FDA Adverse Event Reporting in Clinical Trials: A Complete Guide for Research Professionals
This comprehensive guide details the FDA's requirements for adverse event (AE) and serious adverse event (SAE) reporting during clinical trials of drugs and biologics.
FDA Adverse Event Reporting in Clinical Trials: A Complete Guide for Research Professionals
Abstract
This comprehensive guide details the FDA's requirements for adverse event (AE) and serious adverse event (SAE) reporting during clinical trials of drugs and biologics. Aimed at researchers, scientists, and drug development professionals, it covers the foundational regulations from 21 CFR, step-by-step methodological workflows for detection, documentation, and submission, common pitfalls and optimization strategies for compliance, and a comparative analysis of global regulatory frameworks. The article synthesizes current FDA guidance, including electronic submission mandates (ESG), to provide a practical resource for ensuring rigorous safety monitoring and regulatory compliance throughout the drug development lifecycle.
Understanding the FDA's Regulatory Framework for Clinical Trial Safety
Thesis Context: This technical guide defines the core terms governing safety reporting in clinical trials, which are foundational for compliance with U.S. Food and Drug Administration (FDA) regulations under 21 CFR Parts 312 and 812. Accurate identification, classification, and reporting of these events are critical for protecting human subjects and evaluating the risk-benefit profile of investigational products.
Core Definitions and Regulatory Framework
The FDA's oversight of clinical trial safety is predicated on precise definitions. These terms form the lexicon for all safety data collection and regulatory communication.
- Adverse Event (AE): Any untoward medical occurrence in a patient or clinical investigation subject administered a pharmaceutical product, which does not necessarily have a causal relationship with this treatment. An AE can therefore be any unfavorable and unintended sign (including an abnormal laboratory finding), symptom, or disease temporally associated with the use of a medical (investigational) product, whether or not considered related to the product.
- Serious Adverse Event (SAE): An adverse event is considered "serious" if it results in any of the following outcomes:
- Death
- Life-threatening adverse experience
- Inpatient hospitalization or prolongation of existing hospitalization
- Persistent or significant disability/incapacity
- Congenital anomaly/birth defect
- Other important medical events that may not result in death, be life-threatening, or require hospitalization may be considered serious when, based upon appropriate medical judgment, they may jeopardize the subject and may require medical or surgical intervention to prevent one of the outcomes listed above.
- Suspected Adverse Reaction: For drugs and biologics, any adverse event for which there is a reasonable possibility that the drug caused the event. "Reasonable possibility" means there is evidence to suggest a causal relationship. In the context of an investigational new drug application (IND), this is synonymous with "suspected serious adverse reaction" (SSAR) when the event is serious.
The classification of an event directly mandates specific reporting timelines to the FDA and other stakeholders.
Table 1: FDA Reporting Requirements for Investigational New Drugs (INDs)
| Term | Definitional Criteria | Sponsor Reporting Timeline to FDA (Fatal/Life-Threatening) | Sponsor Reporting Timeline to FDA (Other Serious/Expected) | Sponsor Reporting to Investigators |
|---|---|---|---|---|
| Adverse Event (AE) | Any untoward medical occurrence. | Not applicable as a standalone category. | Not applicable as a standalone category. | Reported per protocol and monitoring plan. |
| Serious Adverse Event (SAE) | Meets seriousness criteria (death, hospitalization, etc.). | 7-Day (Express) Report: Within 7 calendar days of sponsor's knowledge. | 15-Day Report: Within 15 calendar days of sponsor's knowledge. | Informed promptly; updated information provided. |
| Suspected Adverse Reaction (SAR) | AE with reasonable possibility of causal relationship to drug. | 7-Day (Express) Report. | 15-Day Report. | Informed promptly. |
| Unexpected | Not listed in the Investigator's Brochure or is not listed at the specificity or severity observed. | 7-Day Report (if also serious and suspected). | 15-Day Report (if also serious and suspected). | Informed promptly. |
Table 2: Common AE Assessment Scales
| Scale Name | Purpose | Key Grading Categories (Simplified) |
|---|---|---|
| CTCAE (Common Terminology Criteria for Adverse Events) | Standardized grading of severity of AEs in oncology trials. | Grade 1: Mild; Grade 2: Moderate; Grade 3: Severe; Grade 4: Life-threatening; Grade 5: Death. |
| FDA/ICH Intensity Scale | General grading of AE intensity. | Mild, Moderate, Severe. |
| Naranjo Algorithm | Systematic causality assessment. | Scores range from -4 to +13, categorizing causality as Doubtful, Possible, Probable, or Definite. |
Experimental Protocol: Standardized Causality Assessment Workflow
A critical methodological step in differentiating an AE from a Suspected Adverse Reaction is causality assessment.
Protocol Title: Application of the Naranjo Algorithm for Systematic Causality Assessment of Adverse Drug Reactions.
Objective: To provide a reproducible, standardized method for determining the likelihood of a causal relationship between an investigational product and an observed adverse event.
Materials (The Scientist's Toolkit):
| Research Reagent / Tool | Function in Causality Assessment |
|---|---|
| Structured Case Narrative | A chronologically ordered, detailed summary of the subject's clinical course, including dosing timelines, event onset/offset, and concomitant therapies. |
| Naranjo Algorithm Questionnaire | A validated tool consisting of 10 objective questions with weighted scores. |
| Investigator's Brochure (IB) / Prescribing Information | The definitive source for known pharmacology, toxicology, and previously observed adverse reactions to the product. |
| De-challenge & Re-challenge Data | Documentation of the event's outcome after stopping the drug (de-challenge) and, if available and ethical, after re-starting it (re-challenge). |
| Subject's Medical & Medication History | Contextual data to identify alternative causes (e.g., underlying disease, other drugs). |
| Literature & Safety Database Searches | Tools to identify if the event has been previously reported for the drug or drug class. |
Methodology:
- AE Documentation: Ensure the AE is fully documented with onset date, description, severity, duration, actions taken, and outcome.
- Data Compilation: Gather all relevant materials listed above, particularly the structured case narrative.
- Naranjo Questionnaire Application: Answer each of the 10 questions based solely on available evidence:
- Are there previous conclusive reports on this reaction? (+1)
- Did the adverse event appear after the suspected drug was administered? (+2)
- Did the adverse reaction improve when the drug was discontinued or a specific antagonist was administered? (+1)
- Did the adverse reaction reappear when the drug was re-administered? (+2)
- Are there alternative causes that could on their own have caused the reaction? (-1)
- Did the reaction reappear when a placebo was given? (-1)
- Was the drug detected in blood or other fluids in concentrations known to be toxic? (+1)
- Was the reaction more severe when the dose was increased, or less severe when the dose was decreased? (+1)
- Did the patient have a similar reaction to the same or similar drugs in any previous exposure? (+1)
- Was the adverse event confirmed by any objective evidence? (+1)
- Scoring & Classification: Sum the total score.
- ≥ 9: Definite
- 5-8: Probable
- 1-4: Possible
- ≤ 0: Doubtful
- Determination: A score of "Possible" or higher ("Probable"/"Definite") typically provides the "reasonable possibility" needed to classify the event as a Suspected Adverse Reaction.
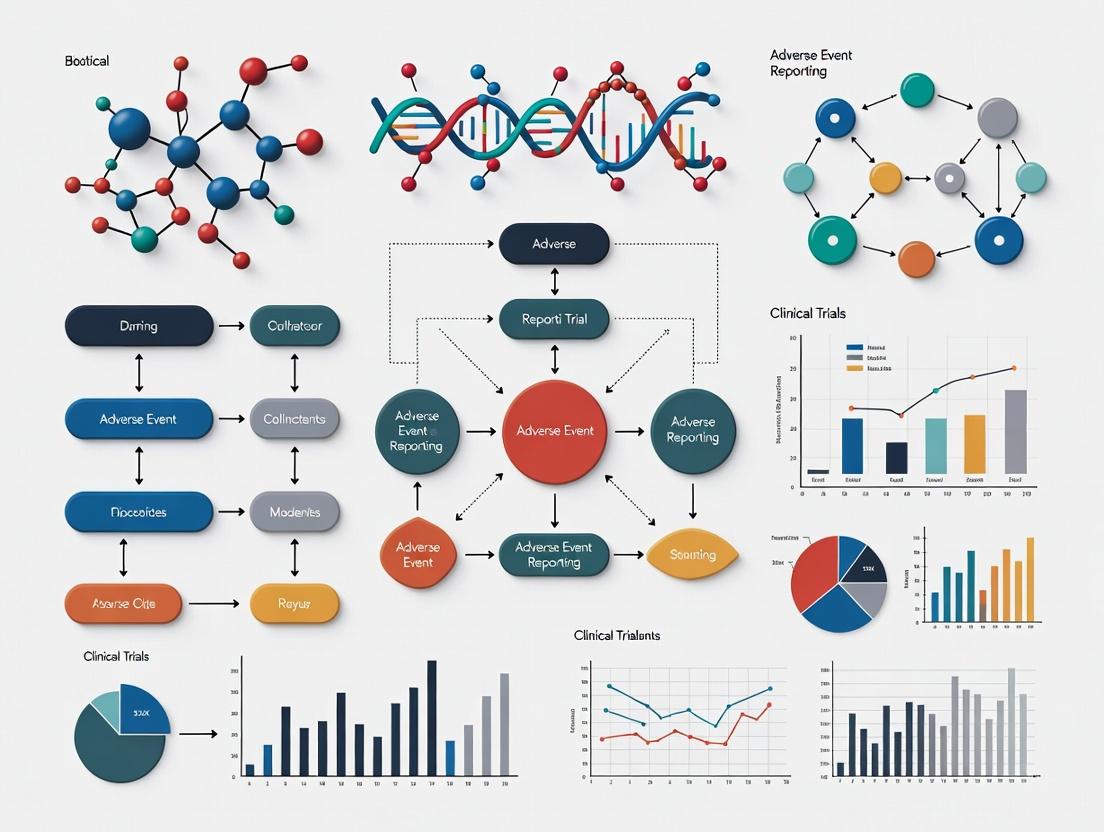
Visualizing the Adverse Event Assessment and Reporting Pathway
Title: AE Classification and Reporting Decision Pathway
Title: Inputs for Systematic Causality Assessment
This whitepaper details the legal and regulatory framework governing the investigation, approval, and post-marketing surveillance of drugs and biological products in the United States. Framed within the context of FDA adverse event reporting requirements for clinical trials research, it elucidates the specific regulations under 21 CFR Parts 312 (Investigational New Drug Application), 314 (Applications for FDA Approval to Market a New Drug), and 600 (Biological Products: General). These regulations collectively establish the lifecycle of product development, from first-in-human studies through post-approval monitoring, with rigorous safety reporting as a continuous thread.
Core Regulatory Provisions and Quantitative Requirements
The following tables summarize the key provisions and quantitative data thresholds for adverse event reporting mandated by these regulations.
Table 1: Key Adverse Event Reporting Requirements in Clinical Development (21 CFR Part 312)
| Requirement | Description | Reporting Timeline |
|---|---|---|
| IND Safety Reports (312.32) | Reporting of serious, unexpected suspected adverse reactions (SUSARs) and findings from other studies. | Sponsor to FDA: Within 15 calendar days for fatal/life-threatening; otherwise within 15 days. |
| Annual Reports (312.33) | Summary of the past year's investigational experience, including individual study information and safety data aggregate. | Within 60 days of the anniversary date the IND went into effect. |
| Investigator's Brochure Updates | Inclusion of new safety information that may affect the risk-benefit assessment of the investigation. | As new significant information becomes available, per 312.55. |
Table 2: Post-Marketing Safety Reporting Requirements (21 CFR Parts 314 & 600)
| Requirement (CFR Citation) | Product Scope | Description | Reporting Timeline |
|---|---|---|---|
| 15-Day Alert Reports (314.80(c), 600.80(c)) | Drugs & Biologics | Domestic and foreign reports of serious, unexpected adverse drug experiences. | Applicant to FDA: Within 15 calendar days of initial receipt. |
| Periodic Adverse Experience Reports (PAERs) (314.80(c)(2), 600.80(c)(2)) | Drugs & Biologics | Quarterly for first 3 years post-approval, then annually. Includes a summary of all adverse experiences and a history of actions taken. | Quarterly reports within 30 days of close of quarter; annual reports within 60 days of anniversary date. |
| Postmarketing Study Commitments (314.81, 600.91) | Drugs & Biologics | Progress reports on required postmarketing studies (e.g., Phase 4 trials, safety studies). | Annual report submission. |
Experimental Protocols for Pharmacovigilance Signal Detection
Robust pharmacovigilance during clinical trials and post-marketing relies on systematic methodologies to detect and evaluate safety signals.
Protocol 1: Disproportionality Analysis for Safety Signal Detection
Objective: To quantitatively identify potential safety signals by comparing the reporting frequency of a specific adverse event (AE) for a given drug against its reporting frequency for all other drugs in a database. Methodology:
- Data Source: Utilize a spontaneous reporting system database (e.g., FDA Adverse Event Reporting System - FAERS).
- Case Selection: Extract all reports for the drug of interest (Drug X) and for a comparator set (all other drugs).
- Contingency Table Creation: Construct a 2x2 table for a specific AE (e.g., hepatic failure):
- a = Reports of Drug X with the AE.
- b = Reports of Drug X with all other AEs.
- c = Reports of all other drugs with the AE.
- d = Reports of all other drugs with all other AEs.
- Statistical Calculation: Compute the Reporting Odds Ratio (ROR) and its 95% confidence interval (CI).
- ROR = (a/b) / (c/d) = (a*d) / (b*c)
- Signal Threshold: A signal is considered if the lower bound of the 95% CI for the ROR is >1.0 and a minimum number of cases (e.g., a ≥ 3) is met.
Protocol 2: Cohort Event Monitoring in a Phase IV Study
Objective: To prospectively quantify the incidence of predefined adverse events of special interest (AESIs) in a large population using a newly approved biologic. Methodology:
- Study Design: Prospective, observational cohort study mandated under 21 CFR 314.81/600.91 as a post-marketing requirement.
- Population: Patients prescribed the biologic in routine clinical practice. Enrollment target: 10,000 patients.
- Data Collection: Follow-up via healthcare provider surveys and patient questionnaires at Months 1, 6, and 12 post-initiation.
- Endpoint Adjudication: A blinded, independent Clinical Endpoint Committee (CEC) reviews all potential AESI cases against pre-specified criteria.
- Analysis: Calculate incidence rates (per 1000 patient-years) with 95% CIs for each AESI. Compare, if applicable, to a matched comparator cohort from a healthcare claims database using Cox proportional hazards models.
