Developing an Effective Bioethics Curriculum for Medical Schools: Evidence-Based Strategies for Integrating Ethics into Medical Education
This article provides a comprehensive framework for developing, implementing, and evaluating bioethics curricula in medical education.
Developing an Effective Bioethics Curriculum for Medical Schools: Evidence-Based Strategies for Integrating Ethics into Medical Education
Abstract
This article provides a comprehensive framework for developing, implementing, and evaluating bioethics curricula in medical education. Drawing on recent global research and evaluation studies, it addresses foundational principles, innovative teaching methodologies, solutions for common implementation challenges, and robust validation techniques. Designed for medical educators, curriculum developers, and institutional leaders, the content synthesizes evidence from successful long-term programs, including integrated spiral curricula, Team-Based Learning (TBL), and performable case studies, offering practical strategies for creating ethically competent physicians prepared for modern biomedical challenges.
Laying the Groundwork: Core Principles and the Evolving Scope of Bioethics Education
Bioethics, broadly defined as the interdisciplinary study of ethical, legal, and social issues arising in the life sciences and health care, emerged as a formal discipline in the late 1960s against a backdrop of profound medical tragedies and societal transformations [1]. This field has since transformed medical practice and policy-making concerning issues ranging from public health and medical care delivery to agricultural biotechnology. The development of structured bioethics curricula represents a direct response to historical events where medical professionalism and research ethics dramatically failed, creating an imperative to equip healthcare professionals with the ethical reasoning necessary to navigate complex moral dilemmas. This whitepaper traces the journey from these tragic origins to the formalized educational frameworks implemented in modern medical education, providing researchers, scientists, and drug development professionals with a comprehensive analysis of evidence-based approaches to bioethics curriculum development.
The historical arc of bioethics education reveals a field continually evolving to address emerging challenges—from initial concerns about human subjects research to contemporary issues involving artificial intelligence, genomics, and global health equity. Modern bioethics curricula now represent essential components of medical education, mandated by accrediting bodies like the Accreditation Council for Graduate Medical Education (ACGME) and integrated throughout undergraduate and graduate medical training [2] [3]. This paper examines the historical imperative driving this educational evolution, assesses current evidence-based curricular models, and provides methodological frameworks for developing effective bioethics education tailored to contemporary medical and research environments.
Historical Foundations: From Tragedy to Formalized Ethics
The formalization of bioethics as a discipline directly reflects medicine's ethical reckoning with twentieth-century tragedies, particularly those involving abuse of human subjects in research. The Nuremberg Doctors' Trial of 1946-1947, where 23 high-ranking Nazi doctors and administrators were tried for war crimes and crimes against humanity including non-consensual medical experiments, established a pivotal historical foundation for modern bioethics [1]. The trial exposed horrific medical abuses and produced the Nuremberg Code (1947), whose first principle established that "the voluntary consent of the human subject is absolutely essential" [1]. This document, while initially having limited immediate impact on research practices, eventually became the cornerstone for all subsequent research ethics frameworks.
Other historical cases further cemented the need for formal ethics oversight and education. The Guatemala Syphilis Studies (1946-1948), where U.S. researchers intentionally infected more than 1,300 Guatemalan soldiers, prisoners, and mental patients with sexually transmitted diseases without consent, remained buried in archives until 2010 but exemplify the ethical breaches that bioethics education seeks to prevent [1]. In response to these and other ethical failures, various codes and declarations emerged throughout the mid-twentieth century, including the Declaration of Geneva (1948) as a new secular physician's oath, the World Medical Association's International Code of Medical Ethics (1949), and principles adopted by the American Medical Association for permissible human experimentation [1].
Table 1: Historical Foundations of Modern Bioethics
| Year | Event | Significance | Impact on Bioethics Education |
|---|---|---|---|
| 1946-1947 | Nuremberg Doctors' Trial | Exposed horrific medical experiments on prisoners without consent | Established necessity of voluntary consent as foundational principle |
| 1947 | Nuremberg Code | First international document specifying principles for human subjects research | Provided core content for research ethics education |
| 1948 | Declaration of Geneva | Established secular physician's oath in aftermath of WWII | Became model for professional ethics training |
| 1960s-1970s | Bioethics as Formal Discipline | Field emerged addressing ethics of new medical technologies | Created need for structured curricula in medical education |
| 1979 | Belmont Report | Established ethical principles for research in United States | Standardized research ethics education requirements |
The evolution of these historical responses demonstrates a pattern: ethical breach, investigation, policy response, and eventual educational integration. This pattern underscores the preventive function of bioethics education—equipping professionals with ethical frameworks before rather than after crises occur. The formalization of bioethics curricula throughout the 1970s and 1980s represented the institutionalization of this hard-won historical knowledge, transforming tragic lessons into proactive educational frameworks [1].
Current Bioethics Curriculum Frameworks and Evidence
Contemporary bioethics education has evolved from historical foundations to become formally integrated throughout medical education, with evidence supporting specific curricular approaches and methodologies. Current frameworks span undergraduate medical education, graduate medical training, and dual-degree programs, incorporating varied pedagogical methods to address increasingly complex ethical challenges in healthcare and research.
Curriculum Integration Models and Effectiveness
Research demonstrates that effective bioethics curricula share several key characteristics: longitudinal integration throughout training, use of interactive pedagogical methods, and application of ethical principles to real-world clinical scenarios. A comprehensive mixed-methods evaluation of a bioethics curriculum implemented for over a decade in a five-year undergraduate medical program demonstrated significant effectiveness in student development [3] [4]. The quantitative results from this study revealed that the majority of students agreed the curriculum contributed to their knowledge acquisition (60.3-71.2%), skill development (59.41-60.30%), and demonstration of ethical/professional behavior (62.54-67.65%) [3] [4].
Table 2: Bioethics Curriculum Effectiveness in Undergraduate Medical Education
| Learning Domain | Student Agreement (%) | Key Contributing Factors | Implementation Recommendations |
|---|---|---|---|
| Knowledge Acquisition | 60.3-71.2% | Spiral integration across curriculum; relevant content | Basic knowledge acquisition in Years 1-2 with reinforcement in clinical years |
| Skill Development | 59.41-60.30% | Case-based learning; small group discussions | Opportunities for application in clinical settings; ethics consultation simulation |
| Ethical/Professional Behavior | 62.54-67.65% | Role modeling; clinical integration | Involvement of clinical faculty; explicit linking of principles to practice |
The study employed a sequential explanatory mixed methods design, beginning with a structured online questionnaire completed by 500 students across all five years of the medical program, followed by focus group discussions and document review to explain and enrich the quantitative findings [3] [4]. This methodology provided both breadth and depth of understanding regarding curriculum effectiveness. Importantly, the research identified that multi-modal instructional methods were particularly effective, with students and faculty emphasizing the value of small group teaching and shorter sessions for fostering discussion and maintaining engagement, while large class formats were significantly less effective [3].
Graduate Medical Education and Team-Based Learning
At the graduate medical education level, Team-Based Learning (TBL) has emerged as an evidence-based approach to bioethics instruction. A comprehensive TBL curriculum implemented with pediatric residents demonstrated significant improvements in knowledge and ethical analysis capabilities [2]. The curriculum, developed around L. Dee Fink's principles of "Significant Learning" and Jonsen et al.'s "Four-Box Method" of ethical analysis, included 10 adaptable modules covering essential bioethics topics including introduction to medical ethics, assent and consent, professionalism and social media, neonatal and perinatal ethics, and pediatric palliative care [2].
The study methodology employed a three-year longitudinal, integrated approach with 348 total resident encounters. Assessment included Individual and Group Readiness Assessment Tests (iRAT/gRAT), pre-work completion measurement, and satisfaction surveys [2]. Results demonstrated that gRAT scores (mean 89%) showed significant improvement compared to iRAT scores (72%) across all TBL sessions and all post-graduate years (p < .001), indicating that collaborative learning enhanced ethical reasoning capabilities [2]. Higher gRAT scores correlated with more advanced training levels, suggesting developing clinical experience enhances ethical analysis skills. Despite low pre-work completion (28%), satisfaction was high (4.42/5 on Likert scale), indicating strong engagement with the TBL methodology [2].
Core Content Areas and Emerging Topics
Modern bioethics curricula have expanded beyond traditional topics to address emerging ethical challenges at the frontiers of medicine and technology. Core graduate-level courses now include:
- Philosophical Bioethics: Examining fundamental questions about life, death, and the provider-patient relationship through ethical frameworks [5]
- Law and Bioethics: Contrasting legal reasoning and ethical analysis of the same issues [5]
- Clinical Ethics: Developing consultation skills for clinical ethical dilemmas [5]
- Global Bioethics: Examining how varying economic, political, social, and cultural contexts shape ethical issues [5]
- Research Ethics: Addressing challenges in human subjects research and professional scientific conduct [5]
Emerging elective courses reflect evolving ethical frontiers, including:
- AI and Bioethics: Addressing the ethical implications of artificial intelligence and machine learning in healthcare, training ethicists to "help steer AI use in safe and productive ways" [5]
- Animals and Bioethics: Examining ethical issues in the use of non-human animals in biomedical research and emerging technologies [5]
- Pandemic Ethics: Exploring ethical decision-making in infectious disease outbreaks, drawing lessons from COVID-19 and historical pandemics [5]
These content areas reflect the expanding scope of bioethics education as it addresses both perennial ethical questions and emerging challenges created by technological and social changes.
Implementation Methodologies and Curricular Design
Effective bioethics education requires deliberate pedagogical strategies and implementation methodologies. Evidence supports specific approaches to curricular design, teaching methods, and integration frameworks that maximize educational effectiveness across different learner levels and institutional contexts.
Pedagogical Frameworks and Instructional Methods
The Team-Based Learning methodology implemented in graduate medical education provides a robust framework for bioethics instruction [2]. The TBL process comprises five essential components: (1) establishing clear learning outcomes; (2) pre-session preparation; (3) Individual Readiness Assurance Test (iRAT); (4) Group Readiness Assurance Test (gRAT); and (5) Team Application Exercise (TApp) where learners apply knowledge to complex ethical scenarios [2]. This methodology promotes significant learning through active discussion and immediate application of ethical concepts to clinically relevant situations.
The "Four-Box Method" of ethical analysis provides a structured approach for evaluating clinical ethical cases [2]. This method, integrated into TBL application exercises, guides learners to analyze cases through four essential dimensions: medical indications, patient preferences, quality of life, and contextual features. This structured approach provides residents with a consistent method of ethical analysis that can be applied across diverse clinical scenarios, becoming a "deliverable skill" similar to other clinical reasoning algorithms [2].
For undergraduate medical education, research supports multi-modal instructional approaches including lectures, discussions, brainstorming, problem-solving exercises, videos/movies, and case studies [3]. The integration of bioethics within existing problem-based learning (PBL) curricular frameworks facilitates contextual understanding and application of knowledge [3]. Studies indicate that learning embedded in an integrated curriculum helps students recognize, critically analyze, and address ethical dilemmas they will encounter in clinical practice [3].
Integration Strategies and Longitudinal Implementation
Research supports longitudinal integration of bioethics throughout the entire medical education continuum rather than as isolated courses or lectures. An effective bioethics curriculum for undergraduate medical education should run across the five-year curriculum, integrated within modules and clerkships [3]. Basic knowledge and skill acquisition occurs in the first two years, with reinforcement and application in clinical years [3]. This spiral approach allows for repeated exposure to ethical concepts at increasing levels of complexity and clinical relevance.
Critical to successful implementation is the involvement and commitment of clinical faculty in reinforcing ethical principles and concepts learned in earlier years [3]. Studies indicate that better integration in clinical years, role modeling, and providing opportunities for application in clinical healthcare settings significantly strengthen bioethics curricula [3]. Participants in evaluation studies have suggested additional topics for modern curricula, including ethical issues related to social media, public health ethics, and the intersection of ethics and law [3].
For graduate medical education, bioethics curricula must be both practical and flexible in implementation, adaptable to different specialties, virtual formats, and specific institutional needs [2]. The TBL approach has demonstrated effectiveness across different situational factors, disciplines, and levels of clinical experience [2]. This flexibility is particularly important given the "crowding in the curriculum" that represents a significant barrier to graduate medical education innovations [2].
Implementing effective bioethics education requires specific resources, tools, and methodological approaches. The following research reagents and solutions represent essential components for developing, implementing, and evaluating bioethics curricula across educational contexts.
Table 3: Essential Research Reagents for Bioethics Curriculum Development
| Reagent/Solution | Function | Application Context | Implementation Considerations |
|---|---|---|---|
| TBL Framework | Structured pedagogical approach for ethics education | Graduate medical education; small group learning | Requires facilitator training; adaptable modules |
| Four-Box Method | Ethical analysis framework for clinical cases | Clinical ethics education; case analysis | Provides consistent approach across cases |
| Mixed Methods Evaluation | Comprehensive curriculum assessment | Program evaluation; quality improvement | Sequential explanatory design: quantitative then qualitative |
| Integrated Spiral Curriculum | Longitudinal educational approach | Undergraduate medical education | Basic concepts in pre-clinical years with clinical application |
| Digital Accessibility Tools | Ensure inclusive educational materials | Online and hybrid education | Color contrast checkers; multiple content modalities |
The TBL framework serves as a primary "research reagent" for effective bioethics education, providing a structured methodology that promotes engagement and application of ethical principles [2]. Essential to this approach are the specific components of iRAT, gRAT, and TApp exercises that create a progressive learning experience from individual knowledge assessment to collaborative application.
The Four-Box Method represents another critical "reagent" for ethical analysis, offering a consistent framework that learners can apply across diverse clinical scenarios [2]. This methodological tool helps structure ethical reasoning while acknowledging the complexity of clinical realities.
Evaluation methodologies, particularly mixed methods approaches combining quantitative surveys with qualitative focus groups and document analysis, serve as essential "reagents" for curriculum assessment and refinement [3] [4]. These methodological tools provide both breadth and depth of understanding regarding curriculum effectiveness, enabling evidence-based improvements.
Future Directions and Emerging Challenges
Bioethics education continues to evolve in response to emerging technologies, changing healthcare systems, and global health challenges. Future curriculum development must address several critical areas to maintain relevance and effectiveness in preparing healthcare professionals for ethical challenges at the frontiers of medicine.
Artificial intelligence and machine learning represent one of the most significant emerging domains requiring ethical analysis. As noted in contemporary curricula, "Computer scientists, coders, and engineers best understand the development and use of Machine Learning, but often lack training in ethics, law, and public policy" [5]. This creates an urgent need for ethicists with understanding of AI to "help steer AI use in safe and productive ways" [5]. Future bioethics curricula must bridge this technical-ethical divide, equipping professionals with the analytical frameworks necessary to address ethical implications of AI in healthcare and research.
Global bioethics represents another expanding frontier, requiring attention to how "varying economic, political, social, cultural, and historical contexts shape these issues" across different regions and resource settings [5]. Multinational research, "reproductive tourism," and differing approaches to end-of-life care across national borders all highlight the need for globally informed ethical frameworks [5]. Bioethics education must prepare professionals for these transnational ethical challenges while respecting cultural diversity and contextual differences.
The COVID-19 pandemic has highlighted persistent challenges in public health ethics, including issues of government preparedness, resource allocation, vaccine development, and public communication [5]. Future curricula must incorporate these lessons, exploring "how bioethical and policy decision-making can have different effectiveness in the context of modern pandemics" [5]. These contemporary challenges underscore the continuing relevance of the historical imperative in bioethics education—applying lessons from past ethical successes and failures to emerging challenges in healthcare and research.
The development of formal bioethics curricula represents a direct response to medicine's ethical failures and a commitment to preventing their recurrence through education. From the tragic origins exemplified by the Nuremberg Trials to contemporary ethical challenges posed by emerging technologies, bioethics education has evolved from historical imperative to educational necessity. Evidence-based approaches including longitudinal integration, Team-Based Learning methodologies, mixed methods evaluation, and structured ethical analysis frameworks provide effective strategies for developing healthcare professionals equipped to navigate complex ethical dilemmas.
For researchers, scientists, and drug development professionals, understanding this historical imperative and its translation into formal educational frameworks is essential both for their own ethical development and for contributing to the evolution of bioethics education. As medical science continues to advance, bringing new ethical challenges, the lessons of history remain relevant: that ethical education is not peripheral but central to medical professionalism, and that preventing ethical breaches requires proactive education rather than retrospective response. The continued refinement of bioethics curricula represents an ongoing commitment to this principle, ensuring that healthcare professionals at all levels possess the ethical reasoning capabilities necessary to navigate the complex moral landscape of modern medicine.
The evolution of medical education highlights a critical shift from a process-time-based model to a competencies-driven framework, focusing on the definitive outcomes graduates must demonstrate. This transition is underscored by global research revealing significant gaps in essential competencies among medical graduates. A seminal European cross-sectional study evaluating 895 final-year students from 26 medical schools found an overall lack of essential prescribing competencies, including poor knowledge of drug interactions and contraindications, and the selection of inappropriate therapies for common diseases [6]. These deficiencies directly impact patient safety and quality of care, signaling an urgent need for standardized competency frameworks. Within this educational landscape, bioethics education serves as a fundamental pillar, not merely as a discrete subject but as an integrative thread that enables the embodiment of humanistic, professional, and ethical principles across all medical practice. The development of a core competencies framework, therefore, provides the necessary structure to ensure medical schools cultivate professionals who are not only technically proficient but also ethically grounded and socially responsible [7] [8].
Global Landscape of Medical Competencies: Current Status and Identified Gaps
Quantitative Deficits in Core Competencies
Table 1: Documented Deficiencies in Medical Graduate Competencies
| Competency Area | Deficiency Documented | Study Population | Impact on Practice |
|---|---|---|---|
| Clinical Pharmacology & Therapeutics | Poor knowledge of drug interactions/contraindications; inappropriate therapy selection [6] | 895 final-year students across 26 European schools | Leads to prescribing errors and potentially unsafe patient care [6] |
| Bioethics Knowledge & Application | Lack of formal, integrated bioethics curriculum in many regions [8] | Medical schools in Africa, Asia, and Portuguese-speaking countries | Inability to critically process ethical dilemmas in clinical settings [7] [8] |
| Mental, Neurological, Substance Use (MNS) Care | Lack of thorough training for general health-care providers [9] | Medical and nursing students globally | Failure to provide care for one in eight people living with MNS conditions [9] |
Bioethics Curriculum Implementation: A Variable Global Picture
The integration of bioethics into medical curricula remains inconsistent worldwide. Studies from Portuguese-speaking countries reveal that while 65.5% of medical schools met the minimum 30-hour workload recommended by UNESCO, the curricular structure, content, and integration point varied significantly, with most offering ethics sporadically at the program's end [8]. This lack of formalization and standardization is a recurring challenge. In contrast, evaluation studies of longitudinal, spiral bioethics curricula, such as one implemented for over a decade in a Pakistani medical college, show more promising results. In such models, a majority of students agreed the curriculum contributed to their knowledge acquisition (60.3–71.2%), skill development (59.41–60.30%), and demonstration of ethical behavior (62.54–67.65%) [7]. These findings highlight that the structure, duration, and integration of ethics education are as critical as its mere presence.
Defining the Core Competency Domains for Medical Graduates
A comprehensive synthesis of global frameworks and research findings reveals three interdependent competency domains essential for every medical graduate.
Professional Competencies and Bioethical Integration
This domain encompasses the attributes, behaviors, and moral reasoning necessary for trustworthy medical practice. The AAMC categorizes these as "Professional Competencies," which include resilience, interpersonal skills, and a service orientation [10]. The University of Saskatchewan's MD program further elaborates these as "Behavioral and Social Attributes," requiring good judgement, self-awareness, ethical responsibility, and cultural humility [11]. Bioethics education is the scaffold upon which these competencies are built, moving beyond theoretical knowledge to foster the demonstration of ethical and professional behavior in patient care [7]. This involves a commitment to lifelong learning, personal integrity, and the ability to navigate complex interpersonal dynamics with empathy and compassion [10] [11].
Thinking, Reasoning, and Scientific Competencies
This domain involves the analytical and knowledge-based skills required for clinical reasoning and scientific inquiry.
- Critical Thinking & Scientific Inquiry: The ability to analyze complex problems, integrate information from histories, physical exams, and lab data to formulate a differential diagnosis and management plan is a core intellectual-conceptual skill [11]. This aligns with the AAMC's "Thinking and Reasoning" competencies, which include critical thinking and quantitative reasoning to evaluate evidence and solve clinical problems [10].
- Living Systems & Human Behavior: A robust understanding of human biology—from molecular to systemic levels—and the psychological, social, and biological factors that influence health is foundational [10]. These "Science Competencies" underpin the ability to understand disease processes and treatment mechanisms.
Functional and Technical Competencies
These are the observable, practical skills required to perform the duties of a physician.
- Communication Skills: The ability to communicate effectively and sensitively with patients, families, and colleagues across cultural, age, and social boundaries is paramount. This includes verbal, non-verbal, and written communication, and the capacity to recognize and respond to emotional cues [11].
- Observational and Procedural Skills: Graduates must possess the sensory and motor functions to perform physical examinations and procedural skills competently and safely. This requires accurate observation of signs of illness and competent use of medical equipment [11].
- Equity, Diversity, and Inclusion: A modern and essential competency is the ability to contribute to inclusive learning and work environments, address personal biases, and ensure equitable care for all patients [11].
Experimental and Methodological Approaches to Curriculum Development
Research Protocols for Competency Framework Development
Establishing a valid and relevant competency framework requires rigorous, multi-method research approaches.
Protocol 1: Mixed-Methods Curriculum Evaluation
- Objective: To assess the effectiveness of an integrated bioethics curriculum in terms of student achievement, content appropriateness, and instructional method efficiency [7].
- Quantitative Phase: Administer a structured online questionnaire to a large sample of students (e.g., N=500) across all years of the program. Utilize a model like Context, Input, Process, Product (CIPP) to develop questions rated on a Likert scale [7].
- Qualitative Phase: Conduct Focus Group Discussions (FGDs) with students and faculty to explain and enrich quantitative findings. Perform document reviews of curriculum materials to check alignment with objectives [7].
- Data Synthesis: Integrate datasets to identify convergent and divergent themes. For example, quantitative data may show high satisfaction with small-group teaching, which qualitative data can then explain by highlighting its interactive nature [7].
Protocol 2: Cross-Sectional Competency Gap Analysis
- Objective: To evaluate the essential competencies of final-year medical students across multiple regions [6].
- Design: International, multicenter, cross-sectional study.
- Sampling: Administer a standardized assessment (e.g., knowledge tests, scenario-based assessments) and questionnaire to a defined number of final-year students (e.g., 50) from each participating medical school [6].
- Analysis: Perform quantitative analysis of assessment scores to identify specific competency gaps at both an aggregate level and per institution.
