes additional safeguards [82].
Process-Based Approach: Consent should be viewed as an ongoing process rather than a one-time event. For participants with fluctuating capacities, staged consent may be appropriate, where formal consent is obtained several times during the research by presenting manageable blocks of information [84].
Population-Specific Safeguards
Table 2: Specific Safeguards for Vulnerable Populations
| Population | Specific Vulnerabilities | Recommended Safeguards |
|---|---|---|
| Pregnant Women | Scientific and social concerns of potential risks to embryo, fetus, and neonate [82] | Justification for inclusion/exclusion; preclinical reproductive/developmental toxicity data; special ERB review for physically invasive procedures; pregnancy registries for follow-up [82] |
| Children & Minors | Limited cognitive/emotional capabilities; cannot legally provide consent [82] | Parental permission; age-appropriate assent process; simplified assent forms; consideration of child's developing autonomy [82] |
| Intellectually Challenged | Difficulty comprehending information and making decisions [82] | Assessment of decisional capacity; use of legally authorized representatives; plan for participants who may regain capacity [82] |
| Institutionally Vulnerable (prisoners, military, hierarchical organizations) | Limited ability to make truly free decisions due to formal authority structures [84] | Consent procedures that insulate participants from hierarchical systems; having persons other than investigators approach potential participants [84] |
| Cognitively or Communicatively Vulnerable | Difficulty comprehending information or communicating decisions [84] | Plain-language consent forms; supplementary educational measures; interpreters; staged consent; delayed enrollment until transient vulnerabilities resolve [84] |
Institutional Safeguards and Oversight Mechanisms
Robust institutional safeguards are essential for protecting vulnerable research participants:
Ethical Review Board (ERB) Oversight: Protection of rights, well-being, safety with measurements of risk-benefit scales, privacy and confidentiality of vulnerable subjects are prerogatives of ERBs [82]. Competent and trained ERBs overseeing sensitive studies should observe full-scheduled reviews and may include representatives from specific populations during deliberations [82].
Data Safety Monitoring Committees (DSMCs): Development of comprehensive safety monitoring plans with DSMC supervision is crucial [82]. Their role may be optimized by involving them in both early and late trial phases soliciting vulnerable subjects [82].
Responsive Safeguarding Systems: Research teams should appoint a safeguarding lead, codesign bespoke study safeguarding approaches, adopt responsive approaches to mental health safeguarding, maintain transparency about safeguarding approaches, and report implementation outcomes [85]. This is particularly important in adolescent mental health research where prevalence of self-harm and suicidal ideation may be unexpectedly high [85].
Special Considerations in Contemporary Research Environments
Online and Digital Research Methodologies
Online research with vulnerable populations presents unique considerations. Participants can complete interviews or surveys from their own homes or other comfortable locations, potentially reducing barriers to participation [86]. However, researchers must pay particular attention to:
- Building Rapport and Trust: Allow extra time to cultivate rapport and trust in remote settings [86].
- Tool Selection: Select digital communications tools that the participant finds comfortable and respect their choices about communication modalities [86].
- Partnership Models: Partner with agencies or centers that offer services to the target population, potentially involving them in recruitment and technical support [86].
Research Security Framework
The National Institute of Standards and Technology (NIST) has developed a Research Security Framework to help institutions manage risks presented by international research collaborations, including theft, misuse, abuse and exploitation of intellectual property and critical technology [87]. This framework promotes a balanced approach that safeguards international science while mitigating risks to the integrity of the open collaborative environment [87]. The framework identifies five categories of engagement for security review: researchers, international travel requests, international collaborations, international requests for products/services/software tools, and funding opportunities [87].
Assessment Tools and Implementation Framework
Vulnerability Assessment Diagram
Ethical Safeguards Implementation Pathway
Research Reagents and Methodological Tools
Table 3: Essential Methodological Tools for Ethical Research with Vulnerable Populations
| Tool Category | Specific Tools/Methods | Function & Application |
|---|---|---|
| Consent Enhancement Tools | Age-appropriate assent forms; Audiovisual aids; Plain-language documents; Comprehension assessment tools [82] | Enhance understanding of research participation; Verify comprehension; Document consent process |
| Capacity Assessment Instruments | Decisional capacity assessment tools; Cognitive screening instruments; Adaptive communication protocols [84] | Evaluate ability to provide informed consent; Identify need for surrogate decision-makers |
| Safety Monitoring Systems | Data Safety Monitoring Committees (DSMCs); Observational Study Monitoring Boards; Adverse event reporting systems [82] | Independent oversight of participant safety; Ongoing risk-benefit assessment; Protocol modification recommendations |
| Data Protection Mechanisms | Secure data storage systems; Confidentiality protocols; Privacy safeguarding measures [82] | Protect sensitive participant information; Prevent unauthorized data access |
| Participant Support Resources | Mental health referrals; Advocacy services; Independent patient liaisons [85] | Provide support beyond research context; Address ancillary needs |
Safeguarding vulnerable populations in research requires a multifaceted approach that recognizes both categorical and contextual vulnerabilities. The historical development of informed consent and research ethics demonstrates that protection of vulnerable participants is not merely a regulatory requirement but a fundamental ethical obligation. By implementing comprehensive safeguards including enhanced consent processes, population-specific protections, robust institutional oversight, and adaptive monitoring systems, researchers can ensure that the rights and welfare of vulnerable participants are protected while maintaining scientific integrity.
Future directions in safeguarding vulnerable populations should emphasize flexible, responsive approaches that can adapt to emerging research contexts, including digital research environments and global collaborative partnerships. Continued attention to both the theoretical foundations and practical implementation of safeguards will be essential to maintaining public trust and advancing ethical research practices.
Addressing Deception and Incomplete Disclosure with Debriefing Protocols
The concept of informed consent has evolved significantly from its early legal foundations to its current status as a cornerstone of ethical research. The principle of patient autonomy was first legally established in a series of early 20th-century court cases, including the landmark 1914 case Schloendorff v. Society of New York Hospital, which asserted that "every human being of adult years and sound mind has a right to determine what shall be done with his own body" [13] [12]. This principle developed in parallel with research ethics, particularly after the Nuremberg Code (1947) codified voluntary consent as the first requirement for ethical human experimentation [12]. These historical developments established a fundamental ethical tension: while complete transparency is the ideal, some research necessitates methodological techniques that temporarily violate this principle to achieve scientifically valid results [88] [89].
Deception and incomplete disclosure represent a careful balancing act between scientific validity and ethical responsibility. They are never to be undertaken lightly and require robust methodological and ethical justification [90]. When researchers deliberately provide false information (deception) or withhold information about the research purpose (incomplete disclosure), they create an ethical debt that must be repaid through a comprehensive debriefing process [89] [91]. This guide provides researchers, scientists, and drug development professionals with a technical framework for implementing these methodologies while maintaining the highest ethical standards required in modern research environments.
Definitions and Key Concepts
Terminology and Applications
Table 1: Definitions of Deception and Incomplete Disclosure
| Term | Definition | Research Application Examples |
|---|---|---|
| Deception | The intentional communication of misleading or false information to participants through study procedures or purpose [89] [91]. | - Telling participants they performed poorly on a task regardless of actual performance [92] [88].- Using confederates who act as research subjects without revealing their true role [88] [91].- Informing anxiety study participants to expect moderate pain when no painful procedures will occur [92]. |
| Incomplete Disclosure | Deliberately withholding or concealing information about the true purpose or nature of the research [89] [90]. | - Not revealing that a study on concentration examines how background noise affects focus [92] [90].- Withholding that a study's true purpose is to measure emotional responses to specific words during a reading task [88].- Informing participants about general study goals while concealing specific research hypotheses [91]. |
It is crucial to distinguish these practices from disclosed concealment, where participants consent in advance to having certain information withheld (e.g., in double-blind, placebo-controlled trials where participants know their treatment assignment will be concealed) [91]. Disclosed concealment does not constitute deception or incomplete disclosure because transparency about the concealment is maintained upfront.
Regulatory and Ethical Framework
Justification Criteria and IRB Review
The use of deception or incomplete disclosure must meet specific regulatory criteria to receive Institutional Review Board (IRB) approval. These methodologies are generally permissible only when the research involves no more than minimal risk to participants [88] [89] [90]. The investigator must provide scientific justification demonstrating that the research could not practicably be carried out without the waiver or alteration of informed consent [88] [89]. The potential benefits of the research must sufficiently outweigh any risks that deception or incomplete disclosure may create, and there must be no undisclosed risks to participants [88] [91].
Table 2: IRB Review Levels and Permissibility
| Review Level | Permissibility of Deception/Incomplete Disclosure |
|---|---|
| Exempt Research | Protocols with incomplete disclosure are eligible for exemption if otherwise qualifying [88] [91].Protocols with deception are only exempt if participants authorize it through prospective agreement in the consent process [92] [89] [91]. |
| Expedited Review | Approved for minimal-risk studies where deception is not disclosed in consent [92]. Suitable when deception/omission is minor and does not involve highly sensitive topics or vulnerable participants [90]. |
| Full Board Review | Required for studies where deception involves sensitive topics or potentially vulnerable participants [90]. The IRB cannot approve research where deception poses more than minimal risk or would likely affect participants' willingness to participate [92] [89]. |
The regulatory framework for informed consent continues to evolve. Recent guidance from the FDA harmonizes with the Office for Human Research Protections (OHRP) requirements, emphasizing the inclusion of a "key information" section at the beginning of consent forms to facilitate participant understanding [6]. This concise presentation of crucial study elements represents the ongoing effort to balance comprehensive information with participant comprehension in complex research environments.
Approval Workflow and Decision Process
The following diagram illustrates the IRB review and approval workflow for research involving deception or incomplete disclosure:
Debriefing Protocol Methodology
Core Components and Implementation
Debriefing serves as the critical corrective mechanism that repairs the breach of informed consent created by deception or incomplete disclosure [89] [90]. An effective debriefing process must include several core components:
Explanation of True Purpose: Provide a clear, non-technical explanation of the study's true goals, hypotheses, and the specific reasons why deception or incomplete disclosure was methodologically necessary [88] [89]. This should include what the researchers expect to learn from the study [88].
Revelation of Deception: Explicitly identify what information was false or incomplete, detailing the precise nature of the deception employed [88] [89]. The explanation should be delivered with unconditional positive regard for the range of emotions participants may experience [88].
Scientific Justification: Explain why the research question required these methodological approaches, emphasizing that awareness of the true purpose would have biased responses or behaviors and compromised scientific validity [89] [91].
Withdrawal Option: Provide participants with the option to withdraw their data from the study after learning the true nature of the research, particularly if the deception could have materially influenced their decision to participate [92] [89]. The IRB may require this option in cases where deception involves sensitive topics or potential invasion of privacy [89] [90].
Debriefing Timing and Delivery Modalities
The timing of debriefing is methodologically significant and should be determined by research design considerations:
Immediate Debriefing: Conducted directly after participants complete study procedures in most cases [89]. This approach promptly addresses potential confusion or discomfort and reinforces ethical transparency [88].
Delayed Debriefing: Implemented when immediate disclosure could compromise study results by enabling participants to share information with others yet to participate [92] [89]. Strategies for delayed debriefing include providing a URL where participants can access debriefing information after study completion [92], having participants self-address envelopes for mailing debriefing materials later [92], or sending debriefing information via email when the study concludes [89].
Staged Debriefing: Used in rare cases where participants might experience strong emotional reactions at different intervals, particularly in greater-than-minimal-risk studies [89]. This approach provides ongoing support and information as participants process their research experience.
Delivery modalities should align with study methods and risks, ranging from in-person conversations for studies involving significant deception to email or website resources for minimal-risk online surveys [89].
Debriefing Workflow and Participant Options
The following diagram illustrates the complete debriefing process and participant options following deception or incomplete disclosure research:
Essential Research Reagents and Tools
Table 3: Research Reagent Solutions for Deception Methodology
| Reagent/Tool | Function in Research Implementation |
|---|---|
| Authorized Deception Language Templates | Pre-approved consent form language that informs participants of incomplete disclosure without revealing specific deceptive elements, enabling prospective agreement to methodological approach [89] [91]. |
| Standardized Debriefing Scripts | Structured debriefing protocols ensuring consistent revelation of deception across all participants, including hypothesis explanation, methodological justification, and emotional support components [88] [89]. |
| Debriefing Information Delivery Systems | Technical mechanisms for delayed debriefing implementation, including dedicated study URLs, encrypted email systems, and physical mailing protocols for debriefing documentation [92] [89]. |
| Data Withdrawal Protocols | Systematic procedures for identifying and removing participant data upon withdrawal request, maintaining necessary identifier links while respecting participant autonomy post-debriefing [89]. |
| Health Literacy Assessment Tools | Screening instruments to evaluate participant comprehension during debriefing, including teach-back methods and simplified risk communication frameworks to verify understanding [13]. |
Deception and incomplete disclosure represent methodologically necessary but ethically complex approaches in specific research contexts. Their justification rests entirely on the foundation of a comprehensive debriefing process that restores participant autonomy and repairs the informed consent process. As regulatory frameworks evolve to include elements like the key information section in consent forms [6], the research community must maintain its commitment to ethical rigor while pursuing scientifically valid outcomes. The protocols outlined in this technical guide provide a framework for balancing these sometimes competing demands, ensuring that respect for research participants remains paramount even when methodological requirements necessitate temporary departures from full transparency.
Informed consent serves as a critical ethical and legal foundation in both clinical practice and human subjects research. The concept has evolved significantly from its origins in early 20th-century legal cases that established patient autonomy to the complex regulatory frameworks governing research today [14]. The digital transformation of healthcare has introduced powerful new tools—artificial intelligence (AI), chatbots, and interactive platforms—that are fundamentally reshaping how consent is obtained, documented, and understood. This transformation addresses long-standing challenges with traditional paper-based consent, including documentation errors, inadequate risk disclosure, and variability in comprehension [93].
The integration of digital technologies occurs alongside growing regulatory acceptance. The U.S. Food and Drug Administration (FDA) has issued guidance supporting electronic informed consent (eConsent), provided key safeguards for identity verification, secure storage, and audit trails are implemented [94] [95]. Similarly, the European Medicines Agency (EMA) recognizes qualified electronic signatures (QeS) as having the same legal standing as handwritten signatures under eIDAS regulation [95]. This technical guide examines the current landscape, evidence base, and implementation considerations for digital consent technologies, providing researchers and drug development professionals with a comprehensive framework for evaluating and deploying these solutions.
Historical Context and The Evolution of Consent Requirements
The intellectual scaffolding supporting informed consent has undergone significant transformation throughout medical history. The foundational principle was established through a series of legal decisions in the early 20th century, including Mohr v Williams (1905), Pratt v Davis (1905), Rolater v Strain (1912), and Schloendorff v Society of New York Hospital (1914), which established the right of patients to determine what happens to their own bodies [14]. The term "informed consent" first appeared officially in the 1957 case Salgo v Leland Stanford Jr University Board of Trustees, which emphasized the physician's duty to disclose potential risks and hazards of procedures [14].
The regulatory framework for research consent emerged largely in response to ethical violations. The Nuremberg Code (1947) established the first explicit rules for human experimentation, emphasizing voluntary consent as its first principle [14]. In the United States, the Public Health Service Tuskegee Syphilis Study revelations and Henry Beecher's 1966 landmark article "Ethics and Clinical Research," which detailed 22 examples of unethical studies in leading medical journals, catalyzed public outrage and regulatory action [83]. This ultimately led to the National Research Act of 1974, the Belmont Report in 1979, and the eventual codification of the Common Rule in 1981 [14] [83].
Modern consent standards continue to evolve, with recent updates to the Common Rule introducing the key information section requirement—a concise, focused presentation at the beginning of consent documents aimed at facilitating participant comprehension [14]. This evolution toward participant-centricity provides the foundation for digital consent innovations that seek to make informed consent more accessible, comprehensible, and meaningful.
Digital Consent Platforms: Evidence and Outcomes
Documented Benefits Over Paper-Based Consent
Robust evidence from multiple studies demonstrates that digital consent offers substantive improvements over traditional paper-based methods across multiple domains, including documentation quality, patient experience, and economic efficiency [93].