Regulatory Workflow Visualization
Diagram Title: Regulatory Pathway & Continuous Safety Reporting Workflow
The Scientist's Toolkit: Key Research Reagent Solutions for Immunogenicity Assays
Immunogenicity testing for biologics is critical for safety assessment under 21 CFR Part 600. The following table outlines essential reagents.
Table 3: Essential Reagents for Anti-Drug Antibody (ADA) Assay Development
| Reagent | Function in ADA Assay | Criticality |
|---|---|---|
| Drug Product (Biotherapeutic) | Serves as the capture and/or detection antigen for ADA binding. | High (Core assay component) |
| Positive Control Antibody | High-affinity antibody (polyclonal or monoclonal) against the drug. Used for assay development, validation, and run acceptance. | High (Assay qualification) |
| Labeled Detection Reagent | Enzyme (e.g., HRP), fluorescent, or chemiluminescent conjugate of the drug or anti-species antibody for signal generation. | High (Signal detection) |
| Blocking Buffer & Assay Diluent | Minimizes non-specific binding; often contains animal sera, irrelevant proteins, or proprietary polymers. | High (Assay performance) |
| Critical Reagents from Qualified Banks | Pre-qualified, consistently sourced reagents (e.g., cell lines for neutralization assays) to ensure long-term assay robustness. | Medium-High (Assay consistency) |
| Pre-Existing ADA/Serum Panels | Characterized human serum samples with known ADA status for cut-point determination and validation. | Medium (Statistical validation) |
The U.S. Food and Drug Administration (FDA) mandates stringent safety oversight in clinical trials to protect human subjects and ensure data integrity. This oversight is a collaborative triad between the Sponsor, the Investigator, and the Institutional Review Board (IRB), each with distinct, codified responsibilities under FDA regulations (21 CFR Parts 312 and 812). The effective execution of these roles is critical for compliance with FDA adverse event (AE) and serious adverse event (SAE) reporting requirements, forming the operational backbone of patient safety in clinical research.
Defining the Core Entities and Their Regulatory Mandates
The Sponsor
The sponsor, typically a pharmaceutical company, medical device manufacturer, or organization, initiates and funds the clinical trial. The sponsor holds the Investigational New Drug (IND) or Investigational Device Exemption (IDE) application and bears ultimate responsibility for the trial's conduct.
- Primary Safety Responsibilities:
- Development of Safety Protocols: Design the trial protocol, including safety monitoring plans, stopping rules, and data safety monitoring boards (DSMBs).
- Safety Reporting to FDA: Submit IND/IDE safety reports for serious and unexpected suspected adverse reactions (SUSARs) within 15 calendar days (or 7 days for fatal/life-threatening events).
- Investigator Notification: Promptly inform all participating investigators of new, important safety information.
- Safety Review: Continuously monitor and evaluate all safety data from all investigational sites.
- Auditing & Compliance: Ensure investigator compliance with the protocol and regulations through monitoring and auditing.
The Investigator
The investigator is the individual (e.g., a physician) who conducts the clinical trial at a study site and has direct, professional responsibility for the trial subjects.
- Primary Safety Responsibilities:
- Subject Protection & Informed Consent: Ensure patient safety and obtain legally effective informed consent, including a discussion of potential risks.
- AE/SAE Identification & Assessment: Promptly identify, diagnose, and document all AEs and SAEs occurring at the site.
- Reporting to the Sponsor: Report all SAEs and protocol-specified AEs to the sponsor within the timeframe specified in the protocol (typically 24 hours for SAEs).
- Protocol Adherence: Conduct the trial in strict compliance with the protocol to minimize risk.
- Reporting to the IRB: Submit all required documents, including SAEs and protocol modifications, for IRB review and approval.
The Institutional Review Board (IRB)
The IRB is an independent administrative body established to protect the rights and welfare of human research subjects.
- Primary Safety Responsibilities:
- Initial Review & Approval: Review and approve the protocol, informed consent document, and all study materials for ethical and safety soundness prior to initiation.
- Continuing Review: Conduct periodic review (at least annually) of the ongoing trial to ensure risks remain minimized and justified.
- Review of Unanticipated Problems Involving Risks to Subjects or Others (UPIRSOs): Assess all reported UPIRSOs, including certain SAEs, to determine if changes to the protocol or consent are needed to protect subjects.
- Suspension/Termination: Has the authority to suspend or terminate approval of research not being conducted in accordance with its requirements or that has caused unexpected serious harm.
Quantitative Data on Safety Reporting Timelines
Table 1: FDA-Mandated Safety Reporting Timelines for Clinical Trials
| Reporting Entity | Report Type | Recipient | Standard Timeline | Key Trigger/Criteria |
|---|---|---|---|---|
| Investigator | Serious Adverse Event (SAE) | Sponsor | Immediately, but not later than 24 hrs* | Any untoward medical occurrence that is serious (results in death, is life-threatening, requires inpatient hospitalization, etc.). |
| Sponsor | IND Safety Report (SUSAR) | FDA & All Investigators | 15 Calendar Days | Any suspected adverse reaction that is both serious and unexpected. |
| Sponsor | IND Safety Report (Fatal/Life-threatening SUSAR) | FDA & All Investigators | 7 Calendar Days | Any suspected adverse reaction that is fatal or life-threatening and unexpected. |
| Sponsor/Investigator | Unanticipated Problem (UP) Report | IRB | As soon as possible, within 14 days | Any incident, experience, or outcome that is unexpected, related or possibly related to participation in research, and suggests the research places subjects or others at greater risk. |
As stipulated in the study protocol. *Per OHRP guidance and common IRB policy.
Detailed Methodology: Protocol for Safety Data Flow & Triage
This experimental protocol outlines the standard operating procedure (SOP) for handling a potential SAE at a clinical trial site, a core process underpinning safety oversight.
Title: Protocol for On-Site SAE Identification, Reporting, and Triage
Objective: To ensure the systematic, timely, and compliant identification, documentation, assessment, and reporting of Serious Adverse Events.
Materials:
- Source documents (medical records, lab reports).
- Case Report Form (CRF), Electronic Data Capture (EDC) system.
- Sponsor-provided SAE reporting form.
- IRB reporting form.
- Study protocol and Investigator’s Brochure.
Procedure:
- Identification: The investigator or site staff identifies a potential SAE through subject interview, examination, or review of source data.
- Immediate Action: Ensure appropriate medical care for the subject.
- Documentation: Thoroughly document the event in the subject's medical record (date/time of onset, description, severity, actions taken, outcome).
- Causality Assessment: The investigator performs an assessment of relatedness to the study intervention using the protocol-specified algorithm (e.g., unrelated, possibly related, probably related, definitely related). This assessment considers temporal relationship, dechallenge/rechallenge, alternative causes, and known pharmacology of the intervention.
- Sponsor Notification: Within 24 hours of awareness, complete the sponsor’s SAE form. Submit it via fax, secure email, or dedicated safety portal. Include all available relevant data.
- Follow-up: Collect all follow-up information until the event resolves or stabilizes. Submit follow-up reports to the sponsor promptly.
- IRB Notification: Prepare and submit an Unanticipated Problem report to the IRB per the IRB's written procedures (typically within 14 days of the site becoming aware).
- Sponsor’s Review & FDA Reporting: The sponsor’s pharmacovigilance unit consolidates reports from all sites, conducts a unified causality assessment, compares the event to the Investigator’s Brochure, and determines if FDA reporting criteria (SUSAR) are met. If so, they generate and submit the IND/IDE Safety Report within regulatory deadlines.
Diagram: Safety Oversight and Reporting Workflow
The Scientist's Toolkit: Essential Reagents & Materials for Safety Assessment
Table 2: Key Research Reagent Solutions for Safety Biomarker Analysis
| Item/Category | Function in Safety Assessment | Example/Application |
|---|---|---|
| Clinical Chemistry Assays | Quantify standard biomarkers of organ function (e.g., liver, kidney) to monitor for systemic toxicity. | ALT, AST, Creatinine, BUN kits (Roche, Siemens). Used in protocol-specified safety labs. |
| Hematology Analyzers & Reagents | Monitor for bone marrow toxicity, anemia, leukopenia, thrombocytopenia. | Complete Blood Count (CBC) with differential reagents (Sysmex, Beckman Coulter). |
| Immunoassay Kits (Multiplex) | Measure specific protein biomarkers indicative of inflammation, cardiac injury, or immunogenicity. | IL-6, TNF-alpha, Troponin I, Cytokine Panels (Meso Scale Discovery, Luminex). |
| PCR & NGS Solutions | Detect viral reactivation (e.g., HBV, JC virus), clonal expansion in gene therapy, or host immune response. | qPCR master mixes, viral load assays, TCR/BCR sequencing kits (Illumina, Qiagen). |
| Biorepository & SAMs | Ensure integrity of safety biomarker samples (serum, plasma, PBMCs) for retrospective analysis. | Stable archive matrices (SAMs), barcoded cryovials, LN2 storage systems (Brooks, Azenta). |
| Toxicogenomics Platforms | Identify gene expression signatures predictive of specific organ toxicities in early-phase trials. | Transcriptomic arrays/RNA-seq platforms (Affymetrix, Illumina). |
This guide details the operational pathway for serious and unexpected adverse event (AE) reporting in clinical trials, a critical component of FDA regulatory compliance under 21 CFR 312.32. The MedWatch Form 3500A serves as the standardized conduit for transmitting individual case safety reports (ICSRs) from investigative sites, through sponsors, to the FDA's Adverse Event Reporting System (FAERS).
The following table summarizes key metrics from recent FDA safety reporting data, illustrating the scale and primary sources of ICSRs.
Table 1: Recent FAERS Data Summary (Annual)
| Metric Category | Reported Figure | Notes & Source |
|---|---|---|
| Total ICSRs Received | ~2.2 Million | Includes direct and expedited reports (FDA 2023 Data) |
| Expedited Safety Reports (7/15-day) | ~15% of total | Reports meeting expedited criteria (Serious, Unexpected) |
| Top Reporter Type | Industry (Sponsors) | Accounts for ~65% of total submissions |
| Most Common Product Types | Biologics (35%), Pharmaceuticals (60%), Other (5%) | Percentage of total expedited reports |
| Median Processing Time (Sponsor to FDA) | 4 Calendar Days | For 15-day reports from receipt by sponsor |
The Reporting Workflow: Protocol and Methodology
The following is the mandated experimental and data collection protocol for AE handling at an investigative site, leading to a Form 3500A submission.
Experimental Protocol: Site-Level AE Assessment & Documentation
Objective: To systematically identify, assess, document, and initiate reporting of any adverse event occurring in a clinical trial subject.
Materials: Subject Case Report Forms (CRFs), source documents, laboratory reports, FDA MedWatch Form 3500A, sponsor-specific safety forms, secure transmission system.
Methodology:
- Detection & Identification: The investigator actively monitors the subject for any untoward medical occurrence during trial participation and follow-up, irrespective of causal relationship to the investigational product (IP).
- Causality Assessment: The investigator assesses the event's relationship to the IP using the FDA-recommended categories: Unrelated, Unlikely, Possibly, Probably, Definitely Related. Assessment is based on temporal relationship, dechallenge/rechallenge, alternative etiologies, and pharmacological profile.
- Seriousness Determination: The event is classified as Serious if it results in any of the following outcomes: death, a life-threatening experience, inpatient hospitalization or prolongation, persistent/significant disability/incapacity, a congenital anomaly/birth defect, or other important medical events requiring intervention to prevent one of these outcomes.
- Expectedness Evaluation: The investigator compares the event's nature and severity to the reference safety information (RSI) found in the Investigator's Brochure (IB) or protocol. An event is Unexpected if it is not listed in the RSI or differs in specificity or severity.
- Expedited Reporting Determination: If the event is assessed as Serious, Unexpected, and has a Reasonable Possibility of Causal Relationship (i.e., not Unrelated or Unlikely), it triggers an expedited report.
- Initial Data Capture: The investigator completes all relevant sections of the FDA Form 3500A (or equivalent electronic form) with accurate patient demographics, suspect product details, event description, outcome, and investigator assessment.
- Transmission: The completed Form 3500A, along with any necessary narratives or supporting documentation, is transmitted to the study sponsor within 24 hours of the investigator becoming aware of the qualifying event. The sponsor then assumes responsibility for FDA submission within regulatory timelines.
The Safety Reporting Ecosystem: Visualized Workflow
The following diagram illustrates the complete logical pathway and data flow from event occurrence to FDA database entry.
The Scientist's Toolkit: Essential Reagents & Materials for AE Investigation
When a serious AE necessitates laboratory investigation to understand mechanism or causality, the following research reagent solutions are commonly employed.
Table 2: Key Research Reagent Solutions for AE Investigation
| Item | Function in Safety Investigation |
|---|---|
| Cytokine Storm Panel (Luminex/MSD) | Multiplex assay to quantify pro-inflammatory cytokines (e.g., IL-6, IFN-γ, TNF-α) in serum/plasma to identify immune-related adverse events (irAEs) like CRS. |
| Drug-Specific Anti-Drug Antibody (ADA) Assay | Validated immunoassay (e.g., ELISA, ECL) to detect neutralizing antibodies against biologic therapeutics, linking immunogenicity to loss of efficacy or hypersensitivity. |
| Hepatic Safety Panel Enzymes (ALT, AST, ALP) | Standardized clinical chemistry assays to quantitatively assess hepatotoxicity, a common dose-limiting AE for many small molecules and biologics. |
| Cardiac Biomarker Kits (Troponin I/T, BNP) | High-sensitivity ELISA or chemiluminescence assays to detect myocardial injury or stress, critical for assessing drug-induced cardiotoxicity. |
| hERG Channel Binding/Functional Assay Kit | In vitro screening tool to evaluate a compound's potential to block the hERG potassium channel, a key predictor of QT prolongation and Torsades de Pointes risk. |
| Metabolite Identification System (LC-MS/MS) | Liquid chromatography-tandem mass spectrometry platform to identify and quantify unique drug metabolites that may be responsible for organ-specific toxicities. |
| Apoptosis/Necrosis Detection Kit (Flow Cytometry) | Uses Annexin V/PI or other fluorescent probes to distinguish mechanisms of cell death in treated cell lines, informing on-target or off-target toxicity. |
| T-Cell Activation Marker Antibody Panel (CD69, CD25) | Flow cytometry antibodies to assess unintended T-cell activation ex vivo, relevant for assessing risk of autoimmune-like irAEs. |
Recent FDA Guidance and ICH E2A/E2B Harmonization Efforts
Within the framework of FDA adverse event reporting requirements for clinical trials research, the harmonization of safety data standards is paramount. Recent FDA guidance, aligned with International Council for Harmonisation (ICH) E2A (Clinical Safety Data Management) and E2B (Electronic Transmission of Individual Case Safety Reports) efforts, aims to create a unified, global system for adverse event (AE) reporting. This whitepaper provides an in-depth technical analysis of these harmonization initiatives, their impact on clinical trial research, and practical implementation methodologies.