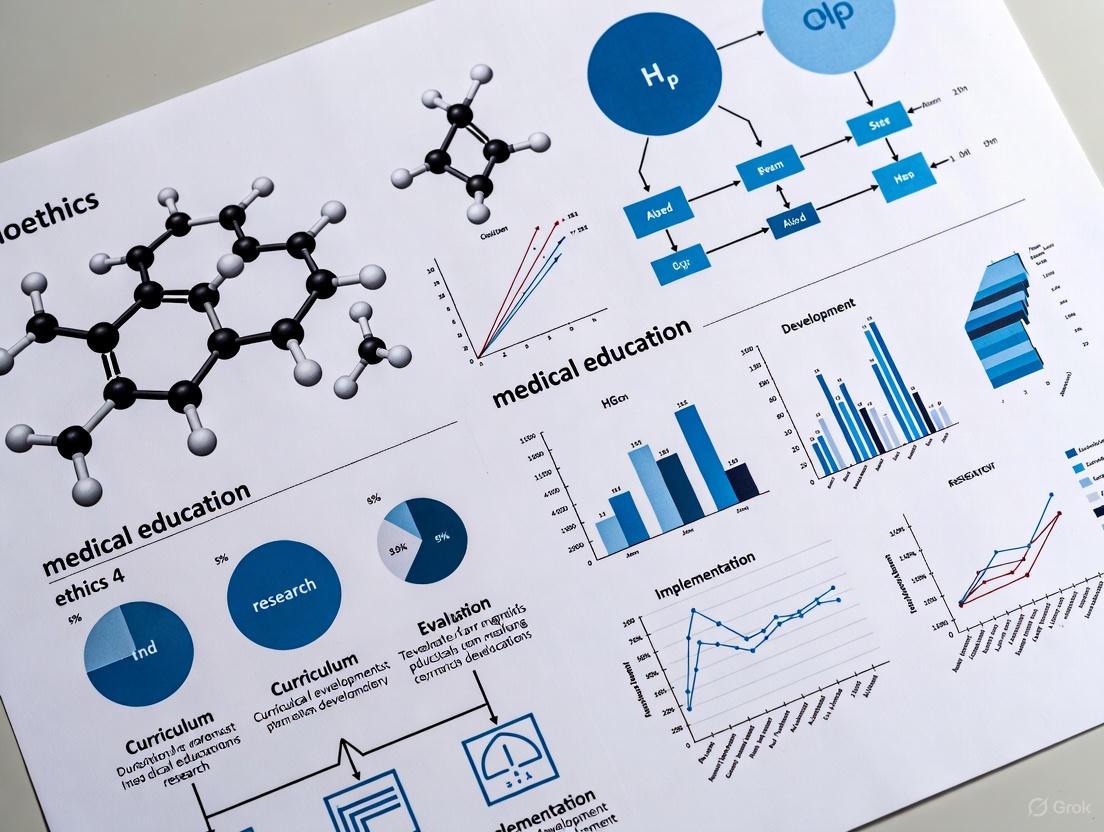
Visualization of Integrated Curriculum Development
The following diagram illustrates the systematic, multi-stakeholder process for developing and evaluating a competencies-based medical curriculum, particularly for bioethics.
Research Reagent Solutions for Educational Research
Table 2: Essential Methodological Tools for Competency Research
| Research 'Reagent' | Function in Curriculum Development | Exemplar Application |
|---|---|---|
| Structured Questionnaire | Quantitatively measures perceptions of competency achievement, curriculum relevance, and teaching effectiveness. | Used with Likert scales to gauge student agreement on knowledge acquisition (60.3-71.2%) and skill development (59.41-60.30%) [7]. |
| Focus Group Discussion (FGD) Guide | Elicits rich, qualitative data on lived experiences, unexplored challenges, and nuanced suggestions for improvement. | Explains why large class formats are less effective and gathers suggestions for topics like social media ethics [7]. |
| Semi-Structured Interview Guide | Gathers in-depth perspectives from key stakeholders (e.g., faculty, clinical preceptors) on implementation barriers and enablers. | Used with faculty to understand challenges in reinforcing ethics in clinical years and the role of hidden curriculum [7] [12]. |
| Standardized Competency Assessment | Objectively measures specific competency levels across different institutions using a validated instrument. | Employed in a European cross-sectional study to identify prescribing deficits among final-year students [6]. |
| Document Analysis Protocol | Systematically reviews official curriculum documents, syllabi, and learning objectives for alignment with competency goals. | Used to analyze 58 medical school curricula in Brazil and Portugal against the UNESCO Core Curriculum benchmark [8]. |
Discussion and Future Directions: Implementing and Sustaining Competency Frameworks
The path to implementing a successful competencies-based curriculum, particularly in bioethics, is fraught with challenges but rich with opportunity. A primary obstacle is the "hidden curriculum" – the unspoken values and behaviors modeled by clinical faculty that can undermine formal ethics teaching if not aligned [8] [12]. Overcoming this requires more than student assessment; it demands faculty development and the explicit involvement and commitment of clinical faculty to model and reinforce ethical principles [7]. Furthermore, as a study of a diverse student elective highlighted, interactive teaching formats are the most preferred for ethics education, and topics must be contextually relevant, with truth-telling emerging as a critical subject [13]. Future efforts must focus on creating longitudinal and spirally integrated curricula that begin in pre-clinical years and are reinforced and applied throughout clinical training [7] [8]. This ensures that learning is embedded, allowing students to progressively build the ability to recognize, analyze, and address ethical dilemmas. Finally, the global movement towards competencies-based education, exemplified by WHO's competency guide for mental and neurological care, provides a replicable model for other domains, advocating for a framework that is adaptable to local contexts and resource settings without being a rigid, one-size-fits-all solution [9].
The globalization of health challenges, from pandemic diseases to disparities in healthcare access, necessitates a paradigm shift in how bioethics is taught to future medical professionals and researchers [14]. A "transplanted" curriculum, developed in one cultural or national context and directly applied in another, risks being ineffective and ethically problematic. It often fails to equip professionals with the nuanced understanding required to navigate the specific ethical dilemmas they will encounter in their local practice [3]. The core thesis of this whitepaper is that bioethics curriculum development must move beyond a one-size-fits-all model. Instead, it must embrace contextual relevance, a deliberate and systematic approach to curriculum design that integrates local cultural values, prevalent health issues, and specific regional ethical challenges into the core of educational content and pedagogy. This is not merely an educational preference but a fundamental component of ethical rigor, ensuring that the principles of autonomy, justice, and beneficence are interpreted and applied in a manner that is both globally informed and locally resonant [15] [3]. For researchers and drug development professionals, this contextual understanding is critical for conducting ethical global clinical trials, addressing issues of consent and equity, and ensuring that scientific advancements are implemented responsibly across diverse populations.
Quantitative Landscape of Bioethics Education Integration
A systematic mapping of the field reveals both the progress and the significant gaps in the institutionalization of bioethics. The following table summarizes data from a review of 444 articles on the integration of bioethics in higher education institutions.
Table 1: Institutionalization of Bioethics in Higher Education: A Systematic Analysis
| Aspect of Integration | Metric (%) | Key Findings | |
|---|---|---|---|
| Program Level Focus | Undergraduate: 40.5% | Postgraduate: 19.4% | A predominant focus on undergraduate education, with relatively less structured attention at postgraduate levels [15]. |
| Disciplinary Distribution | Health Sciences: 81.3% | Social Sciences, Humanities, Biological Sciences, Engineering: 18.7% | Bioethics education is heavily concentrated within the health sciences, indicating a need for greater interdisciplinary reach [15]. |
| Use of Active Methodologies & Ed-Tech | 21.4% | The integration of interactive tools and methods is a significant and growing trend, enhancing engagement and learning outcomes [15]. | |
| Research on Institutionalization | 10.3% | A critical lack of empirical studies documenting and validating the process of embedding bioethics within institutions [15]. | |
| Studies on Comparative/Replicated Practices | 2% | A severe deficit in comparative analyses or replicated studies, hindering the sharing of best practices across contexts [15]. |
Furthermore, evaluation studies of specific curricula provide data on educational effectiveness. A decade-long study of an integrated undergraduate medical bioethics curriculum utilized a mixed-methods approach to assess student achievement, gathering quantitative feedback from 500 students across a five-year program [3].
Table 2: Effectiveness of a Longitudinally Integrated Bioethics Curriculum (n=500 students)
| Domain of Achievement | Agreement among Students (%) | Interpretation |
|---|---|---|
| Knowledge Acquisition | 60.3% - 71.2% | A majority of students confirmed the curriculum's role in expanding their understanding of bioethical principles and issues [3]. |
| Skill Development | 59.4% - 60.3% | Students reported development in critical skills, such as identifying and analyzing ethical dilemmas [3]. |
| Ethical & Professional Behavior | 62.5% - 67.7% | Students acknowledged the curriculum's contribution to their personal ethical positioning and professional conduct [3]. |
Theoretical Frameworks for Contextual Relevance
From Culturally Responsive to Culturally Sustaining Pedagogy
The development of a contextually relevant curriculum is underpinned by established pedagogical theories from general education, which have profound implications for bioethics. Culturally Responsive Teaching (CRT), a term coined by Geneva Gay, is defined as using students' customs, characteristics, experiences, and perspectives as tools for better classroom instruction [16]. It is validating, comprehensive, multidimensional, empowering, transformative, and emancipatory [17]. This framework builds upon Culturally Relevant Pedagogy, introduced by Gloria Ladson-Billings, which rests on three propositions: student learning (intellectual growth), cultural competence (affirming one's culture of origin while developing fluency in others), and critical consciousness (the ability to identify and challenge societal inequities) [16] [17].
A more recent evolution is Culturally Sustaining Pedagogy, which posits that students of color should not be expected to adhere to dominant cultural norms. Instead, their own cultural ways of being should be explored, honored, and nurtured by educators [16]. For bioethics, this means curricula should not simply "add" diverse perspectives but should actively sustain the cultural pluralism that students and their future patients bring to healthcare encounters.
Cosmopolitanism in Global Bioethics
Parallel to these pedagogical theories is the philosophical concept of cosmopolitanism in global bioethics. This perspective aims to further ideals of solidarity, equality, and respect for differences, educating health professionals in their role as 'citizens of the world' [14]. It argues that ethical discourse must first critique the structures of violence and injustice that underlie global health threats. A contextually relevant curriculum, therefore, is not parochial; it situates local ethical challenges within a global framework, enabling professionals to understand the transnational dimensions of issues like resource allocation, pandemics, and medical migration [14] [18].
Experimental and Methodological Protocols for Curriculum Development and Evaluation
Protocol 1: Mixed-Methods Curriculum Evaluation
Objective: To comprehensively assess the effectiveness, relevance, and integration of a bioethics curriculum within a specific institutional context [3].
Workflow:
- Phase 1 - Quantitative Data Collection: Distribute a structured online questionnaire to all student cohorts (e.g., Years 1-5 of a medical program). The questionnaire should be based on an evaluation model like CIPP (Context, Input, Process, Product) and use Likert scales to measure perceived relevance of content, effectiveness of teaching methods, and self-reported achievement in knowledge, skills, and professional behavior [3].
- Data Analysis: Analyze quantitative data to identify trends, strengths, and weaknesses. For example, calculate percentage agreement for key domains as shown in Table 2.
- Phase 2 - Qualitative Data Collection: Conduct Focus Group Discussions (FGDs):
- Separate FGDs with students from different stages of the curriculum (e.g., pre-clinical and clinical years).
- One FGD with faculty involved in teaching bioethics and clinical faculty who reinforce ethics in practice.
- Use semi-structured interview guides to explore quantitative findings in depth, asking about integration, practical application, and specific challenges [3].
- Data Analysis: Transcribe and thematically analyze FGD data to explain and enrich the quantitative results. Key themes might include the need for better clinical integration or the value of specific teaching methods.
- Triangulation and Reporting: Integrate findings from both phases to form a holistic understanding of the curriculum's performance and generate actionable recommendations for improvement [3].
Protocol 2: Digital Tool-Assisted, Discovery-Driven Research
Objective: To leverage educational technology (Ed-Tech) for both teaching bioethics and generating empirical data on the psychological and epistemic factors influencing moral judgment [19].
Workflow:
- Tool Development: Create a mobile application (e.g., "MyBioethics") containing modular lessons on various bioethical topics. Each lesson includes interactive dilemma scenarios [19].
- Data Generation Module:
- Users vote on the ethical alternative in a given scenario.
- Post-vote, users disclose their self-perceived moral certainty and the decisive ethical principle (e.g., autonomy, justice) that guided their choice from a provided list or a free-text field [19].
- The app integrates standardized psychometric and epistemometric surveys to measure users' dispositional tendencies (e.g., optimism, cognitive style) [19].
- Data Analysis: Employ quantitative and explorative data analysis to investigate correlations between users' measured psychological/epistemic traits and their expressed moral judgments. This methodology is hypothesis-generating, aiming to identify previously unarticulated factors behind ethical decision-making [19].
- Educational Feedback: The app provides users with personalized feedback, showing their survey results compared to averages and prompting reflection on how these traits might influence their ethical views. This closes the loop between research and learning [19].
The Scientist's Toolkit: Essential Reagents for Bioethics Education Research
Table 3: Key Methodological Tools for Curriculum Development and Evaluation
| Research 'Reagent' | Category | Function in Bioethics Education Research |
|---|---|---|
| Structured Questionnaire (CIPP Model) | Evaluation Framework | Provides a systematic structure (Context, Input, Process, Product) for developing questions to assess all aspects of a curriculum's implementation and impact [3]. |
| Likert Scale | Psychometric Tool | A reliable and replicable measurement instrument for capturing attitudes and perceptions on a quantitative scale (e.g., 1-5, Strongly Disagree to Strongly Agree), allowing for statistical analysis of student and faculty feedback [3]. |
| Focus Group Discussion (FGD) Guide | Qualitative Instrument | A semi-structured protocol of open-ended questions used to facilitate in-depth group interviews, generating rich, explanatory data on participant experiences and perspectives [3]. |
| Interactive Dilemma Scenarios | Ed-Tech / Pedagogical Tool | Real-life or hypothetical case studies embedded in digital platforms to engage users, elicit moral judgments, and serve as a data source for analyzing decision-making patterns [19]. |
| Psychometric Surveys (e.g., for cognitive style) | Empirical Research Tool | Standardized questionnaires integrated into digital learning environments to measure psychological and epistemic constructs, enabling research into their correlation with ethical judgments [19]. |
| Systematic Mapping Methodology | Literature Review Protocol | A rigorous process for searching, selecting, and analyzing a broad range of literature to quantify the scope and identify gaps in a research field, such as the institutionalization of bioethics [15]. |
A Conceptual Workflow for Contextual Curriculum Design
The following diagram synthesizes the core principles and processes involved in moving from a transplanted to a contextually relevant bioethics curriculum.
Developing contextually relevant bioethics curricula is an empirical and iterative process, not a one-time event. The data and protocols presented provide a roadmap for researchers and educators. Future efforts must focus on strengthening the evidence base for curriculum implementation, particularly through comparative studies and a greater focus on postgraduate and interdisciplinary education [15]. The promising integration of active methodologies and educational technology, such as the MyBioethics app, points toward a future of more engaging, data-enriched, and personally relevant ethics education [19] [15]. For the global community of researchers, scientists, and drug development professionals, embracing this contextual paradigm is essential for fostering a generation of professionals who are not only technically proficient but also culturally competent and ethically astute citizens of the world, prepared to tackle the complex moral challenges of globalized health and science [14] [18].
The formal integration of bioethics into medical curricula represents a critical response to the complex moral challenges posed by rapid advancements in biomedical science and technology. As a discipline, bioethics serves as a branch of ethical inquiry that examines the nature of biological and technological discoveries and the responsible use of biomedical advances, with particular emphasis upon their moral implications for our individual and common humanity [20]. The evolution of medical practice, characterized by groundbreaking developments in genetics, neuroscience, and reproductive technologies, has necessitated a parallel evolution in ethics education to ensure medical professionals can navigate the attendant ethical dilemmas with moral clarity and analytical rigor.
This whitepaper establishes a foundational framework for bioethics curriculum development within medical schools, articulating 30 essential topics organized within a cohesive conceptual structure. The proposed taxonomy is designed to equip future physicians with the ethical reasoning competencies necessary for contemporary clinical practice, research integrity, and policy engagement. By surveying core concepts across clinical ethics, research ethics, foundational principles, and emerging technologies, this curriculum aims to address the documented gap between theoretical ethics and practical application that has been identified in medical education literature [7] [21]. The structured approach outlined herein provides medical educators with evidence-based guidance for developing comprehensive ethics education that spans the entire undergraduate medical curriculum, fostering the development of professionals who are not only clinically competent but also ethically discerning.
Essential Bioethics Topics: A Categorical Taxonomy
The following taxonomy organizes 30 essential bioethics topics into four interconnected domains, providing a systematic framework for curriculum development. This classification reflects the core competencies required for ethical medical practice and facilitates logical sequencing of educational content across a medical training program.
Table 1: Core Bioethics Topics for Medical Education
| Domain | Essential Topics |
|---|---|
| Clinical Ethics & Patient Care | 1. Informed Consent2. Confidentiality & Truth-Telling3. End-of-Life Care4. Physician-Assisted Suicide5. Organ Donation & Transplantation6. Allocation of Healthcare Resources7. Professional Boundaries8. Pediatric Ethics & Assent9. Capacity & Surrogate Decision-Making10. Cultural & Religious Competence |
| Research Ethics & Scientific Integrity | 11. Historical Context & Tragic Lessons12. Informed Consent in Research13. Protection of Vulnerable Populations14. Conflict of Interest15. Good Scientific Practice (GSP)16. Data Manipulation & Fabrication17. Authorship & Intellectual Property18. Plagiarism19. Research with Animals20. Compassionate Use of Experimental Drugs |
| Foundational Principles & Theories | 21. Major Ethical Theories (Deontology, Utilitarianism, Virtue Ethics)22. Principles of Bioethics (Autonomy, Beneficence, Non-maleficence, Justice)23. Moral Reasoning & Dilemma Resolution24. Human Dignity & What It Means to Be Human25. Justice and Fairness in Healthcare |
| Emerging Technologies & Special Populations | 26. Reproductive Technologies & Ethics27. Genetic Testing & Intervention (CRISPR)28. Stem Cell Research & Cloning29. Neuroscience & Psychopharmacology30. Gender Variance & Clinical Care |
This categorical framework enables spiral integration of bioethics throughout medical education, where basic principles introduced in pre-clinical years are reinforced and applied with increasing complexity during clinical training [7]. The taxonomy's structure acknowledges the interdisciplinary nature of bioethics, integrating diverse fields including life sciences, medicine, biotechnology, philosophy, theology, public policy, and law [20]. This approach ensures that graduates develop the analytical skills necessary to recognize, critically analyze, and address ethical dilemmas across the spectrum of medical practice, from bedside decisions to broader healthcare policy considerations.
Quantitative Assessment of Bioethics Education Outcomes
Empirical evaluation of bioethics curricula provides critical evidence for their educational impact and areas for improvement. A comprehensive mixed-methods study of an integrated bioethics curriculum delivered over five years in an undergraduate medical program yielded compelling quantitative data on student outcomes across three core competency domains [7].
Table 2: Bioethics Curriculum Effectiveness: Student Self-Assessed Competency Gains
| Competency Domain | Specific Learning Outcome | Agreement Rate (%) |
|---|---|---|
| Knowledge Acquisition | Understanding of ethical principles and concepts | 71.2 |
| Recognition of ethical dilemmas in clinical practice | 70.5 | |
| Knowledge of professional codes and guidelines | 60.3 | |
| Skill Development | Analytical skills for ethical dilemma resolution | 60.3 |
| Communication skills for ethics discussions | 59.4 | |
| Professional Behavior | Demonstration of ethical professional conduct | 67.7 |
| Application of ethical reasoning in clinical settings | 62.5 |
The data demonstrates that the curriculum was most effective in fostering knowledge acquisition, particularly in understanding ethical principles and recognizing dilemmas, while indicating potential areas for enhancement in skill development components [7]. This pattern suggests the need for increased experiential learning opportunities to bridge the theory-practice gap that often challenges ethics education.
Additional research on Good Scientific Practice (GSP) education reveals startling preliminary knowledge gaps among medical students, with one study showing approximately 25% of students initially unable to recognize forms of plagiarism prior to targeted instruction [22]. However, post-teaching assessment demonstrated statistically significant improvement (<0.0001), with incorrect answers dropping to 3.4%, confirming that structured ethics education effectively addresses these foundational knowledge deficits [22]. These findings underscore the essential role of formal bioethics training in establishing the ethical foundation necessary for both clinical practice and research activities.
Experimental Protocols in Bioethics Education Research
Mixed-Methods Curriculum Evaluation
The effectiveness of bioethics curricula can be rigorously assessed through a sequential explanatory design that combines quantitative and qualitative methodologies [7]. This mixed-methods approach provides comprehensive insights into both the measurable outcomes and experiential dimensions of ethics education.
Phase 1 - Quantitative Assessment: Implement a structured questionnaire administered to students across all years of the medical program (Years 1-5). The survey should utilize Likert-scale items to assess student perceptions of curriculum effectiveness in three domains: (1) knowledge acquisition, (2) skill development, and (3) demonstration of ethical/professional behavior. Employ multiple response rate maximization strategies, including online distribution via curriculum management software, protected time for completion during sessions, and hard copy availability [7].
Phase 2 - Qualitative Analysis: Conduct Focus Group Discussions (FGDs) with separate student cohorts (Years 1-2 and Years 3-5) and faculty actively involved in bioethics teaching. Use semi-structured interview guides to explore: course content relevance, integration approaches, instructional method effectiveness, and challenges in theory-to-practice transition. Complement FGDs with document review of curriculum materials and student feedback to assess alignment between planned objectives and implementation reality [7].
This protocol employs the Context, Input, Process and Product (CIPP) model as an evaluative framework, focusing not only on whether the program is working but also identifying specific areas for improvement [7]. The model facilitates development of questions related to context (curriculum integration), input (content relevance), and process (teaching methodologies), enabling a comprehensive curriculum assessment.
Pre-Post Teaching Assessment with Case Vignettes
A specialized protocol for evaluating specific bioethics competencies employs a pre-post questionnaire design utilizing hypothetical case vignettes to assess knowledge and attitude transformation [22].
Instrument Development: Create three fictitious case vignettes, each representing a typical form of scientific misconduct or ethical challenge (e.g., plagiarism, data manipulation). For each vignette, develop assessment items measuring: (1) knowledge (4 dichotomous "yes/no" items), (2) attitudes (4 items using 5-point Likert scales from "strongly agree" to "strongly disagree"), and (3) previous topic exposure (1 "yes/no" item) [22].
Implementation Protocol: Administer the pre-teaching questionnaire at the beginning of the first instructional session. Conduct the ethics course using a combination of theory-based lectures and practice-based case discussion rounds, employing problem-based learning (PBL) methodology with hypothetical case vignettes and analysis of core guidelines. Administer the identical post-teaching questionnaire at the conclusion of the instructional sequence, typically spanning 2-4 weeks [22].
Statistical Analysis: Apply appropriate statistical tests based on data distribution, utilizing McNemar test for paired categorical data and Wilcoxon signed-rank test for non-normally distributed continuous data, with significance level set at p<0.05 [22].
This protocol provides robust quantitative data on ethics education effectiveness while simultaneously familiarizing students with the analytical processes essential to ethical reasoning in professional practice.
Conceptual Frameworks for Bioethics Education
Integrated Clinical Ethics Learning Pathway
The translation of theoretical ethics knowledge to clinical practice requires a structured pathway that connects educational content with practical application. The following framework visualizes this integrative process, from foundational knowledge to clinical competence.
This framework highlights the developmental progression from theoretical understanding to practical competence, emphasizing that ethical reasoning skills are built upon a foundation of core knowledge [7]. The pathway acknowledges that effective bioethics education requires both cognitive and practical components, with clinical application serving as the crucial bridge to professional competence.
Clinical Ethics Consultation Analysis System
Modern bioethics education increasingly incorporates empirical data and standardized analysis frameworks to enhance learning effectiveness. The Armstrong Clinical Ethics Coding System (ACECS) represents an innovative approach that transforms clinical ethics consultation data into educational content [21].
This system addresses a fundamental challenge in bioethics education: the theory-practice divide [21]. By utilizing actual clinical ethics data, it provides students with exposure to real-world ethical issues and patterns, enhancing the relevance and practical application of their learning. The interactive nature of the visual analytics dashboard facilitates exploration of ethical issue frequency, relationships, and contextual factors, supporting the development of pattern recognition skills essential for clinical ethics practice [21].
Research Reagent Solutions for Bioethics Education
The following toolkit comprises essential methodological approaches and conceptual frameworks that serve as fundamental "reagents" for effective bioethics education and research.