Table 1: Documentation Quality Improvements with Digital Consent
| Metric | Paper-Based Consent | Digital Consent | Study References |
|---|---|---|---|
| Forms with ≥1 Error | 51.1% - 72% | 0% - 7.5% | St John et al. (2017); Dyke et al. (2023) [93] |
| Forms Missing Core Risks | 90.2% | 13.6% | St John et al. (2021) [93] |
| Mortality Risk Documentation | 28% (emergency laparotomy) | Significant improvement | Loughran (2015) [93] |
| Odds Ratio for Errors | Reference | 0.05 (95% CI: 0.03-0.08) | Wong et al. (2024) [93] |
Table 2: Patient Experience and Economic Outcomes
| Domain | Paper-Based Consent | Digital Consent | Study References |
|---|---|---|---|
| Shared Decision-Making | 28% (gold-standard) | 72% (gold-standard) | St John et al. (2022) [93] |
| Patient Understanding | Baseline | Significantly improved | Dyke et al. (2023) [93] |
| Direct Process Cost | Reference | £0.90 less per episode | Houten et al. (2025) [93] |
| Litigation Claims | 248 annual claims (NHS) | Potential for significant reduction | Ainsworth et al. (2023) [93] |
The benefits of digital consent extend across multiple surgical specialties, demonstrating broad applicability beyond any specific clinical context [93]. Research has also explored how digital solutions can be adapted across diverse healthcare systems with different legal frameworks, from the UK's "material risk" Montgomery standard to more paternalistic approaches in some regions [93].
Implementation in Decentralized Clinical Trials (DCTs)
Digital consent platforms have become fundamental components of decentralized clinical trials (DCTs), which leverage digital technologies to bring trial activities closer to participants [94]. The FDA's 2024 guidance "Conducting Clinical Trials With Decentralized Elements" recognizes that most trials exist on a spectrum, incorporating both traditional site-based and remote activities [94].
Modern eConsent platforms integrated with Electronic Data Capture (EDC) systems must provide multiple critical capabilities:
- Identity verification through multiple methods
- Comprehension assessment tools
- Real-time video capability for consent discussions
- Multi-language support with certified translations
- Comprehensive audit trails for every interaction [94]
Integrated full-stack platforms that combine EDC, eConsent, electronic Clinical Outcome Assessment (eCOA), and clinical services in a single system significantly reduce the complexity of managing multiple point solutions [94]. This integration eliminates data silos, simplifies validation processes, and creates more efficient workflows for both sites and patients.
Artificial Intelligence and Chatbots in Consent Processes
AI-Generated Consent Forms: Performance and Limitations
Recent research has evaluated the capability of AI chatbots to generate procedure-specific informed consent forms. A 2025 cross-sectional observational study tested ChatGPT 4o and Deepseek on ten common ophthalmological procedures, including cataract surgery, retinal detachment repair, and trabeculectomy [96]. The AI-generated consents were evaluated on correctness, completeness, language readability, and real-world applicability against standard templates from the All India Ophthalmological Society (AIOS).
Table 3: AI Chatbot Performance in Generating Ophthalmology Consent Forms
| Evaluation Metric | ChatGPT 4o | Deepseek | Study Findings |
|---|---|---|---|
| Readability | Lower average scores | Higher on Flesch Kincaid and Gunning Fog Index | Deepseek produced more elaborate, readable consents [96] |
| Completeness | Variable across procedures | Variable across procedures | 40% of consents from both chatbots were not fit for real-world use in Indian scenarios [96] |
| Correctness | Mostly correct (8/10) | Mostly correct (8/10) | Both chatbots performed similarly on correctness [96] |
| Real-World Applicability | 60% applicable | 60% applicable | Significant limitations in contextual adaptation [96] |
The study concluded that while AI chatbots can generate consent forms quickly, they currently have significant limitations in adapting to specific regional and institutional requirements [96]. This highlights the continued need for human oversight and customization when using AI-generated consent materials.
Ethical Gaps in Digital Health Consent Frameworks
The rapid adoption of digital health technologies (DHTs), including mobile applications, wearable devices, and sensors, has introduced unique ethical challenges that current informed consent practices often fail to address adequately [97]. A 2025 study developing a comprehensive ethical consent framework for digital health research found that none of the 25 informed consent forms reviewed fully adhered to all required or recommended ethical elements, especially those related to technology-specific risks [97].
The highest completeness for required attributes reached only 73.5%, revealing significant gaps in participant protection [97]. The study identified four ethically salient consent elements not present in current national guidance:
- Commercial profit sharing
- Study information disclosure
- During-study result sharing
- Data removal requests [97]
These findings highlight the need for more comprehensive, equity-oriented consent practices that address the unique ethical considerations raised by digital health technologies, particularly regarding data privacy, third-party access, and technological limitations [97].
Mental Health Chatbots: Systematic Ethical Violations
Recent research on AI chatbots in mental health contexts reveals concerning patterns of ethical violations. A Brown University study found that AI chatbots routinely violate core mental health ethics standards established by organizations like the American Psychological Association, even when prompted to use evidence-based psychotherapy techniques [98].
The study identified 15 ethical risks falling into five general categories:
- Lack of contextual adaptation: Ignoring peoples' lived experiences and recommending one-size-fits-all interventions
- Poor therapeutic collaboration: Dominating conversations and occasionally reinforcing users' false beliefs
- Deceptive empathy: Using phrases like "I see you" to create a false connection
- Unfair discrimination: Exhibiting gender, cultural, or religious bias
- Lack of safety and crisis management: Failing to refer users to appropriate resources or responding indifferently to suicide ideation [98]
These violations are particularly concerning given the lack of established regulatory frameworks and accountability mechanisms for AI systems, unlike human therapists who are governed by professional boards and liability structures [98].
Technical Implementation and Regulatory Compliance
Experimental Protocols for Digital Consent Evaluation
Research on digital consent implementation has employed rigorous methodologies to evaluate effectiveness across multiple dimensions. The following experimental protocols represent approaches used in recent studies:
Protocol 1: Evaluation of AI-Generated Consent Forms
- Research Design: Cross-sectional observational study with blinded evaluation
- Intervention: Generation of informed consent forms for 10 ophthalmological procedures using two AI chatbots (ChatGPT 4o and Deepseek)
- Standardization: Clinical scenarios were standardized with age and diagnosis specified
- Evaluation Metrics: Correctness, completeness, language readability, additional relevant information, irrelevant information, real-world applicability
- Assessment Method: Masked evaluation by three senior ophthalmology residents using standardized AIOS consent templates as reference
- Analysis: Chi-square tests for categorical data, Mann-Whitney U test for numerical data, inter-rater agreement assessment using Fliess' Kappa [96]
Protocol 2: Development of Ethical Framework for Digital Health Consent
- Research Design: Qualitative analysis and framework development
- Methodology: Six-step thematic analysis of NIH guidance on digital health technology consent
- Process: Data familiarization, code generation, attribute and subattribute formation, attribute reviews, significance assessment, findings reporting
- Validation: Iterative testing and refinement through review of 25 real-world informed consent forms from ClinicalTrials.gov
- Inclusion Criteria: U.S. studies, active/recruiting/completing status, start date January 2019 or later, publicly available consent forms [97]
The Researcher's Toolkit: Digital Consent Components
Table 4: Essential Components for Digital Consent Implementation
| Component | Function | Implementation Considerations |
|---|---|---|
| Identity Verification | Ensures participant identity is confirmed | Multiple methods required; integrates with qualified trust service providers (QTSPs) for QeS [94] [95] |
| Comprehension Assessment | Evaluates participant understanding of key concepts | Built-in tools with configurable passing thresholds; supports repeated testing [94] |
| Multimedia Content | Enhances understanding through visual and audio aids | Videos, visual aids, glossary features; accommodates diverse learning styles [95] |
| Audit Trail System | Records all participant interactions with consent materials | Comprehensive logging; timestamped and attributable; inspection-ready [94] [95] |
| Remote Re-consenting | Manages consent process updates for protocol amendments | Electronic notification system; tracks version control; ensures current information [95] |
| Multi-language Support | Provides consent materials in participant's preferred language | Certified translations required; maintains conceptual equivalence [94] |
| Diclofenac Diethylamine | Diclofenac Diethylamine, CAS:78213-16-8, MF:C18H22Cl2N2O2, MW:369.3 g/mol | Chemical Reagent |
Regulatory Compliance and Legal Considerations
The regulatory landscape for digital consent is evolving rapidly, particularly concerning AI technologies. Recent state-level legislation in the U.S. has created a complex patchwork of compliance requirements:
- California (effective January 2026): Requires disclosure for AI "companion chatbots" and includes a private right of action with statutory damages of $1,000 per violation [99]
- New York (effective November 2025): Mandates safeguards for AI companions, including safety measures to detect suicidal ideation and disclosures that users are not communicating with a human [99]
- Maine (effective September 2025): Requires businesses using AI chatbots to notify consumers when they are not interacting with a live human [99]
- Utah (effective May 2025): Establishes specific rules for AI mental health chatbots, including advertising restrictions and prohibitions on selling health information without consent [99]
The Federal Trade Commission (FTC) has also increased scrutiny, announcing a marketplace study in September 2025 into seven companies operating consumer-facing generative AI "companion" chatbots to understand their potential impact on children's mental health [99].
Visualizing the Digital Consent Workflow
The following diagram illustrates the ideal data flow in a modern hybrid clinical trial utilizing an integrated digital consent platform, demonstrating how technology components interact to create an efficient, compliant process:
Digital Consent Workflow in Hybrid Trials
This workflow demonstrates the integration points between consent platforms and clinical data systems, highlighting how automated processes reduce administrative burden while maintaining regulatory compliance through comprehensive audit trails.
The digital transformation of informed consent represents a significant advancement in patient-centered care and research ethics. Evidence demonstrates that digital consent platforms can simultaneously improve documentation quality, enhance patient understanding, reduce litigation risk, and generate cost savings [93]. AI technologies show promise for streamlining consent form creation but currently face limitations in contextual adaptation and regional applicability [96].
The future of digital consent will likely involve more sophisticated AI systems capable of better personalization and adaptation, coupled with increasingly specific regulatory frameworks addressing the unique ethical challenges posed by these technologies [97] [99]. Researchers and drug development professionals should prioritize solutions that offer robust integration capabilities, comprehensive audit functionality, and flexibility to adapt to evolving regulatory requirements across multiple jurisdictions.
As digital consent technologies continue to evolve, they offer the potential to transform informed consent from an administrative requirement into a meaningful process that truly respects participant autonomy and enhances the ethical conduct of research. Future development should focus on addressing identified ethical gaps, particularly regarding technology-specific risks, data governance, and equitable access across diverse populations.
Optimizing the Process to Reduce Investigator Time and Enhance Participant Understanding
The doctrine of informed consent constitutes a cornerstone of ethical clinical research, representing a crucial balance between the imperative of scientific progress and the inviolable principle of respect for person autonomy. Its intellectual and legal scaffolding has evolved significantly from its early 20th-century origins in cases like Schloendorff v. Society of New York Hospital (1914), which established that "every human being of adult years and sound mind has a right to determine what shall be done with his own body" [12]. This concept was further solidified in the 1957 Salgo case, which first coined the term "informed consent" and emphasized the physician's duty to disclose potential risks [12]. The aftermath of World War II and the subsequent Nuremberg Code cemented voluntary consent as the first principle of ethical human subjects research, highlighting that consent requires "sufficient knowledge and comprehension" to enable an "understanding and enlightened decision" [12].
In contemporary practice, informed consent has transcended its legalistic origins to become a dynamic communication process between researcher and participant. The 2017 revisions to the Common Rule introduced the "key information" section to facilitate participant comprehension through a concise, focused presentation at the beginning of consent documents [12]. Despite these advancements, the process faces dual challenges: participants often struggle with comprehension of complex trial information, while investigators face significant time burdens in obtaining meaningful consent. This technical guide examines evidence-based strategies to optimize informed consent, simultaneously enhancing participant understanding while creating efficiencies in investigator time—a critical imperative for the sustainable advancement of clinical research.
Current Challenges in the Informed Consent Process
Barriers to Participant Understanding and Engagement
The functional efficacy of informed consent is often compromised by multiple barriers that impede genuine participant understanding:
Comprehension Deficits: Complex medical jargon and varying health literacy levels frequently result in participants agreeing to procedures without fully understanding risks, benefits, or alternatives [13]. A study of Chinese teaching hospitals revealed inadequate personal functional health literacy among hospitalized patients, which compromised the informed consent process [13].
Therapeutic Misconception: Many participants fail to grasp the fundamental distinction between clinical care and research, particularly misunderstanding randomization procedures [100]. This misconception represents a critical failure in the communication of core trial concepts.
Cultural and Linguistic Barriers: In diverse populations, language barriers and inadequate use of professional interpreters further complicate consent comprehension [13]. Cultural factors also significantly impact decision-making processes; in some cultures, decisions are made collectively rather than individually, and written consent may be perceived as a sign of mistrust [13].
Accessibility Challenges: Individuals with sensory impairments (vision and/or hearing difficulties) regularly encounter barriers with inaccessible information and communications, including complex language, lack of alternative formats (braille, large print, audio), and insufficient access to sign language interpreters [101].
Investigator Burden and Process Inefficiencies
Parallel to participant challenges, investigators face substantial operational burdens in the consent process:
Documentation Complexity: Informed consent documents frequently exceed 20 pages, creating substantial administrative overhead [12]. Research indicates that required elements of informed consent—nature of the procedure, risks, benefits, and alternatives—were documented on consent forms only 26.4% of the time, suggesting inefficiencies in process implementation [13].
Time Pressures: Clinical settings often necessitate rushed consent processes where healthcare professionals cannot dedicate adequate time to thorough discussions [13]. Lenze (2021) highlights problematic practices such as obtaining consent shortly before procedures, in preoperative holding areas, or when patients are medicated [13].
Inadequate Training: There is frequently a lack of staff awareness, education, and training around accessibility strategies and communication techniques suitable for diverse populations [101].
Table 1: Global Willingness to Share Health Data for Secondary Purposes
| Category | Pooled Proportion Willing to Share | Key Factors Influencing Willingness |
|---|---|---|
| Overall | 77.2% (95% CI: 71-82%) [102] | Privacy protections, consent processes, transparency |
| By Organization Type | ||
| Research Organizations | 80.2% (95% CI: 74-85%) [102] | Trust in academic institutions |
| Government Agencies | Lower than research organizations [102] | Concerns about data usage |
| For-Profit Organizations | 25.4% (95% CI: 19-33%) [102] | Distrust of commercial motives |
| By Participant Type | ||
| Patients with Cancer | 90.9% (95% CI: 73-97%) [102] | Direct potential benefit perception |
| General Public | 69.7% (95% CI: 62-77%) [102] | Less immediate connection to research benefits |
Evidence-Based Optimization Strategies
Process Enhancements for Improved Comprehension
Several structured interventions have demonstrated efficacy in enhancing participant understanding while creating process efficiencies:
Extended Discussion Protocols: Defined as two-way oral communication between information-provider and participant incorporated into the initial informed consent meeting, extended discussion facilitates value-based decision making [100]. This approach allows participants to openly discuss the trial with the research team, express feelings and beliefs, and have doubts addressed early in the recruitment process [100]. The methodology typically involves:
- Scheduled sessions separate from clinical encounters
- Use of open-ended questions to assess understanding
- Teach-back techniques where participants restate concepts in their own words
- Potentially multiple sessions for complex trials
- Conduct by team members specifically trained in consent communication
Structured Key Information Sections: As mandated by the revised Common Rule, a concise, focused presentation at the beginning of the informed consent document significantly enhances comprehension [12]. Effective implementation includes:
- Limiting to the most critical information for decision-making
- Using plain language at an appropriate literacy level
- Highlighting the research purpose and key differences from standard care
- Emphasizing voluntary participation and right to withdraw
Public Deliberation Methods: This novel engagement approach involves in-depth education, presentation of conflicting perspectives from experts, facilitated discussion, and development of resolutions acceptable to communities [103]. Implementation framework includes:
- Structured education on the research topic
- Presentation of diverse stakeholder perspectives
- Facilitated small-group discussions
- Collective resolution development
- Creation of model briefing reports for dissemination
Accessibility and Inclusion Frameworks
Ensuring accessibility for participants with sensory impairments is both an ethical imperative and a practical opportunity to enhance efficiency:
Multimodal Information Delivery: Evidence supports providing information in multiple accessible formats based on individual needs, including braille, large print, audio, and electronic formats [101]. The International Council for Harmonisation updated Guideline for Good Clinical Practice (2025) recommends varied approaches to information provision, including text, images, videos, and other interactive methods [101].