Evolution of Regulatory Standards: ICH E2A and E2B
ICH E2A defines the definitions and standards for expedited reporting of AEs during clinical trials. ICH E2B(R3) specifies the data elements and format for the electronic transmission of Individual Case Safety Reports (ICSRs). Harmonization seeks to bridge these standards into a seamless workflow from data capture to regulatory submission.
Table 1: Core ICH E2A & E2B(R3) Data Element Harmonization
| Data Category | ICH E2A (Concept) | ICH E2B(R3) Element | FDA eSubmitter Requirement |
|---|---|---|---|
| Patient Demographics | Unique identifier, age, sex | A.1, A.2 | Mandatory |
| Suspected Product | Investigational product name, dose | B.1, B.4.k | Mandatory |
| Adverse Event | Description, onset date, seriousness criteria | D.2, D.10 | Mandatory (MedDRA coded) |
| Reporter Information | Qualification, contact | A.3 | Mandatory |
| Case Narrative | Detailed clinical course | H.1 | Structured and Unstructured |
| Clinical Trial Details | Protocol ID, study site | B.1.k.6, B.4.l | Required for INDs |
Recent FDA Guidance: Integration and Implementation
The FDA's recent guidance documents (e.g., "E2B(R3) Electronic Transmission of ICSRs" and related technical conformance guides) mandate the use of the E2B(R3) format for electronic safety reporting to the FDA Adverse Event Reporting System (FAERS) and for Investigational New Drug (IND) safety reports. This aligns with the FDA's commitment to the International Coalition of Medicines Regulatory Authorities (ICMRA) initiative.
Key Experimental Protocol: Validating E2B(R3) Submission Workflow
- Objective: To ensure accurate generation, validation, and submission of ICSRs in E2B(R3) format from a clinical trial safety database to the FDA Gateway.
- Methodology:
- Data Capture: AEs are captured via electronic Case Report Forms (eCRFs) using CDISC Clinical Data Acquisition Standards Harmonization (CDASH) variables.
- MedDRA Coding: AEs are auto-encoded using MedDRA (version >= 26.0) with manual review by a qualified medic.
- ICSR Generation: An automated mapping script transforms source data into the E2B(R3) ISO/HL7 format. Key validations include checks for seriousness criteria (E2A), expectedness, and sponsor causality assessment.
- Validation & Submission: The generated ICSR file is validated against the FDA's "ICSRS2B3" conformance rules. Upon successful validation, the file is signed and transmitted via the FDA ESG/AS2 Gateway.
- Acknowledgment & Reconciliation: The FDA's automated acknowledgment (MControl number) is received and logged. Failure acknowledgments trigger error resolution and resubmission.
Data Flow and System Architecture Diagram
Diagram Title: E2B(R3) ICSR Submission Data Flow
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Tools for Implementing E2A/E2B Harmonization
| Tool/Reagent Category | Specific Example/Function | Purpose in AE Reporting Workflow |
|---|---|---|
| Medical Dictionary | MedDRA (Maintenance and Support Services Organization) | Standardized terminology for coding adverse events, crucial for E2B data elements (Section D). |
| Safety Database System | Oracle Argus Safety, ARISg, Veeva Safety | Centralized repository for case management, MedDRA coding, causality assessment (per E2A), and E2B(R3) message generation. |
| E2B(R3) Mapping Engine | Custom XSLT/Java tools or commercial integrators (e.g., Lægemiddelstyrelsen validator) | Transforms internal database data into compliant ISO/HL7 XML structure for submission. |
| Validation Suite | FDA "ICSRS2B3" Conformance Rules, ICH E2B(R3) Implementation Guide | Ensures technical and business rule compliance of the ICSR file before submission. |
| Transmission Gateway | FDA ESG (Electronic Submissions Gateway) with AS2 protocol | Secure, encrypted electronic delivery channel for regulatory submissions to the FDA. |
| Protocol & Analysis Tool | CDISC CDASH/SDTM standards, Statistical Analysis Software (SAS) | Standardizes data collection and analysis for integrated safety summaries supporting AE reports. |
Impact on Clinical Trial Research
Harmonization reduces ambiguity, enabling consistent global safety reporting. It facilitates advanced analytics and signal detection in FAERS. For researchers, it mandates upfront integration of E2B data elements into clinical trial design and data management systems, promoting data quality and interoperability from Phase I through post-marketing.
The recent FDA guidance solidifies the adoption of harmonized ICH E2A and E2B(R3) standards, creating a robust, electronic framework for adverse event reporting in clinical trials. For drug development professionals, mastering this integrated workflow—from protocol design to electronic submission—is no longer optional but a critical component of regulatory compliance and patient safety surveillance.
Step-by-Step: Implementing Compliant AE Detection, Assessment, and Submission
Developing a Robust Safety Management Plan and Protocol-Specific AE Pages
Within the framework of FDA regulatory requirements for clinical trials, the development of a comprehensive Safety Management Plan (SMP) and protocol-specific Adverse Event (AE) documentation is foundational. The FDA’s mandate, under 21 CFR Parts 312 and 812, requires sponsors to promptly review all safety information and report serious and unexpected adverse experiences. This technical guide details the operational and scientific components necessary for compliance and participant protection, ensuring data integrity for regulatory submission.
Core Components of a Safety Management Plan
An effective SMP is a living document that dictates the systematic identification, assessment, documentation, and reporting of safety data.
Key Elements:
- Roles & Responsibilities: Clear delineation for Sponsor, CRO, Investigator, IRB/IEC, and Data Safety Monitoring Board (DSMB).
- Safety Data Collection: Definitions of Adverse Events (AEs), Serious AEs (SAEs), Adverse Reactions (ARs), and Suspected Unexpected Serious Adverse Reactions (SUSARs).
- Graded Toxicity Scales: Mandatory use of standardized scales (e.g., NCI CTCAE v6.0, latest version).
- Assessment of Causality: Prescribed methodology (e.g., WHO-UMC system) for investigator assessment of relatedness.
- Reporting Workflows: Internal and external pathways with definitive timelines.
- Data Management & Quality Control: Procedures for SAE reconciliation and data verification.
- Risk-Based Monitoring: Focused monitoring of safety endpoints.
- DSMB/Data Monitoring Committee (DMC) Charter: If applicable, detailing stopping rules.
Protocol-Specific AE Pages: From Design to Execution
Protocol-specific AE pages in the Case Report Form (CRF) are critical for precise data capture. They must be tailored to the investigational product's mechanism, patient population, and known risks.
Design Methodology:
- Risk Profiling: Conduct a pre-protocol literature review of the drug class and preclinical data to predict potential AEs.
- Endpoint Alignment: Design AE pages to capture data necessary for primary and secondary safety endpoints.
- Structured Data Capture: Utilize standardized dropdowns for MedDRA-coded terms, severity, frequency, onset/duration, and action taken.
- Causality Prompt: Include a mandatory field for investigator assessment of relatedness to investigational product.
- Conditional Logic: Implement CRF branching for SAE triggers, requiring immediate detailed narrative and follow-up pages.
Key Experiments and Analytical Methodologies for Safety Signal Detection
Proactive safety management relies on continuous data analysis. The following experimental and statistical protocols are employed for signal detection.
Disproportionality Analysis Using FDA AERS/FAERS Data
Objective: To identify statistically significant reporting associations between a drug and an event in large-scale spontaneous reporting databases.
Protocol:
- Data Extraction: Download and preprocess the latest FDA FAERS quarterly data files (DEMO, DRUG, REAC, OUTC).
- Case Selection: Define the drug of interest (Active Ingredient) and the Medical Event of interest (Preferred Term, PT).
- Contingency Table Construction: Create a 2x2 table for the entire database.
- Statistical Calculation: Compute the Reporting Odds Ratio (ROR) and 95% Confidence Interval.
- Formula: ROR = (a/b) / (c/d)
- Where:
- a = reports with drug and event of interest
- b = reports with drug and other events
- c = reports with other drugs and event of interest
- d = reports with other drugs and other events
- Signal Threshold: A signal is considered if the lower bound of the 95% CI > 1 and N (number of cases) >= 3.
Table 1: Example Disproportionality Analysis Output for Hypothetical Drug "Xylozimab"
| Drug | Adverse Event (PT) | N (a) | ROR | 95% CI (Lower) | 95% CI (Upper) | Signal? |
|---|---|---|---|---|---|---|
| Xylozimab | Hepatic enzyme increased | 42 | 4.2 | 3.1 | 5.7 | Yes |
| Xylozimab | Headache | 125 | 1.1 | 0.9 | 1.3 | No |
| Xylozimab | Cardiac arrest | 5 | 8.5 | 2.8 | 25.9 | Yes* |
*Requires clinical review due to low N.
Laboratory Shift Table Analysis from Clinical Trial Data
Objective: To quantify the magnitude and frequency of clinically significant laboratory abnormalities between treatment and control arms.
Protocol:
- Define Thresholds: Utilize protocol-defined toxicity grade thresholds (per CTCAE) or clinically significant thresholds (e.g., >3x ULN for ALT).
- Categorize Subjects: For each analyte, categorize every subject at their worst post-baseline value.
- Tabulate Frequencies: Count subjects in each category (e.g., Normal at Baseline to >3x ULN Post-Baseline).
- Statistical Testing: Apply Chi-square or Fisher’s exact test to compare the proportion of subjects with clinically significant shifts between treatment groups.
Table 2: Laboratory Shift Table Template (ALT Example)
| Treatment Group | N | Normal to >3x ULN n (%) | Normal to >5x ULN n (%) | Normal to >10x ULN n (%) | p-value vs. Placebo |
|---|---|---|---|---|---|
| Drug X - 100mg | 150 | 15 (10.0%) | 8 (5.3%) | 3 (2.0%) | 0.003 |
| Drug X - 50mg | 148 | 8 (5.4%) | 3 (2.0%) | 1 (0.7%) | 0.12 |
| Placebo | 152 | 3 (2.0%) | 1 (0.7%) | 0 (0.0%) | -- |
Visualizing Safety Management Workflows
Safety Management and Reporting Pathway
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents for Immunogenicity & Safety Assay Development
| Reagent / Material | Function / Application in Safety Assessment |
|---|---|
| Recombinant Human Target Protein | Critical for developing anti-drug antibody (ADA) assays and cell-based neutralizing antibody (NAb) assays to assess immunogenicity. |
| Positive Control Antibody | Used to validate and monitor the sensitivity of immunogenicity assays (e.g., mouse anti-human monoclonal). |
| Cytokine Release Assay (CRA) Kits | Pre-configured kits (e.g., Multi-cytokine Luminex) to assess potential for cytokine release syndrome (CRS) in vitro. |
| hERG Channel Expressing Cell Line | Essential for in vitro cardiac safety screening to assess potential for QT interval prolongation (ICH S7B). |
| Hepatocyte Cultures (Primary/Cell Line) | Used for in vitro hepatotoxicity studies to evaluate drug-induced liver injury (DILI) potential. |
| Complement Activation Assay Kits | To screen for potential infusion-related reactions and complement activation-related pseudoallergy (CARPA). |
| Stable Reporter Gene Cell Lines | Engineered cells for specific signaling pathways (e.g., NF-κB, cytokine release) to mechanistically evaluate immune-related AEs. |
A robust SMP, coupled with precisely designed AE pages, forms the operational spine of participant safety and regulatory compliance in clinical research. By integrating proactive signal detection methodologies, standardized data capture, and clear visual workflows, sponsors can fulfill FDA requirements under 21 CFR 312.32 while ensuring the ethical integrity of the trial. The ultimate goal is a dynamic system where data collection directly informs risk assessment, enabling proactive safety management throughout the drug development lifecycle.
The Investigator's Immediate and Follow-Up Actions for SAEs
Within the framework of FDA adverse event reporting requirements for clinical trials, the management of Serious Adverse Events (SAEs) is a critical component of subject safety and regulatory compliance. This guide details the investigator's mandated immediate actions upon SAE identification and the subsequent follow-up procedures, aligning with 21 CFR 312.64 and ICH E6(R2) Good Clinical Practice.
Immediate Actions Upon SAE Identification
The initial 24-hour period following SAE awareness is crucial. The investigator, as the responsible party at the site, must execute a defined sequence of actions.
Core Immediate Action Protocol
- Subject Care: Ensure the subject receives all necessary medical treatment. The subject's welfare is the absolute priority.
- Verification and Documentation: Immediately verify the event details (onset, description, severity, outcome) and document all available information in the source documents and the subject's case report form (CRF).
- Sponsor Notification: Notify the sponsor (or designated representative) of the SAE within 24 hours of awareness. Initial notification is often via phone or fax, followed by written confirmation.
- IRB Notification: Notify the Institutional Review Board (IRB) within the IRB’s stipulated timeframe, often 5-10 working days, unless the SAE is unexpected, fatal, or life-threatening, which may require more prompt reporting (e.g., within 7 days).
- Unblinding (if necessary): If the study is blinded, assess the need for urgent unblinding to facilitate appropriate clinical management. The protocol must define this procedure.
Table 1: Regulatory Reporting Timelines for Investigators Following an SAE
| Recipient | Event Type | Maximum Reporting Timeframe (from Investigator Awareness) | Regulatory Reference |
|---|---|---|---|
| Sponsor | All SAEs | 24 Hours | ICH E6(R2) Sec 4.11.1 |
| IRB/IEC | Unexpected, fatal, or life-threatening SAE | 7 Calendar Days | 21 CFR 312.66 |
| IRB/IEC | Other SAEs | As stipulated in IRB agreement (e.g., 10-14 days) | ICH E6(R2) Sec 3.1 |
| FDA | Note: Primary reporting to FDA is the sponsor's duty. | Investigator forwards sponsor reports per IRB/FDA requirements. | 21 CFR 312.32 |
Follow-Up Actions and Investigation
The initial report is the starting point. The investigator must actively pursue and document complete information.
Follow-Up Investigation Protocol
- Information Pursuit: Actively obtain all missing information, including:
- Hospital discharge summaries
- Specialist consultation reports
- Laboratory and diagnostic test results
- Autopsy reports (if applicable)
- Causality Assessment: Re-assess the relationship of the SAE to the investigational product. Use a standardized scale (e.g., FDA-defined: Unrelated, Unlikely, Possible, Probable, Related).
