Bridging the Gap: A Practical Guide to Interdisciplinary Methods in Empirical Bioethics for Biomedical Research
This article provides a comprehensive exploration of interdisciplinary approaches in empirical bioethics, tailored for researchers, scientists, and drug development professionals.
Bridging the Gap: A Practical Guide to Interdisciplinary Methods in Empirical Bioethics for Biomedical Research
Abstract
This article provides a comprehensive exploration of interdisciplinary approaches in empirical bioethics, tailored for researchers, scientists, and drug development professionals. It addresses the foundational need to integrate empirical data with normative analysis, moving beyond traditional philosophical inquiry to ground ethical guidance in the realities of clinical practice and research. The scope covers established methodological frameworks for combining qualitative and quantitative research with ethical reasoning, tackles common challenges such as interdisciplinary conflict and the 'is-ought' gap, and evaluates the rigor and acceptability of different approaches. By synthesizing current methodologies and their practical applications, this guide aims to equip professionals with the tools to conduct robust, ethically-informed research that can effectively navigate the complexities of modern healthcare innovations.
The 'Is' and the 'Ought': Laying the Groundwork for Empirical Bioethics
Interdisciplinary Empirical Bioethics (IEB) represents a significant methodological evolution within bioethics, emerging from the concerted effort to bridge the gap between theoretical normative analysis and the lived reality of ethical issues in healthcare, medicine, and science [1]. This field is fundamentally characterized by its integration of empirical research methods from the social sciences—such as sociology, anthropology, and psychology—with the normative analytical frameworks of philosophy and law [2] [3]. The rise of IEB is often attributed to a dissatisfaction with a purely philosophical approach, which was perceived as insufficient to address the complex, context-specific nature of bioethical issues encountered in practice [2]. By systematically incorporating data about the actual beliefs, behaviors, and experiences of relevant stakeholders, IEB seeks to ground ethical analysis in a richer, more nuanced understanding of the practical contexts in which ethical dilemmas arise [4].
The "interdisciplinary" component is crucial; it moves beyond a mere multidisciplinarity where different disciplines work in parallel, and instead fosters a integrative dialogue where empirical findings and normative reasoning mutually inform and reshape one another [5]. This integration aims to produce ethical recommendations that are not only philosophically sound but also practically relevant and applicable [6]. The empirical "turn" in bioethics has been substantial. Surveys of bioethics researchers in twelve European countries found that 87.5% report using or having used empirical methods in their work, indicating a widespread adoption of this interdisciplinary approach [3]. This article outlines the core frameworks, methodologies, and practical protocols that define and guide research in this dynamic field.
Theoretical Frameworks and Classifications
The theoretical foundation of IEB is built upon various models that classify its ambitions and describe the process of integrating empirical data with normative analysis. These frameworks help to structure research projects and clarify the intended contribution of empirical work to bioethical discourse.
Hierarchical Aims of Empirical Bioethics
One influential framework classifies the objectives of empirical research in bioethics into a hierarchy of four levels, ranging from the purely descriptive to the directly normative [6]. This classification helps to map the diverse ambitions of IEB projects, as summarized in the table below.
Table 1: Kon's Hierarchical Framework for Empirical Research in Bioethics
| Category | Description | Exemplary Research Questions |
|---|---|---|
| Lay of the Land | Seeks to define current practices, opinions, beliefs, or other aspects of the status quo [6]. | "What do patients want regarding Z?" "How do nurses perceive Y?" [6]. |
| Ideal vs. Reality | Assesses the extent to which actual clinical or research practice reflects established ethical ideals or norms [6]. | "To what extent is valid informed consent obtained in clinical trials?" "Do healthcare resources get allocated equitably?" [6]. |
| Improving Care | Uses empirical research to develop and test interventions aimed at bringing practice closer in line with ethical ideals [6]. | "Does a new ethics consultation service improve the alignment of care with patient values?" |
| Changing Ethical Norms | Brings together data from multiple empirical studies to inform, critique, and potentially change our ethical ideals and principles [6]. | "Do findings from long-term studies on quality of life compel a re-evaluation of norms surrounding life-sustaining treatment?" |
Recent empirical research on the views of IEB scholars themselves reveals nuanced attitudes towards these objectives. While identifying ethical issues in practice and understanding their context receives nearly unanimous agreement, objectives like "developing and justifying moral principles" are more contested, reflecting ongoing philosophical debates about the is-ought gap [4]. This gap, however, is increasingly viewed not as an insurmountable obstacle but as a warning sign to critically reflect on the normative implications of empirical results [4].
The Mapping-Framing-Shaping Process Framework
A complementary framework conceptualizes the entire IEB research process through a landscaping metaphor of Mapping-Framing-Shaping [5]. This model is particularly useful for designing and planning research projects.
- Mapping: This initial phase involves surveying the existing terrain of a bioethical issue. The researcher conducts comprehensive literature reviews, analyzing previous scholarship from relevant disciplines to understand the "state of the art," identify gaps, and hone research questions. It is primarily a desk-based, analytical stage [5].
- Framing: In this phase, the researcher zooms in to explore specific areas of the mapped terrain in depth. This typically involves qualitative empirical work (e.g., interviews, focus groups) to understand how key issues are "framed" and experienced by relevant stakeholders (e.g., patients, clinicians, researchers). The goal is to gather finely-grained, perspectival data on the lived experience of the ethical problem [5].
- Shaping: The final phase involves seeking to (re)shape the terrain by formulating normative recommendations. Informed by the findings from both the mapping and framing phases, the researcher develops a justified vision for a way forward, issuing guidance, policy recommendations, or theoretical corrections [5].
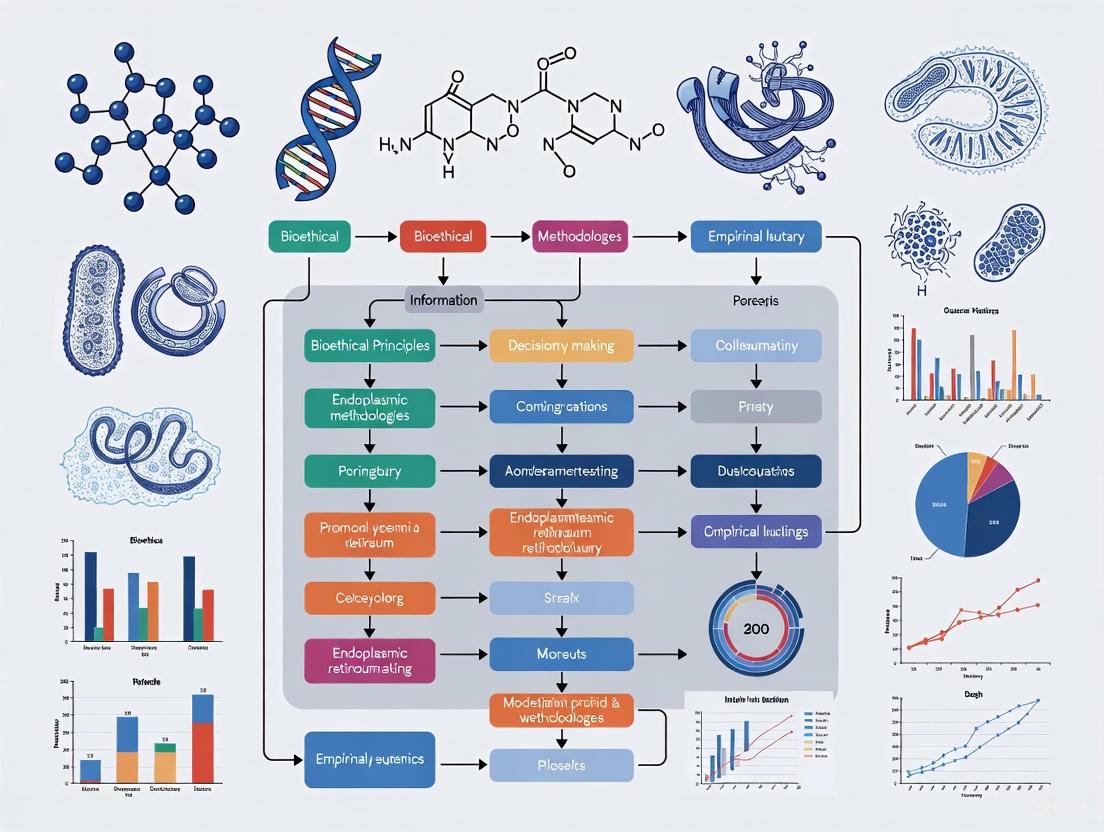
This framework underscores that integration is not a single event but a process that spans the entire research project, with each phase building upon the last [5]. The following diagram illustrates this workflow and its iterative nature.
Methodological Integration: Protocols and Practices
The defining challenge of IEB is the methodological integration of empirical data with normative analysis. This process must be transparent and rigorous to produce credible results.
Common Integration Methodologies
A systematic review has identified at least 32 distinct methodologies for integration, which can be grouped into several categories [2]:
- Consultative Approaches: The researcher acts as the sole integrator, analyzing empirical data and independently developing a normative conclusion. The most prominent example is Reflective Equilibrium, a process where the researcher engages in a back-and-forth deliberation between ethical principles, intuitions, and empirical facts until a state of coherence ("equilibrium") is achieved [4] [2].
- Dialogical Approaches: Integration occurs through structured dialogue among stakeholders (e.g., researchers, participants, professionals). In these methods, the normative conclusion is developed collectively through deliberation, with the ethicist often acting as a facilitator rather than the sole authority [2].
- Inherent Integration Approaches: In some projects, the normative and empirical are intertwined from the outset, with the research design making it difficult to separate the two components [2].
Despite this variety, scholars report that the practical application of these methodologies is often characterized by an "air of uncertainty and overall vagueness" [2]. This highlights the need for clear protocols and standards of practice.
A Protocol Template for Empirical Bioethics Research
To ensure scientific rigor and ethical soundness, IEB research should be guided by a structured protocol. The following table adapts a template specifically designed for humanities and social sciences in health, making it suitable for IEB projects [7].
Table 2: Core Elements of a Research Protocol for Interdisciplinary Empirical Bioethics
| Section | Key Content and Considerations for IEB |
|---|---|
| Title & Abstract | Clearly describe the nature of the study and the interdisciplinary approach used (e.g., "a qualitative empirical bioethics study using reflective equilibrium") [7]. |
| Problem & Rationale | Explain the importance of the bioethical problem and justify the need for an interdisciplinary approach, summarizing key scholarly work [7] [8]. |
| Objectives/Questions | Present specific, answerable research questions. IEB questions often have both an empirical and a normative component (e.g., "How do oncologists experience moral distress in early-phase trials, and what should be done to address it?"). |
| Disciplinary Field & Research Paradigm | Explicitly state the project's location in IEB. Present and justify the methodological framework (qualitative/quantitative/mixed) and the theoretical normative framework (e.g., principlism, care ethics) that will be used [7]. |
| Methodology: Data Collection | Detail the procedures for sampling participants, data collection (e.g., interview guides, surveys), and data management. Justify all choices in relation to the research questions [7] [8]. |
| Methodology: Integration & Normative Analysis | This is a crucial, defining section. Clearly articulate and justify the chosen method for integrating empirical data with normative analysis (e.g., reflective equilibrium, a dialogical approach). Explain how this process will be conducted [2] [5]. |
| Ethical Considerations | Describe issues like informed consent, confidentiality, and management of psychosocial risks. Even studies using only interviews or questionnaires must undergo ethics review [7] [9] [8]. |
This protocol structure ensures that researchers plan for integration from the beginning, rather than treating it as an afterthought.
The Researcher's Toolkit: Essential Reagents and Methods
Conducting robust IEB requires a toolkit composed of both conceptual "reagents" and practical methodological skills. The following table details key components.
Table 3: Essential Toolkit for Interdisciplinary Empirical Bioethics Research
| Tool/Reagent | Category | Function in IEB Research |
|---|---|---|
| Semi-Structured Interview Guides | Data Collection Instrument | Elicits rich, qualitative data on stakeholder perspectives, experiences, and moral reasoning while allowing for flexibility to explore unanticipated themes [3]. |
| Validated Survey Instruments | Data Collection Instrument | Quantifies attitudes, beliefs, or prevalence of practices across a larger population, providing data for "Lay of the Land" or "Ideal vs. Reality" studies [6] [3]. |
| Focus Group Protocols | Data Collection Instrument | Facilitates the collection of data through group interaction, revealing shared views, cultural norms, and points of contention on a bioethical issue [3]. |
| Qualitative Data Analysis Software (e.g., NVivo, MAXQDA) | Data Analysis Tool | Assists in the systematic organization, coding, and analysis of large volumes of qualitative data (e.g., interview transcripts) [2]. |
| Reflective Equilibrium | Integration Methodology | Provides a structured, consultative process for the researcher to critically move back-and-forth between empirical data, ethical principles, and intuitive judgements to achieve normative coherence [4] [2]. |
| Deliberative Dialogues | Integration Methodology | Creates a structured forum for stakeholders to discuss empirical findings and ethical arguments, aiming to produce ethically robust and shared recommendations [2]. |
| Ethical Theory Framework (e.g., Principlism) | Normative Analytic Tool | Provides a coherent set of concepts and principles (e.g., autonomy, beneficence) to systematically analyze the ethical dimensions of the issue under study [7]. |
The effectiveness of these tools is contingent upon researcher competence. Surveys indicate a training gap, with over a fifth of bioethics researchers using empirical methods reporting no formal methodological training [3]. This underscores the need for interdisciplinary education that combines empirical research skills with normative analytical expertise.
Emerging Frontiers: Digital Bioethics
The digital transformation of society has given rise to a novel frontier in IEB: digital bioethics. This emerging sub-field leverages methods from computational social science to study bioethical issues as they are articulated and debated in online spaces [1]. Digital bioethics treats the online space—social media platforms, forums, and other digital agoras—as a legitimate site for rigorous empirical research in bioethics [1].
The methods of digital bioethics include:
- Automated analysis of hyperlink structures to map networked relationships between websites discussing bioethical issues.
- Natural Language Processing (NLP) to trace the emergence and evolution of bioethical discourse and public attitudes at scale.
- Digital ethnography to understand the cultures and practices that form around bioethical issues in virtual worlds and online communities [1].
This "digital turn" expands the empirical gaze of bioethics, allowing researchers to investigate how ethical issues are framed by the public and various stakeholders in real-time, offering new avenues for understanding the societal shaping of bioethical dilemmas [1]. The following diagram outlines the workflow of a typical digital bioethics study.
Interdisciplinary Empirical Bioethics is a maturing field that systematically integrates social science research with normative analysis to address complex ethical challenges in science and medicine. Its strength lies in its methodological commitment to grounding ethical reflection in a deep understanding of real-world contexts, stakeholder experiences, and empirical facts. While theoretical frameworks like Kon's hierarchy and the Mapping-Framing-Shaping process provide structure, the field's vitality comes from its practical, method-driven approach. The ongoing development of detailed protocols, together with the critical adoption of novel methods from fields like computational social science, ensures that IEB will continue to enhance the relevance, rigor, and impact of bioethics research. For researchers and drug development professionals, engaging with these methodologies offers a powerful means to ensure that ethical guidance is not only philosophically sound but also practically applicable and responsive to the complexities of modern science and healthcare.
Empirical bioethics has emerged as a critical interdisciplinary field that integrates empirical research with normative analysis to address complex ethical challenges in healthcare and biomedicine [2]. This field navigates the traditional philosophical tension between "is" (empirical facts) and "ought" (ethical norms) by developing systematic approaches to connect descriptive research with normative conclusions [6] [10]. The growth of empirical methods in bioethics has been substantial, with one analysis of nine major bioethics journals demonstrating a significant increase in empirical research publications from 5.4% in 1990 to 15.4% in 2003 [11].
This application note presents a four-stage hierarchical model for conceptualizing and conducting empirical bioethics research. The framework progresses from fundamental descriptive studies through increasingly sophisticated research that directly engages with ethical norms [6]. For researchers and drug development professionals, this hierarchy provides a structured methodology for designing studies that effectively integrate empirical findings with ethical analysis, ensuring research remains both scientifically rigorous and ethically relevant.
The model addresses a fundamental challenge in interdisciplinary bioethics research: the need for clear methodologies that bridge the empirical-normative divide [2] [10]. By providing a structured pathway from observation to normative recommendation, the framework enables more systematic and transparent empirical bioethics research that can effectively inform both clinical practice and policy development in pharmaceutical and medical research.
Theoretical Framework: Competence and Research Progression
The Four Stages of Competence Learning Model
The psychological process of acquiring new skills through progressive stages provides a valuable framework for understanding research development in empirical bioethics. The Four Stages of Competence model, originally developed in the 1960s, describes the psychological states involved in progressing from incompetence to competence in any skill [12] [13]. This model comprises four distinct stages:
- Stage 1: Unconscious Incompetence - The individual does not understand or know how to do something and does not recognize the deficit
- Stage 2: Conscious Incompetence - Though the individual does not understand or know how to do something, they recognize the deficit and the value of new skills
- Stage 3: Conscious Competence - The individual understands or knows how to do something but requires conscious effort and concentration to execute the skill
- Stage 4: Unconscious Competence - The skill has become "second nature" and can be performed easily, often while executing another task [12] [14]
When applied to empirical bioethics research methodology, this competence model mirrors the researcher's journey from recognizing methodological limitations to achieving integrative mastery in combining empirical and normative approaches.
The Four-Stage Research Hierarchy
Parallel to the competence model, empirical bioethics research can be conceptualized through a four-stage hierarchical framework that progresses from basic description to normative engagement [6]. This research hierarchy provides a systematic approach to interdisciplinary inquiry:
- Stage 1: Lay of the Land - Foundational studies mapping current practices, opinions, beliefs, or status quo
- Stage 2: Ideal Versus Reality - Investigates the alignment between ethical ideals and actual clinical practice
- Stage 3: Improving Care - Develops and tests interventions to bridge gaps between ideal and actual practice
- Stage 4: Changing Ethical Norms - Synthesizes empirical findings to inform and potentially modify ethical norms [6]
The relationship between these frameworks can be visualized through the following competence-research alignment diagram:
Competence-Research Alignment Diagram
Quantitative Landscape of Empirical Bioethics Research
Growth of Empirical Research in Bioethics
The integration of empirical methods into bioethics has steadily increased over recent decades. Analysis of peer-reviewed literature reveals significant trends in publication patterns and methodological approaches. The following table summarizes the prevalence of empirical research in major bioethics journals between 1990-2003:
Table 1: Prevalence of Empirical Research in Bioethics Journals (1990-2003)
| Journal | Total Articles | Empirical Studies | Percentage | Primary Research Focus |
|---|---|---|---|---|
| Nursing Ethics | 367 | 145 | 39.5% | Clinical ethics, patient-provider relationships |
| Journal of Medical Ethics | 762 | 128 | 16.8% | Physician practices, institutional ethics |
| Journal of Clinical Ethics | 604 | 93 | 15.4% | Clinical decision-making, ethics consultation |
| Bioethics | 333 | 22 | 6.6% | Theoretical empirical integration |
| Cambridge Quarterly of Healthcare Ethics | 287 | 19 | 6.6% | Healthcare policy, organizational ethics |
| Hastings Center Report | 487 | 10 | 2.1% | Policy analysis, ethical frameworks |
| Theoretical Medicine and Bioethics | 287 | 9 | 3.1% | Methodological discussions |
| Kennedy Institute of Ethics Journal | 287 | 6 | 2.1% | Philosophical bioethics |
| Christian Bioethics | 287 | 3 | 1.0% | Religious perspectives in bioethics |
| Total/Average | 4029 | 435 | 10.8% |
Data adapted from [11]
The period from 1997-2003 showed a statistically significant increase (χ² = 49.0264, p<.0001) in empirical studies (n=309) compared to 1990-1996 (n=126) [11]. This trend has likely continued, reflecting growing acceptance of empirical approaches in bioethics.
Methodological Approaches and Research Topics
Empirical bioethics research employs diverse methodological approaches, with particular dominance of certain paradigms and subject areas:
Table 2: Methodological Approaches and Research Topics in Empirical Bioethics
| Research Characteristic | Frequency | Percentage | Notes |
|---|---|---|---|
| Methodological Paradigm | |||
| Quantitative Methods | 281 | 64.6% | Surveys, structured observations |
| Qualitative Methods | 154 | 35.4% | Interviews, focus groups, ethnography |
| Primary Research Subjects | |||
| Healthcare Providers | 187 | 43.0% | Physicians, nurses, other clinicians |
| Patients | 153 | 35.2% | Patients, family members |
| Policy-makers/Institutions | 95 | 21.8% | Administrators, policy documents |
| Primary Research Topics | |||
| Prolongation of Life and Euthanasia | 68 | 15.6% | End-of-life decision making |
| Informed Consent | 59 | 13.6% | Consent processes, understanding |
| Patient Autonomy and Rights | 57 | 13.1% | Decision-making, preferences |
| Research Ethics | 49 | 11.3% | IRB processes, participant protection |
| Professional Ethics | 47 | 10.8% | Codes of conduct, professionalism |
| Resource Allocation | 42 | 9.7% | Priority setting, rationing |
Data synthesized from [11]
Most empirical studies (64.6%) employed quantitative methodologies, while qualitative approaches accounted for 35.4% of studies [11]. This distribution reflects different epistemological traditions and research questions within the field.
Stage 1: Lay of the Land Research
Protocol for Descriptive Foundational Studies
Objective: To establish baseline understanding of current practices, opinions, beliefs, or behaviors related to a specific bioethical issue.
Methodology:
- Research Design: Cross-sectional surveys, systematic documentation, qualitative interviews, or observational studies
- Sampling Strategy: Purposeful or representative sampling of relevant stakeholders (patients, providers, administrators)
- Data Collection: Structured instruments (surveys, questionnaires) or semi-structured approaches (interview guides, observation protocols)
- Analysis Plan: Descriptive statistics for quantitative data; thematic analysis for qualitative data
Application Example: Mapping hospital ethics committee composition and function through structured surveys of committee chairs and members [6]. This research documents variation in committee structure, case volume, consultation processes, and policy development roles.
Key Outputs:
- Baseline data on current states and practices
- Identification of patterns and variations
- Foundation for subsequent hypothesis-driven research
Implementation Framework
The workflow for Stage 1 research follows a systematic process from conceptualization to dissemination:
Stage 1 Research Workflow
Stage 2: Ideal Versus Reality Research
Protocol for Gap Analysis Studies
Objective: To assess the alignment between accepted ethical ideals/norms and actual clinical or research practices.
Methodology:
- Research Design: Comparative analysis, audit studies, or mixed-methods approaches
- Normative Framework Identification: Explicit statement of ethical norms or ideals being evaluated
- Data Collection: Direct observation, chart review, or participant reporting of actual practices
- Analysis Plan: Comparison between ideal standards and observed practices with gap characterization
Application Example: Investigating disparities in healthcare delivery by comparing treatment patterns across racial, ethnic, or socioeconomic groups [6]. This research begins with the ethical premise of equitable care and measures deviations from this ideal.
Key Outputs:
- Documentation of practice-norm misalignments
- Quantification of implementation gaps
- Identification of systemic barriers to ethical practice
Implementation Framework
Stage 2 research requires parallel tracking of normative standards and empirical observations:
Stage 2 Research Workflow
Stage 3: Improving Care Research
Protocol for Intervention Studies
Objective: To develop and evaluate interventions that bridge identified gaps between ethical ideals and clinical reality.
Methodology:
- Research Design: Interventional studies, quality improvement initiatives, or implementation science approaches
- Intervention Development: Co-design with stakeholders based on Stage 2 findings
- Evaluation Framework: Mixed-methods assessment of process and outcome measures
- Analysis Plan: Pre-post comparisons, comparative effectiveness, or process evaluation
Application Example: Designing and testing enhanced consent processes for clinical research participation that address previously identified deficiencies in subject comprehension [6]. This directly addresses the gap between the ideal of informed consent and actual understanding.
Key Outputs:
- Tested interventions for improving ethical practice
- Implementation strategies for ethical ideals
- Evidence for practice change initiatives
Stage 4: Changing Ethical Norms Research
Protocol for Normative-Integrative Studies
Objective: To synthesize empirical findings from multiple studies to inform, refine, or potentially modify ethical norms and principles.
Methodology:
- Research Design: Systematic integration, meta-ethnography, or reflective equilibrium approaches
- Data Synthesis: Aggregation of empirical findings across related studies
- Normative Analysis: Critical evaluation of existing ethical frameworks in light of empirical evidence
- Integration Method: Explicit methodology for moving from empirical findings to normative conclusions
Application Example: Reconsidering autonomy frameworks in chronic illness management based on cumulative empirical findings about patient preferences, decision-making patterns, and relational dynamics in ongoing care [2] [10].
