Belmont Report vs. Common Rule: A Practical Guide for Researchers and Drug Developers
This article provides a comprehensive comparison of the Belmont Report's ethical principles and the Common Rule's regulatory requirements, tailored for researchers, scientists, and drug development professionals.
Belmont Report vs. Common Rule: A Practical Guide for Researchers and Drug Developers
Abstract
This article provides a comprehensive comparison of the Belmont Report's ethical principles and the Common Rule's regulatory requirements, tailored for researchers, scientists, and drug development professionals. It explores the historical foundations of human subject protections, details the practical application of these frameworks in modern research, and offers strategies for navigating recent regulatory updates. The scope includes an analysis of the 2019 Revised Common Rule changes, their impact on clinical trials and informed consent, and a direct comparison to help professionals ensure compliance while upholding the highest ethical standards in their work.
The Ethical Bedrock: Understanding the History and Principles of the Belmont Report
The Tuskegee Syphilis Study stands as one of the most notorious examples of unethical human subjects research in United States history. This study, conducted by the U.S. Public Health Service from 1932 to 1972, observed the natural progression of untreated syphilis in 400 African American men from Macon County, Alabama [1] [2]. The participants were deliberately misled about their condition and were not informed they were in a research study; instead, they were told they were being treated for "bad blood" [1] [3]. Even after penicillin became the standard, effective treatment for syphilis in the 1950s, researchers actively withheld it from participants and prevented them from accessing treatment elsewhere [1].
The study's termination in 1972, following public outcry after press exposure, directly prompted the U.S. Congress to pass the National Research Act (NRA) of 1974 [4] [5]. This legislation was signed into law by President Richard Nixon and represented the federal government's decisive response to systemic research ethics failures [4]. The Act created the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research, charging it with identifying the basic ethical principles that should govern human subjects research [4] [3]. The Commission's work culminated in the Belmont Report of 1979, which established the foundational ethical principles of Respect for Persons, Beneficence, and Justice [1] [3]. Furthermore, the NRA mandated the establishment of Institutional Review Boards (IRBs) to provide local oversight and review of federally-funded research [4] [6].
Table: Key Events in the Development of Modern Research Ethics
| Year | Event | Significance |
|---|---|---|
| 1932-1972 | Tuskegee Syphilis Study | Infamous 40-year study on untreated syphilis that violated basic ethical principles [1] [2]. |
| 1974 | National Research Act | U.S. federal law enacted in direct response to Tuskegee; established the National Commission [4] [5]. |
| 1979 | Belmont Report | Published by the National Commission; outlined three core ethical principles for research [1] [3]. |
| 1991 | Federal Policy (Common Rule) | Codified the Belmont principles into federal regulations (45 CFR 46) for most federally-funded research [7] [3]. |
Comparative Analysis: The Belmont Report vs. The Common Rule
The Belmont Report and the Common Rule represent two distinct but interconnected pillars of modern research ethics. The Belmont Report is a philosophical guide that establishes ethical principles, while the Common Rule is the regulatory framework that translates those principles into enforceable requirements for research practice [1] [8].
The Belmont Report: Foundational Ethical Principles
The Belmont Report was designed to provide an ethical framework to help resolve problems surrounding the conduct of research with human subjects [3]. Its three principles have become the cornerstone for ethical research:
- Respect for Persons: This principle acknowledges the autonomy of individuals and requires that those with diminished autonomy (e.g., children, prisoners, individuals with cognitive impairments) are entitled to protection. In practice, this principle is applied through the process of informed consent, which must include information, comprehension, and voluntariness [1] [3].
- Beneficence: This principle obligates researchers to maximize possible benefits for society and the participant while minimizing potential harms. This is applied through a systematic assessment of risks and benefits [1] [3].
- Justice: This principle requires the fair distribution of the burdens and benefits of research. It demands that researchers not systematically select subjects based on their easy availability, compromised position, or manipulability, rather than for reasons directly related to the problem being studied. This is applied through the equitable selection of subjects [1] [3].
The Common Rule: Regulatory Application
The Common Rule (45 CFR Part 46) is the common name for the Federal Policy for the Protection of Human Subjects, which was adopted by 15 federal departments and agencies in 1991 [4] [3]. It operationalizes the principles of the Belmont Report into specific, actionable regulations. The Common Rule defines key terms such as "research," "human subject," and "intervention," and establishes the requirements for IRB membership, function, and review processes [7].
Table: Comparison of the Belmont Report and the Common Rule
| Aspect | The Belmont Report (Ethical Guide) | The Common Rule (Regulatory Framework) |
|---|---|---|
| Nature | Philosophical and principles-based [1] | Legal and procedural [7] |
| Primary Focus | Identifying basic ethical principles [3] | Establishing enforceable regulations for federally-funded research [7] |
| Application of Principles | Respect for Persons → Informed Consent [1] | Detailed requirements for consent form content and process [7] |
| Beneficence → Risk/Benefit Assessment [1] | IRB must determine that risks are minimized and reasonable in relation to benefits [7] | |
| Justice → Selection of Subjects [1] | Explicit protections for vulnerable populations (e.g., prisoners, children) [3] | |
| Oversight Mechanism | Guidance for researchers and IRBs [8] | Mandates local Institutional Review Board (IRB) approval and ongoing review [4] [7] |
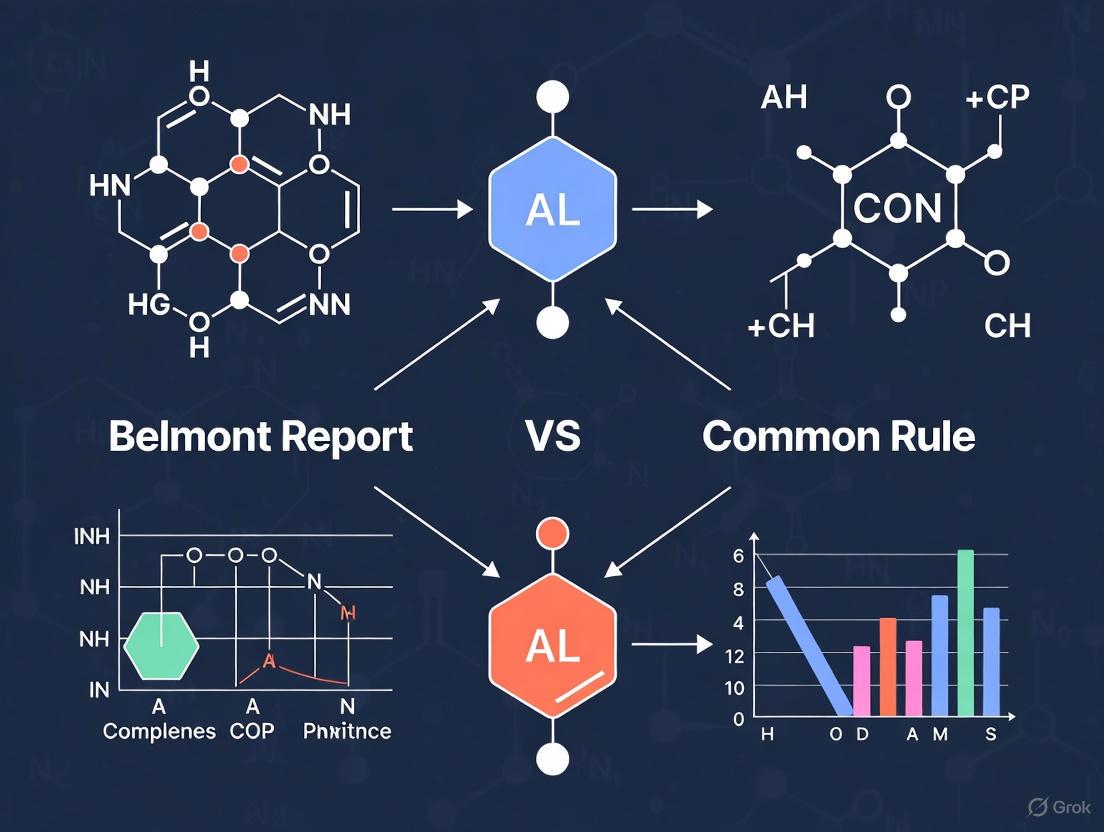
Figure 1: The historical and regulatory pathway from the Tuskegee Syphilis Study to the modern system of research protections.
The Institutional Review Board (IRB) System
The National Research Act formally mandated the use of Institutional Review Boards (IRBs) to review and monitor research involving human subjects [4]. An IRB is an administrative body whose primary mission is to protect the rights and welfare of research participants [6]. The Common Rule sets forth specific requirements for IRB composition, including:
- Having at least five members with varying backgrounds [4] [6].
- Including at least one scientific member, one non-scientific member, and one member not otherwise affiliated with the institution [6].
- Ensuring the IRB can review research with sensitivity to issues such as community attitudes and the needs of vulnerable populations [7].
The IRB has the authority to approve, require modifications to, or disapprove all research activities within its jurisdiction. Its core functions are to ensure that:
- Risks to subjects are minimized and are reasonable in relation to anticipated benefits.
- Selection of subjects is equitable.
- Informed consent is sought from each prospective subject or their legally authorized representative and is appropriately documented [7] [6].
Contemporary Relevance, Challenges, and Evolution
The ethical and regulatory framework born from the Tuskegee tragedy continues to evolve and face new challenges. The Common Rule was significantly revised in 2017, with updates taking effect in 2019, to enhance effectiveness and modernize the rules [7] [9]. Key areas of ongoing development include:
- Single IRB Review: For NIH-funded multisite research, the use of a single IRB of record is now mandated to reduce duplication of effort and speed up the initiation of research [4].
- Addressing Current Gaps: Critics note that the Common Rule's protections apply primarily to federally-funded research, creating a patchwork of oversight [4]. Furthermore, the regulations exclude research using de-identified information and biospecimens, which is increasingly problematic in an era of powerful data re-identification technologies [4].
- Application to Emerging Fields: The principles of the Belmont Report are now being applied to new technological frontiers. For instance, researchers at the National Institute of Standards and Technology (NIST) have proposed using the Belmont framework to guide ethical research in Artificial Intelligence, particularly to address issues of biased data and algorithmic fairness [9].
- Regulatory Burden and Critique: Some voices in the scientific community argue that the current IRB system can be overly burdensome, particularly for social and behavioral research that poses minimal risk, and can even inhibit scholarly inquiry [10].
Essential Framework for Researchers
For professionals in drug development and clinical research, the legacy of Tuskegee is a system of protections embodied in key documents and oversight bodies. The following table details the core components of this system.
Table: Research Ethics Framework: Key Components and Functions
| Component | Function/Purpose | Relevance to Researcher |
|---|---|---|
| Belmont Report | Foundation of ethical principles (Respect for Persons, Beneficence, Justice) [1] [3] | Serves as the ethical compass for designing and conducting studies. |
| Common Rule (45 CFR 46) | Federal regulations incorporating Belmont principles [7] | Legally binding rules for most U.S. research; dictates IRB requirements. |
| Institutional Review Board (IRB) | Local ethics committee that reviews and approves research [4] [6] | Primary point of contact for protocol approval and ongoing oversight. |
| Informed Consent Document | Application of "Respect for Persons"; ensures voluntary participation [1] | Must be obtained from each participant; core to study protocol. |
| Protocol Risk/Benefit Analysis | Application of "Beneficence"; justifies study risks [1] [3] | Critical section of the research proposal reviewed by the IRB. |
| Inclusion/Exclusion Criteria | Application of "Justice"; ensures fair subject selection [1] | Must be scientifically valid and not unfairly target vulnerable groups. |
The Belmont Report, formally published in 1979, established the three core ethical principles—Respect for Persons, Beneficence, and Justice—that serve as the foundational framework for the ethical conduct of research involving human subjects in the United States [8]. Created by the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research, the report was a direct response to historical ethical abuses, most notably the Tuskegee Syphilis Study [8] [11]. Its primary purpose was to identify the basic ethical principles that should guide research and develop guidelines to ensure that research is conducted in accordance with those principles.
The Common Rule (the Federal Policy for the Protection of Human Subjects), codified in 1991 and revised in 2017, is the federal regulation that implements these ethical principles into enforceable rules for federally funded research [12] [9]. While the Belmont Report provides the ethical compass, the Common Rule provides the specific roadmap for institutional review boards (IRBs), investigators, and institutions [8] [13]. This guide compares these two interdependent documents, analyzing how abstract ethical concepts are translated into concrete regulatory requirements that shape modern clinical research and drug development.
Analytical Framework: Principles and Their Regulatory Applications
The following table details the three ethical principles of the Belmont Report and their corresponding applications within the Common Rule's regulatory structure.
Table 1: The Belmont Report's Ethical Principles and Their Common Rule Applications
| Ethical Principle (Belmont Report) | Conceptual Definition | Regulatory Application (Common Rule) | Key Common Rule Requirements |
|---|---|---|---|
| Respect for Persons | Recognizes the autonomy of individuals and requires protection for those with diminished autonomy [14] [15]. | Informed Consent [14] [13]. | Requires a process that includes information disclosure, participant comprehension, and voluntariness [15]. The revised Common Rule mandates a concise key information section and that the consent form facilitates comprehension [13]. |
| Beneficence | Entails an obligation to maximize possible benefits and minimize possible harms [14] [11]. | Assessment of Risks and Benefits [14]. | Requires a systematic, non-arbitrary analysis by the IRB to ensure that risks are minimized and are justified by the anticipated benefits [14]. |
| Justice | Demands fair procedures and outcomes in the selection of research subjects [14] [15]. | Selection of Subjects [14]. | Requires that the research does not systematically select subjects based on easy availability, compromised position, or manipulability [14]. Ensures equitable distribution of the burdens and benefits of research [11]. |
Comparative Analysis: The Belmont Report and the Common Rule
Historical and Functional Relationship
The Belmont Report and the Common Rule have a parent-child relationship, with the former establishing the philosophical foundation and the latter codifying it into law. The Belmont Report was crafted as a direct result of the National Research Act of 1974, which was prompted by public outrage over the Tuskegee Syphilis Study [8] [16] [11]. Its creation aimed to provide a lasting ethical framework that could guide researchers and regulators. The Common Rule (45 CFR Part 46) was subsequently developed in the late 1970s and early 1980s as the uniform federal policy to implement these principles across various federal departments and agencies [14].
While the Belmont Report's principles are broad and aspirational, the Common Rule's requirements are specific and operational. The Report serves as "an analytical framework" more akin to a compass than a checklist, while the Common Rule provides the specific checklist that research protocols must satisfy for approval [11]. This relationship ensures that ethical oversight is not merely a bureaucratic hurdle but is grounded in core moral convictions.
From Ethical Principle to Regulatory Practice
The Pathway of Informed Consent
The principle of Respect for Persons is operationalized through the rigorous requirements of informed consent. The Belmont Report breaks down informed consent into three elements: information, comprehension, and voluntariness [15]. The Common Rule expands these into a detailed regulatory structure. The 2017 revisions to the Common Rule significantly strengthened these requirements by introducing the concept of "key information," requiring that consent begins with a "concise and focused presentation" to facilitate a prospective subject's understanding [13]. This change addresses the critique that traditional consent forms had become long, legalistic documents that undermined true comprehension.
Furthermore, the revised Common Rule introduced new consent requirements that reflect modern research complexities, mandating disclosures about commercial intent, whether clinical results will be returned to subjects, and the potential for biospecimens or data to be used for secondary research [13]. This evolution demonstrates how the static ethical principle of Respect for Persons is dynamically applied through updating regulations to meet new challenges.
The Evolution of Risk-Benefit Analysis
The ethical principle of Beneficence, with its dual mandates to "do not harm" and "maximize possible benefits and minimize possible harms," is put into practice through the systematic assessment of risks and benefits [14]. The Belmont Report conceptualizes this as a careful gathering and weighing of information about the research proposal [14]. The Common Rule makes this a formal requirement for IRB review, stipulating that "risks to subjects are minimized" and "risks are reasonable in relation to anticipated benefits" [14].
The revised Common Rule also introduced greater proportionality into this assessment by eliminating continuing review for some lower-risk studies and creating new categories of exempt research, recognizing that the level of oversight should correspond to the level of risk [12]. This regulatory refinement reflects a more nuanced application of the beneficence principle, focusing protection efforts where they are most needed.
Ensuring Equity in Subject Selection
The Justice principle requires the fair distribution of both the burdens and the benefits of research [11]. The Belmont Report specifically warns against systematically selecting subjects simply because of their easy availability, compromised position, or manipulability [14] [15]. In regulatory practice, the Common Rule requires IRBs to ensure that "selection of subjects is equitable" [14].
This principle has profound implications for study design and recruitment. It prevents researchers from exclusively recruiting vulnerable populations (e.g., prisoners, institutionalized individuals) for studies that could involve a broader cross-section of society [15]. Conversely, it also guards against the inappropriate exclusion of certain demographics, which can create biased datasets and inequitable access to the benefits of research [9]. This is particularly relevant in fields like AI training and drug development, where non-representative data can lead to biased algorithms or therapies that are less effective for underrepresented groups.
Key Regulatory Changes and Modern Interpretations
The 2017 revision of the Common Rule introduced several key changes that reflect a modern interpretation of the Belmont principles:
- Broad Consent for Biospecimens: The revised Rule allows for "broad consent" for the storage, maintenance, and secondary research use of identifiable private information and biospecimens, addressing a key challenge in biobanking [12] [17]. This provides a practical mechanism for respecting persons in the context of future, unspecified research.
- Streamlined IRB Review for Multi-Site Research: The updated regulations mandate the use of a single IRB for cooperative research conducted at multiple sites in the United States, reducing unnecessary duplication and burden while maintaining ethical oversight [12].
- Public Posting of Consent Forms: For clinical trials, the revised Common Rule requires that consent forms be posted on a publicly available federal website, increasing transparency and facilitating a collective raising of standards in the application of the Respect for Persons principle [13].
The following diagram illustrates the historical progression from ethical abuses to the modern regulatory system governed by the Belmont Report and Common Rule.
The Scientist's Toolkit: Essential Components for Ethical Research
For researchers, scientists, and drug development professionals, navigating the requirements derived from the Belmont principles requires familiarity with key tools and concepts. The following table outlines essential components of a compliant and ethical research program.
Table 2: Essential Tools for Implementing Ethical Research Protocols
| Tool or Concept | Primary Function | Relevance to Belmont Principles |
|---|---|---|
| Institutional Review Board (IRB) | An independent committee that reviews, approves, and monitors research involving human subjects to protect their rights and welfare [8]. | Serves as the primary operational mechanism for applying all three Belmont principles through protocol review, risk-benefit assessment, and ensuring equitable subject selection. |
| Informed Consent Document | The legally effective document that provides key information to potential subjects to facilitate their understanding and voluntary decision to participate [13]. | The primary instrument for implementing the Respect for Persons principle, ensuring autonomy and voluntary participation. |
| Protocol Risk-Benefit Analysis | A systematic assessment of the research methodology to identify all potential harms and benefits, quantify their likelihood and severity, and justify the study's design [14]. | The formal process for applying the principle of Beneficence, ensuring that risks are minimized and justified by the potential benefits to subjects and society. |
| Inclusion/Exclusion Criteria | The scientifically and ethically justified parameters that define who can and cannot participate in a research study [14]. | The practical application of the Justice principle, ensuring the equitable selection of subjects and fair distribution of both research burdens and benefits. |
| Broad Consent Form | A type of informed consent used for the storage and future use of identifiable private information or biospecimens in unspecified secondary research [12] [17]. | A modern tool for applying Respect for Persons in the context of biobanking and future research, as authorized by the revised Common Rule. |
| Data Use Agreement (DUA) | A contractual agreement required under HIPAA for disclosing a "limited data set" for research, public health, or healthcare operations [17]. | A regulatory tool that supports Beneficence and Justice by enabling research while protecting participant privacy and confidentiality. |
The relationship between the Belmont Report and the Common Rule is a dynamic and enduring partnership between foundational ethics and practical regulation. The Belmont Report's three principles—Respect for Persons, Beneficence, and Justice—have proven remarkably resilient, providing a stable moral compass for decades. Meanwhile, the Common Rule has evolved, most notably in 2017, to apply these principles to new research contexts, from genomic data sharing to centralized IRB review [17] [12].
For researchers, scientists, and drug development professionals, understanding this framework is not merely a regulatory requirement but a core component of scientific integrity. The principles compel a research culture that prioritizes participant autonomy, well-being, and fairness. As research methodologies continue to advance with AI and big data analytics, the Belmont Report's framework provides the necessary guidance to avoid past mistakes and navigate emerging ethical challenges, ensuring that scientific progress never comes at the cost of human dignity [9].
The Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research stands as a foundational document governing the ethical conduct of research involving human subjects in the United States. Created by the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research and published in 1979, this report emerged from a crucial historical context marked by ethical abuses in research [8] [18]. Its creation was prompted in part by the revelations surrounding the Tuskegee Syphilis Study, a decades-long research project in which U.S. health officials condoned unethical practices [8] [19]. The Belmont Report's enduring significance lies in its establishment of three fundamental ethical principles—Respect for Persons, Beneficence, and Justice—which continue to shape federal regulations, institutional review processes, and ethical decision-making in contemporary research landscapes [8] [14].
Historical Context: The Path to Belmont
Pre-Belmont Ethical Codes and Their Limitations
The ethical framework articulated in the Belmont Report did not emerge in a vacuum but rather built upon earlier international codes developed in response to research abuses. The Nuremberg Code (1947), established after the Nazi doctors' trial following World War II, emphasized the "absolute necessity" of voluntary consent from research participants [16] [19]. This was followed by the Declaration of Helsinki (1964), which distinguished between clinical research combined with professional care and non-therapeutic research, while emphasizing beneficence [16]. However, these foundational documents had significant limitations—the Nuremberg Code was drafted with reference to prisoners in concentration camps, while the Declaration of Helsinki provided only vague frameworks for protecting socially vulnerable groups such as children and adults with diminished decision-making capacity [16].
Catalyzing Events: The Tuskegee Syphilis Study
The immediate impetus for creating the Belmont Report came from the public exposure in 1972 of the U.S. Public Health Service Tuskegee Syphilis Study [19]. This study, which began in 1932 and continued for 40 years, involved approximately 600 African American men—399 with syphilis and 201 without the disease—who were deceived about their condition and denied effective treatment even after penicillin became the standard cure in 1947 [19]. The study revealed striking flaws in existing human subject protection policies and demonstrated that current safeguards were insufficient to protect participants from harm [19]. The ensuing public outrage led to a class-action lawsuit and congressional hearings, which ultimately prompted legislative action.
Legislative Foundation: The National Research Act
In direct response to the Tuskegee scandal, the U.S. Congress passed the National Research Act in 1974, which was signed into law by President Richard Nixon [18] [19]. This landmark legislation created the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research (1974-1978) [18]. The Commission consisted of eleven members—eight men and three women—including physicians, lawyers, scientists, and ethicists such as Kenneth John Ryan, Joseph V. Brady, Robert E. Cooke, Dorothy I. Height (the only African-American member), Albert R. Jonsen, Patricia King, and Karen Lebacqz [18]. The Commission was charged with identifying the basic ethical principles that should underlie the conduct of biomedical and behavioral research involving human subjects and developing guidelines to ensure such research would be conducted in accordance with those principles [18].