Professional Interpreter Engagement: Utilizing qualified sign language and tactile interpreters for hearing-impaired participants ensures accurate communication [13]. This requires:
- Advance planning for interpreter availability
- Training interpreters on trial-specific terminology
- Budget allocation for interpreter services
Universal Design Principles: Implementing accessibility standards as routine practice benefits all participants by improving general comprehension and reducing the need for individual accommodations [101].
Table 2: Accessibility Tools for Inclusive Consent Processes
| Tool Category | Specific Applications | Target Population | Implementation Considerations |
|---|---|---|---|
| Sensory Adaptation Tools | Braille documents, large print formats (18pt), audio recordings | Vision impairment, blindness | Document structure compatibility, timely production |
| Interpretation Services | Qualified sign language interpreters, tactile interpreters | d/Deaf, hard of hearing, Deafblind | Specialist training on trial terminology, scheduling lead time |
| Digital Accessibility Solutions | Screen reader-compatible PDFs, responsive web design, adjustable text sizes | Diverse accessibility needs | Compliance with WCAG 2.1 guidelines, platform testing |
| Communication Facilitators | Augmentative and alternative communication (AAC) devices, picture boards | Speech and communication disabilities | Individual assessment, custom programming |
Diagram 1: Optimization Framework for Informed Consent Processes
Implementation Protocols and Methodologies
Extended Discussion Experimental Protocol
The extended discussion intervention represents a structured approach to enhancing consent comprehension. Implementation requires careful planning and execution:
Session Structure: Conduct one or more dedicated sessions (30-60 minutes) separate from clinical care encounters. Begin with an assessment of the participant's baseline understanding, followed by a structured yet flexible discussion covering trial purpose, procedures, risks/benefits, alternatives, and rights [100].
Communication Techniques: Utilize open-ended questioning, teach-back methods, and value clarification exercises. The conversation should be participant-led, addressing specific concerns and misconceptions as they arise [100].
Facilitator Qualifications: Trained consent educators, research coordinators, or principal investigators with specific communication training should conduct sessions. Competencies include active listening, health literacy adaptation, and cultural humility [100].
Documentation: Record participant questions, concerns, and demonstrated understanding in research records. Note any specific areas of difficulty or misunderstanding for follow-up.
Public Deliberation Methodology
Public deliberation offers a novel approach to engaging communities in consent process design, particularly for complex ethical challenges:
Recruitment and Representation: Deliberately recruit diverse participants representing various stakeholder groups (patients, caregivers, community members, healthcare professionals). Aim for 15-25 participants per deliberation session to ensure diverse perspectives while maintaining functional discussion groups [103].
Structured Deliberation Process: Implement a multi-phase approach including:
- Education Phase: Provide balanced background materials and expert presentations on the consent challenge
- Discussion Phase: Facilitate small-group discussions with trained moderators using structured question guides
- Resolution Development: Guide participants in developing specific recommendations for consent process improvements
Data Collection and Analysis: Employ mixed methods including pre/post surveys, audio recording of discussions, and qualitative analysis of developed resolutions. Use directed content analysis for narrative data and descriptive statistics for quantitative measures [103].
Notification Processes for Consent Waivers
For minimal-risk research conducted under waiver of consent, notification processes promote ethical values while potentially reducing investigator burden:
Notification Modalities: Implement tailored approaches including letters, email campaigns, posters in common areas, conversations with clinicians, and presentations at staff meetings [37]. The amount of information provided can range from a general statement that research is being conducted to detailed study information.
Implementation Framework: Determine appropriate notification strategies on a case-by-case basis considering costs, benefits, and feasibility [37]. Effective notification promotes:
- Respect for persons through transparency
- Participant understanding of research contributions
- Opportunity for questions and concerns
- Enhanced trust in research institutions
Diagram 2: Implementation Workflow for Consent Process Optimization
The optimization of informed consent processes represents a critical convergence of ethical imperative and operational efficiency in clinical research. By implementing evidence-based strategies such as extended discussion protocols, structured key information sections, accessibility frameworks, and innovative engagement methods like public deliberation, researchers can simultaneously enhance participant understanding and reduce investigator time investment. The historical evolution of informed consent—from its legal origins in patient autonomy to its current manifestation as a dynamic communication process—demonstrates an ongoing refinement of the balance between research necessities and participant rights. As clinical trials grow increasingly complex, continued innovation in consent processes will be essential to maintaining public trust, ensuring research validity, and advancing the ethical conduct of science. The methodologies and frameworks presented in this technical guide provide actionable approaches for researchers seeking to optimize this fundamental component of clinical research.
Ensuring Consent Integrity: Validation Methods, Regulatory Comparisons, and Future Trends
The doctrine of informed consent forms a cornerstone of both clinical ethics and human subjects research, with its history deeply rooted in the principle of patient autonomy established by early 20th-century legal cases [13] [12]. The 1914 case of Schloendorff v. Society of New York Hospital powerfully asserted that "every human being of adult years and sound mind has a right to determine what shall be done with his own body" [13]. This ethical foundation was further solidified after World War II by the Nuremberg Code, which made voluntary consent a central requirement for human experimentation [12]. Subsequently, these principles were codified into U.S. regulations, notably the Common Rule [12].
However, the mere provision of information does not ensure understanding. Empirical research has consistently demonstrated that the informed consent process often fails to deliver information in a format comprehensible to individuals with varying levels of health literacy [13] [12]. Lengthy, complex consent documents can hinder, rather than facilitate, genuine understanding [12]. This gap between disclosure and comprehension creates an urgent need for robust, reliable methods to assess and ensure patient or subject understanding. This guide focuses on the Teach-Back method and related assessment tools, providing researchers and clinicians with evidence-based protocols to validate comprehension, thereby fulfilling the ethical promise of informed consent.
The Teach-Back Method: Foundation and Efficacy
Core Principles and Definition
The Teach-Back method is an evidence-based health literacy intervention that moves beyond simply asking patients "Do you understand?" [104]. Instead, it is a structured communication process where a healthcare professional or researcher asks a patient (or research subject) to explain, in their own words, the information they have just received regarding their diagnosis, treatment plan, or a research protocol [104]. This method serves a dual purpose: it confirms that the provider has explained the information clearly, and it verifies that the patient has a accurate understanding of what was communicated [104]. By requiring the recipient to "teach back" the information, the method solidifies their knowledge and actively engages them in the learning process.
Quantitative Evidence of Effectiveness
The efficacy of the Teach-Back method is supported by a growing body of research. Studies have demonstrated its positive impact on patient and system-level outcomes, including improved patient health literacy and reduced hospital readmissions [105]. The table below summarizes key quantitative findings from the literature.
Table 1: Quantitative Evidence for Teach-Back Method Efficacy
| Study Context/Intervention | Key Findings | Significance |
|---|---|---|
| Multimodal Training for Nurses [105] | >40% increase in self-reported use of Teach-Back among nurses post-training. | Demonstrates that training can significantly change provider behavior and increase the application of the method. |
| Nurse Training in a Cardiac Unit [105] | 96% of nurses reported continued use of Teach-Back after receiving demonstration and guided practice. | Highlights the importance of practical, hands-on training for achieving high rates of sustained adoption. |
| Training for Community Health Workers (CHWs) [105] | CHWs reported increased confidence and conviction in using Teach-Back after repeated, structured exposure to the method. | Indicates that Teach-Back is a learnable skill for diverse members of the healthcare team and that repeated practice builds proficiency. |
Experimental Protocols and Implementation Methodologies
A Standardized Teach-Back Protocol
Implementing Teach-Back effectively requires a structured approach. The following workflow provides a detailed, step-by-step methodology for integrating Teach-Back into a patient or research subject interaction.
Detailed Protocol Steps
- Explain the Information: Begin by providing clear, concise information. Use plain language, avoid medical jargon, and break down complex topics into smaller segments. The information can cover a new diagnosis, medication instructions, a treatment plan, or details of a research study [104].
- Request a Teach-Back: Ask the patient or subject to explain the information back to you in their own words. Use open-ended, non-shaming questions such as, "I want to make sure I explained everything clearly. Can you please tell me back, in your own words, what you understand we will be doing?" [104].
- Assess the Response: Listen carefully to the response. Identify any gaps, inaccuracies, or misconceptions. This is the critical assessment phase where comprehension is measured directly.
- Clarify and Re-teach: If the understanding is incomplete or incorrect, gently correct the misinformation. Use alternative explanations, visuals, or models to clarify the points that were misunderstood. Avoid simply repeating the original explanation verbatim [104].
- Repeat Teach-Back: After re-teaching, ask the individual to explain the corrected information again. This iterative process continues until their understanding is complete and accurate.
- Proceed: Once understanding is confirmed, you can proceed with the next steps of care or the formal consent process. Document the use of Teach-Back and the subject's demonstrated understanding in their record or study file.
Specialized Implementation: A Community Health Worker Training Protocol
A 2022 pilot study detailed the development and evaluation of a specialized Teach-Back training for Community Health Workers (CHWs), whose role in addressing social needs and care coordination is crucial for reducing hospital readmissions [105]. The training protocol was designed to be relevant to the CHW scope of work.
Table 2: Key Elements of a Teach-Back Training Curriculum for CHWs
| Training Element | Description | Function |
|---|---|---|
| Didactic Instruction | Provision of foundational knowledge about Teach-Back principles and evidence base. | Establishes the "why" behind the method, linking it to improved patient outcomes and the CHW's professional role. |
| Skill-Building Practice | Guided practice sessions involving role-playing realistic patient interactions. | Allows CHWs to develop muscle memory and confidence in using the technique in a low-stakes environment. |
| Repeated Exposure | A 3-week pilot structure with ongoing practice and reinforcement of concepts. | Prevents skill decay and helps integrate Teach-Back into the CHW's standard clinical workflow. |
| Tailored Content | Curriculum and scenarios designed specifically for CHW tasks in care coordination and follow-up. | Ensures the training is practical and immediately applicable, increasing relevance and adoption. |
The study found that this tailored, practical approach led to high satisfaction among CHWs and a reported increase in their confidence and conviction to use Teach-Back in their daily work [105].
The Researcher's Toolkit: Materials and Assessment Instruments
Beyond the core Teach-Back protocol, several key tools and concepts are essential for rigorously assessing and ensuring comprehension in research and clinical settings.
Table 3: Essential Tools for Assessing and Ensuring Comprehension
| Tool or Concept | Brief Description | Primary Function in Comprehension Assessment |
|---|---|---|
| The "Teach-Back" Method | A communication technique wherein the listener is asked to state in their own words what they just heard. | To directly measure and verify patient/subject understanding of information that was communicated [104]. |
| Health Literacy Screening | Brief tools (e.g., Newest Vital Sign) used to identify patients with limited health literacy. | To flag individuals who may require additional communication support and more intensive use of comprehension checks like Teach-Back [13]. |
| Medical Interpreter Services | Professional interpreters, including American Sign Language (ASL) interpreters, for patients with limited English proficiency. | To ensure accurate, clear communication across language barriers, which is a prerequisite for any valid assessment of comprehension [13]. |
| Graphical and Interactive Media | Visual aids, charts, and interactive digital tools to present risks, benefits, and procedures. | To enhance shared decision-making and present complex statistical information (like risks) in a more understandable format [13]. |
| Key Information Section | A concise, focused presentation at the beginning of an informed consent document, as required by the revised Common Rule. | To facilitate potential participants' initial comprehension of the most critical elements of a research study before reviewing the full, lengthy consent document [12]. |
Advanced Applications and Visual Mapping of Workflow Integration
For research and clinical teams, integrating comprehension checks like the Teach-Back method is not a solitary activity but part of a larger, interdisciplinary workflow. The following diagram maps this process, highlighting key decision points and team interactions.
This end-to-end workflow ensures that assessing comprehension is a shared responsibility, reinforced by multiple team members, and supported by resources that address potential barriers to understanding, such as social needs or health literacy.
Auditing and Monitoring the Consent Process for Compliance
The informed consent process is a cornerstone of ethical clinical research, serving as a vital safeguard for participant autonomy, safety, and rights. For researchers, scientists, and drug development professionals, a robust system to audit and monitor this process is not merely a regulatory formality but a fundamental component of research quality and integrity. Rooted in a history shaped by pivotal legal cases and ethical codes, the modern consent process demands rigorous oversight to ensure it fulfills its ethical and legal promises. This guide provides a technical framework for auditing and monitoring consent processes to ensure compliance with evolving regulatory standards.
Historical and Regulatory Foundations of Informed Consent
The contemporary informed consent process is built upon a foundation of ethical principles and legal precedents. Its modern concept was largely undefined until the term was first recorded in the 1957 case Salgo v Leland Stanford Jr University Board of Trustees [12]. This ruling established a physician's duty to disclose potential risks and benefits, moving beyond simple consent to the notion of informed consent [12].
The imperative for voluntary consent was cemented internationally with the 1947 Nuremberg Code, created in response to the unethical human experiments of World War II [12]. The Code's first principle states that the voluntary consent of the human subject is absolutely essential, requiring that the person involved has "sufficient knowledge and comprehension of the elements of the subject matter involved as to make an understanding and enlightened decision" [12].
In the United States, these principles were codified into federal regulations known as the Common Rule (45 CFR 46) and FDA policies (21 CFR 50) [12]. The 2017 revisions to the Common Rule introduced requirements for a key information section to facilitate participant comprehension, though a lack of specific guidance on its format remains a challenge for consistent implementation [12].
A Framework for Consent Process Audits
Auditing the informed consent process is a systematic, independent examination to verify compliance with the study protocol, Good Clinical Practice (GCP) guidelines, and applicable regulatory requirements [106]. The primary objectives are to protect participant rights and welfare, and to ensure the credibility and reliability of clinical trial data [106].
Core Audit Principles and Timing
A risk-based approach to auditing is now the standard, focusing resources on areas with the highest potential impact on patient safety, ethical considerations, and data integrity [106]. Audits can be categorized as follows:
- Pre-study Audits: Conducted before trial initiation to assess site capability and readiness [106].
- Routine Audits: Performed during the trial to monitor ongoing compliance and data quality [106].
- For-cause Audits: Triggered by specific events or concerns such as protocol deviations or data anomalies [106].
- Close-out Audits: Conducted after trial completion to review the entirety of trial conduct [106].
Essential Documents for Audit Review
A thorough consent process audit involves a detailed review of key documents to verify compliance and proper documentation.
Table 1: Essential Documents for Consent Process Audit
| Document Category | Specific Items to Review | Audit Purpose |
|---|---|---|
| Protocol & Approvals | IRB-approved protocol and amendments; IRB approval letters [107] | Verify that consent is obtained for the currently approved protocol. |
| Informed Consent Forms (ICFs) | All IRB-approved ICF versions; completed ICFs with participant signatures [106] | Confirm use of correct version and proper execution. |
| Supporting Documentation | Experimental Subject's Bill of Rights (for California studies) [107]; filled-out ICF checklists [107] | Ensure all required ancillary documents are provided and completed. |
| Study Records | Source documents (medical records); subject screening and enrolment logs; correspondence [106] | Corroborate information in ICFs and verify adherence to protocol. |
Quantitative Measures and Common Deficiencies
Effective monitoring requires moving beyond qualitative checks to incorporate quantitative assessments of consent quality and comprehension.
Metrics for Assessing Consent Quality
Recent studies provide quantitative insights into participant preferences and comprehension. A 2025 study on digital health consent found that participants were 1.20 times more likely to prefer text modified for improved readability, particularly for sections explaining study risks (P=.03) [49]. The same study found that older participants tended to prefer the original, more detailed text by a factor of 1.95 times (P=.004), highlighting how demographic factors influence consent preferences [49].