Key Outputs:
- Refined ethical frameworks or principles
- Evidence-informed normative recommendations
- Revised practice guidelines or policies
Integration Methodologies
Stage 4 research requires sophisticated integration of empirical and normative approaches, with several methodological options available:
Table 3: Integration Methodologies for Empirical Bioethics Research
| Methodology | Description | Application Context | Key Considerations |
|---|---|---|---|
| Reflective Equilibrium | Back-and-forth process between ethical principles and empirical data to achieve coherence [2] | Individual researcher analysis; theoretical refinement | Requires transparency about weighting of different elements |
| Dialogical Empirical Ethics | Structured dialogue between researchers and stakeholders to develop shared understanding [2] | Practice guideline development; policy formation | Demands skilled facilitation and representative participation |
| Ground Moral Analysis | Iterative process of data collection and normative analysis to develop contextually grounded recommendations [2] | Emerging ethical issues; novel technologies | Time-intensive; requires interdisciplinary team |
| Symbiotic Ethics | Integration of empirical and normative elements throughout research process [2] | Complex practice environments; organizational ethics | Challenges traditional research boundaries |
Researchers report that the most contested objectives in empirical bioethics are "striving to draw normative recommendations" and "developing and justifying moral principles," while "understanding the context of a bioethical issue" and "identifying ethical issues in practice" receive nearly unanimous support [10]. This reflects both methodological challenges and disciplinary tensions within the field.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Methodological Resources for Empirical Bioethics Research
| Research Component | Essential Tools & Methods | Function | Example Applications |
|---|---|---|---|
| Study Design | Mixed-methods frameworks, Case study protocols, Comparative analysis templates | Enables comprehensive approach to complex questions | Integrating quantitative practice data with qualitative experience data |
| Data Collection | Validated survey instruments, Semi-structured interview guides, Systematic observation protocols | Ensures reliable and valid data collection | Assessing quality of life; exploring decision-making experiences |
| Normative Framework | Ethical principle checklists, Deliberative frameworks, Case analysis templates | Provides structure for ethical analysis | Applying four-principles approach; utilizing casuistry methods |
| Integration Methodology | Reflective equilibrium protocols, Dialogical procedure guides, Interdisciplinary team facilitation methods | Supports systematic empirical-normative integration | Translating patient preference data into practice recommendations |
| Analysis Tools | Qualitative analysis software (NVivo, MAXQDA), Statistical packages (R, SPSS), Ethical analysis frameworks | Facilitates robust data analysis and interpretation | Identifying themes in interview data; testing associations in survey data |
Integrated Research Workflow Protocol
The complete four-stage research process can be implemented through the following comprehensive workflow:
Comprehensive Four-Stage Research Workflow
This integrated protocol provides researchers with a systematic approach to addressing bioethical issues through sequential, cumulative stages of inquiry. Each stage builds upon the previous one, creating a comprehensive evidence base for ethical analysis and decision-making.
For drug development professionals and researchers, this framework offers a structured methodology for investigating ethical dimensions of pharmaceutical research, clinical trials, and therapeutic implementation. By progressing through these stages, research teams can ensure their empirical bioethics work progresses from basic understanding to meaningful impact on ethical practice and policy.
Application Notes: Integrating Empirical Data and Normative Analysis
The Challenge of Integration in Empirical Bioethics
Empirical bioethics constitutes an interdisciplinary endeavor that centers on integrating empirical findings with normative, philosophical analysis [2]. This integration is crucial for addressing the complexity of human practices in healthcare and biological sciences, moving beyond purely philosophical approaches that may lack contextual sensitivity [15] [2]. The fundamental challenge lies in successfully merging social scientific, empirical data with philosophical analysis to generate normatively sound and practically applicable conclusions [15].
Despite consensus that empirical research is relevant to bioethical argument, integrating empirical research with normative analysis remains methodologically challenging [2]. A systematic review has identified at least thirty-two distinct methodologies for integration, reflecting both the richness and uncertainty within the field regarding aims, content, and domain of application [2]. Many researchers report an "air of uncertainty and overall vagueness" surrounding integration methods, which represents a double-edged sword—allowing flexibility while potentially obscuring a lack of methodological understanding [2].
Methodological Approaches to Integration
Table 1: Primary Methodological Approaches for Empirical-Normative Integration
| Method Category | Key Characteristics | Representative Methods | Primary Applications |
|---|---|---|---|
| Consultative | Researcher as external thinker analyzing data independently to develop normative conclusions | Reflective Equilibrium, Reflexive Balancing | Issues requiring coherentist moral justification; theoretical analysis of empirical data |
| Dialogical | Reliance on stakeholder dialogue to reach shared understanding of analysis and conclusions | Inter-ethics, Dialogical Empirical Ethics | Clinical ethics support; policy development; stakeholder engagement contexts |
| Inherent Integration | Normative and empirical components intertwined from research project inception | Grounded Moral Analysis, Symbiotic Ethics | Exploratory research; contexts where normative frameworks emerge from empirical data |
Quantitative Data Presentation in Comparative Studies
Effective presentation of quantitative data is essential for empirical bioethics research that incorporates comparative studies. The following table demonstrates proper summarization of quantitative variables across different groups:
Table 2: Exemplary Quantitative Data Summary for Group Comparisons
| Group | Mean | Standard Deviation | Sample Size (n) | Median | Interquartile Range (IQR) |
|---|---|---|---|---|---|
| Group A | 2.22 | 1.270 | 14 | 1.70 | 1.50 |
| Group B | 0.91 | 1.131 | 11 | 0.60 | 0.85 |
| Difference | 1.31 | N/A | N/A | 1.10 | N/A |
When comparing quantitative variables between groups, researchers should calculate differences between means and/or medians, while recognizing that standard deviation and sample size metrics do not apply to these difference measurements [16]. Appropriate visualization methods include back-to-back stemplots for small datasets with two groups, 2-D dot charts for small to moderate amounts of data across multiple groups, and boxplots for larger datasets [16].
Experimental Protocols for Empirical Bioethics Research
Comprehensive Research Protocol Template
A robust protocol template suitable for empirical bioethics investigations must accommodate the epistemological and methodological frameworks specific to humanities and social sciences in the health domain [7] [17]. The following protocol structure has been specifically adapted for empirical bioethics research:
Table 3: Core Protocol Template for Empirical Bioethics Research
| Section | Key Components | Considerations for Empirical Bioethics |
|---|---|---|
| Title & Identification | Nature of study, approach, data collection methods | Clearly identify as empirical bioethics; specify interdisciplinary nature |
| Administrative Information | Sponsors, investigators, research teams | Include ethics committee/IRB details; specify interdisciplinary team composition |
| Study Summary | Context, primary objective, general method | Articulate both empirical and normative dimensions concisely |
| Problem & Objectives | Problem significance, literature, specific research questions | Frame to demonstrate need for empirical-normative integration |
| Disciplinary & Paradigmatic Framework | Disciplinary field, research paradigm, theoretical framework | Explicitly state methodological framework (qualitative/quantitative/mixed) and theoretical framework (e.g., principlism) |
| Methodological Details | Site, duration, participant characteristics, sampling, data collection | Justify participant sampling; specify empirical methods and normative analysis approach |
| Ethical Considerations | Consent procedures, information notices, data protection | Adapt consent approaches (implicit/explicit, oral/written) based on study context; balance autonomy with methodological needs |
Data Collection and Processing Protocols
For data collection in empirical bioethics, researchers should specify the types of data collected, procedures, instruments (interview guides, questionnaires), and equipment used [7]. The protocol should address whether any changes in instruments might occur during the study and whether public members will participate in the process [7].
Data processing, storage, protection, and confidentiality procedures require particular attention in empirical bioethics [17]. Rather than imposing excessive anonymization that might limit analytical depth, responsible pseudonymization is often more appropriate, particularly when working with qualitative data from semi-directed interviews or open-ended questionnaires that may require follow-up data collection [17].
Integration Methodology Protocol
The integration of empirical findings with normative analysis represents the core methodological challenge in empirical bioethics. Researchers must transparently document their approach to integration:
The Scientist's Toolkit: Essential Research Reagents for Empirical Bioethics
Table 4: Essential Methodological Resources for Empirical Bioethics Research
| Research 'Reagent' | Function/Application | Implementation Considerations |
|---|---|---|
| Critical Realism Framework | Philosophical foundation for integrating empirical data with philosophical analysis | Provides mature interdisciplinary approach; addresses fact-value distinction [15] |
| Reflective Equilibrium Methodology | Structured approach for back-and-forth dialogue between ethical principles and empirical data | Enables researcher to achieve moral coherence between normative underpinnings and empirical facts [2] |
| Standardized Protocol Templates | Adapted research protocols for humanities and social sciences in health | Based on SRQR standards but modified for quantitative, qualitative, and mixed methods [7] [17] |
| Dialogical Integration Methods | Facilitates stakeholder collaboration in normative analysis | Particularly valuable when multiple perspectives essential to ethical analysis [2] |
| Adapted Consent Procedures | Flexible informed consent approaches specific to empirical ethics contexts | Balances methodological needs with ethical requirements; considers implicit/oral consent where appropriate [17] |
| Empirical Data Collection Instruments | Interview guides, questionnaires, observation protocols | Must be designed to minimize bias from prior information while maintaining ethical standards [17] |
Implementation Framework and Best Practices
Professional Standards and Quality Assessment
The development of professional standards in empirical bioethics remains contested, with ongoing debates about what constitutes expertise in this interdisciplinary field [18]. Suggested criteria for quality empirical bioethics research include:
- Understanding and executing appropriate empirical and analytic methods [18]
- Awareness of relevant standards and requirements for bioethics research and related disciplines [18]
- Contextualizing findings in relation to further important ethical questions [18]
Peer review processes serve as a primary mechanism for quality assessment, though limitations exist due to varied reviewer attitudes, diverse publication genres within bioethics, and the absence of an established canon of literature against which standards could be judged [18].
Ethical Considerations in Empirical Bioethics Protocols
Ethical review of empirical bioethics research requires special consideration of several factors that distinguish it from biomedical research. The physical or mental health risks to participants are generally small or nonexistent, at least in the domain of empirical bioethics [17]. This risk profile allows for adaptations to standard ethical requirements:
Information notices that are too exhaustive or oriented may influence participant behavior or responses, potentially increasing study bias and decreasing result pertinence [17]. Written consent may be difficult or inappropriate to obtain systematically, particularly in qualitative approaches such as non-participant observations in hospital settings [17]. Excessive anonymization requirements may limit researchers' ability to deepen certain imperative analyses, particularly with qualitative data from interviews or open-ended questionnaires [17].
These considerations support a case-by-case contextualization approach that does not ignore fundamental research policies, standards, and legislations, but adapts them to the specific methodological requirements of empirical bioethics research [17].
Empirical bioethics is an interdisciplinary field that integrates empirical research findings with normative philosophical analysis to address complex ethical challenges in healthcare and scientific research [2]. This hybrid approach recognizes that a purely theoretical ethical analysis is often insufficient for grappling with the nuanced realities of human practices in medicine and scientific investigation [2]. The growing consensus in the field indicates that empirical evaluations alone cannot ensure that practices in areas such as eHealth and neurotechnology are ethically sound, necessitating the integration of robust ethical frameworks into research design and implementation [19] [20]. This document provides detailed application notes and experimental protocols for implementing four dominant ethical theories—utilitarianism, deontology, principlism, and virtue ethics—within interdisciplinary empirical bioethics research, with particular emphasis on contexts relevant to researchers, scientists, and drug development professionals.
Table 1: Core Ethical Theories in Empirical Bioethics Research
| Ethical Theory | Central Principle | Primary Advocates | Key Strengths | Major Limitations |
|---|---|---|---|---|
| Utilitarianism | Maximize overall happiness/utility; greatest good for greatest number | Jeremy Bentham, John Stuart Mill [21] | Provides clear framework for resource allocation; emphasizes measurable outcomes | Can justify sacrificing minority interests; requires difficult utility calculations [21] |
| Deontology | adherence to moral rules and duties; actions inherently right or wrong | Immanuel Kant [22] | Protects individual rights and autonomy; provides consistent moral framework | Can lead to rigid outcomes that ignore consequences; may conflict with pragmatic solutions [22] |
| Principlism | Balance of four core principles: autonomy, beneficence, non-maleficence, justice | Beauchamp and Childress [23] | Flexible framework for clinical ethics; comprehensive consideration of moral dimensions | Lacks hierarchical structure; principles may conflict without resolution method [23] |
| Virtue Ethics | Cultivation of moral character and virtues in practitioners | Aristotle [23] [24] | Focuses on moral motivation and character; emphasizes practical wisdom | Less specific action guidance; challenges in assessing virtuous qualities [24] |
Theoretical Foundations and Research Applications
Utilitarian Ethics: Consequentialist Framework
Utilitarianism is a consequentialist ethical theory that posits the morality of actions should be judged solely by their consequences, with the goal of achieving the greatest balance of good over bad consequences for the greatest number of people [21]. In its modern applications, utilitarianism provides a vibrant moral resource for contemporary bioethics, particularly in contexts requiring resource allocation and public health policy decisions [21]. Unlike deontological approaches, utilitarian ethics judges acts exclusively on the basis of their outcomes, seeking to maximize either happiness, pleasure, or other specified utilities depending on the particular variant endorsed [21].
Within research environments, utilitarianism provides a structured approach for evaluating the potential benefits and harms of studies involving human participants, particularly when dealing with scarce resources or when research might impose burdens on some individuals while generating knowledge that benefits many others [21]. However, critics have highlighted significant limitations, including the theory's potential to justify the sacrifice of minority interests for the greater good and the challenge of making accurate utility calculations in morally pluralistic societies where definitions of "good" consequences may vary substantially [21]. The theory has also been criticized for creating emotional distance between researchers and participants by reducing ethical decisions to mathematical calculations [21].
Deontological Ethics: Duty-Based Framework
Deontology, derived from the Greek "deont" meaning "that which is binding," is an ethical approach centered on rules and professional duties, most famously associated with the German philosopher Immanuel Kant (1724-1804) [22]. Kantian deontology stems from the belief that humans possess the ability to reason and understand universal moral laws applicable across situations [22]. Unlike consequentialist approaches, deontology does not focus on the outcomes of individual actions but rather on the intent behind chosen actions and their adherence to moral principles [22].
Kant divided deontological beliefs between hypothetical and categorical imperatives, with the latter representing unconditional moral absolutes [22]. One of Kant's most famous categorical imperatives requires that individuals never treat people solely as a means to an end, emphasizing respect for each individual's unique worth and dignity [22]. In healthcare contexts, Kantian deontology would strongly emphasize truth-telling, full disclosure of medical errors, and respect for patient autonomy, regardless of potential negative consequences that might result from these actions [22]. This stands in direct contrast to utilitarian approaches that might justify withholding information if it produced better overall outcomes [22].
Principlism: Bridging Theory and Practice
Principlism represents a pluralistic approach to bioethics that balances multiple mid-level principles rather than deriving moral guidance from a single overarching theoretical foundation [23]. This framework dominates contemporary clinical ethics and medical education, offering a structured yet flexible approach to ethical decision-making [23] [24]. The framework incorporates four core principles: respect for autonomy (honoring an individual's right to make informed decisions about their own healthcare), beneficence (the obligation to act in the patient's best interest and promote well-being), non-maleficence (the commitment to "do no harm" and avoid causing unnecessary injury or suffering), and justice (ensuring fairness in the distribution of healthcare resources and treatments) [23].
In research contexts, principlism provides a comprehensive checklist of ethical considerations that must be balanced when designing and implementing studies [23]. For example, in eHealth evaluation research, principlism helps researchers navigate tensions between promoting innovative care (beneficence) and ensuring equitable access to technology (justice) [19]. The approach is particularly valuable in interdisciplinary empirical bioethics because it offers a shared vocabulary and structured framework that team members from different backgrounds can apply to complex ethical dilemmas without requiring deep philosophical expertise [23].
Virtue Ethics: Character-Based Framework
Virtue ethics represents a character-based approach to morality that centers on the moral agent rather than specific actions or their consequences [23]. Originating from Aristotelian philosophy, this perspective emphasizes the cultivation of virtuous character traits such as compassion, honesty, and practical wisdom [23] [24]. In bioethical contexts, virtue ethics encourages healthcare professionals and researchers to develop these moral virtues as guides for ethical behavior in practice [23].
Recent applications in neuroethics research have argued for integrating virtue ethics to address ethical challenges in cutting-edge brain research, emphasizing the development of "moral sensitivities, practical reasoning skills, and other ethical competencies" rather than relying solely on regulations and rules [20]. This approach is particularly valuable for navigating complex conflicts of interest and promoting collaborative ethical deliberation among researchers, ethicists, and participants [20]. In medical ethics education, virtue ethics is increasingly incorporated through a hybrid approach that combines principlist methodologies with virtue cultivation, using tools such as exemplars and case-based learning to foster both moral knowledge and character development [24].
Table 2: Research Applications of Ethical Frameworks in Empirical Bioethics
| Research Context | Utilitarian Approach | Deontological Approach | Principlist Approach | Virtue Ethics Approach |
|---|---|---|---|---|
| eHealth Evaluation | Focus on maximizing population health benefits through technology implementation [19] | Emphasis on truth-telling and full disclosure of technology limitations [22] | Balancing patient autonomy, beneficence, and justice in technology access [19] | Cultivating honesty and integrity in reporting both positive and negative outcomes [20] |
| Invasive Neurotechnology Research | Weighing potential knowledge benefits against risks to participants [20] | Strict adherence to informed consent protocols and never using participants merely as means [22] [20] | Ensuring equitable participant selection (justice) while minimizing harm (non-maleficence) [23] | Developing researchers' moral character to navigate complex conflicts of interest [20] |
| Pharmaceutical Drug Development | Prioritizing research on diseases affecting largest populations [21] | Absolute duty to disclose all trial results, including unfavorable findings [22] | Balancing access to experimental drugs (autonomy) with safety protections (non-maleficence) [23] | Fostering compassion and scientific integrity throughout development process [24] |
| Rare Disease Therapy Development | Allocating resources to interventions with greatest overall health utility [21] | Duty to provide research opportunities for all patient groups regardless of size [22] | Special consideration of justice implications for orphan drug development [23] | Cultivating perseverance and commitment to underserved patient populations [25] |
Experimental Protocols for Ethical Integration
Protocol 1: Reflective Equilibrium for Empirical Bioethics Integration
The reflective equilibrium method represents a systematic approach to integrating empirical findings with normative analysis through iterative deliberation [2]. This protocol adapts the methodology for interdisciplinary research teams in empirical bioethics.
Objective: To achieve coherence between empirical data, ethical principles, and considered moral judgments through a structured reflective process.
Materials Required:
- Empirical research data (qualitative or quantitative)
- Documentation of initial ethical positions
- Framework of relevant ethical principles/theories
- Recording device or notebook for process documentation
Procedure:
- Initial Position Mapping: Research team members individually document their initial ethical judgments about the research dilemma based on intuition and preliminary understanding.
- Principle Formulation: Identify relevant ethical principles and theories applicable to the dilemma, with explicit justification for their selection.
- Data Integration: Systematically compare empirical findings with identified principles, noting areas of alignment and tension.
- Iterative Adjustment: Engage in reflective deliberation to adjust either principles or judgments to achieve greater coherence.
- Equilibrium Achievement: Document the point at which researchers reach a stable equilibrium between principles, judgments, and empirical data.
- Resolution Documentation: Create a comprehensive record of the reflective process, including all adjustments and final normative conclusions.
Validation Method: Peer review by interdisciplinary ethics advisory board to assess coherence and justification of the resulting ethical position.
Expected Timeline: 4-6 weeks for complete process, depending on complexity of ethical dilemma.
Protocol 2: Dialogical Empirical Ethics for Stakeholder Engagement
Dialogical empirical ethics emphasizes collaborative sense-making through structured dialogue between researchers and stakeholders [2]. This approach is particularly valuable for addressing ethical aspects in emerging technologies like eHealth and neurotechnology.
Objective: To co-construct ethical guidance through deliberative dialogue that incorporates diverse stakeholder perspectives.
Materials Required:
- Trained facilitator with ethics expertise
- Diverse stakeholder participants (researchers, patients, clinicians, community representatives)
- Recording and transcription equipment
- Ethical framework guide
- Anonymous voting technology
Procedure:
- Stakeholder Mapping: Identify and recruit relevant stakeholders representing all affected parties.
- Pre-Dialogue Assessment: Administer survey to assess initial ethical positions and concerns.
- Structured Dialogue Sessions:
- Session 1: Case presentation and initial reactions
- Session 2: Ethical principle identification and application
- Session 3: Deliberation on points of disagreement
- Session 4: Consensus-building on ethical recommendations
- Data Analysis: Thematic analysis of dialogue transcripts to identify key ethical considerations.
- Recommendation Formulation: Co-create ethically justified recommendations for practice.
- Implementation Planning: Develop strategy for integrating ethical recommendations into research practice.
Validation Method: Member checking with participants to ensure accurate representation of dialogue and consensus.
Expected Timeline: 8-10 weeks for complete dialogue process and analysis.
Integration Workflow Visualization
Empirical Bioethics Integration Workflow
Research Reagent Solutions: Ethical Analysis Toolkit
Table 3: Essential Methodological Tools for Empirical Bioethics Research
| Tool Category | Specific Method/Instrument | Primary Function | Application Context |
|---|---|---|---|
| Data Collection Instruments | Semi-structured interview guides | Gather rich qualitative data on stakeholder moral experiences | Understanding researcher perspectives on ethical challenges in neurotechnology [20] |
| Ethical Analysis Frameworks | Principlism checklist | Systematic application of four core principles to ethical dilemmas | Clinical ethics consultation and research ethics review [23] |
| Integration Methodologies | Wide reflective equilibrium | Achieve coherence between empirical data and ethical principles | Bridging empirical findings and normative analysis in bioethics research [2] |
| Deliberative Processes | Structured stakeholder dialogues | Facilitate collaborative ethical sense-making among diverse stakeholders | Addressing ethical aspects in eHealth evaluation research [19] [2] |
| Educational Resources | AI-assisted virtue cultivation tools | Develop moral sensitivity and practical wisdom through exemplars | Medical ethics education for students and researchers [24] |
| Validation Instruments | Interdisciplinary peer review | Ensure robustness and justification of ethical conclusions | Quality assessment in empirical bioethics research publications [2] |
Implementation Guidelines and Case Applications
Case Application: Ethical Integration in eHealth Evaluation Research
The protocol for examining ethical aspects in eHealth evaluation research demonstrates the practical integration of ethical frameworks into empirical research design [19]. This scoping review protocol systematically investigates how ethical considerations are addressed in original studies evaluating remote patient monitoring (RPM) applications for cancer and cardiovascular diseases [19]. The protocol employs Joanna Briggs Institute methodology and PRISMA-ScR guidelines, implementing a comprehensive search strategy across multiple databases including MEDLINE, Embase, CINAHL, and Philosopher's Index [19].
The ethical analysis within this protocol focuses on two key domains: process domain ethical aspects (concerned with power distribution and value judgments in the research process) and outcome domain ethical aspects (addressing unintended consequences and dual uses of eHealth technologies) [19]. The protocol specifically examines how evaluation studies address issues such as health disparities, data security, and selection bias, with analysis applying inductive-deductive qualitative content analysis to map ethical considerations [19]. This approach enables the identification of opportunities for more holistic integration of ethics into eHealth evaluation practices and informs future practical guidance for researchers [19].
Implementation Framework for Neuroethics Research
Recent qualitative research with NIH BRAIN Initiative-funded investigators reveals the complex ethical challenges in invasive brain research with humans [20]. The study identifies two major themes: (1) the difficulty of navigating complex conflicts of interest arising from research funding, team structure, data collection and sharing obligations, commercialization, innovation, and the boundaries between research and care; and (2) the need for increased collaboration, community, and participation in neuroethics deliberation [20].
Based on these findings, researchers argue for a shift from focusing solely on ethical guidelines to promoting neuroethical competencies through virtue ethics integration [20]. The proposed implementation framework includes:
- Targeted neuroethics education that develops moral sensitivities and practical reasoning skills
- Opportunities for collective moral deliberation among researchers, ethicists, and participants
- Enhanced engagement practices that recognize researchers as unique stakeholders with significant agency and experiential knowledge [20]
This approach addresses limitations of principle-based and regulatory approaches alone by cultivating the moral character and virtues necessary to navigate ethical issues that emerge throughout the research lifecycle [20].
Protocol 3: Virtue Ethics Integration for Researcher Competency Development
This protocol outlines a structured approach to integrating virtue ethics into research team development, based on findings from neuroethics research demonstrating the value of moral competencies for navigating ethical challenges [20].
Objective: To cultivate neuroethical competencies among research team members through virtue ethics education and collective moral deliberation.
Materials Required:
- Case studies representing ethical challenges in specific research domain
- Exemplar narratives of ethical leadership in science
- Facilitated discussion guides
- Reflective journal templates
- Assessment rubrics for ethical competencies
Procedure:
- Pre-assessment: Evaluate team members' current ethical competencies and identified challenges.
- Exemplar Identification: Select and analyze exemplars of virtuous practice in relevant research contexts.
- Case-Based Deliberation: Engage team in structured analysis of ethical dilemmas using virtue framework.
- Moral Reflection: Implement regular reflective practice sessions for research team.
- Competency Development: Focus on cultivating specific virtues identified as essential for research context.
- Integration Planning: Develop strategies for applying virtuous practice to current research projects.
- Ongoing Support: Establish structures for continued ethical development and consultation.
Assessment Metrics:
- Pre/post self-assessment of ethical confidence
- Peer evaluation of collaborative ethical decision-making
- Documentation of ethical issues identified and addressed
- Reflection journal quality and depth
Implementation Timeline: 12-week intensive program with quarterly follow-up sessions.
The convergence of artificial intelligence (AI) with persistent global health disparities represents a critical frontier for empirical bioethics. This field, characterized by its integration of normative ethical analysis with empirical evidence, provides the essential framework for navigating the complex societal, technical, and ethical challenges of this era [26] [27]. The "empirical turn" in bioethics emphasizes that ethical deliberation must be grounded in the realities of how technologies are developed and how they impact diverse populations [27]. AI's rapid adoption in healthcare underscores an urgent need for this approach. While 88% of organizations report using AI in some business function, most remain in early experimental phases, and a significant 95% of generative AI pilot programs fail to deliver measurable revenue impact [28] [29]. Simultaneously, global health progress is faltering; global life expectancy fell by 1.8 years between 2019 and 2021, reversing a decade of gains and highlighting the vulnerability of health systems [30]. This article applies the lens of empirical bioethics to analyze these parallel challenges, proposing structured application notes and experimental protocols to guide researchers and drug development professionals in fostering equitable and ethically sound innovation.
Application Note 1: AI Adoption and Value Realization
Quantitative Landscape of AI Implementation
The current state of AI adoption is a paradox of widespread experimentation and scarce enterprise-wide value. The following table synthesizes key quantitative findings from recent global surveys.
Table 1: Key Quantitative Indicators of AI Adoption and Impact in 2025
| Indicator | Metric | Source |
|---|---|---|
| Overall AI Adoption | 88% of organizations report regular use in at least one business function [28]. | McKinsey Global Survey |
| Generative AI Pilot Success | Only 5% of generative AI pilot programs achieve rapid revenue acceleration [29]. | MIT NANDA Initiative |
| AI Agent Experimentation | 62% of organizations are at least experimenting with AI agents [28]. | McKinsey Global Survey |
| Enterprise-Level EBIT Impact | 39% of respondents attribute any level of EBIT impact to AI use [28]. | McKinsey Global Survey |
| Leading Driver for AI High Performers | 80% of companies set efficiency as an AI objective, but high performers prioritize growth and innovation [28]. | McKinsey Global Survey |
Protocol for Interdisciplinary AI Impact Assessment
This protocol is designed to evaluate the real-world impact and ethical implications of AI deployments in healthcare and research settings, aligning with empirical bioethics methodologies [26].