Table 3: Essential Methodologies and Analytical Frameworks for Bioethics Education
| Tool/Resource | Primary Function | Application Context |
|---|---|---|
| Four-Box Method | Structured case analysis framework | Clinical ethics decision-making; organizes considerations into medical indications, patient preferences, quality of life, and contextual factors [23] |
| ACECS Coding System | Standardized consultation documentation | Ethics consultation analysis; enables systematic categorization of case types, participants, complexity, and ethical issues [21] |
| Problem-Based Learning (PBL) | Student-centered case-based pedagogy | Classroom instruction; uses hypothetical and real cases to foster analytical skills and ethical reasoning [22] |
| Visual Analytics Dashboard | Interactive data visualization | Curriculum development; identifies patterns in ethics consultation data to inform educational priorities [21] |
| CIPP Evaluation Model | Comprehensive curriculum assessment | Program evaluation; assesses context, input, process, and product dimensions of ethics curricula [7] |
| Sequential Explanatory Design | Mixed-methods research methodology | Curriculum research; combines quantitative and qualitative data for comprehensive program assessment [7] |
These foundational resources enable the systematic implementation and rigorous evaluation of bioethics educational programs. The Four-Box Method, in particular, serves as a widely-adopted analytical framework for clinical ethics case analysis, providing a structured approach to organizing and balancing the diverse considerations inherent in ethical dilemmas [23]. Meanwhile, the ACECS system addresses the critical need for standardized documentation and analysis of ethics consultations, creating a robust empirical foundation for education that reflects actual clinical practice [21].
The 30 essential topics and conceptual frameworks presented in this whitepaper provide a comprehensive blueprint for developing robust bioethics curricula within medical education. The categorical taxonomy spans the critical domains of clinical ethics, research integrity, foundational principles, and emerging technologies, collectively addressing the full spectrum of ethical challenges confronting contemporary medical professionals. This structured approach facilitates the longitudinal integration of ethics education throughout medical training, from pre-clinical instruction through clinical clerkships, ensuring sustained engagement with ethical principles and their practical application.
The quantitative evidence and methodological protocols outlined demonstrate that effective bioethics education requires both theoretical foundation and practical application. As the field continues to evolve in response to technological advancements and societal changes, bioethics curricula must remain dynamic, incorporating empirical data from clinical ethics consultation services and adapting to emerging ethical challenges [21]. The tools and frameworks presented—from the Four-Box Method for case analysis to innovative approaches like the ACECS coding system—provide medical educators with evidence-based resources for developing ethics education that truly prepares graduates for the moral dimensions of medical practice. By implementing such comprehensive bioethics curricula, medical schools can fulfill their essential responsibility to develop professionals capable of navigating the complex ethical terrain of modern healthcare with wisdom, compassion, and moral clarity.
The development of a robust ethical framework is a cornerstone of medical education, essential for preparing clinicians capable of navigating complex moral dilemmas in healthcare. Traditional approaches to ethics education often involved standalone courses or sporadic lectures, which proved insufficient for fostering the deep integration of ethical reasoning into clinical practice. The spiral curriculum model, first conceptualized by Jerome Bruner, offers a transformative alternative by enabling iterative revisiting of core topics with increasing complexity throughout the educational journey [24]. This pedagogical approach recognizes that ethical development is not a singular event but a longitudinal process that evolves with clinical exposure and maturity [25].
In medical education, the spiral curriculum provides the structural foundation for integrating bioethics across a five-year program, ensuring that basic principles introduced in pre-clinical years are reinforced, deepened, and applied in increasingly complex clinical scenarios [3] [26]. This whitepaper examines the implementation, efficacy, and methodological considerations of spiral ethics curricula in undergraduate medical education, drawing upon recent empirical studies to provide a framework for curriculum developers and researchers. By synthesizing quantitative outcomes and qualitative insights from programs implemented in diverse geographical contexts, this analysis aims to establish evidence-based guidelines for optimizing ethics education in medical training.
Theoretical Foundations of the Spiral Curriculum
The spiral curriculum is predicated on cognitive theories advanced by Jerome Bruner, who hypothesized that "any subject can be taught in some intellectually honest form to any child at any stage of development" [24]. This approach challenges linear curriculum models by emphasizing iterative engagement with core concepts at progressively sophisticated levels. Three fundamental principles characterize the spiral curriculum: (1) students revisit topics, themes, or subjects multiple times throughout their educational career; (2) the complexity of the topic increases with each revisit; and (3) new learning continuously relates to and contextualizes previous knowledge [24] [27].
In medical ethics education, this theoretical framework translates to a structured recurrence of ethical concepts across the curriculum, with each encounter building upon previous knowledge while introducing new dimensions appropriate to the learner's clinical experience. The spiral model stands in contrast to non-linear curriculum models that may be better suited to knowledge domains with less structured knowledge domains, such as arts and humanities [27]. Medical ethics, with its foundation in philosophical principles that apply to increasingly complex clinical scenarios, aligns well with the spiral approach's structured progression from simplistic ideas to complicated applications [3] [26].
Table 1: Key Principles of the Spiral Curriculum in Medical Ethics Education
| Principle | Theoretical Basis | Application in Ethics Education |
|---|---|---|
| Iterative Revisiting | Cognitive reinforcement through repeated exposure | Core ethical principles reintroduced in multiple contexts across years |
| Progressive Complexity | Bruner's concept of intellectual development | Basic principles in pre-clinical years advance to complex dilemmas in clinical years |
| Contextual Relationship | Constructivist learning theory | New ethical learning connected to previous knowledge through clinical applications |
Implementation Framework: A Four-Dimensional Model for Ethics Integration
Implementing a spiral curriculum for ethics education requires deliberate structuring across the entire medical program. A recently proposed four-dimensional model offers a comprehensive framework for integrating ethics and professionalism throughout an integrated medical curriculum [26]. This model ensures students learn ethics progressively and apply its principles spontaneously in clinical settings.
The first dimension involves the insertion of ethics issues within modules as part of student-centered activities such as problem-based learning (PBL), case-based learning (CBL), team-based learning (TBL), and hospital-based teaching (HBT). For example, ethical issues related to research are embedded within research methodology modules, while ethical issues of assisted reproduction are integrated into reproductive medicine and women's health curricula [26].
The second dimension consists of structured ethics topics inserted into appropriate modules across all phases of the program. This ensures dedicated attention to fundamental ethical concepts while maintaining their relevance to concurrent coursework.
The third dimension involves implementing a condensed ethics module in the fourth year, which serves to consolidate and synthesize ethical principles before students enter intensive clinical training. This concentrated exposure reinforces previous learning while introducing more nuanced considerations.
The fourth dimension establishes a practice-based ethics course during the internship period, where students encounter ethical issues initially through CBLs and subsequently through direct application with real patients in diverse healthcare situations [26]. This multidimensional approach creates a seamless ethics education trajectory that begins with fundamental principles and culminates in autonomous ethical decision-making.
Table 2: Four-Dimensional Model for Spiral Ethics Curriculum Implementation
| Dimension | Educational Phase | Teaching Modalities | Learning Focus |
|---|---|---|---|
| 1: Embedded Ethics Issues | Years 1-5 | PBL, CBL, TBL, HBT | Contextual application in relevant clinical topics |
| 2: Structured Ethics Topics | Years 1-5 | Dedicated sessions within modules | Foundational knowledge and principle recognition |
| 3: Condensed Ethics Module | Year 4 | Intensive workshops | Synthesis and consolidation of ethical principles |
| 4: Practice-Based Ethics | Internship | CBLs, clinical rotations | Autonomous application in real healthcare settings |
Quantitative Outcomes: Efficacy of Spiral Ethics Curricula
Empirical evidence demonstrates the effectiveness of spiral ethics curricula in developing knowledge, skills, and professional behaviors in medical students. A comprehensive mixed-methods evaluation of a bioethics curriculum integrated across a five-year undergraduate medical program revealed significant positive outcomes across multiple domains [3] [4].
Quantitative data collected through structured questionnaires administered to students across all years of the program indicated that the majority of students agreed the spiral curriculum contributed substantially to their ethical development. Specifically, 60.3-71.2% of students reported enhanced knowledge acquisition, 59.41-60.30% acknowledged improvement in ethical reasoning skills, and 62.54-67.65% recognized development in demonstrating ethical and professional behavior [3]. These quantitative measures demonstrate consistent positive outcomes across the cognitive, psychomotor, and affective domains of learning.
The study employed a mixed methods sequential explanatory design, with quantitative data gathered through structured online questionnaires followed by qualitative data collection through focus group discussions and document review [3]. This methodological approach allowed for comprehensive program evaluation beyond mere satisfaction metrics, capturing substantive learning outcomes across the five-year program.
Table 3: Quantitative Outcomes of Spiral Ethics Curriculum Implementation
| Learning Domain | Student Agreement (%) | Key Measured Elements |
|---|---|---|
| Knowledge Acquisition | 60.3 - 71.2% | Understanding ethical principles, recognition of dilemmas |
| Skill Development | 59.41 - 60.30% | Ethical analysis, moral reasoning, decision-making |
| Professional Behavior | 62.54 - 67.65% | Demonstration of ethical conduct in clinical settings |
Methodological Considerations for Curriculum Evaluation
Rigorous assessment of spiral ethics curricula requires methodological approaches capable of capturing both quantitative outcomes and qualitative insights into the educational process. The mixed methods sequential explanatory design employed in recent studies offers a robust framework for comprehensive curriculum evaluation [3].
In the quantitative phase, researchers utilized a structured online questionnaire administered to 500 students across years 1-5 of the medical program. The questionnaire was developed based on the Context, Input, Process and Product (CIPP) model, which focuses not only on whether the program is working but also identifies areas for improvement [3]. This model facilitated the development of questions related to context (integration in curriculum), input (clarity and relevance of content), and process (teaching methods, assessment, student engagement).
The qualitative phase employed focus group discussions (FGDs) with students and faculty, along with document review, to explain and enrich the quantitative findings [3]. Semi-structured interview guides for FGDs focused on course contents, integration, instructional methods, transition from theory to practice, and student achievement across knowledge, skills, and attitude domains. Faculty FGDs addressed integration, student engagement, course content, methods, assessment, and implementation challenges.
This methodological approach allowed researchers to triangulate findings, with qualitative data providing context and explanation for quantitative results. For instance, while quantitative data indicated overall positive outcomes, qualitative insights revealed specific implementation challenges, such as the need for better integration in clinical years and more opportunities for application in healthcare settings [3].
Instructional Modalities and Pedagogical Approaches
Effective implementation of spiral ethics curricula requires diverse instructional modalities aligned with students' evolving learning needs across the educational continuum. Research indicates that multi-modal instructional methods are particularly effective for ethics education, with student and faculty responses highlighting the value of interactive, engaging approaches [3].
Small group teaching and shorter sessions were identified as preferable formats for fostering discussion and maintaining student engagement and attention [3]. These intimate learning environments facilitate the dialogue and reflection essential for ethical development. In contrast, large class formats were generally perceived as less effective for ethics education, suggesting the importance of personalized interaction in moral development.
Studies highlight the effectiveness of problem-based learning within spiral curricula, using real-life cases and contextually relevant scenarios to facilitate contextual understanding and application of knowledge [3]. In the early years, the content appropriately blends moral philosophy with applied clinical ethics, employing teaching methods that include lectures, discussions, brainstorming, problem-solving exercises, videos/movies, and case studies [3].
As students progress to clinical years, ethics education becomes integrated within clerkships and offered as workshops alongside related topics like gender, culture, and communication [3]. This progression from theoretical foundations to clinical application embodies the spiral approach, reinforcing previously introduced concepts while adding complexity and context-specific considerations.
Digital Infrastructure and Learning Management Systems
The successful implementation of a spiral curriculum requires thoughtful technological support, particularly through Learning Management Systems (LMS) that facilitate students' ability to revisit and build upon previous learning. Research conducted at the University of Cape Town revealed that 70% of medical students revisited previous online courses, primarily to review lecture presentations, lecture notes, and quizzes [28].
This study demonstrated that students perceived significant benefits from maintaining access to previous course materials, particularly for understanding new material, preparation for assessments, and convenience [28]. Although student comments did not always explicitly reference the spiral curriculum, most described processes of building on previous work, with some specifically mentioning the spiral nature of their learning.
These findings have important implications for LMS implementation in medical education. The common practice of archiving and replacing previous online courses may inadvertently hinder the spiral learning process by removing essential reference materials that students use to connect new learning to previous knowledge [28]. Instead, institutions should consider maintaining student access to previous years' course materials to support the iterative revisiting inherent in the spiral approach.
The digital infrastructure should be designed to mirror and support the face-to-face spiral curriculum, with careful attention to how online resource organization either facilitates or impedes students' ability to trace the development of ethical concepts across their educational journey. This alignment between pedagogical philosophy and technological implementation is essential for realizing the full potential of the spiral curriculum model.
Challenges and Implementation Barriers
Despite its theoretical strengths and demonstrated efficacy, implementing spiral ethics curricula presents significant challenges that require strategic addressing. Research identifying a "broken spiral" phenomenon highlights how students may struggle when introduced to more complex new topics without having mastered previous foundational concepts [29].
Studies of spiral curriculum implementation in various contexts reveal several common barriers. Teachers often struggle with the pacing of new concepts, with average instructional time across a year sometimes amounting to less than 30 minutes for 70% of topics [30]. This insufficient exposure time compromises mastery development, essential for the spiral approach. Additional challenges include curriculum congestion, inadequate review periods, and variations in teachers' content knowledge and mastery, all of which impact curriculum continuity [30] [29].
In ethics education specifically, participants have identified needs for better integration in clinical years, enhanced role modeling, and more opportunities for application in clinical healthcare settings [3]. Additionally, both students and faculty have suggested expanding curriculum content to include emerging ethical topics such as ethical issues related to social media use, public health ethics, and the intersection of ethics and law [3].
Faculty development represents another critical challenge, as effective spiral curriculum implementation requires teachers to understand both the philosophical foundations of the approach and its practical application across year levels. Without adequate faculty buy-in and training, the intended spiral progression may fail to materialize in student learning experiences.
Table 4: Essential Methodological Resources for Spiral Ethics Curriculum Research
| Resource Category | Specific Tools/Approaches | Application in Curriculum Development |
|---|---|---|
| Evaluation Frameworks | CIPP Model (Context, Input, Process, Product) | Comprehensive curriculum assessment across multiple dimensions |
| Research Designs | Mixed Methods Sequential Explanatory Design | Integration of quantitative outcomes with qualitative insights |
| Data Collection Methods | Structured questionnaires, Focus Group Discussions, Document Review | Triangulation of data sources for robust evaluation |
| Assessment Modalities | Portfolios, Ethical Reasoning Assessments, Behavioral Observations | Longitudinal tracking of ethical development |
| Theoretical Frameworks | Bruner's Spiral Curriculum, Constructivist Learning Theory | Philosophical foundation for curriculum structure |
Future Directions and Research Agenda
The evolution of spiral ethics curricula in medical education necessitates continued research and innovation. Several promising directions emerge from current literature. First, establishing Entrustable Professional Activities (EPAs) in ethics would provide concrete milestones for assessing students' readiness for increasingly independent ethical decision-making [25]. These EPAs could be mapped to specific points in the spiral curriculum, creating clear developmental trajectories.
Second, further exploration of portfolio-based assessment offers potential for capturing the longitudinal development of ethical reasoning and professional identity formation [25]. Portfolios can document the iterative deepening of ethical understanding central to the spiral approach, providing rich data for both assessment and research.
Third, research should investigate contextual factors influencing curriculum effectiveness across diverse institutional and cultural settings [3]. As ethics education increasingly acknowledges cultural dimensions of moral reasoning, understanding how spiral curricula function in different contexts becomes essential.
Fourth, emerging technologies, including artificial intelligence and virtual reality, present opportunities for creating simulated ethical dilemmas that progress in complexity alongside student development. These technologies could provide controlled environments for practicing ethical decision-making at various spiral curriculum stages.
Finally, research on faculty development models for spiral curriculum implementation would address a critical implementation barrier. Effective faculty preparation is essential for maintaining curriculum fidelity and ensuring the spiral approach's theoretical benefits translate to tangible learning outcomes.
The spiral curriculum model represents a pedagogically sophisticated approach to ethics education that aligns with the longitudinal nature of ethical development in medical training. By enabling iterative engagement with core ethical concepts at progressively complex levels, this approach fosters the deep integration of moral reasoning into clinical practice. Evidence from implemented programs demonstrates significant positive outcomes in knowledge acquisition, skill development, and professional behaviors.
Successful implementation requires careful attention to curriculum design, instructional modalities, assessment strategies, and digital infrastructure. The four-dimensional model offers a comprehensive framework for integrating ethics across the educational continuum, while mixed-methods evaluation provides insights into program effectiveness and areas for improvement. As medical education continues to evolve, the spiral curriculum approach provides a robust foundation for preparing ethically grounded physicians capable of navigating the complex moral landscape of modern healthcare.
From Theory to Practice: Innovative Pedagogies and Engaging Instructional Methods
The evolution of medical education has witnessed a paradigm shift from traditional, teacher-centered didactic lectures toward interactive, student-centered learning approaches. This transformation is particularly crucial in bioethics curriculum development, where navigating complex moral dilemmas requires more than passive knowledge acquisition. Active learning paradigms engage learners through collaborative problem-solving, critical analysis, and practical application—essential competencies for managing ethical challenges in clinical practice and research settings.
Research demonstrates that active learning strategies significantly enhance knowledge retention, critical thinking abilities, and problem-solving skills compared to passive lecture-based formats [31]. In bioethics education, these approaches enable learners to grapple with nuanced ethical dilemmas they will encounter as healthcare providers and researchers. This whitepaper synthesizes current evidence and methodologies for implementing active learning paradigms, with specific application to bioethics education for medical professionals.
Theoretical Framework and Evidence Base
Cognitive Foundations of Active Learning
Active learning aligns with constructivist learning theories, which posit that learners build knowledge through authentic, engaged experiences rather than passively receiving information [31]. The ICAP framework (Interactive, Constructive, Active, Passive) delineates how different learning activities correlate with cognitive engagement and learning outcomes. Interactive activities, such as collaborative debate and problem-solving, generate the deepest level of understanding and knowledge retention [31].
Bloom's revised taxonomy further explains the effectiveness of active learning for developing higher-order thinking skills (HOTS). While didactic lectures primarily target remember and understand levels, active learning strategies effectively facilitate application, analysis, evaluation, and creation [31]. This is particularly valuable in bioethics education, where learners must analyze complex situations, evaluate competing values, and construct ethically sound approaches to clinical and research dilemmas.
Quantitative Evidence of Efficacy
Comparative studies demonstrate the superior efficacy of active learning methodologies over traditional approaches. A mixed-methods study examining Work-Station Learning Activities (WSLA) found significantly improved performance on learning objectives requiring higher-order thinking:
Table 1: Academic Performance Comparison Between Traditional and Active Learning Methodologies [31]
| Learning Objective Type | Traditional Methodology | WSLA Methodology | P-value |
|---|---|---|---|
| Lower-order thinking skills (memorization) | 38.8% | 39.0% | 0.955 |
| Higher-order thinking skills (integration) | 54.2% | 68.5% | <0.001 |
| Probability of mastering complex objectives | Reference | 1.64x higher (OR: 1.15-2.34) | 0.007 |
Multivariate analysis confirmed that students experiencing WSLA methodology were 1.64 times more likely to master complex learning objectives compared to their peers in traditional learning environments [31]. This enhanced performance for higher-order skills is precisely what bioethics education requires for developing clinical ethical reasoning.
Student Perceptions and Engagement Outcomes
Qualitative analyses reveal that students perceive active learning formats as more engaging and effective. In evaluations of integrated ethics modules, medical students rated different teaching modalities significantly differently:
Table 2: Medical Student Perceptions of Different Ethics Learning Modalities [32]
| Teaching Modality | Perceived Usefulness | Key Student Feedback |
|---|---|---|
| Small group discussion/debate | Highest rating | Preferred for fostering dialogue and multiple perspectives |
| Documentary with reflective writing | Intermediate rating | Valued for emotional engagement and contextual understanding |
| Case scenario only | Lowest rating | Found less engaging without structured interaction |
Thematic analysis of student feedback identified three dominant themes: general favorable impression of integrated ethics teaching, perceived learning outcomes including ethical analysis skills, and constructive critiques for improvement [32]. Students particularly valued the opportunity to actively apply ethical frameworks to realistic scenarios.
Implementing Active Learning in Bioethics Education
Integrated Ethics Module Design
Effective integration of bioethics within medical curricula requires strategic design. A cross-sectional study implemented three distinct ethics learning modules within a biomedical science course, demonstrating successful integration approaches:
Table 3: Experimental Protocol for Implementing Integrated Ethics Modules [32]
| Module Component | Implementation Protocol | Cognitive Engagement Level |
|---|---|---|
| Module 1: Documentary | Asynchronous viewing of "The Boy in the Bubble" documentary with reflective writing on surrogate decision-making | Active to Constructive |
| Module 2: Clinical Scenario | Team-based learning on HIV patient case exploring confidentiality versus mandatory reporting | Interactive |
| Module 3: Debate | Small group discussion and formal debate on Jehovah's Witness blood transfusion case | Interactive |
This curriculum design highlighted foundational biomedical sciences alongside ethical dilemmas that physicians likely face in practice [32]. The small group discussion and debate format received significantly higher usefulness ratings from students, indicating the value of highly interactive modalities for ethics education.
Work-Station Learning Activities (WSLA)
The WSLA model provides a structured framework for implementing active learning in medical education. This methodology organizes learning into sequential stations where student teams collaboratively complete tasks integrating basic and clinical sciences:
Table 4: Research Reagent Solutions for WSLA Implementation [31]
| Component | Function | Implementation Example |
|---|---|---|
| Clinical Scenarios | Provide authentic context for learning | Blood typing and transfusion compatibility case |
| Structured Worksheets | Guide team discussion and problem-solving | Question sets progressing from identification to analysis |
| iRAT/eRAT Assessments | Evaluate individual and group understanding | Multiple-choice questions targeting specific learning objectives |
| Facilitator Guidance | Support without directing problem-solving | Prompting questions rather than providing answers |
This methodology has demonstrated particular effectiveness for objectives requiring knowledge integration and application, with quantitative analysis showing significantly improved performance on higher-order thinking questions compared to traditional practical activities [31].
Longitudinal Curriculum Integration
A decade-long evaluation of a bioethics curriculum fully integrated across a five-year medical program demonstrated the effectiveness of longitudinal implementation. This spiral curriculum introduces fundamental concepts in pre-clinical years with reinforcement and application during clinical rotations [3]. Quantitative assessment revealed that the majority of students agreed the curriculum contributed to their knowledge acquisition (60.3-71.2%), skill development (59.41-60.30%), and demonstration of ethical behavior (62.54-67.65%) [3].
Qualitative findings identified small group teaching and shorter sessions as preferable for fostering discussion and maintaining engagement. Participants recommended enhanced clinical integration, particularly through role modeling and applied opportunities during clinical rotations [3]. This longitudinal approach facilitates the development of ethical reasoning that evolves in sophistication throughout medical training.
Emerging Technologies and Future Directions
Immersive Learning Technologies
Mixed reality and virtual reality platforms represent the frontier of active learning innovation. These technologies enable procedural practice and empathy development through realistic clinical scenarios without risking patient safety [33]. Next-generation platforms incorporate narrative elements that follow patients across the care continuum, allowing learners to develop both technical skills and interpersonal abilities [33].
The integration of artificial intelligence as an intelligent tutor creates adaptive learning experiences that customize content based on individual learner performance [33]. This personalization addresses variable learning trajectories while ensuring all students achieve competency standards.
Systematic Implementation Frameworks
A systematic mapping of bioethics institutionalization in higher education revealed significant concentration in health sciences (81.3% of studies) but uneven implementation across educational levels [15]. This analysis identified critical gaps in comparative practices research (2% of studies) and limited evidence on institutionalization of bioethics research (10.3%) [15].