- Endpoint Determination: Document the final outcome (e.g., resolved with sequelae, resolved, fatal, ongoing).
- Supplemental Reporting: Submit all follow-up information to the sponsor and IRB in a timely manner, clearly linking it to the initial report.
- Protocol and Process Review: In collaboration with the sponsor, review the event to determine if any protocol amendments, informed consent updates, or procedural changes are required for ongoing subject safety.
Diagram Title: Investigator SAE Action Workflow: Immediate & Follow-Up Phases
The Investigator's Toolkit for SAE Documentation & Analysis
Effective SAE management relies on precise documentation and assessment tools.
Table 2: Essential Research Reagent Solutions & Tools for SAE Management
| Tool / Reagent Category | Example / Specific Item | Function in SAE Investigation |
|---|---|---|
| Standardized Assessment Scales | FDA Causality Categories (Unrelated, Probable, etc.) | Provides a consistent, auditable framework for determining relationship to investigational product. |
| Medical Diagnostic Kits | Specific biomarker assay kits (e.g., troponin I, liver enzyme panels) | Objectively measures physiological impact and aids in diagnosis and tracking of the SAE. |
| Data Collection Tools | Secure, 21 CFR Part 11-compliant eCRF (Electronic Case Report Form) | Ensures accurate, legible, and contemporaneous recording of SAE data for sponsor and regulatory review. |
| Source Document Templates | Hospitalization Summary Template, Lab Result Tracker | Facilitates systematic collection of all relevant medical information from external care providers. |
| Communication Logs | Sponsor & IRB Communication Log (Phone/Fax/Email) | Provides an audit trail for compliance with mandated notification timelines. |
Integration with Broader FDA Reporting Requirements
The investigator's actions are a primary data feed into the sponsor's mandatory FDA safety reporting obligations under IND regulations (21 CFR 312.32). The investigator's prompt, accurate, and complete reporting enables the sponsor to:
- Fulfill its duty to report unexpected, fatal, or life-threatening SAEs to FDA within 7 calendar days.
- Analyze aggregate safety data for potential signals.
- Submit annual safety reports (IND Annual Reports).
Diagram Title: SAE Information Flow from Investigator to FDA
The investigator's rigorous adherence to immediate and follow-up action protocols for SAEs is non-negotiable. It forms the bedrock of subject protection and ensures the integrity of clinical trial data within the stringent FDA regulatory framework. By systematically executing these actions, investigators fulfill their ethical and legal responsibilities, enabling sponsors to maintain regulatory compliance and, ultimately, contributing to the accurate assessment of a product's safety profile.
Sponsor Review, Causality Assessment, and Expedited Reporting Timelines (7 & 15-Day)
Within the regulatory framework for clinical trials in the United States, sponsors have distinct obligations for the reporting of adverse events (AEs) and serious adverse events (SAEs) to the FDA and other stakeholders. The core regulatory driver is 21 CFR §312.32, which mandates expedited reporting for certain safety findings. This guide details the technical processes of sponsor review, causality assessment, and the critical decision-making that governs adherence to the 7-day and 15-day expedited reporting timelines.
The Core Process: From AE Intake to Regulatory Submission
The workflow from initial site notification to regulatory submission is a multi-stage, interdependent process. The following diagram illustrates the critical path and decision points.
Detailed Methodologies: Sponsor Causality Assessment
Sponsor assessment of causality (relatedness) is distinct from the investigator's initial assessment and follows a structured, reproducible protocol.
3.1 Protocol: Systematic Causality Algorithm
- Objective: To determine if there is a reasonable possibility that the investigational product caused the adverse event.
- Data Sources: Case report forms, medical records, investigator's assessment, drug dispensing logs, known pharmacology, and prior safety data.
- Methodology:
- Temporality Analysis: Establish the chronological relationship between drug administration and event onset. Was the event after exposure?
- Biological Plausibility: Review known mechanism of action, class effects, and preclinical data for supporting evidence.
- Dechallenge/Rechallenge Analysis: Did the event improve upon stopping the drug (dechallenge)? Did it recur upon re-exposure (rechallenge)? Positive dechallenge/rechallenge strongly suggests causality.
- Alternative Etiology Evaluation: Systematically rule out other potential causes (underlying disease, concomitant medications, environment).
- Consistency Check: Compare the event profile with the evolving safety database for similar reports.
- Output: A dichotomous determination: "Related" or "Not Related." The assessment must be documented with rationale. This assessment directly feeds into the SUSAR determination.
Expedited Reporting Timelines: 7-Day vs. 15-Day
The expedited reporting timeline is determined by the outcome of the causality assessment and the severity of the event. The following table summarizes the key criteria and deadlines.
Table 1: FDA Expedited Reporting Timelines for SUSARs (21 CFR §312.32)
| Reporting Timeline | Triggering Criteria | Key Definition (Per FDA Guidance) | Clock Start |
|---|---|---|---|
| 7-Calendar Day Report | Fatal or life-threatening SUSAR | Life-threatening: An event that places the patient at immediate risk of death from the event as it occurred. | Sponsor's first receipt of information meeting minimum criteria for reporting. |
| 15-Calendar Day Report | All other serious SUSARs (not fatal or life-threatening) | Serious: An event that results in death, is life-threatening, requires inpatient hospitalization/prolongation, results in persistent disability, or is a congenital anomaly/birth defect. | Sponsor's first receipt of information meeting minimum criteria for reporting. |
Table 2: Minimum Data Elements for Expedited Reporting (Initial Submission)
| Data Element Category | Specific Items Required for "Clock-Stop" Submission |
|---|---|
| Patient/Subject | Unique identifier (e.g., subject ID) |
| Suspect Product | Investigational drug name and dose |
| Event Details | Event description, seriousness criteria, onset date |
| Outcome | e.g., recovered, resolved, fatal |
| Reporter | Source of information (e.g., principal investigator) |
| Sponsor Assessment | Causality (relatedness) and expectedness assessment |
| Administrative | Sponsor case ID, FDA form 3500A or CIOMS I form |
The Scientist's Toolkit: Essential Reagents & Materials for Safety Analysis
This table outlines key tools and resources used in the modern pharmacovigilance and safety review process.
Table 3: Research Reagent & Solution Toolkit for Safety Assessment
| Item/Tool | Function/Explanation in Safety Analysis |
|---|---|
| Medical Dictionary for Regulatory Activities (MedDRA) | Standardized terminology for coding adverse events, enabling consistent analysis and reporting across trials. |
| Clinical Safety Database (e.g., ARGUS, Oracle Argus) | Validated system for case management, tracking timelines, performing causality assessments, and generating regulatory reports. |
| Electronic Data Capture (EDC) System Linkage | Direct interface with EDC systems for real-time or batch transfer of AE/SAE data from sites to the sponsor's safety database. |
| Signal Detection Software (e.g., Empirica) | Uses statistical algorithms (e.g., disproportionality analysis) on aggregated safety data to identify potential new safety signals. |
| Literature Screening Tools (e.g., BIOMED, NLP agents) | Automated tools to continuously scan scientific literature for potential case reports involving the investigational product. |
| Toxicology & Pharmacology Reference Databases | Provides critical background on mechanism of action, preclinical findings, and class effects to inform causality assessment. |
| FDA Guidance Documents (e.g., E2A, E2B) | Provide the regulatory and technical specifications for data elements, transmission standards (ICH E2B R3), and reporting logic. |
1.0 Introduction: ESG in the Context of Regulatory Reporting The FDA’s Electronic Submissions Gateway (ESG) is the mandated portal for transmitting regulatory information, including safety reports for clinical trials. In the framework of FDA adverse event (AE) reporting requirements (21 CFR 312.32 for INDs), timely and accurate electronic submission via the ESG is critical. It ensures that potential risks to human subjects are communicated expediently, allowing the FDA to monitor trial safety and inform the risk-benefit assessment of investigational products.
2.0 Quantitative Overview of AE Reporting Requirements Submission timelines and categories are defined by severity and unexpectedness. The following table summarizes the core requirements for Investigational New Drug (IND) safety reporting.
Table 1: FDA IND Safety Reporting Requirements and ESG Submission Timelines
| Report Type | Regulatory Basis | Reporting Clock | ESG Submission Goal |
|---|---|---|---|
| Suspected Unexpected Serious Adverse Reaction (SUSAR) | 21 CFR 312.32(c)(1) | 15 calendar days (fatal/life-threatening); 15 calendar days (non-fatal) | Within clock days of sponsor's awareness |
| Aggregate Increase in Risk | 21 CFR 312.32(c)(5) | As soon as possible, minimum 15 calendar days | Promptly upon analysis conclusion |
| Annual Report Safety Summary | 21 CFR 312.33 | Within 60 days of IND anniversary | For consolidated annual submission |
| IND Safety Report (7-Day Report) | 21 CFR 312.32(c)(2) | 7 calendar days | For any fatal/life-threatening SUSAR follow-up |
3.0 The ESG Submission Protocol: A Technical Methodology The successful submission of an IND safety report (Form FDA 3500A or CIOMS I) via the ESG follows a defined experimental protocol.
3.1 Protocol: End-to-End ESG Transmission Workflow
- Preparation: Generate the safety report as an XML file compliant with the FDA’s Electronic Common Technical Document (eCTD) specifications or as a PDF for non-eCTD submissions. Ensure proper data elements per ICH E2B(R3) guidelines.
- Testing (Pre-Production): Transmit the submission via the FDA’s Test ESG environment using test credentials. This validates file structure, packaging, and transmission pathways.
- Validation & Acknowledgment: The Test ESG returns a Gateway Acknowledgement receipt. A subsequent Submission Acknowledgement from the FDA’s center (CDER/CBER) confirms successful technical validation.
- Production Submission: Upon successful testing, transmit the final submission via the Production ESG using live authorized credentials.
- Receipt & Tracking: Secure and archive the two key receipts: the Gateway Acknowledgement (proves FDA receipt) and the Technical Validation Acknowledgement (confirms file is processable). Track submission status via the ESG web interface.
Diagram Title: ESG Safety Report Submission Protocol Workflow
4.0 The Adverse Event Data Flow and Regulatory Logic The decision pathway for determining reportability and submission method integrates regulatory logic with data flow from clinical site to FDA.
Diagram Title: Logic Flow for IND Safety Report Determination
5.0 The Scientist's Toolkit: Essential Resources for ESG Submissions
Table 2: Key Research Reagent Solutions for ESG Safety Reporting
| Tool/Resource | Function & Purpose |
|---|---|
| ESG Web Interface | Primary portal for account management, submission, and tracking. |
| FDA ESG Test System | Critical sandbox environment for validating submission payloads and processes. |
| eCTD Validation Tool | Validates XML structure and compliance with required specifications prior to submission. |
| Study Safety Reporting Plan (SSRP) | Internal protocol defining roles, data flow, and timelines for AE processing. |
| Electronic Data Capture (EDC) & Safety Database | Source systems for consistent, audit-ready AE data compilation and report generation. |
| ICH E2B(R3) Implementation Guide | Defines the standardized data elements and format for electronic safety reports. |
| CDER/CBER Direct Email | Backup transmission mechanism for urgent reports if ESG is inoperable (per guidance). |
1. Introduction: Within the FDA’s AE Reporting Framework The Investigational New Drug (IND) Annual Report (Safety Summary) is a cornerstone of ongoing safety surveillance in clinical research, mandated under 21 CFR 312.32 and 312.33. It operates within a tiered FDA adverse event reporting ecosystem. While serious and unexpected suspected adverse reactions (SUSARs) require expedited reporting (7- or 15-day alerts), the Annual Report provides a consolidated, periodic overview of the investigational product's safety profile. This document is critical for FDA review to assess whether the risk-benefit balance of the ongoing trial remains favorable and to identify new safety signals from aggregated data.
2. Core Content and Structure of the IND Annual Report (Safety Summary) The Safety Summary must present a comprehensive yet concise analysis of all safety information collected over the reporting period (typically the past year). The required elements are detailed below.
Table 1: Mandatory Content of the IND Annual Report Safety Summary
| Section | Required Content Description |
|---|---|
| Individual Study Summaries | Brief narrative of the study's progress, focusing on subject exposure (dose, duration), demographics, and safety observations for each study. |
| Summary of All Serious AEs | A tabular summary of all serious adverse events (SAEs) experienced by trial participants, regardless of causality assessment. |
| Summary of All Non-Serious AEs | A summary of the most common non-serious adverse events, often presented in a table showing frequency by treatment arm and dose. |
| Analysis of Deaths | A listing of all deaths, with an analysis of the cause of death and its relationship to the investigational product. |
| Analysis of Dropouts | A listing of subjects who discontinued the study due to an adverse event, with analysis. |
| Updated Investigator's Brochure | If revised, a copy or summary of key safety-relevant changes must be included. |
| Preclinical Study Updates | Summary of any significant new animal toxicology or safety pharmacology findings. |
| Previous Safety Concerns | An update on any safety issues identified in previous reporting periods and actions taken. |
| Overall Safety Assessment | A integrated, benefit-risk analysis of the safety data, discussing any new risks, increased frequency of known risks, and any recommended protocol modifications. |
3. Methodologies for Signal Detection & Analysis in Annual Reports The annual report requires more than data listing; it necessitates analytical evaluation for emerging safety signals.
Protocol 1: Disproportionality Analysis for Signal Detection
- Objective: To identify potential new safety signals by comparing the reporting frequency of specific event-drug combinations against a background reporting rate.
- Methodology:
- Data Preparation: Pool all AE data from all studies under the IND for the reporting period. Code events using a standard medical dictionary (e.g., MedDRA).
- Calculation of Proportional Reporting Ratio (PRR): For a specific AE (e.g., hepatotoxicity), calculate: PRR = (a / (a+b)) / (c / (c+d)).
- a = Number of cases with the AE and the investigational drug.
- b = Number of cases with all other AEs and the investigational drug.
- c = Number of cases with the AE and all other drugs in comparator database/group.
- d = Number of cases with all other AEs and all other drugs.
- Thresholds: A signal is often considered if PRR ≥ 2, Chi-squared ≥ 4, and a ≥ 3 cases. This analysis is typically performed using specialized pharmacovigilance software.
Protocol 2: Cumulative Analysis of Key Safety Parameters
- Objective: To track trends in laboratory abnormalities or vital signs over time.
- Methodology:
- Parameter Selection: Identify key safety parameters (e.g., ALT, serum creatinine, QTc interval).
- Shift Table Analysis: Create tables showing the number/percentage of subjects shifting from baseline normal values to clinically concerning values at any time during treatment (e.g., shift from Normal to >3x ULN for ALT).