Protocol 1.1: Mixed-Methods AI Impact and Ethics Assessment
- Objective: To quantitatively measure AI implementation outcomes and qualitatively understand the associated ethical challenges and workforce perceptions.
- Materials:
- Data Integration Platform: Secure computing environment for aggregating pre- and post-AI implementation performance metrics (e.g., process efficiency, diagnostic accuracy).
- Structured Interview Guides: Semi-guided questionnaires for leadership, focusing on strategic objectives and perceived value [28] [29].
- Focus Group Frameworks: Discussion guides for line managers and end-users to explore workflow changes, trust, and accountability.
- Bias Audit Toolkit: Software for running statistical analyses on AI model outputs across different demographic subgroups [31] [32].
- Procedure:
- Baseline Measurement: Establish key performance indicators (KPIs) prior to AI integration. Examples include time-to-completion for target tasks, error rates, and resource costs.
- Post-Implementation Measurement: Collect the same KPI data after a minimum of two full operational cycles with the AI tool.
- Stakeholder Engagement:
- Conduct individual interviews with senior leaders to understand strategic drivers.
- Facilitate focus groups with operational staff to gather lived experiences of AI integration.
- Ethical Scrutiny and Bias Audit: Apply the bias audit toolkit to the AI system using a hold-out dataset or simulated cases to test for discriminatory performance patterns.
- Data Triangulation: Integrate quantitative performance data with qualitative thematic analysis from interviews and focus groups. The normative ethical analysis, central to bioethics, is applied here to evaluate findings against principles of justice, fairness, and accountability.
- Output: A comprehensive report detailing quantitative ROI, qualitative insights into organizational disruption, and an ethical impact assessment with recommendations for mitigation.
Visualizing the AI Integration Workflow
The following diagram outlines the core workflow for a responsible AI implementation and assessment, a process that should be iterative and guided by ethical principles.
Application Note 2: AI and Global Health Equity
Quantitative Landscape of Health Disparities and AI Exclusion
The promise of AI in healthcare is starkly contrasted by the reality of global health disparities and the risk of technological exclusion. The data reveals a pressing challenge.
Table 2: Health Disparities and AI Exclusion Risks in 2025
| Category | Metric | Source |
|---|---|---|
| Global Health Setbacks | Global life expectancy fell by 1.8 years between 2019-2021 [30]. | World Health Statistics |
| Maternal Health in Crises | 60% of preventable maternal deaths occur in displacement settings [33]. | Project HOPE |
| AI Diagnostic Bias | Algorithmic bias can lead to 17% lower diagnostic accuracy for minority patients [32]. | ScienceDirect Review |
| Genomic Data Gap | >80% of genetics studies include people of European descent (<20% of global population) [31]. | Deutsche Welle / WEF |
| Digital Divide | 29% of rural adults are excluded from AI-enhanced healthcare tools [32]. | ScienceDirect Review |
| Scale of Exclusion | AI in healthcare risks excluding nearly 5 billion people in low and middle-income countries [31]. | World Economic Forum |
Protocol for Equity-Centric AI Development and Validation
This protocol provides a methodology for developing and validating AI health tools with equity as a core objective, directly addressing the data biases and exclusion risks identified above.
Protocol 2.1: Co-Design and Equity Validation for AI Health Tools
- Objective: To create and validate AI-powered health tools that are effective across diverse genetic, environmental, and demographic populations.
- Materials:
- Diverse Data Repositories: Curated datasets from multiple global regions, ensuring representation of different genetic backgrounds, skin tones, and disease presentations [31] [32].
- Community Engagement Panel: A structured group of stakeholders, including community health workers, patient advocates, and local ethicists from target populations.
- Model Validation Suite: A standardized set of test cases covering a wide spectrum of demographic and clinical scenarios.
- Digital Literacy Materials: Culturally and linguistically appropriate resources to facilitate informed consent and tool usage.
- Procedure:
- Problem Scoping with Communities: Convene the community engagement panel at the outset to define the health priority and design parameters, ensuring the tool addresses a locally relevant need.
- Federated Learning & Data Sourcing: Procure diverse training data. Where data sovereignty is a concern, employ federated learning techniques that train algorithms across multiple decentralized data sources without transferring the data itself.
- Iterative Co-Design Prototyping: Develop initial prototypes and present them to the community panel for feedback on usability, cultural appropriateness, and integration into local workflows.
- Rigorous Equity-Centered Validation: Test the final model using the validation suite. Performance metrics (e.g., sensitivity, specificity) must be disaggregated and reported by subgroup (e.g., ethnicity, gender, geographic location) to identify any performance gaps.
- Implementation with Support: Deploy the tool alongside the necessary digital literacy training for both providers and patients, and with a plan for ongoing monitoring and maintenance.
- Output: An AI health tool documented with performance metrics across diverse subgroups, a report on the co-design process, and implementation guidelines for low-resource settings.
Visualizing the Equity-Centric AI Development Pathway
An equity-first approach requires a fundamental shift in the development lifecycle, as illustrated in the following pathway.
The Scientist's Toolkit: Research Reagent Solutions
For researchers embarking on the empirical bioethics studies and technical developments outlined in these protocols, the following toolkit details essential "research reagents" – the conceptual frameworks and practical resources required.
Table 3: Essential Research Reagent Solutions for Interdisciplinary Bioethics Research
| Item | Function & Application |
|---|---|
| Empirical Bioethics Methodology [26] [27] | The core framework for integrating descriptive empirical research (e.g., surveys, interviews) with normative ethical analysis. It provides the philosophical grounding for the entire research process. |
| Stakeholder Engagement Panel | A pre-recruited and structured group of community representatives, patients, and end-users. Its function is to provide grounded, lived-experience input throughout the technology development lifecycle, from scoping to validation (Protocol 2.1). |
| Bias Audit Toolkit [31] [32] | A suite of software and statistical measures (e.g., fairness metrics, disparate impact analysis) used to proactively identify and quantify algorithmic bias in AI models against protected or underrepresented subgroups. |
| Mixed-Methods Data Collection Instruments | Validated questionnaires, structured interview guides, and focus group protocols. Their function is to systematically gather both quantitative performance data and qualitative perceptual data for triangulation (Protocol 1.1). |
| Federated Learning Infrastructure | A distributed machine learning approach that allows for model training on data that remains in its original location. Its function is to enable the use of diverse datasets while respecting data privacy and sovereignty regulations [31]. |
Synthesis and Forward-Looking Perspective
The interplay between the sluggish, often unsuccessful adoption of AI and the persistent crisis of global health disparities reveals a common root: a lack of deep, integrative, and ethically attuned implementation. The quantitative data shows that high-performing organizations succeed by embedding AI into redesigned workflows and pursuing growth and innovation, not just efficiency [28]. Similarly, overcoming health equity challenges requires more than just advanced algorithms; it demands intentional co-design, investment in local digital infrastructure, and the creation of fair governance frameworks [31] [32]. The empirical bioethics approach is not merely an academic exercise; it is a practical necessity. It provides the methodological rigor to move from simply identifying these complex problems to developing and testing actionable, evidence-based solutions. For researchers and drug development professionals, the path forward lies in embracing this interdisciplinary ethos, ensuring that the powerful drivers of AI and biomedical innovation are steered by a commitment to justice, equity, and tangible human benefit.
The Integrative Toolkit: Methodologies for Combining Empirical Research and Ethical Analysis
Empirical bioethics is an interdisciplinary endeavor that seeks to integrate empirical data with normative analysis to address bioethical questions [34]. Within this field, consultative models represent a distinct methodological approach where the researcher acts as an external thinker who analyzes empirical data and ethical theory independently to develop normative conclusions [2]. This contrasts with dialogical models that rely on direct stakeholder dialogue to reach shared understanding [2]. The consultative approach is particularly valuable when research requires specialized ethical expertise or when dealing with sensitive topics where direct stakeholder engagement may be impractical or ethically problematic.
The systematic review by Davies et al. identified 32 distinct empirical bioethics methodologies, with consultative models representing a significant proportion of these approaches [34]. These methodologies share a common characteristic: the researcher maintains responsibility for the integrative process, systematically moving between empirical findings and normative frameworks to arrive at justified ethical conclusions. This paper provides application notes and protocols for implementing one prominent consultative methodology—Reflective Equilibrium—within interdisciplinary empirical bioethics research, with particular attention to contexts relevant to drug development professionals and clinical researchers.
Theoretical Foundations of Reflective Equilibrium
Conceptual Framework
Reflective Equilibrium (RE), particularly in its "wide" form, is a method of moral justification that seeks coherence among different types of moral considerations [35]. Originally developed by John Rawls and later adapted for bioethics, RE involves a deliberative process where researchers move back-and-forth between ethical principles or theories and concrete moral judgements or empirical data until a state of equilibrium is reached [2]. This process acknowledges that both initial moral intuitions and ethical principles are subject to revision in pursuit of a coherent moral perspective.
The method is fundamentally consultative because the researcher conducts this deliberative process internally, consulting various sources of moral insight but ultimately taking responsibility for the normative conclusions [2]. In empirical bioethics, RE has been tailored to serve research projects by providing a structured approach to integrate empirical findings with ethical analysis [2]. The process does not simply apply pre-existing ethical theories to empirical data but allows for mutual adjustment between theory and data, recognizing that ethical understanding emerges through this iterative process.
Variants and Adaptations
Several adaptations of RE have been developed specifically for empirical bioethics contexts. Wide Reflective Equilibrium expands the elements considered beyond principles and judgements to include ethical theories, background philosophies, and empirical data [35]. Collective Reflective Equilibrium extends the process to incorporate multiple perspectives, making it particularly valuable for policy development where diverse stakeholder views must be considered [36] [37]. This variant is especially relevant for drug development professionals addressing ethical questions that span multiple constituencies including patients, clinicians, researchers, and regulators.
Another significant adaptation is Reflexive Balancing, which emphasizes the critical examination of one's own presuppositions throughout the research process [35]. This approach acknowledges that researchers bring their own moral frameworks and biases to the analytical process and encourages explicit engagement with these factors. For researchers in pharmaceutical contexts, this reflexivity is crucial when addressing ethically complex areas such as clinical trial design, access to experimental medicines, or ethical allocation of scarce resources.
Implementation Protocol: Applying Reflective Equilibrium
Phase 1: Research Preparation and Scoping
Objective: Establish the foundational elements for the RE process and define the ethical question to be addressed.
Procedure:
- Define the Normative Question: Precisely formulate the ethical question or dilemma to be addressed. In drug development contexts, this might involve questions about inclusion criteria for clinical trials, ethical approaches to risk-benefit assessment, or fair allocation of research resources.
- Identify Preliminary Moral Intuitions: Document initial moral judgements about the question. These may include:
- Researcher's own intuitions
- Common moral positions identified in preliminary literature review
- Institutional or professional guidelines
- Regulatory frameworks
- Select Relevant Ethical Theories: Identify ethical frameworks potentially relevant to the question (e.g., utilitarianism, deontology, principlism, virtue ethics, capabilities approach).
- Design Empirical Component: Develop methodology for gathering empirical data that will inform the ethical analysis. This may involve:
- Qualitative interviews with stakeholders
- Survey of professional attitudes
- Analysis of existing practices through document review
- Ethnographic observation of relevant contexts
Table 1: Research Preparation Checklist
| Component | Description | Documentation Output |
|---|---|---|
| Normative Question | Precise formulation of ethical issue | Research protocol with clear question statement |
| Preliminary Moral Intuitions | Initial moral judgements about the issue | Annotated list of intuitions with sources |
| Ethical Theories | Frameworks for systematic ethical analysis | Table of theories with relevance justification |
| Empirical Design | Methodology for data collection | Research protocol with sampling, methods, analysis plan |
Phase 2: Data Collection and Initial Analysis
Objective: Gather and preliminarily analyze both empirical data and normative content.
Procedure:
- Conduct Empirical Research: Implement the planned empirical methodology, ensuring rigorous data collection appropriate to the research question.
- Analyze Empirical Data: Use appropriate analytical methods (e.g., thematic analysis for qualitative data, statistical analysis for quantitative data) to identify key patterns, themes, or findings.
- Conduct Normative Analysis: Systematically analyze the identified ethical theories and principles, identifying their implications for the research question.
- Document Tensions and Agreements: Create a preliminary map of relationships between:
- Different ethical theories
- Ethical theories and preliminary moral intuitions
- Ethical positions and empirical findings
The consultative nature of this model requires meticulous documentation at this stage, as the researcher is building the raw materials for the subsequent reflective process. For drug development professionals, this often involves careful attention to both scientific evidence (e.g., clinical trial data, preclinical studies) and ethical frameworks relevant to pharmaceutical research and development.
Phase 3: Iterative Reflection and Equilibrium Seeking
Objective: Systematically work toward coherence among the various elements through iterative reflection.
Procedure:
- Identify Initial Incongruences: Document specific points of tension between:
- Empirical findings and ethical theories
- Ethical theories and moral intuitions
- Different ethical theories
- Moral intuitions and empirical findings
- Develop Adjustment Strategies: For each identified incongruence, consider possible adjustments:
- Revise interpretation of empirical data
- Modify application of ethical theory
- Reject or modify initial moral intuitions
- Seek additional empirical evidence or theoretical perspectives
- Implement Adjustments: Make reasoned decisions about which elements to adjust, documenting justifications for each decision.
- Test Revised Position: Assess whether adjustments increase overall coherence or create new tensions.
- Repeat Process: Continue cycles of identification, adjustment, and testing until no further enhancements to coherence can be made through reasonable adjustments.
Table 2: Common Incongruence Types and Resolution Strategies
| Incongruence Type | Example from Drug Development | Potential Resolution Strategies |
|---|---|---|
| Empirical findings contradict moral intuitions | Patients value accelerated access to unproven drugs despite safety concerns | Re-examine intuition in light of patient experiences; distinguish between different types of values |
| Ethical theories conflict with each other | Utilitarian approach to trial design conflicts with deontological rights-based approach | Seek hybrid approach; examine scope conditions for each theory; develop priority rules |
| Empirical data challenges ethical theory application | Clinical reality complicates application of idealized consent processes | Modify theory application to accommodate practical constraints while preserving core values |
| Moral intuitions conflict across stakeholders | Researchers, patients, and regulators have different risk tolerance | Identify common ground; distinguish negotiable from non-negotiable differences |
This reflective process is inherently iterative and requires researchers to move beyond simple application of ethical theories to genuine engagement with empirical realities. The diagram below illustrates this iterative process:
Phase 4: Validation and Output
Objective: Verify the robustness of the achieved equilibrium and articulate normative conclusions.
Procedure:
- Test Robustness: Subject the equilibrium position to challenge through:
- Consideration of counterexamples
- Consultation with alternative ethical frameworks
- Examination of potential biases in empirical data or interpretation
- Articulate Normative Conclusions: Clearly state the ethical position reached, including:
- Specific normative recommendations
- Scope and limitations of conclusions
- Remaining uncertainties or areas for further development
- Document Justification: Provide transparent account of:
- Pathway to the equilibrium position
- Key decision points in the reflective process
- Reasons for rejecting alternative positions
- Formulate Implementation Guidance: Where appropriate, provide practical guidance for applying the conclusions in real-world contexts relevant to the target audience.
For drug development professionals, this final phase often involves translating ethical conclusions into practical recommendations for clinical trial design, patient engagement strategies, or drug development pathway decisions.
Quality Standards and Methodological Rigor
Application of Reflective Equilibrium within consultative models should adhere to established quality standards for empirical bioethics research. Based on consensus findings from European scholars, the following standards are particularly relevant [38]:
Table 3: Quality Standards for Reflective Equilibrium Applications
| Domain | Standard | Application to RE |
|---|---|---|
| Aims | Clearly articulate research aims and normative goals | Explicitly state the ethical question and purpose of seeking RE |
| Questions | Formulate research questions that require empirical-normative integration | Develop questions that connect empirical phenomena with normative evaluation |
| Integration | Explain and justify how integration is carried out | Document the RE process, including adjustments and justifications |
| Empirical Work | Conduct empirical work to disciplinary standards | Employ methodologically rigorous data collection and analysis |
| Normative Work | Conduct normative work to disciplinary standards | Apply philosophical rigor to ethical analysis and theory application |
| Expertise | Ensure research team has appropriate empirical and normative expertise | Include or consult relevant expertise in ethics and empirical methods |
Researchers should also address the common challenge of vagueness in integration methodologies [2]. This can be mitigated through transparent documentation of the reflective process, explicit justification of methodological choices, and critical engagement with the limitations of the approach.
Applications in Pharmaceutical and Drug Development Contexts
The Reflective Equilibrium approach has particular relevance for drug development professionals facing complex ethical questions. Specific applications include:
- Clinical Trial Design Ethics: Navigating tensions between scientific validity, patient safety, and accessibility when designing trials for novel therapies.
- Patient Inclusion Criteria: Developing ethically justified inclusion and exclusion criteria that balance scientific needs with equitable access.
- Risk-Benefit Assessment: Formulating approaches to risk-benefit assessment that incorporate diverse stakeholder perspectives and values.
- Resource Allocation Decisions: Addressing ethical questions about resource allocation within drug development programs.
- Post-Trial Access: Developing ethically defensible approaches to providing access to investigational medicines after trial completion.
The three-phase Mapping-Framing-Shaping framework provides a helpful overarching structure for positioning RE within larger research projects [39]. The diagram below illustrates how RE functions within this broader framework:
Research Reagent Solutions: Essential Methodological Tools
Implementing Reflective Equilibrium effectively requires specific methodological tools and approaches. The following table outlines key "research reagents" for consultative empirical bioethics:
Table 4: Essential Methodological Tools for Reflective Equilibrium Research
| Tool Category | Specific Methods/Approaches | Function in RE Process |
|---|---|---|
| Empirical Data Collection Methods | Semi-structured interviews, Focus groups, Surveys, Document analysis, Ethnographic observation | Generate rich understanding of stakeholder perspectives and contextual factors |
| Normative Analysis Tools | Principles analysis, Casuistry, Theory application, Concept clarification | Provide systematic frameworks for ethical evaluation |
| Integration Facilitators | Data triangulation, Perspective-taking exercises, Counterexample testing, Coherence mapping | Support the iterative process of seeking equilibrium between diverse elements |
| Documentation Aids | Reflexive journals, Decision trails, Position justification memos, Adjustment logs | Create transparent records of the reflective process and methodological choices |
| Validation Mechanisms | Peer debriefing, Member checking, Theoretical validation, Case application testing | Assess robustness of equilibrium position and identify potential weaknesses |
Reflective Equilibrium offers a robust, flexible methodology for addressing complex ethical questions in drug development and pharmaceutical research. Its consultative nature positions the researcher as an integrative thinker who systematically moves between empirical evidence and normative frameworks to develop justified ethical positions. By implementing the protocols and application notes outlined above, researchers can bring methodological rigor and transparency to their ethical analyses while remaining responsive to the complex realities of pharmaceutical research and development.
The approach is particularly valuable in interdisciplinary contexts, as it provides a structured process for engaging with diverse forms of evidence and perspective while maintaining philosophical rigor. For drug development professionals facing increasingly complex ethical challenges, Reflective Equilibrium offers a pathway to ethical decisions that are both principled and practically grounded.
Application Notes: The Role of Dialogical Models in Empirical Bioethics
Within interdisciplinary empirical bioethics research, dialogical models provide structured methodologies to integrate diverse stakeholder perspectives, reconciling empirical data with normative analysis. This integration addresses a persistent challenge in the field, where ethical principles must be grounded in the practical realities of healthcare, technology development, and clinical practice [2]. These models move beyond abstract theorizing by creating participatory frameworks that engage stakeholders in deliberative processes, generating ethically sound and practically viable outcomes [40] [41].
For researchers and drug development professionals, structured dialogues offer systematic approaches to identifying and addressing ethical challenges throughout the research and development lifecycle. This is particularly valuable in contexts like artificial intelligence in healthcare, genomic medicine, and clinical trial design, where rapid technological advancement creates novel ethical dilemmas requiring multidisciplinary input [40]. The methodology ensures that resulting ethical frameworks reflect not only theoretical principles but also practical constraints and stakeholder values.
Key Dialogical Approaches for Bioethics Research
Table 1: Structured Dialogical Approaches for Empirical Bioethics
| Methodology | Primary Approach | Integration Mechanism | Application Context in Bioethics |
|---|---|---|---|
| Structured Dialogical Design | Collaborative idea generation and root cause mapping [42] | Interpretive Structural Modeling to build influence maps [42] | Identifying research priorities; Addressing systemic challenges in healthcare [42] |
| Embedded Ethics | Integration of ethicists/social scientists into research teams [40] | Continuous interdisciplinary collaboration throughout project lifecycle [40] | AI health technology development; Genomics research; Neurotechnology [40] |
| Dialogic Change Model | Phased stakeholder engagement process [43] | Structured progression through exploration, formalization, implementation, and sustainability [43] | Health policy development; Institutional ethics framework implementation |
| Deliberative Dialogue | Argumentation-based stakeholder discussion [41] | Critical discussion following normative model of reasonableness [41] | Health policy decision-making; Clinical guideline development |
Comparative Advantages for Drug Development and Healthcare Research
Structured dialogical processes offer distinct advantages for empirical bioethics research in scientific and pharmaceutical contexts. The Embedded Ethics approach, where ethicists work alongside researchers, enables proactive identification of ethical concerns during technology development rather than post-implementation analysis [40]. This is particularly valuable for clinical trial design, biomarker research, and therapeutic algorithm development, where ethical considerations directly impact patient safety and research validity.
The Structured Dialogical Design methodology excels in complex, multi-stakeholder environments by mapping relationships between ethical concerns and identifying leverage points for intervention [42]. For drug development professionals, this systematic approach to identifying root causes of ethical challenges supports the creation of more robust ethical frameworks for translational research and clinical application.
Experimental Protocols
Protocol 1: Structured Dialogical Design for Bioethics Research
This protocol details the implementation of Structured Dialogical Design (SDD) for identifying and addressing ethical challenges in biomedical research contexts, adapted from methodologies successfully applied in healthcare AI and public health settings [42].
Phase 1: Preparation and Triggering Question Formulation (1-2 weeks)
Triggering Question Development: Convene a Knowledge Management Team comprising the dialogue host, 1-2 participants, and at least one trained SDD facilitator [42]. Formulate specific, open-ended triggering questions that frame the ethical discussion (e.g., "What ethical challenges emerge when implementing AI-based diagnostics in clinical dermatology?" or "What stakeholder concerns must be addressed in developing polygenic risk score applications?") [42] [40].
Stakeholder Identification and Recruitment: Apply the "requisite variety" criterion to identify participants representing a spectrum of perspectives relevant to the ethical issue [42]. For drug development contexts, this typically includes:
- Clinical researchers and trial investigators
- Bioethicists and social scientists
- Patient representatives and advocacy groups
- Regulatory affairs specialists
- Industry representatives (pharma/biotech)
- Healthcare providers and clinicians
Pre-Dialogue Preparation: Distribute background materials on the ethical topic and SDD process. Secure informed consent for participation and recording of sessions. Plan for 2-3 day intensive workshop sessions for optimal results [42].
Phase 2: Facilitated Dialogue Process (2-3 days)
Idea Generation (1-2 hours): Using round-robin methodology, participants contribute single-idea statements in response to the triggering question [42]. Each contribution is numbered and recorded verbatim. Facilitators ensure statements contain only one specific observation without generalizations.
Clarification (2-3 hours): Contributors explain the meaning behind their statements while other participants ask clarifying questions without judgment [42]. This process ensures shared understanding of all contributions and protects participant autonomy.
Clustering (2-4 hours): Using bottom-up categorization, participants collaboratively group similar ideas through facilitated discussion [42]. This evolutionary learning process encourages exploration of distinctions and connections between ethical concerns.
Importance Voting (30-45 minutes): Participants individually select five ideas they perceive as most important, comparing across the full set of contributions rather than prioritizing their own ideas [42].
Phase 3: Structural Analysis and Action Planning (1-2 days)
Interpretive Structural Modeling (3-4 hours): Using specialized software (Cogniscope, Concertina, or Logosophia), participants examine pairs of important ideas and determine relationships through constructive debate [42]. Relationships are established only when supported by supermajority (typically 75%) agreement.
Influence Map Generation: Software algorithms process the binary relationships to generate a visual influence map (directed graph) showing hierarchical relationships between ideas [42]. Root causes appear at the base, with influenced elements above.
Root Cause Analysis and Action Planning: Identify root causes (ideas at the base of the influence structure) as strategic intervention points [42]. Develop specific action plans addressing these foundational elements, recognizing that changes here will have positive effects throughout the ethical challenge system.
Protocol 2: Embedded Ethics Integration for Research Consortia
This protocol implements the Embedded Ethics approach, integrating ethicists directly into interdisciplinary research teams to address ethical issues throughout project lifecycles, particularly relevant for AI health research and drug development consortia [40].
Integration and Assessment Phase (Ongoing)
Team Embedding: The embedded ethics researcher participates in regular research team meetings and works in the same physical or virtual venue when possible [40]. This deep immersion builds understanding of technical details, procedural norms, and team dynamics essential for contextual ethical analysis.
Stakeholder Analysis: Identify all stakeholders affected by the research or technology, including seemingly voiceless stakeholders (e.g., future patients, marginalized communities, or nature) [42] [40]. Map stakeholder interests, power dynamics, and potential impacts.
Iterative Ethics Assessment: Conduct ongoing ethical analysis through:
- Literature Review: Systematic examination of relevant ethical, social, and technical literature [40].
- Ethnographic Approaches: Observation of research practices and technology development processes in context [40].
- Peer-to-Peer Interviews: Structured conversations with research team members to understand perspectives and concerns [40].