Table: Key Historical Developments Leading to the Belmont Report
| Year | Document/Event | Key Ethical Contribution | Limitations |
|---|---|---|---|
| 1947 | Nuremberg Code | Established voluntary consent as essential | Focused on prisoners in unique circumstances; limited application to vulnerable populations |
| 1964 | Declaration of Helsinki | Distinguished therapeutic vs. non-therapeutic research; emphasized beneficence | Vague protection framework for vulnerable groups |
| 1932-1972 | Tuskegee Syphilis Study | Revealed systemic ethical failures in U.S. research | Led to public outrage and demand for regulation |
| 1974 | National Research Act | Created National Commission for protection of human subjects | Legislative response to research abuses |
| 1979 | Belmont Report | Articulated three core ethical principles with applications | General moral framework rather than specific regulations |
The Commission's Work and the Belmont Report's Creation
Development Process and Timeline
The National Commission developed the Belmont Report over a comprehensive four-year period from 1974 to 1978 [18]. The Commission was divided into work groups focusing on specific ethical issues, including autonomy, beneficence, non-maleficence, and justice [18]. A particularly intensive four-day discussion period in February 1976 at the Smithsonian Institution's Belmont Conference Center in Elkridge, Maryland (from which the report takes its name) proved pivotal in drafting the document [18]. These discussions were supplemented by monthly deliberations spanning nearly four years, reflecting the complexity and importance of the Commission's charge [18]. The Commission released its final report, "Ethical Principles and Guidelines for the Protection of Human Subjects of Research," on September 30, 1978, with publication in the Federal Register occurring on April 18, 1979 [18].
Charge and Mandate of the National Commission
The National Commission was specifically directed by Congress to consider four crucial areas: (1) the boundaries between biomedical/behavioral research and accepted routine medical practice; (2) the role of risk-benefit assessment in determining appropriate research; (3) appropriate guidelines for selecting human subjects; and (4) the nature and definition of informed consent in various research settings [18]. Unlike most other reports issued by the Commission, the Belmont Report did not make specific recommendations for administrative action but rather was recommended to be adopted in its entirety as a statement of departmental policy for the Department of Health, Education, and Welfare (now Health and Human Services) [18].
The Three Ethical Principles of the Belmont Report
Respect for Persons
The principle of Respect for Persons incorporates two ethical convictions: first, that individuals should be treated as autonomous agents, and second, that persons with diminished autonomy are entitled to protection [14]. This principle divides into two separate moral requirements: the requirement to acknowledge autonomy and the requirement to protect those with diminished autonomy [14]. To fulfill the first requirement, researchers must ensure that subjects enter research voluntarily with adequate information presented in understandable terms, free from duress or coercion [14]. This principle mandates that individuals have the opportunity to ask questions and withdraw from research at any time [14]. For persons with diminished autonomy (such as children, individuals with mental disabilities, or those in compromised circumstances), Respect for Persons requires additional protections that may range from ensuring understanding to excluding them from potentially harmful activities [14]. The extent of protection should depend on the risk of harm and likelihood of benefit, with judgments about autonomy being periodically reevaluated [14].
Beneficence
The principle of Beneficence extends beyond merely respecting decisions and protecting from harm to include affirmative efforts to secure the well-being of research participants [14]. This principle finds expression in two complementary rules: (1) do not harm and (2) maximize possible benefits and minimize possible harms [14]. The Beneficence principle requires researchers and review boards to conduct a systematic assessment of risks and benefits [14]. This entails gathering and assessing comprehensive information about all aspects of the research, considering alternatives systematically, and ensuring that any risks resulting from research participation are justified by potential benefits to either the subject or to society at large [14]. The aim is to make the risk-benefit assessment process more rigorous and communication between institutional review boards (IRBs) and investigators less ambiguous [14].
Justice
The principle of Justice addresses the fair distribution of both the burdens and benefits of research [20] [14]. This principle requires that subjects be selected fairly and that the risks and benefits of research be distributed equitably [14]. The Belmont Report explicitly warns against systematically selecting subjects simply because of their easy availability, compromised position, or due to racial, sexual, economic, or cultural biases in society [14]. The report describes the historical circumstances of the Tuskegee Syphilis Study as a violation of this principle, where economically disadvantaged African American rural men were burdened with the risks of research while the benefits of discovering the natural history of syphilis accrued primarily to others [18]. The report also mentions the exploitation of unwilling prisoners in Nazi concentration camps as another example of distributive injustice [18].
Table: Applications of Belmont Report Principles in Research Practice
| Ethical Principle | Application Area | Specific Requirements | Vulnerabilities Addressed |
|---|---|---|---|
| Respect for Persons | Informed Consent | Information disclosure, comprehension, voluntariness | Coercion, undue influence, deception |
| Beneficence | Risk-Benefit Assessment | Systematic assessment of risks/benefits; minimizing risks | Physical, psychological, legal, social harms |
| Justice | Selection of Subjects | Fair procedures and outcomes in selection | Exploitation of vulnerable populations; biased selection |
The Belmont Report's Relationship to the Common Rule
Incorporation into Federal Regulations
The Belmont Report's principles formed the ethical foundation for the Federal Policy for the Protection of Human Subjects, commonly known as the "Common Rule" [8] [20]. Initially, the Department of Health, Education, and Welfare (DHEW) revised and expanded its regulations for human subject protection (45 CFR part 46) in the late 1970s and early 1980s based on the Belmont framework [18]. In 1991, the Common Rule was formally adopted by 15 federal departments and agencies, establishing uniform rules for federally funded human subjects research [18] [21]. The Common Rule represents the culmination of more than 40 years of development in ethical principles for research, beginning with the Nuremberg Code and extending through the Belmont Report [20]. The procedural requirements of the Common Rule—including informed consent, IRB review, and risk-benefit assessment—are directly based on the three ethical principles articulated in the Belmont Report [20].
Contemporary Relevance and Recent Updates
Despite being over four decades old, the Belmont Report continues to shape research ethics in contemporary settings [8]. In January 2017, the Revised Common Rule was issued with updates that became effective in January 2019 [22] [23]. These revisions were designed to strengthen protections for human subjects while reducing unnecessary burdens on research [21] [13]. Key changes included: broadening categories of research exempt from regulation; streamlining IRB review processes; enhancing informed consent requirements; and implementing a single IRB review for multi-site studies [21] [23]. Notably, the revised regulations incorporated specific elements to address modern research challenges, including requirements to discuss commercial intent, return of research results, and secondary use of data or biospecimens—all reflecting the enduring influence of Belmont's ethical principles in evolving research contexts [13].
Essential Research Ethics Framework Toolkit
For researchers, IRB members, and institutional officials involved in human subjects research, understanding key documents and oversight mechanisms is essential for ethical research conduct. The following toolkit outlines essential components of the research ethics framework:
Table: Essential Research Ethics Framework Components
| Component | Function | Key Features |
|---|---|---|
| Belmont Report | Foundational ethical framework | Articulates three core principles: Respect for Persons, Beneficence, Justice |
| Common Rule (45 CFR 46) | Federal regulatory requirements | Establishes procedures for IRB review, informed consent, risk-benefit assessment |
| Institutional Review Boards (IRBs) | Research oversight committees | Review research protocols, ensure ethical standards, protect subject rights and welfare |
| Informed Consent Documents | Participant information and agreement | Must include key information presented to facilitate understanding, disclose risks/benefits |
| Federalwide Assurance (FWA) | Institutional commitment | Demonstrates institutional compliance with federal human subject protection regulations |
The creation of the Belmont Report represents a watershed moment in the history of research ethics, establishing principled foundations that continue to guide the protection of human subjects nearly five decades later. Born from a specific historical context of ethical failures, particularly the Tuskegee Syphilis Study, the report's framework has demonstrated remarkable resilience and adaptability to evolving research paradigms [8] [19]. The three principles of Respect for Persons, Beneficence, and Justice provide not only historical guidance but also living ethical tools for addressing contemporary challenges in emerging research domains, including genetics, big data analytics, and innovative clinical trial designs [8] [21].
For today's researchers, scientists, and drug development professionals, understanding the origins and ongoing influence of the Belmont Report remains crucial for navigating the complex ethical landscape of human subjects research. The report's principles continue to inform regulatory frameworks, including the recently updated Common Rule, while also providing moral guidance for ethical decision-making in situations not explicitly covered by regulations [13]. As research methodologies and technologies continue to evolve, the Belmont Report's emphasis on fundamental ethical principles ensures its continued relevance in safeguarding human dignity and rights in the research enterprise [8].
The transition from the Belmont Report's ethical principles to the codified Common Rule regulations represents a critical evolution in the protection of human research subjects. This transformation established a systematic framework that has guided researchers, institutions, and oversight bodies for decades. The Belmont Report, formally titled "Ethical Principles and Guidelines for the Protection of Human Subjects of Research," was created by the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research in 1979 following the National Research Act of 1974 [16] [24]. This seminal document emerged from a need to address ethical violations in research, most infamously the Tuskegee Syphilis Study, where researchers deliberately withheld treatment from African American men without their informed consent [24].
The Common Rule, officially known as the Federal Policy for the Protection of Human Subjects, was published in 1991 and represents the regulatory embodiment of the Belmont principles [13] [21]. This regulation established uniform requirements for human subjects research across 15 federal departments and agencies, creating a consistent framework for research oversight [21]. The Common Rule operates primarily through Institutional Review Boards (IRBs) that review research protocols to ensure compliance with these federal standards [24]. Understanding the relationship between the Belmont Report's ethical framework and the Common Rule's regulatory requirements is essential for researchers, scientists, and drug development professionals who must navigate this complex compliance landscape while advancing scientific knowledge.
Historical Context: From Ethical Abuses to Systematic Protections
The path to contemporary research protections began with historical failures that demonstrated the urgent need for standardized ethical guidelines. The Tuskegee Syphilis Study, conducted by the U.S. Public Health Service from 1932 to 1972, exemplified egregious ethical violations where researchers denied effective treatment to 400 African American men with syphilis without their knowledge or consent [24]. This was not an isolated incident; other problematic studies included the Stanford Prison Project and Milgram's obedience studies, which demonstrated that ethical risks extended beyond biomedical research into social and behavioral domains [24].
Prior to the Belmont Report, several international codes had attempted to establish ethical standards. The Nuremberg Code (1947) emerged from the Nazi war crime trials and emphasized "voluntary consent" as an essential condition for research participation, focusing heavily on autonomy principles [16]. The Declaration of Helsinki, first adopted in 1964 by the World Medical Association, distinguished between clinical research combined with professional care and non-therapeutic research, though it provided limited guidance for protecting vulnerable populations [16]. These documents laid important groundwork but proved insufficient to prevent ethical abuses in the U.S. research context.
The U.S. government responded to these ethical failures by passing the National Research Act in 1974, which created the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research [16]. This commission was charged with identifying comprehensive ethical principles for human subjects protection. After four years of deliberation, the commission produced the Belmont Report, named after the Belmont Conference Center where initial discussions were held [24]. The report's publication in 1979 established an ethical foundation that would directly shape federal regulations for decades to follow.
The Ethical Framework of the Belmont Report
The Belmont Report established three fundamental ethical principles that continue to guide human subjects research: Respect for Persons, Beneficence, and Justice [24]. These principles were designed to provide a flexible framework that could be applied across diverse research contexts while maintaining strong ethical safeguards for participants.
Core Ethical Principles
Table 1: Core Ethical Principles of the Belmont Report
| Ethical Principle | Definition | Key Components |
|---|---|---|
| Respect for Persons | Recognition of personal dignity and autonomy of individuals | Recognition of personal dignity and autonomy; Special protection for those with diminished autonomy; Requirement for voluntary informed consent |
| Beneficence | Obligation to protect persons from harm by maximizing benefits and minimizing risks | Maximization of anticipated benefits; Minimization of possible harms; Systematic assessment of risks and benefits |
| Justice | Requirement that the benefits and burdens of research be distributed fairly | Fair distribution of research benefits and burdens; Avoidance of exploiting vulnerable populations; Equitable selection of subjects |
Application Framework
The Belmont Report not only identified these core principles but also specified how they should be applied in practice through three key applications:
Informed Consent: Flowing primarily from the Respect for Persons principle, informed consent requires that participants enter research voluntarily and with adequate information. The process must include information disclosure, participant comprehension, and voluntary participation without coercion or undue influence [16].
Assessment of Risks and Benefits: Derived from the Beneficence principle, this application requires systematic analysis of proposed research to maximize possible benefits and minimize potential risks. Researchers and review boards must carefully assess whether the knowledge gained justifies any risks to participants [16].
Selection of Subjects: The Justice principle applies to the fair selection of research participants at both social and individual levels. This requires examination of research populations to avoid systematically selecting subjects because of their easy availability, compromised position, or manipulability rather than for reasons directly related to the problem being studied [16].
The Common Rule: Regulatory Implementation
The Common Rule (45 CFR Part 46) represents the regulatory codification of the Belmont principles, creating enforceable requirements for federally funded research [13]. First published in 1991 after a decade of development, the Common Rule established uniform human subjects protections across multiple federal agencies [21]. The regulation is organized into subparts that address different research contexts and populations, with Subpart A containing the basic policy that applies to all research, and additional subparts providing special protections for vulnerable populations including pregnant women (Subpart B), prisoners (Subpart C), and children (Subpart D) [13].
The Common Rule operates primarily through the IRB system, requiring that all federally funded research undergo review by an Institutional Review Board to ensure compliance with human subjects protection requirements [24]. These boards are charged with evaluating the risks and benefits of proposed research, reviewing informed consent processes, and ensuring equitable subject selection. The regulatory framework establishes specific criteria for IRB approval, including minimizing risks, ensuring risks are reasonable in relation to anticipated benefits, equitably selecting subjects, and obtaining informed consent [24].
Table 2: Key Regulatory Components of the Common Rule
| Regulatory Component | Description | Connection to Belmont Principles |
|---|---|---|
| IRB Review Requirements | Mandates institutional review of research protocols by an independent board | Implements all three principles through systematic oversight |
| Informed Consent Elements | Specifies required elements of informed consent documents | Direct application of Respect for Persons principle |
| Exempt Research Categories | Defines categories of research exempt from full IRB review | Operationalizes risk assessment based on Beneficence principle |
| Vulnerable Populations Protections | Additional safeguards for prisoners, children, pregnant women | Applies Justice principle to prevent exploitation of vulnerable groups |
| Continuing Review | Requires periodic review of ongoing research | Ensures ongoing adherence to all three ethical principles |
Comparative Analysis: Principle Versus Regulation
The relationship between the Belmont Report's ethical principles and the Common Rule's regulatory requirements represents a complex translation from philosophical framework to enforceable standards. While the Common Rule operationalizes the Belmont principles, the translation is not always direct, with some principles receiving more comprehensive regulatory expression than others.
Direct Regulatory Translations
Table 3: Direct Translation of Belmont Principles into Common Rule Provisions
| Belmont Principle | Common Rule Implementation | Practical Application |
|---|---|---|
| Respect for Persons | Detailed informed consent requirements (§46.116) including required elements and documentation | Mandates specific information that must be provided to research participants; Requires consent process to facilitate understanding |
| Beneficence | IRB risk-benefit assessment requirements (§46.111) | Requires risks to be minimized and reasonable in relation to anticipated benefits; Systematic review of research design |
| Justice | Equitable selection of subjects requirement (§46.111(a)(3)) | Prohibits targeting vulnerable populations without good scientific reason; Ensures fair distribution of research burdens |
Divergences and Limitations
The translation from ethical principle to regulation introduced several important limitations and specific interpretations:
Flexibility vs. Specificity: The Belmont Report provides a flexible ethical framework applicable to diverse research contexts, while the Common Rule establishes specific, enforceable requirements that necessarily reduce flexibility in implementation [16]. This tension between principle and regulation creates challenges in applying the rules to novel research paradigms.
Scope of Application: The Belmont Report was designed as a comprehensive ethical guide for all human subjects research, while the Common Rule initially applied only to federally funded research, creating significant gaps in oversight [9]. This limitation has been partially addressed through the revised Common Rule's extension of protections to all research conducted at U.S. institutions receiving federal funding [21].
Vulnerable Populations: While the Belmont Report's Justice principle broadly addresses fair subject selection, the Common Rule implements specific additional protections for designated vulnerable populations through separate subparts, creating a categorical rather than principles-based approach to vulnerability [13].
The diagram below illustrates the conceptual pathway from ethical principles to regulatory implementation:
Principle to Policy Implementation Pathway
Evolution and Revisions: The 2017 Common Rule Update
The Common Rule underwent significant revision in 2017, with implementation in 2019, representing the first major update since its initial publication in 1991 [25] [13]. These revisions refined the regulatory framework while maintaining the core ethical foundations established by the Belmont Report.
Key Revisions and Their Ethical Implications
Elimination of Continuing Review: The revised Common Rule eliminated continuing review requirements for minimal risk studies that have progressed to data analysis, reducing administrative burden while maintaining protections. This change reflects a more nuanced application of the Beneficence principle, focusing oversight resources where risks are most significant [25].
Informed Consent Revisions: The updated regulations require that consent forms begin with "a concise and focused presentation of key information" to facilitate comprehension, directly enhancing the Respect for Persons principle by promoting genuine understanding rather than mere legal compliance [25] [13].
Exempt Research Categories: The revisions modified and expanded the categories of research exempt from IRB review, including new provisions for benign behavioral interventions and secondary research with identifiable information [25]. These changes reflect a more calibrated approach to oversight based on risk level, consistent with the Beneficence principle's requirement to minimize unnecessary burdens.
Implementation Challenges
The 2017 revisions revealed ongoing tensions between ethical principles and regulatory implementation:
Broad Consent Provisions: The revised Rule introduced new exemption categories for storage and maintenance of identifiable data with broad consent, but some institutions, including Belmont University, chose not to implement these provisions due to concerns about added regulatory burdens and tracking requirements [25].
Comprehension vs. Disclosure: The new requirement that consent forms facilitate comprehension represents a significant shift from a disclosure model to an understanding model, requiring researchers to consider the consent process from the participant's perspective [13]. This change more fully implements the Respect for Persons principle but creates practical challenges in implementation.
Methodological Framework: Analyzing Regulatory Impact
Experimental Protocol for Regulatory Analysis
Researchers studying the impact of regulatory frameworks like the Common Rule employ specific methodological approaches:
Historical Document Analysis: Systematic review of federal register notices, commission reports, and regulatory revisions to trace the development and modification of research protections [16] [21].
Comparative Legal Analysis: Examination of regulatory texts across different time periods (pre-Belmont, post-Belmont, post-Common Rule, revised Common Rule) to identify shifts in regulatory approach and emphasis [16].
Case Study Evaluation: Analysis of specific research ethics cases (e.g., gene therapy trials, international collaborations) to assess how principles are applied in practice [16].
Stakeholder Interview Methodology: Structured interviews with IRB members, researchers, and research participants to evaluate the practical implementation and perceived effectiveness of regulatory frameworks [26].
Research Reagent Solutions for Ethical Analysis
Table 4: Essential Resources for Research Ethics Analysis
| Research Tool | Function | Source/Access |
|---|---|---|
| Belmont Report Text | Primary source document for ethical principles | HHS Office for Human Research Protections website |
| 45 CFR Part 46 | Complete regulatory text of the Common Rule | Electronic Code of Federal Regulations website |
| IRB Decision Databases | Collections of IRB determinations and ethical analyses | Institutional review board records (often available through university libraries) |
| Historical Commission Documents | Records of National Commission deliberations | National Archives and professional bioethics collections |
| International Ethics Codes | Comparative frameworks for analysis | WHO, UNESCO, and Council for International Organizations of Medical Sciences |
Contemporary Applications and Future Directions
The Belmont Report's influence continues to expand beyond traditional biomedical research into emerging fields. Recent applications include:
Artificial Intelligence Research: NIST researchers have proposed applying Belmont principles to AI development, particularly regarding training data collection and algorithm design. The principles of Respect for Persons requires informed consent for data use, Beneficence mandates minimizing harmful biases, and Justice requires addressing potential exclusionary impacts of AI systems [9].
International Research Ethics: The Belmont framework has influenced global research ethics standards, though significant variations persist in how countries implement ethical review processes. Studies show considerable heterogeneity in ethical approval requirements and timelines across different national contexts [26].
Gene Therapy and Emerging Technologies: The ethical framework established by Belmont has been particularly relevant for novel research domains like gene therapy, where the balance between potential benefits and unknown risks requires careful ethical analysis [16].
The enduring relevance of the Belmont Report's principles demonstrates the robustness of its ethical framework, even as research paradigms continue to evolve. The challenge for future policy development will be maintaining the core ethical values while adapting regulatory requirements to address emerging research contexts, from digital health technologies to global collaborative research networks.
The Nuremberg Code and the Declaration of Helsinki established the foundational ethical principles for modern medical research involving human subjects. Developed in direct response to historical atrocities and ethical failures, these documents created the first internationally recognized standards for conducting research with respect, beneficence, and justice. They emerged prior to and influenced the creation of national regulations, most notably the United States' Belmont Report (1979) and the Common Rule (1991). Understanding these cornerstone guidelines is essential for comprehending the evolution of the ethical framework that governs clinical research today. This guide provides an objective comparison of these pivotal documents, detailing their core principles, operational mechanisms, and enduring impact on the field of human subjects research.
Historical Context and Genesis
The development of both the Nuremberg Code and the Declaration of Helsinki was driven by the necessity to prevent the recurrence of ethical abuses in medical research.
The Nuremberg Code (1947) was formulated by the U.S. judges presiding over the "Doctors' Trial" of Nazi physicians after World War II. The trial exposed horrific medical experiments conducted on concentration camp inmates without their consent. The Code was drafted as a part of the legal judgment to outline permissible medical experimentation, establishing for the first time that "the voluntary consent of the human subject is absolutely essential." [27] It was a direct, post-hoc legal and ethical response to unprecedented crimes against humanity.
The Declaration of Helsinki (1964), adopted by the World Medical Association (WMA), was influenced by the Nuremberg Code but designed as a set of ethical principles for the global medical community itself. The WMA recognized that the Nuremberg Code, while crucial, was a legal document created by jurists. Physicians felt a need for their own professional code, which would be more detailed and applicable to the changing landscape of medical research [28]. It has been revised multiple times (most recently in 2024) to address emerging ethical challenges, evidencing its dynamic nature compared to the static Nuremberg Code [29] [28].
The Path to the Common Rule: The principles enshrined in these two documents heavily influenced the U.S. Belmont Report of 1979, which distilled ethical principles into a three-part framework: Respect for Persons, Beneficence, and Justice [8] [14]. The Belmont Report, in turn, became the ethical foundation for the Common Rule (the Federal Policy for the Protection of Human Subjects), formalized in 1991 and revised in 2018, which provides the specific regulatory requirements for U.S. federally-funded research [23].
Comparative Analysis of Core Principles
The following tables provide a detailed, point-by-point comparison of the ethical and operational elements of the Nuremberg Code and the Declaration of Helsinki.