- Time-to-Event Analysis: For critical events, plot Kaplan-Meier curves to estimate the probability of an event occurring over the duration of exposure.
- Dose-Response Relationship: Stratify analysis by dose level to assess if AE frequency or severity increases with higher doses.
4. Visualizing the Safety Reporting and Analysis Workflow
Diagram 1: IND Safety Reporting Ecosystem & Annual Report Integration
Diagram 2: Signal Detection & Assessment Workflow for Annual Reports
5. The Scientist's Toolkit: Essential Reagents & Resources for Safety Analysis Table 2: Key Research Reagent Solutions for Safety Data Analysis
| Item/Category | Function in Safety Reporting & Analysis |
|---|---|
| Medical Dictionary for Regulatory Activities (MedDRA) | Standardized medical terminology for consistent coding of adverse events, enabling accurate aggregation, searching, and analysis across studies. |
| Pharmacovigilance Software (e.g., ARISg, Argus, Veeva Safety) | Database systems for managing adverse event case data, facilitating expedited reporting, and providing tools for trend analysis and report generation. |
| Statistical Analysis Software (e.g., SAS, R) | Essential for performing quantitative signal detection analyses (PRR, regression), generating shift tables, and creating safety graphs (Kaplan-Meier). |
| Electronic Data Capture (EDC) System | The primary source for cleaned, subject-level safety data (AEs, labs, concomitant meds) which is extracted for the annual safety analysis. |
| Laboratory Normal Range Database | Central repository for institution- and assay-specific normal ranges, critical for accurately flagging and assessing laboratory abnormalities. |
| Clinical Trial Management System (CTMS) | Provides key operational data (subject enrollment, site status) to contextualize safety data and calculate subject exposure (patient-years). |
Avoiding Common Pitfalls: Best Practices for Efficient and Compliant Safety Reporting
Critical Errors in Causality Assessment and Under-Reporting
1. Introduction: The Regulatory Imperative Within the U.S. Food and Drug Administration's (FDA) regulatory framework for clinical trials, the accurate assessment and reporting of adverse events (AEs) are critical for patient safety and data integrity. The Code of Federal Regulations (21 CFR 312.32) mandates expedited reporting of serious and unexpected suspected adverse reactions. This whitepaper examines two pervasive threats to this system: flawed causality assessment methodologies and systemic under-reporting, providing a technical guide for researchers to mitigate these risks.
2. Quantitative Landscape of Under-Reporting and Error Data from FDA audits and meta-analyses reveal systemic challenges. The following table synthesizes key quantitative findings on reporting compliance and assessment errors.
Table 1: Metrics of Under-Reporting and Causation Error in Clinical Trials
| Metric | Reported Rate/Prevalence | Source/Study Context |
|---|---|---|
| Under-Reporting of SAEs | 23-50% of eligible events | FDA Bioresearch Monitoring Program findings; meta-analyses of trial data. |
| Inter-Rater Disagreement in Causality | Cohen's κ = 0.40-0.55 (Moderate) | Studies comparing assessments from site investigators, sponsors, and adjudication committees. |
| High "Related" Attribution in Phase I | 75-85% of AEs assessed as drug-related | Analysis of early-phase trial data, reflecting high index of suspicion. |
| Impact of Naranjo Scale | Yields "Probable" rating 3x more often than WHO-UMC | Comparative methodology studies using identical case datasets. |
3. Deconstructing Causality Assessment Methodologies Causality assessment is the process of determining the likelihood that a drug caused an adverse event. Common methods include algorithmic (e.g., Naranjo Scale), probabilistic (Bayesian), and expert judgment (WHO-UMC system).
Experimental Protocol 1: Validating the Naranjo Algorithm
- Objective: To quantify the inter-rater reliability and output distribution of the Naranjo Scale versus clinical gestalt.
- Materials: A validated set of 50 de-identified SAE case narratives from oncology trials.
- Procedure:
- Recruit three blinded physician assessors.
- Each assessor reviews all 50 cases using the Naranjo Scale, scoring each item (e.g., temporal relationship, rechallenge, alternative causes).
- Separately, after a washout period, the same assessors provide a global introspection judgment (Unrelated/Unlikely/Possible/Probable/Definite) for each case.
- Calculate aggregate scores for Naranjo (Definite >9; Probable 5-8; Possible 1-4; Doubtful ≤0).
- Perform statistical analysis (Fleiss' κ for agreement, Chi-square for distribution differences).
- Expected Outcome: The algorithmic Naranjo method will show higher nominal agreement but a significant skew toward "Probable" attribution compared to the broader distribution of global introspection.
Table 2: Research Reagent Solutions for Pharmacovigilance Research
| Reagent/Tool | Primary Function | Application in Causality Research |
|---|---|---|
| WHO-UMC Causality Categories | Standardized taxonomy for causation likelihood. | Gold standard for comparative studies of assessment methods. |
| Naranjo Algorithm Scale | Structured questionnaire for causation probability. | Object of study for algorithmic bias and reproducibility. |
| Bayesian Confidence Propagation Neural Network (BCPNN) | Data-mining algorithm for signal detection. | Used to establish prior probability for Bayesian causal assessments. |
| Electronic Health Record (EHR) Linkage | Longitudinal patient data source. | Provides contextual clinical data to assess alternative causes and completeness. |
| Standardized MedDRA Queries (SMQs) | Grouped terms for medical events of interest. | Ensures consistent identification of AEs across datasets for analysis. |
4. Protocol for Auditing Under-Reporting Under-reporting stems from high workload, ambiguous definitions, and lack of feedback. The following protocol outlines a systematic audit.
Experimental Protocol 2: Source Data Verification for SAE Reporting Compliance
- Objective: To determine the rate of and reasons for under-reporting of Serious Adverse Events (SAEs) at the clinical site level.
- Materials: Site EHR/medical records, monitoring visit reports, SAE tracking logs, case report forms (CRFs).
- Procedure:
- Case Ascertainment: Identify all hospitalized or otherwise medically significant events for all trial participants from source medical records.
- Definition Application: Apply FDA criteria for seriousness (results in death, life-threatening, requires hospitalization, etc.) to each identified event.
- Log Reconciliation: Compare the list of serious events against the site's SAE log and sponsor's safety database.
- Root Cause Analysis: For each discrepant (unreported) event, conduct interviews to categorize cause: Lack of Understanding (of seriousness), Administrative Error, or Deliberate Omission.
- Quantification: Calculate under-reporting rate as:
(Unreported SAEs / Total Identified Serious Events) * 100.
- Expected Outcome: Identification of a significant under-reporting rate (e.g., >20%), most commonly attributed to administrative error and variable interpretation of "hospitalization."
5. Visualizing Workflows and Relationships
Diagram 1: AE Causality Assessment and Reporting Workflow
Diagram 2: Root Causes Leading to Critical Safety Data Errors
6. Mitigation Strategies for the Research Professional
- Standardize with WHO-UMC: Use WHO-UMC as the primary categorization system, supplemented by algorithmic tools for initial screening.
- Implement Bayesian Aids: Develop institution-specific prior probability datasets to inform causal reasoning.
- Automate Case Ascertainment: Where possible, use EHR triggers flagging potential SAEs (e.g., hospitalization codes) for review.
- Enhance Training: Move beyond definitions to include simulated case assessments focusing on confounding and temporal logic.
- Close the Feedback Loop: Implement systems to share aggregate safety data and concluded causality assessments with trial sites.
7. Conclusion Adherence to FDA AE reporting requirements is compromised by subjective, inconsistent causality assessment and significant under-reporting. By understanding the quantitative scope of these issues, implementing rigorous experimental audit protocols, and standardizing methodologies, researchers and drug development professionals can generate more reliable safety data, ultimately protecting public health and ensuring regulatory compliance.
Managing Unblinding Risks in Double-Blind Trials During Safety Reviews
Within the stringent framework of FDA adverse event reporting requirements, maintaining trial integrity is paramount. The mandate for timely reporting of Serious Adverse Events (SAEs) and potential unanticipated problems creates inherent tension with the imperative to preserve blinding. This guide details protocols to manage unblinding risks during essential safety reviews.
The Regulatory Context & Blinding Conflict
The FDA’s Code of Federal Regulations (21 CFR 312.32) requires sponsors to promptly review all safety information and report events that are serious, unexpected, and possibly drug-related. An internal Safety Review Team (SRT) or an independent Data Monitoring Committee (DMC) must perform periodic, unblinded reviews to assess risk-benefit. The core challenge is to enable these reviews while preventing the dissemination of unblinded data to the sponsor's operational team and investigators.
Quantitative Landscape of Unblinding Risks
Data from recent regulatory filings and audits highlight common sources of inadvertent unblinding.
Table 1: Common Sources of Inadvertent Unblinding During Safety Reviews
| Source of Risk | Frequency in Audits* (%) | Primary Mitigation Strategy |
|---|---|---|
| Aggregate AE Tables by Arm | 45% | Review of Dummy Tables |
| SAE Narratives with Drug Details | 30% | Narrative Sanitization |
| Laboratory Shift Tables | 15% | Review by Parameter, Not Arm |
| Communications from DMC to Sponsor | 10% | Firewall & Neutral Communications |
*Hypothetical composite data based on common audit findings.
Core Methodologies for Risk Management
Protocol: The "Sanitized" Safety Review Package
This methodology prepares data for sponsor-internal SRT review without revealing assignment.
- Data Generation: The biostatistics team generates safety outputs (e.g., listings of SAEs, lab abnormalities) using a dummy randomization code. Arms are labeled 'A' and 'B' without indication of treatment identity.
- Narrative Review: All SAE narratives are reviewed by an unblinded medical reviewer to redact any references to study drug identity, specific dose form, or other revealing details (e.g., "the patient reported taste of garlic" for a known garlic-tasting drug).
- Package Assembly: The SRT receives the sanitized package. The unblinded statistician holds the dummy code key but does not participate in SRT discussions that could infer efficacy.
- Decision Logic: The SRT assesses whether safety signals are concerning enough to warrant a formal request to the unblinded statistician for treatment-arm breakdowns, which is a major unblinding event requiring documented justification.
Diagram 1: Sanitized Safety Review Workflow
Protocol: Independent Data Monitoring Committee (DMC) Operations
For higher-risk trials, an independent DMC conducts unblinded reviews.
- Charter: A formal DMC charter defines stopping guidelines and communication rules. The DMC receives fully unblinded data.
- Firewall: Only designated, unblinded team members (usually the statistician) interact with the DMC. All communications to the sponsor are via neutral, pre-agreed statements (e.g., "Continue trial as per protocol," "Please review protocol adherence").
- Output: Recommendations are made to the sponsor without revealing arm-specific data unless absolutely critical for trial continuation.
Diagram 2: DMC Firewall Communication Pathway
The Scientist's Toolkit: Essential Research Reagents for Risk Mitigation
Table 2: Key Tools for Managing Unblinding Risk
| Item / Solution | Function in Managing Unblinding Risk |
|---|---|
| IRT (Interactive Response Technology) System | Centralized, third-party system for randomization and drug supply. Allows generation of dummy arm codes without revealing actual treatment. |
| Dummy Randomization Schedule | A look-up table mapping subject numbers to non-revealing group labels (A/B/X). Held securely by the unblinded statistician. |
| Redaction Software (e.g., Adobe Acrobat Pro) | For systematic sanitization of SAE narrative fields in case report forms and safety reports. |
| Secure, Access-Logged Portals | For sharing sensitive DMC reports. Tracks access and prevents unauthorized downloads. |
| Pre-specified Statistical Analysis Plan (SAP) for DMC | Defines exact, unblinded safety analyses (e.g., time-to-event, lab trends by arm) to prevent data dredging that increases unblinding risk. |
| Neutral Communication Templates | Pre-approved language for DMC-to-sponsor communication to avoid inadvertent information leakage through tone or emphasis. |
Integration with FDA AE Reporting
When an SAE is determined to be reportable (e.g., SUSAR), the unblinded team (not the blinded study staff) must prepare the report. The process must ensure the blinding of all other personnel. This is often managed by segregating the pharmacovigilance function and using the IRT to confirm treatment assignment only at the moment of regulatory report generation.
Conclusion: Effective management of unblinding risks requires a multi-layered, procedural approach integrated into the trial's master protocol. By employing structured methodologies like sanitized reviews and independent DMCs with robust firewalls, sponsors can fulfill their FDA-mandated safety oversight obligations while rigorously protecting the scientific integrity of the double-blind trial.
The integration of Electronic Data Capture (EDC) systems with safety databases is not merely a technical challenge but a critical compliance requirement under FDA regulations for clinical trials. The FDA's 21 CFR Part 11, along with ICH E2A, E2B(R3), and E6(R2) guidelines, mandates the accurate, timely, and secure reporting of adverse events (AEs) and serious adverse events (SAEs). The central thesis driving this integration is that a seamless, automated flow of safety data from point-of-capture in the EDC to the safety database is essential for patient safety, data integrity, and regulatory compliance, directly impacting the success of drug development programs.
The Core Integration Architecture & Data Flow
A robust integration architecture minimizes manual transcription errors, reduces reporting delays, and ensures a single source of truth for safety data. The primary flow involves the automated detection, transformation, and transmission of AE data.
Diagram 1: High-Level Safety Data Flow Architecture
Quantitative Analysis of Integration Impact
The following table summarizes key performance indicators (KPIs) demonstrating the impact of optimized EDC-Safety database integration, based on recent industry benchmarks and regulatory audits.
Table 1: Impact Metrics of Optimized vs. Manual Data Flow
| Key Performance Indicator (KPI) | Manual Process (Benchmark) | Optimized Automated Integration | Improvement / Rationale |
|---|---|---|---|
| Time from AE Entry to Safety DB (Median) | 48 - 72 hours | < 4 hours | > 90% reduction; critical for 1-day SAE reporting. |
| Data Transcription Error Rate | ~5% per field | < 0.1% | Near elimination of manual re-keying errors. |
| Queries on AE Consistency | 15-20% of AEs | < 2% of AEs | Automated mapping reduces discrepancies. |
| Staff Time per SAE Process | 45-60 minutes | 5-10 minutes | Focus shifts from data handling to clinical assessment. |
| FDA Inspection Findings (Data Integrity) | High prevalence in safety | Significantly reduced | Audit trail continuity from EDC to report is ensured. |
Detailed Integration Protocol: The EDC-to-E2B Workflow
This protocol outlines the step-by-step methodology for establishing a compliant, automated data flow.
Experimental Protocol: Real-Time AE Data Transmission
Objective: To automatically detect a new or updated AE/SAE record in the EDC and transmit a fully composed E2B(R3) message to the safety database.