- Bias Analysis: Systematic assessment of potential biases in algorithms, data collection, or research design [40].
Deliberative and Implementation Phase (Quarterly Cycles)
Focus Groups: Conduct structured discussions with external stakeholders, including patient groups, community representatives, and healthcare providers [40]. Use triggering questions to explore specific ethical dimensions.
Interdisciplinary Workshops: Facilitate collaborative sessions between technical researchers, ethicists, and stakeholders to identify and address emerging ethical concerns [40]. Adapt Structured Dialogical Design elements for efficient idea generation and prioritization.
Interdisciplinary Results Dissemination: Translate ethical analysis into practical recommendations tailored to different audience needs [40]. Develop implementation strategies for ethical design modifications, monitoring frameworks, and governance structures.
Table 2: Research Reagent Solutions for Dialogical Bioethics
| Tool/Resource | Function | Application Context | Implementation Considerations |
|---|---|---|---|
| Structured Dialogical Design Software (Cogniscope, Concertina, Logosophia) | Supports Interpretive Structural Modeling by presenting idea pairs and building influence maps [42] | Complex ethical challenges requiring root cause analysis and leverage point identification | Requires trained facilitators; Most effective with in-person or synchronous virtual sessions [42] |
| Stakeholder Mapping Templates | Identifies relevant stakeholders and analyzes their interests, influence, and relationships to the ethical issue [40] | Initial phase of any dialogical process to ensure inclusive participation | Should include seemingly voiceless stakeholders; Requires iterative updating throughout project [42] |
| Embedded Ethics Assessment Framework | Guides ongoing ethical assessment integrated into research workflows [40] | Long-term research projects and technology development consortia | Requires dedicated ethics researcher with interdisciplinary collaboration skills; Dependent on team access and transparency [40] |
| Deliberative Dialogue Protocols | Provides structured approach for reason-based stakeholder discussions following argumentation theory [41] | Health policy development; Clinical guideline creation; Regulatory framework design | Requires trained moderator; Participants need understanding of argumentation principles [41] |
| Hybrid Engagement Platforms | Supports virtual and asynchronous participation in dialogical processes [42] | Geographically distributed stakeholder groups; Pandemic or travel-restricted contexts | Balancing synchronous and asynchronous elements; Maintaining engagement across different participation modes [42] |
Application Notes: Foundations of Interdisciplinary Bioethics Research
Interdisciplinary bioethics research bridges the normative domains of philosophy and ethics with the empirical domains of social and health sciences. This integration requires methodological rigor from the initial design phase to ensure that empirical data collection genuinely informs ethical analysis, and that ethical frameworks meaningfully guide empirical inquiry. The following application notes provide a foundation for this integrated approach.
Methodological Epoché as a Starting Point: A foundational step in interdisciplinary bioethics is the practice of methodical epoché—the temporary suspension of monodisciplinary assumptions and methods at the project's inception [44]. This practice facilitates the development of a genuinely interdisciplinary research question that is not reduced to the priorities of a single discipline. The purpose is to achieve a shared understanding of the problem before breaking it down with specific disciplinary tools [44].
Protocol Development for Integrated Research: A robust research protocol is critical. A suitable template for such investigations should be adaptable to qualitative, quantitative, and mixed-methods approaches, ensuring the research design can accommodate the diverse evidence needs of bioethics [45]. This protocol serves as the master plan, detailing how normative and empirical threads will be woven together throughout the investigation.
Data Presentation for Interdisciplinary Dialogue: Presenting data effectively is crucial for communicating with a broad interdisciplinary audience. Quantitative data, in particular, should be presented clearly to illustrate trends and support arguments without oversimplification [46] [47]. The choice of graphical representation—whether histograms, frequency polygons, or line graphs—should be guided by the specific relationship the researcher intends to show, such as distributions or time trends [46] [47] [48].
Experimental Protocols
Protocol 1: Framework Development Using Methodical Epoché
Objective: To establish a shared, interdisciplinary research framework for a bioethics investigation by suspending disciplinary-specific assumptions.
Background: Interdisciplinarity cannot thrive unless it curbs, from the very start, the inevitable reductions of all monodisciplinary approaches [44]. This protocol operationalizes the methodical epoché to achieve this.
Phase 1: Constitutive Epoché
- Procedure: Assemble the interdisciplinary research team. Each member shall explicitly state their core research question, key definitions, and preferred methodological norms as they would within their native discipline.
- Documentation: Record these statements in a shared document. This serves as the "pre-epoché" baseline.
- Action: As a group, consciously agree to temporarily bracket these individual disciplinary commitments. The goal is not to discard them, but to set them aside to create space for a new, integrated perspective.
Phase 2: Interdisciplinary Question Formulation
- Procedure: Based on the bracketed statements, collaboratively reframe the research problem. Focus on crafting a single, global question that captures the ethical and empirical dimensions of the issue without privileging one type of evidence or analysis.
- Output: A concise, written statement of the interdisciplinary research question. No breakdown of this global question by particular methods of single disciplines should be attempted at this stage [44].
Phase 3: Re-integration of Disciplinary Methods
- Procedure: Only after the global question is agreed upon, the team will determine how the various disciplinary methods (e.g., philosophical analysis, ethnographic observation, survey research) can be deployed to answer specific parts of this overarching question.
- Final Output: A research protocol that details the integrated methodology, showing how the empirical and normative components will interact throughout the project lifecycle.
Protocol 2: Integrated Data Collection and Normative Analysis Workflow
Objective: To provide a structured process for collecting and analyzing data in a way that continuously feeds into normative reflection.
Background: This protocol ensures that data collection is not merely in service of ethical analysis but is intertwined with it, allowing for iterative refinement of both the empirical and normative strands of the research.
Step 1: Parallel Data Collection Planning
- Define the empirical data needed (e.g., interviews, surveys, clinical outcomes).
- Simultaneously, define the normative sources to be analyzed (e.g., ethical guidelines, legal statutes, philosophical literature).
- Create a cross-reference matrix linking each type of empirical data to the specific normative questions it is intended to inform.
Step 2: Concurrent Data Gathering and Analysis
- Empirical Track: Execute the planned data collection. Begin preliminary thematic or statistical analysis.
- Normative Track: Conduct a preliminary analysis of the identified normative sources.
- Integration Loop: Hold regular team meetings to discuss initial findings from both tracks. Use insights from the normative analysis to refine further empirical data collection (e.g., by prompting new interview questions). Conversely, use emergent empirical themes to refine the focus of the ongoing normative analysis.
Step 3: Synthetic Interpretation
- Procedure: Systematically bring the analyzed empirical data and normative analysis into conversation. The output is not a simple summary of both but an interpretation that identifies how the empirical findings challenge, support, or complicate existing ethical norms and how the ethical framework helps to make sense of the empirical observations.
- Output: A draft of the research findings that reflects this synthetic interpretation.
Data Presentation
This table organizes common methods for presenting quantitative data, which is essential for communicating empirical findings to an interdisciplinary audience in bioethics [46] [47] [48].
| Method | Primary Function | Best Use Cases in Bioethics | Key Considerations |
|---|---|---|---|
| Frequency Table [47] | Summarizes data by showing counts in categories or class intervals. | Presenting baseline characteristics of study participants (e.g., age, socioeconomic status); summarizing responses to survey items. | Ensure class intervals are equal; number of classes should be optimal (e.g., 6-16); include clear titles and units [47]. |
| Histogram [46] [47] | Displays the distribution of a continuous numerical variable. | Visualizing the distribution of scores on an attitude scale; showing the age distribution of a patient cohort. | Bars are contiguous (no gaps) because the data is continuous; the area of each bar represents the frequency [47]. |
| Frequency Polygon [46] | Shows the shape of a distribution by connecting points at the midpoints of class intervals. | Comparing the distributions of two or more groups on the same graph (e.g., attitudes of clinicians vs. patients). | Often overlaid on a histogram; effective for comparing multiple distributions on one axis [46]. |
| Line Diagram [47] | Illustrates trends over a period of time. | Depicting changes in public opinion on a bioethical issue over time; tracking the frequency of an ethical dilemma in clinical practice across years. | The X-axis represents time intervals (e.g., months, years); effective for showing clear, continuous trends [47]. |
| Bar Chart [48] | Compares frequencies or magnitudes across different categories. | Comparing the prevalence of different ethical concerns across several professional groups; showing proportional representation. | Bars are separated by gaps, indicating categorical data; can be vertical or horizontal [48]. |
| Pie Chart [48] | Shows the proportion of parts to a whole. | Displaying the breakdown of types of ethical cases reviewed by a hospital ethics committee (if categories are limited). | Use only when parts are mutually exclusive and sum to 100%; limit to 5-7 categories for clarity [48]. |
Visualization Diagrams
Diagram 1: Integrated Research Workflow
Diagram 2: Data Presentation Selection Guide
Research Reagent Solutions
Table 2: Essential Methodological Tools for Empirical Bioethics Research
This table details key conceptual and methodological "reagents" essential for conducting integrated empirical bioethics research.
| Research 'Reagent' | Function / Purpose | Application Context |
|---|---|---|
| Methodical Epoché [44] | To create a neutral starting point by suspending disciplinary assumptions, preventing premature reduction of the research question to a single discipline's framework. | Used during the initial stages of project design to facilitate the development of a truly interdisciplinary research question. |
| Adaptive Protocol Template [45] | Provides a structured yet flexible plan for research that can accommodate qualitative, quantitative, and mixed-methods approaches within a single study. | Serves as the master document guiding the entire research process, ensuring methodological rigor across diverse investigative approaches. |
| Frequency Distribution Table [47] | Organizes raw quantitative data into manageable class intervals with corresponding counts, providing a clear summary of the data's structure. | Used for initial data screening and as the basis for creating histograms and frequency polygons to visualize the distribution of empirical findings. |
| Comparative Histogram/Bar Chart [46] [48] | Allows for the visual comparison of data distributions or frequencies across two or more distinct groups (e.g., patients vs. providers). | Employed to present empirical results in a way that highlights differences and similarities relevant to normative analysis, making data accessible to interdisciplinary audiences. |
| Integration Loop Mechanism | A structured process (e.g., regular team meetings) for comparing preliminary empirical findings with ongoing normative analysis, allowing for iterative refinement of both. | Operationalizes the "weaving" of normative and empirical questions throughout the active research phase, ensuring continuous dialogue between the two strands. |
| Synthetic Interpretation Framework | The guiding methodology for the final stage of analysis, where empirical results and normative conclusions are systematically brought into dialogue to produce novel insights. | Used to generate the final research outputs, ensuring that findings reflect a genuine integration of disciplines rather than a simple reporting of parallel results. |
Narrative approaches represent a significant methodological evolution within empirical bioethics, focusing on the collection and analysis of stories to understand the complex, lived experiences of individuals facing moral dilemmas in healthcare. This method is grounded in the recognition that stories and narratives provide unique access to the moral reasoning and contextual factors that shape ethical decisions, which are often lost in more traditional, abstract ethical analysis [49]. By systematically listening to how people articulate their experiences, bioethicists can ground normative reflection in the rich, detailed reality of practice rather than in sterile, hypothetical environments [50] [49].
The value of these approaches lies in their capacity to address a fundamental tension in empirical bioethics between positivist and interpretive scientific paradigms. Narrative methods resist the loss of depth and context that may occur with more reductionist forms of thematic or content analysis, instead preserving the complexity and nuance of moral experiences as they unfold in real-world settings [49]. For bioethics researchers seeking to understand not just what decisions are made but how and why they are made within specific contexts, narrative approaches offer a powerful methodological toolkit for investigating the interplay between individual values, relational dynamics, and institutional structures in shaping ethical outcomes.
Theoretical Framework and Disciplinary Positioning
Theoretical Foundations
Narrative approaches in bioethics draw theoretical inspiration from multiple disciplines, including Narrative Medicine, qualitative social sciences, and hermeneutic philosophy. These approaches share a common commitment to understanding moral experience as inherently situated within specific contexts and temporal sequences that give actions their meaning [49]. Rather than treating ethical decisions as discrete events, narrative methods frame them as processes embedded within life stories, cultural frameworks, and relational networks.
A central epistemological claim of narrative bioethics is that stories do not merely illustrate ethical principles but actively construct moral understanding. Through the process of narrating experiences, individuals and communities make sense of moral dilemmas, reconcile conflicting values, and articulate what constitutes virtuous action in the face of uncertainty. This positions narrative both as a method of inquiry and as an object of analysis within empirical bioethics research [49].
Position within Empirical Bioethics
Narrative approaches address several challenges that empirical bioethics researchers face in aligning moral epistemology and methods. They occupy a distinctive space within the broader taxonomy of empirical bioethics methodologies, particularly suited to projects that seek to:
- Understand how ethical dilemmas are experienced by various stakeholders
- Examine the discursive patterns through which moral problems are articulated and negotiated
- Develop contextual ethical responses that are grounded in lived reality rather than abstract principles [49]
This positioning makes narrative approaches particularly valuable for researchers who adopt a "diagnostic" mindset focused on deeply understanding ethical problems in their complexity, while maintaining a commitment to ethics' normative task [49].
Key Applications and Research Objectives
Narrative approaches serve several distinct but interconnected research objectives within empirical bioethics. A qualitative exploration of researchers' views on acceptable objectives for empirical research in bioethics has identified those most aligned with narrative methodologies [10].
Table 1: Research Objectives for Narrative Approaches in Bioethics
| Research Objective | Description | Alignment with Narrative Approaches |
|---|---|---|
| Understanding Context | Exploring the circumstances, structures, and environments in which ethical issues arise | High alignment - Narratives naturally reveal contextual factors |
| Identifying Ethical Issues in Practice | Discovering which ethical problems actually emerge in clinical or research settings | High alignment - Stories uncover real rather than theoretical dilemmas |
| Descriptive Ethics | Documenting how people morally reason and what moral opinions they hold | High alignment - Narratives capture moral reasoning processes |
| Lived Experience | Understanding stakeholders' subjective experiences of ethical issues | High alignment - Central strength of narrative approaches |
| Evaluating Recommendations | Assessing how ethical recommendations play out in practice | Moderate alignment - Requires longitudinal narrative elements |
| Drawing Normative Recommendations | Developing specific ethical guidance based on empirical findings | Moderate alignment - Requires careful integration with normative analysis |
| Developing/Justifying Moral Principles | Creating or validating fundamental ethical principles | Lower alignment - Narrative provides input but insufficient alone |
The most strongly supported objectives – understanding context and identifying ethical issues in practice – represent the core strengths of narrative methodologies [10]. These applications reflect what narrative approaches do uniquely well: uncovering the deep context of moral dilemmas and revealing how ethical issues actually manifest in practice rather than in theoretical abstraction.
For bioethics researchers working in drug development and healthcare settings, narrative methods are particularly valuable for investigating:
- Patient and caregiver experiences with experimental treatments and clinical trials
- Clinician moral distress in the context of resource allocation or end-of-life decisions
- Stakeholder perspectives on emerging ethical challenges in novel technologies
- Organizational narratives surrounding ethical dilemmas in healthcare institutions
Experimental Protocol: Narrative Interviewing in Empirical Bioethics
Protocol Template for Narrative Research
This protocol adapts the health research template for humanities and social sciences investigations, specifically designed for narrative approaches in empirical bioethics [7].
Table 2: Protocol Template for Narrative Bioethics Research
| Section | Key Components | Considerations for Narrative Approaches |
|---|---|---|
| Title and Identification | Short title, acronym, nature of study | Identify narrative approach explicitly |
| Administrative Information | Sponsor, principal investigator, research team, ethics committee | Include narrative methodology experts |
| Summary | Context, primary objective, general method | Highlight narrative data collection |
| Problem Studied | Importance, literature review, problem statement | Justify need for narrative understanding |
| Research Objectives | Specific goals and questions | Frame as understanding experiences/stories |
| Disciplinary Field | Principal disciplinary field(s) | Specify "empirical bioethics with narrative approaches" |
| Research Paradigm | Methodological and theoretical frameworks | Narrative paradigm; specified ethical theory |
| Site and Duration | Study site, contextual factors, timeline | Include periods for narrative collection/analysis |
| Researcher Characteristics | Qualifications, experience, reflexivity | Acknowledge researcher positionality |
| Participant Selection | Characteristics, sampling method, sample size | Purposive sampling; continue until narrative saturation |
| Informed Consent | Type of consent, information materials | Address specific narrative concerns (anonymization of stories) |
| Data Collection | Type of data, procedures, instruments | Narrative interviews; story completion tasks; field notes |
| Data Management | Processing, storage, protection, confidentiality | Secure storage of often highly personal narratives |
| Data Analysis | Analytical approach, specific techniques | Narrative analysis; structural analysis; thematic analysis |
| Integration Methodology | Approach to integrating empirical and normative dimensions | Specify how narratives will inform ethical analysis |
| Research Quality | Techniques to ensure rigor and trustworthiness | Narrative validity; member checking; triangulation |
| Dissemination | Plans for sharing results | Consider participatory dissemination with participants |
Detailed Methodological Procedures
Narrative Interviewing Technique
The core narrative interview follows a minimalist structure that encourages rich storytelling while ensuring relevant ethical dimensions are explored:
- Initial Narrative Invitation: Begin with a single, open-ended question designed to elicit a comprehensive story (e.g., "Please tell me the story of your experience with... from the beginning until now").
- Active Narrative Listening: During the subsequent narration, intervene as little as possible, using only non-directive prompts (e.g., "What happened next?" or "How did that feel?") to maintain the narrative flow.
- Systematic Phenomenological Analysis: After the narrative concludes, move to a more structured questioning phase that explores specific ethical dimensions raised in the story, using the participant's own terminology and framing.
This approach enables researchers to "listen in new ways" that privilege the participant's narrative structure and moral categories rather than imposing external theoretical frameworks prematurely [49].
Data Integration and Analysis
The integration of empirical narratives with normative analysis follows a structured process:
Diagram 1: Narrative Data Analysis Workflow
This methodology enables researchers to maintain the integrity of stories while systematically analyzing their ethical content and implications. The process respects what narrative approaches uniquely offer: deep engagement with the particularity and context of moral experience while still enabling the development of ethically normative conclusions that can inform practice and policy [49].
Table 3: Essential Research Reagents for Narrative Bioethics
| Tool/Resource | Function/Purpose | Application Notes |
|---|---|---|
| Semi-Structured Interview Guide | Provides flexible framework for narrative interviews | Balance open-ended narrative prompts with specific ethical probes |
| Digital Audio Recorder | Captures complete narrative data in participants' own words | Essential for accurate transcription and analysis of narrative flow |
| Transcription Software | Converts audio to text for detailed analysis | Verbatim transcription preserves narrative structure and linguistic choices |
| Qualitative Data Analysis Software (e.g., NVivo, Atlas.ti) | Facilitates coding and analysis of narrative data | Enables organization of large narrative datasets and identification of patterns |
| Reflexive Journal | Documents researcher assumptions and reflections | Critical for maintaining methodological rigor and transparency |
| Ethical Framework Toolkit | Provides structured approach to normative analysis | Bridges empirical narratives and ethical reasoning [7] |
| Narrative Analysis Framework | Systematic approach to analyzing story structures | Identifies plot, characters, moral turning points in narratives |
Methodological Considerations and Quality Assessment
Ensuring Methodological Rigor
The quality of narrative research in bioethics depends on several key considerations:
- Narrative Competence: Researchers must develop skills in eliciting stories without imposing structure, listening for narrative patterns, and recognizing different forms of storytelling [49].
- Reflexivity: Given the interpretive nature of narrative analysis, researchers must continuously examine how their own positions, assumptions, and experiences shape the research process, from data collection through to normative analysis.
- Ethical Sensitivity: Narrative research often engages with deeply personal, sometimes traumatic experiences, requiring particular attention to research ethics beyond standard protocols, including ongoing consent and appropriate support for participants.
Addressing Epistemic Injustice
Narrative approaches specifically help address concerns about epistemic injustice in bioethics by creating methodological space for voices and forms of knowledge that may be marginalized in traditional ethical analysis [49]. This includes:
- Prioritizing the stories of patients, caregivers, and other stakeholders whose moral experiences might otherwise be overlooked
- Respecting different forms of moral reasoning that may not align with dominant ethical frameworks
- Recognizing that the same ethical dilemma may be narrated quite differently from various positional perspectives within the healthcare system
Narrative approaches offer empirical bioethics a robust methodology for investigating the complex, context-rich nature of moral experience in healthcare settings. By systematically collecting and analyzing stories, researchers can develop ethical analyses and recommendations that are grounded in the reality of practice while still informed by ethical theory. The protocols and applications outlined here provide researchers with practical guidance for implementing these methods in diverse bioethics research contexts, from clinical ethics to drug development and health policy.
For the field of empirical bioethics more broadly, narrative approaches represent an important development in making the field more interdisciplinary and more rooted in what actually happens in practice [50]. As bioethics continues to grapple with novel ethical challenges from emerging technologies and evolving healthcare systems, narrative methods ensure that ethical analysis remains connected to the human experiences at the heart of these dilemmas.
Application Notes: Interdisciplinary Framework for Reflexive Governance
Theoretical Foundation in Empirical Bioethics
This protocol applies an interdisciplinary empirical bioethics approach to building reflexive governance for One Health surveillance systems. The framework bridges empirical research and normative analysis through pragmatic ethics and reflexive balancing, addressing complex health challenges like antibiotic resistance through integrated human, animal, and environmental health monitoring [51] [52]. The methodology employs empowerment ethics as a form of responsible self-governance, emphasizing that power must lead to awareness of individual and social actions, ultimately fostering accountability mechanisms [51].
The approach is characterized by three core principles: First, a "bottom-up" approach that manages power, knowledge, and interest dynamics that modulate community will and behavior. Second, enabling autonomous change by individuals and communities who acknowledge local values and constraints as criteria for change. Third, establishing abductive approaches that lead to self-responsibility and accountability [51]. This framework operates through "mapping, framing, and shaping" the dynamics of interests and perspectives that could jeopardize a "better" future for health surveillance [52].
Reflexive Governance Model Specifications
The reflexive governance model functions as a community-based action-ethics methodology that hybridizes methods from collective deliberation and expert evaluation [51]. This model intellectualizes the management of democratizing critical thinking locally (collective ethics) while recognizing its broader context (social ethics) [52].
Table 1: Core Components of Reflexive Governance in One Health Surveillance
| Component | Function | Methodological Approach | Output |
|---|---|---|---|
| Mapping | Identifies stakeholders, power dynamics, and knowledge systems | Stakeholder analysis, power mapping, knowledge inventory | Visual maps of governance landscape |
| Framing | Establishes common normative language and values | Deliberative dialogues, consensus-building processes | Shared ethical framework |
| Shaping | Implements adaptive governance structures | Reflexive balancing, iterative design | Collaborative governance regime |
The governance model distinguishes between consultation (gathering information to develop the "best" model) and concertation (seeking consensus about which criteria are "best" to give acceptable orientation to the developing model) [51]. This distinction is crucial for differentiating between descriptive and appreciative knowledge in surveillance system design.
Experimental Protocols
Protocol for Stakeholder Concertation and Deliberative Dialogue
Purpose and Scope
This protocol establishes standardized methodology for conducting stakeholder concertation events to build reflexive governance for One Health surveillance systems, specifically addressing complex issues such as antimicrobial resistance surveillance as demonstrated in the Québec case study (2018-2021) [51] [52].
Materials and Equipment
- Venue capable of accommodating 100+ participants with breakout rooms
- Recording equipment for session documentation
- Anonymous voting system for sensitive deliberations
- Data projection and visualization equipment
- Template materials for structured deliberation exercises
Procedure
Step 1: Participant Recruitment and Saturation
- Recruit participants through extensive recruitment process aiming to saturate perspectives across sectors (industry, academia, government, association, order, etc.)
- Ensure representation across practices (livestock sectors, pets, sports animals) and professions (breeders, veterinarians, nutritionists, researchers, informatics experts)
- Begin with approximately 60 representatives, expanding to 100 as needed for perspective saturation [51]
- Document participant demographics and institutional affiliations
Step 2: Concertation Event Framework
- Conduct two primary concertation events focusing on values and vision criteria
- Facilitate deliberative dialogues using structured ethical analysis frameworks
- Employ adaptive cycle and governance techniques to synthesize alternative governance models [51]
- Utilize reflective equilibrium techniques for back-and-forth deliberation between ethical principles and practical constraints [53]
Step 3: Consensus-Building Mechanism
- Implement modified Delphi approach for consensus-finding [38]
- Conduct iterative rounds of discussion with feedback summarization
- Maintain transparency in methodological choices and theoretical positioning
- Document dissenting perspectives and rationale
Step 4: Governance Model Co-construction
- Facilitate co-construction of common normative language for data governance
- Design collaborative governance regime to shape program functioning
- Establish criteria for "good" actions and "better" future outcomes
- Develop trust-building mechanisms for data systems and information platforms [51]
Quality Control and Standards
- Adhere to empirical bioethics standards of practice regarding aims, questions, integration, conduct of empirical work, conduct of normative work, and training & expertise [38]
- Ensure transparency in how theoretical positions are chosen for integration
- Explain and justify methods of integration between empirical and normative dimensions
- Document the execution of integration methods [53]
Protocol for Reflexive Governance Implementation
Purpose and Scope
This protocol outlines the implementation process for reflexive governance structures in One Health surveillance systems, based on the hybrid method that embeds person-to-person dialogue in collective assemblage to engage social groups in negotiation processes [51].