Table 1: Comparison of Foundational Ethical Principles
| Feature | Nuremberg Code (1947) | Declaration of Helsinki (1964, as amended) |
|---|---|---|
| Primary Origin | Legal judgment from the Nazi Doctors' Trial [27] | Professional body (World Medical Association) [29] [28] |
| Primary Focus | Permissible medical experiments on human subjects | Ethical principles for medical research involving human participants [29] |
| Governance | Static document; not updated [27] | Living document; regularly amended (last in 2024) [29] [28] |
| View of Subject | Autonomous agent who must consent | Participant, who may be a patient; recognizes vulnerability [29] |
| Beneficence | Implied in principles to avoid unnecessary suffering | Explicitly stated; requires risk assessment and monitoring [29] |
| Justice | Not explicitly addressed | Explicitly addressed; mandates fair selection of subjects and consideration of vulnerable groups [29] |
| Scope | Focused on interventional research | Covers all medical research, including identifiable human material/data [29] |
Table 2: Comparison of Operational Requirements and Protections
| Feature | Nuremberg Code (1947) | Declaration of Helsinki (1964, as amended) |
|---|---|---|
| Informed Consent | Absolute and central requirement; must be voluntary, competent, and informed [27] | Essential component of respect for autonomy; must be obtained from participant or legally authorized representative [29] |
| Risk/Benefit Assessment | Requires benefits to outweigh risks; experiment should be based on prior knowledge [27] | Requires research protocol with explicit risk/benefit assessment; risks must be continuously monitored [29] |
| Scientific Validity | Must be based on sound science and prior animal testing [27] | Must have scientifically sound protocol likely to produce reliable and valuable knowledge [29] |
| Oversight Mechanism | No formal external oversight body mentioned; responsibility is on the investigator | Mandates independent research ethics committee (REC/IRB) review and approval before research begins [29] |
| Vulnerable Populations | No specific provisions | Explicit protections for vulnerable individuals and populations; research is only justified if responsive to their health needs [29] |
| Placebo Use | No specific guidance | Specific guidance: new intervention should be tested against best-proven ones, with risk minimization in placebo use [30] |
| Post-Trial Access | No specific guidance | Explicit obligation to provide post-trial access to the best-proven interventions for all who need them [30] |
Experimental Protocols & Methodologies of Ethical Application
The following workflow visualizes the process of applying these historical ethical principles to a modern research protocol, demonstrating how their core tenets are integrated into contemporary practice.
The Scientist's Toolkit: Essential Components for Ethical Research
This table details the key conceptual "tools" derived from the Nuremberg Code and Declaration of Helsinki that researchers must employ to ensure ethical integrity.
Table 3: Essential Ethical Framework Components for Research
| Component | Function in the Ethical Framework | Primary Source |
|---|---|---|
| Informed Consent Form | Documents the process of providing full information to and obtaining voluntary, comprehended agreement from a research participant. | Nuremberg Code [27] |
| Research Protocol | The detailed plan describing the research rationale, objectives, methodology, and statistical considerations, plus an explicit ethical section. | Declaration of Helsinki [29] |
| Ethics Committee (IRB/REC) | An independent committee that reviews, approves, and monitors research to protect the rights, safety, and well-being of human participants. | Declaration of Helsinki [29] |
| Vulnerability Assessment | The process of identifying individuals or groups with diminished autonomy who require specific additional protections to participate in research. | Declaration of Helsinki [29] |
| Risk-Benefit Analysis | A systematic assessment to ensure that the foreseeable benefits of the research justify the risks assumed by the participants. | Nuremberg Code & Declaration of Helsinki [27] [29] |
Data Presentation: Impact and Modern Relevance
The enduring influence of these pre-Common Rule guidelines is evident in their direct lineage to modern regulations and their continued citation in international research standards.
Table 4: Legacy and Modern Relevance
| Aspect | Nuremberg Code | Declaration of Helsinki |
|---|---|---|
| Direct Descendant | Served as a primary model for the ethical principles in the Belmont Report [14]. | Principles incorporated into ICH-GCP E6 guidelines, the international standard for clinical trials. |
| Regulatory Influence | Its emphasis on informed consent is codified in FDA regulations (21 CFR 50) [23]. | Its requirement for ethics committee review is a cornerstone of the Common Rule (45 CFR 46) [8] [23]. |
| Contemporary Citations | Often cited for its powerful, absolute stance on voluntary consent. | Required by most international medical journals; research must conform to its principles for publication. |
| Addressing Modern Challenges | Limited by its static nature, making it less applicable to new data-driven research paradigms. | Actively revised; the 2024 update addresses data-driven research, broad consent, and dynamic consent for data use [30] [28]. |
The Nuremberg Code and the Declaration of Helsinki are not merely historical artifacts; they are the living pillars of research ethics. The Nuremberg Code established the non-negotiable primacy of voluntary informed consent, placing the welfare of the individual subject above the interests of science and society. The Declaration of Helsinki built upon this, providing a more comprehensive and adaptable framework that introduced critical operational structures like independent ethics review, explicit protections for vulnerable populations, and post-trial obligations. Together, they created the ethical DNA that was later codified in national regulations like the U.S. Belmont Report and Common Rule. For today's researchers and drug development professionals, a deep understanding of these documents is not optional. It is essential for designing ethically sound research, navigating complex regulatory landscapes, and, most importantly, maintaining the trust of the public and research participants by upholding the highest standards of ethical conduct.
From Principle to Practice: Implementing the Common Rule in Modern Research
The Common Rule is the foundational set of federal regulations governing human subjects research in the United States. Formally known as the Federal Policy for the Protection of Human Subjects, it provides the core ethical framework and procedural requirements for research involving human participants [20]. Established in 1991 and significantly revised in 2018, the Common Rule represents a collaborative effort across multiple federal departments and agencies to create uniform protections for research subjects [31] [32]. This regulatory framework operationalizes the ethical principles first articulated in the Belmont Report—respect for persons, beneficence, and justice—into concrete requirements for institutional review boards (IRBs), informed consent processes, and research oversight [20] [8]. Understanding the Common Rule's scope, participating agencies, and key definitions is essential for researchers, scientists, and drug development professionals conducting human subjects research.
Historical and Ethical Foundations
The Common Rule has its origins in a series of historical developments responding to research abuses. The Nuremberg Code (1947) established the absolute requirement for voluntary consent after the Nazi experimental atrocities [33]. In the United States, the Belmont Report (1979) subsequently identified three fundamental ethical principles for human subjects research [8] [14]:
- Respect for Persons: Recognizing personal dignity and autonomy through voluntary informed consent
- Beneficence: Obligation to protect from harm and maximize benefits while minimizing risks
- Justice: Fair distribution of research benefits and burdens across populations [14]
The Common Rule represents the regulatory embodiment of these ethical principles, translating them into enforceable requirements for federally conducted or supported research [20].
Scope and Applicability
What Activities Are Covered?
The Common Rule applies to "human subjects research" conducted or supported by any of the federal departments and agencies that have adopted the regulations [34]. The definition encompasses:
- Research: A systematic investigation designed to develop or contribute to generalizable knowledge
- Human Subject: A living individual about whom an investigator obtains either (1) data through intervention or interaction, or (2) identifiable private information [35]
Key Exceptions and Exclusions
Certain activities are specifically excluded from Common Rule oversight, including:
- Scholarly and journalistic activities
- Public health surveillance
- Collection of information for criminal justice purposes
- Operational activities for national security missions [31]
Federal Agencies Subject to the Common Rule
The Common Rule achieves its name from its adoption across multiple federal departments and agencies. The table below summarizes the complete list of participating entities:
| Agency/Department | CFR Citation | Adoption Status |
|---|---|---|
| Department of Agriculture | 7 CFR Part 1c | Full Common Rule |
| Department of Energy | 10 CFR Part 745 | Full Common Rule |
| National Aeronautics and Space Administration (NASA) | 14 CFR Part 1230 | Full Common Rule |
| Department of Commerce | 15 CFR Part 27 | Full Common Rule |
| Consumer Product Safety Commission | 16 CFR Part 1028 | Full Common Rule |
| Agency for International Development (USAID) | 22 CFR Part 225 | Full Common Rule |
| Department of Housing and Urban Development | 24 CFR Part 60 | Full Common Rule |
| Department of Justice/National Institute of Justice | 28 CFR Part 46 | Full Common Rule |
| Department of Defense | 32 CFR Part 219 | Full Common Rule |
| Department of Education | 34 CFR Part 97 | Full Common Rule |
| Department of Veterans Affairs | 38 CFR Part 16 | Full Common Rule |
| Environmental Protection Agency | 40 CFR Part 26 | Full Common Rule |
| Department of Health and Human Services (HHS) | 45 CFR Part 46 | Full Common Rule |
| National Science Foundation (NSF) | 45 CFR Part 690 | Full Common Rule |
| Department of Transportation | 49 CFR Part 11 | Full Common Rule |
| Central Intelligence Agency | Executive Order 12333 | Complies with all subparts of 45 CFR Part 46 |
| Department of Homeland Security | 6 U.S.C. section 112 | Applies all subparts of 45 CFR Part 46 |
| Social Security Administration | 42 U.S.C. section 901 | Applies all subparts of 45 CFR Part 46 |
Table 1: Federal departments and agencies adhering to the Common Rule [34]
Special Considerations for FDA and DOJ Research
The 2018 revised Common Rule does not currently apply to FDA-regulated research or studies supported by the Department of Justice, as these entities have not adopted the updated regulations [31] [32]. Researchers working under these jurisdictions must comply with the pre-2018 requirements.
Key Regulatory Definitions and Concepts
Core Terminology
The Common Rule establishes specific definitions for critical concepts in human research protections:
Diagram 1: Relationship of Core Common Rule Definitions
Minimal Risk: A fundamental concept in the Common Rule framework, defined as situations where "the probability and magnitude of harm or discomfort anticipated in the research are not greater in and of themselves than those ordinarily encountered in daily life or during the performance of routine physical or psychological examinations or tests" [35]. This determination directly affects the level of IRB review required and potential exemptions.
Exempt Research: Certain categories of minimal risk research may be designated as exempt from some regulatory requirements, though note that "exempt" does not necessarily mean exempt from all IRB review [36]. The 2018 revisions modified several exemption categories, including those for educational research, benign behavioral interventions, and secondary research with identifiable data [36].
The Three Review Levels
The Common Rule establishes three distinct levels of IRB review based on risk assessment:
- Exempt Review: For specific minimal risk categories where some regulatory requirements do not apply
- Expedited Review: For minimal risk research not qualifying for exemption
- Full Board Review: For research greater than minimal risk [36]
The 2018 Common Rule Revisions
The Common Rule underwent significant modernization in 2018, with key changes including:
Enhanced Informed Consent Requirements
The revised rule introduced new requirements for informed consent, including:
- Key Information presentation: A concise, focused presentation of the most important information must appear at the beginning of consent documents
- Reasonable Person Standard: Consent must include information a "reasonable person" would want to make an informed decision [31] [32]
New Exemption Categories and Limited IRB Review
The 2018 revisions established:
- Benign Behavioral Interventions: New category for certain low-risk behavioral studies
- Limited IRB Review: A new process for certain exempt categories to ensure adequate privacy and confidentiality protections [36] [32]
Reduced Continuing Review Requirements
The updated regulations eliminated continuing review requirements for:
- Studies reviewed through expedited review procedures
- Research that has progressed to data analysis only
- Studies involving only observational follow-up in standard clinical care [32]
Essential Researcher Toolkit: Common Rule Compliance
| Compliance Tool | Function | Application Context |
|---|---|---|
| Institutional Review Board (IRB) | Independent ethics committee that reviews research protocols | Required for all non-exempt human subjects research |
| Informed Consent Documents | Provides comprehensive study information to potential participants | Required element for most research, with specific content requirements |
| Federalwide Assurance (FWA) | Institutional commitment to comply with Common Rule regulations | Required for institutions receiving federal research support |
| Exemption Determination | Assessment of whether research qualifies for exempt status | Conducted by IRB, not individual investigators |
| Limited IRB Review | Special review for certain exempt categories | Required for exempt research involving collection of sensitive, identifiable data |
| Single IRB Review | Use of one IRB for multi-institutional studies | Required for most collaborative research as of 2020 |
Table 2: Essential Compliance Tools for Common Rule Research
Relationship to the Belmont Report Ethical Framework
The Common Rule operationalizes the ethical principles established in the Belmont Report through specific regulatory requirements:
Diagram 2: Relationship Between Belmont Report Principles and Common Rule Requirements
The Common Rule establishes the essential regulatory framework for human subjects research protection across the federal government. Its comprehensive scope, adoption by multiple agencies, and precise definitions create a uniform system for ethical research oversight that translates the Belmont Report's ethical principles into enforceable standards. For researchers and drug development professionals, understanding the Common Rule's requirements—including the 2018 revisions—is fundamental to designing and conducting compliant, ethical research that protects participant rights and welfare while advancing scientific knowledge.
The Belmont Report, published in 1979, established a foundational ethical framework for research involving human subjects in the United States, built upon three core principles: Respect for Persons, Beneficence, and Justice [37]. The operationalization of these principles, particularly Respect for Persons, is codified in the federal regulations known as the Common Rule, specifically within the informed consent stipulations of 45 CFR 46.116 [38] [20]. For researchers, scientists, and drug development professionals, understanding the direct translation from the Belmont's ethical convictions to the specific, actionable requirements of the Common Rule is critical for designing and conducting ethically sound research. This guide provides a detailed comparison of these two documents, focusing on how the abstract concept of Respect for Persons is concretely realized in the enforceable rules governing informed consent.
The Conceptual Framework: Deconstructing "Respect for Persons"
The Belmont Report's principle of Respect for Persons encompasses two distinct but related ethical convictions [14]:
- First, that individuals should be treated as autonomous agents, capable of forming intentions and acting on them.
- Second, that persons with diminished autonomy are entitled to special protections.
This principle gives rise to corresponding moral requirements: the obligation to acknowledge autonomy and the obligation to protect those with diminished autonomy [14]. In the context of research, the primary application of Respect for Persons is through the process of informed consent, which ensures that individuals have the opportunity to choose what shall or shall not happen to them [14]. The Belmont Report specifies that to respect autonomy is to give weight to individuals' considered opinions and choices while refraining from obstructing their actions unless those actions are clearly detrimental to others. The system of informed consent is the practical instrument that operationalizes this ethical duty.
45 CFR 46.116, a key section of the Common Rule, delineates the general requirements for informed consent [38]. These regulations provide the specific, procedural requirements that Institutional Review Boards (IRBs) and researchers must follow to ensure the protection of human subjects. The Common Rule itself represents the culmination of decades of ethical development, with the Belmont Report serving as its foundational ethical base [20]. The regulations outline several types of consent: standard informed consent with basic and additional elements, broad consent for future research uses of identifiable private information or biospecimens, and provisions for waiver or alteration of consent under specific, limited circumstances [38]. The following sections break down how each aspect of the Belmont's Respect for Persons principle maps onto these regulatory requirements.
Comparative Analysis: Mapping Ethical Principles to Regulatory Requirements
The table below provides a detailed comparison, illustrating how the ethical concepts in the Belmont Report are operationalized into specific regulatory requirements within 45 CFR 46.116.
Table 1: Translation of "Respect for Persons" from Ethical Principle to Regulatory Requirement
| Ethical Component (From Belmont Report) | Regulatory Translation (45 CFR 46.116) | Key Regulatory Citations |
|---|---|---|
| Acknowledgment of Autonomy | Requires that informed consent must be sought only under circumstances that provide sufficient opportunity for discussion and consideration, minimizing possibility of coercion or undue influence. | §46.116(a)(2) [38] |
| Voluntary Participation | Mandates a statement that participation is voluntary, refusal involves no penalty/loss of benefits, and the subject may discontinue at any time without penalty. | §46.116(b)(8) [38] |
| Provision of Comprehensible Information | Stipulates that information given must be in language understandable to the subject or their representative. | §46.116(a)(3) [38] |
| Key Information for Decision-Making | Requires consent to begin with a concise presentation of key information most likely to assist understanding. Requires providing information a reasonable person would want to make an informed decision. | §46.116(a)(4), §46.116(a)(5)(i) [38] |
| Facilitation of Comprehension | Mandates that consent as a whole must be organized to facilitate understanding, not just provide lists of isolated facts. | §46.116(a)(5)(ii) [38] |
| Protection of Legal Rights | Prohibits inclusion of exculpatory language through which the subject appears to waive legal rights or release investigators from liability for negligence. | §46.116(a)(6) [38] |
| Respect for Privacy & Confidentiality | Requires a statement describing the extent to which confidentiality of records identifying the subject will be maintained. | §46.116(b)(5) [38] |
| Opportunity for Questions & Withdrawal | Mandates an explanation of whom to contact for answers about the research and subjects' rights. The right to withdraw is explicitly stated. | §46.116(b)(7), §46.116(b)(8) [38] |
The Informed Consent Workflow: From Principle to Practice
The following diagram visualizes the logical workflow through which the ethical principle of Respect for Persons is translated into the operational components of a legally effective informed consent process as mandated by 45 CFR 46.116.
Essential Research Reagents for Ethical Protocol Development
For researchers designing studies requiring informed consent, specific documents and protocols serve as essential "research reagents" to ensure regulatory compliance and ethical integrity.
Table 2: Key Materials for Developing an Ethically Compliant Informed Consent Process
| Research Reagent | Function & Purpose | Regulatory/Ethical Basis |
|---|---|---|
| IRB-Approved Consent Document | Serves as the physical instrument containing all required elements of informed consent; provides a structured script for the consent conversation. | 45 CFR 46.116(b) [38] |
| Consent Process Script | Guides the researcher in delivering consistent, complete information to all potential subjects, ensuring key points are not omitted. | Belmont Report [14] |
| Vulnerable Population Assessment Tool | A checklist or protocol to identify subjects who may require additional protections due to diminished autonomy. | Belmont Report [14] |
| Documentation of Consent | A system (signed form, electronic record) to provide evidence that consent was obtained appropriately. | 45 CFR 46.117 (Not in results, but implied) |
| HIPAA Authorization Form | If applicable, separate authorization for use and disclosure of protected health information. | HIPAA Regulations |
| IRB Approval Letter | Official documentation that the research protocol, including the consent process, has been reviewed and approved by an ethics board. | 45 CFR 46.109 [20] |
The relationship between the Belmont Report and 45 CFR 46.116 is fundamentally symbiotic. The Belmont Report provides the "why"—the ethical underpinnings and moral imperatives for protecting human subjects—while the Common Rule provides the "how"—the specific, enforceable procedures to realize those ethical commitments in practice [20]. For researchers and drug development professionals, a deep understanding of this relationship is not merely a regulatory obligation but a cornerstone of responsible scientific inquiry. By seeing the informed consent requirements of §46.116 as the direct operationalization of the principle of Respect for Persons, the research community can ensure that its work remains grounded in the fundamental ethical values that protect individual dignity and autonomy.
The principle of beneficence, as articulated in the Belmont Report, forms a foundational pillar for the ethical conduct of human subjects research. This principle imposes a dual obligation: to "do no harm" and to "maximize possible benefits and minimize possible harms" [14]. For Institutional Review Boards (IRBs), applying beneficence is not a abstract concept but a practical requirement enacted through rigorous risk-benefit analysis and continuous safety monitoring. This process ensures that the welfare of research participants is protected and that the potential value of scientific knowledge justifies any inherent risks [39]. The Common Rule operationalizes this principle by mandating that IRBs ensure "risks to subjects are reasonable in relation to anticipated benefits" [39]. Recent evidence, however, reveals significant challenges in this process. A 2025 national survey of IRB chairs found that two-thirds of respondents found risk-benefit analysis for early-phase clinical trials more challenging than for later-phase trials, and more than one-third did not feel "very prepared" to assess the scientific value of these trials or their risks and benefits to participants [40] [41]. This guide examines how beneficence is applied through contemporary IRB practices, comparing methodological approaches and highlighting the tools essential for ethical research oversight.
IRB Review Processes: Operationalizing Beneficence
The IRB review process serves as the primary mechanism for applying beneficence in human subjects research. IRBs are formally designated groups charged with reviewing and monitoring biomedical research to protect the rights and welfare of human subjects [42]. Their review serves to evaluate the ethical dimensions of research protocols, with particular emphasis on the balance of risks and benefits.
Risk Categorization and Assessment
IRBs systematically categorize and evaluate research risks as a foundational step in applying beneficence. The assessment begins with determining whether research presents minimal risk—defined as risks not greater than those encountered in daily life or routine examinations—or greater than minimal risk [39]. This distinction dictates the level of scrutiny and permissible regulatory categories for approval.
IRBs typically evaluate several distinct categories of potential harm:
- Physical risks: Including discomfort, pain, injury, or illness resulting from research procedures [39]
- Psychological risks: Potential for negative affective states such as anxiety, depression, guilt, or loss of self-esteem [39]
- Social risks: Potential damage to relationships with others, including embarrassment or loss of respect [39]
- Economic risks: Financial harms such as loss of wages, costs of non-routine procedures, or damage to employability [39]
- Legal risks: Potential for subjects or others to face criminal or civil liability as a result of participation [39]
Table 1: Risk Categories and Minimization Strategies in Human Subjects Research
| Risk Category | Examples | Minimization Strategies |
|---|---|---|
| Physical | Pain from venipuncture, drug side effects | Combine research procedures with clinical care; use safest available techniques |
| Psychological | Anxiety from survey questions, emotional distress | Provide counseling resources; allow skipping of sensitive questions |
| Social | Stigma from diagnosis disclosure, embarrassment | Protect confidentiality; use coding systems for sensitive data |
| Economic | Lost wages due to study visits, transportation costs | Schedule visits at convenient times; provide compensation for time |
| Legal | Revelation of illegal behaviors | Obtain Certificate of Confidentiality; limit data collection to essentials |
Benefit Assessment and Categorization
In parallel with risk assessment, IRBs must identify and evaluate potential benefits of research participation. These benefits fall into three distinct categories identified by ethicist Nancy King:
- Direct benefit: A therapeutic advantage arising from receiving the intervention being studied [39]
- Collateral benefit: Advantages from being a research subject independent of the experimental intervention (e.g., additional health monitoring, personal gratification of altruism) [39]
- Aspirational benefit: Benefits to society or future patients resulting from knowledge gained through the study [39]
When describing anticipated benefits in consent documents, researchers must clearly distinguish between direct benefits (which are often uncertain in research contexts) and indirect benefits, ensuring participants do not enroll based on unrealistic expectations [39].
Methodological Approaches to Risk-Benefit Analysis
Qualitative and Quantitative Frameworks
The process of risk-benefit analysis has traditionally relied on qualitative, expert-driven assessment. However, there is a growing shift toward more quantitative approaches that offer greater transparency and consistency [43]. A 2025 survey of IRB chairs revealed that over two-thirds of respondents reported that additional resources, like a standardized process for conducting risk-benefit analysis, would be "mostly or very valuable," indicating demand for more structured approaches [40].
A proposed quantitative benefit-risk framework (BRF) incorporates four key factors into a structured equation:
This approach aims to compare benefits and risks on a common scale of health impact, where benefits promote health and harms diminish it [43]. The framework operationalizes beneficence by requiring systematic assessment of each component:
- Frequency of Benefit: The probability that participants will experience the desired therapeutic outcome
- Severity of Disease: The impact of the underlying condition on normal functioning and activities of daily living
- Frequency of Adverse Reactions: The probability of harmful events occurring
- Severity of Adverse Reactions: The impact of harmful events on normal functioning, often graded using standardized scales like the Common Terminology Criteria for Adverse Events (CTCAE) [43]
Challenges in Early-Phase Trial Assessment
Risk-benefit analysis presents particular challenges for early-phase clinical trials (phase 1 and 2), where uncertainty about risks and benefits is highest. The national survey of IRB chairs found specific difficulties in reviewing early-phase neurology trials, where "the unique nature of human cognition, behavior, emotion, and volition means that there are no reliable animal models in which to study these phenomena" [40]. In these contexts, IRBs must rely heavily on preclinical evidence that may be subject to publication bias and design flaws [40].