A sobering study by Bottrell et al. found that the four required elements of informed consent—nature of the procedure, risks, benefits, and alternatives—were documented on consent forms only 26.4% of the time [13]. This points to a significant gap in the fundamental documentation of the consent process.
Common Deficiencies and Root Causes
Audits frequently identify several key areas of non-compliance:
- Lack of Patient Comprehension: Complex medical jargon and varying health literacy levels can prevent true understanding. A study of Chinese hospitals identified inadequacies in functional health literacy that compromised the consent process [13].
- Process Failures: These include inadequate staffing, unclear data management protocols, or non-user-friendly electronic systems that hinder proper consent documentation [106].
- Inadequate Documentation: Beyond missing core elements, this includes failures to use approved ICF versions or to document the consent conversation itself [13].
- Power Dynamics: Patients may feel pressured to consent due to perceived authority of clinicians, especially in vulnerable populations [13].
The diagram below illustrates a systematic quality management approach for investigating audit findings and implementing corrective actions.
Quality Management Investigation Workflow
Methodologies for Monitoring and Evaluation
Experimental Protocols for Consent Research
Empirical research into the consent process provides methodologies that can be adapted for internal monitoring.
Protocol 1: Assessing Readability and Participant Preference (Adapted from JMIR 2025 [49])
- Objective: To evaluate participant preferences for different presentations of consent information.
- Method: Recruit participants eligible for a study and present them with pairs of "text snippets" from the consent form. One snippet is the original IRB-approved text; the other is a modified version improved for readability using tools like a Readability Calculator to monitor character length, Flesch Kincaid Reading Ease, and lexical density [49].
- Data Collection: Survey participants to choose their preferred version and provide qualitative feedback.
- Analysis: Use quantitative analysis (e.g., regression models) to determine if factors like snippet length or participant demographics (age, sex, physical activity) influence preference.
Protocol 2: Evaluating the Surrogate Consent Process (Adapted from Chest 2025 [50])
- Objective: To identify best practices for surrogate decision-maker (SDM) engagement in critical care research.
- Method: Employ a mixed-methods approach across multiple academic medical centers. Conduct quantitative surveys and qualitative focus groups or semi-structured interviews with Principal Investigators (PIs), Research Coordinators (RCs), and SDMs [50].
- Data Collection: Gather perspectives on who should lead the consent conversation (PI vs. RC), optimal timing, setting, and mode of consent (in-person vs. remote).
- Analysis: Use thematic analysis for qualitative data and statistical tests (e.g., t-tests, chi-square) to compare responses across groups. This study found SDMs placed greater importance on the written consent document and were less concerned with its length than PIs/RCs (
P = .001) [50].
Table 2: Key Research Reagent Solutions for Consent Process Evaluation
| Tool or Resource | Function in Consent Evaluation | Application Example |
|---|---|---|
| Readability Calculator | Software to quantitatively assess the reading grade level and complexity of consent form text [49]. | Rewriting consent form snippets to improve Flesch Kincaid Reading Ease score before participant testing [49]. |
| Informed Consent Checklist | A structured tool to ensure all required elements of informed consent are present and properly documented [107]. | Used during site audits to verify ICFs contain nature of procedure, risks, benefits, and alternatives [13] [107]. |
| Verbal Consent Script | A standardized script approved by the REB/IRB for obtaining consent in minimal-risk studies or when written consent is impractical [70]. | Ensures consistent information disclosure during remote or telephone-based consent processes [70]. |
| Health Literacy Assessment Tool | A screening instrument (e.g., BRIEF, REALM) to identify participants who may need additional support to comprehend consent information [13]. | Used during screening to tailor the consent communication process to an individual's health literacy level. |
Advanced Considerations and Future Directions
The landscape of informed consent is evolving, requiring auditors and monitors to stay informed of new modalities and complexities.
- Verbal and Electronic Consent: The COVID-19 pandemic accelerated the adoption of verbal consent, often supported by tele-conferencing and e-consent platforms [70]. While making the process more conversational, it requires meticulous documentation, such as an audio recording or a copy of the consent script, approved by a Research Ethics Board (REB) [70].
- Digital Health Research: New technologies introduce complex risks related to data privacy and security. Consent forms must clearly explain data management protocols for information collected from mobile apps, wearable sensors, and AI algorithms [49].
- Cultural and Linguistic Competency: Language barriers and cultural differences significantly impact comprehension. The use of professional medical interpreters (including ASL interpreters) is mandatory, not optional [13]. In some cultures, collective family decision-making may be the norm, requiring a flexible yet compliant approach [13].
The following diagram outlines a comprehensive audit workflow from planning through to corrective actions, integrating the key principles discussed.
Comprehensive Consent Audit Workflow
A proactive, process-oriented approach to auditing and monitoring the informed consent process is critical for the ethical and legal integrity of clinical research. By moving beyond a simple signature check to a comprehensive evaluation of understanding, documentation, and underlying systems, researchers and sponsors can better protect participant rights and safety. As consent modalities evolve with technology, so too must audit methodologies, ensuring that the foundational ethical principle of respect for persons is upheld in every clinical interaction.
Comparing FDA, HHS, and International Regulatory Standards
The regulatory landscape for informed consent has evolved from a basic ethical concept into a complex, codified requirement essential to global clinical research. This evolution reflects a continuous effort to balance scientific progress with the paramount need for human subject protection. Historically, milestones like the Nuremberg Code and the Declaration of Helsinki established the foundational principle that voluntary informed consent is absolutely essential in research involving human beings. In the United States, these principles were operationalized through the regulatory frameworks of the Food and Drug Administration (FDA) and the Department of Health and Human Services (HHS), which, while overlapping, maintain distinct jurisdictions and requirements.
The development of informed consent is not static; it continuously adapts to new scientific and ethical challenges. Recent developments include adapting to the rise of artificial intelligence (AI) in medical devices, handling complex genetic data, and ensuring comprehension in an era of increasingly sophisticated clinical trials. Furthermore, global harmonization efforts, alongside the persistence of key regional differences, make an understanding of international standards a necessity for researchers and drug development professionals operating in a multinational environment. This guide provides a technical comparison of these standards, framed within this historical context, to equip professionals with the knowledge to navigate this critical area.
US Regulatory Framework: FDA vs. HHS
Agency Jurisdiction and Focus
The US regulatory environment for clinical research is primarily governed by two sets of regulations within HHS: those enforced by the FDA and those under the Common Rule, which is implemented by various departments including HHS itself (45 CFR 46).
- FDA (21 CFR 50 & 56): The FDA's regulations govern clinical investigations involving products regulated by the agency, such as drugs, biological products, and medical devices. Compliance with FDA regulations is required regardless of whether the research is federally funded [41].
- HHS Common Rule (45 CFR 46): The Common Rule applies to all human subjects research conducted or supported by any federal department or agency that has adopted the rule. Its focus is broader, covering all federally funded research [41] [46].
A key distinction is that while the FDA requires that an Institutional Review Board (IRB) review and approve all research, HHS requires institutions to file a formal "assurance" of compliance with HHS regulations [41]. The FDA does not require this assurance mechanism [41].
Key Regulatory Differences in Informed Consent
Although the core principles of informed consent are shared, operational differences exist between the FDA and the revised Common Rule. The FDA has not yet fully harmonized its regulations with the 2018 updates to the Common Rule [46]. Key differences are outlined in the table below.
Table 1: Key Differences Between FDA and HHS Common Rule Informed Consent Requirements
| Feature | FDA (21 CFR 50, 56) | HHS Common Rule (45 CFR 46) | Practical Implications for Researchers |
|---|---|---|---|
| Waiver for Minimal Risk | More restrictive; does not include a waiver aligned with §46.116(f)(3), though will not object if specific additional requirements are met [46]. | Allows an IRB to waive or alter some consent elements for minimal risk research under §46.116(f)(3) [46]. | Research protocol design must account for the more restrictive FDA rules for studies under FDA jurisdiction, even if they are minimal risk. |
| Post-2018 Common Rule Harmonization | Not yet harmonized with the 2018 Common Rule changes [46]. | Incorporated key changes from the 2018 revision. | Researchers must be aware of two slightly different sets of consent requirements depending on the source of regulatory authority. |
| Reimbursement | Does not consider reimbursement for travel/associated costs as coercive; payment for participation should be just and fair [46]. | Similar principles, but payment is not explicitly addressed in the summarized differences. | Clarity is provided that reasonable reimbursement is acceptable and should not be considered a benefit that justifies research risks. |
Recent Developments in US Regulations
- FDA Informed Consent Guidance (2023): The FDA released a final guidance in August 2023 that emphasizes the consent process as continuous, starting with recruitment and continuing through the study. It encourages shorter, clearer consent forms and allows for greater flexibility, such as using visual aids and discussing standard of care benefits verbally rather than in lengthy written text [46].
- HHS/CMS Guidance on Sensitive Exams (2024): In April 2024, HHS issued new guidance requiring hospitals to obtain explicit informed consent for "important surgical tasks" or "sensitive or invasive procedures" performed by practitioners, residents, or students, especially on anesthetized patients. This includes specific mention of breast, pelvic, prostate, and rectal examinations conducted for educational purposes [108].
International Regulatory Standards
European Union and United Kingdom
The EU and UK are undergoing significant regulatory reforms aimed at harmonizing and modernizing their frameworks for medicines and medical devices.
- EU Pharmaceutical Legislation Reform: A major revision of the general pharmaceutical legislation, last updated in 2004, is underway. The goals are to improve patient access, enhance supply chain security, promote innovation, and address antimicrobial resistance. The legislation is projected for adoption by 2026 [109].
- Health Technology Assessment (HTA) Regulation: The EU has implemented a harmonized Joint Clinical Assessment procedure to evaluate the relative effectiveness of new medicines and medical devices. This process became mandatory for new oncology products and advanced therapy medicinal products in January 2025 and will extend to all orphan medicinal products by 2028 [109].
- Medical Device Regulation (MDR): The EU is addressing challenges in implementing the MDR and In Vitro Diagnostics Regulation (IVDR), including certification delays and administrative burdens. The European Parliament has called for revisions with appropriate transition periods [109].
- United Kingdom (UK): The UK's Medicines and Healthcare products Regulatory Agency (MHRA) is progressively updating its UK Medical Devices Regulations (UKMDR), with further updates expected throughout 2025 [109].
Asia-Pacific Region
Major regulatory bodies in Asia are also reforming their processes to encourage innovation and reduce drug approval timelines.
- Japan: Japan's government is pursuing rulemaking to reduce "drug lag" by allowing drug approvals in certain circumstances without a clinical study in Japan, though post-approval safety and efficacy studies within Japan would still be required. Japan is also amending its Act on Pharmaceutical and Medical Devices (PMD Act) and has updated its approval process for software as a medical device (SaMD) [109].
- China: The State Council of China has proposed policy incentives to reform the life sciences industry, including facilitating the partial outsourcing of manufacturing to Chinese facilities by foreign companies. China is also considering amendments to its Medical Device Administrative Law (MDAL) that would raise penalties for non-compliance, particularly for high-risk implants [109].
- India: The Central Drugs Standard Control Organization (CDSCO) is undertaking significant regulatory reform to simplify regulation and enhance efficiency. A key initiative is requiring both sterile equipment manufacturers and small pharmaceutical companies to adhere to Good Manufacturing Practices (GMP) standards under Schedule M by the end of 2025 [109].
Table 2: Key International Regulatory Developments and Focus Areas
| Region/Country | Key Regulatory Developments | Primary Policy Objectives |
|---|---|---|
| European Union | Pharmaceutical Legislation Revision; HTA Regulation; MDR/IVDR review [109]. | Improve access, harmonize assessments, ensure device safety, promote innovation [109]. |
| United Kingdom | Staged updates to UK Medical Devices Regulations (UKMDR) [109]. | Post-Brexit regulatory independence, alignment with international standards, reducing burden [109]. |
| Japan | Rulemaking to reduce "drug lag"; PMD Act amendments; updated SaMD approval [109]. | Accelerate patient access to innovative drugs, support generic supply, embrace digital health [109]. |
| China | Policy incentives for manufacturing outsourcing; proposed amendments to MDAL [109]. | Attract foreign investment and collaboration, strengthen enforcement for device safety [109]. |
| India | CDSCO-led reforms; mandatory GMP (Schedule M) compliance expansion [109]. | Simplify regulation, enhance efficiency, ensure high safety and quality standards [109]. |
Comparative Analysis of Informed Consent Requirements
Informed consent requirements, while globally rooted in the principle of autonomy, exhibit notable variations across jurisdictions, especially for medical devices.
Core Requirements and Cultural Nuances
A comparative analysis reveals both a common core and important regional specifics. The following workflow diagram illustrates the key stages and considerations in the international informed consent development process for medical devices.
A structured comparison of specific requirements highlights critical differences that must be addressed in study documentation.
Table 3: International Comparison of Key Informed Consent Form (ICF) Requirements for Medical Devices [7]
| Informed Consent Requirement | USA | EU | UK | Taiwan | Malaysia |
|---|---|---|---|---|---|
| Recommendations on Layout & Format | Yes | Yes | Yes | No | No |
| Information on Risks, Benefits, Discomforts | Yes | Yes | Yes | Yes | Yes |
| Patient Involvement Recommendations | Yes | Yes | Yes | No | No |
| Transparency Wording Requirements | No | Yes | Yes | No | No |
| Cultural Acceptability Considerations | No | No | No | No | Yes |
| Personal Information Listed on Form | No | No | No | Yes | No |
| Witness Present at Consent Process | Yes | No | No | Yes | No |
Practical and Ethical Considerations for Global Studies
- Clarity and Simplicity: The US FDA specifically recommends against lengthy, complex consent forms, encouraging the use of bullet points, clear headings, and visual aids like diagrams or videos to enhance participant understanding [7]. This is particularly important for medical devices, where animations can effectively explain implantation procedures [7].
- Comprehension Verification: It is considered good practice for researchers to check participant comprehension by asking simple questions about the study before the consent form is signed [7].
- Vulnerable Populations: Special ethical considerations are required when the study involves vulnerable patients, such as those requiring surgical intervention. The FDA provides specific guidance on enrolling groups like children and wards of the state [46].
- AI and Data Usage: With the rise of AI in healthcare, it is crucial to clearly explain in the consent document if data collected will be used to train AI algorithms [7].
Implementation and Operationalization
The Researcher's Toolkit: Essential Components for Compliant Informed Consent
Successfully implementing informed consent in a global context requires a suite of procedural and documentation tools. The following table details key components of this "toolkit."
Table 4: Research Reagent Solutions: Essential Components for Informed Consent
| Toolkit Component | Function and Purpose | Regulatory/Practical Consideration |
|---|---|---|
| Institutional Review Board (IRB) | A formally designated group to review, approve, and monitor biomedical research to protect human subjects [41]. | Required by FDA regulations. Can be institutional or independent (outside). IRB membership must be diverse, including both scientific and non-scientific members [41]. |
| Informed Consent Form (ICF) | The document provided to a participant to ensure they have the information needed to make an informed decision. | Must include basic elements like risks, benefits, and alternatives. Should be clear and concise. Serves as evidence that the consent process occurred [41] [46]. |
| Participant Information Sheet (PIS) | A document, sometimes separate from the ICF, that provides detailed information about the study in lay language. | Can be provided before the ICF to prevent accidental signing without understanding. Helps improve participant comprehension [7]. |
| Visual Aids (Diagrams, Videos) | Pictorial or animated materials used to explain complex medical procedures or devices. | Strongly recommended by FDA to improve understanding, especially for medical device implantation procedures and pediatric studies [7] [46]. |
| Certificates of Confidentiality (CoC) | Protections issued to shield identifiable, sensitive research data from forced disclosure (e.g., legal subpoenas). | The 21st Century Cures Act broadened protections and mandates CoCs for federally funded research. Can be requested from the FDA for other FDA-regulated research [46]. |
| Short Form Consent | A document used when a participant's primary language is not that of the standard ICF. | Requires a witness and a written summary of the verbally presented information. The process can be as complex as using a full translated form [46]. |
Navigating a Dynamic Regulatory Landscape
The global regulatory environment is in a state of flux. Life sciences companies and researchers must adopt proactive strategies to ensure compliance and operational success.