Procedure
Step 1: System Architecture Design
- Design data systems and information platforms with trust as foundational principle
- Implement adaptive governance systems for evaluation, surveillance, and intervention
- Establish feedback mechanisms for continuous system improvement
- Create technical architecture supporting both top-down political incentives and bottom-up democratic processes [51]
Step 2: Empowerment Ethics Implementation
- Facilitate self-critical examination of governance processes
- Establish receptivity to criticism mechanisms
- Implement critical duty to change protocols
- Create accountability structures for responsible self-governance [51]
Step 3: Integration and Adaptation Cycles
- Conduct regular reflexive assessments of governance effectiveness
- Adapt structures based on surveillance system performance data
- Maintain iterative relationship between operation and innovation
- Bridge reflexive, evaluative, and deliberative reasonings [52]
Visualization Schematics
Reflexive Governance Workflow
Empirical Bioethics Integration Model
Research Reagent Solutions
Table 2: Essential Methodological Tools for Reflexive Governance Research
| Research Tool | Function | Application in One Health Governance |
|---|---|---|
| Deliberative Dialogue Framework | Structured conversation for normative development | Building consensus on ethical values and governance principles across sectors |
| Reflective Equilibrium Method | Back-and-forth adjustment between principles and practice [53] | Integrating empirical findings with normative analysis in surveillance ethics |
| Stakeholder Mapping Matrix | Visual representation of stakeholders and interests | Identifying power dynamics and knowledge systems in One Health networks |
| Adaptive Governance Assessment Tool | Evaluation mechanism for governance adaptability | Monitoring and improving governance responsiveness to emerging health threats |
| Empirical-Normative Integration Protocol | Methodology for combining descriptive and prescriptive analysis [53] | Ensuring transparent justification of methodological choices in bioethics research |
| Trust-Building Metric System | Quantitative and qualitative measures of trust | Establishing and maintaining trust in data sharing platforms and governance institutions |
Navigating the Terrain: Overcoming Common Challenges in Interdisciplinary Bioethics
The is-ought problem, also known as Hume's guillotine, represents a fundamental challenge in moral philosophy: the apparent logical barrier between descriptive statements about how the world "is" and prescriptive conclusions about how we "ought" to act [54]. First articulated by David Hume in 1739, this problem questions how factual observations can logically entail moral obligations without introducing additional normative premises [54]. In contemporary empirical bioethics, this philosophical problem takes on practical significance as researchers seek to integrate empirical data with normative analysis to address complex healthcare dilemmas [2]. The growth of this interdisciplinary field reflects a recognition that purely philosophical approaches may be insufficient to address the nuanced reality of clinical practice and healthcare delivery [2]. This document presents application notes and protocols for navigating the is-ought divide through methodologically rigorous approaches that maintain philosophical integrity while generating practically relevant normative guidance.
Theoretical Framework: Conceptualizing the Is-Ought Relationship
Philosophical Foundations and Contemporary Responses
Hume's original observation highlighted the unjustified transition that moral treatises make from descriptive to prescriptive statements without explaining this "new relation or affirmation" [54]. Contemporary responses to this challenge include:
Structural Continuity Principle: This approach redefines "is" not as a static state but as an ongoing structural process of organized matter resisting entropy. From this perspective, "ought" emerges naturally as the logical requirements for a system's persistence and coherence [55]. For living systems, including individuals and communities, normative claims reflect structural necessities for maintaining existence and function.
Institutional Facts Approach: John Searle's argument that institutional facts (such as promises) inherently carry normative force, suggesting that from certain descriptive facts (e.g., "X made a promise"), normative conclusions (e.g., "X ought to keep the promise") can logically follow [54].
Empirical Bioethics Integration: A growing field that explicitly acknowledges the is-ought challenge while developing methodologies to responsibly connect empirical findings with normative analysis through transparent procedures [6] [2].
Hierarchical Model for Empirical-Normative Integration
A constructive framework for conceptualizing how empirical research can inform normative ethics proposes four hierarchical categories of empirical bioethics research [6]:
Table 1: Hierarchical Categories of Empirical Bioethics Research
| Category | Primary Question | Purpose | Example |
|---|---|---|---|
| Lay of the Land | "What are current practices, opinions, or beliefs?" | Define status quo and set stage for further research | Studies examining attitudes toward end-of-life care among patients, families, and providers [6] |
| Ideal Versus Reality | "To what extent does practice match ethical ideals?" | Identify gaps between normative standards and actual practice | Research demonstrating racial and ethnic disparities in healthcare delivery [6] |
| Improving Care | "How can we bring practice closer to ethical ideals?" | Develop interventions to align practice with normative standards | Projects designing and testing approaches to improve informed consent processes [6] |
| Changing Ethical Norms | "How should our ethical frameworks evolve based on evidence?" | Use cumulative empirical findings to refine and revise ethical norms | Synthesizing multiple studies on quality of life with spinal cord injury to inform decision-making norms [6] |
Methodological Protocols for Is-Ought Integration
Reflective Equilibrium Protocol
The method of wide reflective equilibrium provides a structured approach for moving between empirical data and normative principles through an iterative process of adjustment and justification [2].
Table 2: Reflective Equilibrium Implementation Protocol
| Phase | Procedural Steps | Outputs | Quality Control Measures |
|---|---|---|---|
| Initial Mapping | 1. Document considered moral judgments2. Articulate relevant ethical principles and theories3. Gather relevant empirical data | Catalog of moral intuitions, principles, and facts | Peer review of principle selection; methodological review of empirical data quality |
| Iterative Adjustment | 1. Identify conflicts between elements2. Adjust elements to achieve coherence3. Seek most plausible combination | Refined set of judgments, principles, and interpretations | Documentation of revision rationale; transparency about unresolved tensions |
| Equilibrium Achievement | 1. Test coherence across system2. Evaluate justificatory strength3. Formulate normative conclusions | justified ethical position supported by reflective equilibrium | Critical scrutiny from alternative viewpoints; application to test cases |
Figure 1: Reflective Equilibrium Process
Dialogical Integration Protocol
Dialogical empirical ethics emphasizes collaborative sense-making through structured stakeholder engagement, positioning the ethicist as a facilitator rather than sole authority [2].
Protocol Implementation:
- Stakeholder Identification and Recruitment: Identify all relevant stakeholder groups (patients, clinicians, administrators, community representatives) and recruit participants representing diverse perspectives.
- Structured Dialogue Sessions: Conduct facilitated discussions using semi-structured guides that present empirical findings and ethical questions.
- Normative Analysis Integration: Ethicists synthesize discussion insights with ethical frameworks to develop preliminary normative guidance.
- Participant Validation: Return synthesized guidance to participants for validation and refinement.
- Final Normative Formulation: Develop final normative recommendations that incorporate both stakeholder perspectives and ethical analysis.
Quality Assurance Measures:
- Document participant selection criteria and recruitment process
- Audio record and transcribe all dialogue sessions
- Maintain reflexivity journals documenting facilitator perspectives and potential biases
- Use multiple analysts to identify themes and insights
Systematic Integration Framework for Research Design
A comprehensive protocol for designing empirical bioethics research that explicitly addresses the is-ought gap:
Phase 1: Foundational Development
- Normative Framework Specification: Explicitly state the ethical principles, theories, and values relevant to the research question.
- Empirical Methodology Selection: Choose research methods (qualitative, quantitative, or mixed) that can generate data relevant to the normative framework.
- Integration Procedure Planning: Pre-specify how empirical findings will inform normative analysis, including mechanisms for addressing discordant results.
Phase 2: Data Collection and Initial Analysis
- Empirical Data Generation: Collect data using rigorous methodology appropriate to the research question.
- Preliminary Normative Assessment: Conduct initial assessment of how emerging findings relate to existing normative frameworks.
Phase 3: Integration and Conclusion Development
- Systematic Integration: Implement pre-specified integration procedure, documenting all steps transparently.
- Normative Conclusion Formulation: Develop justified normative conclusions that explicitly acknowledge their relationship to empirical findings.
- Limitation Assessment: Identify and articulate limitations in both empirical and normative dimensions of the work.
Data Presentation and Analysis Protocols
Quantitative Data Analysis Framework
Effective bridging of the is-ought divide requires appropriate summarization and presentation of quantitative data to inform normative analysis [56].
Table 3: Quantitative Data Summary Protocol for Empirical Bioethics
| Data Type | Summary Method | Visualization Options | Normative Relevance |
|---|---|---|---|
| Continuous Variables (e.g., quality of life measures) | Histograms with appropriate bin sizing [56] | Frequency tables, box plots, density curves | Documents distribution of outcomes relevant to welfare assessments |
| Discrete Quantitative Data (e.g., survey responses on Likert scales) | Frequency tables with percentages [56] | Bar charts, pie charts, stacked bar charts | Captures patterns in attitudes, beliefs, and preferences |
| Relationship Between Variables | Cross-tabulation, correlation analysis | Scatter plots, stratified analyses | Identifies associations that may reveal equity concerns or differential impacts |
Qualitative Data Analysis Protocol
For qualitative data in empirical bioethics, a structured approach to analysis ensures appropriate connection to normative analysis:
Protocol Steps:
- Systematic Transcription and Familiarization: Convert audio recordings to text and immerse in data.
- Thematic Analysis: Identify, analyze, and report patterns within data using established qualitative methods.
- Normative Interpretation: Interpret thematic findings in relation to relevant ethical concepts and principles.
- Triangulation: Compare qualitative findings with quantitative data where available.
- Ethical Implications Analysis: Explicitly articulate the ethical implications of qualitative findings.
Application in Drug Development and Healthcare Research
Ethical Framework for Clinical Research
The integration of empirical and normative analysis operates within established ethical frameworks for clinical research. The NIH Clinical Center outlines seven guiding principles for ethical research [9]:
- Social and clinical value
- Scientific validity
- Fair subject selection
- Favorable risk-benefit ratio
- Independent review
- Informed consent
- Respect for potential and enrolled subjects
These principles provide a normative foundation that can be informed and refined through empirical investigation of research practices and outcomes [9].
Data Normalization in Medication Research
In pharmaceutical research and development, data normalization represents a practical example of moving from descriptive data to prescriptive action. The process of standardizing medication data across disparate systems enables multiple applications with normative implications [57]:
Figure 2: Data Normalization Workflow
Table 4: Data Normalization Applications with Normative Implications
| Use Case | Technical Process | Normative Significance | Implementation Standards |
|---|---|---|---|
| Clinical Data Repositories | Semantic mapping to standardized terminologies (e.g., RxNorm) [57] | Enables identification of medication errors and redundant prescriptions; supports patient safety obligations | RxNorm, NDF-RT terminology standards |
| Evidence-Based Medicine | Normalization enables like-for-like comparison of outcomes across systems [57] | Facilitates fulfillment of obligation to provide care based on best available evidence | Systematic review methodologies, evidence grading systems |
| Drug Safety Surveillance | Normalized adverse event reporting to improve data mining capability [57] | Supports ethical obligation to monitor and address medication-related harms | FDA AERS standards, pharmacovigilance protocols |
| E-Prescribing Systems | Vocabulary standardization for meaningful use compliance [57] | Enhances medication safety through reduced communication errors | Meaningful Use requirements, interoperability standards |
Table 5: Research Reagent Solutions for Empirical Bioethics
| Tool Category | Specific Resources | Function in Research | Application Notes |
|---|---|---|---|
| Ethical Framework Guides | NIH Clinical Center Guiding Principles [9] | Provides foundational normative structure for research ethics | Should be explicitly referenced in research protocols |
| Integration Methodologies | Reflective Equilibrium, Dialogical Ethics, Grounded Moral Analysis [2] | Structured approaches for connecting empirical data to normative analysis | Selection should be justified based on research question and context |
| Data Standards | RxNorm, NDF-RT, Common Data Models [57] | Enable data normalization and interoperability | Essential for multi-site studies and data aggregation |
| Qualitative Analysis Tools | MAXQDA, NVivo, Dedoose | Support systematic analysis of qualitative data | Facilitates transparent and rigorous interpretation of textual data |
| Quantitative Analysis Tools | R, Python, SPSS, SAS | Enable statistical analysis of quantitative patterns | Supports identification of significant patterns and relationships |
| Protocol Development Resources | WHO Research Protocol Format [8] | Provides comprehensive structure for research planning | Ensures thorough consideration of methodological and ethical aspects |
Bridging the is-ought divide in empirical bioethics requires methodologically rigorous approaches that transparently connect empirical observations with normative conclusions. The protocols and application notes presented here provide structured pathways for this integration, emphasizing methodological transparency, iterative refinement, and respectful engagement with diverse perspectives. By adopting these structured approaches, researchers, scientists, and drug development professionals can contribute to an empirically informed bioethics that remains philosophically sophisticated while addressing pressing practical challenges in healthcare and research. The ongoing development and refinement of these methodologies represents a constructive response to Hume's challenge, enabling practical wisdom grounded in both empirical reality and ethical reflection.
Interdisciplinary collaboration in empirical bioethics research and drug development integrates diverse professional perspectives, yet this diversity is a primary source of conflict. These conflicts often originate in deeply embedded differences in professional training, disciplinary socialization, and approaches to clinical judgment [58]. In the clinical and research setting, such conflicts are not merely interpersonal but are often structural, stemming from divergent epistemologies and methodologies [59]. When poorly managed, they can impede research progress and compromise ethical integrity. A nuanced understanding of these roots enables the development of targeted protocols that move beyond transient dispute resolution to foster a sustainable culture of collaborative excellence. This document provides detailed application notes and experimental protocols, framed within a broader thesis on interdisciplinary empirical bioethics, to systematically identify, analyze, and resolve these conflicts.
Quantitative Data on Interdisciplinary Conflict and Resolution
Effective conflict resolution strategies must be informed by empirical data. The following tables summarize quantitative findings relevant to understanding motivators in collaborative projects and the assessment processes used to align interdisciplinary teams.
Table 1: Motivators for Interdisciplinary Collaborative Projects - This table synthesizes survey responses on factors motivating collaborative projects, illustrating the potential for divergent priorities across disciplines [60].
| Motivator | Percentage Indicating Factor was "Strong" | Confidence Interval (±) | Chi-Square Factor |
|---|---|---|---|
| Growth of library staff | 38.6% | 6.4 | 5.8 |
| Systematic assessment of library operations | 84.8% | 4.7 | 28.3 |
Table 2: Methodologies for Project Assessment and Alignment - This table shows the percentage of projects that employed specific assessment techniques to establish common ground and shared goals, a critical process for conflict mitigation [60].
| Assessment Activity | Percentage of Projects Conducting Activity | Confidence Interval (±) |
|---|---|---|
| Systematic assessment of operations | 84.8% | 4.7 |
| Space utilization analysis | Data Not Available | - |
| Formal post-occupancy evaluation | Data Not Available | - |
Experimental Protocols for Conflict Analysis and Resolution
Protocol for Mapping Disciplinary Epistemologies
Objective: To make explicit the often-implicit epistemological frameworks (e.g., quantitative/positivist vs. qualitative/constructivist) that team members from different disciplines bring to a research problem, thereby identifying a root cause of conflict [59].
Materials:
- Anonymous digital survey platform (e.g., Qualtrics, Google Forms)
- Data analysis software (e.g., SPSS, R, NVivo)
Procedure:
- Survey Design: Develop a survey asking participants to rate their agreement (on a 6-point Likert scale) with statements reflecting different epistemological stances.
- Example Statements:
- "The goal of research is to discover a single, objective truth."
- "Research findings are always interpreted and constructed, never purely discovered."
- "Statistical testing is the most reliable method for establishing evidence."
- "Narrative data is essential for understanding complex human phenomena."
- Example Statements:
- Participant Recruitment: Administer the survey to all members of the interdisciplinary team prior to the project's initiation phase.
- Data Analysis:
- Conduct cluster analysis on the response data to identify natural groupings of participants with similar epistemological profiles.
- Perform descriptive statistics (means, standard deviations) for each statement by disciplinary background (e.g., Medicine, Sociology, Philosophy, Statistics).
- Facilitated Workshop: Present the anonymized, aggregated results in a facilitated workshop. Use the data to spark structured discussion about how these differing starting points might influence the team's approach to research questions, study design, and data interpretation.
Protocol for Facilitative Bioethics Mediation
Objective: To resolve active, ethics-related conflicts through a structured facilitative process that helps parties reach a genuine consensus, distinguishing this from a consultant-led model where solutions are imposed [58].
Materials:
- Neutral meeting space or secure video-conferencing platform
- Trained facilitative mediator
Procedure:
- Intake and Agreement: The mediator meets individually with all primary parties to understand their perspectives and secure agreement to participate in the mediation process in good faith.
- Joint Session:
- The mediator establishes ground rules for respectful communication and confidentiality.
- Each party is given uninterrupted time to陈述 their perspective on the conflict, including underlying interests and concerns, not just stated positions.
- Issue Identification and Framing: The mediator helps the group collaboratively define the core points of disagreement, separating interpersonal issues from substantive methodological or ethical disputes.
- Option Generation: The mediator guides the parties in a brainstorming session to generate a wide range of potential solutions without initial judgment or evaluation.
- Negotiation and Agreement:
- Parties discuss the generated options, assessing them against shared interests and project goals.
- The mediator's role is to manage the process, not to recommend solutions. The parties themselves build the agreement [58].
- Documentation: The final consensus agreement is documented in writing, specifying actions, responsibilities, and timelines. This document is signed by all parties.
Visualization of Conflict Resolution Workflows
The following diagrams, generated with Graphviz, map the logical relationships and workflows in interdisciplinary conflict resolution.
Interdisciplinary Conflict Resolution Pathway
Empirical Bioethics Research Cycle
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Interdisciplinary Conflict Resolution Research - This table details key methodological tools and their functions for investigating and addressing interdisciplinary conflict.
| Item | Function / Explanation |
|---|---|
| Epistemology Survey | A validated instrument to quantify and map the epistemological stances (e.g., positivist, constructivist) of team members, identifying foundational sources of disagreement [59]. |
| Structured Interview Protocol | A semi-structured guide for conducting qualitative interviews to explore nuanced experiences of conflict, professional socialization, and clinical judgment. |
| Facilitative Mediation Framework | A structured process for a neutral third party to guide conflicting parties toward a self-generated consensus, distinct from a consultant who imposes a solution [58]. |
| Quantitative Data Analysis Software (e.g., R, SPSS) | Software for analyzing survey data, performing statistical tests (e.g., chi-square), and computing confidence intervals to objectively assess motivators and responses [60]. |
| Qualitative Data Analysis Software (e.g., NVivo) | Software for coding and thematically analyzing interview transcripts and field notes to identify emergent themes related to conflict roots. |
| Confidentiality Agreement Template | A legal document to ensure that all parties in a mediation or research study can speak freely, knowing their disclosures are protected. |
Application Notes
Empirical bioethics represents a advanced interdisciplinary field that integrates philosophical, qualitative social scientific, and legal methods of analysis to address complex challenges in healthcare and research [61]. The core challenge lies in achieving methodological rigor when integrating diverse datasets and disciplinary perspectives, particularly in avoiding vagueness in how qualitative empirical data informs normative ethical analysis. Penn Bioethics, a leader in the field for over 30 years, exemplifies this approach through work that ensures ethical analysis remains central to innovation and care [50]. This document provides structured protocols to enhance transparency, reliability, and validity in interdisciplinary integration techniques.
Foundational Principles of Rigor
Rigor in qualitative research design—a cornerstone of empirical bioethics—requires a clear and focused research question supported by a strong conceptual framework [62]. This framework must explicitly define and justify the research question, selected methodology, and interpretive perspectives [62]. Scholar reflexivity—where researchers maintain critical awareness of their own biases and decision-making rationales throughout the study—is paramount for rigor and must be documented at every stage, from research design through dissemination [62]. The Glassick Criteria provide six essential elements for assessing scholarly quality, beginning with clear purpose and adequate preparation, which are fundamental to formulating effective research questions and robust conceptual frameworks [62].
Experimental Protocols
Protocol: Iterative Research Question Development
Purpose: To transform broad interdisciplinary questions into focused, researchable inquiries while minimizing conceptual vagueness.
Procedure:
- Initial Formulation: Begin with a problem statement describing relationships between concepts, behaviors, or experiences observed in real-life settings [62].
- Systematic Literature Review: Conduct a thorough, systematic, and iterative review using the Glassick Criteria (clear purpose and adequate preparation) to establish context [62]. Actively identify and integrate key concepts, principles, theories, and prior evidence to establish what is known and unknown [62].
- FINER Refinement: Apply the FINER criteria (Feasible, Interesting, Novel, Ethical, and Relevant) to refine the question, ensuring it is answerable and researchable [62].
- Reflexivity Documentation: Document potential effects of researcher background, beliefs, and experiences on question formulation and any ethical considerations regarding how the question might influence study design and participants [62].
- Conceptual Framework Alignment: Actively construct a conceptual framework that provides a logical argument connecting the research question, selected methodology, and interpretation perspectives [62].
Validation: The final research question should demonstrate explicit alignment with all components of the conceptual framework and satisfy all FINER criteria.
Protocol: Data Integration for Normative Analysis
Purpose: To provide a systematic methodology for integrating empirical qualitative findings with philosophical analysis, addressing vagueness in how "is" informs "ought."
Procedure:
- Data Preparation: Transcribe and code qualitative data (e.g., from interviews, focus groups) using established qualitative methods. The coding process should be modified iteratively as needed to answer the research question [62].
- Thematic Extraction: Identify emergent themes and patterns through validated qualitative analysis.
- Ethical Framework Mapping: Map extracted themes against relevant ethical principles and frameworks (e.g., principlism, care ethics, virtue ethics).
- Deliberative Integration: Conduct structured deliberative sessions where interdisciplinary team members (e.g., ethicists, social scientists, clinicians) review mapped data to:
- Identify points of convergence and divergence between empirical findings and normative frameworks.
- Critically examine underlying assumptions and values present in the data.
- Co-construct ethically justifiable recommendations grounded in both empirical evidence and philosophical rigor [61].
- Documentation: Maintain detailed records of the deliberative process, including how disagreements were resolved and how final conclusions were reached.
Validation: Integration is successful when conclusions demonstrate clear, auditable pathways from empirical data through ethical analysis to normative conclusions.
Data Presentation
Standards of Rigor in Qualitative Research Design
Table 1: Quality Indicators and Best Practices for Qualitative Research Rigor [62]
| Quality Criterion | Definition | Operational Best Practice |
|---|---|---|
| Clear Purpose | Goals and objectives are clearly defined | Formulate a FINER (Feasible, Interesting, Novel, Ethical, Relevant) research question [62]. |
| Adequate Preparation | Understanding of existing scholarship and appropriate methods | Develop an explicit conceptual framework integrating relevant literature, concepts, and theories [62]. |
| Appropriate Methods | Selection and application of methods suited to the purpose | Choose methods that minimize bias and enhance trustworthiness of results; document iterative modifications [62]. |
| Effective Presentation | Communication of methods and findings is effective and appropriate | Apply best practices for visualizations (e.g., diagrams, charts) to enhance clarity and comprehension [63]. |
| Reflexive Practice | Critical self-assessment of researcher biases and influence | Maintain ongoing documentation of researcher reflexivity at all stages, from design to dissemination [62]. |
| Significant Results | Findings are meaningful and contribute to the field | Ensure work impacts ethical policy and practice through scientific inquiry and public-facing scholarship [50]. |
Comparative Analysis of Integration Techniques
Table 2: Approaches to Integrating Empirical Data and Ethical Analysis
| Integration Technique | Primary Function | Data Presentation Method | Protocol for Addressing Vagueness |
|---|---|---|---|
| Deliberative Dialogue | Facilitate co-construction of meaning across disciplines [61] | Charts to visualize thematic frequency; Tables for stakeholder positions | Structured meeting protocols with predefined discussion points and reflexive documentation. |
| Critical Reflexivity | Surface and examine disciplinary and researcher biases [62] | Reflexivity journals; Annotated conceptual frameworks | Mandatory documentation of bias and decision-making rationale at each research phase. |
| Concept-Process Mapping | Visualize relationships between empirical themes and ethical concepts | Node-link diagrams (e.g., DOT scripts) with high-contrast color palette | Explicitly labeled arrows and nodes defining the nature of each relationship [63]. |
| Iterative Framework Analysis | Systematically apply and refine ethical frameworks with data | Comparison tables showing framework application across data segments | Cross-disciplinary validation cycles to ensure consistent application of definitions and codes. |
Mandatory Visualization
Workflow for Rigorous Empirical Bioethics Integration
Conceptual Framework Development Process
The Scientist's Toolkit
Research Reagent Solutions for Empirical Bioethics
Table 3: Essential Methodological Resources for Interdisciplinary Research
| Research 'Reagent' | Function | Application in Empirical Bioethics |
|---|---|---|
| FINER Question Framework | Provides criteria (Feasible, Interesting, Novel, Ethical, Relevant) for formulating research questions [62] | Ensures research questions are answerable and ethically grounded from the outset. |
| Conceptual Framework Template | Structured approach for developing logical arguments connecting question, methods, and interpretation [62] | Creates explicit connections between empirical observations and normative frameworks, reducing vagueness. |
| Reflexivity Journal | Document for recording researcher biases, assumptions, and decision-making rationales [62] | Maintains transparency and critical self-awareness throughout the research process. |
| Deliberative Dialogue Guide | Protocol for structured interdisciplinary discussions [61] | Facilitates co-construction of knowledge between empirical researchers and ethicists. |
| Standards of Rigor Checklist | Quality indicators for qualitative research design (e.g., credibility, transferability) [62] | Ensures methodological trustworthiness and rigor in qualitative data collection and analysis. |
| Integration Mapping Tool | Visual method for linking empirical themes to ethical concepts [63] | Creates transparent audit trails showing how data informs ethical analysis. |
In interdisciplinary empirical bioethics research, the tension between achieving comprehensive thematic breadth and meaningful analytical depth presents a significant methodological challenge. Superficial analysis risks producing findings that are too generalized to offer substantive guidance for complex ethical dilemmas, while an excessively narrow focus may limit the relevance and applicability of the research. Thematic analysis (TA) provides a structured yet flexible framework for navigating this tension, offering a systematic approach to identifying, analyzing, and interpreting patterns of meaning across qualitative datasets [64]. When properly executed within empirical bioethics, this methodology enables researchers to develop ethically grounded insights that remain informed by the nuanced realities of healthcare practice and policy.
The iterative and reflexive nature of thematic analysis makes it particularly suited to empirical bioethics, where ethical reasoning must be continually informed and refined through engagement with empirical data [64]. This paper presents application notes and experimental protocols for implementing rigorous qualitative analysis that maintains both depth and breadth, specifically tailored to researchers, scientists, and drug development professionals working at the intersection of empirical research and ethical inquiry.