Table 2: IRB Chair Preparedness and Challenges in Early-Phase Trial Review (2025 Survey Data)
| Aspect of Risk-Benefit Analysis | Percentage Not Feeling "Very Prepared" | Key Challenges Identified |
|---|---|---|
| Assessing scientific value of trials | ~33% | Reliance on equivocal preclinical evidence; high drug attrition rates in neurology |
| Assessing risks and benefits to participants | ~33% | Extrapolating from preclinical studies to human populations |
| Overall process for early-phase trials | 66% found "more challenging" than later phases | Lack of standardized assessment frameworks; variability in review quality |
The data reveals a concerning gap between IRB confidence in their overall performance (91% rated their IRB as doing an "excellent" or "very good" job) and their personal preparedness for specific challenging aspects of risk-benefit analysis [40] [41]. This suggests that while IRBs feel generally competent, they recognize the particular difficulties presented by early-phase trials and desire more supportive resources.
Data and Safety Monitoring: Ensuring Ongoing Beneficence
Applying beneficence extends beyond initial review to encompass ongoing monitoring throughout the research lifecycle. The Data and Safety Monitoring Plan (DSMP) represents the systematic implementation of beneficence during trial conduct, ensuring continuous evaluation of participant safety and research integrity [44].
Core Components of Safety Monitoring
A comprehensive DSMP must include several essential elements that operationalize the principle of beneficence through active oversight:
- Protocol summary: Including study design, outcome measures, sample size, and target population [44]
- Roles and responsibilities: Identification of qualified individuals responsible for monitoring (e.g., principal investigator, independent safety monitor, Data and Safety Monitoring Board) [44]
- Trial safety provisions: Measures to protect participants, privacy protections, stopping rules, and conflict of interest management [44]
- Reportable events documentation: Processes and timelines for collecting and reporting adverse events and unanticipated problems [44]
- Data management and analysis: Security measures for data protection and quality assurance procedures [44]
Monitoring Intensity and Risk Stratification
The University of Iowa's updated compliance monitoring program exemplifies a risk-based approach to implementing beneficence through stratified oversight. Studies are selected for monitoring based on risk level, with the depth of record review corresponding to the potential for harm:
- Level 1 (Minimal risk): 10% of records reviewed
- Level 2 (Low risk): 20% of records reviewed
- Level 3 (Moderate risk): 50% of records reviewed
- Level 4 (High risk): 100% of records reviewed [45]
This graduated approach directs the most intensive monitoring resources toward studies with the highest potential for harm, maximizing the protective benefits while using institutional resources efficiently.
Data and Safety Monitoring Boards
For higher-risk studies, particularly NIH-defined Phase III trials or multisite clinical trials, the appointment of a Data and Safety Monitoring Board (DSMB) is required [44]. These independent groups of experts provide an additional layer of beneficent oversight by reviewing accumulating study data for:
- Participant safety
- Study conduct and progress
- Data integrity
- Continuing scientific validity [44]
DSMB members must be independent from professional or financial conflicts of interest with the research to ensure objective evaluation that prioritizes participant welfare [44].
Implementing beneficence requires specific tools and frameworks to guide ethical decision-making. The following resources represent essential components for researchers and IRB members engaged in risk-benefit analysis and safety monitoring:
Table 3: Essential Resources for Ethical Review and Safety Monitoring
| Resource/Tool | Function | Application Context |
|---|---|---|
| Belmont Report Ethical Framework | Provides foundational principles (respect for persons, beneficence, justice) for ethical review | All human subjects research; required reference for IRB deliberations [14] |
| Common Terminology Criteria for Adverse Events (CTCAE) | Standardized grading system for adverse event severity using 1-5 scale | Clinical trials, particularly in oncology; enables consistent risk assessment [43] |
| Data and Safety Monitoring Plan (DSMP) Template | Structured framework for ongoing safety oversight | Required for clinical trials; commensurate with study risk level [44] |
| Benefit-Risk Framework (BRF) | Quantitative approach to comparing potential benefits and harms | Protocol development and IRB review; supports transparent decision-making [43] |
| Informed Consent Checklist | Ensures required elements of informed consent are included | Consent document preparation and review; regulatory compliance [14] [42] |
Applying the principle of beneficence through IRB review, risk-benefit analysis, and data safety monitoring remains both a foundational ethical obligation and a practical challenge. While the Belmont Report continues to provide the ethical framework for human subjects protection decades after its publication [8], contemporary research reveals significant gaps in preparedness for reviewing the most challenging protocols, particularly early-phase trials [40]. The development of more standardized, quantitative benefit-risk frameworks and risk-proportionate monitoring approaches represents meaningful progress in operationalizing beneficence. However, the consistent identification of preparedness gaps among IRB chairs suggests a continued need for better tools, training, and support structures. As clinical research methodologies evolve, so too must the frameworks for ensuring participant welfare, requiring ongoing refinement of these essential protective mechanisms.
The pursuit of scientific knowledge through human subjects research carries profound ethical responsibilities, particularly concerning the just selection of participants. The Belmont Report, published in 1978, established a foundational ethical framework for research in the United States, while the Federal Policy for the Protection of Human Subjects, known as the Common Rule, translates these principles into enforceable regulations [18] [20]. This guide examines the requirements for equitable subject selection, comparing the ethical ideals of the Belmont Report with the specific, actionable mandates of the Common Rule. For researchers, scientists, and drug development professionals, understanding the interplay between these two documents is crucial for designing ethically sound and regulatory-compliant research protocols. The principle of justice, a core tenet of the Belmont Report, demands a fair distribution of the burdens and benefits of research, a requirement that the Common Rule seeks to operationalize through specific procedural and review requirements [18] [11].
The historical context of this issue underscores its importance. The Belmont Report itself was created by the National Commission for the Protection of Human Subjects, partly in response to ethical atrocities such as the Tuskegee Syphilis Study, where the burdens of research were unjustly borne by a vulnerable population [18] [11]. The report identifies three core ethical principles: Respect for Persons, Beneficence, and Justice [18]. This article focuses on the principle of justice, which deals with the fair distribution of the costs and benefits of research and the fair selection of subjects, ensuring no group is either unduly burdened or unfairly excluded from the potential benefits of participation [18] [20] [11].
Historical and Regulatory Evolution
The ethical and regulatory landscape for human subjects research has evolved significantly. Table 1 outlines the key milestones from the Belmont Report to the Revised Common Rule.
Table 1: Historical Timeline of Ethical Guidelines and Regulations
| Year | Document/Policy | Key Development |
|---|---|---|
| 1978 | Belmont Report | Established three core ethical principles: Respect for Persons, Beneficence, and Justice [18]. |
| 1979 | Belmont Report Published | Published in the Federal Register on April 18, 1979 [18]. |
| 1991 | Common Rule | Codified as a uniform set of rules for 17 federal agencies to protect human subjects, based on the Belmont principles [46] [20]. |
| 2017 | Revised Common Rule | Final Rule issued on January 19, 2017, introducing significant updates [18] [31]. |
| 2019 | Revised Common Rule Effective | Most revisions took effect on January 21, 2019 [47] [31]. |
The relationship between the Belmont Report and the Common Rule is that of a foundational ethical compass and its subsequent regulatory implementation. The Common Rule's procedural requirements for Institutional Review Board (IRB) review and informed consent are based directly on the ethical principles of respect for persons, beneficence, and justice described in the Belmont Report [20]. The 2019 revision to the Common Rule did not alter these foundational principles but refined the regulatory requirements to address advancements in research and implementation challenges [46] [31]. Notably, the Belmont Report was formally instituted as part of the federal policy with these revisions [18].
Comparative Analysis: Justice in Belmont vs. Common Rule
The principle of justice, as articulated in the Belmont Report, is broad and philosophical. The report states that justice deals with the fair distribution of the benefits and burdens of research, asking whether some classes of subjects are being selected simply for reasons of administrative convenience or because they are easy to manipulate, rather than for reasons directly related to the problem being studied [18]. It specifically mentions the exploitation of unwilling prisoners in Nazi concentration camps and the injustice of the Tuskegee Syphilis Study, where disadvantaged rural Black men were burdened with the risks of research without a fair distribution of the benefits [18]. The report proposes five formulations for distributive justice: equal share, individual need, individual effort, societal contribution, and merit [18].
In contrast, the Common Rule provides the concrete regulatory mechanisms to uphold this principle. Its requirements are less about defining justice and more about creating a system of review and oversight to prevent injustice. Table 2 provides a direct comparison of how the concept of justice is addressed in each document.
Table 2: Comparison of Justice Requirements in the Belmont Report and Common Rule
| Aspect | Belmont Report (Ethical Principles) | Common Rule (Regulatory Requirements) |
|---|---|---|
| Core Focus | Fair distribution of research benefits and burdens; avoidance of exploiting vulnerable populations [18] [11]. | IRB review to ensure equitable selection of subjects; additional protections for vulnerable subjects [20]. |
| Subject Selection | Must be fair and not systematically select subjects based on ease of availability, compromised position, or manipulability [18]. | IRB must review and approve proposed subject selection to ensure equitable (e.g., not limited to specific racial, gender, or institutional groups) [20]. |
| Vulnerable Populations | Recognizes that some groups (e.g., children, those with diminished autonomy) require additional protections [18]. | Includes additional regulatory subparts (B, C, D) for specific protections for pregnant women, prisoners, and children [20]. |
| Regulatory Mechanism | Serves as an analytical framework or moral compass [11]. | Mandates IRB review, informed consent, and adherence to specific procedures for waiver or alteration of consent [20] [31]. |
The following diagram illustrates the logical flow from the ethical principle of justice to its specific regulatory applications in the research protocol lifecycle.
Experimental Protocols for Equitable Selection
Implementing justice in research requires deliberate strategies and methodologies at each stage of study design. The following experimental protocols provide a framework for ensuring equitable subject selection and inclusion, aligning with both Belmont's ethical imperatives and the Common Rule's regulatory standards.
Protocol 1: Systematic Recruitment Strategy Design
The objective of this protocol is to create a recruitment plan that proactively ensures the participant pool is representative of the population that stands to benefit from the research, thereby upholding the Belmont principle of justice and complying with Common Rule requirements for equitable selection [18] [20].
- Step 1: Define the Target Population: Clearly delineate the clinical or demographic population that the research aims to benefit. This definition should be based on scientific objectives, not convenience.
- Step 2: Identify and Map Recruitment Sources: List all potential recruitment sources (e.g., clinical sites, community centers, electronic health records, online platforms). Evaluate each source for potential biases that may lead to the systematic exclusion of certain groups.
- Step 3: Develop Inclusive Outreach Materials: Create recruitment advertisements and informed consent documents that are accessible and understandable to diverse populations. The Revised Common Rule specifically requires that the "Key Information" be presented first in the consent form to facilitate a participant's decision-making process [31].
- Step 4: Implement Continuous Monitoring: Track recruitment demographics (e.g., race, gender, age, socioeconomic status) in real-time against the target population benchmarks. This allows for the timely adjustment of strategies if certain groups are underrepresented.
Protocol 2: Vulnerability and Equity Assessment
This protocol aims to systematically identify and address potential vulnerabilities and inequities in subject selection, ensuring that no group is unfairly burdened or excluded without scientific justification.
- Step 1: Conduct a Vulnerability Analysis: Review the proposed inclusion and exclusion criteria to determine if they unnecessarily or unjustly exclude specific groups (e.g., non-English speakers, pregnant women, individuals with comorbidities). Document the scientific rationale for any restrictive criterion.
- Step 2: Plan for Additional Protections: For populations that may be vulnerable due to compromised autonomy (e.g., children, prisoners, individuals with cognitive impairments), implement the specific additional safeguards required by the Common Rule's subparts or IRB policy [20]. This may involve obtaining consent from legally authorized representatives.
- Step 3: Establish a Justice Review within the IRB Submission: Prepare a dedicated section in the IRB application that explicitly addresses the principle of justice. This section should justify the subject selection plan, explain how the benefits and burdens of the research are distributed, and detail the steps taken to prevent the exploitation of vulnerable groups.
- Step 4: Utilize Revised Common Rule Flexibilities: For minimal risk research, leverage the revised exemption categories, such as those for benign behavioral interventions or secondary research on identifiable data, which may allow for broader inclusion while still requiring a "limited IRB review" to protect privacy and confidentiality [31].
Essential Research Reagent Solutions
In the context of ethical research review and conduct, the "reagents" are the procedural tools and documents required to comply with regulatory standards. The following table details these essential components for upholding justice in human subjects research.
Table 3: Key Research Reagent Solutions for Ethical Compliance
| Item | Function in Upholding Justice |
|---|---|
| IRB Protocol Application | Formal document for IRB review; requires detailed justification of subject selection criteria to ensure equity and avoid systematic selection of vulnerable groups [20]. |
| Informed Consent Form (Revised Common Rule Compliant) | Legal and ethical document ensuring participants are voluntarily enrolled after understanding key information presented clearly and concisely first [31]. |
| Recruitment Monitoring Dashboard | A tracking tool (e.g., spreadsheet or software) to monitor enrollment demographics in real-time, allowing researchers to correct biases in recruitment. |
| Single IRB (sIRB) Agreement | For multi-site studies, a formal agreement mandating the use of one IRB to ensure consistent, efficient, and rigorous ethical review across all sites, as required by the Revised Common Rule [47] [31]. |
| Exemption Determination Worksheet | A tool used by the IRB to assess if research qualifies for an exemption, including categories that now require a "limited IRB review" to ensure privacy and confidentiality protections are adequate [48] [31]. |
| Waiver of Consent Justification Template | A structured document to help researchers justify to the IRB why the research cannot practicably be conducted without a waiver of consent and without using identifiable information, a new criterion under the Revised Common Rule [47] [31]. |
Data Presentation: Regulatory Requirements and Updates
The Revised Common Rule introduced specific, measurable changes to the regulatory landscape. The following tables summarize the key quantitative and categorical changes relevant to the just conduct of research.
Table 4: Key Changes in the Revised Common Rule (Effective 2019)
| Change Area | Pre-2018 Requirement | Revised Common Rule (2018 Requirements) |
|---|---|---|
| Informed Consent | No specific requirement to present "key information" first. | Requires a concise presentation of "Key Information" at the beginning of the consent form [31]. |
| Continuing Review | Generally required for all approved studies on an annual basis. | No longer required for some minimal risk studies, including those that have progressed to data analysis [31]. |
| Exempt Categories | Limited categories for exemption. | New categories added (e.g., benign behavioral interventions), with some requiring a "limited IRB review" [31]. |
| Single IRB Review | Not universally mandated for multi-site studies. | Required for federally-funded, multi-site research, improving consistency (compliance date: Jan. 20, 2020) [47] [31]. |
| Consent Waiver for Screening | Not explicitly addressed. | Allows obtaining information for screening/recruiting without consent under specific conditions [31]. |
| Clinical Trial Consent Posting | Not required. | Requires posting one approved consent form for a clinical trial on a public federal website [47]. |
Table 5: Application of Belmont's Ethical Principles to Common Rule Requirements
| Belmont Ethical Principle | Definition | Common Rule Application |
|---|---|---|
| Respect for Persons | Protecting autonomy; treating with courtesy/respect; allowing informed consent [18]. | Informed consent process; requirement for voluntariness, comprehension, and key information [18] [31]. |
| Beneficence | Maximizing benefits; minimizing potential harms; "Do no harm" [18] [11]. | Systematic assessment of risks and benefits by the IRB [18] [20]. |
| Justice | Fair distribution of costs and benefits of research; equitable selection of subjects [18] [11]. | IRB review to ensure equitable selection of subjects; additional protections for vulnerable populations [18] [20]. |
The Revised Common Rule, the common ethical standard for U.S. publicly funded human subjects research, marked the first significant update to these regulations since 1991. The final rule was published on January 19, 2017, with a general compliance date of January 21, 2019 [49] [50] [51]. These revisions were designed to modernize the regulatory framework, reduce administrative burdens for low-risk studies, and enhance protections for research participants. This guide provides a detailed comparison of the key changes, offering researchers, scientists, and drug development professionals a clear understanding of the updated landscape for human subjects research compliance.
Core Ethical Foundations: The Belmont Report and the Common Rule
The ethical principles of the Belmont Report—Respect for Persons, Beneficence, and Justice—form the foundation upon which the Common Rule's regulations are built. The revisions to the Common Rule can be viewed as a modern operationalization of these principles, particularly strengthening the application of Respect for Persons through enhanced informed consent requirements. The following table outlines how key revisions align with these ethical pillars.
Table 1: Alignment of Common Rule Revisions with Belmont Report Principles
| Belmont Report Principle | Operationalized in the Common Rule Through: | Key Changes in the 2019 Revision |
|---|---|---|
| Respect for Persons | Informed Consent Process | • "Key Information" presented first [25] [50] [31]• New required elements for future research use of data/biospecimens [49] [50] [52]• "Reasonable person" standard for information disclosure [50] |
| Beneficence | Risk Assessment & IRB Review | • Elimination of continuing review for many minimal-risk studies [49] [25] [53]• Expansion of exempt research categories [49] [25] [22]• Mandated use of a single IRB for multi-site trials [49] [52] [53] |
| Justice | Equitable Selection of Subjects | • Clarification of activities not considered "research" (e.g., journalism, public health surveillance) [49] [31] |
Comparative Analysis of Key Regulatory Changes
The 2019 revisions introduced substantial modifications across several domains of human research protections. The data below provides a structured comparison of the pre-2018 and post-2018 requirements for major regulatory areas.
Table 2: Detailed Comparison of Pre-2018 vs. 2018 Common Rule Requirements
| Regulatory Area | Pre-2018 Common Rule Requirements | 2018 Revised Common Rule Requirements | Primary Impact |
|---|---|---|---|
| Informed Consent | • Single, often lengthy, narrative document [50]• 8 basic required elements [50] | • Must begin with a "Key Information" section [25] [50] [31]• 9 basic required elements, including disclosure on future use of identifiable data/biospecimens [50] [31]• 3 new additional elements (e.g., commercial profit, return of results, whole genome sequencing) [50] [52] | Enhances participant comprehension and autonomy; increases transparency. |
| Exempt Research Categories | Limited categories; some only allowed for retrospective data review [49] | New/expanded categories [49] [25] [31]:• Category 3: Benign behavioral interventions [49] [25]• Category 4: Allows prospective data review [49]• Categories 7 & 8: For research using broad consent (note: not yet implemented by many institutions [25] [53] [54]) | Reduces administrative burden for lower-risk studies; allows IRB resources to focus on higher-risk research. |
| Continuing Review | Generally required annually for all non-exempt research [52] | Not required for:• Research eligible for expedited review [49] [25] [53]• Research that has progressed to data analysis only or accessing follow-up clinical data [49] [52] [53] | Reduces investigator and IRB workload for ongoing, minimal-risk studies. |
| Single IRB (sIRB) Review | Not routinely required for multi-site studies. | Mandatory for most federally funded multi-site research located in the U.S. as of January 20, 2020 [49] [52] [53]. | Aims to streamline IRB review process and avoid duplication of effort across sites. |
| Definition of "Research" | Broader interpretation. | Specific exclusions for:• Scholarly & journalistic activities (e.g., oral history, journalism) [49] [31]• Public health surveillance [31] [52] | Clarifies boundaries, exempting certain low-risk activities from formal IRB review. |
Visual Workflow: Navigating the Revised Common Rule
The diagram below outlines the decision-making pathway for implementing the key changes of the Revised Common Rule, based on guidance from multiple institutions.
Institutional Implementation and Compliance Protocols
While the Revised Common Rule sets federal standards, individual institutions have developed specific protocols for implementation. A notable trend among several research universities is the decision to not implement the new "broad consent" option at this time, which is a prerequisite for using new exemption categories 7 and 8 [25] [53] [54]. Institutions like Belmont, UW-Madison, and the University of Hawaii have cited the added regulatory burden and lack of clear federal guidance as reasons for this policy [25] [52] [54].
Visual Guide: Transitioning Existing Studies to the Revised Common Rule
For studies initially approved before January 21, 2019, the transition process to the new rules is not automatic. The following diagram illustrates the pathway for transitioning an existing study, based on institutional policies.
Successfully navigating the Revised Common Rule requires leveraging specific administrative and documentation tools. The following table details essential "reagent solutions" for researchers.
Table 3: Essential Research Reagents for Revised Common Rule Compliance
| Tool/Resource | Function in Compliance Process | Application Example/Notes |
|---|---|---|
| Revised Informed Consent Template | Provides the structure mandated by the new rules, including the key information section and new required elements [48] [50] [52]. | Institutional templates (e.g., from JHM IRB, Ochsner Clinic) include language for future use of data/biospecimens and commercial profit [48] [50]. |
| Exemption Determination Worksheet | Standardized form to assist researchers and IRBs in assessing whether a study qualifies for one of the new exempt categories [48] [54]. | Streamlines the submission process and ensures all criteria for exemption are properly evaluated [54]. |
| Limited IRB Review Protocol | A targeted review process for certain exempt categories to ensure adequate provisions for protecting privacy and maintaining confidentiality are in place [25] [31]. | Applies to exempt categories where identifiable, sensitive information is recorded [49] [25]. |
| Single IRB (sIRB) Agreement Platform | Facilitates the mandatory use of a single IRB for multi-site federally funded research [52] [53]. | Systems like SmartIRB help standardize and track IRB review agreements between collaborating institutions [52]. |
| ClinicalTrials.gov / Regulations.gov | Publicly available federal websites where one IRB-approved consent form for a clinical trial must be posted after the trial is closed to recruitment [49] [52]. | Fulfills the new transparency requirement under §46.116(h) for clinical trials [49] [52]. |
The Revised Common Rule represents a significant evolution in the framework governing human subjects research. Key changes—such as the streamlined continuing review, expanded exemptions, and more robust informed consent requirements—are designed to better calibrate regulatory oversight to the level of study risk. For the research community, mastering these updates is not merely about regulatory compliance; it is about upholding the core ethical principles of the Belmont Report in a contemporary research environment. Researchers must work closely with their local Institutional Review Boards to understand institution-specific implementations and ensure their protocols align with both the federal mandates and the ethical commitment to protecting human subjects.
Navigating Modern Challenges: Updates, Exemptions, and Informed Consent in the Revised Common Rule
The Institutional Review Board (IRB) review process represents a critical checkpoint in human subjects research, ensuring ethical conduct while potentially creating administrative hurdles. The 2017 revisions to the Federal Policy for the Protection of Human Subjects, known as the Common Rule, significantly transformed this landscape by expanding and clarifying exemption categories. These changes aim to streamline IRB review for minimal-risk research, allowing boards to focus resources on higher-risk studies while maintaining ethical protections grounded in the Belmont Report's principles of respect for persons, beneficence, and justice [8] [55]. This guide examines the current exemption categories, their operationalization across research institutions, and excluded research types, providing researchers with essential knowledge for protocol development and submission.
Historical and Regulatory Context
The current regulatory framework for human subjects protection emerged from a history of ethical violations. The Belmont Report, published in 1979, established three core ethical principles following revelations about studies like the Tuskegee Syphilis Study [55]. These principles—respect for persons (embodied in informed consent), beneficence (requiring risk-benefit assessment), and justice (ensuring equitable subject selection)—directly informed the Common Rule regulations [56].
The 2017 Common Rule revisions marked the first major update in over twenty-five years, reflecting dramatic changes in research environments including digital records, genomic data, and mobile technologies [55]. These revisions refined exemption categories to better align with contemporary research methodologies while maintaining ethical safeguards.
Comprehensive Analysis of Exempt Research Categories
The Common Rule specifies eight categories of research that may be exempt from ongoing IRB oversight, though institutions typically require an initial exemption determination [57] [58]. These exemptions apply only to minimal-risk research and maintain ethical requirements consistent with the Belmont framework.