- Proactive Regulatory Intelligence: Establish dedicated teams to monitor policy changes, leadership appointments (e.g., new FDA Commissioner or HHS Secretary), and judicial decisions that may impact regulatory interpretation [109] [110].
- Invest in Digital Compliance Infrastructure: Leverage compliance management platforms to automate monitoring, risk assessment, and reporting, which is especially critical for managing evolving obligations in cybersecurity and AI [110].
- Strengthen Cross-Functional Collaboration: Foster collaboration between regulatory, legal, IT, and product development teams to ensure compliance is integrated throughout the product lifecycle [110].
- Global Harmonization Efforts: The FDA's alignment of its Quality System Regulation with ISO 13485:2016 for medical devices is a significant step toward global harmonization. Companies should leverage such synergies to streamline global quality processes and reduce redundancies [110].
Unique Consent Requirements for Medical Device vs. Drug Clinical Investigations
The concept of informed consent has evolved significantly from a time when physician authority was largely unquestioned to its current status as a cornerstone of medical and research ethics, protecting patient autonomy and rights [62]. This evolution has occurred within a framework of international ethical standards, notably the Declaration of Helsinki, which establishes uniform ethical consent standards [62]. In modern practice, informed consent requires that individuals receive sufficient information presented in an understandable manner about a study's purpose, goals, procedures, and potential risks, enabling them to make a fully voluntary decision regarding participation [62].
While the fundamental ethical principles underlying informed consent apply universally across clinical research, the practical application and specific requirements diverge significantly between medical device and drug investigations. These differences stem from intrinsic variations in how therapies are developed, delivered, and regulated. Medical device trials present unique challenges, including the frequent impossibility of blinding due to the physical nature of the intervention, the involvement of surgical or other invasive procedures, and a distinct regulatory pathway that has historically lacked specific guidance, often forcing device developers to adapt consent frameworks designed for pharmaceuticals [7] [111]. This guide examines these critical distinctions, providing researchers, scientists, and development professionals with a detailed technical analysis of consent requirements specific to medical device investigations within the broader historical and ethical context of informed consent.
Fundamental Differences Between Device and Drug Clinical Investigations
The structural and methodological divergences between medical device and drug trials directly influence the content, process, and emphasis of informed consent. A clear understanding of these foundational differences is prerequisite to appreciating the nuances of consent requirements.
Table 1: Core Structural Differences Between Drug and Device Clinical Trials
| Aspect | Drug Trials | Device Trials |
|---|---|---|
| Trial Structure | 4 phases (I-IV) [111] | 3 stages (Early Feasibility, Pivotal, Post-Market) [111] |
| Initial Participants | Healthy volunteers (Phase I) [111] | Only the intended disease population [111] |
| Control Group | Placebo common [111] | Standard of care or active control; placebo often impossible [111] |
| Blinding | Double-blind standard [111] | Often impossible due to the device's physical nature [111] |
| Primary Initial Focus | Dosage, pharmacokinetics, and toxicity [111] | Safety and functionality/procedural success [111] |
| Typical Duration | Often years per phase [111] | Typically shorter and more focused [111] |
The choice of participants is a critical ethical differentiator. Drug trials commonly begin with healthy volunteers who have no direct therapeutic need for the investigational product, a population that requires particularly rigorous consent processes to ensure understanding of pure research participation. In contrast, device trials almost exclusively enroll the intended disease population from the outset, as the interventions often involve surgical implantation or specific use by patients with a medical condition [111]. This means consent discussions in device trials are framed within the context of a patient's existing illness and treatment options.
Furthermore, the nature of the intervention makes blinding profoundly different. While double-blinding is standard in drug trials, it is frequently unachievable in device trials due to the visible and tangible nature of the device or the required surgical procedure [111]. This lack of blinding heightens the potential for bias, a risk that must be transparently communicated during the consent process. The consent form should clearly state that the participant and investigator will be aware of the treatment assignment.
The following diagram summarizes the distinct pathways and key decision points in the clinical development lifecycle for drugs and medical devices.
Regulatory Frameworks and Consent Requirements
Core Medical Device Consent Regulations
For medical devices in the United States, clinical investigations involving significant risk (SR) devices require an Investigational Device Exemption (IDE) approved by the FDA [111]. The informed consent process for these studies is governed by a triad of core regulations: 21 CFR Part 50 (Protection of Human Subjects), 21 CFR Part 56 (Institutional Review Boards), and 21 CFR Part 812 (IDE regulations) [111] [112]. The FDA's guidance emphasizes that consent is a continuous process, not a single event, requiring that participants be updated if new information arises that could affect their willingness to continue [112].
A key requirement is comprehensive disclosure. Sponsors must provide clear, understandable information covering the device description, study procedures, known and potential risks and side effects, potential benefits, and alternative treatments [112]. The principle of voluntariness is paramount; participation must be free from coercion or undue influence, and participants must feel able to withdraw without penalty [112]. This consent must be documented in writing, signed by both participant and investigator, with electronic signatures acceptable under 21 CFR Part 11 [112].
Special Considerations and Waivers
The FDA also provides for exceptions under limited conditions. A final rule effective January 2024 permits an IRB to waive or alter consent requirements for certain FDA-regulated minimal-risk clinical investigations [113]. To grant such a waiver, an IRB must find and document five criteria:
- The investigation involves no more than minimal risk to subjects.
- It could not practicably be carried out without the waiver.
- If using identifiable private information or biospecimens, the research could not be carried out without using them in an identifiable format.
- The waiver will not adversely affect subjects' rights and welfare.
- Whenever appropriate, subjects will be provided with additional pertinent information after participation [113].
This rule aligns FDA regulations with the Common Rule, facilitating a more consistent ethical review framework [113]. Another evolving concept is broad consent, introduced in the 2019 revision of the Common Rule, which allows for the secondary use of identifiable private information and biospecimens in research [62]. This falls between a waiver and full informed consent, providing a general understanding of potential uses without specifying exact future projects. However, this approach carries ethical risks if it lacks transparency, particularly regarding data sharing with commercial entities for AI development, potentially undermining the principle of informed consent if not implemented carefully [62].
Practical Implementation in Medical Device Consents
Enhancing Comprehension and Format
A major challenge in medical device consent is explaining complex procedures and devices without relying on technical jargon. The FDA recommends creating shorter, clearer ICFs that present information in an easily accessible way [7]. This is particularly important for medical devices, which can often be better explained using visual aids like animations, short videos, or pictorials [7]. For example, an animation can be highly successful in explaining a device to children in paediatric studies [7].
Formatting choices can enhance readability, using bubbles, rounded boxes, bullet points, or two columns to create discrete units of information [7]. However, it is critical to consider the patient population. Text-to-speech software used by visually impaired people may not read tables or formatted text correctly; in such cases, an audio recording or a large-print document may be necessary [7]. Participants with dementia may benefit from simplified ICFs and repeated information [7]. Developers are encouraged to engage patient groups and perform in-depth analysis as part of patient diversity plans to determine the best consent approach [7].
Conveying Risks and the Nature of the Device
A unique challenge for medical devices is the presentation of risks, which often include both procedure-related risks (e.g., from surgery) and device-related risks [7]. The consent must clearly distinguish between the two. Furthermore, for early feasibility studies, the list of adverse events is often based on literature for similar devices rather than actual safety data from the specific investigational device, a fact that must be transparently stated in the ICF to avoid ambiguity [7].
The key information should be presented at the beginning of the consent form. For an implantable device, this includes whether the device is commercially available, the location of implantation, hospitalization requirements, and procedure-specific risks [7]. It is also essential to clearly distinguish between procedures that are part of the clinical investigation and those that constitute standard of care, the latter of which should be mentioned only briefly in the ICF [7]. As artificial intelligence becomes integrated into medical devices, any use of AI to collect or analyze data must be clearly explained in plain language within the participant information sheet [7].
Table 2: Key Content Emphasis in Device vs. Drug Informed Consent Forms
| Content Area | Medical Device Consent Emphasis | Drug Consent Emphasis |
|---|---|---|
| Nature of Intervention | Physical device; often a surgical/procedural intervention [111]. | Chemical/biological compound; administration (oral, IV, etc.). |
| Risk Profile | Procedure-related risks (surgery, anesthesia) + device-specific risks (malfunction, failure, biocompatibility) [7]. | Pharmacological toxicity, side effects, drug interactions. |
| Explanation of Control | Standard of care or active control; explanation of why a placebo is not used or feasible [111]. | Placebo or active comparator; explanation of blinding. |
| Long-Term Implications | For implants: potential for revision, explanation, or long-term monitoring [111]. | Long-term side effects after cessation of dosing. |
| Technical Function | How the device works and its intended mechanism of action, often requiring diagrams. | Pharmacokinetics and pharmacodynamics. |
The Consent Process and Workflow
The informed consent process is a multi-stage workflow that ensures participant comprehension and voluntary agreement. Best practices recommend providing the Participant Information Sheet (PIS) separately from the Informed Consent Form (ICF) initially to prevent accidental signing without full understanding [7]. A face-to-face discussion with an investigator is crucial, and researchers should check comprehension by asking simple questions before the participant signs the ICF [7]. This practice identifies unclear sections and ensures participants are fully informed.
The Researcher's Toolkit: Essential Components for Compliant Consent
Successfully navigating the unique consent requirements for medical device investigations requires a set of essential tools and methodologies. The following table details key components for ensuring an ethical and compliant informed consent process.
Table 3: Essential Components for Medical Device Informed Consent
| Toolkit Component | Function & Purpose | Regulatory/Ethical Basis |
|---|---|---|
| Standardized ICF Template | Master template aligned with FDA IDE guidance and Good Clinical Practice (GCP), adaptable for country-specific requirements [7] [112]. | 21 CFR 812, ICH E6(GCP) [53] [111] |
| Visual Aid Library | Animations, videos, and pictorials to explain complex device functionality and implantation procedures, improving participant comprehension [7]. | FDA recommendation for accessible information [7] |
| Comprehension Assessment Questions | A short set of simple questions used by investigators to verify participant understanding of key study elements before signing [7]. | Ethical principle of ensuring comprehension [7] [112] |
| Electronic Consent (eConsent) System | Digital platform to facilitate consent, streamline enrollment, manage signatures, ensure version control, and comply with 21 CFR Part 11 [53] [112]. | 21 CFR Part 11, FDA encouragement of technology [7] [53] |
| IRB Communication Protocol | Established process for pre-submission consultation and efficient communication with the reviewing IRB for timely approval [53] [112]. | 21 CFR Part 56 [111] |
| Continuous Process SOP | Standard Operating Procedure defining how new information is communicated to participants and re-consent is obtained during the trial [112]. | FDA requirement for continuous consent [112] |
The informed consent process for medical device clinical investigations demands a specialized approach distinct from pharmaceutical trials. Key differentiators include the necessity to convey procedure-related risks, the frequent impossibility of blinding, and the need for visual and clear explanations of physical device functionality. The regulatory landscape is evolving, with recent FDA guidance emphasizing shorter, more comprehensible consent forms and new rules allowing for minimal-risk waivers [7] [113].
Future directions point toward greater use of technology, such as eConsent platforms and multimedia aids, and ongoing ethical deliberation around models like broad consent for data reuse in AI development [7] [62] [53]. For researchers and sponsors, success hinges on viewing informed consent not as a regulatory hurdle, but as a continuous, ethical dialogue with participants. This requires leveraging available tools and methodologies—from standardized templates to comprehension verification—ensuring that the consent process is truly informative, respectful of participant autonomy, and ultimately, scientifically and ethically sound.
Evaluating the Efficacy of Digital and AI-Driven Consent Tools
Informed consent forms the ethical and legal cornerstone of human subjects research, with origins in the Nuremberg Code and its enshrinement in U.S. Federal Regulations (45 CFR 46.116) [48]. This principle mandates that consent must be voluntary, comprehending, and granted by an individual with sufficient knowledge and comprehension of the subject matter involved [48]. Traditional consent processes, however, have consistently faced a fundamental challenge: the significant gap between technical documentation and participant understanding. Studies have repeatedly shown that consent forms frequently exceed recommended readability levels, with one analysis of radiotherapy consent forms revealing a mean readability ranging from grade level 10.6 to 14.2, far exceeding the recommended sixth- to eighth-grade level [114]. This complexity creates barriers to participant comprehension, recruitment, and retention, ultimately compromising the ethical integrity and operational efficiency of clinical research.
Digital and Artificial Intelligence (AI)-driven consent tools represent a paradigm shift in addressing these chronic challenges. By leveraging technologies such as Large Language Models (LLMs) and interactive digital platforms, these tools aim to transform static, complex documents into dynamic, personalized, and comprehensible consent experiences [114]. This technical guide evaluates the efficacy of these emerging solutions within the context of their historical development, providing researchers, scientists, and drug development professionals with evidence-based methodologies for implementation and validation.
The Digital and AI Consent Landscape
The transition from paper-based to digital consent represents more than a simple change of medium. Modern digital platforms, often called eConsent, incorporate multimedia elements, interactive comprehension checks, and accessibility features designed to enhance understanding. The emergence of generative AI, particularly LLMs like GPT-4, marks a second, more profound evolution: the shift from standardized digital forms to adaptive, personalized consent experiences [114].
AI-driven tools are being applied across the consent continuum. In clinical trials, they can create patient-friendly summaries from technically dense informed consent forms (ICFs) [114]. In marketing, consent-first AI personalization is driving a 20% surge in customer engagement by using dynamic content on opted-in lists [115]. For UX research, AI tools like Notably and Granola can synthesize qualitative data from participant interactions, though researchers remain responsible for obtaining proper consent and NDAs [116]. The core capability of these AI systems lies in their ability to process complex language and restructure it for clarity and comprehension, making specialized information accessible to a lay audience without sacrificing factual accuracy.
Quantitative Efficacy Analysis
Rigorous evaluation is critical for adopting any new tool in regulated environments like clinical research. Emerging data on digital and AI-driven consent tools demonstrate measurable impacts on comprehension, engagement, and operational efficiency.
Table 1: Measured Outcomes of AI-Driven Consent Tools
| Metric Category | Specific Metric | Result | Context / Source |
|---|---|---|---|
| Readability & Comprehension | Readability Improvement | Significantly improved vs. original ICFs | AI-generated summaries from clinical trial ICFs [114] |
| Participant-Reported Understanding | >80% reported improved understanding | Survey of participants reviewing AI summary of the BROADBAND trial [114] | |
| Process Efficiency | Multi-Choice Question Answer (MCQA) Concordance | High agreement with human-annotated responses | LLM-generated understanding checks vs. human answers [114] |
| Participant Engagement | Customer Engagement Lift | 20% surge | Consent-first AI personalization on opted-in marketing lists [117] [115] |
| Open Rate Increase | Up to 26% higher | DTC brands using first-party data with consent-orchestration [115] |
Table 2: Performance Comparison of AI Summarization Techniques
| Method | Description | Accuracy & Completeness | Readability Outcome |
|---|---|---|---|
| Direct Summarization | LLM generates a concise summary of an ICF in a single step. | Lower than sequential approach; more inaccuracies or missing details. | Significantly improved over original ICFs. |
| Sequential Summarization | A multi-step process of extracting, processing, and simplifying content while preserving essential information. | Higher accuracy and completeness; fewer inaccuracies. | Significantly improved over original ICFs; potentially better due to retained context. |
The data indicates that the sequential summarization approach, while more resource-intensive, yields superior outcomes in accuracy, making it more suitable for high-stakes environments like clinical trials where missing or incorrect information could have serious ethical and legal consequences [114]. Furthermore, the consent-first application of AI, where personalization is applied only to opted-in populations, demonstrates that respect for autonomy can coexist with, and even enhance, engagement metrics [115].
Experimental Protocols for Validation
Validating the efficacy of an AI-driven consent tool requires a structured experimental protocol. The following methodology, derived from published research, provides a framework for rigorous evaluation.
Protocol: Evaluating LLM-Generated Consent Summaries
1. Objective: To assess the efficacy of an LLM in generating accurate, complete, and comprehensible summaries from technical Informed Consent Forms (ICFs).