Core Principles for Balanced Qualitative Analysis
Philosophical and Methodological Foundations
The pursuit of balanced qualitative analysis in empirical bioethics rests on three foundational principles that inform both methodological design and execution:
Iterative Reflexivity: Researchers must actively engage with their theoretical positioning and biases throughout the analytical process, acknowledging how these perspectives shape interpretation [64]. This reflexive practice is particularly crucial in bioethics, where philosophical frameworks and personal values may unconsciously influence analysis of ethically charged data.
Methodological Cohesion: Empirical bioethics requires thoughtful integration of ethical analysis with social science research methods [61]. This integration must be intentional and transparent, with clear justification for how empirical findings inform ethical reasoning and vice versa.
Contextual Fidelity: Analytical approaches must preserve the context-rich nature of qualitative data, ensuring that ethical interpretations remain grounded in the specific circumstances, relationships, and institutional settings from which the data emerged [50]. As bioethics researchers increasingly recognize, "It is one thing to come up with the right answer in a sterile, hypothetical environment" and another to understand "how these conversations are actually happening on the ground" [50].
Structured Flexibility in Analytical Approaches
A common misconception in qualitative analysis suggests that structured approaches necessarily limit analytical depth. In practice, methodological frameworks provide the necessary foundation for managing complexity without constraining insight. Braun and Clarke's six-phase thematic analysis framework offers this structured flexibility through clearly defined phases that maintain analytical rigor while allowing adaptation to diverse research contexts [64]:
- Familiarization with data
- Generating initial codes
- Searching for themes
- Reviewing themes
- Defining and naming themes
- Writing the report
This phased approach enables researchers to manage large datasets systematically while remaining open to emergent insights and patterns. The framework's inherent adaptability makes it particularly valuable for empirical bioethics, where research questions may span clinical, research, and policy domains [64].
Application Notes: Analytical Protocols for Empirical Bioethics
Phase-Depth Integration Matrix
Successful balancing of breadth and depth requires strategic allocation of analytical attention throughout the research process. The following matrix outlines specific depth-enhancing practices for each standard phase of thematic analysis:
Table 1: Phase-Depth Integration Matrix for Thematic Analysis in Empirical Bioethics
| Analysis Phase | Breadth-Oriented Standard Practice | Depth-Enhancing Protocol for Bioethics |
|---|---|---|
| Data Familiarization | Reading and re-reading entire dataset | Contextual Immersion Protocol: Document initial ethical tensions; Create field effect maps noting power dynamics and relational contexts |
| Initial Coding | Systematic coding across entire dataset | Tiered Coding Protocol: First-pass descriptive coding + second-pass interpretative coding focused on moral reasoning and ethical dilemmas |
| Theme Development | Grouping codes into candidate themes | Dialogical Theme Development: Test candidate themes against contrasting ethical frameworks; Identify both concordant and divergent ethical perspectives |
| Theme Review | Checking themes against coded extracts and full dataset | Triangulation Review: Consult with interdisciplinary team; Validate with participant feedback where ethically appropriate |
| Theme Definition | Articulating essence and scope of each theme | Thick Description Protocol: Develop nuanced definitions capturing ethical complexity; Document boundary cases and exceptions |
| Reporting | Presenting analysis in coherent narrative | Integrated Discourse: Weave together empirical findings and ethical analysis with transparent reasoning |
Experimental Protocol: The Iterative Bioethical Reflection Method
The following detailed protocol adapts standard thematic analysis specifically for empirical bioethics research, incorporating systematic ethical reflection at multiple stages:
Protocol Title: Iterative Bioethical Reflection (IBR) Method for Qualitative Data Analysis
Version: 1.0
Developed for: Empirical bioethics research involving qualitative data collection (interviews, focus groups, observational field notes)
Materials Required:
- Primary qualitative dataset
- Research ethics framework (principilism, casuistry, virtue ethics, etc.)
- Coding software (NVivo, ATLAS.ti, MAXQDA) or manual coding system
- Reflexive journal for documenting analytical decisions
- Interdisciplinary team consultation schedule
Procedure:
Pre-Analysis Ethical Scaffolding (Duration: 1-2 weeks)
- Clearly articulate preliminary ethical concerns and questions driving the research
- Document relevant ethical frameworks, concepts, and principles that might inform analysis
- Establish interdisciplinary consultation team with expertise in ethics, qualitative methods, and substantive domain
- Create reflexive journal template with sections for methodological decisions, ethical dilemmas in analysis, and emerging insights
Data Immersion with Ethical Notetaking (Duration: 2-3 weeks)
- Conduct comprehensive reading/listening/viewing of dataset
- Create two parallel documentation systems:
- Substantive notetaking: Standard observational notes about content
- Ethical resonance mapping: Notes specifically documenting ethically significant moments, moral language, value conflicts, and normative assertions
- Hold initial interdisciplinary team meeting to discuss emerging ethical themes and analytical approach
Multi-Dimensional Coding (Duration: 3-4 weeks)
- Perform first-cycle coding using elemental methods (descriptive, in vivo, process coding)
- Conduct second-cycle coding focused specifically on:
- Moral reasoning patterns: How participants justify decisions or actions
- Ethical tensions: Points of conflict between values, principles, or obligations
- Implicit normative claims: Unstated values or assumptions embedded in descriptions
- Create a codebook with clear definitions and examples for each code
Theme Development with Ethical Integration (Duration: 2-3 weeks)
- Group related codes into candidate themes using thematic mapping
- For each candidate theme, document:
- Empirical substantiation (evidence across dataset)
- Ethical significance (relationship to bioethics literature and concepts)
- Practical implications for healthcare practice or policy
- Test theme robustness against different ethical frameworks
- Refine themes through team discussion and return to raw data
Validation and Integration (Duration: 2 weeks)
- Conduct member validation sessions (where appropriate and ethically justified)
- Present preliminary analysis to interdisciplinary team for critique
- Finalize thematic structure and develop analytical narrative
- Write research report with transparent accounting of how empirical findings and ethical analysis inform each other
Quality Assurance Measures:
- Maintain audit trail of all analytical decisions
- Document how ethical frameworks informed interpretation
- Actively seek disconfirming evidence and alternative explanations
- Ensure proportional representation of diverse perspectives in analysis
Visualization of Analytical Workflows
Integrated Empirical Bioethics Analysis Workflow
The following diagram illustrates the comprehensive workflow for balancing depth and breadth in qualitative analysis for empirical bioethics, highlighting the iterative nature of the process and key integration points:
Diagram 1: Integrated Empirical Bioethics Analysis Workflow showing depth and breadth protocols
Multi-Dimensional Coding Strategy
The coding process represents a critical juncture where depth and breadth must be strategically balanced. The following visualization details the tiered approach to coding that enables comprehensive coverage while facilitating deep analytical insight:
Diagram 2: Multi-Dimensional Coding Strategy for balancing comprehensive coverage and ethical depth
The Scientist's Toolkit: Essential Research Reagents
Methodological Reagents for Empirical Bioethics
Successful implementation of balanced qualitative analysis in empirical bioethics requires specific methodological tools and frameworks. The following table details essential "research reagents" for maintaining both depth and breadth throughout the analytical process:
Table 2: Essential Research Reagents for Balanced Qualitative Analysis in Empirical Bioethics
| Research Reagent | Function | Protocol for Application |
|---|---|---|
| Braun & Clarke Thematic Analysis Framework | Provides structured six-phase approach to qualitative analysis [64] | Implement all six phases (familiarization, coding, theme development, review, definition, reporting) while maintaining reflexive adaptation to research context |
| Interdisciplinary Consultation Team | Ensures integration of ethical analysis with empirical findings [61] | Schedule regular consultations throughout analysis; Create structured feedback protocols for ethical and methodological review |
| Reflexive Journaling System | Documents analytical decisions, ethical tensions, and emerging insights | Maintain detailed records of coding decisions, theme development, and ethical reflections; Review periodically to identify potential biases |
| Qualitative Data Analysis Software (NVivo, ATLAS.ti, MAXQDA) | Manages and organizes large qualitative datasets [65] | Use for systematic coding, memoing, and theme development; Leverage query functions to test analytical hypotheses across dataset |
| SRQR Reporting Guidelines | Ensures comprehensive and transparent reporting of qualitative research [66] | Use as checklist during writing phase to ensure methodological transparency and analytical rigor |
| Ethical Framework Mapping Tool | Connects empirical findings with bioethics concepts and theories | Create visual maps linking empirical themes to relevant ethical frameworks, principles, and theoretical concepts |
| Member Validation Protocol | Tests interpretive validity with participants [65] | Develop structured approach for participant feedback on preliminary analysis; Address ethical considerations of re-engagement |
Quality Assurance Reagents
The following specialized tools address specific challenges in maintaining analytical rigor while balancing depth and breadth:
Table 3: Quality Assurance Reagents for Analytical Rigor
| Quality Assurance Reagent | Function | Application in Empirical Bioethics |
|---|---|---|
| Theme Robustness Assessment Tool | Tests stability and coherence of themes across dataset | Apply systematic challenges to each theme: search for disconfirming evidence, test against alternative explanations, assess conceptual boundaries |
| Ethical Triangulation Matrix | Validates ethical interpretations through multiple perspectives | Cross-reference ethical analysis with different theoretical frameworks, stakeholder positions, and methodological approaches |
| Analytical Depth Audit Protocol | Ensures sufficient interpretive depth beyond surface descriptions | Implement staged review process assessing movement from descriptive to interpretive to ethical analytical levels |
| Breadth Validation Checklist | Confirms comprehensive engagement with dataset | Systematically check that all data segments have been appropriately considered and that minority perspectives are represented |
Analytical Integration Protocols
Empirical-Ethical Integration Framework
The unique challenge in empirical bioethics lies in meaningfully integrating empirical findings with ethical analysis. The following protocol provides a structured approach to this integration:
Protocol Title: Dialogical Integration of Empirical and Ethical Analysis
Purpose: To facilitate deep integration between empirical findings and ethical reasoning while maintaining comprehensive engagement with the full dataset
Materials:
- Coded qualitative dataset
- Preliminary thematic structure
- Relevant bioethics literature
- Interdisciplinary team members
- Visualization tools (whiteboard, digital mapping software)
Procedure:
Empirical Theme Elaboration (Duration: 1 week)
- Develop detailed descriptions of each empirical theme with supporting evidence
- Document variations, boundary cases, and relationships between themes
- Identify areas where empirical data presents ethical questions or tensions
Ethical Framework Alignment (Duration: 1-2 weeks)
- Map empirical themes against relevant ethical frameworks, concepts, and principles
- Identify points of convergence and divergence between empirical findings and existing ethical literature
- Document how empirical data challenges, refines, or extends current ethical understanding
Iterative Dialogue Sessions (Duration: 2-3 weeks)
- Conduct structured discussions between empirical researchers and ethics scholars
- Focus on areas where empirical findings and ethical analysis interface
- Develop integrated interpretations that honor both empirical complexity and ethical reasoning
- Document the dialogue process and analytical developments
Integrated Analysis Validation (Duration: 1 week)
- Test integrated analysis against full dataset
- Assess coherence and explanatory power of integrated interpretations
- Refine analysis based on validation process
Outcome Measures:
- Demonstrated movement between empirical data and ethical concepts
- Transparent accounting of how integration was achieved
- Clearly articulated ethical insights informed by empirical evidence
- Documentation of how integration enhances understanding of research problem
Balancing depth and breadth in qualitative analysis for empirical bioethics requires intentional methodological strategies that prioritize both comprehensive engagement with data and deep ethical reasoning. The application notes and protocols presented here provide concrete approaches for maintaining this balance throughout the research process, specifically tailored to the interdisciplinary nature of bioethics inquiry. By implementing structured yet flexible frameworks like the Iterative Bioethical Reflection Method and utilizing the essential research reagents outlined, researchers can produce findings that are both empirically robust and ethically insightful.
As the field of empirical bioethics continues to evolve, methodological transparency and rigor become increasingly critical. The approaches detailed here offer pathways for avoiding superficiality while doing justice to the complex ethical questions that arise in healthcare, research, and policy contexts. Through continued refinement of these methodological frameworks, empirical bioethics can fulfill its potential to address pressing ethical challenges with both scholarly rigor and practical relevance.
Application Notes: Principles for Inclusive Deliberation
In the context of interdisciplinary empirical bioethics research, managing dominant discourses is critical for ensuring that ethical deliberations are inclusive and representative of diverse perspectives, rather than being skewed by existing social or professional power dynamics.
A primary challenge in deliberation is the potential for "domination by the more advantaged", where participants with higher social status, greater education, or professional authority can disproportionately influence the discussion and outcomes [67]. This undermines the democratic ideal of deliberation, which relies on the "unforced force of the better argument" rather than social privilege [67]. In bioethics, where deliberations can influence health research protocols and policies, ensuring equitable participation is both a methodological and an ethical imperative.
Empirical studies reveal that socially advantaged participants often speak in ways that align more favorably with traditional deliberative standards, which emphasize rational justifiability and formal discourse [67]. Furthermore, specific groups may face representation disadvantages; for example, identical arguments from a female-passing character were found to carry less authority than those from a male-passing character [67]. The structure of the deliberation itself—whether online or in-person—can also impact participation dynamics and the quality of discourse [68].
The core objective for researchers is to create deliberative spaces where a multiplicity of values and preferences can be expressed, reciprocal interactions are encouraged, and the final recommendations reflect a societal—not just individual—perspective [68]. The following protocols are designed to operationalize these principles within empirical bioethics research.
Experimental Protocols and Methodologies
Protocol for a Deliberative Forum on a Bioethics Topic
This protocol provides a structured methodology for conducting an inclusive deliberative forum, suitable for topics in health research and bioethics. The stages are designed to mitigate dominance and foster equitable participation.
Detailed Procedural Steps
Recruitment and Preparation: Recruit a diverse pool of participants (e.g., researchers, clinicians, patients, community members) through purposive sampling to ensure representation across relevant demographics, professional backgrounds, and perspectives [68]. Secure a neutral venue or a robust online platform (e.g., Zoom) that is accessible to all. Obtain ethical approval and informed consent [68].
Pre-Deliberation Survey: Administer a survey to collect baseline data on participants' demographics, initial opinions on the topic, and knowledge levels [67]. This data is crucial for measuring opinion shifts post-deliberation.
Distribution of Briefing Materials: Provide all participants with balanced, accessible briefing materials that cover the key scientific, ethical, and policy dimensions of the topic. These materials should be vetted for clarity and lack of bias.
Expert Presentations and Q&A: Host sessions where domain and method experts (e.g., bioethicists, data scientists, clinicians) present information. This follows the model of "Shaping Our Future" Deliberative Polls and community juries, where expert presentations enhance participant knowledge [67] [68]. A moderated Q&A session allows participants to clarify information.
Facilitated Discussion: Researchers or trained facilitators guide an initial discussion to help jurors think through the topic. The facilitator's role is to ensure that conversation remains respectful, that airtime is distributed equitably, and that quieter participants are encouraged to speak [68].
Unfacilitated Deliberation: The facilitators leave the room or turn off their cameras and microphones. Participants deliberate among themselves to reach a consensus or verdict on the research questions, which have been provided both verbally and in writing [68]. This step is critical for assessing the group's own capacity for self-governance and minimizing facilitator influence.
Post-Deliberation Survey: Re-administer the opinion and knowledge survey to quantify changes in attitudes and understanding resulting from the deliberative process [67].
Analysis and Synthesis: Transcribe and analyze the deliberation recordings. Use a mixed-methods approach, combining quantitative analysis of survey data with qualitative framework analysis of the discourse [67] [68].
Protocol for Quantifying Discourse and Dominance
This protocol outlines a method for empirically investigating the relationship between social advantage and deliberative participation using transcripts, as demonstrated in recent research [67].
Data Collection and Processing
- Data Source: Collect verbatim transcripts from deliberative forums [67] [68].
- Units of Analysis: Define each participant's speech (a contiguous utterance) as a unit. Nest speeches within participants, and participants within discussion groups for hierarchical analysis [67].
- Social Advantage Metrics: Gather demographic data (e.g., gender, education level, professional status) via pre-deliberation surveys. These serve as proxies for social advantage [67].
Quantitative and Qualitative Metrics
The following table summarizes key metrics for assessing deliberation quality and participation inequality, drawing from established frameworks [67] [68].
Table 1: Metrics for Assessing Deliberative Quality and Dominance
| Category | Metric | Description / Operationalization | Data Source |
|---|---|---|---|
| Participation | Speaking Time/Frequency | Number of speeches or total words per participant. | Transcripts [67] |
| Turn-Taking Dynamics | Analysis of interruption patterns and conversational dominance. | Transcripts | |
| Deliberative Quality | Level of Justification | Frequency of reasoned arguments (e.g., use of "because" statements). | Transcripts, LLM/LIWC [67] |
| Common Good Orientation | References to societal welfare vs. individual interest. | Transcripts, Dictionary Methods [67] | |
| Reciprocity & Respect | Engagement with others' views (agreement, clarification, challenging). | Deductive Coding [68] | |
| Outcome & Influence | Opinion Change | Shift in pre- and post-deliberation survey responses. | Survey Data [67] |
| Recommendation Quality | Clarity, justification, and adoption of a societal perspective. | Deliberation Output [68] |
Analytical Procedures
- Transcript Coding: Use a combination of methods:
- Dictionary-Based Methods/Traditional Coding: Apply a pre-defined coding framework to assess deliberative goals, such as expression of values, use of expert information, and consideration of societal perspective [68].
- Machine Learning (ML) & Large Language Models (LLMs): Employ these tools to analyze large volumes of text (e.g., 9,810 speeches) for patterns in speech related to deliberative quality and logical reasoning [67] [69].
- Statistical Modeling: Use regression models, such as Zero-Inflated Poisson models (for count data like speech acts) and Zero-Inflated Beta regression (for proportional data), to test hypotheses about the relationship between social advantage and deliberative metrics [67].
- Network Analysis (Optional): For complex multi-stakeholder deliberations, model influence using network analysis. "Dangling Centrality" is a novel metric that can identify critical nodes (participants) whose absence would disrupt the network's communication flow, highlighting their structural importance [70].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for Empirical Deliberative Research
| Item | Function in Research | Example / Specification |
|---|---|---|
| Video Conferencing Software | Hosting online deliberative forums; ensures geographical diversity and recording capabilities. | Zoom, Microsoft Teams [68] |
| Qualitative Data Analysis Software | Organizing, managing, and coding large volumes of textual transcript data. | NVivo, Dedoose [68] |
| Deductive Coding Framework | A structured set of codes to assess the quality of deliberations against predefined goals. | Framework with goals like "Expressing values," "Reciprocal interactions," "Use of expert information" [68] |
| Linguistic Inquiry and Word Count (LIWC) | Dictionary-based software for automated text analysis of psychological, social, and deliberative constructs in speech. | LIWC dictionaries [67] |
| Large Language Models (LLMs) | Analyzing vast numbers of speeches for deliberative quality (e.g., logical reasoning) when manual coding is infeasible. | Pretrained LLMs (e.g., GPT) [67] [69] |
| Statistical Software | Conducting advanced statistical analyses, including regression modeling of participation data. | R, Python, Stata [67] |
| Social Network Analysis (SNA) Tools | Modeling and visualizing influence and communication patterns among participants in a deliberation. | Tools for calculating centrality metrics (e.g., Dangling Centrality) [70] |
Measuring Impact: Validating Methods and Comparing Outcomes in Empirical Bioethics
The field of bioethics has undergone a significant transformation, transitioning from a discipline focused primarily on philosophical inquiry to one that embraces interdisciplinary approaches and methodological diversity [10]. This "empirical turn" reflects a growing recognition that complex bioethical issues require not only normative analysis but also empirical investigation of real-world contexts, practices, and stakeholder perspectives. The rise of empirical bioethics research represents a fundamental shift in how bioethicists approach their work, bridging the traditional divide between the "is" of empirical description and the "ought" of ethical prescription [6]. As the field has evolved, a crucial question has emerged: Which objectives of empirical research in bioethics (ERiB) do researchers themselves find most acceptable and legitimate?
This application note explores researcher perspectives on acceptable objectives for empirical bioethics research, framing the discussion within the context of interdisciplinary methodologies and their application to drug development, clinical practice, and healthcare policy. By synthesizing qualitative and quantitative findings from recent studies, we provide a comprehensive overview of the current landscape of empirical bioethics, along with practical protocols for implementing these approaches in research settings.
The Evolving Landscape of Empirical Bioethics Research
Quantitative Growth of Empirical Approaches
Empirical research in bioethics has demonstrated substantial growth over recent decades. A comprehensive analysis of nine peer-reviewed bioethics journals from 1990 to 2003 revealed that publications employing empirical designs increased significantly from 5.4% in 1990 to 15.4% in 2003 (χ² = 49.0264, p<.0001) [11]. This trend has likely accelerated in recent years, reflecting the increasing legitimacy and value ascribed to empirical approaches within the field.
Table 1: Prevalence of Empirical Research in Bioethics Journals (1990-2003)
| Journal | Total Articles | Empirical Studies | Percentage |
|---|---|---|---|
| Nursing Ethics | 367 | 145 | 39.5% |
| Journal of Medical Ethics | 762 | 128 | 16.8% |
| Journal of Clinical Ethics | 604 | 93 | 15.4% |
| Bioethics | 332 | 22 | 6.6% |
| Other Journals | 1964 | 47 | 2.4% |
| Total | 4029 | 435 | 10.8% |
The distribution of empirical research across journals reveals important disciplinary patterns, with Nursing Ethics publishing the highest proportion of empirical studies (39.5%), followed by the Journal of Medical Ethics (16.8%) and the Journal of Clinical Ethics (15.4%) [11]. These three journals collectively accounted for 84.1% of all empirical research in bioethics during this period.
Methodological Approaches in Empirical Bioethics
The methodological landscape of empirical bioethics is characterized by diversity, with researchers employing both qualitative and quantitative approaches:
- Quantitative dominance: 64.6% of empirical studies employed quantitative methodologies [11]
- Qualitative value: Qualitative methods are particularly valued for understanding "values, personal perspectives, experiences, and contextual circumstances" [11]
- Emerging digital methods: Recent developments include interactive visualizations and digital platforms for empirical bioethics research [71] [72]
The choice of methodology often reflects the research objective, with quantitative approaches frequently used for "Lay of the Land" studies and qualitative methods applied to explore lived experiences and contextual factors.
Researcher Perspectives on Acceptable Objectives
Hierarchy of Acceptability
A recent qualitative study exploring researchers' views on acceptable objectives for empirical bioethics research revealed a clear hierarchy of acceptability [10]. Researchers evaluated eight distinct objectives, demonstrating varying levels of agreement based on their experience with interdisciplinary work.
Table 2: Researcher Perspectives on Objectives of Empirical Bioethics Research
| Research Objective | Degree of Acceptance | Key Characteristics |
|---|---|---|
| Understanding the context of a bioethical issue | Unanimous agreement | Foundational, descriptive, minimally controversial |
| Identifying ethical issues in practice | Unanimous agreement | Practice-oriented, descriptive, identifies real-world problems |
| Evaluating how ethical recommendations work in practice | High agreement | Assesses implementation, bridges theory-practice gap |
| Informing policy | High agreement | Practical application, policy-relevant |
| Providing a source of morality | Moderate agreement | Ambitious, conceptually challenging |
| Drawing normative recommendations | Contested | Normatively ambitious, faces is-ought challenges |
| Developing and justifying moral principles | Most contested | Theoretically ambitious, direct engagement with normative foundations |
The findings reveal a clear pattern: researchers view more modest, descriptive objectives as most acceptable, while ambitious normative objectives generate greater controversy and disagreement [10]. Objectives focused on producing empirical results without direct normative implications received strongest support, while those aiming to develop or justify moral principles faced significant skepticism.
The Is-Ought Question in Practice
The traditional philosophical challenge of deriving "ought" from "is" emerged as a significant theme in researcher perspectives. However, participants in the qualitative study generally did not view the is-ought gap as an absolute barrier to empirical bioethics research [10]. Instead, they treated it as:
- A warning sign prompting critical reflection on normative implications
- A methodological challenge requiring careful research design
- A consideration for transparently acknowledging limitations
This practical approach to the is-ought question reflects the evolving nature of bioethics as an interdisciplinary field that must navigate traditional philosophical concerns while addressing real-world ethical problems.
Conceptual Framework: Classifying Empirical Bioethics Research
Hierarchical Classification System
Kon (2009) proposed a hierarchical framework for classifying empirical research in bioethics, consisting of four distinct levels that build upon one another [6]. This framework provides a valuable structure for understanding how different research objectives relate to one another and contribute to the field.
This hierarchical model illustrates how empirical bioethics research can progress from foundational descriptive work to more ambitious normative contributions. The framework acknowledges that different research objectives are appropriate for different stages of investigation and carry distinct implications for the relationship between empirical data and normative analysis.
Research Objectives and Methodological Alignment
Different research objectives typically align with specific methodological approaches and levels within the hierarchical framework:
- Lay of the Land studies (Level 1): Map current practices, opinions, or beliefs using descriptive quantitative or qualitative methods [6]
- Ideal Versus Reality studies (Level 2): Compare actual practices with ethical ideals using hypothesis-driven approaches [6]
- Improving Care studies (Level 3): Develop and evaluate interventions to bridge gaps between reality and ideals [6]
- Changing Ethical Norms (Level 4): Synthesize empirical findings to inform ethical norms and principles [6]
This alignment between objectives and methodologies provides guidance for researchers in selecting appropriate approaches for their specific research questions.
Experimental Protocols for Empirical Bioethics Research
Protocol 1: Qualitative Exploration of Researcher Perspectives
Objective: To explore researchers' views on acceptable objectives for empirical bioethics research.