Materials & Systems:
- Production EDC System (e.g., Medidata Rave, Veeva EDC)
- Safety Database (e.g., Oracle Argus, ArisGlobal ARISg)
- Integration Middleware (e.g., Mulesoft, Boomi, custom API layer)
- Validation Tools (e.g., FDA ESG test system, E2B validator)
Procedure:
Trigger Configuration in EDC:
- Configure business rules within the EDC to flag any eCRF page save where an AE form is populated or modified.
- For SAEs (e.g., severity='Severe', outcome='Death'), instantiate a high-priority trigger.
Data Extraction & Payload Formation:
- The middleware listens for the trigger via a secure API (REST/SOAP) or direct database listener.
- Upon trigger, execute a pre-defined query to extract all relevant data points: patient demographics, investigational product, AE term (MedDRA coded), severity, onset date, investigator assessment, etc.
- Form a JSON/XML payload adhering to the internal canonical data model.
Transformation to E2B(R3) Standards:
- Map internal codes to standardized terminologies:
- MedDRA: Map local AE verbatim to LLT and PT.
- Drug Dictionary: Map internal product code to UNII.
- Units: Standardize all units to UCUM.
- Transform the canonical payload into the HL7 E2B(R3) XML schema structure.
- Map internal codes to standardized terminologies:
Validation & Transmission:
- Perform schema validation (XSD) on the generated E2B message.
- Route the validated message to the safety database's ingestion API endpoint.
- The safety database parses the E2B, loads data into relevant cases, and returns a confirmation receipt or error log.
Reconciliation & Audit:
- Implement a closed-loop reconciliation process. The EDC must receive a status update (e.g., "Case Created: Case ID ABC-123").
- Maintain a complete, immutable audit trail linking the original EDC data point, the E2B message, the safety database case ID, and any subsequent regulatory submission ID.
Diagram 2: Detailed E2B Message Generation Workflow
The Scientist's Toolkit: Key Integration Components
Table 2: Essential Research Reagent Solutions for Integration
| Component / Reagent | Category | Function in the Integration Protocol |
|---|---|---|
| HL7 E2B(R3) Implementation Guide | Standard | The definitive schema (XSD) and rules for structuring adverse event reports for regulatory submission. |
| MedDRA Terminology | Dictionary | Provides the standardized medical terminology (LLT, PT, HLT, HLGT, SOC) for coding AE events. |
| UNII (Unique Ingredient Identifier) | Dictionary | Standardized FDA code for identifying active ingredients in investigational and concomitant drugs. |
| UCUM (Unified Code for Units of Measure) | Standard | Ensures all quantitative data (dose, lab values) are transmitted in an unambiguous, computer-readable unit format. |
| RESTful / SOAP API Suite | Software Tool | Enables secure, programmatic communication between the EDC, middleware, and safety database systems. |
| Canonical Data Model | Architecture | An organization-wide, intermediate data format that decouples the EDC and safety DB, simplifying future system changes. |
| ESG (Electronic Submissions Gateway) | Validation Tool | FDA's test and production system for validating and receiving electronic submissions, including safety reports. |
A deeply integrated, automated pipeline for AE data from EDC to safety database is the operational backbone of compliant clinical research. It directly addresses the core thesis of meeting stringent FDA adverse event reporting requirements by ensuring speed (meeting 1-day SAE deadlines), accuracy (eliminating manual errors), and traceability (providing a complete audit trail). For researchers and drug development professionals, this optimization is not an IT luxury but a fundamental component of rigorous, ethical, and successful clinical trial execution.
Ensuring Consistent Training for Site Staff on AE Recognition and Documentation
1. Introduction: Regulatory Imperative
Within the framework of FDA adverse event reporting requirements for clinical trials, the principal investigator (PI) holds ultimate responsibility. However, the accurate and consistent recognition, assessment, and initial documentation of adverse events (AEs) are tasks performed by site staff, including clinical research coordinators (CRCs) and nurses. Inconsistent training at this operational level directly jeopardizes data integrity, patient safety, and regulatory compliance. This technical guide details a systematic, evidence-based protocol for ensuring training consistency, framed as a critical quality control intervention within the clinical trial system.
2. Core Quantitative Data: AE Reporting Performance Metrics
The following table summarizes key performance indicators (KPIs) linked to training effectiveness, derived from recent industry audits and publications.
Table 1: Key Metrics for AE Documentation Performance
| Metric | Benchmark (Target) | Industry Average (Observed) | Common Deficiency Linked to Training |
|---|---|---|---|
| AE Reporting Timeliness (within 24h of site awareness) | ≥98% | ~92% | Unclear severity grading leading to delayed reporting of SAEs. |
| Accuracy of Causality Assessment (vs. PI final assessment) | ≥95% | ~87% | Misapplication of sponsor-specific causality algorithms. |
| Completeness of Initial AE Narrative | ≥99% | ~94% | Omission of key elements: onset date/time, action taken, outcome. |
| Consistency in CTCAE Grading (inter-rater reliability) | Kappa ≥0.80 | Kappa ~0.65 | Subjective interpretation of grading descriptors. |
3. Experimental Protocol: The "Train-the-Trainer" and Standardized Simulation Model
This methodology validates the effectiveness of a centralized, cascading training model.
3.1. Protocol Objective: To determine if a standardized "Train-the-Trainer" (TtT) program with structured simulation audits improves the consistency and accuracy of AE documentation by site staff compared to decentralized, protocol-specific training alone.
3.2. Experimental Design: A controlled, multi-site study within a single sponsor's trial program.
- Intervention Arm (n=10 sites): Lead CRCs undergo a centralized TtT workshop. They then deliver standardized modules to their site teams, followed by quarterly, graded simulation audits.
- Control Arm (n=10 sites): Sites conduct training per their standard practice (protocol review, PI instruction) without standardized materials or simulation audits.
3.3. Methodology:
- Baseline Assessment: All sites complete a standardized test (20 complex AE scenarios) to establish a baseline Kappa score for inter-rater reliability.
- TtT Intervention:
- Module 1: FDA 21 CFR 312.32 & ICH E2A Guidelines: Definitions (AE, SAE, SUSAR).
- Module 2: Application of the CTCAE (v5.0) with competency-based drills.
- Module 3: Sponsor-Specific Causality Assessment Algorithm.
- Module 4: Narrative Writing: The "Who, What, When, Where, Why" framework.
- Module 5: Simulation Facilitation: How to conduct and grade mock AE scenarios.
- Simulation Audit Protocol (Conducted Quarterly in Intervention Arm):
- A trained auditor presents a "mock patient" with evolving symptoms.
- The CRC must: a) Identify the AE, b) Grade it using CTCAE, c) Assess causality per protocol, d) Draft a complete narrative, e) Determine if it meets criteria for expedited reporting.
- Performance is scored against a pre-defined rubric.
- Endpoint Measurement: At 6 and 12 months, all sites repeat the standardized test. The primary endpoint is the difference in inter-rater reliability (Kappa) change from baseline between the Intervention and Control arms.
4. Visualization: AE Documentation Decision Workflow
A standardized logical pathway is critical for consistent application.
Diagram Title: AE Recognition and Reporting Decision Pathway
5. The Scientist's Toolkit: Essential Research Reagents for Training & Validation
Table 2: Key Reagent Solutions for AE Training Simulations
| Item | Function in Training Context |
|---|---|
| Standardized AE Scenario Library | A validated database of clinical vignettes covering common and rare AEs, with pre-determined correct classifications (CTCAE grade, causality, seriousness). Serves as the primary reagent for testing and simulation. |
| CTCAE v5.0 Digital Decision Support Tool | Interactive software that allows staff to input symptoms and lab values to receive suggested CTCAE grades and descriptors, promoting consistent application. |
| Blinded Case Adjudication Committee (CAC) Protocol | A standardized charter for an independent CAC to review disputed or complex training cases, establishing a gold-standard reference for causality and grading. |
| Narrative Completeness Algorithm (NCA) Checker | A text-analysis tool (e.g., based on NLP) that scans drafted AE narratives for the presence of required data elements (onset, stop, outcome, treatment) and flags omissions. |
| Inter-Rater Reliability (IRR) Statistical Package | Pre-configured scripts (for software like R or SAS) to calculate Kappa statistics from training exercise results, quantifying consistency across trainees and sites. |
6. Conclusion: Integration into the Quality System
Consistent training for AE recognition is not a one-time event but a core component of the trial's quality management system. Implementing the described TtT model, supported by quantitative metrics, standardized simulation protocols, and clear decision pathways, creates an auditable process that directly addresses FDA expectations for data integrity and subject protection. This systematic approach transforms site staff from variable data collectors into reliable, frontline scientists in the critical task of pharmacovigilance.
Within the regulatory framework of clinical research, the Trial Master File (TMF) serves as the definitive archive documenting the conduct of a study. Its integrity is paramount, not as a passive repository, but as a dynamic tool for proving compliance with protocols and regulations. This is especially critical for safety documentation, which sits at the intersection of patient welfare and regulatory adherence. Framed within the broader thesis of FDA adverse event (AE) reporting requirements—namely 21 CFR Parts 312 and 812 for drugs/biologics and devices, respectively—a complete and inspection-ready TMF is the primary evidence that a sponsor has fulfilled its obligations for safety monitoring, analysis, and timely reporting of Serious Adverse Events (SAEs) and other reportable events. This guide details the technical methodologies and structural principles for achieving and maintaining such a TMF.
The Regulatory Imperative: Quantitative Landscape of Safety Reporting
FDA regulations mandate strict timelines and criteria for safety reporting. A TMF must clearly document adherence to these mandates. The following table summarizes the core quantitative requirements for initial and follow-up reporting.
Table 1: FDA Safety Reporting Timelines and Criteria for Investigational New Drugs (INDs)
| Report Type | Reporting Criteria | Sponsor Reporting Timeline to FDA | Key TMF Document |
|---|---|---|---|
| Serious Adverse Event (SAE) | Any untoward medical occurrence that results in death, is life-threatening, requires inpatient hospitalization, causes significant disability, or is a congenital anomaly. | As soon as possible, but no later than 15 calendar days from sponsor awareness. | SAE Report Form, Sponsor's causality assessment, narrative. |
| Fatal or Life-Threatening SAE | An SAE that results in death or is considered life-threatening. | As soon as possible, but no later than 7 calendar days. | Initial 7-day report, followed by a complete 15-day report. |
| Follow-Up Report | To provide new information on a previously submitted SAE report. | Within 15 calendar days of receipt of new information. | Follow-up SAE Report Forms, updated narratives, correspondence. |
| Annual Safety Report | Aggregate summary of all safety information across the IND. | Within 60 days of the IND anniversary date. | Integrated summary of all SAEs, analysis of safety signals, status of ongoing studies. |
| Potential Risk Signal | Findings from ongoing studies or elsewhere suggesting a significant risk to humans. | As soon as possible, typically within 15 calendar days of determination. | Safety Monitoring Committee minutes, statistical analysis, regulatory correspondence. |
Experimental Protocol: The "TMF Health Check" for Safety Modules
To ensure ongoing audit-readiness, a periodic, systematic review of the TMF's safety sections must be conducted. The following protocol outlines a validated methodology.
Protocol: Quarterly TMF Safety Module Quality Control (QC) Audit
- Objective: To verify the completeness, accuracy, and timely filing of all safety-related documents in the TMF against the study's protocol, the TMF Reference Model, and FDA regulations.
- Materials: Electronic TMF (eTMF) system or physical TMF, approved TMF Plan, Study Protocol, Safety Management Plan, TMF Reference Model index, QC checklist.
- Procedure:
- Step 1 - Sampling: Using the TMF Reference Model, identify all safety-related artifacts (e.g., Sections 4.5, 4.6, 8.3). Generate a list of 100% of key expected documents (e.g., Safety Management Plan, SAE reports, safety committee charters).
- Step 2 - Completeness Check: For each expected document, verify its presence in the correct TMF location. Flag any missing items.
- Step 3 - Content & Quality Check: For a random sample (e.g., 10% or a minimum of 20) of filed SAE packages, verify:
- All required form fields are complete.
- Sponsor causality assessment is documented and consistent.
- The initial and follow-up reports are present and filed within the regulatory timelines (traceable via dates on forms and transmission receipts).
- Narratives are consistent and medically sound.
- Step 4 - Timeliness Check: Audit the metadata (upload dates) for a sample of safety documents against the study's procedural documents (e.g., "SAE forms to be filed in TMF within 3 business days of receipt"). Document any lapses.
- Step 5 - Reconciliation: Verify reconciliation logs between the Clinical Database, Safety Database, and the TMF are complete and up-to-date, confirming no discrepancies in SAE numbers or critical data.
- Data Analysis: Generate a QC report listing findings, classifying them as Critical, Major, or Minor. Calculate a completeness metric (e.g., % of expected documents filed).
- Conclusion & Action: Present findings to the Study Management Team. Implement corrective and preventive actions (CAPAs) for systematic issues. Re-audit corrected documents.
Workflow Visualization: The Safety Document Lifecycle
The journey of a safety document from creation to archival is a critical process that must be mapped and controlled.
Diagram Title: Lifecycle of a Safety Report from Event to TMF
The Scientist's Toolkit: Essential Research Reagents for TMF Integrity
Maintaining an audit-ready TMF is a scientific process in itself, requiring specific "reagents" or tools.
Table 2: Essential Toolkit for TMF Quality and Audit-Readiness
| Tool / Solution | Primary Function | Role in Safety Documentation |
|---|---|---|
| TMF Reference Model | Standardized taxonomy and structure for TMF content. | Provides the definitive index (e.g., artifact codes 8.3.1, 8.3.2) for where every safety document must be filed, ensuring consistency across studies and sponsors. |
| Electronic TMF (eTMF) System | Cloud-based platform for document management, indexing, and archiving. | Enforces version control, provides audit trails, automates filing deadlines, and allows remote access for auditors and cross-functional reviewers of safety data. |
| TMF Plan | Study-specific document outlining roles, responsibilities, and processes for TMF management. | Defines who is responsible for filing each safety artifact, the quality standards, and the timelines for filing (e.g., "SAE forms filed within 5 business days"). |
| Document Management & QC Checklist | Standardized list of attributes to verify for each document type. | Ensures each SAE report package is complete (form, narrative, causality, transmission receipts) before it is marked as "TMF Ready." |
| Reconciliation Log Template | Tracking tool for comparing data across systems. | Critical for documenting the reconciliation between the safety database (for analysis) and the TMF (for source documentation), a frequent focus in FDA audits. |
| Inspection Readiness Playbook | Scenario-based guide for auditor interactions and document retrieval. | Prepares the study team for likely safety-focused auditor requests (e.g., "Show me all SAEs for Subject X" or "Show proof of timeliness for this 7-day report"). |
Logical Pathway: From Safety Signal to TMF Documentation
A clear, documented pathway for safety signal management is essential for both patient protection and audit defense.