2. Materials & Reagents:
- Source Documents: A set of original, institution-approved ICFs from one or more clinical trials (e.g., downloaded from ClinicalTrials.gov) [114].
- AI Model: Access to a state-of-the-art LLM (e.g., GPT-4 API) [114].
- Human Annotators: Domain experts (e.g., clinical researchers, IRB members) and layperson representatives from the target participant population.
- Evaluation Metrics:
- Readability Scores: Flesch-Kincaid Grade Level and Reading Ease scores [48].
- Accuracy & Completeness Checklist: A pre-defined list of key elements from the original ICF (e.g., study objectives, procedures, risks, benefits, costs, voluntary nature) [114] [118].
- Participant Understanding Survey: A post-comprehension survey, including multiple-choice question-answer pairs (MCQAs) generated by the LLM and validated by human annotators [114].
3. Procedure:
- Step 1: Prompt Engineering. Develop and refine two distinct sets of instructions for the LLM:
- Direct Summarization Prompt: A single instruction to "generate a patient-friendly summary" of the input ICF.
- Sequential Summarization Prompt: A multi-step instruction set [114]:
- "Extract and list the key sections: study objectives, procedures, risks, costs, and potential benefits."
- "For each extracted section, rewrite the content at an 8th-grade reading level."
- "Synthesize the simplified sections into a single, cohesive summary document."
- Step 2: Summary Generation. Execute both prompting strategies for each ICF in the test set.
- Step 3: Readability Analysis. Calculate the readability scores for the original ICF and both AI-generated summaries.
- Step 4: Expert Accuracy Assessment. Domain experts review the AI-generated summaries against the original ICF using the accuracy and completeness checklist.
- Step 5: MCQA Generation & Validation. Prompt the LLM to generate MCQs based on its own summaries. Have domain experts answer the same questions and measure concordance.
- Step 6: Participant Testing. Recruit a cohort representative of the target population. Present them with the AI-generated summary and the MCQA. Solicit feedback on perceived understanding.
4. Data Analysis:
- Compare readability scores using descriptive statistics.
- Calculate accuracy/completeness scores for each method.
- Compute concordance rates between LLM-generated MCQAs and expert answers.
- Analyze participant survey results for subjective understanding.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Digital Consent Research
| Tool / Reagent | Function / Purpose | Implementation Example |
|---|---|---|
| Large Language Model (LLM) | Generates patient-friendly summaries and comprehension questions from technical documents. | Using GPT-4 to simplify ICFs from ClinicalTrials.gov via direct or sequential summarization [114]. |
| Readability Formula | Quantifies the reading grade level required to understand a text, providing an objective measure of clarity. | Using the Flesch-Kincaid Grade Level in Microsoft Word to ensure consent forms meet an 8th-grade target [48]. |
| Consent Form Template | Provides a structurally and ethically sound starting point for creating research consent documents. | Starting with an IRB-approved template that includes all required elements per 45 CFR 46.116 [118]. |
| Preference Center / CMP | Captures and manages user consent preferences for personalization in a compliant manner. | Using a Consent Management Platform (CMP) like OneTrust to orchestrate consent-driven marketing [115]. |
| Multi-Choice Q&A (MCQA) | Objectively assesses a participant's understanding of the key concepts in the consent material. | Using LLM-generated MCQs to gauge patient comprehension of a trial summary, validated against expert answers [114]. |
Implementation Framework and Risk Mitigation
Successfully implementing AI-driven consent tools requires a strategic framework that integrates technology, process, and ethics.
Key Implementation Steps:
- Workflow Redesign: Integrate AI as an assistive tool within a human-led process. High-performing organizations are three times more likely to fundamentally redesign individual workflows to capture AI's value [119]. The clinician or researcher must remain the final decision-maker, using AI-generated summaries as a starting point for discussion rather than a final product [120].
- Compliance and Transparency: Update consent forms to explicitly disclose the use of AI tools in the consent process, describing their role and the data they process in plain language [120]. This transparency is critical for maintaining trust and legal validity.
- Continuous Monitoring and Validation: Establish systems to measure the effectiveness of AI tools, monitoring patient outcomes, diagnostic accuracy, and comprehension rates [120]. Continuous validation is necessary to detect performance degradation or inequitable outcomes across different demographics.
Mitigating Critical Risks:
- AI Hallucinations: LLMs can generate plausible but incorrect or misleading statements [114]. Mitigation: Implement a mandatory human review step for all AI-generated content before use with participants. Define processes for determining when model outputs require human validation, a practice common among AI high performers [119].
- Data Privacy: Protecting sensitive participant data is paramount. Mitigation: Avoid using general-purpose AI models that train on user input by default. Instead, prioritize platforms explicitly designed for data privacy in research [121] and ensure all vendor contracts include provisions for data protection and compliance [120].
- Algorithmic Bias: AI models can perpetuate and amplify biases present in their training data. Mitigation: Conduct regular fairness checks on models and perform ongoing monitoring to ensure equitable performance across diverse patient demographics [120] [115].
Digital and AI-driven consent tools represent a significant advancement in the historical development of informed consent, moving the process from a static, legally focused transaction to a dynamic, participant-centered dialogue. Evidence demonstrates their potential to significantly improve readability, comprehension, and engagement when implemented via rigorous, structured protocols like sequential summarization. However, their efficacy is contingent upon a foundational commitment to ethical principles. Trust, not just technological sophistication, remains the ultimate metric of success. By integrating these powerful tools within a robust framework of human oversight, continuous validation, and transparent communication, researchers can fulfill the enduring promise of informed consent: truly respecting the autonomy and dignity of every research participant.
Informed consent serves as a fundamental ethical and legal doctrine in both clinical practice and human subjects research, ensuring respect for patient autonomy and bodily integrity. The requirement that individuals provide voluntary and informed agreement to medical procedures underpins the modern healthcare relationship. Invalid consent—whether due to lack of information, coercion, or procedural failure—triggers significant legal consequences and professional repercussions. This analysis examines the legal and professional ramifications of invalid consent within the context of its historical development and contemporary regulatory requirements, providing a crucial framework for researchers, scientists, and drug development professionals navigating this complex landscape. Understanding these consequences is essential not only for legal compliance but also for maintaining the highest ethical standards in medical research and practice.
The evolution of informed consent from a simple ethical notion to a rigorous legal requirement reflects its critical role in protecting patient rights. As Bazzano et al (2021) document, the foundation of informed consent was established through early 20th-century judicial decisions that affirmed patient autonomy, including the seminal 1914 case Schloendorff v. Society of New York Hospital where Justice Benjamin Cardozo famously declared: "Every human being of adult years and sound mind has a right to determine what shall be done with his own body" [12]. This principle was further solidified following the unethical medical experiments of the Nazi regime and the Tuskegee Syphilis Study, which highlighted the necessity of voluntary consent in both treatment and research contexts [13].
Historical and Legal Foundations of Informed Consent
The legal framework for informed consent has evolved significantly over the past century, transitioning from medical paternalism to patient-centered autonomy. The early foundational cases established that healthcare providers must obtain consent for procedures, while subsequent rulings expanded this requirement to include adequate disclosure of risks.
Landmark Legal Cases Establishing Consent Requirements
Table 1: Foundational Legal Cases in Informed Consent Doctrine
| Case | Year | Legal Principle Established | Significance |
|---|---|---|---|
| Mohr v Williams | 1905 | Surgeon liable for performing procedure on different site than consented | Established that consent must be specific to the procedure performed |
| Pratt v Davis | 1905 | Physician liable for deceptive consent practices | Affirmed patient's right to bodily integrity and full disclosure |
| Rolater v Strain | 1913 | Provider liable for performing expressly forbidden procedure | Reinforced that consent boundaries must be respected |
| Schloendorff v Society of New York Hospital | 1914 | Patient autonomy as foundational principle | Established right to determine what happens to one's own body |
| Salgo v Leland Stanford Jr. University | 1957 | Coined term "informed consent" | Required disclosure of potential risks and alternatives |
The historical development of informed consent reveals a gradual but consistent strengthening of patient rights. As Rosenfeld (2018) notes in the Harvard Bioethics Journal, "The ability for each of us to make our own decisions about important events and commitments is fundamental to our sense of well-being and control over our lives" [54]. This evolution has established clear legal standards that healthcare providers must meet when obtaining consent for medical procedures or research participation.
Regulatory Frameworks Governing Informed Consent
Contemporary informed consent requirements are codified in multiple regulatory frameworks. The Common Rule (45 CFR 46) establishes the baseline requirement for informed consent in federally funded research, mandating that investigators provide prospective subjects with adequate information about the research, including its purpose, procedures, risks, benefits, and alternatives [54]. The 2017 revisions to the Common Rule introduced additional requirements, including that "informed consent must begin with a concise and focused presentation of the key information that is most likely to assist a prospective subject... in understanding the reasons why one might or might not want to participate in the research" [54].
For clinical practice, state laws and professional licensing boards establish informed consent requirements. As noted in the analysis of Illinois law, healthcare providers must disclose the risks of procedures, and failure to do so can result in liability if patients consent to treatment they would otherwise have refused if properly informed [122].
Legal Consequences of Invalid Consent
Invalid consent exposes healthcare providers and researchers to significant legal liability across multiple domains. The legal theories underpinning these consequences include both intentional torts and negligence claims.
Medical Malpractice and Negligence Claims
Medical malpractice represents the most common legal consequence of invalid consent. To establish malpractice based on inadequate consent, plaintiffs must typically demonstrate that:
- The provider had a duty to disclose specific risk information
- The provider failed to disclose this information or inadequately explained the risks
- The patient consented to treatment based on incomplete information
- The patient suffered harm from the undisclosed risk that materialized [122]
As detailed in the StatPearls article, the standard for adequate disclosure varies by jurisdiction, with most states using the "reasonable patient standard" (what a typical patient needs to know to make an informed decision), while others use the "reasonable clinician standard" (what a typical clinician would disclose) or "subjective standard" (what the particular patient needed to know) [13].
Battery Claims
Unlike malpractice claims which allege negligence, battery claims assert intentional unauthorized touching. When providers perform procedures without any consent or substantially exceed the scope of consent, they may be liable for battery. As illustrated by Brooke Shields' experience where a doctor performed an "unauthorized surgical procedure" that he described as "a bonus," such violations represent fundamental infringements on bodily autonomy [122]. Battery claims do not require proof of physical injury—the unauthorized touching itself constitutes the harm.
Table 2: Legal Theories for Invalid Consent Claims
| Legal Theory | Elements Required | Damages Recoverable | Example Scenarios |
|---|---|---|---|
| Medical Malpractice | - Duty to disclose- Breach of duty- Causation- Harm | - Medical expenses- Lost wages- Pain and suffering- Punitive damages in egregious cases | - Failure to disclose specific risks- Downplaying potential complications- Not explaining alternatives |
| Battery | - Intentional touching- Without consent or beyond scope- Offensive or harmful | - Compensatory damages- Punitive damages- No injury required to claim | - Procedure on wrong site- Performing non-consented procedure- Substantial deviation from consented procedure |
| Professional Discipline | - Violation of standards of practice- Ethical breaches- Unprofessional conduct | - License suspension/revocation- Fines- Practice restrictions- Required education | - Pattern of consent violations- Egregious failure to obtain consent- Fraudulent consent documentation |
Statistical Evidence of Consent-Related Violations
While comprehensive national data on invalid consent cases is limited, several studies highlight the scope of the problem:
- Wrong-site surgeries, often resulting from consent errors, accounted for 6% of the 1,441 sentinel events reviewed by the American College of Surgeons in 2022 [122]
- A study of unnecessary invasive procedures found that in nearly all cases (96.2%), the physician was male and working in private practice (92.4%), with 73.4% billing Medicare for these unauthorized procedures [122]
- Research on consent form adequacy found that required elements of informed consent—nature of procedure, risks, benefits, and alternatives—were documented on consent forms only 26.4% of the time [13]
Professional Discipline and Institutional Consequences
Beyond civil liability, healthcare providers face significant professional consequences for invalid consent practices. State medical boards can impose disciplinary actions including license suspension or revocation, mandatory ethics education, fines, and practice restrictions for consent violations [122]. These disciplinary measures address breaches of professional ethics standards regardless of whether patient harm occurred.
Healthcare institutions also face accreditation consequences for systematic consent failures. The Joint Commission requires documentation of all informed consent elements and may cite institutions for noncompliance during accreditation reviews [13]. Additionally, research institutions conducting human subjects research without valid consent risk suspension of research activities and loss of federal funding.
Risk Mitigation: Protocols for Valid Consent Processes
Implementing robust consent processes is essential for mitigating legal and professional risk. Evidence-based strategies include:
Enhanced Communication and Comprehension Protocols
Effective consent processes must address varying levels of health literacy and comprehension barriers. Research demonstrates that:
- The teach-back method, where patients explain information in their own words, significantly improves understanding and identifies comprehension gaps [13]
- Graphical tools and interactive media enhance risk communication and support shared decision-making [13]
- Implementing health literacy-based consent forms improves patient-provider communication and increases patient comfort in asking questions [13]
Recent studies of consent form readability found that documents often exceed recommended complexity levels, with one analysis of COVID-19 trial consent forms showing all documents assessed were classified as "difficult" for comprehension with reading ages of 14 years or higher, despite recommendations targeting reading ages of 9-11 years [123].
Special Population Considerations
Valid consent requires adapting processes to individual needs and circumstances:
- For patients with language barriers, professional interpreter services are essential, as using family members or untrained interpreters risks inaccurate communication and invalid consent [13]
- For patients with diminished capacity, surrogate decision-makers must be properly identified and engaged in the consent process [124]
- Cultural sensitivity is crucial, as decision-making norms vary—some cultures prioritize family or community decisions over individual autonomy [13]
Research with ethnic minority groups highlights that "trust played an important role and was facilitated by engaging community leaders and ensuring cultural and linguistic sensitivity during discussions" [123].
Documentation and Process Standards
Comprehensive documentation remains essential for demonstrating valid consent. The Joint Commission requires documentation of: (1) the nature of the procedure, (2) risks and benefits, (3) reasonable alternatives, (4) risks and benefits of alternatives, and (5) assessment of patient understanding [13].
The following diagram illustrates the comprehensive risk mitigation protocol for obtaining valid informed consent:
Experimental Protocols and Research Applications
The legal and ethical requirements for informed consent present particular challenges in research contexts, necessitating specialized methodologies and approaches.
Research on Consent Processes
Recent studies have employed innovative methods to evaluate and improve consent processes:
- Public deliberation methods engage diverse communities in developing acceptable consent approaches through structured education, expert perspectives, and facilitated discussion [103]
- Multimodal studies using questionnaires, focus groups, and interviews with multiple stakeholders (investigators, coordinators, surrogates, and patients) provide comprehensive understanding of consent practices and preferences [124]
- Randomized studies comparing telehealth versus in-person consent evaluate comprehension and decision-making outcomes across different consent modalities [123]
Inclusive Research Frameworks
Advancing inclusive research requires systematic approaches to ensure diverse population representation. The Five Principles for Advancing Inclusive Research framework provides a structured approach:
- Population science considerations - Understanding biological, genetic, and demographic factors affecting disease burden and representation [125]
- Data-informed site placement - Ensuring trial enrollment reflects geographical disease burden [125]
- Data-driven trial design - Using population data to inform inclusive trial protocols [125]
- Patient-reported data standards - Implementing consistent collection methods for participant-reported information [125]
- Enabling trial access - Addressing barriers through trust-building, navigation support, and assistance programs [125]
This framework emphasizes measuring representativeness using metrics such as the participation-to-prevalence ratio, which compares the percentage of a population among study participants to their percentage in the disease population, with a range of 80-120% suggesting adequate representation [125].