Table 1: Exemption Categories Under the Revised Common Rule
| Category Number | Description | Key Limitations & Requirements |
|---|---|---|
| 1 | Research in established educational settings involving normal educational practices | Must not adversely impact students' learning or educator assessment [57] |
| 2 | Research involving educational tests, surveys, interviews, or observation of public behavior | (i) Information recorded anonymously; OR (ii) Disclosure would not create risk; OR (iii) Identifiable with limited IRB review [57] [59] |
| 3 | Research involving benign behavioral interventions with adult subjects | Intervention must be brief, harmless, painless, non-invasive; prospective agreement required [57] [60] |
| 4 | Secondary research using identifiable private information or biospecimens | Specific conditions include: public availability, de-identified recording, or designated government research [57] |
| 5 | Research and demonstration projects examining public benefit/service programs | Must be conducted/supported by federal agency; published on list prior to commencement [57] |
| 6 | Taste and food quality evaluation and consumer acceptance studies | Must use wholesome foods without additives or safe levels of ingredients/contaminants [57] |
| 7 | Storage/maintenance of identifiable private information/biospecimens for secondary research | Requires broad consent and limited IRB review [57] |
| 8 | Secondary research using identifiable private information/biospecimens | Requires broad consent, documentation, limited IRB review, and within scope of consent [57] |
Exemption Workflow and Determination Process
The following diagram illustrates the exemption determination process implemented at most research institutions:
Operationalizing Exemptions: Institutional Variations
Research institutions have implemented the Common Rule exemptions with variations reflecting local policy choices:
- Category Limitations: Some institutions, including the University of North Carolina at Chapel Hill and Georgia Southern University, have chosen not to implement exemption categories 7 and 8 (broad consent provisions) [61] [59].
- Flexible Additions: Georgia Tech introduced "FLEX 2" and "FLEX 3" categories allowing minor participants who are enrolled students in specific non-federally regulated research [62].
- Process Harmonization: Organizations like WCG are merging exempt determinations and IRB review into single processes to improve client experience [63].
Excluded Categories and Special Limitations
Certain research types and populations face restrictions under exemption categories:
Table 2: Excluded Categories and Special Limitations
| Research Type/Population | Exemption Limitations | Regulatory Reference |
|---|---|---|
| Prisoners | Exemptions do not apply except for research aimed at broader populations that only incidentally include prisoners | 45 CFR 46.104(b)(2) [57] [58] |
| Children | Exemption 3 does not apply; Exemption 2(iii) does not apply; Exemption 2(i) and (ii) limited to educational tests or observation without investigator participation | 45 CFR 46.104(b)(3) [57] [61] |
| FDA-Regulated Research | Exemptions other than Category 6 (taste and food studies) do not apply to FDA-regulated research | Institutional policies [61] [58] |
Experimental Protocols and Methodologies
Exemplar Protocol: Educational Intervention Study (Category 1)
Research Design: Randomized comparison of two instructional techniques in established classroom settings.
Methodology:
- Participant Recruitment: Classroom-level randomization with entire classes assigned to intervention or control condition
- Intervention: Implementation of novel instructional technique for one semester
- Data Collection: Standardized educational tests administered pre- and post-intervention; classroom observation using validated instruments
- Data Analysis: Comparison of test score improvements between groups; qualitative analysis of observational data
Compliance Considerations: Normal educational practices must not adversely impact students' opportunity to learn required content [57].
Exemplar Protocol: Benign Behavioral Intervention (Category 3)
Research Design: Investigation of cognitive performance under various noise conditions.
Methodology:
- Participant Screening: Adult subjects only; prospective agreement to intervention and data collection
- Intervention: Subjects solve standardized puzzles under controlled noise conditions (silence, white noise, office sounds)
- Data Collection: Accuracy and completion time recorded; post-task subjective experience survey
- Debriefing: Full explanation of study purpose and conditions
Compliance Considerations: Intervention must be brief, harmless, painless, not physically invasive, and unlikely to cause significant adverse lasting impact or embarrassment [57] [60].
The Researcher's Toolkit: Essential Documentation for Exemption Submissions
Table 3: Required Documentation for Exemption Determinations
| Document Type | Function & Purpose | Institutional Examples |
|---|---|---|
| Complete IRB Application | Provides study overview, procedures, and methodology | UNC-Chapel Hill requires Request Exemption section of IRBIS application [61] |
| Recruitment Materials | Allows review of voluntariness and appropriateness of subject selection | All recruitment scripts, flyers, and advertisements [61] |
| Informed Consent/Information Sheet | Demonstrates respect for persons through voluntary participation disclosure | Northwestern requires consent information even for exempt research [58] |
| Data Collection Instruments | Permits assessment of risks related to content and identifiability | All surveys, questionnaires, tests, and interview guides [61] |
| Letters of Cooperation | Documents permission from non-affiliated research sites | Required when research occurs at external institutions [59] |
| Human Research Protection Training Certificates | Verifies investigator knowledge of ethical principles and regulations | Current training documentation for all research team members [61] |
Comparative Analysis: Pre- and Post-Revision Common Rule
The 2017 Common Rule revisions introduced significant changes to exemption categories:
- Expanded Categories: New exemptions for benign behavioral interventions (Category 3) and secondary research with broad consent (Categories 7-8)
- Clarified Provisions: More precise definitions of educational settings, secondary research, and minimal risk
- Limited IRB Review: New requirement for certain exempt categories involving identifiable, potentially sensitive information [57] [55]
These changes reflect regulators' efforts to balance ethical oversight with reduced administrative burden for minimal-risk research, acknowledging the evolution of research methodologies since the original Common Rule implementation.
The revised Common Rule exemption categories represent a significant streamlining of IRB review for minimal-risk research while maintaining the ethical foundations established by the Belmont Report. Understanding these categories—their applications, limitations, and institutional variations—empowers researchers to design appropriate studies and navigate submission processes efficiently. As regulatory evolution continues, with emerging topics like digital health technologies and decentralized clinical trials presenting new challenges [56], researchers must stay informed about both current requirements and forthcoming changes to optimize their protocol development and submission strategies.
The landscape of multi-site clinical trials is undergoing a significant transformation with the implementation of the single Institutional Review Board (sIRB) mandate. This regulatory shift represents a fundamental change in how cooperative research is overseen, moving from a decentralized model of multiple local IRB reviews to a centralized system where one designated IRB provides ethical review for all participating sites. The mandate finds its ethical foundation in the Belmont Report's principles of respect for persons, beneficence, and justice, while operating within the regulatory framework of the Common Rule requirements [23] [21].
The primary rationale for this change is to address systemic inefficiencies in the ethical review process for multi-site studies. Under traditional systems, the same protocol would undergo sequential reviews by multiple local IRBs, creating significant delays, inconsistent feedback, and administrative burdens that hampered research progress without necessarily enhancing human subject protections [64] [21]. By implementing a centralized review model, regulators aim to eliminate redundant reviews while maintaining rigorous ethical oversight, ultimately accelerating the translation of research discoveries into patient benefits [64].
This comparison guide examines the implementation status, operational challenges, and practical solutions associated with the sIRB mandate, providing researchers, scientists, and drug development professionals with evidence-based insights for navigating this transformed landscape.
Regulatory Framework: Tracing the sIRB Mandate from Belmont to Implementation
Ethical Foundations and Regulatory Evolution
The sIRB mandate represents the convergence of ethical principles and regulatory pragmatism. The Belmont Report's ethical framework established the foundational principles governing human subjects research, emphasizing respect for persons (through informed consent), beneficence (through risk-benefit assessment), and justice (through fair subject selection) [23] [21]. These principles were subsequently codified into regulations through the Common Rule (45 CFR 46), which has governed federally funded human subjects research since 1991 [23].
The evolution toward mandatory sIRB use began with the NIH Policy on Single IRB for multi-site research, effective January 2018, which required all domestic sites of NIH-funded studies to use a single IRB [65] [66]. This was followed by the Revised Common Rule (2018), which extended the sIRB requirement to all federally funded cooperative research [23] [66]. Most recently, the FDA has finalized its own sIRB requirement for multi-site clinical trials, with an expected implementation date of May 2025 [64] [67].
Table: Chronological Development of sIRB Policies and Mandates
| Year | Policy/Milestone | Governing Agency | Key Requirement |
|---|---|---|---|
| 1979 | Belmont Report | National Commission | Established ethical foundations for human subjects protection |
| 1991 | Common Rule | 15 Federal Departments | Standardized human subjects regulations across agencies |
| 2018 | NIH sIRB Policy | National Institutes of Health | Required sIRB for all domestic sites of NIH-funded multi-site studies |
| 2020 | Revised Common Rule | HHS | Extended sIRB requirement to all federally funded cooperative research |
| 2025 (Expected) | Final Rule Implementation | Food and Drug Administration | Mandates sIRB for multi-site clinical trials regulated by FDA |
Scope and Exceptions to the sIRB Requirement
The sIRB mandate applies broadly to multi-site studies conducted at domestic institutions, but contains important exceptions. According to current regulations, exemptions may be granted for:
- Research involving international sites [64] [65]
- Studies with tribal nations where review by a single IRB is prohibited by tribal law [64] [65]
- Research contexts where a federal department or agency determines and documents that sIRB review would not be appropriate [65]
- Specific circumstances such as studies conducted at VA facilities [65]
The exception process requires strong justification explaining why sIRB use would not be feasible or beneficial for a particular study context. However, exceptions are granted infrequently, and most researchers should prepare to comply with sIRB requirements as part of their study design [64].
Comparative Analysis: Traditional Multi-IRB vs. Single IRB Models
Efficiency Metrics and Performance Outcomes
Evidence from early implementation of sIRB policies reveals significant differences in performance between traditional multi-IRB and single IRB models. The centralized approach demonstrates advantages in several key operational areas while introducing new challenges that require management.
Table: Comparative Performance Metrics Between Traditional Multi-IRB and Single IRB Models
| Performance Indicator | Traditional Multi-IRB Model | Single IRB Model | Supporting Evidence |
|---|---|---|---|
| Approval Timeline | Sequential reviews causing 3-6 month delays | Parallel process reducing time to approval by 30-50% | [64] |
| Protocol Consistency | Multiple interpretations causing protocol variations | Uniform application of ethical standards | [64] |
| Administrative Burden | High (duplicative submissions at each site) | Moderate (centralized submission with local context review) | [68] |
| Communication Pathway | Direct site-IRB communication | Coordinated through lead study team | [68] |
| Regulatory Harmony | Variable standards across institutions | Consistent ethical framework application | [64] |
| Resource Requirements | Distributed across institutions | Concentrated at reviewing IRB with local administrative requirements | [65] [68] |
Implementation Challenges and Barrier Analysis
Despite the theoretical efficiencies, practical implementation of the sIRB model has faced significant challenges. A 2022 workshop examining sIRB implementation identified several persistent barriers [68]:
New Responsibilities for Study Teams: Research teams often lack the resources and training to manage coordination between reviewing IRBs and relying sites, leading to communication breakdowns and implementation delays [68].
Persistent Duplicative Processes: Many relying institutions continue to require comprehensive internal reviews that essentially duplicate sIRB functions, undermining potential efficiency gains [68] [69].
Harmonization Challenges: Differences in IRB processes, policies, and technology systems create friction in the reliance process, increasing administrative complexity [68].
Local Context Limitations: Reviewing IRBs may lack familiarity with local institutional policies, state laws, or community standards at relying sites, creating potential gaps in protection [68].
These implementation challenges highlight the distinction between theoretical policy objectives and practical operational realities in the transition to centralized ethical review.
Operational Protocols: Methodologies for Successful sIRB Implementation
IRB Reliance Workflow and Authorization Processes
Successful sIRB implementation requires meticulous planning and execution of standardized reliance procedures. The following workflow visualization illustrates the primary pathways for establishing IRB reliance arrangements:
Diagram 1: sIRB Reliance Agreement Workflow illustrating the primary pathways for establishing IRB reliance arrangements for multi-site studies.
The operational implementation of sIRB review requires careful execution of the following methodological protocol:
Pre-Submission Planning (8-12 weeks before grant submission): Investigators must identify the need for sIRB review during study conceptualization, then contact their institutional IRB office to discuss potential reviewing IRB options and obtain commitment letters for grant applications [65].
IRB Selection Criteria: The reviewing IRB should be selected based on specific study requirements, including the entity holding the IND/IDE, the number and location of participating sites, and the IRB's expertise with the research domain [65].
Reliance Agreement Execution: Institutions must formalize their relationship through IRB Authorization Agreements, which may utilize established frameworks like the SMART IRB Agreement or institution-specific contracts [66].
Budgeting and Resource Allocation: Researchers must include sIRB costs in grant applications, with fee structures typically based on either hourly rates (e.g., $62.66/hour for academic IRBs) or fixed fees (e.g., $3,750 for industry-sponsored studies when IRBMED serves as reviewing IRB) [65].
Communication and Coordination Protocol
Effective communication represents a critical success factor in sIRB implementation. The complex relationship between reviewing IRBs, relying institutions, and study teams requires a structured communication framework:
Diagram 2: sIRB Communication Protocol mapping the primary communication pathways and content exchanges between stakeholders in the sIRB model.
The communication protocol requires specific methodological rigor:
Lead PI Coordination Methodology: The lead research team must establish standardized systems for collecting and distributing regulatory documents, tracking site-specific progress, and maintaining communication logs between all parties [68].
Local Context Information Transfer: Relying sites must systematically identify and communicate local considerations to the reviewing IRB, including institutional policies, state-specific legal requirements, and community cultural norms [68] [69].
Issue Escalation Framework: All parties should establish clear pathways for elevating concerns, with defined timelines for response and resolution of regulatory or ethical questions that arise during study conduct.
Essential Research Reagent Solutions for sIRB Implementation
Successful navigation of the sIRB landscape requires access to specialized tools and resources that facilitate the reliance process. The following reagent solutions represent critical components for efficient sIRB implementation:
Table: Essential Research Reagent Solutions for sIRB Implementation
| Reagent Solution | Primary Function | Application Context | Implementation Example |
|---|---|---|---|
| SMART IRB Platform | Master reliance agreement streamlining IRB authorization | Multi-site studies across academic institutions | National implementation with 1,080+ signatory institutions [68] |
| IRB Reliance Exchange (IREx) | Online system for documenting and managing reliance agreements | Tracking ceded review arrangements between institutions | Digital execution of reliance without signatory official involvement [66] |
| Central IRB Partnerships | Pre-negotiated master service agreements with commercial IRBs | Industry-sponsored clinical trials | Stanford's agreements with Advarra, WIRB, and other central IRBs [66] |
| Local Context Assessment Tools | Structured frameworks for identifying site-specific considerations | Ensuring reviewing IRB understands local requirements | Systematic collection of institutional policies, state laws, and resource availability [68] |
| sIRB Budgeting Templates | Standardized cost estimation tools for grant applications | Accurate projection of sIRB-related expenses | IRBMED's fee structure of $62.66/hour for review services [65] |
The implementation of the sIRB mandate represents a significant evolution in the oversight of multi-site research, offering both efficiency opportunities and implementation challenges. As the May 2025 FDA compliance date approaches, research institutions, sponsors, and investigators must proactively develop the infrastructure and expertise necessary for successful adoption [64] [67].
The future of sIRB implementation will likely focus on addressing current friction points through enhanced harmonization of institutional policies, development of more integrated technology solutions, and refinement of communication pathways between all stakeholders [68] [70]. Additionally, as noted in recent analyses, regulatory agencies are expected to increase their focus on vulnerable populations, potentially requiring specialized sIRB expertise for studies involving these groups [70].
For the research community, successful adaptation to the sIRB mandate will require both cultural and operational shifts. Institutions must balance their legitimate interests in maintaining oversight of research conducted at their sites with the regulatory imperative to reduce redundant ethical review. By embracing the ethical foundations of the Belmont Report while implementing the practical requirements of the Common Rule, the research community can achieve the dual goals of enhanced efficiency and robust human subject protection that underpin the sIRB mandate.
The process of informed consent represents a fundamental pillar of ethical clinical research, embodying the core principle of respect for persons enshrined in the Belmont Report [8]. For decades, this 1979 document has provided the ethical foundation for human subjects research in the United States, establishing three primary principles: respect for persons, beneficence, and justice [8] [21]. These principles were subsequently operationalized into federal regulations through the Common Rule (Federal Policy for the Protection of Human Subjects), first established in 1991 and significantly revised in 2017 with a compliance date of January 2019 [50] [25]. The 2017 revisions marked the first major overhaul of these regulations in over 25 years, aiming to reduce administrative burdens for low-risk research while enhancing protections for human subjects enrolled in greater-than-minimal-risk trials [50].
The recent revisions to the Common Rule specifically target the informed consent process, addressing a well-documented problem: traditional consent forms had become excessively lengthy and complex, often exceeding the reading comprehension of many potential subjects [50]. A 2009 review of the literature found that fewer than one-third of research subjects adequately understood important aspects of their studies, including study goals, risks and benefits, and randomization procedures [50]. The modernized regulations seek to bridge this comprehension gap through two key requirements: mandating that consent begins with a concise key information section and presenting all information in a manner that facilitates understanding [50] [71]. These changes represent a significant shift from viewing consent as a mere signature on a form to conceptualizing it as an ongoing process of communication and comprehension assessment between researchers and potential subjects.
Comparative Analysis: Belmont Report Ethical Foundations vs. Common Rule Implementation
Theoretical Framework vs. Regulatory Requirements
The Belmont Report and the Common Rule represent complementary yet distinct aspects of human research protections. The Belmont Report establishes the ethical framework through its three core principles, while the Common Rule translates these principles into specific regulatory requirements that investigators and institutions must follow [8] [21]. The relationship between these documents is foundational to understanding the modernization of informed consent requirements.
The following table compares the key ethical principles from the Belmont Report with their corresponding regulatory manifestations in the revised Common Rule:
Table 1: Comparison of Belmont Report Ethical Principles and Common Rule Implementation
| Belmont Report Ethical Principle | Description | Common Rule Implementation |
|---|---|---|
| Respect for Persons | Recognition of personal autonomy and protection for individuals with diminished autonomy | Informed consent requirements including new "key information" section and presentation to facilitate understanding [50] [8] |
| Beneficence | Obligation to maximize possible benefits and minimize possible harms | Assessment of research risks and benefits; requirement to provide information a "reasonable person" would want [50] [8] |
| Justice | Fair distribution of research burdens and benefits | Equitable selection of research subjects; transparency about future research uses [8] |
The Comprehension Gap: Identifying the Problem
The revisions to the Common Rule's consent requirements directly address documented deficiencies in research subject comprehension. Evidence indicates that nearly half of American adults read at or below the eighth-grade level, while many consent documents are written at significantly higher reading levels [50]. This discrepancy creates a substantial barrier to genuine informed consent. The revised regulations aim to address this through several mechanisms that collectively enhance the consent process's effectiveness as a tool for genuine understanding rather than mere regulatory compliance.
Key Changes in the Revised Common Rule: The "Key Information" Mandate
Structural Reforms to the Consent Process
The revised Common Rule introduced several structural changes to the informed consent process, with two new general requirements fundamentally altering how consent information must be presented:
"Reasonable Person" Standard: Informed consent must now include "information that a reasonable person would want to have to make an informed decision about whether to participate, and an opportunity to discuss that information" [50]. This standard shifts the focus from what investigators believe is important to what potential subjects actually need for decision-making.
Key Information Presentation: Informed consent must "begin with a concise and focused presentation of the key information that is most likely to assist a prospective subject or legally authorized representative in understanding the reasons why one might or might not want to participate in the research" [50]. This requirement directly addresses the problem of lengthy, complex consent forms by forcing prioritization of the most crucial information.
The key information section should include several core elements: a clear statement that participation is voluntary, the purpose of the research, a description of study procedures, the expected duration of participation, the reasonably foreseeable risks and potential benefits, and appropriate alternatives to participation [50]. This structural reorganization aims to ensure that potential subjects encounter the most decision-critical information first, when their attention is most focused.
New Consent Form Elements: Enhanced Transparency Requirements
Beyond structural changes to the consent process, the revised Common Rule introduced four new specific elements for consent forms—one required basic element and three additional elements to be included when applicable.
Table 2: New Consent Form Elements in the Revised Common Rule
| Element Type | When Required | Content Requirements |
|---|---|---|
| Required Basic Element | Research involves collection of identifiable private information or identifiable biospecimens | A statement indicating whether identifiers may be removed and if the deidentified information/biospecimens may be used for future research [50] |
| Additional Element | Use of biospecimens in the research | A statement on whether biospecimens may be used for commercial profit and whether the subject will share in profits [50] |
| Additional Element | Research yields clinically relevant results | A statement on whether clinical results will be returned to subjects and under what conditions [50] |
| Additional Element | Research involves whole genome sequencing | A statement that the research will/will not/might involve whole genome sequencing [50] |
These new elements enhance transparency in areas that have historically generated ethical concerns. The requirement regarding identifiable information and biospecimens addresses issues highlighted by cases like that of Henrietta Lacks, whose cells were used to create an immortal cell line without her knowledge or consent, and the Havasupai Tribe case, where DNA samples collected for one research purpose were subsequently used for other studies without permission [50]. By explicitly stating whether and how deidentified data and specimens may be used in future research, the regulations empower potential subjects to make more fully informed decisions about participation.
Experimental and Implementation Protocols: Assessing Comprehension
Methodologies for Evaluating Consent Understanding
Research into consent comprehension has employed various methodological approaches to assess and improve understanding. These methodologies provide the evidence base supporting the regulatory changes and offer models for implementing the new requirements effectively.
Readability Assessment Protocols: Multiple studies have employed standardized readability metrics (e.g., Flesch-Kincaid, SMOG) to evaluate consent forms against the recommended eighth-grade reading level. The implementation protocol involves: (1) conducting baseline readability assessments of existing consent forms; (2) revising language to reduce complexity and passive voice; (3) validating revisions through additional readability testing; and (4) incorporating plain language principles throughout [50].
Comprehension Evaluation Frameworks: Researchers have developed structured assessment tools to measure subject understanding following consent discussions. The typical methodology includes: (1) developing a standardized questionnaire covering key study aspects (purpose, procedures, risks, benefits, alternatives, rights); (2) administering the questionnaire after the consent discussion but before enrollment; (3) quantifying comprehension scores across different knowledge domains; and (4) providing additional education on poorly understood elements before proceeding with enrollment [50].
Comparative Consent Studies: Some investigations have employed randomized designs comparing traditional consent forms with revised versions incorporating the key information mandate. The experimental protocol generally involves: (1) creating two versions of consent documents for the same study; (2) randomizing potential subjects to receive either the standard or revised format; (3) assessing comprehension, decision-making confidence, and satisfaction with the consent process; and (4) analyzing differences in outcomes between the two formats [50].
Implementation Framework for the Key Information Requirement
The following diagram illustrates the workflow for developing and implementing a compliant key information section in informed consent forms, based on FDA guidance and institutional implementation protocols:
Research Reagents and Tools for Consent Comprehension Research
Table 3: Essential Methodological Tools for Consent Comprehension Research
| Tool/Reagent | Primary Function | Research Application |
|---|---|---|
| Readability Assessment Software | Quantifies reading level required to understand text | Evaluating consent form complexity against the 8th-grade reading level benchmark [50] |
| Structured Comprehension Assessments | Standardized questionnaires measuring understanding of key study elements | Objectively measuring subject comprehension during consent process evaluation [50] |
| Plain Language Thesauruses | Provides alternative wording for complex medical and technical terms | Simplifying consent form language while maintaining accuracy [50] |
| Institutional Consent Templates | Pre-formatted documents incorporating regulatory requirements | Ensuring compliance with Common Rule elements across studies [50] [72] |
Comparative Effectiveness: Pre- and Post-Revision Consent Outcomes
Quantitative Metrics for Consent Process Evaluation
The effectiveness of the revised consent requirements can be evaluated through specific metrics comparing pre- and post-implementation outcomes. While comprehensive systematic reviews of the revised Common Rule's impact are still emerging, preliminary data and evidence from similar interventions provide insight into potential effects.