The integration of active methodologies and educational technologies has enhanced bioethics programs (21.4% of studied implementations), fostering more interactive learning environments [15]. Future development requires cooperation between institutions and research networks to share best practices and facilitate widespread integration across diverse educational contexts.
Active learning paradigms offer powerful alternatives to traditional didactic approaches, particularly for bioethics education where navigating complex dilemmas requires practiced reasoning skills. Evidence demonstrates that methodologies such as small group discussions, work-station learning activities, and longitudinal integrated curricula significantly enhance learning outcomes, particularly for higher-order thinking skills essential to ethical analysis.
Successful implementation requires strategic curriculum design that incorporates authentic clinical scenarios, structured interaction, and progressively challenging applications. Emerging technologies promise enhanced realism and personalization, while systematic institutionalization supports sustainable implementation. For medical education researchers and curriculum developers, these active learning paradigms provide empirically validated approaches for developing the ethical reasoning capacities essential to clinical practice and research.
Team-Based Learning (TBL) represents a transformative active learning methodology that effectively addresses longstanding challenges in bioethics education for healthcare professionals. This technical guide examines the structure, efficacy, and development of TBL modules within bioethics curricula, drawing upon empirical data from implemented programs across medical education contexts. Evidence demonstrates that TBL significantly enhances knowledge acquisition, ethical decision-making capabilities, and learner engagement through its structured sequence of preparation, assessment, and application exercises. The framework presented herein provides researchers and educators with validated methodologies for implementing TBL approaches that develop competencies essential for navigating complex ethical dilemmas in clinical practice and research settings.
Bioethics education faces significant implementation challenges despite its recognized importance in medical training. The Accreditation Council for Graduate Medical Education (ACGME) and numerous medical boards explicitly require ethics training, yet programs struggle with "curricular crowding," lack of faculty expertise, insufficient administrative support, and minimal trainee engagement [2] [34]. Traditional ethics education often fails to bridge the theory-to-practice divide, leaving professionals underprepared for ethical challenges in actual clinical environments [34].
Team-Based Learning offers a promising pedagogical approach that addresses these limitations through its structured, collaborative format. TBL moves beyond passive knowledge transmission to active application of ethical principles, creating a dynamic learning environment where participants develop both conceptual understanding and practical reasoning skills [2] [35]. This guide examines the evidence-based framework for implementing TBL in bioethics education, presenting its core structure, efficacy data, and development methodologies for researchers and educators designing ethics curricula.
TBL Methodology: Core Structure and Implementation
The TBL Instructional Sequence
TBL follows a specific instructional sequence that creates a comprehensive learning experience. The methodology employs a flipped classroom approach where learners prepare individually before engaging in collaborative, facilitator-guided activities [35]. This structure efficiently uses limited instructional time while promoting deeper learning through immediate application of concepts.
The TBL process follows a structured sequence: (1) Pre-class preparation where learners independently study assigned materials; (2) Individual Readiness Assurance Test (iRAT) assessing basic knowledge comprehension; (3) Group Readiness Assurance Test (gRAT) where teams discuss and reach consensus on the same questions; (4) Immediate feedback through scratch-off cards (IFAT) that reveal correct answers; and (5) Team Application Exercises (TApp) where learners apply knowledge to complex, realistic scenarios [2] [35].
Curricular Integration and Theoretical Foundation
Effective TBL implementation in bioethics requires thoughtful curricular integration and theoretical grounding. Successful programs have implemented longitudinal curricula spanning multiple years, with approximately 10 TBL sessions distributed across a three-year residency program [2]. These curricula typically incorporate L. Dee Fink's principles of "Significant Learning" to create transformative educational experiences that integrate foundational knowledge, application, and self-awareness [34].
For ethical analysis, TBL modules frequently utilize structured frameworks such as Jonsen et al.'s "Four-Box Method" (medical indications, patient preferences, quality of life, and contextual features) to provide learners with a consistent approach to ethical dilemmas [2]. This methodological consistency allows learners to develop transferable skills in ethical reasoning that extend beyond individual cases to broader clinical practice.
Efficacy and Outcomes: Quantitative and Qualitative Evidence
Knowledge Acquisition and Application
TBL demonstrates significant effectiveness in improving knowledge acquisition and application in bioethics education. Research across multiple institutions and learner levels consistently shows measurable gains in ethical reasoning capabilities through comparative assessment data.
Table 1: Knowledge Assessment Outcomes in TBL Bioethics Education
| Learner Population | Sample Size | iRAT Scores (Mean) | gRAT Scores (Mean) | Statistical Significance | Citation |
|---|---|---|---|---|---|
| Pediatric Residents | 348 encounters | 72% | 89% | p < 0.001 | [2] |
| Medical Students (Nepal) | 29 students | Median: 7 (TBL1) | Median: 9 (TBL1) | p = 0.006 (TBL1) | [36] |
| Median: 7 (TBL2) | Median: 9.5 (TBL2) | p = 0.001 (TBL2) | [36] |
The consistently higher gRAT scores across studies demonstrate the collaborative learning benefits of TBL, where group discussion and knowledge sharing enhance collective understanding [2] [36]. This pattern holds across different educational levels and cultural contexts, suggesting the methodology's robust effectiveness.
Learner Engagement and Satisfaction
Beyond knowledge acquisition, TBL generates high levels of learner engagement and satisfaction despite initial perceptions of bioethics as less relevant to clinical practice. In a comprehensive study with pediatric residents, satisfaction ratings averaged 4.42/5 on a Likert scale despite low pre-work completion rates (28%), indicating that the in-class TBL process effectively engages learners even when preparatory work is incomplete [2].
Qualitative analysis of learner reflections reveals several thematic benefits:
- Changed attitudes toward ethics' clinical relevance [37]
- Application of ethical principles to contemporary practice [37]
- Effective use of ethical terminology in appropriate contexts [37]
- Enhanced appreciation for collaborative problem-solving [34]
Faculty observers similarly reported increased engagement, deeper understanding, and better application of ethical principles compared to traditional lecture-based formats [37].
TBL Module Development: Framework and Implementation Protocols
Evidence-Based Development Process
Developing effective TBL modules for bioethics follows a systematic process grounded in educational theory and evidence-based practices. The development sequence integrates content expertise with pedagogical principles to create robust learning experiences.
The development process begins with a comprehensive needs analysis identifying specific educational gaps and contextual barriers [34]. Developers then create specific learning objectives aligned with relevant certification requirements (e.g., American Board of Pediatrics content specifications) [2]. Content is structured around high-prevalence ethical challenges encountered in target practice environments, ensuring clinical relevance and learner engagement.
Core Component Specifications
Each TBL module consists of several core components that must be carefully developed to ensure educational effectiveness:
- Pre-reading Materials: Concise, focused resources (typically 2-3 articles or book chapters) that introduce fundamental concepts and principles [37]
- Readiness Assurance Tests (iRAT/gRAT): 10-15 multiple-choice questions assessing comprehension of pre-reading materials, with questions progressing from basic knowledge to preliminary application [2]
- IFAT (Immediate Feedback Assessment Technique) Cards: Scratch-off cards used during gRAT that provide immediate feedback and encourage discussion [35]
- Team Application Exercises: Complex, realistic ethical dilemmas requiring teams to apply ethical frameworks, make specific choices, and defend their reasoning [2]
Implementation Protocol
Successful implementation follows a structured protocol that maximizes learning outcomes while accommodating logistical constraints:
- Session Timing: Dedicate 90-120 minutes per TBL module to allow adequate discussion [35]
- Group Composition: Form diverse teams of 5-7 learners, maintaining consistent groups across sessions when possible [2]
- Faculty Facilitation: Train facilitators in guided questioning rather than didactic instruction, emphasizing discussion management over content expertise [35]
- Sequencing: Introduce ethical frameworks early (e.g., Four-Box Method in initial sessions), then progress to application across various clinical scenarios [35]
Implementing TBL in bioethics education requires specific resources and materials that facilitate the structured learning process. The following table outlines essential components with their functions and implementation considerations.
Table 2: Essential Research Reagents and Resources for TBL Implementation
| Resource Category | Specific Components | Function and Application | Implementation Notes |
|---|---|---|---|
| Assessment Tools | iRAT/gRAT questions | Assess individual and group comprehension of pre-class materials | Questions should progress from knowledge recall to preliminary application [2] |
| Feedback Mechanisms | IFAT (Immediate Feedback Assessment Technique) cards | Provide immediate feedback during group assessment, promote discussion | Available from commercial educational suppliers [35] |
| Analytical Frameworks | Four-Box Method (Jonsen et al.) | Structured approach to ethical case analysis | Introduce in initial module, use consistently across curriculum [2] |
| Application Exercises | Realistic clinical ethical dilemmas | Enable application of ethical principles to complex scenarios | Should reflect challenges learners encounter in practice [2] [37] |
| Content Guidance | American Board of Pediatrics ethics specifications; AAP bioethics modules | Ensure content alignment with certification requirements and standards | Adapt to specific learner levels and specialties [2] |
| Theoretical Foundation | Fink's "Significant Learning" principles | Guide curricular design for transformative learning experiences | Address situational factors and barriers specific to institution [34] |
Discussion and Future Directions
The evidence demonstrates that TBL provides an effective pedagogical approach for bioethics education, addressing persistent challenges in developing ethical reasoning competencies among healthcare professionals. The methodology's structured collaborative process facilitates both knowledge acquisition and application skills, effectively bridging the theory-practice divide that often limits ethics education.
Future development should explore several promising directions:
- Adaptation for hybrid and virtual formats using online collaboration tools [36]
- Expansion to interprofessional ethics education involving diverse healthcare teams
- Integration of emerging ethical challenges including digital health, AI applications, and public health ethics [3]
- Development of specialty-specific modules tailored to unique ethical challenges in various medical disciplines
TBL's demonstrated efficacy across diverse educational contexts, combined with its relatively low resource requirements compared to small-group tutorial models, positions it as a sustainable approach for enhancing bioethics education in an era of curricular constraints. By implementing the structured framework outlined in this guide, educators can develop robust ethics curricula that prepare healthcare professionals for the complex ethical challenges of contemporary practice.
Dramatic Arts Casuistry represents a sophisticated pedagogical innovation that merges the analytical rigor of bioethics case-based learning with the immersive, empathetic engagement of theatrical performance. This methodology employs performable case studies and readers' theater to create dynamic learning environments where medical students, healthcare professionals, and bioethics students can explore complex ethical dilemmas through dialogic form. Rooted in the ancient tradition of Platonic dialogues [38] [39], this approach revitalizes ethics education by transforming passive learning into an active, participatory process that stimulates profound moral reflection.
The theoretical foundation of Dramatic Arts Casuistry bridges the medical humanities with core bioethics education, addressing a critical gap in traditional pedagogical approaches. Where conventional ethics teaching often relies on abstract principles or retrospective case analysis, performable case studies create live ethical encounters that unfold in real time, allowing participants to experience the nuanced complexities of healthcare dilemmas from multiple perspectives simultaneously. This method aligns with the growing recognition within medical education that ethical reasoning is not merely an intellectual exercise but a professional capacity developed through practiced engagement with realistic scenarios [38] [7].
Framed within broader bioethics curriculum development research, Dramatic Arts Casuistry addresses identified gaps in the current educational landscape. Systematic analyses of bioethics integration in higher education reveal significant concentration in health sciences (81.3%) but limited evidence on institutionalization of bioethics research (10.3%) and minimal studies on comparative practices and replicated experiences (2%) [15]. This methodology offers a transferable pedagogical model that can enhance bioethics education across diverse institutional contexts, providing both a theoretical framework and practical implementation strategies.
Theoretical Foundations and Historical Development
Philosophical Origins and Educational Precedents
The conceptual roots of Dramatic Arts Casuistry extend to the dialogic traditions of ancient Greek philosophy and theater. The Platonic Dialogue "Euthyphro" serves as an early exemplar of the performable case study, presenting a fundamental ethical question through conversational form that interrogates issues from multiple perspectives without succumbing to moral absolutism or relativism [38] [39]. This ancient model demonstrates how dialogic exchange can illuminate ethical complexities through what contemporary developers term "dramatic arts casuistry" – the creation and performance of short case studies specifically designed to raise bioethics issues for discussion [38].
Modern medical humanities education has long incorporated ethics teaching through literature, film, and narrative studies. Standard educational resources have included short stories like William Carlos Williams' "The Use of Force," films such as "Whose Life Is It Anyway?" and "Wit" (both originally stage plays), "GATTACA," "The Doctor," and novels including "Never Let Me Go" [38] [39]. These materials present case examples that highlight ethical issues vividly for diverse student populations. However, the distinctive innovation of Dramatic Arts Casuistry lies in shifting students from passive consumers of existing narratives to active creators and performers of ethical scenarios [38].
Programmatic Evolution and Institutional Adoption
The specific methodology of Performable Case Studies emerged from structured academic programming rather than theoretical speculation alone. In 1989-1990, the Department of Social Medicine at the University of North Carolina (UNC)-Chapel Hill School of Medicine introduced "Medicine and Theater" into the preclinical curriculum for second-year medical students [38] [39]. This initiative engaged issues in biomedical ethics, research ethics, and physician-patient relationships through the development and presentation of dramatic literature, representing a radical departure from conventional ethics pedagogy.
The model evolved from extracurricular beginnings into formal curriculum. It originated in 1988 as an enrichment activity for medical students at UNC-Chapel Hill, funded by the North Carolina Humanities Council as community outreach [38] [39]. The first staged reading adapted William Carlos Williams' short story "Mind and Body" from "The Doctor Stories," presented initially at the UNC Student Union and later in community settings. The successful adaptation of this primarily dialogic story established the persistent presentation model: short performances followed by moderated discussions between readers and audience [38]. This format proved sufficiently compelling to generate multi-institutional collaboration, with UNC-Chapel Hill, East Carolina University, and Duke University securing a 3-year Exemplary Award from the National Endowment for the Humanities (1990-1992) to support traveling readers' theater companies [38].
The program demonstrated remarkable institutional transferability when adapted in 2010 for the Graduate Program in Bioethics at Wake Forest University, and in modified form for undergraduate students in the Department of Communication [38] [39]. This successful translation across educational levels and institutional contexts suggests the methodology's robust applicability to diverse learning environments and student populations, from medical trainees to graduate ethics students and undergraduates.
Methodological Implementation and Protocols
Core Structural Framework
The implementation of Dramatic Arts Casuistry follows a structured protocol that transforms ethical analysis into performative exploration. The foundational process involves students researching, writing, and performing original case studies in dialogic form specifically designed to provoke thoughtful consideration and discussion of bioethical issues [38] [39]. This methodology employs the staged reading format where performers read rather than memorize lines, with minimal use of stage movement and props, lowering technical barriers to participation while maintaining dramatic impact [38].
The presentation model has remained consistent through the methodology's evolution: a short performance followed by a facilitated discussion between the readers and audience, moderated by a scholar in medical humanities or bioethics [38]. This structure creates an integrated learning experience where performance stimulates reflection and discussion deepens understanding. The curtain speech explaining this format and the integral role of post-performance discussion establishes clear expectations and prepares audiences for participatory engagement [38].
Table 1: Core Structural Elements of Performable Case Studies
| Component | Description | Educational Function |
|---|---|---|
| Dialogic Case Development | Student-researched and written case studies in dialogue form | Engages research, analysis, and ethical framing skills |
| Staged Reading Performance | Script-in-hand performances with minimal staging | Lowers technical barriers while maintaining dramatic impact |
| Moderated Discussion | Post-performance dialogue between performers and audience | Facilitates reflective analysis and multiple perspective consideration |
| Interdisciplinary Collaboration | Involvement of students from medicine, bioethics, communication | Breaks down disciplinary silos and enriches perspective sharing |
Experimental Protocol for Educational Implementation
The implementation of Dramatic Arts Casuistry in curriculum development follows a replicable protocol with distinct phases:
Phase 1: Research and Scenario Development (2-3 weeks)
- Student teams identify and research current bioethics issues of relevance to both academic and general audiences [38]
- Teams conduct literature reviews covering clinical, ethical, and contextual dimensions of selected issues
- Faculty mentors ensure research comprehensiveness and methodological rigor
Phase 2: Script Development and Dramatization (3-4 weeks)
- Teams transform research findings into dialogic case studies featuring multiple perspectives
- Scripts incorporate authentic clinical language and realistic ethical tensions
- Workshops with dramatic arts faculty enhance theatrical effectiveness while maintaining ethical complexity
Phase 3: Rehearsal and Discussion Preparation (1-2 weeks)
- Readers explore characters and scenarios through guided discussion during rehearsals [38]
- Performers develop questions for post-performance discussion based on character insights
- Moderation preparation establishes discussion framework and key thematic areas
Phase 4: Performance and Facilitated Dialogue (Single Session)
- Staged reading performed for target audience (typically 15-30 minutes)
- Moderated discussion between performers and audience (30-45 minutes)
- Session documentation for subsequent reflection and assessment
This protocol emphasizes the dual engagement central to the methodology's effectiveness: performers gain insights through character embodiment, while audiences engage through witnessed performance and participatory discussion [38]. The combination creates multi-layered learning unavailable through conventional case discussion.
Diagram 1: Implementation Workflow for Dramatic Arts Casuistry. This protocol outlines the phased approach to integrating performable case studies into bioethics curriculum, highlighting key activities at each developmental stage.
Empirical Support and Assessment Data
Documented Outcomes and Effectiveness Metrics
Research on Dramatic Arts Casuistry methodologies demonstrates significant educational impact across multiple dimensions. A comprehensive evaluation study of an integrated bioethics curriculum utilizing mixed methods approaches revealed that students affirmed the contribution of bioethics education to their personal and professional development and ethical positioning [7]. Quantitative findings from this decade-long curriculum implementation showed that the majority of students agreed the curriculum contributed to their knowledge acquisition (60.3-71.2%), skill development (59.41-60.30%), and demonstration of ethical/professional behavior (62.54-67.65%) [7].
Medical Readers' Theater (MRT), a closely related methodology, has shown particular effectiveness in addressing challenging topics in medical education. In geriatrics medical education, MRT provided an innovative approach to helping medical students reflect on difficult-to-discuss topics including aging stereotypes, disability and loss of independence, sexuality, assisted living, relationships with adult children, and end-of-life issues [40]. Program evaluations demonstrated positive benefits for both student and senior participants in terms of greater awareness of each other's perspectives and improved communication [40].
Table 2: Documented Educational Outcomes of Performance-Based Bioethics Education
| Outcome Category | Specific Findings | Methodological Context |
|---|---|---|
| Knowledge Acquisition | 60.3-71.2% student agreement on contribution to knowledge [7] | Integrated bioethics curriculum evaluation |
| Skill Development | 59.41-60.30% student agreement on skill development [7] | Mixed methods assessment across 5-year program |
| Professional Behavior | 62.54-67.65% student agreement on influencing ethical behavior [7] | Longitudinal curriculum evaluation |
| Perspective Recognition | Improved awareness of different viewpoints [40] | Medical Readers' Theater in geriatrics education |
| Communication Skills | Enhanced communication between students and seniors [40] | Intergenerational MRT program |
Comparative Methodological Advantages
The systematic mapping of bioethics institutionalization in higher education reveals that integration of active methodologies and educational technologies has enhanced bioethics programmes (21.4% of studies), fostering more interactive and engaged learning environments [15]. Dramatic Arts Casuistry aligns with this trend while addressing identified gaps in comparative practices and replicated experiences (2% of studies) [15].
Evaluation studies of bioethics curricula have yielded consistent findings regarding optimal instructional methods. Multi-modal instructional methods used in performance-based approaches were stated to be effective and engaging, with small group teaching and shorter sessions preferred for fostering discussion and maintaining student engagement and attention [7]. These findings directly support the structural choices embedded in Dramatic Arts Casuistry, particularly its emphasis on collaborative small-group development and focused, shorter performances followed by discussion.
Practical Applications and Contextual Adaptations
Specialized Implementation Protocols
Geriatrics Medical Education Protocol A required Medical Readers' Theater experience was successfully implemented for third-year medical students on Family Medicine clerkships, incorporating volunteer residents from a continuing care retirement community [40]. This specialized adaptation followed a structured protocol:
- Identification of geriatrics-specific challenging topics (aging stereotypes, disability, end-of-life issues)
- Development of scripted materials addressing these thematic concerns
- Collaborative sessions bringing medical students and senior community residents together
- Facilitated discussions focusing on intergenerational perspectives and communication This implementation demonstrated the methodology's flexibility in addressing domain-specific ethical challenges while maintaining core structural elements.
Pandemic Communication Adaptation Recent innovations have applied dramatic arts principles to healthcare communication challenges during COVID-19, exploring the relationship between face and mask to guide healthcare workers in communicating from behind personal protective equipment [41]. This adaptation drew explicit connections to Ancient Greek theater where actors performed wearing masks and used oratory and gestural communication to engage audiences [41]. The adaptation protocol included:
- Analysis of verbal and gestural communication techniques from dramatic training
- Identification of compensatory communication strategies (eye emphasis, gesture exaggeration, vocal projection)
- Implementation of connection-facilitating tools (photo cards, transparent masks)
- Peer simulation exercises practicing communication through barriers This application demonstrates the methodology's relevance to contemporary healthcare challenges beyond formal ethics education.
Integration Framework for Curriculum Development
The effective integration of Dramatic Arts Casuistry within broader bioethics curricula follows principles identified through longitudinal evaluation studies. Research indicates that an effective bioethics curriculum for undergraduate medical education should run longitudinally across the 5-year curriculum and be integrated in modules and clerkships [7]. Optimal integration places basic knowledge and skill acquisition in Years 1 & 2 with reinforcement and application in Years 3-5 [7].
Successful implementation depends on strategic institutional support and faculty development. Participants in curriculum evaluation studies suggested that bioethics education could be strengthened by better integration in clinical years, role modelling, and providing opportunities for application in clinical health care settings [7]. These findings emphasize that Dramatic Arts Casuistry functions most effectively as part of a comprehensive ethics curriculum rather than as a standalone intervention.
Diagram 2: Curricular Integration Framework. This model illustrates how Dramatic Arts Casuistry integrates within a comprehensive bioethics curriculum, showing developmental progression from foundational to applied learning across undergraduate medical education.
Successful implementation of Dramatic Arts Casuistry utilizes specific tools and resources that facilitate the development and execution of performable case studies. These materials provide both structural frameworks and content resources that support educational effectiveness.
Table 3: Essential Research Reagents for Dramatic Arts Casuistry Implementation
| Tool/Resource | Function | Implementation Role |
|---|---|---|
| Medical Readers' Theater: A Guide and Scripts | Published collection of 14 readers' theater scripts with implementation guide [42] | Provides ready-made performable materials and procedural guidance for initial implementation |
| Literature, Arts, and Medicine Database (NYU) | Extensive database of literary works, films, and artistic resources addressing medical themes [38] [39] | Source materials for adaptation and contextual references for case development |
| Staged Reading Format | Performance approach using scripts without memorization, minimal staging [38] | Lowers technical barriers to implementation while maintaining dramatic impact |
| Post-Performance Discussion Framework | Structured facilitation protocol for audience-performer dialogue [38] | Enables reflective ethical analysis and perspective sharing following performances |
| Interdisciplinary Development Teams | Collaborative groups combining medicine, bioethics, drama, communication [38] | Brings diverse expertise to case development ensuring clinical accuracy and dramatic effectiveness |
Adaptation and Contextualization Protocols
The methodological framework includes specific adaptation tools that enable customization for different educational contexts and learning objectives:
Curricular Integration Assessment Tool
- Mapping of existing bioethics curriculum content and identification of integration points
- Analysis of clinical contexts where ethical dilemmas emerge most prominently
- Sequencing of performable case studies to match student developmental progression
- Faculty development resources for facilitating dramatic arts methodologies
Cultural and Contextual Adaptation Framework
- Template for modifying ethical scenarios to reflect local cultural norms and values
- Guidelines for maintaining ethical complexity while ensuring cultural relevance
- Protocol for engaging diverse stakeholders in scenario development and review
- Assessment rubric for evaluating contextual appropriateness of performable cases
These implementation tools provide the necessary scaffolding for institutions to adapt Dramatic Arts Casuistry to their specific educational contexts while maintaining methodological integrity and educational effectiveness.