Essential Research Reagents and Methodologies
Table 3: Research Methodologies for Studying Informed Consent Processes
| Methodology | Application in Consent Research | Key Outputs | Considerations |
|---|---|---|---|
| Public Deliberation | Engaging communities in developing acceptable consent approaches | Community-informed consent models, Trust-building strategies | Resource-intensive, Requires skilled facilitation, Cultural adaptation needed |
| Mixed-Methods Studies | Comprehensive evaluation of consent practices from multiple perspectives | Identification of barriers/facilitators, Stakeholder preference data | Complex analysis, Integration of qualitative/quantitative data |
| Readability Analysis | Assessing comprehension accessibility of consent documents | Flesch-Kincaid scores, Reading age levels, Complexity metrics | Limited to document analysis, Doesn't assess interpersonal communication |
| Randomized Controlled Trials | Comparing effectiveness of different consent approaches | Evidence-based consent protocols, Modality effectiveness data | Ethical considerations, Generalizability limitations |
| Health Literacy Assessment | Evaluating patient understanding and comprehension gaps | Identification of communication barriers, Targeted improvement strategies | Requires validated tools, Cultural and linguistic adaptation |
Invalid consent exposes healthcare providers and researchers to substantial legal liability including malpractice claims, battery lawsuits, and professional discipline. The historical evolution of informed consent from simple assent to comprehensive shared decision-making reflects its fundamental role in respecting patient autonomy and ethical medical practice. For researchers, scientists, and drug development professionals, implementing robust consent processes that address health literacy, cultural considerations, and special population needs is essential for both legal compliance and ethical research conduct. Contemporary approaches emphasizing comprehension and engagement, as reflected in the revised Common Rule's requirement for "key information" presentation, represent the continuing evolution of consent standards toward truly informed and voluntary decision-making. As consent requirements continue to develop in response to technological advances and increasing research complexity, maintaining focus on the foundational principle of respect for persons remains paramount for both legal protection and ethical practice.
Informed consent represents a cornerstone of ethical research, continuously evolving to meet new scientific and regulatory challenges. This whitepaper examines two significant contemporary consent frameworks—broad consent and dynamic consent—that have emerged to address the complexities of modern biomedical research involving biospecimens and data. Broad consent, formally incorporated into the 2018 revisions of the Common Rule, provides a regulatory mechanism for obtaining prospective consent for the storage, maintenance, and secondary research use of identifiable private information and biospecimens. Dynamic consent, enabled by digital platforms, offers a participant-centric model for ongoing, interactive consent management. This technical guide examines the regulatory foundations, implementation requirements, and practical applications of both models, providing researchers, scientists, and drug development professionals with the knowledge necessary to navigate this evolving ethical landscape.
The evolution of informed consent in research ethics has been marked by key historical developments and ethical guidelines established in response to past abuses. The Common Rule (45 CFR Part 46) serves as the primary federal policy for human subjects protection in the United States, with its 2018 revisions introducing significant changes to consent requirements for biospecimen and data research [126] [127]. These revisions emerged from decades of ethical deliberation, including guidance from the President's Commission for the Study of Bioethical Issues and the National Bioethics Advisory Commission, which addressed controversies surrounding biological specimens and associated data [127].
Prior to the 2018 revisions, researchers faced a binary choice: obtain study-specific informed consent or request an Institutional Review Board (IRB) waiver of consent [126]. The revised Common Rule introduced broad consent as a third option, specifically addressing secondary research with identifiable private information and identifiable biospecimens [126]. Simultaneously, technological advances and the emergence of precision medicine have driven the development of dynamic consent models that leverage digital platforms to provide ongoing transparency and participant control [128] [129].
Table: Historical Development of Consent Models for Biospecimen Research
| Time Period | Primary Consent Models | Key Regulatory/Ethical Developments |
|---|---|---|
| Pre-2018 Common Rule | Study-specific consent or waiver of consent | Common Rule adoption (1991), National Bioethics Advisory Commission Report (1999) |
| 2018 Common Rule Revisions | Study-specific consent, waiver of consent, or broad consent | Introduction of broad consent for storage/maintenance of identifiable information/biospecimens [126] |
| Contemporary Era | Study-specific consent, waiver, broad consent, and dynamic consent | GDPR implementation (2018), Precision medicine advances, Digital health platforms [128] [129] |
Broad Consent: Regulatory Framework and Implementation
Definition and Regulatory Authority
Broad consent is defined as a regulatory mechanism under the revised Common Rule (45 CFR §46.116(d)) for obtaining prospective consent for the storage, maintenance, and secondary research use of identifiable private information or identifiable biospecimens [126]. This consent model is specifically tailored for biomedical researchers who anticipate future research uses of collected materials but cannot specify the exact nature of that research at the time of collection [130].
The scope of broad consent is explicitly limited to secondary research with identifiable materials. Key definitions essential to understanding its application include:
- Secondary research: Re-using identifiable information and identifiable biospecimens collected for other "primary" or "initial" activities, such as medical records, leftover tissue from pathology repositories, or excess blood drawn for clinical purposes [130].
- Identifiable private information: Information about which the subject has a reasonable expectation of privacy and from which identity can be readily ascertained [126].
- Identifiable biospecimen: A biospecimen for which the identity of the subject is or may readily be ascertained by the investigator or associated with the biospecimen [130].
Core Elements and Requirements
Broad consent must include most standard elements of informed consent while incorporating several unique components specific to future research use. The mandatory elements, which cannot be omitted or altered as each is considered essential, are detailed below [126] [130].
Table: Required Elements for Broad Consent Documentation
| Element Category | Specific Requirements |
|---|---|
| Basic Informed Consent Elements | Description of reasonably foreseeable risks or discomforts; description of any benefits to subject or others; statement describing confidentiality protections; statement that participation is voluntary [126] |
| Unique Broad Consent Elements | General description of types of research that may be conducted; description of identifiable information/biospecimens that might be used; whether sharing might occur; types of institutions/researchers that might conduct research [126] [130] |
| Temporal Elements | Description of how long information/biospecimens may be stored and used (may be indefinite) [126] |
| Communication Elements | Statement that subjects will or will not be informed of subsequent research details; statement that research results will or will not be disclosed to subjects [126] |
| Additional Conditional Elements | If appropriate: statement about potential commercial profit and whether subject will share; for biospecimen research: whether it will or might include whole genome sequencing [126] [130] |
Implementation Protocols and IRB Considerations
Successful implementation of broad consent requires careful planning and documentation. Researchers must submit separate IRB proposals for the primary research and for the broad consent process, using different consent forms to prevent participant confusion [130]. The IRB plays a critical role in maintaining records of which subjects provided or declined broad consent, creating a reference for future secondary research proposals [130].
The Common Rule specifies exempt research categories related to broad consent. Research involving the collection of identifiable private information or identifiable biospecimens for secondary research may be exempt under Categories 7 and 8 if broad consent is appropriately obtained and documented [126]. The IRB must conduct a limited review to ensure specific criteria are met, including that the research could not practicably be carried out without the identifiable information/biospecimens [126].
Dynamic Consent: Digital Framework and Applications
Conceptual Foundation and Technological Implementation
Dynamic consent represents a paradigm shift from static, one-time consent to an ongoing, interactive process enabled by digital platforms. This model allows research participants to provide, withdraw, or modify their consent preferences in real-time through online portals or mobile applications [128]. Unlike traditional consent models, dynamic consent establishes a two-way communication channel between researchers and participants, facilitating continuous engagement throughout the research lifecycle [129].
The technological infrastructure for dynamic consent typically includes secure web-based platforms with authentication mechanisms, preference management interfaces, audit trail capabilities, and communication tools for updates and notifications [128] [129]. These platforms align with General Data Protection Regulation (GDPR) principles by enhancing transparency, enabling easier exercise of data subject rights, and ensuring that data processing activities remain lawful and fair through real-time updates [128].
Experimental Protocol: MyHealthHub Case Study
A recent study examining dynamic consent implementation provides valuable insights into practical application and user experience. The MyHealthHub application was developed as a dynamic consent platform to facilitate personalized health data sharing and consent management [129].
Methodology:
- Participant Recruitment: 30 adults aged 18+ from South Korea with interest/experience in digital health services
- Platform Features: Consent management, data sharing history monitoring, personalized options for data usage scope
- Study Tasks: Eight primary tasks exploring dynamic consent principles including providing consent, monitoring consent history, and managing personalized options
- Assessment Methods: Combination of multiple-choice and open-ended questionnaire items based on Technology Acceptance Model (TAM) focusing on perceived ease of use, perceived usefulness, and intention to use [129]
Key Findings: The study demonstrated high task completion rates without assistance, with participants responding favorably to personalized options that allowed them to specify sharing preferences according to institutions and data types, conditions for automatic consent, and communication preferences [129]. While participants acknowledged perceived usefulness and ease of use, concerns were raised regarding security and reliability of the digital consent system, highlighting the need for robust authentication mechanisms [129].
Advantages and Implementation Challenges
Dynamic consent offers several significant advantages over traditional models, including enhanced participant engagement through active collaboration, improved data governance with digital audit trails, and flexibility for evolving research needs without additional paperwork [128]. The model also strengthens ethical foundations by respecting the principle of data sovereignty, ensuring individuals maintain control over their personal health data [129].
Implementation challenges include technological barriers requiring investment in secure, user-friendly platforms; the digital divide potentially excluding those with limited technological access or literacy; and regulatory complexity in navigating varying international data protection laws in cross-border research [128]. Successful implementation requires careful attention to participant education, interdisciplinary collaboration with ethics committees and patient advocates, and continuous system evaluation [128].
Comparative Analysis and Research Applications
Model Selection Framework
Choosing between consent models requires careful consideration of research objectives, participant population, and regulatory context. The following table provides a comparative analysis to guide researchers in selecting appropriate consent frameworks for specific research scenarios.
Table: Consent Model Selection Guide for Research Scenarios
| Research Scenario | Recommended Model | Rationale | Implementation Considerations |
|---|---|---|---|
| Prospective biospecimen collection with anticipated secondary use | Broad Consent | Complies with Common Rule requirements for storage of identifiable materials; efficient for biobanking [126] [130] | Must obtain separate IRB approval; maintain detailed records of consent/declination [130] |
| Longitudinal studies with evolving protocols | Dynamic Consent | Accommodates protocol changes without reconsent paperwork; maintains participant engagement [128] [129] | Requires technology infrastructure; must address digital divide concerns [128] |
| Minimal risk research using existing data | Waiver of Consent with Notification | Ethical principle of respect for persons; promotes trust despite waived consent requirement [37] | Notification should be default; consider letters, emails, posters based on context [37] |
| Genomic research with whole genome sequencing | Broad Consent with specific genomic disclosures | Common Rule requires disclosure of WGS; addresses elevated re-identification risks [127] | Must include appropriate WGS statements; consider future data sharing implications [127] |
Integration in Precision Medicine and Pharmacovigilance
Emerging fields such as precision medicine and advanced pharmacovigilance present unique consent challenges that these models can address. Precision pharmacovigilance requires monitoring drug safety in the context of highly individualized treatments, creating needs for flexible consent approaches that accommodate evolving safety protocols and data sharing requirements [131]. The NIH Genomic Data Sharing Policy emphasizes the importance of obtaining consent for future research use and broad data sharing, particularly for large-scale genomic data generation [127].
In cell and gene therapy research, where long-term follow-up is essential for safety monitoring, dynamic consent offers advantages for maintaining participant engagement over extended periods and adapting to emerging safety information [132]. These therapies present unique safety challenges including prolonged biological activity, immune complications, and potential genotoxicity that require ongoing communication with participants [132].
Research Reagent Solutions for Consent Implementation
Table: Essential Tools and Resources for Consent Implementation
| Tool Category | Specific Solutions | Application & Function |
|---|---|---|
| Digital Consent Platforms | MyHealthHub, PEER Platform, RUDY Study System | Enable dynamic consent management; provide participant interfaces for preference management; maintain audit trails [128] [129] |
| IRB Documentation Templates | Broad consent templates, Waiver justification worksheets | Standardize consent documentation; ensure regulatory compliance; facilitate IRB review [133] [130] |
| Participant Education Resources | Teach-back method tools, Graphical risk communication aids, Health literacy assessment tools | Enhance participant comprehension; assess understanding; facilitate informed decision-making [13] |
| Security & Authentication Tools | Secure authentication mechanisms, Encryption protocols, Access control systems | Protect participant data; ensure system reliability; maintain privacy [129] |
The evolving landscape of informed consent reflects broader transformations in biomedical research, particularly in biospecimen science and data-intensive methodologies. Broad consent and dynamic consent represent complementary approaches addressing different aspects of contemporary research ethics—broad consent providing a regulatory framework for future use of biological materials, and dynamic consent offering a technological solution for ongoing participant engagement and autonomy.
For researchers and drug development professionals, understanding these models is essential for ethical protocol design and regulatory compliance. Implementation requires careful consideration of research context, participant populations, and available infrastructure. As precision medicine and advanced therapies continue to evolve, these consent frameworks will play increasingly important roles in balancing research innovation with robust participant protections, ultimately supporting the advancement of science while respecting individual autonomy and rights.
Conclusion
Informed consent has evolved from a rudimentary signature into a dynamic, communicative process central to ethical clinical research. Its successful implementation requires a deep understanding of its ethical justifications, a meticulous application of complex regulatory requirements, and proactive strategies to address practical challenges. For researchers and drug developers, the future will be shaped by technological innovation, particularly in digitalization and AI, which promise to enhance understanding and accessibility. However, these tools must be implemented with careful oversight to ensure reliability and uphold the core principles of respect for persons, beneficence, and justice. The continued refinement of informed consent processes is not merely a regulatory obligation but a fundamental commitment to fostering trust, ensuring participant safety, and advancing ethical scientific progress.