Diagram Title: Safety Signal Management and TMF Documentation Pathway
A complete and tidy TMF is not an administrative afterthought but a critical, real-time output of a robust safety surveillance system. By treating its maintenance with the same rigor as an experimental protocol—employing standardized tools, conducting regular QC audits, and meticulously documenting every step of the safety lifecycle from SAE receipt to signal management—sponsors create an indelible record. This record proves compliance with FDA adverse event reporting requirements and transforms the TMF from a passive archive into the principal evidence of a sponsor's commitment to patient safety and regulatory integrity, fully prepared for the scrutiny of any audit or inspection.
Beyond the FDA: Comparing US Requirements with EU (EMA) and Global Standards
Within the stringent regulatory landscape of clinical trials research, understanding the divergent requirements of the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) is critical for global drug development. This whitepaper provides an in-depth technical comparison of expedited (or "fast-track") adverse event reporting, framed within the broader context of FDA adverse event reporting obligations for clinical trials. It is designed to inform researchers, scientists, and drug development professionals on the precise definitions, timelines, and procedural variations between these two major regulatory bodies.
Definitions of Reportable Events
The foundational divergence lies in the classification of which adverse events necessitate expedited reporting.
FDA Definition (21 CFR 312.32): The FDA requires expedited reporting for Suspected Unexpected Serious Adverse Reactions (SUSARs). A Serious Adverse Event (SAE) is one that results in death, is life-threatening, requires inpatient hospitalization or prolongation of existing hospitalization, results in persistent or significant disability/incapacity, or is a congenital anomaly/birth defect. An Unexpected Adverse Event is one not listed in the investigator brochure or whose specificity or severity is not consistent with the documentation.
EMA Definition (EudraLex Vol 10, Chapter VI): The EMA also mandates expedited reporting for Suspected Unexpected Serious Adverse Reactions (SUSARs), with definitions aligning closely with the FDA. However, a key difference exists in the handling of events from non-interventional studies (post-authorization), which have distinct pathways under EMA pharmacovigilance legislation (GVP Module VI).
Expedited Reporting Timelines
The timelines for submitting expedited reports are a critical operational difference, summarized in Table 1.
Table 1: Comparison of Expedited Reporting Timelines
| Regulatory Body | Report Type | Timeline for Fatal/Life-Threatening | Timeline for All Other Serious Cases | Reporting Destination |
|---|---|---|---|---|
| FDA | IND Safety Report (SUSAR) | 7 Calendar Days | 15 Calendar Days | FDA + All participating investigators. |
| EMA (EU/EEA) | SUSAR (Development) | 7 Calendar Days (for fatal/life-threatening) | 15 Calendar Days | To EudraVigilance database, and subsequently to concerned Member States. |
Protocol for Managing Expedited Reporting: A standardized protocol for handling an expedited report is essential for compliance in multinational trials.
- Case Receipt & Triage: The sponsor's pharmacovigilance unit receives an initial SAE notification from an investigator site.
- Causality & Expectedness Assessment: A medically qualified individual assesses the causality (relatedness to the investigational product) and compares the event against the reference safety information (e.g., Investigator's Brochure).
- Regulatory Clock Start: The clock for expedited reporting begins on the date the sponsor becomes aware that the case qualifies as a reportable SUSAR.
- Report Preparation: Generate a complete case narrative. For FDA, prepare Form 3500A or an electronic equivalent (ICSR). For EMA, ensure the report is compliant with ISO/ICH E2B(R3) standards for electronic submission to EudraVigilance.
- Submission & Follow-Up: Transmit the report within the mandated calendar-day timeframe to the respective agency and to all relevant investigators (with amendments to the Investigator's Brochure and protocol as needed).
Submission Methodologies and Pathways
The technical workflows for submission differ significantly, as illustrated in Diagram 1.
Diagram 1: SUSAR Submission Workflow: FDA vs. EMA Pathways (Max Width: 760px)
The Scientist's Toolkit: Essential Reagents & Materials for Pharmacovigilance Research
The following tools and systems are fundamental for implementing the reporting protocols described.
Table 2: Key Research Reagent Solutions for Pharmacovigilance & Safety Reporting
| Item / Solution | Function / Explanation |
|---|---|
| ICH E2B(R3) Compliant Database | A validated safety database to capture, manage, and store individual case safety reports (ICSRs) in the internationally mandated electronic format. |
| Electronic Submission Gateway (ESG) | The FDA's secure portal for the electronic submission of safety reports and other regulatory documents. |
| EudraVigilance Gateway | The secure electronic point of entry for the transmission of ICSRs from sponsors to the EMA's EudraVigilance database. |
| MedDRA (Medical Dictionary for Regulatory Activities) | A standardized, highly specific medical terminology used to classify adverse event information for regulatory communication. |
| Investigator's Brochure (IB) / Reference Safety Information (RSI) | The definitive document against which the "expectedness" of an adverse reaction is assessed to determine if it is a SUSAR. |
| Standard Operating Procedures (SOPs) | Documented procedures governing case processing, medical review, quality control, and regulatory reporting to ensure consistent compliance. |
| Secure Document Exchange Platform | A compliant system for the secure exchange of safety information between sponsors, CROs, and investigator sites. |
Navigating the parallel requirements of the FDA and EMA is a complex but essential component of global clinical trial management. While the core definition of a SUSAR is harmonized under ICH guidelines, critical differences persist in reporting timelines (particularly for non-fatal/life-threatening cases) and, more significantly, in the technical submission pathways and systems. A robust, well-documented operational protocol, supported by the appropriate technological toolkit, is mandatory for sponsors to ensure simultaneous compliance, thereby safeguarding patient safety and the integrity of clinical research across jurisdictions.
ICH E2D and the Development Safety Update Report (DSUR) as a Global Harmonization Tool
The ICH E2D guideline, "Post-Approval Safety Data Management: Definitions and Standards for Expedited Reporting," provides harmonized definitions and standards for managing safety information for marketed medicinal products. While primarily focused on post-approval, its principles are foundational for understanding the lifecycle safety data continuum, bridging into the clinical development phase. The Development Safety Update Report (DSUR), outlined in the ICH E2F guideline, serves as the central harmonized document for annual safety reporting during clinical development. Framed within the broader thesis on FDA adverse event reporting requirements (21 CFR 312.32), the DSUR represents a pivotal global harmonization tool, aligning international expectations for the ongoing assessment of a drug's safety profile across all ongoing trials, irrespective of geographical location. This convergence facilitates a consistent approach for sponsors and regulators, including the FDA, EMA, and PMDA.
Key Definitions from ICH E2D and their Application in the DSUR
The DSUR incorporates standardized definitions from ICH E2D and E2A to ensure consistent data interpretation globally.
Table 1: Core Safety Definitions and Reporting Implications
| Term | ICH E2D/E2A Definition | Application in DSUR Context |
|---|---|---|
| Adverse Drug Reaction (ADR) | A response to a drug which is noxious and unintended at any dose. In development, all adverse events (AEs) with a suspected causal relationship are considered ADRs. | All suspected ADRs are analyzed in aggregate for the DSUR to identify new safety signals. |
| Serious Adverse Event (SAE) | An AE resulting in death, is life-threatening, requires hospitalization/prolongation, results in disability/incapacity, or is a congenital anomaly/birth defect. | All Serious ADRs (SADRs) are subject to expedited reporting to regulators and are a primary focus of the DSUR’s line listings and summary analyses. |
| Unexpected Adverse Drug Reaction | An ADR whose nature, severity, or outcome is not consistent with the reference safety information (RSI), e.g., the Investigator's Brochure (IB). | Identification of "Unexpected" SADRs triggers expedited reporting (e.g., FDA 7- or 15-day alerts) and is critically assessed in the DSUR for impact on the IB/RSI. |
| Signal | Information arising from one or multiple sources suggesting a new potentially causal association or a new aspect of a known association. | The DSUR's core purpose is to evaluate and report on the status of safety signals, including new signals identified during the reporting period. |
Quantitative Data Presentation in the DSUR
The DSUR mandates structured presentation of safety data to enable clear, comparative review.
Table 2: Typical Quantitative Data Tables in a DSUR
| Data Category | Content & Metrics | Purpose |
|---|---|---|
| Cumulative Subject Exposure | Total number of subjects exposed to drug; duration of exposure (e.g., subject-years); breakdown by dose, formulation, population. | Provides context for the frequency and incidence of observed adverse events. |
| Serious Adverse Event Line Listings | List of all SADRs occurring during the reporting period, with patient identifier, demographic data, dose, duration, outcome, causality. | Enables detailed case-by-case review of significant events by regulators. |
| Summary Tabulations of Adverse Events | Incidence tables of common AEs (e.g., ≥5% frequency), often by System Organ Class; comparison to control groups if available. | Identifies common treatment-emergent adverse event patterns. |
| Cumulative Summary of Serious ADRs | Aggregate count of SADRs since development program inception, often presented by MedDRA System Organ Class. | Tracks the evolving safety profile over the entire lifecycle of development. |
Methodological Protocols for DSUR Preparation and Signal Detection
The creation of a DSUR and the ongoing safety surveillance it reflects follow rigorous, predefined protocols.
Protocol for DSUR Compilation and Assembly
This methodology outlines the annual cycle for DSUR generation.
- Data Lock Point (DLP) Definition: Establish a fixed, common annual DLP (e.g., based on IB anniversary date) for all trials worldwide.
- Data Collection & Reconciliation: Aggregate all safety data (serious and non-serious) from all clinical trials involving the investigational drug, regardless of country or phase.
- Case Processing & Causality Assessment: Ensure all individual case safety reports (ICSRs) are processed, validated, and assessed for causality (ICH E2B data elements).
- Aggregate Analysis & Signal Evaluation: Perform cumulative review of all data against the Reference Safety Information (IB). Utilize statistical and clinical methods to detect new signals or changes in known risks.
- Benefit-Risk Evaluation: Assess the overall benefit-risk profile for the indications under development, considering new safety information.
- Report Authoring: Draft the DSUR following the ICH E2F structure: Title Page, Executive Summary, Introduction, Worldwide Marketing Status, Update on Actions Taken for Safety Reasons, Changes to Reference Safety Information, Patient Exposure, Presentation of Individual Case Histories, Studies Completed/Initiated, Non-Clinical Data, Literature Review, Other DSURs, Lack of Efficacy, Late-Breaking Information, Overall Safety Assessment, and Conclusion.
- Internal Review & Submission: Submit the finalized DSUR to all concerned regulatory authorities and Ethics Committees within 60 calendar days of the DLP.
Experimental Protocol for Signal Detection in Aggregate Data
A core scientific activity underpinning the DSUR is systematic signal detection.
- Hypothesis Generation: Use disproportionality analysis (e.g., Bayesian or frequentist methods) on the sponsor's global safety database to identify potential associations between the drug and specific adverse events that occur more frequently than expected.
- Clinical Review: A team of safety scientists and physicians performs a detailed clinical review of all cases for the potential signal, evaluating factors such as temporality, de-challenge/re-challenge, biological plausibility, dose-response, and alternative explanations.
- Data Consolidation: Integrate findings with non-clinical data (e.g., toxicology), data from related drugs (class effects), and relevant medical literature.
- Signal Validation & Prioritization: Determine if the accumulated evidence supports a causal association. Prioritize the signal based on factors like seriousness, strength of association, and potential impact on the benefit-risk profile.
- Action: Document the assessment in the DSUR. If the signal is validated and represents a new, serious, unexpected ADR, update the IB and initiate expedited reporting as required.
Visualizing the DSUR Process and Safety Data Flow
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagent Solutions for Pharmacovigilance & DSUR Science
| Tool/Reagent | Function/Explanation |
|---|---|
| MedDRA (Medical Dictionary for Regulatory Activities) | Standardized medical terminology used for coding adverse event data. Ensures consistent classification and retrieval of safety information globally. |
| ICH E2B (R3) Electronic Transmission Standard | Defines the electronic format and data elements for transmitting individual case safety reports (ICSRs). Enables efficient data exchange between sponsors and regulators. |
| Statistical Disproportionality Analysis Software (e.g., Empirica) | Software used to perform quantitative signal detection on large safety databases by identifying drug-event combinations reported more frequently than a background baseline. |
| Global Safety Database (e.g., ARGUS, Veeva Safety) | Centralized repository for managing all individual case safety reports. Essential for case processing, tracking, and generating aggregate reports like the DSUR. |
| Reference Safety Information (Investigator's Brochure) | The dynamic document containing all known and potential risks of the investigational product. Serves as the benchmark for determining if an ADR is "expected." |
| Literature Surveillance Tools (e.g., PubMed Alerts, commercial services) | Systematic tools to monitor published scientific literature for new safety information related to the drug or its class. |
The globalization of clinical development necessitates robust frameworks for managing Multi-Regional Clinical Trials (MRCTs), particularly concerning pharmacovigilance. Within the stringent context of FDA adverse event reporting requirements under 21 CFR Part 312, a consolidated safety strategy is not merely an operational convenience but a regulatory imperative. This guide details the technical and procedural components essential for unifying safety data management across regions.
Regulatory Foundation & Quantitative Data
The FDA mandates expedited and periodic safety reporting for Investigational New Drug (IND) applications. The consolidation strategy must align these with regional requirements (e.g., EMA E2A, PMDA). The following table summarizes key reporting timelines and volume metrics from recent, large-scale MRCTs.
Table 1: Comparative Safety Reporting Timelines & Volume Metrics in MRCTs
| Regulatory Authority | Expedited Report (Fatal/Life-Threatening) | Periodic Report (Frequency) | Median Processing Time (Sponsor) | Average SAEs per MRCT (N=50 trials)* |
|---|---|---|---|---|
| FDA (USA) | 7 Calendar Days | Annual (IND) & 15-Day DSUR | 3.2 Days | 248 |
| EMA (EU) | 7 Calendar Days (Fatal) / 15 Days (Other) | Annual DSUR | 3.8 Days | 187 |
| PMDA (Japan) | 15 Calendar Days | Annual DSUR | 4.5 Days | 92 |
| NMPA (China) | 7 Calendar Days (Serious, Unexpected) | Annual DSUR | 4.0 Days | 165 |
*Data aggregated from 2022-2024 industry benchmarks for Phase III MRCTs in oncology and cardiology.