Dramatic Arts Casuistry represents a significant advancement in bioethics education methodology, addressing identified gaps in current approaches while aligning with evidence-based pedagogical principles. This approach moves beyond conventional case-based learning by creating immersive, multi-perspective ethical encounters that engage students cognitively, emotionally, and morally. The methodology's demonstrated effectiveness across diverse educational contexts and learner populations supports its value as a component of comprehensive bioethics curriculum development.
The integration of performable case studies and readers' theater within broader bioethics education offers a responsive approach to addressing the complex ethical challenges facing healthcare professionals. By creating spaces for simulated ethical practice within safe educational environments, Dramatic Arts Casuistry develops the moral reasoning capacities, perspective-taking abilities, and communicative competencies essential for ethical clinical practice. As medical education continues to evolve in response to emerging healthcare challenges, this methodology provides a flexible, evidence-informed approach to preparing healthcare professionals for the ethical complexities of contemporary practice.
For researchers and curriculum developers, Dramatic Arts Casuistry offers a rich area for further investigation, particularly regarding longitudinal impacts on clinical ethical behavior, comparative effectiveness across different learner populations, and technological innovations that may expand accessibility and implementation scalability. The methodology's strong theoretical foundations, practical implementation protocols, and documented outcomes position it as a valuable contribution to the ongoing development of bioethics education for health professionals.
A significant and persistent challenge in bioethics education is the theory-practice gap, where learners struggle to apply abstract ethical principles to the complex, often ambiguous situations they encounter in clinical and research settings [43]. This divide represents a critical barrier to developing healthcare professionals who can effectively navigate moral dilemmas in practice. Educational research has consistently identified that without explicit strategies to connect theoretical knowledge with practical application, even well-designed ethics curricula may fail to produce graduates who can demonstrate ethical competence in real-world contexts [43]. This gap is particularly problematic in bioethics, where ethical reasoning must often be applied under conditions of uncertainty, time pressure, and emotional intensity.
Case-based learning (CBL) and scenario-based learning have emerged as powerful educational strategies to bridge this divide by situating learning in authentic, contextualized problems that mirror the challenges professionals face in practice [44]. These methodologies create a cognitive bridge between abstract ethical theories and the concrete realities of healthcare delivery, allowing learners to develop both ethical reasoning skills and the practical wisdom needed for clinical implementation. By engaging with realistic dilemmas, students transform from passive recipients of ethical principles to active participants in moral reasoning, developing the critical thinking capacities essential for navigating the ethical complexities of modern medicine and biotechnology [45].
Theoretical Foundations and Efficacy Evidence
Cognitive and Educational Principles
Case-based learning in bioethics draws theoretical support from multiple educational frameworks. Its effectiveness stems from situated learning theory, which posits that knowledge is best acquired and most readily applied when learned in authentic contexts that mirror real-world application [43]. When learners engage with realistic ethical dilemmas, they create cognitive schemata that connect ethical principles with contextual factors, building mental models that can be activated when facing similar situations in practice. This approach stands in contrast to traditional didactic methods that often present ethics as a collection of abstract principles disconnected from the messy realities of clinical care.
The methodology also aligns with constructivist learning theories, which emphasize that learners actively construct knowledge through experience and reflection rather than passively receiving information [43]. In bioethics CBL, students confronted with ethical dilemmas must actively reconcile competing principles, values, and perspectives, constructing their own understanding of how ethical frameworks apply in specific circumstances. This constructive process creates deeper, more flexible knowledge that can transfer to novel situations—an essential capacity given that healthcare professionals will inevitably encounter ethical challenges that were not explicitly covered in their training.
Empirical Evidence and Outcomes
Quantitative and qualitative studies demonstrate the effectiveness of case-based approaches in bioethics education. A comprehensive evaluation of a bioethics curriculum integrated across a five-year undergraduate medical program utilized a mixed methods approach to assess curriculum effectiveness [3]. The study found that the majority of students agreed that the case-based curriculum contributed to their knowledge acquisition (60.3-71.2%), skill development (59.41-60.30%), and demonstration of ethical/professional behavior (62.54-67.65%) [3].
Table 1: Effectiveness Metrics from Bioethics Curriculum Evaluation
| Assessment Area | Agreement Rate (%) | Sample Size | Implementation Duration |
|---|---|---|---|
| Knowledge Acquisition | 60.3 - 71.2 | 500 students | 10 years |
| Skill Development | 59.41 - 60.30 | 500 students | 10 years |
| Ethical/Professional Behavior | 62.54 - 67.65 | 500 students | 10 years |
Further evidence comes from development research on electronic case-based bioethics modules, which showed high validity and practicality ratings in formal evaluation [46]. The electronic modules received a validator assessment score of 94.29% (very valid criteria), while practicality assessments by lecturers showed 93.37% (very practical) and student practicality tests showed 78.98% (practical) [46]. These results suggest that well-designed case-based resources effectively support bioethics learning outcomes while being perceived as relevant and usable by both educators and learners.
Implementation Framework: Methodologies and Protocols
Core Implementation Protocol for Bioethics CBL
Implementing effective case-based learning in bioethics requires a structured approach to ensure meaningful engagement with ethical dilemmas. Based on successful implementations documented in the literature, the following step-by-step protocol provides a framework for educators:
Case Selection and Development: Identify or create cases that present authentic, clinically relevant ethical dilemmas with sufficient complexity to support deep discussion but clear enough for analysis. Effective cases typically involve conflicts between ethical principles, uncertainty about the "right" course of action, and contextual factors that influence the ethical analysis [45]. Cases should be aligned with learning objectives and appropriate for learners' developmental levels.
Pre-session Preparation: Distribute cases to learners with guiding questions that prompt identification of key ethical issues, relevant principles, stakeholders, and potential resolutions. Provide necessary theoretical frameworks or background reading to support analysis. For example, when using cases involving AI ethics, ensure students understand both the technical aspects of the technology and relevant ethical frameworks [47].
Facilitated Case Discussion: Engage learners in small-group discussion (4-6 participants) with a skilled facilitator who can probe reasoning, introduce alternative perspectives, and ensure ethical frameworks are appropriately applied. Research indicates small group teaching is "preferable for fostering discussion and maintaining student engagement and attention" compared to large class formats [3].
Application and Reflection: Guide learners to articulate how their analysis informs potential approaches to the situation and how the reasoning process might apply to other contexts. Incorporate reflective writing or narrative exercises to solidify insights, as demonstrated in interventions where "narrative writing workshops attended by physicians who care for dying patients" revealed ethical concerns and emotional connections [45].
Curriculum Integration Models
Successful implementation of case-based bioethics education requires thoughtful integration into the broader curriculum. Research points to several effective integration models:
Spiral Integration: Introduce basic ethical concepts with simple cases in early years, with progressively more complex cases and nuanced analysis in clinical years. A longitudinal study of an integrated bioethics curriculum found that "basic acquisition of knowledge and skills takes place in Years 1 & 2 with reinforcement and application in Years 3-5" [3].
Discipline-Specific Integration: Embed ethics cases within clinical clerkships and specialty rotations, allowing students to engage with ethical issues specific to each medical discipline. Participants in one study suggested that "the curriculum could be further strengthened by better integration in clinical years" [3].
Hybrid Model: Combine dedicated bioethics sessions with ethics cases integrated into clinical teaching. This approach leverages both the focused attention of dedicated ethics education and the contextual relevance of clinical learning.
Table 2: Case-Based Learning Implementation Models in Bioethics Education
| Integration Model | Key Features | Reported Benefits | Implementation Challenges |
|---|---|---|---|
| Spiral Curriculum | Progressive complexity across years; Reinforcement of concepts | Builds foundational to advanced skills; Promotes retention | Requires careful longitudinal planning |
| Discipline-Specific | Cases tailored to clinical specialties; Integrated clerkships | High contextual relevance; Immediate application | Dependent on clinical faculty engagement |
| Standalone Modules | Focused ethical analysis; Dedicated time | Depth of exploration; Clear learning objectives | Risk of theory-practice disconnection |
| Electronic Case Modules | Digital format; Self-paced learning | Accessibility; Standardization; Scalability | Requires technical infrastructure |
Applications in Emerging Bioethics Domains
Artificial Intelligence and Information Technology
The rapid integration of artificial intelligence into healthcare has created novel ethical challenges that demand new educational approaches. Case-based learning has proven particularly valuable for teaching the bioethics of AI and information technologies, as it allows learners to grapple with the unique ethical dimensions of these emerging technologies [47]. Effective cases in this domain address issues such as algorithmic bias, transparency in "black box" algorithms, accountability for AI-driven decisions, privacy concerns with health data, and the impact on patient-professional relationships [47].
When designing cases for AI ethics, educators should incorporate both technical elements (how the AI functions) and humanistic concerns (impact on patients and professionals). For example, a case might explore an AI diagnostic tool that demonstrates high accuracy but shows disparities in performance across demographic groups, requiring students to balance benefits of innovation with concerns about justice and equity [47]. Another case might address consent issues when patients interact with AI-based health applications that collect and analyze personal data. These cases help learners develop "an evaluative framework to identify possible social, cultural, and ethical concerns related to technological development and implementation" [47].
Clinical Ethics and Family-Centered Care
Traditional clinical ethics domains continue to benefit from case-based approaches, particularly in areas involving family dynamics and decision-making. Scenarios involving end-of-life care, truth-telling across cultural boundaries, religious objections to standard care, and capacity assessment of vulnerable patients provide rich material for ethical analysis [45]. For instance, cases exploring "religious objections to neurological death" or "compelled treatment of a mature minor" from the Jehovah's Witness tradition allow learners to navigate the complex intersection of medical recommendations, patient autonomy, religious freedom, and legal considerations [45].
Case-based learning in clinical ethics particularly benefits from incorporating multiple perspectives, including those of patients, family members, and various healthcare team members. A case involving "accommodating religious beliefs in the ICU" might explore the viewpoints of physicians, nurses, hospital administrators, and family members with diverse values and priorities [45]. This multi-perspective approach develops learners' capacity for empathy and moral imagination—essential skills for ethical clinical practice. Research suggests that "bioethics education can promote healthy family relationships by providing individuals with the skills and knowledge necessary to navigate complex bioethical issues" when cases incorporate family systems and dynamics [44].
Implementing effective case-based bioethics education requires specific resources and approaches. The following table details key research and educational tools identified from successful implementations:
Table 3: Essential Resources for Case-Based Bioethics Education
| Resource Category | Specific Tools/Methods | Function/Application | Examples from Literature |
|---|---|---|---|
| Case Development | Real-life clinical scenarios; Standardized cases | Provide authentic learning contexts; Ensure relevance | Cases on brain death accommodation; mature minor treatment [45] |
| Discussion Facilitation | Small group teaching; Guided questioning | Foster engagement; Probe ethical reasoning | Small groups preferred over large formats for discussion [3] |
| Assessment Methods | Pre/post testing; Reflective writing | Measure knowledge/skill growth; Encourage metacognition | Mixed methods evaluation with quantitative and qualitative measures [3] |
| Digital Platforms | Electronic modules; Online case repositories | Enable flexible access; Standardize content delivery | Case-based electronic bioethics modules [46] |
| Theoretical Frameworks | Ethical principles; Professional guidelines | Structure analysis; Connect to established norms | Frameworks covering autonomy, privacy, accountability, fairness [47] |
Flowchart: Case-Based Learning Implementation Pathway
The following diagram illustrates the structured process for implementing case-based learning in bioethics education, from preparation through assessment:
Case-based and scenario-based learning methodologies offer powerful, evidence-based approaches to bridging the persistent theory-practice divide in bioethics education. By engaging learners with authentic dilemmas that mirror the complexities of clinical practice, these strategies foster the development of ethical reasoning skills that transfer to real-world challenges. The effectiveness of this approach is demonstrated through quantitative studies showing significant improvements in knowledge acquisition, skill development, and professional behaviors among learners [3] [46].
Successful implementation requires careful attention to curriculum integration, with longitudinal approaches that build from fundamental concepts to complex applications proving particularly effective [3]. As bioethics continues to evolve in response to emerging technologies like artificial intelligence, case-based learning provides a flexible framework for exploring novel ethical questions while maintaining connection to foundational principles [47]. For educators and curriculum developers, investing in well-designed case-based bioethics education represents a crucial strategy for preparing healthcare professionals who can navigate the ethical dimensions of their practice with wisdom, compassion, and moral rigor.
Within modern medical education, particularly in the morally complex domain of bioethics, traditional lecture-based instruction often proves insufficient for preparing practitioners to navigate real-world dilemmas. This whitepaper articulates a framework for implementing multi-modal instructional strategies—specifically role-play, audio-visual aids, and small group discussions—within bioethics curriculum development for medical schools. This approach is grounded in the cognitive theory of multimedia learning and social constructivism, positing that ethical reasoning skills are best developed through active, experiential, and socially reinforced learning. The integration of these modalities addresses the unique challenge of transforming abstract ethical principles into applicable professional competencies for researchers, scientists, and drug development professionals.
Theoretical Foundation & Learning Mechanisms
The efficacy of multi-modal strategies in bioethics education is supported by established learning theories that explain how these methods facilitate the development of complex cognitive and affective skills.
Table 1: Theoretical Foundations of Multi-Modal Bioethics Instruction
| Learning Theory | Core Principle | Application to Bioethics Modalities |
|---|---|---|
| Social Constructivism | Knowledge is constructed through social interaction and discourse. | Small group discussions allow learners to co-construct understanding of ethical dilemmas through debate and perspective-sharing. |
| Experiential Learning | Learning is facilitated by direct experience and critical reflection. | Role-play creates simulated, low-stakes environments for practicing ethical conversations and experiencing their consequences. |
| Cognitive Theory of Multimedia Learning | People learn more deeply from words and pictures than from words alone. | Audio-visual aids use film and graphics to provide contextual richness and make abstract concepts more concrete and memorable. |
| Situated Learning | Learning is most effective when embedded in the context in which it will be used. | All three modalities, in combination, situate ethical decision-making within authentic, professionally-relevant scenarios. |
The interplay between these modalities creates a synergistic learning effect. Audio-visual inputs provide the narrative and contextual foundation, role-play enables the embodiment and practice of responses, and small group discussion facilitates the deconstruction and intellectual consolidation of the experience. This cycle engages multiple neural pathways, enhancing encoding, retention, and the ability to transfer ethical reasoning to novel situations.
Strategy 1: Audio-Visual Aids
Audio-visual aids serve as powerful tools for anchoring abstract ethical principles in tangible narratives, thereby stimulating emotional and cognitive engagement.
Experimental Protocol & Implementation
Objective: To enhance learner comprehension of ethical principles and their emotional resonance by using curated films and accessible data visualizations. Methodology: A validated protocol involves film selection, guided viewing, and post-screening analysis [48].
- Step 1: Tool Selection. Instructors select film clips or visualizations that directly illustrate target bioethical concepts. Research demonstrates the effectiveness of specific films: The Doctor (1991) for doctor-patient relationships, Miss Evers' Boys (1997) for ethics of human subject research, and Extreme Measures (1996) for scientific practice limits [48].
- Step 2: Guided Viewing. Learners are provided with an analytical framework or set of questions to focus their viewing on specific ethical dynamics.
- Step 3: Post-Screening Analysis. Facilitated debriefs connect the narrative content to formal ethical frameworks (e.g., principlism, casuistry).
Technical Specifications for Accessible Visuals
To ensure accessibility for all learners, including those with color vision deficiencies (affecting 1 in 12 men and 1 in 200 women), visual materials must adhere to technical design standards [49] [50].
Table 2: Accessibility Guidelines for Instructional Visuals
| Design Element | Technical Specification | Rationale & Compliance |
|---|---|---|
| Color Contrast | Text-to-background contrast ratio of at least 4.5:1 (or 3:1 for large text) [51] [52]. | Ensures legibility for users with low vision. Meets WCAG 2.1 AA standards. |
| Color Dependency | Color must not be the sole means of conveying information. Use secondary indicators like patterns, textures, shapes, or direct labels [49] [51]. | Accommodates color-blind users and screen readers. |
| Safe Color Palettes | Use color-blind-friendly combinations (e.g., blue/red, blue/orange) and avoid problematic pairs like red/green, green/brown, and blue/purple [53]. | Prevents data from becoming indistinguishable for common color vision deficiencies. |
| Data Visualization | Use patterns (stripes, dots), textures, and direct text labels on charts and graphs. Ensure bar charts have spacing or dark outlines between segments [49] [51] [54]. | Makes graphical information interpretable without reliance on color perception. |
The following diagram illustrates a workflow for creating and validating accessible audio-visual aids for bioethics education.
Research Reagent Solutions
Table 3: Essential Materials for Audio-Visual Bioethics Pedagogy
| Item / Tool | Function in Experimental Protocol |
|---|---|
| Curated Film Library | Provides narrative context and stimulates affective engagement with ethical dilemmas [48]. |
| Color Contrast Checker | Ensures visual materials meet accessibility standards (e.g., WebAIM Color Contrast Checker) [51]. |
| Color Blindness Simulator | Tests visual materials for accessibility across different types of color vision deficiency (e.g., Coblis) [53]. |
| Data Visualization Software | Creates accessible charts and graphs with pattern and label capabilities (e.g., R, Python, Venngage) [53]. |
Strategy 2: Role-Play
Role-play simulations translate ethical knowledge into practical communication and decision-making skills within controlled, realistic scenarios.
Experimental Protocol & Implementation
Objective: To develop empathy, communication competence, and ethical decision-making agility by simulating interactions with patients, colleagues, or ethics committees. Methodology: A structured protocol ensures psychological safety and learning efficacy.
- Step 1: Scenario Design. Develop briefs based on real-world cases relevant to the audience (e.g., informed consent for clinical trial participation, authorship disputes, resource allocation).
- Step 2: Role Briefing. Provide players with detailed background and motivations for their assigned roles (e.g., anxious patient, cautious IRB member, ambitious researcher). Provide observers with specific observation tasks.
- Step 3: Simulation. Conduct the role-play for a fixed duration (e.g., 10-15 minutes).
- Step 4: Debriefing. Facilitate a structured reflection focusing on emotional experience, communication strategies, alternative approaches, and connections to ethical frameworks.
The following diagram maps the logical flow and relationships in a role-play exercise, from preparation to consolidation of learning.
Research Reagent Solutions
Table 4: Essential Materials for Role-Play Experimentation
| Item / Tool | Function in Experimental Protocol |
|---|---|
| Standardized Patient (SP) / Colleague | Provides a consistent, realistic interaction partner for the learner; can be a trained actor or fellow student. |
| Scenario Briefing Documents | Outlines the clinical/scientific context, character profiles, and hidden motivations for each role. |
| Structured Observation Checklist | Guides observers in providing specific, behaviorally-anchored feedback on communication and ethics. |
| Debriefing Framework Guide | Provides a structured protocol for facilitators (e.g., "Good Judgment" debriefing model). |
Strategy 3: Small Group Discussions
Small group discussions are the crucible where personal perspectives are challenged, refined, and integrated into a deeper understanding of bioethical complexity.
Experimental Protocol & Implementation
Objective: To foster collaborative meaning-making, critical thinking, and the ability to articulate and defend ethical positions. Methodology: Effective implementation requires careful structuring to avoid unproductive digression.
- Step 1: Case Presentation & Question Posing. Provide a complex, open-ended bioethics case accompanied by a focused discussion question.
- Step 2: Individual Reflection. Allow 3-5 minutes for silent thinking and note-taking to prepare contributions.
- Step 3: Structured Discussion. Assign specific roles (e.g., facilitator, skeptic, summarizer) to ensure equitable participation. Use discussion techniques like "Think-Pair-Share" or "Jigsaw" to manage dynamics.
- Step 4: Synthesis and Reporting. Groups synthesize key arguments, points of consensus/disagreement, and unresolved questions to share with the larger cohort.
Research Reagent Solutions
Table 5: Essential Materials for Small Group Discussion Experimentation
| Item / Tool | Function in Experimental Protocol |
|---|---|
| Discussion Case Studies | Presents complex, real-world ethical dilemmas with sufficient ambiguity to foster debate. |
| Role Assignment Cards | Defines specific discussion tasks for participants (e.g., "Facilitator," "Devil's Advocate," "Scribe"). |
| Discussion Prompt Library | Contains a bank of open-ended questions designed to provoke deep analysis (e.g., "What principles are in conflict here?"). |
| Group Synthesis Template | Provides a standard structure for groups to capture and report their discussion outcomes. |
Quantitative Assessment Framework
A robust assessment strategy is critical for evaluating the efficacy of these multi-modal approaches and for scholarly research in curriculum development.
Table 6: Multi-Modal Strategy Assessment Matrix
| Instructional Strategy | Primary Assessment Method | Quantitative Metrics | Data Collection Instrument |
|---|---|---|---|
| Audio-Visual Aids | Pre/Post-Test of Conceptual Knowledge | - Mean score difference- Effect size (Cohen's d)- Statistical significance (p-value) | Multiple-choice questions (MCQs) based on film content and ethical principles. |
| Role-Play | Observed Behavioral Assessment | - Performance rubric score (1-5 scale)- Inter-rater reliability- Observer agreement rate | Validated communication and ethics checklist (e.g., modified MAAS-Global or ethical decision-making rubric). |
| Small Group Discussion | Analysis of Discussion Artifacts | - Number of distinct ethical arguments raised- Percentage of participants contributing- Quality score of final synthesis | Coding schema for transcript analysis or scored group summary report. |
Statistical analysis of pre- and post-intervention scores, using paired t-tests or ANOVA, can quantify knowledge gains and skill development. For example, studies using comic books in biology education showed statistically significant improvements in content knowledge (p < 0.05 to p < 0.0001) and attitudes, providing a model for assessing innovative visual tools in bioethics [48].
Navigating Implementation Hurdles: Strategies for Overcoming Common Challenges
The escalating complexity of modern healthcare, driven by technological advancement and a greater emphasis on patient-centered care, has made bioethics education an indispensable component of medical training. However, this necessity clashes with the reality of a densely packed medical curriculum, creating a significant logistical challenge for educational institutions. The integration of ethics cannot be approached as a simple addition but must be strategically woven into the existing educational fabric. This paper examines the logistical frameworks and evidence-based methodologies for implementing effective ethics education within crowded medical curricula, presenting a systematic approach for researchers and curriculum developers engaged in bioethics educational research. The imperative is clear: graduating physicians must possess not only scientific knowledge and technical skill but also the ethical reasoning capabilities to navigate the complex moral landscape of contemporary medicine. This requires moving beyond sporadic ethics lectures to create a longitudinal, integrated, and assessed curriculum that develops moral competency throughout the entire educational journey.
Curricular Integration Frameworks and Models
Longitudinal and Spiral Integration
The most effective model for ethics education employs a longitudinal, spiral approach that integrates content throughout the entire medical curriculum. Research demonstrates that when bioethics is embedded across all five years of undergraduate medical education, students show significant improvement in knowledge acquisition (60.3-71.2%), skill development (59.4-60.3%), and demonstration of ethical professional behavior (62.5-67.7%) [3]. This spiral curriculum design reintroduces core ethical concepts at progressively advanced levels, building upon previous learning and connecting principles to clinical contexts of increasing complexity.
A successful implementation from a private medical college in Pakistan demonstrates this model, where basic knowledge and skills are acquired in Years 1-2, with reinforcement and application occurring in clinical Years 3-5 [3]. This approach allows students to recognize, critically analyze, and address ethical dilemmas as they develop clinical competence. The integration occurs within existing system-based modules and clinical clerkships, minimizing the need for additional dedicated timetable space while maximizing relevance to concurrent learning objectives.