References
- 1. Clinicians' experiences of obtaining informed consent for ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-024-01119-8]
- 2. Chapter Two: Eminence-Based Medicine [http://www.nephjc.com/news/2016/7/17/chapter-two-eminence-based-medicine]
- 3. The Physician's Oath: Historical Perspectives - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5755201/]
- 4. Informed consent: Past and present - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3601698/]
- 5. Beyond Medical Paternalism: Restoring Control to the ... [https://www.cato.org/free-society/spring-2025/beyond-medical-paternalism-restoring-control-individual]
- 6. New Informed Consent Expectations Should Aid ... [https://acrpnet.org/2024/11/21/new-informed-consent-expectations-should-aid-participants-understanding-may-catch-professionals-off-guard]
- 7. Enhancing Informed Consent Forms for Medical Devices [https://pmc.ncbi.nlm.nih.gov/articles/PMC12311233/]
- 8. Schloendorff v. Society of New York Hospital [https://en.wikipedia.org/wiki/Schloendorff_v._Society_of_New_York_Hospital]
- 9. Schloendorff v. New York Hospital – Case Brief Summary [https://www.studicata.com/case-briefs/case/schloendorff-v-new-york-hospital]
- 10. Schoendorff v. Society of New York Hosp., 105 N.E. 92, 93 ... [https://biotech.law.lsu.edu/cases/consent/schoendorff.htm]
- 11. Informed Consent - Holland-Frei Cancer Medicine - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK12636/]
- 12. A Modern History of Informed Consent and the Role of Key ... [https://www.ochsnerjournal.org/content/21/1/81]
- 13. Informed Consent - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK430827/]
- 14. A Modern History of Informed Consent and the Role of Key ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7993430/]
- 15. Nuremberg Code [https://en.wikipedia.org/wiki/Nuremberg_Code]
- 16. WMA Declaration of Helsinki – Ethical Principles for ... [https://www.wma.net/policies-post/wma-declaration-of-helsinki/]
- 17. Declaration of Helsinki – WMA [https://www.wma.net/what-we-do/medical-ethics/declaration-of-helsinki/]
- 18. Nuremberg Code - UNC Research [https://research.unc.edu/human-research-ethics/resources/ccm3_019064/]
- 19. The driving forces of research ethics in academia [https://pmc.ncbi.nlm.nih.gov/articles/PMC12576985/]
- 20. About The Untreated Syphilis Study at Tuskegee [https://www.cdc.gov/tuskegee/about/index.html]
- 21. Tuskegee Syphilis Study - Wikipedia [https://en.wikipedia.org/wiki/Tuskegee_Syphilis_Study]
- 22. Fiftieth Anniversary of Uncovering the Tuskegee Syphilis Study: The Story and Timeless Lessons - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9872801/]
- 23. Tuskegee syphilis study | US Government Experiment, African American Impact | Britannica [https://www.britannica.com/event/Tuskegee-syphilis-study]
- 24. Revisionist Accounts of the Tuskegee Syphilis Study and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4568718/]
- 25. Guiding Principles for Ethical Research [https://www.nih.gov/health-information/nih-clinical-research-trials-you/guiding-principles-ethical-research]
- 26. Clinical Trials Guidance Documents [https://www.fda.gov/science-research/clinical-trials-and-human-subject-protection/clinical-trials-guidance-documents]
- 27. Conducting Clinical Trials With Decentralized Elements [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/conducting-clinical-trials-decentralized-elements]
- 28. IFAPP International Ethics Framework - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12245974/]
- 29. Principles of Clinical Ethics and Their Application to Practice [https://pmc.ncbi.nlm.nih.gov/articles/PMC7923912/]
- 30. Ethical Principles [https://www.cdc.gov/niosh/learning/safetyculturehc/module-5/11.html]
- 31. The Four Scientific Ethical Principles [https://researchethics.dk/research-ethics-themes/the-four-scientific-ethical-principles]
- 32. Basic Ethical Principles [https://www.stmarys-ca.edu/academic-affairs/faculty-governance/institutional-review-board/basic-ethical-principles]
- 33. Advancing Patient-Centered Informed Consent in Clinical ... [https://www.ciscrp.org/from-compliance-to-comprehension-advancing-patient-centered-informed-consent-in-clinical-research]
- 34. SPIRIT 2025 statement: Updated guideline for protocols of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037212/]
- 35. Digitalizing informed consent in healthcare: a scoping review [https://pmc.ncbi.nlm.nih.gov/articles/PMC12225439/]
- 36. Informed Consent, Redefined: How AI and Big Data Are ... [https://petrieflom.law.harvard.edu/2025/04/11/informed-consent-redefined-how-ai-and-big-data-are-changing-the-rules/]
- 37. April 22, 2025: New Report Highlights Value of Informing ... [https://rethinkingclinicaltrials.org/news/april-22-2025-new-report-highlights-value-of-informing-participants-about-research-conducted-under-a-waiver-of-consent/]
- 38. Protecting Human Research Subjects: The Past Defines the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3127481/]
- 39. Code of Federal Regulations | Social Science Research Institute [https://ssri.psu.edu/clinicalresearchguidebook/federal-laws-governing-clinical-research-code-federal-regulations]
- 40. Current Federal Regulatory Framework: Common Rule, ... [https://rethinkingclinicaltrials.org/chapters/ethics-and-regulatory/special-privacy-considerations/current-federal-regulatory-framework-common-rule-fda-and-hipaa/]
- 41. Institutional Review Boards Frequently Asked Questions [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/institutional-review-boards-frequently-asked-questions]
- 42. 21 CFR Part 50 -- Protection of Human Subjects [https://www.ecfr.gov/current/title-21/chapter-I/subchapter-A/part-50]
- 43. Comparison of FDA and HHS Human Subject Protection ... [https://www.fda.gov/science-research/good-clinical-practice-educational-materials/comparison-fda-and-hhs-human-subject-protection-regulations]
- 44. 45 CFR 46.116 -- General requirements for informed consent. [https://www.ecfr.gov/current/title-45/subtitle-A/subchapter-A/part-46/subpart-A/section-46.116]
- 45. Protection of Human Subjects; Informed Consent [https://www.fda.gov/science-research/clinical-trials-and-human-subject-protection/protection-human-subjects-informed-consent]
- 46. What You Should Know About FDA Final Informed Consent ... [https://www.wcgclinical.com/insights/what-you-should-know-about-fda-final-informed-consent-guidance/]
- 47. 21 CFR 50.25 -- Elements of informed consent. [https://www.ecfr.gov/current/title-21/chapter-I/subchapter-A/part-50/subpart-B/section-50.25]
- 48. The Requirements for Informed Consent (Series #1) [https://www.tc.columbia.edu/institutional-review-board/irb-blog/2025/informed-consent-the-requirements-for-informed-consent-series-1/]
- 49. Factors Influencing Informed Consent Preferences in ... [https://www.jmir.org/2025/1/e63349/]
- 50. The Performance of the Surrogate Informed Consent ... [https://pubmed.ncbi.nlm.nih.gov/40484371/]
- 51. Comprehensive Guide to Informed Consent in Research [https://www.infonetica.net/articles/Informed-Consent-in-Research]
- 52. ICH E6(R3) Explained: A Guide to the 2025 GCP Update [https://intuitionlabs.ai/articles/ich-e6-r3-gcp-guidelines-2025]
- 53. Regulatory Updates in Clinical Trials: What's New [https://realtime-eclinical.com/2025/01/14/regulatory-updates-in-clinical-trials-whats-new/]
- 54. Informed Consent and the Revised Common Rule [https://bioethics.hms.harvard.edu/journal/consent-common-rule]
- 55. Informed Consent Process: Foundation of the Researcher ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5527718/]
- 56. Drafting the Informed Consent Form - UCI Office of Research [https://research.uci.edu/human-research-protections/subject-enrollment/informed-consent/drafting-the-informed-consent-form/]
- 57. Assent Process (Children under 18 years of age) | University of Kentucky Research [https://www.research.uky.edu/office-research-integrity/assent-process-children-under-18-years-age]
- 58. Assent - Under Age 18 | Office of Human Research Protections | West Virginia University [https://human.research.wvu.edu/guidance/informed-consent/assent-under-age-18]
- 59. eCFR :: 45 CFR 46.408 -- Requirements for permission by parents or guardians and for assent by children. [https://www.ecfr.gov/current/title-45/subtitle-A/subchapter-A/part-46/subpart-D/section-46.408]
- 60. 21 CFR Part 50 Subpart B -- Informed Consent of Human ... [https://www.ecfr.gov/current/title-21/chapter-I/subchapter-A/part-50/subpart-B]
- 61. Consent Requirements - NCATS Toolkit - NIH [https://toolkit.ncats.nih.gov/module/prepare-for-clinical-trials/giving-input-on-the-informed-consent-process/consent-requirements/]
- 62. Broad Consent in Healthcare Research: What Is Efficient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12335335/]
- 63. Replacing Paper Informed Consent with Electronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7233043/]
- 64. Electronic signature vs informed consent: what's the legal ... [https://i-agree.io/blog/electronic-signature-vs-informed-consent-whats-the-legal-difference]
- 65. Understanding Success Criterion 1.4.3: Contrast (Minimum) [https://www.w3.org/WAI/WCAG21/Understanding/contrast-minimum.html]
- 66. Text has minimum contrast[proposed] | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/afw4f7/proposed/]
- 67. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 68. Institutional Review Board Waiver or Alteration of Informed ... [https://www.federalregister.gov/documents/2023/12/21/2023-27935/institutional-review-board-waiver-or-alteration-of-informed-consent-for-minimal-risk-clinical]
- 69. FDA Final Rule - Waiver or Alteration of Informed Consent ... [https://thehrpconsultinggroup.com/fda-final-rule-waiver-or-alteration-of-informed-consent-for-minimal-risk-clinical-investigations/]
- 70. Verbal consent in biomedical research: moving toward a ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1472655/full]
- 71. Strategies for overcoming language barriers in healthcare - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8697718/]
- 72. Health Literacy and Adherence to Medical Treatment in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4912447/]
- 73. The Impact of Language Barriers on Documentation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2078548/]
- 74. Construction and practice of a novel pharmaceutical health ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0311841]
- 75. Communication Strategies for Nurse–Patient Language ... [https://www.ons.org/publications-research/voice/news-views/05-2025/communication-strategies-nurse-patient-language]
- 76. Addressing Low Health Literacy and Limited English ... [https://www.aap.org/en/practice-management/providing-patient--and-family-centered-care/addressing-low-health-literacy-and-limited-english-proficiency/?srsltid=AfmBOop0U0PapSfLxqOXRtFaJl8jNK8aCIkPrX2tHxJyU79RgVFeddGk]
- 77. promoting organizational health literacy to improve ... [https://www.sciencedirect.com/science/article/abs/pii/S1551741125004218]
- 78. Language Barriers in Clinical Trials Participation [https://trialx.com/language-barriers-in-clinical-trials-participation-can-innovation-bridge-the-gaps-improve-diversity/]
- 79. Best Practices for Handling Informed Consent in ... [https://acrpnet.org/2024/12/13/best-practices-for-handling-informed-consent-in-emergency-medical-cases]
- 80. The reality of informed consent: empirical studies on patient ... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-020-04969-w]
- 81. 2025 FDAAA 801 Final Rule Changes Impacting Clinical ... [https://prorelixresearch.com/2025-fdaaa-801-clinical-trial-rule-impact/]
- 82. Vulnerable population and methods for their safeguard [https://pmc.ncbi.nlm.nih.gov/articles/PMC3601707/]
- 83. Beecher's Bombshell and the Complicated History of ... [https://www.facs.org/for-medical-professionals/news-publications/news-and-articles/bulletin/2022/04/beechers-bombshell-and-the-complicated-history-of-informed-consent/]
- 84. Vulnerability in Research: Basic Ethical Concepts and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7122263/]
- 85. Safeguarding in adolescent mental health research [https://pmc.ncbi.nlm.nih.gov/articles/PMC10910574/]
- 86. Online research with vulnerable populations [https://researchmethodscommunity.sagepub.com/blog/online-research-vulnerable-populations]
- 87. Safeguarding International Science: A Research Security ... [https://www.nist.gov/adlp/research-security-office/safeguarding-international-science-research-security-framework]
- 88. Using Deception and Incomplete Disclosure in Research [https://www.tamuk.edu/ori/research-compliance/IRB/Deception-and-Incomplete-Disclosure-in-Research.html]
- 89. Deception and Incomplete Disclosure - Office of Research ... [https://umaine.edu/research-compliance/human-subjects/deception-and-incomplete-disclosure/]
- 90. Incomplete Disclosure and Deception in Research [https://www.seattleu.edu/institutional-review-board-and-office-of-research-oversight/guidance-and-faq/incomplete-disclosure-and-deception-in-research-studies/]
- 91. Deception or incomplete disclosure in research: Guidance [https://research.iu.edu/compliance/human-subjects/guidance/deception.html]
- 92. Research Involving Deception or Withholding of Information [https://research.unc.edu/human-research-ethics/standard-operating-procedures-sops/research-involving-deception-or-withholding-of-information/]
- 93. Digital consent research overview [https://concentric.health/deployment/delivery-playbook/research-summary/]
- 94. Decentralized Clinical Trial Platforms in 2025 - Castor EDC [https://www.castoredc.com/insight-briefs/decentralized-clinical-trial-platforms-in-2025-a-practical-guide-for-clinical-operations/]
- 95. From signatures to success: How digital consent ... [https://pharmaphorum.com/digital/signatures-success-how-digital-consent-accelerates-trials-enhances-compliance-and-engages]
- 96. Artificial intelligence-generated informed patient consent in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12507154/]
- 97. Bridging ethical gaps in digital health research: a framework ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12509369/]
- 98. New study: AI chatbots systematically violate mental health ... [https://www.brown.edu/news/2025-10-21/ai-mental-health-ethics]
- 99. AI Chatbots at the Crossroads: Navigating New Laws and ... [https://www.cooley.com/news/insight/2025/2025-10-21-ai-chatbots-at-the-crossroads-navigating-new-laws-and-compliance-risks]
- 100. Extended discussion of information for informed consent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6483689/]
- 101. Strategies to Enhance Inclusion in Informed Consent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12477491/]
- 102. Worldwide willingness to share health data high but ... [https://www.nature.com/articles/s41746-025-01868-9]
- 103. Improving Consent Processes for Clinical Research Using ... [https://www.pcori.org/research-results/2019/improving-consent-processes-clinical-research-using-public-deliberation-methods]
- 104. Tool: Teach-Back | Agency for Healthcare Research and ... [https://www.ahrq.gov/teamstepps-program/curriculum/communication/tools/teachback.html]
- 105. Development, implementation, and evaluation of Teach Back ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9669070/]
- 106. Clinical Investigator Site Audits: A Guide and Checklist ... [https://www.thefdagroup.com/blog/clinical-trial-investigator-site-audits]
- 107. 2025 Guidelines | State of California - Department of Justice [https://oag.ca.gov/research/guide]
- 108. Updated Requirements for Informed Consent: HHS Issues ... [https://www.healthlawadvisor.com/updated-requirements-for-informed-consent-hhs-issues-new-guidance-on-sensitive-exams]
- 109. Life Sciences Regulatory Outlook 2025: Areas to Watch in ... [https://www.ropesgray.com/en/insights/viewpoints/102jzc4/life-sciences-regulatory-outlook-2025-areas-to-watch-in-the-u-s-eu-uk-and-as]
- 110. Navigating the Shifting U.S. Health Technology Regulatory ... [https://talencio.com/navigating-the-shifting-u-s-health-technology-regulatory-landscape-trends-challenges-and-actionable-solutions/]
- 111. Medical Device Clinical Trials: 2025 FDA Requirements, ... [https://www.complizen.ai/post/medical-device-clinical-trials-complete-guide]
- 112. Informed Consent Requirements for IDE Clinical Investigation [https://biobostonconsulting.com/informed-consent-requirements-for-clinical-investigations-under-ide/]
- 113. FDA Final Rule: IRB Waiver of Informed Consent for ... [https://www.jonesday.com/en/insights/2024/01/fda-final-rule-irb-waiver-of-informed-consent-for-minimalrisk-investigations]
- 114. AI meets informed consent: a new era for clinical trial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11964292/]
- 115. Consent-First AI Turns Trust Into 20% More Engagement in ... [https://completeaitraining.com/news/consent-first-ai-turns-trust-into-20-more-engagement-in-2025/]
- 116. 5 Best AI UX Research Tools in 2025 [https://www.banani.co/blog/best-ai-ux-research-tools]
- 117. AI's Consent Revolution: Boosting Engagement 20% in ... [https://www.webpronews.com/ais-consent-revolution-boosting-engagement-20-in-2025-marketing/]
- 118. IRB Informed Consent - Cornell Research Services [https://researchservices.cornell.edu/resources/irb-informed-consent]
- 119. The State of AI: Global Survey 2025 [https://www.mckinsey.com/capabilities/quantumblack/our-insights/the-state-of-ai]
- 120. AI in Healthcare: Trust, Consent & Compliance [https://www.jimersonfirm.com/blog/2025/11/ai-in-healthcare-trust-consent-and-measuring-effectiveness/]
- 121. Top 10 AI Tools for Research in 2025 [https://avidnote.com/top-10-ai-tools-for-research-in-2025/]
- 122. What Happens If A Doctor Performs A Procedure Without ... [https://www.malmlegal.com/blog/medical-malpractice-lack-of-consent/]
- 123. March 2025 – Center for Informed Consent Integrity [https://ge2p2global-centerforinformedconsentintegrity.org/2025/03/]
- 124. The Performance of the Surrogate Informed Consent ... [https://www.sciencedirect.com/science/article/pii/S0012369225006890]
- 125. Five Data-Informed Principles for Advancing Inclusive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474690/]
- 126. Understanding Broad Consent - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7122261/]
- 127. Federal Regulations and the Ethical Collection of Specimens ... [https://dctd.cancer.gov/research/research-areas/biobanking-biospecimen-science/elsi/federal-regulations]
- 128. Dynamic Consent: A New GDPR Standard for Clinical Trials [https://www.clinicaltrialvanguard.com/article/dynamic-consent-a-new-gdpr-standard-for-clinical-trials/]
- 129. Opportunities and challenges of a dynamic consent-based ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-024-01091-3]
- 130. Broad Consent - Provost's Office [https://www.gettysburg.edu/offices/provost/irb/broad-consent]
- 131. Unveiling the future: precision pharmacovigilance in the era of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11133017/]
- 132. Pharmacovigilance in Cell and Gene Therapy: Evolving ... [https://link.springer.com/article/10.1007/s40264-025-01596-9]
- 133. Biospecimen & Data Research: Informed Consent Requirements [https://irb.wisc.edu/manual/investigator-manual/conducting-human-participant-research/different-types-of-research/biospecimen-and-data-research/biospecimen-data-research-informed-consent-requirements/]