Table 4: Comparative Metrics for Consent Process Effectiveness
| Evaluation Metric | Pre-Revision Baseline | Post-Revision Outcomes | Measurement Method |
|---|---|---|---|
| Consent Form Length | Often 15-20+ pages | Reduced through key information section | Page count and word count analysis |
| Reading Grade Level | Frequently 10th grade or higher | Target of 8th grade or lower | Readability software assessment |
| Subject Comprehension | <33% understood key elements | Preliminary data shows improvement | Structured comprehension tests |
| Decision-Making Confidence | Variable, often lower in complex studies | Higher with improved presentation | Subject self-report scales |
| Discussion Time | Often limited due to form complexity | More focused on key elements | Time tracking during consent process |
Implementation Challenges and Institutional Adaptation
The transition to revised Common Rule requirements has presented implementation challenges that researchers and institutions have addressed through various adaptive strategies:
Templated Consent Documents: Many institutions, including Cornell University and Ochsner Clinic Foundation, have developed standardized consent templates that incorporate the new key information section and required elements [50] [72]. These templates provide a structured framework that ensures regulatory compliance while allowing study-specific customization.
IRB Procedures and Review: Institutional Review Boards have modified their review procedures to specifically assess the key information presentation and compliance with new consent elements [25]. Some institutions, like Belmont University, have implemented selective application of certain exemption categories while opting not to implement the broad consent provisions for secondary research uses at this time [25].
Researcher Training and Education: Comprehensive education programs have been developed to train investigators and research staff on the revised requirements, particularly focusing on how to effectively develop the key information section and facilitate understanding during consent discussions [50].
The modernization of informed consent through the revised Common Rule's key information and comprehension requirements represents a significant advancement in human subjects protections. By addressing the documented shortcomings of traditional consent processes—particularly their complexity and inadequate facilitation of genuine understanding—these changes strengthen the implementation of the Belmont Report's ethical principles, especially respect for persons [50] [8]. The requirement to present key information concisely and facilitate comprehension shifts the consent process from a regulatory hurdle to a meaningful exchange that truly honors participant autonomy.
While implementation challenges remain and further research is needed to fully evaluate the impact of these changes, early evidence suggests that the revised approach better supports potential subjects in making informed decisions about research participation. The increased transparency regarding future research uses of data and biospecimens addresses historical ethical concerns and builds trust between the research community and the public [50]. As these practices evolve, continued refinement of consent processes, coupled with empirical research on their effectiveness, will further enhance the ethical conduct of human subjects research while facilitating valuable scientific inquiry.
The management of biospecimens and associated data for secondary research sits at the intersection of pioneering scientific inquiry and foundational ethical principles. This landscape is primarily governed by two cornerstone frameworks: the Belmont Report, which outlines broad ethical principles, and the Common Rule (45 CFR Part 46), which translates these principles into specific regulatory requirements for federally funded human subjects research [73] [14]. The 2019 revisions to the Common Rule introduced "broad consent" as a new, flexible mechanism specifically for the storage, maintenance, and secondary research use of identifiable private information and identifiable biospecimens [74]. This guide provides a comparative analysis of consent pathways, enabling researchers, scientists, and drug development professionals to navigate these requirements effectively while ensuring the ethical integrity of their work.
Comparative Analysis of Consent Pathways for Secondary Research
Researchers have several pathways for legally and ethically using data and biospecimens for secondary research. The table below objectively compares the operational requirements, advantages, and limitations of the three primary approaches.
Table: Comparison of Consent Pathways for Secondary Research Use of Identifiable Information and Biospecimens
| Feature | Study-Specific Consent | Broad Consent | IRB Waiver of Consent |
|---|---|---|---|
| Definition | Consent obtained for a specific, well-defined research study [74]. | Consent for the storage, maintenance, and secondary research use of identifiable private information or biospecimens for future, unspecified research studies [74] [75]. | An IRB-approved exception to the requirement for informed consent under specific regulatory criteria [74]. |
| Regulatory Basis | 45 CFR §46.116 (Common Rule) [74] [73]. | 45 CFR §46.116(d) (Revised Common Rule) [74]. | 45 CFR §46.116(f) (Common Rule) [74] [17]. |
| Ideal Use Case | Prospective studies where all research procedures and aims are known at the outset. | Creating biorepositories or data repositories for future research in a specific domain (e.g., cancer genomics) [17]. | Minimal-risk research where obtaining consent is impracticable and the research could not proceed without a waiver [74] [17]. |
| Key Advantages | - Provides participants with the most specific information.- Highest level of transparency for a single study. | - Provides flexibility for future research without re-consent.- Respects participant autonomy more than a waiver.- Streamlines the launch of new secondary studies. | - Enables research where re-contacting participants is impossible or impracticable.- Essential for certain types of records-based research. |
| Key Limitations | - Inflexible; new consent required for any unanticipated research.- Impractical for large-scale, long-term biobanks. | - Requires sophisticated tracking systems for consent status [75].- Participants agree to future research they cannot fully preview. | - Cannot be used if the research involves an intervention.- Cannot be used if the research could practicably be carried out with de-identified materials [17]. |
Experimental Protocols and Data Analysis in Regulatory Adherence
Evaluating the effectiveness of different consent models involves methodologies akin to experimental research in the social and ethical domains.
Protocol for Consent Comprehension Studies
Objective: To quantitatively assess and compare participant understanding and retention of key study concepts across different consent models (e.g., traditional vs. broad consent with a key information section).
Methodology:
- Cohort Formation: Recruit a diverse participant pool and randomize them into groups receiving consent forms formatted differently.
- Intervention: One group receives a consent form with a "Key Information" section at the beginning, as required by the revised Common Rule [73]. The control group receives a standard consent form without this focused presentation.
- Data Collection: Administer a standardized questionnaire immediately after the consent process and again after a pre-determined period (e.g., 72 hours). The questionnaire tests comprehension of critical elements: the research purpose, voluntary participation, risks, and the handling of biospecimens and data [74] [73].
- Analysis: Compare comprehension scores and retention rates between the groups using statistical tests (e.g., t-tests) to determine the efficacy of the "Key Information" format in improving participant understanding.
Hypothetical data from a survey of IRB members and investigators illustrates the variability in opinions regarding what risks should be highlighted in a "Key Information" section [73]. This data underscores the challenge of standardizing broad consent forms.
Table: Survey Results on Risks for Inclusion in Consent Form Key Information Section
| Perceived Risk | Percentage of Respondents Advocating for Inclusion in Key Information Section |
|---|---|
| Physical harm from biospecimen collection | 95% |
| Loss of privacy or confidentiality | 92% |
| Potential for genetic information disclosure | 88% |
| Commercial profit from biospecimens | 75% |
| Psychological distress from results | 72% |
| Use of data for future unspecified research | 65% |
Logical Workflow for Ethical Biospecimen Research
The following diagram maps the logical decision pathway a researcher must follow to determine the appropriate regulatory and consent approach for a study involving biospecimens or data, based on the Common Rule.
Decision Workflow for Biospecimen Research Compliance
Navigating the regulatory landscape for biospecimen research requires leveraging specific resources and tools. The following table details key "research reagent solutions" for ethical and compliant study design.
Table: Essential Tools for Managing Ethical Biospecimen and Data Research
| Tool / Resource | Primary Function | Relevance to Researchers |
|---|---|---|
| Institutional Review Board (IRB) | Independent ethics committee that reviews and approves research protocols [73]. | Mandatory for Common Rule compliance. Provides guidance on selecting the correct consent path (waiver, broad, study-specific) and approves consent forms. |
| Informed Consent Templates | Pre-formatted documents containing all required and potential elements of consent [73]. | Ensure regulatory compliance (e.g., key information section, statements on commercial profit, whole genome sequencing). Save time and reduce administrative error [73]. |
| Biobank Management Software | Systems for tracking biospecimens, associated data, and donor consent status [75]. | Critical for implementing broad consent, as it requires sophisticated tracking of what participants have consented to regarding future use [75]. |
| HIPAA Privacy Rule Expertise | Regulations (45 CFR 160 & 164) governing the use of Protected Health Information (PHI) by covered entities [76] [17]. | Essential for research using data from healthcare providers. Determines when authorization is needed or when data can be used as a "limited data set" or de-identified [17]. |
| Certificate of Confidentiality | Issued by NIH to protect the privacy of research subjects by withholding identifiable information from civil, criminal, or other legal demands [17]. | Protects sensitive participant data (e.g., genetic, behavioral) from forced disclosure, strengthening the confidentiality assurances in consent forms. |
The choice between study-specific consent, broad consent, and an IRB waiver is not merely a regulatory checkbox but a critical ethical decision with direct implications for research validity, participant trust, and operational feasibility. Broad consent, as introduced in the revised Common Rule, offers a powerful tool for advancing biobanking and large-scale data initiatives, but it demands robust infrastructure and clear communication to participants. As genomic and data-driven research continues to evolve, the principles of the Belmont Report—Respect for Persons, Beneficence, and Justice—remain the foundational compass. By rigorously applying these principles through the structured pathways of the Common Rule, the research community can ensure that scientific progress is built upon a steadfast commitment to ethical integrity.
The evolution of human subjects research oversight represents a continuous effort to balance rigorous ethical standards with administrative efficiency. The Belmont Report, published in 1979, established the three foundational ethical principles of "Respect for Persons," "Beneficence," and "Justice" that underpin all U.S. human research protections [8]. These principles were subsequently codified into federal regulations through the Common Rule (Federal Policy for the Protection of Human Subjects), creating a unified standard across federal departments and agencies [23]. For decades, the Common Rule required annual continuing review for most approved research studies, regardless of risk level. However, recognizing that the research landscape had transformed significantly since the rule's inception, federal regulators embarked on a modernization effort to reduce unnecessary administrative burden while maintaining strong ethical safeguards. The Revised Common Rule, with its key provisions implemented in 2018 and 2019, represents the most substantial change to this framework, particularly in its approach to continuing review for lower-risk studies [23]. This shift reflects a more nuanced understanding of research oversight, where regulatory resources are directed toward areas of greatest ethical concern while reducing unnecessary burden on researchers and institutional review boards (IRBs).
Table: Historical Progression of Key Human Research Protection Documents
| Document/Regulation | Year Issued | Primary Focus | Key Contribution |
|---|---|---|---|
| Belmont Report | 1979 [8] | Ethical Principles | Established three core principles: Respect for Persons, Beneficence, Justice [8] |
| Common Rule | 1991 [23] | Regulatory Standards | Codified Belmont principles into federal regulations for federally-funded research [23] |
| Revised Common Rule | 2018 [23] | Modernization & Burden Reduction | Eliminated mandatory annual continuing review for many minimal risk studies [23] [25] |
Analytical Framework: Connecting Belmont Principles to Continuing Review Changes
The changes to continuing review requirements in the Revised Common Rule are not merely administrative but are deeply rooted in the ethical principles of the Belmont Report. The following diagram illustrates the logical relationship between these ethical foundations and the resulting regulatory changes.
The principle of Beneficence, which entails maximizing benefits and minimizing harm, directly supports the concept of proportional oversight. By reallocating IRB resources from lower-risk studies to those with greater ethical complexities, institutions can better protect participants in studies where the potential for harm is more significant. Similarly, Justice, which concerns the fair distribution of the benefits and burdens of research, is served by not subjecting lower-risk studies to the same level of ongoing scrutiny as higher-risk studies, creating a more equitable oversight system.
Comparative Analysis: Pre-2018 Requirements vs. Revised Common Rule
The Revised Common Rule fundamentally altered the approach to continuing review, moving from a largely uniform annual requirement to a risk-based, differentiated system. The changes specifically target administrative burden reduction in areas where the ethical justification for intensive oversight was weakest. The following workflow diagram maps the decision process for continuing review under the revised requirements.
Key Changes to Continuing Review Requirements
The Revised Common Rule specifically eliminates the requirement for continuing review in the following circumstances [23] [25]:
- Research eligible for expedited review: Studies that the IRB has determined qualify for expedited review procedures, which are for specific categories of minimal risk research, no longer require automatic annual continuing review.
- Research in data analysis phase: Studies that have completed participant enrollment and all research interventions, and are now only involved in the analysis of identifiable private information or identifiable biospecimens, are exempt from continuing review.
- Research accessing follow-up clinical data: Studies that only involve accessing follow-up clinical data from procedures that subjects would undergo as part of their standard clinical care do not require continuing review.
Table: Comparison of Key Oversight Provisions: Pre-2018 vs. Revised Common Rule
| Oversight Aspect | Pre-2018 Common Rule | Revised Common Rule (2018 Requirements) |
|---|---|---|
| Continuing Review General Rule | Annual continuing review required for most approved research [23] | Eliminated for expedited research and studies only analyzing data or accessing clinical follow-up data [23] [25] |
| IRB Discretion | Limited discretion to waive continuing review | Explicit authority for IRB to require continuing review even when not required by regulation if justified [25] |
| Exemption Categories | Limited categories with narrower scope [23] | Expanded categories, including new benign behavioral interventions category [25] |
| Informed Consent | Standard structure without specific focus requirement | Must begin with "key information" section and be organized to facilitate comprehension [25] |
| Single IRB Review | Generally not required for multi-site studies | Mandated for most federally-funded multi-site research (sIRB requirement) [23] |
Institutional Implementation: A Case Study
Belmont University's implementation of these changes provides a practical example of how the Revised Common Rule is applied at the institutional level. The Belmont IRB eliminated automatic continuing review for expedited research beginning January 21, 2019, unless specific justifying circumstances are identified during the initial review process [25]. Examples of such circumstances include research conducted internationally, amendments or incident reports revealing new findings that require additional oversight, or previous non-compliance by the investigator. This approach demonstrates the risk-based oversight model enabled by the revised regulations, where IRB attention is directed toward areas of genuine ethical concern rather than spread uniformly across all studies regardless of risk profile.
Essential Research Reagent Solutions for Compliance Management
Navigating the revised continuing review requirements demands both expertise and appropriate institutional tools. The following table details key resources and solutions that research institutions utilize to manage compliance effectively in the post-revision regulatory environment.
Table: Research Reagent Solutions for Compliance Management
| Solution/Resource | Function/Purpose | Application Context |
|---|---|---|
| Integrated Compliance Platform | Unified system for managing protocols across multiple committees; prevents version control issues and compliance gaps [77]. | Manakes all committee requirements in one place, ensuring compliance is maintained across connected research activities [77]. |
| IRB Management Guide | Comprehensive reference for IRB operations, protocol review, informed consent, and post-approval monitoring in compliance with federal regulations [78]. | Serves as a foundational resource for IRB administrators, chairs, and members; supports ethical principles from Belmont Report [78]. |
| Grants Management Body of Knowledge | Guide to federal financial assistance governance, grant lifecycle phases, and application of internal controls [78]. | Essential for grants management professionals; references key frameworks like Uniform Guidance (2 CFR Part 200) [78]. |
| Clinical Research Desk Reference | Consolidated regulatory documents, guidance, and policies from FDA, OHRP, and ICH in a single resource [78]. | Used by professionals involved in clinical trials for drugs and medical devices; includes 21 CFR parts and ethical frameworks [78]. |
| AI-Powered Protocol Systems | Uses predictive analytics to identify potential compliance risks and automate routine determinations [77]. | Flags protocols with higher deviation rates for additional oversight; automates training tracking and certification compliance [77]. |
Methodology for Evaluating Burden Reduction Impact
Experimental Protocol for Assessing Administrative Burden
To quantitatively assess the impact of the continuing review changes, research institutions can implement the following methodological approach:
- Data Collection Framework: Retrospectively analyze IRB records for a defined period (e.g., 36 months) before and after implementation of the Revised Common Rule. Key metrics should include: number of studies requiring continuing review, staff time devoted to continuing review processes, average time to complete continuing review, and researcher time spent preparing continuing review submissions.
- Comparative Analysis: Categorize studies by review type (exempt, expedited, full board) and risk level. Compare the volume of continuing reviews conducted pre- and post-implementation, with particular attention to the subset of studies that would have required continuing review under the old system but no longer do under the revised regulations.
- Stakeholder Feedback Integration: Deploy anonymous surveys to researchers, IRB members, and institutional officials to gather qualitative data on perceived burden reduction, resource reallocation, and any unintended consequences of the regulatory changes.
Quantitative Burden Reduction Metrics
While specific metrics will vary by institution, the Belmont University implementation provides evidence of significant burden reduction. Their policy shift eliminated automatic continuing review for all expedited research, reserving such review only for specifically justified circumstances [25]. This approach aligns with the broader regulatory goal of reducing unnecessary administrative work. The University of Kentucky's research administration also highlights the importance of tracking federal changes, indicating the ongoing need for institutions to adapt their processes in response to evolving requirements [79].
The changes to continuing review requirements in the Revised Common Rule represent a significant evolution in human subjects research oversight, strategically reducing administrative burden while maintaining ethical protections. By eliminating mandatory annual review for lower-risk studies—particularly those eligible for expedited review and those in the data analysis phase—the revised regulations allow IRBs to focus their limited resources on higher-risk studies where oversight provides the greatest ethical benefit. This shift toward proportional oversight is firmly grounded in the Belmont Report's principles of Beneficence and Justice, ensuring that the level of review corresponds to the potential risks faced by research participants. For researchers and institutions, understanding these changes is crucial for efficient compliance management. Successful adaptation involves implementing smart systems, training personnel on the revised requirements, and continuously evaluating the impact of these regulatory changes on both administrative burden and research participant protection.
A Head-to-Head Comparison: Belmont Report Ethical Principles vs. Common Rule Regulatory Mandates
The ethical conduct of human subjects research in the United States is governed by a foundational partnership between ethical principles and codified regulations. This framework is built upon the Belmont Report, which establishes the core ethical principles, and the Common Rule (the Federal Policy for the Protection of Human Subjects), which translates these principles into enforceable regulatory requirements [8] [23] [80]. This guide provides a comparative analysis of these two pillars, offering researchers, scientists, and drug development professionals a clear understanding of their distinct roles, interconnectedness, and practical impacts on research protocols and outcomes.
The Belmont Report, published in 1979, was a direct response to historical ethical abuses in research, such as the Tuskegee Syphilis Study [8] [16]. It provides the moral compass for the research community. The Common Rule, first published in 1991 and revised in 2018, is the regulatory embodiment of these principles, creating a uniform policy adopted by multiple federal departments and agencies [23] [80]. Understanding the relationship between the guiding "ought" of Belmont and the specific "must" of the Common Rule is essential for navigating the modern clinical research landscape responsibly and effectively.
Core Ethical Principles of the Belmont Report
The Belmont Report establishes three fundamental ethical principles that form the bedrock for the protection of human research subjects. The table below summarizes their definitions and primary applications.
Table 1: Foundational Ethical Principles of the Belmont Report
| Ethical Principle | Core Definition | Application in Research Practice |
|---|---|---|
| Respect for Persons | Recognizes the autonomous nature of individuals and requires that those with diminished autonomy are entitled to protection [14]. | - Informed Consent: Ensuring prospective subjects understand the research and voluntarily agree to participate [14] [81].- Protection of Vulnerable Populations: Providing additional safeguards for groups with reduced autonomy (e.g., children, prisoners) [14]. |
| Beneficence | Entails an obligation to secure the well-being of research subjects by maximizing anticipated benefits and minimizing possible harms [14] [16]. | - Risk-Benefit Assessment: Systemically analyzing the research to ensure risks are justified by the potential benefits to the subject or society [14].- Ongoing Safety Monitoring: Ensuring participant safety throughout the study duration. |
| Justice | Requires the fair distribution of the burdens and benefits of research, ensuring that no group is unfairly selected for research or excluded from its benefits [14]. | - Equitable Subject Selection: Avoiding the systematic selection of subjects based on convenience, vulnerability, or prejudice [14].- Fair Access: Ensuring research opportunities and resulting therapies are available to a diverse population. |
From Principle to Regulation: The Common Rule
The Common Rule (formally known as the Federal Policy for the Protection of Human Subjects) is the primary regulatory framework that operationalizes the ethical principles of the Belmont Report for most federally funded or conducted research in the United States [23] [80]. The following diagram illustrates the workflow from ethical foundation to research implementation.
The Revised Common Rule (the "2018 Requirements") was implemented to modernize the regulations, reflecting significant changes in the volume, type, and methods of human subjects research [23]. Key updates aimed to reduce administrative burden, facilitate research, and address new ethical challenges, such as those posed by genomic research and large datasets [23] [80].
Comparative Analysis: Principle, Regulation, and Outcome
The following table provides a direct comparison of how each ethical principle from the Belmont Report is translated into specific regulatory requirements by the Common Rule, and the resulting practical outcomes for research.
Table 2: Comparative Analysis: Ethical Principle vs. Regulatory Application vs. Practical Outcome
| Ethical Principle(Belmont Report) | Regulatory Application(Common Rule) | Practical Outcome & Researcher Responsibilities |
|---|---|---|
| Respect for Persons | - Informed Consent (45 CFR 46.116): Mandates a process that provides key information a reasonable person would want, in an understandable format, allowing voluntary participation [80].- Documentation of Consent (45 CFR 46.117): Requires signed consent forms, with certain narrow exceptions [23].- Broad Consent: A new option for obtaining prospective consent for the storage, maintenance, and secondary research use of identifiable private information or biospecimens [23] [80]. | - Action: Develop and obtain IRB-approved informed consent documents.- Outcome: Participants are better equipped to make autonomous decisions about their involvement, fostering trust and ethical integrity. |
| Beneficence | - IRB Review (45 CFR 46.109): Requires review of research to ensure risks are minimized and are reasonable in relation to anticipated benefits [23] [14].- Continuing Review: The Revised Common Rule eliminates the requirement for annual continuing review for some minimal-risk studies [23]. | - Action: Submit a detailed research protocol to the IRB for risk-benefit analysis.- Outcome: A systematic, independent evaluation safeguards participant welfare and ensures study design is scientifically sound and ethically justified. |
| Justice | - IRB Membership (45 CFR 46.107): Requires diverse membership, including consideration of race, gender, cultural backgrounds, and sensitivity to community attitudes.- Equitable Selection (45 CFR 46.111): Directs IRBs to ensure the selection of subjects is equitable. | - Action: Justify inclusion and exclusion criteria in the protocol to avoid systematically targeting vulnerable groups or unfairly excluding eligible populations.- Outcome: Promotes diversity in clinical trials and ensures the benefits and burdens of research are shared more fairly across society. |
| General Principles | - Exemptions & Limited IRB Review (45 CFR 46.104): The Revised Common Rule expanded categories of exempt research and introduced "limited IRB review" for some categories, reducing administrative burden for low-risk studies [23] [80].- Single IRB (sIRB) of Record (45 CFR 46.114): For most federally-funded multi-site research, a single IRB must be used to streamline the review process and enhance consistency [23]. | - Action: Work with the IRB to correctly categorize studies and comply with sIRB mandates for collaborative projects.- Outcome: Increased efficiency in launching and conducting research while maintaining ethical oversight, particularly beneficial for large-scale studies. |
Successfully navigating the requirements of the Belmont Report and the Common Rule requires familiarity with key resources and institutional bodies.