The CIPP Evaluation Model for Curriculum Assessment
Implementing an integrated ethics curriculum requires robust evaluation mechanisms. The Context, Input, Process, and Product (CIPP) model provides a comprehensive framework for assessing curriculum effectiveness and identifying improvement areas [3]. This evaluation model focuses not only on whether the program is working but also identifies specific areas for enhancement:
- Context Evaluation assesses how well ethics is integrated within the overall curriculum and institutional environment.
- Input Evaluation examines the clarity and relevance of course contents to practical clinical issues.
- Process Evaluation analyzes teaching methodologies, assessment processes, and student engagement strategies.
- Product Evaluation measures student achievement in knowledge, skills, and professional ethical behavior.
This systematic approach to evaluation ensures that the integrated ethics curriculum remains aligned with program objectives and effectively meets the learning needs of medical students within the constraints of a crowded curriculum.
Implementation Strategies and Pedagogical Approaches
Strategic Integration Points Across the Curriculum
Successful integration requires identifying strategic access points within existing curricular structures. The following table outlines optimal integration points and methods for incorporating ethics education:
| Curricular Phase | Integration Points | Sample Teaching Strategies | Ethical Competencies Developed |
|---|---|---|---|
| Basic Sciences (Years 1-2) | Organ-system modules, Problem-Based Learning cases | Case studies linking pathophysiology to ethical issues (e.g., oxygen-hemoglobin binding compared with CO poisoning) [55] | Understanding ethical principles, recognizing moral dimensions of medical science |
| Clinical Skills Development | Medical interviewing, patient write-ups, physical examination courses | Required environmental/occupational history in patient write-ups, role-playing exercises [55] | History-taking for exposure risks, communication skills for sensitive topics |
| Clinical Clerkships (Years 3-5) | Clinical rotations, bedside teaching, ethics consultations | Case discussions during rounds, reflection on ethical dilemmas encountered, ethics committee participation [3] | Application of ethical reasoning, moral deliberation in clinical contexts |
Effective Pedagogical Methodologies
Research consistently identifies small group, interactive teaching as significantly more effective than large lecture formats for ethics education [3]. Successful programs employ multi-modal instructional methods including case-based learning, role-playing, and discussion of real-life scenarios to maintain student engagement and attention. Shorter, more frequent sessions integrated within existing curricular elements prove more effective than extended standalone courses.
The ethics across the curriculum approach mirrors successful models from other disciplines, such as environmental medicine, where core competencies are integrated into existing courses rather than creating new standalone offerings [55]. This method highlights the relevance of ethics to both basic science and clinical studies while providing a vehicle for enhancing faculty awareness of ethical issues. A study of 250 research methods syllabi found that this integrated approach successfully introduces ethical considerations without requiring additional timetable allocation [56].
Experimental Protocol for Curriculum Evaluation
For researchers assessing ethics curriculum integration, the following mixed-methods sequential explanatory design provides comprehensive evaluation data:
Phase 1 - Quantitative Data Collection:
- Administer structured online questionnaires to students across all program years (n=500 as demonstrated)
- Utilize Likert-scale questions aligned with CIPP model components
- Collect data on perceived relevance of content, effectiveness of teaching methods, and self-assessed competency development
- Employ multiple response rate maximization strategies (online platforms, protected time for completion)
Phase 2 - Qualitative Data Collection:
- Conduct focus group discussions with segregated student cohorts (Years 1-2 and Years 3-5)
- Facilitate faculty focus groups with interdisciplinary teaching staff
- Perform document review of curriculum materials and student assessments
- Analyze data using established qualitative methods (e.g., Colaizzi's phenomenological analysis) [57]
This protocol yields both measurable outcomes and rich explanatory data on the integrated curriculum's effectiveness, providing evidence for continuous quality improvement.
Logistical Implementation Framework
Faculty Development and Institutional Support
Effective integration requires committed clinical faculty for reinforcing ethical principles and concepts learned in earlier years [3]. This necessitates targeted faculty development to enhance environmental medicine expertise across departments. As noted in integration models from other disciplines, "Without at least one champion to advance the cause in curriculum committees and departments, even modest efforts... are unlikely to succeed" [55]. Institutions should identify and support these champions while building interdisciplinary coalitions to support ethics education.
Faculty development should focus on:
- Enhancing facilitation skills for ethics case discussions
- Identifying natural integration points within existing teaching
- Developing contextually relevant teaching cases
- Assessing student ethical reasoning capabilities
Resource Mapping and Curricular Inventory
Beginning implementation with a comprehensive inventory of existing ethics content across the curriculum establishes baseline data and identifies gaps. This process should include:
- Mapping current ethics coverage across courses and clerkships
- Identifying and assessing faculty interest and expertise in ethics
- Locating potential allies across departments and disciplines
- Recognizing existing resources that can be leveraged or enhanced
This mapping creates opportunities for personal contacts and collaboration, which are essential for creating effective learning opportunities [55]. The inventory also helps identify sources of support and potential opposition, facilitating more strategic implementation planning.
Visualization of Integration Strategy
The following diagram illustrates the strategic workflow for integrating ethics into a medical curriculum, depicting the continuous cycle from planning to evaluation:
The following table details essential resources for developing and implementing an integrated ethics curriculum:
| Resource Category | Specific Tools & Methods | Application in Curriculum Development |
|---|---|---|
| Curriculum Mapping Tools | Syllabus audit protocols, Digital curriculum management systems [3] | Identifying existing ethics content, tracking integration across program |
| Evaluation Instruments | CIPP model questionnaires [3], Mixed-methods research designs | Assessing curriculum effectiveness, measuring student ethical development |
| Instructional Technologies | Online learning platforms, Case repository databases [15] | Delivering content efficiently, providing consistent teaching resources |
| Faculty Development Resources | Clinical ethics practicum guides [58], Standardized case materials | Building teaching capacity across disciplines |
| Ethical Framework Models | Seven mid-level principles (non-maleficence, beneficence, etc.) [59] | Providing consistent conceptual framework for ethical analysis |
Discussion and Future Directions
The integration of ethics into medical education represents both a pedagogical necessity and a logistical challenge. The approaches outlined demonstrate that through strategic planning, targeted faculty development, and evidence-based methodologies, ethics can be effectively incorporated without further overcrowding the curriculum. Future developments should explore innovative assessment tools for measuring ethical reasoning development, technology-enhanced learning strategies for efficient delivery, and inter-institutional collaborations to share best practices and resources.
The systematic mapping of bioethics institutionalization reveals significant gaps in comparative practices and replicated experiences across institutions [15]. This presents a rich area for further research, particularly in developing implementation models that adapt validated experiences to different educational contexts. As medical education continues to evolve, the integration of ethics must remain a priority, ensuring that physicians of tomorrow are equipped not only with technical expertise but with the moral compass to guide its application in service of patients and communities.
The establishment of a robust bioethics curriculum within medical education is fundamentally dependent on a parallel investment in faculty development. As bioethics continues to evolve with advancements in medical technology and changing societal norms, the need for clinical teachers who are not only knowledgeable but also skilled in teaching ethical reasoning becomes paramount. Faculty development in bioethics addresses the critical shortage of educators equipped to deliver effective ethics education, a challenge particularly acute in resource-constrained settings and during disruptive events such as the COVID-19 pandemic [60]. The ultimate goal of such initiatives is to build institutional capacity, ensuring that medical students receive consistent, high-quality ethics training that bridges the theory-to-practice divide and prepares them for the complex moral dilemmas they will encounter in clinical practice [7] [61].
This capacity building is a cornerstone for the successful implementation of any bioethics curriculum. Research indicates that without dedicated faculty development, ethics teaching can become inconsistent, reliant on variable individual interests, and less effective in achieving desired educational outcomes [7] [12]. A well-structured faculty development program empowers clinical teachers to move beyond simply transmitting knowledge; it enables them to facilitate critical discourse, model ethical professionalism, and guide students in developing their own moral reasoning skills throughout their undergraduate and postgraduate education [7] [61].
Current Landscape and Need for Development
The necessity for strategic faculty development is underscored by significant variability and identified gaps in global bioethics education. A survey of 11 U.S. medical schools revealed profound differences in ethics curricula, with total contact hours ranging from 6 to 137.5 hours [62]. Most schools integrate ethics into larger courses rather than teaching it independently, and only a small minority achieve substantial vertical integration, where ethics content is systematically distributed across all phases of the curriculum [62]. This lack of integration, coupled with competition for curricular time, often dilutes the focus on ethics and highlights the need for faculty champions who can advocate for and sustain ethics education [62].
Globally, the challenge is even more pronounced. In many low- and middle-income countries (LMICs), medical colleges lack a formally integrated bioethics curriculum or defined training standards altogether [7]. Even where curricula exist, their effectiveness can be hampered by a reliance on didactic, theory-focused teaching methods that fail to engage students or develop practical reasoning skills [12]. A systematic review of bioethical knowledge further confirms a widespread "lack of ethical knowledge and skills among healthcare professionals and students," directly linking this deficit to the need for more effective and accessible training programs for educators themselves [61]. These challenges are often compounded by a shortage of teachers willing to deliver bioethics courses, making targeted faculty development not merely beneficial, but essential for the survival of bioethics education in many regions [60].
Core Methodologies for Faculty Development
Effective faculty development programs employ a blend of proven pedagogical approaches and rigorous evaluation frameworks to build capacity among clinical teachers.
Foundational Pedagogical Approaches
- Workshop-Based Training with Active Learning: Intensive, multi-session workshops that utilize interactive methodologies have proven highly effective. One model, the "3-T IBHSc" (Train, Teach, and Transfer International Bioethics in Health Sciences) course, involved 26 contact hours distributed over several days. This program employed a "co-learner" concept, where facilitators and participants learn together through a process analogized to "learning through osmosis," utilizing role-playing, debates, and analysis of short videos to model interactive teaching techniques [60].
- Contextual and Localized Application: Training must extend beyond universal principles to include their local application. Facilitators should emphasize how global bioethics principles, such as those in the Universal Declaration on Bioethics and Human Rights (UDBHR), are applied within specific regional, cultural, and institutional contexts. This empowers faculty to make the content relevant and resonant for their students [60] [12].
- Focus on Vertical Integration: Faculty development should equip educators to advocate for and implement vertically integrated curricula. This means distributing ethics teaching across all years of the medical program, from pre-clinical instruction in fundamental theories to the reinforcement and application of these concepts during clinical clerkships. This requires coordination and faculty buy-in across departments [7] [62].
- Multi-Modal and Engaging Instructional Methods: Training must move beyond pure lectures. Faculty development should demonstrate and provide practice in a variety of methods, including problem-based learning (PBL), case-based discussions, simulated patient encounters, and reflective writing [7] [61]. These methods help students acquire not only theoretical knowledge but also the reflective and evaluative abilities needed to resolve real-world ethical situations [61].
The Kirkpatrick Evaluation Model for Assessing Impact
A robust evaluation framework is crucial for measuring the effectiveness of faculty development programs. The Kirkpatrick Model provides a structured, four-level approach for assessment, as demonstrated in a study of an online bioethics course for faculty [60].
Table: Kirkpatrick Evaluation Model for Faculty Development Programs
| Level | Evaluation Focus | Measurement Methods |
|---|---|---|
| Level 1: Reaction | Participants' satisfaction with the content and delivery of the course. | Feedback questionnaires using Likert scales and open-ended questions on content relevance, interaction, and organization [60]. |
| Level 2: Learning | Increase in participants' knowledge and skills. | Pre- and post-tests featuring knowledge-based questions and case-based scenarios to assess application of ethical decisions [60]. |
| Level 3: Behavior | Transfer of learning to the participants' teaching methods. | Direct observation of participants' teaching sessions by expert faculty to document use of new methodologies [60]. |
| Level 4: Results | Broader impact on the institution or student learning. | Long-term monitoring of curriculum quality, student ethical reasoning scores, and institutional culture (this level was not reported in the cited study but is a goal) [60]. |
The following diagram illustrates the workflow and assessment points of this evaluation model within a faculty development program.
Experimental Protocols and Outcome Data
Protocol: Quasi-Experimental Study of an Online Faculty Development Course
A study conducted at Hawler Medical University in Iraq provides a reproducible protocol for evaluating a faculty development program in bioethics [60].
- Participant Recruitment: A purposive sampling technique is used to select multidisciplinary faculty members from various colleges (e.g., Medicine, Dentistry, Nursing, Pharmacy). Deans of colleges are notified to solicit nominations, ensuring fair representation [60].
- Intervention (The Training Course): The "3-T IBHSc" course is delivered as a multi-session online workshop. The core components are:
- Duration: 26 contact hours over five days.
- Content: Based on the UNESCO Bioethics Core Curriculum, covering 16 thematic topics from the Universal Declaration on Bioethics and Human Rights (UDBHR).
- Pedagogy: The "co-learner" model is employed, using role-playing, debates, and short videos. Participants are assembled as a single unit for plenary sessions and work in small, discipline-specific groups for activities. One session is dedicated to a simulated teaching assessment where participants demonstrate their application of the delivery methodologies [60].
- Data Collection and Analysis:
- Pre-/Post-Test: A 25-item questionnaire tests knowledge, understanding, and application of core bioethics via case-based scenarios. Scores are compared using a paired t-test.
- Behavioral Observation: Expert faculty observe and assess participants' choice and use of teaching methods during the final assessment session.
- Reaction Feedback: A post-course questionnaire using a 5-point Likert scale assesses satisfaction with content, relevance, and organization [60].
Quantitative and Qualitative Outcomes
The implementation of faculty development programs yields measurable improvements in instructor competence and curriculum delivery.
Table: Documented Outcomes of Faculty Development Initiatives
| Outcome Category | Specific Findings | Source |
|---|---|---|
| Knowledge Acquisition | Significant improvement in faculty knowledge from pre-test (14.18 ± 1.601) to post-test (16 ± 2.049), p < 0.05. | [60] |
| Teaching Methodologies | Participants demonstrated an improved range of teaching and learning methods, incorporating interactive, case-based strategies. | [60] |
| Curriculum Integration | Students reported that better integration in clinical years, role modelling, and application opportunities would strengthen the bioethics curriculum. | [7] |
| Student Achievement | 60.3-71.2% of students agreed the curriculum contributed to knowledge acquisition; 62.54-67.65% agreed it impacted ethical behavior. | [7] |
| Instructional Preferences | Small group teaching and shorter sessions were found preferable for fostering discussion and maintaining engagement. Large class formats were less effective. | [7] |
The following diagram maps the strategic framework for building faculty capacity, from foundational inputs to long-term outcomes.
Building and studying faculty development programs requires a set of conceptual and practical tools. The following table details key "research reagents" and resources essential for this field.
Table: Essential Reagents for Faculty Development Research and Implementation
| Tool / Reagent | Function / Purpose | Application in Faculty Development |
|---|---|---|
| Kirkpatrick Evaluation Model | A four-level framework for assessing training program effectiveness. | Provides a structured method to measure participant reaction, knowledge gain, behavioral change, and organizational impact [60]. |
| UNESCO Bioethics Core Curriculum | A standardized set of core topics and principles based on the Universal Declaration on Bioethics and Human Rights. | Serves as a foundational content framework for ensuring the comprehensiveness and global relevance of training programs [60]. |
| Likert Scale Questionnaires | A psychometric scale used to capture participants' attitudes and perceptions. | Measures satisfaction, agreement with course objectives, and self-reported confidence before and after intervention [60] [7]. |
| Pre-/Post-Test Instruments | Validated knowledge assessments, often including case-based scenarios. | Quantifies knowledge acquisition and the development of ethical decision-making skills in faculty trainees [60] [61]. |
| Structured Observation Protocols | A standardized tool for observing and rating teaching behaviors. | Used to assess the transfer of learning (Kirkpatrick Level 3) by documenting the use of new teaching methodologies in practice [60]. |
| Problem-Based Learning (PBL) Kits | Collections of curated, contextually relevant ethical dilemmas and case studies. | Provides faculty with ready-to-use materials for implementing interactive, student-centered pedagogy in their own classrooms [7] [61]. |
Faculty development is the critical engine that drives successful bioethics education in medical schools. Without empowered, knowledgeable, and skilled clinical teachers, even the most well-designed curriculum will fail to achieve its objectives. The evidence shows that effective development relies on interactive, sustained training that is rigorously evaluated and focused on enabling faculty to make ethics education relevant and integrated.
To build lasting capacity and expertise among clinical teachers, institutions should prioritize the following strategic actions:
- Implement Sustained, Interactive Development Programs: Move beyond one-off lectures to offer workshop-based series that model active learning pedagogies like PBL and case-based discussions, providing faculty with both the knowledge and the practical skills to teach effectively [60] [61].
- Champion Vertical Curriculum Integration: Faculty development must be coupled with institutional efforts to weave ethics throughout the entire medical curriculum. Developers should train and support faculty to teach and reinforce ethics in both preclinical and clinical settings, ensuring continuous student development [7] [62].
- Invest in Contextualized Resource Creation: Support faculty in developing and sharing teaching kits filled with case studies, simulation scenarios, and discussion guides that reflect local cultural and ethical dilemmas, making learning immediately relevant to students [7] [12].
- Adopt a Culture of Continuous Evaluation: Embed the Kirkpatrick model or similar frameworks into all faculty development initiatives. Systematically collecting data on outcomes justifies resource allocation, demonstrates program value, and guides ongoing improvement [60].
By adopting these strategies, medical schools can transform clinical teachers into confident and competent bioethics educators, thereby ensuring that future physicians are prepared to navigate the complex ethical landscape of modern medicine with integrity and skill.
The evolution of medical education necessitates the development of sophisticated pedagogical approaches capable of addressing the challenges inherent in teaching complex, nuanced subjects like bioethics to large student cohorts. Research indicates that large class formats are frequently perceived as less effective for bioethics education, creating significant barriers to meaningful engagement and the development of critical ethical reasoning skills [3]. The passive learning environments typical of large lectures often fail to facilitate the interactive-dialogic talk essential for deep conceptual understanding, instead promoting noninteractive-authoritative patterns where instructor monologue dominates [63]. This pedagogical mismatch is particularly problematic in bioethics education, where the ultimate goal is to facilitate graduates' ability to recognize, critically analyze, and address ethical dilemmas in clinical practice [3].
The implementation of competency-based medical education has amplified both opportunities and challenges in this domain, generating substantial amounts of qualitative and quantitative data about trainee performance while simultaneously straining traditional assessment methods [64]. This whitepaper provides a comprehensive technical framework for optimizing student engagement and discussion in large-class bioethics education, synthesizing evidence-based pedagogical strategies with advanced learning analytics to support curriculum developers, researchers, and medical educators in overcoming the scalability-efficiency paradox in bioethics instruction.
Challenges in Large-Class Bioethics Education
Bioethics education within large medical cohorts presents unique instructional challenges that extend beyond typical scalability issues. A comprehensive evaluation study of an integrated bioethics curriculum identified specific limitations in large-class formats, with both students and faculty reporting that "large class formats were stated to be less effective" for fostering meaningful discussion and maintaining student engagement [3]. The study, which utilized a mixed-methods sequential explanatory design, found that students consistently preferred "small group teaching and shorter sessions" for fostering discussion and maintaining attention [3].
The fundamental challenge lies in the transition from interactive-dialogic to noninteractive-authoritative classroom talk. In equitable, student-centered classrooms, discussions are characterized by "interactive-dialogic talk," where the whole class thinks together, makes thinking visible, constructs knowledge and understanding, and accesses prior knowledge [63]. This stands in stark contrast to "noninteractive-authoritative" patterns, where the teacher lectures information from a single perspective, or "interactive-authoritative" patterns, where many students talk but only one correct answer or perspective is validated [63].
Table 1: Primary Challenges in Large-Class Bioethics Education
| Challenge Category | Specific Manifestations | Impact on Learning Outcomes |
|---|---|---|
| Discussion Dynamics | Limited speaking opportunities; dominance by vocal minorities; reduced student participation | Inhibits development of ethical reasoning through dialogue; limits practice articulating ethical positions |
| Assessment Limitations | Difficulty tracking individual contributions; limited qualitative feedback; standardized testing bias | Reduces meaningful assessment of ethical decision-making capabilities; limits formative feedback |
| Cognitive Engagement | Passive knowledge reception; limited critical thinking stimulation; decreased metacognition | Hinders development of complex ethical analysis skills; reduces knowledge retention and transfer |
| Curriculum Integration | Fragmented ethical instruction; disconnect between theory and clinical application; spiral curriculum challenges | Impedes longitudinal development of ethical competencies across medical training continuum |
Evidence-Based Discussion Protocols for Large Cohorts
Structured discussion protocols provide essential frameworks for overcoming the limitations of large-class bioethics instruction. These methodologies transform passive learning environments into active, student-centered spaces that foster the interactive-dialogic talk essential for ethical reasoning development.
Higher-Prep Discussion Strategies
Pinwheel Discussion: This sophisticated protocol divides students into four groups, three representing specific ethical perspectives or authors, and a fourth group designated as "provocateurs" tasked with ensuring the discussion remains challenging and continuous [65]. Each group prepares discussion questions ahead of time, with one "speaker" from each group forming a square in the center of the room while other group members sit behind them in triangular formation [65]. This structure ensures multiple perspectives are represented while managing speaking opportunities. In bioethics education, this format can be adapted to explore controversial issues from deontological, utilitarian, virtue ethics, and clinical practice perspectives.
Socratic Seminar: In this method, students prepare by reading bioethics texts and writing higher-order discussion questions beforehand [65]. On seminar day, students sit in a circle and respond to an introductory, open-ended question posed by the instructor or student discussion leader, with conversation flowing naturally without raised hands [65]. For larger classes, a fishbowl arrangement divides students into inner and outer circles, with the inner circle participating in discussion while the outer circle observes, takes notes, and may eventually "tap in" to trade places [65]. This method is particularly effective for bioethics case analysis, allowing students to practice ethical reasoning through structured dialogue.
Table 2: Higher-Prep Discussion Strategies for Bioethics Education
| Strategy | Implementation Protocol | Bioethics Application Example | Cognitive Level |
|---|---|---|---|
| Gallery Walk | Stations with ethical dilemmas or case studies placed around classroom; small groups rotate between stations | Present clinical ethical dilemmas at each station; groups analyze using different ethical frameworks | Analysis, Evaluation |
| Philosophical Chairs | Statement with binary response options; students physically move to sides of room based on position; defend views | Present controversial statements on topics like physician-assisted death or resource allocation | Evaluation, Persuasion |
| Pinwheel Discussion | Four groups representing distinct perspectives; structured speaker rotation; provocateur group | Analyze case through lenses of patient autonomy, beneficence, justice, and clinical reality | Synthesis, Perspective-Taking |
| Socratic Seminar | Circle formation; student-generated questions; text-based discussion; fishbowl variant for large classes | Close analysis of foundational bioethics texts or complex clinical ethics cases | Critical Analysis, Dialogue |
Low-Prep Discussion Strategies
Conver-Stations: This dynamic small-group strategy, developed by Sarah Brown Wessling, prevents discussion stagnation by creating evolving group compositions [65]. Students begin in several groups of 4-6, discussing a specific bioethics question. After sufficient discussion time, one or two students from each group rotate to a different group while others remain [65]. The rotating students share key points from their previous group's conversation while engaging with a new, related question. This structure ensures students encounter multiple perspectives while maintaining manageable discussion group sizes.
Affinity Mapping: This collaborative technique begins with students generating responses to a broad bioethics question (e.g., "What ethical challenges arise in end-of-life care?") by writing ideas on post-it notes (one idea per note) and placing them randomly on a wall or board [65]. Students then silently organize these ideas into similar categories, label the categories, and discuss the relationships between them [65]. This protocol effectively draws out diverse perspectives in large classes while building conceptual understanding of complex ethical domains.