Methodology Adapted from Mihailov et al. (2022) [10]:
Participant Sampling:
- Conduct systematic literature search in PubMed and SCOPUS using key terms: "Empirical Bioethics," "Empirical Ethics," "Interdisciplinary Ethics"
- Apply inclusion/exclusion criteria to identify relevant publications
- Categorize publications into: (a) Empirical, (b) Methodological, (c) Empirical-Argumentative
- Use random selection within categories to identify first authors for recruitment
- Aim for balanced representation of gender, career stage, and geographical location
Data Collection:
- Develop semi-structured interview guide with three sections:
- Researcher background and experience
- Attitudes toward eight specific ERiB objectives
- Experiences with and challenges of doing empirical bioethics
- Conduct interviews via videoconference (45-90 minutes duration)
- Audio record and transcribe verbatim
- Develop semi-structured interview guide with three sections:
Data Analysis:
- Use thematic analysis framework following Braun and Clarke (2006)
- Employ iterative coding process with multiple coders
- Develop themes and subthemes through research team discussion
- Ensure methodological transparency through audit trail
Applications: This protocol is suitable for investigating disciplinary norms, methodological preferences, and epistemological attitudes within bioethics and related fields.
Protocol 2: Scoping Review of Empirical Research
Objective: To map and characterize existing empirical research on a specific bioethics topic.
Methodology Adapted from Anderson et al. (2025) [73]:
Research Question Formulation:
- Define primary research question and specific sub-questions
- Identify key concepts and variables of interest
Search Strategy:
- Conduct systematic searches across multiple databases (PubMed, PsychINFO, Scopus, Google Scholar)
- Combine terms related to the specific bioethics topic with methodological terms
- Supplement with hand-searching of key journals and citation tracking
Study Selection:
- Develop explicit inclusion/exclusion criteria
- Use multiple reviewers for title/abstract screening and full-text review
- Resolve disagreements through consensus or third-party adjudication
Data Charting:
- Develop standardized data extraction form
- Extract relevant descriptive and methodological characteristics
- Include numerical and thematic analysis as appropriate
Synthesis and Reporting:
- Collate and summarize findings according to research questions
- Identify gaps in the literature
- Present results using descriptive statistics and narrative synthesis
Applications: This protocol is valuable for mapping research landscapes, identifying methodological trends, and establishing foundations for future empirical studies.
Research Reagent Solutions for Empirical Bioethics
Table 3: Essential Methodological Resources for Empirical Bioethics Research
| Tool/Resource | Function | Application Context |
|---|---|---|
| Semi-structured interview guides | Elicit researcher or stakeholder perspectives | Qualitative studies of professional practices or ethical dilemmas |
| Thematic analysis framework | Analyze qualitative data systematically | Identifying patterns in interview or focus group transcripts |
| Reflective equilibrium | Integrate empirical findings with normative analysis | Methodological approach for bridging is-ought gap [2] |
| Digital data collection platforms | Facilitate online data collection and management | Large-scale surveys or distributed collaborative research [72] |
| Interactive visualizations | Translate ethical frameworks into accessible formats | Ethics education and stakeholder engagement [71] |
| Mixed methods designs | Combine qualitative and quantitative approaches | Comprehensive investigation of complex bioethical issues |
| Scoping review methodology | Map existing literature and identify research gaps | Foundation for new research programs or systematic reviews [73] |
Integration Methodologies for Empirical Bioethics
A systematic review identified 32 distinct methodologies for integrating empirical and normative approaches in bioethics [2]. The most prominent include:
- Reflective Equilibrium: A back-and-forth process between ethical principles and empirical data to achieve moral coherence [2]
- Dialogical Empirical Ethics: Relies on stakeholder dialogue to reach shared understanding and normative conclusions [2]
- Grounded Moral Analysis: Develops normative positions through systematic analysis of empirical data [2]
Researchers report that the process of integration often remains vague and uncertain in practice, highlighting the need for more explicit methodological development and reporting [2].
Implementation Workflow for Empirical Bioethics Studies
The following workflow diagram illustrates the key stages in designing and implementing an empirical bioethics research project, from conceptualization through to dissemination:
This workflow emphasizes the importance of carefully considering research objectives at the outset, selecting appropriate methodological approaches, and explicitly addressing the relationship between empirical data and normative analysis throughout the research process.
Researcher perspectives on acceptable objectives for empirical bioethics reveal a field that values empirical investigation while maintaining critical awareness of its philosophical foundations and limitations. The clear preference for modest, descriptive objectives over ambitious normative aims reflects both practical and theoretical considerations, including ongoing engagement with the is-ought problem.
Future development in empirical bioethics will likely focus on:
- Refining integration methodologies to address current vagueness and uncertainty [2]
- Developing digital tools and platforms to facilitate empirical research [72]
- Enhancing interdisciplinary collaboration between ethicists, social scientists, and healthcare professionals [10]
- Addressing global health ethics and expanding beyond current Western-centric focus [11] [73]
As empirical approaches continue to evolve within bioethics, researcher perspectives on acceptable objectives will likely become more nuanced, potentially embracing more ambitious normative goals while maintaining methodological rigor and philosophical sophistication.
The field of bioethics is experiencing a significant transformation, marked by an increasing integration of empirical research methods with traditional normative analysis. This "empirical turn" represents a fundamental shift toward interdisciplinary scholarship that combines philosophical inquiry with data-driven approaches from the social sciences [3]. Historical analysis reveals that the proportion of empirical studies in leading bioethics journals has steadily increased from 5.4% in 1990 to 15.4% in 2003, demonstrating a growing methodological evolution within the field [11]. This interdisciplinary approach acknowledges that complex bioethical challenges require not only theoretical reflection but also empirical understanding of real-world contexts, stakeholder perspectives, and practical implementation challenges.
Contemporary bioethics now engages with rapid technological advancements in artificial intelligence, gene editing, and biotechnology, while simultaneously addressing persistent healthcare disparities affecting marginalized populations [23]. This expanding scope necessitates robust methodological frameworks that can accommodate both normative and empirical dimensions. However, this integration presents significant challenges for establishing and maintaining scholarly rigor. Researchers must navigate diverse epistemological traditions, methodological standards, and theoretical frameworks while developing approaches that respect the integrity of both normative and empirical disciplines [3]. This article identifies five core challenges in establishing rigor within this emerging interdisciplinary field and provides practical protocols to address them.
Core Challenges and Analytical Framework
The Methodological Pluralism Challenge
Interdisciplinary bioethics research draws upon diverse methodological traditions, creating fundamental tensions between disciplinary standards and practices. A survey of European bioethics researchers revealed that 87.5% use empirical methods in their work, yet significant training gaps exist—approximately 22.9% of empirical researchers had received no formal methodological training in the methods they employed [3]. This training deficit poses a substantial threat to methodological rigor, as researchers may lack the expertise to properly design, implement, and interpret empirical studies.
The table below illustrates the methodological landscape and training disparities among bioethics researchers:
Table 1: Methodological Training and Application Among Bioethics Researchers
| Aspect | Finding | Implication for Rigor |
|---|---|---|
| Empirical Method Use | 87.5% of researchers use or have used empirical methods [3] | High engagement with empirical approaches necessitates quality standards |
| Interdisciplinary Background | 16% of researchers have combined educational backgrounds (e.g., philosophy and psychology) [3] | Diverse training creates potential for methodological innovation |
| Methodological Training Gaps | 22.9% of empirical researchers had no methodological training; only 6% self-identified as experts in methods they used [3] | Significant risk of inadequate methodological execution and interpretation |
| Qualitative Methods Training | 61.0% received at least some qualitative methods training [3] | Substantial portion may lack formal qualitative research skills |
| Quantitative Methods Training | 59.0% received at least some quantitative methods training [3] | Substantial portion may lack formal quantitative research skills |
The Integration Challenge
A fundamental challenge in empirical bioethics concerns how to effectively integrate normative analysis with empirical findings. This integration remains methodologically underdeveloped, with only 35% of researchers reporting successful integration in completed projects, though 59.8% planned to do so in current work [3]. This aspiration-integration gap highlights the methodological difficulties in achieving meaningful synthesis between these distinct modes of inquiry.
The integration challenge stems from epistemological differences between normative and empirical approaches. Normative analysis typically deals with prescriptive questions (what ought to be), while empirical research addresses descriptive questions (what is). Without thoughtful integration, empirical bioethics risks committing the "naturalistic fallacy" of deriving normative conclusions directly from empirical data without sufficient philosophical justification [3]. The field has developed numerous approaches to bridge this divide, with scholars identifying at least 32 distinct methodologies for integrating empirical and normative dimensions, though no consensus exists on optimal approaches [3].
The Interdisciplinary Communication Challenge
Effective interdisciplinary collaboration requires researchers to articulate their disciplinary assumptions, methods, and limitations to colleagues from different backgrounds. This necessitates developing meta-cognitive skills that enable researchers to understand and communicate their own thought processes and methodological approaches [74]. The Institute for Interdisciplinary Studies (IIS) model addresses this challenge by emphasizing communication and collaboration throughout the research process, recognizing that interdisciplinary work requires more continuous reflection than traditional disciplinary research [74].
Process mapping techniques adapted from systems science offer one promising approach to facilitate interdisciplinary communication. These methods help research teams visually represent complex processes "as envisioned" by different disciplines and "as realized" in practice, identifying points of conceptual divergence and convergence [75]. By making implicit assumptions explicit, these techniques help bridge disciplinary divides and create shared conceptual frameworks for interdisciplinary collaboration.
The Methodological Rigor Challenge
Ensuring methodological rigor in interdisciplinary bioethics requires adhering to quality standards from multiple disciplinary traditions. Scholars have emphasized that integrated empirical-normative research must comply with two distinct quality standards: the standards of rigorous conceptual analysis characteristic of philosophical ethics and the epistemological standards of the empirical disciplines whose methods are employed [3]. This dual requirement creates unique challenges for researchers who must demonstrate competence across methodological domains.
The field has witnessed concerns about the quality of empirical work in bioethics, with doubts raised about whether studies meet established social scientific standards for research design, data collection, and analysis [3]. This concern is particularly acute given the training gaps identified among bioethics researchers employing empirical methods. Without adequate methodological expertise, researchers risk producing empirical work that lacks reliability, validity, or generalizability, thereby undermining the normative conclusions drawn from it.
The Institutional Recognition Challenge
Interdisciplinary bioethics faces challenges in gaining full institutional recognition within traditional academic structures organized around disciplinary boundaries. This manifests in curriculum design, funding mechanisms, and promotion criteria that may not adequately value interdisciplinary work. Educational programs must balance disciplinary depth with interdisciplinary breadth, preparing students to navigate multiple methodological traditions while developing specialized expertise [74].
The empirical bioethics summer school model represents one response to this challenge, providing specialized training for researchers already familiar with basic bioethics concepts [76]. Such initiatives create spaces for developing interdisciplinary methodological competence outside traditional departmental structures. However, broader institutional recognition requires developing evaluation criteria that appropriately assess the quality and impact of interdisciplinary work, acknowledging its distinct methodologies and contributions.
Experimental Protocols for Interdisciplinary Bioethics Research
Protocol 1: Multi-Method Process Mapping for Implementation Ethics
This protocol adapts process mapping techniques from implementation science to identify and analyze ethical challenges in healthcare delivery systems [75]. The approach is particularly valuable for studying "ad hoc modifications" to protocol-driven interventions, where frontline providers deviate from established protocols in response to contextual factors.
Research Materials and Equipment
Table 2: Research Reagent Solutions for Process Mapping
| Item | Function | Application Notes |
|---|---|---|
| Focus Group Guide | Elicits implementation team perspectives on process "as envisioned" | Includes structured activities for individual and collective process mapping [75] |
| Semi-Structured Interview Protocol | Captures frontline administrator experiences of process "as realized" | Incorporates guided process mapping activity to identify actual practices [75] |
| Process Mapping Templates | Visualizes sequential steps in intervention implementation | Uses standardized symbols for decision points, actions, and outputs [75] |
| FRAME Coding Framework | Systematically characterizes modifications | Documents content, context, and motivations for adaptations [75] |
| Member-Checking Protocol | Validates preliminary findings with stakeholders | Uses focus groups to present synthesized process maps for verification [75] |
Procedural Workflow
Implementation Notes
- Sampling Strategy: Employ purposive sampling to include both implementation team members (those who designed the protocol) and frontline administrators (those who implement it) [75]
- Data Collection: Conduct focus groups with implementation teams to develop consensus process maps "as envisioned." Follow with semi-structured interviews incorporating process mapping activities with frontline administrators to identify processes "as realized" [75]
- Analysis: Use constant comparison analysis to identify discrepancies between envisioned and realized processes. Code identified modifications using the Framework for Reporting Adaptations and Modifications-Enhanced (FRAME) to characterize content, context, and motivations [75]
- Integration: Analyze identified modifications for their ethical implications, considering how deviations from protocols affect core ethical principles including autonomy, beneficence, and justice [23]
Protocol 2: Integrated Empirical-Normative Analysis Framework
This protocol provides a structured approach for integrating empirical findings with normative analysis, addressing a key methodological challenge in interdisciplinary bioethics research.
Procedural Workflow
Implementation Notes
- Iterative Design: The process is deliberately iterative, allowing movement between phases as empirical findings inform normative analysis and vice versa [74]
- Methodological Triangulation: Employ mixed methods to capture both breadth (through quantitative approaches) and depth (through qualitative approaches) of the phenomenon under study [3]
- Explicit Integration: Create specific "integration points" in the research process where empirical findings and normative analysis are systematically brought into conversation, documenting how each informs the other
- Reflexivity: Maintain a reflexivity journal documenting how researcher backgrounds, assumptions, and disciplinary orientations might influence interpretation of both empirical data and normative frameworks
Educational Initiatives and Training Programs
Specialized training programs have emerged to address the methodological challenges in interdisciplinary bioethics. The Empirical Bioethics Summer School exemplifies this approach, offering structured training over four days for researchers at beginner/intermediate levels [76]. The curriculum progresses from foundational concepts to practical application:
Table 3: Empirical Bioethics Summer School Curriculum Structure
| Day | Focus | Key Activities | Learning Outcomes |
|---|---|---|---|
| Day 1 | Foundations of Empirical Bioethics | Understanding empirical bioethics typologies; attendee work presentations in breakout groups [76] | Articulate different approaches to empirical bioethics; situate own work within methodological landscape |
| Day 2 | Research Design and Methods | Exploring empirical research methods; practical exercises on qualitative methods [76] | Identify appropriate empirical methods for research questions; design empirical components |
| Day 3 | Integration Methodologies | Examining approaches to integrating empirical and normative analysis; lessons from experienced researchers [76] | Understand different integration strategies; identify challenges and solutions |
| Day 4 | Application to Student Projects | Small group discussions of participant projects; putting learning into practice [76] | Apply methodological insights to specific research projects; receive expert feedback |
Feedback from previous participants highlights the value of creating collaborative spaces for methodological development, with one respondent noting: "Aside from the actual knowledge gained in the EB summer school, it was lovely to meet the conveners and the other participants. I think for me it has been a rather lonely field and getting to see others working in the field was very encouraging" [76]. This underscores the importance of community building in establishing rigor in an emerging interdisciplinary field.
Establishing rigor in interdisciplinary empirical bioethics requires addressing five core challenges: methodological pluralism, integration, interdisciplinary communication, methodological rigor, and institutional recognition. The protocols and frameworks presented here provide concrete approaches for navigating these challenges, emphasizing structured methodologies, explicit integration procedures, and specialized training. As the field continues to evolve, developing more sophisticated approaches to interdisciplinary methodology will be essential for addressing complex bioethical challenges in an era of rapid technological advancement and persistent health disparities [23]. Future work should focus on creating more comprehensive evaluation criteria for interdisciplinary quality, expanding training opportunities, and fostering institutional structures that support rigorous interdisciplinary scholarship.
Within interdisciplinary empirical bioethics, the integration of diverse perspectives is not merely beneficial but essential for tackling complex issues at the intersection of values, science, and patient care. Two distinct methodological paradigms for achieving this integration are consultative integration and dialogical integration. The former often positions researchers as experts who gather and analyze stakeholder data, while the latter redefines researchers as facilitators of a collaborative process where participants themselves become co-investigators [77]. This analysis weighs the strengths and applications of these approaches, providing a structured comparison and practical protocols for their implementation in bioethics research, including the growing field of digital bioethics [78].
Defining the Paradigms: Core Characteristics and Philosophical Foundations
Consultative Integration
Consultative integration is characterized by a structured process where researchers seek input from participants to inform a study that remains fundamentally directed by the research team. The primary relationship is one of data exchange; researchers ask questions, and participants provide answers. The analysis, interpretation, and application of the findings are primarily conducted by the researchers.
This approach is often operationalized through established qualitative and quantitative methods. For instance, researchers might employ surveys to quantify attitudes or conduct semi-structured interviews and focus groups to explore participant experiences in depth [79] [80]. The recent scoping review on ethics in pragmatic clinical trials exemplifies a consultative approach, where empirical data on ethical themes is gathered and synthesized by investigators to inform future practice [81].
Dialogical Integration
Dialogical integration, in contrast, is rooted in a philosophy of empowerment and collaborative knowledge construction. Drawing on the work of theorists like Paulo Freire, it seeks to create a space where participants and researchers engage as equals in a dialogue to critically examine problematic aspects of everyday life [77]. The goal is not only to understand the world but to change it, with the research process itself being a form of empowerment.
This paradigm uses specially structured dialogue in small groups to reveal connections between personal troubles and broader social structures [77]. A sophisticated implementation of this is Structured Dialogical Design (SDD), a method designed to help heterogeneous groups reach consensus on complex issues. SDD uses a rigorous process including idea generation, clarification, clustering, and Interpretive Structural Modeling (ISM) to build a collective "influence map" of the issues at hand, revealing root causes and leverage points for action [42].
Comparative Analysis: Weighing the Strengths and Applications
The table below summarizes the core differences and respective strengths of these two integration paradigms.
Table 1: Comparative Analysis of Consultative and Dialogical Integration
| Characteristic | Consultative Integration | Dialogical Integration |
|---|---|---|
| Primary Goal | To gather data and insights from participants to answer research questions defined by the investigator. | To empower participants through collaborative dialogue and generate a shared understanding that leads to action [42] [77]. |
| Role of Researcher | Expert and director of the research process. | Facilitator and co-learner in a collaborative process [77]. |
| Role of Participant | Subject or informant providing data. | Co-investigator and agent of change [77]. |
| Typical Outputs | Research reports, publications, identified themes, quantitative findings. | Collective action plans, root cause maps, newly defined research agendas, shared consensus [42]. |
| Handling of Power Dynamics | Power resides primarily with the researcher who controls the research process and interpretation. | Explicitly aims to flatten power hierarchies and foster equitable dialogue [42] [77]. |
| Ideal Application Context | - Testing specific hypotheses.- Measuring prevalence of phenomena.- Informing policy with generalizable data [79] [81]. | - Addressing "wicked problems" with no clear solution.- Building consensus among diverse stakeholders.- Situations where community ownership of the outcome is critical [42]. |
A key strength of consultative integration is its efficiency and scalability, especially when paired with modern digital tools. It can generate generalizable data that is highly valued in evidence-based policy. Dialogical integration's paramount strength is its ability to produce a deep, systemic understanding of complex issues and to foster a high degree of commitment to the outcomes from the participants, as the results are authentically their own [42].
Experimental Protocols for Empirical Bioethics Research
Protocol for Consultative Integration: A Mixed-Methods Study
This protocol is ideal for exploring a bioethics issue where both the scale of the problem (the "what") and the underlying reasons (the "why") need to be understood.
Workflow Overview:
Detailed Methodology:
Phase 1: Qualitative Exploration
- Objective: To explore the landscape of the issue and generate hypotheses.
- Procedure: Conduct 15-20 semi-structured interviews or 3-4 focus groups with key stakeholders (e.g., patients, clinicians, ethicists). Use open-ended questions to elicit rich, contextual narratives.
- Analysis: Employ thematic analysis to code transcripts and identify emergent themes and patterns. These themes directly inform the development of the quantitative survey [80] [82].
Phase 2: Quantitative Measurement
- Objective: To test and measure the prevalence of the themes identified in Phase 1.
- Procedure: Develop and administer a structured survey based on the qualitative findings. The sample size should be sufficient for statistical analysis (e.g., N > 200).
- Analysis: Use statistical methods (e.g., descriptive statistics, correlation analysis) to quantify attitudes, experiences, and relationships between variables [79] [80].
Phase 3: Interpretation and Integration
- Objective: To merge findings into a coherent whole.
- Procedure: Use a joint display table to visually relate quantitative results to qualitative themes. For example, a quantitative finding that "70% of respondents expressed concern about data privacy" is explained by qualitative quotes describing specific fears.
- Output: A set of integrated conclusions and actionable recommendations that are both statistically representative and deeply contextualized [80].
Protocol for Dialogical Integration: Structured Dialogical Design (SDD)
This protocol is designed for situations requiring deep consensus and systemic understanding among diverse stakeholders, such as setting research priorities or developing ethical guidelines for new technologies.
Workflow Overview:
Detailed Methodology:
Step 1: Formulate the Triggering Question
- A Knowledge Management Team (including a facilitator and key participants) crafts a open-ended question that frames the discussion, e.g., "What are the most pressing ethical shortcomings in our current system of informed consent for pragmatic trials?" [42].
Step 2: Idea Generation
- In a facilitated round-robin session, all participants contribute one idea at a time in response to the triggering question. This continues until all ideas are exhausted, ensuring equitable participation and countering groupthink [42].
Step 3: Clarification
- Each participant clarifies the meaning behind their statements. Others may ask questions for understanding, but no critique or judgment is allowed, protecting participant autonomy [42].
Step 4: Clustering
- Participants work together to categorize the ideas using a bottom-up approach, discussing similarities and distinctions. This process fosters evolutionary learning as participants refine their collective understanding [42].
Step 5: Importance Voting
- Each participant votes for a set number of ideas (e.g., five) they deem most important. This identifies the most salient issues for the group, and participants often discover that their initial priorities change ("erroneous priorities effect") [42].
Step 6: Interpretive Structural Modeling (ISM)
- The voted ideas are entered into specialized software (e.g., Cogniscope). Participants, presented with pairs of ideas, debate and decide with a super-majority (e.g., 75%) whether one influences the other. This constructs a network of relationships [42].
Step 7: Generate Influence Map
- The software produces a visual influence map (a directed graph). Ideas at the bottom are root causes (high leverage), while those at the top are effects. The group then focuses strategic action on the root causes, as addressing them will have positive knock-on effects throughout the system [42].
The Scientist's Toolkit: Essential Reagents for Integration
Table 2: Key Research Reagent Solutions for Consultative and Dialogical Methods
| Tool / Reagent | Primary Function | Application Context |
|---|---|---|
| Semi-Structured Interview Protocol | A guide with key questions and probes to ensure coverage of topics while allowing flexibility to explore participant-led narratives. | Consultative Integration: Data collection in qualitative phases [79]. |
| Validated Survey Instrument | A quantitatively reliable and valid tool to measure attitudes, beliefs, or behaviors across a larger population. | Consultative Integration: Quantitative phase of mixed-methods studies [79] [80]. |
| Digital Platform for Data Analysis | A software platform (e.g., a modular research platform as in [78]) that simplifies the use of digital methods like NLP for analyzing large textual datasets (e.g., social media). | Consultative/Dialogical: Can support either paradigm, e.g., analyzing interview transcripts or facilitating virtual SDD components [78]. |
| Triggering Question | A carefully crafted open-ended question that frames the entire dialogue and defines the stakeholders for an SDD process. | Dialogical Integration: The foundational first step of Structured Dialogical Design [42]. |
| Interpretive Structural Modeling (ISM) Software | Software (e.g., Cogniscope, Concertina) that supports the pairwise comparison of ideas and generates the structural influence map from group decisions. | Dialogical Integration: The core analytical engine of the SDD process [42]. |
| Facilitation Guide for Dialogue | A protocol for facilitators to ensure equitable participation, manage power dynamics, and guide the group through the SDD steps without imposing content. | Dialogical Integration: Essential for maintaining the integrity of the dialogical process [42] [77]. |
The choice between consultative and dialogical integration is not a matter of which is universally superior, but which is most appropriate for the research context and objectives. Consultative mixed-methods approaches provide a powerful, generalizable evidence base that is crucial for informing policy and practice from an external standpoint. Dialogical approaches, particularly Structured Dialogical Design, offer a transformative pathway for generating deep consensus and empowering communities to address the root causes of complex ethical challenges from within. The future of robust empirical bioethics lies in the discerning application of both paradigms, and potentially their thoughtful combination, to ensure that research is not only about stakeholders, but also genuinely with and for them.
Ethicametrics (EM) represents an emerging, interdisciplinary scientific research area dedicated to the systematic quantification of ethical phenomena. It is formally characterized by its dual focus on the Metrics of Ethics (MOE), which involves the measurement of ethical behaviors and impacts, and the Ethics of Metrics (EOM), which concerns the ethical evaluation of the measurement tools and statistical models themselves [83] [84]. This framework is particularly salient for empirical bioethics research, where it provides a rigorous methodology for integrating normative ethical analysis with quantitative, empirical data.
The core of Ethicametrics is its scientific nature; it employs behavioural mathematical models that are statistically validated and tested, often using panel or longitudinal data to ensure robustness [84]. This addresses a critical gap in interdisciplinary research, where mutual improvements between traditional and non-traditional fields are essential [83]. For researchers, scientists, and drug development professionals, this framework offers a structured approach to move beyond implicit, often biased, ethical assessments toward explicit, scientifically grounded evaluations.
Theoretical Foundations and Key Components
The Ethicametrics framework is built upon a comprehensive methodological core that integrates ethics into a behavioural mathematical model, which is then estimated using multi-level statistical analyses. This process is crucial for avoiding under-specification and obtaining unbiased ethical assessments [84]. The framework is inherently interdisciplinary, spanning diverse fields such as biomedical ethics, business management, environmental sustainability, and artificial intelligence, with essential mutual improvements gained across these domains [83] [3].
A fundamental principle of EM is its conceptualization of ethics as a stock of values, beliefs, and principles that produces a flow of individual or social behaviors with beneficial or detrimental impacts [84]. Proper ethical evaluation, therefore, requires including a specific ethics within a behavioural model alongside other factors affecting the same behaviour. This model must then be estimated using multiple observations of the same impact for various individuals across different contexts [84].