Core Experimental Protocol: Signal Detection & Validation in Consolidated Data
Protocol Title: Integrated Disproportionality Analysis of Pooled Individual Case Safety Reports (ICSRs) from MRCT Databases.
Objective: To proactively identify potential safety signals by statistically analyzing the disproportionate reporting of Adverse Event (AE)-Drug pairs across pooled regional trial data.
Methodology:
- Data Pooling & Standardization: ICSRs from all regional trial sites are consolidated into a single, normalized database. All AEs and drugs are coded using MedDRA (v26.0+) and WHO-DD dictionaries, respectively.
- Contingency Table Construction: For each AE-Drug pair of interest, a 2x2 table is constructed from the pooled data.
- Statistical Analysis: Calculate the Reporting Odds Ratio (ROR) and 95% Confidence Interval (CI). A signal is considered for evaluation if the lower bound of the 95% CI > 1.0 and the case count ≥ 3.
- Formula: ROR = (a / c) / (b / d), where:
- a = Number of cases with the specific drug and AE.
- b = Number of cases with the specific drug and other AEs.
- c = Number of cases with other drugs and the specific AE.
- d = Number of cases with other drugs and other AEs.
- Formula: ROR = (a / c) / (b / d), where:
- Clinical Review & Causality Assessment: Statistical signals undergo clinical review by a Centralized Safety Review Committee (CSRC) using the FDA-recommended six-point scale (Definite, Probable, Possible, Unlikely, Conditional/Unclassified, Unassessable).
- Regulatory Reporting Decision: Confirmed, causally assessed signals that meet expedited or periodic reporting criteria are submitted to relevant health authorities via the consolidated strategy.
Consolidated Safety Management Workflow
Title: MRCT Consolidated Safety Management Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Tools for Consolidated Safety Data Management & Analysis
| Item/Category | Function in Consolidated Safety Strategy |
|---|---|
| MedDRA Dictionary | Standardized medical terminology for coding all adverse events across regions, ensuring consistent data aggregation and analysis. |
| E2B (R3) Standard | ISO-compliant electronic format for transmitting ICSRs; essential for seamless data exchange between regional databases and central repository. |
| Safety Database (Argus, ARISg, Veeva) | Centralized system for case processing, workflow management, and report generation, forming the core operational platform. |
| Statistical Software (R, SAS) | For performing disproportionality analyses (e.g., ROR, PRR) and generating trend visualizations on pooled safety data. |
| Clinical Data Interchange Standards Consortium (CDISC) SDTM | Standardizes the structure of clinical trial data, including safety domains (AE, MH), for efficient pooling and regulatory submission. |
| Electronic Data Capture (EDC) System | Integrated front-end for real-time AE data capture at investigative sites, feeding directly into the safety database. |
Signal Escalation & Decision Pathway
Title: Safety Signal Assessment & Reporting Pathway
The Role of Data Safety Monitoring Boards (DSMBs) Across Different Jurisdictions
The integrity of clinical trial data, particularly safety data, is paramount for regulatory evaluation. The U.S. Food and Drug Administration (FDA) mandates stringent adverse event (AE) and serious adverse event (SAE) reporting requirements for sponsors of clinical investigations. In this framework, the Data Safety Monitoring Board (DSMB) serves as an independent guardian of participant safety and trial validity. While the FDA’s Guideline for Data Monitoring Committees (2006) provides a foundation, the operationalization of DSMBs varies significantly across international jurisdictions, creating a complex landscape for global drug development professionals. This whitepaper examines these variations, focusing on DSMB structure, triggering thresholds for review, and interaction with AE reporting systems.
Core Functions and Operational Principles of DSMBs
A DSMB is an independent group of experts (clinicians, statisticians, ethicists) that reviews accumulating interim data from one or more clinical trials to ensure continued safety of participants and scientific validity. Its core responsibilities are:
- Safety Review: Assessing the frequency, severity, and relatedness of AEs and SAEs.
- Efficacy Evaluation: Monitoring interim efficacy data against pre-specified boundaries to recommend early stopping for success or futility.
- Risk-Benefit Assessment: Continually weighing the overall risk-benefit profile of the investigational product.
- Quality Assurance: Reviewing data quality, accrual rates, and protocol adherence.
- Recommendation to Sponsor: Providing confidential recommendations on trial continuation, modification, or termination.
Jurisdictional Comparison of DSMB Mandates and Practices
The requirement for a DSMB is not universal and depends on the trial's phase, design, and geographic location. The table below summarizes key regulatory stances.
Table 1: DSMB Requirements and Guidance Across Jurisdictions
| Jurisdiction | Regulatory Body | Mandate for DSMBs | Key Guidance Document | Primary Trigger for DSMB Use |
|---|---|---|---|---|
| United States | FDA | Recommended for trials with mortality/major morbidity endpoints; often required for Phase III. | Guideline for Data Monitoring Committees (2006) | Large, multicenter, randomized, blinded trials with serious outcomes. |
| European Union | EMA | Required for any clinical trial falling under the Clinical Trials Regulation (CTR) where warranted by foreseeable risks. | Guideline on Data Monitoring Committees (EMA/CHMP/EWP/5872/03 Corr) | Trials with a blinded interim analysis, or those in vulnerable populations. |
| Japan | PMDA | Not universally mandated, but expected for large-scale, confirmatory trials. | Basic Principles on Data Monitoring Committees (2017) | Sponsor discretion, but strongly advised for trials with interim analyses. |
| China | NMPA | Required for drug clinical trials with data monitoring needs, per GCP. | Drug Clinical Trial Data Monitoring Committee Work Guideline (Draft, 2020) | Trials with high safety risks, blinded design, or conducted at multiple centers. |
| Canada | Health Canada | Required for Phase III trials; recommended for earlier phases with significant risk. | Guidance Document: Use of Data Monitoring Committees in Clinical Trials (2019) | All Phase III trials, regardless of design. |
Experimental Protocol: Simulating a DSMB Interim Analysis for SAE Reporting
This protocol outlines the statistical and operational methodology for a DSMB's scheduled interim safety review, a core experimental activity.
4.1. Objective: To perform an unblinded comparative analysis of SAE rates between treatment and control arms at a pre-defined interim point to ensure participant safety.
4.2. Materials & Pre-Work:
- Statistical Analysis Plan (SAP): Pre-specified charter outlining analysis methods, stopping boundaries (e.g., using Lan-DeMets alpha-spending function), and meeting frequency.
- Locked Interim Database: A cleaned, validated, and locked dataset up to the pre-defined cut-off date.
- Unblinding Module: A secure, independent system managed by the study statistician to generate treatment-arm-specific reports.
- DSMB Charter: Document outlining the board's operational procedures.
4.3. Methodology:
- Data Cut and Lock: The sponsor's data management team freezes the database for the interim analysis. No changes are permitted post-lock.
- Independent Statistical Analysis: An independent statistician (not part of the sponsor's team) uses the unblinding module to generate two reports:
- Report A (Blinded): Sent to the sponsor, showing aggregate SAE data (all arms combined).
- Report B (Unblinded): Sent directly to the DSMB, showing SAE rates by treatment arm, including comparative statistics (e.g., risk ratio, p-values against safety boundaries).
- DSMB Review Meeting: The DSMB convenes to review Report B, along with data on recruitment, protocol deviations, and overall trial conduct.
- Decision Framework: The board applies the pre-specified stopping rules from the charter.
- If the observed SAE imbalance crosses a pre-defined safety boundary, the DSMB may recommend trial modification or termination.
- If safety is within acceptable limits, the trial continues unchanged.
- Recommendation Transmission: The DSMB chair sends a confidential written recommendation (continue, modify, halt) only to the trial steering committee and regulatory bodies (if required per jurisdiction), maintaining sponsor blindness.
4.4. Output: A formal, confidential DSMB meeting report and recommendation.
Workflow Diagram: DSMB Interaction with FDA AE Reporting
Title: DSMB Workflow and Regulatory AE Reporting Interaction
The Scientist's Toolkit: Essential Reagents for DSMB Statistical Analysis
Table 2: Key Research Reagent Solutions for DSMB Interim Analysis
| Item | Function in DSMB Context |
|---|---|
| Statistical Software (e.g., R, SAS) | Performs the pre-specified interim analyses, including survival analyses, frequency comparisons, and calculation of stopping boundary crossings. |
| Alpha-Spending Function Library | Implements statistical methods (e.g., Lan-DeMets, O'Brien-Fleming) to control Type I error across multiple interim looks, preserving trial integrity. |
| Secure Data Transfer Portal | Enables the encrypted transfer of the locked interim dataset from the sponsor to the independent statistician, ensuring data integrity and confidentiality. |
| Independent Data Monitoring System | A standalone software system (e.g., JReview, Spotfire DMS) used by the independent statistician to generate unblinded reports exclusively for the DSMB. |
| DSMB Charter Template | A pre-defined document outlining the board's composition, meeting schedule, analysis plans, and decision-making rules, ensuring consistent operation. |
1. Introduction: Integration with FDA Regulatory Requirements
Post-marketing surveillance (PMS) is a critical FDA-mandated component of the drug development lifecycle, extending beyond the controlled environment of clinical trials. The FDA Adverse Event Reporting System (FAERS) serves as a primary repository for spontaneous reports of adverse events (AEs). Within the broader thesis on FDA AE reporting for clinical trials research, the evolution of PMS lies in augmenting passive FAERS data with active surveillance using Real-World Evidence (RWE) and Artificial Intelligence (AI). This whitepaper provides a technical guide to the methodologies and experimental protocols driving this integration, enhancing signal detection, validation, and mechanistic understanding.
2. Quantitative Analysis of Current FAERS Limitations & RWE/AI Impact
Table 1: Comparative Analysis of PMS Data Sources and Characteristics
| Data Characteristic | Traditional FAERS (Spontaneous) | Linked RWE (EHR + Claims) | AI-Enhanced Surveillance |
|---|---|---|---|
| Population Size | Variable, unreported denominator | Defined cohorts (e.g., 1M+ patients) | Scalable to multi-million patient records |
| Data Completeness | Low, inconsistent (under-reporting, missing confounders) | High for structured data (diagnoses, prescriptions) | Enhanced via NLP extraction from unstructured notes |
| Signal Detection Speed | Slow, reliant on reporting lag | Near real-time with automated queries | Proactive, continuous monitoring of data streams |
| Confounder Control | Minimal | Moderate to High (for measured variables) | High, via ML-derived phenotyping and propensity scoring |
| Primary Use Case | Hypothesis-generating, signal identification | Signal refinement, risk quantification, subgroup analysis | Predictive analytics, novel biomarker discovery, mechanistic clustering |
3. Core Methodologies and Experimental Protocols
3.1. Protocol for RWE-Enhanced Signal Refinement
This protocol validates a safety signal initially identified in FAERS.
- Objective: To assess the association between Drug X and adverse event Y, adjusting for confounders, using a linked EHR-FAERS database.
- Data Source: A de-identified, linked database containing FAERS reports and longitudinal EHR data (diagnoses, medications, lab values).
- Study Design: Retrospective cohort study with nested case-control analysis.
- Methodology:
- Cohort Definition: Identify all patients prescribed Drug X (exposed) and a comparable group prescribed a therapeutic alternative (unexposed) within the EHR.
- Phenotyping: Use validated ICD-10 and RxNorm code algorithms to define the outcome (AE Y) and key confounders (e.g., renal function, comorbidities).
- Linkage: Deterministically link cohort patients to FAERS reports using anonymized identifiers.
- Analysis: Calculate incidence rates. Use multivariable Cox regression to estimate Hazard Ratios (HR) for AE Y, adjusting for age, sex, and comorbidities. Compare HR from the RWE cohort to the proportional reporting ratio (PRR) from FAERS alone.
3.2. Protocol for AI-Driven Novel Signal Detection
This protocol uses deep learning to identify complex, non-linear patterns in multi-modal data.
- Objective: To discover novel drug-AE associations or risk clusters not captured by traditional disproportionality analysis.
- Data Source: FAERS reports (structured fields: drug, AE, demographics) with linked clinical notes (unstructured text) from a partner health system.
- Model Architecture: A multi-modal neural network.
- Structured Data Stream: Process drug codes and AE terms (MedDRA) through embedding layers, followed by dense layers.
- Unstructured Data Stream: Process clinical notes via a BioBERT model (a domain-specific transformer) to generate feature vectors.
- Fusion & Output: Concatenate feature vectors from both streams. Pass through final classification layers to output a risk score or cluster assignment for each drug-AE pair.
- Training & Validation: Train on historical data with known safety signals. Validate using prospective data hold-out and positive/negative controls (e.g., known toxicities of withdrawn drugs).
4. Visualization: Integrated RWE/AI PMS Workflow
Diagram 1: Integrated RWE and AI Post-Marketing Surveillance Workflow (82 chars)
5. The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Tools for Advanced PMS Research
| Tool/Resource | Category | Function in PMS Research |
|---|---|---|
| OMOP Common Data Model | Data Standardization | Enables scalable analytics across disparate RWE databases by transforming data into a consistent format. |
| MedDRA (Medical Dictionary for Regulatory Activities) | Terminology | Provides standardized hierarchical terminology for coding adverse event reports in FAERS and RWE. |
| BioBERT / ClinicalBERT | NLP Model | Pre-trained language models fine-tuned for biomedical text, used to extract concepts from clinical notes. |
| PROC AE / PHV PM (FDA's Tools) | Signal Detection | FDA's statistical tools for quantitative disproportionality analysis in FAERS data. |
| R, Python (Pandas, PyTorch/TensorFlow, SciKit-learn) | Programming & ML | Core languages and libraries for data manipulation, statistical analysis, and building custom AI models. |
| Sentinel Initiative / FDA-Catalyst | RWE Infrastructure | FDA's national electronic system for monitoring medical product safety using distributed claims and EHR data. |
| Propensity Score Matching Algorithms | Causal Inference | Statistical method to adjust for confounding in observational RWE studies, estimating treatment effects. |
Conclusion
Navigating FDA adverse event reporting requirements is a cornerstone of ethical and compliant clinical research, demanding a deep understanding of regulatory foundations, meticulous methodological execution, proactive process optimization, and awareness of global standards. Mastery of these areas ensures not only patient safety but also protects trial integrity and facilitates regulatory review. For researchers and drug developers, the future points toward greater electronic integration, real-world data utilization, and continued global harmonization. Investing in robust, well-trained safety systems is not merely a regulatory checkbox but a critical component of successful therapeutic development that builds trust with regulators, participants, and the public. The evolving landscape underscores the need for professionals to stay current with FDA guidance and international standards to advance biomedical innovation responsibly.