Table 3: Essential Research Reagent Solutions for Human Subjects Protection
| Resource | Function & Purpose |
|---|---|
| Institutional Review Board (IRB) | An administrative body established to protect the rights and welfare of human research subjects. It reviews, approves, and provides ongoing oversight of research protocols [8] [80]. |
| Informed Consent Documents | The legally and ethically required forms and process that convey all necessary information about the research study to a potential subject, enabling an informed decision about participation [14] [80]. |
| Office for Research Compliance | A university or institutional office that assists researchers in interpreting and applying federal regulations, institutional policies, and ethical standards to their specific projects [80]. |
| Good Clinical Practice (GCP) Training | An international ethical and scientific quality standard for designing, conducting, recording, and reporting trials that involve human subjects. Compliance with GCP provides public assurance that the rights and well-being of subjects are protected [8]. |
| The Belmont Report | The foundational document that researchers, IRB members, and institutional officials are expected to know, as it provides the ethical basis for HHS regulations [14]. |
The relationship between the Belmont Report and the Common Rule is symbiotic. The Belmont Report provides the enduring ethical foundation—the "why" behind the rules—while the Common Rule provides the dynamic regulatory framework—the "how" of implementation [8] [23] [14]. For researchers, scientists, and drug development professionals, a deep understanding of both is not merely a regulatory obligation but a prerequisite for conducting scientifically valid and ethically sound research. The 2018 revisions to the Common Rule demonstrate that this framework continues to evolve, striving to balance rigorous participant protection with the efficiency needed to advance public health in a rapidly changing research environment [23] [80].
The Belmont Report of 1979 established an ethical framework for human subjects research in the United States, articulating three core principles: Respect for Persons, Beneficence, and Justice [14]. These principles were later codified into federal regulations through the Federal Policy for the Protection of Human Subjects, known as the Common Rule [8] [23]. While the Common Rule is heavily influenced by the Belmont Report, it is not a direct transcription; it expands upon, operationalizes, and in some instances diverges from the foundational ethical ideals. This guide provides a detailed comparison of the two frameworks, highlighting key areas where the Common Rule establishes specific regulatory requirements that exceed the Belmont Report's general principles or introduces new concepts not originally present. Designed for researchers, scientists, and drug development professionals, this analysis uses structured data and visual workflows to clarify these critical relationships for modern research practice.
Foundational Frameworks: From Ethical Principles to Regulatory Code
The table below summarizes the core ethical principles from the Belmont Report and their primary manifestations within the Common Rule's regulatory structure.
Table 1: Core Ethical Principles and Their Regulatory Applications
| Belmont Report Principle | Core Ethical Meaning | Primary Common Rule Applications |
|---|---|---|
| Respect for Persons | Acknowledging individual autonomy and protecting those with diminished autonomy [14]. | Informed consent process and documentation (45 CFR §46.116) [31] [13]. |
| Beneficence | The obligation to maximize benefits and minimize potential harms [14]. | Assessment of risks and benefits by an Institutional Review Board (IRB) [14] [16]. |
| Justice | Ensuring the fair distribution of the burdens and benefits of research [14]. | Equitable selection of subjects in research studies [14] [82]. |
The following diagram illustrates the foundational relationship between the Belmont Report and the Common Rule, showing how ethical principles are translated into enforceable regulations.
Key Areas of Regulatory Exceedance and Dissonance
The Common Rule extends beyond the Belmont Report's foundational principles by establishing specific, actionable regulatory requirements. The following sections detail the most significant areas of this exceedance and divergence.
Informed Consent: From Ethical Concept to Regulated Process
While the Belmont Report emphasizes the importance of informed consent as part of "Respect for Persons," the Common Rule provides detailed, prescriptive requirements for its implementation [13]. The 2018 revisions introduced significant changes that further refined these requirements.
Table 2: Evolution of Informed Consent Requirements
| Aspect of Consent | Belmont Report Guidance | Common Rule (Pre-2018) Requirements | Revised Common Rule (2018) Exceedances |
|---|---|---|---|
| Content & Presentation | Recommends providing information about procedures, purposes, risks, benefits, and alternatives [14]. | Required a list of eight basic elements of consent in language understandable to the subject [31]. | Mandates a "concise and focused" key information section first and requires the consent form as a whole to facilitate understanding [31] [13]. |
| Standard for Understanding | Implicit in the goal of ensuring the subject has "sufficient information" for a decision [14]. | Information must be "in language understandable to the subject" [13]. | Introduces the "reasonable person" standard to determine what key information should be presented [13]. |
| New Consent Elements | Does not address contemporary research contexts like biospecimens or genomic data. | N/A | Requires new consent elements for broad consent for future biospecimen use, commercial profit, and return of research results [31] [13]. |
| Public Transparency | Not addressed. | N/A | Requires informed consent forms for clinical trials to be publicly posted on a federal website [13]. |
Operational Oversight: The IRB and Review Categories
The Belmont Report suggests that a review body should systematically consider the risks and benefits of research [14]. The Common Rule operationalizes this by mandating and defining the role of the Institutional Review Board (IRB) and creating specific categories of research review.
Table 3: Oversight Structures and Review Categories
| Oversight Feature | Belmont Report Mention | Common Rule Implementation & Exceedance | |
|---|---|---|---|
| IRB Mandate | Describes a method IRBs can use for review but does not mandate them [14]. | Mandates IRB review for all non-exempt human subjects research and details IRB composition, functions, and operations [31]. | |
| Exempt Research | Does not differentiate levels of review based on risk. | Establishes specific categories of "exempt" research that do not require ongoing IRB oversight, which were expanded in the 2018 revisions [31] [12]. | |
| Expedited Review | Does not differentiate levels of review based on risk. | Allows for "expedited review" procedures for certain minimal-risk research [31]. | |
| Continuing Review | Implied in ongoing assessment of research. | Required continuing review at least annually for most approved research. | Eliminates continuing review requirement for some studies that have progressed to data analysis or follow-up clinical care [31] [23]. |
| Single IRB Mandate | Not addressed. | Requires U.S.-based multi-institutional research to use a single IRB of record to streamline review (effective 2020) [31] [23]. |
Defining the Boundaries of Research
The Belmont Report does not explicitly define what activities constitute "research." A key area where the Common Rule exceeds Belmont is in its precise definitions and exclusions, which determine whether an activity falls under its regulatory purview.
Table 4: Activities Not Considered Human Subjects Research under the 2018 Common Rule
| Activity | Description |
|---|---|
| Scholarly & Journalistic Activities | Includes oral history, journalism, biography, literary criticism, legal research, and historical scholarship focused directly on specific individuals [31]. |
| Public Health Surveillance | Activities conducted, supported, or authorized by a public health authority to monitor public health signals or disease outbreaks [31]. |
| Criminal Justice Activities | Collection and analysis of information by or for a criminal justice agency for criminal justice or investigative purposes authorized by law [31]. |
| Operational Activities | Activities in support of intelligence, homeland security, defense, or other national security missions [31]. |
Emerging Dissonance: Protection vs. Inclusion of Vulnerable Populations
A critical area of modern dissonance lies in the application of the principle of Justice. The Belmont Report emphasizes protecting vulnerable populations from exploitation, which historically led to their exclusion from research [83] [16]. The contemporary ethical and regulatory landscape is shifting toward a model of fair inclusion, creating tension with overly protective policies.
Recent empirical research indicates that Institutional Review Board (IRB) policies may contribute to the unfair exclusion of populations with uncertain or impaired decision-making capacity (DMC), such as those with cognitive disabilities, psychiatric conditions, or dementia [83]. A 2025 cross-sectional study of 94 top-funded U.S. research institutions found that:
- 41.5% of institutions had policies that require exclusion of people with uncertain or impaired DMC unless inclusion is scientifically justified.
- Only 5.3% had policies that require inclusion of these populations unless exclusion is scientifically justified [83].
This protectionist stance is increasingly viewed as a violation of the principle of justice and, with the 2024 updates to Section 504 of the Rehabilitation Act, may constitute disability discrimination [83]. The diagram below outlines the ethical dilemma and regulatory shift concerning vulnerable populations.
Limitations in Addressing Group Harms and Indigenous Sovereignty
Another significant area of dissonance is the Common Rule's focus on individual-level risks and benefits, which fails to adequately address group harms. This is particularly salient in research involving Indigenous communities, where the Common Rule's underlying ethical framework, derived from Belmont, prioritizes individual autonomy over collective, community-level interests [84]. The regulations place the burden on Tribal nations to establish their own research oversight infrastructure to protect against exploitative research, a significant financial and administrative challenge [84]. This contrasts with frameworks like Indigenous Data Sovereignty (IDSov) and the CARE Principles, which are grounded in collective self-determination and ensure research benefits the community and aligns with its values [84].
The Researcher's Toolkit: Navigating the Regulatory Environment
For researchers and drug development professionals, navigating the interplay between the Belmont principles and Common Rule regulations requires a set of conceptual tools and resources.
Table 5: Essential Resources for Ethical Research Compliance
| Tool or Resource | Primary Function | Relevance to Belmont & Common Rule |
|---|---|---|
| Institutional Review Board (IRB) | Provides independent ethical review and approval of research protocols [14] [82]. | Operationalizes the Belmont principle of Beneficence and enforces the specific requirements of the Common Rule. |
| Informed Consent Templates (Institution-approved) | Provide a structured format for disclosing all required information to potential participants. | Ensures compliance with both the ethical goal of Respect for Persons and the detailed regulatory elements of §46.116. |
| Exemption & Limited Review Checklists | Tools to help determine if research qualifies for an exemption or limited IRB review. | Helps researchers apply the specific categories defined in the Common Rule that have no direct counterpart in the Belmont Report. |
| Office for Human Research Protections (OHRP) Website | A federal repository of guidance, FAQs, and educational resources on the Common Rule. | Provides official interpretation of regulations that translate Belmont's principles. |
| Public Consent Form Repositories | Publicly accessible databases of consent forms from clinical trials. | A result of the 2018 Common Rule revisions, this tool promotes transparency and helps researchers design better consent documents. |
The relationship between the Belmont Report and the Common Rule is one of dynamic interplay between foundational ethics and enforceable regulation. While the Common Rule is firmly rooted in the principles of Respect for Persons, Beneficence, and Justice, it necessarily exceeds the Belmont Report by establishing detailed, procedural requirements for informed consent, IRB oversight, and categories of research review. Furthermore, significant dissonance has emerged in areas such as the inclusion of populations with impaired decision-making capacity and the recognition of group-level harms, particularly for Indigenous communities. For the modern researcher, understanding where the Common Rule harmonizes with, exceeds, or diverges from the Belmont Report is not merely an academic exercise—it is a practical necessity for conducting ethical, compliant, and impactful research in a rapidly evolving landscape.
For drug development professionals, navigating the U.S. regulatory landscape for human subject research requires understanding two parallel regulatory frameworks: the Food and Drug Administration (FDA) regulations (21 CFR Parts 50 and 56) and the Federal Policy for the Protection of Human Subjects, commonly known as the Common Rule (45 CFR Part 46, Subpart A). While both frameworks share common ethical foundations rooted in the Belmont Report's principles of respect for persons, beneficence, and justice, they contain significant differences in application, scope, and specific requirements that directly impact clinical trial design and execution.
The 21st Century Cures Act has mandated harmonization between these frameworks to reduce unnecessary duplication and burden, yet important distinctions remain that drug developers must recognize [85]. This guide provides a detailed comparative analysis of these regulations, focusing on practical implications for pharmaceutical research and development.
Regulatory Foundations and Historical Context
Origins and Ethical Underpinnings
Both the FDA regulations and the Common Rule trace their ethical foundation to the 1979 Belmont Report, which established the three fundamental principles governing research with human subjects [23]. Despite this shared heritage, the regulations developed separately to address different needs:
- Common Rule: First published in 1991 and codified by 15 federal departments and agencies, it establishes the baseline ethical standards for federally conducted or supported human subject research [23].
- FDA Regulations (21 CFR 50/56): Specifically govern clinical investigations related to products regulated by the FDA, including drugs, biological products, medical devices, and dietary supplements [86].
The Common Rule underwent significant revision in 2017 (the "2018 Requirements"), while the FDA has proposed but not yet finalized similar updates to 21 CFR 50 and 56 [87] [85]. This has created a period of regulatory misalignment that drug developers must carefully navigate.
Scope and Applicability
The most fundamental difference between these frameworks lies in their scope of application:
Table: Scope and Applicability Comparison
| Regulatory Aspect | FDA Regulations (21 CFR 50/56) | Common Rule (2018 Requirements) |
|---|---|---|
| Governed Research | Clinical investigations supporting applications for FDA-regulated products [86] | Research conducted or supported by federal departments that have adopted the rule [31] |
| Key Products Covered | Drugs, biologics, medical devices, food additives, dietary supplements with health claims [86] | All research involving human subjects conducted or supported by federal departments adhering to the rule |
| Funding Dependency | Applies regardless of funding source [42] | Applies only to federally conducted or supported research [31] |
| Current Status | Proposed harmonization changes pending [85] | Revised requirements effective as of January 21, 2019 [32] |
Key Regulatory Differences: Comparative Analysis
Institutional Review Board (IRB) Oversight
Both frameworks require IRB review and approval of research, but differ in specific operational requirements:
Table: IRB Requirements Comparison
| IRB Element | FDA Regulations (21 CFR 50/56) | Common Rule (2018 Requirements) |
|---|---|---|
| Continuing Review | Required at least annually for all research [85] | No longer required for certain categories, including expedited research and studies involving only data analysis [32] |
| Expedited Review | May be used for research on FDA's expedited review list involving no more than minimal risk [85] | Similar provisions, but with requirement to evaluate expedited review list at least every 8 years [85] |
| Single IRB Mandate | Proposed for cooperative research [85] | Required for multi-institutional research (as of January 20, 2020) [23] |
| Limited IRB Review | Not currently addressed in FDA regulations [85] | New process for certain exempt categories to ensure privacy/confidentiality protections [32] |
Informed Consent Requirements
Informed consent represents a cornerstone of human subject protection in both frameworks, with the recent Common Rule revisions introducing significant changes that FDA-regulated research may eventually adopt:
Key Differences in Informed Consent Requirements:
Key Information Presentation: The revised Common Rule mandates that consent begins with "a concise and focused presentation of the key information" most likely to assist a prospective subject's decision-making [32]. The FDA has proposed adopting this requirement to harmonize with the Common Rule [85].
Future Research Use: For research involving collection of identifiable private information or identifiable biospecimens, the Common Rule requires one of two specific statements regarding future research use [32]. The FDA has proposed a more flexible approach requiring a "description" of how information or biospecimens may be used or distributed for future research [85].
New Additional Elements: The revised Common Rule added three new additional elements of consent addressing:
- Commercial profit from biospecimens
- Disclosure of clinically relevant research results
- Whole genome sequencing [32]
The FDA has proposed incorporating these same additional elements into its regulations [85].
Exemptions and Waivers
The frameworks differ significantly in their approach to research exemptions and consent alterations:
Table: Exemptions and Waivers Comparison
| Category | FDA Regulations (21 CFR 50/56) | Common Rule (2018 Requirements) |
|---|---|---|
| Research Exemptions | Limited exemptions [23] | Expanded categories, including benign behavioral interventions and secondary research with identifiable information/biospecimens [31] |
| Consent Alteration/Waiver | Permitted under 21 CFR 50.23 (emergency) and 50.24 (exception from informed consent) | Additional criterion: research could not practicably be carried out without using identifiable information [31] |
| Limited IRB Review | Not addressed | Required for certain exemption categories to ensure adequate privacy/confidentiality protections [32] |
Harmonization Efforts and Future Directions
The 21st Century Cures Act Mandate
Section 3023 of the 21st Century Cures Act directs the Secretary of Health and Human Services to harmonize differences between the Common Rule and FDA's human subject regulations to the extent practicable and consistent with statutory provisions [85]. This mandate has prompted the FDA to issue proposed rules to align certain aspects of its regulations with the revised Common Rule.
Key Proposed FDA Revisions
In September 2022, the FDA published two proposed rules addressing harmonization:
- Protection of Human Subjects and Institutional Review Boards: Would revise informed consent requirements and eliminate continuing IRB review in certain circumstances [85].
- Institutional Review Boards; Cooperative Research: Would require single IRB review for multisite research in the U.S., with limited exceptions [85].
These proposed changes represent significant steps toward alignment but do not address all differences between the frameworks. The FDA has explicitly noted that harmonization efforts are ongoing regarding provisions on broad consent, limited IRB review, exempt research, and public health surveillance activities [85].
Practical Implications for Drug Developers
Protocol Design Considerations
Drug developers must design clinical trials to satisfy both regulatory frameworks when research involves FDA-regulated products and federal funding:
Table: Key Research Resources for Regulatory Compliance
| Resource Category | Specific Examples | Application in Drug Development |
|---|---|---|
| Regulatory Documentation | Investigator's Brochure, Protocol, Informed Consent Documents [42] | Provides essential safety and procedural information required for IRB review and subject consent |
| IRB Submission Systems | Electronic IRB submission platforms [32] | Streamlines protocol submission, tracking, and communication with review boards |
| Informed Consent Templates | FDA-compliant and Common Rule-compliant templates [32] | Ensures all required regulatory elements are addressed in consent documentation |
| Guidance Documents | FDA Guidance on Informed Consent, OHRP Guidance [88] [42] | Provides current interpretation and implementation strategies for complex regulatory requirements |
| Training Programs | CITI Program, Institutional Training [87] | Ensures research team competency in human subject protection requirements |
Strategic Implementation Approach
Drug developers should implement a systematic approach to regulatory compliance:
- Conduct Dual Framework Analysis: For each clinical trial, assess applicability of both FDA and Common Rule requirements.
- Adopt Most Stringent Standards: When requirements differ, apply the more protective standard to ensure compliance with both frameworks.
- Implement Harmonized Procedures: Develop standard operating procedures that incorporate elements from both frameworks, focusing on recently revised areas.
- Monitor Regulatory Updates: Track FDA's ongoing harmonization efforts and implement changes as proposals become final rules.
The regulatory landscape governing human subject research in drug development continues to evolve toward greater harmonization between the FDA regulations and the Common Rule. While significant progress has been made through the FDA's proposed rules, drug developers must currently navigate a hybrid system with important distinctions in IRB review requirements, informed consent elements, and exemption categories.
Successful navigation of this complex environment requires understanding both the current requirements and the direction of proposed changes. By adopting a proactive approach that anticipates further harmonization while respecting current distinctions, drug developers can ensure both regulatory compliance and robust protection for human subjects participating in clinical trials.
The shared ethical foundation provided by the Belmont Report continues to guide both regulatory frameworks, ensuring that despite technical differences in implementation, the fundamental principles of respect for persons, beneficence, and justice remain central to human subject research in drug development.
The design of industry-sponsored clinical trials is undergoing a significant transformation, driven by concurrent updates to both foundational ethical frameworks and practical regulatory requirements. The Belmont Report's ethical principles (Respect for Persons, Beneficence, and Justice) and their codification in the Common Rule provide the enduring ethical foundation for human subjects research in the United States [8]. Meanwhile, recent regulatory developments—including the International Council for Harmonisation's (ICH) E6(R3) Good Clinical Practice (GCP) guideline, updates to the FDA Amendments Act (FDAAA) 801 Final Rule, and a growing emphasis on decentralized trials and diversity—are fundamentally reshaping trial design and execution [89] [90] [91]. This guide objectively compares the practical implications of these changes for industry-sponsored research, analyzing how new regulatory approaches align with or implement core Belmont Report principles, with supporting data on their impact on trial performance metrics.
Comparative Analysis of Core Ethical Principles and Modern Regulatory Implementation
The following table maps key 2025 regulatory changes to their corresponding ethical principles from the Belmont Report, providing a structured comparison of their practical implications for industry-sponsored trial design.
Table 1: Mapping of 2025 Regulatory Changes to Belmont Report Ethical Principles
| Belmont Report Ethical Principle | 2025 Regulatory Manifestation | Practical Impact on Industry-Sponsored Trial Design | Performance Consideration |
|---|---|---|---|
| Respect for Persons (Protecting autonomy through informed consent) | - FDAAA 801: Mandatory posting of redacted informed consent forms [90]- ICH E6(R3): Promotes proportional, participant-focused approaches [89]- LLM-Generated ICFs: Technology to improve readability and comprehension [92] | - Increased transparency forces higher scrutiny of consent documents.- Drives adoption of tech solutions (e.g., LLMs) to create simpler, more actionable consent forms at lower reading levels. | LLM-generated ICFs showed significant improvements in readability (76.39% vs 66.67% on RUAKI score) and understandability (90.63% vs 67.19%) versus human-generated forms [92]. |
| Beneficence (Minimizing risk, maximizing benefit) | - ICH E6(R3): Mandates flexible, risk-based approaches and quality-by-design [89]- IRB Challenges: Documented difficulties in assessing risk-benefit for early-phase trials [40] | - Requires more upfront risk assessment and critical thinking in protocol design, not just compliance checking.- Necessitates more robust pre-clinical data packages for IRB review, especially in neurology and other high-attrition areas. | 66% of IRB chairs find risk-benefit analysis for early-phase trials more challenging than for later phases; over 1/3 feel unprepared for assessing scientific value and risks [40]. |
| Justice (Fair distribution of research burdens and benefits) | - FDA/EMA Diversity Initiatives: Emphasis on inclusive trial design and recruitment [91]- Decentralized Clinical Trials (DCTs): Updated FDA/EMA guidance facilitating remote participation [91] | - Requires proactive diversity plans and strategies to overcome recruitment barriers.- Demands investment in digital and logistical infrastructure to support remote participants, increasing access to underserved populations. | DCTs increase accessibility for participants in remote or underserved areas, directly addressing historical underrepresentation [91]. |
Experimental Protocols and Methodologies for Modern Trial Design
Protocol for Implementing Risk-Based Monitoring (RBM) in Alignment with ICH E6(R3)
Objective: To implement a monitoring strategy that ensures participant protection and data reliability while optimizing resource allocation, as required by ICH E6(R3)'s focus on risk-based quality management [89].
Methodology:
- Centralized Data Monitoring: Implement a centralized system for near real-time review of key risk indicators (KRIs) like protocol deviations, eligibility criteria, and adverse event reporting patterns. This reduces the need for frequent, costly on-site visits.
- Targeted On-Site Visits: Conduct on-site monitoring visits based on triggered risk alerts (e.g., high screen-failure rates, data inconsistencies) rather than a fixed schedule.
- Source Data Verification (SDV) Reduction: Drastically reduce 100% SDV, focusing instead on critical data points pre-identified in the risk assessment.
Workflow Visualization: The diagram below illustrates the cyclical, risk-adapted monitoring process.
Protocol for Generating Participant-Centric Informed Consent Using Large Language Models (LLMs)
Objective: To generate the key information section of an Informed Consent Form (ICF) that meets the Common Rule's requirement for a "concise and focused presentation" using LLMs, thereby enhancing participant comprehension [92].
Methodology:
- Input Processing: Feed the complete clinical trial protocol into the LLM (e.g., Mistral 8x22B, chosen for its 64K token context window and open-source license) [92].
- Structured Prompting: Use a "Least-to-Most" prompting approach:
- Step 1: Extract relevant information for each key section from the protocol.
- Step 2: Refine the output using Readability, Understandability, and Actionability of Key Information (RUAKI) indicators.
- Step 3: Adjust content to achieve a Flesch-Kincaid grade level below 8.
- Step 4: Format the final output according to institutional templates [92].
- Human-in-the-Loop Review: A multidisciplinary team (e.g., clinical researchers, IRB officers) must review the LLM output for accuracy and completeness before use.