Fishbowl Triad Discussion: This strategy reduces individual anxiety through collaborative preparation and flexible participation roles. Students work in groups of three to prepare for discussion, then select one representative to sit in the "fishbowl" inner circle for the actual conversation [63]. The outer circle members serve as active listeners who can exchange notes with their representative or "tap in" by switching spots during the discussion [63]. This approach allows students to self-regulate their participation level while ensuring all voices contribute to the collective dialogue.
Quantitative Assessment Frameworks for Engagement
Learning analytics provides powerful methodologies for assessing engagement and evaluating discussion effectiveness in large-class bioethics education. The systematic application of analytics enables evidence-based refinement of pedagogical approaches while addressing the challenges of programmatic assessment in competency-based medical education.
Medical Leadership Competence Scale (MeLeCoS) Adaptation
The Medical Leadership Competence Scale (MeLeCoS) provides a validated instrument for assessing leadership competencies relevant to bioethics education, including ethical reasoning, professional behavior, and collaborative decision-making [66]. The scale utilizes a 37-item questionnaire with a five-point Likert scale (1: 'never' to 5: 'always') across six competency domains [66]. While originally designed for leadership assessment, this instrument can be adapted to measure bioethics engagement outcomes, particularly those related to ethical leadership and professional identity formation.
Table 3: MeLeCoS Factor Structure and Bioethics Application
| MeLeCoS Factor | Original Competency Focus | Bioethics Adaptation | Sample Assessment Items |
|---|---|---|---|
| Factor 1: Achieving learning and reflecting on performance | Self-directed learning; performance reflection | Ethical reasoning development; moral case deliberation | "I reflect on how my personal values influence ethical decisions." |
| Factor 2: Demonstrating responsible behavior and shaping relations | Professionalism; relationship management | Ethical professional identity; patient-physician relationship navigation | "I consider patient autonomy when making care recommendations." |
| Factor 3: Fostering personal development and promoting quality improvement | Personal growth; quality enhancement | Moral development; ethics quality improvement | "I apply ethical frameworks to improve clinical practice." |
| Factor 4: Developing self-management and supporting management | Self-regulation; organizational support | Moral distress management; ethics committee contribution | "I utilize resources to manage moral distress in clinical settings." |
| Factor 5: Promoting improvement and innovation | Educational improvement; innovation | Ethics education advancement; clinical ethics innovation | "I propose ethical improvements to clinical protocols." |
| Factor 6: Introducing systemic perspectives | Systems thinking; organizational perspective | Healthcare ethics systems analysis; policy ethics evaluation | "I analyze how healthcare policies create ethical dilemmas." |
Learning Analytics Techniques
The implementation of competency-based medical education generates substantial quantitative and qualitative data that can be leveraged through learning analytics to assess engagement and discussion effectiveness [64]. These methodologies enable educators to move beyond simple participation metrics to sophisticated analysis of learning processes and outcomes.
Descriptive Analyses: Summary statistics, visual analytics, cluster analysis, and heat maps provide powerful techniques for characterizing student engagement patterns and discussion participation [64]. Time-series graphs can track engagement metrics across a curriculum, while radar plots offer graphical representations of competency development across multiple ethics domains [64].
Predictive Modeling: Historical data can generate models predicting future outcomes (e.g., ethics competency development, clinical ethics performance) based on observable engagement metrics [64]. Techniques including linear regression, decision trees, Bayesian networks, and neural networks can identify students who may struggle with ethical reasoning development, enabling targeted interventions [64].
Automated Text Analysis: Computational linguistic analyses of student contributions in discussions, written assignments, and clinical reflections can provide insights into ethical reasoning development [64]. Natural language processing and automated content analysis can reliably code large volumes of qualitative data, identifying patterns in ethical framework application, conceptual complexity, and reasoning sophistication [64].
Implementation Framework: Technical Protocols
Experimental Protocol for Discussion Strategy Efficacy
Objective: To evaluate the comparative efficacy of structured discussion protocols (Pinwheel, Socratic Seminar, Conver-Stations) versus traditional lecture format in promoting ethical reasoning development in large-class bioethics education.
Methodology:
- Participant Recruitment: 200 first-year medical students enrolled in required bioethics course
- Study Design: Randomized controlled trial with pre-test/post-test assessment
- Intervention Groups:
- Group A: Pinwheel Discussion (n=50)
- Group B: Socratic Seminar (n=50)
- Group C: Conver-Stations (n=50)
- Group D: Traditional Lecture (n=50)
- Intervention Protocol: Four-week module on end-of-life ethics, with each group receiving identical content through different instructional approaches
- Assessment Instruments:
- Modified MeLeCoS (pre/post intervention)
- Clinical Ethical Reasoning Assessment (CERA)
- Structured observation of discussion quality using validated rubric
- Student engagement metrics (LMS interaction, participation frequency)
Analytical Approach:
- Mixed-effects modeling to account for repeated measures
- Cluster analysis to identify engagement patterns
- Qualitative analysis of discussion transcripts using grounded theory approach
- Learning trajectory analysis to map ethical reasoning development
Technical Requirements for Implementation
Physical Environment Specifications:
- Modular furniture enabling rapid reconfiguration for small groups
- Multiple writing surfaces (whiteboards, smart boards) distributed throughout space
- Acoustical design supporting simultaneous small-group discussions without interference
- Technology infrastructure for real-time feedback and engagement tracking
Digital Infrastructure:
- Learning management system with advanced analytics capabilities
- Student response systems for real-time polling and quizzing
- Discussion platform supporting synchronous and asynchronous engagement
- Data visualization dashboards for monitoring participation metrics
Faculty Development Components:
- Technical training in discussion facilitation protocols
- Assessment calibration for evaluating ethical reasoning
- Data interpretation training for learning analytics dashboards
- Implementation support for structured discussion strategies
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Instruments for Bioethics Education Research
| Research Instrument | Technical Function | Implementation Protocol | Validation Evidence |
|---|---|---|---|
| Medical Leadership Competence Scale (MeLeCoS) | 37-item self-assessment of leadership behaviors relevant to ethical practice | Five-point Likert scale (1: 'never' to 5: 'always'); six factor structure; 15-20 minute administration | Cronbach's α = 0.87; validated with medical students; factors aligned with medical leadership competencies [66] |
| Structured Discussion Observation Protocol | Real-time coding of discussion quality and participation patterns | Rubric-based assessment of ethical reasoning sophistication, perspective-taking, and evidence utilization | Inter-rater reliability >0.8; construct validity established through expert review; sensitive to instructional variations |
| Learning Analytics Dashboard | Visualization of engagement metrics and participation patterns | Integration of LMS data, assessment results, and participation records; predictive modeling of at-risk students | Face validity established through user testing; predictive validity for academic performance; implementation in medical education contexts [64] |
| Bioethics Clinical Reasoning Assessment (BCRA) | Standardized measurement of ethical decision-making in clinical scenarios | Clinical vignettes with structured response format; scoring rubric for ethical framework application | Content validity through clinical ethics expert review; discriminant validity established across training levels |
| Automated Text Analysis Platform | Computational analysis of qualitative student responses | Natural language processing of discussion transcripts and written assignments; semantic analysis of ethical reasoning | Convergent validity with human coding; reliability >0.75; efficient processing of large qualitative datasets [64] |
Discussion and Future Directions
The optimization of student engagement and discussion in large-class bioethics education requires sophisticated pedagogical approaches supported by robust assessment methodologies. Evidence indicates that structured discussion protocols effectively transform large classes into interactive learning environments, addressing the fundamental limitation of traditional lecture formats [3] [65]. The integration of learning analytics provides unprecedented opportunities for evidence-based refinement of instructional strategies, enabling medical educators to overcome the historical challenges of scale without sacrificing educational quality [64].
Future research should explore the longitudinal impact of enhanced discussion strategies on clinical ethical performance, particularly during the transition from preclinical to clinical training. The development of more sophisticated learning analytics approaches, including natural language processing of ethical reasoning in clinical documentation, offers promising avenues for assessing the translational impact of bioethics education. Additionally, research examining the resource implications of implementing structured discussion protocols at scale will provide essential guidance for curriculum developers and educational policymakers.
As medical education continues to evolve toward competency-based frameworks, the systematic implementation and evaluation of evidence-based discussion strategies will play an increasingly vital role in ensuring graduates develop the ethical competencies essential for high-quality patient care. The technical protocols and assessment frameworks presented in this whitepaper provide a foundation for this essential work, supporting the development of bioethics education that is both scalable and effective in preparing physicians for the complex ethical challenges of contemporary medical practice.
In the evolving landscape of medical education, bioethics has transitioned from a peripheral consideration to a fundamental component of physician training. This shift recognizes that ethical reasoning is not an innate skill but a core competency that must be systematically cultivated throughout medical training. The challenge lies in creating a cohesive educational journey that bridges the theoretical foundation of pre-clinical years with the complex practical dilemmas encountered in clinical rotations. Vertical and horizontal integration models, established in healthcare organizational structures, offer a powerful framework for achieving this continuity [67].
Vertical integration in bioethics education creates a seamless continuum from foundational knowledge to advanced application, connecting different levels of learning throughout the medical program. Horizontal integration unites bioethics with other concurrent disciplines, fostering interdisciplinary connections and reinforcing ethical reasoning across multiple clinical contexts simultaneously. Together, these approaches address the documented pitfalls of fragmented ethics education, where students often fail to connect abstract principles with clinical practice [7] [8]. The imperative for such integration is clear: without a deliberately structured pathway, ethics education risks becoming disconnected from the lived experience of clinical training, ultimately compromising the development of ethical practitioners.
Theoretical Framework: Integration Models from Health Systems
The concepts of vertical and horizontal integration, while increasingly applied in medical education, originate from organizational structures in healthcare delivery systems. Understanding these foundational models provides valuable insight for their application to curriculum design.
Horizontal Integration in Healthcare
Horizontal integration occurs when organizations operating at the same level of care merge or collaborate to improve efficiency and standardize operations [68] [67]. In healthcare, this manifests as mergers between hospitals, multi-specialty group practices, or networks of primary care clinics. These integrated structures share infrastructure, coordinate care, and reduce duplication of services. The key characteristic is the unification of similar entities or services to create a more cohesive and efficient system at a particular level of care [67].
Vertical Integration in Healthcare
Vertical integration connects providers offering different levels of services along the care continuum [67] [69]. This model brings together disparate elements—such as primary care, specialty care, and hospital services—into a unified system. The defining feature is the connection across different levels of care to create a continuous patient journey. Portugal's establishment of Local Health Units, integrating hospitals and primary care centers into single management entities, exemplifies this approach aimed at ensuring care continuity and strengthening community services [69].
Table 1: Comparison of Horizontal and Vertical Integration Models in Healthcare
| Integration Type | Structural Relationship | Primary Goal | Healthcare Example | Key Characteristics |
|---|---|---|---|---|
| Horizontal Integration | Unites entities at the same level of care | Improve efficiency, reduce costs, standardize operations | Multihospital systems; multispecialty group practices | Shared governance; unified infrastructure; economies of scale |
| Vertical Integration | Connects different levels of care along a continuum | Ensure continuity of care; create seamless patient journey | Hospital ownership of physician practices; Local Health Units in Portugal | Coordinated service delivery across settings; unified management |
Application to Educational Context
In bioethics curriculum design, these models translate into:
- Horizontal Integration: Coordinating ethics teaching across concurrent courses (e.g., linking ethics discussions in cardiology with similar dilemmas in oncology during the same academic period)
- Vertical Integration: Creating a developmental trajectory from basic ethical principles in pre-clinical years to complex clinical ethical decision-making in later years [7]
The successful implementation of these integration models in healthcare provides a validated framework for addressing fragmentation in bioethics education, offering a structured approach to creating the continuity essential for effective ethical development.
Current Landscape of Bioethics Curriculum Integration
The state of bioethics education globally reveals significant variation in implementation approaches, with increasing recognition of the need for more integrated models. Studies across different regions highlight both progress and persistent challenges in creating cohesive ethics curricula.
Evidence of Successful Integration Models
A ten-year evaluation of a spirally integrated bioethics curriculum at a private medical college in Pakistan demonstrated the effectiveness of longitudinal integration [7]. This program embedded bioethics throughout the five-year curriculum, beginning with moral philosophy and applied clinical ethics in the first two years, integrated within system-based modules. In subsequent clinical years, bioethics was incorporated into clerkships and workshops. The mixed-methods evaluation revealed that 60.3-71.2% of students agreed the curriculum contributed to their knowledge acquisition, while 62.54-67.65% reported positive impacts on ethical and professional behavior [7]. This successful implementation highlights the potential of carefully planned vertical integration.
The International Pediatric Emergency Medicine Elective (IPEME), bringing together medical students from Canada and the Middle East, demonstrated the value of horizontal integration through interactive, cross-cultural ethics education [13]. This program created a shared learning environment where students from diverse backgrounds engaged with ethical issues collectively, fostering both ethical reasoning and cultural competence simultaneously.
Identified Gaps and Challenges
Despite these promising examples, significant gaps persist in bioethics curriculum integration. Analysis of medical schools in Portugal and Brazil revealed that while 65.5% met the UNESCO-recommended minimum of 30 bioethics teaching hours, most offered ethics sporadically at the end of the medical program rather than using a longitudinal approach [8]. This fragmentation represents a critical missed opportunity for vertical integration.
Additional challenges include:
- Disconnection from Clinical Application: Students and faculty consistently report insufficient connection between theoretical ethics and clinical practice [7]
- Limited Faculty Engagement: Clinical faculty often lack involvement in ethics teaching, reducing opportunities for clinical integration [7] [12]
- Cultural and Contextual Considerations: Global bioethics education must balance universal principles with local cultural values and practices [13] [12]
Table 2: Quantitative Analysis of Bioethics Curriculum Implementation
| Metric | Pakistan Study [7] | Portugal/Brazil Study [8] | International Elective [13] |
|---|---|---|---|
| Duration/Structure | 5-year spiral integration | Variable; mostly end-of-program | 4-week intensive cross-cultural program |
| Minimum Hours | Not specified | 65.5% schools met 30-hour UNESCO minimum | Not specified |
| Student Agreement on Knowledge Acquisition | 60.3-71.2% | Not measured | All participants desired formal ethics training |
| Impact on Professional Behavior | 62.54-67.65% | Not measured | Not measured |
| Preferred Teaching Format | Small groups and shorter sessions (qualitative) | Not measured | Interactive formats most preferred |
The evidence suggests that while recognition of bioethics importance is growing globally, the implementation of truly integrated curricula remains inconsistent. Successful programs share characteristics of deliberate longitudinal planning, clinical relevance, and interactive teaching methods, providing valuable models for future curriculum development.
Methodological Framework for Integrated Bioethics Curriculum
Implementing an effective integrated bioethics curriculum requires systematic methodological approaches drawn from successful programs and curriculum design principles. The following framework provides a structured approach to development and implementation.
Vertical Integration Methodology
The spiral curriculum model provides the foundation for effective vertical integration, building complexity through revisiting core concepts at increasing levels of sophistication across the five-year program [7].
Table 3: Vertical Integration Implementation Framework
| Academic Phase | Curricular Focus | Integration Methodology | Assessment Approach |
|---|---|---|---|
| Years 1-2 (Pre-clinical) | Foundational principles: ethical theories, core concepts (consent, confidentiality) | Integration within system-based modules; case-based learning | Knowledge-based assessments; case analyses; reflective writing |
| Year 3 (Early Clinical) | Application of principles: truth-telling, professionalism, communication skills | Clinical vignettes in clerkships; structured clinical observations | Direct observation; clinical evaluations; structured reflections |
| Years 4-5 (Clinical Clerkships) | Complex ethical dilemmas: end-of-life care, resource allocation, conflict resolution | Ethics rounds; clinical ethics consultations; interprofessional learning | Clinical performance assessments; ethical reasoning evaluations; portfolio development |
The Pakistan program evaluation emphasized that "basic acquisition of knowledge and skills takes place in Years 1 & 2 with reinforcement and application in Years 3–5" [7], highlighting the developmental progression essential to vertical integration.
Horizontal Integration Methodology
Horizontal integration requires strategic coordination across concurrent learning experiences:
- Interdisciplinary Connections: Embedding ethics discussions within clinical specialties simultaneously being studied
- Cross-Cultural Integration: Incorporating diverse ethical perspectives from different cultural contexts [13]
- Clinical Correlation: Linking ethical principles with concurrent clinical skills training and patient interactions
The International Pediatric Emergency Medicine Elective demonstrated that interactive teaching formats were most preferred for fostering engagement across diverse student groups [13], highlighting the importance of pedagogy in supporting horizontal integration.
Implementation Protocol
Based on successful implementations, the following protocol ensures effective integration:
Needs Assessment Phase
- Evaluate existing ethics curriculum gaps and opportunities
- Identify key clinical transitions where ethical dilemmas emerge
- Assess institutional resources and faculty capacity
Curriculum Mapping
- Identify horizontal integration points across concurrent courses
- Establish vertical progression of learning objectives
- Align assessment methods with developmental stages
Faculty Development
- Train clinical faculty in ethics facilitation
- Create shared understanding of integration goals
- Develop mentoring programs for junior faculty
Implementation Strategy
- Pilot integration in selected modules before full implementation
- Establish regular curriculum review cycles
- Create feedback mechanisms for continuous improvement
The CIPP (Context, Input, Process, Product) model provides a useful framework for evaluation, focusing on whether the program is working while identifying improvement areas [7]. This model assesses context (integration appropriateness), input (content relevance), process (teaching methods), and product (student achievement).
Successful implementation of an integrated bioethics curriculum requires specific resources and structural supports. The following toolkit outlines essential components identified from successful programs.
Research and Educational Reagents
Table 4: Essential Resources for Integrated Bioethics Education
| Resource Category | Specific Tools/Components | Function/Application | Implementation Notes |
|---|---|---|---|
| Curriculum Framework | UNESCO Core Curriculum [8]; Spiral curriculum design [7] | Provides structural foundation and content guidance | Adapt to local cultural context; ensure minimum 30-hour requirement [8] |
| Teaching Modalities | Small group discussions; case-based learning; clinical vignettes [7] [13] | Facilitates interactive engagement and clinical application | Preferred over lectures; fosters critical discussion and reflection |
| Assessment Instruments | Knowledge tests; clinical evaluations; reflective portfolios; ethical reasoning assessments | Measures knowledge acquisition, skill development, and behavioral impact | Use multiple assessment methods aligned with developmental stage |
| Faculty Development | Ethics facilitation training; clinical faculty engagement programs; interdisciplinary teaching workshops | Builds teaching capacity and ensures consistent approach | Essential for overcoming faculty resistance and variable expertise [12] |
| Digital Infrastructure | Learning management systems; case repositories; virtual patient platforms | Supports delivery and accessibility of integrated content | Enables standardized implementation across clinical sites |
Implementation Recommendations
Based on analysis of successful programs, the following recommendations emerge as critical for effective integration:
Longitudinal Structure: Bioethics should run across the entire five-year curriculum, integrated within modules and clerkships rather than as isolated courses [7]
Clinical Faculty Involvement: Engagement of clinical faculty is essential for reinforcing ethical principles and concepts learned in earlier years [7]
Interactive Pedagogy: Small group teaching and shorter sessions are preferable for fostering discussion and maintaining student engagement [7]
Contextual Relevance: Curriculum content must balance universal principles with local cultural considerations and practical clinical realities [13] [12]
Structured Transitions: Deliberate scaffolding is needed to help students transition from theoretical understanding to clinical application of ethical principles
The mixed-methods evaluation from Pakistan emphasized that "learning embedded in an integrated curriculum can help students recognize, critically analyze and address ethical dilemmas" [7], highlighting the ultimate goal of these methodological approaches.
Vertical and horizontal integration represents not merely an organizational strategy but a fundamental reimagining of bioethics education. By creating deliberate connections between pre-clinical and clinical learning, and unifying ethics education across simultaneous disciplines, medical schools can transform bioethics from an abstract exercise into a lived professional competency. The evidence demonstrates that integrated approaches significantly enhance student achievement in knowledge acquisition, skill development, and professional behavior [7].
Future development should focus on strengthening the often-problematic transition to clinical applications, expanding faculty capacity for ethics teaching, and developing more nuanced assessment tools that capture ethical reasoning in complex clinical environments. As medical education continues to evolve, the principles of integration offer a roadmap for developing practitioners who are not only technically proficient but also ethically grounded throughout their professional careers.
The rapid evolution of medical science and technology, coupled with shifting societal dynamics, has created an urgent need for modernization of bioethics education in medical training. Bioethics, which involves the study of ethical issues emerging from advances in biology and medicine, provides a critical framework for navigating the complex moral terrain of modern healthcare [70]. The field has expanded from its initial focus on clinical relationships and research ethics to encompass pressing contemporary issues including public health crises, digital technology integration, and social media engagement [71] [72]. This whitepaper contends that a comprehensive bioethics curriculum for modern medical education must systematically integrate three emerging domains: public health ethics, social media ethics, and technology-related ethical dilemmas. The approach must be both multidisciplinary and empirically grounded, drawing on philosophy, law, clinical medicine, and empirical research to equip future clinicians and researchers with the analytical tools needed for ethical decision-making in increasingly complex environments [70].
The integration of these topics is not merely an academic exercise but a fundamental component of preparing healthcare professionals for the ethical challenges they will inevitably face. From allocating scarce medical resources during public health emergencies to navigating patient privacy concerns in social media research, today's medical professionals require ethical frameworks that address both individual patient care and broader societal impacts [71] [70]. This technical guide provides a structured approach to curriculum development, complete with empirical data, conceptual frameworks, and practical implementation strategies designed to bridge the theory-practice divide in bioethics education for medical schools, research institutions, and drug development professionals.
Public Health Ethics: From Theory to Practice
Conceptual Foundations and Current Challenges
Public health ethics represents a distinct subdomain of bioethics that focuses on the moral dimensions of population health, contrasting with clinical ethics' emphasis on individual practitioner-patient relationships [71]. This field has gained unprecedented relevance in light of recent global health crises, which have highlighted the ethical tensions between individual rights and community health needs [71]. The COVID-19 pandemic, in particular, "flooded the public's consciousness with some of the most challenging ethical questions of our time," bringing concepts like justice, health equity, interconnectedness, and solidarity into contentious public debate [71]. Public health personnel found themselves at the center of these discussions, "managing the urgency of the situation while helping communities identify and address tough ethical questions" [71].
The field of public health ethics emerged as an organized scholarly discipline in the late 1990s and early 2000s as practitioners and scholars recognized that the tools of clinical ethics were insufficient for addressing the value trade-offs required in public health decision-making [71]. Where clinical ethics typically focuses on the individual patient-practitioner relationship, public health ethics must balance the interests of individuals against the needs of communities, creating unique ethical challenges that require distinct analytical frameworks [71]. Contemporary public health ethics addresses diverse issues including "using novel data sources for public health surveillance, developing artificial intelligence to advance public health action, considering the role of solidarity in the context of libertarian societies, addressing ethical dimensions of the social determinants of health, [and] mitigating the impact of social and wealth inequity on community health" [71].
Table 1: Key Ethical Challenges in Public Health Practice
| Challenge Category | Specific Ethical Dilemmas | Stakeholders Affected |
|---|---|---|
| Resource Allocation | Rationing scarce resources (e.g., ICU beds, vaccines), priority setting, cost-benefit analyses of interventions | Patients, providers, healthcare organizations, public health agencies |
| Health Equity | Addressing social determinants of health, reducing disparities in access to care, prioritizing vulnerable populations | Marginalized communities, rural populations, low-income individuals |
| Legal & Authority Issues | Balancing public health mandates with individual liberties, managing political relationships, justifying restrictive measures | Government agencies, health departments, general public, businesses |
| Data Ethics | Public health surveillance, privacy concerns with data collection, use of novel data sources (including social media) | Researchers, the public, technology companies, public health officials |
| Emergency Response | Ethical decision-making during pandemics and disasters, altering standards of care during crises, global vaccine distribution | Health systems, frontline workers, international organizations, communities |
Empirical Assessment of Curriculum Integration
Research on bioethics curriculum implementation provides critical insights into effective educational approaches. A mixed-methods evaluation study of an integrated bioethics curriculum at a private medical college in Pakistan demonstrated the effectiveness of longitudinal integration across the five-year undergraduate medical program [7]. The study revealed that "the majority of students agreed that the curriculum contributed to their knowledge acquisition (60.3—71.2%), skill development (59.41—60.30%) and demonstration of ethical/professional behavior (62.54—67.65%)" [7]. These quantitative findings were further enriched by qualitative data from focus group discussions, which highlighted the importance of clinical integration and practical application.