Table 1: Core Components of the Ethicametrics Framework
| Component | Description | Primary Function |
|---|---|---|
| Metrics of Ethics (MOE) | The quantitative measurement of ethical behaviors, impacts, and outcomes. | To provide scientifically grounded measures of ethical phenomena for analysis and comparison. |
| Ethics of Metrics (EOM) | The critical evaluation of measurement tools and models against ethical criteria from theological/philosophical literature. | To ensure the metrics and models used are themselves ethically sound and unbiased. |
| Behavioural Mathematical Model | A formal model representing the relationship between ethics, other influencing factors, and observable behaviors. | To provide a testable structure for understanding how ethics produces measurable effects. |
| Multi-Level Statistical Analysis | A statistical approach applied to panel or longitudinal data to estimate model parameters. | To avoid biased estimations and account for data structure complexity. |
The framework's interdisciplinarity is evidenced by its application across diverse fields. In business ethics, studies have explored the links between corporate social responsibility and financial performance [84]. In environmental ethics, research has quantified the impacts of religious and secular ethics on sustainability outcomes [83] [84]. In bioethics, the empirical trend has grown significantly, with empirical publications rising from 5.4% in 1990 to 15.3% in 2003, highlighting the field's increasing reliance on measurable data [3].
Essential Methodologies and Protocols
Implementing Ethicametrics requires adherence to specific methodological protocols to ensure scientific rigor and valid, interpretable results. The following sections detail the core experimental workflows and analytical approaches.
General Workflow for Ethicametrics Research
The following diagram illustrates the standardized workflow for conducting Ethicametrics research, from model specification to the application of results.
Diagram 1: Ethicametrics Research Workflow
Protocol for Integrated Empirical-Normative Analysis
This protocol is designed for bioethics researchers seeking to quantitatively assess ethical behaviors, such as those in drug development or clinical practice, while ensuring the measurement process itself is ethically sound.
- Objective: To provide a step-by-step procedure for conducting an Ethicametrics study that integrates empirical data with normative analysis, resulting in both MOE and EOM outputs.
- Background: Conventional approaches in bioethics often relegate ethics to an external, procedural role, leading to delayed engagement and associated challenges [85]. A structured, stage-wise procedure is essential for systematic integration.
Table 2: Protocol for Integrated Empirical-Normative Analysis
| Step | Action | Detailed Methodology | Output |
|---|---|---|---|
| 1. Model Specification | Formulate an explicit behavioural mathematical model. | Define the relationship: Ethical Impact = f(Ethical Stock, Control Variables, ε). The "ethical stock" represents values/beliefs; "impact" is the measurable outcome. | An ethically explicit mathematical model ready for statistical testing. |
| 2. Data Collection | Gather panel or longitudinal data. | Use surveys, administrative records, or observational data tracked over time. For bioethics, this may involve patient outcomes, clinician decision patterns, or institutional review board (IRB) records. | A dataset with repeated measures suitable for multi-level analysis. |
| 3. Statistical Analysis | Perform multi-level statistical analysis. | Apply hierarchical linear modeling or mixed-effects models to account for nested data structures (e.g., patients within clinics). Validate models statistically and conduct sensitivity analyses. | Validated model coefficients quantifying the relationship between ethics and outcomes (MOE). |
| 4. Ethical Evaluation | Critically assess the metrics and model. | Evaluate the measurement approach against ethical criteria (e.g., justice, fairness, rights) drawn from relevant philosophical/ethical literature. This is the Ethics of Metrics (EOM). | An assessment of the ethical soundness of the measurement process itself. |
| 5. Integration & Interpretation | Synthesize empirical and normative findings. | Interpret the quantitative MOE results in light of the EOM evaluation. Formulate coherent conclusions that address both the empirical findings and their normative significance. | Integrated insights for ethical decision-making or policy formulation. |
The Researcher's Toolkit: Essential Reagents and Materials
Successful implementation of the Ethicametrics framework requires leveraging a suite of conceptual and technical tools. The following table details key "research reagents" essential for conducting EM studies.
Table 3: Essential Research Reagents for Ethicametrics Studies
| Tool Category | Specific Tool/Technique | Function in Ethicametrics Research |
|---|---|---|
| Conceptual Frameworks | Rights-Based Ethics [86] | Provides a normative basis for EOM by evaluating metrics against fundamental individual rights. |
| Virtue Ethics [86] | Focuses EOM evaluation on the character virtues (e.g., honesty, courage) embodied by the measurement approach. | |
| Utilitarianism [86] | Informs EOM by assessing whether the metrics and their application maximize overall benefit and minimize harm. | |
| Data Collection Methods | Ethics Hotlines & Reporting Systems [87] | Generates quantitative data on ethics incidents (e.g., report frequency, type) for MOE analysis. |
| Employee/Stakeholder Surveys [87] | Captures perception data on ethical culture, satisfaction, and observed misconduct for MOE. | |
| Longitudinal/Panel Datasets | Provides repeated measures over time, essential for robust statistical analysis in MOE. | |
| Analytical Techniques | Multi-Level Statistical Modeling [84] | The core analytical method for MOE, accounting for nested data structures and reducing bias. |
| Sensitivity Analysis [84] | Tests the robustness of MOE findings to different model assumptions or data conditions. | |
| Technology Platforms | Dynamic Risk Dashboards [88] | Aggregates data from multiple sources (HR, procurement, reports) for proactive E&C monitoring and MOE. |
| Generative AI for Policy Guidance [88] | Provides real-time, natural language guidance on policies, supporting consistent ethical behavior and data collection for MOE. |
Application in Bioethics: A Specific Workflow
The following diagram details how the Ethicametrics framework can be applied to a specific bioethics research context, such as evaluating the ethical impact of a new drug development policy.
Diagram 2: Ethicametrics in Bioethics Research
Ethicametrics provides a novel, robust framework for researchers and drug development professionals to move beyond theoretical ethical discussions into the realm of empirical, quantitative analysis. By systematically combining the Metrics of Ethics (MOE) with the Ethics of Metrics (EOM), it enables a more rigorous and scientifically grounded approach to bioethics research. The structured protocols, visual workflows, and essential toolkits outlined in these application notes offer a practical pathway for implementing this framework, ultimately fostering more ethical outcomes in science and healthcare through measurable, evidence-based methods.
Application Notes: The Role of Empirical Data in Bioethical Inquiry
Empirical bioethics (EB) is an interdisciplinary field that integrates empirical social scientific analysis with ethical analysis to draw normative conclusions [38]. This integration addresses the classic philosophical challenge of the 'is-ought' gap—the notion that one cannot directly derive ethical prescriptions ('ought') from factual observations ('is')—by using empirical data as a testing ground for elements of normative theory [4]. The most significant contribution of empirical research lies in its capacity to test and refine ethical theories against the complexities of real-world contexts and lived experiences.
Researchers broadly accept several key objectives for empirical research in bioethics. These range from modest ambitions focused on understanding context to more ambitious goals that directly influence normative recommendations [4]. Table 1 summarizes the spectrum of acceptable objectives for Empirical Research in Bioethics (ERiB), based on qualitative research with scholars in the field.
Table 1: Acceptable Objectives of Empirical Research in Bioethics (ERiB)
| Objective | Level of Acceptance | Primary Function |
|---|---|---|
| Understanding the context of a bioethical issue | Unanimous agreement [4] | Descriptive |
| Identifying ethical issues as they arise in practice | Unanimous agreement [4] | Descriptive |
| Evaluating how ethical recommendations play out in practice | High support [4] | Normative assessment |
| Informing the development or refinement of specific ethical norms | Supported with varying agreement [4] | Normative development |
| Informing the development or justification of general moral principles | Contested [4] | Normative development |
| Serving as a source of morality | Contested [4] | Normative foundation |
The consensus within the field is that the most readily accepted objectives are those that focus on producing empirical results to illuminate the context and practical manifestations of ethical problems [4]. The more ambitious objectives, which involve drawing normative recommendations and justifying moral principles, remain contested but are recognized as legitimate, albeit methodologically challenging, ambitions for the field [4] [38].
Experimental Protocols in Empirical Bioethics
To ensure rigor and quality in empirical bioethics research, a consensus project has established 15 standards of practice, organized into six domains [38] [89]. These standards provide a framework for designing and conducting studies that effectively integrate empirical and normative work.
General Protocol Template for Empirical Bioethics Research
A robust research protocol is fundamental. The following template, adapted from a recently formalized tool, is suitable for quantitative, qualitative, and mixed-methods approaches in humanities and social sciences health research [7].
Table 2: Core Elements of an Empirical Bioethics Research Protocol
| Section | Description | Key Considerations |
|---|---|---|
| Title & Summary | Concisely describe the nature, subject, and methodological approach of the study [7]. | Include a short title, acronym, and a summary of context, primary objective, and general method. |
| Problem & Objectives | Explain the importance of the problem and state the specific research objectives or questions [7]. | Summarize significant prior work and state the problem clearly. |
| Disciplinary Field & Research Paradigm | Present the principal disciplinary field(s) and the research paradigm [7]. | Specify the methodological (e.g., qualitative, quantitative) and theoretical framework (e.g., principlism). |
| Site, Duration & Team | Present the study site, its context, and the study duration [7]. | Specify the period for inclusion, data collection, analysis, and publication. Detail the research team's qualifications and characteristics. |
| Participant Sampling & Consent | Specify participant characteristics, sampling method, and informed consent procedures [7]. | Explain how and why sampling occurs and the criteria for stopping. Justify the type of consent and provide information notices. |
| Data Collection | Present and justify the types of data, procedures, instruments, and tools for collection [7]. | Detail instruments (e.g., interview guides) and equipment (e.g., recorders). Note any planned changes during the study. |
| Data Processing & Analysis | Detail methods for data transcription, input, analysis, storage, protection, and confidentiality [7]. | Describe analytical approaches and measures to ensure data security and participant anonymity. |
| Integration & Normative Analysis | Explain the procedure for integrating empirical findings with normative analysis [7]. | This is a crucial, specialized section for empirical bioethics, detailing how 'is' informs 'ought'. |
Detailed Experimental Methodology: A Digital Bioethics Case Study
The following protocol illustrates the application of digital methods to an empirical bioethics question, leveraging novel data sources like social media.
Study Aim: To analyze public discourse and moral attitudes regarding a specific bioethical issue (e.g., CRISPR gene editing or COVID-19 risk communication) on digital platforms like Twitter [78] [90].
Workflow Overview: The diagram below outlines the key stages of this digital methodology.
Protocol Steps:
Data Acquisition & Pre-processing:
- Tool: A modular research platform prototype [78] or specialized social media API.
- Action: Collect publicly available data (e.g., tweets) using relevant keywords and hashtags over a defined period.
- Output: A raw dataset of text and metadata.
Data Analysis:
- Tool: Natural Language Processing (NLP) libraries (e.g., Hugging Face [78]) and network analysis software (e.g., Gephi [78]).
- Actions:
- Thematic Analysis: Identify recurring themes, concerns, and values in the discourse.
- Sentiment Analysis: Gauge the emotional valence of the discourse.
- Network Analysis: Map how ideas and information spread within the network of users.
- Output: Structured empirical findings on the content and structure of public moral deliberation.
Normative Integration:
- Method: Employ a recognized empirical bioethics methodology such as Reflective Equilibrium [38] [4] or a Dialogical Practice [38].
- Action: Systematically compare the empirical findings (public attitudes, reasoning patterns) with existing ethical theories and principles. The goal is to identify points of alignment and tension, using the empirical data to test, refine, or reveal limitations in the theoretical frameworks.
- Output: Refined ethical arguments, recommendations for policy or practice, or proposals for modifying theoretical principles.
Table 3: Essential Materials and Tools for Empirical Bioethics Research
| Tool / Resource | Function | Application Note |
|---|---|---|
| Semi-structured Interview Guide | To collect rich, qualitative data on lived experiences and moral reasoning of stakeholders (patients, professionals) [7]. | Should be flexible, with open-ended questions. Piloting is recommended. |
| Standardized Survey Instruments | To quantify attitudes, beliefs, or prevalence of specific ethical issues within a larger population [7]. | Must be validated for the target population to ensure reliability and validity. |
| Digital Methods Platform | To enable researchers without advanced programming skills to collect and analyze data from digital sources (e.g., social media) [78] [90]. | Overcomes the technical bottleneck, empowering broader use of digital methods. |
| NLP Libraries (e.g., Hugging Face) | To perform computational analysis on large text corpora, such as theme identification and sentiment analysis [78]. | Requires some technical expertise; collaboration with data scientists is beneficial. |
| Qualitative Data Analysis Software (e.g., NVivo, Dedoose) | To manage, code, and analyze qualitative data (interviews, focus groups) systematically [7]. | Facilitates rigorous and transparent analysis of complex textual data. |
| Ethical Theory Framework | To provide the normative structure for analyzing and interpreting empirical findings [7] [38]. | Examples include Principlism, Care Ethics, or Virtue Ethics. Must be explicitly stated. |
Consensus Standards for Research Practice
A cornerstone for ensuring quality in empirical bioethics is the adherence to agreed-upon standards. A modified Delphi consensus process involving European experts established 15 standards across six domains [38] [89].
Table 4: Domains and Selected Standards of Practice for Empirical Bioethics Research
| Domain | Description | Example Standard |
|---|---|---|
| Aims | The research should have clearly defined aims. | The aims of the research should be clearly stated and include both empirical and normative components [38]. |
| Questions | The research questions should reflect the interdisciplinary nature of the work. | Research questions should be answerable through interdisciplinary collaboration [38]. |
| Integration | The empirical and normative components must be integrated. | The way in which the empirical and normative components of the research are integrated should be clearly described and justified [38]. |
| Conduct of Empirical Work | The empirical work must be conducted and reported to a high standard. | The design of the empirical work should be appropriate to the normative questions [38]. |
| Conduct of Normative Work | The normative work must be conducted and reported to a high standard. | The normative analysis should be rigorous [38]. |
| Training & Expertise | The research team must possess or have access to relevant expertise. | The research team should possess, or have access to, appropriate expertise in the relevant empirical methods and normative analysis [38]. |
These standards provide a vital roadmap for researchers, funders, and journals, helping to cement empirical bioethics as a distinct and rigorous community of practice [38]. The domain of Integration is particularly critical, as it demands a transparent and justified methodology for bridging the factual and the evaluative, which is the defining task of the field.
Conclusion
Interdisciplinary empirical bioethics is not merely an academic exercise but a vital practice for ensuring that ethical guidance remains relevant, robust, and applicable to the rapidly evolving landscape of biomedical research and clinical care. The key takeaway is that successful integration of empirical data with normative analysis requires a deliberate and transparent methodological choice, whether it be consultative, dialogical, or inherent. Moving forward, the field must prioritize the development of clearer standards of rigor, foster greater collaboration across disciplines from the outset of research projects, and continue to adapt its methodologies to novel challenges posed by artificial intelligence, genomics, and global health inequities. By doing so, researchers and drug development professionals can ensure that their work is not only scientifically sound but also ethically grounded, socially responsible, and capable of earning public trust.
References
- 1. Digital bioethics: introducing new methods for the study of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10646908/]
- 2. Researchers' Views on Doing Empirical Bioethics [https://link.springer.com/article/10.1007/s11673-023-10286-z]
- 3. The use of empirical research in bioethics - BMC Medical Ethics [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-017-0239-0]
- 4. Acceptable objectives of empirical research in bioethics [https://pmc.ncbi.nlm.nih.gov/articles/PMC9794471/]
- 5. a framework for empirical bioethics research projects [https://link.springer.com/article/10.1186/s12910-019-0428-0]
- 6. The Role of Empirical Research in Bioethics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2826359/]
- 7. Health research protocols: a template for empirical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12183882/]
- 8. Recommended format for a 'research protocol' [https://www.who.int/groups/research-ethics-review-committee/recommended-format-for-a-research-protocol]
- 9. Guiding Principles for Ethical Research [https://www.nih.gov/health-information/nih-clinical-research-trials-you/guiding-principles-ethical-research]
- 10. Acceptable objectives of empirical research in bioethics [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-022-00845-1]
- 11. Empirical research in bioethical journals. A quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2565792/]
- 12. Four stages of competence [https://en.wikipedia.org/wiki/Four_stages_of_competence]
- 13. The Four Stages of Competence Model [https://www.innovationtraining.org/the-four-stages-of-competence-model/]
- 14. Four Stages of Competence: How We Learn Every New Skill [https://themindcollection.com/four-stages-of-competence/]
- 15. Critical Realism and Empirical Bioethics: A Methodological ... [https://pubmed.ncbi.nlm.nih.gov/25716752/]
- 16. 14 Comparing quantitative data between individuals [https://bookdown.org/pkaldunn/SRM-Textbook/BetweenQuantData.html]
- 17. Health research protocols: a template for empirical bioethics ... [https://health-policy-systems.biomedcentral.com/articles/10.1186/s12961-025-01362-4]
- 18. IEEN workshop report: Professionalism in interdisciplinary and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4466098/]
- 19. Examining Practices Related to Ethical Aspects in eHealth ... [https://www.researchprotocols.org/2025/1/e60849]
- 20. Conflicting Interests and New Frontiers: A Role for Virtue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12540520/]
- 21. Utilitarian Ethic - an overview [https://www.sciencedirect.com/topics/psychology/utilitarian-ethic]
- 22. Deontology - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK459296/]
- 23. Global Bioethics: Addressing Current Challenges ... [https://www.intechopen.com/chapters/1217243]
- 24. AI-based medical ethics education: examining the potential of ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-025-06801-y]
- 25. 2025 RARE Drug Development Symposium [https://globalgenes.org/rare-drug-development-symposium-2025/]
- 26. Empirical Bioethics: Theoretical and Practical Perspectives [https://research-information.bris.ac.uk/en/publications/empirical-bioethics-theoretical-and-practical-perspectives/]
- 27. Bioethics at the intersection of politics, society, and ... [https://pubmed.ncbi.nlm.nih.gov/40615835/]
- 28. The State of AI: Global Survey 2025 [https://www.mckinsey.com/capabilities/quantumblack/our-insights/the-state-of-ai]
- 29. MIT report: 95% of generative AI pilots at companies are ... [https://fortune.com/2025/08/18/mit-report-95-percent-generative-ai-pilots-at-companies-failing-cfo/]
- 30. WHO warns of slowing global health gains in new statistics ... [https://www.who.int/news/item/15-05-2025-who-warns-of-slowing-global-health-gains-in-new-statistics-report]
- 31. AI in healthcare risks could exclude 5 billion people [https://www.weforum.org/stories/2025/10/ai-in-healthcare-risks-could-exclude-5-billion-people-here-s-what-we-can-do-about-it/]
- 32. Bridging the digital divide: artificial intelligence as a ... [https://www.sciencedirect.com/science/article/pii/S1386505625002680]
- 33. 4 Health Issues We're Watching in 2025 [https://www.projecthope.org/news-stories/story/4-health-issues-were-watching-in-2025/]
- 34. A systematic review of empirical bioethics methodologies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4357052/]
- 35. 10 - Reflective Equilibrium as a Normative Empirical Model [https://www.cambridge.org/core/books/empirical-bioethics/reflective-equilibrium-as-a-normative-empirical-model-the-case-of-ashley-x/A88B3BB65D39CD91FA3C60FCF2411F41]
- 36. Collective Reflective Equilibrium, Algorithmic Bioethics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7617835/]
- 37. Collective Reflective Equilibrium and algorithmic bioethics [https://www.antitheses.net/blog/collective-reflective-equilibrium-and-algorithmic-bioethics-a-new-approach-to-complex-ethical-dilemmas]
- 38. Standards of practice in empirical bioethics research [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-018-0304-3]
- 39. Mapping, framing, shaping: a framework for empirical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6880497/]
- 40. Embedded Ethics in Practice: A Toolbox for Integrating the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11668859/]
- 41. Dialogue as Stakeholder for Decision Making in Health... Deliberation [https://pubmed.ncbi.nlm.nih.gov/28059875/]
- 42. Structured dialogical design – Integration and Implementation Insights [https://i2insights.org/2024/07/09/structured-dialogical-design/]
- 43. Learn How the Dialogic Change Model Works › Collective Leadership... [https://www.collectiveleadership.de/blog/article/the-dialogic-change-model/]
- 44. but where do we start? A reflection of epochè as method [https://pubmed.ncbi.nlm.nih.gov/7142847/]
- 45. a template for empirical bioethics and other investigations [https://pubmed.ncbi.nlm.nih.gov/40551148/]
- 46. Presenting Quantitative Data Graphically [https://courses.lumenlearning.com/waymakermath4libarts/chapter/presenting-quantitative-data-graphically/]
- 47. Presentation of Quantitative Data [https://ihatepsm.com/blog/presentation-quantitative-data]
- 48. Figures and Charts - UNC Writing Center [https://writingcenter.unc.edu/tips-and-tools/figures-and-charts/]
- 49. the value of narrative approaches in empirical (bio)ethics [https://pubmed.ncbi.nlm.nih.gov/34530832/]
- 50. One of the first, still foremost: Penn Bioethics marks 30 years [https://www.pennmedicine.org/news/one-of-the-first-still-foremost-penn-bioethics-marks-30-years]
- 51. Bio-Ethics and One Health: A Case Study Approach to ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2022.648593/full]
- 52. Bio-Ethics and One Health: A Case Study Approach to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8971560/]
- 53. The Vagueness of Integrating the Empirical and the Normative [https://pmc.ncbi.nlm.nih.gov/articles/PMC11288993/]
- 54. Is–ought problem [https://grokipedia.com/page/Is%E2%80%93ought_problem]
- 55. Hume's 1739 “Is–Ought” Problem Revisited [https://medium.com/@arina.solntzeff/humes-1739-is-ought-problem-revisited-why-it-becomes-solvable-in-2025-02d2d9534f60]
- 56. 11 Summarising quantitative data | Scientific Research and ... [https://bookdown.org/pkaldunn/SRM-Textbook/SummariseQuantData.html]
- 57. Four medication use cases that require a data ... [https://www.wolterskluwer.com/en/expert-insights/4-medication-use-cases-that-require-a-data-normalization-solution]
- 58. in the Conflict Setting: A Story Beyond Resolution ... Clinical Bioethics [https://pubmed.ncbi.nlm.nih.gov/26711422/]
- 59. Interdisciplinary Studies in Health Science (IDS) [https://libguides.fau.edu/ids-boca/quantitative-qualitative]
- 60. Part 2: Data Tables and Charts [https://www.clir.org/pubs/reports/pub122/part2/]
- 61. Empirical Ethics [https://aabhl.org/stream/empirical-ethics/]
- 62. A Review of the Quality Indicators of Rigor in Qualitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7055404/]
- 63. The function of diagram with numbered arrows and text in ... [https://www.sciencedirect.com/science/article/abs/pii/S0747563216302345]
- 64. Using thematic analysis in qualitative research [https://www.sciencedirect.com/science/article/pii/S2949916X25000222]
- 65. Qualitative Data Analysis: Step-by-Step Guide (Manual vs. ... [https://getthematic.com/insights/qualitative-data-analysis]
- 66. Standards for reporting qualitative research [https://www.equator-network.org/reporting-guidelines/srqr/]
- 67. Do the More Advantaged Dominate Deliberation? Using ... [https://delibdemjournal.org/article/id/1549/]
- 68. Assessing the Quality of Community Jury Deliberations in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12614172/]
- 69. GraphiT: Efficient Node Classification on Text-Attributed ... [https://arxiv.org/html/2502.10522v1]
- 70. Dangling centrality highlights critical nodes by evaluating ... [https://www.nature.com/articles/s41598-025-24930-8]
- 71. How Interactive Visualizations Compare to Ethical ... [https://pubmed.ncbi.nlm.nih.gov/37074681/]
- 72. A Platform to Develop and Apply Digital Methods for ... [https://www.sciencedirect.com/science/article/pii/S2561326X22005091]
- 73. A Scoping Review of Empirical Research on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12490803/]
- 74. A process model for teaching interdisciplinary research [https://i2insights.org/2016/08/09/teaching-interdisciplinarity/]
- 75. Multi-method process maps: An interdisciplinary approach to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7348036/]
- 76. 2025: Empirical Bioethics Summer School [https://www.bristol.ac.uk/population-health-sciences/centres/ethics/seminars/2025/empirical-bioethics-summer-school.html]
- 77. Using Dialogical Research Methods in Group Interviews [https://methods.sagepub.com/book/edvol/successful-focus-groups/chpt/using-dialogical-research-methods-group-interviews]
- 78. A Platform to Develop and Apply Digital Methods for Empirical ... [https://formative.jmir.org/2022/5/e28558/]
- 79. Types of Research Methods: Quantitative & Qualitative ... [https://paperguide.ai/blog/types-of-research-methods/]
- 80. Mixed Methods Research: Combining Qualitative & ... [https://www.zonkafeedback.com/blog/mixed-methods-research-combining-qualitative-quantitative-analysis]
- 81. October 16, 2025: New Article Surveys Landscape of ... [https://rethinkingclinicaltrials.org/news/october-16-2025-new-article-surveys-landscape-of-empirical-ethics-research-related-to-pragmatic-clinical-trials/]
- 82. Qualitative vs. Quantitative Data & Why Data Matters to ... [https://www.swydo.com/blog/qualitative-vs-quantitative-data/]
- 83. : A New Interdisciplinary Science Ethicametrics [https://ideas.repec.org/a/gam/jstats/v8y2025i3p50-d1684726.html]
- 84. Ethicametrics: A New Interdisciplinary Science [https://www.mdpi.com/2571-905X/8/3/50]
- 85. An SOP for advancing ethics engagement in science [https://www.sciencedirect.com/science/article/pii/S2405805X25000912]
- 86. What are Ethical Frameworks ? An In-Depth Overview [https://www.theknowledgeacademy.com/blog/ethical-frameworks/]
- 87. How Today's Leaders Are Measuring Ethics [https://www.ethicaladvocate.com/how-todays-leaders-are-measuring-ethics/]
- 88. Why Strategic Investment in Ethics and Compliance Is Non- ... [https://ethisphere.com/ethics-and-compliance-investment-2025/]
- 89. (PDF) Standards of practice in empirical bioethics research [https://www.academia.edu/87548617/Standards_of_practice_in_empirical_bioethics_research_towards_a_consensus]
- 90. A Platform to Develop and Apply Digital Methods for Empirical ... [https://pubmed.ncbi.nlm.nih.gov/35511234/]