Workflow Visualization: The diagram below outlines the multi-step, iterative process for generating a participant-centric ICF.
The Scientist's Toolkit: Essential Reagents & Solutions for 2025 Trial Design
The following table details key solutions and methodologies required to implement modern, compliant clinical trials.
Table 2: Essential Research Reagent Solutions for Modern Clinical Trial Implementation
| Tool/Solution | Function in Modern Trial Design | Regulatory/Ethical Justification |
|---|---|---|
| Risk-Based Monitoring (RBM) Software | Enables centralized, remote monitoring of key risk indicators and critical data points from multiple sites in near real-time. | Aligns with ICH E6(R3) mandate for risk-based quality management, improving efficiency while safeguarding data integrity (Beneficence) [89]. |
| Large Language Models (LLMs) e.g., Mistral 8x22B | Automates and enhances the generation of informed consent forms by improving readability, understandability, and actionability. | Addresses Belmont's "Respect for Persons" by making consent truly informed; meets Common Rule requirement for a concise key information section [92] [8]. |
| Decentralized Clinical Trial (DCT) Platforms | Facilitates remote participant engagement through telemedicine, electronic consents (eConsent), and direct-to-patient drug shipment. | Supports Belmont's "Justice" by expanding access to underserved populations; operationalizes FDA/EMA DCT guidance [91]. |
| Real-World Evidence (RWE) Data Repositories | Provides data from electronic health records, registries, and wearables to complement traditional trial data and support more adaptive designs. | Embraced by FDA's Advancing RWE Program and EMA to enhance understanding of drug effects in broader, more diverse populations (Justice, Beneficence) [91]. |
| Digital Compliance & Reporting Systems | Automates tracking and submission of trial registration and results to meet tighter FDAAA 801 deadlines and public posting mandates. | Ensures compliance with FDAAA 801 Final Rule's shortened timelines and new penalties, enforcing transparency (Respect for Persons, Justice) [90]. |
The 2025 regulatory landscape for clinical trials represents a significant evolution toward operationalizing the ethical principles of the Belmont Report. The ICH E6(R3) guidelines modernize trial conduct by embedding flexibility and a focus on human participants, directly supporting the principles of Beneficence and Respect for Persons [89]. Concurrently, the FDAAA 801 Final Rule changes enforce greater transparency, publicly holding sponsors accountable for timely results reporting and providing participants with clearer information through public ICFs [90]. For industry sponsors, success now depends on integrating these frameworks from the earliest stages of trial design. This requires a shift from viewing compliance as a series of checkboxes to embracing it as a strategic imperative that, when aligned with core ethical principles, ultimately leads to more efficient, credible, and successful clinical development programs.
For researchers, scientists, and drug development professionals, navigating the regulatory environment is a fundamental part of experimental design. The foundational Belmont Report's ethical principles of Respect for Persons, Beneficence, and Justice continue to provide the ethical compass for human subjects research [8]. These principles are operationalized through the Federal Policy for the Protection of Human Subjects (the Common Rule), which was significantly updated in a 2018 revision [93] [49]. Concurrently, the 21st Century Cures Act (Cures Act), enacted in 2016, introduced sweeping changes designed to accelerate medical product development and biomedical research [94] [95].
This guide provides a comparative analysis of these frameworks, offering a strategic toolkit to help researchers future-proof their protocols, enhance compliance, and leverage new opportunities for data sharing and innovation.
Comparative Analysis of Regulatory Frameworks
The modern research environment is shaped by the interplay between established ethical rules and new legislative mandates. The table below compares the core components of the Revised Common Rule and the 21st Century Cures Act.
Table 1: Key Regulatory Framework Comparison
| Feature | The Revised Common Rule (Effective 2019) | The 21st Century Cures Act (Enacted 2016) |
|---|---|---|
| Primary Focus | Protection of human subjects in research [93] [49] | Accelerating medical product development and biomedical innovation [94] [95] |
| Informed Consent | Requires a concise summary of key information; mandates specific new disclosures for clinical trials [25] [49] | Promotes patient access to their own electronic health information to facilitate participant-partnered research [96] |
| Oversight & Review | Eliminates continuing review for many minimal risk studies and studies in data analysis stage [25] [49] | Accelerates review of novel products via new programs like Regenerative Medicine Advanced Therapy (RMAT) [94] |
| Data Sharing & Use | Establishes new categories of exempt research and provisions for secondary research use of data/biospecimens [25] [49] | Mandates interoperability of electronic health information and prohibits information blocking [96] [97] |
| Multi-Site Research | Mandates use of a single Institutional Review Board (sIRB) for federally-funded multi-site research [49] | Aims to create a nationwide health information exchange network to facilitate data flow [96] |
Ethical Foundations and Operational Harmony
The relationship between these frameworks is synergistic. The Belmont Report establishes the enduring ethical principles [8]. The Revised Common Rule translates these principles into concrete regulatory requirements for research conduct [93] [49]. The Cures Act then creates an infrastructure for faster innovation and data fluidity that operates within this ethical and regulatory system [94] [96]. For researchers, compliance now means harmonizing all three layers.
Diagram 1: Regulatory Framework Relationships
Experimental Protocols for Compliance and Data Interoperability
A future-proofed research protocol must embed compliance with these interconnected frameworks from its inception. The following experimental workflows are critical for modern study design.
Protocol for Information Blocking Compliance
The Cures Act's prohibition on information blocking—practices that interfere with access, exchange, or use of electronic health information (EHI)—has significant implications for research data sourcing [96] [97]. The diagram below outlines a validation protocol to ensure compliance.
Diagram 2: Information Blocking Compliance Workflow
Methodology: This workflow should be integrated into the study's data management plan.
- Initiation: Define the specific EHI data set required from a healthcare provider's Electronic Health Record (EHR) system [96] [98].
- Request & Logging: Submit a formal data request through the approved channel (e.g., a certified API) and log the request with a timestamp [96].
- Monitoring & Analysis: Monitor the fulfillment timeline. Analyze any delays or denials for a documented justification that aligns with one of the eight recognized exceptions defined by the Office of the National Coordinator for Health IT (ONC) [96] [97].
- Assessment & Reporting: If no valid exception is documented and provided, the practice may constitute information blocking. Developers and Health Information Networks/Exchanges determined to have committed information blocking are subject to civil monetary penalties of up to $1 million per violation [96] [97]. Healthcare providers can be subject to disincentives within Medicare programs [97].
Protocol for Integrating Real-World Evidence
The Cures Act encourages the use of real-world evidence (RWE) to support medical product development and modernize clinical trials [94]. This protocol leverages patient-accessed data from EHRs via APIs, a key provision of the Act [96].
Methodology:
- Patient Recruitment & Consent: Recruit patients for an observational or interventional study. The informed consent process must be revised per the Revised Common Rule, beginning with a "concise and focused presentation" of key information and including clear language about how the patient's data will be used and shared for research [25] [49].
- Patient-Mediated Data Access: Utilize the patient's right to access their EHI under HIPAA and the Cures Act. Patients can use an application of their choice (e.g., a research app with a certified API) to pull their longitudinal health data from multiple provider EHRs [96].
- Data Aggregation & De-identification: The research application aggregates the data from participating patients. For analysis, data is de-identified in accordance with HIPAA standards to protect patient privacy.
- Analysis & Application: The aggregated, de-identified RWE dataset is analyzed to generate insights into disease progression, treatment effectiveness, or population health trends, which can be used to support regulatory submissions or inform clinical trial design [94] [96].
The Scientist's Toolkit: Essential Research Reagent Solutions
Beyond biological reagents, a modern researcher's toolkit must include solutions for regulatory compliance and data interoperability. The following tools are essential for operating within the current research ecosystem.
Table 2: Essential Regulatory & Data Reagent Solutions
| Research 'Reagent' | Function & Application in Protocol |
|---|---|
| Certified EHR API | A standardized application programming interface that is certified to allow health information to be accessed, exchanged, and used without special effort, enabling patient-mediated data transfer [96] [98]. |
| Revised Consent Template | An informed consent form template that complies with the Revised Common Rule, featuring the required key information summary and new disclosure elements for clinical trials [25] [49]. |
| sIRB Agreement | A formal agreement for multi-site studies that designates a Single IRB of Record, as now mandated for most federally-funded research, streamlining the ethical review process [49]. |
| Information Blocking Compliance Checklist | An internal auditing tool to document data requests, fulfillment timelines, and justifications for any delays/denials, serving as a defense against potential enforcement actions [97] [98]. |
| Broad Consent Framework | A protocol for obtaining and managing prospective patient consent for the storage and future secondary research use of identifiable data and biospecimens, as defined in new exemption categories 7 and 8 of the Revised Common Rule [25]. |
Success in the evolving research landscape requires a proactive, integrated approach. Researchers and drug development professionals must view the Revised Common Rule and the Cures Act not as separate burdens, but as complementary components of a modern research infrastructure. Key strategies include:
- Embrace Interoperability: Design studies with data sharing in mind, utilizing certified APIs and understanding the rules against information blocking to enrich data assets [96] [98].
- Streamline Oversight: Leverage provisions like the elimination of continuing review for low-risk studies and the sIRB mandate to reduce administrative delays [25] [49].
- Engage Patients as Partners: Utilize the new frameworks that empower patients to access and share their health data, thereby facilitating innovative research models like the All of Us program [96] [95].
By harmonizing the ethical guidance of the Belmont Report with the updated regulations of the Common Rule and the innovative drive of the Cures Act, the research community can build robust, efficient, and future-proofed research programs that accelerate the delivery of new treatments to patients.
Conclusion
The Belmont Report and the Common Rule form a symbiotic relationship where foundational ethics inform enforceable regulations. For researchers and drug developers, a deep understanding of both is non-negotiable. The Belmont Report's principles of Respect for Persons, Beneficence, and Justice provide the ethical compass, while the Common Rule, especially its 2019 revisions, provides the structured roadmap for compliance. The ongoing modernization of the Common Rule, with its focus on streamlined review and enhanced consent, demonstrates a dynamic system adapting to new research landscapes. The future will likely see further harmonization between FDA and Common Rule regulations, increased focus on data sharing and privacy, and continuous evolution of guidelines for complex research areas like genomics and artificial intelligence. Success in this environment requires professionals to be not just compliant, but ethically engaged, using these frameworks to build unwavering trust with research participants and the public.
References
- 1. How Did the Tuskegee Study Influence Modern Research ... [https://encoredocs.com/2024/05/24/how-did-the-tuskegee-study-influence-modern-research-ethics/]
- 2. Research Ethics Timeline [https://www.niehs.nih.gov/research/resources/bioethics/timeline]
- 3. History of Research Ethics - IRB [https://ori.umkc.edu/facilities-compliance-and-commercialization/compliance/irb/history-of-research-ethics.html]
- 4. National Research Act at 50: An Ethics Landmark in Need ... [https://www.thehastingscenter.org/national-research-act-at-50-it-launched-ethics-oversight-but-it-needs-an-update/]
- 5. National Research Act [https://en.wikipedia.org/wiki/National_Research_Act]
- 6. Ethical Guidelines and the Institutional Review Board [https://pmc.ncbi.nlm.nih.gov/articles/PMC10885741/]
- 7. 45 CFR Part 46 -- Protection of Human Subjects [https://www.ecfr.gov/current/title-45/subtitle-A/subchapter-A/part-46]
- 8. Still Timely After All These Years: How the Belmont Report ... [https://acrpnet.org/2025/08/06/still-timely-after-all-these-years-how-the-belmont-report-continues-to-shape-research-ethics]
- 9. NIST Researchers Suggest Historical Precedent for Ethical ... [https://www.nist.gov/news-events/news/2024/02/nist-researchers-suggest-historical-precedent-ethical-ai-research]
- 10. Stop Overregulating Research — The James G. ... [https://jamesgmartin.center/2025/01/stop-overregulating-research/]
- 11. The Belmont Report - Human Subjects Office [https://hso.research.uiowa.edu/about-human-subjects-office/regulations-and-policies/belmont-report]
- 12. Common Rule Research Alert: New Proposed "Federal ... [https://www.hinshawlaw.com/en/insights/healthcare-alert/common-rule-research-alert-new-proposed-federal-policy-for-the-protection-of-human-subjects]
- 13. Informed Consent and the Revised Common Rule [https://bioethics.hms.harvard.edu/journal/consent-common-rule]
- 14. Belmont Report - Human Research Protection Program [https://irb.wisc.edu/regulatory-information/belmont-report/]
- 15. Ethical Principles - Inside NKU - Northern Kentucky University [https://inside.nku.edu/rgc/research-compliance/irb/resources/ethical-principles.html]
- 16. The creation of the Belmont Report and its effect on ethical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9700634/]
- 17. Federal Regulations and the Ethical Collection of Specimens ... [https://dctd.cancer.gov/research/research-areas/biobanking-biospecimen-science/elsi/federal-regulations]
- 18. Belmont Report [https://en.wikipedia.org/wiki/Belmont_Report]
- 19. The History of the Belmont Report | 2020 | IRB Blog [https://www.tc.columbia.edu/institutional-review-board/irb-blog/2020/the-history-of-the-belmont-report/]
- 20. The "Common Rule" | National Institute of Justice [https://nij.ojp.gov/funding/common-rule]
- 21. The Importance of Proposed Changes in the “Common ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5439896/]
- 22. Key Points for New Common Rule [https://www.endicott.edu/about/research-at-endicott/institutional-review-board-irb/key-points-for-new-common-rule]
- 23. The Common Rule Changes and Update - Key Solutions Blog [https://www.keyusa.com/blog/common-rule]
- 24. IRB Background and Purpose [https://www.belmont.edu/irb/about/background.html]
- 25. Revised Common Rule - Institutional Review Board [https://www.belmont.edu/irb/common-rule.html]
- 26. Global comparison of research ethical review protocols [https://pmc.ncbi.nlm.nih.gov/articles/PMC11975204/]
- 27. The Nuremberg Code–A critique - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3121268/]
- 28. Declaration of Helsinki – WMA [https://www.wma.net/what-we-do/medical-ethics/declaration-of-helsinki/]
- 29. WMA Declaration of Helsinki – Ethical Principles for ... [https://www.wma.net/policies-post/wma-declaration-of-helsinki/]
- 30. Declaration of Helsinki: ethical norm in pursuit of common ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11019506/]
- 31. Common Rule and Other Changes - Research Support [https://researchsupport.psu.edu/orp/irb/irb-resources-training-and-events/common-rule-and-other-changes/]
- 32. The Revised Common Rule | Columbia | Research [https://research.columbia.edu/revised-common-rule]
- 33. The Regulatory Framework for Protecting Humans in Research [https://www.ncbi.nlm.nih.gov/books/NBK215883/]
- 34. Federal Policy for the Protection of Human Subjects ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK217985/]
- 35. Frequently Asked Questions: Research Involving Human ... [https://www.nsf.gov/funding/faq/research-involving-human-subjects]
- 36. Common Rule Basics | Office of Research Institutional Review ... [https://research.usu.edu/irb/basics/]
- 37. The Belmont Report - Ethical Principles [https://www.washington.edu/research/hsd/guidance/ethical-principles/belmont/]
- 38. 45 CFR 46.116 -- General requirements for informed consent. [https://www.ecfr.gov/current/title-45/subtitle-A/subchapter-A/part-46/subpart-A/section-46.116]
- 39. Risks and Benefits of Research - IRB - UC Davis [https://irb.ucdavis.edu/project-guidance/risks-and-benefits/]
- 40. Results of a National Survey of IRB Chairs - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609048/]
- 41. Challenges of Conducting Risk-Benefit Analysis of Early ... [https://pubmed.ncbi.nlm.nih.gov/41222508/]
- 42. Institutional Review Boards Frequently Asked Questions [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/institutional-review-boards-frequently-asked-questions]
- 43. An Approach to a Benefit-Risk Framework [https://acrpnet.org/2024/04/12/an-approach-to-a-benefit-risk-framework]
- 44. Guidance: Data and Safety Monitoring of Clinical Trials ... [https://research.lehigh.edu/policies-guidance-forms/guidance-data-and-safety-monitoring-clinical-trials-research]
- 45. November 2025 IRB Connection Newsletter [https://hso.research.uiowa.edu/1125]
- 46. Revised Common Rule | Slippery Rock University [https://www.sru.edu/offices/institutional-review-board/revised-common-rule]
- 47. The Common Rule - IRB - UC Davis [https://irb.ucdavis.edu/project-guidance/federal-funding/]
- 48. Revised Common Rule [https://www.hopkinsmedicine.org/institutional-review-board/revised-common-rule]
- 49. Revised Common Rule (Human Subject Regulations) [https://research.fiu.edu/irb/revised-common-rule/]
- 50. Revised Common Rule Changes to the Consent Process ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7122264/]
- 51. Revised Human Research Protection Rule Delayed until 2019 [https://hrpp.msu.edu/news/2018-06-18-delay.html]
- 52. Final Revisions to the Common Rule [https://research.hawaii.edu/orc/human-studies/final-revisions-to-the-common-rule/]
- 53. Common Rule - Human Research Protection Program [https://irb.wisc.edu/regulatory-information/common-rule-changes/]
- 54. Common Rule Changes Frequently Asked Questions [https://research.uoregon.edu/manage/integrity-compliance/human-subjects-research/common-rule-faq]
- 55. The Changing Landscape of Human Subjects Research [https://www.socra.org/blog/the-changing-landscape-of-human-subjects-research/]
- 56. Evolving Regulatory Protections for Research Participants [https://www.theregreview.org/2024/12/29/spotlight-evolving-regulatory-protections-for-research-participants/]
- 57. 45 CFR 46.104 -- Exempt research. [https://www.ecfr.gov/current/title-45/subtitle-A/subchapter-A/part-46/subpart-A/section-46.104]
- 58. Exempt Review: Institutional Review Board (IRB) Office [https://irb.northwestern.edu/submitting-to-the-irb/types-of-reviews/exempt-review.html]
- 59. Exempt Review Types | Research Integrity [https://ww2.georgiasouthern.edu/research/researchintegrity/institutional-review-board/new-common-rule-guidance/exempt-review-types/]
- 60. Exempt Category 2 and 3 Examples [https://research.osu.edu/research-responsibilities-and-compliance/human-subjects/exempt-research/exempt-research-0]
- 61. Office of Human Research Ethics SOP 0601: Exempt Studies [https://policies.unc.edu/TDClient/2833/Portal/KB/ArticleDet?ID=132222]
- 62. Exempt IRB Review - Office of Research Integrity Assurance [https://oria.gatech.edu/irb/submitting-protocol/exempt-irb-review]
- 63. Notice of IRB Exemption Changes [https://www.wcgclinical.com/insights/upcoming-irb-exemption-changes-coming-jan-2/]
- 64. Centralized sIRB Oversight: Enhancing Efficiency and Compliance in... [https://abrsolution.com/centralized-sirb-oversight-enhancing-efficiency-and-compliance-in-multisite-studies/]
- 65. Single IRB ( sIRB ) and Cooperative Multi - Site Research – Medical... [https://az.research.umich.edu/medschool/guidance/single-irb-sirb-and-cooperative-multi-site-research/]
- 66. Getting Started with Single IRB (sIRB) - Stanford IRB [https://irb.stanford.edu/for-researchers/singleirb]
- 67. FDA's Single IRB Requirement, Expected but Not ... [https://www.wcgclinical.com/insights/fdas-single-irb-requirement-expected-but-not-guaranteed-in-2025/]
- 68. of single IRB review for Implementation human subjects... multisite [https://pmc.ncbi.nlm.nih.gov/articles/PMC10225260/]
- 69. The Upcoming sIRB Mandate and the Critical Role of Site ... [https://www.wcgclinical.com/insights/the-upcoming-sirb-mandate-and-the-critical-role-of-site-selection-your-questions-answered/]
- 70. New Predictions for 2025 [https://globalforum.diaglobal.org/issue/january-2025/additional-predictions-for-2025/]
- 71. Key Information and Facilitating Understanding in ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/key-information-and-facilitating-understanding-informed-consent-guidance-sponsors-investigators-and]
- 72. IRB Consent Form Templates - Cornell Research Services [https://researchservices.cornell.edu/forms/irb-consent-form-templates]
- 73. Implementation of Common Rule Changes to the Informed ... [https://www.ochsnerjournal.org/content/20/1/76]
- 74. Understanding Broad Consent - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7122261/]
- 75. Broad Consent | Research and Innovation - University of Oregon [https://research.uoregon.edu/manage/integrity-compliance/human-subjects-research/guidance-library/broad-consent]
- 76. Informed Consent - Registries for Evaluating Patient Outcomes [https://www.ncbi.nlm.nih.gov/books/NBK562584/]
- 77. The Future of Research Compliance in 2025 and Beyond [https://www.keyusa.com/blog/future-of-research-compliance]
- 78. Back to the Basics: Reference Guides Every Research ... [https://www.srainternational.org/blogs/srai-news/2025/08/07/back-to-the-basics-reference-guides-every-research]
- 79. Federal 2025 | UK Research Changes [https://research.uky.edu/federal-changes-2025]
- 80. What is the Common Rule, and how does it affect my research? [https://rdc.iu.edu/faqs/policies-procedures/federal-common-rule-research-impact]
- 81. Ethical Principles | Human Research Protection Program ... [https://hrpp.research.virginia.edu/resources/ethical-principles]
- 82. Guiding Principles for Ethical Research [https://www.nih.gov/health-information/nih-clinical-research-trials-you/guiding-principles-ethical-research]
- 83. An Analysis of Institutional Review Board Policies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12227281/]
- 84. Why Revise When We Should Reconcile? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12005093/]
- 85. FDA Proposes Rules on Informed Consent and Institutional ... [https://www.cov.com/en/news-and-insights/insights/2022/10/fda-proposes-rules-on-informed-consent-and-institutional-review-boards]
- 86. 21 CFR Part 50 -- Protection of Human Subjects [https://www.ecfr.gov/current/title-21/chapter-I/subchapter-A/part-50]
- 87. FDA Proposes Revisions to Rules: 21 CFR 50 and 56 [https://about.citiprogram.org/blog/fda-proposes-revisions-to-rules-21-cfr-50-and-56/]
- 88. Investigational New Drug (IND) Application [https://www.fda.gov/drugs/types-applications/investigational-new-drug-ind-application]
- 89. E6(R3) Good Clinical Practice (GCP) September 2025 [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/e6r3-good-clinical-practice-gcp]
- 90. 2025 FDAAA 801 Final Rule Changes Impacting Clinical ... [https://prorelixresearch.com/2025-fdaaa-801-clinical-trial-rule-impact/]
- 91. Clinical trial regulations in 2025: navigating the constraints [https://clinicaltrialrisk.org/clinical-trial-design/clinical-trial-regulations-navigating-the-constraints/]
- 92. Transforming Informed Consent Generation Using Large ... [https://medinform.jmir.org/2025/1/e68139]
- 93. Revised Common Rule | Emory University | Atlanta GA [https://irb.emory.edu/guidance/getting-started/common-rule.html]
- 94. 21st Century Cures Act [https://www.fda.gov/regulatory-information/selected-amendments-fdc-act/21st-century-cures-act]
- 95. The 21st Century Cures Act [https://www.nih.gov/21st-century-cures-act]
- 96. The 21st Century Cures Act and electronic health records ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7646899/]
- 97. HHS steps up enforcement on health information blocking [https://www.dlapiper.com/en-bh/insights/publications/2025/09/hhs-steps-up-enforcement-on-health-information-blocking]
- 98. 21st Century Cures Act & What It Means for Your Practice [https://www.glenwoodsystems.com/post/understanding-21st-century-cures-act]