Table 2: Student Perceptions of Bioethics Curriculum Effectiveness (n=500)
| Learning Domain | Agreement Rate (%) | Key Insights from Qualitative Data |
|---|---|---|
| Knowledge Acquisition | 60.3 - 71.2% | Students found content relevant and appropriate to learning objectives |
| Skill Development | 59.4 - 60.3% | Small group teaching and case discussions were particularly effective |
| Ethical/Professional Behavior | 62.5 - 67.7% | Students appreciated integration with clinical scenarios but requested more clinical exposure |
| Instructional Methods | N/A | Multi-modal methods effective; large class formats less engaging; shorter sessions preferred |
The study identified several key factors for successful curriculum implementation: basic knowledge and skills acquisition should occur in the first two years of medical education, with reinforcement and application in clinical years (Years 3-5); learning should be embedded in an integrated curriculum to help students "recognize, critically analyze and address ethical dilemmas"; and "involvement and commitment of the clinical faculty is essential for reinforcing the ethical principles and concepts learnt in the earlier years" [7]. Participants in the study suggested that the curriculum could be further strengthened by "better integration in clinical years, role modelling and providing opportunities for application in clinical health care settings" [7]. Additionally, they recommended expanding content to include "ethical issues related to the use of social media, public health ethics and ethics and law" [7], highlighting the need for the very curriculum enhancements this whitepaper advocates.
Social Media Ethics: Navigating Digital Frontiers
Ethical Frameworks for Social Media Engagement and Research
The pervasive use of social media has introduced complex ethical challenges for healthcare professionals and researchers, particularly in the realms of public health communication and data collection. Social media platforms offer "great potential for effectively communicating about public health risks so people make healthier and safer choices" and can "strengthen trust between the public and the institution" when used appropriately [73]. However, inappropriate use "may also create distrust" and introduce significant ethical risks [73]. These concerns have led experts to recommend that organizations develop "a code of engagement be included in corporate social media policies that contain guidance as to what conduct is or is not appropriate with a view to maintaining public trust in the institution" [73].
For researchers, social media represents "a veritable goldmine of opportunity" because "every day, reams of naturally occurring data are produced by users of social media such as Twitter, Instagram and Facebook" [74]. Yet this research avenue is "riddled with ethical challenges, and no clear consensus has emerged as to the ethical handling of such data" [74]. Key issues include "privacy; anonymity and confidentiality; authenticity; the rapidly changing SM environment; informed consent; recruitment, voluntary participation, and sampling; minimizing harm; and data security and management" [74]. The fundamental challenge lies in balancing the public availability of social media data with users' reasonable expectations of privacy and autonomy.
Research ethics committees (RECs) often struggle with reviewing social media research proposals due to "a lack of personal and professional experience of SM, compounded by a lack of institutional and professional guidelines" [74]. One study found that "REC members with less experience of reviewing SM held inflexible notions of consent and risk that could be categorized as either relying on traditional notions of requiring direct consent, or viewing publicly available data as 'fair game'" [74]. In contrast, "more experienced REC members took a more nuanced approach to data use and consent" [74]. This suggests that both researcher education and REC development are necessary for the ethical advancement of social media research in healthcare.
Experimental Protocols for Social Media Research Ethics
Establishing methodologically sound and ethically rigorous protocols for social media research requires careful consideration of several key dimensions. The following workflow outlines a systematic approach to ethical decision-making in social media studies:
This decision protocol should be implemented alongside specific methodological safeguards. For studies involving analysis of existing social media content, researchers should: (1) conduct a privacy risk assessment that considers both technical accessibility and users' reasonable expectations of privacy; (2) implement robust data anonymization techniques that remove or obscure identifying information; (3) consider the vulnerability of the population being studied; and (4) develop a plan for secure data storage and eventual destruction [74]. When research involves interacting with users or recruiting participants through social media, informed consent processes must be adapted to the digital context while maintaining ethical rigor [74].
Research Reagent Solutions: Social Media Ethics Toolkit
Table 3: Essential Methodological Tools for Ethical Social Media Research
| Research Tool | Function | Ethical Considerations |
|---|---|---|
| Data Anonymization Protocols | Remove personally identifiable information from social media datasets | Balance between data utility and privacy protection; consider re-identification risks |
| Platform API Agreements | Govern formal data access and usage terms | Compliance with platform policies that may prohibit certain research uses |
| Customized Consent Frameworks | Adapt informed consent processes for digital contexts | Digital consent must be equally valid as traditional written consent |
| Vulnerability Assessment Matrix | Identify potentially vulnerable groups in social media spaces | Extra protections may be needed for minors, marginalized communities, or trauma survivors |
| Ethical Advisory Panels | Provide specialized review for social media research projects | Address the limitation of traditional RECs in evaluating digital methodology |
Technology-Related Dilemmas: Digital Health Ethics
Ethical Challenges in Digital Healthcare Technology
The rapid adoption of digital healthcare technologies, including telemedicine, wearable devices, and artificial intelligence, presents novel ethical challenges at multiple levels of the healthcare system. Digital healthcare may be defined as "the use of advanced technologies including 'big data', artificial intelligence and genomics to achieve health objectives for patients" [72]. While proponents point to benefits including "improving access to healthcare services, enabling greater autonomous active patient participation, facilitating better clinical decision making as well as allowing for cost savings and greater efficiency in the delivery of health services," these technologies also introduce significant ethical tensions [72].
Fritz and Cox succinctly summarize the fundamental issue: whilst organizations balance financial as well as clinical obligations and physicians manage interpatient demands for current and future generations, they all do so "in the absence of a philosophical framework to face novel healthcare challenges fairly and justly for the different users of healthcare services" [72]. This framework is essential for navigating the complex interplay between technological capabilities and ethical responsibilities in digital health.
The diagram below illustrates the key ethical dimensions and their interrelationships in digital healthcare:
At the organizational level, the high cost of technology represents "one of the largest challenges to organisations with respect to installation and subsequent maintenance" [72]. This creates tension between the potential long-term benefits of digital health technologies and the immediate financial constraints facing healthcare systems. Additionally, issues of interoperability—"integration and cross-access of data and usage between different systems or even different versions"—pose significant ethical concerns related to continuity of care and efficient resource use [72].
For healthcare providers, the "technological imperative" refers to "the inevitability of new technology and its essential nature which denotes the need for acceptance for societal good" [72]. In healthcare, this imperative "arguably modulates the purpose of healthcare from preservation and restoration under responsible autonomy to death prevention," potentially violating patient autonomy by making patients "both '(the) battlefield and (the) prize'" [72]. This creates moral distress for physicians who feel compelled to utilize the latest technologies even when they may not align with patient values or preferences.
For patients, fundamental issues of access and equity emerge. "From a utilitarian viewpoint with regards to if, for example, remote monitoring enables greater access; for the majority, we know that no such improvements in access have been reported" [72]. Similarly, research does not support the notion that digital health technologies necessarily benefit the most disadvantaged populations, failing to fulfill Rawlsian principles of justice [72]. This raises critical ethical questions about whether digital health innovations may inadvertently exacerbate existing health disparities.
Curricular Integration Strategies
Effectively integrating technology ethics into medical education requires a multi-pronged approach that addresses both conceptual understanding and practical application. The foundational elements should include:
Case-Based Learning: Curated case studies examining real-world ethical dilemmas in digital health, such as AI diagnostic tools, wearable health monitors, and telemedicine platforms. These cases should highlight tensions between ethical principles, such as the conflict between beneficence (using technology to improve outcomes) and justice (equitable access to technological benefits).
Interdisciplinary Perspectives: Incorporating viewpoints from philosophy, law, computer science, and social sciences to provide students with a comprehensive understanding of the societal implications of healthcare technologies [70]. This multidisciplinary approach reflects the reality that "bioethics is a multidisciplinary field, combining philosophy, theology, history, and law with medicine, nursing, health policy, and the medical humanities" [70].
Hands-on Technology Assessment: Practical exercises in evaluating digital health technologies using ethical frameworks, including the Four Principles approach (respect for autonomy, beneficence, non-maleficence, and justice) [72] and Rawlsian theories of justice [72].
Critical Theory Application: Analysis of how digital technologies may reinforce or exacerbate health disparities, with particular attention to underserved populations. This aligns with the recognition that "the literature is not supportive of cost reductions benefiting the majority of those who are most disadvantaged" by digital health technologies [72].
Implementation Framework: Integrated Curriculum Design
Longitudinal Integration Strategy
A successful bioethics curriculum incorporating emerging topics must be systematically integrated throughout medical education rather than being confined to standalone courses. Research demonstrates that "an effective bioethics curriculum for undergraduate medical education should run longitudinally across the 5 year curriculum and be integrated in the modules and clerkships" [7]. The specific implementation should follow a spiral curriculum model where "basic acquisition of knowledge and skills takes place in Years 1 & 2 with reinforcement and application in Years 3–5" [7].
The diagram below illustrates this comprehensive integration approach:
Faculty Development and Institutional Support
Successful implementation of this modernized bioethics curriculum requires substantial faculty development and institutional commitment. Clinical faculty members, in particular, need support to effectively integrate ethical discussions into clinical teaching. As the evaluation study found, "involvement and commitment of the clinical faculty is essential for reinforcing the ethical principles and concepts learnt in the earlier years" [7]. Institutions should establish ongoing faculty development programs that include:
- Ethics Content Updates: Regular sessions on emerging ethical issues in public health, social media, and healthcare technology.
- Teaching Methodology Training: Instruction in case-based teaching, small group facilitation, and ethical dilemma resolution techniques.
- Interdisciplinary Collaboration Opportunities: Structured forums for dialogue between clinical faculty, ethics specialists, and technology experts.
- Resource Sharing: Curated collections of teaching cases, multimedia resources, and assessment tools for ethics education.
Additionally, institutions should consider establishing centers or programs specifically dedicated to bioethics education and consultation. The absence of such structures is particularly notable at HBCU medical schools, where "none of the HBCU medical schools have a bioethics department" despite the fact that "70% of Black doctors in the US attended an HBCU at some point in their path to becoming physicians" [75]. This represents a significant opportunity to address health equity through educational innovation.
The integration of emerging topics in social media ethics, public health ethics, and technology-related dilemmas into medical bioethics curricula is an essential response to the rapidly evolving healthcare landscape. This whitepaper has provided a comprehensive framework for developing, implementing, and evaluating such a curriculum, drawing on current research and best practices in bioethics education. The approach emphasizes longitudinal integration, multidisciplinary perspectives, and practical application to prepare future healthcare professionals for the complex ethical challenges they will face.
By adopting the strategies outlined here, medical schools and research institutions can create robust ethics education programs that not only address traditional bioethical concerns but also engage with the pressing emerging issues at the intersection of technology, public health, and digital communication. Such curricula are fundamental to developing healthcare professionals who are both clinically excellent and ethically equipped to navigate the complexities of modern medicine, ultimately contributing to more equitable and ethically grounded healthcare systems.
Conclusion
Developing an effective bioethics curriculum requires a deliberate, longitudinal, and integrated approach that spans the entire medical education journey. Evidence confirms that successful programs embed ethics spirally from pre-clinical to clinical years, utilize engaging pedagogies like TBL and performable cases, and proactively address implementation barriers through faculty development and resource allocation. Robust mixed-methods evaluation is critical for continuous improvement. Future directions must focus on enhancing clinical application through role modeling, addressing emerging ethical challenges in technology and public health, and strengthening the evidence base linking ethics education to long-term professional conduct. For biomedical researchers and drug development professionals, these educational advancements ensure future collaborators in clinical practice possess the ethical framework necessary for navigating complex research dilemmas and patient care challenges.
References
- 1. The Hastings Center Bioethics Timeline - The Hastings Center for... [https://www.thehastingscenter.org/bioethics-timeline/]
- 2. Meeting the challenge of teaching bioethics : a successful residency... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8820793/]
- 3. curriculum for undergraduate medical students: an... Bioethics [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-024-05376-4]
- 4. " Bioethics for undergraduate medical students: An..." curriculum [https://ecommons.aku.edu/pakistan_fhs_mc_ded/61/]
- 5. Academics | Master's Degrees | Bioethics | Degrees and Courses [https://sps.columbia.edu/academics/masters/bioethics/master-science/curriculum-courses/course-list-schedule]
- 6. in prescribing: A first european... Essential competencies [https://pubmed.ncbi.nlm.nih.gov/27648725/]
- 7. Bioethics curriculum for undergraduate medical students: an evaluation study utilizing mixed methods approach - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11003031/]
- 8. Bioethics curriculum in medical schools in Portuguese-speaking countries | BMC Medical Education | Full Text [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-022-03250-9]
- 9. Educating future doctors and nurses in mental, neurological and... [https://www.who.int/news/item/29-04-2025-educating-future-doctors-and-nurses-in-mental--neurological-and-substance-use-care]
- 10. AAMC Core for Pre-Med: What to Know in Competencies | Leland 2025 [https://www.joinleland.com/library/a/aamc-core-competencies-pre-med-guide]
- 11. Technical Standards/ Functional Core - College of... Competencies [https://medicine.usask.ca/policies/com-technical-standards.php]
- 12. Evolution of bioethics education in the medical programme: a tale of two medical schools | International Journal of Ethics Education [https://link.springer.com/article/10.1007/s40889-020-00112-0]
- 13. Developing a bioethics curriculum for medical students from divergent geo-political regions - PubMed [https://pubmed.ncbi.nlm.nih.gov/27461194/]
- 14. in Global | SpringerLink Education Bioethics [https://link.springer.com/book/10.1007/978-3-319-78984-2]
- 15. Institutionalization of Bioethics in Higher Education Institutions... [https://link.springer.com/article/10.1007/s11673-025-10442-7]
- 16. What Is Culturally Responsive Teaching? [https://www.edweek.org/teaching-learning/culturally-responsive-teaching-culturally-responsive-pedagogy/2022/04]
- 17. Culturally Relevant and Culturally Responsive | NSTA [https://www.nsta.org/science-and-children/science-and-children-marchapril-2021/culturally-relevant-and-culturally]
- 18. MDSC404 Global | School of Bioethics | University of... Medicine [https://www.liverpool.ac.uk/medicine/study-with-us/cpd/globalbioethics/]
- 19. MyBioethics: How Ed-Tech Enables Discovery-Driven Empirical Bioethics Research | Digital Society [https://link.springer.com/article/10.1007/s44206-024-00119-w]
- 20. Bioethics: Core Concepts | CBHD Site Topic Issues [https://www.cbhd.org/issues/bioethics-core-concepts]
- 21. Developing Novel Tools for Bioethics Education: ACECS and the Visual Analytics Dashboard | Cambridge Quarterly of Healthcare Ethics | Cambridge Core [https://www.cambridge.org/core/journals/cambridge-quarterly-of-healthcare-ethics/article/developing-novel-tools-for-bioethics-education-acecs-and-the-visual-analytics-dashboard/F8277806881FC5BFB341ED5A48EBB31D]
- 22. Medical Students’ Acquaintance with Core Concepts, Institutions and Guidelines on Good Scientific Practice: A Pre- and Post-questionnaire Survey | Science and Engineering Ethics [https://link.springer.com/article/10.1007/s11948-020-00215-3]
- 23. 2025 Summer Seminar in Healthcare Ethics | UW Department of Bioethics & Humanities [https://depts.washington.edu/bhdept/bioethics-training/2025-summer-seminar-healthcare-ethics]
- 24. ERIC - ED538282 - The Spiral Curriculum. Research into Practice, Education Partnerships, Inc., 2012-Mar [https://eric.ed.gov/?id=ED538282]
- 25. Postgraduate ethics training programs: a systematic scoping review [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-021-02644-5]
- 26. Introducing professionalism and medical ethics in undergraduate... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11639436/]
- 27. ERIC - EJ1286824 - Perspectives on Curriculum Design: Comparing the Spiral and the Network Models, Research Matters, 2020 [https://eric.ed.gov/?id=EJ1286824]
- 28. The Spiral Curriculum: implications for online learning | BMC Medical Education | Full Text [https://bmcmededuc.biomedcentral.com/articles/10.1186/1472-6920-7-52]
- 29. (DOC) ASSESSMENT ON THE SPIRAL PROGRESSION OF THE K-12 CURRICULUM In Partial Fulfilment of the Requirement on Seminar on Educational Measurement and Evaluation (EDAD 206 [https://www.academia.edu/36040423/ASSESSMENT_ON_THE_SPIRAL_PROGRESSION_OF_THE_K_12_CURRICULUM_In_Partial_Fulfilment_of_the_Requirement_on_Seminar_on_Educational_Measurement_and_Evaluation_EDAD_206]
- 30. (DOC) Spiral Progression Delimma [https://www.academia.edu/29017585/Spiral_Progression_Delimma]
- 31. Quantitative and qualitative evaluation of a learning model based on workstation activities - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7406050/]
- 32. Building connections between biomedical sciences and ethics for medical students | BMC Medical Education | Full Text [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-022-03865-y]
- 33. The Future Of Medical Is Realistic And Immersive Education [https://www.forbes.com/sites/cortneyharding/2025/10/30/the-future-of-medical-education-is-realistic-and-immersive/]
- 34. Team-Based Learning in Bioethics Education: Creating a Successful Curriculum for Residents in an Era of “Curricular Squeeze” - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8368489/]
- 35. Bioethics TBL | Team-Based Learning For Bioethics [https://bioethicstbl.org/]
- 36. The effectiveness of online team-based learning in introduction to medical ethics education for medical students at a medical college of Nepal: a pilot study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9643934/]
- 37. Using Team-Based Learning to Teach Human Subjects Research Ethics - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8368337/]
- 38. Performable Case Studies in Ethics Education - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5618185/]
- 39. Performable Case Studies in Ethics Education [https://www.mdpi.com/2227-9032/5/3/57]
- 40. Medical readers' theater: relevance to geriatrics medical education - PubMed [https://pubmed.ncbi.nlm.nih.gov/22087781/]
- 41. Caring from behind the face mask in healthcare: Learning from the... [https://link.springer.com/article/10.1007/s40037-021-00691-8]
- 42. Medical Readers Theater: A Guide and Scripts | University of Iowa Press - The University of Iowa [https://uipress.uiowa.edu/books/medical-readers-theater-guide-and-scripts]
- 43. Toward narrowing the theory–practice gap: characterizing evidence from in-service biology teachers’ questions asked during an academic course | International Journal of STEM Education | Full Text [https://stemeducationjournal.springeropen.com/articles/10.1186/s40594-019-0174-3]
- 44. Family Life Education: Integrating Bioethics [https://www.numberanalytics.com/blog/family-life-education-bioethics-integration]
- 45. CASE STUDIES - Narrative Inquiry in Bioethics [https://nibjournal.org/education/case-studies/]
- 46. Development of Case- Based Electronic Bioetics Modules for... Learning [https://ijsshr.in/v6i2/35.php]
- 47. Teaching the bioethics of information technologies and artificial... [https://link.springer.com/article/10.1007/s40889-025-00218-3]
- 48. A proposal for teaching bioethics in high schools using appropriate visual education tools | Philosophy, Ethics, and Humanities in Medicine | Full Text [https://peh-med.biomedcentral.com/articles/10.1186/s13010-018-0064-1]
- 49. Color and Graphics | Understanding Web Accessibility | Web Accessibility | Brandeis University [https://www.brandeis.edu/web-accessibility/understanding/color.html]
- 50. The Science of Accessibility: Designing for Colorblind and Visually Impaired Users - RMCAD [https://www.rmcad.edu/blog/the-science-of-accessibility-designing-for-colorblind-and-visually-impaired-users/]
- 51. Color Guidelines for Digital Accessibility | Engineering Technology Services (ETS) [https://ets.osu.edu/color-guidelines-digital-accessibility]
- 52. Color Considerations | Digital Accessibility at Princeton [https://digital.accessibility.princeton.edu/how/design/color-contrast]
- 53. Colorblind-Friendly Palettes: Why & How to Use in Design - Venngage [https://venngage.com/blog/color-blind-friendly-palette/]
- 54. Colour for online teaching materials — Manitoba Flexible Learning Hub [https://mbhub.ca/resources/colour-for-online-teaching-materials/]
- 55. 3 Implementation Strategies | Environmental Medicine : Integrating ... [https://nap.nationalacademies.org/read/4795/chapter/5]
- 56. Reframing data ethics in research methods education: a pathway to critical data literacy | International Journal of Educational Technology in Higher Education | Full Text [https://educationaltechnologyjournal.springeropen.com/articles/10.1186/s41239-023-00380-y]
- 57. Journal of Medical Internet Research - Trust-Building Strategies of... [https://www.jmir.org/2025/1/e80299]
- 58. | Doctorate of Professional Studies in Curriculum Bioethics [https://www.amc.edu/education/alden-march-bioethics-institute/doctorate-of-professional-studies-bioethics/doctorate-of-professional-studies-in-bioethics-clinical-ethics-curriculum/]
- 59. Teaching seven principles for public health ethics : towards... [https://pubmed.ncbi.nlm.nih.gov/25288039/]
- 60. Virtual faculty program in development evaluated by... bioethics [https://pmc.ncbi.nlm.nih.gov/articles/PMC10615268/]
- 61. Bioethical knowledge in students and health professionals: a systematic review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11041021/]
- 62. A Survey of Medical Ethics Curricula at 11 US Medical Schools | Medical Science Educator [https://link.springer.com/article/10.1007/s40670-024-02254-y]
- 63. How to Engage More Students in Middle and High School Classroom Discussions | Edutopia [https://www.edutopia.org/article/how-engage-more-students-classroom-discussions/]
- 64. Learning Analytics in Medical Education Assessment: The Past, the Present, and the Future - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6001721/]
- 65. The Big List of Class Discussion Strategies | Cult of Pedagogy [https://www.cultofpedagogy.com/speaking-listening-techniques/]
- 66. Development of medical leadership competence during undergraduate... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-025-07635-4]
- 67. and Horizontal of Health Care Providers... Vertical Integration [https://pmc.ncbi.nlm.nih.gov/articles/PMC6978994/]
- 68. Healthcare technology integration : benefits, challenges, types. [https://neklo.com/blog/healthcare-technology-integration]
- 69. in health: An oasis or a mirage? Vertical integration [https://accscience.com/journal/GHES/articles/online_first/5388]
- 70. Bioethical Issues in Healthcare Management | CSP Global [https://online.csp.edu/resources/article/bioethical-issues-health-care-management/]
- 71. in Ethical Practice and a New Department... Challenges Public Health [https://pmc.ncbi.nlm.nih.gov/articles/PMC9730179/]
- 72. The ethical challenges facing the widespread adoption of digital healthcare technology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7612237/]
- 73. in Ethical engagement and challenges ... social media research [https://pubmed.ncbi.nlm.nih.gov/27270048/]
- 74. (PDF) Ethics oversight and challenges to empirical research based... [https://www.academia.edu/108067165/Ethics_oversight_and_challenges_to_empirical_research_based_on_social_media_platforms]
- 75. On Tech Ethics Podcast on Bioethics in HBCU Medical Schools [https://about.citiprogram.org/blog/on-tech-ethics-podcast-the-essential-role-of-bioethics-in-hbcu-medical-schools/]